Chronic Medial Instability of the Elbow
IV – Elbow Reconstruction > Part B – Evaluation and Treatment of
Elbow Disorders > 49 – Chronic Medial Instability of the Elbow
participation in sports that involve increased stress on the elbow.
Much of the attention on the medial pathology around the elbow used to
be related to throwing; presently, there are other sports that strain
the medial structures, causing chronic medial instability. The process
of better understanding the mechanics and pathophysiology of the elbow
has increased our knowledge and treatment of chronic medial instability.
baseball pitching, javelin throwing, tennis, throwing in football, and
also floor gymnastics, expose elbows repetitively to valgus stress
forces.
flexion, the congruous osseous anatomy is the primary restraint. With
lesser elbow flexion, between 20 and 120 degrees, the medial soft
tissue restraints adopt a primary role in medial stability. In that arc
of motion, the radial head is the secondary restrain on valgus stress.
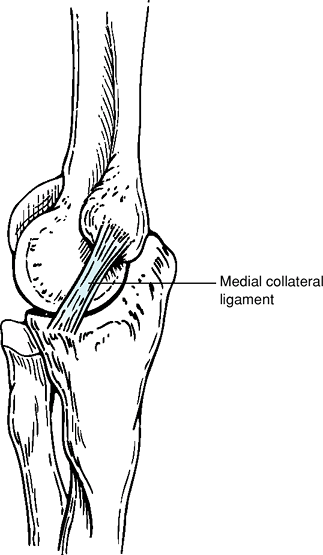
structures that reinforce the capsule and form the medial collateral
ligament (MCL) (Fig. 49-1). The anterior bundle
of the MCL is the most important portion of the complex; it originates
from the anteroinferior surface of the medial epicondyle and ends at
the sublime tubercle of the ulna. Recent evidence suggests a two-band
structure for the anterior bundle: the anterior band, which functions
between 30 and 90 degrees of flexion (with 70 degrees being the
position of greatest contribution to stability) and the posterior band,
which is stressed most when flexion reaches 120 degrees. The posterior
bundle of the MCL originates from the epicondyle and ends in the medial
margin of the semilunar notch. It plays a secondary role in valgus
stability. The transverse bundle originates from the medial olecranon
and ends in the medial coronoid process and also plays a minor role in
valgus stability.
as throwing. With repetitive movements that produce valgus stress
moments, the medial soft tissue structures are subjected to combined
tension and bending stresses. An extension moment may also be present,
producing internal shear stresses on the deep fibers of the MCL. This
process is often a component of a multiple-compartment involvement (Table 49-1)
that affects both the anterior and posterior compartment of the elbow.
This can be best understood as a result of valgus extension overload
syndrome.
flexion-to-extension motion is accompanied by valgus stress moments.
These combined forces produce medial tension forces of 300 N and
external compression forces of 900 N. The repetitive nature of throwing
puts the medial structures at risk of suffering chronic microtrauma,
with partial or full rupture of the structures through chronically
stressed ligaments.
extreme positions of flexion, wrist extension, and shoulder abduction,
the pressures in the ulnar tunnel increase up to six times. Additional
pathology such as osteophytes, calcification of the MCL, and
inflammation of the MCL can contribute to compression. Posteromedial
osteophyte formation at the olecranon usually occurs in the latter
stages of disease. With combined extension and valgus, early contact
between the olecranon and the fossa is produced, resulting in
posteromedial impingement. As a result of compression
forces
across the radiocapitellar compartment, degenerative changes can be
found beginning with chondromalacia of the capitellum to complete bone
degeneration. In young athletes, osteochondritis dissecans may occur.
 |
|
Figure 49-1 Medial collateral ligament.
|
involve overuse activities related to repetitive motion in sports, the
history is essential. The examiner should investigate about the events
that initiate the pain and if the evolution was acute in onset or
chronic. In chronic medial elbow instability, pain is usually
indistinct around the medial side with a slow progression over the
season. Typically athletes complain about their inability to throw with
the same power and speed before the onset of the injury, accompanied by
pain in the late acceleration phase. On occasion a sudden dramatic pop
may be felt by the patient when the medial collateral ligament ruptures.
|
TABLE 49-1 Spectrum of Involvement
|
|
|---|---|
|
recorded with the forehand in supination for extension and flexion. If
degenerative changes are present in the posterior compartment, pain may
result at full extension during testing
palpate the MCL through its normal course distal to the epicondyle. A
valgus stress can also be applied to the elbow to examine for medial
joint opening. Ulnar nerve palpation should also be done posterior to
the course of the MCL to examine for tenderness or a possible Tinel
sign.
while the examiner applies a valgus stress, the arm is extended from a flexed position (Fig. 49-2). Pain is reproduced at about 70 degrees of flexion. Pain should be similar to the one produced by sports activities.
 |
|
Figure 49-2
Moving valgus stress test. The examiner must put the arm in 90 degrees of abduction and external rotation, and, while applying a valgus stress, the arm is extended from a flexed position. |
 |
|
Figure 49-3
Milking maneuver. The affected elbow is flexed >90 degrees and the other hand grasps the thumb under the injured arm, exerting a valgus stress. |
other hand grasps the thumb under the injured arm, exerting a valgus
stress (Fig. 49-3). The examiner palpates the MCL for pain.
instability, the history and physical exam are most important.
