Congenital Deformities
orthopaedics includes the surgeon’s demeanor, which has often been
called “bedside manner.” The evaluation and treatment of congenital
deformities requires the appropriate application of both science and
art in order to effectively deal with an infant or child with a
congenital deformity, or with his or her parents and extended family.
We live in a society where physical perfection is highly valued, so the
words of Robert E. Carroll in 1989 bear repeating:
scrutiny: the face and the hands. These areas are rarely covered, and
are perceived as symbolic of the individual. Furthermore, they are very
sensitive areas used for communication. Since there is constant
awareness of these two body areas, what can be more important than the
functional and esthetic restoration of the upper extremities? The
management of these complex problems carries with it both great
responsibility and rewards.”
frustration, fear, and rejection. The initial doctor visit or
evaluation is often associated with anxiety or even guilt, which can
alter what might be considered normal responses in other medical
situations. Upper limb deformities are very noticeable and are
difficult to conceal. This often worsens the deformity’s social or
emotional impact on the patient and family.
support and information. Positive comments about other physical
attributes of the child are helpful to the parents and to the patient.
Your projection of a caring and accepting caregiver will do much to
help the parents along their difficult path of acceptance of the
deformity. Information about support groups will be helpful to the
family. Upper extremity surgeons will need to offer more than technical
expertise; they will need to become part of a team of thoughtful and
experienced professionals including pediatricians, geneticists, and
social workers. Finally, the use of inappropriate descriptive and
potentially offensive terms such as lobster claw hand or club hand
should be abandoned. A suitable and internationally accepted system of
classification and nomenclature has been developed and is best used to
write and speak about these deformities. Some have proposed that
“congenital differences” is a more appropriate descriptive phrase than
“congenital deformities.”
upper limb is necessary to exchange ideas and concepts for diagnosing
and treating them. The currently accepted classification system is
given in Box 2-1. It is based on embryonic failure during development
and relies on clinical diagnosis for placement of the various and most
prominent anomalies. This system has been revised and adopted by the
Congenital Anomalies Committee of the International Federation of
Societies for Surgery of the Hand (IFSSH). Although no classification
system is perfect, the current system is the best that exists at this
time and is used worldwide. It has also been observed that research on
embryogenesis has rendered some of the information outdated regarding
pathogenesis of limb malformations used in this classification.
Although many investigators have expressed difficulties in classifying
specific anomalies in this system, it has provided a framework for
discussion. Central deficiencies (cleft hand) and brachysyndactyly,
along with ulnar deficiencies in particular, have provided areas of
controversy since the original classification system was adopted, but
it is beyond the scope of this text to further define them. Defects in
human limb formation have been connected to gene mutations that may
encode signaling proteins, transcription factors, and receptor
proteins. Some limb defects have been mapped to a specific chromosomal
segment and molecular defect. Table 2-1 provides a currently available genetic classification.
wall. The transition from embryo to fetus occurs at about 8 weeks, and
is hallmarked by the appearance of the primary ossification center in
the proximal humerus. Embryogenesis is characterized by the appearance
of new organ systems and the fetal period by differentiation,
maturation, and enlargement of existing organs. The changes in the
early limb bud into the mature arm, forearm, and hand rely on four
interdependent developmental processes: morphogenesis (the process by which a part assumes a particular shape); cell differentiation (the process by which individual cells, under genetic control, become specialized for carrying out specific functions); pattern formation (the process by which cellular differentiation is spatially organized); and growth (the enlargement of the structure reflecting both cell proliferation and matrix elaboration).
-
Failure of formation of parts (arrest of development)
-
Transverse arrest
-
Shoulder
-
Arm
-
Elbow
-
Forearm
-
Wrist
-
Carpal
-
Metacarpal
-
Phalanx
-
-
Longitudinal arrest
-
Radial ray deficiency
-
Ulnar ray deficiency
-
Central ray deficiency
-
Intersegmental deficiency (phocomelia)
-
-
-
Failure of differentiation of parts
-
Soft-tissue involvement
-
Disseminated
-
Arthrogryposis
-
-
Shoulder
-
Elbow and forearm
-
Wrist and hand
-
Cutaneous syndactyly
-
Camptodactyly
-
Thumb-in-palm deformity
-
Deviated/deformed digits
-
-
-
Skeletal involvement
-
Shoulder
-
Elbow
-
Elbow synostosis
-
-
Forearm
-
Proximal radioulnar synostosis
-
Distal radioulnar synostosis
-
-
Wrist and hand
-
Osseous syndactyly
-
Synostosis of carpal bones
-
Symphalangia
-
Clinodactyly
-
-
-
Congenital tumorous conditions
-
Hemangiotic
-
Lymphatic
-
Neurogenic
-
Connective tissue
-
Skeletal
-
-
-
Duplication
-
Whole limb
-
Humeral segment
-
Radial segment
-
Ulnar segment
-
Mirror hand
-
-
Digit
-
Polydactyly
-
Radial (preaxial)
-
Central
-
Ulnar (postaxial)
-
-
-
-
Overgrowth
-
Whole limb
-
Partial limb
-
Digit
-
Macrodactyly
-
With fibrolipoma of nerve
-
No fibrolipoma of nerve
-
-
-
-
Undergrowth
-
Whole limb
-
Whole hand
-
Metacarpal
-
Digit
-
Brachysyndactyly
-
Brachydactyly
-
-
-
Congenital constriction band syndrome
-
Generalized skeletal abnormalities
-
Chromosomal
-
Madelung’s deformity
-
-
from Kozin, S. Congenital anomalies. In: Trumble T, ed. Hand surgery
update 3, hand, elbow and shoulder. Rosemont, IL: American Society for
Surgery of the Hand, 2003:603–604.
The upper limb develops from the arm bud, which is an outgrowth from
the ventrolateral body wall located opposite the fifth through seventh
cervical somites. The arm bud first appears at approximately 26 to 27
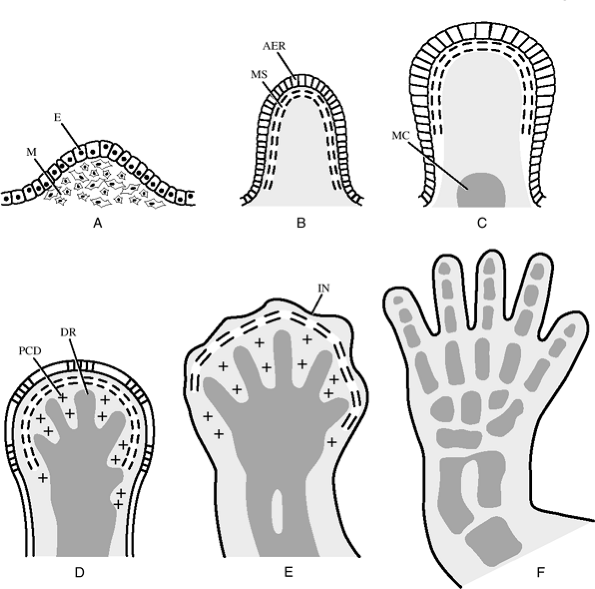
days of gestation (3 to 5 mm crown-rump length; Table 2-2 and Fig. 2-1).
