PEDIATRIC APPLICATIONS OF CIRCULAR AND UNILATERAL EXTERNAL FIXATION
IX – PEDIATRIC DISORDERS > CHAPTER 171 – PEDIATRIC APPLICATIONS OF
CIRCULAR AND UNILATERAL EXTERNAL FIXATION
increasing acceptance as a surgical technique in children. The most
common applications include incidences of trauma, correction of limb
deformity, and limb-length equalization.
categories: circular fixators and cantilever external fixators.
Biomechanical studies have demonstrated that bone formation is enhanced
by cyclic axial micromotion and, perhaps, by limited-bending
micromotion (23). Torsion, on the other hand,
is generally deleterious to bone formation. The Ilizarov-type of
circular external fixator, which is less stable to axial loading than
are most cantilever systems but relatively resistant to torsion,
provides an excellent biomechanical environment for bone formation (42).
it is applicable to patients of virtually any size from toddler to
large child, obese adolescent, or adult. The system provides
three-dimensional adjustability, allowing angulation, translation,
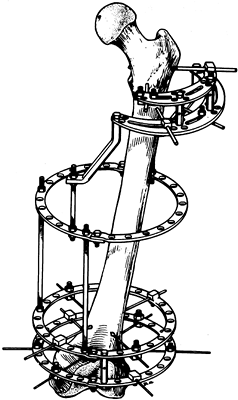
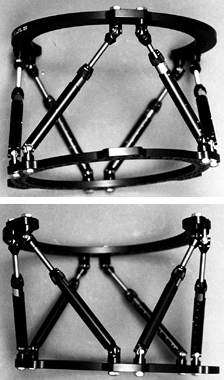
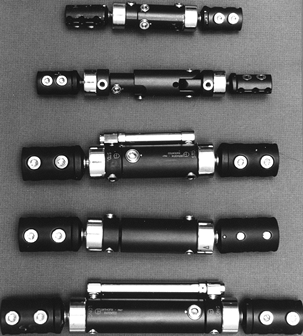
rotation, and lengthening when necessary. The Taylor Spatial Frame (5) now allows these parameters to be corrected simultaneously but currently has some ring-size limitations (Fig. 171.1). The traditional Ilizarov external fixator can be constructed with hinges to correct existing limb deformity (Fig. 171.2).
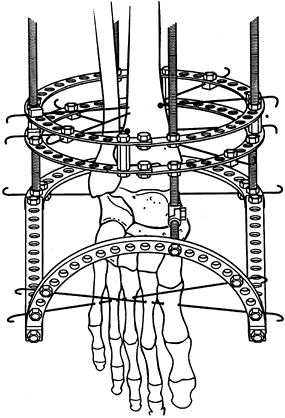
Circular external fixation can be used to span adjacent limb segments,
to protect potentially unstable joints, or to treat joint contractures (Fig. 171.3).
 |
|
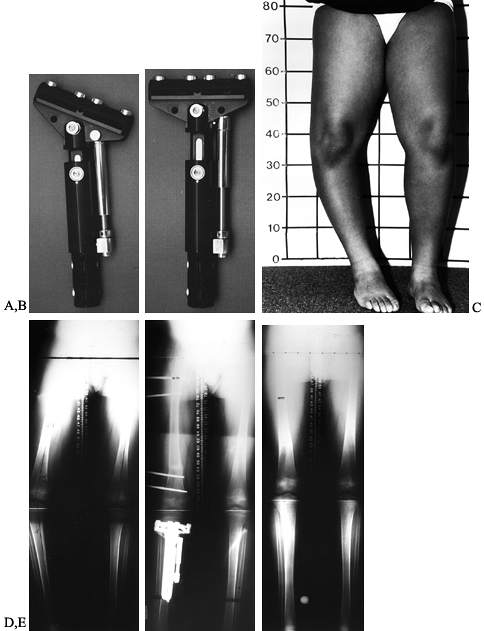
Figure 171.1.
The Taylor Spatial frame allows simultaneous correction of angulation, rotation, length, and translation through the use of six struts and universal ball joints. |
 |
|
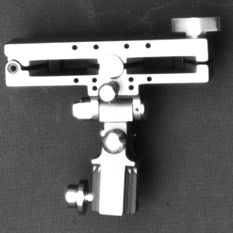
Figure 171.2.
Preconstructed Ilizarov tibial fixator mimics the deformity and allows gradual correction through hinges placed at the level of the deformity. |
 |
|
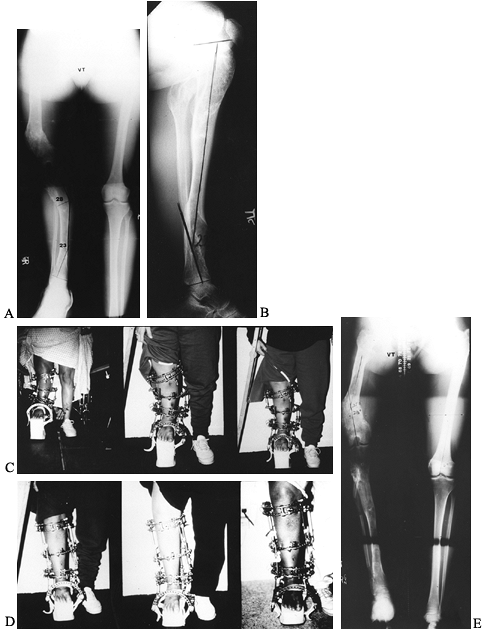
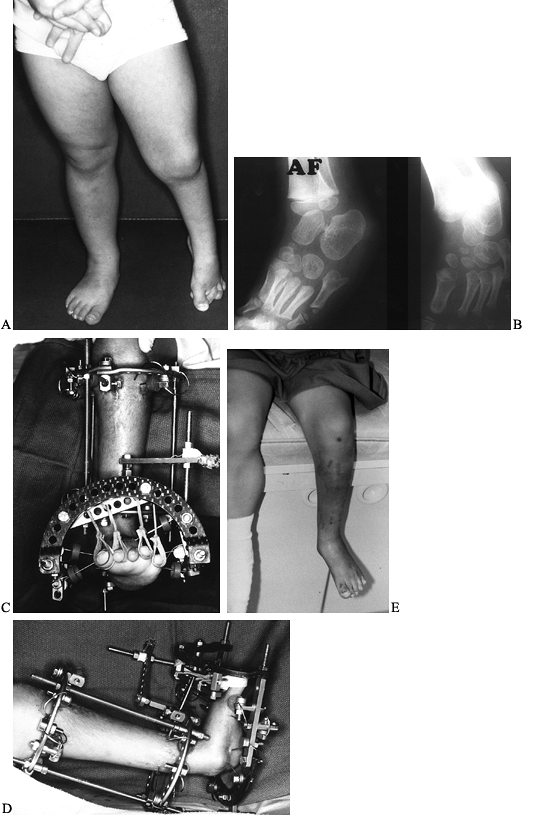
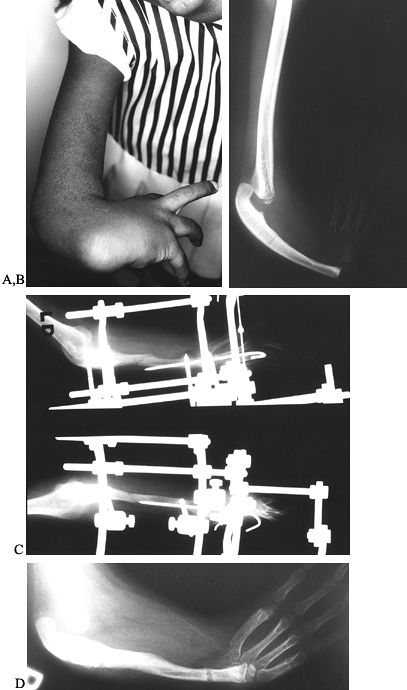
Figure 171.3. A: Preoperative photograph of a 3-year-old patient with arthrogryposis and a nearly 90° flexion deformity of the knee. B: Appearance of Ilizarov fixator affixed to the femur and tibia, spanning the knee joint with corrective hinges.
