The Neck
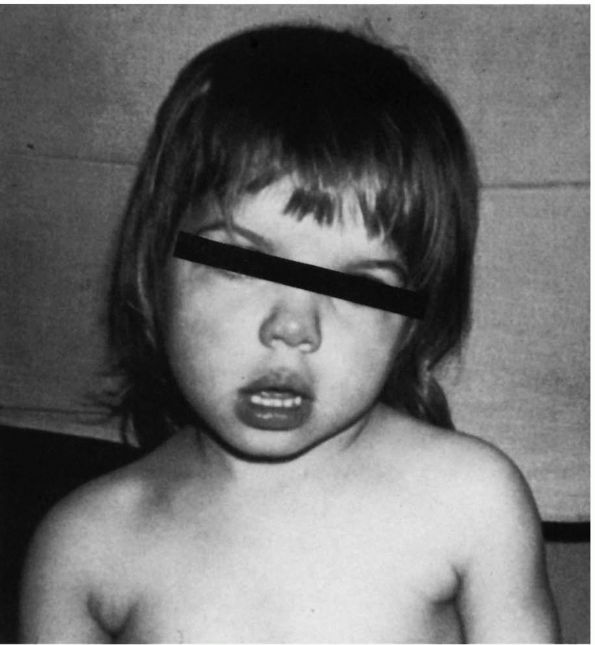
sign found in a variety of situations, is a rotational deformity of the
upper cervical spine that causes a turning and tilting of the head (Figure 11-1).
The head is tilted to the involved side and the chin rotated to the
opposite side. This is most often seen in the newborn period. It is
often associated with deformity of the head (plagiocephaly). If
torticollis is present in the newborn period, the usual cause is
congenital muscular torticollis. Roentgenograms of the cervical spine,
however, should be obtained to exclude other less common congenital
conditions, such as fixed or bony torticollis resulting from
Klippel-Feil syndrome, or other anomalies of the atlantoaxial portion
of the cervical spine.
 |
|
FIGURE 11-1.
Torticollis is head tilt with rotation. Congenital muscular torticollis and rotatory subluxation of the atlas on the axis are the two most common causes in children. Facial asymmetry is present. |
respiratory tract illnesses. When torticollis is present after the
newborn period one should be highly suspicious of a problem in the
upper cervical spine as 50% of the rotation of the cervical spine
occurs at C1-C2. Therefore, conditions that would cause a rotational
deformity are likely present at the atlantoaxial level.
the first month of life. It presents as unilateral tightness of the
sternocleidomastoid muscle. Seventy-five percent of the involved
muscles are on the right side. There may be a palpable mass “tumor”
that is generally nontender, firm to soft and mobile beneath the skin,
and attached to or located within the body of the sternocleidomastoid
muscle. This mass often enlarges during the first 4 to 6 weeks of life
and then gradually decreases in size. By 4 to 6 months of age, the mass
is usually absent, and the only clinical findings that may remain are
the contracture of the sternocleidomastoid muscle and the torticollic
posture with the head tilted toward the involved side and the chin
rotated toward the opposite shoulder.
|
TABLE 11-1. Differential Diagnosis of Torticollis
|
||||||||
|---|---|---|---|---|---|---|---|---|
|
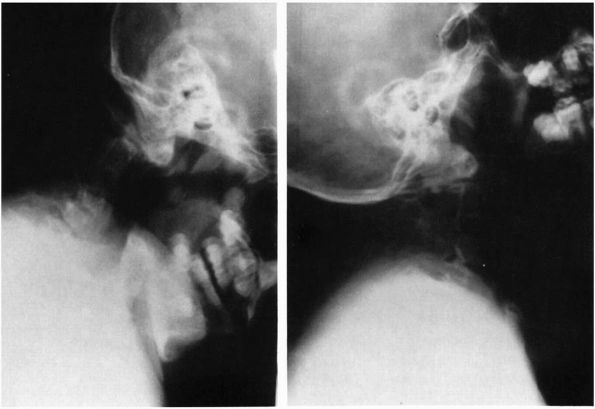
the cause can pose a difficult diagnostic problem. Radiographs are
often difficult to obtain because the mastoid overlies the upper
cervical spine. A radiograph of the cervical spine taken as a lateral
to the skull can image the atlantoaxial region where the problem
usually exists.
may be an odontoid anomaly, C1-C2 instability, Klippel-Feil syndrome,
and so forth (Table 11-1). All children with
torticollis should be evaluated with roentgenograms to exclude bony
abnormality or fracture. Roentgenographic evaluation may be difficult
in any child with a rotational deformity, but this is particularly true
in the neonate.
the usual cause is congenital muscular torticollis. If the child is
less than 2 months of age, the palpable lump usually is diagnostic.
Congenital
muscular
torticollis is painless, is associated with a contracted
sternocleidomastoid muscle, and is unaccompanied by any bony
abnormalities or neurologic deficit. Any findings of pain or neurologic
deficit should lead one to seek out other causes. Soft tissue problems
are less common and include abnormal skin webs or folds (pterygium
colli). Tumors in the region of the sternocleidomastoid include
brachial cleft cyst and teratomas, which are rare but should be
considered.
involvement of the cervical nodes is the primary cause of torticollis.
Spontaneous atlantoaxial rotatory subluxation may follow an acute
pharyngitis. Radiographic confirmation is difficult, and computed
tomographic (CT) scans and magnetic resonance images (MRIs) may be
necessary for diagnosis. If torticollis goes untreated for more than
several weeks, there may be secondary soft tissue deformities that
result in fixed rotatory subluxation.
part of the evaluation. Torticollis most commonly follows injury to the
C1-C2 level. Fractures of the odontoid may not be apparent in the
initial radiographic views; if a high index of suspicion is present,
special radiographic studies should be undertaken. Children with bone
dysplasias, such as Morquio’s disease, spondyloepiphyseal dysplasia,
and Down syndrome, have a high incidence of C1-C2 problems and should
be evaluated if torticollis is present.
of the central nervous system, such as tumors of the posterior fossa or
spinal column and syringomyelia, may be accompanied by torticollis.
Generally, there are additional neurologic findings such as long tract
signs, weakness in the upper extremities, and hearing or visual
problems that may also cause head tilt.
by local trauma to the soft tissues of the neck just before or during
delivery. Two-thirds of children are associated with difficult labor
and delivery, and these children often have had breech or difficult
forceps deliveries. Torticollis can occur after otherwise normal
delivery, however, and has been reported following cesarean section.
The fibrosis in the muscle may be due to venous occlusion and pressure
on the neck in the birth canal because of cervical and skull position.
The persistent clinical deformity is probably related to the ratio of
fibrosis in the muscle to the remaining functional muscle. If
sufficient normal muscle is present, it usually stretches with growth,
and the child does not develop torticollis. In three of four children,
the lesion is on the right side. Up to 20% of these children have
congenital dysplasia of the hip associated with torticollis.
deformities of the face and skull can result, including asymmetry of
the eyes and ears. Flattening of the face on the side of the contracted
sternocleidomastoid may be impressive and is due to the position of the
head when the child sleeps. If the child sleeps prone, it is more
comfortable to have the affected side down. The face on the affected
side remodels to conform to the surface. In children who sleep supine,
the modeling of the contralateral aspect of the skull is evident.
stretching exercises. The exercises include positioning the ear
opposite the contracted muscle to the shoulder and also stretching the
chin to the shoulder on the opposite side. When adequate stretching has
been obtained in the neutral position, these maneuvers should be
repeated with the neck extended. Other measures include positioning of
crib toys so the sternocleidomastoid are stretched when trying to reach
and grasp. If exercises are unsuccessful, surgical resection may be
required to release a portion of the tendon at the clavicular
attachment. Surgery is usually performed before school age. Asymmetry
of the skull and face corrects as long as adequate growth potential
remains after the deforming force of the sternocleidomastoid is
removed. The results of surgery are usually good with a low incidence
of complications and recurrence, although some children require a
repeat procedure during adolescence. More severe deformities may
require both proximal and distal sternocleidomastoid release.
