Rotator Cuff Tear: Arthroscopic Treatment
III – Shoulder Reconstruction > Part B – Evaluation and Treatment of
Shoulder Disorders > 40 – Rotator Cuff Tear: Arthroscopic Treatment
a routine procedure following a general trend toward using less
invasive procedures. Proponents of this technique emphasize the
decreased risk of complications such as infection, stiffness, and
deltoid avulsions, whereas critics mention the lack of long-term
studies, the controversy over the strength of fixation, and the
technical challenge of all-arthroscopic repair of large tears for
inexperienced practitioners. To help address the latter, this chapter
will provide an overview of the indications, technique, and
rehabilitation associated with arthroscopic rotator cuff repair.
combination of intrinsic and extrinsic factors is likely responsible
for most rotator cuff tears. Intrinsic factors relate to the quality of
the tendon substance itself, such as the chronic degeneration brought
on by the relative hypoperfusion of a watershed area close to the
insertion on the greater tuberosity, in conjunction with repetitive
microtrauma.
implicated in rotator cuff tears. External or outlet impingement, the
most common form, is caused by compression of the rotator cuff tendons
as they pass underneath the coracoacromial arch. Narrowing of the
subacromial space can be caused by the acromion itself as a result of
arthritic changes of the acromioclavicular joint or by posttraumatic
changes after proximal humerus fractures, especially with displacement
of the greater tuberosity. In contrast, internal impingement is a
controversial entity that has been described more recently and is
thought to occur primarily in overhead and throwing athletes. Its
anatomic correlate consists of undersurface fraying of the
infraspinatus tendon where it contacts the posterior glenoid as the arm
is placed in maximum abduction and external rotation, such as the late
cocking phase of throwing. Although this contact may often be present
physiologically, the repetitive injury and eccentric loading associated
with throwing can lead to labral and rotator cuff tears. Last, and
intrinsically related to internal impingement, is secondary or
nonoutlet impingement. This is often described as a dynamic process in
which subtle subluxation of the humeral head with activity can acutely
narrow the subacromial space and thus lead to impingement symptoms. It
is associated with mild glenohumeral instability but can also result
from contracture of the posterior capsule, which causes obligate
anterosuperior humeral head translation with forward flexion.
tears enables the physician to formulate a treatment plan to address
the specific pathology present in a particular patient.
at 7% to 25% and the incidence at 10 per 1,000 per year, peaking at 25
per 1,000 per year among those 42 to 46 years of age. However, these
are likely underestimates, as a large proportion of patients with
rotator cuff tears remain asymptomatic. It is clear, nonetheless, that
rotator cuff tears are strongly related to age; magnetic resonance
imaging (MRI) scans of participants without shoulder pain reveal
partial- and full-thickness rotator cuff tears in 4% of individuals
younger than 40 years of age and in >50% older than 60 years.
Furthermore, autopsy studies have demonstrated a prevalence of
full-thickness rotator cuff tears of 6% in subjects younger than 60
years and 30% in those older than 60 years, although it was unknown how
many of these had shoulder pain. Overall, the number of individuals
with
rotator
cuff dysfunction is expected to grow with an aging population that is
increasingly active and less willing to accept functional limitations.
and extrinsic factors leads to chronic tendon degeneration with
eventual tensile failure. Rarely, acute tensile overload can lead to
rupture of a healthy or minimally degenerated tendon. Most tears occur
in and around the critical zone of the supraspinatus, an area between
the bony insertion and musculotendinous junction, with relative
hypoperfusion leading to increased susceptibility to damage. The
natural history of rotator cuff dysfunction is not well understood.
