Magnetic Resonance Imaging
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Magnetic Resonance Imaging
Magnetic Resonance Imaging
Laura M. Fayad MD
Description
-
MRI is a noninvasive diagnostic technique that uses hydrogen atoms in the body to create an image.
-
MRI has several advantages over other imaging techniques:
-
Higher contrast resolution
-
More sensitive than CT in detecting bone marrow/soft-tissue disease
-
-
No exposure to irradiation
-
Multiplanar imaging capability
-
Indications:
-
Evaluation of joints
-
Detection of ligament or tendon
pathology; fibrocartilage tears (e.g., menisci, glenoid labrum);
hyaline cartilage defects; and associated bone marrow changes of
arthritis -
Detection and characterization of synovial disease (e.g., PVNS, synovial osteochondromatosis)
-
-
Evaluation of bone marrow:
-
Determination of extent of bone marrow
tumors for treatment planning; residual or recurrent bone tumor after
treatment (distinction between viable tumor and necrosis, degeneration,
hemorrhage, and fibrosis) -
Detection of osteomyelitis, bone marrow
edema, and (occasionally) tumors (although plain radiographs often
serve as the 1st line of diagnosis for tumors)
-
-
Evaluation of soft tissues:
-
Detection and definition of extent of
soft-tissue tumors with respect to muscle, compartmental involvement,
and extension to neurovascular bundles -
Determination of residual or recurrent
disease after treatment (distinction between viable tumor and necrosis,
degeneration, hemorrhage, and fibrosis) -
Characterization of a limited number of soft-tissue tumors
-
-
Tests
-
Technique:
-
Prescription of MRI sequences varies, depending on the indication.
-
In general, sequences for joint
evaluation are designed to depict the anatomy and detect fluid around
injured articular structures, whereas for the evaluation of bone and
soft-tissue tumors, T1 and T2 properties of the tissue are used to
detect and characterize disease. -
Sequences for joint evaluation:
-
High-resolution noncontrast sequences
-
Intermediate-weighted (proton density)
-
T1-weighted
-
3D gradient echo
-
-
Fluid-sensitive noncontrast sequences:
-
Fat-suppressed T2-weighted
-
STIR
-
-
MRA (postcontrast, T1-weighted):
-
Direct MRA: Contrast directly into the joint
-
Indirect MRA (1): Contrast injected intravenously; imaging shortly thereafter
-
Used for increased specificity for
ligament injuries, evaluation of OCDs, detection of intra-articular
bodies, and postoperative determination of recurrent injuries
-
-
-
Sequences for tumor/infection evaluation:
-
T1-weighted
-
Fluid-sensitive sequences (as noted earlier)
-
Gradient echo for detecting calcification or hemosiderin
-
Contrast-enhanced T1-weighted images:
-
For posttreatment evaluation to determine residual or recurrent disease
-
Adds specificity to detection of osteomyelitis and soft-tissue tumor characterization
-
-
-
Advanced techniques (e.g., diffusion
weighted imaging and magnetic resonance spectroscopy) are under
investigation and may become useful clinically.
Pathological Findings
-
Internal derangement of joints:
-
Shoulder:
-
Fluid signal in the rotator cuff tendon indicates a tear; partial is distinguished from full-thickness by depth of fluid signal.
-
Fatty atrophy of rotator cuff muscles is seen as increased signal on T1-weighted images.
-
Biceps tendon subluxation or dislocation
is well visualized on axial views; tendon splits or complete tears are
detected in 3 planes (axial, coronal, sagittal). -
Glenoid labral tears are identified by
abnormal morphology and fluid dissecting deep to or within the labrum;
paralabral cysts may be located in the suprascapular or spinoglenoid
notch. -
Acromial shape (flat, curved, hooked) and subacromial spurs are detected on sagittal oblique views.
-
-
Elbow:
-
Collateral ligament tears are detected by fluid or contrast through the ligament, best seen on coronal oblique views (Fig. 1).
-
Medial and lateral epicondylitis present
as flexor or extensor tendinosis (increased T2 signal), partial tear
(fluid signal partly dissecting through the tendon), or complete tear
(complete disruption of tendon with only fluid at origin); may be
accompanied by bone marrow edema at epicondyles.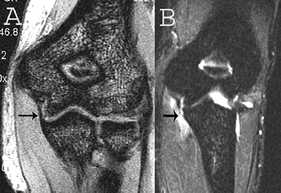 Fig. 1. Coronal images of the MCL. A: 3D gradient echo showing the normal anterior bundle of the MCL (arrow). B: Fat-suppressed T2-weighted images showing a completely torn distal attachment.
Fig. 1. Coronal images of the MCL. A: 3D gradient echo showing the normal anterior bundle of the MCL (arrow). B: Fat-suppressed T2-weighted images showing a completely torn distal attachment. -
Biceps tendon pathology is best seen on axial views at the insertion on radial tuberosity.
