Staying Out of Trouble with Growth and Development
– Staying Out of Trouble in Pediatric Orthopaedics > 1 – Staying Out
of Trouble with Growth and Development
|
|
caring for children and staying out of trouble in pediatric
orthopaedics, because growth is the factor that fundamentally separates
pediatric orthopaedic surgery from adult orthopaedic surgery. By
understanding a range of normal physical and radiographic milestones,
you can reassure the worried well and move on to help those children
who have true orthopaedic problems. Likewise, it is important to be
able to spot deviations—such as developmental delays and aberrations in
growth—that may be the only sign that a real problem has suddenly
appeared in the middle of your office hours. Many aspects of normal
growth and development are covered elsewhere in this text in more
detail, particularly in the areas of gait and limb alignment. This
chapter focuses on the specific elements of growth and development that
may help the orthopaedist to stay out of trouble while caring for
children.
“normal” depends on whether you are dealing with an underlying
condition. Normal size and normal motor milestones are different for
children with Down syndrome, achondroplasia, or Marfan syndrome. In
some cases, specific growth charts have been made for these conditions.
Most orthopaedic surgeons—even most pediatric orthopaedic surgeons—have
no desire to function as developmental pediatricians. If you or the
parents suspect an important deviation in growth and development, be
sure to bring the primary care doctor on board.
neurologic system. Therefore, if you pick up a delay in milestone, you
may be the first physician to find a clue to an underlying undiagnosed
condition. Regardless of the age of the skeletally immature child, an
increase in height and weight over time should be expected. Any child
who is losing weight (not intentionally) over a few months could be
showing signs of trouble. Such changes are monitored best through the
primary care doctor. An accurate height and weight chart is extremely
valuable in tracking the adolescent growth storm that can cause rapid
worsening of spinal deformities. Accurate height measurements are
particularly valuable in managing children and adolescents with
scoliosis. Little el al.1 showed
that height velocities generated from clinical height measurements for
patients with idiopathic scoliosis document the growth peak and predict
cessation of growth reliably. Knowing the timing of the growth peak
provides valuable information on the likelihood of progression to a
magnitude requiring spinal arthrodesis. Likewise, orthopaedists who are
monitoring leg length inequalities find a growth chart valuable.
 |
|
▪ FIGURE 1-1
To stay out of trouble, you need to know the contribution of each physis, both in proportional and absolute growth. (Reprinted with permission from Morrissy RT, Weinstein SL, eds. Pediatric Orthopaedics, 5th ed. Philadelphia: Lippincott Williams & Wilkins, 2001.) |
half of the child’s sitting height is obtained by 5 years of age. Such
information is crucial in managing spinal deformities in very young
children. Remember that there are important patterns of onset of
ossifications centers. Understanding these ossifications centers and
their appearance is essential in diagnosing occult fractures of the
elbow and other areas. Orthopaedic surgeons caring for children also
need to have a good understanding of the percentage of growth that is
contributed by each physis (Fig. 1-1). Such
knowledge of normal growth and development helps the orthopaedic
surgeon time epiphysiodesis and understand the effects of a traumatic
growth arrest.
the predicted limb-length discrepancy (LLD) at skeletal maturity,
without the need to plot graphs, and is based on as few as one or two
measurements. This method is independent
of
percentile groups and is the same for the prediction of femoral,
tibial, and total-limb lengths. The multiplier values are also
independent of generation, height, socioeconomic class, ethnicity, and
race. Paley et al. verified the accuracy of this method clinically by
evaluating patients who had been managed with limb lengthening or
epiphysiodesis. The method was also comparable with or more accurate
than the Moseley method of limb length prediction.2 It is more accurate than the Anderson method and easier to use than the Mosely method, according to its developers.3
The multiplier method has also been shown to accurately predict LLD and
outcome of epiphysiodesis, and to be more accurate than the Moseley
method in predicting LLD at maturity after epiphysiodesis.4
flexion contractures. The hips are generally externally rotated. Genu
varum and flat feet are normal. Be alert for possible early handedness
as it may be a sign of hemiplegia or any other unilateral problem. The
orthopaedist caring for infants and toddlers should be generally
familiar with a series of milestones that can help quickly identify a
child who is lagging behind (Table 1-1). Such
an understanding of milestones is important in managing a potential
musculoskeletal problem and counseling families as to whether further
investigation is needed. Again, involving a developmental pediatrician
is essential should children be falling short of their developmental
milestones.
deformation and a malformation. Malformations, such as syndactyly or
PFFD, are defects in organ development that occur early in fetal life.
