Distal Femur Fractures
fractures, fractures of the distal femur present considerable
challenges in management. No single method of management has overcome
all of the problems associated with these injuries. Before 1970, most
supracondylar fractures were treated nonoperatively; however,
difficulties were often encountered, including persistent angulatory
deformity, knee joint incongruity, loss of knee motion, and delayed
mobilization (especially in patients with multiple injuries).22,34,43,58
During the past few decades, as operative techniques and technology
have improved, most surgeons have favored internal fixation for the
management of displaced distal femoral fractures.* The
surgical goals of treatment are anatomic reduction of the articular
surface, restoration of limb alignment, length, and rotation, and
stable fixation that allows for early mobilization. Nonetheless,
internal fixation of the distal femur can be difficult for several
reasons. Thin cortices, a wide medullary canal, relative osteopenia,
and fracture comminution make stable internal fixation difficult to
achieve. Although better methods of fixation have dramatically improved
clinical results, the operative management of these difficult fractures
is not uniformly successful.
is thought to be axial loading with varus, valgus, or rotational
forces. A bimodal distribution of high-energy injuries in
younger
patients and low-energy elderly patients is typically seen with these
injuries, but those lines are less distinct as high-energy injuries in
elderly patients become more common. In younger patients, these
fractures typically occur after high-energy trauma related to motor
vehicle or motorcycle accidents. In these patients there may be
considerable fracture displacement, comminution, open wounds, and
associated injuries. On the other hand, in elderly osteoporotic
patients, fractures frequently occur after a minor slip and fall on a
flexed knee, leading to fragility fractures through compromised bone.
Notching of the anterior cortex of the distal femur while making
femoral chamfer cuts during knee arthroplasty may predispose the distal
femur to fracture.54,62
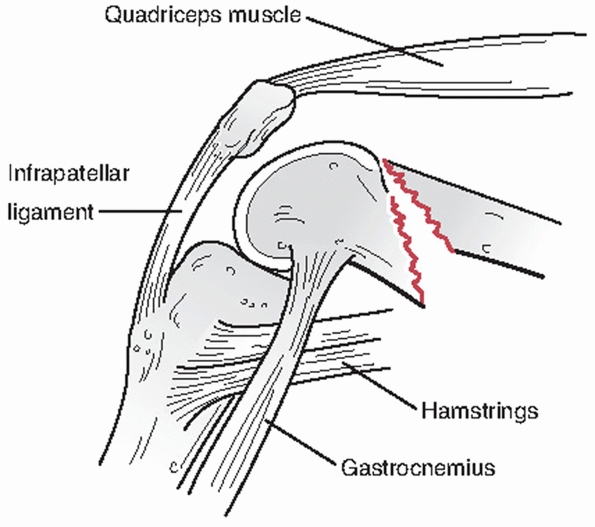
are produced primarily by the direction of the initial fracture
displacement and secondarily by the pull of the local musculature (Fig. 51-1).
Spasm and irritability in the quadriceps and hamstrings often lead to
limb shortening with varus angulation at the fracture site as a result
of the strong pull of the adductor muscles. Contraction of the
gastrocnemius often produces apex posterior angulation and displacement
of the distal fragment. In fractures with intracondylar extension,
soft-tissue attachments to the respective femoral condyles tend to
produce splaying and rotational malalignment of the condyles that
contributes to joint incongruity. These are the forces that fracture
reduction and the stabilizing implant must overcome and resist if an
anatomic outcome is to be achieved.
fracture the distal femur may produce additional injuries in the same
extremity and to other body parts. Because these injuries often result
from moderate to high-energy trauma, associated nonskeletal injuries
are common. These injuries and their sequelae (e.g., pulmonary
problems), may delay definitive fracture fixation for days or weeks.
This delay may increase the technical difficulty of the procedure,
contributes to patient morbidity, and may compromise the full benefits
of internal fixation. Temporizing external fixation has been used
effectively in these circumstances to stabilize the fracture, prevent
further soft-tissue trauma to the area, and allow for patient
mobilization.
mechanism, ipsilateral hip and femoral shaft fractures are fairly
common and complicate treatment. Furthermore, in up to 50% of these
patients there is diaphyseal fracture extension of the distal femur
fracture.71 Same-sided injuries to
the tibia, ankle, and foot are quite common. Five to ten percent of
distal femur fractures are open injuries. The site of the open wound is
usually over the anterior thigh proximal to the patella, leading to
damage to the quadriceps muscle and extensor mechanism. Although the
femoral and popliteal arteries are in close proximity to the distal
femur, vascular injury is less common than in patients with a knee
dislocation. This potentially catastrophic injury must not be
overlooked, and a complete vascular examination is mandatory.
 |
|
FIGURE 51-1 Typical supracondylar femur fracture pattern and deformity.
|
examination must be performed to understand the injury and identify
associated injuries. Significant bleeding into the thigh may occur
after fractures of the distal femur, and evaluation for systemic signs
of shock should be identified and treated aggressively. Collaboration
with a general trauma surgeon and/or medical internist is strongly
recommended when there are significant associated injuries or medical
comorbidities.
fracture crepitans with thigh swelling, limb deformity, shortening, and
external rotation. The skin should be examined for bruising, contusion,
or open fracture. Other injuries to the same extremity should be
suspected when there is pain or swelling in the limb above or below the
fracture site. A careful neurovascular examination including the
presence or absence of distal pulses, as well as a sensorimotor
assessment, should be performed and documented. If there are
differences in distal pulses between the injured and noninjured sides,
or there is suspicion of an occult vascular injury, ankle-ankle indices
should be checked. If the results between sides are within 10%, then
vascular injury is unlikely. Conventional and CT angiography are also
useful tools for evaluating for vascular injury. A gentle reduction and
splinting of the injured limb should be performed early after arrival
to the emergency department, if not already done by prehospital
caregivers.
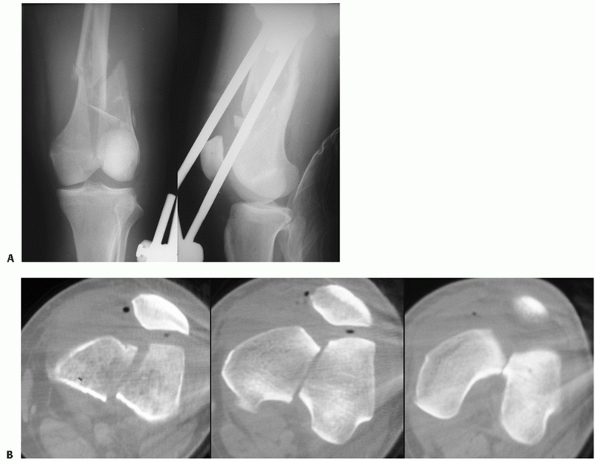
are routinely obtained and are usually sufficient for diagnosis. In
most patients, x-rays of the pelvis, ipsilateral hip, and femoral shaft
are necessary to rule out associated injuries. Additional radiographs
are obtained as dictated by the clinical examination. Traction
radiographs are helpful if there is significant shortening and
deformity and provide a better understanding of the fracture
morphology. This can often be combined with the reduction and splinting
process.
reconstruction of the distal femur are an important adjunct to plain
radiographs and are recommended with most displaced fractures.
Intra-articular injuries can be better delineated and a number of
potentially important occult fractures identified. Nork et al.44
showed a 40% rate of coronal plane or Hoffa’s fractures with
intercondylar fractures, many of which are missed with plain
radiographs alone.35
distal femur fracture and may influence the method of treatment. If
osteoporosis is evident on plain radiographs, a loss of 40% or
more bone density has occurred. These patients should be identified, educated, and treated to avoid future fractures.
 |
|
FIGURE 51-2 OTA classification of distal femur fractures (33A-C).
|
classification for supracondylar fractures of the femur. Essentially
all classifications distinguish among extra-articular, intra-articular,
and isolated condylar lesions. Fractures are further subdivided
according to the degree and direction of displacement, amount of
comminution, and involvement of the joint surfaces. Unfortunately,
anatomic fracture classifications fail to address the conditions
commonly associated with supracondylar femur fractures, which often
influence treatment or outcome. These factors, which play a dynamic
role in management, determine the “personality” of a fracture. Among
these are: (1) amount of fracture displacement, (2) degree of
comminution, (3) extent of soft-tissue injury, (4) associated
neurovascular injuries, (5) magnitude of joint involvement, (6) degree
of osteoporosis, (7) presence of multiple trauma, and (8) complex
ipsilateral injuries (i.e., patella or plateau fractures).
because it is easy to use and applicable to most parts of the skeleton.
It distinguishes among extra-articular (type A), partial articular
(type B), and complete articular (type C) injuries, and accounts for
fracture complexity (Fig. 51-2). A basic
treatment plan for distal femur fractures usually can be formulated
based on this classification system. Because of the large number of
fracture patterns seen in clinical practice, however, some fractures do
not fit neatly into any classification scheme. This emphasizes the fact
that every patient must be individually evaluated, and the
“personality” of the fracture must be considered in selecting the
method of treatment.
with the femoral diaphysis. This comprises approximately the distal 15
cm of the femur, as measured from articular surface. It is important to
distinguish extra-articular fractures from intercondylar, as well as
diaphyseal fractures of the distal femur because the methods of
treatment and prognosis may be considerably different.
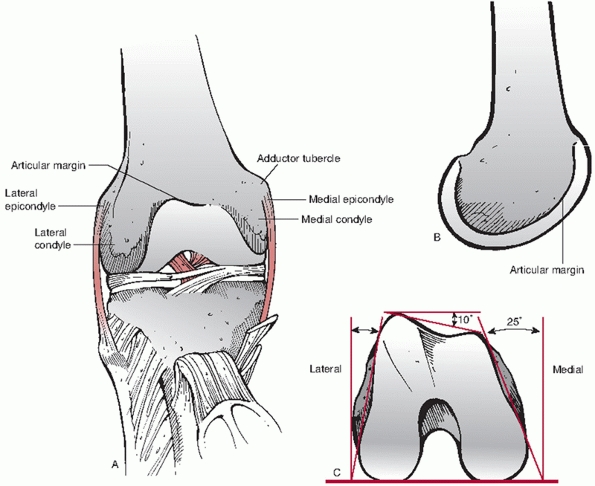
If viewed on end, the shape of the distal femur is trapezoidal
(narrower anteriorly than posteriorly) with an angle of inclination of
the medial surface of about 25 degrees. This becomes important when
placing implants across the condyles from lateral to medial; on AP
radiographs anterior implants that appear of appropriate length may be
too long and cause painful irritation. Anteriorly, the articular
surfaces of the two condyles come together to form a joint for
articulation with the patella. Posteriorly, they are separated by a
deep intercondylar fossa that gives attachment to the cruciate
ligaments of the knee. The contact surface for the patella includes
parts of both condyles, but is derived predominantly from the lateral
condyle. The lateral condyle is broader and extends farther proximally.
The lateral epicondyle arises from the lateral condylar surface, giving
rise to the fibular collateral ligament. Immediately below the lateral
epicondyle is an oblique groove that houses the popliteus tendon. The
medial epicondyle is longer than the lateral condyle and extends
farther distally. Its medial surface is convex and contains an
epicondyle that gives attachment to the tibial collateral ligament.
Situated on the proximal-most part of the condyle is the adductor
tubercle, into which the tendon of the adductor magnus muscle inserts.
 |
|
FIGURE 51-3 A.
Diagram of the distal femur demonstrating the typical condylar anatomy. When instrumenting the distal femur, particular attention must be given to the obliquity of the anterior joint surface (wider laterally than medially, B) and the trapezoidal shape of the condyles when viewed on end (wider posteriorly than anteriorly, C). |
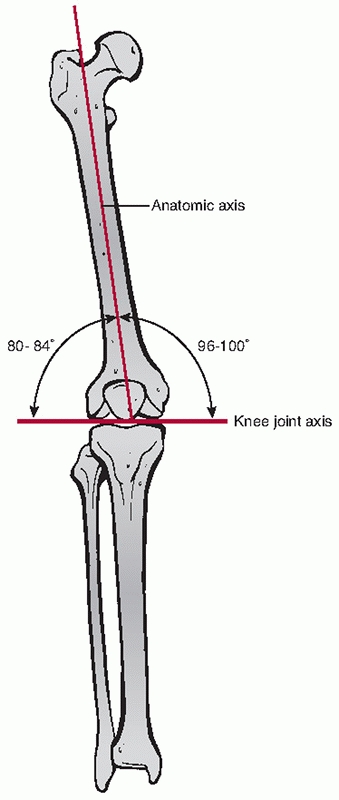
ankle and ground. The anatomic axis of the femoral shaft relative to
the knee averages about 8 degrees of valgus, with some variability
between individuals (range, 5 to 12 degrees) (Fig. 51-4).
The contralateral limb (if not injured) can be used to radiographically
define the limb axis for each person. The expanded femoral and
corresponding tibial condyles are adapted for the direct forward
transmission of weight. During weight bearing, the two condyles rest on
the horizontal plane of the tibial condyles and the shaft of the femur
inclines inferomedially. This inclination is an expression of the
greater width of the body at the hips than the knees.
hip adductors, knee extensors, and knee flexors. The latter two cross
the knee and are integral to its function. Anteriorly the quadriceps
muscles provide power to the knee extensor apparatus and are supplied
by the femoral nerve. The quadriceps muscle distally
becomes
tendon and envelopes the patella and terminates via the patellar tendon
at the tibial tubercle. Posteriorly, the “hamstring” muscles that flex
the knee are supplied by the sciatic nerve. The semitendinosus and
semimembranosus muscles terminate medially and biceps femoris laterally
on the proximal tibia as multiple tendon insertions. The gastrocnemius
muscle bellies also cross the posterior aspect of the knee from their
origin in the supracondylar area.
 |
|
FIGURE 51-4 Typical anatomic limb axis of the femur.
|
the mid-thigh in Hunter’s canal between the extensor and adductor
compartments, beneath the sartorius muscle. The femoral vessels pierce
the adductor magnus approximately 10 cm above the knee to enter the
posterior compartment and join the sciatic nerve in the popliteal
fossa. The popliteal fossa is diamond shaped and is bounded superiorly
by semimembranosus and semitendinosus medially and by the biceps
femoris laterally. The inferior boundaries are the two heads of the
gastrocnemius. At this level, the femoral vessels are renamed the
popliteal artery and vein, and the sciatic nerve has branched into the
tibial and peroneal nerves. In the popliteal fossa, the artery is deep
and medial to the popliteal vein and tibial nerve.
described and one is chosen based on a preoperative plan incorporating
the fracture and soft-tissue injury pattern, patient factors, implant
selection, and surgical experience.42
The patient is positioned supine with a bump beneath the ipsilateral
hip to internally rotate the leg. The skin incision is longitudinal and
distally is centered over the lateral epicondyle. It should be long
enough to allow gentle soft tissue retraction. The length of the
incision should be determined based on the preoperative plan. The
fascia lata is incised in line with its fibers exposing the vastus
lateralis, which is reflected off the intermuscular septum along the
linea aspera in the anterior direction. Perforators are identified and
ligated or cauterized. This careful dissection is started distally and
carried proximally. Wide soft tissue stripping is avoided and no
soft-tissue dissection should be performed on the medial side of the
femur to minimize disruption of the soft tissues.2,37
Visualization of the articular surface of the lateral condyle is
satisfactory, but exposure of the intercondylar notch and medial
condyle are more limited. When more access to the joint is needed, the
incision can be extended distally and curved medially to allow for
greater patellar subluxation. Occasionally a tibial tubercle osteotomy
can be performed to allow for reflection of the extensor mechanism and
wide articular exposure.38 Knee flexion must be restricted for a period of time after tibial tubercle osteotomy; thus its use has been limited.
