Arthroscopy of the Ankle
management of many synovial, chondral, and osteochondral lesions of the
ankle. Mastering this challenging technique requires a good
understanding of the regional anatomy and familiarity with the various
arthroscopic portals. Many potential complications are associated with
ankle arthroscopy. However, with proper indications and in the hands of
an experienced surgeon, this technique usually yields a high percentage
of excellent to good results, with the added advantages of minimal
morbidity, shorter hospitalization, and rapid recovery time for the
patient.
with the arthroscopic portals are two prerequisites for a successful
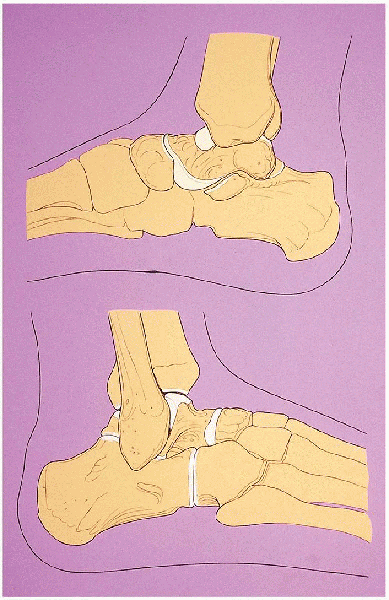
ankle arthroscopic procedure. Three bones constitute the ankle joint:
the tibia with its medial malleolus, the fibula with its lateral
malleolus, and the talus. The tip of the medial malleolus is located
approximately 2.0 cm distal to the joint line, and the tip of the
lateral malleolus is placed approximately 2.0 cm distal and 2.0 cm
posterior to the tip of the medial malleolus. The posterior margin of
the joint is situated approximately 0.5 cm distal to the anterior
articular margin (Fig. 31-1). The talar dome is
wider anteriorly than posteriorly and has a convexity in the sagittal
plane and a slight concavity in the coronal plane.
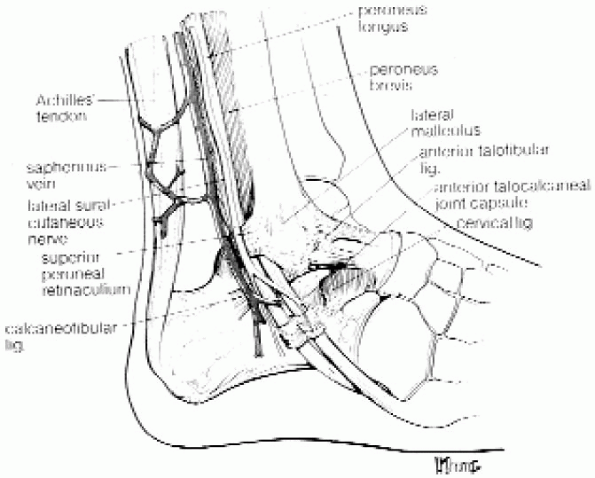
peroneal, and sural nerves—are present in the subcutaneous layer. The
deep layer contains, anteriorly, the tibialis anticus tendon, the
extensor hallucis longus, and the extensor digitorum longus. Between
the extensor hallucis longus and the extensor digitorum longus lie the
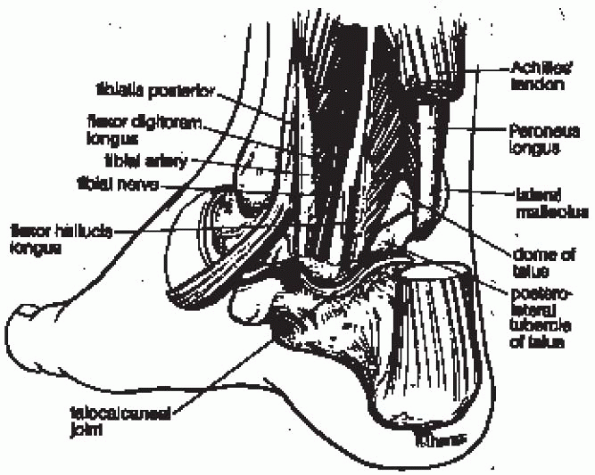
deep peroneal nerve and the dorsalis pedis artery. On the medial aspect
of the joint, within the tarsal tunnel, are found the posterior tibial
tendon, the flexor digitorum longus tendon, the posterior tibial artery
and nerve, and the flexor hallucis longus tendon. Laterally, the
peroneus brevis and peroneus longus lie behind the lateral malleolus
and insert on the tuberosity of the fifth metatarsal and onto the first
metatarsal and medial cuneiform, respectively (Figs. 31-2 and 31-3).
Medially, the deep and superficial fibers of the deltoid ligament give
stability to the joint. The superficial, extraarticular layer runs from
the anterior prominence of the medial malleolus and
inserts
onto the talus, calcaneus, spring ligament, and navicular. The deep,
intraarticular layer originates from the posterior aspect of the medial
malleolus and inserts on the posterior aspect of the talus. The lateral
malleolus anteriorly gives rise to the anterior talofibular ligament
and anteroinferior tibiofibular ligament and, more posteriorly, to the
calcaneofibular ligament, posterior talofibular ligament, and
posteroinferior tibiofibular ligament with its extension, the
transverse tibiofibular ligament.
 |
|
FIGURE 31-1. Bony components of the ankle joint.
|
 |
|
FIGURE 31-2. Lateral aspect of the ankle joint. (From Parisien JS. Arthroscopic surgery of the ankle. In: Arthroscopic surgery. New York: McGraw-Hill, 1988:260, with permission.)
|
 |
|
FIGURE 31-3. Medial aspect of the ankle joint. (From Parisien JS. Arthroscopic surgery of the ankle. In: Arthroscopic surgery. New York: McGraw-Hill, 1988:260, with permission.)
