Arthroscopy
Editors: Berry, Daniel J.; Steinmann, Scott P.
Title: Adult Reconstruction, 1st Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Section II – Knee > Part C – Operative Treatment Methods > 22 – Arthroscopy
22
Arthroscopy
Justin Strickland
Diane L. Dahm
Knee arthroscopy is the most common operative
orthopaedic procedure performed in the United States. It is usually
performed as an outpatient procedure and is associated with low
morbidity and quick recovery. In addition, multiple types of pathology
can be addressed at a single operation. Though the natural history of
osteoarthritis is unchanged by arthroscopy, symptomatic relief can be
achieved with this modality depending on the pathology found at the
time of surgery. Recently, the efficacy of arthroscopy in the treatment
of osteoarthritis has been questioned. Patient education and surgical
indications are important in the discussion regarding the expectations
following arthroscopy in the setting of osteoarthritis.
orthopaedic procedure performed in the United States. It is usually
performed as an outpatient procedure and is associated with low
morbidity and quick recovery. In addition, multiple types of pathology
can be addressed at a single operation. Though the natural history of
osteoarthritis is unchanged by arthroscopy, symptomatic relief can be
achieved with this modality depending on the pathology found at the
time of surgery. Recently, the efficacy of arthroscopy in the treatment
of osteoarthritis has been questioned. Patient education and surgical
indications are important in the discussion regarding the expectations
following arthroscopy in the setting of osteoarthritis.
Preoperative Evaluation
Indications
The preoperative evaluation of patients with
osteoarthritis is paramount in determining the outcome and expectations
following arthroscopy. The following factors suggest higher likelihood
of favorable response to arthroscopy:
osteoarthritis is paramount in determining the outcome and expectations
following arthroscopy. The following factors suggest higher likelihood
of favorable response to arthroscopy:
-
Acute onset of pain
-
Mechanical symptoms
-
Normal or near normal alignment
-
Mild to moderate radiographic degenerative changes
-
Failure of appropriate nonoperative management program
-
Reasonable patient expectations
Clinical Evaluation
When obtaining a history of knee pain from a patient, it
is important to note the onset of symptoms and any recent change in
symptoms. These patients frequently have a history of chronic knee
pain; however, an acute exacerbation or change in the nature of the
symptoms may indicate new pathology that may be amenable to
arthroscopic treatment. If mechanical symptoms such as catching and
locking are present, this may represent meniscal pathology, loose body
formation, or an unstable articular cartilage fragment. Localization of
pain is also an important factor. Isolated medial or lateral tenderness
may indicate a focal articular lesion or symptomatic meniscal
pathology. On physical exam, one should note any excessive varus or
valgus malalignment or flexion/extension lags. A patient with
malalignment in the coronal plane may be a candidate for osteotomy.
Finally, patients should be given a trial of nonoperative measures
before any operative procedure is undertaken. This might include
shoe/heel wedges, use of braces, nonsteroidal anti-inflammatory drugs
(NSAIDs) or other medications, injections (steroid and
viscosupplementation) and physical therapy. Low-impact exercise and
weight loss are also often effective for symptomatic relief in patients
with osteoarthritis of the knee.
is important to note the onset of symptoms and any recent change in
symptoms. These patients frequently have a history of chronic knee
pain; however, an acute exacerbation or change in the nature of the
symptoms may indicate new pathology that may be amenable to
arthroscopic treatment. If mechanical symptoms such as catching and
locking are present, this may represent meniscal pathology, loose body
formation, or an unstable articular cartilage fragment. Localization of
pain is also an important factor. Isolated medial or lateral tenderness
may indicate a focal articular lesion or symptomatic meniscal
pathology. On physical exam, one should note any excessive varus or
valgus malalignment or flexion/extension lags. A patient with
malalignment in the coronal plane may be a candidate for osteotomy.
Finally, patients should be given a trial of nonoperative measures
before any operative procedure is undertaken. This might include
shoe/heel wedges, use of braces, nonsteroidal anti-inflammatory drugs
(NSAIDs) or other medications, injections (steroid and
viscosupplementation) and physical therapy. Low-impact exercise and
weight loss are also often effective for symptomatic relief in patients
with osteoarthritis of the knee.
Radiographic Evaluation
Standing anteroposterior (AP), lateral, posteroanterior
(PA) flexion, and sunrise views of the knee should be obtained. One may
consider standing full-length hip to ankle films to evaluate alignment.
Severe degenerative disease on plain films is a contraindication for arthroscopic treatment of osteoarthritis.