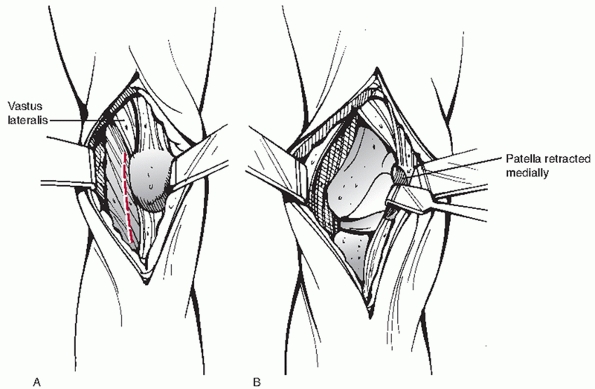
repair of intercondylar fractures (type C), the authors favor using a
modification of lateral parapatellar arthrotomy (Fig. 51-6).67
This provides adequate access to the articular surfaces (although
perhaps not quite as much as tibial tubercle osteotomy), and can be
extended proximally into the quadriceps mechanism as an extensile
anterolateral approach to include the femoral shaft. The extensor
mechanism is divided longitudinally not horizontally; thus, concerns
about its repair failing or additionally restricting mobility are
minimized. The vastus lateralis is elevated off the lateral femoral
cortex as in the standard lateral approach. Both reduction and
stabilization of the condyles, as well as plate application and
fixation, can be applied through this approach. Medial soft tissue
dissection should be avoided. In some cases, an approach that is open
distally and proximally can be used in which the plate and screws are
fitted and fixed directly in these areas, but the intermediate tissues
are mobilized only by the submuscular plate insertion. This approach
may provide the enhanced biology of minimally invasive methods while
still allowing the surgeon to be confident in plate placement and allow
for direct screw insertion.
plating of selected distal femur fractures, a 5- to 6-cm lateral
incision limited to the area of the lateral condyle and distal
metaphysis is used.8,30,31
The incision is placed more distal to allow for retrograde submuscular
plate insertion. Condylar screws are placed through the incision used
for plate insertion. Proximal
screws
are placed using multiple stab incisions or a short open lateral
approach and a radiolucent guide. In this setting, a longer plate may
be desirable to increase construct stability and minimize dissection in
the zone of injury.
 |
|
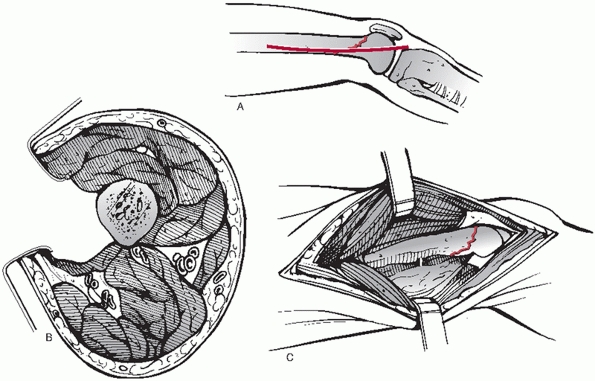
FIGURE 51-5 Lateral open approach to the distal femur. A. Lateral skin incision. B.
The plane of incision is through the lateral iliotibial band and between the vastus lateralis and the lateral intermuscular septum to the bone. C. Visualization of the distal lateral femur with the lateral approach. |
 |
|
FIGURE 51-6 Anterolateral approach to the distal femur. At the knee a lateral parapatellar incision (A, superficial) allows for excellent visualization of the articular surface (B, deep). More proximally the exposure is extended by splitting the vastus intermedius.
|
reduction and internal fixation of displaced medial condyle fractures
(B2 and B3). A straight medial incision is made over the medial
epicondyle and extended proximally into the distal thigh. Proximal
extension with this approach should be performed carefully, as the
femoral vessels pierce the adductor magnus 10 to 12 cm above the knee
joint. If necessary, an intraoperative Doppler examination may be
useful to identify the path of the vessels and avoid iatrogenic injury.
Exposure of the medial femoral condyle is obtained by incising the
medial retinaculum and reflecting the joint capsule. Care should be
taken to stay anterior to the medial collateral ligament and to avoid
injury to the medial meniscus.
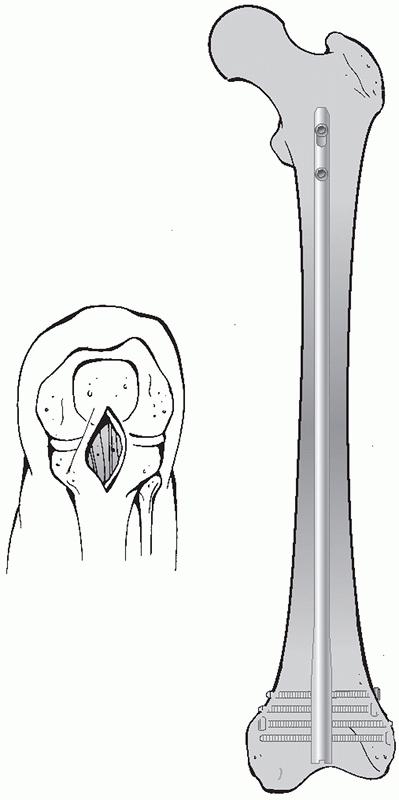
medial parapatellar incision, but if an intra-articular split or more
complex articular injury is present, an open medial or lateral
arthrotomy can be performed for reduction and stabilization of the
femoral condyles prior to nail in insertion. For retrograde nailing of
extra-articular fractures (type A), make a 3- to 4-cm incision along
the medial border of the patellar tendon between the inferior border of
the patella and the tibial tubercle (Fig. 51-7).
With intra-articular fractures (type C) a long midline skin incision
with either medial or lateral parapatellar arthrotomy is necessary for
exposure and reduction of the fracture. It is important to leave 5 to 6
mm of capsular tissue for a stable side-to-side repair during closure.
nondisplaced fractures and those who are not surgical candidates
because of significant medical comorbidities. Relative indications for
nonoperative treatment include nonambulatory patients (e.g.,
paraplegia), significant underlying medical diseases (e.g., severe
cardiopulmonary risk) or imminent death, infected fractures or severely
contaminated open fractures (e.g., type IIIB) (not typically
definitively repaired until they can be made “clean”), and a lack of
modern internal fixation devices. Nonoperative treatment of a displaced
distal femur fracture includes closed reduction with skeletal traction
with or without subsequent cast-bracing. This method requires
confinement to bed, is time consuming and expensive, and is not well
suited for multiply injured or elderly patients.3,9,10,15,23
Although the risks of surgery are avoided with closed methods, the
risks of nonoperative treatment may be significant and potentially
severe; including deep venous thrombosis, pulmonary embolus, decubitus
ulcer, pneumonia, urinary retention, and others.
 |
|
FIGURE 51-7
Approach to the distal femur for retrograde femoral nailing. The knee is bent over a radiolucent triangle or bolster. The authors prefer a medial (or rarely lateral) approach to the patellar tendon. This can be extended into a formal parapatellar approach if necessary for articular reduction. |
predate modern internal fixation methods. Early attempts at internal
fixation of distal femur fractures were associated with a high
incidence of malunion, nonunion, and infection. Because of these poor
early operative results, numerous authors concluded that nonoperative
methods were preferable. For example, Neer et al.43
reviewed a large series of supracondylar fractures and reported good
results in 84% of patients treated nonoperatively, but only 54% good
results in surgically treated patients. Despite “generally good
results,” those authors pointed out several pitfalls with the use of
traction therapy, including excessive deformity,
stiffness
of the knee joint, and many of the complications of bed rest. Only one
study has compared nonoperative and operative treatment. Butt et al.4
compared elderly patients treated with skeletal traction for 3 to 6
weeks followed by cast bracing with those treated operatively using a
supracondylar screw and side plate (i.e., dynamic condylar screw, DCS).
The results overwhelmingly favored operative treatment with a threefold
decreased risk for complications of immobilization (DVT, UTI, pressure
sores, and pneumonia) and a 33% risk reduction for poor results.
supracondylar femoral fractures have gained widespread acceptance as
operative techniques and implants have improved. Until the introduction
of fixed-angle plating, thin cortices, osteoporosis, a wide
intramedullary canal, and fracture comminution had made stable fixation
of these injuries difficult to achieve and maintain. The combination of
properly designed implants, a better understanding of soft-tissue
handling, and improved anesthetic methods have made internal fixation
practical for most patients. The goals of operative treatment of distal
femur fractures are anatomic reduction of the articular surface,
restoration of limb alignment and length, stable internal fixation,
rapid mobilization, and early functional rehabilitation of the knee.42
Using more biologic approaches and improved implants (e.g., locked
plating and improved retrograde intramedullary nails) has made
treatment of distal femur fractures much more predictable and
successful. As a result, the operative treatment of distal femur
fractures should be considered for virtually all displaced distal femur
fractures in adults.
advantages and disadvantages and are dependent to a large degree on the
fracture pattern, host factors, and the surgeon’s experience and
resources. Operative treatment is generally carried out with either a
combination of plates and screws or retrograde intramedullary nails.
 |
|
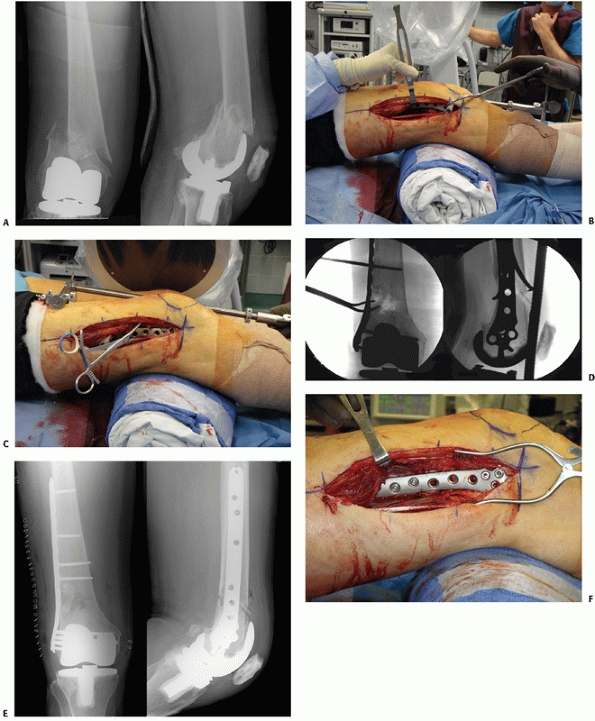
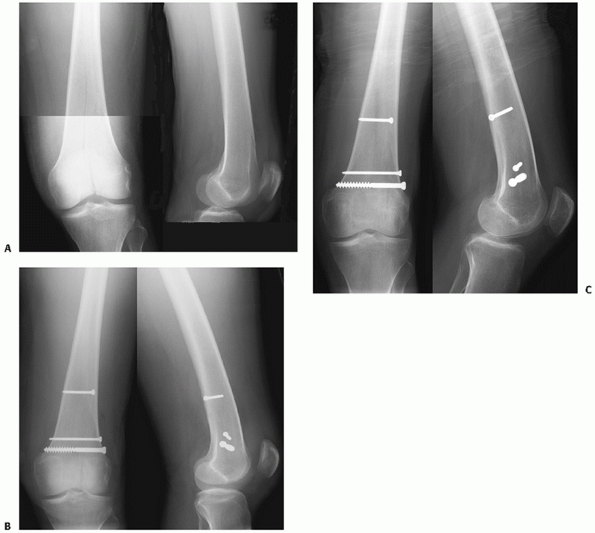
FIGURE 51-8 Case demonstrates (A) an OTA A-type distal femur fracture, (B) treated with indirect reduction and internal fixation with a 95-degree blade plate. (continues)
|
were most commonly treated with an anatomically contoured, but angular
unstable (nonlocking) distal femur plate (e.g., condylar buttress
plate). Relatively high complication rates were reported, which
adversely affected clinical results,* including infection,
nonunion or delayed union, malunion (especially varus collapse), the
need for bone graft, and knee stiffness owing to delayed mobility.
Subsequently alternative methods were proposed, including double
plating, use of plates for endosteal substitution, and fixed angled
plates, which met with varied success.
and others began popularizing indirect reduction of the fracture with
minimal soft tissue stripping to improve the fracture biology. With
advances in plate-screw design, which improved stability, the 95-degree
angled blade plate (Fig. 51-8) and DCS (Fig. 51-9)
became popular. When these two methods were combined, dramatically
improved rates of bone healing with fewer complications were found
compared with historical controls.2,47 However, insertion of these implants was technically demanding, limiting their widespread use.
developed in which screws are inserted that lock into the plate,
forming a fixed-angle construct.17,20
Most of these systems are also designed for insertion through minimally
invasive techniques, which may decrease problems with fracture healing
and infection.30 One example, the Less Invasive Stabilization System or LISS (Synthes USA, Paoli, PA) was the first system to use these
technologies and gain widespread popularity (Fig. 51-10).
This system was designed as an “internal fixator” in which the plate
may be applied using minimally invasive techniques after fracture
reduction and fixed with unicortical locking screws so that the plate
is not compressed to bone, which might affect the local biology (Fig. 51-11).
Condylar fixation is thought to be mechanically improved over earlier
implants (e.g., blade plate or DCS) by spreading out fixation points
among a number of locking screws (Fig. 51-12).