|
fixator are its bulk, the fact that it is difficult to apply and
adjust, and that it requires multiple sites for transfixing wires. The
traditional Ilizarov external fixator uses 1.5 or 1.8 mm transfixing
tensioned wires for bone fixation, with half-pin fixation in the
proximal femur. Over the last 5 to
6
years, a number of surgeons have modified the originally described
techniques, substituting half-pins for some of the wires. Specifically,
in children, the traditional “medial face” tibial wire (parallel to the
medial face of the tibia) has been eliminated in favor of an
anteroposteriorly directed half-pin. Affixing half-pins to a circular
fixator permits 360° adjustability at the same time it avoids some of
the soft-tissue problems of transfixing wires.
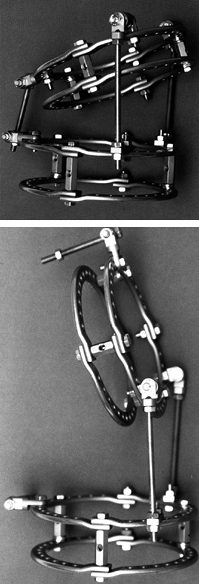
They are applied to only one side of the limb and require usually no
more than four to six half-pins per limb segment depending on the type
of application. Cantilever systems have some disadvantages. They can be
used only on limbs of a certain size, they have less stability to shear
stress than circular fixators, they cannot span joints easily, and
their ability to correct angulation, rotation, and translation
gradually is limited. With many current systems, significant
adjustments such as device and pin clamp exchange must be made under
general anesthesia. Some systems, including the Heidelberg (5), Orthofix (5), and EBI (5) systems, have gradual but limited correction capabilities.
America for trauma or limb reconstruction applications, including the
Orthofix device (Orthofix, Winston-Salem, NC), EBI Dynafix (EBI Corp.,
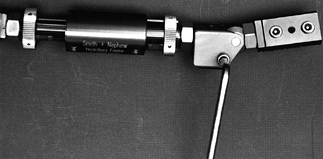
Parsippany, NJ), Smith and Nephew Heidelberg fixator (Smith and Nephew,
Memphis, TN), the Hex-Fix (Smith and Nephew, Memphis, TN), and the
Synthes External Fixator (Synthes USA, Philadelphia, PA). In each case,
application requires pin clamps or pin clamp templates through which
half-pins are inserted. The choice of fixator is usually determined by
the problem to be addressed and size of the patient. The most commonly
used limb reconstruction systems are the Orthofix and EBI, with the
Heidelberg system having been recently introduced. These fixators are
lightweight devices with the ability to telescope. The technique for
insertion of the half-pins, and application of these types of fixators
is discussed in detail in Chapter 11 and specifically for the tibia in Chapter 24.
The short or standard length devices are used most often on children.
Orthofix has two articulating ball joints and uses tapered predrilled
half-pin fixation. The telescoping body can be unlocked once fracture
or osteotomy callus formation is evident radiographically. This
capacity theoretically allows axial loading or dynamization of the bone
facilitating callus formation and bone healing. The standard
articulated device is used for fracture management and osteotomies (16,35,40,50,53). Its ball-and-joint articulation permits approximately 30° to 35° of angulation; it can be freely rotated.
 |
|
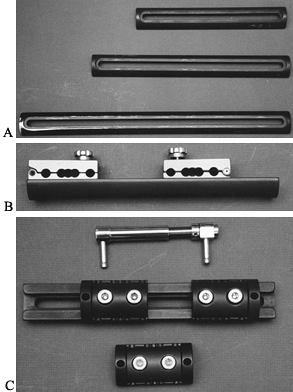
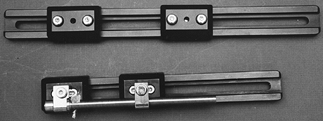
Figure 171.4. Several lengths of the Orthofix pediatric (top two) and adult (bottom 3) fixators are available.
|
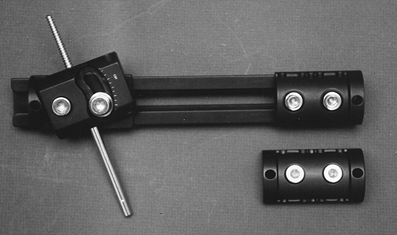
can be substituted for straight clamps at one or both ends of the bone (Fig. 171.6);
this technique may be useful for bifocal osteotomies with acute
deformity correction or to eliminate deformity that may develop during
lengthening. A variety of angulation and rotation template clamps are
now available for more accurate multiplanar corrections (Fig. 171.7). Do not use the standard swivel clamps for lengthening; they are less stable than the standard pin
clamps. With either the standard articulated body fixator or LRS,
insert tapered predrilled half-pins through the clamp templates. Then
replace the template with the standard pin clamps and tighten them. For
fractures and osteotomies, generally two half-pins above and below the
fracture or osteotomy are adequate. The widest pin spread in the clamp
provides the best stability. For limb lengthening, use three pins
proximal to the lengthening site in the femur and tibia. Two or three
are adequate distally, depending on the size of the patient and amount
of anticipated lengthening (Fig. 171.8) (1,22,25,46,47,48).