-
Triceps tendon pathology is best seen on sagittal and axial views at the insertion on the olecranon.
-
Bone marrow edema secondary to arthritis or fracture is detected on fluid-sensitive sequences.
-
Intra-articular bodies may have variable signals.
-
-
Wrist:
-
TFCC normally is dark on all sequences:
Degeneration, perforations, and tears are defined by abnormal signal
within the fibrocartilage; tears are associated with distal radioulnar
joint effusion. -
Intrinsic ligament (scapholunate and
lunotriquetral ligaments) tears are detected by fluid or contrast
passage through the ligament. -
All abnormalities and extrinsic ligaments may be better shown by MRA.
-
Carpal tunnel is assessed on axial views for median nerve enlargement or signal abnormality and flexor tendon pathology.
-
Ulnar nerve and Guyon canal are assessed on axial views for possible mass or ulnar artery aneurysm.
-
Articular cartilage defects may be detected directly or indirectly (the latter through associated bone marrow changes).
-
Kienböck disease typically is accompanied by diffuse decreased signal in the lunate.
-
Hook of hamate fractures: Axial views are best.
-
-
Hip:
-
Fractures can be identified by linear signal abnormality and surrounding bone marrow edema.
-
MRI is useful for rapid detection of occult hip fractures (2) and AVN, identified by low signal intensity on T1-weighted and “double line sign” on fluid-sensitive sequences.
-
The degree of involvement of weightbearing surface is aided by sagittal views.
-
-
Acetabular labrum morphology/tears are better identified by direct than indirect MRA.
-
Gluteus and hamstring tendons normally are dark on all sequences, but when torn, the MRI shows fluid signal.
-
-
Knee:
-
The most sensitive sequence for meniscal
tears is the intermediate-weighted sequence, which shows tears as
increased signal reaching the meniscal surface. -
Flipped fragments may be detected as a double PCL sign (sagittal view) or occasionally seen in the medial gutter (coronal view).
-
Postoperative meniscal evaluation may be aided by MRA.
-
Complete ACL tears are detected by frank
disruption with abnormal signal, failure to parallel Blumensaat line,
and secondary signs (anterior tibial translation, specific contusion
pattern). -
Collateral ligament sprains may be grade
1 (abnormal signal adjacent to ligament), grade 2 (fluid signal within
and adjacent to ligament), or grade 3 (complete disruption of ligament)
(3). -
Patellar tendinosis manifests with abnormal thickness and signal, and tendon tears are accompanied by fluid signal.
-
Quadriceps tendon tears should be assessed in all 3 planes (sagittal, coronal, and axial) for width of involvement.
-
Articular cartilage defects may be
detected in several ways: T1-weighted 3D gradient echo sequences, as
decreased signal; fluid-sensitive sequences, as fluid at the defect
site, often accompanied by underlying bone marrow abnormalities;
contrast-enhanced T1 sequences, as contrast at site of defect
-
-
Ankle:
-
The Achilles tendon normally is dark on
all sequences: Degeneration may be detected by abnormal thickness and
internal signal; tears are seen as fluid signal. -
PTT pathology is seen as abnormal tendon
thickness or abnormal signal within the tendon; associated findings are
PTT dysfunction (heel valgus deformity, midfoot fault, and os
naviculare). -
Peroneal tendon subluxation is detected
by axial views: Presplit condition (boomerang deformity) or actual
split of the peroneus brevis tendon is detectable in 3 planes; complex
fluid in peroneal sheath suggests tenosynovitis. -
Lateral ankle ligament (talofibular and
tibiofibular) injuries are classified as grade 1 (increased signal),
grade 2 (partial tear with fluid signal), or grade 3 (complete
disruption) (4). -
Sinus tarsi normally contains fat and is
best evaluated on a sagittal T1-weighted image for loss of fat signal
in sinus tarsi syndrome. -
Plantar fasciitis accompanied by
increased signal and abnormal thickness of the plantar fascia may have
associated reactive bone marrow edema in the calcaneus.
-
P.243 -
-
Tumors:
-
Bone:
-
A tumor appears as a marrow replacement process on T1-weighted images (5).
-
T2-weighted images are useful for defining extension into adjacent soft tissues.
-
Contrast-enhancement is useful for differentiating posttreatment residual or recurrent disease from fibrosis.
-
Fluid levels may be identified in bone
cysts, giant cell tumors, chondroblastomas, telangiectatic
osteosarcoma, and any lesion with a fracture (Fig. 2).
-
-
Soft tissue:
-
Only a small percentage of tumors (including lipomas, cysts, and vascular malformations) can be characterized definitively.
