Ulnar Nerve
-
Subjective complaints include loss of dexterity in the hand, which results in clumsiness, dropping things, or weakness.
-
Numbness in the ring and little fingers may be prominent symptoms, and may be verified on physical examination.
-
Motor weakness of the intrinsic muscle
may be present in early cases, and atrophy of the intrinsic muscles may
be present in late cases or severe compression of the motor component
of the nerve. -
A characteristic claw deformity of the ring and little fingers may be observed with motor deficit.
the ulnar nerve and artery traverse to gain entrance to the hand from
the forearm. Guyon’s canal begins at the proximal edge of the palmar
carpal ligament and ends at or beyond the fibrous arch of the
hypothenar muscles. Beginning from proximal to distal, the roof of the
canal is formed by the palmar carpal ligament, portions of the palmar
aponeurosis, and the palmaris brevis muscle. The floor is formed by the
TCL, the pisohamate and pisometacarpal ligaments, and the FDM. The
ulnar wall is composed of the flexor carpi ulnaris (FCU), the pisiform,
and the ADM. The radial wall is formed by the tendons of the extrinsic
flexors, the TCL, and the hook process of the hamate. The average
length of Guyon’s canal is 27 mm, with a range from 20 to 34 mm. The
ulnar nerve and artery branches in this region are covered by the
palmaris brevis muscle, and are surrounded by a thick fat pad.
 |
|
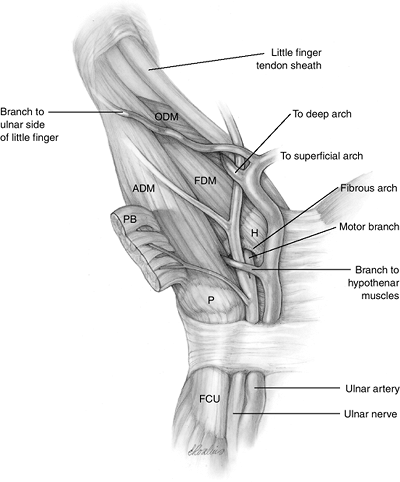
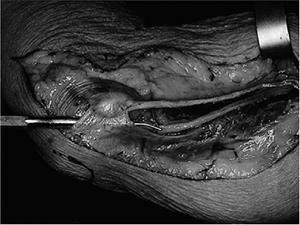
Figure 7.2-1
The ulnar nerve in Guyon’s canal. The ulnar nerve may divide into motor and sensory components proximal to, at, or in Guyon’s canal, but the most common configuration is division in Guyon’s canal an average of 8.6 mm (range, 0–15 mm) from the proximal edge of the pisiform. H, hook process of hamate; P, pisiform. |
radial side, enters the hand on the radial side of the pisiform bone
through Guyon’s canal (Figure 7.2-1). The ulnar
nerve may divide into motor and sensory components proximal to, at, or
in Guyon’s canal, but the most common configuration is division in
Guyon’s canal at an average of 8.6 mm (with a range of 0 to 15 mm) from the proximal edge of the pisiform.
pisiform is ulnar and dorsal. The motor branch gives off one to three
(usually two) branches to the hypothenar muscles before it enters the
depths of the palm. Its course into the palm has been variously
described as passing between the origin of the FDM and ODM, or beneath
the proximal origin of the FDM. It then courses around the ulnar and
distal aspect of the base of the hook process of the hamate. The
proximal edge of the FDM often demonstrates a fibrous arcade, where the
motor branch may become entrapped. It then traverses the hand to
innervate the ring and small finger lumbricals, the palmar and dorsal
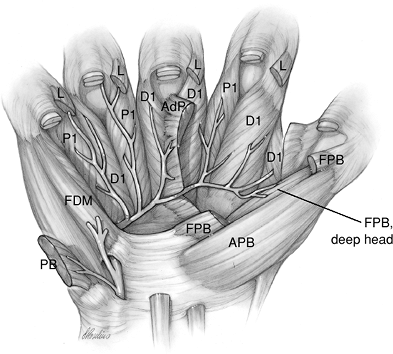
interossei, the adductor pollicis, and the deep head of the FPB (Figure 7.2-2).
in Guyon’s canal, the sensory component divides into the sensory branch
to the ulnar side of the little finger, and the common sensory nerve to
the fourth web space, which subsequently divides into the PDN to the
radial side of the little finger and the ulnar side of the ring finger.