|
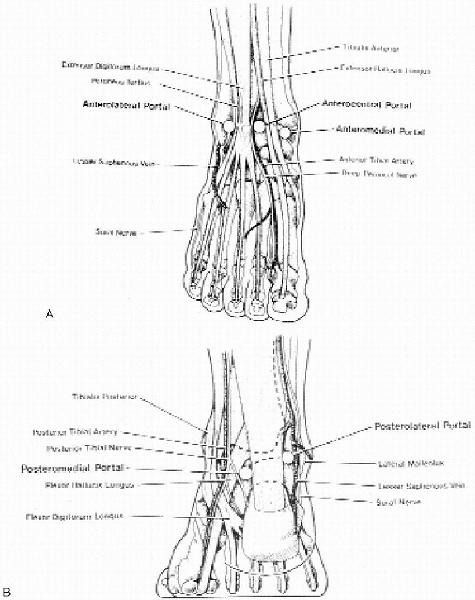
diagnostic and surgical arthroscopy of the ankle: the anteromedial, the
anterolateral, and the posterolateral. Two accessory anterior portals
can be used in addition to the primary portals. The anteromedial portal
is developed medial to the tibialis anticus tendon at the joint line
level. The saphenous vein and nerve are in proximity and located close
to the anterior aspect of the medial malleolus. The anterolateral
portal is located lateral to the peroneus tertius and extensor
digitorum longus at or a little proximal to the joint line. This portal
is in proximity to the terminal branches of the superficial peroneal
nerve (Fig. 31-4). This nerve bifurcates
approximately 6.5 cm proximal to the tip of the lateral malleolus into
the medial dorsal and intermediate dorsal cutaneous branches. Whereas
the medial sensory branches cross the anterior aspect of the ankle
overlying the common extensor tendon,
the
intermediate dorsal, the most lateral sensory branch, crosses the
anterolateral joint line over the common extensor tendon of the fourth
and fifth toes, making it vulnerable to injury while placing the
anterolateral portal.
 |
|
FIGURE 31-4. A: Anterior aspect of the ankle joint and the arthroscopic portals. B: Posterior aspect of the ankle joint and the arthroscopic portals. (From Parisien JS. Arthroscopic surgery of the ankle. In: Arthroscopic surgery. New York: McGraw-Hill, 1988:264-265, with permission.)
|
approximately 1.0 cm inferior to the primary anteromedial portal. The
accessory anterolateral portal is established approximately 1.0 cm
anterior to the tip of the lateral malleolus. The anterocentral portal,
located lateral to the extensor hallucis longus, is not recommended
because of the potential injuries to the neurovascular bundle (i.e.,
deep peroneal nerve and anterior tibial artery).
above the tip of the lateral malleolus, adjacent to the lateral border
of the Achilles tendon, to avoid injury to the sural nerve.
proximity to the posterior neurovascular structures. It passes between
the Achilles tendon and the posterior tibial neurovascular bundle. The
lateral and medial coaxial portals, which have been described in
hemophilic patients, are parallel to the bimalleolar axis of the ankle
joint. They allow complete synovectomy of the posterior compartment of
the ankle. Contrary to the conventional approaches, the coaxial
posterolateral portal is established posterior to the peroneal tendon
sheath, 1.5 cm to 2.0 cm proximal to the distal tip of the fibula.
Using a blunt-tipped obturator through the posterolateral portal, the
capsule is entered anterior to the posterior tibial tendon and behind
the posterior surface of the medial malleolus to develop the
posteromedial portal.
 |
|
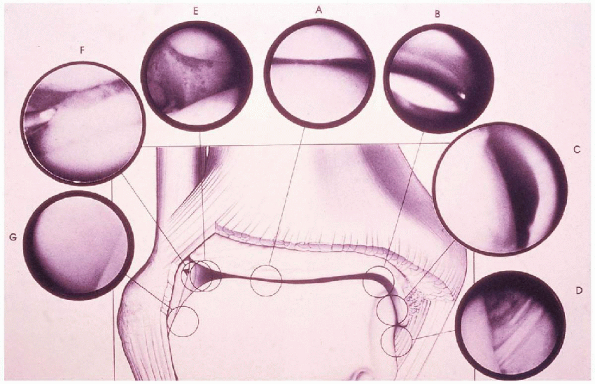
FIGURE 31-5.
Middle area of tibiotalar space (A), medial aspect of talotibial space (B), medial talomalleolar space (C), intraarticular structures: deep portion of deltoid ligament (D), lateral aspect of tibiotalar space (E), lateral aspect of joint (F), and lateral talomalleolar space (G). (From Parisien JS. Arthroscopic surgery of the ankle. In: Arthroscopic surgery. New York: McGraw-Hill, 1988:261, with permission.) |
Medially, the medial malleolus articulates with the corresponding
articular surface of the medial dome of the talus to form the medial
talomalleolar space. The deep portion of the deltoid ligament is seen
as it originates from the tip of the medial malleolus and runs
vertically to insert onto the medial surface of the talus. The medial
corner of the ankle, the area where the tibial plafond articulates with
the medial dome of the talus, has a notch (i.e., notch of Harty). The
anterior synovial recess is between the anterior tibial lip and the
superior insertion of the capsule onto the distal tibia. Within the
recess lies an irregular area of periosteum-covered bone that can be
the site of the so-called impingement exostosis. Laterally, the
anteroinferior tibiofibular ligament is seen along with the distal
aspect of the lateral tibial plafond and the lateral aspect of the
talus. Behind the anteroinferior tibiofibular ligament are located a
synovial recess and the tibiofibular articulation. The space between
the fibular and the lateral border of the talus forms the lateral
talomalleolar space. It extends distally to the anterior talofibular
ligament to form the lateral gutter. The anterior talofibular ligament
is seen as a capsular reflection extending
from
the tip of the lateral malleolus to the lateral aspect of the talus.