Magnetic resonance imaging can be helpful to evaluate for focal
cartilage defects. New techniques are now available that may
differentiate articular cartilage from synovial fluid and subchondral
bone, which makes it easier to identify these sometimes discrete
lesions. One should interpret MRI findings in patients older than 65
years of age with osteoarthritis cautiously because a very high
percentage of these patients will have a degenerative meniscus tear. As
always, the radiographic findings should be correlated with the history
and physical examination.
(PA) flexion, and sunrise views of the knee should be obtained. One may
consider standing full-length hip to ankle films to evaluate alignment.
Severe degenerative disease on plain films is a contraindication for arthroscopic treatment of osteoarthritis.
Magnetic resonance imaging can be helpful to evaluate for focal
cartilage defects. New techniques are now available that may
differentiate articular cartilage from synovial fluid and subchondral
bone, which makes it easier to identify these sometimes discrete
lesions. One should interpret MRI findings in patients older than 65
years of age with osteoarthritis cautiously because a very high
percentage of these patients will have a degenerative meniscus tear. As
always, the radiographic findings should be correlated with the history
and physical examination.
 |
|
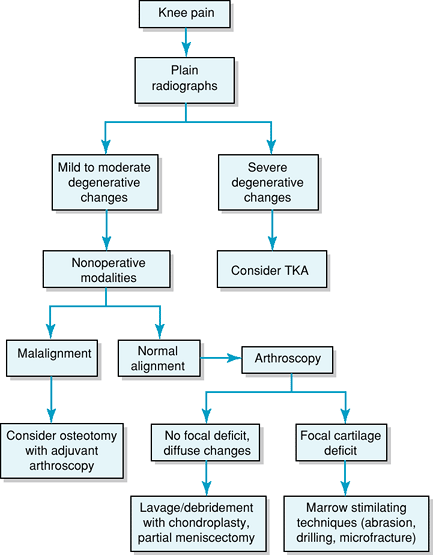
Figure 22-1 Algorithm for treatment of knee osteoarthritis. TKA, total knee arthroplasty.
|
 |
|
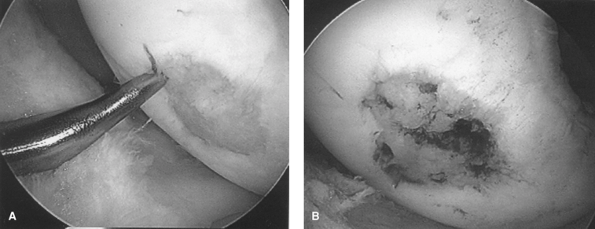
Figure 22-2 A: Arthroscopic technique of microfracture for a focal articular cartilage defect. B: Confirmation of bleeding subchondral bone in lesion bed.
|
Diagnostic Workup Algorithm
An algorithm for evaluation of knee pain for arthroscopic intervention is presented in Figure 22-1.
Treatment
Options
The following options are available when performing arthroscopy in the setting of osteoarthritis:
-
Lavage and debridement
-
Marrow stimulating techniques
-
Abrasion arthroplasty
-
Microfracture/drilling
-
Thermal chondroplasty
P.156
Multiple goals may be met when a patient with
osteoarthritis undergoes an arthroscopic debridement. The degenerative
knee has many potential mechanical irritants that may exacerbate a
patient’s symptoms. These include meniscal tears, unstable flaps of
cartilage, and loose bodies. All pathology should be addressed at the
time of surgery. It is recommended that chondroplasty and synovectomy
be limited to areas that are symptomatic or have the potential to
become problematic. Lavage of the joint may be beneficial as this will
dilute the degradative enzymes present in the arthritic knee.
Osteophytes may also be removed if found to be causing obvious
impingement. The advantages of this approach include low morbidity,
quick recovery, and the ability to perform a direct assessment of the
articular cartilage. It is important to document the findings at the
time of arthroscopy as this may influence future reconstructive options
such as unicompartmental versus total knee arthroplasty. Even though
arthroscopy is a relatively low morbidity, outpatient procedure, the
surgeon and patient must remember that no surgical procedure is without
risk. Complications such as infection, hematoma, and postoperative
stiffness can rarely occur, and patients should be counseled about this
possibility before the procedure.
osteoarthritis undergoes an arthroscopic debridement. The degenerative
knee has many potential mechanical irritants that may exacerbate a
patient’s symptoms. These include meniscal tears, unstable flaps of
cartilage, and loose bodies. All pathology should be addressed at the
time of surgery. It is recommended that chondroplasty and synovectomy
be limited to areas that are symptomatic or have the potential to
become problematic. Lavage of the joint may be beneficial as this will
dilute the degradative enzymes present in the arthritic knee.