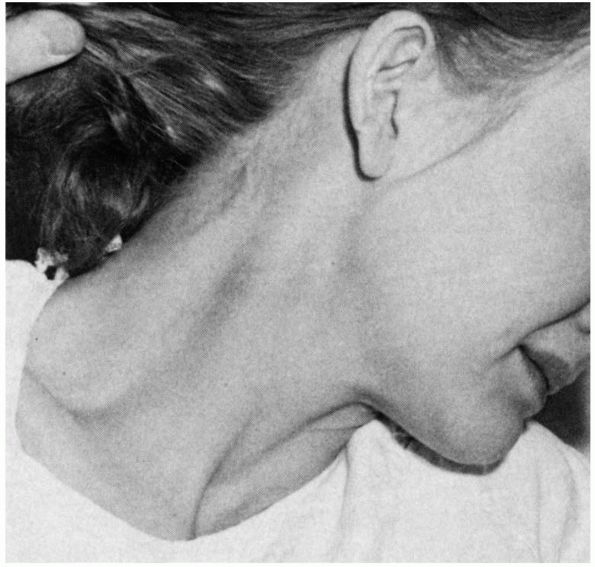
subluxation or C1-C2 rotatory displacement (rotatory subluxation of
childhood; Figure 11-2).
This condition may occur following trivial trauma or a viral upper
respiratory tract inflammatory condition but also can occur following
tonsillectomy or other oral pharyngeal surgery. Grisel’s syndrome is
not a cervical infection but a rotatory displacement of C1-C2 secondary
to local inflammation, which can allow capsular or synovial
interposition of tissue at the atlantoaxial level.
 |
|
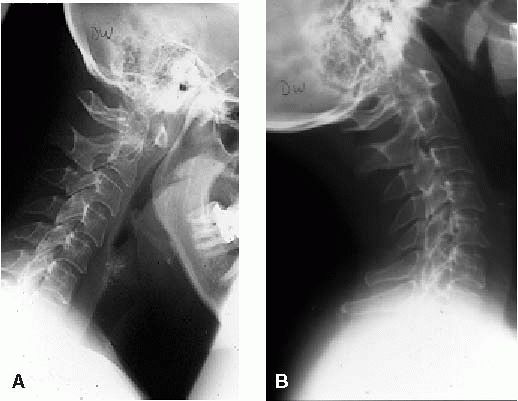
FIGURE 11-2.
Rotatory subluxation, C1 on C2. This open mouth view is consistent with atlantoaxial rotatory subluxation. There is tilt of the skull as well as a shift of the lateral masses of C1 on C2, with overlap of the lateral mass of C1 on C2 on the left side. Cineradiography or dynamic CT scan is the best method to confirm fixed rotatory subluxation of C1 on C2. |
muscle spasm, torticollis, and pain on cervical motion. Usually the
range of motion is not significantly altered, but motion is
uncomfortable if moved from the torticollic position. This condition
occurs most commonly in children 3 to 12 years of age. There is no
spasm or contracture of the sternocleidomastoid muscle. The sudden
onset of torticollis in this age group or in adults should lead to
radiographs of the upper cervical spine. If these are not rewarding,
further radiographic studies should be done in this area to look for
the cause of torticollis.
either some type of central nervous system tumor or a visual
abnormality. As children compensate for various abnormal vision-related
problems, they may tilt their head to be more comfortable with the
image.
with or without treatment. Occasionally, it becomes fixed and requires
treatment. Most patients are in between these extremes and may require
anti-inflammatory medication, soft collar, or head halter traction to
resolve the torticollis. Treatment should be persistent and early to
avoid the fixed rotatory problem. If the torticollis becomes fixed, in
situ fusion may be indicated.
adults with painful spasms producing a wry neck deformity. Radiographic
studies are normal. The cause is idiopathic; however,
electromyelographic studies show involvement of many muscles in the
area, including the sternocleidomastoid, trapezius, and splenius. This
condition is resistant to the usual forms of treatment, including
surgery. Often these patients have concomitant or develop severe
psychiatric disturbances.
accessory nerves and the first three anterior cervical nerve roots.
Minimal involvement on one side and severe involvement on the other may
require nerve root section on one side only. When the pain is intense
and bilateral and many muscles are at fault, section of the fourth
anterior cervical nerve root may be added without fear of compromising
diaphragmatic function. Postoperatively, neck function is weak but the
patient’s painful spasms have improved.
This condition is, however, temporary and usually resolves in a few
weeks with application of heat, rest, and, occasionally, local
injection of the spinal accessory nerve.
exposure to direct cool air on the neck. There are multiple causes for
neck stiffness, and many of these
problems
may come from the degenerative processes discussed later. Patients may
present with torticollis that lasts for several days or more. A
significant amount of discomfort is commonly associated with any motion
of the cervical musculature leading one to rotate the thorax with the
head. This condition is more commonly seen in adolescents and young
adults than in older patients. The exact cause is variable and often
not identified. Causes can include muscle spasm, early disc herniation,
multiple sclerosis, rheumatoid arthritis, primary or metastatic
neoplasm, and vertebral osteomyelitis.
 |
|
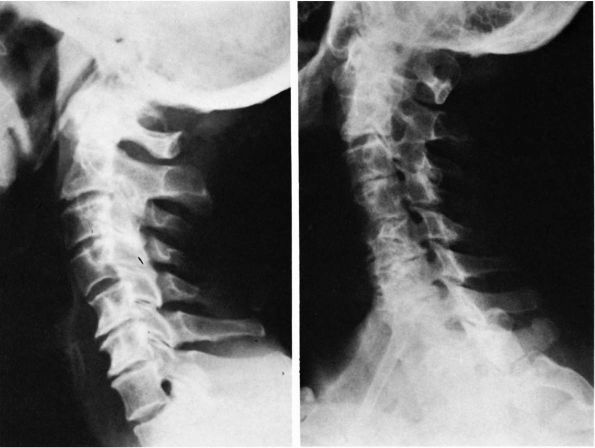
FIGURE 11-3.
Acute torticollis due to neuritis of the spinal accessory nerve. The severely painful spasms were unilateral, temporary, and relieved by infiltration of the nerve with a local anesthetic. In contrast, spasmodic torticollis is bilateral, persistent or intermittent, and unaffected by injection of the nerve. |
The area of discomfort may be the entire neck but is usually located in
the paraspinous muscles posteriorly and in the occipital area. Often
patients are tender to palpation and with any passive or active motion
is painful. Lying down, using traction or cervical collars, or
employing other measures to relax the cervical muscles are the only
methods that tend to give any relief from the complaint. Associated
symptoms such as nausea, dizziness, or headache may accompany the neck
discomfort. Patients with this problem are usually obvious because when
they turn their head, they turn their entire body, or they may use
their hands for support of their head with any active movement. Pain
may be referred to the scapula, occipital area, or the shoulders, and
there may be diffuse tenderness in the area of the trapezius.
radiographic evaluation should include anteroposterior (AP) and lateral
flexion-extension radiography to evaluate the bony portions of the
cervical spine. Early with muscle spasm, there is loss of cervical
lordosis as seen in the lateral cervical spine radiograph. There is
little movement of the cervical spine on motion studies, which are
often not helpful in evaluating for stability or injury because
patients guard the spine against attempts at motion. Depending on
history and physical examination, other studies (e.g., myelogram or
MRI) may be important to arrive at the exact diagnosis for a stiff neck.
