The Adult Ankle and Foot
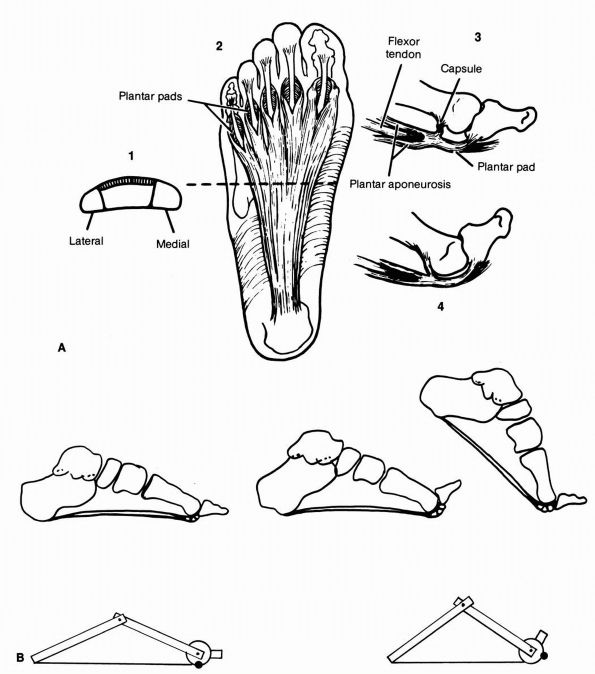
center on the first metatarsophalangeal (MTP) joint. This articulation
alone bears one-third of the weight of the forefoot and helps stabilize
the longitudinal arch through the attachment of the plantar aponeurosis
into its base. Immediately after the foot hits the ground during
ambulation, weight is rapidly transferred from the heel to the
metatarsal head region. As a step is taken, the toes are pushed into
dorsiflexion. The plantar aponeurosis, which arises from the medial
tubercle of the calcaneus and inserts into the base of the proximal
phalanx, is pulled over the metatarsal head. In turn, this passively
depresses the metatarsal heads and raises the arch (Figure 21-1).
This construct is commonly called the “windlass mechanism” after the
nautical term for a device for raising a sail by pulling on a rope.
the potential to disrupt this critical mechanical function. Weight is
then transferred to the lesser metatarsals, and secondary pathology in
the remainder of the forefoot can develop. Because of their significant
implications for the function of the foot, disorders of the hallux
deserve special consideration.
 |
|
FIGURE 21-1. (A)
Plantar aponeurosis. (1) Cross-section. (2) Division of plantar aponeurosis around flexor tendons. (3) Components of the plantar pad and its insertion into the base of the proximal phalanx. (4) Toe in extension with the plantar pad drawn over the metatarsal head. (B) The windlass mechanism functions by the passive dorsiflexion of the metatarsophalangeal joints in the last half of the stance phase, which tightens the plantar aponeurosis and mechanically causes the longitudinal arch to rise. This is probably the main stabilizer of the longitudinal arch of the foot. (A from Mann R, Inman VT. Structure and function. In: Du Vries HL. Surgery of the Foot, 2nd Ed. St Louis: CV Mosby, 1965) |
deformities of the forefoot. It is characterized by lateral deviation
of the first toe and, usually, by medial deviation of the first
metatarsal. It is commonly known as a bunion deformity after the
noticeable prominence on the medial side of the foot. Patients often
confuse the medial prominence of hallux valgus with the dorsal
osteophyte of hallux rigidus and may refer to both disorders as
“bunions.”
directly related to constrictive shoe wear. The disorder was
essentially undescribed until
the
rise of fashionable shoes in France in the 1700s. Numerous surveys of
foot deformities in indigenous populations that go unshod demonstrate
almost a complete absence of hallux valgus except its relatively rare
congenital form. The narrow toe box and raised heel of modern women’s
shoe wear in particular appear to be the primary culprits in the
development of the problem.
The toe not only deviates, but it also rotates into pronation. The nail
turns to face toward the instep. As these deformities develop, the
lateral capsule and the adductor hallucis tendon on the lateral side of
the first MTP joint become contracted. The medial capsule becomes
attenuated. In the majority of cases, the first metatarsal itself
deviates to the medial side, a deformity known as metatarsus primus varus.
While this happens, the intermetatarsal ligament between the second
metatarsal head and lateral sesamoid remains unchanged in length. The
sesamoids therefore retain their original position with regard to the
rest of the foot and the first metatarsal head subluxates off of them.
 |
|
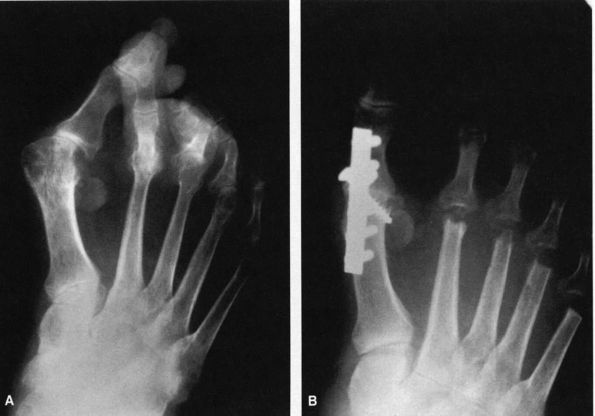
FIGURE 21-2.
Radiograph of a hallux valgus deformity. Note the lateral deviation of the proximal phalanx on the metatarsal head, the medial deviation of the metatarsal head, and subluxation of the sesamoids. |
there is no conservative maneuver that will restore the normal anatomy.
Bunion night splints, toe spacers, and orthotics have all proven
unsuccessful. Nevertheless, a large number of patients find relief with
simple shoe modifications. In general, shoes should be made of soft
material with a minimum of seams over the medial side. The toe box
should be wide and accommodative, and the heel should be minimal. If a
patient has a significant transfer callus under the second metatarsal
head, an orthotic with a metatarsal pad placed immediately behind the
painful site may provide relief.
regardless of the specifics of the deformity, a number of factors must
be evaluated when choosing a strategy for surgical correction. There
are over 100 described operations to correct hallux valgus, and the
choice of procedure is critical to a successful outcome.
bunion deformity are pain at the first MTP joint itself or,
occasionally, pain from secondary pathology in the adjacent toes caused
by overload and crowding from the hallux. The complication rate in
bunion surgery is significant, and there is no role for operations
performed only for cosmesis or to allow a return to highly constrictive
shoe wear.
the neurovascular status is important. Patients without palpable
dorsalis pedis and tibialis posterior pulses should be evaluated by
Doppler exam and, if necessary, referred to a vascular surgeon. Hallux
valgus in particular can cause irritation of the dorsomedial cutaneous
nerve of the hallux, a sensory nerve on the dorsomedial aspect of the
toe. Its status should be assessed carefully.
assessed carefully. Almost all bunion procedures result in some loss of
motion and the patient should be made aware of this outcome. In many
cases, a significant pes planus deformity
would
need to be corrected simultaneously with the hallux valgus and the
status of the arch should be evaluated. The stability of the first
metatarsocuneiform joint should be assessed by stabilizing the lateral
forefoot with one hand while dorsiflexing the first ray separately with
the other.
 |
|
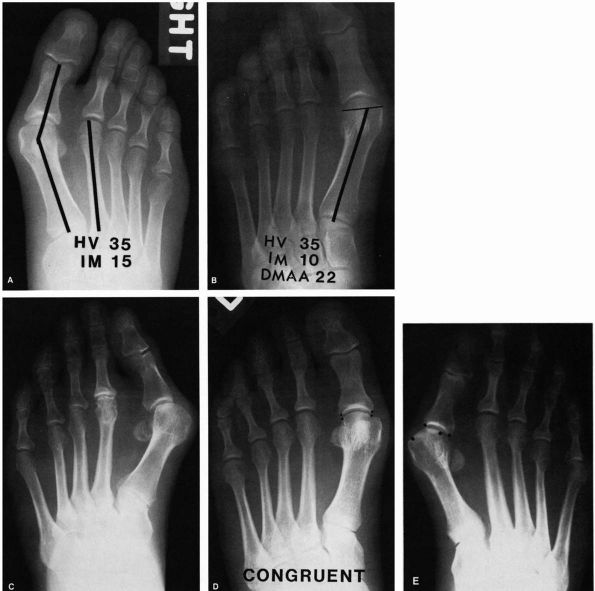
FIGURE 21-3. Radiographic observations of the hallux valgus deformity. (A) Hallux valgus angle: normal (less than 15°). Intermetatarsal angle: normal (less than 9°). (B) Distal metatarsal articular angle (DMAA): normal (less than 10° lateral deviation). (C) Marked obliquity of the metatarsocuneiform joint should alert clinician to possible instability of this joint. (D)
A congruent joint is one in which there is no lateral subluxation of the proximal phalanx on the articular surface of the metatarsal head. (E) The incongruent or subluxated joint has lateral deviation of the proximal phalanx on the metatarsal head. |
-
The intermetatarsal angle formed by the axes of the first and second metatarsals on the AP view.
-
The hallux valgus angle formed by the axes of the first metatarsal and the proximal phalanx of the hallux.
-
The congruity of the joint. In other
words, does the articular surface of the proximal phalanx line up with
that of the metatarsal head or is it subluxated? -
The distal metatarsal articular angle
formed by the alignment of the first metatarsal and the margins of the
joint surface of the first MTP. -
The presence or absence of deformity in the hallux itself.
-
The presence or absence of arthritis at the first MTP or in the midfoot.
-
The presence or absence of instability at the first metatarsocuneiform joint.
-
The relative lengths of the first and second metatarsals.
surgical correction will involve a widened intermetatarsal angle and an
incongruent joint. The magnitude of the intermetatarsal angle is the
primary factor that drives the choice of surgical procedure in these
cases.
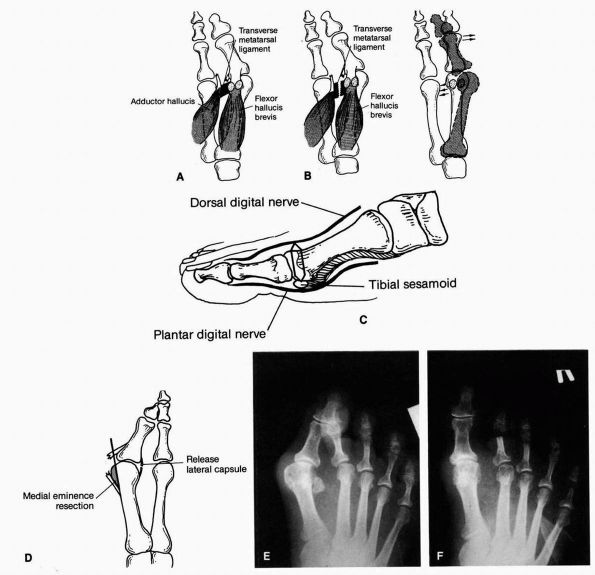
It involves releasing the contracted lateral structures (the lateral
capsule, the adductor tendon, and the intermetatarsal ligament) and
imbricating the attenuated medial capsule. As originally described by
McBride, the procedure also included resection of the lateral sesamoid.
This component of the procedure was abandoned due to a significant rate
of late hallux varus, and the procedure is now known as the “modified”
McBride procedure. Although clinically successful for mild deformities,
the distal soft tissue procedure performed by itself is less commonly
used than the Chevron procedure because of a tendency for some
deformity recurrence. Nevertheless, it is always performed in
conjunction with a proximal osteotomy or fusion for correction of more
severe deformities.
