Glenohumeral Arthritis: Osteoarthritis
Editors: Berry, Daniel J.; Steinmann, Scott P.
Title: Adult Reconstruction, 1st Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Section
III – Shoulder Reconstruction > Part B – Evaluation and Treatment of
Shoulder Disorders > 44 – Glenohumeral Arthritis: Osteoarthritis
III – Shoulder Reconstruction > Part B – Evaluation and Treatment of
Shoulder Disorders > 44 – Glenohumeral Arthritis: Osteoarthritis
44
Glenohumeral Arthritis: Osteoarthritis
John W. Sperling
Osteoarthritis is recognized as the most common type of
glenohumeral arthritis. It is characterized by a progressive
arthropathy with loss of articular cartilage and hypertrophic changes
in the subchondral bone. In treating the patient with glenohumeral
osteoarthritis, multiple facets need to be incorporated to formulate a
successful treatment plan. The process begins with a thorough
understanding of the severity of the patient’s symptoms, functional
demands, and ability to comply with postoperative restrictions.
Appropriate imaging studies, in conjunction with a careful examination,
allow the physician to outline a proper treatment plan for the patient.
glenohumeral arthritis. It is characterized by a progressive
arthropathy with loss of articular cartilage and hypertrophic changes
in the subchondral bone. In treating the patient with glenohumeral
osteoarthritis, multiple facets need to be incorporated to formulate a
successful treatment plan. The process begins with a thorough
understanding of the severity of the patient’s symptoms, functional
demands, and ability to comply with postoperative restrictions.
Appropriate imaging studies, in conjunction with a careful examination,
allow the physician to outline a proper treatment plan for the patient.
Pathogenesis
Osteoarthritis of the shoulder is significantly less
common than that of the hip or knee. There is a progressive increase in
the incidence with increasing age. Subclinical stages of osteoarthritis
may exist for decades. Subchondral cysts may be present in both the
humeral head as well as the glenoid. The typical pathologic findings of
osteoarthritis include thinning or complete loss of cartilage on the
humeral head. In addition, the humeral head may flatten with
progressive sclerotic changes. Osteophytes frequently develop at the
margin of the articular surface in a circumferential pattern. These
osteophytes may increase tension on the capsule with resultant loss of
shoulder motion.
common than that of the hip or knee. There is a progressive increase in
the incidence with increasing age. Subclinical stages of osteoarthritis
may exist for decades. Subchondral cysts may be present in both the
humeral head as well as the glenoid. The typical pathologic findings of
osteoarthritis include thinning or complete loss of cartilage on the
humeral head. In addition, the humeral head may flatten with
progressive sclerotic changes. Osteophytes frequently develop at the
margin of the articular surface in a circumferential pattern. These
osteophytes may increase tension on the capsule with resultant loss of
shoulder motion.
One of the characteristics that differentiates
osteoarthritis from rheumatoid arthritis and other inflammatory types
of glenohumeral arthritis is the typical preservation of the rotator
cuff. Multiple studies have demonstrated that the rotator cuff is
intact in 90% to 95% of patients with osteoarthritis.
osteoarthritis from rheumatoid arthritis and other inflammatory types
of glenohumeral arthritis is the typical preservation of the rotator
cuff. Multiple studies have demonstrated that the rotator cuff is
intact in 90% to 95% of patients with osteoarthritis.
Also typical of osteoarthritis is the posterior glenoid
wear pattern frequently present. This disease pattern results in
posterior glenoid wear with associated posterior humeral subluxation.
There is progressive stretching of the posterior capsule with
thickening and contracture of the anterior capsule.
wear pattern frequently present. This disease pattern results in
posterior glenoid wear with associated posterior humeral subluxation.
There is progressive stretching of the posterior capsule with
thickening and contracture of the anterior capsule.
Patient Evaluation
History
Evaluation of the patient with glenohumeral arthritis
begins with taking a thorough history. It is critically important to
understand the severity of the patient’s symptoms and functional
demands. It is essential to understand the primary complaint of the
patient—is it weakness, pain, or loss of motion?
begins with taking a thorough history. It is critically important to
understand the severity of the patient’s symptoms and functional
demands. It is essential to understand the primary complaint of the
patient—is it weakness, pain, or loss of motion?