usually is self-limiting and responds to rest and anti-inflammatory
agents. The problem may clear without treatment. If one of the more
significant degenerative, infectious, or neoplastic processes are
found, treatment should be appropriate to that condition.
examination are within normal limits, treatment usually consists of
application of heat, nonsteroidal anti-inflammatory medication, and a
soft collar or supine cervical traction to relax cervical musculature.
occur in the middle or later years of life. Cervical disc degeneration
can be manifested as axial pain, radiculopathy, or myelopathy. The
process can be acute as seen with disc herniations and cause symptoms
resembling those of an acute lumbar disc herniation (i.e., clear
radicular pattern of pain, motor, and sensory deficits); the clinical
picture may also be more indolent from chronic cervical disc
degeneration and may be confusing. Several terms
are commonly used to describe the degenerative cervical spine. The most frequent term is cervical spondylosis; other synonyms are osteoarthritis, osteoarthrosis, chronic herniated disc, chondroma, and spur formation.
radiographic evidence of cervical degeneration. Degeneration of
cervical discs is a natural process associated with aging, which is
difficult to distinguish from the disc disease that is a deteriorative
process and may produce pain. DePalma reported that in people older
than 70 years, 72% had severe radiographic abnormalities. Rothman found
myelographic abnormalities were common in asymptomatic patients.
Abnormalities were seen in 21% of cervical myelograms, 24% of lumbar
myelograms, and 8% of lumbar and cervical myelograms. Thus, no clear
correlation exists between radiographic changes and symptoms.
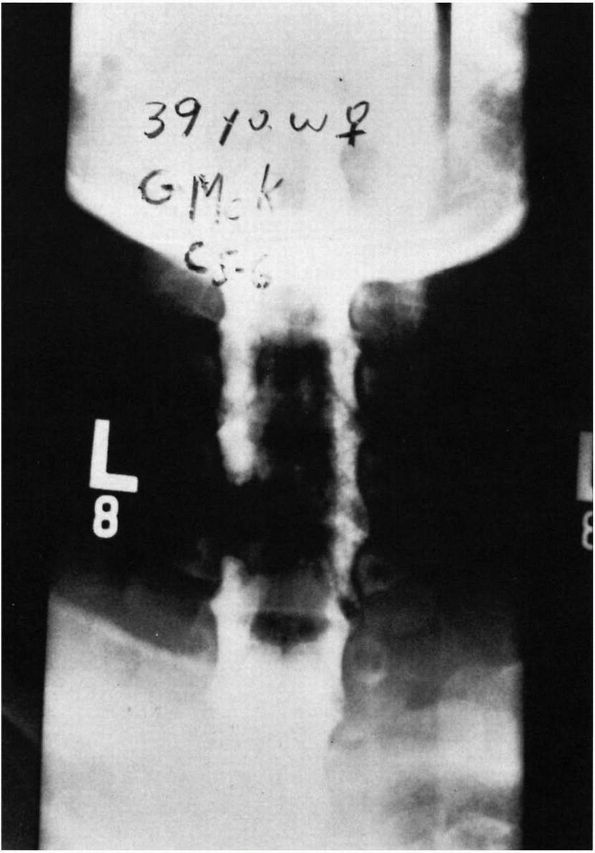
Radiographically, the most frequently involved level is C5-C6 followed
by C6-C7, and C4-C5. Upper-level (occiput-C3) involvement is less
common.
dysfunction (i.e., radiculopathy or myelopathy). Radiculopathy—root
compression—is a lower motor neuron problem and is manifested by pain
in the distribution of a nerve root. It can be associated with neck
pain, sensory deficit, and motor deficiency. Ideally, these findings
would all correlate with a specific root but at times can be more vague
with some overlap of adjacent roots as demonstrated by Marzo et al.
The associated reflex may be diminished. Myelopathy involves
compression of the spinal cord, and thus, it can effect the upper and
lower extremities with a mixture of upper and lower motor neuron
lesions. Patients with myelopathy do not necessarily complain of pain.
The hallmark is extremity dysfunction such as hand clumsiness with fine
motor tasks and gait instability.
directly compressed. Osteophytes, which develop as a reaction to the
process of degenerative disc disease extending across the posterior and
posterolateral aspect of the vertebral bodies, may cause direct
compression. An inflammatory component of the neuroelements may be a
more significant cause of pain than actual mechanical changes. Studies
have shown that compression of a normal nerve root results in
paresthesia while compression of an inflamed root results in pain.
instability. This can usually be identified on lateral flexion and
extension radiographs. Anterior-posterior movement of one vertebral
body on another of 3.5 mm or greater in the adult is considered
abnormal. Traction (horizontal) osteophytes may be an indicator of
hypermobility.
the spinal canal itself becomes compromised by bone or soft tissue
hypertrophy. In addition, the canal may be congenitally narrow.
Hyperextension in the spondylotic cervical spine may cause further
compromise with inward bulging of the posterior ligamentum flavum and
by disc protrusion. Ischemic changes of the spinal cord may result from
compression of its blood supply as the vessels pass through the pia
mata. The vertebral artery, which ascends through an osseous canal
formed by the foramen transversarium in the transverse processes of the
sixth to the second cervical vertebrae, may be compressed creating a
constellation of symptoms from the cerebellum, posterior fossa or
brainstem.
cervical spine may be a source of a dull, aching axial pain or
radiating pain secondary to direct nerve root compression. Likewise,
the pathophysiological changes that occur within the aging disc may be
a direct source of axial pain. Additional mechanical sources of pain
are microfractures in the vertebral bodies and pseudarthrosis of the
cervical spine.
of neck pain must include tumors, either primary such as osteoid
osteomas or metastatic. A pancoast (superior sulcus) tumor in the apex
of the lungs can mimic neck pain or create neurological deficits within
the lower brachial plexus that can be confused with cervical disease.
Additional causes of neck pain are compressive lesions of the brachial
plexus and shoulder pathology.
differential diagnosis and may result in vertebral artery syndrome. The
symptoms are intermittent in nature and include headaches, vertigo,
tinnitus, and momentary loss of consciousness particularly when
associated with extension or rotation
maneuvers
of the head and neck. The patient may experience dizziness, ataxia,
headaches, nystagmus, and visual aberrations. Vertebral artery
compression syndrome resulting by ingrowth of osteophytes from the
lateral aspect of the vertebral bodies are more common than realized.
|
TABLE 11-2. Cervical Radiculopathy: Differential Diagnosis
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
patient may experience supraclavicular pain with radiation to the arm
increased by use of the arm. There may be a history of paresthesia,
particularly in the ulnar distribution, and blanching or coldness of
the fingers. Physical examination may reveal tenderness about the
brachial plexus and a positive Adson test in which patients place their
hands on the thighs in a sitting position, turn the head to the side,
and inhale deeply, resulting in a reproduction of the symptoms. Other
peripheral compressive neuropathies, such as cubital tunnel syndrome
and carpal tunnel syndrome, can be confused with cervical
radiculopathies.
occipital nerve neuralgia in which the posterior primary ramus of the
C2 nerve becomes irritated or inflamed. Physical examination may reveal
subjective paresthesia to percussion. The patient may experience
limited neck motion, and symptoms may be reproduced by vertical loading
or by maintaining the neck in extension.
and 70. The onset of pain is insidious or sudden, and there may or may
not be a history of trauma. The location of pain varies with the nerve
root involved. Referred pain and soreness in the intrascapular region
via the dorsal ramus of C6, or suboccipital headache secondary to
greater occipital nerve involvement may occur (Table 11-3).
