Distal Humerus
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > III – Upper Extremity Fractures and Dislocations > 17 – Distal Humerus
17
Distal Humerus
EPIDEMIOLOGY
-
Fractures of the adult distal humerus are
relatively uncommon, comprising approximately 2% of all fractures and
one-third of all humerus fractures. -
Intercondylar fractures of the distal humerus are the most common fracture pattern.
-
Extension-type supracondylar fractures of the distal humerus account for >80% of all supracondylar fractures in adults.
ANATOMY
-
The distal humerus may be conceptualized
as medial and lateral “columns,” each of which is roughly triangular
and is composed of an epicondyle, or the nonarticulating terminal of the supracondylar ridge, and a condyle, which is the articulating unit of the distal humerus (Fig. 17.1). -
The articulating surface of the
capitellum and trochlea projects distally and anteriorly at an angle of
40 to 45 degrees. The centers of the arcs of rotation of the articular
surfaces of each condyle lie on the same horizontal axis; thus,
malalignment of the relationships of the condyles to each other changes
their arc of rotation, thus limiting flexion and extension (Fig. 17.2). -
The trochlear axis compared with the longitudinal axis is 4 to 8 degrees of valgus.
-
The trochlear axis is 3 to 8 degrees externally rotated.
-
The intramedullary canal ends 2 to 3 cm above the olecranon fossa.
MECHANISM OF INJURY
-
Most low-energy distal humeral fractures
result from a simple fall in middle-aged and elderly women in which the
elbow is either struck directly or is axially loaded in a fall onto the
outstretched hand. -
Motor vehicle and sporting accidents are more common causes of injury in younger individuals.
CLINICAL EVALUATION
-
Signs and symptoms vary with degree of
swelling and displacement; considerable swelling frequently occurs,
rendering landmarks difficult to palpate. However, the normal
relationship of the olecranon, medial, and lateral condyles should be
maintained, roughly delineating an equilateral triangle. -
Crepitus with range of motion and gross
instability may be present; although this is highly suggestive of
fracture, no attempt should be made to elicit it because neurovascular
compromise may result. -
A careful neurovascular evaluation is
essential because the sharp, fractured end of the proximal fragment may
impale or contuse the brachial artery, median nerve, or radial nerve.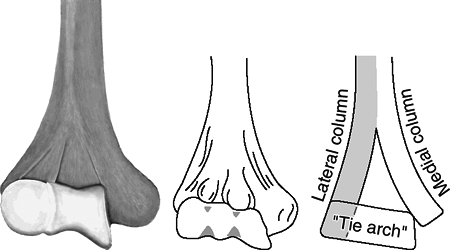 Figure
Figure
17.1. The distal most part of the lateral column is the capitellum, and
the distal most part of the medial column is the nonarticular medial
epicondyle. The trochlea is the medial most part of the articular
segment and is intermediate in position between the medial epicondyle
and capitellum. The articular segment functions architecturally as a
“tie arch.”![]() Figure
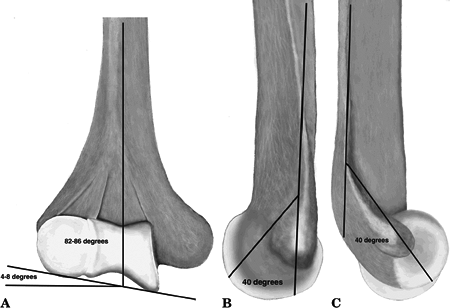
Figure
17.2. The joint surface to shaft axis is 4 to 8 degrees of valgus—the
A-carrying angle (A). The articular segment juts forward from the line
of the shaft at 40 degrees and functions architecturally as the tie
arch at the point of maximum column divergence distally. The medial
epicondyle is on the projected axis of the shaft, whereas the lateral
epicondyle is projected slightly forward from the axis (B,C). -
Serial neurovascular examinations with
compartment pressure monitoring may be necessary with massive swelling;
cubital fossa swelling may result in vascular impairment or the
development of a volar compartment syndrome resulting in Volkmann
ischemia.
P.180
P.181
RADIOGRAPHIC EVALUATION
-
Standard anteroposterior (AP) and lateral
views of the elbow should be obtained. Oblique radiographs may be
helpful for further fracture definition. -
Traction radiographs may better delineate the fracture pattern and may be useful for preoperative planning.
