Adult Deformity
treatment because of a combination of symptoms, including back pain,
radiculopathy, progression of deformity, and global imbalance. The
spinal deformity is categorized according to whether the predominant
malalignment occurs in the coronal (scoliosis) or sagittal
(kyphosis/lordosis) plane. An important distinction for coronal and
sagittal deformities is whether the deformity developed de novo in
adulthood or had its onset before skeletal maturity with progression
over time. This chapter discusses the evaluation and treatment for
adult scoliosis and iatrogenic sagittal deformities in ambulatory
patients who do not have a paralytic or congenital etiology.
deformity is a thorough understanding of the spine’s normal
architecture and alignment. In the coronal plane, the spine is normally
straight. A vertical line (plumb) from the
tip of the dens (C2) on a standing anteroposterior radiograph should
nearly bisect each distal vertebra below, including the sacrum.
Significant deviation of the vertebra from this vertical line indicates
a scoliotic deformity. By tradition, coronal curvature of the spine is
termed scoliosis if the Cobb measurement
is greater than 10 degrees. Normal alignment in the sagittal plane is
defined less easily owing to marked variation in global and regional
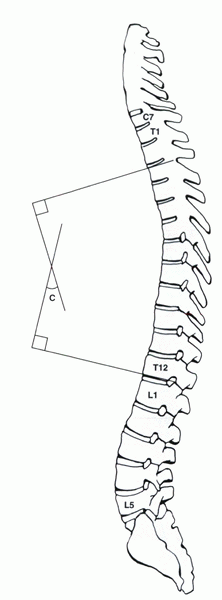
parameters. In evaluating global sagittal balance, the center of the C7
body is a useful reference. It is usually visible on long cassette
radiographs, and a plumb line drawn through the center of the C7 body
usually intersects with the posterior-superior body of S1 (Fig. 21-1).
Normal thoracic kyphosis in adults has a broad range (20 degrees to 60
degrees) with a mean value that tends to increase with age. The apex of
thoracic kyphosis usually falls between T6 and T8. Normal lumbar
lordosis (L1-S1) ranges from approximately 30 degrees to 80 degrees.
Two thirds of the lumbar lordosis usually exists between L4 and the
sacrum with 40% at L5-S1. Eighty percent of the lumbar lordosis occurs
through wedging of the intervertebral discs, whereas only 20% is
derived from the trapezoidal shape of the vertebral bodies.
-
Adults with a deformity dating back to adolescence with or without superimposed degenerative changes (adult idiopathic scoliosis)
-
Older adults with degenerative de novo scoliosis who did not have any deformity before age 40 (adult de novo scoliosis)
With advancing age, the normal spinal degenerative process may
contribute to the progression of an adult idiopathic scoliosis curve or
the development and progression of a de novo scoliosis deformity.
treated before skeletal maturity is variable. Smaller curves and curves
in patients with good overall spinal alignment may progress little over
time. Conversely, larger curves and curves associated with global
imbalance may progress at a rate of 1 degree or more per year during
adulthood. In general, thoracolumbar and lumbar curves are more likely
to progress than more stable thoracic curves. With advancing age, the
rate of progression may increase as patients undergo degenerative
changes in discs, facets, and ligaments. Older patients with de novo
degenerative scoliosis curves may progress at a rate of 3.3 degrees per
year.
patient as a loss of trunk height, a change in trunk contour, or a
shift in the position of the head relative to the pelvis (global
balance). Although both types of adult scoliosis may increase in
magnitude, the change for degenerative idiopathic curves tends to be
clinically noticeable, whereas for degenerative de novo curves, the
change tends to be more radiographic.
idiopathic scoliosis in that patients have no history of previous
spinal deformity. It occurs in the lumbar spine in the absence of any
significant thoracic deformity. Mild-to-moderate de novo adult
scoliosis deformities may be well tolerated, especially when global
balance is maintained. Larger curves and curves with advanced
degeneration tend to be symptomatic.
 |
|
Figure 21-1 Sagittal alignment showing the C7 plumb and its typical relationship relative to the sacrum.
|
 |
|
Figure 21-2 Sagittal alignment of the spine showing the Cobb method of quantifying spinal deformities.
|
|
TABLE 21-1 COMPARISON OF CLINICAL CHARACTERISTICS ASSOCIATED WITH ADOLESCENT AND ADULT SCOLIOSIS
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
of back pain, leg pain, or progressive deformity. Axial discomfort
arises from advanced degeneration of spine motion segments and
paraspinal muscle fatigue resulting from the body’s attempt to maintain
regional and global balance. Degeneration of the disc, facet complex,
and segmental listhesis also can result in stenosis of the canal,
lateral recess, or foramen causing claudicatory symptoms or
radiculopathy or both. Stenosis and neural compression occur most
frequently in the areas of greatest force concentration within the
spine. These areas are principally the concavity of the scoliotic curve
or within the remaining segments between the distal aspect of the
thoracolumbar or lumbar curve and the sacrum (fractional curve) (Fig. 21-3).
to that recommended for symptomatic lumbar disc degeneration.