Deformations are changes in the limbs, trunk, head, or neck caused by
mechanical force. During the rapid period of fetal growth, such a force
can lead to a deformation such as a calcaneo-valgus foot or metatarsus
adductus. Unlike malformations, deformations can be corrected by gentle
manual forces.
|
TABLE 1-1 Key Motor Milestones to Keep the Orthopaedist Out of Trouble
|
||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
about 18 months. Of all the developmental milestones listed in various
textbook charts, a delay in walking is probably the most common reason
that parents bring their children to an orthopaedist for a
developmental delay. To stay out of trouble, get a sense of whether
other members of the family walked late. Give the child a careful
evaluation, and try to assess whether other milestones are delayed as
well. It is essential to understand the birth history; premature
children may be predisposed to cerebral palsy and may have a different
corrected developmental age than their true chronologic age.
which should improve as they approach 5 years of age. The 3-year-old
who has significant, persistent, true genu varum warrants radiographic
evaluation.
“clumsy.” It’s tempting to brush off such complaints, explaining that
the child is accident-prone or that clumsiness is common in all
children during periods of rapid growth. While these observations are
true, it is particularly important to be vigilant for the child whose
clumsiness is increasing during the toddler years. The parents may be
bringing you a child showing the first manifestations of a disorder
such as muscular dystrophy. If someone brings you a 3- or 4-year-old
boy with increasing clumsiness, do a very careful neurologic exam—and
be sure to do a Gower’s test.
matured into a near adult-like pattern, and their lower-extremity limb
alignment (genu varum and genu valgum) should be approaching normals
for adults. Be alert to asymmetries of size. At this age, children
sometimes present with limb asymmetry. While this can be a limb-length
inequality, it can also be an asymmetry in limb girth. This
presentation of growth abnormality may be the first manifestation of
hemihypertrophy or even hemiplegia. Again, in the school-age child, be
alert to clumsiness or a decrease in motor abilities. The classic
example is the 5- or 6-year-old boy who is having trouble climbing the
stairs, representing the first manifestation of Duchenne muscular
dystrophy. Understanding proportional growth in children can help in
counseling of families and in keeping the orthopaedist out of trouble.
One valuable rule of thumb for leg length inequalities5
is that if growth inhibition stays constant in a short limb, a limb
length inequality in a girl of 3 and a boy of 4 years of age will be
twice as large at maturity. Predicting ultimate leg lengths in this age
group can be very troublesome and not necessarily made easier by the
use of skeletal age. Kasser and Jenkins6
concluded that skeletal age, as determined by the Gruelich and Pyle
Atlas, does not improve the accuracy of prediction of ultimate leg
length in children younger than 10 years of age, except in girls with
advanced bone age.
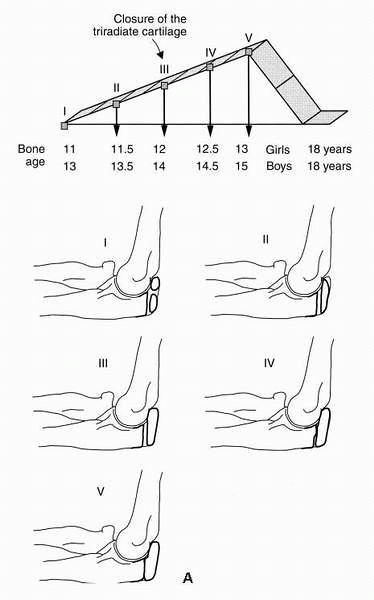
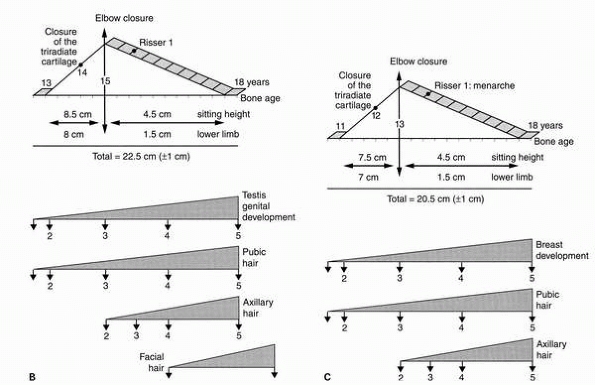
been done in timing the adolescent growth spurt to help the
orthopaedist to manage such conditions as spinal deformities and limb
length inequalities. Much of this work can be credited to Dr. Alain
Demiglio. Although the Risser sign is a routine maturity assessment
tool of adolescents with scoliosis, it is very unreliable. The Risser
sign is at “0” for the first two-thirds of the pubertal growth spurt.7 It is more
valuable to look at olecranon ossification and the status of the
triradiate cartilage. At the beginning of puberty, two ossification
centers appear in the olecranon, and they close completely at the peak
velocity of the pubertal growth spurt (Fig. 1-2).
