Phalanx Dislocation
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Phalanx Dislocation
Phalanx Dislocation
Tung B. Le MD
Andrew M. Richards MD
Description
-
Dislocations involve the following joints of the hand
-
MCP joint
-
PIP joint
-
DIP joint
-
-
Dislocations can be associated with fractures, ligament, tendon, or joint capsule injury.
-
Classification is by the joint and the direction of dislocation:
-
PIP dislocations:
-
Dorsal: Most common, resulting from volar plate injury
-
Volar: Rare, associated with central slip disruption
-
Rotatory: Rare, from “buttonholing” of 1
condyle of the head of proximal phalanx through the space between the
central slip and the lateral band
-
-
MCP dislocations:
-
Lateral: Collateral ligament injuries
-
Dorsal: Volar plate injury, may be irreducible closed
-
-
DIP dislocations:
-
Simple: Reducible
-
Complex: Irreducible closed because of entrapment of the volar plate between 2 dislocated middle and proximal phalanges
-
-
-
Synonym (MCP joint dislocation): Skier’s thumb
General Prevention
Simple changes have been proposed to decrease hand
injuries in children’s sports, including softening the ball, increasing
awareness of parents and coaches, and having weight categories (1).
injuries in children’s sports, including softening the ball, increasing
awareness of parents and coaches, and having weight categories (1).
Epidemiology
-
Joint dislocation usually occurs in skeletally mature patients.
-
In the pediatric population, the physes are weaker than the capsular structures.
-
Therefore, physeal fractures or separations are more common than joint dislocations in children.
-
-
Thumb MCP dislocations are common among skiers (2).
Incidence
A study of pediatric hand injuries showed that 68% were fractures, 26% were soft-tissue injuries, and 11% were dislocations (3).
Prevalence
-
Common
-
In 1 study, 28% of all visits to an emergency department were secondary to hand injury (4).
Risk Factors
-
Basketball
-
Skiing
Genetics
No known Mendelian pattern exists.
Etiology
-
Trauma is the cause of phalanx dislocations.
-
Dorsal dislocation is caused by a hyperextension force.
-
Volar dislocation is caused by a hyperflexion force.
-
Associated Conditions
-
Phalangeal fractures:
-
Look carefully for small fracture fragments because they usually are indicators of a soft-tissue avulsion injury.
-
-
Injuries of the periarticular structures of the involved joints (especially volar plate, ligaments)
Signs and Symptoms
-
Pain
-
Deformity (Fig. 1)
-
Ecchymosis
-
Loss of motion
-
Altered sensation or perfusion (or both) from neurovascular compression
History
-
Mechanism of injury
-
Time and events since injury
-
Dominant hand of the patient
Physical Exam
-
Assess the neurovascular status of the hand.
-
Examine the skin for open wounds.
-
Clinical assessment for instability and
tenderness should be performed a few days after injury to allow the
worst of the swelling to resolve.
Tests
Imaging
-
To evaluate adequately the phalangeal bones and joints, initial radiographs include true lateral, AP, and oblique views.
-
Stress views of the relocated joint may be important in assessing dislocations when ligamentous disruptions are possible.
Pathological Findings
-
Dislocations of the phalangeal joints often result in injuries to surrounding soft-tissue structures.
-
Lateral dislocations of these joints lead to collateral ligament tears.
-
The volar plate is at risk in hyperextension injuries and dorsal dislocations.
-
In skier’s thumb (dislocation of the
thumb MCP joint with or without avulsion fracture of the metacarpal
base), both the collateral ligament and the volar plate are torn.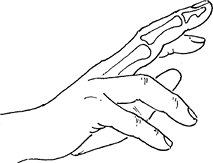 Fig. 1. IP joint dislocations are almost always dorsal because of hyperextension injuries.
Fig. 1. IP joint dislocations are almost always dorsal because of hyperextension injuries.
P.327
Differential Diagnosis
-
Fracture dislocation
-
Chronic dislocation
-
Collateral ligament injury
-
Associated volar plate injury
-
Rheumatoid arthritis
-
Septic arthritis
General Measures
-
Phalangeal dislocations:
-
Attempt closed reduction (Fig. 2).
-
Once reduced, minimize swelling with RICE protocol.
-
-
Joint reduction:
-
Gentle traction coupled with additional hyperextension/flexion to disimpact the dislocation
-
Gradually reduce the phalanx to its anatomic position.
-
-
Dislocations that are not reducible require surgical intervention.
-
Ligamentous tears:
-
Protective immobilization with “buddy” taping for collateral injuries.
-
-
Volar plate disruption:
-
Extension block splint
-
-
Complete ruptures of the collateral ligaments, volar plates, or central slips:
-
Immobilize for 3–6 weeks.
-
-
PIP joints:
-
Splint in 15° of flexion after reduction of dorsal dislocations.
-
-
MCP joints:
-
Immobilize in 50–70° of flexion.
-
-
Central slip disruptions:
-
Use an extension splint for 3 weeks, followed by dynamic splinting.
