Ankylosing Spondylitis
arthritis of the spine with an unknown etiology. It affects about 0.2%
to 0.3% of the U.S. population and is more common in men than women. It
presents in its early stages with inflammatory arthritic pain typically
involving the sacroiliac joints that spreads to involve other portions
of the spine. Early on, there is normal or mildly limited range of
motion. As the disease progresses, however, with ossification of the
spinal ligaments, the spine eventually may fuse in a kyphotic position.
This can involve the lumbar, thoracic, and cervical areas of the spine.
It also may affect the hip joints.
by erosion and sclerosis of the bone adjacent to the sacroiliac joints.
Occasionally, this erosive sclerotic process extends into the
intervertebral disc and adjacent bone, and is termed spondylodiscitis.
It has a reported incidence of 5% to 6% and is most common in the lower
thoracic spine. Spondylodiscitis frequently is asymptomatic, noted on
routine radiographic studies, but it may become symptomatic with minor
injury or stress.
rheumatoid arthritis, with a different serology. Rheumatoid arthritis
is more common in women and tends to affect the joints of the
appendicular skeleton, whereas ankylosing spondylitis is more common in
men and usually affects the spine and major joints. The following
features commonly are used for the diagnosis of ankylosing spondylitis:
-
Pain and stiffness begin in the
sacroiliac joints and subsequently spread to the lumbar, thoracic, and
cervical regions. The symptoms are of at least 3 months’ duration and
are improved by exercise but not relieved by rest. -
Spinal motion in the coronal and sagittal planes becomes limited.
-
There is decreased chest expansion relative to normative values for age and sex.
-
Radiographic evidence of arthritic
changes in the sacroiliac joints is considered the hallmark of
ankylosing spondylitis. In addition, there is ossification of the
ligaments of the spine and squaring of the lumbar vertebrae. -
As the disease progresses, spinal
deformity may result from loss of the normal cervical and lumbar
lordosis and increasing thoracic kyphosis, resulting in flexion
deformity of the spine. It also may affect the hip joints. -
The HLA-B27 antigen test is positive in 90% of patients.
the spine may occur in patients with ankylosing spondylitis. Despite
emphasis on early recognition and current advances in medical
treatment, patients still are seen with advanced kyphotic deformities
of the trunk, who are severely disabled and who present a major
challenge for definitive surgical correction.
-
Smith-Peterson type (removal of a V-shaped wedge of bone from the posterior spinal column)
-
Thomasen type (removal of bone from all
three spinal columns through a posterior approach by a combination of
laminectomy, pedicle resection, and posterior decancellation of the
vertebral body, also called pedicle subtraction osteotomy)
osteotomy for ankylosing spondylitis in 1945. This is the first
description of surgical correction for kyphotic deformity in ankylosing
spondylitis. The initial procedure as reported by Smith-Peterson et al
was done under general anesthesia with the patient lying prone. This
procedure was revised further by LaChappelle, Herbert, Nunziata, Wilson
and Turkell, Law, and others. To avoid difficulties with the use of the
prone position for a patient with kyphotic deformity, Adams recommended
that surgery be done with patients on their sides, and he used a
three-point rack to manipulate the spine for correction.
to perform a single-stage posterior wedge resection of the midlumbar
spine in a “V” fashion with controlled fracturing of the ossified
anterior longitudinal ligament. A midline resection was carried upward
and outward through the superior facet of the vertebrae above and the
inferior facet of the vertebrae below in an oblique fashion. The
obliquity of the osteotomy was to allow locking of the vertebrae after
correction in an effort to prevent displacement. This technique is the
basis for our current procedure.
deformity of the spine occurs primarily in the cervical region. This
deformity can be severely disabling with restriction of the field of
vision. Multiple, undiagnosed, healed fractures of the cervical spine
are often the cause of flexion. Surgical correction is fraught with
great potential hazards. It was reported that isolated attempts to
correct this deformity under general anesthesia resulted in a high rate
of disastrous neurologic complications. The current technique of
correction under local anesthesia has allowed for satisfactory
correction with relative safety.
osteotomy to be done from a single-stage posterior approach in the
lumbar or cervical spine and allow for a high degree of correction to
be obtained in a safe manner with the least morbidity to the patient.