Development in the arm bud occurs from proximal to distal and is
composed of a mass of somatic mesoderm-derived mesenchyme covered by
ectoderm. As the arm bud grows, it assumes a flipper-like shape. At day
33, blood circulation is established to the paddle-like arm bud.
grow into the limb from proximal to distal. At 5 weeks, a constriction
demarcates the arm from the forearm. A more proximal depression will
become the axillary fossa. At 41 to 43 days (11 to 14 mm crown-rump
length), the finger rays appear. At 50 days, individual digital
metacarpal and phalangeal mesenchymal condensations are histologically
visible. At day 52 or 53 (22 to 24 mm crown-rump length), the fingers
are entirely separate. In the seventh week, the upper limb rotates 90
degrees on its longitudinal axis, so that the elbow points dorsally.
Embryogenesis ends during the eighth week.
|
Table 2-1 Genetic Classification of Limb Defects
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Table 2-2 Streeter Stages of Human Embryonic Development
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 |
|
Figure 2-1 Normal limb bud development. (A) At 28 days. (B) At 34 days. (C) At 36 days. (D) At 40 days with programmed cell death of mesenchymal tissue between digital ray mesenchymal condensations. (E) At 42 days. (F)
At 50 days showing individual digits and well-defined web spaces. AER, apical ectodermal ridge; DR digital ray; E, ectoderm; IN, interdigital notch; M, mesoderm; MC, mesenchymal condensation; MS, marginal sinus; PCD, physiologic cell death. (Taken from Yasuda M. Pathogenesis of preaxial polydactyly of the hand in human embryos. J Embryo Exp Morph 33:745–756, 1975.) |
is between the mesenchyme of the limb bud and the apical ectodermal
ridge (AER). This interaction influences and guides proximal to distal
axis limb differentiation, and is the process that distinguishes the
arm from the forearm and the forearm from the hand. The second set of
interactions controls differentiation along the dorsal to palmar axis,
the distinction between the dorsum of the finger with a fingernail, and
the soft tissue of the pulp. The third set of interactions controls
cellular differentiation across the anteroposterior (AP) axis and
causes the thumb to assume a morphologic form distinctly different from
the little finger.
or control outgrowth and pattern formation are the AER, the dorsal
ectoderm, and the zone of polarizing activity (ZPA). The dorsal
ectoderm controls palmar to dorsal differentiation, which results in
distinctly different flexor and extensor surfaces.
a cluster of mesenchymal cells along the postaxial border of the limb
bud, the zone of polarizing activity (ZPA). The morphogens elaborated
within the ZPA diffuse and create a gradient that helps control
differentiation in the AP plane. Retinoids are vitamin A-derived
substances that may signal digital differentiation from the polarizing
region.
of the limb bud that is present during critical transitions in limb
development. The AER induces the differentiation of the underlying
mesoderm. The mesoderm elaborates morphogens that maintain the AER. The
progress zone is a region of subectodermal mesoderm that defines
proximodistal relationships. The theory of positional information
suggests that the ultimate role or position of an individual cell is
determined by the length of time that a cell spends in the progress
zone, and by the number of times the cell undergoes mitosis before
exiting from the progress zone. These interactions are critical for
coordinating limb pattern formation.
cell death, is an integral element of orderly limb embryogenesis. The
resorption of tissue between the digital mesenchymal condensations
results from the release of lysosomal enzymes from cells. The
antichondrogenic effects of the ectoderm and digital cartilage inhibit
interdigital mesenchymal cells from forming cartilage. As those
interdigital cells migrate toward digital condensations to participate
in chondrogenesis, the interdigital zone experiences a decrease in cell
density and cell death.
the development of the limbs, and help regulate the timing and extent
of local growth rates within the embryonic limb. Mutation in the HoxDl3
position has been demonstrated to lead to human synpolydactyly
deformities in the hands and feet. Three proteins (Sonic hedgehog
[Shh], FGFs, and Wnt-7a) are believed to establish the pattern of Hox
gene expression. The Hox code, in conjunction with other gene products,
is thought to provide more detailed positional and morphogenic
information to competent mesenchymal cells, enabling them to form
precartilaginous skeletal cell condensations of appropriate size and at
appropriate sites.
embryogenesis, and limbs grow rapidly during fetal development. Areas
of cartilage are replaced by expanding primary ossification centers,
and joints move in utero in response to muscle contraction
Initial behaviors are shaped by subcortical reflexes. By the end of the
first year of life, the child begins to purposefully manipulate
objects, using his or her hands in a coordinated fashion. Hand
preference or dominance is evident by 3 or 4 years of age
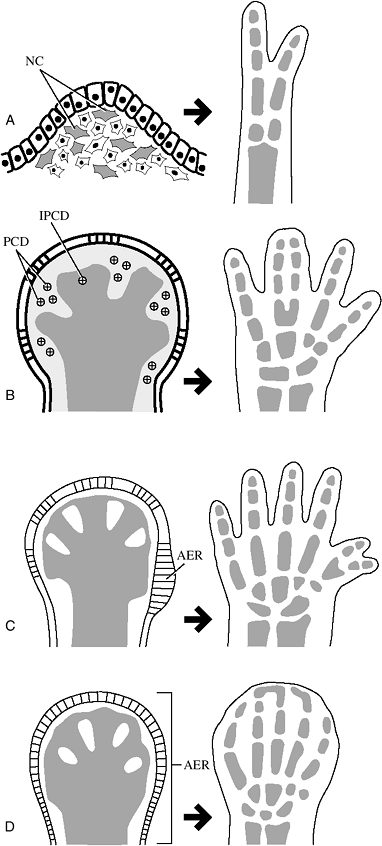
between the AER and the underlying mesoderm. Syndactyly represents the
failure of the normal separation of the digital rays from one another.
When there is a failure of the normal interdigital programmed cell
death, interdigital webbing will persist as syndactyly (Fig. 2-2).
 |
|
Figure 2-2 Pathogenesis of limb deformities. (A) Mesenchymal cell death leads to a reduction deformity of the hand. (B) Failure of cell death results in syndactyly of adjacent digits. (C) Polydactyly results from hyperplasia of the apical ectodermal ridge (AER). (D)
Disrupted ridge metabolism that results in failure of breakdown of the AER may result in complete complex syndactyly. AER, apical ectodermal ridge; IPCD, inhibited physiologic cell death; NC, necrotic cells; PCD, physiologic cell death. |
digital rays, reflecting an abnormality in the interaction between limb
bud ectoderm and mesoderm. Thumb polydactyly may be related to
prolonged ectodermal cells in the tip of the limb bud that induce an
abnormal notch in the radial mesenchymal tissue. Studies have shown
that implantation on the anterior side of the limb bud of FGF-soaked
beads or of portions of the ZPA will result in a mirror duplication of
the limb. In some instances, an inappropriate number of digital
condensations are formed. In other instances of polydactyly, one of the
five digital condensations becomes partially split longitudinally.
