Diastasis of the Symphysis Pubis: Open Reduction Internal Fixation
Editors: Wiss, Donald A.
Title: Master Techniques in Orthopaedic Surgery: Fractures, 2nd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > Section
III – Pelvis and Acetabulum > 38 – Diastasis of the Symphysis Pubis:
Open Reduction Internal Fixation
III – Pelvis and Acetabulum > 38 – Diastasis of the Symphysis Pubis:
Open Reduction Internal Fixation
38
Diastasis of the Symphysis Pubis: Open Reduction Internal Fixation
David C. Templeman
Andrew H. Schmidt
S. Andrew Sems
Indications/Contraindications
The pubic symphysis is a cartilaginous joint where the
pubic bones meet. The articulation is composed of a fibrocartilaginous
disc that is reinforced by the superior and inferior pubic ligaments.
The arcuate ligament forms an arch between the two inferior pubic rami
and is thought to be the major soft-tissue stabilizer of the symphysis
pubis (1).
pubic bones meet. The articulation is composed of a fibrocartilaginous
disc that is reinforced by the superior and inferior pubic ligaments.
The arcuate ligament forms an arch between the two inferior pubic rami
and is thought to be the major soft-tissue stabilizer of the symphysis
pubis (1).
Injuries to the pubic symphysis include diastasis,
fractures into the symphysis, and fracture-dislocations. Following
trauma, if the pubic symphysis is not disrupted, the anterior
pelvic-ring injury commonly consists of pubic rami fractures. These
fractures are usually vertically oriented but may be comminuted or
horizontal (2). Diastasis of the symphysis pubis rarely coexists with fractures of the pubic rami (3,4).
fractures into the symphysis, and fracture-dislocations. Following
trauma, if the pubic symphysis is not disrupted, the anterior
pelvic-ring injury commonly consists of pubic rami fractures. These
fractures are usually vertically oriented but may be comminuted or
horizontal (2). Diastasis of the symphysis pubis rarely coexists with fractures of the pubic rami (3,4).
Open reduction and internal fixation (ORIF) is usually
indicated when diastasis of the pubic symphysis exceeds 2.5 cm.
Internal fixation is performed to relieve pain and improve stability of
the anterior pelvic ring. The indications for surgery are based on the
patient’s overall condition and the stability of the entire pelvic ring.
indicated when diastasis of the pubic symphysis exceeds 2.5 cm.
Internal fixation is performed to relieve pain and improve stability of
the anterior pelvic ring. The indications for surgery are based on the
patient’s overall condition and the stability of the entire pelvic ring.
Several different classifications can be used to
characterize pelvic injuries. Early classifications were based on
either the location of the fracture or the mechanism of injury. Most
modern classifications, however, are based on the degree of pelvic
stability (5,6). The
Tile classification of pelvic ring injuries is used to predict the
mechanical instability of the injured pelvic ring and are categorized
as A, stable; B, rotationally unstable but vertically stable, and C,
rotationally and vertically unstable. Tile B and C injuries may have
associated disruption of the symphysis pubis (6).
characterize pelvic injuries. Early classifications were based on
either the location of the fracture or the mechanism of injury. Most
modern classifications, however, are based on the degree of pelvic
stability (5,6). The
Tile classification of pelvic ring injuries is used to predict the
mechanical instability of the injured pelvic ring and are categorized
as A, stable; B, rotationally unstable but vertically stable, and C,
rotationally and vertically unstable. Tile B and C injuries may have
associated disruption of the symphysis pubis (6).
Diastasis of the symphysis pubis and external rotation
of one innominate bone results in the so-called “open-book” injury.
This is a Tile B injury in which the posterior pelvic ligaments are
intact and prevent cephalad displacement of the involved innominate
bone.
of one innominate bone results in the so-called “open-book” injury.
This is a Tile B injury in which the posterior pelvic ligaments are
intact and prevent cephalad displacement of the involved innominate
bone.
P.640
When disruption of the symphysis pubis is greater than
2.5 cm, internal fixation is indicated. Displacement of this magnitude
is thought to be accompanied by injuries to the sacrospinous ligament
and the anterior sacroiliac ligaments, which are thought to allow the
involved innominate bone to rotate externally. Stable fixation of the
symphysis is sufficient to correct this innominate-bone instability (2).
2.5 cm, internal fixation is indicated. Displacement of this magnitude
is thought to be accompanied by injuries to the sacrospinous ligament
and the anterior sacroiliac ligaments, which are thought to allow the
involved innominate bone to rotate externally. Stable fixation of the
symphysis is sufficient to correct this innominate-bone instability (2).
