Tibial Pilon Fractures: Open Reduction Internal Fixation
surface (pilon fractures) represent approximately 1% of all fractures,
and approximately 3% to 9% of all tibia fractures (1).
Generally, two types of tibial pilon fractures have been recognized.
Rotational type fractures usually arise from a relatively low-energy,
rotational force, similar to that which may occur during recreational
skiing. These fractures typically are spiral in nature and are
generally associated with little articular comminution and limited
surrounding soft-tissue injury. The more problematic type of pilon
fracture is the high-energy, axial compression-type fracture. These
fractures typically occur in high-energy motor-vehicle crashes, falls
from a considerable height, and crush injuries like those incurred in
industrial accidents. This fracture is commonly associated with
articular and metaphyseal comminution and significant soft-tissue
injury 2. In either case, the fibula may or
may not be fractured. It is important that the treating physician
recognize the difference between these two fractures types, for
although the indications for operative treatment are the same, the
timing for definitive treatment, the patient’s prognosis, and the
outcome, will differ.
the following: (a) articular fracture displacement of ≥2 mm, (b)
unstable fractures of the tibial metaphysis, and (c) open pilon
fractures. Contraindications to formal open reduction and internal
fixation (ORIF) include severe soft-tissue injury where blistering and
skin necrosis or persistent swelling precludes safe surgical
intervention, and severe articular comminution, which would make
satisfactory articular reduction and stabilization extremely difficult
or impossible. Relative contraindications to formal ORIF include
infirmity of the patient; advanced patient age and osteopenia; prior
local surgery or previous soft-tissue transfers; advanced, peripheral,
vascular disease (associated with a history of smoking, and/or
diabetes); and other co-morbidities that would make surgical
intervention too risky. Also, patients who would be unable or unwilling
to cooperate in postoperative weight bearing restrictions (i.e., those
with generalized weakness, dementia, or neurologic deficit) are also
felt to have relative contraindications for surgery.
outcome following treatment of a pilon fracture. Thorough preoperative
planning is dependent upon the surgeon developing a complete
understanding of the fracture pattern, surgical approaches, blood
supply to the fracture fragments, and awareness of the availability,
applicability, and limitations of the various surgical implants. A
thorough history and physical examination of the patient and the limb
is essential. Particular attention is paid to the condition of the soft
tissues in the lower leg and ankle. A detailed neurovascular exam and
evaluation of the compartments of the leg must be documented. Fracture
blisters are common and may influence the timing and method of
treatment.
pattern, a detailed study of the radiographic images is necessary.
Routine radiographic assessment of pilon fractures includes
anteroposterior (AP), mortise, and lateral views of the ankle (Fig. 31.1).
In case of fracture displacement or shortening, traction radiographs
may be extremely helpful. These are often obtained following
application of a spanning external fixator. Axial computed tomography
(CT) scans are necessary for understanding the fracture pattern in
general and the articular injury in particular. The CT scan of the
distal tibia and ankle is most helpful when performed after a
preliminary reduction and application of the spanning external fixator.
Axial, sagittal, and coronal reconstructions of the CT scans are
recommended (Fig. 31.2). Plain radiographs of
the contralateral ankle can be helpful for preoperative planning as
they serve as a template for the fractured side.
step-by-step description of how the surgery is to be carried out and a
diagram of the fractured distal tibia and of the desired final fixation
construct. In general, the plan begins with patient positioning,
site(s) to be prepared for surgery, a description of the approach(es)
to be used, the steps necessary to restore articular congruity, and the
restoration of length, alignment, and rotation of the limb. It also
includes the creation of a stable fixation construct that will allow
early mobilization of the patient and the ankle.