The medial capsule is imbricated. Osteonecrosis of the metatarsal head
has been reported after the Chevron procedure, and opinion varies as to
whether it is safe to perform a concurrent lateral release. In any
case, stripping of the lateral side of the metatarsal head must be
minimized when performing the procedure.
well tolerated by patients. Because the amount of displacement of the
metatarsal head that can be achieved is limited, the procedure is
restricted to correction of less severe deformities with an
intermetatarsal angle of less than 13°.
intermetatarsal angles of over 13° require greater correction of the
angle of the first metatarsal. This correction can only be achieved by
an osteotomy at the proximal end of the bone. Numerous osteotomy
techniques have been described, including the curved (crescentic)
osteotomy (Figure 21-6), a short oblique
(Ludloff) osteotomy, and a V-shaped (proximal Chevron) osteotomy. Long
osteotomies involving the diaphysis of the bone have also been
described that can essentially accomplish the same goals (the Mitchell
osteotomy, the SCARF osteotomy). All have their own technical
advantages and pitfalls, and most surgeons become comfortable with one
technique. In all cases, the toe is also rebalanced with a distal soft
tissue procedure. There is no lower limit to the degree of deformity
that can be corrected with a proximal osteotomy, but the intrinsic
stability of the distal Chevron makes it the procedure of choice for
most deformities of lesser magnitude.
categorized by the intermetatarsal angle alone. A number of unique
exceptions to the usual surgical strategies must also be accounted for.
metatarsocuneiform (MTC) joint that allows the metatarsal to deviate
dorsally and medially. This can be detected both clinically and by the
presence of subluxation and angular deformity at the first
metatarsocuneiform joint on the lateral weight-bearing radiograph (Figure 21-7). The true
incidence of this problem continues to be a subject of controversy, but
it is felt to represent at least 3 to 5% of cases. If instability at
the first MTC exists, the joint must be fused in order to restore the
weight-bearing function of the first metatarsal head. The metatarsal is
positioned during the fusion to correct the intermetatarsal angle and
the toe is rebalanced with a distal soft tissue procedure. This
combination of deformity correction, first MTC fusion, and distal soft
tissue release is called the Lapidus procedure. The Lapidus procedure
can also be used in cases in which the first metatarsocuneiform joint
is arthritic.
 |
|
FIGURE 21-4. The distal soft tissue procedure. (A) The adductor tendon is released from its insertion into the base of the proximal phalanx and fibular sesamoid. (B) The transverse metatarsal ligament is transected and the lateral joint capsule released. (C) Through a longitudinal medial incision, a portion of the medial joint capsule is excised. (D) The medial eminence is excised in line with the medial aspect of the metatarsal shaft. (E) Preoperative radiograph. (F)
Postoperative radiograph with satisfactory realignment of the metatarsophalangeal joint. (Mann RA, Coughlin MJ. The Video Textbook of Foot and Ankle Surgery. St Louis: Medical Video Productions, 1991) |
deformity that has been present since their adolescence. Typically the
first MTP joint is congruent, and the lateral deviation of the hallux
is due to the abnormal development of the joint in a deviated position.
Although it can be difficult to
assess
radiographically, the distal metatarsal articular angle (DMAA) will
typically be above 10°. These bunions are not due to shoe wear but
rather to a congenital deformity.
 |
|
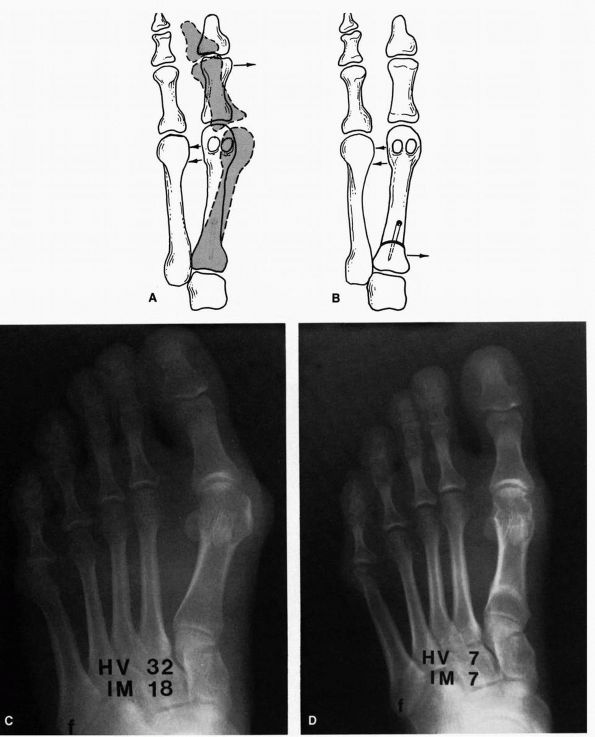
FIGURE 21-5. Chevron procedure. (A) The apex of the chevron osteotomy starts in the center of the metatarsal head and is brought proximally. (B) The osteotomy site is displaced laterally 20 to 30% of the width of the shaft. Preoperative (C) and postoperative (D)
radiographs demonstrating the Chevron osteotomy. (Mann RA, Coughlin MJ. The Video Textbook of Foot and Ankle Surgery. St Louis: Medical Video Productions, 1991) |
deviation of the joint surface may result in creating an incongruent
joint out of a congruent one, resulting in stiffness and arthritis. The
angle between the joint surface and the metatarsal shaft can be
corrected by means of a closing-wedge modification of the Chevron
osteotomy. More severe cases require the addition of a proximal
procedure as well.
lateral side is due to a deformity at the level of the interphalangeal
joint of the hallux itself rather than at the level of the MTP. The MTP
joint is congruent in these situations and the phalanx is not deviated.
This deformity of the toe can be corrected by a closing-wedge osteotomy
of the base of the proximal phalanx, also called the Akin procedure (Figure 21-8).
second metatarsal projects significantly more distally than the first,
there is a great deal of potential for overload pathology of the second
MTP joint. All the osteotomies and fusions involved in hallux valgus
correction involve shortening of the first ray at least by the kerf of
the saw blade. Because of this, patients who have a long second
metatarsal and preoperative transfer pain may also require shortening
of the second metatarsal in addition to hallux valgus correction to
more fully rebalance the forefoot.
 |
|
FIGURE 21-6. Distal soft tissue procedure with proximal crescentic metatarsal osteotomy. (A)
To determine whether an osteotomy is necessary after the soft tissue release has been carried out, the first metatarsal head is pushed laterally. If there is any tendency for the metatarsal head to spring open, an osteotomy should be considered. We add an osteotomy to the distal soft tissue procedure about 85% of the time. (B) The osteotomy site is reduced by freeing the soft tissues about the osteotomy and displacing the proximal fragment medially while pushing the meta-tarsal head laterally. Preoperative (C) and postoperative (D) radiographs demonstrating correction of a moderate hallux valgus deformity with a distal soft tissue procedure and basal metatarsal osteotomy. (Mann RA, Coughlin MJ. The Video Textbook of Foot and Ankle Surgery. St Louis: Medical Video Productions, 1991) |
is a common problem. These patients develop a large dorsal osteophytic
ridge on the metatarsal head, which results in an impingement of the
proximal phalanx to dorsiflexion, limitation of motion, and pain. As
the arthritic process advances, the entire joint becomes involved.
During normal gait, dorsiflexion occurs at the metatarsophalangeal
joint, and if there is an obstruction to the dorsiflexion, then a
significant impairment in gait may occur. This is particularly
bothersome in patients who engage in athletics. The proliferative bone
around the metatarsal head can also result in significant increased
bulk of the joint, which makes wearing shoes difficult.
rigidus is that of pain with dorsiflexion of the metatarsophalangeal
joint. This pain is aggravated by increased activities, particularly
running and other athletic endeavors. The patient may also complain
that, owing to the increased bulk of the joint, wearing shoes is
difficult. With advanced hallux rigidus, an arthritic pain pattern of
the first metatarsophalangeal joint predominates.
abrasion or ulceration over the osteophyte on the dorsal or dorsomedial
aspect of the
metatarsal
head. The joint itself is enlarged, there is synovial thickening, and
there is significant tenderness around the joint, particularly along
the lateral aspect of the metatarsophalangeal joint and over the dorsal
ridge (Figure 21-9).
There is usually significant restriction of dorsiflexion, and
occasionally the proximal phalanx is held in a position of slight
plantar flexion if the deformity is severe. Forced dorsiflexion of the
joint causes pain. In advanced presentation, motion may be severely
limited. Pain and crepitus is elicited throughout the remaining arc of
motion.
 |
|
FIGURE 21-7. Subluxation of the first metatarsocuneiform joint demonstrated by plantar joint widening suggestive of joint instability.
|
 |
|
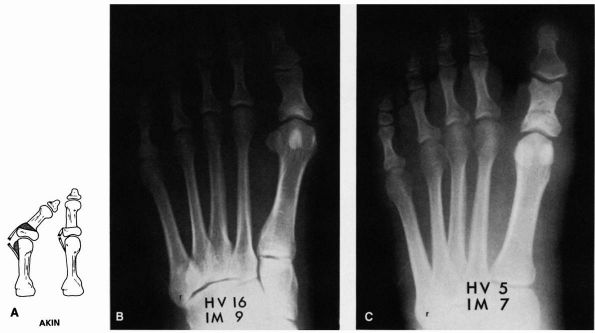
FIGURE 21-8. Akin procedure. (A) The medial eminence is excised, and a medially based wedge of bone is removed from the proximal phalanx. Preoperative (B) and postoperative (C) radiographs demonstrating an Akin procedure.
|
characteristic, demonstrating degenerative arthritis of the
metatarsophalangeal joint on the anteroposterior (AP) view. Besides the
narrowing of the joint, significant osteophyte formation is often
present along the lateral aspect of the joint. Medially, there rarely
is significant osteophyte formation. On the lateral view, there is a
dorsal osteophyte of varying degrees. Occasionally, there is an
osteophyte on the dorsal aspect of the proximal phalanx as well. In
advanced stages, the entire joint space may be compromised. This
continuum of disease has been staged as follows:
 |
|
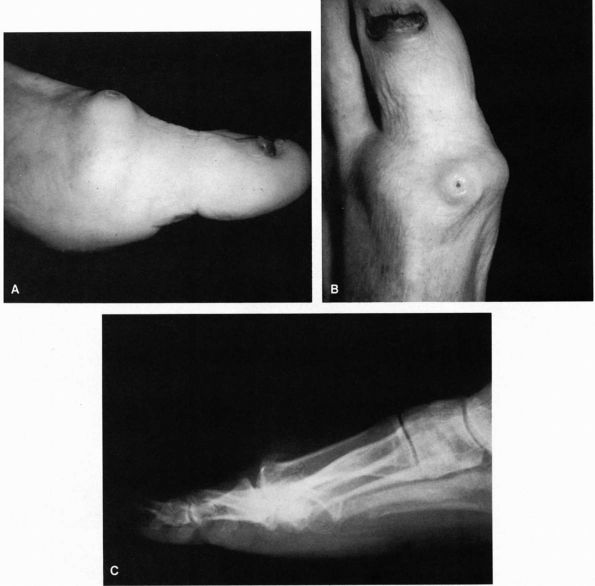
FIGURE 21-9. (A and B)
First metatarsophalangeal joint in a patient with hallux rigidus. Note the increased bulk of the joint and marked osteophyte formation. (C) Lateral radiograph of a patient with hallux rigidus, with a large dorsal osteophyte that mechanically blocks dorsiflexion of the proximal phalanx. |
spurring and more significant joint space narrowing; proximal phalanx
may show dorsal spurring; reactive changes about the joint; plantar
joint space is preserved
significant joint space narrowing and extensive proliferative bone
formation; loss of plantar joint space
activity modification, shoe adjustments ensuring adequate room for the
metatarsophalangeal joint, and stiffening the shoe by inserting either
an orthotic device or a piece of spring steel in the sole to decrease
dorsiflexion at the metatarsophalangeal
joint. Occasionally, nonsteroidal anti-inflammatory medications can be beneficial.
intervention may be indicated if the neurovascular status of the foot
is satisfactory. The appropriate operative procedure depends on the
amount of arthrosis the patient demonstrates. For early stages of
hallux rigidus (grades 1 and 2), a cheilectomy procedure can be
effective. Cheilectomy involves resection of the dorsal 20 to 30% of
the metatarsal head along with the osteophytes along the lateral side
of the metatarsal head. The principle is to relieve the dorsal
impingement of the proximal phalanx as dorsiflexion occurs, which
usually relieves most of the pain. The procedure only reestablishes
about half of normal dorsiflexion but this is usually sufficient to
permit the patient to ambulate comfortably and resume most activities.
excellent procedure for patients who have severe deformity or
significant arthroses (grade 3 hallux rigidus). Arthrodesis is also
useful for patients who have failed a previous cheilectomy and as a
salvage procedure for a failed bunion operation. The optimal
positioning of the arthrodesis is 15° of valgus and 10 to 15° of
dorsiflexion in relation to the plantar aspect of the foot (or 25 to
30° of dorsiflexion in relation to the first metatarsal shaft, which is
inclined in a plantar direction about 20°) (Figure 21-10).
After arthrodesis, the patient can be ambulated in a postoperative
wooden shoe until the arthrodesis site is solid, which is usually about
10 to 12 weeks after surgery. The main complications of arthrodesis are
malalignment of the arthrodesis site and nonunion, although uncommon.