In Tile C injuries, the symphysis pubis (or the anterior
pelvic ring) is disrupted as is the posterior pelvic ring, resulting in
complete instability of the pelvis. Fixation of the anterior ring alone
is insufficient to restore pelvic stability and must be accompanied by
reduction and fixation of the posterior pelvic injury (6,7).
pelvic ring) is disrupted as is the posterior pelvic ring, resulting in
complete instability of the pelvis. Fixation of the anterior ring alone
is insufficient to restore pelvic stability and must be accompanied by
reduction and fixation of the posterior pelvic injury (6,7).
Contraindications to internal fixation of the symphysis
pubis include unstable, critically ill patients; severe open fractures
with inadequate wound debridement; and crushing injuries in which
compromised skin may not tolerate a surgical incision. Suprapubic
catheters placed to treat extraperitoneal bladder ruptures may result
in contamination of the retropubic space and is a relative
contraindication to internal fixation of the adjacent symphysis pubis.
Additional conditions that may preclude secure fixation are
osteoporosis and severe fracture comminution of the anterior pelvic
ring.
pubis include unstable, critically ill patients; severe open fractures
with inadequate wound debridement; and crushing injuries in which
compromised skin may not tolerate a surgical incision. Suprapubic
catheters placed to treat extraperitoneal bladder ruptures may result
in contamination of the retropubic space and is a relative
contraindication to internal fixation of the adjacent symphysis pubis.
Additional conditions that may preclude secure fixation are
osteoporosis and severe fracture comminution of the anterior pelvic
ring.
When the diastasis of the symphysis pubis is less than
2.5 cm, internal fixation is seldom necessary. Patients may be safely
mobilized and allowed to exercise toe-touch weight bearing on the side
of the externally rotated hemipelvis. Radiographs are repeated within
the first few weeks to ensure further displacement has not occurred. By
8 weeks, the pelvis is usually healed enough to allow full weight
bearing. Any increase in pain associated with activity must be
evaluated with radiographs so hardware failure or late instability can
be detected.
2.5 cm, internal fixation is seldom necessary. Patients may be safely
mobilized and allowed to exercise toe-touch weight bearing on the side
of the externally rotated hemipelvis. Radiographs are repeated within
the first few weeks to ensure further displacement has not occurred. By
8 weeks, the pelvis is usually healed enough to allow full weight
bearing. Any increase in pain associated with activity must be
evaluated with radiographs so hardware failure or late instability can
be detected.
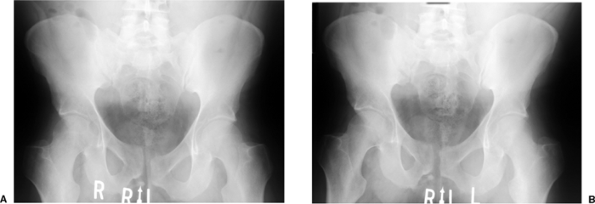
Chronic pelvic-ring instability may follow nonoperative
treatment or unrecognized pelvic-ring injuries. This subset of patients
commonly presents with pain in the symphyseal or sacroiliac region when
undergoing weight-bearing activities. For this group of patients,
single leg stance radiographs may be useful. The radiographs are taken
as standard anteroposterior (AP) pelvis x-rays, and the three-film
series should include a standing AP pelvis as well as an AP of the
pelvis during left leg stance and an AP of the pelvis during right leg
stance. Subtle instability may manifest as a vertical displacement at
the symphysis pubis with single leg stance on the unstable side (Fig 38.1).
These chronic instabilities may be approached with the same technique
of fixation that one would use to treat an acute injury, but retropubic
scarring of the bladder to the posterior aspect of the pubic bones and
symphysis may be encountered.
treatment or unrecognized pelvic-ring injuries. This subset of patients
commonly presents with pain in the symphyseal or sacroiliac region when
undergoing weight-bearing activities. For this group of patients,
single leg stance radiographs may be useful. The radiographs are taken
as standard anteroposterior (AP) pelvis x-rays, and the three-film
series should include a standing AP pelvis as well as an AP of the
pelvis during left leg stance and an AP of the pelvis during right leg
stance. Subtle instability may manifest as a vertical displacement at
the symphysis pubis with single leg stance on the unstable side (Fig 38.1).
These chronic instabilities may be approached with the same technique
of fixation that one would use to treat an acute injury, but retropubic
scarring of the bladder to the posterior aspect of the pubic bones and
symphysis may be encountered.
 |
|
Figure 38.1. AP pelvic radiographs in single leg stance show increased vertical displacement with weight bearing on the unstable side (A) compared to the contralateral single-leg stance radiograph (B).
|
P.641
Preoperative Planning
To determine the direction and magnitude of the
symphysis pubis disruption and the relative position of the pubic
bones, the surgeon should obtain AP, 40-degree caudal and 40-degree
cephalad views (Fig. 38.2A–C). Differences in
the height of the pubic rami usually indicate that the hemipelvis is
displaced in more than one plane. The most common deformity associated
with disruption of the symphysis pubis is cephalad migration, posterior
displacement, and external rotation of one hemipelvis (5).
