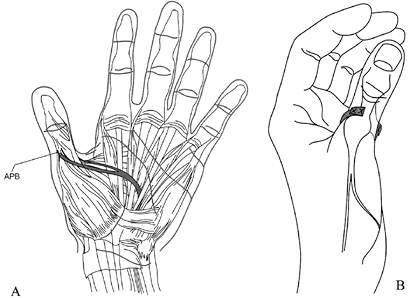
ULNAR NERVE PARALYSIS
-
Flexion and ulnar deviation of the wrist
-
Flexion of the ring and little fingers
-
Independent flexion at the metacarpal (MP) joints of all fingers
-
Interphalangeal (IP) extension of all fingers
-
Abduction–adduction of all fingers
-
Adduction–flexion of the carpometacarpal joint
-
Adduction–flexion of the MP joint of the thumb
flexor carpi ulnaris (FCU), the strongest muscle in the forearm. The
FCU is an important element in many physical actions such as swinging
an ax, hammer, or club; cutting with a knife; and pounding on a desk.
Paralysis results in a general sense of weakness in a variety of
actions, but there is no total loss of any action, nor is there a
deformity at rest.
performing tendon transfers to balance the wrist following high ulnar
nerve palsy. For some manual workers, however, the loss of this
powerful muscle is a handicap. For a carpenter, who might feel disabled
by an ulnar-flexor quadrant weakness at the wrist, for example, it
might be practical for the surgeon to transfer the flexor carpi
radialis (FCR) to the insertion of the FCU, inasmuch as the
radial-flexor quadrant is unaffected in ulnar palsy.
weakened in high ulnar palsy, with loss of flexor profundus function in
both fingers, in particular because the strength
of
the surviving median-supplied flexor digitorum superficialis (FDS) to
the little finger is less than one-third the strength of the profundus.
In the ring finger, the FDS is two-thirds the strength of the
profundus, so that only two fifths of the flexor strength of the ring
finger survives. The flexor weakness of the ring finger, however, is
partially masked by the fact that the paralyzed ulnar-supplied part of
the profundus moves to some extent with the median-supplied profundus
to the middle finger. This cross-finger support is variable and only
partial, because the actual muscle fibers are not shared but are linked
by connective tissue, which allows some independence.
fingers; for this reason, no deformity is caused by paralysis of the
long flexors. Because deformity is more obvious than functional
disability, substitution is rarely offered for the paralyzed long
flexors. If the weakness seems really disabling, the profundus tendons
of the ring finger and little finger may be sutured side-to-side to the
profundus of the middle finger in the forearm so that they move fully
together. This technique does not really add strength; it merely
“shares” the weakness more evenly. If one adds the tension fractions
(see Chapter 54, Chapter 54, Fig. 54.1, Fig. 54.2)
of all the muscles that normally combine to flex the little finger and
ring finger, including the intrinsic muscles, the total is 14.6. Of
these, only 2.9—about one fifth—survive in high ulnar palsy.
by replacing the intrinsic muscles by transfers, the total tension
fraction is commonly 1.0 to 3.0, shared between four fingers. The
result is a gross weakness of ulnar-side grip, only about 25% of normal
strength. Yet most forearm muscles remain unparalyzed, and the forearm
and hand retain at least 70% of their total tension capability.
specific weakness of ulnar-side grip results in a significant
disability for all actions that use the width of the hand to control
radial-ulnar torque. One of the most common of these actions of the
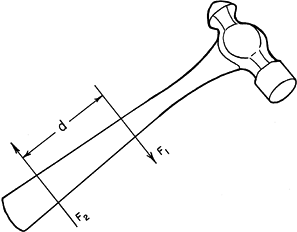
hand is the use of a hammer (Fig. 57.1). All
hand movements that require a twist or turn, either in a
pronation-to-supination direction or in ulnar deviation, require that
the object be held in such a way as to transmit a torque, by means of a
force couple. The handle of a hammer is
moved by a force couple when one force (F2) pulls upward and a
simultaneous force (F1) pushes downward, with a distance between them,
along the handle. The hammer head is forced down while the end of the
handle may move up, or the whole hammer may move, with F1 moving more
than F2. This produces a torque on the hammer proportional to the
magnitude of the forces multiplied by the perpendicular distance
between them.
 |
|
Figure 57.1. To strike with a hammer, it is necessary to produce a “force couple”: Two forces move in opposite directions.
|
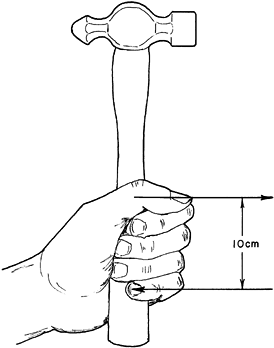
is just as important as the amount of force. In the case of a couple,
twice as much total force is needed to produce the same torque if the
two components are moved 50% closer together. In a medium-sized hand,
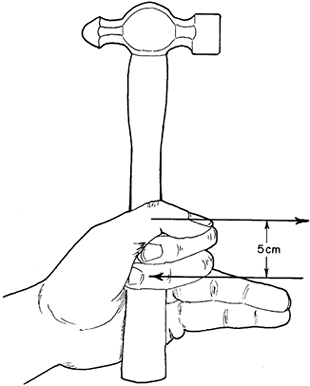
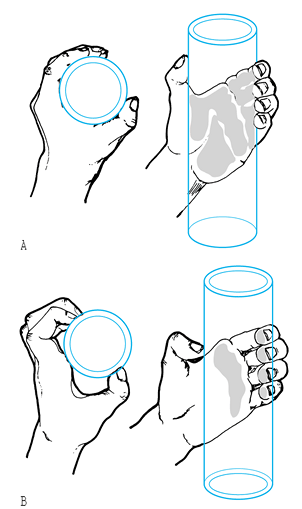
the width of an effective grip is about 10 cm (Fig. 57.2). In the same hand, if only the index and middle fingers are strong, the effective width of the hand is reduced to about 5 cm (Fig. 57.3).
 |
|
Figure 57.2.