Multiple published studies have shown the distal femoral LISS to be
effective in achieving stable fixation with good short-term results.8,27,28,29,50,60,61
A variety of other plating systems have since been developed that offer
additional advantages for distal femur fractures, including better
anatomic contouring, improved fixation in the condylar segment, and
options for conventional screws, bicortical or unicortical solid
locking screws, and cannulated nonlocking or locking screws.
 |
|
FIGURE 51-8 (continued) Healing with abundant callus and maintenance of alignment is seen on 8-month postoperative radiographs (C).
|
 |
|
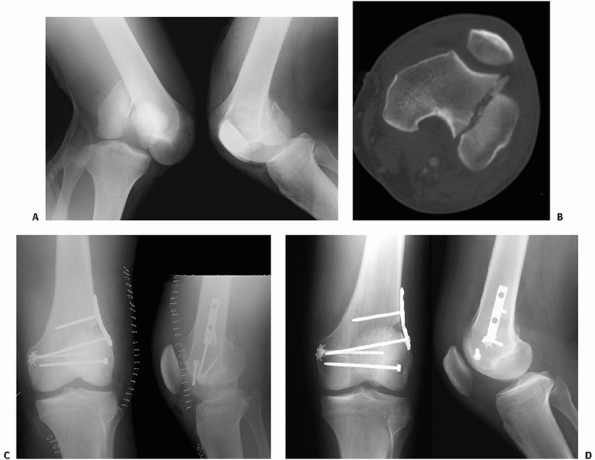
FIGURE 51-9 Case demonstrates an open OTA C1-type distal femur fracture (A) treated with early debridement and application of external fixator. (B) CT shows a simple articular fracture. (continues)
|
 |
|
FIGURE 51-9 (continued) The wounds appeared clean on postinjury day number 4 and open biologic plating was (C)
performed using a 95-degree dynamic condylar screw device. Healing with abundant callus is seen on 11-month postoperative radiographs (D). The device was removed at 14 months because of ongoing irritation to the iliotibial band and the condylar screw tract is well appreciated (E). |
traditional non-fixed-angle plates has been associated with relatively
high rates of delayed or nonunion and infection. The need for
supplemental bone graft was reported as high as 90% in comminuted
fractures.39,43,45,46
These problems may be reflective of the wide dissection required for
the fracture fixation and the lack of stability in early nonlocking
implants. Dramatically improved results have been published using
biologic approaches and improved angle stable implants such as the
95-degree blade plate and DCS. Reports by Bolhofner et al.2 and Ostrum and Geel47
in treating distal femur fractures with techniques of indirect fracture
reduction and internal fixation using 95-degree fixed angle devices
showed markedly improved results compared with previous methods. They
found early union in 93% to 100% of fractures and infections in only 0%
to 2% of cases.
the principles of minimally invasive locked plating using the LISS
system have shown promising early results. Schutz et al.60 described their early results from multiple European centers, where they found early healing in 37 of 40 patients (93%)
treated for fractures with indirect reduction and plating with the LISS system. Kregor et al.29
reported early union in 58 of 61 patients (95%) with distal femur
fractures treated similarly. The authors attributed successful early
healing to vigilant maintenance of the fracture biology and strict
adherence to modern fixation principles, but early in these series,
malalignment was recognized as a significant potential problem with
these methods. Subsequently, Ricci et al.50
treated 26 distal femur fractures in multiply injured patients using
the methods of LISS. Results included no nonunions, no infections, none
required bone grafting, and excellent range of motion and alignment was
seen. Finally, Weight and Collinge71
reported that using similar techniques and implants maintained fracture
alignment and allowed for early healing in a cohort of 27 high-energy,
mechanically unstable fractures (OTA 33 A2, A3, C2, and C3).
 |
|
FIGURE 51-10 A.
Case demonstrating minimally invasive plating of C1 distal femur fracture. The skin and IT band incisions as noted by the staples are moved slightly distal to the lateral femoral condyle to allow for retrograde submuscular plate insertion. B. Anatomic reduction and fixation of the condylar segment is performed first followed by indirect fracture reduction of the metaphyseal injury. Long plates are preferred with thoughtful application of screws. Early medial callus is typically seen at which point weight bearing is typically initiated. C. Fractures are well healed on these 8-month follow-up radiographs. |
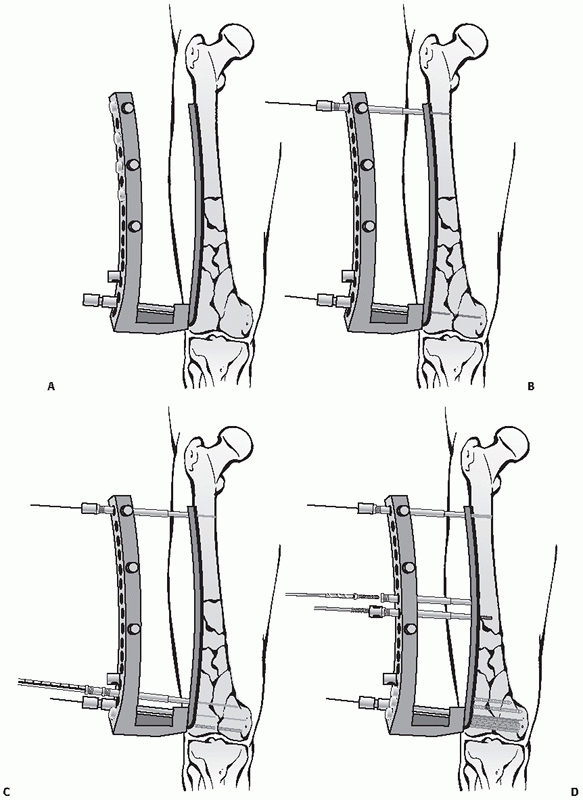
There are several potential advantages with this method of treatment:
The intramedullary nail is a load-sharing device compared with a plate;
it has the potential to stabilize complex fractures with less
soft-tissue dissection; and it can often be inserted quickly in a
patient with multiple injuries. Modern nailing systems allow multiple
distal locking screws in different planes to improve stabilization of
the condylar block (Figure 51-13). Although
there are short and long retrograde nails, we favor full-length nails
inserted to the level or just above the lesser trochanter to avoid
potential problems with injuring local anatomy with proximal AP
interlocking70 and prevent windshield-wipering by crossing the isthmus and thereby improving stability.24 Finally in patients with
ipsilateral hip and distal femoral fractures, both fractures can be
independently stabilized and the distal fracture securely fixed with a
retrograde nail. Antegrade nailing has been advocated for distal femur
fractures and may be especially useful in segmental fractures, although
retrograde femoral nailing is more effective than antegrade nailing for
obtaining and maintaining alignment of a distal fracture.12,51,53,72
 |
|
FIGURE 51-11
Most modern distal femur plating systems have radiolucent guides to allow for ease of plate insertion and simple percutaneous screw insertion. The guide system is used to apply the plate to the lateral femur (A) and most systems use a guide pin placed above and parallel to the articular surface to ensure proper varus-valgus alignment (B) and provisional fixation proximally. Instrumentation allows for minimally invasive provisional pin and screw insertion (C), as well as gentle reduction of the bone to the anatomically contoured plate (D). |
 |
|
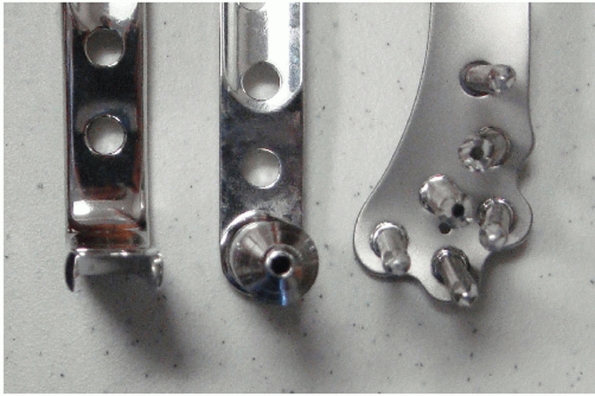
FIGURE 51-12
Photograph demonstrating differing designs of condylar fixation for plates used in distal femur fractures. From left to right, the blade plate, DCS, and modern distal femur locking plate. Note the varying amounts of condylar bone that may be captured with the different devices. |
 |
|
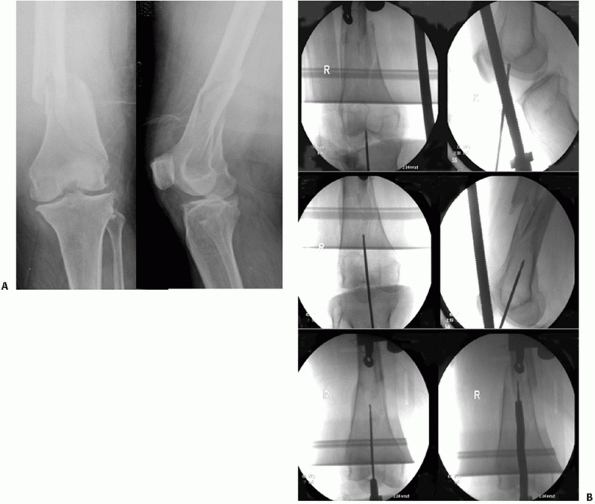
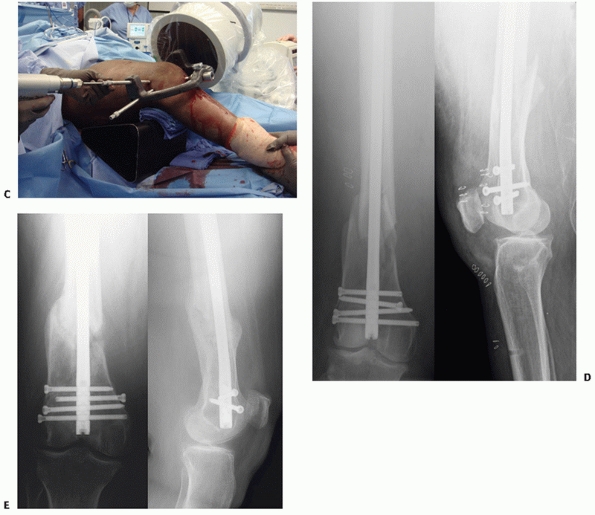
FIGURE 51-13 Illustrative case of retrograde femoral nailing for an OTA A-type distal femur fracture (A). B.
Intraoperative fluoroscopy images showing the guide pin (or awl) is inserted in line with the femoral canal in the intercondylar notch at the distal end of the Blumensaat line. Indirect reduction methods are similar to those used for bridge plating. Protection of the patella and soft tissues is mandatory. (continues) |
knee sepsis, stiffness, patellofemoral pain, and synovial metallosis
resulting from nail or screw fretting or breakage.32,41,69
Although no long-term studies have been done to assess effects of
retrograde nailing on the knee, it seems clear that poor operative
technique may cause injury. Although the authors have seen no
deleterious effects in technically well-done retrograde nailings (Fig. 51-14), leaving the nail proud by even 1 mm in the notch41
or inadvertently reaming the patella places the patellofemoral joint at
risk for destruction. Furthermore, with complex intra-articular C3
injuries, the condylar segment, especially if comminuted, may not be
optimally stabilized with a nail and relatively few points of fixation.
 |
|
FIGURE 51-13 (continued) Intraoperative photograph during distal interlocking (C). Postoperative (D) and 8-month follow-up (E) radiographs show stable fixation of condyles using a modern nailing system that allows for maintenance of alignment.
|
 |
|
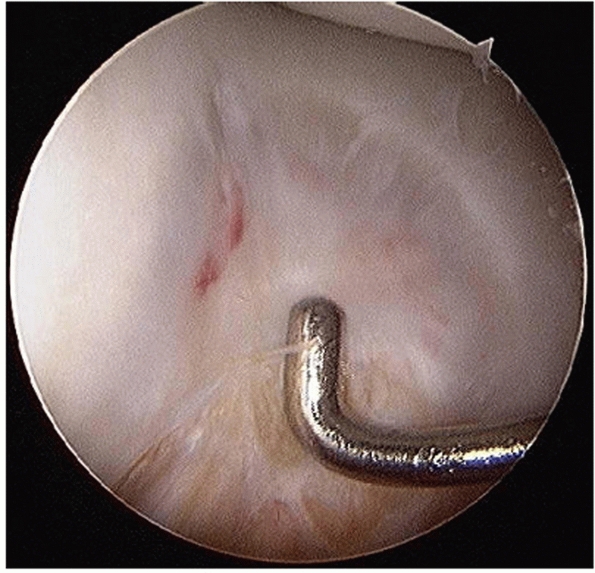
FIGURE 51-14
Arthroscopic photograph at 10 months shows that reparative cartilage may fill in the nail insertion channel after retrograde femoral nailing. |
less relevant today as implant technology and techniques have improved.
Published reports over the last decade using retrograde nailing for
distal femur fractures have reported mostly good results with
relatively few complications. To our knowledge there are no large
randomized studies comparing retrograde nailing with plating for these
injuries. Nevertheless, three small series have been published
comparing the two implants. Hartin et al.21 reported on 23 supracondylar femur fractures randomized to a retrograde intramedullary nail fixation (n = 12) or a fixed-angle blade plate fixation (n=11).
Both fixation methods gave generally good outcomes, but there was a
trend in patients treated with a retrograde nail to require revision
surgery for removal of implants (3 vs. 0) and to experience more pain
on SF-36 outcome measures. Christodoulou et al.7
reported management of distal femur fractures (types A and C) in mostly
elderly patients with the use of a DCS or a retrograde nail.