Initially, nonsteroidal antiinflammatory drugs, exercise, weight
management, and, in some cases, orthotic devices are recommended. None
of these measures has been shown to arrest the progression of deformity
or relieve symptoms resulting from neurologic compression. A trial of
nonoperative measures is indicated, however, in patients who have mild
deformities or who have sizable deformities but for a variety of
organic and psychosocial reasons are not candidates for surgical
intervention.
-
Large deformity based on Cobb measurement, vertebral rotation, coronal balance, and the sagittal plane
-
Documented deformity progression
-
Function limiting axial or radicular pain that is poorly responsive to nonoperative measures
-
Pulmonary dysfunction related to the spinal deformity
-
emotional state, and an intact social support structure ideally should
be present. Modifiable risk factors for the development of
perioperative complications should be optimized before surgery is
undertaken (e.g., smoking, malnutrition, skin compromise, steroid use).
patient based on their specific complaints, physical and radiographic
findings, and overall state of health. Radiographic evaluation includes
long cassette anteroposterior and lateral views to assess regional and
global balance. Flexibility radiographs in the coronal and sagittal
plane provide valuable insight into the rigidity of the curve. When it
is difficult to assess degenerative changes at the lumbosacral
junction, a true anteroposterior radiograph (the Ferguson
anteroposterior view) of the lumbosacral joint with the beam angled up
to the degree of lumbosacral lordosis is helpful.
myelography followed by computed tomography (CT). Myelography may be
obtained in supine and standing positions to define the dynamic nature
of the stenosis. Thin (1-mm) CT axial slices provide for a precise
assessment of the central canal, lateral recess, and foramen. Magnetic
resonance imaging (MRI) is helpful for assessing the disc degeneration
and foraminal stenosis, especially at the distal lumbar segments. For
the central canal and lateral recess, MRI is not as helpful for
defining the extent of stenosis as CT-myelography. Many surgeons find
provocative discograms helpful in deciding where to stop a fusion
distally. To date, there is no universal agreement, however, on the
reproducibility and reliability of discograms.
patient’s complaints are addressed adequately with the smallest
magnitude of surgery, while minimizing the potential for perioperative
and subsequent complications (Table 21-2). For
adult idiopathic scoliosis without significant spinal degeneration, an
anterior-only or posterior-only fusion is indicated.
For
degenerative scoliosis, a variety of surgical strategies are possible
depending on the patient’s constellation of symptoms (see Table 21-2).
If the patient’s complaints can be localized to a specific level, a
focused treatment strategy of limited decompression or fusion, or both,
may be employed. A focused intervention often is best suited for
patients with mild scoliotic deformities, hyperstable spines, or
significant comorbidities who would not tolerate more extensive
reconstruction procedures. This strategy must be considered carefully
in terms of its effect on segmental stability, regional alignment, and
the potential for subsequent deformity progression.
|
TABLE 21-2 DEGENERATIVE SCOLIOSIS: SURGICAL STRATEGIES
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
significant amount of lumbar degeneration. The principles of selecting
fusion levels for these patients are similar to those for patients with
adolescent scoliosis. The highest and lowest instrumented vertebrae
should be stable (intersected by the center sacral line) and nonrotated
(neutral), and the sagittal profile, especially lumbar lordosis, should
be corrected to as near normal as possible.
distal lumbar spine typically has degenerative changes and becomes
increasingly stiff. Segments to be included in the fusion include
segments with subluxation, spinal stenosis, and posterior column
deficiencies due to previous laminectomies or spondylolysis. Whether to
include distal segments with mild-to-moderate disc degeneration is
controversial. Provocative discography may provide the answer in select
cases, but the procedure is not universally accepted. In general,
segments in the distal lumbar spine with only mild degenerative changes
do not need to be included in the fusion if there is no underlying
degenerative deformity, central, lateral recess, or foraminal stenosis.
After surgical treatment, the cephalad and caudad ends of the fusion
should be neutral and stable. In most cases, it is preferable for the
top and bottom of the fusion to end up parallel to the shoulders and
the sacrum.