A normal hand may be about 10 cm wide where it holds a hammer. In the force stroke, the thumb web pushes while the little and ring fingers pull. In retracting the hammer, the hypothenar mass pushes, and the index and middle fingers pull. |
 |
|
Figure 57.3.
In high ulnar palsy, the little and ring fingers may be so weak that only the middle finger can pull firmly enough to complete the couple. This is only half as wide as in a normal hand. The hammer is unstable and its action is weak. For many tasks involving torque, it is better to have strong index and little fingers, even if the middle finger is weak. |
grip an object, it will have only 25% of its power to turn, twist, or
swing an object. The patient has difficulty describing the weakness,
saying only, “I feel my hand is
weak.”
The dynamometer is not a measure of the dexterity strength of a hand,
but only of squeeze power. Most manual tasks demand multidirectional
torque, which requires a broad hand with strength at each of its
borders.
finger flexors is the reversal of the metacarpal arch, usually thought
of as being caused by paralysis of the intrinsic muscles. The best
muscles to control the arch, however, are those that cross the fifth
carpometacarpal joint on the palmar side, thus serving as
carpometacarpal flexors. These are the hypothenar muscles and the long
flexors to the ring and little fingers. Brandsma has noted that
patients with ulnar palsy who retain ulnar-supplied profundus rarely
have severe arch reversal (W. Brandsma, Carville, Louisiana, personal
communication, 1984).
in the ulnar-paralyzed hand should suggest rethinking the patterns of
correction. An obvious method to increase ulnar-side grip strength is
to use the extensor carpi radialis longus (ECRL) to reactivate the
flexor profundus tendons to the ring finger and little finger. The
muscle fibers of the ECRL are long enough to allow a good range of
finger flexion with a little synergistic extension of the wrist. The
ECRL is also strong enough to compensate for the ulnar profundus loss
and helps to rebalance the wrist, which is relatively overpowered by
the dorsal and radial side in high ulnar palsy.
palsy is independent flexion at the MP joints. This loss of flexion is
important because it is the basis for the deformity of claw hand.
Uncontrolled extension of the MP joints results in failure of the long
extensor tendons to extend the IP joints. It also changes the sequence
of flexion of the fingers, making it impossible to flex the proximal
segment ahead of the distal segments. Therefore, when the hand closes
on an object, the force of grasp is transmitted only through the
fingertips rather than through the whole palmar surface of the fingers.
High localized tip pressure results, leading to inhibition of the use
of strength in sensitive fingers, or to pressure sores and injuries to
fingertips in insensitive fingers (Fig. 57.4 and Fig. 57.5).
 |
|
Figure 57.4. A: Normal hand grasping a cylinder. The area of skin contact is shaded. B: Claw hand grasping a cylinder. The area of contact is limited to the fingertips and the metacarpal heads. (From Brand PW. Clinical Mechanics of the Hand, 3rd ed. St. Louis: CV Mosby, 1999:215–216.)
|
 |
|
Figure 57.5.
This patient had loss of sensation from Hansen’s disease. The little ulcers and scars are in the most characteristic position for a patient with functional clawing. The high stress occurs just in front of the fingernail at the end of the phalanx. (From Brand PW. Clinical Mechanics of the Hand, 3rd ed. St. Louis: CV Mosby, 1999:290.) |
fingers, not just in the ring and little fingers. Clawing may occur
earliest and most obviously in the ulnar-side fingers,
because
they lose all intrinsic muscles in ulnar palsy, whereas the index and
middle fingers usually have median-supplied lumbricals. The lumbricals,
however, can exert only about one tenth the tension of the combined
interossei. The presence of intact lumbricals may delay the onset of
clawing or make it less severe; however, when the end of the finger is
pushed backward, as when pinching against the thumb, the MP joint
retreats into extension and the proximal interphalangeal (PIP) joints
hyperflex.
thumb. It can be tested in a patient who has no clawing of the index
and middle fingers by asking her to hold the intrinsic-plus position
(MP joint flexed and IP joints extended) while the examiner pushes
backward with a finger against the middle of the front of the proximal
phalanx of the patient’s finger. If this test causes the finger to
buckle into PIP flexion, weakness of the intrinsic muscles is
indicated, as is a need to rebalance the finger to compensate for
present weakness and to prevent clawing later.
the next section, but first let us emphasize that we are recommending
the restoration of active flexion, not just the provision of a block to
limit extension of the MP joints.
may be easily corrected simply by providing a passive block to prevent
hyperextension, thus allowing the long extensors to extend the IP
joints. Surgery proposed to provide a passive block includes tenodesis,
capsulodesis, bone block, or even an extensive scar on the palmar side
of the MP joint. The result in each case is a beautiful, straight hand.
not cosmetic, in that as the hand begins to close on an object the
sequence of closure is reversed. The proximal segment should flex
first, followed by the distal segments, each making contact with the
object and accepting a share of the load and the pressure; in ulnar
palsy, the tips flex first, and the fingers curl down into the fist,
tips first. Thus the object is grasped with all the pressure on the
fingertips (Fig. 57.4).
