Chronic Massive Rotator Cuff Tears: Evaluation and Management
III – Shoulder Reconstruction > Part B – Evaluation and Treatment of
Shoulder Disorders > 42 – Chronic Massive Rotator Cuff Tears:
Evaluation and Management
treatment challenge. Because of unique pathologic anatomic features,
they must be considered distinct from both smaller chronic tears and
acute traumatic massive rotator cuff tears. For the purposes of this
review, chronic massive rotator cuff tearing implies that there has
been long-standing pathology, not necessarily with concurrent symptoms,
leading to the presentation of a patient with a massive rotator cuff
tear and substantial rotator cuff muscle atrophy. This implies that the
tear is difficult to repair primarily, if not sometimes irreparable.
With an aging population and increasing functional expectations, it is
likely that we will encounter this difficult problem with increasing
frequency.
management, nonoperative rehabilitation, subacromial debridement,
biceps tenodesis or tenotomy, rotator cuff repair, and rotator cuff
reconstruction, all of which have some demonstrated efficacy. The goals
and expectations of the treatment of this difficult problem must be
clearly understood and defined to maximize the outcome. Determining the
best treatment for an individual patient with a chronic massive rotator
cuff tear can be difficult. There are no randomized prospective studies
that compare nonoperative and operative treatment, nor are there any
studies that compare the various surgical options. The purpose of this
review is to present a current understanding of chronic massive rotator
cuff tears and discuss the evaluation and management of patients with
chronic massive rotator cuff tears.
extensive debate, and there are several factors that are implicated in
the development of rotator cuff tears. Interestingly, the presence of a
tear does not a priori render a shoulder symptomatic. Studies of large
numbers of patients with symptomatic rotator cuff tears note that the
size of a tear does not directly correlate with self-reported symptoms.
as either intrinsic or extrinsic. Intrinsic factors relate to pathology
of the rotator cuff muscles and tendons. This includes degenerative
changes that occur with aging, tendon overload, and relative
hypovascularity of the anterior aspect of the supraspinatus tendon.
Extrinsic factors include subacromial impingement, glenohumeral
instability, and unstable os acromiale. Patients with chronic massive
rotator cuff tears usually do not have a history of significant
shoulder trauma. In occasional cases there is a remote history of
trauma that may have caused the tearing. The context of the onset of
symptoms is an important consideration. Although many patients with
chronic massive rotator cuff tears have an insidious onset of symptoms
with gradual worsening, some report a more acute onset of symptoms
sometimes related to a traumatic event.
usually older. This is consistent with the results of studies that
demonstrate that there is an increasing prevalence of rotator cuff
tears even in asymptomatic individuals with advancing age. Less
frequently, younger patients, often males with a history of substantial
labor or physical activity involving the upper extremities, present
with chronic massive rotator cuff tears.
|
TABLE 42-1 Rotator Cuff Tear Size Classification
|
||||||||
|---|---|---|---|---|---|---|---|---|
|
the chronicity and size of the tear. The chronicity of a rotator cuff
tear can refer to either the duration of symptoms or the duration of
pathology. There are several approaches to classifying the size of
rotator cuff tears. The most commonly used approach is based on the
dimensions of the tear (Table 42-1). Rotator
cuff tears can also be classified according to the number of tendons
that are involved, with massive tears involving at least two complete
tendons. Additionally, the extent of tendon retraction and the tissue
quality are important factors that are not generally accounted for by
the various size-based classification systems. Nevertheless, muscle
quality is especially important in the context of larger rotator cuff
tears. Muscle quality can be appreciated on physical examination as
atrophy of the spinati muscles, as well as on CT and MR imaging. Based
on CT and MR imaging, the rotator cuff muscles are graded as stage 0
(completely normal), stage 1 (some fatty streaks), stage 2 (marked
fatty infiltration but more muscle than fat), stage 3 (as much fat as
muscle), or stage 4 (more fat than muscle).
-
Tear size
-
Number of tendons involved
-
Tendon retraction
-
Rotator cuff muscle status
typically present with pain and shoulder dysfunction and tend to be
older than the average patient with a rotator cuff tear. Less commonly,
younger patients present with chronic massive rotator cuff tears.
Chronic massive rotator cuff tears can present in three different
clinical settings. Although most patients present with an insidious
onset of shoulder pain and dysfunction, some present with a history of
a previous significant traumatic injury that caused the tear or a
recent traumatic event that aggravated an underlying pre-existing
rotator cuff tear. Patients with the latter presentation,
acute-on-chronic tears, present in two clinical scenarios. The first
includes patients with pre-existing chronic symptomatic rotator cuff
tearing who sustain an injury that causes an acute extension of the
tear. The second group has pre-existing asymptomatic rotator cuff tears
and an acute injury that results in the onset of shoulder pain. In
either case, there was pre-existing rotator cuff tearing. After an
acute traumatic injury, patients may be unable to actively elevate
their arm. In some cases there is extensive anterior arm ecchymosis.
The important point is that patients who deny pre-existing symptoms but
have the typical clinical features of chronic rotator cuff tearing;
spinatus atrophy, external rotation weakness, and characteristic plain
radiographic findings are likely to have had pre-existing rotator cuff
tearing.
determined with a detailed physical examination. Any evaluation for
shoulder pathology should also include examination of the cervical
spine and a focused neurologic evaluation. Cervical spondylosis,
stenosis, and radiculopathy can cause shoulder pain that mimics the
pain of rotator cuff pathology. Shoulder girdle weakness can also be
the result of brachial plexus disorders (Parsonage-Turner syndrome and
brachial neuritis, or tumor) or suprascapular neuropathy. Last, the
presentation of chronic septic arthritis can mimic a chronic massive
rotator cuff tear and should not be forgotten when evaluating patients.