The anterior gutter represents the reflection of the capsule as it
attaches onto the neck of the talus anteriorly. It contains a synovial
recess and a bare area of talar bone not covered by articular
cartilage. With adequate distraction posteriorly, the posterior
inferior tibiofibular ligament can be seen as a strong band running
obliquely at a 45-degree angle from the tibia to the fibula. Inferior
to this ligament is located the transverse tibiofibular ligament.
With the arthroscope placed through the posterolateral portal, the
posterior capsular pouch can be visualized that is smaller than its
anterior counterpart. The posterior aspect of the deltoid ligament, the
posterior aspect of the medial talus and tibial plafond, as well as the
central and posterolateral aspects of the joint, can also be examined.
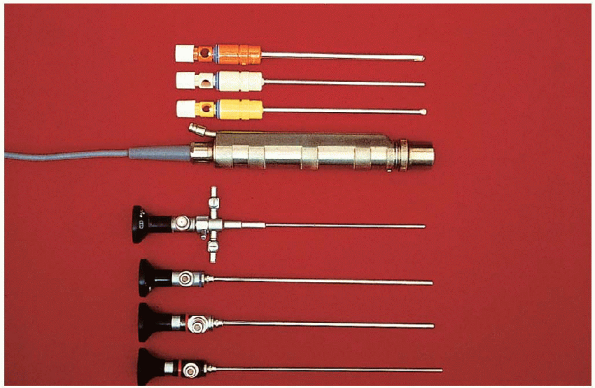
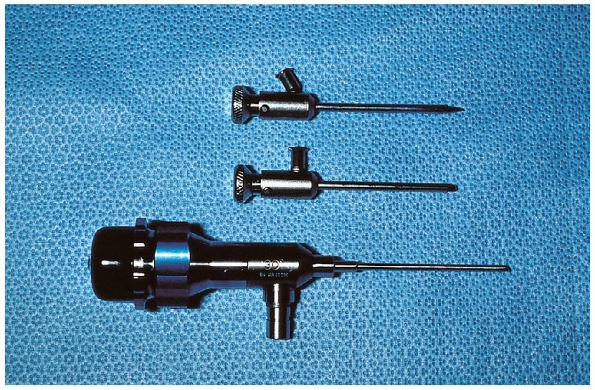
30-degree obliquity that can be used for ankle arthroscopy. The
70-degree arthroscope is also useful to visualize the posterior aspects
of the gutters and better evaluate a posteriorly located osteochondral
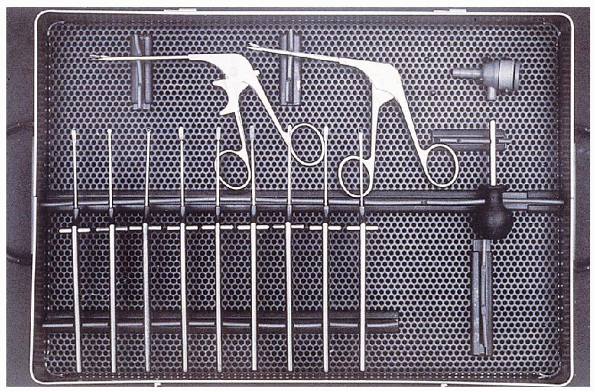
lesion of the talus. Small-joint instruments are necessary to cut,
retrieve, and repair (Figs. 31-6, 31-7 and 31-8).
small mosquito clamp, an 18-gauge spinal needle, a probe, a curved
dissector, a grasping forceps, a small basket forceps, various surgical
blades, small curettes, an osteotome, a rasp, and a small owl.
Motorized instruments (i.e., full-radius resector, cartilage cutter,
synovectomy blade, and small burrs) with various blades are available.
Biodegradable pins are also available to reattach viable osteochondral
lesions of the talus. An aiming device for adequate positioning of
guide wires or screws is also available.
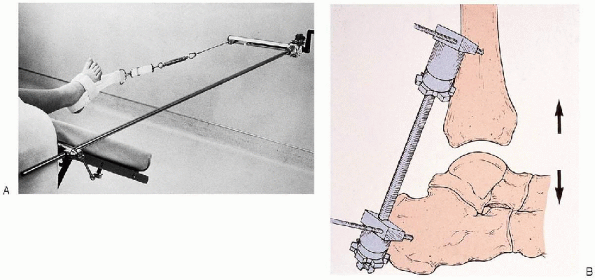
improve visualization of the joint. Two types of distraction technique
are available: the invasive and the noninvasive. For the invasive
technique, a 0.187-inch-diameter, threaded pin is drilled into the
lateral aspect of the tibia approximately 2 inches proximal to the
joint and behind the anterior tibial crest. A second pin is inserted
distal to the joint into the lateral aspect of the os calcis, 0.5 inch
anterior to its posterior border and 0.5 inch above its inferior
border. The pins do not have to penetrate the medial cortex of the
bones, and a pin cannula is used to protect the soft tissues while
drilling. The distractor is secured with the locking thumb nuts, and
distraction is applied until a joint space opening of 4 to 5 mm is
obtained at the beginning. Distraction up to 8 mm can be achieved
gradually. Distraction for more than 90 minutes is not recommended to
avoid stretching the ligaments. Potential complications of the invasive
technique are broken pins, pin tract problems, neurovascular damage,
and stress fractures.
 |
|
FIGURE 31-6. Shown are 4-mm, 30- and 70-degree arthroscopes (bottom) and motorized shaver with various blades (top).
|
 |
|
FIGURE 31-7. Shown is a 2.7-mm, short, 30-degree video arthroscope (bottom) with a trocar in the cannula (top).