Additional imaging studies can give further information to help confirm
the diagnosis. Standard radiographic evaluation is routinely done,
searching for calcification of the MCL. Degenerative changes may also
be found, especially loose bodies and posteromedial osteophytes of the
olecranon.
under anesthesia may be helpful. However, it is important to remember
that medial joint opening with stress radiographs can also be found in
the asymptomatic thrower. Thus, a careful correlation with the clinical
examination should be performed.
high-demand overhead athlete with suspected medial instability in whom
clinical evaluation suggests chronic medial elbow instability. The use
of intra-articular gadolinium increases the positive results of MCL
tears.
with medial elbow instability. Initially, the management includes a
nonoperative program of rest combined with anti-inflammatory
medications A formal rehabilitation program should be initiated. This
should be done with an emphasis on regaining motion, followed by a
dynamic stabilization and strengthening process that might permit the
return to sports activities. Rehabilitation may require ≤16 weeks. With
a nonoperative treatment, only between 50% and 60% of the patients may
return to their previous level of throwing.
the technique of choice for those patients who fail conservative
treatment. Direct repair of the ligament is not usually possible.
Either autograft or allograft can be used. It is unclear in the
literature if there is an advantage of one over the other. Ipsilateral
palmaris or plantaris tendon has often been used for reconstruction.
Many patients will have an inadequate palmaris, and for this reason,
allograft hamstring tendons are often quite helpful.
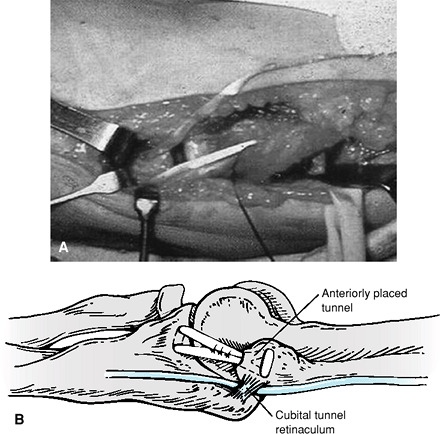
or a posterior incision. A posterior incision will provide access to
the medial side but will help protect the underlying cutaneous nerves
to a greater extent. A muscle split of the flexor carpi ulnaris allows
for good surgical exposure and lowers the morbidity produced by a
detachment of the flexor/pronator group. Transposing the ulnar nerve
routinely is often not necessary and can increase the morbidity of the
procedure.
other, with the first one locmated slightly anterior to the sublime
tubercle of the ulna in the medial aspect of the coronoid. The
principal humeral drill hole is located at the anatomic origin, and two
additional holes are placed anterior in the lateral column. Next, the
graft is passed initially through the distal holes and through the
anatomic hole in the humerus (Fig. 49-4). The
graft is then sutured on itself with multiple nonabsorbable sutures.
The split in the flexor pronator muscles is closed. A posterior splint
at 90 degrees of flexion is used to immobilize the elbow. After 10 to
14 days, sutures are removed and the rehabilitation process begun.
After discontinuing the splint, active progressive ROM exercises are
started in the shoulder and elbow. A brace can be used during
rehabilitation to protect the elbow from valgus stress. After restoring
full range of motion, a strengthening program is begun first with
isometric exercises, followed by resistance exercises. Attention should
be focused on the flexor pronator group, which provides dynamic
stabilization on the medial side of the elbow.
the athlete may throw at 50% of maximum velocity and can increase to
75% by the ninth month. Full rehabilitation of the athlete will take at
least a year of treatment.
 |
|
Figure 49-4 Tendon graft in place.
|
the athlete is returned to the previous level of competition. Reports
in the literature vary between 68% and 96% of athletes obtaining a good
to excellent result after MCL reconstruction.
JE, Jobe FW, Glousman RE, et al. Medial instability of the elbow in
throwing athletes: treatment by repair or reconstruction of the ulnar
collateral ligament. J Bone Joint Surg Am. 1992;74:67–83.
WH, Jobe FW, Yocum LA, et al. Ulnar collateral ligament reconstruction
in athletes: muscle splitting approach without transposition of the
ulnar nerve. J Shoulder Elbow Surg. 2001;10:152–157.