Table 42-2 lists differential diagnosis disorders.
|
TABLE 42-2 Differential Diagnosis for Chronic Massive Rotator Cuff Tear
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|
|
anatomic information. Several findings are consistent with chronic
massive rotator cuff tearing. These include anterior superior
subluxation and prominence of the humeral head, infraspinatus and
supraspinatus atrophy, and chronic rupture of the proximal tendon of
the long head of the biceps. Supraspinatus atrophy is more difficult to
detect beneath the trapezius muscle. In many cases massive rotator cuff
tears can be detected as a palpable defect at the supraspinatus
insertion at the anterior lateral aspect of the shoulder. Swelling
owing to subdeltoid synovial fluid can also be present. Deltoid
detachment is rare but is usually visible as a defect at the anterior
aspect of the origin of the middle deltoid.
 |
|
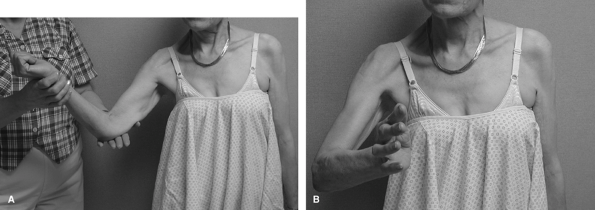
Figure 42-1 The right shoulder has an external rotation lag sign in this patient with a massive rotator cuff tear. A: The arm can be passively externally rotated. B: The patient cannot actively externally rotate the arm. (From
Green A. Chronic massive rotator cuff tears: evaluation and management. J Am Acad Orthop Surg. 2003;11:321–331
, with permission.) |
scapular plane elevation, external rotation with the arm at the side
and in 90 degrees abduction, internal rotation behind the back and at
90 degrees abduction, and across-chest adduction. When motion is
assessed, the scapulohumeral rhythm is also assessed. Several studies
have noted alterations in scapulohumeral rhythm in the presence of
shoulder pathology. Significant loss of passive shoulder motion is
uncommon in the presence of a massive rotator cuff tear. Nevertheless,
patients can have subtle loss of motion in specific directions that can
contribute to symptoms. It is important to recognize shoulder stiffness
in the presence of rotator cuff tear for two reasons. First, strength
is more difficult to evaluate when there is substantial stiffness.
Second, the cause of the stiffness (adhesive capsulitis, capsular
contracture, or glenohumeral arthritis) may be the cause of the
patient’s symptoms. Despite severe rotator cuff deficiency, some of
these patients have good elevation strength owing to compensatory
deltoid strength. Consequently, many patients with chronic massive
rotator cuff tears have full active shoulder elevation. Patients with
significant deltoid weakness may be unable to actively elevate their
arm.
 |
|
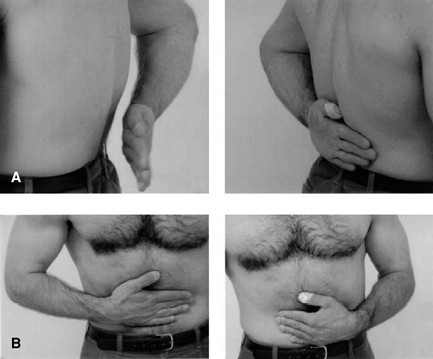
Figure 42-2 A: A positive lift-off maneuver in a patient with a subscapularis tendon tear of the left shoulder. B: A positive belly-press test of the left shoulder in the same patient. Note the posterior position of the left elbow. (From
Lyons RP, Green A. Subscapularis tendon tears. J Am Acad Orthop Surg. 2005;13:353–363
, with permission.) |
massive rotator cuff tears. Elevation weakness is a less consistent
finding. Some patients have sufficient deltoid strength to mask the
absence of supraspinatus strength. The Jobe empty can test, which
assesses strength with the shoulder elevated about 90 degrees and
internally rotated with the thumb pointing downward, will usually cause
pain and elicit weakness. Pain can also be the cause of inability to
elevate the arm. A subacromial injection with 10 centiliters (100 mL)
of 1% lidocaine can eliminate the pain and allow a better assessment of
rotator cuff strength.
rotation weakness and external rotation lag are signs of massive
rotator cuff tearing that involves the infraspinatus tendon (Fig. 42-1).
An external rotation lag sign is elicited by passively positioning the
arm in maximal external rotation. When there is marked weakness, the
patient is unable to hold the arm in this position and the hand falls
toward the abdomen. The horn blower’s sign, inability to externally
rotate the elevated arm, also demonstrates severe infraspinatus
weakness. Associated subscapularis tearing is less common but may also
be present. Patients with chronic atraumatic subscapularis tearing have
internal rotation weakness, variable excessive passive external
rotation, and a positive lift-off test or belly-press maneuver6 (Fig. 42-2).