Digital definition occurs as the process of interdigital apoptosis
defines separate rays. If this process occurs in an abnormal location,
further splitting of the hand plate results in polydactyly.
of local injury or ischemia. The resulting hand may have a
corresponding area of dysplasia or deficiency. It has been suggested on
the basis of experimental studies that disruption of the AER may lead
to transverse defects, whereas loss of cells in the mesenchyme may
result in longitudinal deficiency patterns. Poland’s association, the
occurrence of brachysyndactyly with absence of the sternal costal
portion of the pectoralis major, may be related to unilaterally
diminished vascular flow.
potential effect of drug ingestion on limb morphogenesis. Thalidomide
was marketed outside the United States in the late 1950s for the
treatment of nausea associated with pregnancy. Administration of these
drugs to pregnant rats has been demonstrated to result in fetal
anomalies. The specific anomalies are related to the dose and timing of
the drug administration.
congenital constriction band syndrome, is usually the result of
intrauterine injury to a normally developed hand. In response to the
altered intrauterine environment, the fetus may be deformed, as fingers
are forced together to create a secondary syndactyly. The mechanical
constriction of amniotic tissue may disrupt or amputate fingers or toes.
clinical facts about some of the more common congenital anomalies based
on the currently accepted classification system. Not all of the
conditions listed in Box 2-1 will be presented.
longitudinal. Transverse failure is represented by congenital
amputation that may occur from the shoulder region to the phalanx.
Longitudinal failure of development is characterized by radial,
central, ulnar or intersegmental deficiency. Examples of these
deformities are complete or partial absence of the radius, cleft hand,
complete or partial absence of the ulna, and phocomelia.
 |
|
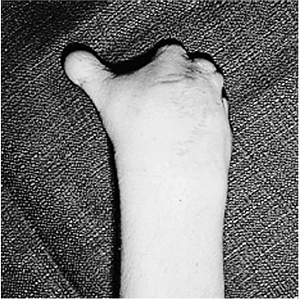
Figure 2-3 An example of transverse arrest at the metacarpal level.
|
demonstrates the appearance of a transverse arrest at the level of the
metacarpal region. The condition is believed to be associated with
severe hemorrhage in the hand plate. These deficiencies differ from
constriction ring amputations in that the proximal parts are
hypoplastic and the amputation is usually at or near a joint.
-
Treatment of arm and forearm amputations
involves prosthetic fitting of a dynamic or static device depending on
the age of the patient and level of the amputation. -
Transcarpal deficiency and foreshortened fingers (nubbins) are often present.
-
A palmar splint may provide rudimentary prehension.
-
Digital lengthening of one or more digits may be considered.
-
Separation of the radius and ulnar to
form prehensile appendages may be considered in bilateral transverse
arrest, especially if it is associated with visual impairment.
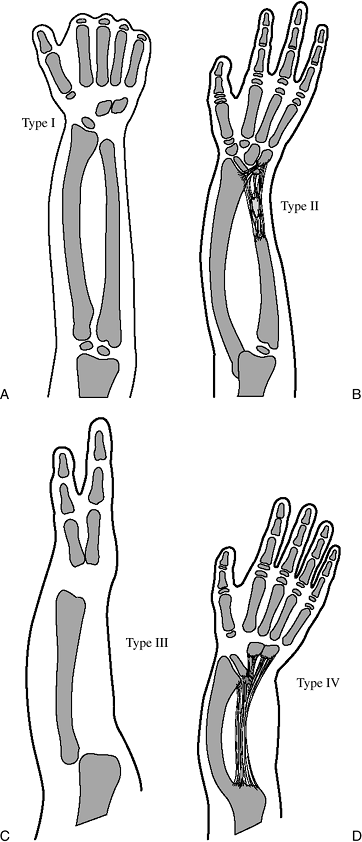
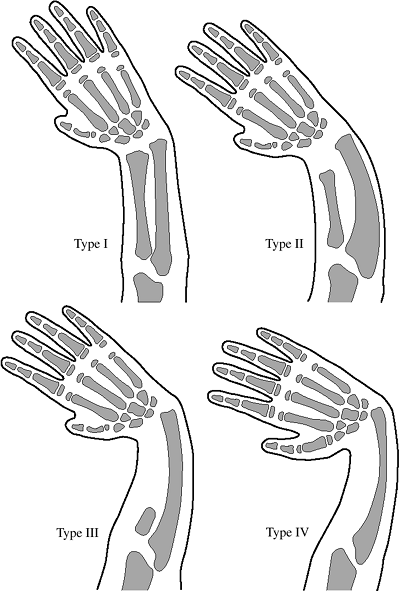
hypoplasia of the radius. Four types have been classified and are described in Table 2-3.
A more recent and global classification of radial longitudinal
deficiency that includes carpal and thumb anomalies is presented in Table 2-4. The x-ray appearance of the four types listed in Table 2-3 is depicted in Figure 2-4.
Ossification of the radius is delayed in radial deficiency and the
differentiation between types III and IV may not be established until 3
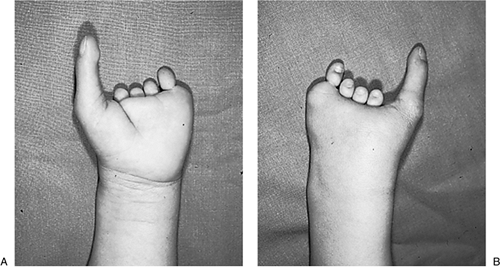
years of age. The clinical appearance of a type III patient is seen in Figure 2-5. Syndromes associated with radial deficiency are presented in Table 2-5.
|
Table 2-3 Radial Deficiency Classification
|
||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||
-
Treatment is aimed at improvement of
appearance by correcting the radial deviation of the wrist, balancing
the hand and wrist on the forearm, maintaining and improving wrist and
finger motion, promoting growth of the forearm, and improving overall
function of the upper extremity. -
This can be achieved by stabilizing the
carpus on the end of the ulna by centralization or ulnocarpal fusion.
This can be achieved with or without ulnar osteotomy and/or tendon
transfers. -
These procedures work best in children, because functional patterns developed over many years in adults are best left unaltered.
-
The radial deviation deformity allows the
hand to reach the mouth. Bilateral conditions associated with
non-correctable stiff elbows should have only one side corrected. -
Surgery is most often needed in types II to IV.
|
Table 2-4 Global Classification of Radial Longitudinal Deficiency
|
||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||
is based on the status of the ulna and the humeral articulation. A more
recent classification system based on the characteristics of
the
thumb and first web has been advocated due to the fact that most
surgeries for this condition involved the thumb and first web (Table 2-7).
 |
|
Figure 2-4 The osseous appearance of the four types of radial deficiency: type I, type II, type III, and type IV. See Tables 2-2 and 2-3 for details.
|
-
Principles of treatment include splinting
to correct any significant ulnar deviation of the wrist and early
excision of the fibrous anlage of the ulna if it is not possible to
correct the ulnar deformity of the wrist. -
The radial head may be excised in those patients with minimal forearm rotation and elbow movement.
-
Creation of a one-bone forearm using the proximal ulna and the distal radius may be indicated.
-
Hand function may be significantly
improved by corrective surgery to the thumb and first web when there is
web deficiency, absence of the thumb or thumb hypoplasia, malposition,
and loss of opposition.
-
Typical cleft hand represents dysplasia
of the central portion of the hand, and is not seen in conjunction with
forearm or elbow anomalies. -
The deformity is characterized by a
V-shaped cleft in the central aspect of the hand that may be associated
with absence of one or more digits. -
Syndactyly may occur in the adjacent digits. The first web space may be compromised.
-
Transverse bones may be noted on an
x-ray, and there may be an absence of multiple digits with only one
digit present (usually the little finger). -
Some cleft hands may be caused by the split hand/split foot gene localized on chromosome 7q21; see Table 2-1.
-
Treatment of cleft hands should improve
any compromise of the first web space, close the cleft, and correct the
syndactyly if present. -
Cleft closure may be achieved by transposition or translocation of the appropriate ray.