This pattern indicates a posterior pelvic injury (Tile C) that requires
posterior reduction and internal fixation to achieve a stable pelvis (6,7,8).
symphysis pubis disruption and the relative position of the pubic
bones, the surgeon should obtain AP, 40-degree caudal and 40-degree
cephalad views (Fig. 38.2A–C). Differences in
the height of the pubic rami usually indicate that the hemipelvis is
displaced in more than one plane. The most common deformity associated
with disruption of the symphysis pubis is cephalad migration, posterior
displacement, and external rotation of one hemipelvis (5).
This pattern indicates a posterior pelvic injury (Tile C) that requires
posterior reduction and internal fixation to achieve a stable pelvis (6,7,8).
Patients with hemodynamic instability require immediate
evaluation and resuscitation. A multidisciplinary team consisting of
general surgeons, orthopedists, urologists, and interventional
radiologists is frequently required to treat patients with multiple
injuries (9,10,11,12).
evaluation and resuscitation. A multidisciplinary team consisting of
general surgeons, orthopedists, urologists, and interventional
radiologists is frequently required to treat patients with multiple
injuries (9,10,11,12).
Urologic injuries are common in patients with anterior
pelvic trauma. In male patients, a retrograde urethrogram should be
obtained to ensure that the urethra is intact before passing a Foley
catheter. Extravasation of dye during the urethrogram is a
contraindication to blind passage of a Foley catheter and requires
consultation with a urologist. The presence of blood at the tip of the
penile meatus is frequently cited as a sign of urethral trauma;
however, it is not present in the majority of cases. When the urethra
is intact, a Foley catheter is passed and a cystogram is obtained.
Because the female urethra is only several centimeters in length, a
retrograde urethrogram is not required before inserting a Foley
catheter (10).
pelvic trauma. In male patients, a retrograde urethrogram should be
obtained to ensure that the urethra is intact before passing a Foley
catheter. Extravasation of dye during the urethrogram is a
contraindication to blind passage of a Foley catheter and requires
consultation with a urologist. The presence of blood at the tip of the
penile meatus is frequently cited as a sign of urethral trauma;
however, it is not present in the majority of cases. When the urethra
is intact, a Foley catheter is passed and a cystogram is obtained.
Because the female urethra is only several centimeters in length, a
retrograde urethrogram is not required before inserting a Foley
catheter (10).
The bladder should be studied by cystography with an
intravenous pyelogram or retrograde cystogram. External compression of
the bladder is frequently caused by a pelvic hematoma.
intravenous pyelogram or retrograde cystogram. External compression of
the bladder is frequently caused by a pelvic hematoma.
The management of extraperitoneal bladder ruptures in
patients with pelvic fractures is controversial. Traditional Foley
catheter drainage of extraperitoneal ruptures avoids the need for a
laparotomy and direct repair. Kotkin and Koch (10)
found that patients with extraperitoneal bladder ruptures and pelvic
fractures have higher rates of complications, and these authors
stressed the need for adequate bladder drainage.
patients with pelvic fractures is controversial. Traditional Foley
catheter drainage of extraperitoneal ruptures avoids the need for a
laparotomy and direct repair. Kotkin and Koch (10)
found that patients with extraperitoneal bladder ruptures and pelvic
fractures have higher rates of complications, and these authors
stressed the need for adequate bladder drainage.
When an extraperitoneal bladder rupture exists, the
patient is at an increased risk for infection due to seeding of the
pelvic hematoma. When internal fixation of the symphysis is planned,
the risk of infection from the ruptured bladder must be considered. We
favor primary bladder repair, irrigation of the anterior pelvic-ring
injury, and the use of antibiotics. The timing of the bladder repair is
determined on an individual basis (10).
patient is at an increased risk for infection due to seeding of the
pelvic hematoma. When internal fixation of the symphysis is planned,
the risk of infection from the ruptured bladder must be considered. We
favor primary bladder repair, irrigation of the anterior pelvic-ring
injury, and the use of antibiotics. The timing of the bladder repair is
determined on an individual basis (10).
After the patient has been stabilized, radiographic
studies are obtained. In addition to the plain films, a computed
tomography (CT) scan is recommended to assess the posterior pelvic
anatomy. The anterior structures are best studied with plain films (6,11).
studies are obtained. In addition to the plain films, a computed
tomography (CT) scan is recommended to assess the posterior pelvic
anatomy. The anterior structures are best studied with plain films (6,11).