Indications for extension to the sacrum include advanced degeneration
of the L5-S1 disc, oblique take of L5 on the sacrum, previous L5-S1
decompression, or presence of spondylolysis. In the absence of these
conditions, stopping the fusion at L5 should be considered.
multiple theoretical advantages. With a long fusion to L5, challenges
involved with obtaining and maintaining lumbosacral fixation and fusion
are negated. Adjunctive anterior discectomy and fusion procedures
selectively may be avoided, and postoperative bracing requirements are
decreased. The smaller magnitude of surgery involved with arthrodesis
to L5 also theoretically may lead to a decreased incidence of
perioperative complications.
fusion level. For long fusions stopping at L5, the remaining
lumbosacral motion segment is subjected to supraphysiologic forces and
may undergo accelerated degeneration. A “transition syndrome” at L5-S1
may result in pain, radiculopathy, and forward shift in sagittal
balance. Conversely, long fusions to the sacrum are limited by the
larger initial scope of surgery required, an increased risk of
perioperative morbidity, and the increased possibility for the
subsequent development of pseudarthrosis. The decision of whether to
stop a long fusion at L5 or the sacrum should be evaluated on a
case-by-case basis with consideration of the preoperative sagittal
balance, degenerative status of the L5-S1 disc, and medical status of
the patient.
instrumented vertebrae should extend into areas of lordosis. It almost
always is a mistake to stop a fusion at the apex of a sagittal
kyphosis, because a progressive junctional kyphosis commonly follows.
|
TABLE 21-3 ADVANTAGES OF TERMINATING A LONG FUSION AT L5 VERSUS THE SACRUM
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
-
Length of the fusion
-
Curve flexibility
-
Quality of the posterior bone for fixation and fusion
-
Patient’s sagittal balance
subluxation usually are treated best with circumferential surgery. In
these cases, anterior structural grafting of a distracted disc space
tends to create a ligamentotaxis effect to help reduce subluxations.
Retensioning the anulus and the posterior longitudinal ligament also
often normalizes alignment. The presence of a previous laminectomy or
the need for a concurrent extensive decompression results in a
decreased surface area for posterior fusion and is another relative
indication for a circumferential fusion. Anterior surgery increases the
amount of correction achieved and the likelihood of obtaining a solid
fusion (see Fig. 21-3). The potential benefits
of a supplemental anterior procedure must be balanced on a case-by-case
basis, however, against the added operative time, operative risks, and
recovery.
 |
|
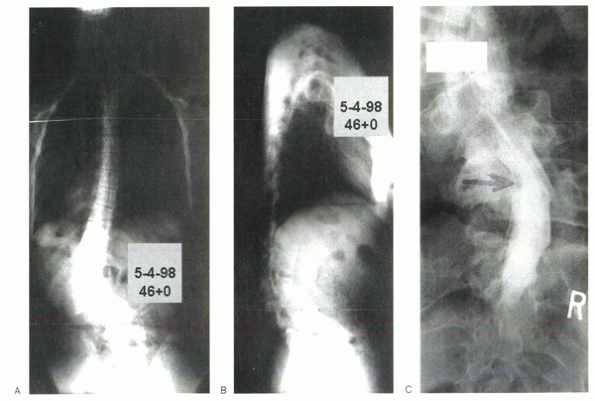
Figure 21-3 Anteroposterior (A) and lateral standing (B)
radiographs of a 46-year-old woman with a known history of untreated adolescent idiopathic scoliosis who experienced the progressive onset of back discomfort, left leg radicular symptoms, and worsened cosmesis over the past few years. Standing anteroposterior myelogram (C) shows decreased dye filling in the area of the lateral recess on the left side at L5. A combination of factors, including facet hypertrophy (inferior facet of L4 and superior facet of L5), scoliosis, listhesis, and capsular hypertrophy, contributes to the stenosis at the L4-5 level. Displacement of the cauda equina and compression of the left L5 nerve root shown on the postmyelogram CT scan (D) account for the left leg radicular symptoms experienced by the patient. Standing anteroposterior (E) and lateral (F) radiographs 2.3 years status post spine decompression and reconstruction. The patient underwent a two-stage procedure beginning with anterior discectomies and fusion from T11 to the sacrum using a combination of structural interbody cages, fresh frozen femoral rings, and autogenous autograft. One week later, the patient underwent a posterior decompression at L4-5 and instrumented fusion from T10 to the sacrum with significant deformity correction. The decision was made to fuse to the sacrum owing to the presence of advanced L5-S1 disc degeneration. Posterior Smith-Peterson osteotomies were performed to improve the sagittal alignment beyond that achieved with anterior discectomies and structural grafting alone. At more than 2 years after surgery, the patient’s regional coronal and sagittal alignment are much improved, and global balance is well maintained. The leg pain has resolved. Preoperative lateral photograph (G) shows forward shift in global sagittal balance and marked thoracolumbar kyphosis. H: Postoperative lateral photograph (H) shows restoration of a normal spine sagittal alignment. Preoperative posterior photograph (I) shows a left thoracolumbar prominence and asymmetric abdominal creases. Postoperative posterior photograph (J) shows significant improvement in the chest wall and abdominal crease symmetry. Global coronal balance is maintained. The patient’s preoperative back and radicular complaints have resolved, and her function has improved greatly. |
considered for patients with severe, out-of-balance, or highly
inflexible curves. Three basic types of osteotomies exist:
-
Osteotomies that involve posterior element wedge resection (Smith-Peterson osteotomy)
-
Posterior wedge resection in association with anterior discectomy and structural grafting (circumferential osteotomy)
-
Posterior three-column wedge resection (pedicle subtraction or decancellation osteotomy)
of sagittal imbalance, coronal deformity correction also may be
achieved by resecting additional bone in the coronal plane from the
side of the convexity. If circumferential procedures are contemplated,
it is usually advisable to start with the anterior approach. The
exceptions to this principle
are
cases with severe stenosis in which the canal could be compromised
further by an anterior grafting and extension at the level of an
already stenotic canal.