|
sterile ankle distractor and a foot strap. Many noninvasive sets are
available on the market. Twenty-five pounds of traction for 1 hour are
recommended. With increased distraction time and force, symptoms of
paresthesia of the deep and superficial peroneal nerves may occur. The
noninvasive mode
is preferred to the invasive to avoid possible complications with the use of pins in the tibia and talus or calcaneus.
 |
|
FIGURE 31-8. Set of hand instruments, including baskets, knives, and curettes.
|
surgery of the ankle. However, when an increased fluid pressure is
desirable, an infusion pump can be used during the procedure. Careful
monitoring of the outflow system during the use of the pump is
mandatory to avoid extravasation of fluid into the foot and lower leg.
include soft tissue lesions and osteochondral lesions. The soft tissue
lesions include localized or generalized posttraumatic synovitis;
anterior or posterior soft tissue impingement from a chronic ankle
sprain; syndesmotic impingement due to trauma; some rheumatologic
disorders, such as rheumatoid arthritis; pigmented villonodular
synovitis; hemophilia; synovial chondromatosis; some infectious
synovitides; and some cases of arthrofibrosis.
 |
|
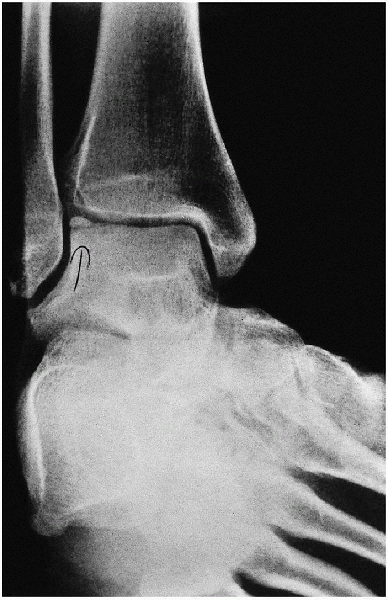
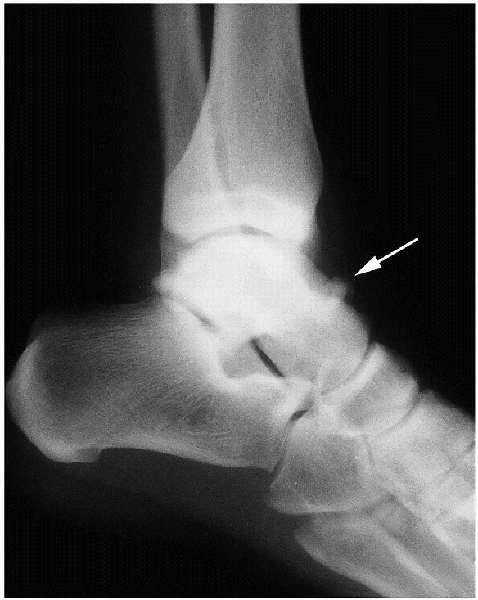
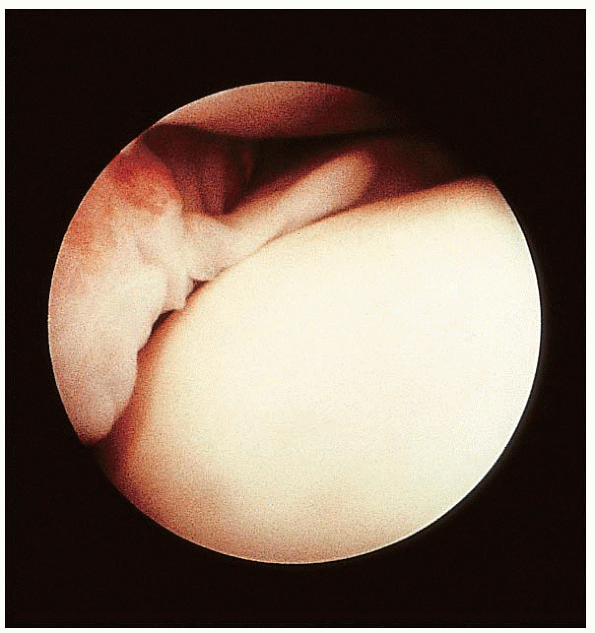
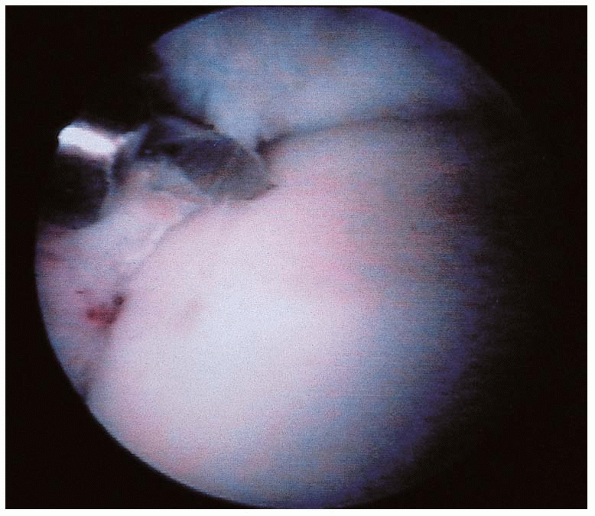
FIGURE 31-9. Osteochondral lesion on the medial aspect of the talus.