The results can be gratifying in terms of overall improvement in
functional status and quality of life.
is the normal center of lumbar lordosis, below the termination of the
conus medullaris. The spinal canal volume is relatively capacious at
this level. These factors decrease the neurologic risk of an osteotomy
at L3-4 compared with more proximal levels, where the presence of the
distal spinal cord and conus within the spinal canal increases the risk
of neurologic injury. A computed tomography (CT) scan should be
obtained to evaluate the spinal canal preoperatively and to assess for
spinal stenosis.
done at L3-4 or L4-5 are the increased mobility of the aortic
bifurcation and iliac arteries related to lower limb motion. The
reasons for greater vascular risk of osteotomies at higher levels are
that the aorta becomes less mobile proximally; the renal arteries arise
at L2-3, tethering the aorta; and the segmental vessels increase in
size proximally.
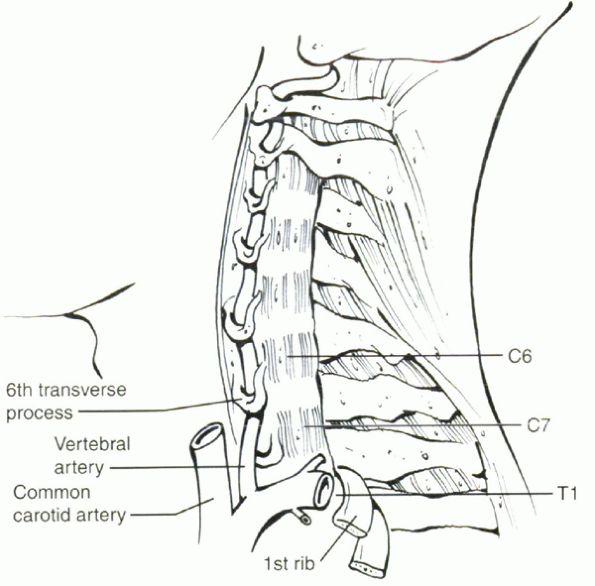
in the cervical spine. The cervical osteotomy is carried out at C7-T1,
which is just below the entry point of the vertebral arteries at C6 and
above the fixed thoracic spine. Because it is at the base of the neck,
it also provides for the maximal amount of head position correction per
osteotomy angle (this being a geometric part of the longer lever arm of
action). This site protects the vertebral arteries from the likelihood
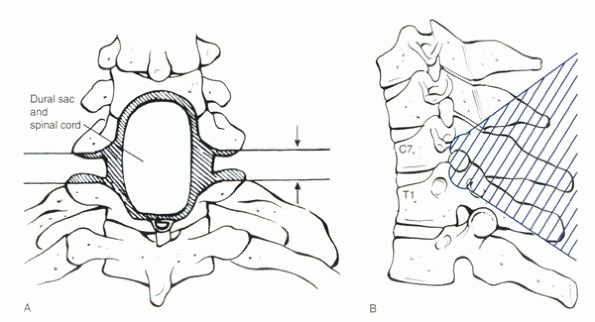
of injury during osteotomy (Fig. 23-1). The
spinal canal of C7-T1 is relatively spacious, and the cervical spinal
cord and the eighth cervical nerve roots have reasonable flexibility.
Injury to the C8 nerve root also would cause less disability than
injury to more proximal cervical nerve roots.
deformities leading to impairment of the visual field to see ahead
(horizon), difficulty with personal hygiene, and compromised function.
Difficulty with swallowing is common. The most severe case of this is
the “chin on chest” deformity. Because cervical osteotomy has high
potential risks, it is most important that the patient must have the
earnest desire to accept these risks and the rehabilitative measures
required for correction.
 |
|
Figure 23-1
Diagram showing position of vertebral artery and veins in front of the transverse process of the seventh vertebra entering into spine through transverse foramen of the sixth vertebra. (From Simmons EH. The cervical spine in ankylosing spondylitis. In: Bridwell KH, DeWald RL, eds. The textbook of spinal surgery, 2nd ed. Vol 1. Philadelphia: Lippincott-Raven, 1997:1144, with permission.) |
correction of lumbar hypolordosis or kyphosis giving rise to a fixed
flexion deformity. The indications are variable and depend on the
extent of the deformity, the degree of functional impairment, the age
and general condition of the patient, the feasibility of correction,
and the commitment of the patient to the risks and necessary
rehabilitation measures.
spondylitis usually does not reach proportions that require surgical
correction. Combined anterior and posterior approaches are necessary.