-
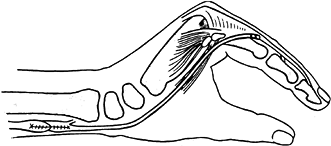
Direct action of the lumbricals together
with those interosseus muscles that insert into the lateral band create
direct extension of the PIP and distal interphalangeal (DIP) joints.
This mechanism is effective even in radial nerve palsy, which
inactivates the long extensors. -
The intrinsic muscles hold the MP joint
flexed without flexing the IP joints. Thus the long extensors can be
prevented from extending the MP joints, while they remain effective on
the IP joints. -
The unique action of the lumbricals pulls
the profundus tendons distally (by their origins on profundus tendons),
while pulling the lateral bands proximally to facilitate IP extension
with MP flexion.
reproduced by tendon transfer, so we shall consider only the other two
mechanisms. By bringing the tendon of any muscle across the palmar side
of the intermetacarpal ligament and attaching it to the lateral band,
both extension mechanisms are accomplished. Such a transfer, which
flexes the MP joints and extends the IP joints, corrects both elements
of the claw hand deformity (Fig. 57.6). We have found this pattern most successful.
 |
|
Figure 57.6.
Tendon transfer to correct intrinsic-minus hand. The transferred tendon or graft passes in front of the transverse intermetacarpal ligament and into the lateral band. (From Milford L. The Hand, 2nd ed. St. Louis: CV Mosby, 1982.) |
The greater part moves directly into bone and flexes only the MP joint.
Thus the fingers are free to flex at the MP joint with or without IP
extension. Following tendon transfer into the lateral band, with no
intrinsic transfer into the proximal phalanx, the total force of the
transfer for MP flexion must also provide tension for IP extension. In
hypermobile fingers, this constant pull on the lateral bands may result
in a degree of progressive hyperextension of the PIP joints that can
become a true swan-neck deformity—most common in cases where the FDS
tendon has been removed and used for transfer to the lateral band (1). The PIP joint is thus deprived of its prime flexor, which has then become an uncontrolled extensor.
Stiles–Bunnell transfer of the superficialis tendons for claw hand
correction except in cases where the PIP joints have become so stiff in
flexion, even after preoperative therapy, that hyperextension is very
unlikely to develop. Do not perform attachment of any transfer for
intrinsic replacement to the lateral band in fingers that have
hypermobile PIP joints. In such cases, and especially in those deprived
of their FDS, it is better to attach the tendon transfer to the flexor
tendon sheath, as suggested by Brooks (4) and Zancolli (13,14).
In such cases, the long extensors hold the IP joints in extension in
the first stage of total finger flexion, although at a higher total
cost of energy (because the intrinsic MP flexors must work against and
overcome the MP extension moment from the extrinsic extensors).
intrinsic muscles supplied by the ulnar nerve. The median-supplied
lumbricals are weak enough and are near enough to the
abduction–adduction axis of the MP joints that they have only a small
active abduction capability.
abductor (away from the midline of the hand) unless there is an
effective adductor to restore the side-by-side position of all fingers.
Most tasks can be accomplished by side-by-side fingers, as long as they
have independent flexion and extension. Fingers that can abduct but not
adduct look strange, and the projecting fingers become caught on the
edges of pockets or bags and are subject to injury in the workplace.
tendons are needed, one to each side of each finger. The first editions
of Bunnell’s famous book on hand surgery (5)
described how all superficialis tendons should be split to give the
required eight tendon insertions, and instructed us to transfer both
slips of any one tendon to the same side of adjacent fingers.
India in 1948, the first edition of Bunnell was my “bible” and I
faithfully did as instructed, and my therapists struggled without
success to teach my leprosy patients how to spread and adduct their
fingers after surgery. Years later, I visited Bunnell and asked if I
could see his results. He confessed that he had never succeeded in
getting any patient to control abduction and adduction with the
split-superficialis operation that formed the frontispiece of the first
edition of his book. It had just seemed a sensible pattern to use.
Nevertheless, I am grateful for the book.]
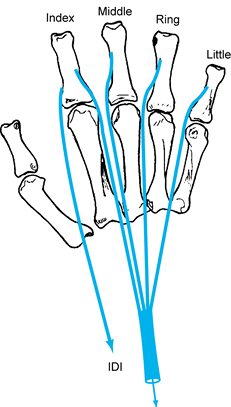
of lateral movement of fingers, we now recommend that all intrinsic
replacement tendons or grafts should be attached on the side of the
finger that will pull it toward the line between the index and middle
fingers. Thus, the middle, ring, and little fingers are moved radially
by the insertions on their radial sides, and the index finger is moved
toward the ulna by its ulnar-side insertion. The result will be that
all fingers will ordinarily be held side by side. In addition, a
replacement for the first dorsal interosseous muscle may be added to
the radial side of the index finger, if deemed necessary (Fig. 57.7).
 |
|
Figure 57.7.
