Frozen Shoulder
III – Shoulder Reconstruction > Part B – Evaluation and Treatment of
Shoulder Disorders > 46 – Frozen Shoulder
by functional restriction of both active and passive motion.” Zuckerman
et al. further classified frozen shoulder into primary and secondary
groups. Primary frozen shoulder was considered idiopathic. Secondary
frozen shoulder was divided into intrinsic, extrinsic, and systemic
subtypes (Table 46-1). More specific,
quantitative definitions have been sought. Diagnostic criteria have
included duration of symptoms, loss of motion, and radiographic
evaluation. Significant variability in the diagnostic criteria has made
treatment and outcome studies difficult to compare (Table 46-2).
definition no clear cause. There are, at best, associations that link
underlying disease processes to loss of soft tissue compliance. A
cellular basis for disease has been speculated. Deficiencies in
cellular immunity, identified in some studies, have been thought to
result in an autoimmune disease resulting in capsular contracture.
However, reports have not been consistent among investigators, and this
proposed cause remains controversial.
shoulder capsule tissue culture analysis has demonstrated trisomy seven
and eight in seven patients with frozen shoulder. Trisomy seven has
been identified in the tissue of the Dupuytren contracture suggesting a
similar common pathway. In addition, cellular mechanisms related to
metalloproteinases, enzymes that control collagen remodeling, and
cytokines have been implicated.
fracture, nonsurgical soft tissue trauma such as rotator cuff tear or
contusion, tendonitis, and arthritis. These are considered causes of
secondary frozen shoulder that are intrinsic to the shoulder joint
itself. Extrinsic conditions may occur with secondary frozen shoulder.
These include neurologic injuries from head trauma, brain surgery or
cerebrovascular accident, cervical radiculitis, brachial plexopathy,
thoracic outlet syndrome, and peripheral nerve palsy. Antiepileptic
treatment with phenobarbitone has been associated with frozen shoulder.
Other associated conditions include cardiac disease and cardiac
surgery, thoracic tumors such as bronchogenic carcinoma and Pancoast
tumor. Desmoid tumors of the shoulder girdle presenting as frozen
shoulder have been recently reported. Systemic disease may also be
associated with secondary frozen shoulder. These diseases include
diabetes, hypothyroidism, hyperthyroidism, polymyalgia rheumatica,
myositis, and many other systemic illnesses.
the shoulder joint capsule. Advanced glycosylation end products (AGEs)
accumulate in the basement membranes of diabetics. The accumulation of
AGEs results in irreversible cross-links between adjacent protein
molecules. This appears related to acquired defects in vascular
compliance in diabetics and may reflect a common pathway that leads to
arthrofibrosis in the diabetic population. Association of frozen
shoulder with diabetes, thyroid disease (both hypothyroidism and
hyperthyroidism), hyperlipidemia, and other systemic illnesses is
clearly seen. The exact mechanism(s) that lead to capsular restriction
have yet to be delineated definitively.
5% in the general population. It is generally considered more common in
women than men, but this is not consistent across all studies. The age
presentation is most commonly 40 to 60 years. However, it may occur
earlier in long-standing insulin-dependent diabetics. Incidence of
frozen shoulder in diabetics has been reported from 10% to as high as
35%. Diabetics with frozen shoulder are more likely to have additional
organ involvement.
disease are unusual in the general population, but may occur in
diabetics. Both shoulders may be affected in 6% to 34% of patients
across multiple studies. Diabetics appear to be more likely to develop
bilateral stiffness (≤40%).
|
TABLE 46-1 Primary and Secondary Frozen Shoulder
|
||||||
|---|---|---|---|---|---|---|
|
decreased capsular compliance. Loss of external rotation with
associated scarring and contracture of the rotator interval capsule,
coracohumeral, and superior glenohumeral ligaments is pathognomic of
frozen shoulder.