The pain of cervical radiculopathy may be described as dull, aching,
boring, and related to neck motion. It may or may not be related to
sneezing or coughing. Extension with ipsilateral tilt of the neck,
Spurling’s sign, may exacerbate the arm symptoms. Patients sometimes
get relief by placing their arm on top of their head, relaxing any root
tension.
degeneration with posterior osteophyte formation is the most common
cause of spinal cord dysfunction in patients older than 55 years. The
patient may present with a stooped wide-based or spastic gait and
complain of weakness and clumsiness in the hands. Pain may not even be
present, although many of these patients include axial or radicular
pain. The symptoms may be dynamic with paresthesias into the upper
extremities on flexion and extension, L’hermittes’s sign.
motor neuron involvement in the lower extremities, and a combination of
upper and lower motor neuron involvement in the upper extremities. In
other words, the lower extremities are spastic with increased deep
tendon reflexes and a positive or upgoing Babinski test. They often
have several beats even sustained clonus. The upper extremities show
weakness and atrophy. A Hoffmann’s reflex is frequently positive.
Several proposed mechanisms describe the pathophysiology of cervical
myelopathy. Anterior compression of the spinal cord results from
posterior osteophytes. Posterior compression may result by infolding of
the ligamentum flavum particularly in extension. Nutritional and
vascular involvement with decreased blood supply through the spinal
arteries resulting in ischemic changes to the spinal cord has been
identified.
level or levels of spine disease that may be responsible for the
radicular syndrome in cervical spondylosis. Studies can include AP,
bilateral obliques, lateral, odontoid open mouth, and lateral flexion
and extension views (Figure 11-4). Look for
evidence of foraminal encroachment, vertebral malalignment, sclerosis,
facet joint subluxation, osteophyte protrusions, destructive changes
within the disc or vertebral body, and ossification of the posterior
longitudinal ligament. Canal dimensions can be inferred by measuring
the Torg ratio of canal width (posterior vertebral body to posterior
laminar line) to vertebral body, with anything less than 0.8 is
considered stenosis. Further evaluation may include MRI, myelography
using water-soluble contrast followed by contrast-enhanced CT scanning.
An extension lateral view taken during the myelogram may illustrate
infolding of the ligamentum flavum and dynamic encroachment in the
spinal canal.
|
TABLE 11-3. Cervical Radiculopathy
|
||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
FIGURE 11-4.
Degenerative arthritic changes in the cervical spine following loss of disc material particularly between C5 and C6. However, the oblique view shows spur formation encroaching on the intervertebral foramina from C3 to C7, which can cause nerve root symptoms. |
the size of the neuroforamina, which are normally 5 to 8 mm in vertical
diameter. Scans must be performed using thin overlapping slices,
appropriate bone windows, and reconstructions in the parasagittal plain
to show the neuroforamina in profile. Anoncontrasted CT scan is also
very useful in delineating bone from soft tissue in planning a
decompressive procedure.
myelography in combination with CT scanning remains the securest way of
defining root sleeve pathology (Figure 11-5).
It must be remembered that myelography does not define the most lateral
component of the neuroforaminal encroachment because the subarachnoid
space does not extend out to the full extent of the neuroforamen along
with the nerve roots. Myelography with flexion and extension views can
demonstrate dynamic cord compression related to bulging of the
posterior longitudinal ligament and ligamentum flavum, or to spinal
instability.
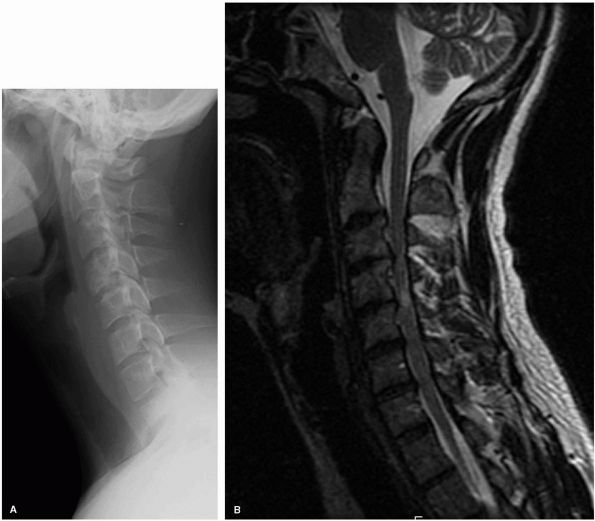
the cervical spine. Although CT scanning is still better at delineating
bone from soft tissue, the MRI is far superior in defining soft tissue
anatomy (Figure 11-6). The disc material and
nerve anatomy can be seen as well as demonstrating pathophysiolocal
effects such as “gliosis” associated with chronic spinal cord
compression. Be careful in assessing the amount of canal compromise on
T2-weighted image because the degree of stenosis can be overestimated.
Under those circumstances a CT or myelogram can be a complimentary
study. Infections, hematomas, and tumors are also much better
visualized by MRI.
injecting it with a radiopaque substance, thus obtaining a cervical
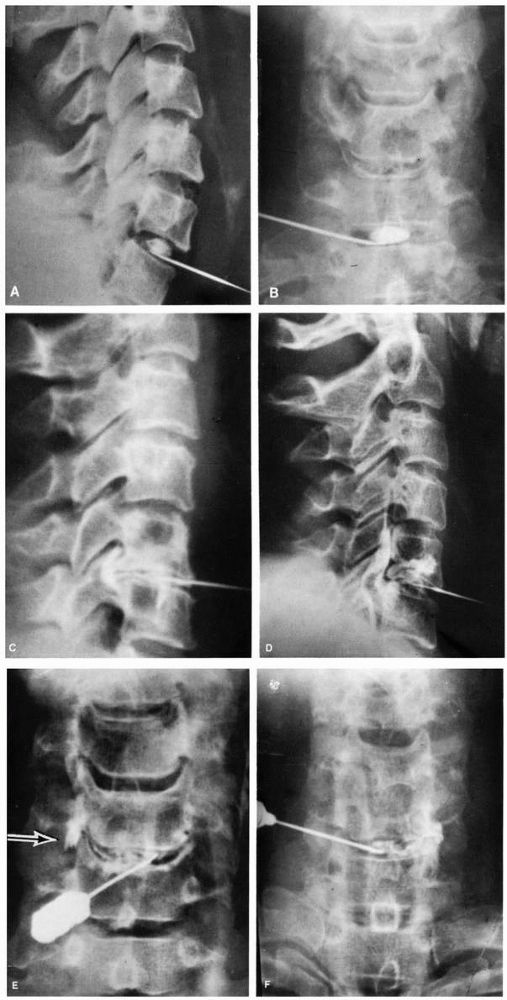
diskogram (Figure 11-7). Distinctive diskogram
determinations are dynamic tension on injection, the actual diskogram
appearance on radiograph, and the reproduction of pain response. In the
cervical spine, reproduction of clinical symptoms with injection is
more important than the actual descriptive interpretation of the
diskogram. Diskography is not a routine diagnostic procedure. It is
important, however, to recognize that abnormal diskograms and pain
produced locally and at a distance by injecting can be demonstrated in
some asymptomatic people. The percentage of false-positive examinations
increases with advanced age. The procedure itself, therefore, is not
infallible proof of an abnormal symptom.
 |
|
FIGURE 11-5. Cervical myelogram demonstrating herniated disc with left C5-C6 nerve root compression.
|
 |
|
FIGURE 11-6. (A)
A sagittal T2-weighted MRI scan of the cervical spine demonstrates chronic disc protrusions at C3-C4 and C4-C5 along with infolding of the ligamentum flavum at those same levels. This is typical of cervical spondylosis and the resultant cord compression has created “gliosis” changes within the cord as illustrated by the increased signal intensity within the cord at the C3-C4 disc level. (B) The corresponding T2 axial images at C3-C4 in the same patient further defines the degree of cord deformity from the compression. |
 |
|
FIGURE 11-7. Normal cervical diskograms: (A) lateral view; (B) AP view. (C) “Mushroom” diskogram. (Dye around the posterior osteophyte beneath the posterior longitudinal ligament.) (D) Massive posterior disc rupture. (E) and (F) Examples of unilateral disc rupture.
|
the diagnosis particularly by documenting the distribution of
involvement, and distinguishing peripheral entrapment syndromes and
generalized peripheral neuropathy, from radiculopathy. Nerve conduction
studies can indicate that the nerve lesions are axonal rather than
demyelinated. Conduction velocities within the involved nerve are
normal or reduced in proportion to the degree of axonal loss.
