Spine I: Staying Out of Trouble with Scoliosis in Children
|
|
complications in spine surgery in particular can be catastrophic for
the patient and family.
doctor’s primary job at the initial consultation is to find out if
there is an underlying cause of the scoliosis. There are many clues on
history, physical examination, and radiographs that scoliosis may not
be idiopathic (see Red Flags box). The authors have seen a child with each one of the listed clues in which the scoliosis was not idiopathic.
-
Back pain that is well-localized and constant
-
Pain that is becoming progressively worse over time (Fig. 19-1)
-
Feelings of weakness or clumsiness
-
Gait abnormality
-
Episodes of bowel or bladder incontinence
-
Ejaculation problems
-
Foot deformity, particularly unilateral
-
A lack of rotational asymmetry on the Adam’s forward bending test
-
A lack of thoracic
kyphosis is normal in idiopathic scoliosis—if there is increased
kyphosis be suspicious that the curve is not idiopathic. This point is
very important and easily overlooked (Fig. 19-2) -
Tight hamstrings: popliteal angle over 50-60 degrees (Fig. 19-3)
-
Abnormal pattern: not right thoracic, and/or left lumbar
-
Unequal or abnormal reflexes
-
Widened pedicles suggest diastematomyelia (Fig. 19-4)
-
Kyphosis (Fig. 19-2)
-
Atypical curve pattern (Figs. 19-1, 19-5, and 19-6)
-
Lack of vertebral rotation (see Figs. 19-5 and 19-6)
-
Rapid curve progression: >1 degree/month
-
Absent pedicles: (winking owl sign) infection or tumor
-
Limb length discrepancy (Fig. 19-7)
-
Sharp curvature: look for congenital scoliosis or neurofibromatosis (Fig. 19-8)
-
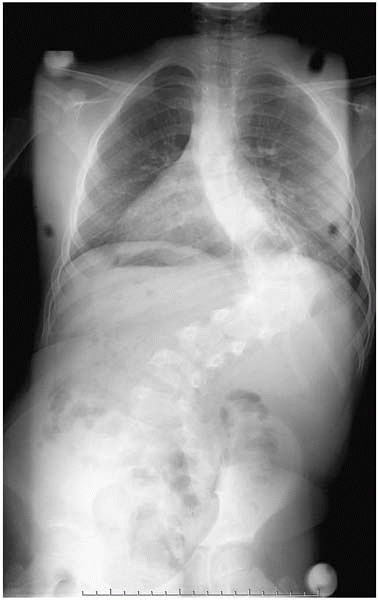
Remember first to look beyond the spine on radiographs for hidden trouble (Fig. 19-9)
important information— that a family member may have scoliosis, or the
child is complaining of back pain, etc. Often the referring doctor’s
diagnosis of scoliosis is not what is bothering the patient. If a
family member is said to have scoliosis, a quick Adams forward bending
test of the family member provides useful information. It gives the
surgeon more confidence that the patient’s scoliosis is more likely to
be idiopathic, though Dr. Emans points out the pitfall of incorrectly
assuming the child has AIS. We still must look for other causes of
scoliosis in the child. Looking at the parent is useful for explaining
the consequences of mild disease and usually makes the family member
feel better when you rule out significant scoliosis. Epidemiologic
studies tell us that back pain in early adolescents begins to approach
that seen in adults, so this should not raise a red flag unless it is
abnormal pain (positive finger test, night pain, pain which is not
activity related, etc.; see Chapter 20 on back
pain). Of adolescents with known idiopathic scoliosis, 23% present with
back pain, and 9% complain of back pain during the course of
observation.1
 |
|
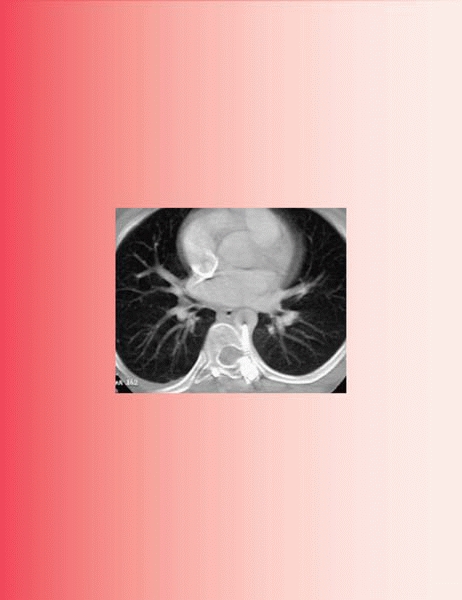
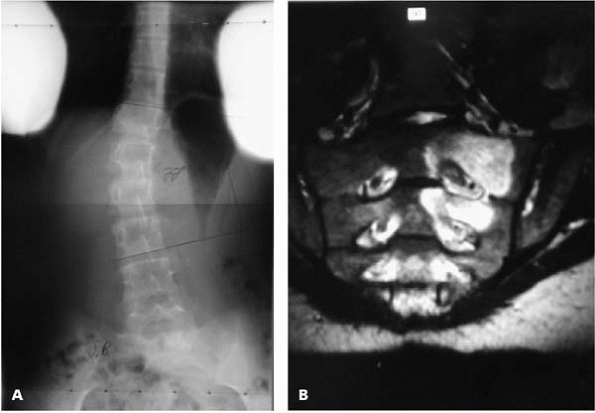
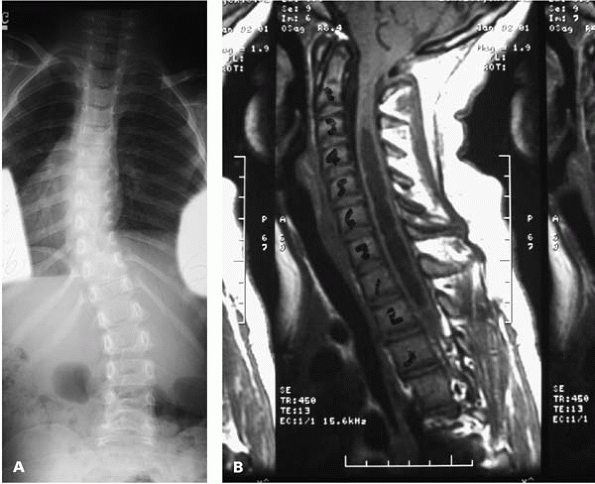
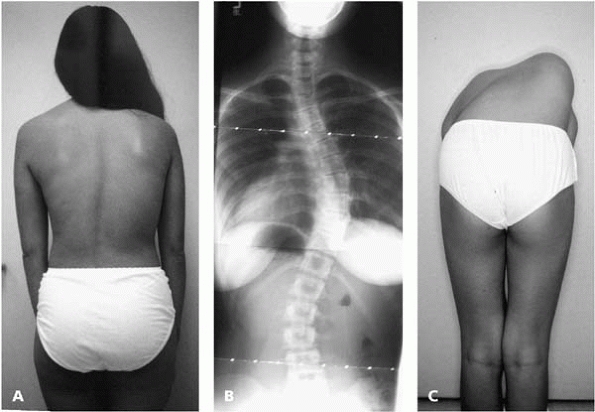
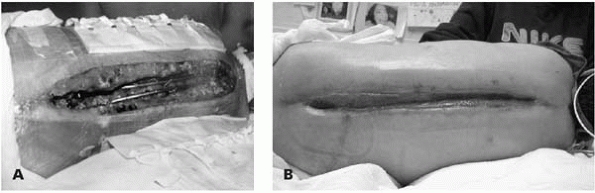
▪ FIGURE 19-1 (A)
Twenty-two degrees of scoliosis in a 12-year-old girl with constant back pain and popliteal angles of 90 degrees, suggesting tight hamstrings and nerve root irritation. (B) MRI reveals increased signal, which proved to be a osteoblastoma at biopsy. |
 |
|
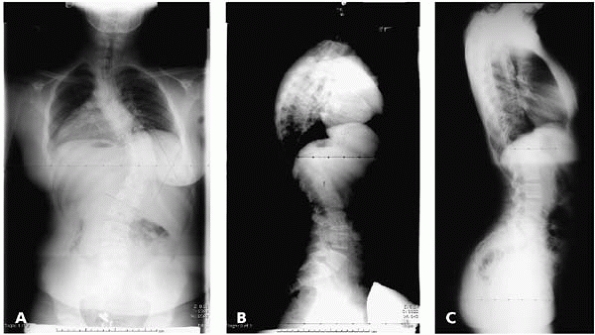