Surgery
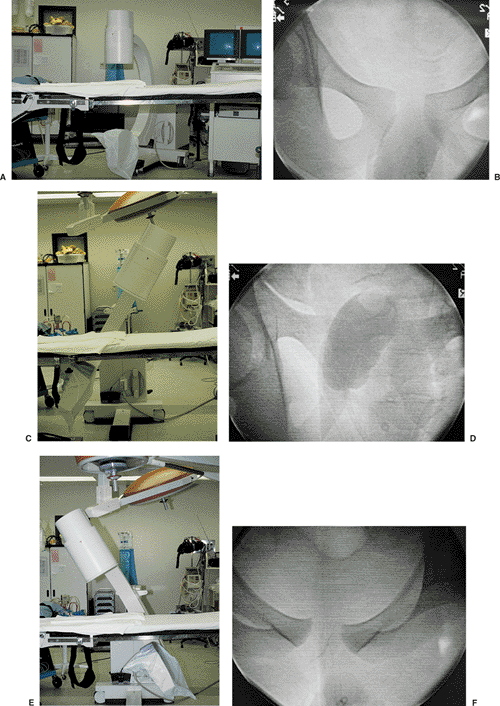
Surgery is performed under general anesthesia. The
patient is positioned supine on a radiolucent table that can
accommodate a mobile C-arm image intensifier (see Fig. 38.2A).
The imager permits evaluation of the reduction, placement of the
hardware, and assessment of the remainder of the pelvis after the
symphysis is reduced. Before prepping and draping the surgical field,
the surgeon obtains AP, cephalad, and caudal (Fig. 38.2E,F)
views of the pelvis with the c-arm to ensure adequate visualization;
these views are particularly important if the combined fixation of the
anterior and posterior pelvic-ring is required (Fig. 38.2B–D). The cephalad projection provides the best image to visualize screw length after internal fixation of the pubic symphysis.
patient is positioned supine on a radiolucent table that can
accommodate a mobile C-arm image intensifier (see Fig. 38.2A).
The imager permits evaluation of the reduction, placement of the
hardware, and assessment of the remainder of the pelvis after the
symphysis is reduced. Before prepping and draping the surgical field,
the surgeon obtains AP, cephalad, and caudal (Fig. 38.2E,F)
views of the pelvis with the c-arm to ensure adequate visualization;
these views are particularly important if the combined fixation of the
anterior and posterior pelvic-ring is required (Fig. 38.2B–D). The cephalad projection provides the best image to visualize screw length after internal fixation of the pubic symphysis.
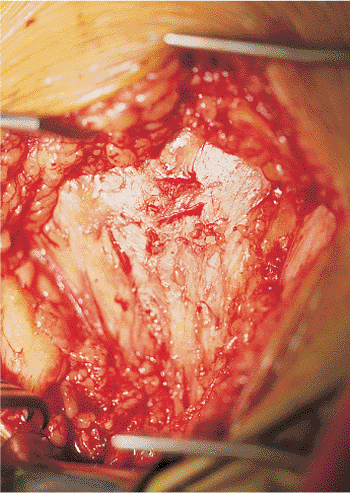
A transverse Pfannenstiel incision is used for reduction and fixation of the symphysis (Fig. 38.3).
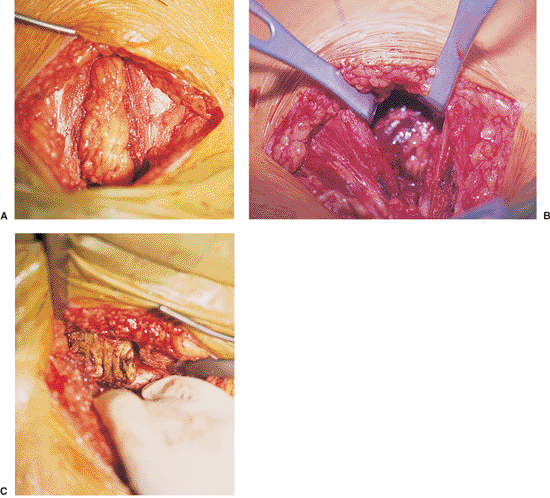
When marked disruption of the symphysis is encountered, detachment of
one head of the rectus abdominis is common. The linea alba is divided
longitudinally, with lateral elevation of the insertion of the
abdominis muscle laterally (Fig. 38.4).
Transverse sectioning of the rectus abdominis should be avoided because
it impairs subsequent repair and healing of the abdominal wall (8).
When marked disruption of the symphysis is encountered, detachment of
one head of the rectus abdominis is common. The linea alba is divided
longitudinally, with lateral elevation of the insertion of the
abdominis muscle laterally (Fig. 38.4).