Seventy-two patients were randomized to nailing (n = 35) or plating (n = 37). Mean operative time, and estimated blood loss were lower in the nailing group (P < 0.001). Healing times were comparable and clinical results as assessed by Schatzker and Lambert’s criteria58 were similar with good to excellent results in greater than or equal to 80% of patients. Recently,
Thomson et al.58,69
evaluated outcomes at an average of 6.7 years for 11 patients with
traditional open reduction internal fixation versus 11 others treated
with limited open reduction with retrograde intramedullary nailing for
C-type distal femur fractures. The rate of subsequent bone-grafting
procedures (67% vs. 9%) and malunion (42% vs. 0%) were significantly
higher in ORIF compared with the less invasive retrograde
intramedullary nailing treatment. A nonsignificant trend was noted for
increased infection (25% vs. 0%) and nonunion (33% vs. 9%) in the group
treated with open plating. The physical function component of the SF-36
was approximately 2 standard deviations below the US population mean,
and 50% of patients demonstrated radiographic changes of posttraumatic
arthritis for all patients. There was no significant difference in any
domain of the Short Form-36 or Short Musculoskeletal Functional
Assessment, or the Iowa knee score between the two treatment groups.
advocated for some distal femur fractures, especially in adolescents or
in patients with a fracture above a total knee implant. The benefit of
this method is that it may be applied through small incisions after
closed fracture reduction. Dynamic “controlled” motion at the fracture
site occurs that may encourage early healing with callus. The problem
with this method of treatment is its inability to predictably maintain
length and alignment, particularly in comminuted fractures. These
limitations restrict its use to a few cases in which a locked plate or
standard locked intramedullary nail are contraindicated.
reported the use of closed Rush pinning in 98 patients with
supracondylar femoral fractures. Excellent and good results were
obtained in 84% of patients, with only two nonunions and one deep
infection. The nails provided enough stability at the fracture site to
allow early knee motion. Several authors, however, have reported
complications after Rush pin fixation of supracondylar femoral
fractures, including pin migration, knee irritation, loss of reduction,
and malunion. Kolmert et al.26
described the use of Ender nails connected to cancellous screws by a
coupling device. This technique allows anatomic reduction of the
femoral condyles with screws as well as semirigid connection of the
condyles to the femoral shaft. Most patients, however, require a cast
or cast-brace for 8 weeks after surgery. The routine use of flexible
nails is not recommended.
treatment for supracondylar femoral fractures. Unlike tibial plateau
fractures, ring fixators have a limited role in the acute management of
supracondylar femur fractures. Circular femoral frames tend to be large
and bulky and frequently impede soft-tissue access in open fractures.
Additionally they require considerable time and expertise in
application. The major indications for definitive
external fixation is active infection that has been recalcitrant to
aggressive treatment or severe open fractures, particularly type IIIB
open injuries. In complex fracture patterns, supplemental lag screws
are often necessary to fix intra-articular extensions. Depending on the
location of the wounds and degree of fracture comminution, fixation
across the knee is often necessary.
 |
|
FIGURE 51-15
Temporizing external fixation of distal femur fractures may allow for damage control in polytrauma patients and decreased complication rates in patients with significant associated soft-tissue injury. |
fixation for temporary stabilization of severely injured patients or
when a delay to surgical repair of more than 24 to 36 hours is
anticipated, so-called damage control orthopaedics. The advantages of
external fixation include rapid application, minimal soft-tissue
dissection, and the ability to maintain length, wound access, and
mobilization of the patient. Once the patient and the soft tissues have
improved, definitive internal fixation should be undertaken. Therefore,
initial fixator pin placement should avoid areas of planned surgical
incisions and implant placement whenever possible (Fig. 51-15).
As a general rule, 5.0-mm half-pins are inserted anteriorly or
laterally above and below the fracture usually in the mid- to proximal
shaft of the femur and proximal tibia, and connected to a unilateral
half frame. If instability remains, a second plane of fixation can be
added.
the use of external fixation as definitive treatment for distal femur
fractures, mostly after high-energy open fractures.1,6,25,33,56 The literature describing the use of temporizing external fixation for injuries in this area18,48,71 and elsewhere13,49,65 is compelling. Damage control orthopaedics is described in detail elsewhere in this textbook.
adults are best treated with internal fixation. We recommend locked
plating or closed retrograde intramedullary nailing for these fractures
(Table 51-1). We still use the 95-degree angled
blade plate in the management of selected nonunions or after corrective
osteotomies in the distal femur. Regardless of which implant is used,
the goal is anatomic reduction of the joint surface and stable internal
fixation to safely start range of knee motion. In isolated closed
fractures, internal
fixation
should optimally be performed within the first 24 to 48 hours. If
surgery must be delayed for more than 24 to 36 hours, a temporary
external fixator or tibial pin traction should be considered.
|
TABLE 51-1 General Surgical Tactics for Bony Reconstruction of Distal Femur Fractures
|
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||
so great, no single implant will be optimal for every case. Careful
assessment of the patient and critical review of the x-rays and the
“personality” of the fracture are essential. Some factors to be
considered in the surgical decision-making process include: (1) patient
age, (2) ambulatory status, (3) degree of osteopenia, (4) degree of
comminution, (5) condition of the soft tissues, (6) presence of absence
of open wounds, (7) involvement of the joint surfaces, and (8) whether
the fracture is an isolated injury or part of a multiply injured
patient.
alignment with stable fixation and early functional rehabilitation
remain the goal of surgery. In elderly osteoporotic patients, impaction
of metaphyseal fragments with small amounts of shortening may be a
reasonable tradeoff for rapid fracture union. Struhl et al.68
advocated the use of cemented internal fixation for supracondylar femur
fractures in geriatric osteoporotic patients, but with the widespread
use of periarticular locked plates this technique is less frequently
necessary today.
supports immediate or early internal fixation after débridement in type
I, II, and IIIA fractures in a stable patient in whom the wounds can be
made “clean.” Nonetheless, in type IIIB and IIIC open fractures with
massive wounds or gross contamination, external fixation with delayed
internal fixation is preferred. Temporizing knee spanning external
fixation is a valuable tool to treat this subset of patients. A variety
of frame configurations are possible, but typically two pins are placed
anteriorly in the proximal tibia and two anteriorly or laterally in the
mid-proximal femur superior to the anticipated proximal extent of plate
fixation (Figure 51-15). When the soft tissues
have recovered and the patient’s condition has improved, internal
fixation can be performed. Repeat débridement at 48-hour intervals
until all devitalized tissue is removed from the wound is necessary to
reduce the risk of infection. A wound VAC or antibiotic beads may be a
useful adjunct to stabilize the zone of injury, prevent infection, and
promote soft-tissue healing. Once a clean wound has been achieved and
the patient is stable, internal fixation is carried out.
become less clear with the increased use of indirect reduction
techniques and soft-tissue preservation methods. Whereas in the past
comminution of the medial cortex was an absolute indication for bone
grafting, current methods of fixation have decreased the use of bone
grafting in many complex distal femur fractures. Strong indications for
the use of bone grafts are fractures with bone loss or residual major
bone defects. Relative indications include selected OTA A3, C2, and C3
fracture patterns, as well as many severe open fractures treated on a
delayed basis to prevent nonunion. When significant defects in the
metaphysis or medial cortex exist, supplemental allograft or bone
morphogenic protein graft may be appropriate. Historically, the most
common donor site is the ipsilateral iliac crest, which can be prepped
into the operative field if grafting is anticipated. Intramedullary
harvesting of autograft from long bones (Reamer Irrigator Aspirator,
Synthes) and bone morphogenic proteins are other useful options.
implants. The method of fixation should be based on a preoperative plan
that incorporates the fracture pattern, soft tissue injury, patient
factors, surgeon’s preference/familiarity, and hospital resources.
Modern concepts in the surgical management of distal femoral fractures
were provided by the Association for the Study of Internal Fixation
(ASIF) in Switzerland. An essential component in the Swiss philosophy
of fracture care is detailed preoperative planning. The surgeon is
likely to deduce the best method of solving difficult problems through
a set of preoperative plans, and the “trial and error” performed on
paper instead of in the operating room. Executed properly, this
surgical tactic shortens operative time, minimizes intraoperative
decision making, and improves results. The sequential steps in the
surgical management of supracondylar femoral fractures include: (1)
restoration of the articular surface, (2) stable internal fixation, (3)
grafting of bone loss, if necessary, (4) impaction of the fracture in
osteoporotic elderly patients, (5) repair of associated ligament
injuries and patellar fractures, as indicated, (6) early range of
motion of the knee, and (7) delayed protected weight-bearing.
a radiolucent table. A small bump can be used beneath the ipsilateral
hip. The entire leg and hip region should be prepped and draped to
allow proximal extension of the surgical exposure if necessary. If an
external fixator is in place, it is carefully cleansed as part of the
prep and can be used as a grip to control the limb for remaining prep.
Iodine- or saline-moistened sponges can be placed around the pin sites
and
held in place with elastic gauze to isolate them from the operative
field. If bone grafting is anticipated, the iliac crest can be prepped
into the sterile field. In many cases a sterile tourniquet can be used
for part or all of the case. Confirm that an unhindered AP and lateral
view with fluoroscopy can be obtained.
based on the fracture pattern and the need for access to the articular
surface for reduction, implant location based on the preoperative plan.
For extra-articular fractures, minimally invasive submuscular plating
or retrograde nailing is recommended. Importantly, using either
approach, reduction is gained using indirect methods. If reduction is
difficult in minimally invasive plating, the lateral incision can
easily be extended to accommodate for reduction and plating.
Anatomically Contoured Lateral Condylar Plate. Fracture reduction is
critical to restoring normal function and has been the “holy grail”
with minimally invasive plating or nailing when using indirect
reduction techniques. Although modern implants and biologic sparing
techniques have decreased the incidence of delayed union and nonunion
compared with historical methods of ORIF, the incidence of malalignment
has increased significantly. There is a considerable learning curve
with indirect reduction methods, and particular attention to detail is
required to avoid malreduction and subsequent malunion.
In simple fracture patterns, reduction using manual longitudinal
traction alone may suffice. A well-placed pointed reduction forceps or
“King Tong” clamp can also aid reduction by holding the fracture in
proper position. The authors have found the universal (femoral)
distractor to be a valuable tool and it is used in most cases. Placed
directly into the femoral shaft proximally and anchored in the proximal
tibia (or distal femur), distraction usually restores overall length
and alignment. Initial overdistraction permits gentle teasing of
comminuted fracture fragments into nearanatomic position. A large or
medium sterile towel roll or bump can be effective at controlling
sagittal alignment; moving it distally or proximally even a few
centimeters may be very helpful. Finally, if correctly applied, certain
periarticular plates (not LISS) can fine tune the reduction by pulling
the bone to the anatomically contoured plate using conventional screws.
Combining standard nonlocked screws to lag the bone to the plate
followed by locked screws to aid in construct stability is a useful
tactic and employs benefits of both screw types. Remember, if a
combination of nonlocking screws and locking screws is used, the
nonlocking cortical screws must be inserted first before any locking
screws are inserted (lag before you lock), or the fixation of those
screws can be compromised.
carefully scrutinized to assess limb alignment, rotation, and length.
This is especially true in comminuted fracture patterns in which
mismatch of the width of the major fragments or cortices cannot be
compared to judge rotation or length. A radiolucent ruler may be
helpful to avoid unrecognized shortening and the contralateral limb may
be used for comparison as a radiographic template. Excessive external
rotation is not uncommon after this particular form of treatment, as
the weight of the leg and/or targeting device rotates the distal
segment. Rotation is checked clinically and compared with the
contralateral limb as assessed preoperatively or intraoperatively (some
surgeons will prep it into the surgical field).
that is well-visualized on a lateral fluoroscopic image that is very
useful for gauging reduction in flexion-extension and can be captured
with large pointed reduction forceps to key in the reduction. If this
produces an anatomic reduction, a 3.5- or 4.5-mm lag screw can often be
placed across this typically oblique fracture and then the plate can be
applied in a neutralization mode. In more transverse fractures, once
reduction is achieved, one or two stout (2.0- to 3.2-mm) provisional
Kirschner or guidewires can be placed obliquely through the
nonarticular part of the medial femoral condyle and aimed across the
fracture and slightly anterior into the shaft segment so that it lies
anterior to the path of the plate.
evolution of locked implants, but also potentially more effective with
options for screws being standard or locked, cannulated or
noncannulated bicortical or unicortical, and plates inserted open or
through minimally invasive techniques. When using the plate as a
reduction tool it is important to align the most distal locking screws
(or their guidewires) parallel to the knee joint to ensure that the 8
degrees or so of valgus built into the plate is achieved (Fig. 51-17).
Apply all nonlocked screws into the proximal or distal segment before
any locked screws are inserted. If a stable OTA type A1 fracture is
well reduced, compression should be applied to optimize stability and
allow for earlier weight-bearing. Eccentric drilling, the articulated
tensioner, and a push-pull screw with a large Verbrugge are three
effective methods for producing compression across stable fractures
with plates. Nonetheless, only when the medial cortex is restored can
the plate be effectively loaded. Properly done, the plate is placed
under tension and in theory subject to load sharing,
rather than load bearing. In cases with significant comminution, the
plate is fixed to the proximal and distal fracture, bridging the zone
of comminution. In this environment, the plate acts as an internal
splint. Nonetheless, the fracture fragments spanned by the plate are
left viable and capable of rapid consolidation if their soft-tissue
attachments have been respected.
always best achieved with the aid of a femoral distractor or external
fixator. Most of the reduction methods used for simple fractures are
applicable to comminuted fractures. We have found that it is often
easier to reduce the fracture to the plate rather than the plate to the
fracture in complex fracture patterns. In this situation the plate must
be used to aid reduction. It is important to re-emphasize that the most
distal locking screws must be parallel to the joint surface as assessed
on AP image as a guide for restoring limb alignment.
authors treat comminuted and/or osteoporotic fractures with less
soft-tissue dissection, longer plates, more screws in each segment, and
more locked screws. In general, a longer plate with spaced screws
provides better mechanical stability compared with shorter plates. It
is recommended that when selecting plate length, allow for at least
five screw holes above the most proximal aspect of the fracture.
Reference the position of the plate to Blumensaat’s line and the
subchondral margin of the trochlear groove (Figure 51-16).
Center the plate on the lateral aspect of the femur and apply a K-wire
in a wire hole in the plate (if available) or cannulated wire guide.
Center the plate on the distal diaphyseal fracture fragment and
provisionally fix the plate close to the fracture. Obtain
intraoperative confirmation of fracture alignment and implant position.
The guide pin closest to the joint is typically designed to restore
varus-valgus alignment if placed parallel to the joint axis (Figures
16-18). A series of standard followed by locked screws (hybrid
technique) allows the benefits of both screw types to be realized. The
condylar segment is stabilized with all or nearly all locked screws.
The surgeon should be careful when placing the most distal and
posterior screw in the condylar segment; if this hole is posterior to
the Blumensaat line a short (e.g., 28-mm) screw should be placed to
avoid violating the intercondylar notch. An intraoperative notch view
may be helpful to prevent this problem.
 |
|
FIGURE 51-16 Illustrative case of open lateral plating for periprosthetic OTA A-type distal femur fracture. A. Injury radiographs. B-D. Open lateral approach using a number of reduction methods (indirect: femoral distractor, towel roll, and King Tong clamp applied to plate and direct: carefully applied Weber clamp). Intraoperative radiographs (E) and photograph (F) showing maintenance of the bone’s muscle attachments.
|
 |
|
FIGURE 51-17 A.