-
In nondisplaced fractures, an anterior or
posterior “fat pad sign” may be present on the lateral radiograph,
representing displacement of the adipose layer overlying the joint
capsule in the presence of effusion or hemarthrosis. -
Minimally displaced fractures may result
in a decrease in the normal condylar shaft angle of 40 degrees seen on
the lateral radiograph. -
Because intercondylar fractures are much
more common than supracondylar fractures in adults, the AP (or oblique)
radiograph should be scrutinized for evidence of a vertical split in
the intercondylar region of the distal humerus. -
Computed tomography may be utilized to delineate fracture fragments further.
CLASSIFICATION
Descriptive
-
Supracondylar fractures
-
Extension-type
-
Flexion-type
-
-
Transcondylar fractures
-
Intercondylar fractures
-
Condylar fractures
-
Capitellum fractures
-
Trochlea fractures
-
Lateral epicondylar fractures
-
Medial epicondylar fractures
-
Fractures of the supracondylar process
OTA Classification of Fractures of the Distal Humerus
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
GENERAL TREATMENT PRINCIPLES
-
Anatomic articular reduction
-
Stable internal fixation of the articular surface
-
Restoration of articular axial alignment
-
Stable internal fixation of the articular segment to the metaphysis and diaphysis
-
Early range of elbow motion
P.182
SPECIFIC FRACTURE TYPES
Extension-type Supracondylar Fracture
-
This results from a fall onto an outstretched hand with or without an abduction or adduction force.
Treatment
NONOPERATIVE
-
This is indicated for nondisplaced or
minimally displaced fractures, as well as for severely comminuted
fractures in elderly patients with limited functional ability. -
Posterior long arm splint is placed in at
least 90 degrees of elbow flexion if swelling and neurovascular status
permit, with the forearm in neutral. -
Posterior splint immobilization is
continued for 1 to 2 weeks, after which range-of-motion exercises are
initiated. The splint may be discontinued after approximately 6 weeks,
when radiographic evidence of healing is present. -
Frequent radiographic evaluation is necessary to detect loss of fracture reduction.
OPERATIVE
-
Indications
-
Displaced fracture
-
Vascular injury
-
Open fracture
-
-
Open reduction and internal fixation:
Plate fixation is used on each column, either in parallel or preferably
set at 90 degrees. Plate fixation is the procedure of choice, because
this allows for early range of elbow motion. -
Total elbow replacement may be considered
in elderly patients who otherwise are active with good preinjury
function in whom a severely comminuted fracture of the distal humerus
is deemed unreconstructable. The medial, triceps-sparing approach
should be utilized, rather than an olecranon osteotomy, for exposure of
the elbow joint. -
Range-of-motion exercises should be initiated as soon as the patient is able to tolerate therapy.
Complications
-
Volkmann ischemic contracture: This may
result from unrecognized compartment syndrome with subsequent
neurovascular compromise. A high index of suspicion accompanied by
aggressive elevation and serial neurovascular examinations with or
without compartment pressure monitoring must be maintained. -
Stiffness: Up to a 20-degree decrease in the condylar-shaft angle may be tolerated owing to compensatory motion of the shoulder.
-
Heterotopic bone formation may occur.
Flexion-type Supracondylar Fracture
-
This uncommon injury is frequently
associated with open lesions as the sharp, proximal fragment pierces
the triceps tendon and overlying skin. -
Associated vascular injuries are rare, accounting for 2% to 4% of supracondylar fractures.
P.183
Mechanism of Injury
-
Force is directed against the posterior aspect of a flexed elbow.
Treatment
NONOPERATIVE
-
Nondisplaced or minimally displaced
fractures may be immobilized in a posterior elbow splint in relative
extension. Elbow flexion may result in fracture displacement.
OPERATIVE
-
Open reduction and internal fixation: Plate fixation is used in each column, either in parallel or preferably set at 90 degrees.
-
Range-of-motion exercises should be initiated as soon as the patient is able to tolerate therapy.
-
Total elbow replacement may be considered
in elderly patients who otherwise are active with good preinjury
function in whom a severely comminuted fracture of the distal humerus
is deemed unreconstructable.