 |
|
Figure 21-3 (Continued)
|
structural autogenous bone (rib or iliac crest), morcellized or
structural allograft (fresh frozen femoral rings), and mesh cages
filled with morcellized autograft or allograft. Advantages of fresh
frozen femoral rings and mesh cages are that anterior structural
support is provided, and the disc space is held open to increase
lordosis and theoretically to expand the foramen. Morcellized
autogenous bone is recommended for posterior fusion. The role of
bone-stimulating factors, such as bone morphogenetic protein, in
stimulating bone formation in the presence of a long adult deformity
fusion is investigational at this time.
an arthrodesis for adult deformity. Fixation at each level provides for
not only better correction, but also superior maintenance of correction
and theoretically a higher rate of fusion. The benefits of segmental
fixation are most pronounced in older patients with osteoporosis who
are at especially increased risk for subsequent implant
pull-out/failure and loss of alignment. The use of cement augmentation
in association with pedicle screw placement and prophylactic
vertebroplasty of adjacent unfused levels has been advocated in these
cases, but these methods have not been widely adopted.
instrumentation for certain lumbar and thoracolumbar curves in young
and flexible patients. For most patients, some form of posterior
segmental spinal instrumentation
should
be used, however. Constructs using pedicle screws in the lumbar spine
and either pedicle screws or hooks in the thoracic spine with
cross-link placement is the current state-of-the-art. With long fusions
to the sacrum, it is mandatory to have four points of fixation in the
sacrum. Alternatives include bilateral S1 and S2 screws, sacral screws
with supplemental iliac screws, sacral screws with two intrasacral
rods, or bilateral S1 screws with a Galveston-type technique in the
ilium.
 |
|
Figure 21-3 (Continued)
|
obtaining a successful fusion is greater if the sagittal C7 plumb line
falls through or behind the sacrum. Many patients with progressive
degenerative scoliosis have had previous decompressions and have
decreased posterior bone stock. This situation often is a relative
indication for a circumferential fusion procedure. Anterior structural
grafting at L4-5 and L5-S1 also improves maintenance of alignment and
successful fusion by reducing the mechanical stress on the bone-implant
interface.
normal lumbar lordosis, an increase in thoracic kyphosis, or both. Mild
changes in regional sagittal alignment typically are well compensated
for by an alteration in the alignment of another region of the spine
and with mild hip flexion. To maintain a relatively erect posture (head
over sacrum), these patients usually have to hyperextend their necks
and stand with knees and hips slightly flexed. When these compensatory
mechanisms are exceeded, patients become symptomatic, and a change in
global alignment (forward shift in the sagittal C7 plumb) ensues. The
combination of clinical and radiographic findings associated with a
forward shift in global balance that exceeds the body’s compensatory
mechanisms is termed fixed sagittal imbalance.
Efforts to maintain an erect posture result in early fatigue, pain,
poor cosmesis, and functional limitations. In cases of previous spine
fusion, accelerated degeneration of adjacent motion segments also can
result in the development of mechanical back pain and neurologic
compression. Adjacent segment degeneration is especially prevalent when
a fusion ends at an area of focal hypolordosis or hyperkyphosis.
aging, the intervertebral disc gradually loses hydration and decreases
in height. Because 80% of lumbar lordosis is derived from the discs,
loss of disc height at multiple levels results in shortening of the
anterior column and diminished lordosis. In cases of trauma, fusion of
the thoracolumbar or lumbar spine in kyphosis often leads to regional
and global imbalance. Deformity correction procedures that involve
shortening of the anterior column or, alternatively, procedures
that
lengthen the posterior column (Harrington scoliosis correction) also
often result in loss of normal lordosis. The loss of lordosis
associated with the treatment of idiopathic scoliosis with posterior
distraction instrumentation may result in a subset of fixed sagittal
imbalance termed flat back syndrome.
sagittal imbalance when lumbar segments are fused in kyphosis. Great
care should be taken when performing lumbar arthrodesis procedures to
maintain a lordotic sagittal alignment over the fused segments. This
alignment is achieved best by positioning the patient on the operating
table with the hips fully extended. Additional lordosis may be added by
administering compression across the posterior implants or by
performing an osteotomy if necessary.
deteriorate over time for a few reasons, including nonunion, loss of
distal fixation at L5 or the sacrum, or accelerated degeneration at a
motion segment above or below the existing fusion. Vertebral fracture
at the level above a long adult fusion also can lead to increased
thoracic kyphosis and the development of positive sagittal imbalance.