The diaphragm must not be violated because these patients breathe
solely with their diaphragms owing to absence of motion through the
costovertebral joints.
who are not suitable candidates for medical reasons and patients in
whom the severity of the deformity does not warrant the procedure.
Severe osteopenia also is a relative contraindication.
Although all areas of the spine may be involved, there is usually one
particular region that is primarily responsible for the overall
malalignment and functional handicap. If any major correction is to be
attempted, the correction must be done at the site of the main
deformity.
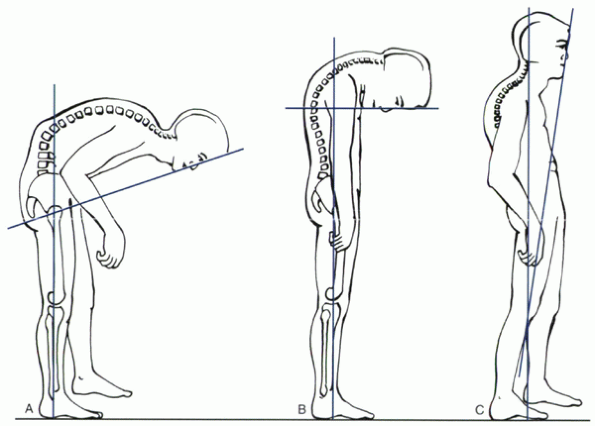
are required in planning surgical treatment and in evaluating its
results. The most effective and consistent measure of trunk flexion
deformity is the chin-brow to vertical angle. This is a measure of the
angle from a line extending from the chin to the brow measured to the
vertical, when the patient stands with the hips and knees extended and
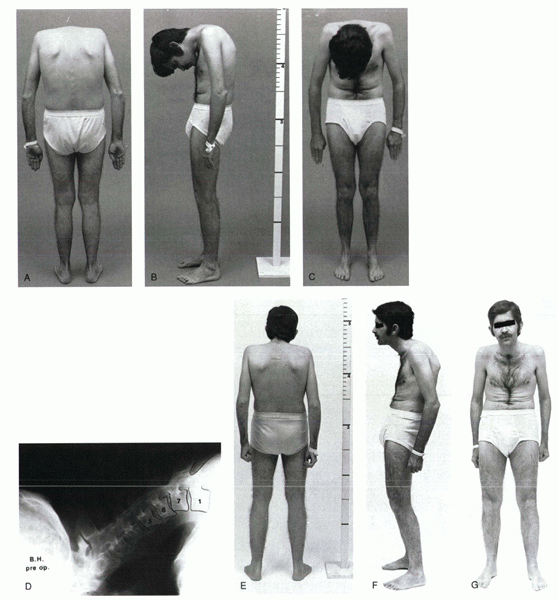
the neck in neutral or fixed position (Fig. 23-2).
Based on this measurement, the size of the wedge in the spine to be
removed posteriorly is determined. For lumbar flexion deformity, this
angle is transposed to a lateral radiograph of the lumbar spine with
the apex of the angle at the posterior longitudinal ligament of the
L3-4 disc space.
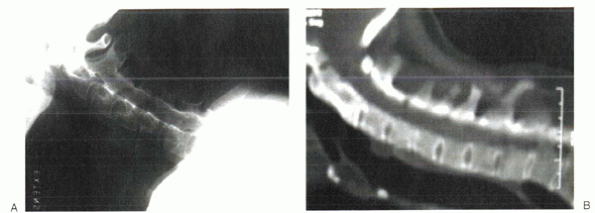
anteroposterior, neutral, flexion/extension lateral (if any motion
persists), and swimmer’s views. These radiographs outline the shape and
size of the spinous processes of C6, C7, and T1, allowing these
processes to be recognized more readily at surgery (Fig. 23-3A).
