Supracondylar Humerus Fractures: Operative Management
fractures about the elbow and have a peak incidence in the first decade
of life. These fractures often instill fear in the treating physician
because of the young age of the child, the often gross displacement,
and the risk of neurovascular compromise from the injury and treatment.
Taking a careful systematic approach to the operative care and
postoperative management of these fractures helps alleviate these
concerns. This enables the surgeon to have confidence in the operating
room and enables the child to have the best possible outcome.
lying beyond the proximal extensions of the joint capsule. Appreciation
of the anatomic relationships between the structures that make up the
elbow complex while in extension is paramount to understanding the
mechanisms of injury responsible for these fractures.
fibers become most taut with hyperextension of the humeroulnar joint.
Remodeling of the metaphysis peaks during the second half of the first
decade of life creates a radiographic picture dominated by poorly
defined trabeculae, thinned cortices, and metaphyseal flaring.
Specifically, there is structural insufficiency about the coronoid and
olecranon fossae because of deficiency in the thickness of the anterior
and posterior cortices of the medial and lateral supracondylar columns.
Furthermore, normal ligamentous laxity of childhood contributes to the
mechanisms of injury implicated in supracondylar fractures. In
hyperextension, the linear force vector transmitted along the olecranon
is converted into a bending force that becomes concentrated in the
supracondylar region and propagates through the supracondylar columns
as the olecranon, acting as a fulcrum, is driven into the olecranon
fossa (Fig. 12-1). Supracondylar fractures are typically transverse and are located at the level of the olecranon fossa.
classification), the risk of neurovascular complication is significant.
The regional anatomy includes the brachial artery and median nerve
located anteriorly in the antecubital fossa, the ulnar nerve coursing
posterior to the medial epicondyle, and the radial nerve
anterolaterally. Injuries to these neurovascular structures have all
been reported.
anterior humeral line still passes through the middle third of the
ossification center of the capitellum.
fractured; type III supracondylar fractures can be subclassified
(Wilkins’ subclassification) based on the position of the distal
fragment in the coronal plane, that is, posteromedial and
posterolateral (Fig. 12-3).
with closed reduction and casting above the elbow, unstable types II
and III fractures require closed reduction with percutaneous pinning to
maintain the reduction.
-
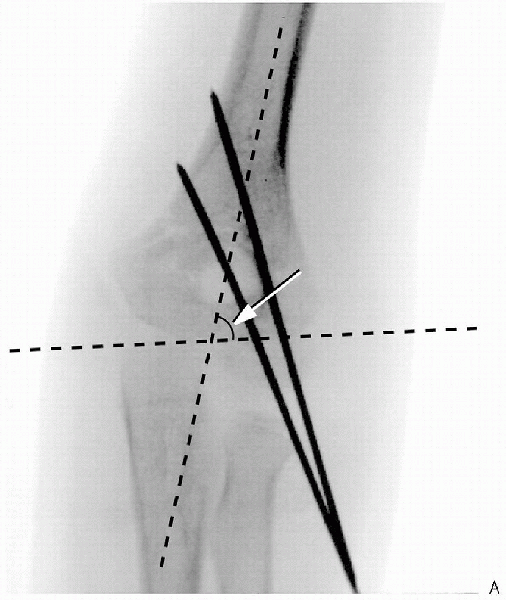
Evaluation of Baumann’s angle, the
humeroulnar angle, and the metaphyseal-diaphyseal angle. Baumann’s
angle is the angle created between the physeal line of the lateral
condyle and the long axis of the humerus. An increased angle compared
with the opposite side signifies a varus deformity (Fig. 12-4). -
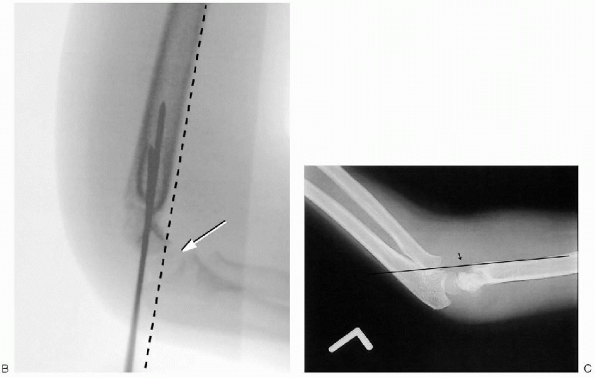
Translation as well as comminution of the
medial and lateral columns should be assessed on the AP film. The
presence of translation of the fracture fragment represents an unstable
fracture, because translation requires disruption of both anterior and
posterior cortices (Fig. 12-5). -
Full elbow extension is a prerequisite
for obtaining a true AP of the elbow. Often the child’s elbow is
swollen, painful, and difficult to range. In these circumstances, an AP
of the distal humerus can be obtained despite incomplete elbow
extension. The distal humerus can be placed on the cassette without
forcing the patient to extend the elbow. In addition, an AP of the
proximal radius can also be obtained by placing the forearm on the
cassette.