The triradiate cartilage closure tells you that the adolescent is
two-thirds of the way through the most rapid phase of growth. At
menarche in girls and the first shaving episode in boys, the adolescent
will generally be at Risser I. Tanner staging is much more accurate,
but most orthopaedists do not feel that they are comfortable making
this a routine part of the musculoskeletal exam. Dr. Kasser recommends
when timing any operation for which the stage of growth remaining is
important for a good result, the best way to stay out of trouble is to
ignore chronologic age and focus on bone age. Very little lower limb
growth occurs after a bone age of 13 in a girl and 15 in a boy. Also,
bone age will often accelerate during puberty. Stay out of trouble by
shortening the followup for an epiphysiodesis visit from 6 months to 4
months and always order a bone age during this period.
weaning a scoliosis brace. Demiglio has shown that at Risser III, there
is a 12% chance that a 20° scoliosis will progress 5° or more. During
the adolescent period, there are sometimes other manifestations of
rapid growth. Children often see the orthopaedist for postural round
back (flexible thoracic kyphosis). Such a deformity is common in
teenage boys, and parents need reassurance that there is not some spine
problem that demands treatment. It is wise to check a PA and lateral of
the entire spine to rule out spondylolysis or some congenital
abnormality.
Some parents still need something in addition, such as a prescription
for physical therapy and “postural education.”
 |
|
▪ FIGURE 1-2 A.
The olecranon ossification center can act as a helpful guide early in puberty, because it signals the start of the most rapid period of growth. Stage 1 occurs long before the closure of the triradiate cartilage, or menarche. The graph depicts the steep part of growth—a time period you miss completely if you are waiting for Risser I B. Dimeglio’s summary diagram of growth, presented combined with Tanner findings in boys. By the time you see axillary or facial hair on exam, the fastest period of growth is over. C. Dimeglio’s summary diagram of growth, presented combined with Tanner findings in girls. (Reprinted with permission from Morrissy RT, Weinstein SL, eds. Pediatric Orthopaedics, 5th ed. Philadelphia: Lippincott Williams & Wilkins, 2001.) |
 |
|
▪ FIGURE 1-2 (continued).
|
studied the radiographs of 30 children and concluded that there is a
uniform skeletal age, or “narrow window,” during which epiphyseal
slipping occurs, regardless of the child’s chronologic age. In another
recent study of 83 children with SCFE, puberty was staged at the time
of diagnosis using bone age, closure of triradiate cartilage, and
Risser index. A total of 95% of boys and 83% of girls presented with
their SCFE during the accelerating phase of puberty. The triradiate
cartilage was still open at the time of diagnosis in 65% of boys and
64% of girls. These investigators determined that once the triradiate
cartilage is closed, there is a only a 4% chance of a contralateral
SCFE.9
during this most rapid period of growth and development. Such muscle
contractures cause a tremendous amount of trouble for adolescent
athletes, particularly any muscle that crosses or attaches to the
rapidly growing femur. Contractures of the quadriceps, hamstrings, and
gastrocs are normal but can cause a host of symptoms such as
patellofemoral pain and heel problems. Refer to Chapter 12 for further discussion of this manifestation of growth and development.
-
The definition of
“normal” depends on whether you are dealing with an underlying
condition. Normal size and normal motor milestones are different for
children with Down syndrome, achondroplasia, or Marfan syndrome. -
Look at the growth
chart. Lack of normal growth over a 6-month period represents a
significant deviation from normal, and evaluation by an endocrinologist
should be considered. Four centimeters is the minimal acceptable growth
in any one-year period. -
It is tempting to
brush off a complaint of “clumsiness.” It is particularly important to
be vigilant for the child whose clumsiness is increasing during the
toddler years. The parents may be bringing you a child showing the
first manifestations of a disorder such as muscular dystrophy. -
Olecranon ossification and bone age are much more reliable than Risser sign in assessing the most rapid period of growth.
-
In SCFE, there is a
uniform skeletal age or “narrow window” during which epiphyseal
slipping occurs, regardless of the child’s chronologic age. Once the
triradiate cartilage is closed, there is a only a 4% chance of a
contralateral SCFE.
DG, Song KM, Katz D, et al. Relationship of peak height velocity to
other maturity indicators in idiopathic scoliosis in girls. J Bone Joint Surg Am. 2000;82-5:685-693.
JA, Paley D, Paley J, et al. Clinical validation of the multiplier
method for predicting limb length at maturity, part I. J Pediatr Orthop. 2005;25-2:186-191.
JA, Paley D, Paley J, et al. Clinical validation of the multiplier
method for predicting limb length discrepancy and outcome of
epiphysiodesis, part II. J Pediatr Orthop. 2005;25-2:192-196.
D, Dimeglio A, Bentahar T. Staging puberty in slipped capital femoral
epiphysis: importance of the triradiate cartilage. J Pediatr Orthop. 2004;24-2:144-147.