-
Some lesions (e.g., nerve sheath tumors,
giant cell tumor of a tendon sheath, some fibrous tumors such as
elastofibroma and desmoid tumors) have a few specific MRI
characteristics. -
Contrast enhancement characteristics may
help distinguish benign and malignant soft-tissue lesions, but much
overlap occurs in enhancement (6).
-
-
Differential Diagnosis
-
Notes on interpretation:
-
An MRI scan should be reviewed in conjunction with a plain radiograph.
-
Magic angle effects occur in cartilage,
tendons, and ligaments when they are oriented 55° to the main magnetic
field and cause increased signal on short time-to-echo sequences. -
MRI of the shoulder: Much normal variant anatomy occurs at the anterosuperior labrum and may simulate a labral tear.
-
MRI of the elbow: A pseudodefect of the capitellum occurs posteriorly, whereas OCDs of the capitellum occur anteriorly.
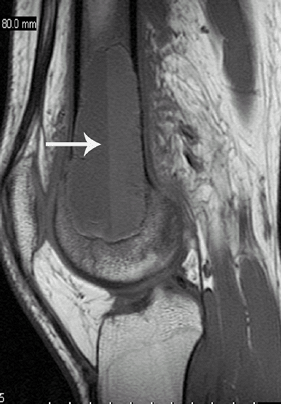
![]() Fig. 2. Sagittal T1-weighted image showing distal femur telangiectatic osteosarcoma with fluid-fluid levels (arrow).
Fig. 2. Sagittal T1-weighted image showing distal femur telangiectatic osteosarcoma with fluid-fluid levels (arrow). -
MRI of the wrist: Ulnar variance by MRI
must be assessed with caution because positioning of the wrist during
scan affects apparent variance. -
MRI of the hip: The sacrum and pubic bones always are evaluated for causes of referred hip pain.
-
MRI of the knee: Menisci should be evaluated in all planes (7).
-
Pediatric Considerations
Pediatric patients, particularly those <5 years old, usually require sedation.
Pregnancy Considerations
MRI is considered safe in pregnancy, although informed
consent is obtained before the examination is performed and contrast is
administered with great caution.
consent is obtained before the examination is performed and contrast is
administered with great caution.
Complications
Contraindications to MRI include cardiac pacemaker,
implanted cardiac defibrillator, aneurysm clips, carotid artery
vascular clamp, neurostimulator, insulin or infusion pump, implanted
drug infusion device, bone growth/fusion stimulator, and cochlear,
otologic, or ear implants.
implanted cardiac defibrillator, aneurysm clips, carotid artery
vascular clamp, neurostimulator, insulin or infusion pump, implanted
drug infusion device, bone growth/fusion stimulator, and cochlear,
otologic, or ear implants.
References
1. Steinbach LS, Palmer WE, Schweitzer ME. Special focus session. MR arthrography. Radiographics 2002;22:1223–1246.
2. Quinn
SF, McCarthy JL. Prospective evaluation of patients with suspected hip
fracture and indeterminate radiographs: use of T1-weighted MR images. Radiology 1993;187:469–471.
SF, McCarthy JL. Prospective evaluation of patients with suspected hip
fracture and indeterminate radiographs: use of T1-weighted MR images. Radiology 1993;187:469–471.
3. Schweitzer
ME, Tran D, Deely DM, et al. Medial collateral ligament injuries:
evaluation of multiple signs, prevalence and location of associated
bone bruises, and assessment with MR imaging. Radiology 1995;194:825–829.
ME, Tran D, Deely DM, et al. Medial collateral ligament injuries:
evaluation of multiple signs, prevalence and location of associated
bone bruises, and assessment with MR imaging. Radiology 1995;194:825–829.
4. Erickson SJ, Smith JW, Ruiz ME, et al. MR imaging of the lateral collateral ligament of the ankle. AJR Am J Roentgenol 1991;156:131–136.
5. Nomikos GC, Murphey MD, Kransdorf MJ, et al. Primary bone tumors of the lower extremities. Radiol Clin North Am 2002;40:971–990.
6. van
der Woude HJ, Verstraete KL, Hogendoorn PCW, et al. Musculoskeletal
tumors: does fast dynamic contrast-enhanced subtraction MR imaging
contribute to the characterization? Radiology 1998;208:821–828.
der Woude HJ, Verstraete KL, Hogendoorn PCW, et al. Musculoskeletal
tumors: does fast dynamic contrast-enhanced subtraction MR imaging
contribute to the characterization? Radiology 1998;208:821–828.
7. Magee T, Williams D. Detection of meniscal tears and marrow lesions using coronal MRI. AJR Am J Roentgenol 2004;183:1469–1473.
Patient Teaching
-
The patient should expect to be in the MRI scanner, motionless, for 20–40 minutes.
-
Intravenous contrast may be administered, depending on the indication.