-
In cases without a thumb, rotation of a radial ray, if present, should be considered.
likeness to a seal limb, is distinguished from transverse deficiencies
because of the presence of digital structures. Three types have been
identified based on the presence or absence of an intermediate segment
between the shoulder and hand. In type A, the hand is attached to the
trunk, and there are no limb bones; type B is characterized by the
absence or significant hypoplasia of the humerus so that the hand is
attached to the trunk by the forearm; type C is characterized by
absence of the forearm, with the hand attached to the humerus.
Prosthetic or orthotic devices may be useful.
there are multiple forms of this disorder, the one most likely to be
encountered on an orthopaedic service is known as amyoplasia congenita,
or arthrogryposis.
-
The classic patient with arthrogryposis
demonstrates adduction and internal rotation of the shoulders, extended
elbows, and pronated forearms.P.22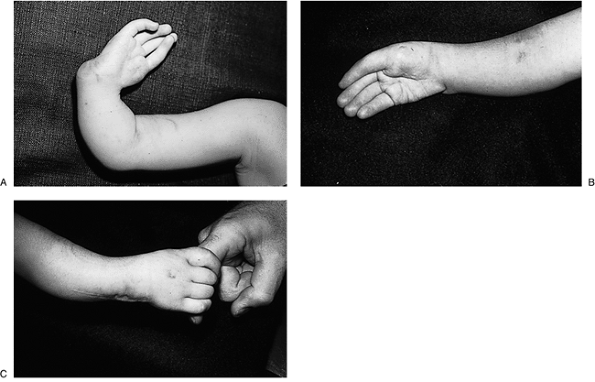 Figure 2-5 Type III radial deficiency. (A) Preoperative appearance. (B) Postoperative appearance following transposition of the ulna. (C) Improved appearance and function.Table 2-5 Syndromes Associated With Radial Deficiency
Figure 2-5 Type III radial deficiency. (A) Preoperative appearance. (B) Postoperative appearance following transposition of the ulna. (C) Improved appearance and function.Table 2-5 Syndromes Associated With Radial DeficiencySyndrome Characteristics Holt-Oram Heart defects, most commonly cardiac septal defects TAR Thrombocytopenia Absent Radius syndrome. Thrombocytopenia present at birth, but improves over time. VACTERL Vertebral abnormalities, Anal atresia, Cardiac abnormalities, Tracheoesophageal fistula, Esophageal atresia, Renal defects, Radial dysplasia, Lower limb abnormalities Fanconi’s anemia Aplastic anemia not present at
birth, develops at about 6 years of age. Fatal without bone marrow
transplant. Chromosomal challenge test now available for early
diagnosis.Taken
from Kozin, S. Congenital anomalies. In: Trumble T, ed. Hand surgery
update 3, hand, elbow and shoulder. Rosemont, IL: American Society for
Surgery of the Hand, 2003:610.Table 2-6 Classification of Ulnar DeficienciesType Grade Characteristics I Hypoplasia Hypoplasia of the ulna with presence of distal and proximal ulnar epiphysis, minimal shortening II Partial aplasia Partial aplasia with absence of the distal or middle one-third of the ulna III Complete aplasia Total agenesis of the ulna IV Synostosis Fusion of the radius to the humerus Taken
from Kozin, S. Congenital anomalies. In: Trumble T, ed. Hand surgery
update 3, hand, elbow and shoulder. Rosemont, IL: American Society for
Surgery of the Hand, 2003:608. -
The wrists are palmar flexed and the hands ulnar deviated. The fingers are flexed and stiff. The thumb is flexed into the palm.
-
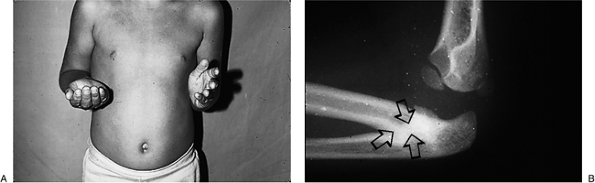
This classic posture is demonstrated in Figure 2-9.
-
As with all congenital anomalies, treatment is directed toward the individual needs of each patient.P.23
![]() Figure 2-6 The four types of ulnar deficiency: type I, type II, type III, and type IV. See Table 2-6 for details.
Figure 2-6 The four types of ulnar deficiency: type I, type II, type III, and type IV. See Table 2-6 for details. -
The classic treatment goals include
independent toilet (perineal care) and self-feeding. In general, toilet
care requires an extended elbow; self-feeding requires some degree of
elbow flexion. -
Early treatment is directed at passive
movement and static progressive splinting of joints to promote what
function may be present and as a useful precursor to surgical
intervention in the form of joint releases and tendon transfers.Table 2-7 Classification of Ulnar Deficiency According to First-Web Space AbnormalityType Grade Characteristics A Normal Normal first web space and normal thumb B Mild Mild first web deficiency and mild thumb hypoplasia, with intact opposition and extrinsic tendon function. C Moderate to severe Moderate-to-severe first web
deficiency and similar thumb hypoplasia with malrotation into the plane
of the digits, loss of opposition, and dysfunction of the extrinsic
tendonsD Absent Absence of the thumb Taken
from Kozin, S. Congenital anomalies. In: Trumble T, ed. Hand surgery
update 3, hand, elbow and shoulder. Rosemont, IL: American Society for
Surgery of the Hand, 2003:608. -
Many of these children develop “trick
motions” to meet their functional needs, and surgical intervention must
be calculated to improve and not diminish function. -
Tendon transfers such as triceps to
biceps, and pectoralis major or latissimus dorsi to the front of the
elbow, can restore active elbow flexion if a suitable muscle is
available for transfer. -
A recent study of various transfers to achieve elbow flexion revealed the following:
-
Exercises to obtain and maintain passive elbow flexion are initiated at birth.
-
If at least 90 degrees of flexion has not
been achieved by 18 to 24 months of age after at least 6 months of
supervised therapy, an elbow capsulotomy with triceps lengthening is
recommended. Figure 2-7 Clinical appearance of a true cleft hand deformity.P.24
Figure 2-7 Clinical appearance of a true cleft hand deformity.P.24![]() Figure 2-8 Clinical appearance of an atypical cleft hand or brachysyndactyly.
Figure 2-8 Clinical appearance of an atypical cleft hand or brachysyndactyly. -
After the age of 4 years, tendon
transfers for elbow flexion on the dominant arm are recommended with
triceps to biceps transfer giving the most predictable results. -
The muscle to be transferred should have muscle strength of at least grade 4.