It takes 4 to 28 days for electromyelographic (EMG) changes to develop
in acute radiculopathy. One-third of patients have abnormalities in
only the arm muscles, one-third are abnormal in only the paraspinal
muscles, and one-third have electrical abnormalities in both paraspinal
and arm muscles. The EMG is an electronic extension of the physical
examination.
shown on radiologic and other imaging studies in whom cervical
radiculopathy cannot be localized, injection of local anesthetic into
the interspace under fluoroscopic control and injections of local
anesthetic into the facet joints may be useful in localizing the pain
syndrome.
degeneration, including physical stress, biochemical abnormalities,
genetic defects, psychophysiologic effects, and autoimmune processes.
aging, there is decreased water content of the disc and diminished
water-binding capacity. Collagen, the main structural component of the
disc, increases, and its orientation and pattern change with age. These
and other biochemical changes lead to a loss of the gel behavior of the
nucleus and a loss of the desired biomechanical properties of the
annulus, which becomes weakened and inelastic. The mechanical
properties change from liquid to solid. Radiographically, this is
manifested by gradual narrowing of the cervical disc space, sclerosis
of the vertebral bodies, and the presence of osteophytes.
nuclear herniation, annular protrusion or bulging, and diffuse
degenerative changes. Degenerative changes commonly seen include
osteophytes, both anterior and posterior, fissures in the discs,
nuclear extrusion, abnormality and sclerosis at the joints of Luschka,
foraminal narrowing, rounding of the anterosuperior vertebral bodies,
and disc space narrowing.
narrows. Encroachment into the neuroforamina may be caused by the
joints of Luschka (uncovertebral joints), products of disc, or
hypertrophic or subluxed facet joints. Osteophytes may develop
posteriorly and extend across the entire width of the vertebral body as
a protuberant ridge. Additionally, the posterior longitudinal ligament
may become hardened or calcified. Hypertrophy of the ligamentum flavum
may also occur, which, on hyperextension, results in a rigid
encroachment or bulging into the spinal canal with resultant
compression on the posterior aspect of the thecal sac. The average
spinal canal diameter between C3 and C6 is 17 mm. Degenerative changes
in the cervical spine may result in a decreased canal diameter, thus
reducing the space available for the cord (SAC). A SAC of 11 mm or less
implies spinal cord compression.
involves the use of rest and splinting. Often a soft cervical collar is
adequate to provide gentle support. Philadelphia collars and other
rigid cervical collars are frequently not well tolerated. Gentle
traction using 5 to 10 lb with a head halter and a neutral position of
flexion-extension to open up the neuroforamina may be of value.
Traction applied in either flexion or extension may aggravate the
patient’s pain problem. Salicylates and the application of hot moist
packs may be effective.
treatment of radiculopathy. Approximately 80% of radiculopathy patients
can be successfully treated nonoperatively.
indicated if there has been a documented failure of appropriate
nonoperative treatment or if there is
progressive neurologic deficit with a radiculopathy. Options are anterior or posterior decompression with or without fusion (Figure 11-8),
depending on location and type of compressive pathology. Cervical
myelopathy resulting from degenerative spondylosis or disc herniation
is typically treated surgically. Patients presenting with cervical
myelopathy seldom improve with nonoperative management and roughly
one-third will continue to deteriorate, sometimes suddenly with
hyperextension. The intent of surgical decompression in myelopathy
patients is to prevent progression with neurological improvement being
secondary and unpredictable. Because one cannot foresee those patients
that will deteriorate while being treated nonoperatively, surgical
management is favored. Options are anterior decompression via
corpectomy, diskectomy, and fusion versus posterior complete
laminectomy and decompression. In the case of multilevel disease (3 or
more levels), open door hinged laminoplasty, in which the lamina is cut
on one side and hinged on the other side to create a flap-type opening
and thus expand the spinal canal, has been gaining favor (Figure 11-9).
Open-door laminoplasty for multiple-level decompression seems to
prevent postoperative swan-neck-type deformities, which sometimes occur
after extensive multilevel posterior laminectomies.
 |
|
FIGURE 11-8.
A lateral radiograph demonstrating an anterior cervical fusion with plating done in conjunction with a corpectomy and C5-C6 diskectomy used to decompress the spinal cord in a patient with cervical myelopathy. |
congenital fusion of the cervical vertebrae whether it be two segments
or the entire cervical spine. The incidence is less than 1% of the
population.
congenital cervical fusion represents a failure of the normal
segmentation of the cervical somites during the third to 8th week of
life. There can be congenital blocked vertebrae with complete fusion of
two or more adjacent vertebral bodies or a congenital bar with partial
fusion of two or more vertebrae. This syndrome is usually most apparent
in children in the posterior elements and radiographically may appear
as a bar between the bones (Figure 11-10). The embryologic abnormality is not limited to the cervical spine.
minor cervical fusions, may be at risk for other less apparent but
serious defects in the genitourinary, nervous, and cardiopulmonary
systems. Many have hearing impairment. These hidden abnormalities may
be far more detrimental to the child’s general well-being than the
deformity of the neck.
clinical appearance. There is, however, a classic syndrome triad that
includes a low posterior hairline, a short neck, and limitation of head
and neck motion. The limitation of motion is predominantly in lateral
side bending. Despite severe congenital fusion, many with this syndrome
are able to maintain a deceptively good range of motion. Associated
conditions, which are commonly seen when congenital cervical fusion is
present, include Sprengel’s deformity, scoliosis, deafness, synkinesis,
and hand, renal, and cardiac deformities. Individuals with this
syndrome may present because of an incidental radiologic finding or in
association with the workup of other conditions or because of cosmetic
concerns about their neck web or low hairline.
positioning for AP, lateral, and oblique views of the cervical spine.
Often there are overlapping shadows from the mandible, occiput, and
mastoid areas. Lateral flexion-extension views, CT scans, and other
studies may be necessary to fully evaluate the cervical spine
deformity. If pain is present (as may be evident in older patients with
this problem), serial lateral flexion-extension views may be necessary
to evaluate for segmental instability with blocked motion at other
levels. Other special studies, such as cineradiography, CT scans, and
MRIs, may be necessary in certain situations.
 |
|
FIGURE 11-9.
Lateral plain radiographs and sagittal T2 MRI in a patient with multilevel congenital cervical stenosis with associated spondylosis causing severe cord compression, including signal change within the cord, in a patient with spastic gait and clumsy hand consistent with cervical myelopathy (A, B). Because of the multilevel nature of the problems the treatment selected was a posterior laminoplasty with excellent recovery of neurological complaints (C, D). |
flexion-extension views; however, there may be persistent cartilaginous
endplates, which look as if they are normal disc spaces. As the
vertebral body completes its ossification, the fusion often becomes
obvious.