A first-generation cephalosporin is administered and continued for 24
to 48 hours postoperatively. The use of a tourniquet is
left
to the discretion of the surgeon. Formal ORIF of displaced pilon
fractures should be carried out in two stages to minimize the risk of
surgical complications. For each of these two stages, the patient is
positioned supine with a padded bump beneath the ipsilateral greater
trochanter and hip to help maintain the operative leg in neutral
rotation. The first stage, which includes application of a spanning
external fixator and internal fixation of the fibula, should be
performed within 24 to 36 hours of the fracture, when possible. The
fibula is approached through a slightly more posterolateral incision
than usual and the fracture is reduced and plated with either a
one-third tubular plate (metaphyseal fracture) or a 3.5 limited-contact
dynamic-compression (LCDC) plate (diaphyseal fracture). When
appropriate for the fracture pattern, the construct should be
supplemented with a lag screw placed across the fracture. Occasionally
the fibula can be stabilized with a single, partially threaded,
cancellous screw placed from distal to proximal within the medullary
canal of the fibula as an intramedullary splint. This method is
particularly effective when the fracture is transverse and helpful when
it is associated with lateral soft-tissue compromise.
 |
|
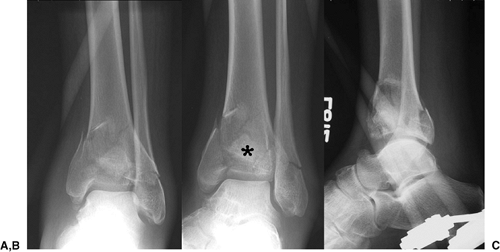
Figure 31.1. A. AP, (B) lateral, and (C)
mortice plain radiographs of a high-energy tibial-plafond fracture. The fibular fracture is relatively transverse, and the articular surface of the tibia is comminuted with a portion of the cartilage impacted into the distal tibia. |
 |
|
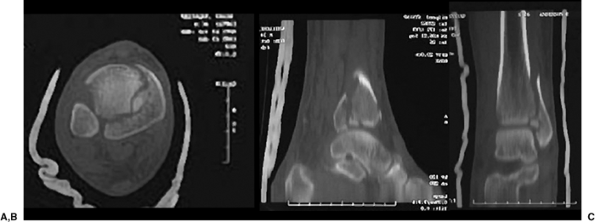
Figure 31.2. A. Axial, (B) sagittal, and (C)
coronal reconstructions of a CT scan demonstrate clearly the fracture pattern and the presence of an impacted articular fragment. |
reapproximate the tibial fracture fragments through ligamentotaxis,
provide pain relief, prevent further soft-tissue injury, and allow
mobilization of the patient (Fig. 31.3). When
the fixator is applied, barring any other serious injuries, the patient
can be mobilized with crutches and subsequently discharged to home.
This treatment strategy is reflected in the term “traveling traction,”
which has been used to refer to the use of this simple spanning
external fixator.
two 16-mm carbon-fiber rods, two 4.5-mm or 5.0-mm half pins, and a
5.0-mm transfixation pin, a multiple pin clamp, and several pin-to-bar
clamps (Fig. 31.4). Occasionally, this frame is
supplemented with a 4.0-mm half pin placed into the first metatarsal
and an additional pin-to-bar and bar-to-bar clamp and short
carbon-fiber rod. Using the multipin clamp as a guide, the two half
pins are placed in the midsagittal plane of the tibial diaphysis. The
Schanz screws should be placed proximal to the zone of injury to avoid
the fracture hematoma and the path of subsequent incisions. These
Schanz screws should gain purchase in both the anterior and posterior
cortices and therefore should be started one-half fingerbreadth medial
to the tibial crest. The calcaneal transfixation pin should be placed
from medial to lateral through the posterior-plantar aspect of the
calcaneal tuberosity. Manual traction is applied on the transfixation
pin to restore limb length and reapproximate the fracture fragments
while maintaining the talus beneath the tibial plafond. When the limb
is brought to length, the carbon fiber rods are attached to the
multipin clamp proximally (1 bar medially and 1 bar laterally) and the
transfixation pin is added distally. If the talus is unstable beneath
the plafond, ORIF of the fibula or modification of the frame will be
necessary.
modification of the frame includes the placement of a 4.0-mm half pin
into the base of the first metatarsal and the attachment of this pin to
the medial carbon-fiber rod with a third rod and a bar-to-bar clamp.