Transverse sectioning of the rectus abdominis should be avoided because
it impairs subsequent repair and healing of the abdominal wall (8).
 |
|
Figure 38.2. A,B. An operating room table with a radiolucent extension. This table allows tilting of the fluoroscopic unit to obtain cephalad (C,D) and caudad (E,F) images of the pelvis (B,C).
The cephalad view superimposes the symphysis on the sacrum; this makes the diastasis of the symphysis difficult to view. Many operating room tables do not allow enough movement of the C-arm to obtain cephalad and caudal views. |
 |
|
Figure 38.3. Pfannenstiel incision to expose the linea alba, which is located in the midline.
|
 |
|
Figure 38.4. Division of the linea alba (A) and lateral retraction of the two heads of the rectus abdominis (B).
Further retraction reveals disruption of the right rectus abdominis muscle. The bone of the pubic body is visible above the surgeon’s hand (C). |
P.642
P.643
P.644
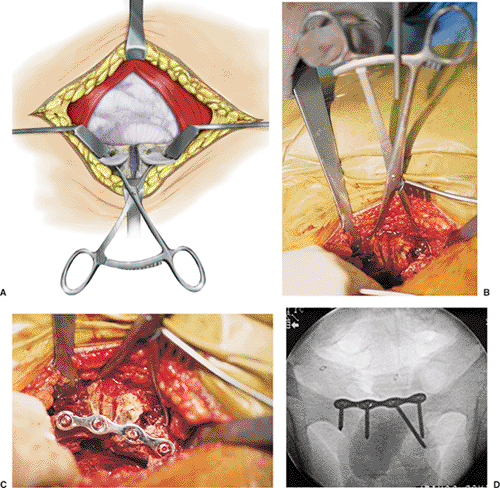
Narrow Homan retractors are carefully placed in the
obturator foramen, which enhances exposure and may assist in partially
reducing the displaced symphysis (Fig. 38.5A).
Several methods can be used to achieve reduction. The simplest method
is to place large, pointed reduction clamps on each side of the
symphysis (see Fig. 38.5B). Because this clamp
exerts a limited amount of control and force, it works best in patients
with lesser degrees of displacement.
obturator foramen, which enhances exposure and may assist in partially
reducing the displaced symphysis (Fig. 38.5A).
Several methods can be used to achieve reduction. The simplest method
is to place large, pointed reduction clamps on each side of the
symphysis (see Fig. 38.5B). Because this clamp
exerts a limited amount of control and force, it works best in patients
with lesser degrees of displacement.
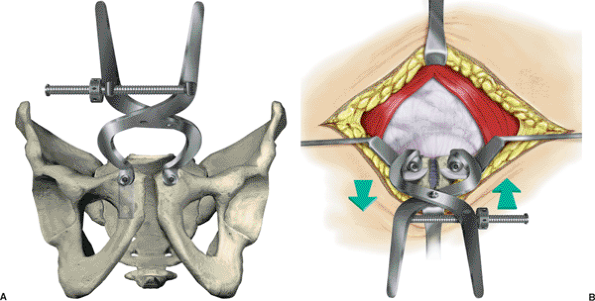
In patients with disruption of the symphysis and the
posterior pelvic ring, a three-dimensional deformity is usually
present: posterior, cephalad, and external rotation of the innominate
bone. Therefore, the reduction requires manipulation of the entire
innominate bone. Matta (13) popularized the technique in which a pelvic-reduction clamp (Fig. 38.6A,B)
is secured to the pubis with 4.5-mm screws inserted into the pubic
bodies in an anterior-to-posterior direction. The screws are placed so
they do not interfere with the subsequent application of the symphysis
plate. For an innominate bone that is displaced in a posterior
direction, placement of a plate on the inner surface of the displaced
hemipelvis prevents screw pullout when the clamp is used to manipulate
the innominate bone anteriorly. Reduction of the symphysis often
improves alignment of the posterior injury, making its subsequent
reduction and fixation easier.
posterior pelvic ring, a three-dimensional deformity is usually
present: posterior, cephalad, and external rotation of the innominate
bone. Therefore, the reduction requires manipulation of the entire
innominate bone. Matta (13) popularized the technique in which a pelvic-reduction clamp (Fig. 38.6A,B)
is secured to the pubis with 4.5-mm screws inserted into the pubic
bodies in an anterior-to-posterior direction. The screws are placed so
they do not interfere with the subsequent application of the symphysis
plate. For an innominate bone that is displaced in a posterior
direction, placement of a plate on the inner surface of the displaced
hemipelvis prevents screw pullout when the clamp is used to manipulate
the innominate bone anteriorly. Reduction of the symphysis often
improves alignment of the posterior injury, making its subsequent
reduction and fixation easier.
 |
|
Figure 38.5. A. Line diagram of Homan retractors and the use of pointed reduction clamps to reduce the diastasis of the symphysis pubis. B. Intraoperative application of clamp with reduction of the pubic symphysis. C. Application of plate on superior aspect of the pubic bodies. D. Cephalad view to confirm screw length.
|
P.645
Several different implants may be used for fixation of the disrupted symphysis. Lange and Hansen (14) and Webb et al (15)
advocated two-hole 4.5-mm plates. With this method, implant loosening
may permit the return of physiologic motion of the symphysis after
fixation. Thus, late problems of implant fatigue failure may be avoided.
advocated two-hole 4.5-mm plates. With this method, implant loosening
may permit the return of physiologic motion of the symphysis after
fixation. Thus, late problems of implant fatigue failure may be avoided.