Transcondylar Fractures
-
These occur primarily in elderly patients with osteopenic bone.
Mechanism of Injury
-
Mechanisms that produce supracondylar
fractures may also result in transcondylar fractures: a fall onto an
outstretched hand with or without an abduction or adduction component
or a force applied to a flexed elbow.
Treatment
NONOPERATIVE
-
This is indicated for nondisplaced or
minimally displaced fractures or in elderly patients who are
debilitated and functioning poorly. -
Range-of-motion exercises should be initiated as soon as the patient is able to tolerate therapy.
OPERATIVE
-
Operative treatment should be undertaken for open fractures, unstable fractures, or displaced fractures.
-
Open reduction and plate fixation are the preferred treatment.
-
Total elbow arthroplasty
(semiconstrained) may be considered in the elderly patient with good
preinjury functional status if fixation cannot be obtained.
Intercondylar Fracture
-
This is the most common distal humeral fracture.
-
Comminution is common.
-
Fracture fragments are often displaced by
unopposed muscle pull at the medial (flexor mass) and lateral (extensor
mass) epicondyles, which rotate the articular surfaces.
P.184
Mechanism of Injury
-
Force is directed against the posterior aspect of an elbow flexed >90 degrees, thus driving the ulna into the trochlea.
Classification
OTA CLASSIFICATION
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
 |
|
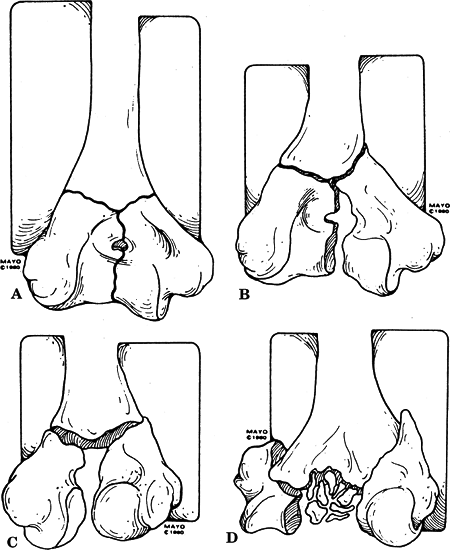
Figure
17.3. Riesborough and Radin classification. (A) Type I undisplaced condylar fracture of the elbow. (B) Type II displaced but not rotated T-condylar fracture. (C) Type III displaced and rotated T-condylar fracture. (D) Type IV displaced, rotated, and comminuted condylar fracture. (From Bryan RS. Fractures about the elbow in adults. AAOS Instr Course Lect 1981;30:200–223.)
|
P.185
Treatment
-
Treatment must be individualized according to patient age, bone quality, and degree of comminution.
NONOPERATIVE
-
This is indicated for nondisplaced
fractures, elderly patients with displaced fractures and severe
osteopenia and comminution, or patients with significant comorbid
conditions precluding operative management. Nonoperative options for
displaced fractures include:-
Cast immobilization: This has few
advocates; it represents the “worst of both worlds”—inadequate fracture
reduction and prolonged immobilization. -
Traction with an olecranon pin: This is
placed overhead to reduce swelling; it is problematic in that
longitudinal traction alone will not derotate the intercondylar
fragments in the axial plane, and this leads to malunion. -
“Bag of bones”: The arm is placed in a
collar and cuff with as much flexion as possible after initial
reduction is attempted; gravity traction helps effect reduction.
-
OPERATIVE
-
Open reduction and internal fixation
-
The indication is a displaced reconstructible fracture.
-
Goals of fixation are to restore articular congruity and to secure the supracondylar component.
-
Methods of fixation
-
Interfragmentary screws
-
Dual plate fixation: one plate medially and another plate placed posterolaterally, 90 degrees from the medial plate
-
-
-
Total elbow arthroplasty
(semiconstrained): This may be considered in markedly comminuted
fractures and with fractures in osteoporotic bone. -
Surgical exposures
-
Tongue of triceps
-
Does not allow full exposure of joint.
-
Deters early active motion for fear of triceps rupture.
-
-
Olecranon osteotomy: intraarticular; A chevron is best for rotational stability.