-
-
A persistent wrist flexion deformity may
require surgical intervention. A proximal row carpectomy may be
beneficial in mild to moderate deformities, but more severe flexion
deformities may require a dorsal wedge mid-carpal osteotomy, along with
a central transfer of the extensor carpi ulnaris (ECU) to help the
wrist extend.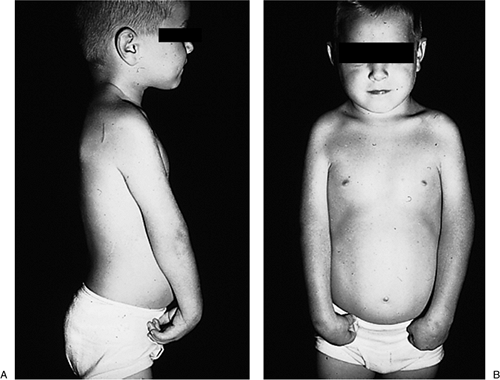 Figure 2-9 Clinical appearance of arthrogryposis in the upper extremities.Table 2-8 Clinical Features of Typical Cleft Hand and Atypical Cleft Hand
Figure 2-9 Clinical appearance of arthrogryposis in the upper extremities.Table 2-8 Clinical Features of Typical Cleft Hand and Atypical Cleft HandTypical Cleft Hand Atypical Cleft Hand (Brachysyndactyly) Familial, Autosomal dominant Sporadic, spontaneous 1–4 limbs involved 1 limb involved (no feet) V-shaped cleft U-shaped cleft No finger “nubbins” Finger “nubbins” may occur Syndactyly (especially first web) Unusual Bilateral Unilateral -
The palm-clutched thumb may be repositioned, and the fingers realigned, by osteotomy.
inheritable, or associated with a syndrome. The conditions currently
known to be associated with syndactyly are given in Box 2-2.
Inheritable syndactyly is associated with genetic defects on certain
regions of the second chromosome
(2q34–q36).
The mode of inheritable transmission is said to be autosomal dominant,
with variable expressivity and incomplete penetrance.
-
Trisomy 13
-
Trisomy 14
-
Trisomy 21
-
Partial trisomy 10q
-
Triploidy syndrome
-
Aglossia adactylia syndrome
-
Apert syndrome
-
Carpenter syndrome
-
Pfeiffer syndrome
-
Cohen syndrome
-
Cryptophthalmos syndrome
-
Ellis-van Creveld syndrome
-
Familial static Ophthalmoplegia syndrome
-
Glossopalatine ankylosis syndrome
-
Greig cephalopolysyndactyly syndrome
-
Hanhart syndrome
-
Hypertelorism and syndactyly syndrome
-
Möbius syndrome
-
Noack syndrome
-
Oculodentodigital
-
Oculomandibulofacial syndrome
-
Oral-facial-digital
-
Oto-palato-digital
-
Pierre-Robin
-
Saethre-Chotzen
-
Acropectoral-vertebral dysplasia-F-form (F syndrome)
-
Aarskog
-
Bloom syndrome
-
Brachydactyly A-2
-
Brachydactyly B
-
Chondrodysplasia punctata (Conradi) syndrome
-
Cornelia de Lange syndrome
-
EEC syndrome
-
Escobar syndrome
-
Fraser syndrome
-
Goltz focal dermal hypoplasia syndrome
-
Holt-Oram syndrome
-
Incontinentia pigmenti syndrome
-
Jarcho-Levin syndrome
-
Lawrence-Moon-Biedl syndrome
-
Lacrimoauriculodentodigital syndrome
-
Lenz-Majewski hyperostosis syndrome
-
Lenz microphthalmia syndrome
-
McKusick-Kaufman syndrome
-
Meckel syndrome
-
Miller syndrome
-
Neu-Laxova syndrome
-
Pallister-Hall syndrome
-
Pancytopenia dysmelia syndrome
-
Poland’s anomaly
-
Popliteal pterygium syndrome
-
Prader-Willi syndrome
-
Roberts-SC phocomelia syndrome
-
Rothmund-Thomson syndrome
-
Sclerostenosis syndrome
-
Scott craniodigital mental retardation syndrome
-
Short rib-polydactyly (Saldino-Noonan) syndrome
-
Smith-Lemli-Opitz syndrome
-
Spondylothoracic dysplasia syndrome
-
Summit syndrome
-
Thrombocytopenia-absent radius syndrome
-
Wardenberg syndrome
from Ezaki MB. Syndactyly. In: Green DP, Hotckiss RN, Pederson WC, eds.
Green’s operative hand surgery. 4th Ed. New York: Churchill
Livingstone, 1999:414–428.
In incomplete syndactyly, the interdigital web is extended, but soft
tissue union does not extend as far as the distal aspect of the digits.
Simple syndactyly involves only the skin and underlying soft tissues,
whereas complex syndactyly also manifests some form of union of the
underlying osseous terminal phalanx. Another classification system has
been developed to guide the timing and extent of separation (Table 2-9).
This system indicates the value of early (the first few months of life)
separation of border digits (thumb-index and ring-little finger web
space) or digits with marked differences in length. Separation prevents
tethering of the longer digit and may prevent flexion contracture or
rotational deformity. Surgery after 18 months of age has a lower
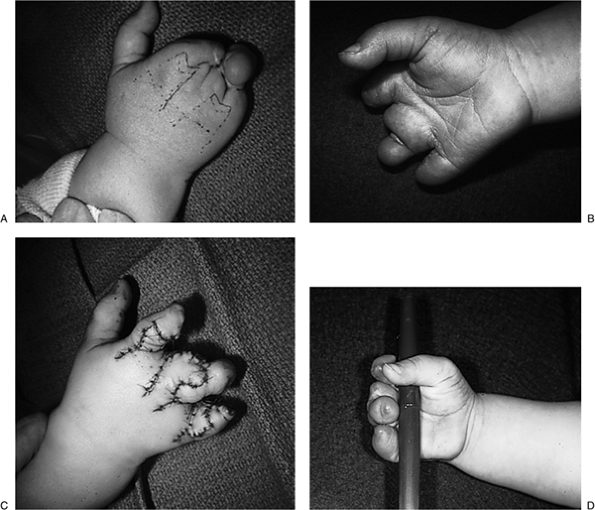
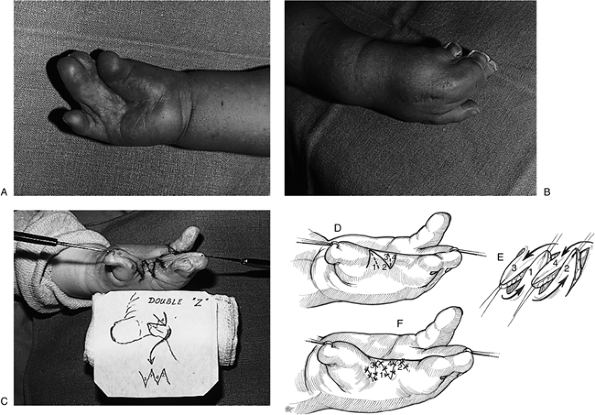
incidence of complications such as web advancement. Figure 2-10 shows a case of complete, simple syndactyly, and Figure 2-11 is an example of complex syndactyly as seen in Apert’s syndrome.
-
The most common site of webbing is between the middle and ring finger.
-
Differential motion between the fingertips in complete syndactyly indicates absence of bony involvement.
-
Confluence of the nails (synechia) or the
absence of differential motion is most often associated with bony
involvement as seen in complex syndactyly. -
Radiographs are an important part of the
evaluation of syndactyly. They assist in differentiating between
complex and simple syndactyly and in noting the presence or absence of
a hidden polydactyly. -
The interdigital web has unique anatomy:
-
It is a three-dimensional space that allows normal finger movement in more than four planes.
-
It slopes from proximal to distal as
viewed from the dorsal aspect of the hand. This slope is most
noticeable when the digits are extended and abducted. -
The web closes when the digits are flexed.