to identify the specific factors resulting in symptoms. An assessment
of global balance is made by having the patient stand erect with the
hips and knees fully extended. Flexibility at different regions of the
spine is assessed with either active or passive bending maneuvers and
radiographs. Sagittal deformities that seem stiff on initial evaluation
may show remarkable flexibility if subjected to gentle supine bending
over a bolster over 5 to 10 minutes. Physical examination should
include an assessment of hip range of motion because a hip flexion
contracture may occur in patients with fixed sagittal imbalance.
standing erect with hips and knees extended provide for quantitative
assessment of global sagittal balance (C7 plumb relative to the
posterior cortex of the body of S1). Short cassette radiographs and
“cone-down” views of an area of particular interest provide additional
information regarding local anatomy and the extent of disc and facet
degeneration. Radiographs in standing, flexion/extension, and passive
extension over a bolster show the amount of motion present at the
kyphotic or previously fused levels and the amount of compensatory
motion available at adjacent levels. These “dynamic” views also may
show the presence of any pathologic motion, such as listhesis,
hypermobility, or motion within a previously fused segment.
of disc degeneration that may be important in determining the distal
extent of the fusion. Myelography followed by CT with thin
(approximately 1 mm) axial slice images is a superior means of
characterizing the location and magnitude of cauda equina and nerve
root compression. Standing myelograms, in particular, are helpful in
defining the extent to which dynamic stenosis is present.
respiratory function, and expectations need to be assessed carefully
for each patient in whom surgical intervention is being considered. The
surgeon has the responsibility to weigh honestly the likelihood for
significant improvement against the potential for perioperative
complications and late morbidity. In some patients with fixed sagittal
imbalance, the risks of surgery and the modest likelihood of
significant functional improvement make surgical intervention ill
advised.
-
Restoring normal regional sagittal alignment
-
Establishing global sagittal balance
-
Minimizing the potential for complications and late failure
on a sagittal standing radiograph should fall through or behind the
lumbosacral disc (Fig. 21-4).
on bending radiographs, a posterior instrumented fusion without
osteotomies may be sufficient. The most effective means of achieving
significant sagittal deformity correction is through the performance of
spinal osteotomies, however, at one or more levels. Three classes of
osteotomies commonly are employed:
-
Posterior column wedge resection (Smith-Peterson)
-
Combination of posterior column wedge resection osteotomy with anterior discectomy and structural grafting
-
Three-column wedge resection procedure (pedicle subtraction, eggshell)
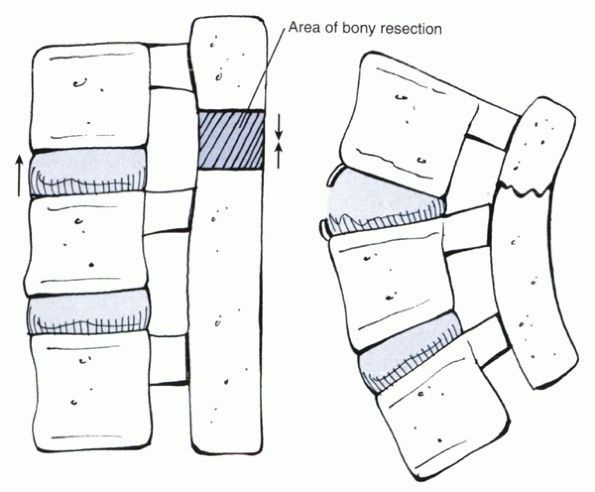
chevron V portion of the posterior elements at the level of the facet
joint (Fig. 21-5). The ligamentum flavum and a
portion of the lamina and spinous processes also are removed to provide
for a complete posterior column defect. The amount of facet and lamina
removed depends on the amount of angular correction desired. A good
rule of thumb is that for every 1 mm of posterior element removed, 1
degree of sagittal correction is achieved. Undercutting the ventral
surface of the lamina and facets is advised to minimize the potential
for the development of iatrogenic central, lateral recess, or foraminal