-
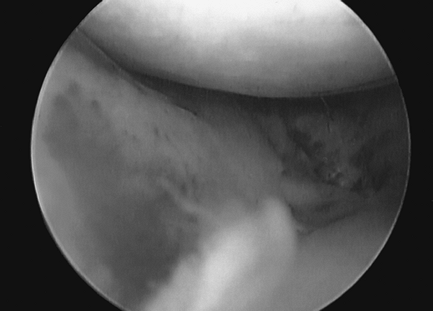
The initial phase (“freezing phase”) is
marked by insidious onset of pain of increasing severity. This lasts
from a few weeks up to 9 months. It is associated with the loss of
active and passive motion. Arthroscopy and histology studies
demonstrate acute synovitis (Fig. 46-1). -
The second phase (“frozen phase”) is
associated with less pain. The hallmark of this phase is global
shoulder stiffness. Comfort for activities of daily living is achieved
within the patient’s limited range. The duration of this phase may be 3
to ≥12 months. Pathologic specimens demonstrate extensive fibrosis with
high cellular populations of fibroblasts and myofibroblasts. -
The final phase
(“thawing phase”) is characterized by return of motion toward normal
over a period of 5 to 26 months on average. This phase, however, has
been cited in the literature to extend as far as 8 to 10 years
following the onset of symptoms. Outcome studies regarding the natural
history of the thawing phase are clouded by lack of consistent study
inclusion criteria. Methodology frequently has been retrospective and
without control groups. Patient numbers have generally been small, and
frequently studies have included mixed treatments and causes. Despite
this, reports suggest persistent mild pain and/or stiffness in ≤50% of
patients. At mean follow-up, Binder, Bulgen and colleagues reported
little functional impairment in 40 out of an initial study group of 42
patients. However, 45% of patients continued to have pain and/or
restricted range of motion.
|
TABLE 46-2 Clinical Diagnosis of Frozen Shoulder
|
|
|---|---|
|
 |
|
Figure 46-1 Joint synovitis encountered at arthroscopy.
|
phases of clinical presentation. The physician is challenged to
identify the stage and evaluate the patient for other causes or
associated disease processes. Concurrent bilateral involvement is
relatively uncommon. Initial presentation of concurrent bilateral
frozen shoulder may suggest systemic disease. It is incumbent on the
clinician at all stages to evaluate for possible associated conditions.
This necessitates a careful and thorough general medical history.
characterized by pain without history of significant trauma. Aching
unrelieved by rest and worsening at night is frequent. Loss of range of
motion is pathognomic. The patient may present with protective
posturing of the arm in an adducted internally rotated position against
the body. The physical examination is generally notable for severe pain
with range of motion. X-ray films taken at this time are generally
negative, though there may be slight osteopenia.
pain. Significant motion restriction is noted with pain generally at
the extremes of available motion. There is functional restriction of
activities of daily living. Night pain remains common.
activity limitations associated with loss of range of motion. Generally
over the course of observation, both range of motion and night pain
demonstrate gradual improvement. Despite improvement, studies suggest
that motion remains limited relative to the contralateral normal
extremity in ≥50% of patients.
complexes as well as the upper extremity is essential. Exam of the
shoulder should include the following:
-
Inspection and palpation of the neck and shoulder to include both the glenohumeral and scapulothoracic articulations
-
Cervical spine range of motion with the Spurling test
-
Assessment of range of motion according
to the American Shoulder and Elbow Surgeons (ASES) standard format.
Motion arcs of the affected and unaffected shoulder are recorded for
the following:-
Forward elevation in the sagittal plane
-
External rotation at the side (ERS)
-
External rotation at 90 degrees of coronal abduction if possible (ERA)
-
Internal rotation at 90 degrees of coronal abduction if possible (IRA)
-
Cross-body adduction measuring the difference from the antecubital fossa to the opposite shoulder (XBA)
-
Internal rotation/extension up the back (IRB)
-
-
Strength is recorded for forward
elevation, abduction, and external and internal rotation. Ancillary
strength testing may include belly press. The lift-off test may be
difficult to assess if significant posterior capsular contracture
and/or pain does not allow adequate glenohumeral internal rotation.
Additional active tests may include the supraspinatus stress test and
the Whipple test.A distal upper extremity exam should be performed to
assess range of motion and strength. This will assist in evaluating for
secondary neurologic conditions (i.e., cervical radiculopathy, complex
regional pain syndrome, brachial plexopathy, and others).
external rotation. Outlet and true axillary views complete the shoulder
series. Radiographs are inspected for fracture, tumor, calcific
tendonitis, arthritis, and subacromial spurring.
rotator cuff and bony anatomy in a patient with weakness or unusual
presentation. Common findings in frozen shoulder are thickening of the
coracohumeral ligament and rotator interval capsule. Synovitic
abnormalities at the top of the subscapularis tendon and volume loss at
the axillary recess are noted.
and treatment of frozen shoulder. The clinician may elect to order
selective tests if an underlying systemic disease or infection is
suspected.
the relief of pain and restoration of motion in 90% of patients.