The motor branch to the palmaris brevis usually arises from the sensory
branch to the little finger.
in identification of the most common or likely causes of nerve
compression in the ulnar tunnel. Zone 1 is from the proximal edge of
the proximal commissural ligament (PCL) to the bifurcation of the ulnar
nerve. Zones 2 and 3 are parallel zones that begin at the bifurcation
of the nerve and that end at the region just beyond the fibrous tissue
arch of the hypothenar muscles. Zone 2 contains the motor branch of the
ulnar nerve, and zone 3 contains the sensory branch of the nerve. Zones
2 and 3 are not divided by an anatomic structure, but rather are
arbitrary divisions that have useful clinical applications.
|
Table 7_2-1 Areas and Causes of Ulnar Nerve Compression in Guyon’s Canal
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 |
|
Figure 7.2-2 The deep motor branch of the ulnar nerve in the palm. See text for details.
|
These zones are useful for the localization and correct prediction of
the cause of ulnar neuropathy in Guyon’s canal. This information, along
with a careful history, sensory and motor examination, careful
palpation, Allen’s test, and radiographs of the wrist, may lead to an
accurate prediction of the cause of the ulnar deficit.
-
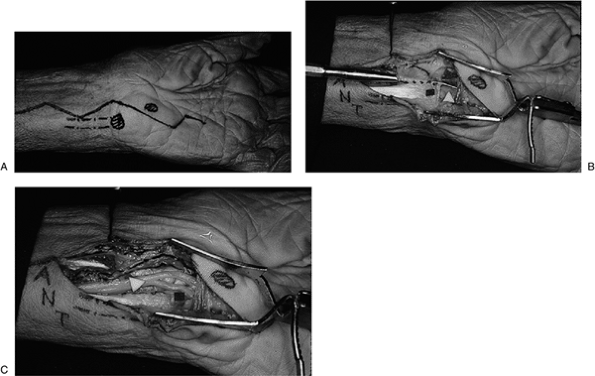
Decompression of the ulnar nerve in
Guyon’s canal is performed through a longitudinal zigzag incision
centered over the interval between the pisiform and the hook process of
the hamate (Figure 7.2-3). -
The roof of the canal is incised to reveal the underlying nerve and artery on the radial side of the FCU tendon.
 |
|
Figure 7.2-3 Surgical approach to Guyon’s canal. (A) A longitudinal zigzag incision is used in the interval between the pisiform and hook process of the hamate (dots) in order to unroof the canal. (B–C)
Note the arrangement of the artery, nerve, and tendon (ANT) from radial to ulnar, and also note the relationship of the nerve to the FCU tendon, pisiform, and hook process of the hamate bone. |
identify a specific site of entrapment of the ulnar nerve, and to
distinguish it from tardy ulnar palsy that is associated with
posttraumatic cubitus valgus
at approximately the midpoint of the arm, and continues distally toward
the elbow behind the medial intermuscular septum on the medial head of
the triceps muscle. The nerve continues to the elbow, where it enters
the fibroosseous cubital tunnel. The tunnel can be divided into three
parts. The first part of the cubital
tunnel is the entrance of the tunnel formed by the ulnar groove in the
medial epicondyle. At this level, the ulnar nerve usually provides one
or several small articular branches to the elbow joint, and these
branches usually are proximal to the branches given off to innervate
the FCU.
of the tunnel consists of a fascial arcade that is a fan shaped
ligament covering the tunnel. It attaches to the medial epicondyle and
to the olecranon, and connects the ulnar and humeral heads of the
origin of the FCU muscle. In this area, the nerve lies on the posterior
and oblique portions of the ulnar collateral ligament, and usually
gives off two branches to innervate the FCU. One branch usually
supplies the humeral head, and one supplies the ulnar head. The first
branch exits the main nerve trunk horizontally. The second branch
continues distally for several centimeters before entering the FCU. Up
to four motor branches to the FCU may be given off, exiting the main
nerve at a point between 4 cm proximal and 10 cm distal to the medial
epicondyle. The motor branches enter the FCU on its deep surface. The
distance between the medial humeral epicondyle and the olecranon is
shortest with elbow extension. This distance increases with elbow
flexion. The roof or fascial arcade becomes taut with elbow flexion.
of the tunnel consists of the muscle bellies of the FCU. The FCU
provides a portion of the roof in this area. The nerve courses through
the interval between the humeral and ulnar heads of the FCU, or between
the FCU and the FDP muscles. It continues distally in the forearm
between the FDP, located dorsally and laterally to the nerve, and the
FCU, located anteriorly and medially. The volume of the tunnel
decreases with elbow flexion, and the pressure within it increases—even
in the normal elbow when the aponeurotic arch or surrounding soft
tissues are not thickened.