Klippel-Feil syndrome; however, there can be radiculopathy, myelopathy,
quadriplegia, and sudden death from abnormal motion in the neck.
 |
|
FIGURE 11-9. (Continued)
|
syndrome. Spinal deformity may be present in up to 60% of patients with
Klippel-Feil syndrome. There is a 20% incidence of renal abnormalities
reported in patients with congenital scoliosis. Usual evaluation of
Klippel-Feil syndrome includes an ultrasound of the kidneys and, if
there is any doubt about a diagnosis, an intravenous pyelogram.
may be associated with Klippel-Feil syndrome. Few children are
symptomatic, and most patients who develop symptoms are in at least the
second or third decade of life. Usually patients with Klippel-Feil
syndrome can be expected to lead a normal, active life with only minor
restrictions. Many of the severely involved patients may require fusion
of abnormally mobile levels.
arthritis (JRA) is usually limited to polyarticular and systemic JRA.
The major problem associated with the cervical spine in JRA is slow,
progressive, clinical stiffness and anatomic fusion of segments of the
cervical spine. The usual reason to evaluate this problem early is to
provide cervical protection during the active stage of the disease to
direct the iatrogenic fusion of segments to a position of function.
with the disease. Radiographic evidence of cervical spine abnormalities have been found in 27 to 80% of children with JRA.
 |
|
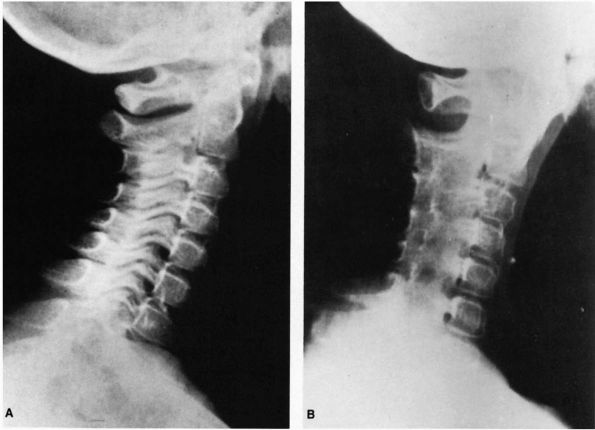
FIGURE 11-10.
Lateral flexion-extension radiographs of a 10-year-old child with occipital and shoulder pain. There is fusion of C2-C4 (Klippel-Feil syndrome), the odontoid is absent, and motion of C1 on C2 is abnormal. |
The pain is characteristically in the posterior area of the neck,
radiating up into the occipital area and down into the shoulders and is
worse with any motion of the head and neck. Usually the pain and loss
of motion occur before the radiographic abnormalities, although severe
neck pain is not common in the juvenile form of this disease.
compressive, or myelopathic, are rare. They may occur in those few
children with C1-C2 instability or with one motion segment following
spontaneous fusion above and below.
is inflammation of synovial tissues that spread to involvement of the
supporting ligamentous structures around the cervical spine. Synovial
joints in the cervical spine include the posterior apophyseal joints,
which rapidly become ankylosed with developing arthrosis, and the area
around the odontoid both in the anterior articulation with the ring of
C1 as well as with the transverse ligament. This results in the
radiographic apple core odontoid.
in adult rheumatoid arthritis. Early changes consist of erosion of the
odontoid or the so-called apple core odontoid. There may be apparent
C1-C2 instability because of narrowing of the odontoid from this
process. There is erosion of the odontoid at the level of the synovial
membrane with the transverse ligament.
may be evident because of attrition or fracture of the odontoid. There
may also be collapse of the C1-C2 facet area laterally, resulting in
torticollis or abnormal positioning.
apophyseal joint ankylosis resulting from inflammatory disease of the
facet joints (Figure 11-11). There may be
decreased height secondary to this fusion if it occurs when the growth
plates are still open. Spontaneous fusion usually has no associated
neurologic problems. There may be decreased size of the vertebral body,
but the spinal canal is not compromised. Subluxation and instability
may be a problem because of segmental fusion and abnormal motion
occurring at fewer mobile levels.
spine, particularly the joints between the second and third cervical
vertebrae, is considered characteristic of JRA. As these areas fuse,
the mechanical cervical pain improves but results in an inability to
move the
neck.
This may result in instability if there are levels between fused
segments that become hypermobile. The usual course of the cervical
spine disease parallels the systemic course of the disease and also
usually correlates with the severity of involvement of the individual
patient. The stiffness of the cervical spine usually results in
stiffness in extension and is a common early finding in polyarticular
or systemic onset juvenile arthritis. Severe neck pain or torticollis
is not common. When a severe amount of pain or torticollis is present,
look for either a fracture or infection as the cause of that complaint.
 |
|
FIGURE 11-11. (A)
Radiograph of a 9-year-old child with neck pain and polyarticular juvenile rheumatoid arthritis, illustrating early sclerotic change in posterior cervical joints. (B) Radiograph of the same patient 13 months later shows complete ankylosis of the apophyseal joints of the cervical spine typical of juvenile arthritis. |
consists of splinting the neck in a functional position. The patient
should be encouraged to sleep without a pillow or in a position with a
small amount of flexion. A cervical collar, either hard or more
commonly soft, is the usual treatment method. Occasionally, surgical
treatment for instability is required to further fuse areas of the
cervical spine. Rarely, atlantoaxial subluxation requiring surgery may
be present.
rheumatoid arthritis varies significantly from the juvenile
counterpart. Stiffness is the rule in JRA, whereas looseness and
instability is frequently a problem in adults who have cervical spine
involvement. Only rarely is there autofusion of the subaxial spine as
in JRA. Adults tend to develop instability patterns that generally fall
into one of three types; occipital cervical settling (basilar
invagination), atlantoaxial (C1-C2) instability, or subaxial
subluxation. Atlantoaxial subluxation is probably the most common and
significant manifestation of involvement of the cervical spine. Its
incidence has been estimated to be somewhere between 25 to 60% of
patients with rheumatoid arthritis. About 33% of patients with
rheumatoid arthritic involvement demonstrate C1-C2 subluxation on
flexion-extension radiographs. These patterns can occur in combination
or as isolated
areas of disease. The patients with severe erosive extremity disease and nodules are at greatest risk for cervical involvement.
arthritic patients regardless of the radiographic findings. This pain
can be suboccipital indicating upper cervical disease or more
generalized. The most significant concern is that of myelopathy, which
is manifested by upper extremity dysfunction, paresthesias, and gait
instability. If these symptoms are secondary to cord compression, they
may not be associated with pain. Some patients will also have
radiculopathy from root compression and can complain of upper extremity
radiating pain in that root distribution.
their extremities, such as contractures and joint instability, their
hand function and gait can be difficult to accurately assess. Often the
patient can distinguish progressive dysfunction secondary to neurologic
impairment as opposed to peripheral extremity disease progression.
Particular attention should be paid to identifying signs of spasticity
such as hyperreflexia, Hoffmann’s sign, clonus, and Babinski sign. If
the cord compression is due to basilar invagination, there may be brain
stem manifestations such as dysphagia, nystagmus, or other cranial
nerve findings. Consider the possibility of peripheral neuropathies,
which are also common in rheumatoid patients. Another less common
manifestation of instability is vertebral artery insufficiency
resulting from intermittent mechanical blockage.
The atlantodental interval (ADI) is measured from the anterior surface
of the odontoid to the posterior surface of the anterior ring of C1.