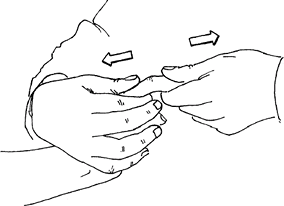 Fig. 2. IP dislocation is reduced by longitudinal traction and gentle flexion.
Fig. 2. IP dislocation is reduced by longitudinal traction and gentle flexion.
-
Special Therapy
Physical Therapy
-
Active and gentle passive ROM exercises are begun once stability of the joint is confirmed.
-
Therapy to reduce swelling and prevent stiffness is extremely important after surgical repair (5).
Medication
First Line
Analgesics or NSAIDs are used as needed.
Surgery
-
Surgery is indicated when closed reduction fails.
-
Failure occurs when:
-
A blockage of a bone fragment or soft tissue occurs within the joint.
-
A buttonholed fragment is present.
-
-
-
Volar or dorsal approach both allow the joint to be cleared and reduced.
-
Surgery also may be required to stabilize associated fractures or attend to wounds.
-
Dislocations of the thumb MCP joint:
-
May lead to interposition of the UCL of the thumb (the Stener lesion)
-
Requires open repair (6)
-
Disposition
Issues for Referral
Injuries to the MCP joint of the thumb, fracture
dislocations, open injuries, and irreducible dislocations should be
referred to an orthopedic surgeon.
dislocations, open injuries, and irreducible dislocations should be
referred to an orthopedic surgeon.
Prognosis
Some loss of motion can be expected.
Complications
-
Persistent pain and swelling (up to 12 months)
-
Instability with recurrent dislocation
-
Stiffness
-
Associated neurovascular injuries (rare)
Patient Monitoring
-
Patients are followed at 3–6-week intervals to ensure that they maintain adequate ROM.
-
After reduction (with or without surgery), patients should be followed by a hand therapist.
References
1. Macgregor DM. Don’t save the ball! Br J Sports Med 2003;37:351–353.
2. Deibert
MC, Aronsson DD, Johnson RJ, et al. Skiing injuries in children,
adolescents, and adults. J Bone Joint Surg 1998;80A:25–32.
MC, Aronsson DD, Johnson RJ, et al. Skiing injuries in children,
adolescents, and adults. J Bone Joint Surg 1998;80A:25–32.
3. Choyce MQ, Potts M, Maitra AK. A profile of sports hand injuries in an accident and emergency department. J Accid Emerg Med 1998;15:35–38.
4. Packer GJ, Shaheen MA. Patterns of hand fractures and dislocations in a district general hospital. J Hand Surg 1993;18B:511–514.
5. Chinchalkar SJ, Gan BS. Management of proximal interphalangeal joint fractures and dislocations. J Hand Ther 2003;16:117–128.
6. Catalano
LW, III, Cardon L, Patenaude N, et al. Results of surgical treatment of
acute and chronic grade III [corrected] tears of the radial collateral
ligament of the thumb metacarpophalangeal joint. J Hand Surg 2006;31A:68–75.
LW, III, Cardon L, Patenaude N, et al. Results of surgical treatment of
acute and chronic grade III [corrected] tears of the radial collateral
ligament of the thumb metacarpophalangeal joint. J Hand Surg 2006;31A:68–75.
Additional Reading
Glickel
SZ, Barron OA, Catalano LW, III. Dislocations and ligament injuries in
the digits. In Green DP, Hotchkiss RN, Pederson WC, et al., eds.
Green’s Operative Hand Surgery, 5th ed. Philadelphia: Elsevier Churchill Livingstone, 2005:343–388.
SZ, Barron OA, Catalano LW, III. Dislocations and ligament injuries in
the digits. In Green DP, Hotchkiss RN, Pederson WC, et al., eds.
Green’s Operative Hand Surgery, 5th ed. Philadelphia: Elsevier Churchill Livingstone, 2005:343–388.
Freiberg A, Pollard BA, Macdonald MR, et al. Management of proximal IP joint injuries. J Trauma 1999;46:523–528.
Glickel SZ, Barron OA. PIP joint fracture dislocations. Hand Clin 2000;16: 333–344.
Green DP, Butler TE, Jr. Fractures and dislocations in the hand. In: Rockwood CA, Jr, Green DP, Bucholz RW, et al., eds. Rockwood and Green’s Fractures in Adults, 4th ed. Philadelphia: Lippincott-Raven, 1996:607–744.
Codes
ICD9-CM
834.0 Dislocation, phalanx
Patient Teaching
-
Advise patients that recovery up to 12 months depends on continuing rehabilitation.
-
Prescribe strict initial immobilization of the involved joint to achieve stability and healing.
-
Advise patients to use protective hand wear or finger taping during sports.
Prevention
-
Be aware of the risk of injury, particularly in children’s sporting events.
-
Use the lightest ball possible in sporting events.
FAQ
Q: How long does a finger dislocation take to heal?
A:
Continued swelling of the finger and knuckle often is seen for at least
1 year after injury. In some cases, finger size does not return to
normal.
Continued swelling of the finger and knuckle often is seen for at least
1 year after injury. In some cases, finger size does not return to
normal.