If sufficient valgus and dorsiflexion is not placed into the
arthrodesis at the time of surgery, excessive wear on the
interphalangeal joint occurs—a potential problem.
capacity is limited, a Keller procedure can be used for advanced hallux
rigidus. In this procedure, the proximal one-third of the proximal
phalanx is excised along with the dorsal osteophyte. The problem with
this procedure is that it detaches the intrinsic muscles from the base
of the phalanx, and as a result, the toe may drift into dorsiflexion or
possibly varus or valgus. It is, however, useful in the older patient
with marginal circulation.
metatarsophalangeal joint is rarely indicated because stability of the
joint is compromised, which may result in a transfer lesion to the
adjacent metatarsal head. The active movement of the
metatarsophalangeal joint is usually significantly impaired because of
the inability to reinsert the intrinsic muscles once the prosthesis has
been placed. At times, there is a reaction to the prosthetic materials
and a silicon synovitis results. The life expectancy of a prosthesis is
rarely more than 5 years. Therefore, it should not be used in any
patient who is young and expects to place a great deal of stress on the
metatarsophalangeal joint.
than the great toe. They include mallet toe, hammertoe, and claw toe
deformities. Hard and soft corns also occur on the lesser toes. The
underlying cause is generally idiopathic or a combination of improper
shoe wear. Subtle or overt neuropathy may be contributory. The general
patterns of lesser toe deformities are described below:
of the distal interphalangeal joint, usually involving the second toe
but possibly involving the third or fourth toes.
proximal interphalangeal joint, which may be either fixed or flexible.
The fixed deformity is one in which the proximal interphalangeal joint
cannot be straightened, and a flexible deformity is one in which the
proximal interphalangeal joint can be brought back into anatomic
alignment.
aforementioned mallet toe or hammertoe deformities along with
dorsiflexion at the metatarsophalangeal joint. This deformity may
involve a single metatarsophalangeal joint or multiple
metatarsophalangeal joints. The deformities can be either fixed or
flexible.
abnormal positioning. Mallet toes usually result in pain on the tip of
the toe secondary to pressure from the ground or pain over the distal
interphalangeal joint region secondary to pressure against the shoe.
With hammertoes, pain occurs over the tip of the toe and over the
proximal interphalangeal joint. The patient may develop callus
formation beneath the tip of the toe or over the proximal
interphalangeal joint region. Claw toes cause pain over the proximal
interphalangeal joint
region
where the toes strike the top of the shoe. If the hyperextension
deformity is severe at the metatarsophalangeal joint, progressive
dorsiflexion of the proximal phalanx with depression of the metatarsal
heads occurs causing plantar metatarsal head prominence. Increased load
over the prominence leads to callus formation and pain.
 |
|
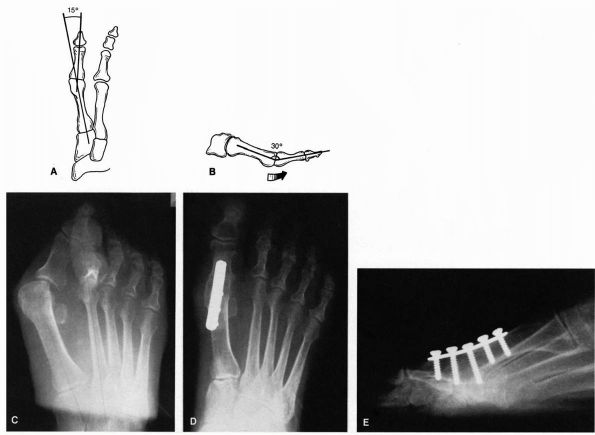
FIGURE 21-10. Arthrodesis of the metatarsophalangeal joint. Proper alignment of the arthrodesed joint is 15° of valgus (A) and 30° of dorsiflexion (B)
in relation to the first metatarsal shaft, which translates to about 10 to 15° of dorsiflexion in relation to the ground. Preoperative (C) and postoperative (D and E) radiographs of an arthrodesis of the first metatarsophalangeal joint using plate fixation. (Mann RA, Coughlin MJ. The Video Textbook of Foot and Ankle Surgery. St Louis: Medical Video Productions, 1991) |
consists of adequate padding, offloading with orthotic management, and
shoe wear modifications with an adequate shoe box to provide sufficient
space for the toes. Orthotic management may be accomplished by simple
(i.e., metatarsal pads) or complex (i.e., custom orthotics with
offloading bars) means with good results.
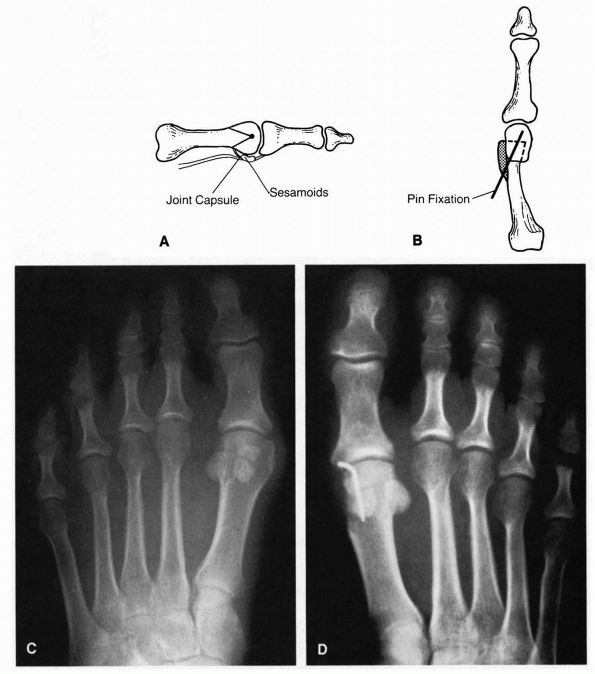
undertaken when conservative measures fail to provide relief. The goal
is to realign the toes at all involved levels to a more anatomic
alignment, eliminating prominent sources of irritation. The operative
treatment of a mallet toe consists of removing the distal portion of
the middle phalanx, which decompresses the distal interphalangeal joint
(Figure 21-11). If the deformity is extremely
fixed, then a release of the flexor digitorum longus tendon may also be
carried out. The operative treatment of a hammertoe consists of
excising the distal portion of the proximal phalanx and then holding
the toe in correct alignment for about 6 weeks, until a satisfactory
fibrous union has occurred (Figure 21-12).
Arthrodesis of the proximal interphalangeal joint can be attempted,
although the fusion rate is low (about 50%). For this reason, usually a
fibrous union is the procedure of choice. Claw toes require correction
of the hammer toe or mallet toe deformity as described above as well as
addressing the metatarsophalangeal joint
deformity (Figure 21-13).
If the patient has a fixed deformity, then release of the contracted
structures on the dorsal aspect of the metatarsophalangeal joint, which
consists of both extensor tendons, the joint capsule, and the
collateral ligaments, is undertaken to straighten the contracture at
the metatarsophalangeal joint. A Girdlestone flexor tendon transfer, in
which the flexor digitorum longus tendon is transposed to the dorsal
aspect of the proximal phalanx, is carried out to provide increased
plantar flexion pull at the metatarsophalangeal joint region. In these
cases, pin fixation is often used to maintain satisfactory alignment of
the corrected hammertoe and metatarsophalangeal joint until the soft
tissues have had a chance to heal. If the deformity is a dynamic one
and does not involve any fixed deformity, then a Girdlestone flexor
tendon transfer alone may produce a satisfactory clinical result.
 |
|
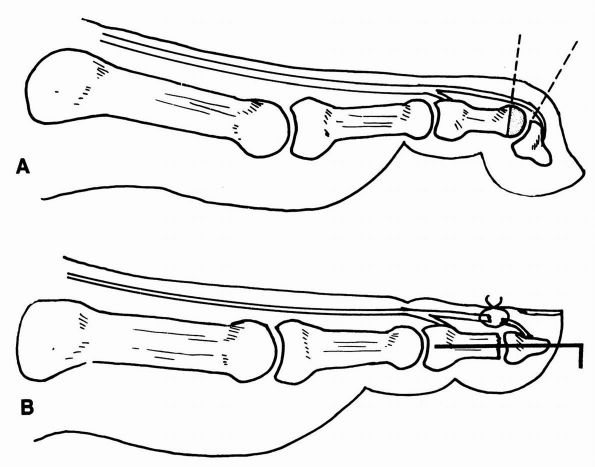
FIGURE 21-11. Mallet toe repair. (A) Resection of the condyles of the middle phalanx. (B)
Intramedullary Kirschner wire fixation. (Mann RA, Coughlin MJ. The Video Textbook of Foot and Ankle Surgery. St Louis Medical Video Productions, 1991) |
 |
|
FIGURE 21-12. Fixed hammertoe repair. (A) Resection of the condyles of the proximal phalanx. (B)
Intramedullary Kirschner wire fixation. (Mann RA, Coughlin MJ. The Video Textbook of Foot and Ankle Surgery. St Louis: Medical Video Productions, 1991) |
 |
|
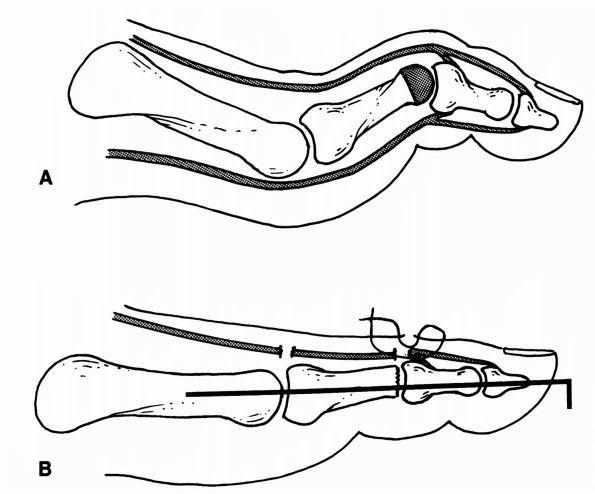
FIGURE 21-13. Fixed claw toe repair. (A) Excision of the condyles of the proximal phalanx, metatarsophalangeal joint capsular release, and extensor tenotomy. (B)
Intramedullary Kirschner wire fixation stabilizes the toe. (Mann RA, Coughlin MJ. The Video Textbook of Foot and Ankle Surgery. St Louis: Medical Video Productions, 1991) |
generalized term for pain beneath the metatarsal head region. During
normal walking, maximal pressure is applied to the metatarsal region
for 50 to 60% of the stance time. As a result, any type of abnormality
in this area may cause the patient significant disability. Most
commonly, metatarsalgia is secondary to a problem at the
metatarsophalangeal joint level. This may be a primary bony problem,
joint problem, or less commonly other causative dysfunction may exist.
Dysfunction of the metatarsophalangeal joint may be secondary to
synovitis associated with inflammatory arthropathy, nonspecific
synovitis, plantar plate degeneration, Freiberg infarction, or
dysfunction secondary to subluxation or dislocation of the
metatarsophalangeal joint. In
many
patients, metatarsalgia can be treated conservatively by obtaining a
shoe of adequate size and then adequately padding the metatarsal area
to relieve the areas of maximal pain. At times, however, this
conservative management fails, and operative intervention is indicated.
patient develops synovial proliferation around the second
metatarsophalangeal joint. This usually starts spontaneously, and
patients often feel as if they are walking on a painful lump on the
bottom of the foot. The physical examination demonstrates generalized
synovial thickening around the metatarsophalangeal joint. This is
sometimes associated with a hammertoe. This condition often responds to
conservative management consisting of adequate shoes and padding and
nonsteroidal anti-inflammatory medications. Occasionally, injection of
corticosteroid into the joint relieves the condition. If the condition
persists, synovectomy of the metatarsophalangeal joint should be
considered. At times, this condition results in a patient developing a
subluxation of the metatarsophalangeal joint frequently associated with
a fixed hammertoe deformity. If symptomatic, this deformity
additionally requires correction as discussed previously.
and is due to cystic changes in the dense plantar plate, which helps to
stabilize the metatarsophalangeal joint. It is associated with pain
beneath the metatarsal head and often a progressive cockingup of the
metatarsophalangeal joint may develop. Usually, patients do not develop
the generalized synovial reaction noted in patients with nonspecific
synovitis. The problem can usually be handled conservatively, although
occasionally arthroplasty of the metatarsophalangeal joint is indicated.
joint are due to multiple causes, including degeneration of the plantar
plate, which permits the extensor tendons to pull the proximal phalanx
up into dorsiflexion; chronic pressure of the great toe against the
second toe, which may result in a dislocated second metatarsophalangeal
joint; nonspecific synovitis; or an undetermined cause. When a severe
subluxation or dislocation occurs, the proximal phalanx pushes the
metatarsal head into a plantar position (Figure 21-14).