The lift-off test is difficult to perform when there is pain or limited
shoulder motion that prevents positioning of the arm and hand behind
the back. Unfortunately, subscapularis tears are often overlooked or
ignored by inexperienced examiners, both surgeons and radiologists.
 |
|
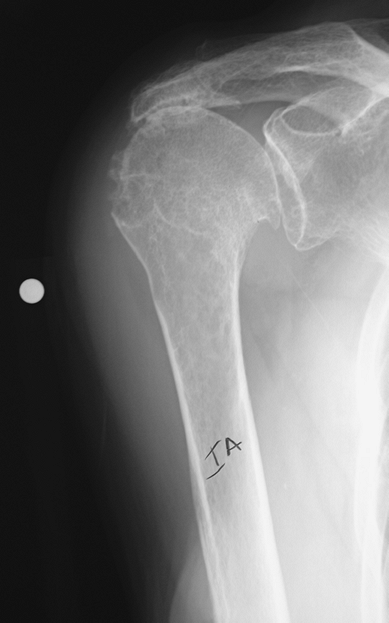
Figure 42-3
True anterior posterior radiograph of a shoulder with a chronic massive rotator cuff tear. Although, there is reduction of the acromial humeral space and the humeral head is elevated relative to the glenoid, there is no glenohumeral arthritis. |
 |
|
Figure 42-4
True anterior posterior radiograph of a shoulder with rotator cuff tear arthropathy. There is no acromiohumeral space, there are degenerative changes of the glenohumeral joint, and the greater tuberosity is rounded off. |
performed and assessed to evaluate patients with rotator cuff
disorders. Park et al. evaluated eight physical examination tests. The
combination of the painful arc sign, drop-arm sign, and infraspinatus
muscle test produced the best posttest probability (91%) for
full-thickness rotator cuff tears, especially in patients older than 60
years of age.
physical examination often provides sufficient information to establish
a diagnosis of massive rotator cuff tearing. Imaging studies provide
information to confirm the diagnosis and assist in treatment selection.
-
Spinati atrophy
-
Anterior superior humeral head position
-
Rupture of the proximal tendon of the long head of biceps
-
Weak external rotation
of five plain radiographs. These views include a true anteroposterior,
anteroposterior in internal and external rotation, axillary lateral,
and outlet. Although plain radiographs do not visualize soft tissues,
they demonstrate skeletal and osseous changes that suggest the presence
of rotator cuff pathology and are particularly helpful in assessing
patients with chronic massive rotator cuff tears (Fig. 42-3).
and narrowing of the acromiohumeral space are findings that are
consistent with long-standing rotator cuff pathology (Fig. 42-4).
It has been suggested that an acromiohumeral space <7 mm is
consistent with a rotator cuff tear and that when the space is <5
mm, there is a massive tear. Erosion or rounding off of the greater
tuberosity (femoralization) is typical of long-standing massive rotator
cuff tearing. Similarly, long-standing contact of the greater
tuberosity with the acromion can lead to the formation of a facet on
the underside of the lateral acromion as well as spurring and
excrescences on the greater tuberosity that can be visualized on
anterior posterior radiographs. The true anteroposterior and axillary
lateral radiographs can also demonstrate glenohumeral arthritis. The
axillary lateral view also demonstrates the relative anteroposterior
position of the humeral
head.
Anterior subluxation on an axillary lateral radiograph is consistent
with anterior superior instability or subscapularis tendon tear. The
outlet view is used to demonstrate the acromial morphology.
 |
|
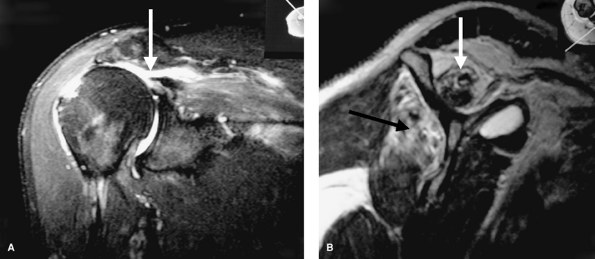
Figure 42-5 MRI scans of the right shoulder of a 64-year-old male with a chronic rotator cuff tear. A:
T2 coronal oblique image demonstrates the supraspinatus tendon tear, atrophy of the muscle, and fatty replacement in the supraspinatus fossa. The supraspinatus tendon (arrows) is at the glenoid. B: T1 sagittal oblique image demonstrates fatty replacement in the supraspinatus fossa and lipoatrophy of the infraspinatus muscle. (From Green A. Chronic massive rotator cuff tears: evaluation and management. J Am Acad Orthop Surg. 2003;11:321–331
, with permission.) |
arthropathy include loss of the glenohumeral joint space, elevation of
the humeral head, erosion and rounding off of the greater tuberosity,
and articulation of the humeral head with the acromion (Fig. 42-4).
It is important to recognize the presence of significant glenohumeral
arthritis as it is a relative contraindication to rotator cuff repair
and reconstruction.
-
Superior humeral head subluxation
-
Acromial humeral space narrowing
-
Femoralization of the humeral head
for the diagnosis of rotator cuff tearing. However, newer imaging
modalities such as ultrasonography and MRI provide better information
and have replaced arthrography as the imaging tests of choice for
rotator cuff pathology.
cuff has been variable. Centers with extensive experience report high
rates of sensitivity and specificity. Other centers are not able to
confirm these findings. Although some of the variability is related to
inexperience, some is also related to differing diagnostic criteria.
More recent technologic advances are encouraging a re-evaluation of the
value of ultrasonography for imaging the rotator cuff. This includes
use of ultrasound by the examining physician.
art for imaging the rotator cuff. It can be highly accurate and
demonstrates detailed anatomic information, including tear size and
muscle quality. The latter information can help establish the
chronicity of the rotator cuff tearing and the potential functional
status of the cuff. Goutallier et al, reported that higher grades of
presurgical fatty degeneration of the rotator cuff muscles are
associated with inferior outcomes.
primarily used to evaluate the supraspinatus tendon and muscle. The
extent of retraction and the size and quality of the supraspinatus
muscle can be determined (Fig. 42-5A). Fatty
replacement of the supraspinatus muscle in the supraspinatus fossa
indicates chronic pathology. The size of the supraspinatus tear in the
anterior-to-posterior direction can be assessed by noting the tear on
sequential images. The sagittal oblique images demonstrate the
anterior-to-posterior extent of tearing as well as the quality of all
of the rotator cuff muscles (Fig. 42-5B). The
axial images can demonstrate the biceps tendon, as well as
subscapularis, infraspinatus and teres minor tearing and muscle
quality. Axial T2 images are essential for a complete magnetic
resonance imaging (MRI) evaluation of the shoulder.
disorders that can mimic massive rotator cuff tearing. Specifically,
patients with external rotation weakness should be evaluated with MRI.