 |
|
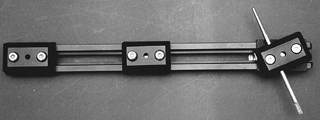
Figure 171.5. A: Orthofix LRS slide lengtheners are available in various lengths, as well as pediatric and adult sizes for limb lengthening. B: Template clamps are placed directly on the lengthening device for parallel pin placement. C: LRS system with pin clamps in place and distraction device above the fixator.
|
 |
|
Figure 171.6. Swivel template clamps and swivel pin clamps are available for angular correction.
|
 |
|
Figure 171.7. A and B: A new rotation template clamp is now available to allow accurate planning and pin insertion for acute rotational corrections. C:
The new angulation template clamp can be affixed to the end of the slide for planned acute angular correction 90° orthogonal to the plane of the swivel clamp. |
 |
|
Figure 171.8. A:
Clinical appearance of a patient with Ollier’s disease after tibial lengthening with residual varus deformity of the femur and shortening. B: AP and lateral radiographs following application of LRS system and acute correction of femoral deformity. C to E: Clinical and radiographic appearance at the conclusion of lengthening and bone consolidation. |
correction of frontal plane deformity in the tibia—for example, in
adolescent Blount’s disease (Fig. 171.9) (59).
Small lengthenings can also be achieved with this device. A new
template clamp allows correction of acute sagittal plane deformity
before application of the device following osteotomy (Fig. 171.10).
It is not recommended for large lengthenings; the hinge may not
withstand large lengthening forces, and the device, for the most part,
accommodates only two proximal tibial pins (Fig. 171.11).
 |
|
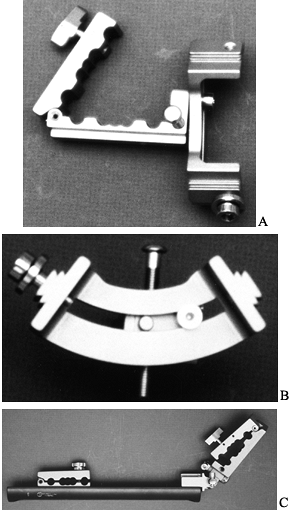
Figure 171.9. A and B: The T-Garches external fixator is ideal for correction of proximal tibial frontal plane deformity. C and D:
Clinical and radiographic appearance of a 12-year-old boy with adolescent Blount’s disease and varus deformity of both the tibia and the femur. E: Radiographic appearance following osteotomy of the femur and tibia, and application of an Orthofix external fixator to the femur and T-Garches external fixator to the tibia. F: Radiograph following fixator removal with restoration of normal limb mechanical axis. |
 |
|
Figure 171.10.
The new T-Garches template clamp allows accurate pin placement for simultaneous sagittal and frontal plane deformity correction. |
 |
|
Figure 171.11.
Only two pins can be placed in the proximal T-Garches fixator. This potentially limits its use, particularly for significant lengthenings. |
and the T-Garches, it is important to note the length of the device and
the pin spread for the particular application. Be certain, for example,
in a limb lengthening, that the device is long enough. At least 10%
extra length is needed for the tibia and 20% for the femur. The
bone-to-fixator distance is relatively large, particularly in the
femur. Thus, there is not always a 1:1 ratio between the amount of
lengthening the device can achieve (ie, number of turns) and the actual
distraction achieved in the limb. Start with some extra length in the
device to avoid running out of space.
-
In the case of fracture reduction or
osteotomy, anticipate whether the device will need to be lengthened or
shortened to achieve the correct bone position before determining pin
placement. Add a supplemental pin to the fixator body if necessary for
segmental fracture stabilization. -
Once pins are in place, remove the
template. Obtain provisional reduction of a fracture or positioning of
the bone ends following osteotomy before applying the fixator. -
Apply the fixator and tighten the pin
clamps. Attach the reduction forceps to the clamps and fine-tune the
bone position under image intensifier control.
the Dynafix (manufactured by EBI Medical Systems) is that the Dynafix
itself is used as its own template. Tissue protectors and drill guides
are placed directly through the pin clamps. The Dynafix articulated
body fixator has mobile joints that allow angulation in the frontal and
sagittal
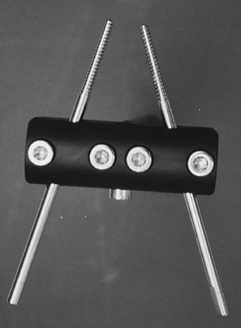
plane and rotation through the center of the fixator (Fig. 171.12).
The snakelike configuration of the device and the multiple fixator body
joints permit translation and rotational corrections as well as
approximately 30° of angulation at each joint. As with the standard
Orthofix unit, these corrections need to be completed during surgery.
 |
|
Figure 171.12. The EBI Dynafix external fixator allows angulation, translation, and rotation through its “snake-like” configuration.
|
-
With the articulated body fixator, always
secure the ball joints with methylmethacrylate to avoid slippage during
weight bearing, which can lead to loss of position in fractures or
after osteotomy. -
Small articulated fixators are available for specialized application in the pediatric forearm, humerus, and tibia (5).
-
In general, an adult-size fixator is
recommended for the femur of all except the smallest children (those
weighing less than 50 to 60 lb); it can also be applied to the tibia in
older children. -
Use the larger 6.0 to 5.0 mm tapered pins
when possible except in the forearm or in bones smaller than 15 mm in
diameter. Two pin sizes are available for small bones.
Both systems use pins with an external shaft diameter of 6.0 mm. The
pin clamp spacing and configuration are different between the two
devices; thus, it is impossible to exchange devices without changing
pin locations.
 |
|
Figure 171.13. The EBI lengthening system is similar to the Orthofix LRS system.
|
 |
|
Figure 171.14. Swivel clamps are available for the Dynafix lengthening system.
|
Because the pin clamps are applied to the T portion of the device, more
than two pins can be inserted if desired. The pins may also be applied
either proximal or distal to the T allowing some longitudinal spread of
the proximal metaphyseal pins.
 |
|
Figure 171.15. Like the T-Garches, the EBI T-fixator allows gradual angular correction in the proximal tibia and lengthening.
|
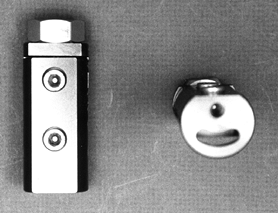
fixator, designed by Dr. Joachin Pfeil, has recently been introduced to
North America (Fig. 171.16). This device is yet
another cantilever system. Its proposed benefit, however, is the
ability to achieve gradual angular correction through a device called
the angulator (Fig. 171.17). Pins are inserted through a drill guide template (Fig. 171-18), which can be applied to the fixator in any plane and allows correction of oblique plane deformity or correction of deformity
that may arise during limb lengthening such as procurvatum and valgus
in the tibia. The surgeon can also apply supplemental bone screws when
necessary to enhance stability. A special clamp is also available to
allow fixation to the Ilizarov ring system (Fig. 171.19).