 |
|
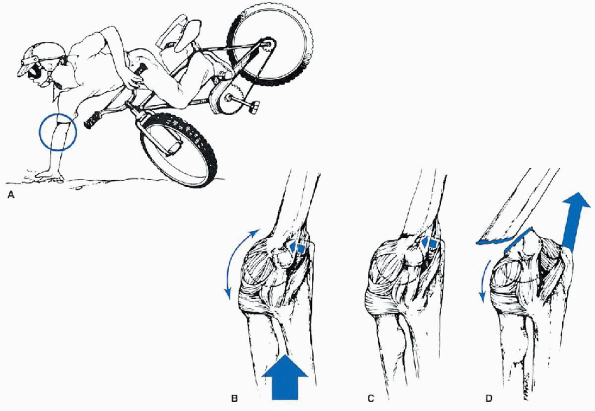
FIGURE 12-1. Hyperextension forces. A:
Most young children attempt to break their falls with the upper extremity extended. Because of the laxity of the ligaments, the elbow becomes locked into hyperextension. B: This converts the linear applied force (large arrow) to an anterior tension force. Posteriorly, the olecranon is forced into the depths of the olecranon fossa (small arrow). C: As the bending force continues, the distal humerus fails anteriorly in the supracondylar area. D: When the fracture is complete, the distal fragment becomes posteriorly displaced. The strong action of the triceps (large arrow) produces proximal displacement of the distal fragment. (From Beaty JH, Kasser JR. Supracondylar fractures of the distal humerus. In: Beaty JH, Kasser JR, eds. Rockwood and Wilkins’ fractures in children, 5th ed. Philadelphia: Lippincott Williams & Wilkins, 2001:577-624, with permission.) |
 |
|
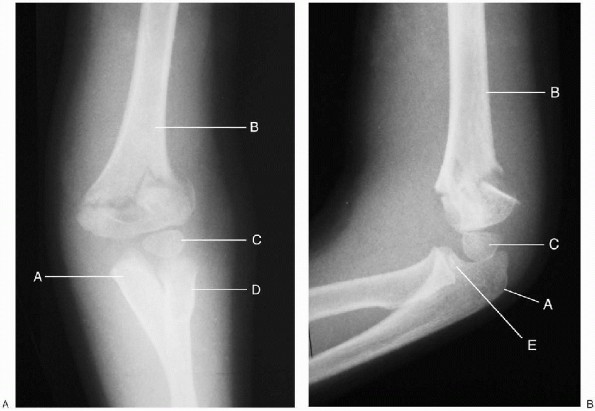
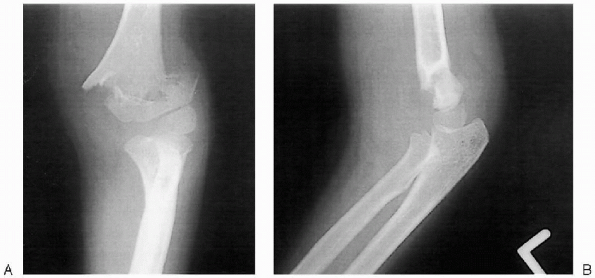
FIGURE 12-2. Type II extension supracondylar humerus fracture (left elbow). A: Anterior-posterior. B: Lateral. A, ulna; B, humerus; C, capitellar epiphysis; D, radius; E, radial head.
|
 |
|
FIGURE 12-3. Type III extension supracondylar humerus fracture (right elbow).