A well-positioned plate is centered on lateral imaging with the plate 1 cm or so posterior to the lateral articular surface. This provides space anteriorly for lag screws to repair intercondylar fractures, if necessary. B. Anatomically contoured plating systems typically use an alignment system with one or more distal pins designed to be parallel with the joint surface on AP imaging if anatomic coronal limb alignment has been restored. C. Guide pins or drills are aimed down the condylar axis. D-F. Cannulated or noncannulated screws can be used in the condylar segment, along with noncannulated screws in the shaft. |
Contoured Lateral Condylar Plate. The successful use of minimally
invasive plating (MIPO) for the treatment of complex fractures is
technique dependent and there is a learning curve. The principles of
fixation and preserving biology are similar to those for open plating.
The majority of the operation is performed though a short lateral
incision over the lateral femoral condyle (Fig. 51-18).
With MIPO, a radiolucent targeting device is often used as a handle to
insert the plate extra-periosteally on the lateral femur through a
submuscular tunnel beneath the vastus lateralis. Periarticular plates
are designed to fit the anatomy of the distal femur and are applied
along the metaphyseal flare and lateral condyle of the distal femur by
sliding it proximally and distally. Once the plate is inserted, a
mini-open approach can be performed
at
the proximal end of the plate to ensure that the plate is centered on
the lateral side of the femur. Alternatively, all shaft screws can be
inserted through the targeting device, but the surgeon must be certain
that the plate is well centered proximally to ensure accurate screw
fixation.5
A locking cannulated drill sleeve is inserted into the most proximal
screw hole to add stability through the aiming device. The plate is
centered on bone both proximally and distally and oriented flush with
the lateral femoral condyle. A large periarticular clamp can be used
distally to gently hold the bone to the plate, which also aids in the
sagittal plane fracture reduction. Any gross adjustment of fracture
reduction is done before provisional fixation, using K-wires or a drill
bit through the cannulated stabilization guide. Many supracondylar
femur fractures have some degree of comminution and the goal is
restoration of length, alignment, and rotation. A standard nonlocking
screw or “push-pull” device can be applied to “pull” the shaft of the
femur toward the plate, which fine tunes the varus-valgus alignment and
augments stability of the provisional construct. The opposite uninjured
limb can be used as a template in comminuted cases in which the bony
landmarks on the injured side are fractured. Coronal plane alignment
(varus-valgus), flexion-extension, as well as rotation, must be
confirmed before definitive fixation when using indirect reduction
methods. Quality intraoperative imaging is mandatory. Restoration of
limb alignment in rotation and length is assessed in a similar fashion
as described for open plating using indirect reduction.
 |
|
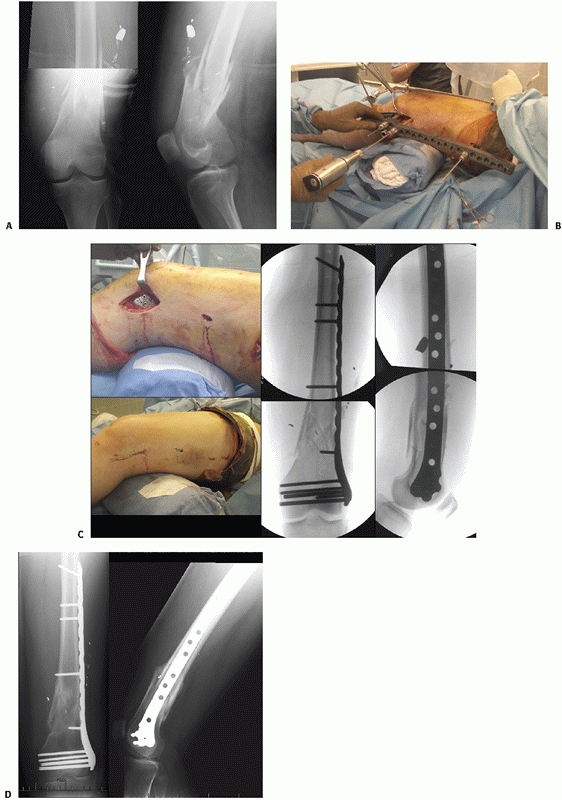
FIGURE 51-18 Case of minimally invasive plating for an OTA A-type distal femur fracture. A. Injury radiographs. B.
Intraoperative photograph shows plate application and screw insertion using radiolucent targeter and reduction tools including femoral distractor, well-placed towel roll, and periarticular clamp. C. Intraoperative photographs of MIPO incisions and fluoroscopy images. D. Five-month follow-up radiographs show healed fractures. |
Screw. The use of a 95-degree condylar blade plate or DCS is less
frequent today (Figs. 51-8 and 51-9).
Periarticular locked plates have replaced use of these traditional
implants for most fractures. When periarticular locked plates are
unavailable or contraindicated, the 95-degree condylar blade plate
remains a useful implant, although we use it most often for
stabilization of nonunions and malunions. There is a large body of
literature from both North America and Europe documenting success with
this implant. When used by an experienced surgeon, this device can
restore alignment and provide stable internal fixation. Because it is a
stout fixed angled device, it provides excellent control of the
fracture. Nonetheless, placement of the 95-degree condylar blade plate
is a technically demanding procedure, because the surgeon is required
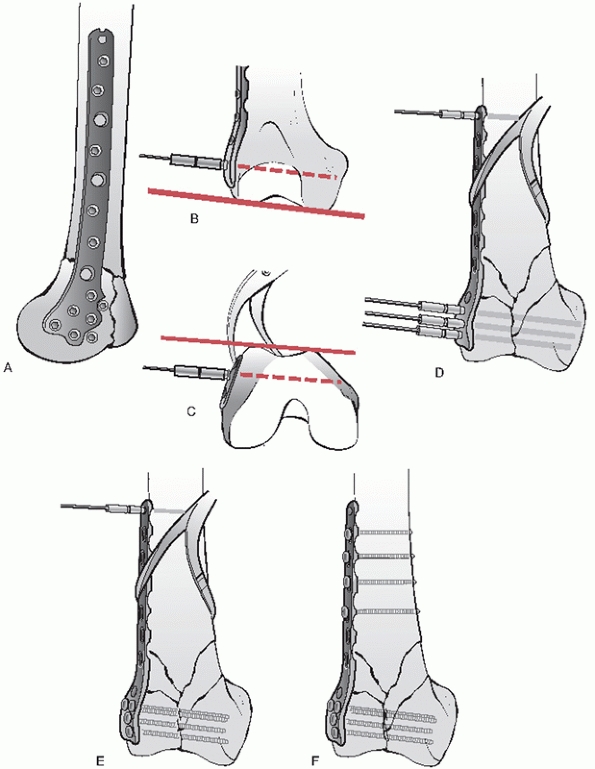
to place the blade correctly in three planes simultaneously (Fig. 51-19).
Incorrect insertion of the chisel and blade will result in condylar
malalignment, resulting in malunion. A technique using three guide pins
is very useful for correctly applying the blade to restore limb
alignment: this is summarized in Figure 51-19.
The first guidewire is inserted parallel to the knee joint. A second
one follows the inclination of the anterior articular surface of the
femur (patellofemoral joint). A third guidewire is the definitive or
summation guidewire and parallels the first two wires. The correct
starting point for the insertion of the seating chisel or triple reamer
is in the anterior half of the femoral condyles—in a line with the
femoral shaft and exactly parallel to the summation guidewire. The
starting point is 1.5 to 2.5 cm proximal to the articular margin of the
knee joint. In young patients with hard bone, insertion of a seating
chisel may be difficult. To prevent iatrogenic comminution, a window
should be created and predrilled to receive the seating chisel. Once
the window is precut, the seating chisel is inserted to a predetermined
distance. It is important to remember that the distal femur is
trapezoidal and the medial cortex slopes 25 to 30 degrees (Fig. 51-3).
When using either the blade plate or DCS, the tip of the implant should
be 1 cm or so short of the medial femoral cortex to prevent inadvertent
penetration. This technique leaves little room for error in an already
fractured bone. There is a learning curve associated with the use of
this implant before consistent and reproducibly good results are
achieved. It can be used in intra-articular fractures, providing the
distal lateral femoral condyle is intact. In cases in which comminution
extends distally and laterally compromising fixation, an anatomically
contoured locked plate is preferred.
This device is based on the compression screw commonly used in hip
fractures. The implant shares many of the features of a compression hip
screw, making it familiar to most surgeons and therefore easier to
master. Other advantages include its ability to apply interfragmentary
compression across the femoral condyles, better purchase in
osteoporotic bone, and the need for only two-plane alignment. By
allowing a degree of freedom in the sagittal plane, insertion of this
device is technically easier than a 95-degree blade plate. Should a
nonunion develop after its use, the side plate can be replaced without
revising the transcondylar screw. The major disadvantage with the DCS
and plate is the bulky size of the implant at the screw-plate junction.
This frequently requires removal of considerable bone from the lateral
femoral condyle to ensure a low-profile fit. Despite modifications in
its manufacture, the “shoulder” of this device is more prominent than
that of a comparable angled blade plate or condylar buttress plate. In
many patients this causes knee symptoms as the iliotibial band slides
over the prominent edge of the implant. Additionally, the dynamic
condylar screw and plate must be key-locked to prevent rotation with
the barrel. In low supracondylar fractures, the condylar screw may not
provide as much rotational control of the distal fragment as the
95-degree blade plate. At least one additional screw placed through the
plate and anchored in the distal fragment is necessary to ensure stable
fixation. The principles of plate application and maintaining biology
are similar to other methods of plating. For proper positioning of a
95-degree angled blade plate or a DCS, orientation guidewires are
helpful (Fig. 51-19).
postoperatively; for example, in conscious patients on day 1 or 2 with
physical therapy or using a continuous passive motion machine (CPM) in
patients remaining intubated or in the intensive care unit. Early
isometric muscle-strengthening exercises and active-assisted range of
motion is encouraged. In patients with stable internal fixation,
partial weight bearing (i.e., up to 20 pounds of body weight with
crutches or a walker) at 3 to 6 weeks is allowed, whereas in patients
with less stable fixation weight bearing must be delayed until advanced
signs of fracture healing appear on the x-rays. Progressive weight
bearing is encouraged once there is radiographic evidence of healing.
By 12 weeks, most patients
should tolerate substantial weight bearing, although still requiring an assist device.
 |
|
FIGURE 51-19 The correct insertion site and “summation wire” technique for application of a DCS (A-D),
and is demonstrated for a 95-degree blade plate. Diagrams demonstrating how optimal application of a fixed-angle plate, in this case a 95-degree blade plate, can be used as a reduction tool to realign the distal femur (E,F). Misapplication can result in a variety of malalignments of a distal femur fracture into varus (G), valgus (H), translation (I,J), apex posterior- (K), or apex anterior-angulation (L). |
planning is no less important for intramedullary nailing than it is for
osteosynthesis with plates and screws. Limitations of nails used for
distal femur fractures make planning very important, such as the size
of the condylar segment, the insertional depth of the nail, the number
and distances of locking screws from the nail’s end, and others.
Nonetheless, the goals of surgery remain the same as for plating:
anatomic reduction of the articular surface, restoration of axial
alignment and length, fracture stabilization, and maintenance of a
biologic environment conducive to healing with avoidance of infection.
Many of the same surgical tactics and reduction methods are useful for
intramedullary nailing distal femur fractures. Surgery is done on a
radiolucent table with the aid of an image intensifier.
affected limb supported on a radiolucent triangle or large bump to a
20- or 30-degree angle (Fig. 51-13). The C-arm
unit should come in from the opposite side of the table, and the
underside of the table should be clear to navigate a C-arm freely
distally and proximally beyond the intertrochanteric region for AP and
lateral x-rays. When possible the fracture
should
be reduced before nailing. Many of the indirect reduction methods
described in femoral plating are useful for nailing. Schantz pins
applied unicortically can be used with the femoral distractor or as joy
sticks.
limited medial parapatellar arthrotomy is used for retrograde femoral
nailing as described previously (Fig. 51-7).
The patella and local soft tissues should be protected from reamers and
other instrumentation during nailing. A working “soft-tissue” cannula
is available in most nailing sets or carefully placed right-angle
retractors are effective. Patients with a simple nondisplaced or
minimally displaced C1 fracture may be treated with a percutaneously
applied pointed reduction clamp with reduction of the intra-articular
extension and placement of lag screws before nail passage. Most
displaced intra-articular fractures (displaced types C1, C2, and C3)
must be exposed, reduced, and stabilized using an open medial or
lateral parapatellar arthrotomy based on the fracture pattern. The
intramedullary nail can then be inserted through the open incision.
fractures must not block the path of the intramedullary nail. As such,
interfragmentary screws must be thoughtfully placed anteriorly or
posteriorly so as not to impede eventual nail passage. Screws placed
through the articular surface (e.g., for a Hoffa fracture) should be
countersunk and carefully measured before insertion, and carefully
scrutinized radiographically to avoid articular injury.
notch just anterior to the femoral attachment of the posterior cruciate
ligament (Fig. 51-13B). A threaded tipped guide
pin and cannulated drill are used to prepare the distal femur before
nailing. The pin is carefully inserted in line with the femoral shaft
to ensure restoration of coronal plane alignment (on the AP image).