stenosis after osteotomy closure. The osteotomy is closed by
compressing the posterior elements proximal and distal to the osteotomy
and maintaining the reduction with spinal implants. With the middle
column as its fulcrum, the disc space hinges open with widening of the
anterior disc space. Smith-Peterson osteotomies may be performed at
multiple adjacent levels. Advantages of this type of osteotomy are that
it may be performed rapidly; it involves minimal blood loss; it does
not necessitate neural element manipulation; it is performed safely at
cord, conus, or cauda levels; and it provides for a harmonic lordotic
correction. Smith-Peterson osteotomies are limited, however, by the
following:
 |
|
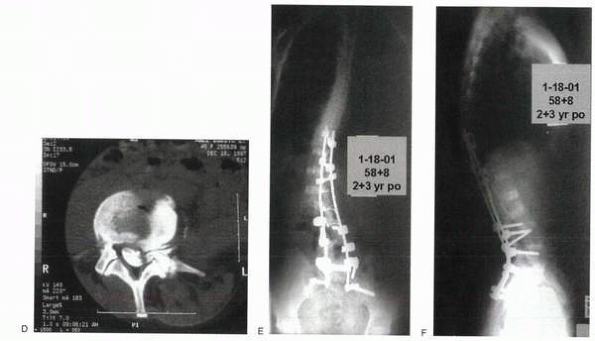
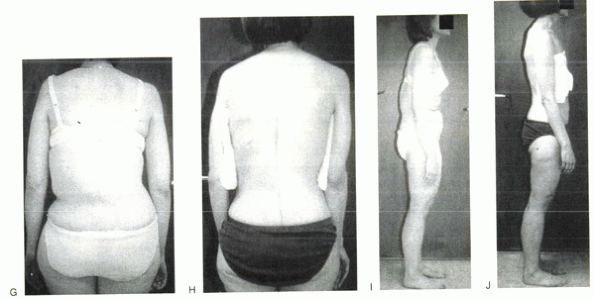
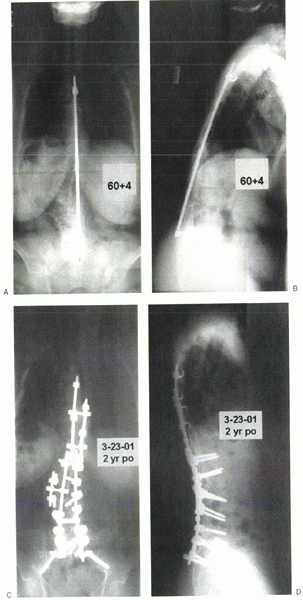
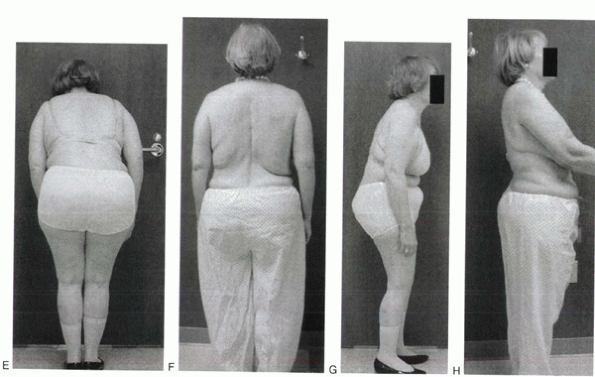
Figure 21-4 Anteroposterior (A) and lateral standing (B)
radiographs of a 60-year-old woman who was treated for idiopathic scoliosis as a teenager with a posterior Harrington instrumented fusion from T4-L5. Her chief complaints on presentation were back discomfort and loss of ambulatory endurance. She experienced regular back fatigue, radicular leg pain, and an increasingly forward-pitched posture. Anteroposterior and lateral preoperative standing radiographs show a Harrington distraction rod from T4-L5, loss of lumbar lordosis, and a significant forward shift in the global sagittal balance. Anteroposterior (C) and lateral (D) radiographs show status post spinal reconstruction. Arthrodesis was extended to the sacrum with an anterior L5-S1 discectomy and fusion using a structural mesh cage and cancellous iliac crest autograft followed by posterior instrumented fusion using sacral and iliac screws. Additional sagittal correction was achieved with a pedicle subtraction osteotomy at L2. (E-H) Clinical photographs show preoperative (E and G) sagittal imbalance, decreased lumbosacral lordosis, and a tendency to stand with hips slightly flexed. At 3 years postoperatively (F and H), the patient stands with hips extended, head centered over the pelvis, and has normal lumbosacral lordosis. |
 |
|
Figure 21-4 (Continued)
|
 |
|
Figure 21-5
Schematic depicting a Smith-Peterson spinal osteotomy. The hatched portion of the posterior elements is resected, and the posterior elements are compressed, increasing the amount of lordosis. |
-
The modest amount of correction that can be achieved at each level (10 degrees to 15 degrees)
-
A single (posterior) column is relied on for fusion
-
Lengthening of the anterior spinal column and adjacent vascular structures
surgery are best suited for younger patients with modest deformities in
whom sagittal correction at several levels is desirable. The presence
of a mobile disc also is beneficial because it accommodates anterior
column distraction and posterior column shortening.
releases and grafting offer certain advantages. When the discs are
relatively immobile, anterior releases and morcellized grafting can
increase the amount of correction subsequently achieved at a given
level. Anterior morcellized grafting also is beneficial for fusion,
especially in cases of previous nonunion, or for poor fusion candidates.
-
Broad anterior disc space gapping is present after closure of the osteotomy.
-
Sagittal restoration is incomplete after completion of the osteotomies.
-
In the presence of a long fusion to the
sacrum, anterior structural grafting at L4-5 and L5-S1 helps to
maintain the correction and protect the posterior fixation.
previous anterior and posterior spinal fusion, circumferential
osteotomies or a transpedicular osteotomy is needed.