One should determine how long the shoulder pain has been
present as well as whether there was a specific traumatic event.
Patients are asked to rate their pain on a 1 to 10 scale at rest, with
activities, and at night. Alleviating and aggravating factors are
determined. Patients are asked to specifically localize the pain. Does
the pain occur in the superior-lateral aspect of the shoulder? Does the
pain occur in a radicular pattern down the arm, possibly consistent
with a neurologic cause?
present as well as whether there was a specific traumatic event.
Patients are asked to rate their pain on a 1 to 10 scale at rest, with
activities, and at night. Alleviating and aggravating factors are
determined. Patients are asked to specifically localize the pain. Does
the pain occur in the superior-lateral aspect of the shoulder? Does the
pain occur in a radicular pattern down the arm, possibly consistent
with a neurologic cause?
One should ask about prior evaluations and treatment.
What studies have been performed in the past and what were the results?
Has the patient had a trial of physical therapy? Has the patient had
prior injections? If so, what was the location and response? Has there
been prior shoulder surgery? If so, what was the indication,
postoperative therapy, and outcome? Were there any problems with wound
healing?
What studies have been performed in the past and what were the results?
Has the patient had a trial of physical therapy? Has the patient had
prior injections? If so, what was the location and response? Has there
been prior shoulder surgery? If so, what was the indication,
postoperative therapy, and outcome? Were there any problems with wound
healing?
Review of Systems
A focused review of systems should be documented. Is
there a history of metabolic or rheumatologic disease? Does the patient
have a history of other joint involvement, and in what order should
they be addressed? Is there a history of neurologic symptoms or neck
pain?
there a history of metabolic or rheumatologic disease? Does the patient
have a history of other joint involvement, and in what order should
they be addressed? Is there a history of neurologic symptoms or neck
pain?
P.311
One needs to determine whether there is a history of
cough, shortness of breath, or weight loss. Although uncommon, patients
may present with shoulder pain as a symptom of lung cancer. A list of
medications and associated medical problems should also be compiled to
assist with planning of medical clearance prior to surgery.
cough, shortness of breath, or weight loss. Although uncommon, patients
may present with shoulder pain as a symptom of lung cancer. A list of
medications and associated medical problems should also be compiled to
assist with planning of medical clearance prior to surgery.
Physical Examination
The first step in the physical examination is inspection
with evaluation for atrophy and appearance of prior incisions. One
examines for atrophy associated with long-standing rotator cuff disease
as well as evidence of deltoid deficiency. Palpation begins at the
cervical spine. Cervical motion is evaluated, and testing for potential
cervical radiculopathy is performed with a Spurling test. Examination
is bilateral and should include the wrist, elbow, and shoulder.
Examination of the upper extremities includes assessment of reflexes,
strength, and sensation.
with evaluation for atrophy and appearance of prior incisions. One
examines for atrophy associated with long-standing rotator cuff disease
as well as evidence of deltoid deficiency. Palpation begins at the
cervical spine. Cervical motion is evaluated, and testing for potential
cervical radiculopathy is performed with a Spurling test. Examination
is bilateral and should include the wrist, elbow, and shoulder.
Examination of the upper extremities includes assessment of reflexes,
strength, and sensation.
Shoulder range of motion and strength is carefully
assessed. Active and passive shoulder abduction is recorded. One needs
to determine whether there is a component of anterior-superior humeral
head escape or altered scapular motion with shoulder elevation.
External rotation and internal rotation are recorded. Typically,
shoulder strength is graded on a 1 to 5 scale for internal rotation,
external rotation, flexion, extension, and abduction. Deltoid and
periscapular muscles are also tested.
assessed. Active and passive shoulder abduction is recorded. One needs
to determine whether there is a component of anterior-superior humeral
head escape or altered scapular motion with shoulder elevation.
External rotation and internal rotation are recorded. Typically,
shoulder strength is graded on a 1 to 5 scale for internal rotation,
external rotation, flexion, extension, and abduction. Deltoid and
periscapular muscles are also tested.