With multiplanar displacement of the pubic symphysis,
the use of a more stable implant is recommended. The most frequently
used implants are pelvic reconstruction plates (Synthes, Paoli, PA)
with either four or six holes. Precurved plates (which are 3.6 mm thick
and unlike straight plates of 2.8 mm thickness) provide additional
stability. Plates that use either 4.5- or 3.5-mm screws can be used at
the discretion of the surgeon. We favor the use of the 3.5-mm implants
with three screws inserted on each side of the symphysis (Fig. 38.5C).
the use of a more stable implant is recommended. The most frequently
used implants are pelvic reconstruction plates (Synthes, Paoli, PA)
with either four or six holes. Precurved plates (which are 3.6 mm thick
and unlike straight plates of 2.8 mm thickness) provide additional
stability. Plates that use either 4.5- or 3.5-mm screws can be used at
the discretion of the surgeon. We favor the use of the 3.5-mm implants
with three screws inserted on each side of the symphysis (Fig. 38.5C).
 |
|
Figure 38.6. Reduction of the displaced hemipelvis as recommended by Matta. A.
The pelvis-reduction clamp is anchored to the pubic bodies with 4.5-mm cortical screws directed in an anterior-to-posterior direction. The placement of the screws requires protection of the bladder. The clamp allows multidirectional control of the displaced hemipelvis. B. In addition to closing the diastasis of the pubic symphysis, posterior translation of the pelvic ring can be partially corrected (arrows). This will not usually obtain an anatomic reduction of displaced posterior injuries. |
P.646
In addition to visualization of the reduction, palpation
of the inner surface of the symphysis confirms the adequacy of the
reduction. Similarly, palpation behind each pubic body assists in
accurately directing screws into the distal space of the pubic body. In
acute injuries, this space is readily accessible. However, when
encountering chronic injuries, the surgeon should take care when
developing this space to protect the bladder because it may be adherent
to the posterior aspect of the pubic bones and symphysis. After
fixation, the C-arm is used to verify the reduction and position of the
implants (Fig. 38.5D).
of the inner surface of the symphysis confirms the adequacy of the
reduction. Similarly, palpation behind each pubic body assists in
accurately directing screws into the distal space of the pubic body. In
acute injuries, this space is readily accessible. However, when
encountering chronic injuries, the surgeon should take care when
developing this space to protect the bladder because it may be adherent
to the posterior aspect of the pubic bones and symphysis. After
fixation, the C-arm is used to verify the reduction and position of the
implants (Fig. 38.5D).
The linea alba is reapproximated with interrupted
sutures. The wounds are closed over a drain placed in the space of
Retzius and exits proximal to the incision.
sutures. The wounds are closed over a drain placed in the space of
Retzius and exits proximal to the incision.
Postoperative Management
The spectrum of injuries associated with disruption of
the pelvic ring is diverse and prevents the use of rigid postoperative
protocols. However, several principles guide patient care. Early
patient mobilization improves pulmonary care and decreases the risks
associated with bed rest. An upright posture is usually possible within
24 hours after surgery.
the pelvic ring is diverse and prevents the use of rigid postoperative
protocols. However, several principles guide patient care. Early
patient mobilization improves pulmonary care and decreases the risks
associated with bed rest. An upright posture is usually possible within
24 hours after surgery.
Deep venous thrombosis (DVT) occurs in 35% to 60% of
patients with pelvic fractures. Proximal thromboses form in 25% to 35%
of these patients and are more likely to embolize than are more distal
thrombi (16,17). Based on the high incidence of DVT in patients with pelvic fractures, we strongly recommend aggressive DVT prophylaxis.
patients with pelvic fractures. Proximal thromboses form in 25% to 35%
of these patients and are more likely to embolize than are more distal
thrombi (16,17). Based on the high incidence of DVT in patients with pelvic fractures, we strongly recommend aggressive DVT prophylaxis.