This pin will improve stability of the talus as well as help avoid the
development of an equinus contracture of the ankle, but it is not
routinely necessary. It is important when applying this spanning
external fixator that the hind foot and mid foot be positioned in
neutral or slight valgus alignment.
 |
|
Figure 31.3. A. AP, (B) mortice, and (C)
lateral plain radiographs after application of a spanning external fixator. The limb has been realigned, fracture fragments reapproximated, and the limb brought out to length. Note that the impacted fragment (*) with no soft tissue attachments remains impacted in the metaphysis. |
soft tissues have recovered, generally 14 to 21 days after injury, it
is possible to embark on the second stage, internal fixation of the
distal tibia.
proximal thigh, and the leg is prepped and draped in the usual sterile
fashion. Although using a tourniquet during the surgery will provide a
bloodless field, its use may lead to increased postoperative swelling
and should be limited to 2 to 21½ hours at 250 to 300 mmHg. Several
approaches to the distal tibia have been described: The anteromedial
approach is most consistently used, with the anterolateral
approach used for selected fracture patterns. A direct medial incision to the distal tibia should be avoided at all costs because of the high rate of soft-tissue complications.
 |
|
Figure 31.4. Clinical photograph of a patient with bilateral pilon fractures treated initially with spanning external fixators.
|
just above, the proximal extent of the fracture, one-half fingerbreadth
lateral to the tibial crest. It is extended distally, curving gently
toward the talonavicular joint, paralleling the path of the anterior
tibialis tendon. Leaving the periosteum attached to the underlying bone
and bone fragments, the anterior tibialis, extensor hallucis longus,
and the extensor digitorum tendons, along with the dorsalis pedis
artery and venae, and the superficial peroneal nerve are retracted
laterally, and an arthrotomy performed. With gentle retraction of the
skin and tendons, the articular fragments of the distal tibia are
reconstructed. In general, the largest and least displaced fracture
fragments are reduced first and then the smaller, more displaced
fragments are addressed.
oblique views will aid in assessing the reduction of the articular
fragments. Assessment of the reduction can also be performed under
direct visualization by looking into the joint from below. It is
important to keep in mind that if the very distal aspect of the fibula
has been plated, then the plate will obscure the articular surface when
the fluoroscope is in the true lateral position. If recognized in
advance, temporary stabilization of the fibula can be performed with
pointed reduction forceps, and then definitive fixation performed after
the tibial plafond has been reduced and stabilized. If the fibula has
been previously reduced and plated, oblique images of the distal tibia
can be used to assess the adequacy of the reduction. Temporary
stabilization of the reduced articular fragments is obtained with
Kirschner (K) wires (either 1.6 mm or 2.0 mm) and pointed reduction
forceps, and these are subsequently replaced with interfragmentary
small-fragment lag screws. When these fragments are stabilized, the
articular block is then reduced to the tibial shaft and again held with
pointed reduction forceps and/or K wires while length, alignment, and
rotation are restored.
carried out with small fragment implants. Generally, plates are placed
along the medial aspect of the tibia to secure the articular block to
the shaft and buttress the distal tibia, which will help avoid varus
mal-alignment. Often a small fragment plate is needed anteriorly to
buttress the anterior articular and metaphyseal fragments. Again,
small-fragment low-profile plates are best for this area (Fig. 31.5).
If respect for the soft-tissue attachments is maintained during the
surgery, large metaphyseal fragments will heal relatively quickly, and
large fragment plates are not needed for strength. Because of their
size, the large fragment plates can become quite bothersome to the
overlying soft tissues.
stabilization of the articular fragments is not possible or large
articular fragment may only be minimally displaced from the diaphysis.
In these situations, it is often better to anatomically reduce these
fragment(s) to the intact diaphysis initially and then build the
remaining articular fragments back to them. If this method is employed,
it is essential that the large fragments are anatomically reduced to
the shaft because any malreduction at the metaphyseal level will lead
to an even greater malreduction at the articular level.
address displaced articular fragments, including a limited
anterolateral incision to address and fix displaced, anterolateral,
Chaput tubercle fragments.
process as well as to fill metaphyseal voids, the use of bone grafts
has been advocated in the past. A variety of bone graft materials are
currently available. Cost, morbidity, and proven efficacy should be
taken into consideration before deciding on whether to harvest an
iliac-crest bone graft or use a bone graft substitute. In general, only
large metaphyseal defects resulting from impaction of the cancellous
bone are routinely bone grafted. Bone grafts should not be placed in
acute, open, distal, tibia fractures. In the setting of an open
fracture, use of a bone graft to improve the chances of distal tibia
healing following bone loss should be performed only after the soft
tissues have completely healed or soft tissue coverage has matured.