|
 |
|
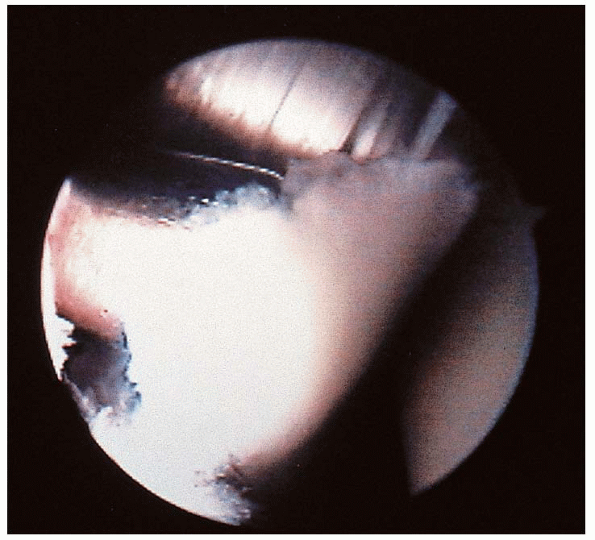
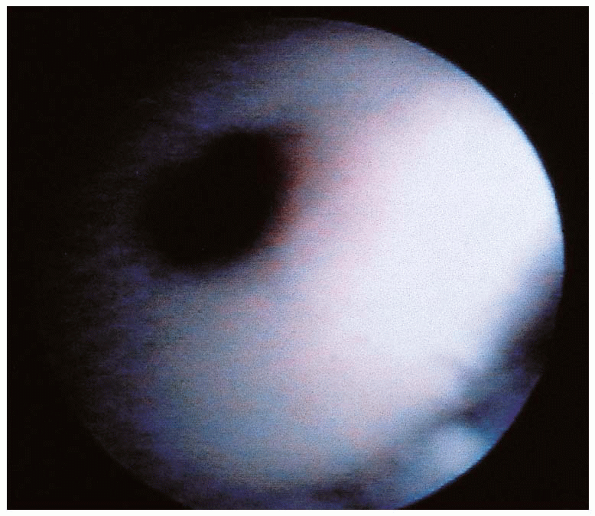
FIGURE 31-10. Osteochondral lesion on the lateral aspect of the talus.
|
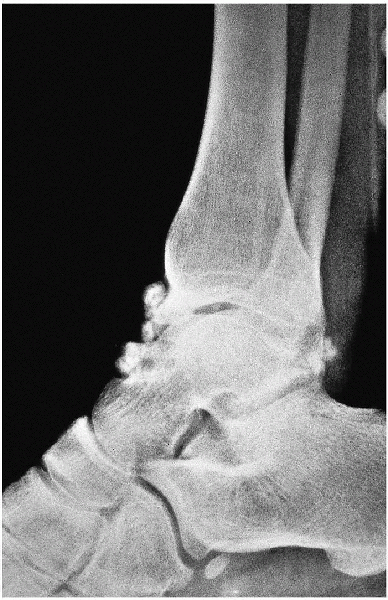
of chondral and osteochondral lesions of the ankle (i.e.,
osteochondritis dissecans of the talus, impingement exostosis, and
loose bodies (Figs. 31-9, 31-10, 31-11 and 31-12).
Arthroscopy is being used in some centers for the management of acute
ankle fractures to assess the articular surfaces, to obtain an anatomic
reduction, and to remove loose articular fragments and debris from the
joint. In chronic ankle fractures, arthroscopy has been very useful. It
allows identification and removal of loose chondral or osteochondral
loose fragments and the excision of scar tissue and proliferative
synovium.
minimizing the amount of soft tissue dissection, is an alternative to
an open procedure, provided that there is no preexisting major varus or
valgus deformity of the joint. The major benefits in the hands of the
experienced arthroscopist seem to be a better tolerance by the
patients, increased rate of fusion, and a low infection rate.
 |
|
FIGURE 31-11. Impingement exostoses of the tibial plafond and talus.
|
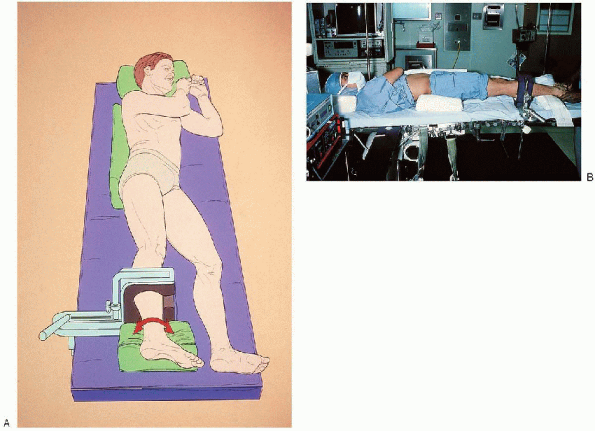
The leg is immobilized in a leg holder and the foot placed on a
well-padded box or a roll of sheet. With this setup, the anterior and
posterior aspects of the ankle are accessible with rotation of the leg.
After preparing and draping the extremity in the standard fashion, the
external landmarks are outlined with a marking pen: anterior tibialis,
peroneus tertius tendons, joint line, medial and lateral malleoli, and
superficial peroneal nerve branches.
18-gauge needle medial to the tibialis anticus tendon. The joint is
distended with normal saline solution. While
palpating and retracting the tendon with the thumb of the opposite
hand, a vertical skin incision is made with a no. 11 blade. A small
mosquito clamp is used to dissect the subcutaneous tissue down to the
capsule. The blunt trocar with the arthroscopic cannula is
inserted into the anterior pouch of the ankle joint. From the
anteromedial portal, the joint is visualized. The scope is then
removed, and the blunt obturator is reinserted into the joint to
develop the anterolateral portal lateral to the peroneus tertius and
extensor tendons. This anterolateral portal is
close to the intermediate branch of the superficial peroneal nerve.