Suprascapular nerve palsy, spinoglenoid notch cysts with compression of
the infraspinatus branch of the suprascapular nerve, and cervical spine
disorders are examples of such disorders. Myopathic changes on MRI are
more consistent with neurologic abnormality.
evaluation of the rotator cuff. However, it can be helpful in imaging
the rotator cuff after surgery when it is difficult to differentiate
scar tissue from tendon.
magnetic resonance imaging of the rotator cuff, the specific
indications for MRI are rarely addressed. Overuse of MRI is a pervasive
problem, and careful clinical evaluation can help to define the
appropriate usage of this excellent imaging technique. In most cases
the diagnosis of a chronic massive rotator cuff tear can be made with a
careful history and physical examination alone. MRI is clearly
indicated early in the evaluation of shoulder pain and dysfunction
after an acute traumatic injury.
rotator cuff tearing depends on selecting the best treatment option for
the specific case at hand. Chronic massive rotator cuff tears present
in various patients, and treatment options include nonoperative
methods, surgical debridement, repair, and reconstruction. Studies have
reported high success rates with each of these approaches. In some
cases, more than one of the options may be appropriate. Thus, careful
consideration of many factors is important, and treatment should be
individualized to the case at hand.
can be successfully treated without surgery. The rationale behind
nonoperative treatment is that some individuals have asymptomatic
rotator cuff tears and never present for evaluation and treatment.
Activity modification, oral nonsteroidal anti-inflammatory medications,
and corticosteroid injections can help some individuals manage their
symptoms. Studies of nonoperative treatment of full-thickness rotator
cuff tear note improvement in about 50% to 85% of patients. The
duration of symptoms seems to correlate with the long-term success of
nonoperative treatment.
injections have a detrimental effect on the rotator cuff and articular
surfaces. In addition, some studies note a negative correlation between
the results of rotator cuff repair and the number of preoperative
corticosteroid injections. Other studies suggest that the association
is less clear-cut. Injections can be very helpful in the initial phases
of physical therapy and rehabilitation. With less pain, patients are
better able to participate in a rehabilitation program. Nevertheless,
repeated corticosteroid injections should be avoided.
shoulder motion and strengthening of the intact portions of the rotator
cuff and the periscapular and deltoid muscles. Passive motion is
improved with stretching exercises. Strengthening of the internal and
external rotators is best achieved with resisted exercises performed
with the arms below chest level. Deltoid strengthening should be
initiated in the supine position with the effects of gravity minimized
and then progressed to an upright seated or standing position. In
addition, scapular muscle strengthening can enhance the function of a
weak rotator cuff. There are various techniques for strengthening,
including isometric, isotonic, and isokinetic exercises. Strengthening
should be progressed gradually and within the patient’s comfort level.
spinati atrophy, evidence of chronic rotator cuff tearing, are ideal
candidates for nonoperative treatment. In many such cases it is
unlikely that the massive rotator cuff tear will be repairable. Thus,
nonoperative management should be the first line of treatment.
tears encompasses a spectrum of complexity ranging from minimally
invasive arthroscopic approaches to major reconstructive surgery. There
are advocates for all options but few objective data to guide selection.
rotator cuff debridement as treatment for massive irreparable rotator
cuff tears. The rationale behind subacromial smoothing and rotator cuff
debridement includes our knowledge that there are asymptomatic
individuals with rotator cuff tears, and the fact that a substantial
proportion of patients who have a satisfactory result from a repair of
a massive rotator cuff tear have persistent rotator cuff defects after
the repair.
lower-demand individuals. More active individuals who fail nonoperative
treatment are probably better served with attempted rotator cuff
repair. Some authors report that the results of debridement of
full-thickness rotator cuff tears deteriorate with time.
repairable, in some cases the tear is either not repairable or repair
would be unlikely to substantially alter shoulder function. The ideal
candidate for debridement is an individual with shoulder pain who has
good elevation strength, can actively elevate the arm overhead, and can
externally rotate the arm with gravity eliminated. This suggests that
there is good shoulder kinematics and that the internal and external
rotators are balanced.
subacromial debridement. The arthroscopic approach has the advantage of
an easier and more rapid rehabilitation because the deltoid origin is
preserved. Acromial smoothing as opposed to formal acromioplasty is
performed to remove undersurface spurring and rough excrescences.
Similarly, the greater tuberosity is smoothed; a so-called reverse
acromioplasty arthroscopic subacromial decompression. Thus, the
coracoacromial arch is maintained by avoiding an excessive
acromioplasty and by preserving the coracoacromial ligament. This helps
to prevent loss of the restraint to superior
humeral head subluxation that the intact coracoacromial arch provides.
adjunct to arthroscopic debridement of chronic massive rotator cuff
tears. If there is subluxation or dislocation of the tendon of the long
head of the biceps or partial tearing, this can be an effective
procedure to alleviate shoulder pain associated with chronic massive
rotator cuff tears. In the older patient, arthroscopic tenotomy is a
minimally invasive procedure that does not require the postoperative
immobilization or protection that a tenodesis requires.
arthroscopic treatment of chronic massive rotator cuff tears include
preoperative superior migration of the humeral head, the presence of
subscapularis tearing or weakness, the presence of glenohumeral
arthritis, and decreased range of motion. Most authors point out that
although the short-term results of arthroscopic treatment are
encouraging, the long-term results often deteriorate.
and the results of rotator cuff repair. Most recent studies of rotator
cuff repair have reported successful outcome in 80% to 90% of cases.