Prior investigations have demonstrated that 50% of individuals with
asymptomatic tears developed pain within 5 years, although only 30%
demonstrated increases in tear size. Studies investigating partial
tears of the rotator cuff have demonstrated enlargement or progression
to full-thickness tears in 80% of patients over a period of 2 years
with nonoperative therapy. Once tears occur, there seems to be little
to no evidence of spontaneous healing. A histopathologic study showed
no signs of healing in pathologic specimens from partial-thickness
tears. Furthermore, although shoulder complaints may be short lived,
one study reported persistence or recurrence of symptoms in 40% to 50%
of individuals 1 year after the initial presentation. It should also be
understood that irreversible changes occur over time in the muscle
tendon complex in the setting of rotator cuff detachment.
thickness and do not lead to retraction of the muscle. Depending on the
location within the rotator cuff tendon, partial-thickness tears can be
classified as intrasubstance, bursal sided, or articular sided
(undersurface), the latter constituting approximately 90% of partial
tears. Weakness is uncommon in partial thickness tears but can arise
from pain, which is often greater than in complete tears.
discontinuity of rotator cuff fibers resulting in communication between
the articular and bursal spaces. The extent of the lesion on imaging
studies is described in both anteroposterior and mediolateral
directions. One centimeter is generally considered small, 1 to 3 cm
medium, 3 to 5 cm large. and >5 cm massive. Tears that involve two
or more tendons can also be classified as massive and require more
complex reconstruction. In larger tears, chronically retracted muscles
undergo fatty degeneration over time that may be irreversible and may
make results of direct repair unsatisfactory.
tear configuration. Crescent-shaped, L-shaped, and U-shaped tears have
been described, all of which require slight modifications in repair
technique to achieve excellent fixation (see below).
of insidious onset extending over the lateral arm and shoulder.
Overhead activities exacerbate the pain, and pain frequently increases
at night and may awaken the individual from sleep. Weakness with the
inability to abduct and elevate the arm is seen in more advanced cases;
patients frequently describe difficulties combing hair, holding a hair
dryer, and removing the wallet from their back pocket. Acute onset of
weakness, especially in association with trauma, may indicate an acute
tear.
rotator cuff repair follows the standard shoulder exam described in
earlier chapters. As in any preoperative evaluation, assessment of
associated pathology that could be encountered at the time of surgery
is crucial. The biceps tendon, capsulolabral complex, acromioclavicular
joint, acromion, and especially the subscapularis tendon are structures
that may require additional interventions that could considerably
prolong and complicate an all-arthroscopic procedure. Recognition of
the size, shape, and tissue quality is crucial to a successful
arthroscopic repair.
and osteophyte formation may indicate arthritis of the glenohumeral or
acromioclavicular joints. Calcium deposits from calcifying tendonitis
usually present just proximal to the rotator cuff insertion. Elevation
of the humeral head on AP radiographs, especially when the subacromial
space is decreased to less than <5 to 7 mm, has been associated with
large rotator cuff tears. The axillary view is essential to exclude the
possibility of a dislocation. This view also shows the joint space and
helps identify the rare but occasionally symptomatic os acromiale,
which is a persistent and ununited ossification center at the end of
the acromion. The 30-degree caudal tilt view is useful to assess the
condition of the acromioclavicular joint. Finally, the supraspinatus
outlet view allows visualization of the bony structures of the
scapulothoracic motion interface and shows acromial spurs or
calcification of the coracoacromial ligament that might compress the
underlying rotator cuff.
inexpensive. Recent studies using arthroscopy or MRI for validation of
ultrasound have demonstrated sensitivities of 58% to100% and
specificities of 78% to 100% for full-thickness tears. It is less
accurate in the detection of partial-thickness tears with sensitivities
ranging from 25% to 94%.
100% for full-thickness tears and has all but replaced arthrography for
the diagnosis for rotator cuff pathology. Moreover, the additional
quantitative and qualitative information gleaned from this
cross-sectional
study aids in the surgical planning and prognosis. The combination of
MRI and gadolinium arthrography further improves sensitivity,
especially for the detection of partial tears, to >90%, and of
labral pathology to >80%. Important concerns regarding MRI include
the associated cost and high frequency of false-positives. Up to 30% of
asymptomatic volunteers have findings of rotator cuff anomalies, and up
to 50% show labral anomalies.
images preoperatively to determine tear size and location, as well as
tissue quality, since massive tears with retraction and fatty
degeneration of the muscle might prove to be irreparable. Coronal
images best show the supraspinatus and degree of tendon retraction,
axial images best display subscapularis disruption, and sagittal images
will give an estimate on the width of the cuff insertion that is
disrupted.