-
The web begins near the head of the metacarpal and ends near the mid-portion of the proximal phalanx.P.26Table 2-9 Syndactyly Classification
Type Description Simple syndactyly (SS) Standard (SSs) Straightforward, simple syndactyly of non-border digit. Surgery can be delayed until 18 months of age. Complicated (SSc) Simple syndactyly associated
with additional soft tissue interconnections, syndromes (such as
Poland’s syndrome or central deficiency), or abnormal bony elements
(such as hypoplasia). Treatment must be individualized. Beware of
neurovascular anomalies.Urgent (SSu) Soft tissue syndactyly of
borders digits or digits of unequal length, girth, or joint level.
Requires early separation to prevent angular and rotational deformity
of tethered digit.Complex syndactyly (CS) Standard (CSs) Complex syndactyly of adjacent phalanges without additional bony anomalies (such as delta phalanx or symphalangism). Complicated (CSc) Complex syndactyly associated
with additional bony interconnections, (such as transverse phalanges,
symphalangism, or polysyndactyly), or syndromes (such as constriction
band syndrome). Treatment must be individualized, and digits may
function better as a unit.Unachievable (CSu) Complex syndactyly with severe
anomalies of the underlying bony structures, which often prohibits
formation of a five-digit hand without extensive surgical intervention.Taken
from Kozin, S. Congenital anomalies. In: Trumble T, ed. Hand surgery
update 3, hand, elbow and shoulder. Rosemont, IL: American Society for
Surgery of the Hand, 2003:616. -
Transversely oriented natatory fibers of
the palmar fascia span the mid and distal aspects of the web, and are
important support structures for the overlying skin and subcutaneous
tissues.
-
-
The goals of treatment are to improve the overall appearance of the hand and to improve function.
-
Contraindications include any condition
that would preclude general anesthesia (in children), the lack of
adequate vascular supply, soft tissue insufficiency, or lack of a
potentially stable skeleton for each digit. -
Early separation at 4 to 6 months of age
is advised for complex syndactyly involving the border digits where
continued growth may be expected to cause tethering or progressive
deformity with growth. -
Surgery is technically easier, and anesthesia is safer, after 1 year of age.
-
Surgery is designed to try to reproduce
this three-dimensional space. Many methods have been designed to
achieve this, but the basic principles to achieve this goal are based
on the formation of a dorsally based flap that is advanced to the
palmar surface of the hand. The advancement will form a new web in
association with zigzag incisions that run distally from the web area
to the fingertips. -
The zigzag incisions are used to prevent a linear scar and its resultant contracture.
-
The triangular flaps thus formed are
applied to the opposing surfaces of the separated digits; the gaps that
inevitably result are covered with full thickness skin grafts from a
suitable donor site such as the hairless aspect of the groin. -
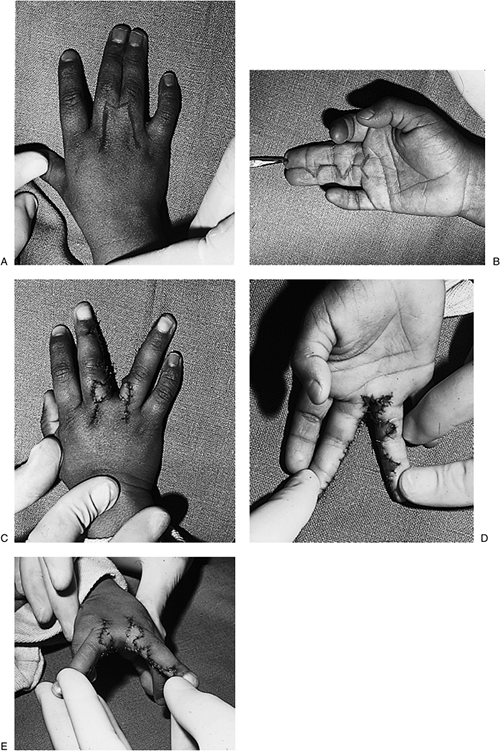
Figure 2-10 demonstrates the surgical technique used to separate a case of simple, complete syndactyly.
-
A four-tailed Z-plasty may also be used to deepen the first web, and is demonstrated in Figure 2-12.
flexion deformity of the proximal interphalangeal (PIP) joint of the
little finger. The term may be used less accurately to describe any
congenital flexion deformity of a digit. This deformity has been noted
in 70 or more syndromes.
-
The finger assumes variable degrees of
flexion contracture at the PIP joint. The neck and head of the proximal
phalanx at the PIP joint may be deformed. -
The clinical and x-ray appearance of the condition is presented in Figure 2-13.
-
The etiology is unknown, although various
anatomic abnormalities have been implicated, such as skin deficiency,
intrinsic and extrinsic tendon contracture, and abnormal insertions,
infection, and circulatory problems. -
Abnormalities of insertion and contracture are most commonly found in the superficialis and or the lumbrical.
-
Dynamic and static splinting may be useful if continued through adolescence.
 |
|
Figure 2-10
A case of simple, complete syndactyly showing the technique for release and web formation using a dorsal pantaloon flap developed by L.D. Howard. |
 |
|
Figure 2-11 An example of complex syndactyly as seen in Apert’s syndrome.
|
 |
|
Figure 2-12 (A–C) Clinical appearance of a child with Apert’s syndrome in which a 4-tailed Z-plasty was used to deepen the first web. (D–F) Details of surgical technique.
|
 |
|
Figure 2-13 Clinical appearance of camptodactyly.
|
-
Splinting is usually continued only at night once correction has been obtained.
-
Surgical intervention is not always
required. It is indicated for contractures of 30 degrees or more, or
those digits that have failed to improve with splinting. -
Corrective procedures for this condition
are quite variable, but the basic principles relate to the release of
the intrinsic or extrinsic contractures in and about the PIP joint. The
principles also relate to the rebalancing of any deforming forces. -
A full-thickness skin graft or local flap is usually required to treat the associated skin contracture.
is represented by synostosis. This condition may occur in the elbow,
forearm, wrist, and hand.
 |
|
Figure 2-14 (A) Clinical appearance of left sided forearm synostosis in a young child with the forearm fixed in neutral. (B) X-ray showing coalition of the proximal radius and ulna (arrows).
|
in three entities: as part of a systemic disorder manifested by
multiple synostosis; dysgenesis of the ulna; and as a part of ulnar
malformation and oligodactyly.
-
The position of the elbow may vary from
full extension to 90 degrees of flexion, and there may be associated
rotational deformities. -
Treatment for this rare condition is directed at improving the placement of the hand, which is sometimes directed posteriorly.
-
A derotational osteotomy may be useful.
-
The exact procedure to be utilized will
vary from patient to patient, depending on whether or not the condition
is bilateral or unilateral. -
The elbow is positioned to maximize hand function.
demonstrates the clinical and x-ray appearance of a unilateral forearm
synostosis in the left upper extremity, which is fixed in neutral
rotation.
-
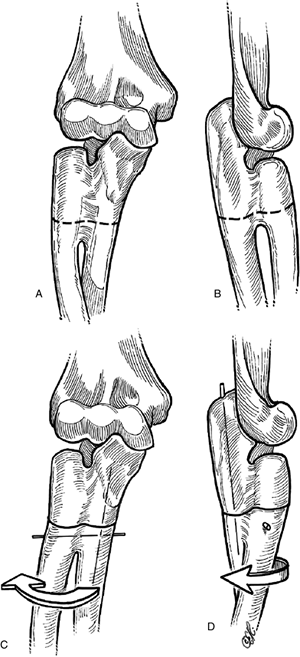
A proximal rotational osteotomy may be performed based on the functional needs of the patient (Figure 2-15).