-
A triceps-sparing extensile posterior approach (Bryan and Morrey) can be used.
-
-
Postoperative care: Early range of motion of the elbow is essential unless fixation is tenuous.
Complications
-
Posttraumatic arthritis: This results
from articular injury at time of trauma as well as a failure to restore
articular congruity. -
Failure of fixation: Postoperative
collapse of fixation is related to the degree of comminution, the
stability of fixation, and protection of the construct during the
postoperative course. -
Loss of motion (extension): This is
increased with prolonged periods of immobilization. Range-of-motion
exercises should be instituted as soon as the patient is able to
tolerate therapy, unless fixation is tenuous. -
Heterotopic bone.
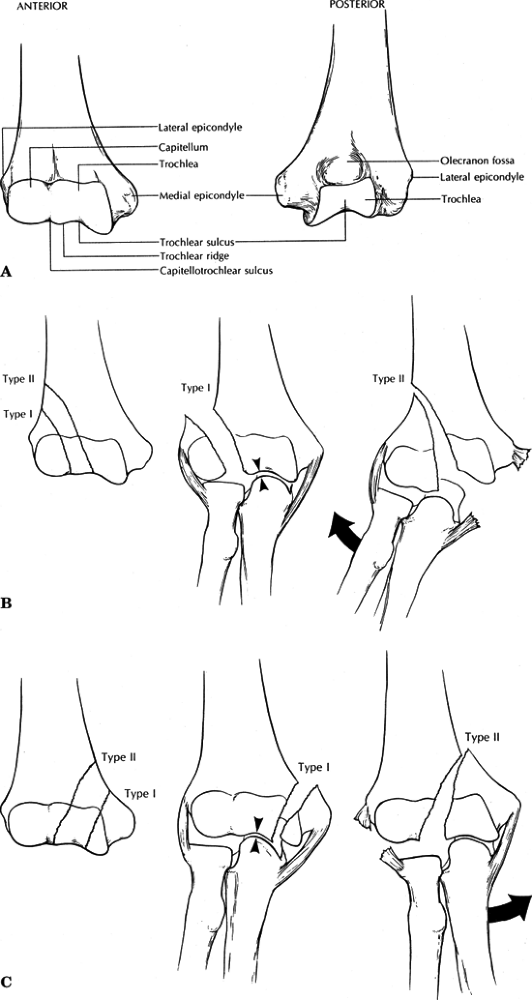
![]() Figure
Figure
17.4. Classification of condylar fractures according to Milch and the
location of the common fracture lines seen in Type I and II fractures
of the lateral (B) and medial (C) condyles. (A) Anterior view of the
anatomy of the distal articular surface of the humerus. The
capitellotrochlear sulcus divides the capitellar and trochlear
articular surfaces. The lateral trochlear ridge is the key to analyzing
humeral condyle fractures. In Type I fractures, the lateral trochlear
ridge remains with the intact condyle, providing medial to lateral
elbow stability. In Type II fractures, the lateral trochlear ridge is a
part of the fractured condyle, which may allow the radius and ulna to
translocate in a medial to lateral direction with respect to the long
axis of the humerus. (B) Fractures of the lateral condyle. In Type I
fractures, the lateral trochlear ridge remains intact, therefore
preventing dislocation of the radius and ulna. In Type II fractures,
the lateral trochlear ridge is a part of the fractured lateral condyle.
With capsuloligamentous disruption medially, the radius and ulna may
dislocate. (C) Fractures of the medial condyle. In Type I fractures,
the lateral trochlear ridge remains intact to provide medial-to-lateral
stability of the radius and ulna. In Type II fractures, the lateral
trochlear ridge is a part of the fractures medial condyle. With lateral
capsuloligamentous disruption, the radius and ulna may dislocate
medially on the humerus.(From Rockwood CA Jr, Green DP, Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 4th ed, vol. 1. Philadelphia: Lippincott-Raven, 1996:954.) -
Neurologic injury: The ulnar nerve is most commonly injured during surgical exposure.
P.186
P.187
Condylar Fractures
-
These are rare in adults and are much more common in the pediatric age group.
-
Less than 5% of all distal humerus fractures are condylar; lateral fractures are more common than medial.