much of its course, and also is partially fixed in a fibroosseous
canal. Because of its exposed position, and the fact that it wraps
around the medial condyle in flexion, prolonged elbow flexion—which
stretches the nerve and narrows the tunnel—combined with resting the
elbow on a hard surface may result in paresthesias in the ring and
little fingers. This occurs even in normal people. When swelling of, or
elbow inflammation or congestion of, the flexor-pronator
muscles
is added to this stretch–compression, the vascular supply of the ulnar
nerve may be compromised, and nerve symptoms may result. Sustained
elbow flexion combined with vigorous finger and wrist motion—such as
that which a musician might perform—can also result in ulnar nerve
symptoms. The motions used to throw a ball and for a tennis serve are
similar, and can place significant stress on the ulnar nerve. They may
be associated with ulnar nerve symptoms. Perioperative ulnar
neuropathies are more common in men than in women. Although there is no
gross anatomic difference between the sexes regarding the course of the
ulnar nerve in the upper extremity, there is a significantly larger (2
to 19 times greater) fat content on the medial aspect of the elbow in
women compared to men. Also, the tubercle of the coronoid process on
the ulna is 1.5 times larger in men.
facilitated by knowledge of the potential sites of compression, and of
the anatomy specific to each of those areas.
 |
|
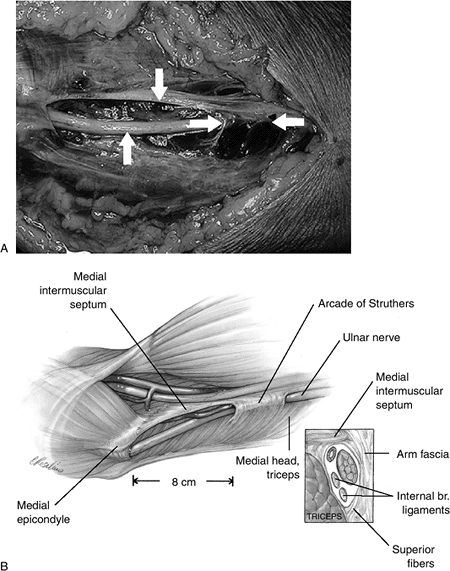
Figure 7.2-4 Fresh cadaver dissection of the so-called arcade of Struther’s. (A)
The appearance of the arcade over the ulnar nerve and its relationship to the medial intermuscular septum (MIMS). Here, the upper vertical arrow marks the MIMS, the lower vertical arrow marks the ulnar nerve, and the opposed horizontal arrows mark the arcade. (B) Artist’s depiction of the relationship of the arcade to the MIMS and the medial epicondyle. |
name and occurrence, there is a potential site of entrapment of the
ulnar nerve that lies 8 cm proximal to the medial epicondyle called the
arcade of Struthers. When the arcade is present, both the ulnar nerve
and the superior ulnar collateral vessels pass through it. In a study
of 25 arms, the arcade of Struthers was present 68% of the time. The
arcade has a medial-facing roof, formed by the deep investing fascia of
the arm, superficial muscle fibers from the medial head of the triceps,
and the internal brachial ligament arising from the coracobrachialis
tendon. The floor, which is lateral, is formed by the medial aspect of
the humerus, and is covered by the deep muscular fibers of the medial
head of the triceps. The anterior border is the medial intermuscular
septum (Figure 7.2-4).
triceps muscle, and this overlying muscle roof may be a source of
compression. When it is, it should be incised.
 |
|
Figure 7.2-5 Fresh cadaver dissection of the medial aspect of the arm and elbow. Note the probe under the cubital tunnel retinaculum.
|
intermuscular septum (MIMS)—and when the ulnar nerve is transposed
anteriorly—it can represent a sharp edge that may cause impingement of
the nerve. The MIMS should be excised as part of ulnar transposition,
as discussed under the treatment section (see Figure 7.2-4).
forearm transits the cubital tunnel, which is an osseous canal formed
by the medial epicondyle and the proximal ulna. It is covered by a
retinaculum formed by the deep investing fascia of the arm that is
attached to the medial epicondyle and the olecranon. This cubital
tunnel retinaculum (CTR) is 2 to 3 cm wide from proximal to distal, and
0.5 to 0.75 mm thick—and its distal margin blends with the investing
fascia of both the humeral and ulnar heads of the FCU. Osborne’s band
and the arcuate ligament are other names often used to describe this
fibrous tissue roof of the ulnar tunnel (Figure 7.2-5).