Typically, this is done approximately 3 to 6 weeks after soft tissue
closure.
meticulously to avoid further soft-tissue injury. After closure of the
deep tissues, the skin is closed with nylon sutures
through
the use of Allgöwer’s modification of the Donati stitch. In the
operating room, final plain radiographs are made to assure articular
reduction. Also, a well-padded short-leg splint, with the ankle in
neutral position, is applied.
 |
|
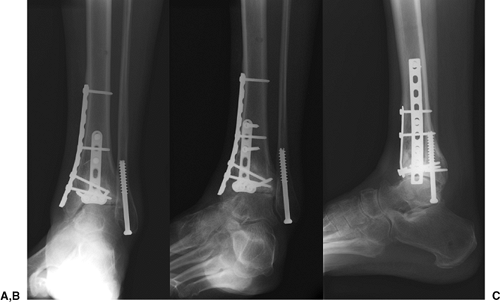
Figure 31.5. A. AP, (B) mortice, and (C) lateral plain radiographs 15 months after ORIF of a high-energy tibial-plafond fracture.
|
hours after surgery. They are released in their postoperative splint
and maintaining toe-touch weight bearing. At approximately 8 to 12
postoperative days, the patient is brought back to the clinic where the
splint is removed and the incisions are inspected. If the incisions are
each clean and dry and without evidence of skin necrosis, the sutures
are removed and Steri-Strips applied. It is not uncommon to find small
areas of superficial skin necrosis at the central portion of the tibial
incision. In these cases, the sutures are generally left in place and a
sterile dressing (Xeroform) is reapplied, and the ankle is immobilized
again in a short-leg splint.
and when the sutures are removed, the patient is placed in a removable
boot and active-assisted range of motion of the ankle, subtalar joint,
and foot/toes is initiated. Patients are encouraged to perform these
exercises three to four times each day for 20 minutes each session.
Radiographs are routinely taken at 2, 6, and 12 weeks after surgery. If
at the 6-week postoperation exam there is no change in the fracture
fragments, alignment, and fixation construct, the patients are advanced
to partial weight bearing and begin a formal physical
therapist–directed program. This program should include aggressive
active-assisted range of motion of the ankle as well as active-assisted
and passive range of motion of the subtler join and foot. Muscle
strengthening and pro-preconception training can also be initiated at
this time if motion has improved. At 12 postoperative weeks, as long as
there is evidence of further healing and no evidence of fracture
instability, the patients are advanced to full weight bearing and
weaned from the boot and crutches. In ideal situations, physical
therapy is continued until near normal muscle strength and ankle,
subtalar, and foot range of motion is recovered. Often laborers require
a period of work hardening to regain labor-specific function and
strength.
complications associated with the treatment of pilon fractures, a
two-staged approach has been proposed. Although this treatment protocol
appears to have its roots in the late 1980s, it was not until the late
1990s that the benefits of this protocol were published (3,4).
randomized prospective study of two methods of fixation of tibial
plafond fractures. Two groups of patients were studied including those
who underwent ORIF of the tibia and fibula (n = 18) and a second group of patients (n
= 20) who were managed with external fixation with or without limited
internal fixation. Attesting to the high energy nature of these
fractures, 26 were open fractures and 44% were Rüedi and Allgöwer type
III fractures (6,7).