For correction of ulnar paralysis, a single motor may be used for the radial side of the middle, ring, and little fingers and the ulnar side of the index finger. A separate motor may be used for the radial side of the index finger if necessary. (From Brand PW. Clinical Mechanics of the Hand, 3rd ed. St. Louis: CV Mosby, 1999:291.) |
as a piano player or typist might require. This motion does not need a
strong muscle, and even the extensor indicis proprius (EIP), properly
rerouted, might be adequate. The second is to stabilize the index
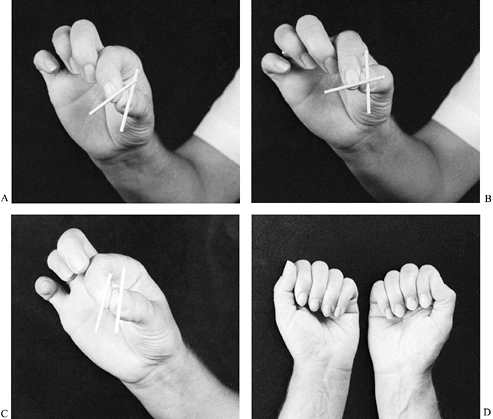
finger against the thrust of the thumb in pinch. A normal pinch is not
“square,” pulp to pulp. There is at least a 30° angle between the
thumbnail and the fingernail, so the transverse vector of the thumb
force that pushes the finger across the palm is perhaps half as great
as the vector that pushes the finger dorsalward from palmarly (Fig. 57.8A).
 |
|
Figure 57.8. A: Normal pinch angle of about 30° between markers on thumbnail and fingernail. Pinch is stable by action of intrinsic muscles. B: With index finger abducted, the angle between thumbnail and fingernail is greater, making an unstable pinch. C:
Desirable pinch in an ulnar palsy patient. An ulnar-side intrinsic transfer to the index finger acts like a first palmar interosseous and circumducts the index MP joint so as to oppose the thumb pulp. This results in a true square pinch that needs no other intrinsic muscle support. D: Key pinch does not demand much intrinsic muscle support of the index finger, providing it is supported by all the fingers flexed together. |
finger abductor about half as strong as the flexors. The first dorsal
interosseous muscle, at a tension fraction of 3.2, is about right. The
index finger has no true adduction–abduction axis, however, but moves
around a variable cone (2). There is also a
link between abduction and rotation. Thus, a replacement for the first
dorsal interosseous will twist the finger while it abducts, so that it
faces more across the palm than before, providing a pinch that is less
square.
it increases the angle between the line of thrust of the thumb and that
of the index finger (Fig. 57.8B). This
configuration makes the pinch more unstable, requiring support by a
force vector that opposes the result of the two major flexion forces of
the thumb and index finger. In effect, the first dorsal interosseous
muscle, by being a rotator, increases the need for itself as an
abductor.
made for the first dorsal interosseous muscle, but one is provided for
the first palmar interosseous on the ulnar side of the finger, the
result will be to twist the finger into external rotation and diminish
the angle by which the index finger meets the thumb. The result of an
“ulnar-side
only”
attachment of an intrinsic replacement to the index finger is that the
thumb and index finger meet in a true square pinch, with fingernail and
thumbnail parallel and with thumb flexors opposing finger flexors
squarely, so that no lateral stabilization is necessary (Fig. 57.8C).
dorsal interosseous is not advised, except as a device for spreading
the fingers apart. For the purposes of pinch, the first palmar
interosseous (we may call it “the opponens indicis”) is all that is
needed.
or pulp pinch, then there is more reason for a first dorsal
interosseous replacement, since it directly supports the side of the
index finger against the thumb. Even in key pinch, however, this is
unnecessary if the patient usually pinches against an index finger,
which is supported by all four fingers flexed together (Fig. 57.8D).
the hand, therefore, it is best to use one muscle only as a replacement
for the intrinsics to all four fingers, and to extend it by four
strands of tendon or tendon graft. Attach the tendon to the lateral
band on the radial side of the middle, ring, and little fingers, and to
the ulnar-side lateral band of the index finger.
muscles to the fingers is greater than the total of the flexor
profundus. Thus, it would seem that a powerful muscle would be required
for each finger to replace the lost tension. In the normal hand,
however, the total intrinsic tension to any finger is divided between
multiple insertions, and it would lead to gross imbalance to apply that
total tension to any one insertion on only one side of a finger.
one muscle, such as a single superficialis tendon, split into four
strands in the proximal palm and taken to one lateral band of each
finger. The ECRL (tension fraction, 3.5) is our favorite. It may be
used, with a free graft split into four insertions; or two weaker
muscles, such as the EIP and the extensor digiti quinti (EDQ) may be
used, with two insertions each (5).
we have sometimes used the palmaris longus (PL) (average tension
fraction, 1.2) with grafts to all four fingers; we have found that it
does correct the claw deformity in cases that are operated on early,
before bad habit patterns have developed and before the palmar plate
has become grossly stretched. The advantage of using the PL is that the
operation may be done immediately after any ulnar nerve injury in the
arm or upper forearm with the confidence that nothing has been lost,
even if the intrinsic muscles recover later. This is an important
advantage. Early surgery prevents the development of any deformity and
leaves the option of adding a stronger muscle a year or two later, if
the intrinsic muscles have not recovered and if the patient needs more
grasp strength.
popularized a technique for moving the FDS tendons from their insertion
on the middle phalanx to be attached to the flexor sheath in front of
the MP joint. This “lasso” operation deprives the PIP joint of its
prime flexor, but it leaves the muscle as a flexor of the MP joint.