Radiographic Studies
Three shoulder views are routinely obtained: an axillary
view and 40- degree posterior oblique views with internal and external
rotation. On the anteroposterior (AP) view, one evaluates both the
medial-lateral and superior-inferior acromiohumeral distance. Among
patients with glenoid erosion, there is a decrease in the amount of
humeral head offset from the lateral border of the acromion.
Specifically, among patients with significant glenoid erosion, the
lateral border of the humeral head is medial to the lateral edge of the
acromion. In patients with rotator cuff deficiency, which is less
common in osteoarthritis, there may be superior subluxation of the
humeral head with a decrease in the acromial-humeral distance. One
caveat is that with posterior subluxation that is frequently present in
osteoarthritis, there can be the false appearance of superior humeral
head subluxation.
view and 40- degree posterior oblique views with internal and external
rotation. On the anteroposterior (AP) view, one evaluates both the
medial-lateral and superior-inferior acromiohumeral distance. Among
patients with glenoid erosion, there is a decrease in the amount of
humeral head offset from the lateral border of the acromion.
Specifically, among patients with significant glenoid erosion, the
lateral border of the humeral head is medial to the lateral edge of the
acromion. In patients with rotator cuff deficiency, which is less
common in osteoarthritis, there may be superior subluxation of the
humeral head with a decrease in the acromial-humeral distance. One
caveat is that with posterior subluxation that is frequently present in
osteoarthritis, there can be the false appearance of superior humeral
head subluxation.
The AP radiographs are also helpful in determining the
overall degree of osteopenia, thickness of the cortices, and size of
the humeral canal. Serial radiographs taken over time will allow one to
confirm the diagnosis of osteoarthritis compared with other diagnoses
that may include rheumatoid arthritis, osteonecrosis, cuff tear
arthropathy, and traumatic arthritis. The axillary view allows
assessment of glenoid erosion and glenohumeral subluxation. CT scans
have become an extremely valuable tool in evaluating the patient prior
to consideration of operative intervention, especially total shoulder
arthroplasty. In the setting of glenoid erosion, CT scans provide
important information concerning glenoid version and quantifying the
amount of bone loss (Fig. 44-1). Three-dimensional CT is a new development that can further assist in evaluating the humerus and glenoid.
overall degree of osteopenia, thickness of the cortices, and size of
the humeral canal. Serial radiographs taken over time will allow one to
confirm the diagnosis of osteoarthritis compared with other diagnoses
that may include rheumatoid arthritis, osteonecrosis, cuff tear
arthropathy, and traumatic arthritis. The axillary view allows
assessment of glenoid erosion and glenohumeral subluxation. CT scans
have become an extremely valuable tool in evaluating the patient prior
to consideration of operative intervention, especially total shoulder
arthroplasty. In the setting of glenoid erosion, CT scans provide
important information concerning glenoid version and quantifying the
amount of bone loss (Fig. 44-1). Three-dimensional CT is a new development that can further assist in evaluating the humerus and glenoid.
 |
|
Figure 44-1 Preoperative CT scan used to evaluate degree of glenoid erosion.
|
Treatment
After integrating the information obtained from the
history, physical exam, and imaging studies, one determines the
specific diagnosis and can present treatment options to the patient. In
the setting of glenohumeral arthritis, conservative therapy plays an
important role in the early stages of disease. Nonsteroidal
anti-inflammatories and intra-articular steroid and/or hyaluronic acid
injections may provide temporary pain relief. A physical therapy
program that focuses on restoring and maintaining range of motion and
strength may be tried. Heat and cold therapy as well as ultrasound may
reduce the inflammatory response and provide pain relief.
history, physical exam, and imaging studies, one determines the
specific diagnosis and can present treatment options to the patient. In
the setting of glenohumeral arthritis, conservative therapy plays an
important role in the early stages of disease. Nonsteroidal
anti-inflammatories and intra-articular steroid and/or hyaluronic acid
injections may provide temporary pain relief. A physical therapy
program that focuses on restoring and maintaining range of motion and
strength may be tried. Heat and cold therapy as well as ultrasound may
reduce the inflammatory response and provide pain relief.