▪ FIGURE 19-2 (A)
AP radiograph of this 12-year-old girl may raise a suspicion of her condition being slightly atypical for idiopathic scoliosis as the apex is a bit low. (B) The lateral view of the girl shows 58 degrees of kyphosis. While this much kyphosis in an otherwise normal child is not alarming, in the setting of scoliosis this raises a red flag, suggesting the scoliosis may not be idiopathic. An MRI is indicated in that circumstance. MRI revealed a Chiari malformation and a large syrinx. (C) A lateral radiograph of a patient with adolescent idiopathic scoliosis. In contrast to the “normal” sagittal profile, a complete lack of kyphosis, or even slight thoracic lordosis, is not uncommon in idiopathic scoliosis, and is generally not considered a red flag for an underlying disorder. |
 |
|
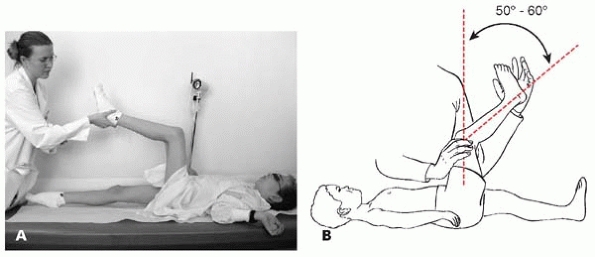
▪ FIGURE 19-3 (A,B) Tight hamstrings. The popliteal angle may be considered positive if the angle is >50-60 degrees.
|
 |
|
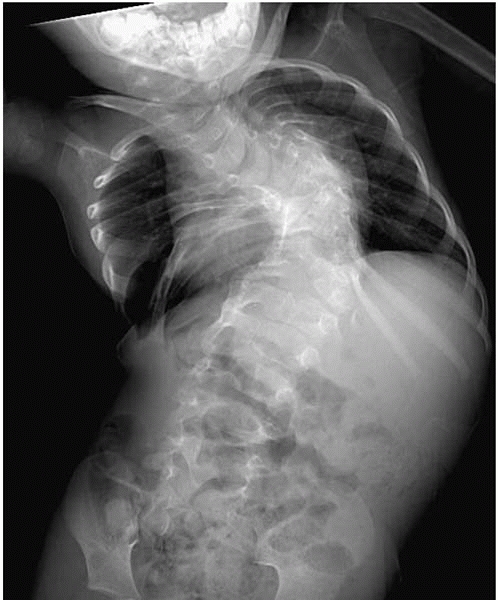
▪ FIGURE 19-4
In addition to the multiple congenital vertebral anomalies, note that the pedicles are wider at L1 than L5. Widened pedicles suggest diastematomyelia, which was confirmed with MRI and CT. A bony spicule is not always appreciated on radiographs as the diastematomyelia may be predominantly cartilaginous, especially in young children. Prior to any surgery to correct spinal deformity, removal of the diastematomyelia should be considered to prevent tethering of a split cord or nerve roots over the diastematomyelia, which may lead to neurologic injury. This 16-month-old child with congenital scoliosis and fused ribs is being considered for a vertical expandable rib prosthesis. |
 |
|
▪ FIGURE 19-5 (A)
Radiograph of a 14-year-old girl. The 26-degree left thoracic scoliosis is an atypical curve pattern for idiopathic scoliosis. The lack of significant vertebral rotation on this radiograph also suggests that this curve may not be idiopathic. On physical examination, a lack of rotatory asymmetry and an asymmetric umbilicus reflex were present as well, both suggesting that the curve may not be idiopathic. (B) MRI demonstrated a significant syrinx of the cervical and thoracic spine. |
 |
|
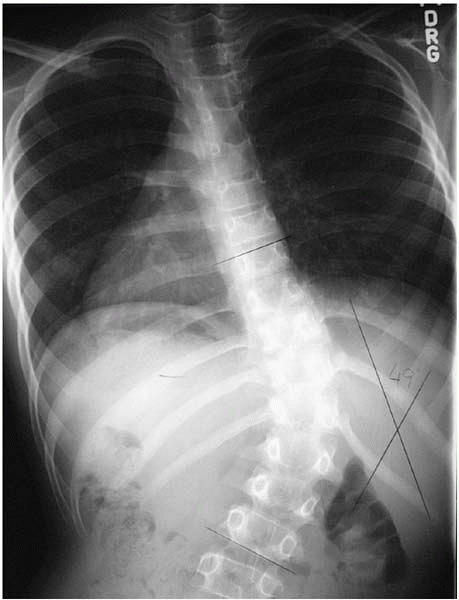
▪ FIGURE 19-6
Age 10 year old boy with 49 degree scoliosis. Note there is no rotation of the vertebrae, and an atypical right thoracolumbar apex. MRI revealed a significant syrinx the entire length of the thoracic spine. |
 |
|
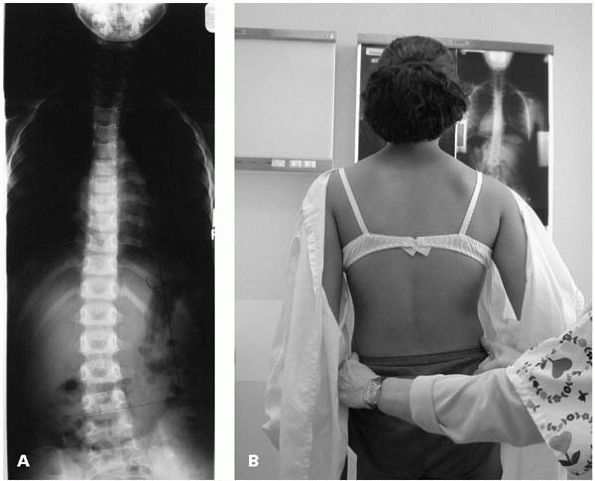
▪ FIGURE 19-7 (A)
Scoliosis may be compensatory for a leg length discrepancy. This patient was referred for consultation for her scoliosis with the radiograph shown in Fig. 19-5A. (B) By placing one’s fingers on the top of each iliac crest a limb length discrepancy was suggested, and was radiographically confirmed at 1.2 cm by scanogram. |
 |
|
▪ FIGURE 19-8 This curve has sharp angulation, which provides a clue to the patient’s underlying diagnosis of neurofibromatosis.
|
 |
|
▪ FIGURE 19-9
Remember to look beyond the spine on each radiograph. The need for this is aptly demonstrated here: the child’s right hip was noted to be at risk (arrow). This is easy to overlook during a scoliosis evaluation, but may be made to appear obvious to a jury years later. |
patient is standing. This is particularly true in double major curves,
in which curves over 50 degrees may add up to a rather straight torso (Fig. 19-10).