Experience thus far in North America is limited, but the device has
some potentially significant advantages, particularly when gradual
deformity correction is desirable. Translational correction must
nonetheless be obtained intraoperatively.
 |
|
Figure 171.16.
The Heidelberg fixator has been recently introduced to North America. Similar to other systems, it has several pin clamp types. Lengthening occurs through the body of the fixator itself. |
 |
|
Figure 171.17. The Heidelberg “angulator” allows gradual deformity correction following lengthening.
|
 |
|
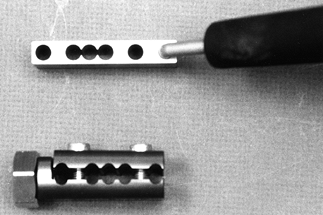
Figure 171.18. Pins are introduced through a hand-held template that matches the pin clamp.
|
 |
|
Figure 171.19. A special Heidelberg clamp allows fixator attachment to the Ilizarov ring system.
|
fractures definitively and in osteotomies in small children or children
with particularly small bones, as in the skeletal dysplasias. I prefer
to use it for proximal femoral fractures or fractures in very small
children (those younger than 4 to 5 years of age) in whom stable
fracture fixation is desired. The device can accommodate predrilled or
self-drilling (eg, Schanz) half-pins of 4, 5, or 6 mm. There are
several types of pin clamps available that accommodate one or two bone
pins (Fig. 171.20). The single pin clamps
permit flexible pin spacing. The clamps also allow some angulation and
rotation, enabling multiplanar half-pin fixation on a cantilever device.
 |
|
Figure 171.20.
The Hex-Fix is particularly useful for fracture fixation in small children. Four, five, or six millimeter pins may be introduced through the pin clamps, which act as their own template. They are available as single or double clamps as shown. Pins and pin clamps are secured using the universal tool. |
the fracture or osteotomy; pin spacing is dependent on the individual
situation. There is no limit to the number of pins that can be used
other than the ability to put the pin clamps on the bar. The actual bar
on which the pin clamps are assembled is available in several lengths,
the shortest being 8 inches. Although a distractor unit is available
for lengthening, I have no experience using this device for limb
lengthening.
Ilizarov apparatus. This device is applicable to all limb segments in
both the upper and the lower extremities and can be used for deformity
correction of both bone and soft tissue, and for limb lengthening (3,5,6,7,8,9,10,11 and 12,15,17,19,20 and 21,24,27,29,30 and 31,32,38 and 39,41,42,43,44 and 45,51,56,57 and 58,61,62 and 63).
Acute trauma applications in the child are limited. It is used most
commonly for segmental bone loss, in which it can be used for bone
transport (11).
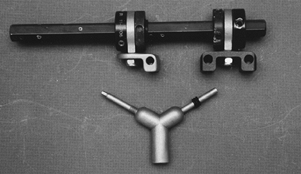
commonly to the femur or the tibia. The standard tibial fixator
consists of one or two rings proximally and distally depending on the
size of the patient. The standard tibial wire “formula” calls for the
insertion of four wires proximally and distally (Fig. 171.21) (26).
These wires are either 1.5 or 1.8 mm in diameter. Use 1.5 mm wires in
the tibia of smaller children, and 1.8 mm wires in the femur and the
tibia of heavier children. At each end of the bone, place two “olive”
wires and two smooth wires. Generally, place the olive wires
transversely in the frontal plane, one olive from the medial and one
from the lateral aspect of the bone. Transfix the fibula and tibia with
a smooth wire, both proximally and distally. Finally, place two wires
from
anterolateral to posterolateral (one proximal and one distal), parallel
to the medial border of the tibia. When bifocal—proximal and distal
tibial osteotomies—are planned, use another ring fixed to the
mid-diaphysis by two wires (Fig. 171.22).
These wires are often two olive wires, or an olive wire and plain wire,
depending on the direction or nature of the deformity.
 |
|
Figure 171.21. A and B: Transverse “Olive” wires are first placed on the most proximal and distal rings. C and D: Two additional olive wires are placed from the opposite direction on the two middle rings. E and F:
Smooth wires are placed from the lateral aspect of the leg, parallel to the medial face of the tibia both proximally and distally. G and H: Two smooth wires are placed through the proximal and distal fibula, transfixing the tibia. |
 |
|
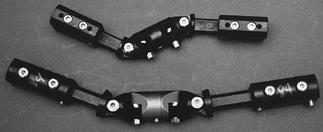
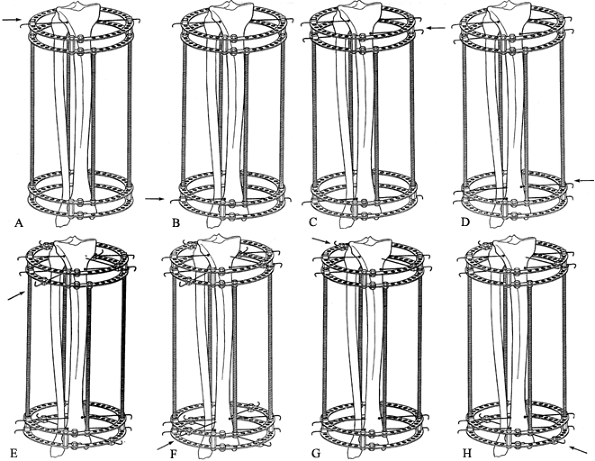
Figure 171.22. Bifocal treatment for deformity or lengthening requires an additional middle ring with two-wire or wire and half-pin fixation.
|
“formula” in recent years, generally the substitution of half-pins for
wires (discussed in Chapter 32).
fixator. Because the standard medial face tibial wire can often
interfere with the pes anserinus tendons, I substitute a half-pin for
this wire, leaving the remaining wires as described earlier (Fig. 171.23).