Although many patients with early shoulder
osteoarthritis can be successfully treated with nonoperative
modalities, patients with more advanced disease may require surgical
intervention. In determining the most appropriate treatment, it is
critical to clearly understand the patient’s goals. Patients must be
accepting of the postoperative restrictions and comply with the
rehabilitation. The gold standard for severe osteoarthritis is total
shoulder arthroplasty; however, in the young active patient or those
patients who are unable to accept the restrictions associated with a
prosthesis, this option may not be suitable. In these select cases,
arthroscopic treatment or interposition arthroplasty may provide
symptomatic relief.
osteoarthritis can be successfully treated with nonoperative
modalities, patients with more advanced disease may require surgical
intervention. In determining the most appropriate treatment, it is
critical to clearly understand the patient’s goals. Patients must be
accepting of the postoperative restrictions and comply with the
rehabilitation. The gold standard for severe osteoarthritis is total
shoulder arthroplasty; however, in the young active patient or those
patients who are unable to accept the restrictions associated with a
prosthesis, this option may not be suitable. In these select cases,
arthroscopic treatment or interposition arthroplasty may provide
symptomatic relief.
P.312
Arthroscopic Treatment
The ideal candidate for arthroscopic debridement is a
young, active, high-demand patient with isolated Outerbridge grade I to
III chondral lesions. In addition, ideal candidates have congruent
joint surfaces and minimal osteophyte formation. A thorough
arthroscopic lavage may help remove inflammatory enzymes and proteins
from the joint fluid. In addition, debridement of surface
irregularities, displaced chondral flaps, and labral tears with removal
of loose bodies may alleviate mechanical symptoms. Capsular
contractures can also be released to help restore motion.
young, active, high-demand patient with isolated Outerbridge grade I to
III chondral lesions. In addition, ideal candidates have congruent
joint surfaces and minimal osteophyte formation. A thorough
arthroscopic lavage may help remove inflammatory enzymes and proteins
from the joint fluid. In addition, debridement of surface
irregularities, displaced chondral flaps, and labral tears with removal
of loose bodies may alleviate mechanical symptoms. Capsular
contractures can also be released to help restore motion.
There have been limited reported results of arthroscopic
treatment of arthritis. Ogilvie-Harris and Wiley were the first to
report results of arthroscopic debridement for glenohumeral arthritis.
The authors reported that 60% of patients with mild disease had
improvement; however only 30% of patients with moderate to severe
disease had relief. Weinstein et al. evaluated the extent and duration
of pain relief after arthroscopic debridement for stages I to III
glenohumeral arthritis. Among the 25 patients with a mean follow-up of
34 months, there were 2 excellent, 18 good, and 5 unsatisfactory
results. A trend was noted toward worse results with increasing
severity of cartilage changes. The authors also reported that 10 of 12
patients with marked preoperative stiffness had significant improvement
of motion. Patients with large osteophytes and/or nonconcentric joints
had worse results.
treatment of arthritis. Ogilvie-Harris and Wiley were the first to
report results of arthroscopic debridement for glenohumeral arthritis.
The authors reported that 60% of patients with mild disease had
improvement; however only 30% of patients with moderate to severe
disease had relief. Weinstein et al. evaluated the extent and duration
of pain relief after arthroscopic debridement for stages I to III
glenohumeral arthritis. Among the 25 patients with a mean follow-up of
34 months, there were 2 excellent, 18 good, and 5 unsatisfactory
results. A trend was noted toward worse results with increasing
severity of cartilage changes. The authors also reported that 10 of 12
patients with marked preoperative stiffness had significant improvement
of motion. Patients with large osteophytes and/or nonconcentric joints
had worse results.
Cameron et al. reported on arthroscopic debridement and
capsular release among patients with Outerbridge grade IV lesions.
There were 45 patients with a minimum 2-year follow-up. Patient
satisfaction scores improved significantly with 87% of patients
indicating they would have the surgery again. Osteochondral lesions
>2 cm2 were associated with earlier return of pain and failure of the procedure.
capsular release among patients with Outerbridge grade IV lesions.