The traditional goal of rotator cuff repair is to repair the rotator
cuff tendons to the proximal humerus and to decompress the subacromial
space without disrupting the coracoacromial arch. The role of
acromioplasty has been recently questioned, and some authors do not
routinely perform it as part of a rotator cuff repair. Repair of
chronic massive rotator cuff tears is particularly difficult because of
tendon substance loss, retraction, scarring, and poor mechanical
properties. Several techniques and maneuvers are used to mobilize the
rotator cuff tendons and facilitate the repair. Traditional open
techniques, mini-open, and all arthroscopic repairs have been
advocated. Determining the feasibility of a repair is of primary
importance as not all chronic massive rotator cuff tears are repairable.
third of the acromion in the Langer lines. This is a very cosmetic
incision and can be extended anteriorly to permit a deltopectoral
approach if required to repair a concomitant subscapularis tear. The
skin and subcutaneous tissue are elevated as full-thickness flaps to
expose the acromion and the origins of the anterior and middle heads of
the deltoid muscle. The anterior deltoid is elevated off the anterior
acromion, and the deltoid fibers are split laterally just posterior to
the deltoid raphe for about 3 to 4 cm. In doing this, the
coracoacromial ligament is released from the acromion but not resected.
This approach allows ample access to the subacromial and subdeltoid
spaces, as well as the supraspinatus, infraspinatus, and teres minor
tendons.
undersurface of the anterior acromion, decompress the subacromial
space, and create a smooth acromial surface, without disrupting the
coracoacromial arch. Spurring on the undersurface of the distal
clavicle is also removed. Care is taken to avoid excessive resection,
especially shortening of the acromion to prevent anterior superior
instability.
excess bursal tissue can be excised to allow visualization of the
rotator cuff tear. Adhesions under the anterior deltoid are often more
tenacious and require more formal dissection to clearly visualize the
rotator cuff interval and subscapularis tendon.
of the upper third of the subscapularis tendon can often be repaired
through this exposure. More extensive tears may require a separate
deltopectoral approach. Similarly, the biceps tendon is visualized both
within the glenohumeral joint and by pulling the more distal aspect up
from the biceps groove.
are identified and traction sutures are placed. In contrast to cases of
acute massive tears that can usually be easily mobilized to the
tuberosity, additional steps are required to mobilize chronic massive
tears. Fascial adhesions superficial to the supraspinatus and
infraspinatus muscles are bluntly released. Releasing the rotator cuff
interval and the coracohumeral ligament at the base of the coracoid
helps to mobilize the supraspinatus tendon. Capsular releases
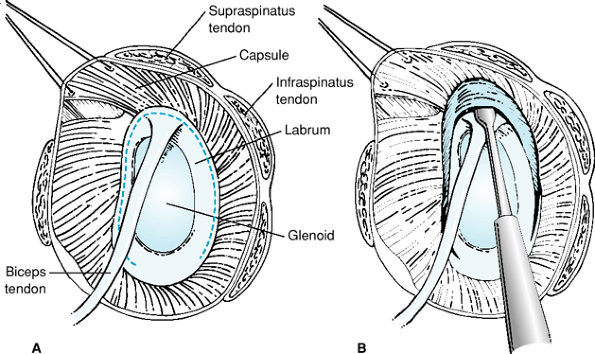
superiorly and posteriorly will also improve mobility (Fig. 42-6).
Occasionally, the interval between the supraspinatus and infraspinatus
tendons, the so-called posterior interval, is released to allow
differential mobilization of the supraspinatus and infraspinatus
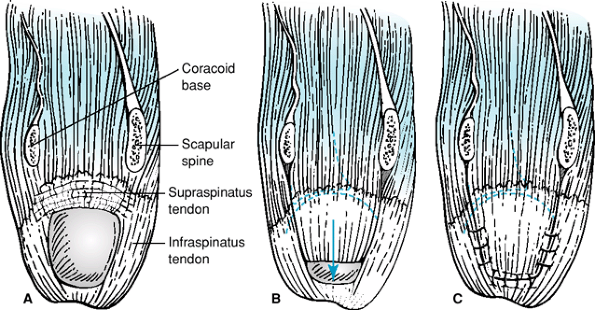
tendons (Fig. 42-7). The limit of mobilization
of the supraspinatus and infraspinatus muscles is determined by the
extent to which the suprascapular nerve can be mobilized. The standard
anterosuperior approach allows only 1 cm of lateral advancement of the
tendons whereas the mobilization of the supraspinatus muscle from the
supraspinatus fossa of the scapula permits ≤3 cm of lateral advancement.
site on the proximal humerus is prepared by decorticating the bone just
lateral to the articular surface. Tendon reattachment can be
accomplished by passing no. 2 braided nonabsorbable sutures through
transosseous tunnels or by using suture anchors. Many suture techniques
are available. The Mason-Allen suture technique is usually recommended.