In the tibia, the addition of an extra ring in the diaphysis allows
bifocal treatment. It is useful for patients with deformities at more
than one level (Fig. 171.24), when extensive lengthening is necessary, and in bone transport (Fig. 171.25).
 |
|
Figure 171.23. A half-pin is often substituted for the traditional Ilizarov medial face wire and affixed to a Rancho cube.
|
 |
|
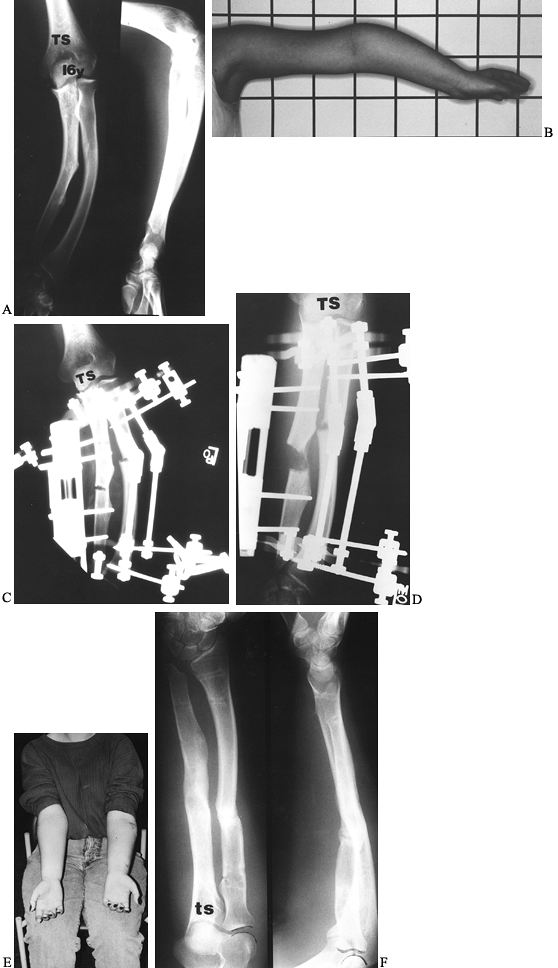
Figure 171.24. A and B:
Standing and lateral teleoroentgenograms of a patient with Ollier’s disease and a 13 cm limb-length inequality with bifocal tibial deformity. C and D: The Ilizarov external fixator with bifocal application was used for gradual correction of the proximal and distal deformities as well as 8 cm of lengthening. E: Radiographs at the conclusion of tibial consolidation. |
 |
|
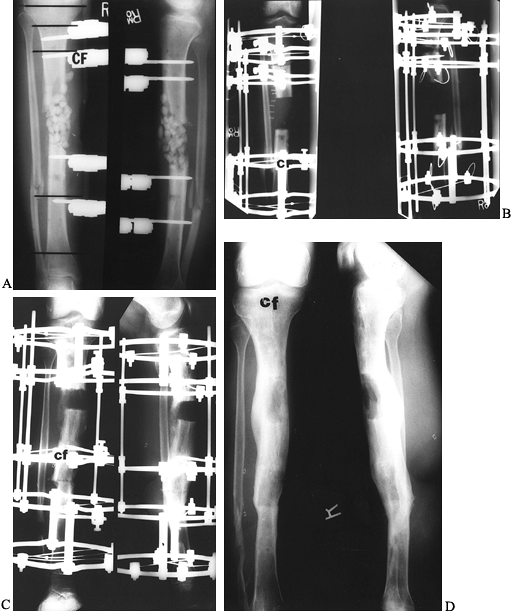
Figure 171.25.
Tibial radiographs of a 16-year-old boy who presented following a pedestrian motor vehicle accident with 6 cm of missing bone. Antibiotic cement beads were used as a spacer, and external fixation was applied using a Synthes external fixator. B: The Ilizarov apparatus was applied over the Synthes fixator, which was then removed. A proximal osteotomy was performed and bone transport was initiated to restore the defect. C: Radiographs at the conclusion of bone transport. D: Radiographs following fixator removal. |
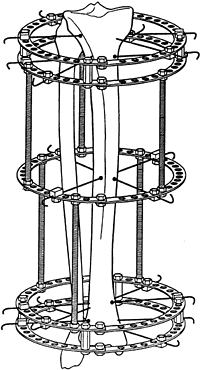
using partial rings proximally, as compared with the original Russian
technique, which uses full rings for both the proximal and distal
thigh. My technique is as follows.
-
Generally, I use four wires distally—two 1.8 mm olive wires and two plain wires fixed to one or two rings (Fig. 171.26).
![]() Figure 171.26.
Figure 171.26.
Schematic drawing of the Italian modification of standard Ilizarov
fixation of the femur. Note that proximal fixation is achieved using
half-pins. An empty middle ring is used to facilitate angular or
rotation correction as well as lengthening. Distal fixation is
traditional through four 1.8 mm transfixing wires. -
Connect these rings to an empty diaphyseal ring via lengthening rods or hinges depending on the application.
-
Achieve proximal fixation by half-pin,
rather than by wire fixation. Determine the diameter of the half-pin by
the size of the child. -
Connect the distal rings to the proximal thigh fixation through oblique supports.
-
Attach the proximal half-pins to one or two “arches,” depending on the size of the patient.
-
Introduce wires or half-pins on the
diaphyseal ring for bifocal application to the femur. Although bifocal
lengthening is not recommended, proximal angular or rotational
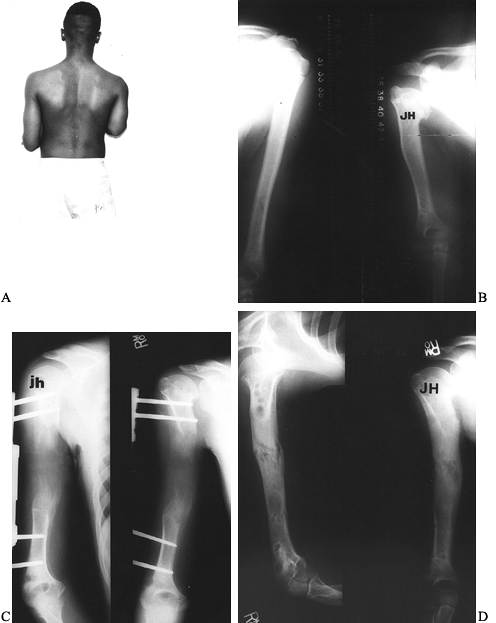
osteotomy can be performed acutely (Fig. 171.27), combined with distal deformity correction and lengthening.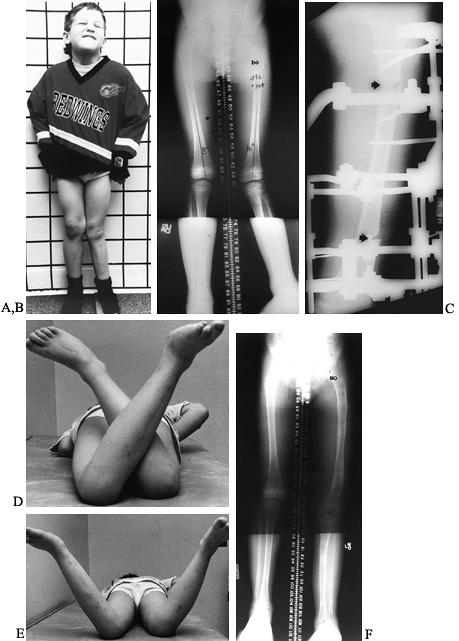 Figure 171.27. A and B:
Figure 171.27. A and B:
Preoperative photographs and teleoroentgenogram of a 6-year-old boy
with congenital shortening of the femur, fibular hemimelia, and a
three-ray foot. C: The Ilizarov technique
was used for bifocal application. Acute rotational correction was
performed proximally. Elimination of distal femoral valgus and
subsequent lengthening was done distally. D and E: The photographs demonstrate symmetric internal and external rotation at the conclusion of treatment. F: Radiographs demonstrate excellent healing of both femoral and tibial lengthening sites.