The rotational asymmetry of the spine, however, will be easily
appreciated in the Adam’s forward bending position. Stay out of trouble
by never considering an examination of the spine to have been done
unless rotational asymmetry has been evaluated. If on Adam’s forward
bending test the prominence is on the “wrong” side (curve concavity)
the curve is usually not structural, but compensatory for a leg length
discrepancy. A quick way to test for pelvic obliquity, which is most
often caused by a leg length discrepancy, is by placing the examiner’s
fingers on the iliac crests (see Fig. 19-7B).
Pelvic asymmetry may result from causes other than a leg length
discrepancy such as a dislocated hip, hip abduction or adduction
contractures, or previous Salter osteotomy. For significant pelvic
obliquity in the standing patient, a scanogram may provide more
information. And, of course, the importance of a neurologic examination
in evaluation of the patient with scoliosis cannot be overemphasized
(see Chapter 2, 60 Second Neuro Exam).
 |
|
▪ FIGURE 19-10 Shortly after this photograph (A),
this young lady was runner-up Miss California. Note that her back does not appear grossly deformed when viewed from behind despite a 47-degree primary right thoracic scoliosis (B). In the Adams forward bending test her scoliosis is more easily appreciated (C). |
scoliosis than supine radiographs. Do not mistake this for progression.
You can verify the patient is standing by the air bubble in the
stomach, which is flat on the bottom (see Figs. 19-2, 19-5A, and 19-8).
When lateral radiographs are taken, if patients hold their arms
straight out in front of them (parallel to the floor) as appears to be
the standard
teaching
for radiology technicians, this results in a sagittal vertical axis
that is at least 3 to 4 cm more posterior than normal, and likely
changes the kyphosis and lordosis as well.2
By having the patients place their hands on their shoulders, with their
elbows pointing forwards, the arms will not be superimposed on the
spine, and the effect on sagittal contour will be minimalized. Bending
films can produce highly variable results depending on how they are
done (Fig. 19-11). Bending radiographs taken
supine or over a bolster will most likely demonstrate much less
curvature than standing radiographs. Explain to parents at the first
visit that there is up to 7 degrees of measurement error in
determination of the Cobb angle, so that parental focus on minor
changes of Cobb angle, and many minutes of discussion, could be avoided
in the future. In children ≤10 years of age with scoliosis in the range
of 20 degrees or greater, an MRI of the cervical, thoracic, and lumbar
spine is indicated to rule out intraspinal pathology.3,4
 |
|
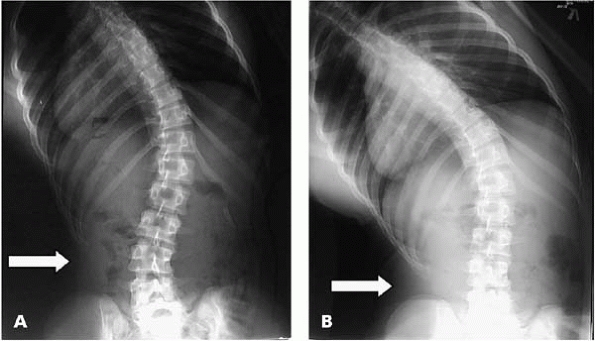
▪ FIGURE 19-11 (A)
The degree of effort a patient puts into bending during bending radiographs can make a significant difference in straightening of the curve (arrow). These two radiographs were taken minutes apart. The radiology technician gave routine instructions for a bending film. (B) The surgeon encouraged to bend as far as possible, and the film was repeated. Note that when there is maximal bending effort the lower ribs almost touch the iliac crest (arrow). |
important in predicting curve progression and length of bracing, but is
also highly variable. Hoppenfeld, et al.5
has recently shown that capping of the iliac apophysis is not the final
indicator for the end of spinal growth. After capping of the iliac
apophysis (Risser 4) there was continued growth in overall height of
75% of patients, with a mean of 1.8 cm in girls and 2.5 cm in boys. No
growth occurred in patients after iliac apophysis fusion (Risser 5) or
closure of either the rib epiphysis or proximal humerus growth plates.
them that there is a lot of misinformation in places such as the
Internet. Some of these “secret” oral formulas have led to metabolic
imbalances requiring emergent hospitalization for the child. More
commonly, though, the only negative consequences of unproven therapies
are a monetary loss for the families (tens of thousands of dollars for
some) and delay of standard treatment.
a disease. One way to stay out of trouble is to make certain you offer
bracing to patients, and document that you offered it. There have been
lawsuits taking the position that if bracing had been used, surgery
could have been prevented. When a patient’s curve warrants observation
or bracing, it is important to gain the family’s confidence that you
are “doing all that can be done,” but the curve may progress anyway.
Make certain the family understands that efficacy of a brace is quite
controversial, and usage in no way guarantees cessation or improvement
of curve. A reasonable approach is to say that, at best, the curve will
not progress, and that lasting improvement is highly unlikely. A
discussion of rebound effect6 (that
the curve will worsen after brace treatment is discontinued) best
occurs early in the course of brace treatment to prevent later feelings
of failure.
degrees of scoliosis, with growth remaining, and usually documented
progression of at least 5 degrees, though the last requirement may be
overlooked for immature patients with open triradiate cartilage or if a
strong family history is present. Take a radiograph in the brace to
evaluate correction, as a poorly-made brace might not be doing anything
of value.
understand enough about bracing to make suggestions. In patients with
thoracic hypokyphosis or lordosis, bracing may worsen the sagittal
contour. Pads should be placed laterally, to eliminate any anterior
force on the spine. Lateral radiographs of such patients should be
taken in the brace to make certain the thoracic spine is not pushed
more anteriorly in the brace.
stay out of trouble is a family conference in which the surgeon sets
expectations, completes an explicit and exhaustive consent process, and
shows models for optimum understanding. Complete correction of
deformity should never be guaranteed, and it is important to clarify
that the child’s back will never be completely normal. While it is our
experience, and that of others7 that
scoliosis surgery often relieves back pain, this outcome is
unpredictable and should never be an expectation. Families should
understand that a second operation is quite possible, and we suspect is
more likely than most surgeons admit to themselves.
-
Thoracic curve ≥50 degrees, or slightly smaller curves in patients with significant growth remaining.
-
Lumbar or thoracolumbar curves ≥45 to 50 degrees.
correction, and selection of levels to be fused are shrouded in
controversy and mysticism. We will attempt to share a few basic
principles and pitfalls.