|
-
The distal end of the teardrop is formed
by the ossific center of the capitellum. An obscured teardrop may
represent a displaced fracture. -
The shaft-condylar angle decrease with
extension-type supracondylar fractures as the distal fragment is
displaced posteriorly; this angle increases in the less common
flexion-type fractures as the distal fracture fragment with the
capitellum is driven anteriorly. -
With extension-type supracondylar
fractures, the anterior humeral line passes anterior to the to the
middle of the capitellum. Similarly, the coronoid line passes anterior
to the lateral condyle with these fractures. Conversely, the anterior
humeral and coronoid lines line pass posteriorly with respect to their
described landmarks with flexion-type supracondylar fractures (Fig. 12-4).
nondisplaced or minimally displaced supracondylar fracture. A high
index of suspicion in the setting of negative AP and lateral
radiographs
warrants this view. This view is also used during the pinning of a fracture to see the reduction of the columns.
 |
|
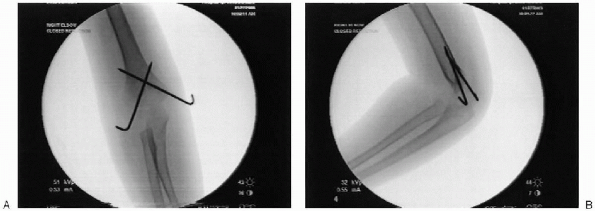
FIGURE 12-4. A: Two lateral pins used to obtain fixation for supracondylar humerus fracture. Note divergence of pins and Baumann’s angle (arrow).
|
 |
|
FIGURE 12-4. (Continued) B: Note lateral reduction of fracture on lateral film. Note anterohumeral line and relationship with capitellum (arrow). C: Anterior humeral line falling in front of capitellum (left elbow).
|
be debated in the literature. Contemporary textbooks of pediatric
orthopaedics describe the crossed-pin configuration as the preferred
treatment, except when the medial epicondyle or the ulnar nerve cannot
be palpated. Several studies report that lateral pin fixation performed
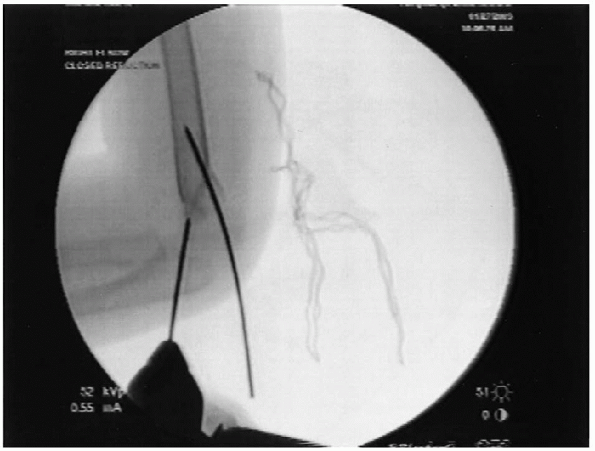
correctly is effective in maintaining reduction (Fig. 12-5).
 |
|
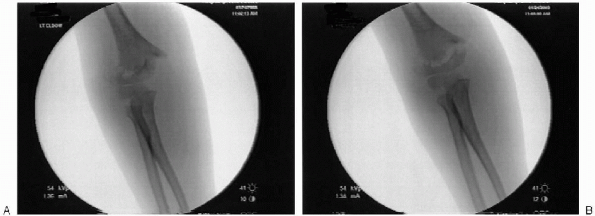
FIGURE 12-5. Supracondylar humerus fracture demonstrating lateral translation of the distal fragment: A: Anteroposterior. B: Lateral (left elbow).
|
-
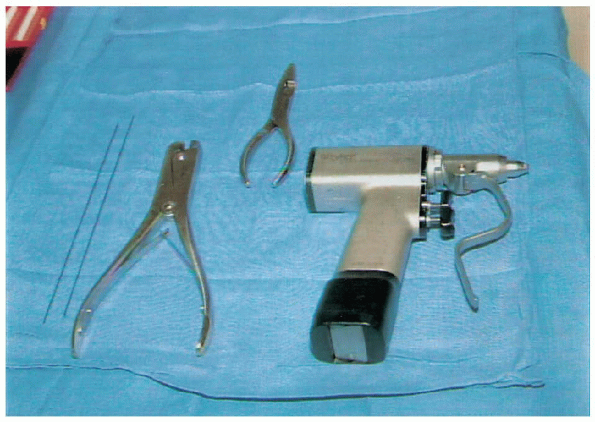
Power wire driver
-
0.062-inch Kirschner wires (K-wires) for percutaneous pin fixation
-
C-arm fluoroscopic image intensifier
-
3-inch plaster slabs
-
Webril/Ace bandages
 |
|
FIGURE 12-6. Instruments (left to right): 0.062 K-wires, wire cutter, needle-nose pliers, and power wire driver.