Osteophytes may also be removed if found to be causing obvious
impingement. The advantages of this approach include low morbidity,
quick recovery, and the ability to perform a direct assessment of the
articular cartilage. It is important to document the findings at the
time of arthroscopy as this may influence future reconstructive options
such as unicompartmental versus total knee arthroplasty. Even though
arthroscopy is a relatively low morbidity, outpatient procedure, the
surgeon and patient must remember that no surgical procedure is without
risk. Complications such as infection, hematoma, and postoperative
stiffness can rarely occur, and patients should be counseled about this
possibility before the procedure.
Marrow stimulating techniques such as abrasion
arthroplasty, microfracture, and drilling are options typically used
for focal cartilage defects. These are more frequently used in younger,
active patients with otherwise absent or mild degenerative changes on
x-ray views. The goal of these procedures is to penetrate the
subchondral bone overlying the defect to stimulate bleeding and the
release of marrow contents. This will allow pluripotential mesenchymal
cells to invade the defect and begin the process of fibrous metaplasia.
Varying amounts of fibrocartilage will eventually fill the defect.
Small amounts of hyaline cartilage may be present. Abrasion
arthroplasty uses an arthroscopic burr to perform the technique. Simple
drilling can also be performed; however, because of its ease of use and
lack of heat generation, the so-called microfracture technique has
become more widely used. Microfracture is a relatively simple technique
using a specialized awl to penetrate the subchondral bone (Fig. 22-2).
A depth of 2 to 4 mm is recommended. A bridge of at least 4 mm should
be maintained between holes to sustain the integrity of the subchondral
bone. Thermal necrosis is not an issue with microfracture as it may be
with
arthroplasty, microfracture, and drilling are options typically used
for focal cartilage defects. These are more frequently used in younger,
active patients with otherwise absent or mild degenerative changes on
x-ray views. The goal of these procedures is to penetrate the
subchondral bone overlying the defect to stimulate bleeding and the
release of marrow contents. This will allow pluripotential mesenchymal
cells to invade the defect and begin the process of fibrous metaplasia.
Varying amounts of fibrocartilage will eventually fill the defect.
Small amounts of hyaline cartilage may be present. Abrasion
arthroplasty uses an arthroscopic burr to perform the technique. Simple
drilling can also be performed; however, because of its ease of use and
lack of heat generation, the so-called microfracture technique has
become more widely used. Microfracture is a relatively simple technique
using a specialized awl to penetrate the subchondral bone (Fig. 22-2).
A depth of 2 to 4 mm is recommended. A bridge of at least 4 mm should
be maintained between holes to sustain the integrity of the subchondral
bone. Thermal necrosis is not an issue with microfracture as it may be
with
P.157
abrasion arthroplasty, standard drilling, or thermal chondroplasty.
Thermal chondroplasty is a technique that uses a
radiofrequency probe to generate heat to denature collagen. This is
effective in smoothing and stabilizing articular cartilage defects.
However, it has not been proven that this method prevents the
propagation of these lesions or that there is a benefit over mechanical
chondroplasty. In addition, significant chondrocyte death has been
reported with both bipolar and monopolar systems in in vitro studies.
This is concerning as it can be difficult to control the temperature of
the probe at the cartilage surface. Irreversible damage to articular
cartilage occurs at >55°C. Because of these uncertainties, we
recommend using this modality with extreme caution and suggest that
further studies are needed to justify its routine use to treat
cartilage defects.
radiofrequency probe to generate heat to denature collagen. This is
effective in smoothing and stabilizing articular cartilage defects.
However, it has not been proven that this method prevents the
propagation of these lesions or that there is a benefit over mechanical
chondroplasty. In addition, significant chondrocyte death has been
reported with both bipolar and monopolar systems in in vitro studies.
This is concerning as it can be difficult to control the temperature of
the probe at the cartilage surface. Irreversible damage to articular
cartilage occurs at >55°C. Because of these uncertainties, we
recommend using this modality with extreme caution and suggest that
further studies are needed to justify its routine use to treat
cartilage defects.