-
Any surgery that disrupts the chest wall,
including anterior surgery in the chest and posterior thoracoplasties,
is detrimental to short-term pulmonary function, and may have long-term
implications as well. -
If there is a history of pulmonary
problems, pulmonary consultation and pulmonary function tests should be
considered for curves greater than 90 degrees or with significant thoracic lordosis. Pulmonary compromise in the postop period, which is most severe on postop day 3, can be predicted by preoperative PFTs.8 -
Early reports of success with new
techniques are often written by surgeons with a financial and/or
profession stake in the success of the technique or
instrumentation—waiting for confirmation by other groups may be
warranted.
-
For anterior instrumentation of the
thoracic spine, expect continued posterior growth to contribute to
about 15 degrees of increased kyphosis over time in 60% of patients who
are Risser 0 and 27% of patients Risser 1-5.9 -
For anterior instrumentation, single rods smaller than ¼-inch have a high incidence of breakage and should be avoided.
-
For posterior instrumentation there is
little place for a single rod, which has been shown to have an
unacceptably high failure rate.10,11 -
For selective anterior fusion of
thoracolumbar/lumbar curves in adolescents, the associated thoracic
curve can probably be left unfused if:-
The thoracic curve is less than 55 degrees, and bends out to 20 degrees or less
-
The thoracolumbar Cobb angle is at least 25% greater than that of the thoracic curve
-
-
For anterior instrumentation in the
lumbar or thoracolumbar spine, place screws as posterior as possible to
prevent kyphosis during compression. Also consider use of a structural
graft or cage, which will maintain lordosis and decrease stress on
screws. -
In patients with open triradiate
cartilages, surgery performed before or during the peak height velocity
is a strong predictor of the crankshaft phenomenon.12 -
Posterior sublaminar wires are safe and
strong in the treatment of idiopathic scoliosis. They are useful as
primary instrumentation or as a bailout if other fixation was not
optimal.13 -
Consider including an upper left thoracic
curve in a posterior spinal fusion if T1 is tilted high on the left on
the preoperative standing film, the left shoulder is high
preoperatively, the curve is greater than 35 degrees, bends out to less
than 25 degrees or has greater than 20 degrees of kyphosis from T2-T5. -
The use of pedicle screws instead of
hooks in the lowest level(s) may help improve correction and/or save a
level, with a smaller likelihood of pullout.14 -
When preparing a pedicle for screw
insertion, if it doesn’t feel just right, don’t use a pedicle screw.
Other anchors have been used effectively for years, and a misplaced
pedicle screw can cause lots of harm (Figs. 19-12, 19-13 and 19-14). -
Use only a pedicle hook finder with a
“stop” to prevent inadvertent entrance into the spinal canal. Paralysis
and lawsuits have been associated with pedicle hook finders without
stops (Fig. 19-15). -
In verifying vertebral level
intraoperatively, an AP image with the transverse process marked avoids
the pitfall of thinking you are on the more caudal vertebrae, as the
lower lamina shingles caudally over the next vertebra (Fig. 19-16). -
While conclusive, long-term data is
lacking, it is generally accepted that avoiding fusing down to L5, and
if possible L4, is beneficial long term in minimizing back pain. -
Similarly, maintenance of lumbar lordosis within and below instrumentation is likely to be beneficial long term.
 |
|
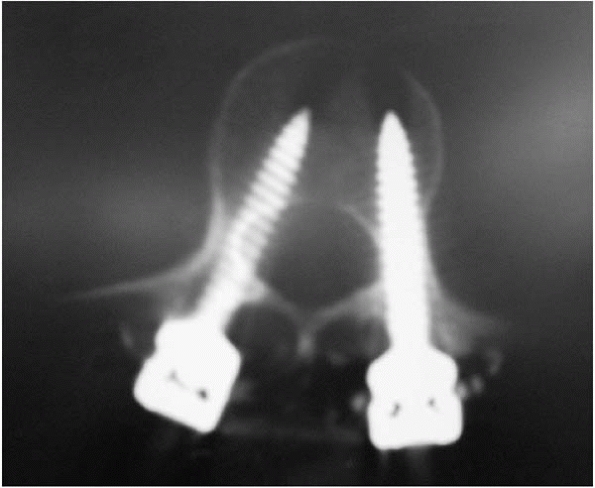
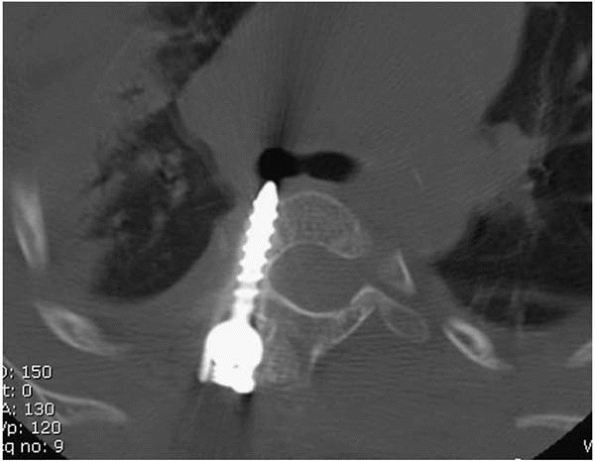
▪ FIGURE 19-12
Although penetration of pedicle screws are usually benign, in this case the child had nerve-root pain and paresthesias. Removal of screw was accompanied by immediate improvement of nerve root SSEPs and complete relief of symptoms. In the lumbar spine, palpating the pedicle from inside the canal with a Penfield #4 may help identify such a protrusion if you are uncertain when palpating from within the pedicle. |
 |
|
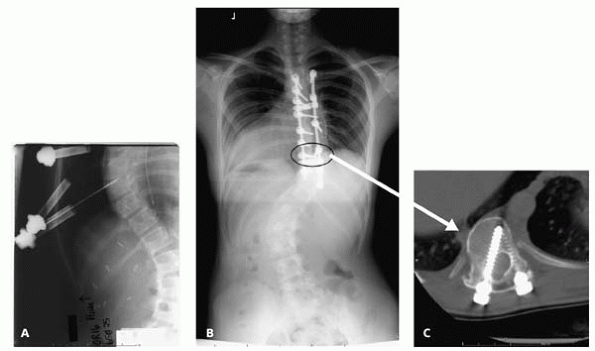
▪ FIGURE 19-13
Following surgery for idiopathic scoliosis this child had discomfort deep in the chest. The screw was removed and a bypass graft of the aorta was placed across the damaged part of the aorta. |
 |
|
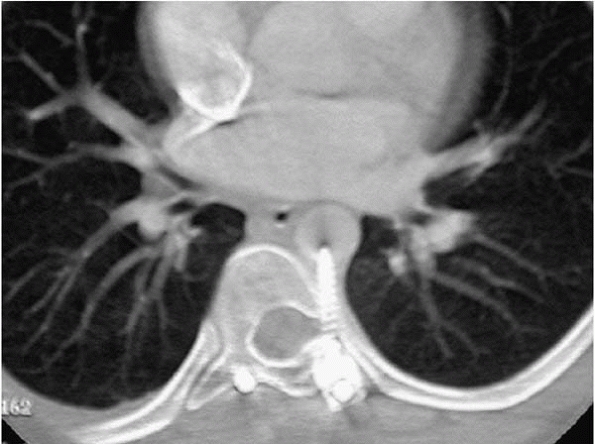
▪ FIGURE 19-14
The smallest pedicle screw in the set was 25 mm, which was too long for this 3-year-old, which resulted in impingement on the right mainstem bronchus. Either the screw could have been cut shorter with a bolt cutter or an alternative fixation could have been used. |
 |
|
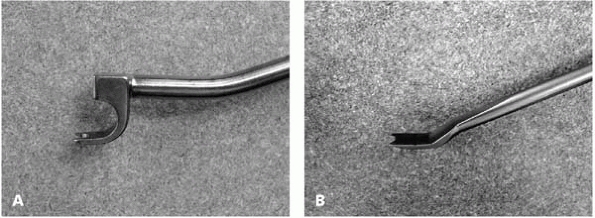
▪ FIGURE 19-15 Pedicle hook finders with stop (A) prevents excessive entrance into the spinal canal. Pedicle hook finder without stop (B).