This nerve can be seen or palpated by placing the ankle in forced
inversion. Visualization also can be achieved by means of
transillumination. With the superficial peroneal nerve precisely
localized and under constant observation, the skin is tented with the
blunt obturator of the arthroscope. A vertical incision is made over
the tip of the obturator for the placement of a small cannula into the
joint through this newly created anterolateral incision (Fig. 31-14). The posterolateral portal may be used for inflow, if necessary. The 18-gauge needle can be used close
to the Achilles tendon, 2.0 cm proximal to the tip of the lateral
malleolus, to obtain a backflow before making a vertical skin incision
and using the curved mosquito clamp to dissect the subcutaneous tissue.
 |
|
FIGURE 31-12. Loose bodies of the ankle joint.
|
 |
|
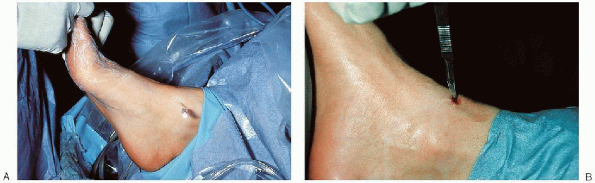
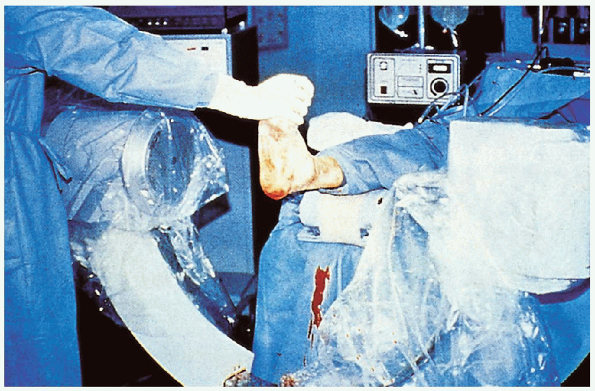
FIGURE 31-13. A: The illustration shows positioning for ankle arthroscopy. B: The photogaph shows positioning for ankle arthroscopy.
|
 |
|
FIGURE 31-14. A: A spinal needle is placed medial to the tibialis anterior to distend joint capsule with normal saline. B: Vertical skin incision is made after removal of the needle.
|
 |
|
FIGURE 31-14. Continued. C: A small mosquito clamp is used to spread the soft tissue down to the capsule. D: An arthroscope is placed through the anteromedial portal. E: Development of the anterolateral portal.
|
and soft tissue lesions can be addressed with the two anterior portals.
Débridement of localized, nonspecific synovitis and excision of scar
tissue can be done with a motorized shaver. The anterolateral soft
tissue impingement (which can be caused by the so-called meniscoid
lesion or the presence of thick, inflamed synovial tissue in the
lateral gutter or a separate fascicle from the anterior tibiofibular
ligament) can be treated the same way (Figs. 31-15, 31-16 and 31-17).
Syndesmotic impingement due to scarring and inflammation in the area of
the anterior tibiofibular ligament and distal tibiofibular joint can
benefit from arthroscopic débridement. After closure
of
the portals with 3-0 nylon sutures, a compression dressing is applied
for 2 to 3 days. Range-of-motion exercise is encouraged very early.
 |
|
FIGURE 31-15. Synovial impingement in the anterolateral aspect of the right ankle.
|
 |
|
FIGURE 31-16. Meniscoid lesion on the anterolateral aspect of the ankle.
|
 |
|
FIGURE 31-17. A fibrotic band on the anterior aspect of the ankle causing impingement.
|
generalized with posterior involvement, distraction may be helpful to
allow complete visualization. The use of the tourniquet with an
infusion pump may speed the procedure. In general, if the ankle joint
is tight and the pathology generalized or localized posteriorly, a
noninvasive system can be used for the distraction before the start of
the procedure (Fig. 31-18). The noninvasive
clamp is attached to the table, and soft tissue distraction is obtained
with the sterile strap over the dorsum of the foot and around the heel.
and a suction Hemovac is used before closure. A compression dressing is
applied, and ambulation with crutches is advisable for the first 7 days.
 |
|
FIGURE 31-18. A: Noninvasive distraction. B: Invasive distraction
|
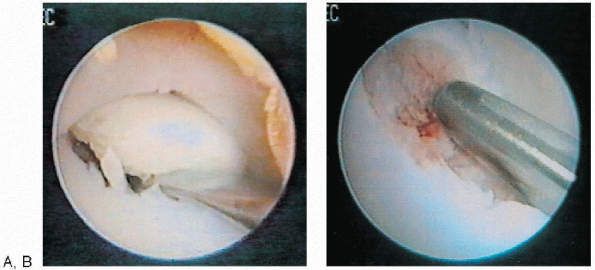
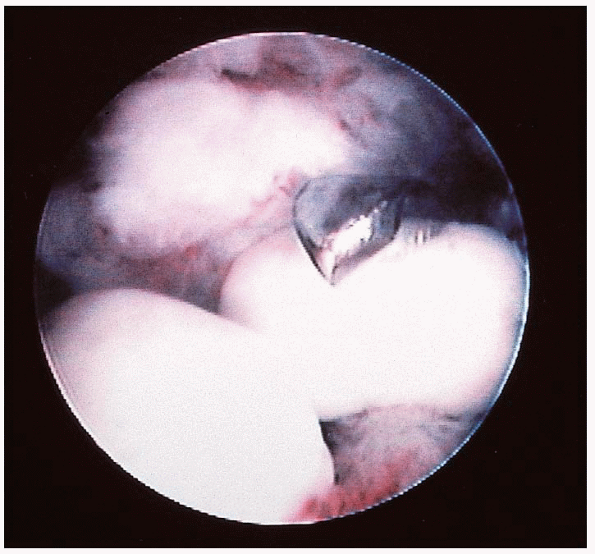
the middle aspect of the dome of the talus, sometimes with posterior
extension. They are managed with the scope placed in the anterolateral
portal and the surgical instrument through the anteromedial portal.