They reported 15 operative complications in 7 patients who had been
managed with ORIF and four complications in 4 patients who had been
managed with external fixation. At an average follow-up of 39 months
(range, 25 to 51 months) they concluded that external fixation of
tibial plafond fractures was associated with fewer complications than
was internal fixation. However, the patients who underwent ORIF were
typically operated on within 48 hours of the injury, “unless severe
swelling or fracture blisters were present” (average time of 5 days
[range of 3 hours to 17 days]). It is quite possible that the many
complications and adverse outcomes following formal ORIF was related to
the fact that these fractures were treated before the soft tissues had
fully recovered. Internal fixation of high-energy tibial-plafond
fractures should only be performed after the soft tissues have
recovered, generally in 14 to 21 days.
their experience using this two-staged protocol in the treatment of 46
Orthopedic Trauma Association (OTA) type C fractures. Twenty-nine of
these fractures were closed and 17 fractures were open. This entire
group was made up of patients with particularly high-energy, distal,
tibial fractures. In all cases, a temporary, spanning, external fixator
was applied within 24 hours of the injury, and the fibula was plated.
Open fractures were treated with serial debridement and soft-tissue
closure or flap coverage, generally within 5 to 7 days of injury.
Definitive fixation of the closed tibia fractures was performed on an
average of 12.7 days (range of 4 to 30 days), whereas the average time
to definitive fixation in the open pilon group was 14 days (range of 4
to 31 days). At a minimum follow-up of 12 months, one patient in the
closed-fracture group had a deep infection (5%). In the open fracture
group, three patients had a deep infection that resulted in a below
knee amputation (BKA) in one patient and resolution of the infection in
the others. In general, the authors felt that the patients in these
groups who had been treated with this two-step protocol had an overall
good result and an acceptably low complication rate 4.
their experience with the treatment of 22 patients also with OTA type C
fractures. Each patient was treated with a spanning external fixator
and internal fixation of the fibula shortly after injury. Definitive
fixation of the tibia was performed at an average of 24 days (range, 15
to 49 days) postinjury. At the 24-month follow-up, they reported no
infections or soft-tissue complications, and their clinical results
were similar to other studies reporting on ORIF of pilon fractures.
They too concluded that patients with high-energy, distal tibial
fractures are best treated with a two-staged protocol.
impairment after pilon fractures and to determine which patient,
injury, or treatment characteristic influence outcome most, Pollak et
al 8 reported on 80 patients at 3.2 years
after injury. Patients were recruited from two separate trauma centers,
one that generally treats these injuries with formal internal fixation,
and the other where most patients are treated with external fixation.
They found that patients treated with external fixation, with or
without limited-internal fixation, had greater loss of ankle motion and
reported more pain and ambulatory dysfunction than did patients treated
with internal fixation (p < 0.05).
Although the general physical health of patients the two treatment
groups was not significantly different, the average Sickness Impact
Profile ambulation subscale score was 19.8 points higher (poorer) for
patients treated with external fixation with or without
limited-internal fixation. Based on these data, the authors concluded
that patients who sustain a pilon fracture continue to experience major
physical
and psychosocial health problems long after the initial injury and that
well-controlled prospective studies are needed to identify the best way
to treat these injuries.
feared complications following fixation of high-energy tibial plafond
fractures (9,10,11,12,13,14).
When deep infections occur they commonly follow soft tissue
complications, but occasionally the deep infections develop without
postoperative wound complications. Aggressive treatment of soft-tissue
complications and infections should be initiated when recognized. For
full-thickness skin loss or deep infection, management includes
aggressive surgical debridement of the dead and/or infected skin,
subcutaneous tissue, and free bone fragments as well as the
administration of culture-specific intravenous antibiotics. In
addition, consideration is given for placement of a vascularized muscle
flap for the residual soft-tissue defect. If the fracture remains well
fixed and the implants are stable, efforts should be made to leave the
implants in place until the fracture has healed; this strategy is an
attempt to prevent the development of an infected nonunion. If the
fracture or implants are unstable, serious consideration must be given
to removal or exchange of the implants and application of a spanning or
nonspanning external fixator.
commonly involve the metaphyseal portion of the tibia. Signs and
symptoms of a nonunion include persistent pain and swelling about the
ankle, progression of deformity, and at times, gross motion at the
fracture site and failed screws and/or plates. Intraoperatively, soft
tissue–friendly techniques, which include preservation of the
soft-tissue attachments to the fracture fragments, and infection
avoidance, are probably the best ways to minimize the development of a
nonunion. When nonunion is diagnosed, measures (including the use of
laboratory tests and occasionally open biopsy) should be taken to make
sure an occult infection is not present. Treatment for nonunions is
typically operative and includes the correction of limb alignment,
revision internal fixation, and bone grafting.
nonunion and usually involve varus mal-alignment of the distal tibia.