Flexion/extension lateral radiographs rule out the presence of
instability at the craniocervical junction. A CT scan centered at the
C7-T1 level should be obtained preoperatively. The CT scan provides
evidence of previous compression fracture and allows assessment of the
size of the spinal canal at the proposed site of osteotomy so that any
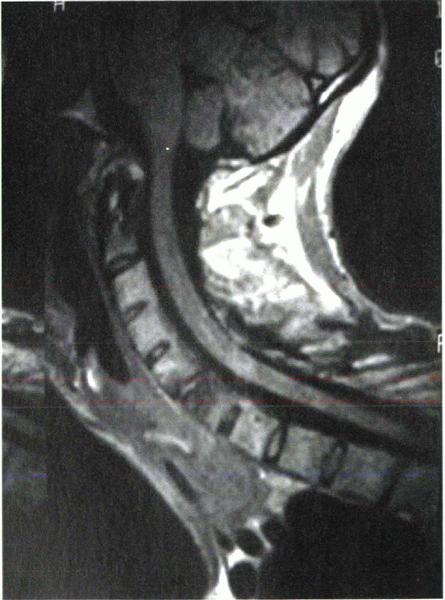
area of stenosis can be decompressed adequately (Fig. 23-3B). In addition, preoperative magnetic resonance imaging may be considered for complex cases (Fig. 23-4).
 |
|
Figure 23-2
The chin-brow to vertical angle is used to measure the degree of flexion deformity of the spine in ankylosing spondylitis, which is from the brow to the chin to the vertical line with the hips and knees extended and the neck in its fixed or neutral position. (A) For thoracolumbar deformity. (B) For cervical deformity. (C) For postoperative assessment. (From Hammerberg KW. Ankylosing spondylitis, and Simmons EH. The cervical spine in ankylosing spodylitis. In: Bridwell KH, DeWald RL, eds. The textbook of spinal surgery, 2nd ed. Vol 1. Philadelphia: Lippincott-Raven, 1997:1114, 1136, with permission.) |
pulmonary function tests and electrocardiography. Many patients have
concomitant medical illnesses and cardiac problems and must be
evaluated carefully preoperatively from a medical standpoint. A
physiotherapy program of deep breathing and extremity exercises is
given, as will be used postoperatively. Psychological preparation
includes preoperative visits by the anesthesiologist and the surgeon,
to explain the whole procedure to the patient and gain his or her
confidence.
patient is positioned on the operating table prone in the knee-chest
position. The position is adjusted until the patient is comfortable,
avoiding any strain on the neck or elsewhere. Spinal cord monitoring is
done throughout the procedure.
It
is important to have valid preoperative tracings for comparison with
findings during surgery. When the hips are extended to produce anterior
osteoclasis with extension of the lumbar spine, the knees should be
kept flexed to avoid any sciatic nerve tension that would alter the
evoked spinal responses if posterior tibial nerve stimulation is used
at the ankles.
 |
|
Figure 23-3 (A) Lateral radiograph of a patient with cervical flexion deformity. (B) Lateral CT scan of the cervical spine of the same patient showing the spinal canal.
|
monitoring are done throughout the procedure. A wake-up test also can
be used if necessary. Pulse oximetry, carbon dioxide analyzer, and
systemic blood gases are used to monitor the patient. A Doppler
apparatus is fixed to the patient’s chest to detect any possible air
embolisms.
 |
|
Figure 23-4
Lateral magnetic resonance imaging of the cervical spine of a patient with cervical flexion deformity showing the spinal canal and cord. |
described earlier), the patient is placed in the prone position on an
adjusted Tower or Andrews table. The patient must be positioned
carefully on the operating table in a flexed knee-chest position.
Careful positioning also is necessary because these patients have fixed
ankylosed spines, and undue pressure in any one particular area must be
avoided. The thoracic chest support often must be elevated considerably
to accommodate the patient on the operating table.
exposure is made, and the proposed osteotomy site is confirmed
radiographically because operative localization is difficult owing to
the fused confluent nature of the posterior elements of the spine.
usually are ossified, and the osteotomy can be started with large bone
cutters to trim away the intervening bone and spinous processes in a
V-shaped fashion. The laminae can be thinned out with Leksell rongeurs
and the bone fragments maintained for autogenous bone graft. A
high-powered bur can be used alternatively; however, if this is used
exclusively, less bone is available for the bone grafting.
carefully from the bone with a seeker and protected with cottonoid
patties. In many long-standing cases, the dura is atrophic, similar to
that of long-standing spinal stenosis. Rarely the dura may be adherent
to the laminae, making its separation difficult. The entire L4 lamina
is removed along with a portion of the L3 and L5 laminae with
undercutting of the laminae to bevel them so that there is no
impingement on closure of the osteotomy site. The cauda equina must be
decompressed well laterally out to the level of the pedicles. The
entire superior L4 facet is removed, and the L3-4 neuroforamina are
exposed widely laterally and undercut with a medium-angle Kerrison
rongeur to prevent any impingement on closure of the osteotomy site.