Augmentation of the bone of the greater tuberosity with small plates or
washer-type devices is advocated when there is substantial osteopenia
to improve the strength of the suture bone interface
deltoid origin is reattached to the anterior acromion with
nonabsorbable sutures passed through drill holes in the acromion. This
repair is reinforced with additional nonabsorbable sutures. A secure
repair of the deltoid is critical to avoid postoperative deltoid
avulsion. Again, the coracoacromial ligament is preserved and
essentially reattached to the acromion as part of the deltoid repair.
the side. A repair with excessive tension is likely to fail. If this is
not possible, a partial repair is performed or rotator cuff
reconstruction is considered. Burkhart has espoused the concept of
partial repair that re-establishes the cable construct of the rotator
cuff. This is in part achieved by repairing the cuff defect side to
side. In many cases the infraspinatus can be mobilized laterally and
superiorly to be
repaired
to the greater tuberosity. Although some authors have advocated
reattachment of the rotator cuff more medially into the articular
surface, this is not a widely accepted technique.
 |
|
Figure 42-6 A, B: Glenohumeral capsular releases to mobilize the rotator cuff. (From
Green A. Chronic massive rotator cuff tears: evaluation and management. J Am Acad Orthop Surg. 2003;11:321–331
, with permission.) |
 |
|
Figure 42-7 Anterior and posterior rotator cuff interval releases to mobilize a large tear of supraspinatus and infraspinatus tendons. A: Dotted lines indicate the releases. B: Supraspinatus tendon mobilized separate from infraspinatus. C: Tendon sutured into place for the repair. (From
Green A. Chronic massive rotator cuff tears: evaluation and management. J Am Acad Orthop Surg. 2003;11:321–331
, with permission.) |
advantages of arthroscopic and open surgery. Advocates of mini-open
rotator cuff repair stress that there is less deltoid morbidity than
with an open repair. This claim is controversial. The access through
the deltoid split is more limited than with an open repair and may lead
to more aggressive deltoid retraction. Consequently, the mini-open
technique should be applied carefully when repairing massive tears.
Additionally, the rate of postoperative infection appears to be higher
after mini-open rotator cuff repair.
becoming the preferred technique for rotator cuff repair. As the
technique has evolved, it has been applied to larger rotator cuff
tears. Although the early functional outcomes appear similar to the
outcomes of open repairs, the incidence of persistent or recurrent tear
is higher for all-arthroscopic repairs. All-arthroscopic techniques
attempt to perform all of the essential steps of an open repair to
mobilize and repair the rotator cuff. New techniques are being
developed to improve the fixation and tendon apposition.
between debridement and complete rotator cuff repair. This generally
refers to repair of the infraspinatus. Margin convergence without
tendon-to-bone repair is also advocated. It is thought that this
restores the anterior-to-posterior stabilizing characteristics of the
rotator cuff. Partial rotator cuff repair can be performed with open or
arthroscopic techniques.
 |
|
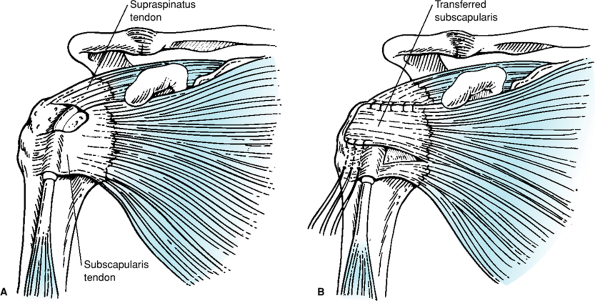
Figure 42-8 Subscapularis transfer. A: The upper portion is elevated off of the anterior capsule and transferred superiorly. B: Note that the inferior muscular insertion is left intact. (From
Green A. Chronic massive rotator cuff tears: evaluation and management. J Am Acad Orthop Surg. 2003;11:321–331
, with permission.) |
lengthy. The repair is protected with an arm sling or abduction
immobilizer for 6 to 8 weeks. Abduction positioning is used to relieve
tension on a repair that can be accomplished with the arm at the side,
but not to allow repair of an irreparable tear. Passive stretching
exercises to regain shoulder motion are begun the day after surgery.
After repair of chronic massive tears, passive internal rotation and
horizontal adduction are avoided for the first 6 weeks to protect the
infraspinatus repair. Light active use and active assisted range of
motion is initiated after 6 weeks. Formal strengthening is delayed
until 12 weeks after surgery. The overall recovery can take >12
months. Overly aggressive early rehabilitation, especially
strengthening, has been implicated as a cause of failure.
results of repair of massive rotator cuff tears. Most studies combine
the repairs of a spectrum of tear sizes and find that the results of
repair of larger tears are inferior to the results of repair of smaller
tears. The results of the repair of chronic massive rotator cuff tears
vary. Most patients have significant reduction in pain and some
functional improvement. Harryman et al. and Gerber found that repair
integrity rather than the original tear size best correlated with the
functional outcome of rotator cuff repair. Bigliani et al. evaluated
the long-term results of repair of chronic massive rotator cuff tears
and reported 85% good and excellent results. Bjorkenheim et al. found
that the results of repair of large and massive rotator cuff tears were
markedly inferior to the results of repair of smaller tears. Most
recently, Jost et al. studied the clinical outcome after failed healing
of rotator cuff repairs. They found that the outcome was significantly
correlated with the size of the postoperative tear and the extent of
fatty degeneration of the infraspinatus and subscapularis muscles. They
also found that the size of the tear at follow-up was related to the
size of the original tear; larger persistent tears were associated with
larger initial tears. Goutallier et al. demonstrated that recurrent
tear was greater for tendons whose muscle showed fatty degeneration
>grade 1. Fatty degeneration of the infraspinatus or subscapularis
muscles had an influence on supraspinatus tendon outcome. Rokito et al.
found that all of their patients were satisfied after repair of a
chronic large or massive rotator cuff tear, that >1 year was
required for restoration of strength, and that the final strength was
less than in the contralateral shoulder. Duralde and Bair reported good
and excellent results in 67% of patients who had partial rotator cuff
repair.
irreparable massive rotator cuff tears. These include transfers of the
rotator cuff tendons, other muscle and tendon transfers, and tissue and
synthetic substitution and augmentation. These procedures attempt to
restore the function of the rotator cuff muscles and tendons.