|
 |
|
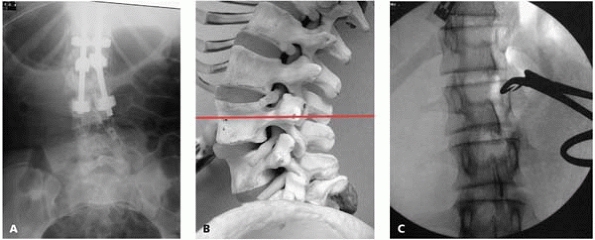
▪ FIGURE 19-16 (A)
In this case, the surgeon planned instrumentation to L3, and the intraoperative radiograph was misinterpreted as ending at L3. (B) This model demonstrates that when the lumbar spine with lordosis is viewed in an AP direction, the spinous process and the inferior lamina of the superior vertebra may appear superimposed on the inferior vertebrae. (C) Intraoperative marking of the transverse process rather than the spinous process or lamina may help avoid this error. |
-
Apex of kyphosis, usually T6-T8, will fall into more kyphosis
-
Apex of coronal curve, especially lumbar, will lead to decompensation
-
Below T2 or T3 for a
high left thoracic curve with the left shoulder high on exam, or the
left clavicle high on AP radiograph, or the left shoulder, will end up
high15 -
Thoracolumbar junction if it is kyphotic
-
Do not do selective
thoracic fusion if lumbar curve has significant rotation on clinical
exam (either supine or in Adam’s forward bending position); include
lumbar curve
make certain the patient’s abdomen is hanging free, as a shifted
bolster may increase venous pressure. When significant forces arise
during correction of large or stiff curves, waiting a few minutes
before the next maneuver takes advantage of the viscoelasticity of the
spine and surrounding structures, permitting stress on the implants to
decrease over time. Prior to beginning closure, ask yourself if you
have forgotten to do anything, and double-check final tightening of
implants (Fig. 19-17).
 |
|
▪ FIGURE 19-17 A systematic final tightening of all implants prior to closure may have prevented this implant failure.
|
has a negative pulmonary effect, the cosmetic and body-image
improvement can be substantial. This procedure may be explained to the
family as a way to get bone graft, as it has to come from somewhere,
with subsequent cosmetic improvement. It is important to set
expectations for this procedure that the rib prominence will improve,
but the back will never be “normal.”
incision in tissue that will develop into breast tissue can lead to
significant deformity of breasts. In newborns, breast tissue extends
vertically from the second or third rib to the sixth rib and from close
to the sternal edge medially, almost to the anterior axillary line
laterally. This is important for orthopaedic surgeons to be aware of as
thoracic insufficiency surgery is becoming more common in young
children. An example of deformity as a result this incision placement
can be seen in Fig. 19-18.
 |
|
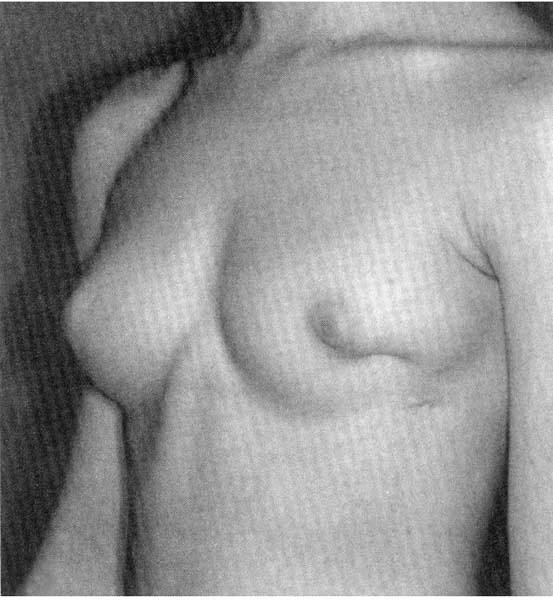
▪ FIGURE 19-18
This 16-year-old girl had a chest tube placed as an infant, with the resulting breast deformity. (Reprinted with permission from Rainer C, Gardetto A, Fruhwirth et al. Breast deformity in adolescence as a result of pneumothorax drainage during neonatal intensive care. Pediatrics. 2003;111(1):80-86. |
paraspinal muscles and latissimus in lumbar spine. Try to cut the ribs
as medially as possible, adjacent to the transverse process, or the
remaining rib will be prominent. Following rib resections, the
operative site may be filled with warm saline, and a Valsalva
maneuver
performed by anesthesia, with bubbles signifying entrance into the
chest. If so, make certain that a drain is place in the chest. Consider
placing a drain at the site, as the postoperative hematoma could lead
to a pleural effusion.
reductions in ulnar nerve somatosensory evoked potential (SSEP)
amplitude was observed in 18 limbs of 500 patients (4%). All resolved
with repositioning of the arm. Stay out of trouble by abducting the
shoulders no more than 90 degrees, padding the ulnar nerve at the
elbow, and considering monitoring of the ulnar nerve, though the last
suggestion is not common practice.16
fusion are evolving. Many studies on crankshaft phenomenon are limited
in that they generally rely on Cobb angle, while clinically rotation is
difficult to quantify. With this limitation in mind, it appears that
the best indication from the literature is to do an anterior fusion in
addition to a posteror fusion to prevent crankshaft if surgery is
performed before the peak height velocity12 (Fig. 19-19).
Practically, many times there is not sufficient data to determine peak
height velocity, so the triradiate cartilage becomes the second choice.
To stay out of trouble, discuss with family members ahead of time that
there is about a 40% chance of crankshaft if a posterior fusion is
performed before closure of the triradiate cartilage, and let them
participate in the decision.12,17 There is a potential role for pedicle
screw constructs in preventing crankshaft, but is not yet conclusively
proven.
 |
|
▪ FIGURE 19-19
This patient had a posterior fusion only at age 6 for a progressive scoliosis. Her shoulders are now 90 degrees rotated to her pelvis due to crankshaft. A concomitant anterior fusion in skeletally immature children may play a role in minimizing crankshaft. |
a combined procedure, the traditional recommendations of curves >70
degrees or >40 degrees on bending as indications for an anterior
procedure are no longer valid. With current techniques, larger and
stiffer curves can be successfully treated with posterior surgery
alone, though the limits of this approach have yet to be defined and
are probably somewhat surgeon dependent. Stay out of trouble by doing
what you are comfortable with, and evolving to doing bigger and stiffer
curves posterior only in an incremental fashion. Thoracoscopic release
and fusion may be less of a pulmonary hit to the patient, but this is
still an invasive procedure whose risks must be weighed against the
benefits.
cord monitoring should be employed as well as an early warning, and
thus allow corrective steps earlier. SSEPs monitor primarily the
posterior columns, and changes may occur up to 20 minutes after an
insult.18
occurred and could prove disastrous if SSEPs are used alone.