to arrive at the amount of correction desired. On closure of the
osteotomy with osteoclasis of the spine anteriorly, the lateral masses
should meet with good bone surface contact. The pedicles also must be
undercut, removing the superior edge of the L4 pedicle and inferior
edge of the L3 pedicle to allow adequate room for the nerve root during
extension of the spine.
in L1, L2, L3, L5, and S1. The pedicle screws are inserted in a
standard fashion, using anatomic and image-guided techniques as
required. It is not usually possible to have screws in L4 because they
impinge on the L3 screws after extension correction of the spine.
of the table, bringing the hips and thighs up into an extended
position. On doing so, pressure also can be applied manually by pushing
downward at the L3-4 site, causing a fulcrum for the osteoclasis to
occur. An audible and palpable osteoclasis of the spinal column often
is present, and the lateral masses then come together in apposition.
The lower extremities and hips now are kept in an extended position,
preferably with the knees flexed, so as to avoid any tension on the
sciatic nerve roots. Rods are cut and contoured to the appropriate
length and shape for each side of the spine, then fitted into the
pedicle screws and secured (Fig. 23-5). Posterolateral and posterior bone grafting is done using the autologous local bone graft fragments from the decompression.
 |
|
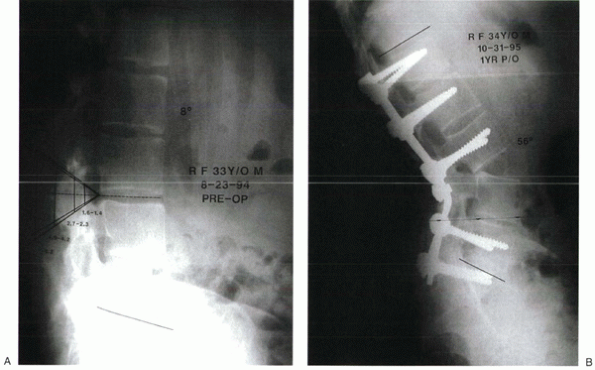
Figure 23-5
The chin-brow angle of a patient with lumbar flexion deformity was 70 degrees, and the lumbar lordosis was decreased to 8 degrees. (A) Lateral radiograph of lumbar spine showing the measured angle superimposed with the apex at the L3-4 disc space. (B) Postoperative lateral radiograph shows the angle of correction obtained after closure of the resected defect posteriorly with an opening anterior osteoclasis at the L3-4 disc level. Pedicle screws are placed bilaterally at L1, L2, L3, L5, and S1 with rods. The 56 degrees of normal lumbar lordosis has been created with solid fusion mass. (C and D) Diagrams showing areas of posterior resection for L3-4 osteotomy and pedicle screw fixation with osteoclasis. |
head to knee. The patient is strapped into the shell and transferred in
the shell to a Roto-rest bed. This is an essential part of the
procedure.
is more prominent than the pelvis, and if the patient is lying on a
flat surface, forces tend to push the thorax forward and allow the
pelvis and lower lumbar spine to move posteriorly. If the trapdoor of
the bed is removed for a bowel movement, the spine would be
unsupported. A well-contoured, padded rigid posterior plastic shell
provides a contoured, well-fitted surface on which the rigid trunk can
lie protecting the osteotomy site. A nasogastric suction tube is placed
before the patient leaves the operating room. It is maintained until
the patient is passing gas, with normal gastric function.
important factor is to correct the deformity completely, shifting the
weight-bearing line posterior to the osteotomy site so that gravity
helps maintain the correction with stimulation of bone formation across
the osteotomy site. Postoperatively the patient is fitted with a
thoracolumbosacral orthosis brace and mobilized with physical therapy.
 |
|
Figure 23-5 (Continued)
|
spine is the possibility of injury to the major vessels, particularly
the abdominal aorta. We reviewed all the reported cases of major
vascular injury associated with resection/extension osteotomy of the
lumbar spine for ankylosing spondylitis, and the level at which the
osteotomy was performed in each case was documented. In all cases, with
injury to the abdominal aorta, the osteotomy was done at T12-L1, L1-2,
or L2-3. There is no reported case of aortic injury with osteotomy
performed at L3-4 or L4-5.
is gastric dilation and abdominal ileus. When the spine is extended
with the costal margin moving away from the pelvis, the superior
mesenteric artery is stretched over the third part of the duodenum,
producing a functional block to the outlet of the stomach, predisposing
to gastric dilation. If this hazard is not anticipated, patients may
vomit a large amount. With a stiff rigid neck in the supine position,
there is a risk of aspiration, which could prove fatal. It is necessary
to have a nasogastric tube in position postoperatively with suction
drainage until intestinal motility is established and the patient is
passing gas.
occur. Major neurologic problems are relatively infrequent but can be a
major problem when they occur. Potential complications specific to this
procedure include intraspinal hematoma, intestinal obstruction,
problems related to instrumentation due to osteopenia, and difficulty
with surface landmarks in terms of inserting the instrumentation.
