Humeral Shaft Fractures
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > III – Upper Extremity Fractures and Dislocations > 16 – Humeral Shaft Fractures
16
Humeral Shaft Fractures
EPIDEMIOLOGY
-
Common injury, representing 3% to 5% of all fractures.
ANATOMY
-
The humeral shaft extends from the
pectoralis major insertion to the supracondylar ridge. In this
interval, the cross-sectional shape changes from cylindric to narrow in
the anteroposterior direction. -
The vascular supply to the humeral
diaphysis arises from perforating branches of the brachial artery, with
the main nutrient artery entering the medial humerus distal to the
midshaft (Fig. 16.1). -
The musculotendinous attachments of the humerus result in characteristic fracture displacements (Table 16.1).Table 16.1. Position of fracture fragments
Fracture Location Proximal Fragment Distal Fragment Above pectoralis major insertion Abducted, rotated externally by rotator cuff Medial, proximal by deltoid and pectoralis major Between pectoralis major and deltoid tuberosity Medial by pectoralis, teres major, and latissimus dorsi Lateral, proximal by deltoid Distal to deltoid tuberosity Abducted by deltoid Medial, proximal by biceps and triceps
MECHANISM OF INJURY
-
Direct (most common): Direct trauma to
the arm from a blow or motor vehicle accident results in transverse or
comminuted fractures. -
Indirect: A fall on an outstretched arm
results in spiral or oblique fractures, especially in elderly patients.
Uncommonly, throwing injuries with extreme muscular contraction have
been reported to cause humeral shaft fractures. -
Fracture pattern depends on the type of force applied:
-
Compressive: proximal or distal humeral fractures
-
Bending: transverse fractures of the humeral shaft
-
Torsional: spiral fractures of the humeral shaft
-
Torsional and bending: oblique fracture, often accompanied by a butterfly fragment
-
CLINICAL EVALUATION
-
Patients with humeral shaft fractures typically present with pain, swelling, deformity, and shortening of the affected arm.
-
A careful neurovascular examination is
essential, with particular attention to radial nerve function. In cases
of extreme swelling, serial neurovascular examinations are indicated
with possible measurement of compartment pressures. -
Physical examination frequently reveals gross instability with crepitus on gentle manipulation.
-
Soft tissue abrasions and minor lacerations must be differentiated from open fractures.
-
Intraarticular extensions of open
fractures may be determined by intraarticular injection of saline
distant from the wound site and noting extravasation of fluid from the
wound.
RADIOGRAPHIC EVALUATION
-
AP and lateral radiographs of the humerus should be obtained, including the shoulder and elbow joints on each view. To
P.173P.174
obtain views at 90° from each other, the patient, NOT the arm, should
be rotated, as manipulation of the injured extremity will typically
result in distal fragment rotation only.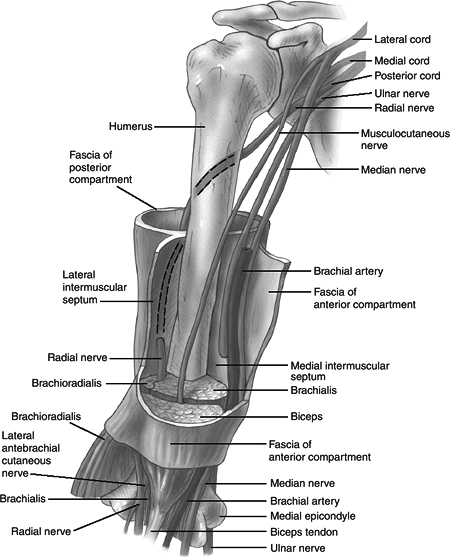 Figure 16.1. The neurovascular anatomy of the upper arm.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 16.1. The neurovascular anatomy of the upper arm.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Traction radiographs may aid in fracture definition in cases of severely displaced or comminuted fracture patterns.
-
Radiographs of the contralateral humerus may aid in preoperative planning.
-
Computed tomography, bone scans, and MRI are rarely indicated except in cases in which pathologic fracture is suspected.
CLASSIFICATION
Descriptive
-
Open vs. closed.
-
Location: proximal third, middle third, distal third.
-
Degree: nondisplaced, displaced.
-
Direction and character: transverse, oblique, spiral, segmental, comminuted.
-
Intrinsic condition of bone.
-
Articular extension.