virtually all patients with rotator cuff pathology. One exception is
the young patient presenting with acute weakness owing to a traumatic
event. Conservative treatment includes subacromial steroid injections
and anti-inflammatory medications to control pain in the acute period,
followed by a physical therapy program designed to increase muscle
strength and balance. This is best accomplished with attention to
proper rehabilitation of the scapular stabilizers, the remaining intact
rotator cuff, and the anterior deltoid.
follow those of open rotator cuff repair. The primary indication for
surgical treatment is persistent pain unresponsive to nonoperative
measures; poor function and diminished strength are secondary
indications. The ideal surgical candidate is a compliant patient with
adequate tendon quality who can follow a rigorous postoperative
rehabilitation program. All patients should recognize that the results
are dependent on many factors including tear size and retraction,
tissue quality, muscle degeneration and atrophy, and overall health of
the patient.
repair include active or recent infection, medical comorbidities that
make surgery or anesthesia unsafe, and advanced glenohumeral arthritis
requiring arthroplasty. Relative contraindications may include
significant fatty infiltration of the involved muscles and fixed
superior migration of the humeral head with marked retraction of tendon
edges on MRI.
relieve pain and improve shoulder function while addressing all
concomitant intra-articular pathology in a minimally invasive manner.
Many technical aspects of arthroscopic rotator cuff surgery are
evolving as our understanding of failure mechanisms and patient
outcomes grows. Many issues remain controversial, such as the need for
routine acromioplasty, the management of incomplete tears, optimal
suture management, and anchor configuration—single row versus double
row. Nonetheless, the successful arthroscopic treatment of rotator cuff
tears depends on recognition of tear patterns, appropriate use of
releases, secure fixation with restoration of the footprint under
minimal tension, and proper rehabilitation.
acromioplasty as part of the decompression prior to initiating repair.
This may improve visualization in addition to reducing potential
external compression of the cuff from the anterolateral acromion while
affording space for the repaired tendon to clear the acromion during
rotation. However, recent studies have suggested that routine
performance of an acromioplasty may not be necessary. The primary
technical concern while performing the acromioplasty relates to release
of the coracoacromial (CA) ligament. A complete release of the ligament
should be avoided, especially in large and massive rotator cuff tears,
since it provides a restraint to superior escape of the humeral head in
the rotator cuff deficient shoulder. An adequate acromioplasty,
however, can easily be performed even without complete release of the
CA ligament. Also, sparing the most anterior attachment of the CA
ligament, as well as the deltoid fascia, helps to minimize fluid
extravasation during subacromial arthroscopy.
under general anesthesia with endotracheal intubation, laryngeal mask
ventilation, regional anesthesia through an interscalene nerve block,
or a combination thereof. The decision is made in collaboration with
the patient and anesthesiologist. Regional anesthesia is beneficial
especially for same-day surgical procedures since its analgesic effects
commonly continue for several hours past discharge. Pre-emptive
analgesia with nonsteroidal anti-inflammatories (NASAIDs) given the
night before the operation is being used by an increasing number of
surgeons and is usually continued for several days postoperatively.
Concerns are emerging, however, regarding the potential inhibitory
effects that NSAIDs might have on the early healing process.
in either the beach-chair or lateral decubitus position. Although each
position has unique advantages and limitations, both are acceptable
choices for arthroscopic rotator cuff repair.
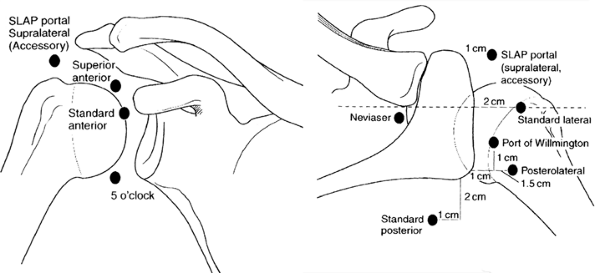
include standard posterior, anterior, anterolateral, and posterolateral
portals (Fig. 40-1) as described in previous
chapters. Anchor placement occasionally requires accessory portals that
deviate from the standard portals described above. These portals should
be kept as small as possible to minimize injury to the deltoid muscle
and used only for percutaneous anchor placement without the use of a
cannula. Another portal that we have recently described and find
particularly
useful
is the posteromedial portal, which is placed approximately 3 cm medial
to the standard posterior portal and allows an in-line passage of a
suture retrieving instrument (i.e., penetrating suture grasper).