There were 45 patients with a minimum 2-year follow-up. Patient
satisfaction scores improved significantly with 87% of patients
indicating they would have the surgery again. Osteochondral lesions
>2 cm2 were associated with earlier return of pain and failure of the procedure.
 |
|
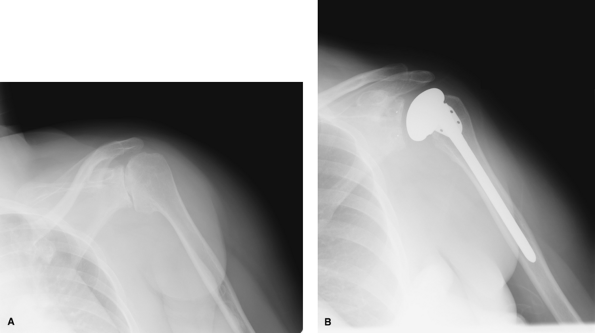
Figure 44-2 Preoperative (A) and postoperative (B) radiographs.
|
Biologic Resurfacing
In the setting of osteoarthritis, biologic resurfacing
of the glenoid alone or in combination with hemiarthroplasty has been
reported to provide good pain relief. Traditionally these patients,
especially heavy laborers, have been considered candidates for
glenohumeral fusion. Although fusion results are satisfactory in 80% of
cases, persistent scapulothoracic muscle pain and significant loss of
motion make this an unattractive option for many active patients.
of the glenoid alone or in combination with hemiarthroplasty has been
reported to provide good pain relief. Traditionally these patients,
especially heavy laborers, have been considered candidates for
glenohumeral fusion. Although fusion results are satisfactory in 80% of
cases, persistent scapulothoracic muscle pain and significant loss of
motion make this an unattractive option for many active patients.
Techniques described usually involve an open approach;
however, an all-arthroscopic resurfacing technique has recently been
published. The goals of interposition arthroplasty and hybrid
interposition arthroplasty are pain relief and restoration of function
while preserving bone stock for future procedures. Several different
materials have been described for use as an interposition material
including anterior capsule, fascia lata autograft, and allografts of
Achilles tendon, lateral meniscus, dura mater, and purified porcine
submucosa.
however, an all-arthroscopic resurfacing technique has recently been
published. The goals of interposition arthroplasty and hybrid
interposition arthroplasty are pain relief and restoration of function
while preserving bone stock for future procedures. Several different
materials have been described for use as an interposition material
including anterior capsule, fascia lata autograft, and allografts of
Achilles tendon, lateral meniscus, dura mater, and purified porcine
submucosa.
Hybrid arthroplasty combining biologic resurfacing of
the glenoid and hemiarthroplasty was first described by Burkhead and
Hutton in 1995. A recent review of Burkhead’s long-term results (5 to
13 years) of 26 shoulders that underwent interposition arthroplasty
demonstrated excellent results in 12 of 26 (46%), 9 of 26 a
satisfactory result (35%), and 5 of 26 an unsatisfactory result (19%)
using Neer’s criteria.
the glenoid and hemiarthroplasty was first described by Burkhead and
Hutton in 1995. A recent review of Burkhead’s long-term results (5 to
13 years) of 26 shoulders that underwent interposition arthroplasty
demonstrated excellent results in 12 of 26 (46%), 9 of 26 a
satisfactory result (35%), and 5 of 26 an unsatisfactory result (19%)
using Neer’s criteria.
P.313
Shoulder Arthroplasty
Total shoulder arthroplasty is the gold standard treatment for osteoarthritis of the shoulder (Fig. 44-2).
Several studies have been published that demonstrate the superiority of
total shoulder arthroplasty compared with hemiarthroplasty for
osteoarthritis of the shoulder. The chance of good to excellent pain
relief with total shoulder arthroplasty is >90% whereas it is 80% to
85% with hemiarthroplasty.
Several studies have been published that demonstrate the superiority of
total shoulder arthroplasty compared with hemiarthroplasty for
osteoarthritis of the shoulder. The chance of good to excellent pain
relief with total shoulder arthroplasty is >90% whereas it is 80% to
85% with hemiarthroplasty.