-
Medial condyle fractures: These include
the trochlea and medial epicondyle and are less common than medial
epicondylar fractures. -
Lateral condyle fractures: These include the capitellum and lateral epicondyle.
Mechanism of Injury
-
Abduction or adduction of the forearm with elbow extension.
Classification
MILCH
Two types are designated for medial and lateral condylar fractures; the key is the lateral trochlear ridge (Fig. 17.4):
| Type I: | Lateral trochlear ridge left intact |
| Type II: | Lateral trochlear ridge part of the condylar fragment (medial or lateral) |
-
These are less stable.
-
They may allow for radioulnar translocation if capsuloligamentous disruption occurs on the contralateral side.
JUPITER
This is low or high, based on proximal extension of fracture line to supracondylar region:
P.188
OTA CLASSIFICATION
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
-
Low: equivalent to Milch type I fracture
-
High: equivalent to Milch type II fracture
Treatment
-
Anatomic restoration of articular
congruity is essential to maintain the normal elbow arc of motion and
to minimize the risk of posttraumatic arthritis.
NONOPERATIVE
-
Indicated for nondisplaced or minimally
displaced fractures or for patients with displaced fractures who are
not considered candidates for operative treatment. -
It consists of posterior splinting with
the elbow flexed to 90 degrees and the forearm in supination or
pronation for lateral or medial condylar fractures, respectively.
OPERATIVE
-
Indicated for open or displaced fractures.
-
Consists of screw fixation with or
without collateral ligament repair if necessary, with attention to
restoration of the rotational axes. -
Prognosis depends on:
-
The degree of comminution.
-
The accuracy of reduction.
-
The stability of internal fixation.
-
-
Range-of-motion exercises should be instituted as soon as the patient can tolerate therapy.
Complications
-
Lateral condyle fractures: Improper
reduction or failure of fixation may result in cubitus valgus and tardy
ulnar nerve palsy requiring nerve transposition. -
Medial condyle fractures: Residual
incongruity is more problematic owing to involvement of the trochlear
groove. These may result in:-
Posttraumatic arthritis, especially with fractures involving the trochlear groove.
-
Ulnar nerve symptoms with excess callus formation or malunion.
-
Cubitus varus with inadequate reduction or failure of fixation.
-
Capitellum Fractures
-
These represent <1% of all elbow fractures.
-
They occur in the coronal plane, parallel to the anterior humerus.
-
Little or no soft tissue attachments result in a free articular fragment that may displace.
-
Anterior displacement of the articular fragment into the coronoid or radial fossae may result in a block to flexion.
P.189
Mechanism of Injury
-
A fall onto an outstretched hand with the
elbow in varying degrees of flexion; force is transmitted through the
radial head the capitellum. Fracture occurs secondary to shear. -
These are occasionally associated with radial head fractures.
Classification
OTA CLASSIFICATION
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
Treatment
NONOPERATIVE
-
This is primarily used for nondisplaced fractures.
-
It consists of immobilization in a posterior splint for 3 weeks followed by range of elbow motion.
 |
|
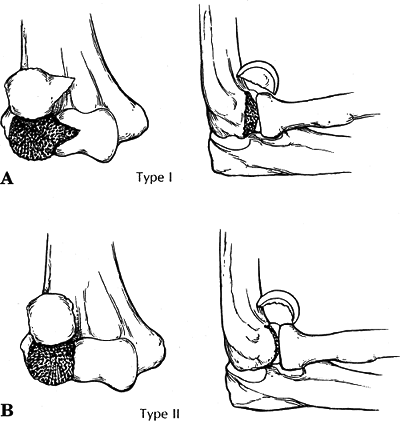
Figure
17.5. (A) Type I (Hahn-Steinthal) capitellar fracture. A portion of the trochlea may be involved in this fracture. (B) Type II (Kocher-Lorenz) capitellar fracture. Very little subchondral bone is attached to the capitellar fragment. (From Rockwood CA Jr, Green DP, Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 4th ed, vol. 1. Philadelphia: Lippincott-Raven, 1996:960.)
|
P.190
OPERATIVE
-
The goal is anatomic restoration.
-
Open reduction and internal fixation
-
This technique is indicated for displaced type I fractures.