In this patient, no treatment was required because the synostosis on
the left was in neutral, and the opposite extremity had full pronation
and supination.
little fingers, but may also present between the ring and middle finger
metacarpals. The most common form is represented by fusion of the ring
and little finger metacarpals, with abduction and hypoplasia of the
little finger.
 |
|
Figure 2-15
Surgical technique for proximal osteotomy in forearm synostosis after Green and Mital, showing a proximal osteotomy and reposition that is held in place by a longitudinal and a transverse K-wire through the synostosis mass. |
-
Indications for surgery include the need
to improve the appearance of the hand, but if severe little finger
abduction is present this may interfere with function as the little
finger may “catch” on things when the hand is used. -
Osteotomy and realignment are designed to improve both function and appearance.
 |
|
Figure 2.16 X-ray appearance of a luno-triquetral coalition in the wrist.
|
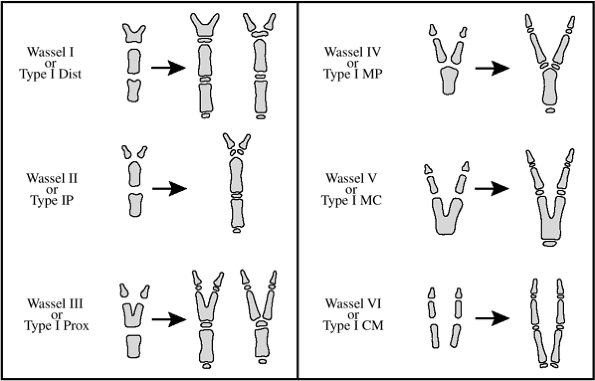
thumb polydactyly. The first was by Wassel and the second was by
Buck-Gramko and Behrens. Both systems classify the condition by the
extent of bifurcation of the thumb. A comparison of these two systems
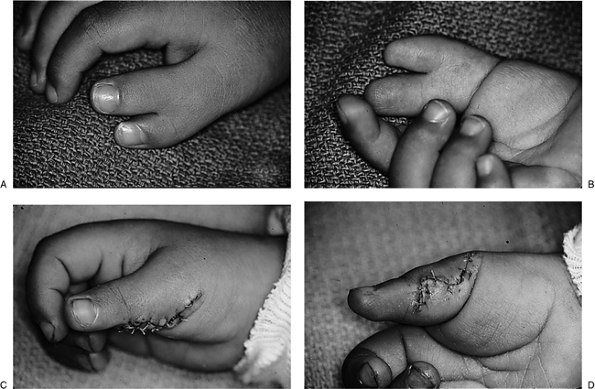
is given in Figure 2-17. Wassel type IV thumbs
are the most common. The preoperative and postoperative appearances of
a type IV thumb polydactyly are shown in Figure 2-18.
-
Central polydactyly may be present in one hand, while cleft hand is noted in the opposite extremity.
-
A radiograph is needed to adequately
diagnose the condition because the polydactylous digit may be concealed
within a syndactyly. -
Treatment varies with the form of polydactyly encountered, but the goal is improved function and appearance.
-
In some instances, separation or excision may result in lessened function and appearance.
-
The vascularity in synpolydacylous digits may be abnormal, and digital separation may be associated with digital ischemia.
-
Small digits with a narrow stalk may be ligated when seen in the newborn nursery. These digits will then necrose and fall off.
-
Small nubbins may be ignored or surgically removed.
-
More substantial and formed digits may require a more comprehensive approach to achieve better function and appearance.
 |
|
Figure 2-17
The classification systems for thumb polydactyly demonstrating the systems of Wassel and Buck-Gramcko and Behrens. The first column depicts immature thumbs, while the second shows maturing thumbs. The metacarpal or phalanges may partially or completely separate at the epiphysis, metaphysis, or diaphysis. (Taken from Light TR. Congenital anomalies: syndactyly, polydactyly and cleft hand. In: Peimer CA, ed. Surgery of the hand and upper extremity. New York: McGraw-Hill, 1996:2211–2144.) |
 |
|
Figure 2-18 The preoperative (A, B) and postoperative (C, D) appearance of a type IV thumb polydactyly treated by removal of the less dominant appendage.
|
 |
|
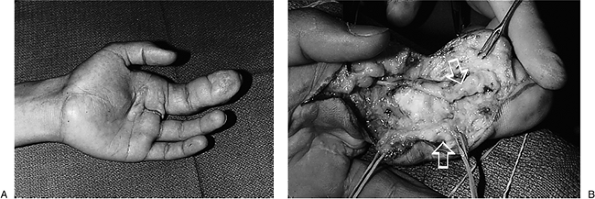
Figure 2-19 (A) Preoperative appearance of macrodactyly of the index finger (the middle finger was amputated previously; note scar). (B) Enlarged digital nerves (arrows) and generalized fibrofatty infiltration of the digit as seen at operation.
|
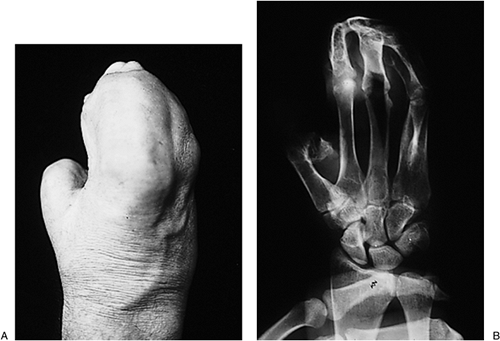
presents in two forms: static, with a single enlarged digit that is
present at birth and that grows proportionately to the other digits;
and progressive, with a digit that may not be enlarged at birth but
begins to enlarge in early childhood. Growth in digits with this
progressive type is much faster than the normal digits, and may
demonstrate angular deviation. The progressive type is more common.
-
The index finger is most commonly involved, and multiple digits are frequently involved.
![]() Figure 2-20 The clinical appearance of brachydactyly. Note the comparatively normal thumb, but the digits are represented as “nubbins.”
Figure 2-20 The clinical appearance of brachydactyly. Note the comparatively normal thumb, but the digits are represented as “nubbins.” -
Motion in the affected digits becomes diminished with age.
-
Phalangeal enlargement occurs in transverse and longitudinal axes.
-
The digital nerves are thickened by
fibrofatty tissue, which renders identifying the conducting or
functional portions of the nerve difficult. -
Both the median and ulnar nerve may enlarge proximal to the digital nerve involvement.
-
Treatment has included a variety of
debulking, shortening procedures, including epiphyseal plate excision
and osteotomies, to correct angular and rotational deformities. -
Another form of treatment is amputation, usually in the form of a ray amputation.
-
Amputation is often the last operation for a stiff, unsightly, and anesthetic digit.
-
Figure 2-19 shows a classic index finger macrodactyly.
metacarpal, or digits. Brachysyndactyly and brachydactyly (short
fingers with and without webbing, respectively) will be discussed. As
previously noted, these two conditions should not be confused with true
cleft hand. Table 2-8 lists the features that differentiate atypical and typical cleft hand.
-
The affected hand is smaller in patients with brachydactyly, which is a unilateral condition.
-
The thumb and little finger are often
present and the central digits are represented by “nubbins” of tissue
rather than fingers. Figure 2-20 depicts the clinical appearance of brachydactyly in a child.
-
-
Brachysyndactyly is similar to brachydactyly in that the condition is unilateral and the affected hand smaller.