infraspinatus leaves a residual superior defect. The upper third of the
subscapularis tendon is separated from the anterior capsule and is then
transferred superiorly (Fig. 42-8).
 |
|
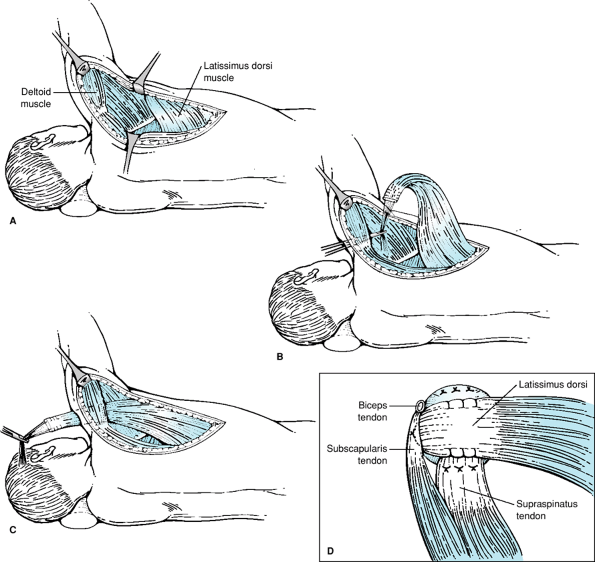
Figure 42-9 Latissimus dorsi transfer for massive irreparable rotator cuff tear. A: The latissimus dorsi muscle and tendon are dissected. B: The latissimus dorsi tendon is released from the humerus, and sutures are placed into the tendon. C: The tendon is passed inferior to the posterior deltoid and the acromion to the superior wound. D:
The transferred tendon is sutured to the edge of the mobilized but deficient cuff edge and the greater tuberosity. (Modified from Green A. Chronic massive rotator cuff tears: evaluation and management. J Am Acad Orthop Surg. 2003;11:321–331
, with permission.) |
transfer. Subscapularis transfer does have the risk of causing internal
rotation weakness or internal rotation contracture.
the supraspinatus muscle and found that the results of repair of larger
rotator cuff tears were improved by this procedure. Ha’eri and Wiley
also reported good results with lateral advancement of the
supraspinatus muscle. In addition, they found that the muscle was not
denervated by the procedure. Although Warner et al. demonstrated that
the supraspinatus could be safely mobilized up to 3 cm laterally,
formal lateral advancement of the supraspinatus muscle is not widely
performed.
The transfer uses a healthy and strong muscle to restore external
rotation and head depression forces that are lost in chronic massive
rotator cuff tears. Gerber found that the
results
of latissimus dorsi transfer for massive rotator cuff tear were better
if the subscapularis tendon was intact. Iannotti et al. report that
patients with better preoperative elevation and external rotator
function have better results. Miniaci and MacLeod reported 82%
satisfactory results after latissimus dorsi transfer in patients with
previously failed operative treatment of massive rotator cuff repair.
Other reports have not been as favorable. The results of primary
latissimus dorsi transfer appear to be superior to the results of
salvage for failed rotator cuff repair.
are infrequently reported. These include teres minor transfer, deltoid
muscular flap transfer, and trapezius transfer. Although all of these
procedures attempt to substitute for the absence of supraspinatus
function, they do not address or restore the balance between the
anterior and posterior force couples of the rotator cuff.
synthetics, autologous and autogenous tissue grafts, and xenograft
material has been attempted. The results have been limited, and these
techniques are not broadly used. Neviaser et al. reported >80% good
and excellent results when they used freeze-dried rotator cuff to
repair chronic massive rotator cuff tears. Aside from the potential for
foreign body reaction to synthetics or tissue rejection, these
techniques do not replace the atrophic and weakened rotator cuff
muscles that are typically present with chronic massive rotator cuff
tears. Recently, several biologic tissue implants, including xenograft
tissue, have been developed to augment rotator cuff repairs. The effect
of these implants on outcome is unclear. Despite promising findings in
animal rotator cuff repair models, concerns remain about tissue
compatibility. Early human clinical studies have not reproduced the
same successful findings. Inflammatory reactions after small intestinal
submucosal tissue augmentation were recently reported and may be owing
to retained cells and DNA.
procedure. Arthrodesis can be performed for painful chronic massive
irreparable rotator cuff tears if the goal is a strong, stable shoulder
girdle. This may be appropriate for the painful shoulder with anterior
superior dislocation because of loss of the coracoacromial arch.
However, rotator cuff reconstruction is preferred if the articular
surfaces are intact. Otherwise, shoulder arthrodesis may actually
result in undesirable loss of upper extremity function below the chest
level. Arthrodesis is also difficult to achieve in the typical
osteopenic elderly patient who presents with chronic massive rotator
cuff tearing. Arntz et al. reported that the results of humeral head
replacement for rotator cuff tear arthropathy were better than
arthrodesis.
shoulder pain and dysfunction. Several treatment options are
appropriate in different clinical settings. Consequently, careful
patient evaluation and treatment selection are critically important.
Many patients with chronic massive rotator cuff tears can be treated
nonoperatively. The goals of surgical treatment must be considered in
the context of the individual patient and the complexity of the
procedure itself as well as the postoperative recovery and
rehabilitation. In some cases, a complete primary repair is possible
whereas in others only a partial repair can be achieved. Reconstruction
of the rotator cuff is most appropriate for younger, more active
patients for whom functional restoration is important. Latissimus dorsi
transfer is the preferred reconstructive option for active individuals
who are disabled by shoulder pain and weakness of elevation and
external rotation and have good deltoid strength. Most of the other
reconstructive options have more limited indications and have not been
conclusively shown to be superior to debridement procedures. Older,
inactive patients, especially those with significant medical
comorbidities, are better served by less complicated management
approaches that provide pain relief.