Motor-evoked potentials (MEPs) provide almost immediate feedback on
neurologic changes, but have been found to be more difficult to perform
in many centers. In terms of staying out of trouble, more monitoring is
better.
-
Ask if there has been a change in inhalational agents—simply decreasing the inhalational agents may cause signals to return.
-
Verify electrode placements.
-
If signal loss
occurred immediately following correction maneuver, assume the
correction was causative and reverse the mechanical stress if it can be
done safely. -
Increase blood pressure.
-
Transfuse if hematocrit is low.
-
Perform wake-up test.
-
Solumedrol 30mg/kg bolus, and 6.5mg/kg × 23 hours.
-
This is controversial—the Journal of Neurosurgery is against steroids in trauma situations.
-
-
Verify that no instrumentation has moved into canal, e.g., upper pedicle hook may rotate into canal during rod rotation.
-
Release distraction, untwist wires, bend rods into less correction.
-
If all of above fails, remove instrumentation, if spinal stability will allow it.
greater likelihood than in adolescents that the scoliosis is not
idiopathic. In one center, of children ≤10 years of age believed to
have idiopathic scoliosis with curves >20 degrees, an MRI of the
entire spine revealed intraspinal anomalies in 20% of children 3 to 10
years of age and up to 50% of children <3 years of age.3
Even though young children may require anesthesia or sedation to lie
still during an MRI, we suggest staying out of trouble by getting an
MRI in young children with presumed idiopathic scoliosis in curves
>20.
with early onset scoliosis have quite significantly increased
mortality, which becomes apparent at age 40 to 50, primarily due to
respiratory and cardiovascular causes.20
Treating the chest wall deformity, and maximizing the space available
for the lungs should be the primary goal in the treatment of young
children with scoliosis, with correction of spinal deformity as the
secondary goal. Unfortunately, treatment options (including bracing,
growing rods, and titanium ribs) are all controversial, thus not great
solutions. Keeping parents informed of all options (including referral
to centers with large populations of young children with scoliosis) and
not missing underlying problems is the best way to keep out of trouble.
screw as an anchor, as it is possible to erode distally over time with
potential damage to nerve roots. One may also want to consider use of
titanium instrumentation for future imaging, including CTs to assess
implant location.
surgeons view the young child with scoliosis. Fusing the scoliotic
spine of a 2-year-old may lead to a straight child and good radiograph
in the short term; however, the long-term pulmonary implications of an
adult with a thoracic spine the length of that of a 2-year-old is
clearly troubling (Fig. 19-20).
growing instrumentation (growing rods or vertical titanium rib
prosthesis) is not yet clear, common sense suggests it is likely to be
better than performing a long fusion in a young child (Fig. 19-21).
|
|
 |
|
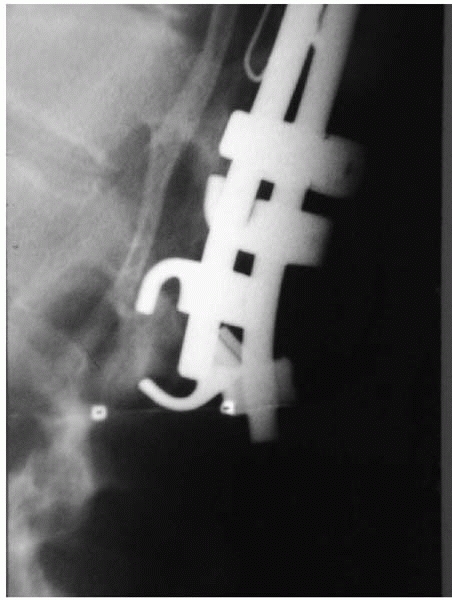
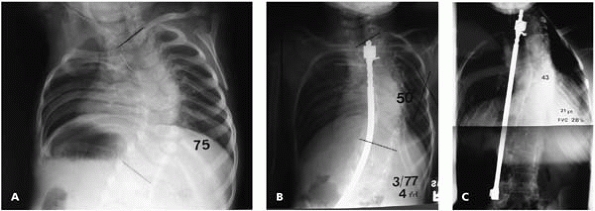
▪ FIGURE 19-20 (A) Radiograph shortly after birth of an infant with congenital scoliosis with a Cobb angle of 75 degrees. (B)
A spinal fusion with a Harrington rod was successful at improving the Cobb angle, as demonstrated by this radiograph at 4 years of age. (C) At age 21 this patient’s scoliosis correction had been maintained, but an inherent part of the “successful” spine fusion was a cessation of growth of the involved spine. The patient had a functional vital capacity of 28% at age 21. At age 25, the patient died after catching pneumonia. |
 |
|
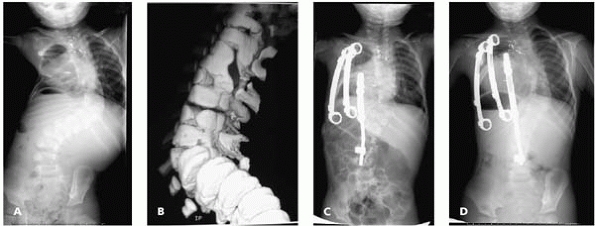
▪ FIGURE 19-21
A 2-year-old boy with a progressive 92-degree congenital scoliosis with multiple anomalies, including a hemivertebra opposite a multilevel unilateral bar. (A) Preoperative AP radiograph. (B) Three-dimensional CT. (C) Surgery included an opening wedge thoracostomy and placement of vertical expandable prosthetic titanium rib (VEPTR) devices. Note that the scoliosis is improved and the bilateral lung fields appear more symmetrical. The child gained 3 inches in height from the initial procedure. (D) At 3-year followup, following multiple lengthening procedures and an exchange of the hybrid device (rib-to-spine device), improvement of the scoliosis and deformed thorax is maintained. The scoliosis measures 51 degrees, and the child is playing on a soccer team. |
trouble by looking for associated abnormalities. The prevalence of an
intraspinal anomaly is approximately 40%. An MRI is warranted in a
child with congenital scoliosis who has signs or symptoms of a
neurologic problem, shows significant curve progression, or will be
undergoing surgery. Unlike children with infantile “idiopathic”
scoliosis, an MRI is not necessarily automatic as there is already a
known cause of the scoliosis—the congenital anomaly. Sixty one percent
of patients in one center had associated abnormalities affecting seven
systems. The most common abnormalities associated with vertebral
malformation were cranial nerve palsy, radial hypoplasia, club feet,
dislocated hip, Sprengel deformity, imperforate anus, and hemifacial
microsomia.27 Renal anomalies (about
20%) may be evaluated with an ultrasound; cardiac anomalies (about 12%)
may be evaluated at the discretion of the primary care physician, who
may order an echocardiogram.
-
Unilateral bar opposite a hemivertebra
(or a large unilateral bar without a contralateral hemivertebra) will
progress, so early treatment is indicated. -
Significant deformity from hemivertebrae amenable to resection, e.g., hemivertebrae at L5-S1.