-
Via a posterolateral or posterior
approach, screws may be placed from a posterior to anterior direction;
alternatively, headless screws may be placed from anterior to posterior. -
Fixation should be stable enough to allow early range of elbow motion.
-
-
Excision
-
This is indicated for severely comminuted type I fractures and most type II fractures.
-
Proximal migration of the radius with distal radioulnar joint pain is uncommon.
-
This is relatively contraindicated in the presence of associated elbow fractures owing to compromise of elbow stability.
-
This is the recommended treatment in chronic missed fractures with limited range of elbow motion.
-
Complications
-
Osteonecrosis: This is relatively uncommon.
-
Posttraumatic arthritis: The risk is
increased with failure to restore articular congruity and excision of
the articular fragment. -
Cubitus valgus: This may result after
excision of articular fragment or with an associated lateral condylar
or radial head fracture. It is associated with tardy ulnar nerve palsy. -
Loss of motion (flexion): This is
associated with retained chondral or osseous fragments that may become
entrapped in the coronoid or radial fossae.
Trochlea Fractures (Laugier’s Fracture)
Mechanism of Injury
-
Tangential shearing force resulting from elbow dislocation.
Treatment
-
Nondisplaced fractures may be managed with posterior splinting for 3 weeks followed by range-of-motion exercises.
-
Displaced fractures should receive open reduction and internal fixation with Kirschner wire or screw fixation.
-
Fragments not amenable to internal fixation should be excised.
Complications
-
Posttraumatic arthritis may result with
retained osseous fragments within the elbow joint or incongruity of the
articular surface. -
Restricted range of motion may result from malunion of the trochlear fragment.
Lateral Epicondylar Fractures
-
Extremely rare.
Mechanism of Injury
-
Direct trauma is the mechanism in adults.
-
Prepubescent patients may experience avulsion fractures.
Treatment
-
Symptomatic immobilization is followed by early range of elbow motion.
Complications
-
Nonunion may result in continued symptoms of pain exacerbated by wrist or elbow motion.
Medial Epicondylar Fractures
-
These are more common than lateral
epicondylar fractures owing to the relative prominence of the
epicondyle on the medial side of the elbow.
Mechanism of Injury
-
In children and adolescents, the medial epicondyle may be avulsed during a posterior elbow dislocation.
-
In adults, it is most commonly the result
of direct trauma, although it can occur as an isolated fracture or
associated with elbow dislocation.
Treatment
-
Nondisplaced or minimally displaced
fractures may be managed by short-term immobilization for 10 to 14 days
in a posterior splint with the forearm pronated and the wrist and elbow
flexed. -
Operative indications
-
Relative indications include displaced
fragments in the presence of ulnar nerve symptoms, elbow instability to
valgus stress, wrist flexor weakness, and symptomatic nonunion of the
displaced fragment. -
Open reduction and internal fixation
versus excision: Excision is indicated for fragments not amenable to
internal fixation or are incarcerated within the joint space.
-
Complications
-
Posttraumatic arthritis: This may result from osseous fragments retained within the joint space.
-
Weakness of the flexor mass: This may result from nonunion of the fragment or malunion with severe distal displacement.
Fractures of the Supracondylar Process
-
The supracondylar process is a congenital
osseous or cartilaginous projection that arises from the anteromedial
surface of the distal humerus. -
The ligament of Struthers is a fibrous
arch connecting the supracondylar process with the medial epicondyle,
from which fibers of the pronator teres or the coracobrachialis may
arise. -
Through this arch traverse the median nerve and the brachial artery.
-
Fractures are rare, with a reported
incidence between 0.6% and 2.7%, but they may result in pain and median
nerve or brachial artery compression.
P.192
Mechanism of Injury
-
Direct trauma to the anterior aspect of the distal humerus.
Treatment
-
Most of these fractures are amenable to
nonoperative treatment with symptomatic immobilization in a posterior
elbow splint in relative flexion until pain free, followed by
range-of-motion and strengthening exercises. -
Median nerve or brachial artery compression may require surgical exploration and release.
Complications
-
Myositis ossificans: The risk is increased with surgical exploration.
-
Recurrent spur formation: This may result
in recurrent symptoms of neurovascular compression, necessitating
surgical exploration and release, with excision of the periosteum and
attached muscle fibers to prevent recurrence.