As a result, pain and often a large callus develop beneath the
metatarsal head. The patient often complains of pain over the dorsal
aspect of the toe as well because this strikes the top of the shoe.
Under these circumstances, conservative management consists of a shoe
with an adequate toe box to alleviate the pressure on the toe and
metatarsal head along with adequate padding to relieve the pressure
beneath the metatarsal head. If conservative measures fail, then an
operative procedure to reduce the metatarsophalangeal joint may be
indicated. These procedures are often successful in alleviating this
condition.
origin that occurs in the metatarsal head. This infarction results in
collapse of the metatarsophalangeal joint (Figure 21-15).
This process is often associated with generalized discomfort around the
joint, and the joint may develop a significant synovial reaction or
enlargement due to collapse of the bony structures. This condition can
often be managed conservatively with adequate shoes and padding,
although nonsteroidal anti-inflammatory medications are useful during
the acute phases. If the problem significantly limits the patient,
arthroplasty may be indicated to remove some of the proliferative bone
about the joint.
arthritis, psoriatic arthritis, or gout, proliferative synovial tissue
develops around the metatarsophalangeal
joint,
which results in an enlargement of the joint as well as a significant
inflammatory response by the body. Under these circumstances, placing
pressure on the metatarsal head region causes the patient significant
discomfort and may make walking extremely difficult. Gout is usually
localized to the first metatarsophalangeal joint, whereas rheumatoid
and psoriatic arthritis involve multiple metatarsophalangeal joints.
 |
|
FIGURE 21-14. Subluxation of the second metatarsophalangeal joint in a dorsomedial direction.
|
 |
|
FIGURE 21-15.
Radiograph of Freiberg infraction involving the second metatarsal head. This is an avascular necrosis of undetermined cause producing collapse of the metatarsal head. |
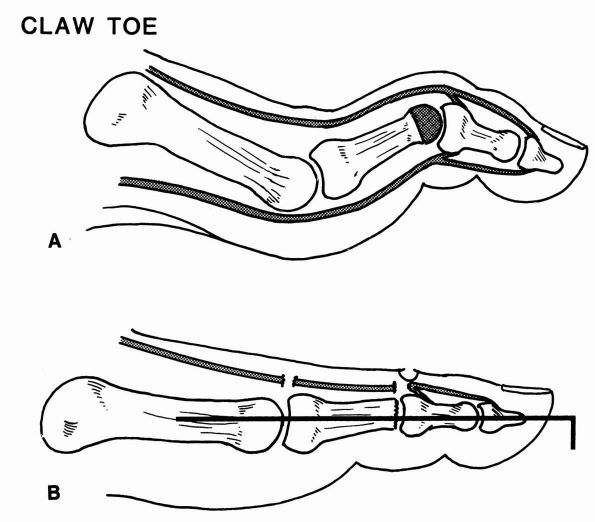
the patient into an adequate shoe, often extra-depth shoe that has a
large toe box with enough room for the patient’s forefoot deformities
and for an orthotic device to help relieve the stress on the metatarsal
heads (Figure 21-16). Gout can often be handled
therapeutically, although in some cases with large tophaceous deposits,
alteration in shoe wear is necessary.
reconstructive procedure should be considered. The early joint changes
begin with a synovitis-type picture, and over time, the deformities may
progress to subluxations and dislocations. This process, particularly
in the rheumatoid forefoot, can be helped if synovectomies of the
metatarsophalangeal joints are performed before significant capsular
destruction has occurred. For advanced rheumatoid forefoot deformity,
arthrodesis of the first metatarsophalangeal joint to deformity and
lesser metatarsophalangeal joints’ decompression by surgical resection
of the metatarsal heads is the procedure of choice (Figure 21-17).
This procedure allows the fat pad to be drawn back down onto the
plantar aspect of the foot and creates a soft cushion for the foot that
relieves the metatarsalgia. The lesser toe deformities are corrected by
manual osteoclasis and pinning, which corrects the fixed deformities.
After this procedure, patients often have increased ambulatory capacity
and can wear store-bought shoes.
a so-called Morton foot in which the first metatarsal is short, a
hypermobile first ray in which the first metatarsocuneiform joint is of
insufficient stability to provide adequate weight bearing, or after
trauma in which a metatarsal may be pushed into a plantar or dorsal
angulation. Occasionally, after metatarsal surgery to alleviate
pressure on one metatarsal, a condition known as a transfer lesion
may occur. This results in pressure beneath the adjacent metatarsal
head due to lack of weight bearing on the previously operated
metatarsal. In most of these
cases,
a callus develops beneath the prominent metatarsal head, which is
usually the source of the patient’s pain. Conservative treatment
involves modifications to provide adequate padding around the area to
alleviate the pressure on the involved metatarsal head. If this fails,
then a surgical procedure may be indicated either to relieve the
prominence or to elevate or shorten the metatarsal and correct any
associated joint deformity. One such procedure is the Weil osteotomy,
which involves an extra-articular osteotomy of the distal metatarsal
allowing decompression and shortening, relieving plantar prominence and
joint subluxation.
 |
|
FIGURE 21-16. An extra-depth shoe provides extra room in the toe box as well as extra width to accommodate a deformed foot.
|
 |
|
FIGURE 21-17. A rheumatoid foot. (A)
Preoperative radiograph of typical rheumatoid changes with a severe hallux valgus deformity and subluxation and dislocation of the lesser metatarsophalangeal joints. (B) Reconstruction using an arthrodesis of the first metatarsophalangeal joint and arthroplasties of the lesser metatarsophalangeal joints. |
a significant cause of discomfort for the patient. The most frequently
encountered problems include hard or soft corns, plantar warts, seed
corns, or hyperkeratotic skin. A wart is a vascular lesion secondary to
a virus and can be differentiated from keratotic skin by carefully
trimming the area and observing small punctate bleeders secondary to
the fine end arteries, which are present in a wart and not in a
keratotic lesion. Treatment includes
dermal
burning with liquid nitrogen; by using Cantharone, which after multiple
applications usually relieves the wart; or occasionally by curettage.
Burning the bottom of the foot with electrocautery or surgically
excising the wart are not recommended unless other options fail,
because they result in a scar on the plantar aspect of the foot, which
may become symptomatic.
 |
|
FIGURE 21-18.
The presence of a long second metatarsal in the forefoot metatarsal cascade results in excessive pressure beneath metatarsal head, which may predispose to “metatarsalgia” pain. |
in a small keratotic lesion, which at times can be painful. These
usually can be managed by trimming the lesion; or if this fails,
curettage may alleviate it. Hyperkeratotic skin is observed in some
patients and is probably due to a biochemical abnormality that is
poorly understood. In these patients, surgical intervention is not
indicated; rather, frequent trimming of the hyperkeratotic skin usually
is adequate treatment and often can be taught to the patient.
in response to pressure against the skin by an external force (a shoe).
As a general rule, a small bony prominence, termed an exostosis,
lies beneath the skin, and the shoe covering the foot chafes against
this area. Corns are divided into hard and soft corns, depending on
their location. A hard corn occurs between the skin and the shoe,
whereas a soft corn occurs between one toe and an adjacent toe. In both
cases, however, the cause is due to an underlying exostosis. The
patient’s main complaint is that of buildup of hypertrophic skin over
the exostosis. In time, this may become rather large and painful. The
conservative management is to trim the lesion and place a soft support
around it to alleviate the pressure on the involved area. Usually, a
broader, softer shoe helps to accommodate this problem. If conservative
management fails, then a surgical procedure may be undertaken that
removes the offending prominence.
include atrophy of the plantar fat pad, synovial cyst arising from the
metatarsophalangeal joint, soft tissue tumors such as a lipoma,
permanent changes secondary to a crush injury, or a plantar scar
secondary to trauma. Atrophy of the plantar fat pad occurs most
frequently in older people and can present a significant problem for
the patient. Because of loss of adequate padding beneath the metatarsal
heads, some callus formation often results, and the metatarsal heads
are sensitive to weight bearing. Unfortunately, there is no way to
remedy this situation other than to place the patient in a soft-soled
shoe with adequate support in the metatarsal area to alleviate the
discomfort.
metatarsalgia due to its physical prominence. If this fails to respond
to conservative management, such as adequate padding and shoe wear,
surgical excision may be carried out.
origins. The presence of pes planus itself is not necessarily
pathologic. Rather, it is a sign that the underlying cause of the foot
deformity should be explored in order to guide treatment. An attempt
should be made to differentiate between a congenital versus acquired
condition, after which specific diagnoses within each category may be
considered. Asymptomatic flexible flatfoot is extremely prevalent,
generally requires no treatment, and can be considered a normal variant
of foot architecture.
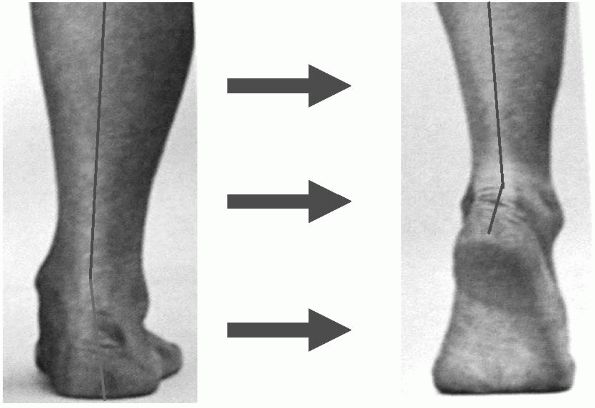
longitudinal arch and assessment of alignment reveals excessive
hindfoot valgus and forefoot abduction. From behind, the excessive
forefoot abduction is demonstrated as the “too many toes” sign, in
which an excess of the toes are visualized because of the marked
abduction of the forefoot (Figure 21-19).
Patients should be thoroughly accessed for motion limitations,
particularly of the subtalar joint, which may suggest an underlying
coalition. Posterior tibial tendon strength and function should be
accessed. When testing the posterior tibial tendon, the foot should
begin in a plantarflexed and everted position. The patient should then
be asked to invert the foot against the examiner’s resistance from this
position, eliminating the inversion power of the anterior tibial
tendon, which may mask posterior tibial tendon weakness. The ability to
perform multiple single heel-rises with initiation of heel inversion
confirms intact posterior tibial tendon function (Figure 21-20).
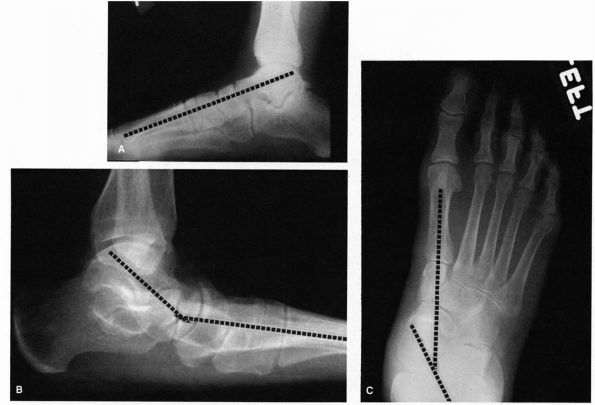
evaluation of a patient with pes planus are present irrespective of the
underlying cause. On the lateral radiograph, a line drawn through the
long axis of the talus should nearly bisect the navicular and first
metatarsal shaft (Figure 21-21). Mild flatfoot is indicated by a sag in this line of up to 15°; a sag from 15 to 40° indicates moderate flatfoot; and a sag greater than 40° indicates severe flatfoot.
In the AP radiograph, a line drawn through the long axis of the talus
and calcaneus should measure about 15°. An increase in this angle
indicates varying degrees of
flatfoot. Observation of the talonavicular joint demonstrates lateral subluxation of the navicular off the head of the talus (Figure 21-21).
Associated radiographic findings may suggest the specific underlying
cause of the deformity (i.e., midfoot arthrosis, tarsal coalition).
 |
|
FIGURE 21-19.
Clinical examination finding of “too many toes” sign consistent with excessive hindfoot valgus and forefoot abduction resultant from posterior tibial tendon dysfunction. |
 |
|
FIGURE 21-20.
Clinical examination demonstrating heel inversion with a single heel-rise consistent with intact posterior tibial tendon function. |
asymptomatic flexible pes planus, tarsal coalition (peroneal spastic
flatfoot), and residual congenital deformity (i.e., residual clubfoot).