 |
|
Figure 40-1 Standard portals in shoulder arthroscopy.
|
standard anterior and posterior portals to evaluate potentially
associated pathology. After the rotator cuff tear is visualized, it is
often helpful to mark the exact location by passing a suture
percutaneously through the tear into the subacromial space, especially
in small tears, which can be difficult to visualize once the
subacromial space is entered.
an arthroscopic bur and radiofrequency ablation device to control
bleeding. The rotator cuff tear is judiciously debrided simply to
freshen the leading edge. The insertion site on the greater tuberosity
(footprint) is cleaned of soft tissues and gently superficially
debrided to create a bleeding subcortical surface.
their capsular attachments or are adherent to surrounding tissue.
Releasing these attachments and adhesions with an electrothermal device
or an arthroscopic elevator is crucial to obtaining full cuff
mobilization. With a grasper or traction suture on the leading edge,
the surgeon can evaluate the results of the performed release. If the
tendon can be reduced to the footprint only by applying significant
tension, further releases should be performed to allow for a
tensionfree repair.
 |
|
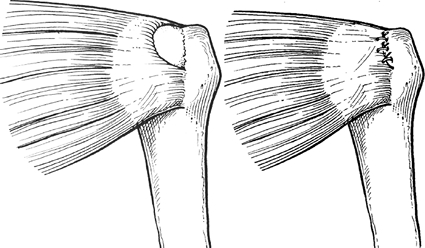
Figure 40-2 Crescent-shaped tear and repair.
|
and the undersurface of the acromion. Anterior releases in the rotator
interval region can separate adhesions between the supraspinatus and
the coracoid and subscapularis. Occasionally, posterior release between
the supraspinatus and infraspinatus is required. In long-standing
tears, the cuff may be adherent to the glenoid neck, and releasing the
capsule adjacent to the superior and posterior labrum is particularly
useful. However, the suprascapular nerve and vessels are at risk during
this dissection, which should not extend further than 1 to 2 cm medial
to the glenoid rim.
been described. Crescent-shaped tears are more commonly found acutely
or subacutely and usually are easily mobilized and repaired directly to
bone with suture anchors (Figure 40-2).
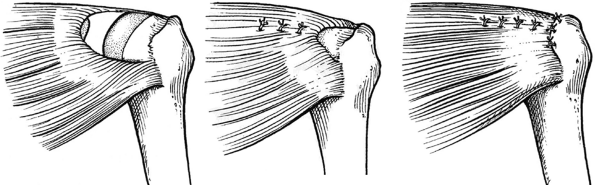
U-shaped tears are usually larger and may require side-to-side repair
(i.e., margin convergence) to reduce tear size and decrease tension on
the leading edge, thus allowing for a more stable repair to the
tuberosity (Figure 40-3). L-shaped tears are
best addressed with a side-to-side repair of the longitudinal limb
before securing the horizontal limb to bone with suture anchors (Figure 40-4).
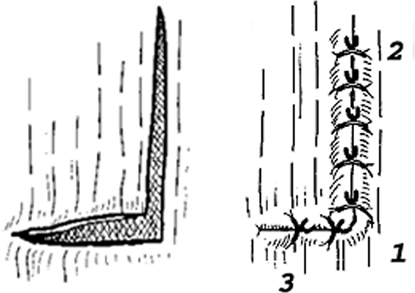
Side-to-side repairs are performed with free sutures that can be passed
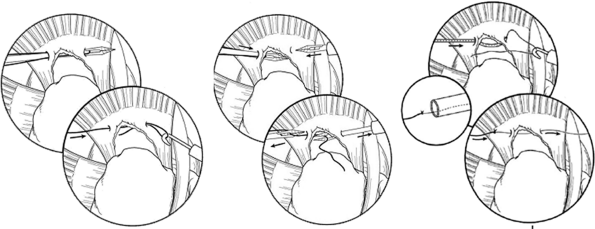
through the tendon substance with various instruments and techniques (Figure 40-5).