|
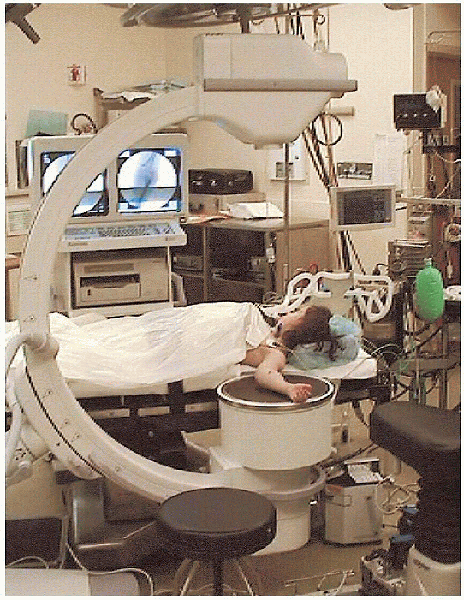
at the edge of the table. No tourniquet is applied; however, a sterile
one should be available. The affected upper extremity is prepped and
draped in a sterile fashion. The C-arm image intensifier is positioned
adjacent, parallel to the table and covered with a sterile drape. The
patient’s elbow is placed on the image intensification machine. The
image intensifier is used as the operating table so further radiographs
can be obtained to reevaluate the fracture pattern, assess the closed
reduction, and confirm K-wire placements. The monitor is placed on the
opposite side of the table in the surgeon’s direct line of vision. The
surgeon and assistant are seated for the procedure. The surgeon sits on
the lateral side of the elbow (Fig. 12-7).
 |
|
FIGURE 12-7. Patient positioning for the left elbow.
|

-
Correction of medial/lateral displacement. Medial
or lateral translation is corrected by applying a translational force
with or without a valgus or varus moment in the coronal plane to the
distal fragment. Confirmation of fragment placement is achieved with image intensification with the elbow in extension. Minimal traction is used to achieve this reduction (Fig. 12-8). -
Correction of rotation. Posteromedial
displacement usually may require pronation of the forearm and
posterolateral displacement may require supination of the forearm. The correction of medial/lateral translation and rotation must be corrected before the elbow is flexed. -
Correction of posterior displacement/angulation. Minimal traction is maintained. Posterior
displacement is corrected as the distal fragment is lifted anteriorly
as the surgeon places a thumb on the olecranon, slowly pushing it
distally and anteriorly. The elbow is flexed during this
maneuver to tighten the posterior periosteal hinge and reduce the
fracture. Pronation may be needed in full flexion in order to lock the
fracture fragments (Fig. 12-9). -
Confirmatory radiographs—four views. AP
and lateral films should be obtained to document acceptable reduction.
The AP view is often unobtainable for fractures with the elbow in full
flexion; therefore, oblique medial and lateral column views should be
used instead. Any residual medial/lateral angulation in the coronal
plane must be corrected to prevent cubitus varus and valgus. Residual
malrotation of the distal fragment, suggested when the two segments at
the fracture appear to have different diameters, should also be
corrected, although the patient often compensates clinically because of
the multiple degrees of freedom available at the glenohumeral joint.
The lateral view should be used to check flexion-extension alignment
and confirm restoration of the shaft-condylar angle. The presence of
the crescent sign, created with overlap of the ossification center of
the lateral condyle and olecranon, suggests residual angulation in the
distal fragment.
 |
|
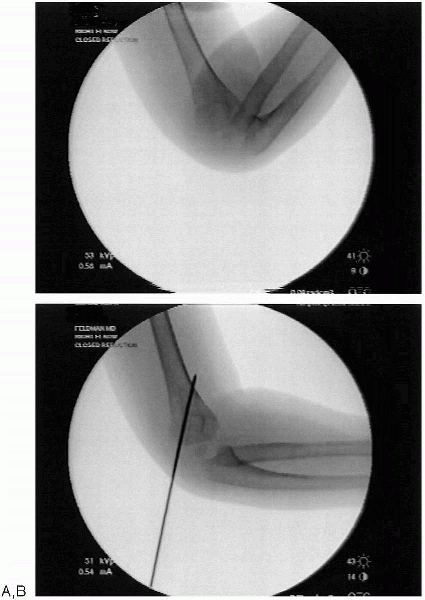
FIGURE 12-8. A: Lateral translation of supracondylar humerus fracture. B: Post reduction in extension (right elbow).