Physical therapy may be done at home with monthly visits to the
therapist and surgeon, or more extensive formal evaluation and
treatment may be performed as indicated. Basic exercises include supine
active assisted forward elevation, supine external rotation with a
stick, cross-body adduction, and standing towel exercises for internal
rotation up the back. Multiple repetitions are performed and held for
firm end field stretch without pain. The hallmark of stretching in
frozen shoulder is repetition of exercises multiple times throughout
the day. Prospective studies suggest “supervised neglect,” described as
supportive therapy and exercises within the pain limit, produced
superior 24-month outcome compared with vigorous stretching. Techniques
of translational manipulations or glides may also be used by the
therapist. Range of motion and visual analog pain scores have been
noted to improve with this technique using regional anesthesia.
demonstrated to assist with pain relief. Patients who used analgesics
and exercise were shown to have greater improvement than with exercise
alone. Short-course oral prednisolone was shown to have short-term
benefit over placebo with regard to pain and motion at 3-week
follow-up. Benefits compared with placebo were not maintained beyond 6
weeks.
controversial. Results of intra-articular injections are difficult to
interpret because they are frequently associated with other treatment
modalities. In patients with painful stiffness, a 50% improvement in
pain scores associated with injection has been reported. Bulgen et al.
reported early improvement in pain and range of motion with no
long-term advantage in comparing patients receiving intra-articular
injection with
an
untreated control group. Intra-articular glucocorticoid injection with
and without joint distension was compared prospectively.
Intra-articular lidocaine (19 mL volume) and 20 mg of triamcinolone
hexacetonide was compared with triamcinolone hexacetonide alone.
Injection was confirmed by ultrasound and repeated with an end point of
a maximum of six weekly injections or no symptoms. Pain measured by
visual analog scale was no different between groups, but the distension
group showed improvement in range of motion. Comparison with normal
controls or opposite shoulder evaluation was not provided.
glucocorticoid injection may assist in pain relief in frozen shoulder.
Thus, injection may facilitate early rehabilitation.
months of worsening symptoms despite compliance with home exercise or
failure to improve motion over 6 months of treatment. Loew et al. have
reported on 30 consecutive patients with primary frozen shoulder
resistant to analgesics and therapy for 6 months. They noted excellent
restoration of range of motion with manipulation. Manipulation was
performed gently following their standard protocol. This included the
following:
-
General anesthesia in a supine position
-
Measurement of premanipulation range of motion
-
Manipulation with the humerus held close to the axilla to diminish lever arm effect
-
Forward elevation and internal rotation with light traction
-
Cross-body adduction to stress and release the posterior capsular contracture
-
External rotation stretch from neutral (ERS)
-
External rotation at 90 degrees of scapular abduction
demonstrated capsular ruptures anteriorly (24 of 30), posteriorly (16
of 30), and superiorly (11 of 30). Four patients had acute superior
labral anterior posterior (SLAP) tears. Four patients had anterior
labral detachments; one of which was osteochondral. Three patients had
partial tears of the subscapularis tendon, and two had middle
glenohumeral ligament tears.
or after local anesthetic intra-articular distension. Harryman and
Lazarus describe a protocol for manipulation under anesthesia. Their
protocol is as follows:
-
Sagittal plane elevation with observation for crepitant lysis of scar
-
Cross-body adduction
-
Abducted internal rotation followed by internal rotation with the arm adducted
-
Internal rotation up the back if the patient is awake and cooperative
-
External rotation in 90 degrees of
coronal abduction followed by external rotation after carefully
lowering the arm to an adducted position
benefit in that it allows for painless patient cooperation in the
instruction and reinforcement of the postsurgical stretching program.
Stretches are repeated multiple times daily following hospital
discharge with emphasis on achieving forward elevation, rotation, and
posterior capsular stretching. Postmanipulation intra-articular
injections with steroids may be used to diminish postsurgical
inflammation and pain. Injection, however, has not been shown to
enhance outcome.
the obvious inability to visualize intra-articular pathology available
with arthroscopy. A cumulative 1% complication rate has been reported.