OTA Classification
-
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
TREATMENT
-
The goal is to establish union with an acceptable humeral alignment and to restore the patient to preinjury level of function.
-
Both patient and fracture
characteristics, including patient age and functional level, presence
of associated injuries, soft tissue status, and fracture pattern, need
to be considered when selecting an appropriate treatment option.
Nonoperative
-
Nonoperative treatment requirements are:
-
An understanding by the treating physician of the postural and muscular forces that must be controlled.
-
Dedication to close patient supervision and follow-up.
-
A cooperative and preferably upright and mobile patient.
-
An acceptable reduction.
-
-
Most humeral shaft fractures (>90%) will heal with nonsurgical management.
-
Twenty degrees of anterior angulation, 30
degrees of varus angulation, and up to 3 cm of bayonet apposition are
acceptable and will not compromise function or appearance. -
Hanging cast: This utilizes dependency traction by the weight of the cast and arm to effect fracture reduction.
-
Indications include displaced midshaft
humeral fractures with shortening, particularly spiral or oblique
patterns. Transverse or short oblique fractures represent relative
contraindications because of the potential for distraction and healing
complications. -
The patient must remain upright or semiupright at all times with the cast in a dependent position for effectiveness.
-
It is frequently exchanged for functional bracing 1 to 2 weeks after injury.
-
More than 95% union is reported.
P.175 -
-
Coaptation splint: This utilizes
dependency traction to effect fracture reduction, but with greater
stabilization and less distraction than a hanging arm cast. The forearm
is suspended in a collar and cuff.-
It is indicated for the acute treatment
of humeral shaft fractures with minimal shortening and for short
oblique or transverse fracture patterns that may displace with a
hanging arm cast. -
Disadvantages include irritation of the patient’s axilla and the potential for splint slippage.
-
It is frequently exchanged for functional bracing 1 to 2 weeks after injury.
-
-
Thoracobrachial immobilization (Velpeau
dressing): This is used in elderly patients or children who are unable
to tolerate other methods of treatment and in whom comfort is the
primary concern.-
It is indicated for minimally displaced or nondisplaced fractures that do not require reduction.
-
Passive shoulder pendulum exercises may be performed within 1 to 2 weeks after injury.
-
It may be exchanged for functional bracing 1 to 2 weeks after injury.
-
-
Shoulder spica cast: This has limited application, because operative management is typically performed for the same indications.
-
It is indicated when the fracture pattern necessitates significant abduction and external rotation of the upper extremity.
-
Disadvantages include difficulty of cast
application, cast weight and bulkiness, skin irritation, patient
discomfort, and inconvenient upper extremity position.
-
-
Functional bracing: This utilizes
hydrostatic soft tissue compression to effect and maintain fracture
alignment while allowing motion of adjacent joints.-
It is typically applied 1 to 2 weeks
after injury, after the patient has been placed in a hanging arm cast
or coaptation splint and swelling has subsided. -
It consists of an anterior and posterior shell held together with Velcro straps.
-
Success depends on an upright patient and brace tightening daily.
-
Contraindications include massive soft
tissue injury, an unreliable patient, and an inability to obtain or
maintain acceptable fracture reduction. -
A collar and cuff may be used to support the forearm, but sling application may result in varus angulation.
-
The functional brace is worn for a minimum of 8 weeks after fracture or until radiographic evidence of union.
-
Operative
-
Indications for operative treatment are:
-
Multiple trauma
-
Inadequate closed reduction or unacceptable malunion
-
Pathologic fracture
-
Associated vascular injury
-
“Floating elbow”
-
Segmental fracture
-
Intraarticular extension
-
Bilateral humeral fractures
-
Open fracture
-
Neurologic loss following penetrating trauma
-
Radial nerve palsy after fracture manipulation (controversial)
-
Nonunion
P.176 -
-
Surgical approaches to the humeral shaft include:
-
Anterolateral approach: preferred for
proximal third humeral shaft fractures; radial nerve identified in the
interval between the brachialis and brachioradialis and traced
proximally. This can be extended proximally to the shoulder or distally
to the elbow. -
Anterior approach: muscular interval between the biceps and brachialis muscles.
-
Posterior approach: provides excellent
exposure to most of the humerus, but cannot be extended proximally to
the shoulder; muscular interval between the lateral and long heads of
the triceps.