This pin is started at the apex of the intercondylar notch and aimed
centrally through the supracondylar region. On the lateral image it is
started just anterior to the Blumensaat’s line. Once the guide pin
placement is confirmed with AP and lateral radiographs, advance the
step reamer through the working channel soft tissue sleeve over the
entry wire to enlarge the insertion site to the appropriate depth.
pins attached to a T-handle chuck (joysticks) in the femoral shaft or
condyles, a well-placed sterile towel roll, or the femoral distractor
to reduce the major fragments. A beaded tip guidewire is inserted into
the intramedullary canal and advanced past the fracture site, into the
proximal femur under fluoroscopic control. With the fracture reduced,
confirm the position of the guidewire to be center-center in the AP and
lateral views. An intramedullary fracture reducer or “finger” is
available in most nailing sets and can be used to facilitate reduction
and guidewire passage across the fracture site. Blocking screws are
sometimes used to narrow the effective canal diameter of distal femur
to improve alignment and prevent deformity. When necessary, blocking
screws should be applied in the short condylar segment. A rule of thumb
is to apply the screws on the concave side of existing deformity. This
technique is discussed in more detail in the section on nailing
proximal tibia fractures.
during reaming and insertion of the nail. The guidewire is removed
after nail insertion. The nail must be countersunk several millimeters
to prevent cartilage damage to the patellofemoral articulation. Final
nail positioning should be checked in both the AP and lateral
radiographs to ensure nail depth and proper alignment.
sleeves using a radiolucent guide. Proximal locking is accomplished
typically in the AP plane using a freehand technique. The C-arm is
aligned with the desired locking hole in the nail, so that the hole
appears to be a perfect circle. A knife blade is placed on the skin,
with the incision point verified with radiographic image and a 1-cm
incision is made over the hole in the nail. The tip of the drill bit
appears as a solid circle in the center of the screw hole and both
cortices are drilled. The pilot hole is measured or alternatively a 30-
or 35-mm screw may be preselected and inserted. Placing the screw using
a screwdriver with the ability to “capture” the screw or a suture lasso
may aid in screw recovery if the screw disengages.
remove reamings or other debris that may cause mechanical problems or
heterotopic bone formation. The arthrotomy is anatomically repaired and
the skin closed in standard fashion.
initiated on day 1 or 2 in awake patients with a physical therapist or
with a continuous passive motion machine (CPM) in patients remaining
intubated or in the intensive care unit. Weight bearing is encouraged
once there is radiographic evidence of callus formation, typically 6 to
8 weeks postoperatively. Clinical and radiographic examinations are
performed at 4- to 6-week intervals until the fracture is healed and
patients are able to ambulate without discomfort.
condyle are uncommon. Open reduction and internal fixation is the most
reliable method to ensure articular surface restoration. In patients
with good bone quality in whom anatomic reduction is achieved with
closed means, the fracture may be stabilized with several percutaneous
lag screws (Fig. 51-20). In displaced
fractures, an open approach and plate fixation along with lag screws is
routinely used. A direct lateral or medial approach may be used for
simple B1 fracture patterns in which anatomic reduction of the joint
can be gained without arthrotomy. In comminuted fractures such as B2 or
B3 fractures, a medial or lateral parapatellar approach is preferred,
and extended proximally as necessary. Fixation of the articular surface
must be anatomic and stable, as shearing stresses are common without
weight bearing. With the typical vertical condylar fracture (medial or
lateral), the use of an antiglide plate with supplemental lag screws is
recommended (Fig. 51-21).
involving the lateral or medial condyle, is not uncommon and is usually
seen with other bony or ligamentous injuries around the knee (Fig. 51-22).
This fracture pattern is often missed on plain films, but is readily
visualized on CT scans. The posterior condyle fragment is mostly
articular and fixation
may
be problematic. In isolated fractures a limited arthrotomy can be
performed and screw fixation applied. If any displacement of Hoffa
fracture is present or other parts of the distal femur are to be
addressed, then an extensive approach is necessary. Fixation is with
two or more carefully measured and placed 2.7-, 3.5-, or 4.0-mm lag
screws inserted anteriorly to posteriorly and countersunk beneath the
anterior articular surface (Fig. 51-20).
Occasionally, a nonarticular fracture spike extends superiorly from the
posterior fragment that is useful for assessing reduction and
application of an antiglide plate (Fig. 51-22).
 |
|
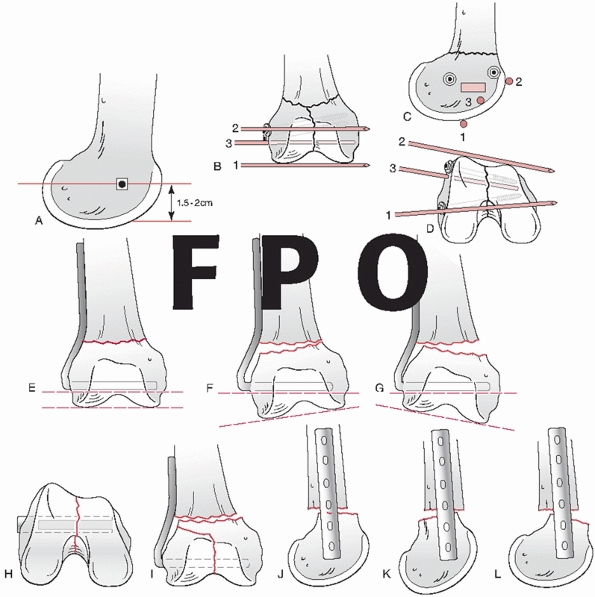
FIGURE 51-20
Illustrative case showing a minimally displaced OTA B-type distal femur fracture (lateral condyle) treated with percutaneous screws. A. Injury radiographs. B. A percutaneous applied clamp was used to optimize reduction followed by fixation with lag screws. C. Six-month follow-up radiographs. |
treatment are precise anatomic reduction and fixation of the articular
surface as well as stabilization of the meta-diaphyseal component. The
authors currently use both locked plates and intramedullary nails for
these difficult fractures. Using either fixation method, the initial
step is anatomic reduction and stabilization of the articular surface.
With nondisplaced or minimally displaced simple articular splits in OTA
type C1 injuries, the condyles can often be anatomically held or
reduced with a large clamp, and stabilized through a standard open or
minimally invasive lateral approach using long 3.5-, 4.5-, or 6.5-mm
lag screws applied outside the footprint of the plate on the lateral
femoral condyle or path of the nail. Sometimes inserting lag screws
from the medial side simplifies their placement.
involvement (the vast majority of C2 and C3 fractures), the authors
prefer the modified lateral (or medial) parapatellar approach to allow
access to the joint (Figs. 51-6 and 51-23).
In these cases our preference is to use small fragment fixation for the
condylar injuries in conjunction with distal femoral locked plates.
Temporarily, secure articular fragments using K-wires and/or reduction
forceps. Place provisional and/or definitive fixation using 3.5- and
4.5-mm cortical screws nested peripherally in the contours of the
plate. If a posterior coronal or Hoffa fracture is present, fixation
can be obtained by placing countersunk 2.7- or 3.5-mm cortical, or 4-mm
cancellous screws through the articular surface from anterior to
posterior. After adequate surgical exposure, the femoral condyles are
reduced and provisionally fixed with Kirschner wires. Once reduction is
confirmed clinically and/or radiographically, the condyles are
definitively fixed with long screws anterior and/or posterior in the
condyles, allowing
sufficient
room for the plate. The condylar block can then be reattached to the
shaft segment using whichever fixation method the surgeon prefers (Figs. 51-24 and 51-25).
 |
|
FIGURE 51-21 Injury radiographs of fracture-dislocation of knee with (A) an OTA B-type lateral condyle fracture and (B) corresponding CT images. C.
Repair was performed with open reduction and internal fixation using lateral approach and a small fragment buttress plate and lag screws. The medial knee ligaments were grossly unstable, so the medial collateral ligament was repaired to the medial femoral condyle. D. Nine-month follow-up radiographs. |
fractures. The traumatic wound is nearly always anterior and is
associated with a variable degree of damage to the extensor mechanism.
As with all fractures, urgent but thoughtful treatment is required.
Thorough irrigation and débridement of the fracture and traumatic
wounds remains the single most important step in the prevention of
infection. Serial débridement may be necessary in many type III open
fractures. Antibiotic beads or a wound VAC are useful tools in this
setting. Immediate internal fixation is not indicated for all fracture
patterns. The risk-benefit ratio to the patient must be carefully
assessed when contemplating primary internal fixation. Fracture
stabilization for open fractures is particularly useful in patients
with multiple injuries, massive and mutilating limb injuries, open
fractures and vascular injuries, and open intra-articular fractures.
Advantages of immediate internal or external fixation in these
fractures include stabilization of the fracture and surrounding soft
tissues, ease of wound care, pain relief, and mobilization of the
patient and the injured limb. Nonetheless, immediate internal fixation
in open supracondylar fractures must be tempered by the increased risk
of infection as a consequence of further soft-tissue dissection and
interference with local blood supply. If infection develops, it may
affect not only the fracture site but also the knee joint.
supracondylar fractures, many fracture surgeons favor definitive
internal fixation after debridement of the traumatic wounds, if
the wounds can be made “clean.” Nonetheless, most grade IIIB and IIIC
open distal femur fractures are more safely managed with knee-spanning
external fixation and delayed internal fixation. Subsequent surgery can
be carefully planned with optimal operating
room personnel and resources, with transfer to a tertiary center an option if desired.
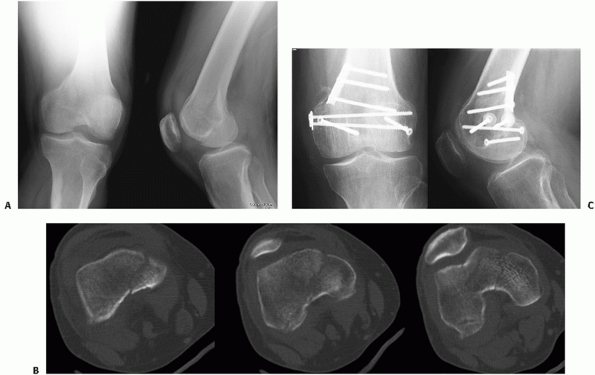 |
|
FIGURE 51-22 Coronally oriented OTA B-type distal femur fractures of the medial and to a lesser degree the lateral condyle. A. Injury radiographs and (B) corresponding CT. C.
A small antiglide plate was placed over this fracture’s extra-articular apex. Screws placed through the articular surface must be countersunk. |
supracondylar femur fracture is unknown, but is estimated to be 2% to
3%. Most injuries to the superficial or profunda femoral arteries occur
after fractures of the femoral shaft. On the other hand, blunt injury
to the popliteal artery most commonly accompanies dislocations of the
knee or displaced fractures of the proximal tibia. It is surprising,
therefore, that the incidence of popliteal artery injury is so low
after supracondylar fracture, because the vascular bundle is tethered
proximally in the hiatus of the adductor magnus muscle and distally by
the arch of the soleus. These tight attachments leave little room for
skeletal distortion after fracture. Vessel injury can be caused by
direct laceration or contusion of the artery or vein by fracture
fragments or indirectly by stretching, leading to intimal damage.
Clinical examination of the leg for signs of ischemia with evaluation
of pulses and motor and sensory function is essential.
intra-arterial injection or CT based) include an absent or diminished
pulse, expanding hematoma, diminished ankle-ankle index, bruit,
persistent arterial bleeding, and injury to anatomically related
nerves. Displaced supracondylar fractures in close proximity to the
femoral or popliteal vessels despite apparent normal peripheral pulses
may have occult vascular injury patterns and require careful judgment
regarding the need for exploration or angiography. If any doubt exists
about the integrity of the vessels, a consultation with a vascular
surgeon may be helpful.
supracondylar femur fractures depends on the severity of the ischemia
and amount of time elapsed since the injury. If distal pulses are
present (indicating distal tissue perfusion), the fracture should be
stabilized first. If arterial compromise is severe or the time elapsed
from injury is more than 6 hours, re-establishment of circulation takes
priority. Consideration should be given to rapid application of an
external fixator to restore length and provide stability before
arterial reconstruction. A temporary vascular shunt followed by
definitive vascular repair may be useful. Arterial repairs are usually
accomplished by interposition vein grafts or synthetic grafts. Whenever
possible, concomitant femoral or popliteal vein injuries should be
repaired. One of the most common and preventable mistakes is to repair
the vessel with the fracture in a displaced position. During subsequent
fixation of the fracture, manipulation of overriding fragments can
disrupt the vascular anastomosis. This problem can be avoided or
minimized by the use of an external fixator or a femoral distractor to
maintain length and alignment before the vascular repair. Fasciotomy of
the lower leg should be considered in
all
patients with ischemia time exceeding 6 hours and those with tenseness
of the of the fascial compartments after reperfusion or extensive
soft-tissue injuries. Compartment pressure monitoring may be helpful.
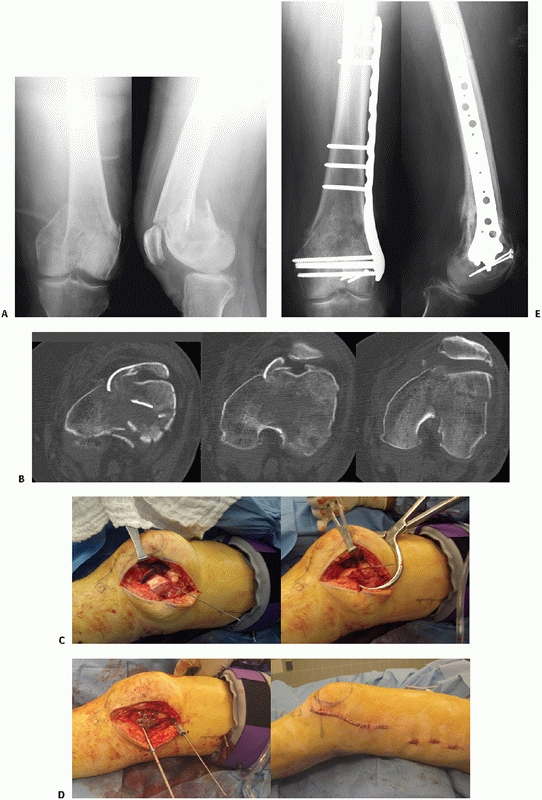 |
|
FIGURE 51-23 Illustrative case showing treatment of an OTA C2-type distal femur fracture with submuscular plating. A. Injury radiographs and (B) corresponding CT scan images. C.
The anterolateral approach allows removal of fracture hematoma from intracondylar split to allow for anatomic reduction and provisional fixation. D. Definitive fixation has been applied with a lag screw anterior to the plate and submuscular plating. E. Follow-up radiographs at 6 months show healed fractures. |
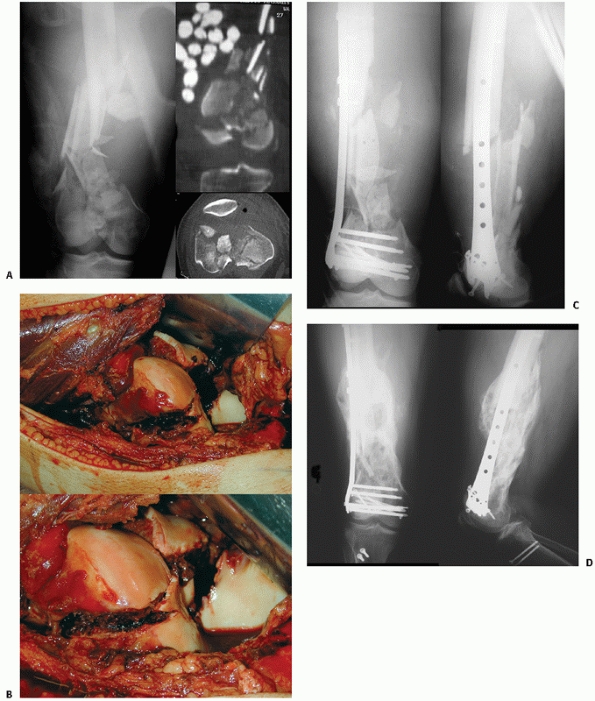 |
|
FIGURE 51-24 Case showing treatment of extreme open OTA C3-type distal femur fracture treated with plating. A. injury radiographs and CT after debridement and application of spanning external fixator. B. Intraoperative photograph showing severe articular comminution, and (C) radiographs showing bridge plating. D. Massive early callus formation rendered anticipated bone grafting unnecessary.
|
primary amputation may be indicated. This is particularly true if the
injury is associated with sciatic or posterior tibial nerve disruption.