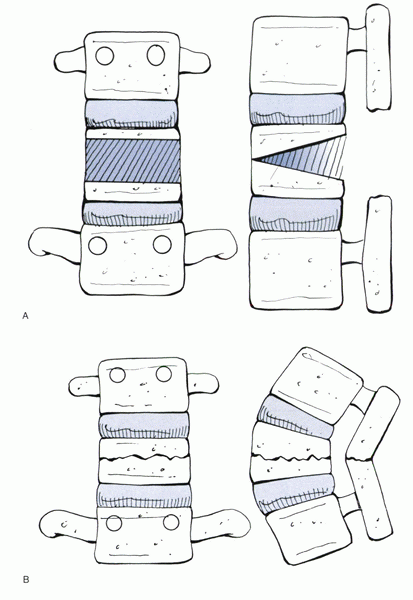
osteotomies involve the resection of a bone wedge extending from the
posterior elements through the pedicles and into the anterior cortex of
the vertebral body (Fig. 21-6). As the
posterior and middle column bone defects are closed, the anterior
vertebral cortex length remains unchanged, and the disc shape remains
unchanged. With closure of the osteotomy, anterior, middle, and
posterior bone surfaces are in contact, providing a significant surface
area for fusion. The level of the osteotomy generally should be at the
area of greatest focal kyphosis. Although pedicle subtraction osteotomy
may be performed at thoracic levels, selection of a level below L1
limits the potential for spinal cord or conus compression. Either L2 or
L3 is usually the best level for a pedicle subtraction osteotomy for
three reasons:
-
L2 and L3 are the normal apex of lumbar lordosis.
-
The levels are typically distal to the cord and conus.
-
Remaining vertebrae caudal to the
osteotomy provide sufficient distal fixation sites without mandating
arthrodesis extension to the sacrum.
producing a greater correction global balance than a more proximal
osteotomy for the same amount of sagittal angular correction. In
general, 30 degrees to 35 degrees of correction may be generated from a
single pedicle subtraction osteotomy. With a 30-degree to 35-degree
correction, the sagittal C7 plumb usually shifts posteriorly 12 to 15
cm (see Fig. 21-4).
-
Ability to produce significant correction at a single level
-
High likelihood of maintenance of reduction and successful osteotomy fusion due to three columns of bone contact
-
Avoidance of the need for a supplemental anterior approach
demanding. Significant mobilization of the dura is required, with the
potential for dural tears and spinal fluid leaks. Bleeding from
epidural veins and osteotomy surfaces can be brisk. The surgeon may
have to go back and forth between multiple osteotomy sites using
thrombin packing and bone wax where necessary to control bleeding.
surgical procedures, which carry an attendant increased risk for
complications. Although nonunion at the level of the osteotomy is
uncommon for pedicle subtraction osteotomy if done through a previous
fusion mass, nonunion may occur at any level after Smith-Peterson
procedures. Degenerated levels above and below a pedicle subtraction
osteotomy are at risk for nonunion and should be addressed with
circumferential fusion. Procedures that require more than 10 to 12
hours of operating time should be staged. Administration of total
parenteral nutrition between stages has been shown to reduce morbidity
associated with infectious complications of the wound, urinary system,
and respiratory system. Medical complications, including pneumonia,
venous thrombosis, and postoperative ileus, are common and are managed
best with an aggressive preventive strategy and postoperative team
approach.
not be regarded as a “cure.” Although a high degree of satisfaction is
reported after these procedures, patients often continue to experience
some degree of discomfort, although markedly less than preoperatively.
When solid arthrodesis is achieved, the patient’s function may return
to near-normal levels, with restrictions only on heavy lifting,
repetitive activities, and contact sports. Correction of adult spinal
deformity has been shown to have positive effects on self-image, pain,
and function as measured by the Scoliosis Research Society outcomes
instrument.
of the fusion have significant bearing on the scope of surgery required
and how well it is tolerated by the patient. Elderly patients tend to
have more preoperative medical comorbidities and less physiologic
reserve than younger adults. As a result, older patients are at greater
risk for medical complications, such as pneumonia, postoperative ileus,
deep venous thrombosis, and infection. Osteoporotic bone, common in
older adult deformity patients, makes obtaining and maintaining secure
implant fixation more challenging. Multiple points of fixation,
anterior interbody structural grafting, and use of a postoperative
brace help “protect” the corrected position of the spine while fusion
takes place.