Routine screening is not helpful because of the high
percentage of patients who develop DVT. Screening is considered when
surgery is delayed more than 48 hours from the time of the injury. The
diagnosis and treatment of thromboses that are identified
preoperatively may help prevent an intraoperative pulmonary embolism (18).
percentage of patients who develop DVT. Screening is considered when
surgery is delayed more than 48 hours from the time of the injury. The
diagnosis and treatment of thromboses that are identified
preoperatively may help prevent an intraoperative pulmonary embolism (18).
P.647
The perfect form of prophylaxis and treatment for venous
thrombosis remains elusive. Pharmacologic agents should be safe and
easy to administer, monitor, and reverse. The use of pharmacologic
anticoagulation in trauma patients is further complicated when the
patient presents with associated head injuries, retroperitoneal
bleeding, and thoracoabdominal injuries. Treatment cannot be started
until bleeding is controlled (18). Mechanical
devices that increase venous blood flow by intermittent mechanical
compression offer an alternative to pharmacologic agents. However, when
used as a sole form of therapy, they are ineffective. One study found
that combined use of mechanical compression and low-dose heparin was
effective in reducing the incidence of DVT (19).
thrombosis remains elusive. Pharmacologic agents should be safe and
easy to administer, monitor, and reverse. The use of pharmacologic
anticoagulation in trauma patients is further complicated when the
patient presents with associated head injuries, retroperitoneal
bleeding, and thoracoabdominal injuries. Treatment cannot be started
until bleeding is controlled (18). Mechanical
devices that increase venous blood flow by intermittent mechanical
compression offer an alternative to pharmacologic agents. However, when
used as a sole form of therapy, they are ineffective. One study found
that combined use of mechanical compression and low-dose heparin was
effective in reducing the incidence of DVT (19).
With stable fixation, patients can be mobilized from bed
to chair on the first or second day after surgery. Ambulation depends
on the specific injury. For the isolated open-book injuries (Tile B),
we recommend protected weight bearing on the injured side for 8 weeks.
Follow-up radiographs at this time usually indicate some new bone
formation in the region of the symphysis. This is interpreted as
sufficient healing and stability. In patients with combined internal
fixation of the anterior and posterior pelvic ring (Tile C), weight
bearing should be delayed for 8 to 12 weeks.
to chair on the first or second day after surgery. Ambulation depends
on the specific injury. For the isolated open-book injuries (Tile B),
we recommend protected weight bearing on the injured side for 8 weeks.
Follow-up radiographs at this time usually indicate some new bone
formation in the region of the symphysis. This is interpreted as
sufficient healing and stability. In patients with combined internal
fixation of the anterior and posterior pelvic ring (Tile C), weight
bearing should be delayed for 8 to 12 weeks.
When full weight bearing is permitted, physical therapy
may be helpful. Most patients have muscle atrophy as a result of injury
and inactivity. Physical therapy, directed at increasing hip abductor
strength and aerobic conditioning, helps restore a normal gait. Lower
back–strengthening exercises and work-increasing programs may be
beneficial in patients who need to return to heavy labor.
may be helpful. Most patients have muscle atrophy as a result of injury
and inactivity. Physical therapy, directed at increasing hip abductor
strength and aerobic conditioning, helps restore a normal gait. Lower
back–strengthening exercises and work-increasing programs may be
beneficial in patients who need to return to heavy labor.
Discharge from the hospital is dependent on the presence
of associated injuries. Many patients can use crutches or are able to
perform bed-to-chair transfers within a week after surgery.
of associated injuries. Many patients can use crutches or are able to
perform bed-to-chair transfers within a week after surgery.
Matta and Tornetta (7) reported
the results of open reduction for anterior fixation of pelvic ring
injuries. In a series of 127 patients with pelvic ring injuries, these
authors noted that 88 of 105 fractures of the obturator ring were not
internally fixed, and none required subsequent treatment for nonunion
or loss of reduction.
the results of open reduction for anterior fixation of pelvic ring
injuries. In a series of 127 patients with pelvic ring injuries, these
authors noted that 88 of 105 fractures of the obturator ring were not
internally fixed, and none required subsequent treatment for nonunion
or loss of reduction.
Based on this study, Matta (13)
recommended that internal fixation of the anterior pelvic ring should
be reserved for symphysis pubis dislocations and only a minority of
pubis rami fractures that remain widely displace after ORIF of the
posterior pelvic ring.
recommended that internal fixation of the anterior pelvic ring should
be reserved for symphysis pubis dislocations and only a minority of
pubis rami fractures that remain widely displace after ORIF of the
posterior pelvic ring.
Complications
Complications related to internal fixation of the
symphysis pubis are uncommon. Loss of fixation is usually associated
with inadequate reduction and fixation of the posterior pelvic ring. If
this occurs, the entire fixation construct, in both the anterior and
posterior pelvic ring, requires revision osteosynthesis.
symphysis pubis are uncommon. Loss of fixation is usually associated
with inadequate reduction and fixation of the posterior pelvic ring. If
this occurs, the entire fixation construct, in both the anterior and
posterior pelvic ring, requires revision osteosynthesis.