This is similar to the old Stiles operation, except that the insertion
is central rather than to the lateral band (12).
It is also rather simple to perform, but it may create long-term
problems because the PIP joint is deprived of a flexor except by
contraction of the profundus, which is more effective at the DIP joint
than at the PIP joint when working against resistance (2).
of the thumb in Froment’s sign of ulnar palsy. In the fingers, the
deformity develops slowly, but finally a hyperflexed DIP joint and a
hyperextended PIP joint give rise to a swan-neck deformity. The lasso
operation should be reserved for the late correction of clawed fingers
that have become somewhat stiff in PIP joint flexion and therefore are
unlikely to become fully corrected or hyperextended.
Stiles–Bunnell with transfer of superficialis tendons) and the DIP
joints begin to show signs of persistent flexion, it is best to
intervene early with a profundus tenodesis in the middle segment with
the DIP joint just short of full extension. This technique transfers
profundus power from DIP joints to PIP joints and provides a more
satisfactory hand, even though active flexion of the DIP joints is lost
(Fig. 57.9).
 |
|
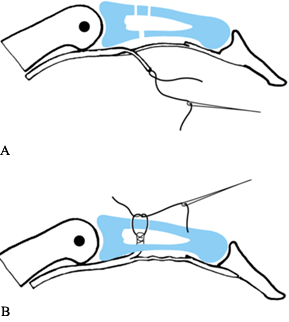
Figure 57.9. Profundus tenodesis in the middle segment. A:
The profundus tendon is split, and half divided distally. The proximal end of the middle phalanx has a 2 mm drill hole in the anterior cortex and two 1 mm holes in the dorsal cortex. B: The cut end of the profundus slip is drawn into bone, leaving half of the profundus in continuity. |
correction of claw hand. It is easy to misunderstand the relative
usefulness of each. Since surgeons and patients are so often concerned
about deformity, procedures such as the Stiles–Bunnell (12) or the lasso of Zancolli (13)
are often preferred because they are “strong” correctors of deformity.
They do not really add strength to the fingers, however; they take
strength away from PIP flexion and move it proximally to the MP joint.
area is relatively stronger, because it adds something to the fingers
from an area that is unaffected by paralysis. From the point of view of
added strength, Fowler’s operation using the EIP and EDQ (tension
fractions 1 plus 1 equal 2) is better, and the transfer of the ECRL or
the extensor carpi radialis brevis (ECRB) (tension, 3.5 or 4.2) may be
the best of all (11).
and patient appreciate quick correction of deformity. It is in the long
term, however, that the patient realizes the extent of the weakness and
how the removal of a strong flexor from the PIP joint is a high price
to pay for the flexion of the MP joint.
operations is that the tendons are all long enough for direct transfer
without grafts. If a single superficialis tendon is to be used for four
fingers (modified Stiles–Bunnell), the tendon should be withdrawn in
the proximal palm, just distal to the roof of the carpal tunnel, so
that each tendon strand can be passed to its own finger without having
to cross a palmar septum (5).
-
Divide the tendons of the EIP or EDQ over
the back of the MP joints, and withdraw them back to the carpal area.
Split each into two strands. -
Pick up each strand by its tip, using a curved tunneler that has been passed from the base of one side of each finger, in front of the transverse metacarpal ligament,
through an intermetacarpal space, appearing in the dorsal incision to
pick up its tendon and withdraw it to its point of insertion.
Accomplish this tunneling without penetrating the dorsal fascia that
overlies the extensor tendons. Some strands of fascia that lie on the
palmar and dorsal surfaces of the interosseous muscles in each space
may have to be penetrated. Most, however, may be avoided by gentle and
sensitive passage of the rounded nose of the tendon tunneler; feel for
weak areas or gaps in the fascia. -
It is best to pass the tendon strands to
the index and middle fingers through the second intermetacarpal space,
and the two strands to the ring and little fingers through the third
space. The strand to the little finger crosses the neck of the fourth
metacarpal on the palmar side on its way to the proximal phalanx of the
little finger. -
This route to the little finger sounds
complex, and there may be concern that adhesions will occur as the
tendon hugs the neck of the fourth metacarpal bone. It is not
difficult, however, if a curved, blunt-nosed tunneler is passed empty
from the little finger and angled across until the bone of the fourth
metacarpal neck is felt. Then slip the tunneler between the bone and
the flexor tendons, and turn immediately dorsally, through the
intermetacarpal space, and then proximally to the rerouting incision
over the wrist where the tendon strand is grasped and pulled through,
back to the finger.
that are common in the original Fowler’s operation: reversal of the
metacarpal arch and continued abduction of the little finger. If
adhesions form in this modification of Fowler’s operation, they occur
at the point of perforation of the fascia in the interosseous space,
not to the bone.
we prefer to use a wrist-moving muscle, such as the ECRL or the PL,
extended by grafts. The fingers are approached through the carpal
tunnel and along the lumbrical canals. The junction between the tendon
and the grafts is made in the distal forearm, proximal to the carpal
tunnel.