of the fixator. During lengthening, adjacent joints are at risk for
progressive contracture, subluxation, or dislocation. The risk of
dislocation is particularly significant in the case of congenitally
short limbs, such as the ankles associated with fibular hemimelia,
knees or hips in the congenital short femur, and proximal femoral focal
deficiency (PFFD). Pre-existing contracture due to trauma, burn, or
infection may warrant use of circular fixation for gradual correction
of deformity with combined femoral and tibial lengthening. Consider
prophylactic incorporation of the foot or tibia in tibial or femoral
lengthening, respectively, at the beginning or if there is any
indication of subluxation or progressive contracture as lengthening
proceeds. Consider extending the fixator to the pelvis when the hip is
at risk for subluxation (Fig. 171.28). I
recommend fixation of the foot at the initial surgery in any patient
undergoing tibial lengthening who has fibular hemimelia or a
pre-existing equinus contracture. Comprehensive release of the foot can
be maintained with foot fixation and combined with tibial lengthening (Fig. 171.29).
 |
|
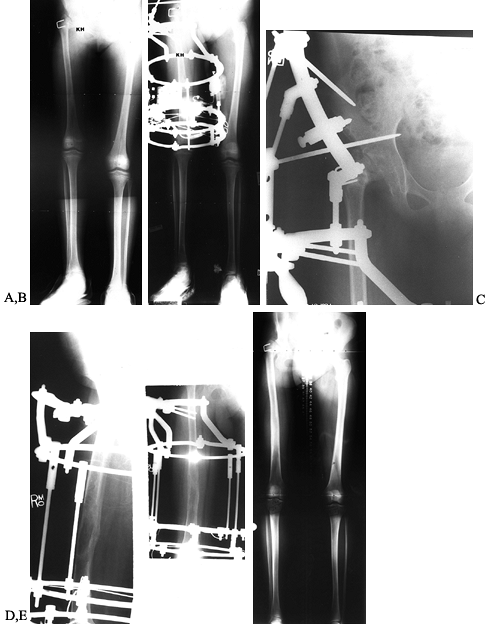
Figure 171.28. A:
Radiographs of an 11-year-old girl with a painless fibrous pseudarthrosis of her right hip and a projected limb length inequality of 9 cm. B and C: Radiographs demonstrate Ilizarov fixation of the femur with extension of the fixation to the pelvis to protect the potentially unstable hip. D and E: Radiographs at the conclusion of lengthening demonstrate excellent consolidation of the bone and no disruption of the hip joint. |
 |
|
Figure 171.29. A and B:
Clinical appearance and radiographs of a 2 1/2-year-old girl with hemisacral agenesis, recurrent club foot deformity, and a leg-length inequality. C and D: An open soft-tissue release of the foot was combined with gradual correction of residual foot deformity and tibial lengthening using the Ilizarov technique. E: Clinical appearance at the end of treatment. |
-
Try to use two metatarsal olive wires and two calcaneal olive wires.
-
In the forefoot, introduce the medially
based olive wire through the first and second metatarsals and the
lateral wire through the two lateral metatarsals. Fix them to an arch,
tensioned no more than 50 to 80 kg. Place the wires in this fashion to
avoid flattening the forefoot arch and preclude weight bearing on wires. -
Introduce one calcaneal wire from the medial side and one from the lateral side, usually diverging no more than 45° (Fig. 171.30).
![]() Figure 171.30.
Figure 171.30.
A variety of options are available for foot fixation using the Ilizarov
technique. I prefer hindfoot fixation through the calcaneus using
opposing olive wires and forefoot fixation, with the lateral olive wire
transfixing the two lateral metatarsals and the medial Olive wire
transfixing the two medial metatarsals. -
Fixation of both the hindfoot and
forefoot avoids midfoot deformity and forefoot equinus, which can
result from tension on the long toe flexors during lengthening. -
Once the distraction phase has been
completed, remove the foot fixation, allowing the ankle and foot to
regain motion while the tibial lengthening site consolidates. If
prophylactic circular fixation has been applied to the tibia during
femoral lengthening, remove it once femoral
P.4374P.4375P.4376
distraction has been completed as long as there is no significant concurrent contracture of the hip.
-
Perform osteotomy of long bones for
deformity correction or lengthening through a 1 to 1.5 cm incision,
with minimal periosteal stripping generally using a sharp, thin ¼-inch
osteotome. -
Predrill the bone with a 2.7 mm or 3.2 mm
drill to avoid crack propagation from the osteotomy into the adjacent
half-pins, which could considerably weaken fixation. -
Avoid large incisions with subperiosteal
exposure of the bone and insertion of retractors to minimize scarring
and promote bone healing. -
There is no need to make a true
“corticotomy” as described by Ilizarov, because the periosteal blood
supply is more critical than the endosteal supply. Furthermore, the
endosteal blood supply usually re-establishes itself within a matter of
days following osteotomy.
osteotomy and distraction. The choice of method depends on the child’s
age and whether the deformity is bony alone or combined with
soft-tissue contractures. Ilizarov originally described correction of
all soft-tissue deformity through closed distraction or “bloodless”
surgery (28,32). This
situation may present itself in the child younger than 4 to 5 years old
with a multiply operated club foot in poor position. In my experience,
an attempt at correction by closed distraction alone may be
unacceptably painful and, owing to the scar stiffness, may result in
wire cut-out thorough osteopenic bone. In this situation, perform a
conventional comprehensive release first, followed by fixation of the
foot and tibia with appropriate hinge placement and subsequent gradual
correction (Fig. 171.31). This surgery avoids the problem of wire migration.