When removing a loose, degenerated, nonviable fragment, it is almost
the rule that excision is achieved through the anteromedial portal. The
following steps are usually necessary. The 70-degree scope is used
through the anterolateral portal for visualization after a partial
synovectomy is done with a small shaver. A sharp banana knife or smooth
dissector is used through the medial portal to complete the dissection
of the fragment. A small grasping forceps is used for the excision and
a small curette to débride the base of the crater down to a bleeding
bed (Figs. 31-19 and 31-20).
Depending on the location of the lesion on the talar done, drilling can
be done with 0.062-inch Kirschner wires (K-wires) through the medial
malleolus (i.e., transmalleolar approach) or through the anteromedial
portal. If the fragment is viable and is not too posterior, it can be
fixated with absorbable pins or small, cannulated screws. When
absorbable pins are used, stable fixation is achieved by using two or
three pins. Stabilization of the lesion before
drilling may be obtained through an accessory anteromedial portal with
a small probe or a smooth K-wire. If the fragment is too posterior, fixation may be
achieved through an arthrotomy incision. Preoperative computed
tomography or magnetic resonance imaging in the coronal and sagittal
planes can be helpful in planning the procedure.
 |
|
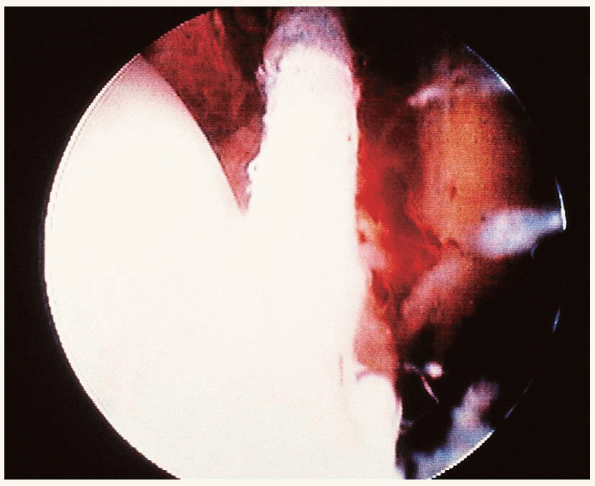
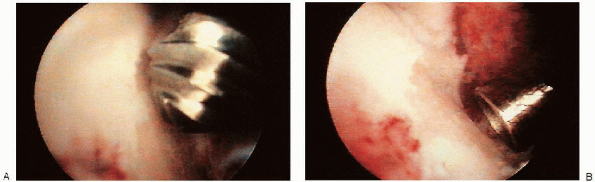
FIGURE 31-19. Excision of a posteromedial lesion of the talus in the right ankle. A: Manipulation of an osteochondral lesion of the talus. B: The defect is abraded with a motorized shaver.
|
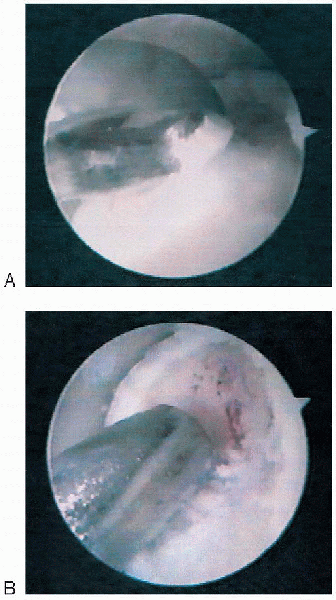
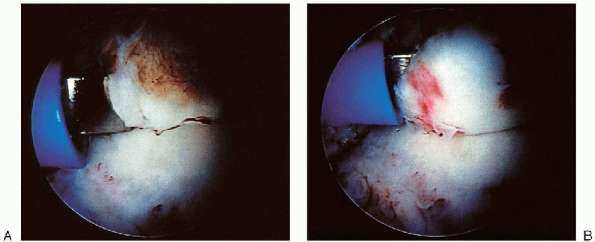
through the anteromedial portal with the scope placed laterally.
Drilling, pinning, or excision can be achieved when indicated.
 |
|
FIGURE 31-20. Excision of a posteromedial lesion of the talus in the left ankle. A: Curettage with a curette. B: Formal débridement with a motorized saw.
|
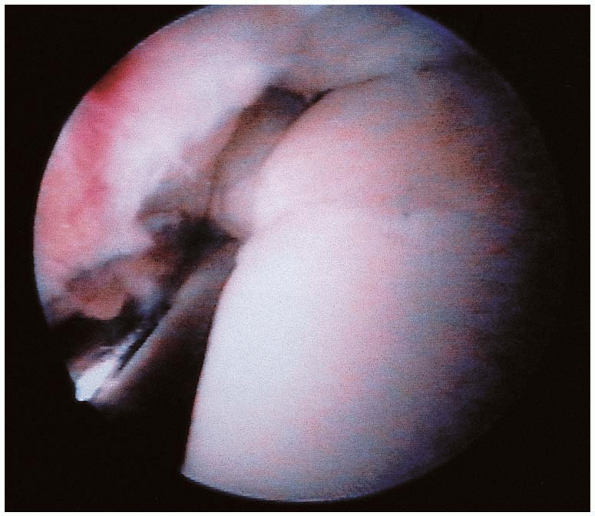
easily accessible. They are approached with the scope placed medially
and the surgical instrument laterally. A loose, viable articular
fragment can be reduced and pinned. A degenerated fragment can be
excised and the bed drilled with a small K-wire (Figs. 31-21, 31-22 and 31-23).
articular cartilage, bone grafting can be performed. Under fluoroscopy,
a K-wire is placed into the osteochondral defect anteriorly through the
anteromedial portal. A small window is removed with a core of
subchondral bone. With the 70-degree scope placed laterally, the cyst
can be curetted under direct vision with a long curette. If necessary,
a small, 2.5-mm scope can be placed into the cyst to confirm the
adequacy of the curettage. Bone graft is inserted into the cystic
defect of the talus.
scope. Excision can be done through the anterolateral portal using the
same steps described for the excision of posteromedial lesions.