Complications include rotator cuff tear, fracture, nerve palsy, and
dislocation. Insulin-dependent diabetics have poor outcomes with regard
to maintenance of range of motion following manipulation. The overall
recurrent stiffness rate is between 5% and 20% including diabetic and
nondiabetic patients.
stiffness with glenohumeral scarring, muscle contracture, and excessive
extra-articular scarring. An open approach is indicated when
lengthening of the subscapularis is required following an anterior
instability procedure. Resection of spurs and heterotopic bone may also
be performed efficiently via an open approach.
incision may be used for release of the rotator interval capsule and
coracohumeral ligament. This may be combined with gentle manipulation
to restore motion.
the posterior capsule from this anterior approach. If it is necessary
to release the middle and inferior glenohumeral ligaments, a
subscapularis take-down may be necessary. This necessitates restriction
of rehabilitation postsurgically to protect the subscapularis repair.
Open release followed by manipulation under anesthesia has been shown
to improve range of motion and pain relief with mean follow-up
approaching 7 years in some studies.
joint. Inflamed synovium may be resected with a shaver and capsular
release performed with arthroscopic basket or cautery.
-
Inability to achieve full range of motion with gentle manipulation under anesthesia
-
Consideration in insulin-dependent diabetics with resistant contractures
-
Patients with significant osteopenia in whom there is a concern of fracture with manipulation
-
Postsurgical and posttraumatic stiff shoulder where recurrent fracture or soft tissue injury may occur with manipulation
positioned just cephalad to the standard posterior portal. Entry into
the joint may be difficult secondary to scarring and contracture. The
blunt trocar is advanced into the joint carefully to avoid iatrogenic
articular injury. A secondary anterior portal is selected just superior
to the rolled board of the subscapularis. This may be localized using a
spinal needle from an outside-in technique. The cannula enters the
joint slightly laterally along the upper border of the subscapularis.
associated pathology. If the biceps is scarred and immobile, it is
tenotomized at the glenoid rim.
posterior capsular resection first. They note that fluid extravasation
posteriorly is limited by the infraspinatus muscle. They recommend
using arthroscopic basket forceps to spread the muscle off the capsule.
A posterior superior followed by direct posterior and posterior
inferior release are performed. A rotary shaver is used to resect the
edges of the capsular release.
arthroscope may be used from the front or the arthroscope alternatively
may be positioned in the posterior superior portal. An additional
posterior portal is positioned approximately 2 cm caudal and 1 cm
lateral to the high posterior portal. A spinal needle can be used to
localize the best position such that the approach is parallel to the
floor of the axillary pouch. The capsule is incised outside the labrum
and close to the glenoid. The axillary nerve passes obliquely
anteromedial to posterolateral along the inferior margin of the
capsule. Authors suggest that an arthroscopic basket forceps be used to
spread the extracapsular tissue off the inferior capsule prior to
incising the capsule. This is preferred to avoid axillary nerve injury.
release with attention to the coracohumeral and superior glenohumeral
ligament is performed. The anterior superior release is performed above
the biceps and labrum. The coracoacromial ligament and conjoined tendon
are visualized from the posterior intra-articular arthroscopy portal.
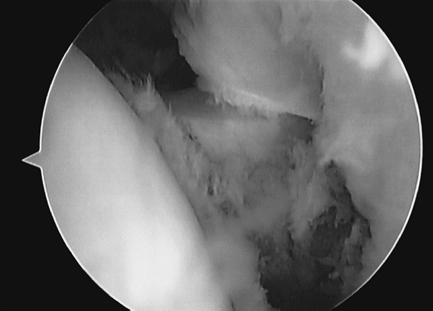
Attention is turned to release of the middle glenohumeral ligament (Fig. 46-2)
and anterior aspect of the inferior glenohumeral ligament connecting
the release inferiorly. Debris may be resected with a motorized shaver.