Our preference is to use a straight penetrating suture grasper when
working in the posterior two thirds of the cuff as well as during
repair of the more medial extent of the side-to-side
component of the tear. More laterally and anteriorly, a straight shuttle-type suture passing device is more effective.
 |
|
Figure 40-3 U-shaped tear and repair.
|
 |
|
Figure 40-4 L-shaped tear and repair.
|
performed with various techniques. The two most common portal
configurations involve visualization through the lateral portal with
instrumentation through the posterior or posteromedial portal (our
preference), and vice versa. The first step is to prepare the footprint
on the greater tuberosity to obtain an optimal environment for healing.
Increasingly, surgeons refrain from extensive decortication during
preparation of the footprint with an arthroscopic bur since it does not
appear to improve healing and can compromise suture anchor fixation.
footprint uses suture anchors, which can be either bioabsorbable or
metal, depending on surgeon preference. Advantages of bioabsorbable
anchors include decreased artifacts on follow-up MRI and eventual
resorption, potentially making revisions easier and reducing concerns
over loose anchors that could damage the joint. Advantages of metal
anchors include lower cost, decreased risk of anchor breakage during
insertion, and lack of reactivity in the surrounding bone. Anchors are
placed in the lateral aspect of the footprint for a single-row
technique, or medially and laterally for a double-row technique in
larger tears amenable to this anchor/suture configuration. The
double-row technique reduces tension on the lateral anchors and secures
the tendon to a larger bony surface.
be passed through the rotator cuff tendon. There are many devices on
the market to facilitate this process; however, the senior author
prefers working with low-profile penetrating suture graspers for the
posterior cuff in combination with a 45-degree ipsilateral (i.e., right
curve for right shoulder) curved suture shuttle device for the more
anterior aspect of the tear. Alternatively, there are several excellent
devices that can be passed with a loaded suture directly through the
anterolateral or lateral portal (while viewing from posteriorly) and
passed antegrade directly through the lateral tendon edge. Whenever
shuttling or making use of the antegrade suture passing device, it is
helpful to avoid having more than a single suture limb within the
cannula at any given time to avoid entanglement.
retraction when placing sutures. Since most tears of the supraspinatus
and infraspinatus tendons retract in a posteromedial fashion, sutures
should be placed more posteriorly relative to the anchor to restore
proper tendon orientation. Suture anchors should be placed in a
methodical order to help with suture management, often from posterior
to anterior. Sutures should be stored in unused cannulas to avoid
entanglement, and only one suture should be kept in a working cannula
during knot tying. We typically, whenever possible, place a central and
medial anchor loaded with two sutures and retrieve all four limbs with
a penetrating suture grasper placed through the posteromedial or
posterior portal, creating two independent horizontal mattress sutures.
Next, we place at least two additional anchors beginning more posterior
and lateral to the first medial anchor already in position. The final
anchor is placed typically just behind the bicipital groove in line
with the second more laterally placed anchor.
 |
|
Figure 40-5 Side-to-side repair techniques for margin conversion sutures: antegrade (left), antegrade hand-off (middle), and antegrade shuttle (right) techniques.
|
a successful repair. Although many different sliding and nonsliding
techniques have been described, the senior author prefers simple half
hitches on alternating posts. This reliable and simple method does not
require sliding of the suture through the tissue, which has been
incriminated in suture cutout. Irrespective of the technique used, care
must be taken to ensure that the knot tightly reduces the tendon to the
anchor and bony bed of the footprint to allow healing.
have been comparable to open reconstruction, despite the fact that
radiologic investigations have demonstrated a comparatively higher rate
of recurrent tears on MRI follow-up. Between 77% and 98% of patients
are satisfied with their outcome after rotator cuff repair, with
excellent pain relief and functional improvement in >80%. Benefits
of arthroscopic repair versus open or mini-open techniques include
smaller incisions with less soft tissue dissection, avoidance of
deltoid detachment, improved visualization of the entire glenohumeral
joint for evaluation and treatment of concomitant pathology, and
decreased postoperative pain. However, arthroscopic repair has been
associated with a significant rate of recurrent tears. Our own results
have demonstrated a retear rate of ≤47% at 2 years on MRI examination.