Asymptomatic flexible pes planus is a variation of normal foot
architecture. This diagnosis generally requires no treatment beyond
simple reassurance. Conservative treatment for symptomatic patients
involves fitting the foot with a firm shoe that has an extended medial
counter to help support the talonavicular joint, a medial heel wedge to
help tilt the heel into a neutral position, or a well-molded,
semiflexible arch support to further support the longitudinal arch.
These treatment modalities suffice in most patients with symptomatic
hypermobile flatfoot of congenital origin. If surgery becomes
necessary, it is usually in the form of extra-articular osteotomies
meant to improve hindfoot alignment (i.e., lateral column lengthening
procedures). Rarely, stabilization of the foot with arthrodesis of the
joints of the hindfoot may be necessary. The surgeon must always be
cautious, however, when carrying out a stabilization procedure of the
hindfoot because an excessively flexible foot is being replaced with a
rigid foot, and this does not always ensure that the patient will
become asymptomatic. In contrast to hypermobile congenital flatfoot,
patients with tarsal coalition as a cause of congenital pes planus
demonstrate a limitation of tibiotalar, subtalar, or transverse tarsal
joint range of motion. This is a condition created by a failure of
segmentation of
the tarsal bones in early development (Figure 21-22).
Most often, the talocalcaneal and calcaneonavicular joints are
affected. Incidence is reported to be less then 1%, and bilateral
coalitions may be present in approximately 50% of those affected.
Afflicted individuals notice the condition in adolescence, as the
coalition may mature from a cartilaginous to a bony interface and cause
symptomatic mechanical irritation. Pain along the peroneal muscles may
be present and this is thought to be due to the patient’s attempt to
compensate and correct the overall hindfoot alignment. It is this
latter symptom that lends an alternative name to tarsal coalition:
peroneal spastic flatfoot. The acute treatment of a symptomatic
coalition is based on relieving the stress at the site of the
coalition, generally best performed with immobilization. Patients who
have recurrent symptoms despite conservative care may require surgical
resection or fusion of the involved areas of the coalition.
 |
|
FIGURE 21-21. Radiographs of the flatfoot deformity. (A) Normal lateral radiograph demonstrating the relation between the long axis of the talus and first metatarsal. (B) In the flatfoot deformity, there is a sagging of the talonavicular joint. (C)
In the AP view, there should be a straight line relation between the long axis of the talus and first metatarsal. In flatfoot, this line is disrupted, and there is medial deviation of the head of the talus. |
posterior tibial tendon dysfunction (PTTD) and midfoot arthrosis. These
patients can be differentiated from those with congenital flatfoot by
history. Patients with acquired flatfoot had at one time a normal
architecture of the foot and have since suffered progressive collapse
to flatfoot deformity. PTTD is the most common cause of adult acquired
flatfoot deformity. The process is initiated by tenosynovitis with
progressive inflammation that subsequently causes enlargement and
fraying of the tendon, which may progress to frank rupture. As the
tendon weakens, the hindfoot demonstrates valgus malalignment secondary
to medial column structural laxity. In addition, forefoot abduction
occurs.
mild pain along the tendon. The patient retains strength as
demonstrated by a preserved ability to perform a single heel-rise. This
is the tenosynovitis or tendonitis stage and the patient
can
generally be managed nonoperatively with a period of immobilization. In
no instance should the tendon be injected with corticosteroid, for a
number of studies suggest an increased risk of tendon rupture (as high
as 25%) with steroid administration. If symptoms persist, a
tenosynovectomy of the posterior tibial tendon sheath should be
performed to prevent progression of disease. Stage 2 PTTD is
characterized by pain along the tendon, inability to perform a single
heel-rise or initiate inversion of the heel on heel rise, and postural
foot changes (excessive hindfoot valgus or forefoot abduction). The
foot does, however, remain supple and motion is retained. This is the
“flexible” stage, and the tendon is generally no longer functional.
Nonoperative treatment can produce acceptable results with aggressive
orthotic management and potentially the long-term use of a solid
plastic ankle-foot orthosis, particularly in elderly patients. Many
patients, however, improve only with surgical intervention. The most
common surgical procedures include posterior tibial tendon debridement,
tendon transfer (i.e., flexor digitorum longus [FDL] transfer), and
extra-articular osteotomy procedures to correct bony malalignment
(i.e., medial calcaneal slide, lateral column lengthening procedures).
Stage 3 PTTD is defined by fixed postural abnormalities secondary to
severe chronic malalignment and joint involvement. This is the “rigid”
stage and cannot be managed effectively surgically with extra-articular
alignment correction or soft tissue procedures alone. If the patient
fails nonoperative management, hindfoot arthrodesis is required
(selective or triple arthrodesis procedures) to correct the foot to a
plantigrade position. Stage 4 PTTD includes the rigid hindfoot changes
and additionally involves the tibiotalar joint. If orthotic treatment
is ineffective, pantalar fusion (ankle arthrodesis and triple
arthrodesis) is required.
 |
|
FIGURE 21-22. Tarsal coalitions. (A) Talocalcaneal middle facet coalition (arrow). (B) Calcaneonavicular coalition. (C)
Changes secondary to a tarsal coalition consist of beaking and irregularity of the talonavicular joint, abnormal appearance of the subtalar joint, and lack of dorsiflexion pitch to the calcaneus. |
cause a symptomatic acquired flatfoot deformity. Individuals sustaining
a calcaneus or talus fracture may develop hindfoot valgus and collapse
of the transverse tarsal joints leading to a flatfoot posture. Primary
or posttraumatic midfoot arthrosis may lead to a collapse of the arch
and pain (Figure 21-23). These deformities may
be the direct result of the fracture and residual deformity, or it may
be secondary to collapse following the development of arthrosis. The
treatment for this complication must be individualized given the
flexibility and severity of the deformity. Simple arch supports,
University of California Berkeley Laboratories (UCBL) inserts, or an
ankle-foot orthosis may be sufficient. Surgical stabilization generally
involves arthrodesis with interposition of bone graft to lengthen
collapsed joints and restore overall foot alignment.
 |
|
FIGURE 21-23. Radiographs of midfoot arthrosis. (A)
Lateral views demonstrating midfoot arthritic change and collapse. The normal talus to first metatarsal relationship is altered, consistent with flatfoot deformity. (B) In the AP view, the midfoot arthrosis at the second and third tarsometatarsal joints is noted. (C and D) Postoperative radiographs demonstrating a satisfactory selective midfoot fusion using screw fixation. |
flatfoot deformity. The foot is often stiff, and the elevated arch does
not normalize with weight bearing. The deformity itself may have
primarily a hindfoot basis, a forefoot basis, or a combination of both.
There should be high index of suspicion for an underlying neuromuscular
disorder, although the most common cause is idiopathic. Any new onset
presentation should be considered evidence of a possible spinal cord
lesion until proven otherwise. The neuromuscular origins associated
with a cavus foot include Charcot-Marie-Tooth and polio. Congenital
causes (i.e., clubfoot residual) and posttraumatic causes (i.e.,
compartment syndrome sequelae) may also cause the deformity.
distribution of weight and decreased surface area present for weight
bearing. The rigid deformity compounds the problem as the foot is
unable to absorb the weight-bearing impact. As progressive deformity
develops, patients may experience pain on the lateral aspect of the
foot, over the fifth metatarsal head, and with severe hindfoot varus
secondary ankle instability complaints.
deformity demonstrates a high arch while standing, which is associated
with a varus deformity of the heel, adduction of the forefoot, and
often clawing of the toes. The foot frequently is rigid with restricted
motion in all the joints, fixed dorsiflexion contracture of the
metatarsophalangeal joints, and fixed hammering of the proximal
interphalangeal joints. Muscle testing is essential to determine the
cause of the deformity, as most cases are due to hindfoot or forefoot
muscle imbalances. This testing allows for localization of deformity
and for accurate surgical planning if tendon transfer procedures are
being considered. The degree of rigidity of the hindfoot varus can be
assessed with the Coleman block test. The heel is placed on a block of
wood and the forefoot is allowed to contact the ground, leaving the
hindfoot unrestricted. If the hindfoot varus corrects to neutral, the
deformity is considered flexible. In a rigid deformity, the hindfoot
varus will not correct.
obtained to determine the source of the deformity. Primary hindfoot
cavus will demonstrate an elevated calcaneal pitch angle with an
increased pitch of the calcaneus in relation to the floor of greater
than 30°, a normal talometatarsal angle, an elevated longitudinal arch,
and forefoot supination (Figure 21-24).
Forefoot cavus will demonstrate a normal calcaneal pitch angle, an
elevated arch, loss of alignment of the talometatarsal angle, and
increased forefoot plantar flexion.
to provide an accommodative shoe with adequate support and cushioning
to help absorb some of the impact of ground contact. If a neurologic
disorder
exists,
a polypropylene ankle-foot orthosis (AFO) may be necessary to provide
stability. Surgical treatment of the cavus foot depends on the precise
cause of the problem. The main goals of surgery are to produce a
plantigrade foot and, if possible, to lower the longitudinal arch. The
type of surgical procedure indicated depends on the specific bony
abnormality present and the location of the maximal deformity.
Correction should be performed with extra-articular osteotomies with or
without tendon transfers at the sites of involvement (i.e., Dwyer
calcaneal osteotomy, first metatarsal osteotomy, and plantar fascia
release) (Figure 21-25).
For patients with severe deformity or with progressive neurologic
disease, arthrodesis procedures may be optimal. The goal of all of the
surgical procedures is a plantigrade foot, which is stable for
weight-bearing.
 |
|
FIGURE 21-24. Radiographs of the cavus foot. (A) Marked dorsiflexion pitch of the calcaneus. Normal calcaneal pitch is 20 to 40°. (B)
Forefoot equinus resulting in a cavus foot. Note the almost normal-appearing pitch to the calcaneus. (Mann RA, Coughlin MJ. The Video Textbook of Foot and Ankle Surgery. St Louis: Medical Video Productions, 1991) |
 |
|
FIGURE 21-25. Operative correction of a cavus foot. (A) Preoperative deformity demonstrating the increased dorsiflexion pitch of the calcaneus and mild equinus of the forefoot. (B)
Postoperative radiograph after a calcaneal osteotomy permitting dorsiflexion of the proximal fragment, dorsiflexion osteotomy of the first metatarsal, release of the plantar fascia, and fusion of the interphalangeal joint of the great toe. The longitudinal arch has been lengthened as a result of this procedure. (Mann RA, Coughlin MJ. The Video Textbook of Foot and Ankle Surgery. St Louis: Medical Video Productions, 1991) |
secondary. Although primary arthrosis of the ankle and subtalar joint
is uncommon, it does occur in the talonavicular, tarsometatarsal, and
first metatarsophalangeal joints. Why some joints are affected by
primary arthroses and others are usually affected after trauma remains
an enigma. Because the foot and ankle are weight-bearing structures,
joint afflictions may severely limit a person’s ability to remain
functional. As a general rule, the diagnosis of arthrosis is not
difficult to make, and in most cases conservative management can
benefit the patient. If conservative management fails, then
stabilization of the involved joint may be considered.
arthrosis, but after an ankle fracture or other various traumas to the
ankle joint, degenerative arthritis can occur. The patient complains of
pain that is well localized to the ankle joint, and this pain can often
lead to a significant degree of disability. After a fracture of the
ankle joint, a varus or valgus deformity may result in improper
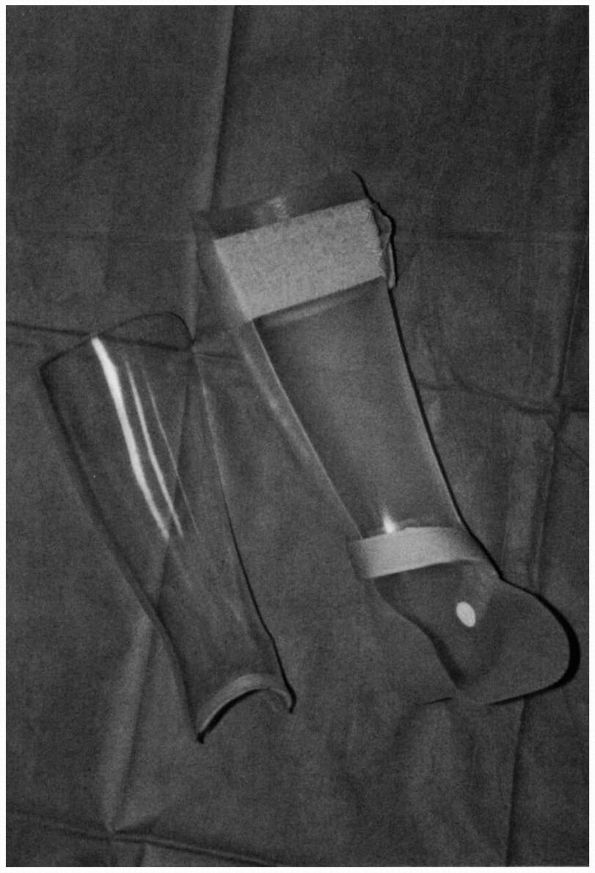
placement of the foot on the ground. The management of the patient with
osteoarthritis of the ankle joint is often helped by use of a
polypropylene AFO that maintains the ankle joint in a fixed position,
relieving the stress across the joint (see Figure 21-26).