Removal of too little or too much bone posteriorly can result in too
little or too great a correction. Careful preoperative planning is
necessary to determine the amount of correction desired and the
appropriate amount of bone removal.
-
The nasogastric tube always should be
left in place postoperatively for at least several days, until proven
intestinal motility has occurred. Failure to do so may result in emesis
and aspiration due to the inability of the patient to rotate the neck
and clear the airway. -
Extra assistance usually is required at
the time of the osteoclasis to assist in extending the hips and
repositioning the patient adequately on the operating table. -
The positioning of the patient must be
evaluated carefully before, during, and after the procedure to be
certain there is no undue pressure on the facial area or eyes and there
is appropriate padding and positioning of the upper extremities.
cervical spine may place increased stress at the craniocervical
junction. Inflammation may cause erosion of the transverse ligament and
associated hyperemia at its bony attachments. As these conditions
progress, atlantoaxial subluxation and dislocation may occur.
-
Gallie technique with a modified H graft (most commonly used) (Fig. 23-6)
-
Brooks technique with a bone block graft and sublaminar wires
-
Transarticular fixation with screws (Fig. 23-7)
-
Halifax clamp-type device
cause of progressive flexion deformity. Sudden pain with minor trauma
(e.g., car accident), with or without forward flexion of the cervical
spine, often indicates a fracture even though the trauma was relatively
trivial. An undiagnosed fracture can go on to settle and heal in a
forward flexed position. When such a fracture is recognized, a halo
should be applied with traction to restore the alignment of the head
and the neck to its prefracture position.
If the head was in a previously flexed position, pulling it with
traction into a neutral alignment may cause neurologic injury. When the
appropriate alignment has been obtained, the patient should be
immobilized in a halo vest for 4 months. A high union rate is
associated with this protocol. If pseudarthrosis develops, posterior
fusion or anterior cervical fusion can be undertaken.
 |
|
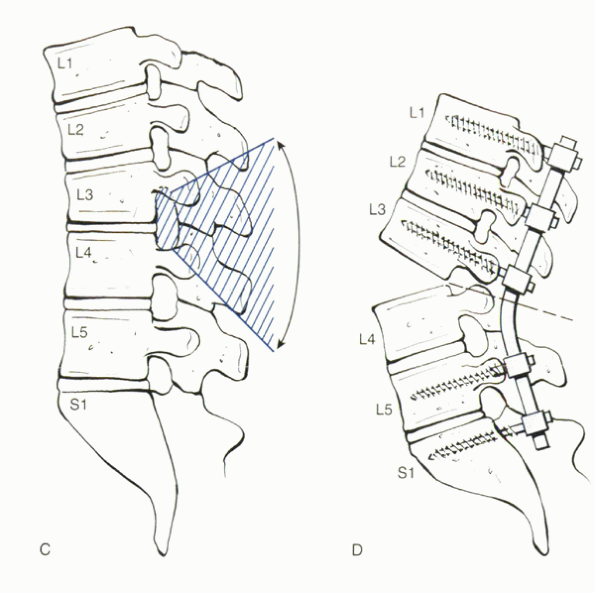
Figure 23-6
Gallie fusion. The graft is harvested from the posterior iliac crest and fashioned to allow maximal bony contact with C1 and C2. Posterior view shows the graft in position. The loop of wire shown has been passed under the posterior arch of C1, then is pulled inferiorly over the C1 lamina and graft and around the C2 spinous process, which must be preserved. The free ends of the wire are crossed over the graft and twisted. (Modified from Drummond DS. Congenital anomalies of the pediatric cervical spine. In: Bridwell KH, DeWald RL, eds. The textbook of spinal surgery, 2nd ed. Vol 1. Philadelphia: Lippincott-Raven, 1997:965, with permission.) |
intravenous sedation, with the patient awake and in the sitting
position using a dental chair. This approach allows the best form of
active spinal cord monitoring and immediate assessment of the patient’s
vital functions and neurologic status. A halo-vest is applied to the
patient preoperatively, and a 9-lb weight of traction is applied in
direct line with the neck to stabilize the head throughout the
procedure.