Premature removal of the implants, particularly the medial buttress
plate, has been associated with the development of a malunion, and
therefore, the implants should not be removed until the fracture has
completely healed. Fractures are considered completely healed when the
fracture lines are absent, bridging bone across the fractures line is
present on the plain radiographs, and weight bearing activities are
tolerated. Treatment for the malunion includes the correction of
alignment and revision internal fixation of the tibia and fibula.
Typically this requires an osteotomy at the site of the malunion,
correction of alignment, and the insertion of a tricortical bone-graft
wedge prior to fixation. This technique has been very effective for
correcting the alignment of the limb while maintaining limb length.
pilon fractures and is felt to be related to primary cartilage injury,
residual articular incongruity, and joint instability. Although little
can be done at this time to reverse the primary cartilage injury, many
feel that at least cartilage nutrition, which is dependent on joint
motion, can be maximized by fracture stabilization and early joint
motion. Articular incongruity should be minimized by paying particular
attention to the reduction of the articular fragments during surgery.
The hallmarks of treatment remain accurate articular reduction, stable
internal fixation, early range of motion exercises, and delayed weight
bearing. Only after sufficient time has elapsed to allow healing of the
articular fragments can protected weight bearing be initiated.
fixation and healing, but there is experimental evidence that
alteration in joint stability may occur after fracture, particularly if
articular incongruity is present. Therefore, all efforts should be made
to restore the tibial plafond and stability of the joint.
nonsteroidal anti-inflammatory agents, ankle bracing, and shoe and
activity modification. Intermediate and end-stage posttraumatic
osteoarthritis can be treated with a solid ankle-foot orthosis and
cane. If these
measures
provide comfort for patients with advanced posttraumatic
osteoarthritis, then only in the elderly or very low-demand individuals
should total ankle arthroplasty be considered. In physiologically young
patients with symptomatic disabling arthritis, an ankle fusion remains
the gold standard.
treat and their treatment is associated with considerable risks. To
minimize the risks of complications, a two-staged protocol has been
developed. In the initial stage, shortly after injury, a spanning
external fixator should be applied and the fibular fracture plated.
When the surrounding soft tissues have recovered (marked by wrinkling
of the skin about the foot and ankle) and the fracture blisters have
resolved, internal fixation of the distal tibia can be performed and
the spanning external fixator removed.
treat wound complications aggressively. The typical postoperative
protocol includes 6 weeks of touch-toe weight bearing and 6 weeks of
partial weight bearing before full weight bearing is allowed and formal
physical therapy initiated. As a result of the severe nature of these
injuries, some loss of ankle and hind foot motion occurs, and some
patients have pain, which requires shoe and lifestyle modifications.
JF, Waddell JP. Fractures of the distal tibial metaphysis with
intra-articular extension: the distal tibial explosion fracture. J Trauma 1979;19:593–601.
M, Sanders R, DiPasquale T, et al. A staged protocol for soft tissue
management in the treatment of complex pilon fractures. J Orthop Trauma 1999;13:78–84.
B, McFerran MA, McAndrew M, et al. Operative treatment of fractures of
the tibial plafond: a randomized, prospective study. J Bone Joint Surg Am 1996;78:1646–1657.
T. Fractures of the lower end of the tibia into the ankle joint:
results 9 years after open reduction and internal fixation. Injury 1973;5:130–134.
L, Slabaugh P. Delayed wound healing, infection, and nonunion following
open reduction and internal fixation of tibial plafond fractures. J Trauma 1986;26:1116–1119.
SM, Wiss DA. Open reduction and internal fixation of tibial plafond
fractures: variables contributing to poor results and complications. Clin Orthop 1993:108–117.