-
Very large curve in a young child with resultant thoracic insufficiency.
hemiepiphysiodesis, with the hope that improvement may occur with
growth. A posterior-only fusion has been
shown
to be relatively successful in preventing crankshaft in children with
congenital scoliosis, with only 15% of cases showing >10 degrees
progression of Cobb angle. However, children in two subsets did not
fare so well: children ≤4 years of age or with curves >50 degrees
had an incidence of crankshaft of 36% and 33%, respectively.28
significantly and never need spine surgery. However, once progression
is confirmed, surgery should be performed before a major deformity
results. Traditional teaching is that no spinal instrumentation is
needed and that most of the curve improvement comes from the position
of the spine in the cast. With modern pediatric spinal instrumentation
systems, or cervical systems in the very small children, significant
correction of curve can be achieved. In our experience, a posterior
fusion or anterior-posterior hemiepiphysiodesis in the young child with
congenital scoliosis frequently does not prevent significant rotational
deformity from progressing despite an apparently solid fusion with
little change in Cobb angle. Though encouraging, it is too early to
tell if pedicle screw fixation may help prevent this progression of the
rotational deformity. Parents should be warned that the “hump” may get
worse with growth.
often achieve significant curve correction and cosmetic improvement via
movement through adjacent open discs. Brace treatment is not effective
for congenital scoliosis.
and anomalies, and useful for identifying otherwise unrecognized lamina
defects preoperatively. Stay out of trouble by exposing the spine
carefully as there are frequently unrecognized osseous defects in the
posterior elements, making an inadvertent plunge into the spinal canal
an all-too-real possibility. Exposure of a child’s spine with
congenital scoliosis is best not left to unsupervised surgeons in
training.
anecdotal evidence that performing the anterior and posterior
procedures on separate days may be associated with less complications
overall, including a decreased chance of neurologic injury. This may
never be proved conclusively due to large numbers needed and the rarity
of neurologic injury. However, in high-risk cases such as
hyperkyphosis, when extensive correction is anticipated, or anterior
blood vessels are ligated, it may be wise to perform the surgery in two
stages. When doing surgery in two stages, pay close attention to
nutrition and do not hesitate to begin parenteral nutrition.29
wheelchair—truncal balance is more important than magnitude of curve
correction. These children have a higher likelihood of pulmonary
complications; stay out of the chest, and do not take down the
diaphragm if the goal of truncal balance can be met with posterior
instrumentation alone. Progression of the curve above or below the
primary curve over time is much more likely in neuromuscular scoliosis
than idiopathic. Think of T2-pelvis as your default plan for
neuromuscular scoliosis, and only change if special circumstances
exist. We have seen many, many more children we wished were fused to
the pelvis at the first operation than those we wished were not fused
to the pelvis initially.
 |
|
▪ FIGURE 19-22 In children with neuromuscular and/or pulmonary problems the biggest issue we often face is nutrition.
|
It is really nice to know ahead of time that your patient with
camptomelic dysplasia is likely to have thin or missing lamina before
directing a Cobb in that direction. For neuromuscular children
nutritional status is overwhelmingly important; if in doubt, get a
nutrition consult or g-tube first (Fig. 19-22).
significantly increased bleeding hours into the surgical procedure.
Valproic acid, a seizure medication frequently used in children with
neuromuscular disease, has been shown to be associated with
significantly increased blood loss during spine surgery. Unfortunately,
routine laboratory tests of complete blood count, prothrombin time, and
partial thromboplastin time will not adequately screen for the
plateletmediated effects of valproic acid, so consider having the
neurologist change medications one month prior to a major elective
surgery.30,31
The hematology literature recommends caution for elective surgery, and
suggests perioperative use of DDAVP (desmopressin acetate) to increase
von Willebrand factor levels and improve platelet function as
appropriate in some cases.31
loss in children with neuromuscular disease undergoing spine surgery,
as well as the postoperative drainage.33,34 But be aware that a second exposure to aprotinin within 6 months is associated with a 5% risk of anaphylaxis.35
Although there is a lack of scientific evidence, anecdotal evidence of
many surgeons suggests that once cell saver is given, bleeding becomes
more significant. Consider not using cell saver in children with
neuromuscular conditions. Dr. Emans suggests considering administering
fresh-frozen plasma to children with neuromuscular conditions rather
than throwing out the cell saver.
completed and returning to the OR in a few days after the coagulopathy
resolves can be a life-saving decision. For the surgeon with less
experience in neuromuscular scoliosis surgery, this is difficult yet
particularly important.
of the risks and limited benefits in this population. Unfortunately,
many family members have expressed disappointment that their
nonambulatory child did not begin walking as a result of the spinal
fusion. Quote the families a 25% or greater risk of complications for
this surgery, including medical problems postop, and a significant risk
of death in the perioperative period.
that there is an infection. A small amount of drainage in the first few
days to weeks is unlikely to be an infection, though prophylactic oral
antibiotics may help prevent bacterial seeding through a draining
wound. Drainage, increasing pain, or progressive feelings of
generalized malaise months after surgery are highly suggestive of
infection. Do not be lulled into security
by a normal erythrocyte sedimentation rate (ESR) and c-reactive protein
(CRP) and lack of fever. This is common in long-standing spinal implant
infections.
fusion may be performed in the office, but a negative result does not
rule out an infection. The best information is from operative
evaluation, and at times these cultures will remain negative. If the
fusion appears solid at time of surgery, consider taking out all
implants (see Dr. Lenke’s opinion). Ongoing research suggests that when
only a partial implant removal is performed; it is likely that another
surgery will be needed in the future to remove the rest of the implants
for persistent infection.36
presents a patient whose spinal implants had to be removed. Despite the
fact that SSEPs returned rapidly to normal after loosening implants,
the patient had no movement of her feet during the wake-up test.
Implants were removed at that time, followed by decortication of the
spine and placement of iliac crest bone graft. The patient’s feet began
moving within 20 minutes of waking from anesthesia. At this point
options included instrumentation with less correction in 1 to 2 weeks
or a Risser cast; the family chose the latter. Note that even with a
significant residual curve radiographically, the patient’s appearance
was clinically quite acceptable and fusion stable.
in place. A single irrigation and debridement, with closure over
multiple drains (as one may clog) is usually adequate. Pay careful
attention to nutritional needs during this period. In problem cases a
wound VAC can be used as a last resort (Fig. 19-24).
typed and crossed, and available for irrigation and debridement of the
spine. There is usually more blood lost at time of implant removal than
at the initial surgery.
 |
|
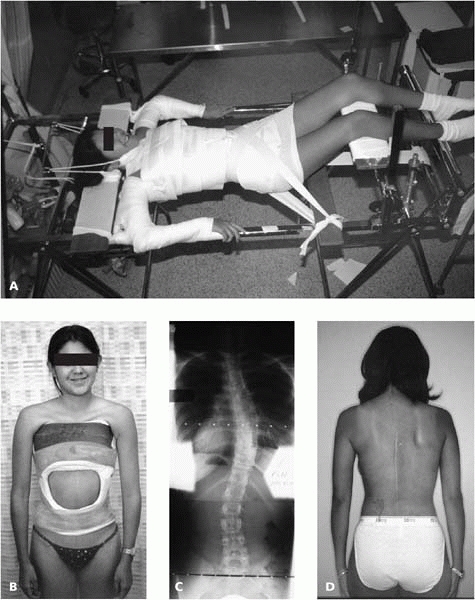
▪ FIGURE 19-23 (A) Patient on Risser Table for application of a well-molded cast. (B) The cast is worn for 6 months. (C) Oblique views help verify significant fusion. This radiograph shows residual curve present in fused spine. (D) One year following surgery.