Results
The clinical results obtained following arthroscopy for
osteoarthritis are difficult to interpret. Most published reports are
retrospective with variable inclusion criteria, definition of
procedures, and outcome measures. These studies have found that
arthroscopic debridement yields satisfactory results in 60% to 70% of
patients at 2- to 4-year follow-up. There appears to be no clear
advantage to subchondral drilling or abrasion arthroplasty in these
patients. One prospective study comparing arthroscopic debridement
versus placebo surgery found no difference in clinical outcome at
2-year follow-up. In this study, however, patients were not stratified
with respect to presence or absence of meniscal pathology, mechanical
symptoms/signs, or malalignment. In another prospective outcome study,
44% of patients were found to have improvement in pain at 2-year
follow-up. Variables associated with improvement included medial joint
line tenderness, a positive Steinman test, and the presence of an
unstable meniscus tear at arthroscopy. Older patients (>70 years of
age) were more likely to be treated with early total knee arthroplasty
following arthroscopic debridement compared with patients younger than
60 years of age. This is consistent with the fact that arthroscopic
debridement does not change the natural history of osteoarthritis.
osteoarthritis are difficult to interpret. Most published reports are
retrospective with variable inclusion criteria, definition of
procedures, and outcome measures. These studies have found that
arthroscopic debridement yields satisfactory results in 60% to 70% of
patients at 2- to 4-year follow-up. There appears to be no clear
advantage to subchondral drilling or abrasion arthroplasty in these
patients. One prospective study comparing arthroscopic debridement
versus placebo surgery found no difference in clinical outcome at
2-year follow-up. In this study, however, patients were not stratified
with respect to presence or absence of meniscal pathology, mechanical
symptoms/signs, or malalignment. In another prospective outcome study,
44% of patients were found to have improvement in pain at 2-year
follow-up. Variables associated with improvement included medial joint
line tenderness, a positive Steinman test, and the presence of an
unstable meniscus tear at arthroscopy. Older patients (>70 years of
age) were more likely to be treated with early total knee arthroplasty
following arthroscopic debridement compared with patients younger than
60 years of age. This is consistent with the fact that arthroscopic
debridement does not change the natural history of osteoarthritis.
With respect to marrow stimulating techniques, the
available data support the use of microfracture for focal cartilage
defects. Significant improvements in outcome can be expected in 70% to
80% of patients. Improved results are found in those patients with
lower body mass index (<30 kg/m2), relatively short
duration of preoperative symptoms, and higher fill grade as measured by
postoperative MRI. In addition, microfracture combined with medial
opening wedge osteotomy has been shown in one study to decrease pain
and improve function in those patients with chondral defects and varus
malalignment at a minimum follow-up of 2 years.
available data support the use of microfracture for focal cartilage
defects. Significant improvements in outcome can be expected in 70% to
80% of patients. Improved results are found in those patients with
lower body mass index (<30 kg/m2), relatively short
duration of preoperative symptoms, and higher fill grade as measured by
postoperative MRI. In addition, microfracture combined with medial
opening wedge osteotomy has been shown in one study to decrease pain
and improve function in those patients with chondral defects and varus
malalignment at a minimum follow-up of 2 years.
In summary, the role of arthroscopy for osteoarthritis
of the knee remains controversial. Symptomatic relief can be expected
when patients are carefully selected and properly counseled. The best
outcomes are found in patients with a short duration of symptoms of
which mechanical symptoms are a significant component, those with
unstable meniscal tears and mild to moderate changes on x-ray films,
and those who are in the early stages of the disease process without
significant malalignment (Table 22-1). Despite
these findings, one study showed surgeons were only 60% accurate in
predicting which patients would have a successful outcome following
arthroscopy.
of the knee remains controversial. Symptomatic relief can be expected
when patients are carefully selected and properly counseled. The best
outcomes are found in patients with a short duration of symptoms of
which mechanical symptoms are a significant component, those with
unstable meniscal tears and mild to moderate changes on x-ray films,
and those who are in the early stages of the disease process without
significant malalignment (Table 22-1). Despite
these findings, one study showed surgeons were only 60% accurate in
predicting which patients would have a successful outcome following
arthroscopy.
|
TABLE 22-1 Results
|
||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||
Postoperative Management
Patients may weight-bear as tolerated following simple
arthroscopic debridement and lavage for osteoarthritis of the knee.
Pain control measures may include intraoperative subcutaneous
anesthetic injection, intra-articular anesthetic, corticosteroid or
narcotic injection, intra-articular pumps for postoperative local
anesthetic delivery, oral pain medications, and edema control. Based on
data from experimental and clinical studies, the use of continuous
passive motion and protected weight bearing is widely used for 6 weeks
following marrow stimulating procedures. There is some evidence to
suggest that dynamic compression may facilitate a better-quality repair
tissue, which in theory would contain a higher percentage of hyaline
cartilage. It is unknown if this protocol affects long-term clinical
outcomes following microfracture.
arthroscopic debridement and lavage for osteoarthritis of the knee.