-
Divide the ECRL tendon near its insertion
and withdraw it proximally about midforearm through a transverse
incision. Make a second transverse incision in the anterior distal
forearm about 5 cm proximal to the wrist crease, centered over the PL. -
Pass a blunt-nosed tunneler into this
incision and direct it proximally beneath the tendons of PL, FCR, and
brachioradialis (BR) to appear in the proximal incision over the ECRL. -
Grasp the end of the tendon and pull it
through to the distal incision, where it is joined to a four-tailed
graft, either of a plantaris tendon (folded in two and each
P.1663
limb
split in two) or to a 12 mm wide strip of fascia lata, taken from the
lateral thigh and split into four tails in its distal two thirds. -
Make a rerouting incision in the center
of the proximal palm, just distal to the carpal tunnel. Pass a curved
tunneler through a split in the palmar fascia, deep and proximally,
until the bony-ligamentous floor of the carpal tunnel is felt, deep to
all tendons and sheaths. Then direct the tunneler toward the distal
forearm incision, between the FCU and the flexor tendons to the
fingers, until it appears in the wound. -
Grasp all the ends of the four tendon
strands with the tunneler and pull them into the palm. From here, pull
each strand separately to each finger, and attach it to the lateral
band (Fig. 57.6), or else to the flexor sheath in front of the MP joint, as suggested by Brooks (4). -
If the ECRB is to be used as a motor,
divide it at its insertion and withdraw it 10 cm up the forearm,
pulling a black thread behind it to identify its sheath. Remove the
distal 1–2 cm if required and attach a four-tailed graft to the stump. -
Grasp the four graft tails with tunneling
forceps and pull them back through the sheath, following the thread
marker. From there, tunnel each graft through an interosseous space to
its own finger. Grafts to the index and middle fingers pass through the
second intermetacarpal space, and grafts to the ring and little fingers
pass through the third space, using the same technique described for
the modified Fowler’s operation. -
Suture all grafts into position with the
wrist flexed (for tendons that pass through the carpal tunnel) or
extended (for the ECRB and the dorsal route). The MP joints are flexed
and the IP joints extended (Fig. 57.6). In this position, tendon tension should be minimal or even zero. -
In the postoperative splint, position the wrist straight and the fingers in full MP flexion and IP extension.
of the ECRB as a motor is that both the tendon or the tendon grafts
cross the carpometacarpal joints on the dorsal side. The result is an
increase of extensor torque on these joints for the ring and little
fingers, where there is already severe loss of flexor torque due to
high ulnar paralysis.
joints, especially in the fifth ray, producing a marked reversal of the
metacarpal arch. This is one more reason we prefer to route transfers
for intrinsic replacement across the palmar side of the hand, where, in
addition to their effect on the fingers, they can help stabilize the
mobile metacarpals and may even make it possible to cup the palm.
and usually results in deformities with hyperextension of the
metacarpophalangeal (MCP) joint (Jeanne’s sign) and hyperflexion of the
IP joint (Froment’s sign). These deformities result from loss of the
intrinsic muscles, which are strong MCP and carpometacarpal (CMC)
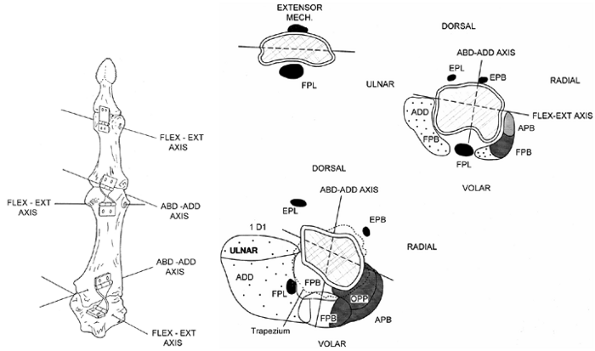
flexors (Fig. 57.10). The basic imbalance
producing these deformities is loss of flexion power at the proximal
and middle joints in the chain. There is also a loss of adduction power
at the CMC and MCP joints.
 |
|
Figure 57.10.