Flexion-extension views can identify how much motion is present at that
level. The ADI is thought to be abnormal when greater than 3 mm in an
adult and greater than 5 mm in a child. Perhaps a better indication of
the potential for neurological involvement is the space available for
the cord (SAC), measured from the posterior cortex of the odontoid to
the anterior cortex of the posterior C1 ring. This can also be called
the posterior atlanto-dens interval (PADI). Measurement of 14 mm or
less indicate significant risk for neurologic involvement. MRI
flexion-extension views may also be helpful in cord compression because
these views allow better visualization of the soft tissues such as the
cord itself and pannus formation anterior to the cord at C1 odontoid
joint. If the pannus is large enough, it alone can create cord
compression.
 |
|
FIGURE 11-12. Lateral flexion (A) extension (B) cervical radiographs demonstrating instability at the C1-C2 junction.
|
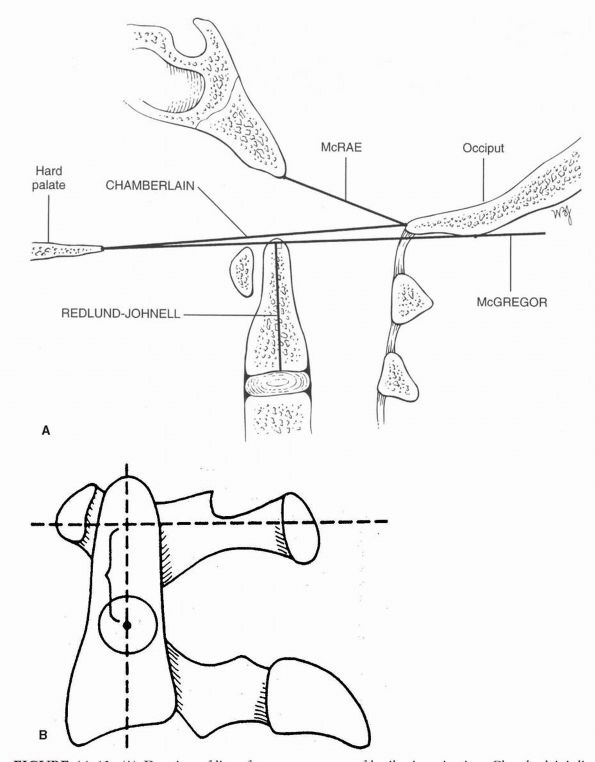
assess with plain radiographs and may be better seen on an MRI or CT
scan. Similar measurements can be made for translocation of the
odontoid into the foramen magnum. This is usually done by measuring the
McGregor line as well as the Chamberlain line to determine the degree
of odontoid projection (Figure 11-13). The line
drawn across the foramen magnum described by McRae should be well above
the tip of the odontoid process. It is often difficult to visualize the
pertinent structures at the base of the skull. Under those
circumstances Ranawat’s line can be useful. Cervicomedullary angle
measured via a sagittal MRI scan can also be used and anything less
than 135° signifies neurological risk to the patient (Figure 11-14).
This measures with a line parallel to the brainstem and intersecting a
second line parallel to the cervical cord. This disease is a systemic
disease, so nearly all elements of the cervical spine are involved,
including the bone ligaments, capsules, and so forth. Further changes
can occur if the patient has been using steroids. The severity of
cervical spine involvement usually parallels the severity of the
disease.
spine is somewhat controversial. The greatest concern with regard to
natural history of the cervical disease is to predict those patients
that are at risk to develop progressive myelopathy. Once a patient is
identified with extremity dysfunction from myelopathy, any improvement
in function as a result of surgical treatment is unpredictable, thus it
is ideal to identify these patients at risk prior to or early in their
course of myelopathy. Boden et al analyzed
patients based on the PADI and found that a measurement of 14 mm or
less was predictive of paralysis and surgical treatment was warranted
even in patients thus far asymptomatic.
 |
|
FIGURE 11-13. (A)
Drawing of lines for measurements of basilar invagination. Chamberlain’s line: odontoid tip > 6 mm above the line. McRae’s line: odontoid tip above this line. McGregor’s line: males, odontoid tip > 8 mm above the line; females, odontoid tip > 9.7 mm above the line. Redlund-Johnell distance: males < 34 mm; females, < 29 mm. (B) The distance described by Ranawat and associates is between the sclerotic ring, which represents the pedicle of the axis, and the transverse axis of the atlas, as measured along the longitudinal axis of the odontoid process. As this distance becomes shorter, the severity of cranial settling increases. Normal values are 17 mm + 2 in females. (Reprinted with permission from Clark CR, Goetz DD, Menezes AH. Arthrodesis of the cervical spine in rheumatoid arthritis. J Bone Joint Surg 1989;71A:381-392) |
 |
|
FIGURE 11-14.
A midline sagittal MRI reveals basilar invagination with the odontoid extending into the foramen magnum and a decrease in the cervicomedullary angle to 135°. |
at risk for sudden death due to upper cervical cord compression above
the root supply to the diaphragm (C3, C4, C5). Once a patient develops
myelopathy from upper cervical disease, the risk of sudden death is
significant as demonstrated on autopsy studies by Delamarter, Dodge,
and Bohlman.
some degree of comfort. A firm Philadelphia collar may give some
support. However, there may be skin sensitivity and difficulty in using
the collar and it does not protect from progressive neurological
deterioration nor death. Thus, it is a symptomatic treatment for pain
component only.
(2) neurologic dysfunction, and (3) radiographic parameters. Because
the location of pain is difficult to pinpoint, surgical treatment via
fusion can prove to be unreliable in resolving this complaint. Thus,
when pain is present in the absence of neurological involvement or
radiographic parameters then every effort is made to treat it
nonoperatively. If recalcitrant to nonoperative treatment then fusion
is generally carried out at the most involved segments.
involvement or specific radiographic parameters predictive of
neurological problems, then the only treatment likely to aid the
patient is surgical. In general the procedure is to adequately
decompress the neural elements, either by directly removing the
compressive structure or indirectly by realigning the spinal canal. In
order to maintain the decompression and prevent recurrence a fusion is
warranted in essentially all of these patients.
Techniques that provide the best immediate stability are favored in
order to avoid the need for postoperative halo immobilization. Basilar
invagination can be more difficult to treat. If the occipital migration
can be reduced via traction then a simple occipital cervical posterior
fusion may be adequate, occasionally including posterior C1
laminectomy. If this cannot be accomplished then a similar posterior
fusion can be utilized followed by direct decompression of the anterior
cord with an odontoid resection. For subaxial subluxations the surgical
technique is generally a posterior fusion. A laminectomy decompression
is included if the anatomic alignment of the segment cannot be restored
with the fusion.
 |
|
FIGURE 11-15.
One technique of posterior atlantoaxial (C1-C2) fusion using transarticular screws in combination with a Brooks wiring. This allows for enough immediate stability to avoid the need for postoperative halo immobilization. |
their medical complications rates high. In addition they tend to be
osteopenic with poor tissue quality giving risk to frequent
instrumentation related complications. The mortality rates within a
year of surgery on the cervical spine, particularly the upper cervical
spine in patients with rheumatoid arthritis, range as high as 50%.
These patients have a high incidence of failure of fusion and a
tendency to resorb bone graft particularly in upper cervical fusion.
Infection rates, wound healing problems, and difficulty with
postoperative immobilization are other significant problems in the
treatment of this condition. Adjacent segment instability can be a late
problem particularly given the predisposition to instability in these
patients.
article that reviews 624 cases of infantile torticollis treated over a
period of 7 years. Ninety-seven percent of all cases resolved with a
passive stretching exercise program.