|
and III fractures. After closed reduction is achieved, 0.062-inch
K-wires are introduced under image intensification control to secure
the reduction.
fragment and should pass through the medial and lateral columns, cross
proximal to the fracture site, and penetrate the opposite cortices (Fig. 12-10).
In the coronal plane, the pins should be oriented 30 to 40 degrees to
the long axis of the humerus so that they are fixed in the center of
the supracondylar columns. Less stable fixation is achieved when the
pins cross at the fracture site.
-
![image]()
The lateral K-wire is introduced first while the surgeon holds the
elbow in acute flexion while palpating the lateral condyle. Under image
intensification, a lateral column view can be used to ensure that the
K-wire enters the cortex distal to the fracture. Confirmation of the
position of the pin is performed on the lateral view. The medial cortex
must be penetrated to achieve adequate stability. A
second lateral pin should be inserted more medial and this pin may go
through the olecranon fossa and then through the medial cortex. The
pins should be slightly convergent proximal to distal (Fig. 12-4). This
P.131may be the only fixation that is required, or one can insert a medial
pin for added fixation if the fracture is noted to be unstable on
fluoroscopy.For
the preferred cross-wire fixation, insertion of the lateral pin first
allows the surgeon to introduce the medial pin with the elbow
maintained in less than full flexion, thus reducing potential injury to
the ulnar nerve.![image]()
The thumb of the left hand of the (right-handed) surgeon palpates the
inferior edge of the medial epicondyle and drops into the ulnar groove
to palpate the ulnar nerve before the medial K-wire is introduced. The
medial pin begins at the center of, or anterior to, the medial
epicondyle and is directed from anteromedial to posterolateral. As
reported in clinical studies, the ulnar nerve is at risk during
placement of the medial pin (Fig. 12-11).
 |
|
FIGURE 12-9. Post reduction lateral.
|
 |
|
FIGURE 12-10. A: Demonstration of lateral column closed reduction. B: Pin fixation of lateral column.
|
 |
|
FIGURE 12-11. Medial pin being inserted. Note anterior to posterior direction on lateral film.
|
four views (AP, lateral, internal oblique, and external oblique) to
confirm reduction. Motion at the fracture site should be evaluated
under image intensification (Fig. 12-12). Following acceptable reduction, the pins are cut and bent over to facilitate easy removal on follow-up.
 |
|
FIGURE 12-12. A: Post reduction anteroposterior with pins crossing above the fracture. B: Post reduction lateral.
|
 |
|
FIGURE 12-13. Post surgical splint in 60 degrees of elbow flexion.
|
amount of flexion. This is determined by the degree of swelling. No
pressure on the antecubital fossa skin or soft tissue is allowed. If
the arm is very swollen one may immobilize the arm in as little as 20
to 30 degrees of flexion. The forearm is in neutral position.
Remember that the pins not the splint are maintaining reduction. The
arm is wrapped with generous padding that may then be split, and the
plaster splint is appropriately secured with a loose Ace bandage. Care
must given to secure the splint to allow for postoperative swelling (Fig. 12-13).
The patient often goes home the next day if he or she is comfortable.
At 1 week, AP and lateral radiographs are obtained to ensure that the
reduction has been maintained. If the patient was placed in a splint
with little flexion, the splint can be changed at this time. The
patient is then seen again 2 weeks later (3 weeks postoperatively), and
radiographs are obtained with the splint off. If there is evidence of
healing, which is almost uniformly the case, the pins are removed in
the office. The parents are asked to encourage the child to flex and
extend the elbow but not to do it for the child, that is, no assisted
or passive range of motion. A sling or removable splint may be used to
protect the child when he or she is playing or in danger of injury. For
the most part immobilization is not used. The child is then seen again
3 weeks later to assess range of motion. Most often, radiographs are
not needed at that time, and physical and occupational therapy are
rarely needed. Further follow-up depends on the outcome and specific
case.