Because of physiologic motion at the symphysis pubis,
screw backout or plate failure is occasionally seen. These events
seldom become symptomatic, and in our experience, late hardware removal
is infrequently needed.
screw backout or plate failure is occasionally seen. These events
seldom become symptomatic, and in our experience, late hardware removal
is infrequently needed.
Wound dehiscence or infection is rare. Irrigation and
debridement should include exposure of the plate and retropubic space.
When a prior urologic injury has been treated, reevaluation of the
urinary system is necessary. The procedure should include urinalysis,
urine cultures, and may even require imaging studies. A consultation
with an urologist is recommended.
debridement should include exposure of the plate and retropubic space.
When a prior urologic injury has been treated, reevaluation of the
urinary system is necessary. The procedure should include urinalysis,
urine cultures, and may even require imaging studies. A consultation
with an urologist is recommended.
Impotence may result from the initial injury. Because
patients may be reluctant to discuss this issue, polite questioning in
the private setting of an examination room may identify those patients
with sexual dysfunction.
patients may be reluctant to discuss this issue, polite questioning in
the private setting of an examination room may identify those patients
with sexual dysfunction.
Recommended Readings
1. Hollinshead WH. Anatomy for Surgeons. 3rd ed. Philadelphia: Harper & Row; 1982.
2. Letournel E. Surgical fixation of displaced pelvic fractures and dislocations of the symphysis pubis. Rev Chir Orthop 1981;67(8):771–782.
P.648
3. Gamble JG. The symphysis pubis: anatomic and pathological considerations. Clin Orthop 1986;203:261–272.
4. Letournel E. Pelvic fractures. Injury 1978;10:145–148.
5. Bucholz RW. The pathological anatomy of Malgaigne fracture-dislocation of the pelvis. J Bone Joint Surg Am 1981;63:400.
6. Tile M. Pelvic ring fractures: should they be fixed? J Bone Joint Surg Br 1988;70(1):1.
7. Matta JM, Tornetta, P. Internal fixation of unstable pelvic ring injuries. Clin Orthop 1996; 329:129–140.
8. Matta JM, Saucedo T. Internal fixation of pelvic ring fractures. Clin Orthop 1989;242:83–97.
9. Dalai
SA, Burgess AR, Siegel JH, et al. Pelvic fracture in multiple trauma:
classification by mechanism is the key to pattern of organ injury:
resuscitative requirements and outcome. J Trauma 1989;29(7):981–1000.
SA, Burgess AR, Siegel JH, et al. Pelvic fracture in multiple trauma:
classification by mechanism is the key to pattern of organ injury:
resuscitative requirements and outcome. J Trauma 1989;29(7):981–1000.
10. Kotkin L, Koch M. Morbidity associated with nonoperative management of extraperitoneal bladder injuries. J Trauma 1995;38:895.
11. Tile M, Pennal GF. Pelvic disruption: principles of management. Clin Orthop 1980;151:56.
12. Geerts
WH, Code KI. Thrombo-prophylaxis after major trauma: a double-blind
study comparing LDH and the LMWH enaparin [abstract]. Thromb Haemost 1985;73:284.
WH, Code KI. Thrombo-prophylaxis after major trauma: a double-blind
study comparing LDH and the LMWH enaparin [abstract]. Thromb Haemost 1985;73:284.
13. Matta JM. Indications for anterior fixation of pelvic fractures. Clin Orthop 1996;329:88–96.
14. Lange RH, Hansen ST Jr. Pelvic ring disruptions with symphysis diastasis. Clin Orthop 1985;201:130–137.
15. Webb LX, Gristina AG, Wilson JR, et al. Two-hole plate fixation for traumatic symphysis pubis diastasis. J Trauma 1988;28(6):813–817.
16. Geerts WH, Code K, Jay RM, et al. A prospective of DVT after major trauma. N Engl J Med 1994; 331(24):1601–1606.
17. Montgomery KD, Geertz WH, Potter HG, et al. Thromboembolic complications in patients with pelvic trauma. Clin Orthop 1996;329:68–87.
18. Montgomery
KD, Potter HG, Helfet DL. Magnetic resonance venography to evaluate the
deep venous system of the pelvis in patients who have acetabular
fractures. J Bone Joint Surg Am 1995;77(11):1639–1649.
KD, Potter HG, Helfet DL. Magnetic resonance venography to evaluate the
deep venous system of the pelvis in patients who have acetabular
fractures. J Bone Joint Surg Am 1995;77(11):1639–1649.
19. Stickney J, Delp SL. Deep venous thrombosis: prophylaxis. J Orthop Trauma 1991;227.