-
Surgical Techniques
OPEN REDUCTION AND PLATE FIXATION
-
This is associated with the best
functional results. It allows direct fracture reduction and stable
fixation of the humeral shaft without violation of the rotator cuff. -
Radiographs of the uninjured, contralateral humerus may be used for preoperative templating.
-
A 4.5-mm dynamic compression plate with fixation of eight to ten cortices proximal and distal to the fracture is used.
-
Lag screws should be utilized wherever possible.
-
One should preserve soft tissue attachments to butterfly fragments.
INTRAMEDULLARY FIXATION
-
Indications include:
-
Segmental fractures in which plate placement would require considerable soft tissue dissection.
-
Humerus fractures in extremely osteopenic bone.
-
Pathologic humerus fractures.
-
-
It is associated with a high incidence of shoulder pain following antegrade humeral nailing.
-
Two types of intramedullary nails are available for use in the humeral shaft: flexible nails and interlocked nails.
-
Flexible nails
-
Rationale: Fill the canal with multiple nails to achieve an interference fit.
-
These nails have relatively poor stability.
-
Use should be reserved for humeral shaft fractures with minimal comminution.
-
-
Interlocked nails
-
These nails have proximal and distal interlocking capabilities and are able to provide rotational and axial fracture stability.
-
With antegrade nailing, the axillary
nerve is at risk for injury during proximal locking screw insertion.
Screws protruding beyond the medial cortex may potentially impinge on
the axillary nerve during internal rotation. Anterior to posterior
screws are avoided because of the potential for injury to the main
trunk of the axillary nerve. -
Distal locking usually consists of a
single screw in the anteroposterior plane. Distal locking screw can be
inserted anterior to posterior or posterior to anterior via an open
technique to minimize the risk of neurovascular injury. Lateral to
medial screws risk injury to lateral antebrachial cutaneous nerve.
P.177 -
-
Either type of nails can be inserted through antegrade or retrograde techniques.
-
If antegrade technique is elected, most methods attempt to avoid the rotator cuff to minimize postoperative shoulder problems.
-
The proximal aspect of the nail should be countersunk to prevent subacromial impingement.
EXTERNAL FIXATION
-
Indications include:
-
Infected nonunions.
-
Burn patients with fractures.
-
Open fractures with extensive soft tissue loss.
-
-
Complications include pin tract infection, neurovascular injury, and nonunion.
Postoperative Rehabilitation
Range-of-motion exercises for the hand and wrist should
be started immediately after surgery; shoulder and elbow range of
motion should be instituted as pain subsides.
be started immediately after surgery; shoulder and elbow range of
motion should be instituted as pain subsides.
COMPLICATIONS
-
Radial nerve injury occurs in up to 18% of cases.
-
It is most common with middle third
fractures, although best known for its association with Holstein-Lewis
type distal third fracture, which may entrap or lacerate the nerve as
it passes through the intermuscular septum. -
Most injuries are neurapraxias or
axonotmesis; function will return within 3 to 4 months; laceration is
more common in open fractures or gunshot injuries. -
With secondary palsies that occur during
fracture reduction, it has not been clearly established that surgery
will improve the ultimate recovery rate compared with nonsurgical
management. -
Delayed surgical exploration should be
done after 3 to 4 months if there is no evidence of recovery by
electromyography or nerve conduction velocity studies. -
Advantages of late over early nerve exploration:
-
-
Vascular injury: This is uncommon but may
be associated with fractures of the humeral shaft lacerating or
impaling the brachial artery or with penetrating trauma.-
The brachial artery has the greatest risk for injury in the proximal and distal third of arm.
-
It constitutes an orthopaedic emergency;
arteriography is controversial because may prolong time to definitive
treatment for an ischemic limb. -
Arterial inflow should be established within 6 hours.
-
At surgery, the vessel should be explored and repaired and the fracture stabilized.
-
If limb viability is not in jeopardy, bone repair may precede vascular repair.
-
External fixation should be considered an option.
-
-
Nonunion occurs in up to 15% of cases.
-
Risk factors include fracture at the
proximal or distal third of the humerus, transverse fracture pattern,
fracture distraction, soft tissue interposition, and inadequate
immobilization. -
It may necessitate open reduction and internal fixation with bone grafting
-
-
Malunion: This may be functionally
inconsequential; arm musculature and shoulder, elbow, and trunk range
of motion can compensate for angular, rotational, and shortening
deformities.