In addition to retrospective reviews, prospective
studies have been performed demonstrating superior pain relief with
total shoulder arthroplasty. Gartsman et al. performed a prospective
study of 51 shoulders with osteoarthritis, a concentric glenoid, and an
intact rotator cuff. The shoulders were randomly assigned to
hemiarthroplasty or total shoulder arthroplasty (TSA). Total shoulder
arthroplasty had significantly better pain relief. In addition, there
were no revisions in the TSA group and three revisions in the
hemiarthroplasty group for painful glenoid arthritis.
studies have been performed demonstrating superior pain relief with
total shoulder arthroplasty. Gartsman et al. performed a prospective
study of 51 shoulders with osteoarthritis, a concentric glenoid, and an
intact rotator cuff. The shoulders were randomly assigned to
hemiarthroplasty or total shoulder arthroplasty (TSA). Total shoulder
arthroplasty had significantly better pain relief. In addition, there
were no revisions in the TSA group and three revisions in the
hemiarthroplasty group for painful glenoid arthritis.
Conclusion
Arthroscopic debridement for glenohumeral arthritis may
be indicated in young active patients with mild to moderate disease or
in carefully selected patients with advanced disease who do not want
prosthetic replacement. Debridement of chondral and labral lesions,
loose body removal, and capsular releases are the goals of arthroscopic
treatment. Long-term results of arthroscopic debridement are unknown,
but in patients with mild disease, short-term results are encouraging.
Biologic resurfacing of the glenoid alone, or in combination with
hemiarthroplasty, may provide a reasonable option in the young patient
with glenohumeral arthritis. Total shoulder arthroplasty, however,
remains the gold standard for treatment of end-stage glenohumeral
osteoarthritis.
be indicated in young active patients with mild to moderate disease or
in carefully selected patients with advanced disease who do not want
prosthetic replacement. Debridement of chondral and labral lesions,
loose body removal, and capsular releases are the goals of arthroscopic
treatment. Long-term results of arthroscopic debridement are unknown,
but in patients with mild disease, short-term results are encouraging.
Biologic resurfacing of the glenoid alone, or in combination with
hemiarthroplasty, may provide a reasonable option in the young patient
with glenohumeral arthritis. Total shoulder arthroplasty, however,
remains the gold standard for treatment of end-stage glenohumeral
osteoarthritis.
Suggested Readings
Brislin KJ, Savoie FH III, Field LD, et al. Surgical treatment for glenohumeral arthritis in the young patient. Tech Shoulder Elbow Surg. 2004; 5:165-169.
Burkhead WZ, Hutton KS. Biologic resurfacing of the glenoid with hemiarthroplasty of the shoulder. J Shoulder Elbow Surg. 1995; 4:263-270.
Cameron BD, Galatz LM, Ramsey ML, et al. Non-prosthetic management of grade IV osteochondral lesions of the glenohumeral joint. J Shoulder Elbow Surg. 2002; 11:25-32.
Cofield RH. Shoulder arthrodesis and resection arthroplasty of the shoulder. Instr Course Lect. 1985; 34:268-277.
Gartsman
GM, Roddey TS, Hammerman SM. Shoulder arthroplasty with or without
resurfacing of the glenoid in patients who have osteoarthritis. J Bone Joint Surg. 2000; 82:26-34.
GM, Roddey TS, Hammerman SM. Shoulder arthroplasty with or without
resurfacing of the glenoid in patients who have osteoarthritis. J Bone Joint Surg. 2000; 82:26-34.
Nowinski
RJ, Burkhead WZ Jr. Hemiarthroplasty with biologic glenoid resurfacing:
5-13 year outcomes. 70th Annual Meeting, New Orleans, LA, February 5-9,
2003.
RJ, Burkhead WZ Jr. Hemiarthroplasty with biologic glenoid resurfacing:
5-13 year outcomes. 70th Annual Meeting, New Orleans, LA, February 5-9,
2003.
Ogilvie-Harris DJ, Wiley AM. Arthroscopic surgery of the shoulder: a general appraisal. J Bone Joint Surg. 1986; 68B:201-207.
Weinstein DM, Bucchieri JS, Pollock RG, et al. Arthroscopic debridement of the shoulder for osteoarthritis. Arthroscopy. 2000; 16:471-476.