A rocker-bottom shoe sole permits the patient to roll over the foot,
thereby relieving the stress on the ankle joint. If the pain and
disability persist, surgical intervention should be considered.
for the treatment of end-stage ankle arthritis. The ankle should be put
into neutral position in terms of extension and flexion and into about
5° of valgus (Figure 21-27). The rotation of
the foot in relation to the knee joint should be the same as on the
uninvolved side. After a successful ankle arthrodesis, patients still
maintain some dorsiflexion and plantar flexion motion of the foot,
which is mediated through the talonavicular and subtalar joints.
Arthrodesis usually results in restoration of function, although most
patients cannot participate in running or jumping activities.
improvement in design and technique have combined with the significant
long-term complications with ankle arthrodesis procedures and have
renewed the interest in total ankle arthroplasty. Recent reports of
modern implants have demonstrated improved results. The indications for
ankle arthroplasty are evolving; the ideal candidate may be an elderly,
low demand patient with bilateral disease. Previous infection or
neuropathic joint changes are absolute contraindications to this
procedure. Obesity, significant articular malalignment, muscle
paralysis, instability, severe bone loss, and high demand patients are
relative contraindications. The advantage of ankle joint replacement
includes preservation of ankle motion, diminishing the risk of adjacent
joint arthrosis development as occurs subsequent to ankle arthrodesis
and improving functional outcome. The significant risks of soft tissue
problems and difficulties with subsequent reconstruction after failure
of the implant must be considered before undergoing this procedure.
 |
|
FIGURE 21-26. An ankle-foot orthosis may be used with and without an anterior shell to help contain the foot and ankle.
|
talonavicular, and calcaneocuboid joints) can occur as a result of
primary osteoarthritis, however, more commonly occur secondary to
previous trauma. The subtalar joint, for example, rarely develops
primary osteoarthritis but frequently develops posttraumatic arthrosis
after an intra-articular calcaneal fracture. These changes result in
loss of motion of the subtalar joint and sometimes in a lateral
impingement against the fibula. Likewise, the transverse tarsal joints
(talonavicular and calcaneocuboid joints) may develop primary
arthrosis, or arthrosis may follow trauma to this area. Significant
deformity of the talonavicular joint may occur, and the head of the
talus tends to drop in a plantar and medial direction. This results in
a secondary deformity of the foot in which the calcaneus drifts into
valgus and the forefoot into abduction, causing an acquired flatfoot
deformity.
use of a polypropylene AFO, but in this case, the trim line of the
brace can be made to permit 50% ankle joint motion, which gives the
patient a smoother gait while providing support to the hindfoot
complex. If conservative measures fail, then arthrodesis of the
hindfoot joints may be considered. Selective arthrodesis of the
talonavicular, calcaneocuboid, or subtalar joints may be effective
depending on the clinical circumstances. The hindfoot joints do,
however, function as a unit and thus significant compromise of motion
may occur even with limited arthrodesis. Selective fusion of the
talonavicular joint decreases motion 85%, the subtalar joint 50%, the
calcaneocuboid 35%, and any combination thereof (double or triple
arthrodesis) nearly 100%. Because of the marginal retention of motion
of the hindfoot complex with some selective arthrodesis procedures
(i.e., double arthrodesis or talonavicular arthrodesis), a more
extensive fusion (i.e., triple arthrodesis) may be the procedure of
choice because of the improved union rates with this technique.
joint is placed into about 5° of valgus. If a lateral impingement
exists beneath the fibula, this should be excised at the time of the
fusion.
The transverse tarsal joints (calcaneocuboid and talonavicular joints)
should be fused in a neutral position, avoiding excessive pronation or
supination.
For
the talonavicular joint, an isolated arthrodesis produces a
satisfactory result in patients older than 50 years of age, but this
usually should be combined with a fusion of the calcaneocuboid joint. A
triple arthrodesis involves fusion of the subtalar (talocalcaneal),
talonavicular, and calcaneocuboid joints. When a triple arthrodesis is
carried out, only ankle joint motion is present, and all inversion and
eversion function of the foot is lost. Optimal positioning of the
subtalar and transverse tarsal joints is necessary to create a
plantigrade foot, so that when the foot comes into contact with the
ground, there is no abnormal varus or valgus configuration to either
the heel or forefoot (Figure 21-29).
If the triple arthrodesis is carried out incorrectly, abnormal weight
bearing may result. After a successful triple arthrodesis, patients are
functional, although there is some added stress to the ankle joint,
which can be a problem in some cases. As a general rule, these patients
can carry out most functions of daily living, although sports and
running are difficult.
 |
|
FIGURE 21-27. Ankle fusion. (A and B) Preoperative radiographs. (C and D)
Postoperative radiographs demonstrating a satisfactory ankle fusion using screw fixation. (Mann RA, Coughlin MJ. The Video Textbook of Foot and Ankle Surgery. St Louis: Medical Video Productions, 1991) |
 |
|
FIGURE 21-28. Subtalar joint arthrodesis. (A) Preoperative radiograph of arthrosis of the posterior facet of the subtalar joint. (B) Postoperative radiographs demonstrating satisfactory arthrodesis using screw fixation.
|
primary, or it can be secondary to a Lisfranc fracture dislocation. In
both cases, patients note progressive pain and sometimes a progressive
abduction deformity of the forefoot, which results in flattening of the
longitudinal arch (see Figure 21-23). A
prominence often develops, particularly near the first
metatarsocuneiform articulation on the plantar medial aspect of the
foot. A polypropylene AFO with a trim line cut to permit ankle joint
motion and a full-length foot piece often helps provide support. If a
large plantar medial prominence is present, however, wearing a brace
may be difficult. If conservative management is unsuccessful,
arthrodesis to realign the tarsometatarsal articulations can be
undertaken.
be carried out to realign the foot, addressing all involved areas of
degeneration and deformity. Often, marked forefoot abduction and
dorsiflexion at the tarsometatarsal articulation is present and
requires correction. After a successful arthrodesis, the patient has a
plantigrade foot and stability of the involved joints. Some patients,
however, complain of persistent stiffness in the foot after the fusion,
and although they are highly functional, they are encouraged not to
engage in high-impact sports.
athletic populations. Although the majority of patients who suffer an
ankle sprain go on to heal without instability, a small percentage
develop chronic laxity of the lateral ankle ligaments. The broad and
strong deltoid ligament on the medial side of the ankle is rarely
affected. Essentially all cases of lateral ankle ligament laxity
involve the anterior talofibular ligament, a thickening of the ankle
capsule from the anterior margin of the fibula to the neck of the talus
that prevents anterior translation of the talus in the ankle mortise.
More severe cases also demonstrate involvement of the stronger
calcaneofibular ligament that runs from the tip of the fibula and
courses deep to the peroneal tendons to cross the subtalar joint and
inserts on the calcaneus. It serves to prevent direct inversion
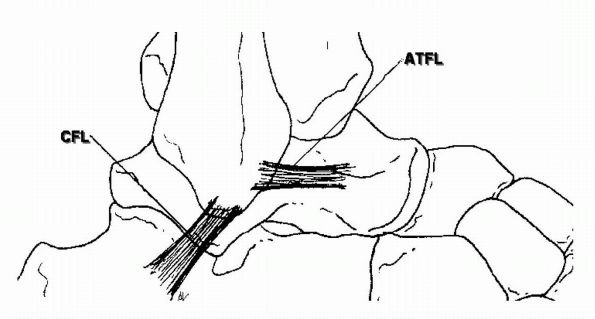
instability both of the ankle and subtalar joint (Figure 21-30).
lateral ankle ligament laxity. When weight bearing, the axis of the
calcaneus ordinarily rests in approximately 5 to 7° of valgus compared
with the axis of the tibia. This places the line of force lateral to
the center of the ankle and does not stress the lateral ankle
ligaments. When a varus alignment to the hindfoot is present, however,
the lateral ankle ligaments are subject to repetitive loading. The
clinical examination of a patient with chronic ankle sprains should
include a standing examination from the rear to check hindfoot
alignment. Hindfoot varus is most often seen in conjunction with a
cavus foot.
dynamic support from the peroneal tendons is also important in
maintaining ankle stability. The peroneal muscles contract reflexively
in response to sudden inversion moments about the subtalar joint and
ankle. Because of the peroneal muscle action, many patients with lax
ankles on clinical examination do not have a clinical problem with
major ankle sprains. In those that do, physical therapy
aimed
at peroneal strengthening and proprioceptive training can be effective
in reducing the risk for further major episodes. The mechanism of
action is unclear. It takes approximately 50 ms for electrical activity
to appear in the peroneal musculature following a sudden unexpected
inversion force. Another 70 ms is required for the muscle to develop
any significant tension. There is little data to suggest that training
can reduce this reaction time. More likely, patients develop more
strength in the peroneal tendons and develop motor patterns in which
the muscles begin to fire before the foot hits the
ground.
While this can be effective, some degree of ligament integrity is
required to prevent ankle sprains when the foot is going to be subject
to sudden unexpected loads as is common in cutting and jumping sports.
 |
|
FIGURE 21-29. The triple arthrodesis consists of fusion of the subtalar, talonavicular, and calcaneocuboid joints. Preoperative (A) and postoperative (B) lateral radiographs demonstrating reestablishment of the longitudinal arch. (C and D)
AP view demonstrating correction of the abduction deformity of the forefoot. (Mann RA, Coughlin MJ. The Video Textbook of Foot and Ankle Surgery. St Louis: Medical Video Productions, 1991) |
 |
|
FIGURE 21-30.
Schematic diagram depicting course of major lateral ankle ligaments: ATFL (anterior talofibular ligament) and CFL (calcaneofibular ligament). Ligament repair or reconstruction techniques should attempt to recreate ligament isometry. |
both a history of major recurrent ankle sprains and evidence of
mechanical laxity on the clinical examination. The ankle should be
tested both in direct anterior subluxation (the anterior drawer test)
and in inversion (Figure 21-31). Stress
radiographs, in which an ankle mortise view is taken while an inversion
force is applied, are unreliable. No standards exist to define a
threshold of ankle laxity and a large number of false-negative results
can be expected because a patient will guard the joint with the
peroneal muscles during this awkward test.
ligament laxity yield a high rate of associated injuries in other
structures about the hindfoot. A high index of suspicion should be
maintained in particular for tears of the peroneal tendons and
osteochondral lesions of the talus.
 |
|
FIGURE 21-31.
Anterior drawer physical examination finding in the evaluation of ankle ligament instability. With one hand cupping the heel, an anterior stress is placed on the ankle to elicit the degree of tibiotalar subluxation. |
imbrication into a small bone trough around the front of the fibula, is
known as the Broström procedure. Because it uses the native ligaments
and restores the normal anatomy, no limitation of ankle or subtalar
motion occurs after the procedure and it is highly effective in
restoring stability to the joint. It is the preferred technique for the
majority of patients.
approximately 15% of cases. One important risk factor for failure is
benign joint hypermobility syndrome, a subtle disorder of collagen
leading to global ligamentous laxity. It is now regarded by most
authorities as synonymous with the mild type III variant of
Ehlers-Danlos syndrome. Patients being considered for ligament repair
should be evaluated clinically for signs of global ligamentous laxity
and for a history of instability problems in other joints.
failed or global ligamentous laxity is present, an augmented
reconstruction of the lateral ankle ligaments is appropriate. Over 30
procedures have been described to accomplish this using a variety of
materials including split or whole peroneus brevis, fascia lata,
hamstring tendon, and tendon allograft. All of these augmentation
procedures have some potential for causing a pathologic limitation of
subtalar motion if the grafts are not placed at the origin and
insertion of the anterior talofibular ligament and the calcaneofibular
ligament. Whatever graft material is used, the repair should attempt to
mimic the normal anatomy as possible.
a significantly disabling problem. Heel pain has multiple origins, and
it is imperative that a careful history and physical examination be
carried out to pinpoint, as precisely as possible, the cause of the
pain. In this way, specific treatment can be formulated to relieve the
condition. Heel pain can result from disorders of the Achilles tendon,
soft tissue disorders near the heel, hindfoot bony injury (i.e. stress
fracture), bony prominence irritation, or neurologic disorders about
the hindfoot.
 |
|
FIGURE 21-32. MRI images of Achilles tendinosis demonstrating intrasubstance tendon degenerative change.
|
common problem, particularly with the athlete. Multiple descriptive
terms (i.e., tendinitis, tendonitis, tendinosis, tendinopathy,
peritendinitis, partial rupture, and so on) have been ascribed to the
specific Achilles tendon disorders based on the location of disease and
affect on the tendon. These terms are often confusing, occasionally
misleading, and many of these disorders often coexist. Perhaps a more
simplistic approach is to consider these disorders as a spectrum of
disease of the Achilles. The origin, pathogenesis, and natural course
of many of these disorders are unknown. Patients generally present with
complaints of pain with activities, particularly those sports related.