Pain control measures may include intraoperative subcutaneous
anesthetic injection, intra-articular anesthetic, corticosteroid or
narcotic injection, intra-articular pumps for postoperative local
anesthetic delivery, oral pain medications, and edema control. Based on
data from experimental and clinical studies, the use of continuous
passive motion and protected weight bearing is widely used for 6 weeks
following marrow stimulating procedures. There is some evidence to
suggest that dynamic compression may facilitate a better-quality repair
tissue, which in theory would contain a higher percentage of hyaline
cartilage. It is unknown if this protocol affects long-term clinical
outcomes following microfracture.
A gradual return to primarily low-impact activities is
suggested when pain and swelling have decreased and strength has
returned. Return to higher-level impact activities and sports has not
been well studied in this population, and recommendations should be
individualized based on the patient’s goals and clinical outcome.
suggested when pain and swelling have decreased and strength has
returned. Return to higher-level impact activities and sports has not
been well studied in this population, and recommendations should be
individualized based on the patient’s goals and clinical outcome.
Suggested Readings
Bert
JM, Maschka K. The arthroscopic treatment of unicompartmental
gonarthrosis. A five year follow-up study of abrasion arthroplasty plus
arthroscopic debridement and arthroscopic debridement alone. Arthroscopy. 1989;5:25–32.
JM, Maschka K. The arthroscopic treatment of unicompartmental
gonarthrosis. A five year follow-up study of abrasion arthroplasty plus
arthroscopic debridement and arthroscopic debridement alone. Arthroscopy. 1989;5:25–32.
Dervin
GF, Stiell IG, Rody K, et al. Effect of arthroscopic debridement for
osteoarthritis of the knee on health-related quality of life. J Bone Joint Surg Am. 2003;85:10–19.
GF, Stiell IG, Rody K, et al. Effect of arthroscopic debridement for
osteoarthritis of the knee on health-related quality of life. J Bone Joint Surg Am. 2003;85:10–19.
Harwin SF. Arthroscopic debridement for osteoarthritis of the knee: Predictors of patient satisfaction. Arthroscopy. 1999;15(2):142–146.
Hsieh YS, Yang SF, Chu SC, et al. Expression changes in gelatinases in human osteoarthritic knees and arthroscopic debridement. Arthroscopy. 2004;20(5):482–488.
Lu
Y, Edwards RB, Colby J, et al. Thermal chondroplasty with
radiofrequency energy. An in vitro comparison of bipolar and monopolar
radiofrequency devices. Am J Sports Med. 2001;29:42–49.
Y, Edwards RB, Colby J, et al. Thermal chondroplasty with
radiofrequency energy. An in vitro comparison of bipolar and monopolar
radiofrequency devices. Am J Sports Med. 2001;29:42–49.
P.158
Marder
RA, Hopkins G Jr, Timmerman LA. Arthroscopic microfracture of chondral
defects of the knee: a comparison of two postoperative treatments. Arthroscopy. 2005;21(2):152–158.
RA, Hopkins G Jr, Timmerman LA. Arthroscopic microfracture of chondral
defects of the knee: a comparison of two postoperative treatments. Arthroscopy. 2005;21(2):152–158.
Mithoefer
K, Williams RJ III, Warren RF, et al. The microfracture technique for
the treatment of articular cartilage lesions in the knee. A prospective
cohort study. J Bone Joint Surg Am. 2005;87:1911–1920.
K, Williams RJ III, Warren RF, et al. The microfracture technique for
the treatment of articular cartilage lesions in the knee. A prospective
cohort study. J Bone Joint Surg Am. 2005;87:1911–1920.
Mosley JD, O’Malley K, Peterson NJ, et al. New Eng J Med. 2002;347:81–88.
Rand JA. Role of arthroscopy in osteoarthritis of the knee. Arthroscopy. 1991;7:358–363.
Rodrigo
JJ, Stedman JR, Stillman JS, et al. Improvement of full thickness
chondral defect healing in the human knee after debridement and
microfracture using submersion. Am J Knee Surg. 1994;7:109–116.
JJ, Stedman JR, Stillman JS, et al. Improvement of full thickness
chondral defect healing in the human knee after debridement and
microfracture using submersion. Am J Knee Surg. 1994;7:109–116.
Sterett WI, Steadman JR. Chondral resurfacing and high tibial osteotomy in the varus knee. Am J Sports Med. 2004; 32: 1243–1249.
Wai
EK, Kreder HJ, Williams JI. Arthroscopic debridement of the knee for
osteoarthritis in patients 50 years of age or older: Utilization and
outcomes in the province of Ontario. J Bone Joint Surg Am. 2002;84-A:17–22.
EK, Kreder HJ, Williams JI. Arthroscopic debridement of the knee for
osteoarthritis in patients 50 years of age or older: Utilization and
outcomes in the province of Ontario. J Bone Joint Surg Am. 2002;84-A:17–22.