The blades of the shaver are positioned away from the axillary nerve
and rotator cuff with judicious use of suction.
 |
|
Figure 46-2 Anterior capsular release. Middle glenohumeral ligament has been incised revealing subscapularis tendon.
|
to the inferior glenoid neck protects the axillary nerve. General
anesthesia is preferred. If the deltoid is stimulated, the bipolar
direction is changed. Maintaining the cautery along the glenoid rim and
using accessory portals for improved access in the axillary pouch is
helpful.
 |
|
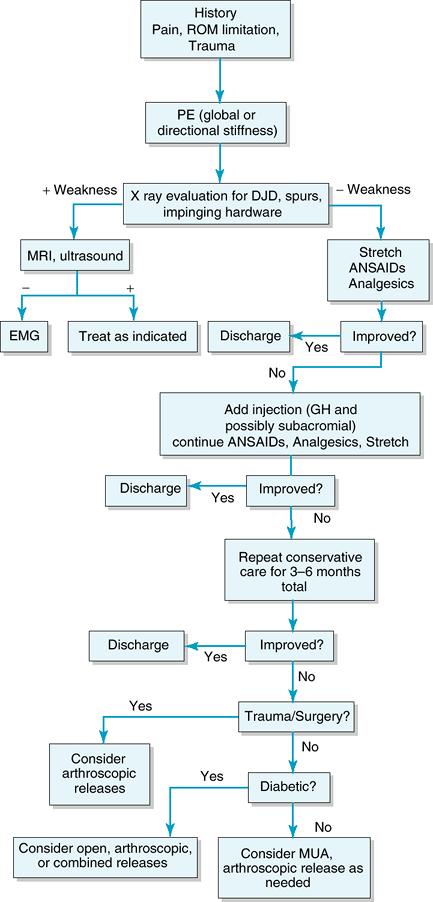
Figure 46-3
Algorithm for treatment of frozen shoulder. ROM, range of motion; PE, physical examination; DJD, degenerative joint disease; MRI, magnetic resonance imaging; NSAIDs, nonsteroidal anti-inflammatory drugs; EMG, electromyogram; GH, glenohumeral; MUA, manipulation under anesthesia. |
performed. Idiopathic frozen shoulder pathology is classically a
primary intra-articular capsular fibrotic process, and subacromial
findings may be limited. However, in the posttraumatic stiff shoulder,
significant subacromial adhesions may be present, necessitating
extensive debridement. Acromioplasty is performed if there is abrasion
of the undersurface of the coracoacromial ligament or significant
spurring.
manipulation to assess range of motion is performed. An intra-articular
steroid may be used.
immediately. Interscalene anesthesia can be helpful, and the patient
may be discharged with a home exercise program. Postsurgical admission
may be beneficial if pain control or medical factors are of concern.
Continuous interscalene anesthesia may also be used to facilitate early
and frequent range of motion.
been reported extensively throughout the literature. Studies have
generally found significant increase in both Constant scores and ASES
scores. Ogilvie-Harris et al. noted in a comparative series of 20
patients undergoing manipulation under anesthesia and 20 patients
undergoing arthroscopic release that range of motion was similar but
surgical arthroscopic release provided better function and pain relief
overall at a mean follow-up of 2 to 5 years.
include risks and complications inherent to surgical procedures
including infection, bleeding, and nerve injury. One report of
transient axillary neurapraxia was found. Postoperative instability has
not been noted. Persistent stiffness has been reported. Despite 50% of
their patients demonstrating persistent stiffness in internal rotation,
Segmuller et al. demonstrated 88% satisfactory outcome. Two of three
patients dissatisfied with their final outcome were diabetic. In
stratifying groups based on causes, patients with idiopathic frozen
shoulder appear to do better than those with secondary posttraumatic or
postsurgical stiffness. Diabetics have been demonstrated to do
initially worse in terms of motion and pain relief with comparable
final outcomes to those of patients without diabetes.
demanding procedure, but is generally a safe procedure with few
complications noted in the literature (Fig. 46-3).
R, Hoving JL, Green S, et al. Short course prednisolone for adhesive
capsulitis (frozen shoulder or painful stiff shoulder): a randomized,
double blind, placebo controlled trial. Ann Rheum Dis. 2004; 63:1460-1469.
AN, Schydlowsky P, Rossel I. Treatment of “frozen shoulder” with
distention and glucocorticoid compared with glucocorticoid alone: a
randomized controlled trial. Scand J Rheumatol. 1998; 6:425-430.