The goal of aggressive limb salvage should be functional viability, not
just a perfused limb.
often difficult, and until recently most published studies report
relatively small numbers of patients. Risk factors for fractures
include osteopenia, rheumatoid arthritis, prolonged corticosteroid
therapy, anterior notching of the femoral cortex, and revision
arthroplasty. Nonoperative treatment is commonly associated with
prolonged period of traction, malalignment, and knee stiffness.
Operative treatment, particularly revision arthroplasty, is a major
surgical undertaking that often requires a long-stem or custom implant.
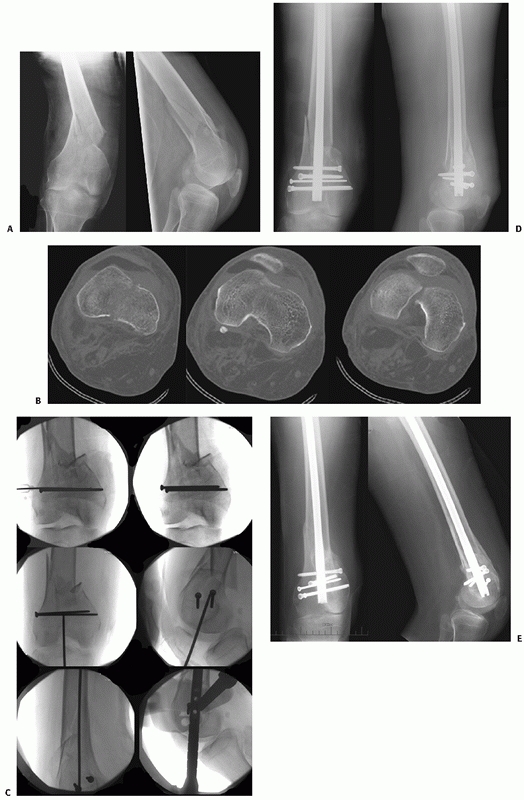 |
|
FIGURE 51-25 Case demonstrating an OTA C1 type distal femur fracture treated with intramedullary nailing. A. Injury radiographs and (B) CT scan showing simple articular split. C.
Intraoperative images showing reduced intercondylar fracture with lag screws placed anterior and posterior to anticipated nail path. D. Postoperative and (E) 9-month follow-up radiographs demonstrating healed fractures with maintained alignment. |
on the integrity of the knee prosthesis. If the prosthesis is loose,
revision arthroplasty with a stemmed prosthesis is favored. On the
other hand, in the more common setting of a stable femoral component,
the advantages of surgical stabilization with locked plating or
retrograde nailing appear to outweigh conservative care. Internal
fixation, if successful, prevents malalignment while allowing early
ambulation and knee motion. Locked plating, in particular, has
decreased the extent of complications after periprosthetic distal femur
fracture and improved results have been seen. Periprosthetic fractures
are considered in more detail elsewhere in this textbook.
uncommon and are not usually diagnosed preoperatively. Infrequently,
bony avulsion injuries of the collateral or cruciate ligaments can be
identified on the initial injury x-rays. Midsubstance tears and
capsular disruptions cannot be assessed clinically owing to the close
proximity to the fracture site. The most commonly injured ligament is
the anterior cruciate. In supracondylar fractures with significant
comminution of the articular surface, the anterior cruciate ligament
can be detached with one of the fracture fragments. Whenever possible,
this osteochondral fragment should be repaired at the time of fixation
of the supracondylar fracture. There is no consensus regarding the
timing of treatments of midsubstance tears of the cruciate ligaments
associated with supracondylar fractures. Primary repairs, ligament
augmentation, and formal reconstruction are made much more difficult by
the presence of the fracture and associated internal fixation devices.
Large-caliber drill holes, or tunnels, made through the intercondylar
notch of the femur for ligament reconstruction are usually
contraindicated. They may cause further comminution of the fracture,
compromise the stability of internal fixation, or be technically
impossible because of the fixation hardware. Primary ligament repairs
or reconstruction prolongs operating time and may increase the risk of
postoperative infection, intra-articular adhesions, or loss of knee
motion. Initial nonoperative treatment of midsubstance tears of the
cruciate ligaments is recommended. Protected motion in conjunction with
a knee orthosis together with vigorous rehabilitation may obviate the
need for late reconstructive surgery in some patients. In those
patients with persistent functional disability, late ligament
reconstruction can be undertaken once the fracture has healed and the
hardware can be removed safely.
state-of-the-art implants has improved results, their use does not
guarantee a favorable outcome. The surgeon must have a thorough
understanding of the local anatomy, mechanics of fracture fixation, and
patterns of fracture healing after internal fixation if consistently
good results are to be achieved. Common problems associated with
operative treatment are described in the following sections.
to affect knee mechanics and gait. Increased varus or valgus may lead
to overloading of the joint and subsequent arthrosis of the medial or
lateral compartment, respectively. Flexion-extension, rotational
deformity, or shortening may affect gait and comfort during activities
of daily living. In early series using traditional plates and screws,
problems with fixation failure, varus collapse, and malalignment for
unstable injuries occurred commonly. Schandelmaier et al.57
reported four patients whose fixation failed because of proximal screw
pullout following internal fixation with a locking plate. Caution is
necessary in applying unicortical locking screws (i.e., LISS) to the
femoral shaft if a mini-open approach is not used proximally. Quality
lateral radiographs must demonstrate that the plate is centered on the
bone to ensure optimal screw purchase. Multiple studies using locked
plates or retrograde nails have shown improved fixation in the
relatively osteopenic distal or condylar segment. With minimally
invasive reduction and fixation techniques, alignment has become more
problematic, as indirect reduction methods do not allow for direct
assessment of the fracture. Careful attention to detail is necessary in
the operating room to ensure correct alignment.
fixation with traditional plates of distal femur fractures was
associated with delayed or nonunion in 29% to 38% of fractures and
infection rates of 7% to 20%. These problems likely reflect the effects
of further trauma to the surrounding soft tissues during the wide
dissection required for the technique. Dramatically improved results
have been reported in similar injuries using more biologic approaches
and improved implants. Bolhofner et al. and Ostrum and Geel47
reported improved results treating distal femur fractures with indirect
fracture reduction and internal fixation using 95-degree fixed-angle
devices. The authors found union in 93% to 100% of fractures and
infections in only 2% of cases. Complications after internal fixation
using LISS have shown relatively low complication rates. For example,
Schutz et al.59 described the
results for operative treatment of distal femur fractures from multiple
European centers using LISS. They found healing in 37 of 40 patients
(93%). Kregor et al.28 reported
union in 58 of 61 patients (95%) treated with the femoral LISS device.
The authors attribute successful early healing to vigilant maintenance
of the fracture biology and strict adherence to the fixation principles
of locked plating. Weight and Collinge71
used similar methods in a selected high-energy cohort of patients with
mechanically unstable distal femur fractures. They also reported a high
union rate without bone grafting and no problems with maintaining
alignment in this at-risk population.
prior surgical procedures. Aseptic nonunions in patients with
reasonable bone stock should be treated by repeat osteosynthesis and
bone grafting. Hypertrophic nonunions usually respond to stable
internal fixation of the nonunion site. The 95-degree condylar blade
plate remains an excellent tool for treating nonunions (and malunions);
excellent compression can be applied with this device to increase
stability. In patients with atrophic nonunions or bone loss,
supplemental autologous bone or bone morphogenic protein graft is
required. In rare instances, methylmethacrylate or resorbable
tricalcium phosphate cements can be used to augment screw fixation in
the short osteopenic condylar segment.
supracondylar femoral fractures is the risk of infection. In major
trauma centers with experienced fracture surgeons, infection rates
should not exceed 3% or 5% in operatively treated cases, although an
individual’s fracture risk depends on a number of factors. If deep
infection develops postoperatively, aggressive irrigation and
débridement are indicated. A deep infection with abscess formation
should be packed open or temporarily treated with a wound VAC or
antibiotic beads. The wound is closed secondarily when it appears
“clean” and the signs of infection have resolved. Type-specific
antibiotics are given intravenously for 3 to 6 weeks. The duration of
the antibiotic therapy must be correlated with the clinical appearance
of the wound, laboratory assessment of infection (i.e., erythrocyte
sedimentation rate, C-reactive protein, and white blood cell studies)
and bacteriologic reports. In the presence of infection, implants that
provide stability should be retained to maintain stability.
Nonetheless, if the implant is loose, it should be removed and the
fracture treated temporarily with external fixation. The use of
hardware after sepsis requires careful judgment and should only be
replanted when signs of infection have abated. The fracture should be
followed carefully and bone grafting may be necessary to prevent
nonunion. The role of antibiotic-impregnated beads and Ilizarov
external fixator remains controversial.
fractures is loss of knee motion. This untoward complication invariably
results from damage to the quadriceps mechanism and joint surface as a
consequence of the initial trauma or surgical exposure for fixation or
both. Quadriceps scarring with or without arthrofibrosis of the knee or
patellofemoral joint is thought to restrict knee movement. These
effects are greatly magnified by immobilization after fracture or
internal fixation. Immobilization of the knee for periods of more than
3 weeks usually results in some degree of permanent stiffness.
meticulous soft-tissue handling and immediate immobilization of the
knee joint maximize the chance for an optimal outcome after a distal
femur fracture. Most patients should have 90 degrees of knee flexion 4
weeks postoperatively. Patients who fail to regain knee motion during
the first month are best treated with aggressive range-of-motion
exercises under the direction of a physician and physical therapist.
Failure to regain at least 90 degrees of knee flexion between 8 and 10
weeks postoperatively is worrisome and usually warrants additional
treatment in physiologically young patients. One approach is to combine
arthroscopic lysis of adhesions with gentle manipulation of the knee in
an effort to regain functional knee motion. Forceful manipulation
should be avoided, and immediate mobilization of the knee is essential
to maintain knee motion. In open distal femur fractures, some component
of knee stiffness is common. Patients with significant loss of motion
after injury may be candidates for quadricepsplasty as a late
reconstructive procedure.
fracture fixation often leads to local symptoms. This is particularly
true for older implants such as the dynamic condylar screw, in which
the “shoulder” between the compression screw and barrel of the side
plate is prominent and a subset of patients may develop irritation over
the implants laterally with symptoms of activityrelated pain and
crepitance. There are no firmly established criteria for hardware
removal after supracondylar femur fracture fixation, but the most
common indication for metal removal is local discomfort over the
implant with activity in a physiologically young patient with a healed
fracture.
irritation problems after modern locked plating. First, patients
sometimes complain of pain over the plate on the lateral femoral
condyle where the iliotibial band may rub and become irritated as the
tendon moves anterior and posteriorly with knee motion. Second,
surgeons who are unfamiliar with the trapezoidal shape of the distal
femur (Figure 51-3) may insert screws that
penetrate the medial cortex and irritate the medial soft tissues of the
distal thigh and knee. To avoid this problem intraoperatively, surgeons
must carefully measure length for condylar screws, especially those
placed anteriorly, and a 20- to 25-degree rollover C-arm view may be
used to confirm length. Postoperatively, when long screws are
bothersome, they can usually be removed as an outpatient procedure with
minimal technical difficulty.
femur fractures is chosen, primary bone healing is desired. With this
pattern of fracture healing there is little or no external callus if
bone graft is not used. Because most supracondylar fractures involve
both the metaphysis and lower diaphysis, internal remodeling is slow.
Therefore, it seems prudent to defer hardware removal for 18 to 24
months in most patients to avoid refracture. In cases in which flexible
fixation was used and callus is abundant, it may be safe to remove
implants earlier, although this has not been proved clinically.
elderly patients, the risk of anesthesia and surgery probably exceeds
the benefits to justify routine hardware removal. Nonetheless, if an
elderly patient has persistent local pain and the fracture is healed,
the implant can be removed if there are no medical contraindications.
In physiologically young patients with little or no symptoms related to
the implant, routine metal removal is not justified.
from full weight bearing with the use of crutches for 4 to 6 weeks.
Return to vigorous activities and sports can be individualized, but
probably should be deferred for 3 to 6 months.
studies have been published. Nonetheless, incongruity of the joint
surfaces is the leading cause of early arthritis. For many patients
with fractures involving a weight-bearing joint, the injury often
affects the normal function of the joint. Unfortunately, many patients
with degenerative arthritis of the knee occurring after fracture are
young adults and are not ideal candidates for knee arthroplasty. If the
arthritis is limited to the medial or lateral compartment, a corrective
osteotomy may be appropriate. In patients with severe disabling
bicompartmental or tricompartmental arthritis, a total knee replacement
may be indicated. Factors such as age, range of knee motion, presence
or absence of flexion contractures, and infections play a major role in
surgical decision making.
recently reviewed the English language literature summarizing and
comparing the results of different fixation techniques (traditional
compression plating, antegrade nailing, retrograde nailing, submuscular
locked internal fixation, and external fixation) in the operative
management of acute nonperiprosthetic distal femur fractures (OTA types
33A and C). This is summarized as follows. There are no large
prospective randomized English language studies (Level 1 evidence) reported on the treatment of distal femur fractures, although these may be forthcoming in the next few years.
reported a randomized controlled trial comparing 17 patients treated
with a DCS for distal femur fracture with 19 patients treated
nonoperatively (traction for 3 to 6 weeks followed by cast bracing).