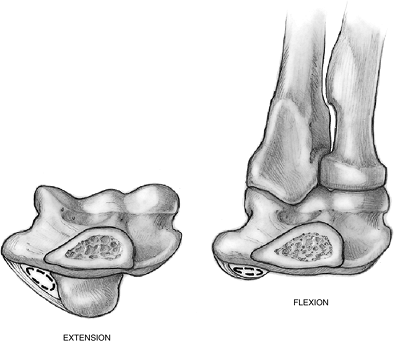
Because of the somewhat eccentric origin of this fascial roof, the
cubital tunnel changes contour and volume during elbow flexion and
extension. In flexion, the cross-sectional contour changes from
slightly ovoid to elliptical (Figure 7.2-6). Any swelling in the canal—or inflammation or thickening of the fascial roof—may compress the nerve or its vasculature.
enters the forearm through the flexor pronator group of muscles,
usually between the humeral and ulnar heads of the FCU. The
flexor-pronator muscles are arranged in two groups. The superficial
group is formed by five muscles (the PT, FCR, PL, FDS, and FCU) that
originate from a common origin created by the fusion of several fibrous
septae. Those septae arise from the anterior surface of the medial
humeral epicondyle, the ulnar collateral ligament, and medial surface
of the coronoid process. They form well-defined fascial compartments
for the muscles, as well as a common aponeurosis from which adjacent
muscles originate. These septae fuse, beginning approximately 3.5 to 4
cm distal to the epicondyle. This fused structure is commonly known as
the flexor-pronator origin, or the flexor-pronator aponeurosis. An
additional aponeurosis in this area is present between the FDS to the
ring finger and the humeral head of the FCU that did not fuse with the
previously described common flexor pronator origin but rather arose
from the medial surface of the coronoid process 0.3 to 0.5 cm medial to
it. If present, it may not be possible to transpose the ulnar nerve
adjacent to the median nerve in a relatively straight course unless
this septum is detached along with the radial two-thirds of the
flexor-pronator group. Others have identified a structure deep to the
FDS, and superficial to both the FDP and the FCU, that provided a point
of origin for all of these muscles. That structure extended
approximately 5 cm distal to the epicondyle. This deep aponeurosis of
the FCU, which bridges and forms a common origin for muscle fibers of
the FCU, FDS, and FDP, should be released by separating the two heads
of the FCU and exploring the deep surface of the muscle for at least 5
cm distal to the epicondyle.
 |
|
Figure 7.2-6 Changes in the cubital tunnel with flexion and extension.
|
-
Clinical findings include complaints of
medial elbow pain, numbness and tingling—or burning—in the ring and
little fingers, hand clumsiness, and weakness of pinch. -
Physical findings may include tenderness
behind the medial condyle over the course of the ulnar nerve, as well
as a positive Tinel’s sign over the nerve 2 cm proximal and distal to
the cubital tunnel. -
Other physical findings include decreased
sensibility in the ring and little fingers, as well as decreased pinch
and grip strength. -
Claw deformity of the ring and little fingers, as well as intrinsic muscle atrophy, are seen in severe and prolonged cases.
-
Physical findings that aid in the
diagnosis are tenderness over the ulnar nerve at the elbow,
reproduction of the patient’s symptoms with elbow flexion, and positive
findings with sensory evaluation. -
Electrodiagnostic studies have a high rate of false negatives.
-
Other causes of symptoms that mimic
cubital tunnel syndrome (such as thoracic outlet syndrome) should be
eliminated by appropriate tests. -
Weakness of the FDS to the little finger
may be present in cubital tunnel syndrome, but not in ulnar nerve
compression at the wrist. This finding may be helpful in distinguishing
these two conditions.
-
Conservative treatment is appropriate for mild and early cases of cubital tunnel that present without motor deficit.
-
Avoidance of elbow flexion and pressure
over the point—or medial aspect—of the elbow, along with oral
anti-inflammatories, may be beneficial.
-
Common to all ulnar nerve transpositions
is elimination of compression or traction problems by removing the
nerve from the fibroosseous tunnel and permanently transposing it to an
anterior location. -
Permanent transposition has been achieved
by subcutaneous transposition, subcutaneous transposition with some
form of tether to prevent the nerve from assuming its original
position, or submuscular or intramuscular transposition. -
The sine qua non
of ulnar nerve transposition is permanent realignment of the ulnar
nerve in an anterior position, without entrapment (absence of
compression) or fixation (traction). Such complications would prevent
the nerve from gliding. -
It also must be recognized that the ulnar
nerve remains subcutaneous throughout most of its new course, and that
even submuscular or intramuscular transposition eliminates only a
portion of this subcutaneous position. -
The effectiveness of transposition is
based on decompression of the nerve and on elimination of any potential
for traction injury. -
A factor in the avoidance of secondary
entrapment following transposition might be early and protected
mobilization of the elbow joint.
ulnar nerve neurolysis without transposition (with or without medial
epicondylectomy) is not addressed in this text. Rather, the reader is
referred to the suggested reading list at the end of this chapter.