 |
|
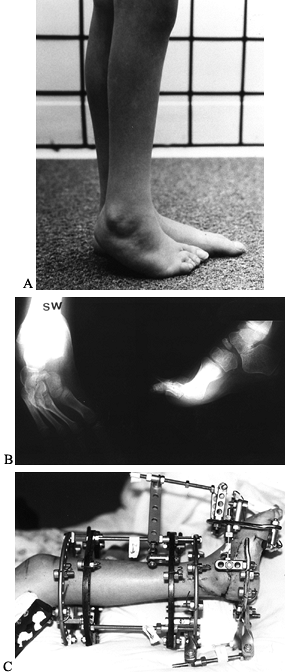
Figure 171.31. A and B:
Clinical and radiographic appearance of a girl with fibular hemimelia and a four-ray equinovarus foot following two previous attempts to correct her foot deformity. C: Comprehensive foot release was combined with gradual independent correction of the forefoot and hindfoot deformities and tibial lengthening. |
limited by patient discomfort, skin tension, and the tolerance of
neurovascular structures. Slight overcorrection is recommended due to
soft-tissue elasticity which can cause rebound following apparatus
removal. Once correction has been achieved, maintain the fixation an
additional 6 to 8 weeks. Use orthotics after the removal of the fixator
to maintain the correction.
total of four wires, or two wires and two half-pins, are adequate
fixation in the tibia because there is no tibial osteotomy. The number
of wires in the foot and complexity of the apparatus depends entirely
on the nature of the deformity.
The nature of the deformity determines the location of the osteotomy.
If the hindfoot is neutral and the problem is midfoot cavus or
supination, use a midtarsal osteotomy. Hindfoot fixation can be neutral
with respect to the tibial fixation. Place hinges between the hindfoot
and forefoot, centered over the apex of the deformity. A hindfoot that
is not in neutral may be addressed in one of two ways. If cavus exists
with hindfoot deformity, use a V-shaped osteotomy to address the
hindfoot and midfoot independently. Additional fulcrum wires are
necessary, usually in the midfoot and talus to ensure that correction
occurs through the osteotomy and not
through
joint distraction. If the midfoot and forefoot are relatively neutral
with respect to one another and the hindfoot is the problem, use a
crescent-shaped osteotomy. Perform the osteotomy from the lateral side
through the calcaneus and neck of the talus. Place wires superior and
inferior to the osteotomy with appropriate hinge location to avoid translation of the foot during correction.
 |
|
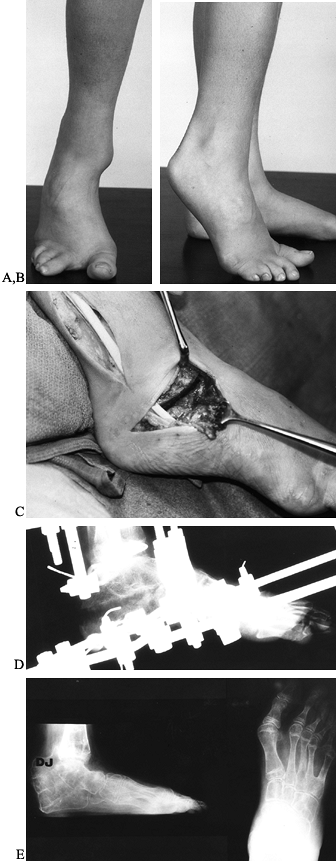
Figure 171.32. A and B: This nearly skeletally mature boy with fibular hemimelia has a fixed deformity of his foot and limb shortening. C:
An open crescentic osteotomy was performed through the talus and calcaneus with resection of the deforming tight fibular anlage. D: Lateral foot radiograph at the conclusion of correction. E: Radiographs following fixator removal. |
infection, and burns. Unfortunately, to date, most surgeons’ long-term
experience has been disappointing. As with conventional soft-tissue and
capsular release, the recurrence rate is high despite prolonged periods
of posttreatment bracing. Furthermore, as with conventional surgery,
depending on the duration of the deformity and the nature of the
articular cartilage, the surgeon’s goal may be limited to reorienting
rather than increasing the arc of motion. The joints most commonly
involved in the pediatric patient are the knee and ankle. The usual
deformities are knee flexion and ankle equinus contractures.
 |
|
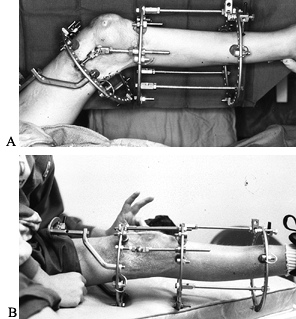
Figure 171.33. A:
A lawnmower accident resulted in a severe flexion deformity of this knee. Open posterior release achieved no improvement in knee position, and the Ilizarov external fixator was applied to the femur and tibia with hinges at the approximate center of rotation of the knee. B: Appearance at the conclusion of correction. |
Apply circular fixation to span the adjacent femur and tibia to provide
an efficient lever arm. Hinges must be located as close to the center
of rotation of the knee joint as possible to avoid joint compression or
subluxation. After obtaining correction, depending on the preoperative
range of motion, use the hinges to assist in moving the knee during
physical therapy. At the ankle, center the hinge placement over the
center of the talar dome to avoid anterior subluxation of the talus in
the ankle mortise.
than circular fixation to the upper extremity. At present, circular
fixation is optimal for complex deformities that cannot be corrected
acutely (Fig. 171.34). It is also useful if the wrist needs to be spanned, for example, in lengthening of radial or ulnar club hand (12,37). Metacarpal wires can be fixed to a half-ring and attached to the forearm fixation (10,12,37,49,64).
 |
|
Figure 171.34. A and B: Clinical and radiographic appearance of 6-year-old girl with a right radial club hand and no history of prior intervention. C:
The ulna was centralized through an open procedure and the wrist stabilized with a transfixing Kirschner wire. Lengthening of forearm was then undertaken. D: The ulna was lengthened by more than 89%. |
fixation of the forearm, and the two methods can be used independently
for deformities such as those associated with multiple hereditary
exostosis (Fig. 171.35). In general, half-pin
fixation is easier and safer to apply to the forearm than transfixing
wires. The fact that the ulna is subcutaneous throughout its length
makes half-pin fixation
attractive.