|
 |
|
▪ FIGURE 19-24 (A)
Getting out of trouble with infection. Despite exemplary care, infections will occur at times in children with neuromuscular scoliosis. This child with mental retardation and quadriplegic cerebral palsy had over 90 degrees of scoliosis treated with T2-to-pelvis fusion. Infection occurred within months of surgery, and persisted after three attempts at irrigation and debridement. (B) Following use of a wound VAC, granulation tissue grew over the implant, allowing her instrumentation to remain in, and fusion to solidify. She required implant removal for clinically evident infection approximately 3 years later. |
pediatric orthopaedics in which technology is changing as rapidly as
spinal instrumentation. It is dangerous for a surgeon to see a new
technique at a meeting and immediately use this new technology on the
assumption that “if the presenting surgeon can do it, so can I” or from
the desire to keep up with the latest advances. Surgeons who develop
new technology often go through years of incremental advances and
training prior to clinical success and safety, which may not be obvious
from a presentation at a meeting. Fortunately, there are many training
opportunities available with the introduction of new technology.
Training with cadaver courses prior to operating on a live patient is
particularly helpful. Figure 19-25 presents a
case example of use of a technological advance before the surgeon was
experienced enough to implement it successfully.
 |
|
▪ FIGURE 19-25 (A)
A 13-year-old girl with idiopathic scoliosis (63 degrees supine) underwent thoracoscopic discectomy and fusion, followed by selective posterior spinal fusion with a pedicle screw construct. (B) Unfortunately, it appears the wrong fusion levels were chosen, the indication for an anterior fusion is unclear, and (C) not one pedicle screw was contained within the pedicle and vertebral body. New technology did not help this child. Note that when the tips of pedicle screws cross on an AP radiograph, chances are that at least one of the screws is in the spinal canal. |
-
For “idiopathic”
scoliosis, the surgeon’s primary job is to discover if there is an
underlying cause—be on the lookout for red flags. -
Do not bring a
patient to surgery until necessary preparation is complete, possibly
including an MRI, CT, pulmonary workup, nutritional optimization, etc. -
Children with nonidiopathic scoliosis often have more associated troubles, and require more attention.
-
If a pedicle screw doesn’t feel right, don’t use it.
MC, Stanford CF, Mahar AT, et al. Standing lateral radiographic
positioning does not represent customary standing balance. Spine. 2003;28(11):1176-1182.
P, Lenke LG, Bridwell KH. Incidence of neural axis abnormalities in
infantile and juvenile patients with spinal deformity: is a magnetic
resonance image screening necessary? Spine. 1998;23(2):206-210.
MB, Lenke LG, Szymanski DA, et al. Prevalence of neural axis
abnormalities in patients with infantile idiopathic scoliosis. J Bone Joint Surg Am. 2002;84(12):2230-2234.
AA, Haher TR, Brkaric M, et al. A multicenter study of the outcomes of
the surgical treatment of adolescent idiopathic scoliosis using the
Scoliosis Research Society (SRS) outcome instrument. Spine. 2002;27(18):2046-2051.
LP, Betz RR, Lenke LG, et al. The effect of continued posterior spinal
growth on sagittal contour in patients treated by anterior
instrumentation for idiopathic scoliosis. Spine. 2000;25(7):813-818.
HW, Hresko MT, Carlson J, et al. Comparison of single- and dual-rod
techniques for posterior spinal instrumentation in the treatment of
adolescent idiopathic scoliosis. Spine. 2000;25(15):1944-1949.
JM, Richards BS, Herring JA. A comparison of single-rod instrumentation
with double-rod instrumentation in adolescent idiopathic scoliosis. Spine. 2000;25(13):1680-1688.
FP, Boachie-Adjei O, Rawlins BA. Safety of sublaminar wires with Isola
instrumentation for the treatment of idiopathic scoliosis. Spine. 2000;25(6):691-695.
CL, Lenke LG, Bridwell KH, et al. The use of pedicle screw fixation to
improve correction in the lumbar spine of patients with idiopathic
scoliosis. Is it warranted? Spine. 1996;21 (10):1241-1249.
TR, Lenke LG, Graham EJ, et al. Correlation of radiographic, clinical,
and patient assessment of shoulder balance following fusion versus
nonfusion of the proximal thoracic curve in adolescent idiopathic
scoliosis. Spine. 2002;27(18):2013-2020.
CL, Bridwell KH, Lenke LG, et al. Posterior arthrodesis in the
skeletally immature patient. Assessing the risk for crankshaft: is an
open triradiate cartilage the answer? Spine. 1997;22(12): 1343-1351.
Y, Owen JH, Lenke LG, et al. Use of sciatic neurogenic motor evoked
potentials versus spinal potentials to predict early-onset neurologic
deficits when intervention is still possible during overdistraction. Spine. 1993;18(9):1134-1139.
Z, Lenke LG, Bolon SM, et al. Hypotension-induced loss of
intraoperative monitoring data during surgical correction of
scheuermann kyphosis: a case report. Spine. 2004;29(12):15.
K, Larsson S, Oden A, et al. Long-term follow-up of patients with
untreated scoliosis. A study of mortality, causes of death, and
symptoms. Spine. 1992;17(9):1091-1096.
S, Smith JT, White SK, et al. The volume of lung parenchyma as a
function of age: a review of 1050 normal CT scans of the chest with
three-dimensional volumetric reconstruction of the pulmonary system. Spine. 2004;29(18):2061-2066.
RM, Smith MD, Mayes TC, et al. The characteristics of thoracic
insufficiency syndrome associated with fused ribs and congenital
scoliosis. J Bone Joint Surg. 2003;85-A:399-408.
RM, Smith MD, Mayes TC, et al. The effect of opening wedge thoracostomy
on thoracic insufficiency syndrome associated with fused ribs and
congenital scoliosis. J Bone Joint Surg. 2004;86-A,1659-1674.
KL, Lonstein JE, Denis F, et al. The crankshaft phenomenon after
posterior spinal arthrodesis for congenital scoliosis: a review of 54
patients. Spine. 2003;28(3):267-271.
MA, Bridwell KH, Lenke LG, et al. Prospective randomization of
parenteral hyperalimentation for long fusions with spinal deformity:
its effect on complications and recovery from postoperative
malnutrition. Spine. 2001;26(7):809-817.
GD, Lin YX, Berge C, et al. Absence of bleeding complications in
patients undergoing cortical surgery while receiving valproate
treatment. J Neurosurg. 1997;87(2):252-256.
S, Farlo J, et al. Use of Aprotinin in Neuromuscular Spinal Surgery in
Children. 11th International Meeting on Advanced Spine Techniques,
Bermuda, 2004.
C, Skaggs D, et al. Management of infected spinal wounds in pediatric
scoliosis patients. Pediatric Orthopaedic Society of North America,
Ottawa, Canada, 2004.
LG, Betz RR, Harms J, et al. Adolescent idiopathic scoliosis: a new
classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001;83-A(8):1169-1181.