JM III, Atkinson TS, Mallon WJ. Combined pectoralis major and
latissimus dorsi tendon transfer for massive rotator cuff deficiency. J Shoulder Elbow Surg. 2004;13:621–629.
J, Paavolainen P, Ahovuo J, et al. Surgical repair of the rotator cuff
and surrounding tissues: factors influencing the results. Clin Orthop. 1988;236:148–153.
MP, Tung G, Green A. Overutilization of shoulder magnetic resonance
imaging as a diagnostic screening tool in patients with chronic
shoulder pain. J Shoulder Elbow Surg. 2005;14:233–237.
J, Patte D, Elmelik E. Repair of ruptures of the rotator cuff of the
shoulder with a note on advancement of the supraspinatus muscle. J Bone Joint Surg. 1965;47-B:36–42.
JM Jr, Chase JM, Rushton SA, et al. Tuberoplasty: creation of an
acromiohumeral articulation—a treatment option for massive, irreparable
rotator cuff tears. J Shoulder Elbow Surg. 2002;11:136–142.
LM, Ball CM, Teefey SA, et al. The outcome and repair integrity of
completely arthroscopically repaired large and massive rotator cuff
tears. J Bone Joint Surg. 2004;86A:219–224.
D, Postel JM, Bernageau J, et al. Fatty muscle degeneration in cuff
ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78–83.
D, Postel JM, Gleyze P, et al. Influence of cuff muscle fatty
degeneration on anatomic and functional outcomes after simple suture of
full-thickness tears. J Shoulder Elbow Surg. 2003;12:550–554.
DT, Mack LA, Wang KY, et al. Repairs of the rotator cuff: correlation
of functional results with integrity of the cuff. J Bone Joint Surg. 1991;73-A:982–989.
JP, Ciccone J, Buss DD, et al. Accuracy of office-based ultrasonography
of the shoulder for the diagnosis of rotator cuff tears. J Bone Joint Surg. 2005;87-A:1305–1311.
JP, Hennigan S, Herzog R, et al. Latissimus dorsi tendon transfer for
irreparable posterosuperior rotator cuff tears. Factors affecting
outcome. J Bone Joint Surg Am. 2006;88:342–348.
JP, Zlatkin MD, Esterhai JL, et al. Magnetic resonance imaging of the
shoulder: sensitivity, specificity, and predictive value. J Bone Joint Surg. 1991;73-A:17–29.
S, Bishop J, Lin J, et al. Prospective evaluation of the effect of
rotator cuff integrity on the outcome of open rotator cuff repairs. Am J Sports Med. 2004;32:1716–1722.
HM, Steckel H, Ernstberger T, et al. Arthroscopic debridement of
massive rotator cuff tears: negative prognostic factors. Arch Orthop Trauma Surg. 2005;125(4):261–266.
HL, Bonar F, Murrell GA. Early inflammatory reaction after rotator cuff
repair with a porcine small intestine submucosal implant: a report of 4
cases. Am J Sports Med. 2005;33:907–911.
A, MacLeod M. Transfer of the latissimus dorsi muscle after failed
repair of a massive tear of the rotator cuff: a two to five-year
review. J Bone Joint Surg. 1999;81-A:1120–1127.
JS, Neviaser RJ, Neviaser TJ. The repair of chronic massive ruptures of
the rotator cuff of the shoulder by use of a freeze dried rotator cuff.
J Bone Joint Surg. 1978;60-A:681–684.
HB, Yokota A, Gill HS, et al. Diagnostic accuracy of clinical tests for
the different degrees of subacromial impingement syndrome. J Bone Joint Surg Am. 2005;87:1446–1455.
AS, Cuomo F, Gallagher MA, et al. Long-term functional outcome of
repair of large and massive chronic tears of the rotator cuff. J Bone Joint Surg. 1999;81-A:991–997.
SG, Tibone JE, Itamura JM, et al. Six-month magnetic resonance imaging
follow-up of large and massive rotator cuff repairs reinforced with
porcine small intestinal submucosa. J Shoulder Elbow Surg. 2004;13:538–541.
SA, Hasan SA, Middleton WD, et al. Ultrasonography of the rotator cuff.
A comparison of ultrasonographic and arthroscopic findings in one
hundred consecutive cases. J Bone Joint Surg. 2000;82-A:498–504.
G, Edwards TB, Boulahia A, et al. Arthroscopic tenotomy of the long
head of the biceps in the treatment of rotator cuff tears: clinical and
radiographic results of 307 cases. J Shoulder Elbow Surg. 2005;14(3):238–246.
JJ, Parsons IM IV. Latissimus dorsi tendon transfer: a comparative
analysis of primary and salvage reconstruction of massive, irreparable
rotator cuff tears. J Shoulder Elbow Surg. 2001;10:514–521.
JJP, Krushell RJ, Masquelet A, et al. Anatomy and relationships of the
suprascapular nerve: anatomical constraints to mobilization of the
supraspinatus and infraspinatus muscles in the management of massive
rotator cuff tears. J Bone Joint Surg. 1992;74-A: 36–45.
MH, Chen J, Kirilak Y, et al. Porcine small intestine submucosa (SIS)
is not an acellular collagenous matrix and contains porcine DNA:
possible implications in human implantation. J Biomed Mater Res B Appl Biomater. 2005;73(1):61–67.
JE, Levy HJ, Lemak LJ. Arthroscopic subacromial decompression in the
treatment of full thickness rotator cuff tears: a 3 to 6 year
follow-up. Arthroscopy. 1994;10:518–523.