-
The fingers are shorter than normal, and the webbing of the digits may be simple and incomplete, or complex.
-
Figure 2-21 is an example of brachysyndactyly as seen in Poland’s syndrome.
-
Figure 2-22 represents a more complex form of brachysyndactyly.
-
-
In brachydactyly, treatment is directed
at obtaining an adequate first web and thumb reconstruction, if needed.
The thumb may be reconstructed by a toe transplant or by lengthening,
and the digits may be lengthened by free toe phalangeal transfers into
the small nubbins or skin pockets. -
In brachysyndactyly, if a thumb and adequate web are present, treatment is focused on the release of the webbed fingers.
-
This condition is said to be a defect in the amnion (the innermost layer of the placenta).
-
Strands or threads of this membrane detach and wrap around digits or limbs.
-
The end result of these constricting bands is intrauterine amputation, constriction rings, and syndactyly.
 Figure 2-21 Brachysyndactyly as seen in Poland’s syndrome. (A) The pectoralis muscle is absent on the left side. (B) The index and middle fingers are foreshortened, and the second and third web spaces have partial (incomplete) webbing.
Figure 2-21 Brachysyndactyly as seen in Poland’s syndrome. (A) The pectoralis muscle is absent on the left side. (B) The index and middle fingers are foreshortened, and the second and third web spaces have partial (incomplete) webbing. -
Secondary syndactyly results from abnormal tissue between the digits, which does allow separation.
-
If the ring does not result in amputation, the clinical findings are present in the soft tissues.
-
Some rings are comparatively superficial, but some extend to the underlying osseous structures.
-
In the digits, the ring is deepest on the dorsal aspect.
-
The surgeon must distinguish between
shallow and deep rings, because deep rings may have little or no venous
or lymphatic drainage. In these cases, the only venous drainage is the
vena comitantes of the digital arteries. -
Minimal rings of little or no cosmetic
consequence require no particular treatment, but deep rings are treated
with excision of the ring and closure by a series of continuous or
interconnected Z-plasties.P.34![]() Figure 2-22 (A–B) A more complex form of brachysyndactyly. (C) Initial treatment by release of the border fingers by dorsal flaps and skin grafts. (D) The early result.
Figure 2-22 (A–B) A more complex form of brachysyndactyly. (C) Initial treatment by release of the border fingers by dorsal flaps and skin grafts. (D) The early result. -
Although some surgeons have corrected the
deformity in a one-stage procedure, it is customary to excise and
correct no more than half the ring at the first procedure. -
The technique involves excision of the
ring, followed by mobilization of the skin and soft tissues as one
composite layer. This extends down to the level between the fat and
underlying fascia or vital structures. -
A series of Z-plasties at angles of 60 degrees are then laid out.
-
The length of each limb of the Z-plasty
should be equal to one-third to one-half the diameter of the digit or
limb being treated. -
The flaps should be contoured and/or
thinned to produce a smooth nonbulging contour. Skin closure is with
5-0 or 6-0 chromic catgut (Fig. 2-23).
-
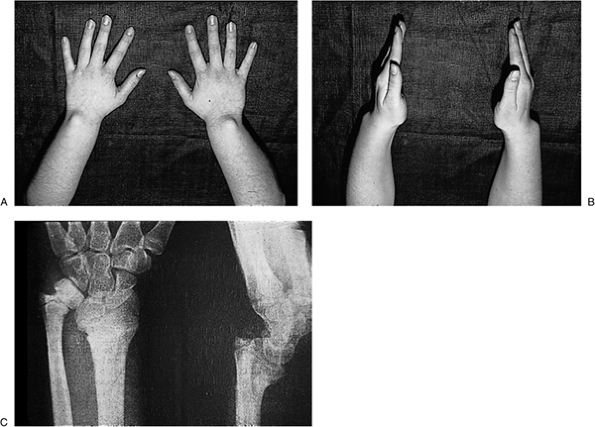
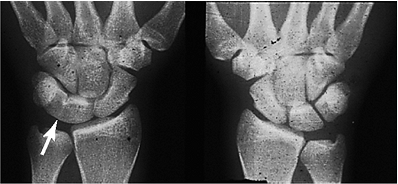
Most cases of Madelung’s deformity are
caused by hereditary dyschondrosteosis in the form of a lesion in the
volar-ulnar zone of the distal radial physis. This retards growth
asymmetrically, especially in late childhood.
-
The condition is seen most often in females.
-
The distal ulna is very prominent.P.35
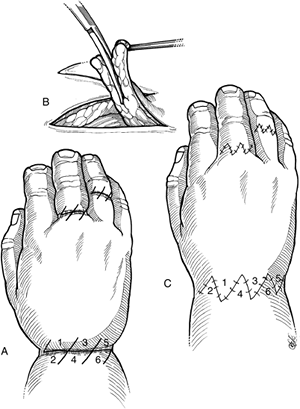 Figure 2-23 Z-plasty technique for constriction ring syndrome. (A)
Figure 2-23 Z-plasty technique for constriction ring syndrome. (A)
The constriction ring is excised down to the interval between the fat
and underlying vital structures or fascia. Redundant fat is excised
from the deep side of the flaps to achieve the appropriate contour. (B) Sixty-degree interconnected Z-plasties are laid out and the major arteries, veins, and nerves identified and preserved. (C)
The flaps are rotated and sutured in place with 5-0 or 6-0 chromic
catgut. (Taken from Doyle JR. Constriction ring reconstruction. In:
Blair WF, Steyers CM, eds. Techniques in hand surgery. Baltimore:
Williams and Wilkins, 1996.)![]() Figure 2-24 Clinical and x-ray appearance of Madelung’s deformity.
Figure 2-24 Clinical and x-ray appearance of Madelung’s deformity. -
The hand is displaced palmarward along with the carpus, and is pronated in reference to the long axis of the forearm.
-
The clinical and x-ray appearance is seen in Figure 2-24.
-
Surgical treatment is indicated in those
patients with a significant and symptomatic deformity who are
unresponsive to conservative management. -
In the adolescent, performing a
physiolysis procedure in the ulnar aspect of the distal radius and then
filling the defect created with fat may be considered as a possible
prophylactic procedure. -
In the adult, surgical treatment is in
the form of corrective osteotomy of the distal radius, with shortening
or resection and stabilization of the distal ulna as needed.
BJ, Carter PR, Ezaki M. Volar surgical correction of Madelung’s
deformity. Techniques in Hand and Upper Extremity Surg 2002;6:30–35.
MA, McCarroll HR Jr, Manske PR. The spectrum of radial longitudinal
deficiency: a modified classification. J Hand Surg 1999;24A:1145–1155.
S. Congenital anomalies. In: Trumble T, ed. Hand surgery update 3,
hand, elbow and shoulder. Rosemont, IL: American Society for Surgery of
the Hand, 2003:599–624.
TR. Congenital anomalies: syndactyly, polydactyly and cleft hand. In:
Surgery of the hand and upper extremity. New York: McGraw-Hill,
1996:2211–2144.
TR. Development of the hand. In: Green DP, Hotckiss RN, Pederson WC,
eds. Green’s operative hand surgery. 4th Ed. New York: Churchill
Livingstone, 1999:333–338.
D, Nielsen G. Madelung deformity: surgical prophylaxis (physiolysis)
during the late growth period by resection of the dyschondrosteosis
lesion. J Hand Surg 1992;17B:401–407.