The mechanics of the thumb in ulnar palsy. The thumb is comprised of four bones linked by three joints. Each joint moves about one or more axes of rotation. The carpometacarpal joint has two axes, a flexion–extension axis in the trapezium and an abduction–adduction axis in the metacarpal. The metacarpophalangeal joint has two axes of rotation, a flexion–extension (FE) axis in the metacarpal head and an abduction–adduction (AA) axis in the proximal phalanx. The interphalangeal joint has one axis in the distal proximal phalanx. The muscles of the thumb and the external loads act across these axes, and the balance of the thumb depends on the balance of the torques about all of the axes of rotation of the thumb. The force the muscles can generate is determined by
their cross-sectional area. The mechanical advantage of the muscles is determined by their distances from, and directions of pull relative to, the axes. Cross sections of each thumb joint showing the bones, muscles, and axes of rotation are a good way to conceptualize the actions of the muscles on each axis. We can see that the FPL crosses the CMC joint palmar to the FE axis and just ulnar to the AA axis. It is a flexor and an adductor, but it has a small mechanical advantage at either axis. At the MCP joint, it lies palmar to the FE axis, and the AA axis passes through the tendon. The FPL has a good mechanical advantage for flexion of the MCP joint, but it does not have any effect on AA motions or torques since the axis passes though it. It is a flexor of the IP joint. In these cross sections, the ulnar-innervated muscles are stippled and the median and radial innervated muscles are shaded or black to illustrate the effect of ulnar palsy on the thumb mechanism. The deficit is the paralysis of the first dorsal interosseus, adductor pollicis, and flexor pollicis brevis. This leads to loss of flexor torques at the MCP and CMC joints, loss of adductor torques at the CMC and MCP joints, and weakness of IP extension. (From Brand PW, Hollister AM. Clinical Mechanics of the Hand, 2nd ed. Chicago: Mosby, 1982:85.) |
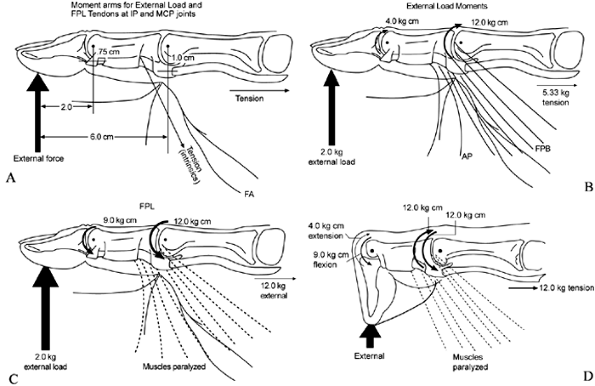
the CMC, MCP, and IP joints. The moment arms of the flexor pollicis
longus (FPL) at the IP and the MCP joints are 0.75 and 1.0,
respectively (Fig. 57.11). For equilibrium at
the IP joint, a 2 kg load on the thumb pulp may require 5.33 kg of
tension in the FPL tendon. At the MCP joint, the added moments of the
adductor pollicis (AP) and the flexor pollicis brevis (FPB) maintain
equilibrium. For equilibrium at the MCP joint, a 2 kg load on the thumb
pulp needs a 12.0 kg tension in the FPL tendon if other muscles are
paralyzed. The 12.0 kg tension that is needed to stabilize the MCP
joint is much too great at the IP joint. The latter goes into sharp
flexion. Once the IP joint goes into flexion, the moment arm of the
load is shortened and may even run through the axis. This is the
mechanics of Froment’s sign for ulnar palsy.
external load to push it to the limits of MCP extension. This is the
mechanics of Jeanne’s sign.
 |
|
Figure 57.11.
The mechanics of Froment’s sign. The ulnar-palsied thumb will collapse with IP joint hyperflexion (Froment’s sign) and MCP hyperextension when lateral pinch is attempted. The loss of flexor torque at the MCP joint is particularly pronounced since the short flexor and adductor have the largest tension fractions and mechanical advantages for flexion of the MCP joint. The balance of torques about each joint of the thumb is
dependent on the magnitude of the force and its distance from the axis of rotation (A). We can see that both the external load and the tendons act across multiple joints simultaneously. The moment arms for the FPL increase only slightly as one moves from the IP (0.75 cm) to the MCP joint (1.0 cm), but the moment arm for the external load applied at the tip increase from 2 cm at the IP joint to 6 cm at the MCP joint (B,C). The flexor moments needed to stabilize the MCP joints are three times greater than those needed to stabilize the IP joints. If the FPL is the only flexor for the two joints, there will be an excessive flexor torque at the IP joint and insufficient flexor torque at the MCP joint, resulting in hyperflexion of the IP joint and hyperextension of the MCP joint (D). The imbalance can be treated by fusion of the MCP joint,
by tendon transfers to increase the flexion torque at the MCP joint, or by a combination of these procedures. |
be analyzed by considering the mechanics of the thumb joints
individually and as a chain. Any muscle or tendon transfer acts on the
axes of rotation of the joints of the thumb (Fig. 57.11)
with the muscles crossing them, showing ulnar palsy. The CMC and the
MCP joints have two axes of rotation each, one for flexion–extension
(FE) movements and one for abduction–adduction (AA) movements (8).
perpendicular to the FE axis or the bones. As a result, the path of the
bones when they move is cone shaped, producing combined AA and
pronation and supination movements. The IP joint has only one axis. The
effects of a generic ulnar nerve palsy on the joints of the thumb can
be seen in Fig. 57.10. In this specific case, there is loss of flexion and adduction at the proximal thumb joints.
innervation of the short flexor and adductor muscles of the thumb.
Sometimes, the median nerve supplies enough of
the
short flexor muscles so that ulnar palsy does not leave much deficit.
In other cases, the FPL is the only thumb flexor that survives ulnar
palsy. More commonly, enough of the short flexor is paralyzed to
produce weakness in flexion of the proximal joints. In the latter two
instances, any attempt at firm pinch results in flexion of the IP joint
and extension of the MP joint. This functional test may be used to
determine the need for tendon transfer. If the patient can pinch
strongly without IP flexion, there is probably no need for a transfer.
-
If a transfer is needed, the best tendon to use is the FDS of the middle finger. Divide it in the middle of the
P.1666
proximal segment of the finger and withdraw it into the palm through an
incision parallel to, and just to the ulnar side of, the thenar crease,
just distal to the midpalm. The palmar fascia must be split (not cut),
leaving a significant strand to the radial side of the split. -
In the middle segment of the thumb,
through an incision on its dorsiradial aspect, expose the edge of the
dorsal expansion. Insert tendon-tunneling forceps halfway between the
MP and IP joints and direct them subcutaneously to the palmar incision.