MB, Harris LE. Congenital muscular torticollis in infancy: some
observations regarding treatment. J Bone Joint Surg 1959;41A:815. This
is an excellent classic review of 35 patients with congenital muscular
torticollis. The physical and pathologic findings and treatment with
follow-up are well recorded.
article evaluates the relation between the sternomastoid tumor and
congenital muscular torticollis. It reviews the etiology and
pathogenesis of the condition and presents the cases of 152 children
with torticollis.
C, SU J, Lin G, Lin S. Ultrasonographic study of the coexistence of
muscular torticollis and dysplasia of the hip. J Pediatr Orthop
2001;21:343. This article demonstrates that DDH
coexists with torticollis about 17% of the time and that in cases that
they found of treated DDH they found torticollis in about 85% of the
time.
article describes the surgical treatment for spasmodic torticollis and
discusses the differential diagnosis and how to arrive at the diagnosis
of true spasmodic torticollis.
is a retrospective review of 23 children treated for atlantoaxial
rotatory subluxation. In children seen less than 1 month after the
onset of symptoms the subluxation was able to be reduced either
spontaneously or with traction. Of the other seven children seen more
than a month after the onset of symptoms, three eventually needed C1-C2
fusion. Dynamic CT scans made in maximum rotation to each side proved
to be an excellent method of documenting the presence of rotatory
subluxation.
HS. Section 1. Degenerative cervical disorders. Instr Course Lectures,
Spine 2003; 5-58. Rosemont, IL: American Academy of Orthopaedic
Surgeons. This book offers an excellent
up-to-date review of cervical degeneration pathology, clinical
findings, a variety of treatment techniques, and complications. Each
chapter is written by experts and addresses an aspect of cervical
degenerative disease in detail.
AF, Rothman RH, Levitt RL, et al. The natural history of severe
cervical disc degeneration. Acta Orthop Scand 1972; 43:392-96. Natural history of symptomatic and assymptomatic radiographic degenerative disc disease.
MJ, Eismont FJ. Surgical options for the treatment of cervical
spondylotic myelopathy. Orthop Clin North Am 2002; 33(2):329-48. A
review of the various surgical treatment options for myelopathy
resulting from cervical spondylosis and offers a guide as to the
procedure that would best address the patients’ pathology.
review of the literature and techniques of cervical fusion comparing
allograft versus autograft. Iliac crest and fibula graft are discussed
for reconstruction of the anterior column supports of the cervical
spine.
cadaveric study that demonstrates the extent of intradural connections
between adjacent nerve roots that offers anatomic evidence supporting
the common clinical finding of motor, sensory, or reflex changes that
are frequently noted at levels cephalad or caudal to the
radiographically identified root of compression.
RH, Rashbaum RF. Pathogenesis of signs and symptoms of cervical disc
degeneration. AANS Instructional Course Lectures 1978:27:203-15. Instructional
course on signs, symptoms, and diagnoses of cervical disc disease. Many
patients have abnormal radiographic findings that are not associated
with symptoms.
FF, Wippold FJ II, Goado M et al. Comparison of computed tomography,
myelography and magnetic resonance imaging in the evaluation of
cervical spondylotic myelopathy and radiculopathy. Spine
1999:24(17):1781-1785. This is a retrospective
radiographic study done blindly and in a random fashion to assess the
concordance rates between the interpretations of the two radiographic
studies in 20 patients.
SM, Ducker TB, Raycroft J. Trends and complications in cervical spine
surgery: 1989-1993. J Spinal Disord 1997;10(6): 523-526. Data collection on 4,589 patients operated on by 35 surgeons is reviewed to assess diagnosis, procedure, and complications.
RN, Lang JE, MacEwen GD. Klippel-Feil syndrome: a constellation of
associated anomalies. J Bone Joint Surg 1974;56A:1246. This
is an evaluation of 50 patients with Klippel-Feil syndrome to evaluate
associated anomalies. Less than half had the classic triad, more
than half had scoliosis, and a third had renal anomalies. All patients
with Klippel-Feil syndrome were found to be at risk for having other
serious but less apparent anomalies including the Sprengel deformity,
impairment of hearing, and congenital heart disease.
chapter is the best single reference for reviewing Klippel-Feil
syndrome. The triad of short-neck, low posterior hairline, and limited
range of motion, as well as other clinical findings in Klippel-Feil
syndrome are discussed thoroughly. The history, embryology, associated
problems, natural history, and treatment are also discussed.
SW, Sarwark JF, Vora A et al. Evaluating congenital spine deformities
for intraspinal anomalies with magnetic resonance imaging. J Pediatr
Orthop 2001;21:525. This study looking at
multiple and congenital spine deformities found that 32% of their
patients had no symptoms although there was intraspinal pathology found
on MRI. It is their recommendation that all patients with congenital
deformity as torticollis have an MRI.
G, Babini JC, Maldonado-Cocco JA et al. Radiologic review: the cervical
spine in juvenile rheumatoid arthritis. Semin Arthritis Rheum
1988;17:185. This is a good radiographic review
of involvement of the cervical spine in juvenile rheumatoid arthritis.
The most common radiographic abnormality found was apophyseal joint
fusion, with paraspinal calcifications and growth disturbance being
next in frequency. About 20% of patients in this study of 120 had
atlantoaxial subluxation or odontoid erosion.
RN, DeVito PD, Ragsdale CG. Changes in the cervical spine in juvenile
rheumatoid arthritis. J Bone Joint Surg 1986;68A:189. This
article sought evidence of disease in the cervical spine in 121
patients with juvenile rheumatoid arthritis. The authors reported that
clinical stiffness and radiographic changes occurred most commonly in
patients with polyarticular-onset disease and systemonset disease.
Despite extensive roentgenographic involvement of the cervical spine,
neck pain was not a common complaint.
SD, Dodge LD, Buhlman HH et al. Rheumatoid arthritis of the cervical
spine: a long-term analysis with predictors of paralysis and recovery.
J Bone Joint Surg 1993;75A:1282-1297. This is an
analysis of radiographic parameters that may be predicative of
neurologic deterioration in patients with cervical disease due to
rheumatoid arthritis. It reinforces the use of the posterior atlanto
dems interval (PADI less than 14 mm) as an indication for surgical
intervention.
AT, Crockard HA, Pringle J et al. Rheumatoid arthritis of the cervical
spine: current techniques for management. Orthop Clin North Am
2002:33(2):291-309. This is a review article offering an algorithm for treatment decision in the cervical patient affected by rheumatoid arthritis.
RB, Dodge L, Bohlman HH et al. Postmortem neuropathelogic analysis of
eleven patients with paralysis secondary to rheumatoid arthritis of the
cervical spine. Orthop Trans 1988;12:54. In this
study 10 of 11 patients with cervical myelopathy due to rheumatoid
disease were identified as having cervical cord compression as their
main cause of death on postmortem study.
article summarizes the radiographic involvement of the cervical spine
in rheumatoid arthritis and focuses on the use of special studies such
as CT and MRI in evaluating these patients both for patterns of
involvement as well as in treatment.
excellent review article covering the various common definitions,
clinical manifestations, natural history, and treatment options.
KD, Hilibrand AS, Palumbo MA et al. Diagnosing basilar invagination in
the rheumatoid patient: the reliability of radiographic criteria. J
Bone Joint Surg 2001:83A(2):194-200. This article
analyzed cervical radiographs of 131 rheumatoid patients to assess them
for basilar invagination using a variety of radiographic measurement.
It offers insight into which ones appear to be the most reliable and
directive in further radiographic assessment.