In acute conditions, pain may occur with all activities. In chronic
conditions, pain may initially occur only with exertional activities
and over time may progress to constant pain, occurring even at rest.
Clinical examination may reveal a diffuse selling, crepitation, and
tenderness along the tendon in acute disorders. Chronic disorders may
present with more subtle and variable findings; often, nodular swelling
of the tendon may present suggestive of tendinosis (Figure 21-32).
Pain may occur directly over the Achilles tendon proximally, however,
it may also occur distally at the heel. If the pain is located at the
insertion of the Achilles tendon into the calcaneus, it may be due to
some degeneration of the Achilles tendon. In this case, there is
thickening of the tendon
near
its insertion, which at times may become large. This can be associated
with increased warmth over the area as well. Calcification at the
insertion of the Achilles tendon may indicate some degeneration and on
rare occasions is a source of pain. At times, pressure from a
prominence on the posterosuperior aspect of the calcaneus, known as a Haglund deformity,
can be the cause of the pain. In the patient with a Haglund deformity,
a lateral radiograph of the calcaneus reveals a large posterosuperior
prominence on the calcaneus that is responsible for the problem.
Initial conservative treatment should be directed toward activity
modification, inflammation control, and occasionally immobilization.
Corticosteroid use is generally not recommended. If patients fail
conservative treatments, surgical intervention may be considered. The
procedure of choice depends on the spectrum of disease present and
should address all pathology. This may include synovectomy, tendon
debridement, tendon repair, tendon augmentation (i.e., tendon transfer
[FHL] or Achilles turndown flap), or resection of any bony pathology
(i.e., Haglund deformity). The goal of treatment is to return the
patient to their desired level of activity without pain.
fasciitis and atrophy of the heel pad. Heel pad atrophy is most
frequently seen in older patients who develop thinning of the fat pad,
which decreases the cushion on the heel. The diagnosis is made by
palpation of the heel pad and the observation of lack of adequate fatty
tissue. Treatment is conservative with orthotic management for adequate
heel cushioning. Plantar fasciitis is the most common cause of inferior
heel pain and is very common. It commonly occurs with the first step
after a period of rest (e.g., first step in morning) and often improves
with activity. This disorder is an inflammatory process and it is
postulated that with repeated stress, microtears occur at the bony
attachment of the fascia to the calcaneus leading to a chronic
inflammatory process. Obesity, repetitive stress in athletics, middle
age, and the presence of abnormal foot mechanics (i.e., pes cavus or
pes planus) have been associated as risk factors. Although commonly
associated with “heel spurs,” only 50% of patients with plantar
fasciitis have “heel spurs” present radiographically and this finding
of itself is not the cause of the patient’s subcalcaneal discomfort.
Pain is usually located near the tubercle of the calcaneus or just
distal to it and palpation along this region reproduces the patient’s
discomfort. At times, the fasciitis involves the origin of the abductor
hallucis muscle, and in these cases, the pain is located along the
plantar medial aspect of the heel and is aggravated by palpation of the
origin of the muscle. The condition is usually self-limiting and if
treatment is begun soon after the onset of symptoms, most patients can
expect resolution within 6 weeks. A multitude of treatment options
exist and should be exhausted prior to considering surgical
intervention. Initial treatment most often consists of Achilles tendon
stretching exercises (particularly when limited dorsiflexion is
present), oral anti-inflammatory drugs, shoe inserts, and night splints
(preventing plantar flexion). For more recalcitrant cases, periodic
immobilization may be necessary. Corticosteroid injection at the site
of maximal tenderness may be beneficial, but should be used in
moderation, rarely exceeding 2 to 3 injections. Extracorporeal shock
wave therapy has recently shown benefit in the treatment of refractory
fasciitis and should be considered prior to surgical intervention. In
rare cases where 6 to 12 months of nonsurgical management has failed to
provide relief, surgical intervention, consisting of partial plantar
fascia release with or without decompression of the first branch of the
lateral plantar nerve and adductor hallucis fascia, should be
considered.
Occasionally, a stress fracture may involve a calcaneal spur on the
plantar aspect of the calcaneus as a cause of heel pain. This
occasionally can be demonstrated radiographically, however, often a
bone scan is necessary. A bony ridge along the medial or lateral aspect
of the insertion of the Achilles tendon may also be a source of heel
pain. This bony ridge results in a mechanical problem causing chafing
against the counter of the shoe.
imperative that the clinician accurately diagnoses the origin and
directs treatment accordingly. In general, treatment consists of
nonsteroidal anti-inflammatory medications, relief of stress over the
involved bony prominence, use of a soft orthotic device in the shoe to
relieve the heel, cast immobilization, or some combination of these. As
a general rule, surgery is not necessary for heel pain. There certainly
are exceptions, but the physician should be as conservative as possible
in the management of heel pain.
forefoot. The patient may describe a welllocalized area of burning pain
on the plantar aspect of the foot, which often radiates out toward the
tips
of
the toes. It most frequently involves the third interspace, although it
occasionally involves the second interspace. The origin of an
interdigital neuroma is not precisely known, although the nerve often
becomes thickened secondary to increased hyalinization of the tissues
surrounding it and the bursal structures above and below the transverse
metatarsal ligament usually enlarge. The pain associated with an
interdigital neuroma can be reproduced by squeezing the interspace in a
dorsal plantar direction and, when pressure is applied to the
interspace, squeezing the foot in a mediolateral direction (Figure 21-33).
Conservative management consists of fitting the patient in a wide, soft
shoe that also provides metatarsal support. If this fails, excision of
the neuroma can be carried out through a dorsal approach to the web
space, sectioning the transverse metatarsal ligament and resecting the
nerve proximal to the metatarsal head region. This results in a
satisfactory response in about 80% of patients.
or without involvement of the medial calcaneal nerve can be a
neurologic cause of medial ankle and heel pain. The posterior tibial
nerve may become compressed within the fibro-osseous tunnel posterior
and inferior to the medial malleolus. This may be diagnosed by
percussion over the posterior tibial nerve or its terminal branches,
which demonstrate a Tinel’s sign with radiation toward the heel. The
medial calcaneal nerve may be involved at the level of the ankle or at
the level of the abductor digiti quinti muscle as the nerve is
stretched over the plantar fascia as it passes over it to cross the
foot. In these cases, pain is often noted along the plantar medial
aspect of the foot, just below the abductor hallucis muscle. Treatment
is conservative, with orthotic modifications and measures to decrease
the inflammation surrounding the involved nerve. Surgical decompression
is performed only in refractory cases, with best results obtained in
patients with clearly defined space occupying lesions or masses
obstructing the canal.
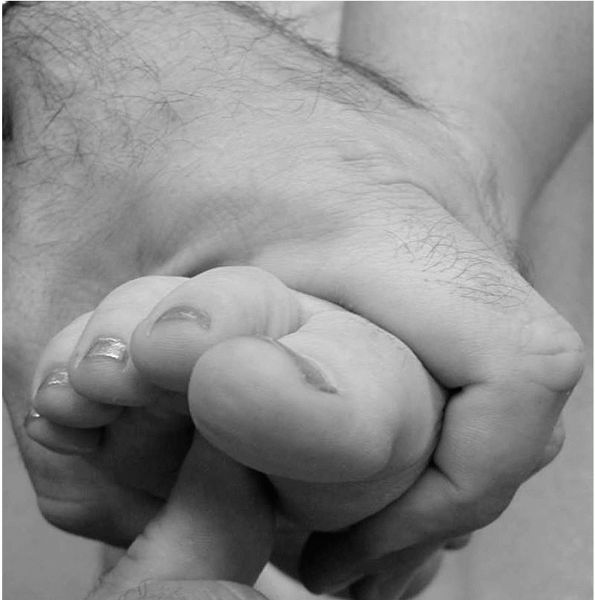 |
|
FIGURE 21-33.
Clinical examination finding of intradigital neuroma (“Mulder’s click”). Reproduction of pain and mechanical subluxation of the thickened nerve and surrounding tissues is produced by squeezing the interspace in a dorsal plantar direction with one hand and applying pressure to the interspace by squeezing the foot in a mediolateral direction with the other hand. |
public health problem. A typical newly diagnosed patient with diabetes
has a roughly 15% chance of developing a foot ulcer over the course of
his or her
disease.
At any given time, roughly 5% of neuropathic diabetics have an ulcer of
the foot. Given the increasing trends toward obesity and type II
diabetes in Western society, the problem is only likely to become more
acute.
distinct clinical problems: neuropathic ulceration and the Charcot
foot. Both are secondary phenomena to diabetic neuropathy. A recent
important prospective study, the Diabetes Control and Complications
Trial, demonstrated the arrested progression of diabetic neuropathy
with intensive glucose control and close monitoring of glycosylated
hemoglobin levels. As a rule, the risk of foot pathology is greatly
reduced by diabetics who are successful at long-term diabetic control
and can maintain their glycosylated hemoglobin levels under 8%.
repetitive unrecognized trauma to an insensate foot as a neuropathic
patient ambulates. It occurs under load-bearing sites in the foot, most
commonly under the metatarsal heads or the heel. A critical level of
the loss of sensation appears to be required to lead to ulceration.
Semmes-Weinstein monofilaments are short lengths of nylon fishing line
of varying thicknesses that can provide a reproducible stimulus to the
skin. Ninety percent of patients that are able to feel the
Semmes-Weinstein 5.07 monofilament will not develop an ulcer.
threshold must maintain a strict regimen of self-care to avoid
ulceration. Daily self-examination of the soles of the feet is
mandatory. Autonomic neuropathy can lead to a loss of sweat and the
resulting cracks and fissures can create portals for infection. The use
of a lanolin-rich moisturizer on all dry locations is critical. The
single most important measure, however, is the use of appropriate shoe
wear. The vast majority of diabetics do not need fully custom shoes.