Half-pins can be attached in a multidirectional fashion to rings if
desired. Two half-pins proximal and distal to the osteotomy site are
enough for deformity correction or lengthening.
 |
|
Figure 171.35. A and B:
Radiographs and clinical appearance of a 16-year-old girl with multiple hereditary exostoses with forearm shortening and deformity. C and D: Circular fixation was applied to the radius around a small Orthofix LRS fixator for gradual correction of radial deformity and ulnar lengthening. E and F: Clinical and radiographic appearance of the forearm at the conclusion of treatment. |
Perform osteotomy distal to the deltoid insertion. Two half-pins
proximal and distal to the osteotomy or lengthening site are adequate
in the arm. Insert the most distal pin just proximal to the olecranon
fossa. The next most proximal pin must avoid the path of the radial
nerve. Place it with open technique.
 |
|
Figure 171.36. A and B:
Clinical appearance and radiographs of 13-year-old boy with 10 cm of right humeral shortening due to septic growth arrest of the proximal humerus at the age of 2 years. C and D: Radiographs at the conclusion of distraction and following consolidation. |
Depending on the size of the limb segment, apply a four-pin fixator
(Hex-Fix, Orthofix, Dynafix) after irrigation and debridement of the
open wound. Locate the fixator to minimize interference with subsequent
wound management such as local or free flaps and skin grafts. In the
case of segmental bone loss, circular fixation can be used to transport
bone for definitive bone reconstruction of bone loss.
concurrent severe closed head injury, is a strong indication for
fixation of major long bone fractures in the pediatric patient. Those
patients who require frequent computed tomography (CT) scans, magnetic
resonance imaging (MRI) studies, or the operations for treatment of
their associated injuries are more easily managed with stable fracture
fixation. Traction or spica casts make this difficult, and spica casts
may interfere with management of abdominal or chest trauma. Patients
who experience spasticity or who are uncooperative following head
injury are best managed with rigid stabilization of their long-bone
fractures. Even in the very young child, small cantilever unilateral
external fixators, such as the Hex-Fix, can be adapted to long-bone
fractures, particularly of the femur and tibia.
fractures using external fixation has become accepted in patients older
than 5 to 6 years of age (14,22,34,35,50,52,55).
Immediate spica treatment is still preferred in small children, and
older adolescents may be treated with intramedullary rodding. Current
literature supports operative treatment of this intermediate age group
between age 5 and 11 to 12 years, reporting excellent results with
external fixation decreasing hospitalization, promoting early patient
mobilization and return to school, decreasing psychosocial family
stress, with an acceptable complication rate (2,4,14,16,34,50,52,53,55). A recent report (18)
also demonstrated a clear cost savings when compared with traditional
skeletal traction followed by spica-cast immobilization. The major
concern when using external fixation in these fractures is the risk of
refracture. The incidence of refracture can be minimized by early
weight bearing, early fixator dynamization, and mobilization of the
knee. Anecdotal reference is made by some to suggest that the most
common fracture pattern susceptible to refracture is a transverse
diaphyseal fracture. In my experience, the most important factors in
refracture are a stiff knee and lack of weight bearing during fracture
healing.
the tibia produces a floating knee. Operative stabilization of both the
tibia and the femur are indicated. Depending on the skeletal maturity
of the patient, intramedullary fixation of the femur, using either
reamed or flexible implants, can be combined with external fixation of
the tibia. In the younger child, external fixation can be applied to
both the femur and the tibia. It allows rapid mobilization of the
patient, motion of the knee and ankle, and normal shoe wear. Weight
bearing can be initiated as soon as patient can tolerate it in most
cases.
pelvic fractures, particularly open-book type fractures of the pelvis,
can be treated with external fixation as in the adult (52). Posterior disruptions can be addressed by internal fixation and combined with an anterior fixator (see Chapter 17). For more details on the treatment of pediatric fractures, see Chapter 164.
scheme. *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
DF, Boyer MI, Armstrong PF. The Use of the Ilizarov Technique in the
Correction of Limb Deformities Associated with Skeletal Dysplasia. J Pediatr Orthop 1992;12:283.
R, Catagni M, Johnson EE. The Treatment of Infected Nonunions and
Segmental Defects of the Tibia by the Methods of Ilizarov. Clin Orthop Rel Res 1992;280:143.
R, Villa A, Catagni MA, Bell DF. Lengthening of the Humerus Using the
Ilizarov Technique. Description of the Method and Report of 43 Cases. Clin Orthop Rel Res 1990;250:117.
CM, Peterson HA. Isolated Closed Diaphyseal Fractures of the Femur in
Children. Comparison of Effectiveness and Cost of Several Treatment
Methods. Orthopaedics 1997;20:1131.
RM, Stanitski DF, Stanitski CL. Treatment Cost of Isolated Femoral
Shaft Fractures in Children. External Fixation Versus Traction.
Submitted to Journal Pediatric Orthopaedics.
C, Pouliquen JC, Langlais J, et al. Femoral Lengthening Using the
Callotasis Method. Study of the Complications in a Series of 70 Cases
in Children and Adolescents. J Pediatr Orthop 1996;16:161.
M, Shinohara Y, Shinada Y. Limb Lengthening and Correction of
Angulation Deformity. Immediate Correction by Using a Unilateral
Fixator. J Pediatr Orthop 1996;16;477.
J, Mukherjee A, Van Eygen P, Fabry B. Forearm Realignment with Elbow
Reconstruction Using the Ilizarov Fixator. A Case Report. J Bone Joint Surg 1991;73B:412.
F, Renzi-Brivio L, deBastiani G. Psychologic, Vascular and Physiologic
Aspects of Lower Limb Lengthening in Achondroplastics. Clin Orthop Rel Res 1990;250:138.
JC, Coelin JD, Langlais J, Pauthier F. Upper Metaphyseal Lengthening of
the Tibia by Callotasis. Forty-seven Cases in Children and Adolescents.
J Pediatr Orthop 1993;2B:49.
JC, Gorodischer S, Vernevet C, Richard L. Femoral Lengthening in
Children and Adolescents. A Comparative Study of a Series of 82 Cases. Fr J Orthop Surg 1989;3:162.
RB. The Use of External Fixation Devices in the Management of Severe
Lower Extremity Trauma and Pelvic Injuries in Children. Clin Orthop Rel Res 1984;188:22.
M, Ebskov LB, Sloth C, Torholm C. External Fixation with the Orthofix
System in Dislocated Fractures of the Lower Extremities in Children. J Pediatr Orthop 1993;2:161.
DF, Srivastava P, Stanitski CL. Correction of Proximal Tibial
Deformities in Adolescents Using the T-Garches External Fixator. J Pediatr Orthop 1998;18:512.
RJ, Bell DF, Armstrong PF, et al. Complications Using the Ilizarov
Technique in the Correction of Limb Deformities in Children. J Bone Joint Surg 1993;75A:1148.
JM, Ginebreda I, Jimeno E. Lengthening of the Lower Limbs and
Correction of Lumbar Hyperlordosis in Achondroplasia. Clin Orthop Rel Res 1990;250:143.
NL, Bell DF, Anthony A. Paediatric Pain Patterns During the Ilizarov
Treatment of Limb Length Discrepancy and Angular Deformity. J Pediatr Orthop 1994;14:352.
NL, Davis RJ, Bell DF, Redmond DM. Electromyographic and Nerve
Conduction Changes after Tibial Lengthening by the Ilizarov Method. J Pediatr Orthop 1993;13:473.