pulse oximetry, carbon dioxide analyzer, and systemic blood gases are
used for patient monitoring. A Doppler apparatus is fixed to the
patient’s chest to detect any possible air embolisms. The
anesthesiologist may administer oxygen to the patient during the
procedure by a facemask or nasal catheter. The patient is allowed to
listen to the radio or other music throughout the procedure and usually
converses with the anesthesiologist.
posterior portion of the angle is centered over the posterior arch of
C7. This site is below the entry point of the vertebral arteries, which
typically enter at the foramen transversarium at C6. This approach
protects these vessels from the likelihood of injury during osteotomy
at C7-T1. The spinal canal of C7-T1 is relatively spacious, and the
cervical spinal cord and the eighth cervical nerve roots have
reasonable flexibility. Also, any injury to the C8 nerve root would
cause less disability than injury to other cervical nerve roots.
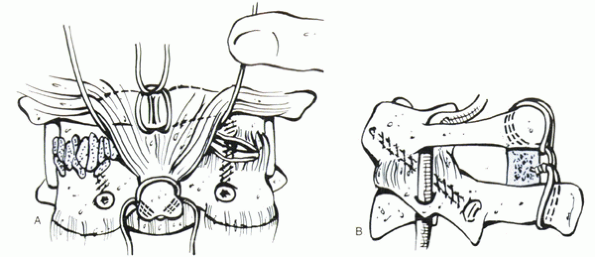
portion of C6 and the superior portion of T1 are removed. The eighth
cervical nerve roots are identified at the C7-T1 neuroforamen and are
decompressed widely, removing the overlying bone at the foramen,
decompressing widely laterally through the lateral recesses (Fig. 23-8).
Kerrison rongeur to allow ample room for the eighth cervical nerve root
when the osteotomy site is closed. The amount of bone to be resected is
assessed carefully preoperatively and intraoperatively to avoid any
compression of the nerve roots on closure of the osteotomy. The
residual portions of the laminae of C6 and T1 must be beveled carefully
and undercut to avoid any impingement or kinking of the spinal cord on
closure of the osteotomy site.
procedure is done. The patient is given an intravenous dose of
short-acting barbiturate, usually methohexital sodium (Brevital Sodium)
or thiopental sodium (Pentothal). The surgeon grasps the halo and
brings the neck into an extended position, with closure of the
osteotomy site posteriorly as the osteoclasis occurs anteriorly. An
audible snap and sensation of osteoclasis usually are noted. The
lateral masses and osteotomy site laterally should be well
approximated. With the surgeon holding the head in the corrected
position, the assistants attach the vest to the halo with the upright
supports anteriorly.
at the C7-T1 area, then autogenous bone graft is packed on each side
over the decorticated areas. The local bone removed from the posterior
decompression is used for the bone graft.