Instead, manufactured accommodative shoes with a wide forefoot and an
extra-depth toe box are readily available. These are usually paired
with accommodative custom orthotics. The goal of protective diabetic
inserts is to accommodate any foot deformities rather than correct
them, and no attempt is usually made to significantly reposition the
foot. The inserts are usually made of several layers of varying
durometer, or hardness. The deeper layers provide a measure of
durability while the superficial layers conform to the surface of the
foot. Because they are not made of rigid materials, protective
orthotics do wear out and compress rapidly. They must typically be
replaced several times a year.
vascular gangrene also seen in diabetics with associated
atherosclerosis. Vascular gangrene typically strikes distally about the
toes and is not purely associated with load-bearing locations in the
foot. Numerous studies have demonstrated that poor arterial inflow is
not a risk factor for the development of plantar pressure ulcers from
weight bearing. Notably, however, a diminished arterial supply can
severely affect the ability of those ulcers to heal once they are
established.
of unrecognized force applied to the neuropathic foot are also at work
in developing ulceration. Neuropathic patients will not alter their
gait in the presence of any foot deformity. If the patient also has a
midfoot or hindfoot collapse from a Charcot arthropathy, these can be
severe. Charcot patients have a 350% relative risk of developing
ulcerations compared to neuropathic patients without Charcot.
important mechanical risk factor. Tight heel cords are prevalent in
diabetes because the collagen within the tendon undergoes direct
glycosylation with long-standing disease. This leads to abnormal
cross-link formation, reduced pliability, and contracture of the motor
unit. A tight heel cord paradoxically causes pathology in the forefoot;
if the ankle is unable to dorsiflex the heel is brought off the ground
earlier in the stance phase of gait. The metatarsal heads are on the
ground longer and bear more weight and are therefore highly susceptible
to ulceration. Several series have now demonstrated the healing of
recalcitrant forefoot ulcers following the release of a heal cord
contracture.
debrided. Superficial calluses must be removed to determine the health
of the underlying tissues. Radiographs should be obtained to look for
signs of bony erosion indicative of osteomyelitis. These can be
deceptive, however, and erosions may not appear for the first several
weeks after it develops. If an ulcer clinically probes to bone, there
is a 90% chance that osteomyelitis is present based on several studies
using
histologic diagnosis as the criterion. Osteomyelitis in an adult is a
surgical disease; the infected bone must be removed or the ulcer cannot
permanently heal.
important to diagnose. The only role for MRI in the evaluation of the
diabetic foot is to evaluate for the presence of a deep abscess. Bony
edema in the diabetic foot, particularly in the presence of Charcot
change, makes it extremely difficult to accurately determine the
presence of osteomyelitis on MRI criteria, and nuclear medicine studies
are more appropriate for this purpose. The overinterpretation of
superficial wound culture swabs is another common error. All diabetic
ulcers are superficially colonized with a wide variety of organisms
including anaerobes. Superficial swabs often differ dramatically from
deep, surgically obtained biopsies and treatments based on them may
lead to unnecessarily long or risky antibiotic regimens.
its ability to heal. If the dorsalis pedis and tibialis posterior
pulses are not palpable, a Doppler examination is mandated. If there is
still suspicion, vascular noninvasive studies are appropriate. The
ankle-brachial index (ABI), a ratio of the systolic pressure at the
ankle to that in the arm is commonly used. A ratio of 0.4 is a
minimally acceptable value, above 0.7 there is little concern.
Unfortunately, ABIs can be unreliable in the presence of extensive
atherosclerosis. The reduced capacitance of the vascular tree in the
leg can falsely elevate the systolic pressure and the ABI reading. Toe
pressures represent a simple additional test that can be more
informative, but must usually be specifically ordered. A small pressure
cuff is placed over the toe and a pressure reading generated. Absolute
toe pressures above 40 mm Hg or the presence of pulsatile flow are
usually indicative of adequate healing. Transcutaneous oxygen tension
within the foot is an excellent means of assessing the vascularity of a
foot but is not widely available. If none of these methods can
establish the integrity of the arterial blood supply, angiography and
referral to a vascular surgeon are required.
to evaluate. The tightness of the heel cord should be assessed both
with the knee extended (gastrocnemius tight) and with the knee flexed
(gastrocnemius relaxed). The presence of any varus or valgus
deformities in the midfoot or any forefoot deformities should be noted.
Bony prominences that would be well-tolerated in a normal individual
sometimes lead to disaster for the neuropathic diabetic.
mechanical problems, their treatment is primarily mechanical. Reducing
the mechanical stress on the tissues is the primary means of achieving
healing. For the forefoot and midfoot, a variety of manufactured
pressure-relieving boots and shoes are available. The gold standard in
pressure relief, however, continues to be the total contact cast. Most
forefoot ulcerations can be healed in 6 to 8 weeks with serial cast
treatment and ulcer debridement. Unfortunately, casts and boots do no
provide adequate pressure relief for heel ulcerations, and these must
be treated with strict non-weight bearing and dressing changes alone.
biologic activity may be appropriate. Becaplermin gel contains
recombinant platelet-derived growth factor and may be used in
marginally vascularized wounds with atrophic granulation.
Copper-containing compounds also provide a stimulatory effect. Mesh
embedded with cultured human fibroblasts that secrete an array of
growth factors has also been used. Finally, silver-containing gels or
slow-release films can be used in the presence of superficial
colonization by pseudomonas. It is important to note, however, that all
of the biologic adjuvants for wound healing must be used in conjunction
with adequate pressure relief.
support as an adjunctive measure in diabetic ulceration. There is clear
support for its use in life- or limb-threatening anaerobic infections
following aggressive surgical debridement. For routine neuropathic
ulcerations, however, its benefit is unclear. From a practical
standpoint the advent of the recombinant wound gels makes them the
usual current choice when a biologic adjuvant treatment is desired.
There is absolutely no well-controlled evidence that topical normobaric
oxygen therapy (placing the foot in an oxygen-filled bag) provides any
benefit.
famous French neurologist Jean-Martin Charcot, who originally described
the condition in syphilitics. Typically a dense peripheral neuropathy
must be present for approximately 10 to 15 years before the disorder is
manifest. Concordantly, the first cases in diabetics were described in
the
1930s, approximately 10 years after the availability of insulin
extended their lives long enough to develop the complication.
obscure. The neurotraumatic hypothesis is the classic model. It holds
that accumulated microtrauma to the joint in an insensate limb causes
breakdown of the bony architecture. There are, however, well-documented
cases of Charcot arthropathy occurring in completely bedridden
individuals. In the 1960s, it became clear that Charcot arthropathy is
associated with autonomic dysfunction. The neurovascular hypothesis was
developed to tie in this observation. It proposed that a loss of the
autonomic control of bone blood flow occurs, leading to a “wash out” of
bone mineral. There is no causal mechanism to link the increase bone
blood flow in Charcot arthropathy to the loss of bone mineral, however.
Charcot had originally proposed the neurotrophic hypothesis, theorizing
some important “trophic factor” from nerves was critical in maintaining
the health of the joints. He may yet prove correct. Evidence from serum
markers of bone metabolism indicates a dramatic amount of osteoclastic
activity without concordant elevations in osteoblastic activity. A
direct link between peripheral nerve and the regulation of osteoclast
activity remains to be established.
Charcot joint that remain at least broadly useful for communication,
although no clear standards exist to define the precise transitions
from one phase to another. Stage I disease represents the acute
fracture-like state with dramatic soft-tissue swelling and instability (Figure 21-34).
Stage II represents early coalescence with a stable soft tissue
envelope. In stage III, the joint has coalesced and has developed
mature calluses and, usually, stability. Classically in the foot the
entire process takes approximately 18 months to fully progress to the
quiescent stage III, although the time may vary. Approximately 30% of
diabetic patients who develop a Charcot foot on one side will
eventually suffer the same fate on the contralateral extremity.
 |
|
FIGURE 21-34. Diabetic Charcot foot. (A)
Lateral radiograph demonstrating severe midfoot fracture subluxation with midfoot collapse consistent with rocker-bottom deformity. (B) Clinical consequence of ulceration secondary to plantar bony prominence associated with collapse. |
stable, braceable foot that can be used for ambulation. Any hope of a
completely normal foot must be abandoned, and patients must be made
aware of this early on. Midfoot Charcot arthropathy accounts for
roughly 60% of the cases, and the majority of these can be treated
conservatively. During the early stages of the disease, total contact
casts are changed at very frequent intervals until the patient’s volume
status stabilizes. At this point a fully custom clamshell ankle-foot
orthosis or Charcot Restrained Orthotic Walker (CROW) is fabricated (Figure 21-35).
This device should be used until the foot achieves stability both
clinically and radiographically. A portion of patients with midfoot
neuropathic arthropathy will go on to develop plantar prominences and
ulcers from the collapse of the arch. If the overall degree of collapse
is mild and the foot is stable, simple excision of the plantar
prominence can be undertaken. In more advanced cases, the arch
collapses to the point that it actually reverses, creating a
rocker-bottom foot. These cases may require midfoot fusion and
reconstruction of the arch to achieve a successful result.
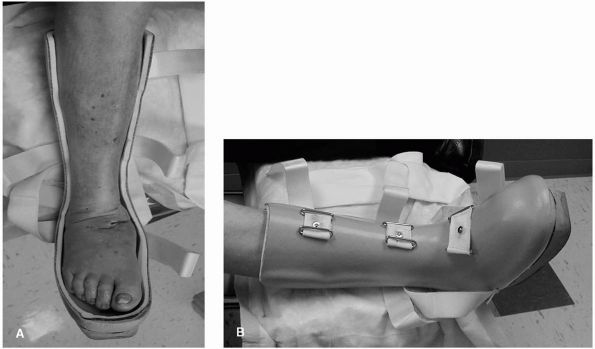 |
|
FIGURE 21-35. (A and B) Orthotic management of Charcot deformity with a Charcot Restrained Orthotic Walker (CROW) device.
|
less common than in the midfoot but has a much more grim prognosis.
This pattern of disease can present in both sporadic forms and after
seemingly simple rotational ankle fractures. It often goes on to severe
early deformity, ulceration, and osteomyelitis. Although stabilization
surgery in the early stages of Charcot arthropathy is usually best
avoided, it may be mandatory in the ankle if the patient develops
severe early deformity that places the limb at risk. Special fusion
techniques including the use of retrograde intramedullary nails are
sometimes necessary.
some form of orthosis. Patients without significant swelling can use a
polypropylene molded AFO, but many obese patients find that the degree
of day-to-day volume change in the foot requires a less confining
brace. A conventional double metal upright AFO attached to the shoe
remains an attractive option in this group.
RA. Biomechanics of the foot and ankle. In: Mann RA, Coughlin MJ, eds.
Surgery of the Foot and Ankle, 6th Ed. St. Louis: Mosby-Year Book,
1993:3-43. This general review article describes the biomechanics of the foot and ankle.
article discusses the history of arthrodesis and the indications,
surgical technique, results, and complications of this procedure.
article discusses the basic concepts used and presents an algorithm
that is helpful in the decision-making process in hallux valgus surgery.
review article discusses the origin, physical findings, radiographic
findings, and treatment of hallux rigidus using various techniques. It
emphasizes cheilectomy and arthrodesis as the main surgical procedures.
RA, Coughlin MJ. The great toe. In: The Video Textbook of Foot and
Ankle Surgery. St Louis: Medical Video Productions, 1991:145. This
book chapter presents a concise overview of hallux valgus surgery,
including the indications, surgical technique, and complications of
various surgical procedures.
article discusses treatment of the hallux valgus deformity using the
distal soft tissue procedure. It points out the technical aspects of
the procedure, results, and complications.
RA, Rudicel S, Graves S. Repair hallux valgus with a distal soft-tissue
procedure and proximal metatarsal osteotomy: a long-term follow-up. J
Bone Joint Surg 1992;74A:124. This is a detailed
analysis of the surgical technique, postoperative results, and
complications of a review of 109 operative procedures in 75 patients.
PF, Van Manten JW. Results of Akin type proximal phalangeal osteotomy
for correction of hallux valgus deformity. Orthopaedics 1990;13:989. This
article discusses results of the Akin procedure on a series of
patients. It points out the indications and complications of this
procedure.
RA, Coughlin MJ. Lesser toe deformities. In: The Video Textbook of Foot
and Ankle Surgery. St Louis: Medical Video Productions, 1991:37. This
concise book chapter reviews the various lesser toe deformities. It
discusses the definition, evaluation, surgical treatment, and
complications of these various deformities.
article reviews the various types of callus formation on the plantar
aspect of the foot. It outlines the conservative and operative
management of these problems.
article discusses the history, physical findings, and surgical
procedure for treatment of the interdigital neuroma. It then analyzes
the results of this procedure.
RA, Coughlin MJ. Postural problems of the foot. In: The Video Textbook
of Foot and Ankle Surgery. St Louis: Medical Video Productions,
1991:17. This book chapter presents an overview
of the various types of acquired flatfoot deformities. It points out
the physical findings, methods of treatment, and technical aspects of
surgery. The chapter further discusses the treatment of the cavus foot.
FW. The diabetic foot and amputations of the foot. In: Mann RA, ed.
Surgery of the Foot, 5th Ed. St Louis: CV Mosby, 1986:421. This
book chapter presents the problem of the diabetic foot along with a
logical approach to treatment. It presents a series of algorithms that
enables the clinician to better understand the various modalities of
treatment of the diabetic foot.
RA, Coughlin MJ. Rheumatoid arthritis and arthrodesis about the foot.
In: The Video Textbook of Foot and Ankle Surgery. St Louis: Medical
Video Productions, 1991:105. This chapter
describes the surgical treatment of the rheumatoid forefoot, presenting
the various types of surgical procedures and postoperative care. It
further discusses arthrodesis about the foot, which includes subtalar,
talonavicular, and tarsometatarsal arthrodeses. It presents a
discussion on triple arthrodesis and double arthrodesis.