Nonetheless, clinical results do not seem to suffer in these patients.
We have found significantly improved functional and pain scores, as
well as improved strength, even in the setting of a recurrent tear,
with patients rating their postsurgical shoulder at 85% of their normal
contralateral side.
reported in <1% of cases. Traction injuries of the brachial plexus
occur as very rare complications when shoulder arthroscopy is performed
in the lateral decubitus position, but are usually transient. The
incidence of minor complications related to edema from fluid
extravasation is unknown and is typically inconsequential; however,
there have been reports of subcutaneous emphysema causing serious
pulmonary complications during shoulder arthroscopy, which emphasizes
the need for continued monitoring of the patient’s shoulder and neck
for excessive swelling or crepitus.
most important factors in achieving a good result. Postoperatively,
patients are typically placed in a sling and a supportive abduction
pillow, which is worn at all times, except for hygiene and therapeutic
exercise. The rehabilitation program is divided into three phases,
which are based on the progression of healing with increasing strength
of the reconstruction:
passive range of motion (ROM), with limits of motion based on
intraoperative assessment of repair stability. Therapeutic exercises
during this phase include pendulum exercises; elbow, wrist and hand
ROM; grip strengthening; and isometric scapular stabilization.
and ROM is progressed to 140 degrees of forward flexion, 40 degrees of
external rotation, abduction to 60 to 80 degrees, and posterior
capsular stretching to maintain or improve internal rotation.
Therapeutic exercises are advanced to gentle active-assisted exercises
in the supine position with progression to active exercises with
resistance at 6 weeks. Deltoid and biceps strengthening is initiated,
with the arm kept close to the side to minimize lever arm forces on the
rotator cuff.
by progression to full motion as tolerated. Scapular strengthening is
continued, and internal and external rotation isometric exercises are
added to the program. During the
final
phase of rehabilitation, sport-specific activities are initiated,
flexibility is maintained, and strengthening exercises are continued.
Usually, formal physical therapy is discontinued after approximately 4
months, with return to unrestricted athletic activities at 6 months.
JE, Flanagan CL, Thomopoulos S, et al. The effects of overuse combined
with intrinsic or extrinsic alterations in an animal model of rotator
cuff tendinosis. Am J Sports Med. 1998;26: 801–807.
B, Weishaupt D, Zanetti M, et al. Fatty degeneration of the muscles of
the rotator cuff: assessment by computed tomography versus magnetic
resonance imaging. J Shoulder Elbow Surg. 1999;8:599–605.
LM, Ball CM, Teefey SA, et al. The outcome and repair integrity of
completely arthroscopically repaired large and massive rotator cuff
tears. J Bone Joint Surg Am. 2004;86A:219–224.
GM, O’Connor DP. Arthroscopic rotator cuff repair with and without
arthroscopic subacromial decompression: a prospective, randomized study
of one-year outcomes. J Shoulder Elbow Surg. 2004;13:424–426.
SH, Ha KI, Park JH. et al. Arthroscopic versus mini-open salvage repair
of the rotator cuff tear: outcome analysis at 2 to 6 years’ follow-up. Arthroscopy. 2003;19:746–754.
HC, Dewan N, Crosby L. Subcutaneous emphysema, pneumomediastinum, and
potentially life-threatening tension pneumothorax. Pulmonary
complications from arthroscopic shoulder decompression. Chest. 1992;101:1265–1267.
N, Zehetgruber H, Kainberger F, et al. Rotator cuff tears in
asymptomatic individuals: a clinical and ultrasonographic screening
study. Eur J Radiol. 2004;51(3):263–268.
SN, Seitz WH Jr. Sonography of the shoulder in patients with tears of
the rotator cuff: accuracy and value for selecting surgical options. AJR Am J Roentgenol. 1993;160:103–107; discussion 109–110.
K, Tetro AM, Blam O, et al. Natural history of asymptomatic rotator
cuff tears: a longitudinal analysis of asymptomatic tears detected
sonographically. J Shoulder Elbow Surg. 2001;10(3): 199–203.