There were good or excellent results in 53% of the patients treated
operatively compared with 31% treated nonoperatively using Schatzker’s
criteria. There were no nonunions or deep infections in either group,
and only one fixation failure (6%) in the DCS group. Significant
complications such as DVT, UTI, pneumonia, pressure sores, malunion,
and delayed union were commonly seen in the nonoperative group compared
with few in the operatively treated group. Markmiller et al.36
presented a prospective cohort study comparing patients with 20
patients treated with internal locked fixation using the LISS and 19
treated with locked retrograde femoral nailing. They found no
significant differences with regard to rates of nonunion (both 10%),
fixation failure (both 0%), infection (locked plating 0% vs. nailing
6%), and secondary surgical procedures (both 10%) at 1-year follow-up.
with compression plating, antegrade nailing, retrograde nailing, and
internal (locked) or external fixation. In all treatment options,
additional internal screw and/or plate fixation was performed first if
the articular surface was fractured. All operatively treated cases were
summarized. The average follow-up was 2.5 years. The articular surface
was fractured in 58% of the cases; in 22% severely (OTA type C3).
Twenty-seven percent of all fractures were open, and according to the
Gustillo-Anderson classification, 10% of all fractures were grade III
open. Overall, the average nonunion rate was 6.0%, the fixation failure
rate was 3.3%, the deep infection rate was 2.7%, and the average
secondary surgical procedure rate was 16.8%.
fixation techniques; therefore, a comparison of outcome parameters was
limited. A comparison of outcome parameters between compression plating
(blade plate, DCS, or condylar buttress plate) and locked internal
fixation revealed no statistically significant differences for any
outcome parameter; however, there was a statistically nonsignificant
relative risk (RR) reduction of 55% for deep infection when submuscular
locked internal fixation was performed as opposed to traditional
compressionplating techniques (P = 0.056) despite a significantly higher percentage of all open fractures (36% vs. 25%, P < 0.001) and grade III open fractures (17% vs. 7%, P
< 0.001) in the locked internal fixation group. On the other hand,
there was a nonsignificant RR increase in secondary surgical procedures
of 28% (P = 0.145) and a nonsignificant RR increase in fixation failure of 89% (P = 0.062) with compression plating.
fractures have been achieved over the past decade. Improved biology and
fixation have improved outcomes to good or excellent in 80% of cases.
Current problems with distal femur fractures, such as the optimal
implant, bone loss, injury to the extensor mechanism, as well as
postoperative knee stiffness, require further investigation.
M, Memik R, Ogun TC, Yel M. Ilizarov external fixation for severely
comminuted supracondylar and intercondylar fractures of the distal
femur. J Bone Joint Surg Br 2001; 83(5):663-667.
BR, Carmen B, Clifford P. The results of open reduction and Internal
fixation of distal femur fractures using a biologic (indirect)
reduction technique. J Orthop Trauma 1996;10(6):372-377.
BD, Kenzora JE, Edwards CC. The use of modified Neufeld traction in the
management of femoral fractures in polytrauma. J Trauma
1981;21(9):779-787.
MS, Krikler SJ, Ali MS. Displaced fractures of the distal femur in
elderly patients. Operative versus non-operative treatment. J Bone
Joint Surg Br 1996;78(1):110-114.
G, Wolinsky P, Hak D. Failure of less invasive stabilization system
plates in the distal femur: a report of four cases. J Orthop Trauma
2004 Sep;18(8):565-570.
AT, Ozsoy MH, et al. The use of a low-profile Ilizarov external fixator
in the treatment of complex fractures and non-unions of the distal
femur. Acta Orthop Belg 2009;75(2):209-218.
A, Terzidis I, Ploumis A, et al. Supracondylar femoral fractures in
elderly patients treated with the dynamic condylar screw and the
retrograde intramedullary nail: a comparative study of the two methods.
Arch Orthop Trauma Surg 2005;125(2): 73-79.
JF, Dehne E, Lafollette B. Closed reduction and early cast-brace
ambulation in the treatment of femoral fractures. II. Results in one
hundred and forty-three fractures. J Bone Joint Surg Am
1973;55(8):1581-1599.
JF, King P. Closed reduction and early cast-brace ambulation in the
treatment of femoral fractures. I. An in vivo quantitative analysis of
immobilization in skeletal traction and a cast-brace. J Bone Joint Surg
Am 1973;55(8):1559-1580.
BL. Varus collapse of comminuted distal femur fractures after open
reduction and internal fixation with a lateral condylar buttress plate.
Am J Orthop 2003;32(1): 27-30.
I, Moro Rodriguez E, De Pedro Moro JA, et al. Antegrade nailing for
fractures of the distal femur. Clin Orthop Relat Res 1998
May(350):74-79.
KA, Su E, Tejwani NC, et al. Treatment of complex tibial plateau
fractures using the less invasive stabilization system plate: clinical
experience and a laboratory comparison with double plating. J Trauma
2004;57(2):340-346.
and dislocation compendium. Orthopaedic Trauma Association Committee
for Coding and Classification. J Orthop Trauma 1996;10( Suppl 1):v-ix,
1-154.
DJ, Alms M, Cruz MM. Hinged cast and roller traction for fractured
femur. A system of treatment for the Third World. J Bone Joint Surg Br
1985;67(5):750-756.
GJ. Temporary external fixation for the management of complex intra-
and periarticular fractures of the lower extremity. J Orthop Trauma
2002;16(9):678-685.
GJ, Berry DJ, Jacofsky DJ, et al. Treatment of supracondylar femur
nonunions with open reduction and internal fixation. Am J Orthop
2003;32(11):564-567.
NL, Harris I, Hazratwala K. Retrograde nailing versus fixed-angle blade
plating for supracondylar femoral fractures: a randomized controlled
trial. ANZ J Surg 2006; 76(5):290-294.
JH, Lane JM. Treatment of pathologic fractures of the distal femur with
the Zickel supracondylar nail. Clin Orthop Relat Res 1990
Jan(250):216-220.
WL, Brooker AF Jr. Distal femoral fractures. Comparison of open and
closed methods of treatment. Clin Orthop Relat Res 1983
Apr(174):166-171.
SL, Trager S, Green S, et al. Management of supracondylar fractures of
the femur with the GSH intramedullary nail: preliminary report. Contemp
Orthop 1991;22(6): 631-640.
C, Synnott K, McCormack D. Above-knee Ilizarov external fixation for
early periprosthetic supracondylar femoral fracture—a case report. Knee
2005;12(2): 145-147.
L, Persson BM. Supracondylar femoral fractures as a complication to
Ender nailing of trochanteric fractures. A new device for
osteosynthesis. Arch Orthop Trauma Surg 1980;97(1):51-55.
PJ. Distal femur fractures with complex articular involvement:
management by articular exposure and submuscular fixation. Orthop Clin
North Am 2002;33(1): 153-175, ix.
PJ, Stannard JA, Zlowodzki M, et al. Treatment of distal femur
fractures using the less invasive stabilization system: surgical
experience and early clinical results in 103 fractures. J Orthop Trauma
2004 Sep;18(8):509-520.
PJ, Stannard J, Zlowodzki M, et al. Distal femoral fracture fixation
utilizing the Less Invasive Stabilization System (L.I.S.S.): the
technique and early results. Injury 2001; 32( Suppl 3):SC32-47.
C, Muller M, Miclau T. Evolution of minimally invasive plate
osteosynthesis (MIPO) in the femur. Injury 2001;32( Suppl 3):SC14-23.
C, Schandelmaier P, Miclau T, et al. Transarticular joint
reconstruction and indirect plate osteosynthesis for complex distal
supracondylar femoral fractures. Injury 1997;28( Suppl 1):A31-41.
A, Jasani V, Butt MS. Management of distal femoral fractures in elderly
patients using retrograde titanium supracondylar nails. Injury
2000;31(3):169-173.
P, Singh GK, Singh M, et al. Treatment of Gustilo grade III B
supracondylar fractures of the femur with Ilizarov external fixation.
Acta Orthop Belg 2006;72(3): 332-336.
GS. Symposium. Rigid internal fixation of fractures. Supracondylar
fractures of the femur: editorial comment and comparative results. Clin
Orthop Relat Res 1979 Jan-Feb(138):9-12.
SL, Pozo JL, Muirhead-Allwood WF. Coronal fractures of the lateral
femoral condyle. J Bone Joint Surg Br 1989;71(1):118-120.
M, Konrad G, Sudkamp N. Femur-LISS and distal femoral nail for fixation
of distal femoral fractures: are there differences in outcome and
complications? Clin Orthop Relat Res 2004 Sep(426):252-257.
RD, Bucholz RW, Grogan DP. Surgical treatment of displaced, comminuted
fractures of the distal end of the femur. J Bone Joint Surg Am
1982;64(6):871-879.
TJ, Watson T, Green SA, et al. Complications of surgically treated
supracondylar fractures of the femur. J Trauma 1987;27(4):402-406.
E, Ostrum RF, DiCicco J, et al. Effects of retrograde femoral
intramedullary nailing on the patellofemoral articulation. J Orthop
Trauma 1999;13(1):13-16.
ME, Perren SM, Allgöwer M, Arbeitsgemeinschaft für Osteosynthesefragen.
Manual of internal fixation: techniques recommended by the AO-ASIF
Group. 3rd ed. Berlin: Springer-Verlag; 1991.
CS 2nd, Grantham SA, Shelton ML. Supracondylar fracture of the adult
femur. A study of one hundred and ten cases. J Bone Joint Surg Am
1967;49(4):591-613.
SE, Segina DN, Aflatoon K, et al. The association between
supracondylar-intercondylar distal femoral fractures and coronal plane
fractures. J Bone Joint Surg Am 2005; 87(3):564-569.
S. Operative treatment of supracondylar-condylar fractures of the
femur. Technique and results in fifteen cases. J Bone Joint Surg Am
1972;54(5):1015-1032.
S. Supracondylar, intraarticular fracture of the femur. Results of
operative reconstruction. Acta Orthop Scand 1971;42(5):435-437.
RF, Geel C. Indirect reduction and internal fixation of supracondylar
femur fractures without bone graft. J Orthop Trauma 1995;9(4):278-284.
AA, Smith WR, Silva S, et al. Treatment of distal femur and proximal
tibia fractures with external fixation followed by planned conversion
to internal fixation. J Trauma 2008;64(3):736-739.
MJ, Cole JD. Two-sstaged delayed open reduction and internal fixation
of severe pilon fractures. J Orthop Trauma 1999;13(2):85-91.
AR, Yue JJ, Taffet R, et al. Less invasive stabilization system for
treatment of distal femur fractures. Am J Orthop 2004;33(5):250-255.
WM, Bellabarba C, Lewis R, et al. Angular malalignment after
intramedullary nailing of femoral shaft fractures. J Orthop Trauma
2001;15(2):90-95.
WM, Loftus T, Cox C, et al. Locked plates combined with minimally
invasive insertion technique for the treatment of periprosthetic
supracondylar femur fractures above a total knee arthroplasty. J Orthop
Trauma 2006;20(3):190-196.
J, Tornetta P 3rd, Ritter C, Geller J. Neurologic and vascular
structures at risk during anterior-posterior locking of retrograde
femoral nails. J Orthop Trauma 1998; 12(6):379-381.
MA, Faris PM, Keating EM. Anterior femoral notching and ipsilateral
supracondylar femur fracture in total knee arthroplasty. J Arthroplasty
1988;3(2):185-187.
R, Regazzoni P, Ruedi TP. Treatment of supracondylar-intracondylar
fractures of the femur using the dynamic condylar screw. J Orthop
Trauma 1989;3(3):214-222.
P. Ilizarov external fixation for severely comminuted supracondylar and
intercondylar fractures of the distal femur. J Bone Joint Surg Br
2002;84(1):148-149.
P, Gossling T, Partenheimer A, et al. [Distal fractures of the femur].
Chirurgie 2002;73(12):1221-1233; quiz 33-34.
M, Muller M, Kaab M, et al. Less invasive stabilization system (LISS)
in the treatment of distal femoral fractures. Acta Chir Orthop
Traumatol Czech 2003;70(2): 74-82.
M, Muller M, Krettek C, et al. Minimally invasive fracture
stabilization of distal femoral fractures with the LISS: a prospective
multicenter study. Results of a clinical study with special emphasis on
difficult cases. Injury 2001;32( Suppl 3):SC48-54.
M, Muller M, Regazzoni P, et al. Use of the less invasive stabilization
system (LISS) in patients with distal femoral (AO33) fractures: a
prospective multicenter study. Arch Orthop Trauma Surg
2005;125(2):102-108.
RD. Anterior femoral notching and ipsilateral supracondylar femur
fracture in total knee arthroplasty. J Arthroplasty 1988;3(4):381.
KD, Brueckmann FR. Rush-pin fixation of supracondylar and intercondylar
fractures of the femur. J Bone Joint Surg Am 1982;64(2):161-169.
JA, Franklin A. Supracondylar fracture of the femur following
Attenborough stabilized knee arthroplasty treated by a long-stem
prosthesis plus internal fixation. Injury 1984;16(1):65-66.
M, Sanders R, DiPasquale T, et al. A staged protocol for soft tissue
management in the treatment of complex pilon fractures. J Orthop Trauma
1999;13(2):78-84.
P, Ryoppy S, Huittinen VM. AOI osteosynthesis of fractures of the
distal third of the femur. Acta Orthop Scand 1971;42(2):162-172.
AJ, Jones AL, Reinert CM. The “swashbuckler”: a modified anterior
approach for fractures of the distal femur. J Orthop Trauma
1999;13(2):138-140.
S, Szporn MN, Cobelli NJ, et al. Cemented internal fixation for
supracondylar femur fractures in osteoporotic patients. J Orthop Trauma
1990;4(2):151-157.
AB, Driver R, Kregor PJ, et al. Long-term functional outcomes after
intra-articular distal femur fractures: ORIF versus retrograde
intramedullary nailing. Orthopedics 2008;31(8):748-750.
P 3rd, Tiburzi D. Anterograde interlocked nailing of distal femoral
fractures after gunshot wounds. J Orthop Trauma 1994;8(3):220-227.
M, Collinge C. Early results of the less invasive stabilization system
for mechanically unstable fractures of the distal femur (AO/OTA types
A2, A3, C2, and C3). J Orthop Trauma 2004;18(8):503-508.
RA, Hansen ST Jr, Clawson DK. Closed intramedullary nailing of femoral
fractures. A report of five hundred and twenty cases. J Bone Joint Surg
Am 1984;66(4): 529-539.
M, Bhandari M, Marek DJ, et al. Operative treatment of acute distal
femur fractures: systematic review of 2 comparative studies and 45 case
series (1989 to 2005). J Orthop Trauma 2006;20(5):366-371.