Drilling of the bed can be done through the posterolateral portal.
 |
|
FIGURE 31-21. Arthroscopic view of an anterolateral lesion of the talus.
|
 |
|
FIGURE 31-22. The lesion was drilled before fixation with a biodegradable pin.
|
compression dressing is applied for 2 to 3 days. Range-of-motion
exercise of the ankle is begun immediately. After removal of the
dressing, ice applications are started. Weight bearing is allowed
gradually, as tolerated by the patient, if the lesion is less then 1.0
cm in diameter. For larger lesions, non-weightbearing ambulation is
prescribed for 6 to 8 weeks. Rehabilitation is started under guidance
of a physical therapist after complete healing of the wound and
diminution of the swelling.
 |
|
FIGURE 31-23. Biodegradable pin in a reduced fragment.
|
 |
|
FIGURE 31-24. Grasping forceps excising loose osteochondral fragments from the ankle joint.
|
When they are located in the anterior compartment, they can be removed
through the two anterior portals. When placed posteriorly,
visualization and extraction through the posterolateral portal are
improved with some type of noninvasive distraction if the ankle is
tight. After retrieval of the loose bodies, a careful assessment of the
articular cartilage is done to rule out the presence of any chondral or
osteochondral defect. In the latter situation, proper débridement
should complete the procedure. Postoperatively, the patient is allowed
to bear full weight, as tolerated.
above the anterior lip of the tibial plafond and can be associated with
a corresponding osteophyte on the opposing surface of the talus. They
can also be found in the front of the malleoli, mostly the medial
malleolus. This condition is common in runners, dancers, gymnasts, high
jumpers, and football players. It may be caused by forced dorsiflexion
injuries or capsular avulsion injuries after forced plantar flexion.
Plain radiographs can demonstrate the presence of the lesions, and
lateral radiographs in forced dorsiflexion can document the impingement
when the two anterior spurs are present.
be asymptomatic. When they are symptomatic and do not respond to
conservative treatment, arthroscopic surgery is
indicated
for their removal. No distraction is necessary because the pathology is
usually anterior. The standard anterolateral and anteromedial portals
are used for the procedure. Partial synovectomy is very often necessary
to improve visualization. The small shaver is then used to peel off the
capsular insertion from the anterior aspect of the osteophyte. The
osteophyte is removed with a small straight or curved osteotome (Fig. 31-25).
The bone fragment is excised with a grasper. The remaining irregular
surface can be smoothed off with a small burr or a rasp. An osteophyte
on the talus can be removed with an abrader (Fig. 31-26). Before
completion of the procedure, switching the scope between the anterior
portals and intraoperative lateral radiographs can help to determine
the adequacy of the anterior resection. Compression dressing is
applied. After a short period of immobilization and ambulating with
crutches, rehabilitation is started. Full return to sports activities
or dancing may take 6 to 8 weeks.
 |
|
FIGURE 31-25. A: Exostosis on the anterior aspect of the tibial plafond. B: Exostosis being excised with an osteotome.
|
 |
|
FIGURE 31-26. A: Exostoses, with the talar dome being removed with an abrader. B: After excision of the exostoses from the talar dome.
|
with noninvasive or invasive distraction attached to the ankle. To
obtain the maximum visualization, the procedure is done under an image
intensifier (Fig. 31-27). The three standard
portals are used, the two anterior and the posterolateral portals. A
motorized shaver is used to excise the adhesions with a synovectomy.
The articular surfaces of the tibial plafond, talar dome, and medial
and lateral malleolar spaces are excised with a combination of
motorized shaver, curette, and rasps. The cancellous bone is exposed
and small dimples are made on the opposing articular surfaces with the
small burr. Anterior osteophytes, if present, are excised to achieve
adequate reduction of the convex articular surface of the talus into
the concave surface of the tibial plafond. Two guide
pins are drilled from the malleoli and angled 45 degrees anteriorly and inferiorly. After
the tips of the pins are seen with the arthroscope, the distraction is
released, and fluoroscopy is used to confirm the placement of the
tibial and talar surfaces in a neutral position. The guide pins are
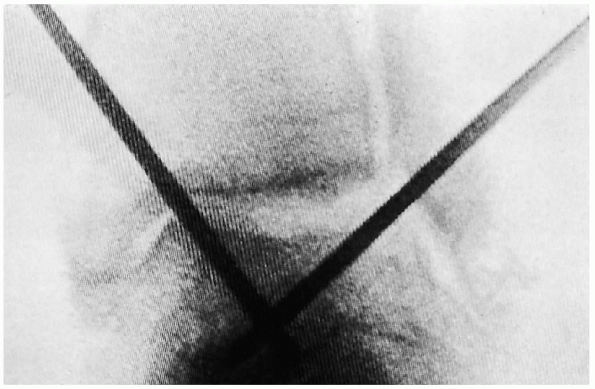
then advanced distally into the talus (Fig. 31-28), and
after determining the proper length of the screws to be used for
fixation, two 6-5 mm cannulated screws are placed over the guide pins
and advanced into the talus without violating the subtalar joint
distally. Permanent x-ray films are used to confirm the
reduction and position of the fusion site and verify screw placement.
The distraction apparatus is removed, and the arthroscopic portals are
closed with 3-0 nylon sutures. The ankle is first placed in a posterior
splint. After removal of the stitches, a short leg cast is applied.
Weight bearing is allowed in 2 to 3 weeks, as tolerated by the patient.
The cast is removed in 6 to 8 weeks, when full union is seen on
radiographs.
 |
|
FIGURE 31-27. The procedure is done with image intensifier
|
 |
|
FIGURE 31-28. Guide pins are advanced into the talus.
|