The nose of the forceps must appear in the palmar incision superficial
to the palmar fascia. Thus, when the tendon is pulled into the thumb,
the radial strand of palmar fascia serves as a pulley, preventing the
tendon from losing its angle of approach to the thumb (Fig. 57.12).![]() Figure 57.12.
Figure 57.12.
The flexor digitorum superficialis tendon is divided through the finger
incision and withdrawn in the palmar incision. The tunneling forceps
picks it up there and takes it to the thumb. Note that in the palmar
incision (A), the tunneling forceps lies
superficial to the palmar fascia. The tendon comes from deep to the
fascia but turns around the fascia edge and uses that edge as a pulley.
(B) Insertion points of the transferred tendon.
joints both have two axes of rotation. The IP-2 joint has one axis or
hinge. None of the hinges are perpendicular to the bones or to one
another, so there are conjunct rotations with flexion–extension at all
of the joints and with abduction–adduction at the CMC and MCP joints.
The mechanical advantage of the muscles is determined by their distance
from, and angle of pull relative to, the axes of rotation. For
instance, the FPL is a flexor and adductor of the CMC joint, and a pure
flexor of the MCP and IP joints (3).
interosseus, the adductor, and a variable portion of the short flexor.
This results in a loss of power for CMC and MCP flexion and adduction.
and attached to the extensor pollicis longus (EPL) tendon while the IP
joint is fully extended. Alternatively, half the tendon transfer may be
attached to the EPL and the other half closer to the MP joint, to the
tendon of attachment of the abductor pollicis brevis. This double
insertion (or yoke) (Fig. 57.12B) serves as a check to prevent excessive MP flexion and abduction or adduction.
if the MCP joint is hypermobile, the double insertion should be used or
it may be better to fuse the MCP joint just short of extension and with
some medial rotation of the phalanx on the metacarpal. The transfer
will still act as a flexor and adductor of the CMC joint, allowing good
lateral and tip pinch.
flexors in which only the FPL is left for CMC and MCP flexion, the
transfer may not be able to add sufficient flexor force to the CMC
joint to prevent IP joint hyperflexion,
even when the MCP joint has been fused. In these cases, tenodesis of the IP joint with suture of the FPL to the A1 pulley will give a stable IP joint in a useful position as well as preserving the FPL as a CMC flexor and adductor.
-
Immobilize the hand with the IP joint
extended, the MP joint slightly flexed, and the thumb in a pinching
position. The middle (or donor) finger should be splinted in IP
extension to discourage proximal attachment of the stump of the
superficialis tendon.
FDS of the middle finger. We always regret having to deprive any finger
of its superficialis tendon, for reasons already discussed. Dr. Selcuc
Sozen (11a) has demonstrated a way to avoid the
development of a swan-neck deformity in a finger after removal of its
superficialis tendon.
-
Divide the tendon only halfway through, just proximal to the PIP joint, and then split it back to the level of the A1
pulley, at which level the other half of the tendon is divided. Now
attach the half-thickness tendon that remains in the finger to the A1
pulley at a tension just enough to hold the PIP joint short of full
extension. This tenodesis prevents any hyperextension of the PIP joint
and thus of any gross deformity (3). -
Now withdraw the main tendon proximally
through a longitudinal incision parallel to and just to the ulnar side
of the thenar crease, just distal to the midpalm. Split the palmar
fascia (do not cut it), leaving a good strand of palmar fascia radial
to the split. -
Using an incision on the dorsiradial
aspect of the middle segment of the thumb, expose the edge of the
dorsal expansion. Insert the tendon-tunneling forceps halfway between
the MP and IP joints and direct them subcutaneously to the palmar
incision. The nose of the forceps must appear in the palmar incision superficial
to the palmar fascia. Thus, when the tendon is pulled into the thumb,
the radial strand of palmar fascia serves as a pulley, preventing the
tendon from losing its angle of approach to the thumb (Fig. 57.10).
while the IP joint is fully extended. Alternatively, half the tendon
transfer may be attached to the EPL and the other half closer to the MP
joint, to the tendon of attachment of the abductor pollicis brevis.
This double insertion (or yoke) serves as a check to prevent excessive
MP flexion.
-
Immobilize the hand with the IP joint
extended, the MP joint flexed, and the thumb in a pinching position.
Splint the middle (or donor) finger just short of IP extension.
these operations, exercise only one of the two joints in each digit.
Apply cylindrical plaster casts to the IP joints (finger and thumb) in
the corrected position, while encouraging the MP joints to move. After
a few days, free up the IP joints, and prevent the MP joints from
extending with a knuckle-bender splint.
and IP joints be released at the same time. Even then, if there is a
tendency to MP hyperextension or clawing, reimpose the alternating
restrictions. In the thumb, the MP joint is difficult to immobilize,
and IP extension may be continued longer if needed.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
A, Buford W, Giurintano DG, Myers L. The Axes of Rotation of the Thumb
Interphalangeal and Metacarpophalangeal Joints. Clin Orthop 1995;320:188.
S. Opponens plasty. Videotape presented at the annual meeting of the
American Society for Surgery of the Hand, September 1987.