 |
|
Figure 23-7 C1-2 transarticular fixation and posterior interspinous bone block graft and wiring. (A) After reduction, transarticular C1-2 screws are placed, and joints are packed with cancellous bone. (B)
Lateral view of the transarticular technique. Fixation and grafting are enhanced by an intraspinous graft as shown here. (From Aebi M. Surgical treatment of cervical spine fractures by AO spine technique. In: Bridwell K, DeWald RL, eds. The textbook of spinal surgery. Philadelphia: JB Lippincott, 1991:1086, with permission.) |
 |
|
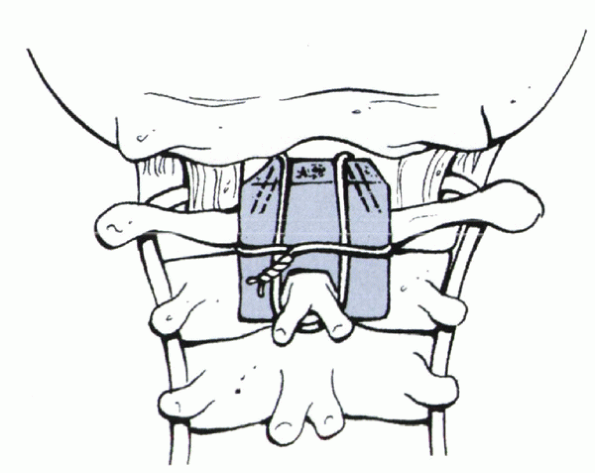
Figure 23-8 (A)
Diagrammatic outline of the posterior view of the area of cervical resection. The lines of resection of the lateral fused joints are beveled slightly away from each other, extending posteriorly so that the two surfaces are parallel and in apposition after correction. The pedicles must be undercut to avoid impingement on the C8 nerve roots. The midline resection is beveled on its deep surface above and below to avoid impingement against the dura after extension correction. (B) Lateral diagram of the area of resection. (Modified from Simmons EH. The cervical spine in ankylosing spondylitis. Bridwell KH, DeWald RL, eds. The textbook of spinal surgery, 2nd ed. Vol 1. Philadelphia: Lippincott-Raven, 1997:1143, 1144, with permission.) |
 |
|
Figure 23-9 (A)
Posterior view of a man with rigid flexion deformity of the cervical spine of such magnitude that the head is not visible from behind. (B) Lateral view shows his chin rigidly fixed against his chest, with marked restriction of the field of vision and interference with the ability to open his mouth. (C) Anterior view shows complete restriction of the field of vision. (D) Lateral view x-ray of cervical spine shows complete ossification of posterior joints and previous subluxation of C6-7. (E-G) Postoperative posterior, lateral, and anterior views of patient shows correction of deformity with nearly normal chin-brow to vertical angle. (From Simmons EH. The cervical spine in ankylosing spondylitis. In: Bridwell KH, DeWald RL, eds. The textbook of spinal surgery, 2nd ed. Vol 1. Philadelphia: Lippincott-Raven, 1997:1148, with permission.) |
|
TABLE 23-1 THE KEY POINTS OF SINGLE-LEVEL CERVICAL AND LUMBAR OSTEOTOMY
|
|||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
upright supports also are connected to the halo, and these all are
secured fully.
to a revolving circular (CirOlectric) bed, which is in a vertical
position. The bed can be tilted to the horizontal position, and the
patient is taken to the surgical intensive care unit. When the patient
is sufficiently mobile to get in and out of a regular bed, he or she is
transferred to a regular bed with or without a trapeze attachment. The
patient is instructed to leave the vest and halo intact and is left in
this for 4 months. When the vest and halo are removed, lateral
tomography or CT evaluation centered at C7-T1 is necessary to evaluate
the radiographic union. Further bracing with a sternal occipital
mandibular immobilization brace can be done for an additional 2 months (Fig. 23-9).
If osteotomy is performed proximal to C7, injury to the vertebral
arteries may occur. If osteotomy is performed below C7-T1, little or no
correction is obtained. Radiographic confirmation always is necessary.
Other pitfalls include inadequate or excessive removal of bone,
resulting in too little or too great correction.
the region of the osteotomy and result in kinking of the spinal cord.
If this problem is noted, the dura can be opened carefully to relieve
compression. Most C8 nerve root problems resolve as long as they are
partial. Some postoperative distraction through the halo vest can be
carried out if C8 nerve root compression is noted postoperatively.
because this surgery is performed in the sitting position. A Doppler
monitor with sound amplification is fixed to the patient’s chest
preoperatively and can be monitored during the procedure. To prevent
air embolisms, the wound should be filled with irrigation fluid and wet
sponges during procedure.
A. Ankylosing spondylitis. In: Kelly WN, Harris ED, Ruddy S, Sledge CB,
eds. Textbook of rheumatology. Philadelphia: WB Saunders, 1981:1017.
JJ. Vertebral osteotomy for kyphosis, especially in Marie-Strumpell
arthritis: a report on 50 cases. J Bone Joint Surg 1959; 41A:291.
EH. Osteotomy of the lumbar spine for correction of kyphosis in a case
of ankylosing spondylarthritis. J Bone Joint Surg 1959;28A:270.
ED, Capicotto PN. Clinical cervical deformity and postlaminectomy
kyphosis. In: White AH, Schofferman JA, eds. Spine care. St. Louis:
Mosby, 1995:1633-1650.
MR. Osteotomy of the cervical spine: report of a case of ankylosing
rheumatoid spondylitis. J Bone Joint Surg 1958;40A:833-843.