 |
|
Figure 21-6 (A)
Schematic depicting a pedicle subtraction osteotomy. After the posterior element resection has been performed, the pedicles are cannulated, and a wedge of the vertebral body is decancellated. When the vertebral body is decancellated sufficiently, the triangular portion of cortical bone is resected from the lateral aspect of the vertebral body bilaterally. Finally, a rectangular portion of the posterior cortex of the vertebral body is resected. Closure of the osteotomy may occur spontaneously with gravity or may require lordotic force application through patient repositioning or posterior instrumented compression. (B) Schematic depiction of pedicle subtraction osteotomy closure with restoration of regional lordosis. Ideally, boneto-bone posterior element contact is achieved after closure of the osteotomy. The central canal, lateral recess, and foramen should be evaluated during and after osteotomy closure to confirm that stenosis has not occurred inadvertently. |
fusions (5% to 30%) often is recognized by a shift in spinal alignment,
new onset of pain, or radiographically by loosening at the bone-implant
interface or implant failure. Pseudarthrosis may present early or late
depending on the rigidity of the implant construct used, the level
involved, and the demands of the patient. With the use of segmental
fixation points and more rigid implant systems, it is becoming
increasingly common for a pseudarthrosis to go unrecognized for 5 years
or more after surgery. Multiple risk factors for pseudarthrosis have
been identified (Table 21-4). Areas
particularly prone to the development of pseudarthrosis are the
lumbosacral junction, the thoracolumbar junction, and segments that
have undergone decompression. For long fusions to the sacrum, four
points of fixation in the sacrum and ilium provide the greatest
resistance to implant loss of fixation. Anterior discectomies and
interbody fusion with either structural cages or femoral ring
allografts provide additional biomechanical stability and surface area
for fusion. Consideration should be made for performing anterior
discectomies and structural grafting at levels that are at increased risk.
spinal deformity are uncommon, occurring in less than 5% to 15% of
cases. Risks are greater for cases with severe rigid curves that are
managed through anterior and posterior approaches and with correction
of a severe kyphotic deformity. Direct injury to neural elements can
result from instrumentation (hooks, wires, and screws) or from indirect
injury caused by ischemic insult or neurapraxia due to distractive
forces. In these cases, consideration should be given to a staged
correction to provide for stress relaxation of the tensioned structures
and accommodation of neural elements to any borderline ischemia. In the
case of osteotomies, nerve root or dural constriction may result if the
edges of the osteotomy site are not undercut carefully to allow for
adequate space for the neural elements after correction of the
deformity. Neurologic sequelae may be detected intraoperatively with
the use of neurophysiologic monitoring, including somatosensory evoked
potentials, motor evoked potentials, and selective nerve
electromyography. Although these modalities are relatively efficacious
for detecting spinal cord and conus dysfunction, select cauda equina
nerve root compression (especially unilateral) may go unnoticed. Early
detection provides the opportunity to intervene and possibly to reverse
the offending process. Despite many monitoring advances, a wake-up test
remains the gold standard.
|
TABLE 21-4 RISK FACTORS FOR PSEUDARTHROSIS AFTER LONG FUSIONS FOR ADULT SPINAL DEFORMITY
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
to 6% of patients undergoing posterior spinal fusion. Infection after
anterior spinal fusion is far less common. Nutritional depletion has
been shown to predispose to the development of infection. Total
parenteral nutrition is recommended in patients who are malnourished
(decreased albumin, prealbumin, and transferrin) preoperatively. In
addition, elderly patients and patients at risk for nutritional
depletion who are undergoing staged procedures should be administered
parenteral nutrition between stages.
is more challenging than what is observed with pediatric patients. Most
adults with flexible thoracic and thoracolumbar deformities fare well
with posterior surgery alone. Adults with decompensated deformities,
rigid curves, and involvement of the lumbosacral junction often benefit
from combined anterior discectomies and fusion and posterior segmental
instrumented fusion. Sagittal malalignments are corrected reliably
using a combination of spinal osteotomies and segmental fixation.
Although complications commonly occur, studies show a significant
improvement in patient-reported pain and function and a high degree of
satisfaction in most adult deformity patients after spinal
reconstruction.
M, Bridwell KH. Segmental analysis of the sagittal plane alignment of
the normal thoracic and lumbar spines and thoracolumbar junction. Spine
1989;14:717.
JH, Mirkovic S, Noble PC, et al. Results of operative treatment of
idiopathic scoliosis in adults. J Bone Joint Surg 1995;77A: 513-523.
CC, Bridwell KH, Patel A, et al. Thoracolumbar deformity arthrodesis to
L5 in adults: the fate of the L5-S1 disk. Spine 2003; 28:2122-2131.
DE, Lenke LG, Bridwell KH, et al. An analysis of sagittal plane
alignment in 100 asymptomatic middle and older aged volunteers. Spine
1995;12:1351-1358.
RP, McManus AC. Radiographic analysis of sagittal plane alignments and
balance in standing volunteers and patients with low back pain matched
for age sex and size: a prospective controlled clinical study. Spine
1994;9:1611.
TR, Bridwell HH, Lewis SJ, et al. Minimum two-year analysis of
sacropelvic fixation and L5/S1 fusion utilizing S1 and iliac screws.
Spine 2001;26:1976-1983.
MO, Bradford DS, Moe JH, et al. Treatment of symptomatic flatback after
spinal fusion. J Bone Joint Surg 1988;70A:569-580.
