NONUNIONS AND MALUNIONS OF THE UPPER EXTREMITY
II – FRACTURES, DISLOCATIONS, NONUNIONS, AND MALUNIONS > Malunions
and Nonunions > CHAPTER 27 – NONUNIONS AND MALUNIONS OF THE UPPER
EXTREMITY
second edition was written by Deborah F. Bell and James F. Kellam.
Portions of their chapter were used in this revision. Their
contribution is greatly appreciated.
weight unless crutches or a cane are used routinely, osteoarthritis
resulting from malalignment does not appear to be a major problem.
However, malalignment compromising precise mobility of the hand or the
ability to place the hand in space may be a major disability. The
decision to correct malunions or nonunions in the upper extremity
depends on the patient’s functional demands and the presence of pain.
If function is suitable without correction
and pain is not a problem, surgery is not indicated.
of heavy muscles and lies on the posterior aspect of the thoracic cage,
fractures that progress to symptomatic nonunion or malunion are
exceedingly rare. Personally, I have never had to treat surgically
either a nonunion or a malunion of the scapula. There are reports of
nonunions of the base of the coracoid process, the scapular body and
spine, and the acromion (2,21,33,52,55,105). Gupta et al. (33)
reported successful treatment of a nonunion of the inferior third of
the body of the scapula (the only case reported in the literature) with
plate fixation and bone graft, resulting in dramatic improvement in
function and relief of pain.
unite and occasionally does not unite, remaining as an os acromiale.
This should not be mistaken for a nonunion. True nonunions, if
displaced inferiorly, can interfere with motion and cause impingement
on the rotator cuff tendons. If symptoms justify, a small fragment can
be excised. Reattachment of the deltoid must be solid and protected
until healed to avoid deltoid deficiency. Excision of any substantial
part of the acromion can lead to permanent deltoid weakness, and
therefore, nonunions producing large fragments deserve repair. Repair
can be challenging because of the thin cortical bone of the acromion,
in which it is difficult to obtain secure fixation. Dounchis et al. (21)
reported successful treatment of a nonunion of a fracture at the base
of the acromion with plate and screw fixation combined with a tension
band wire construct and autologous bone graft.
secondary to an osteotomy performed for reconstructive shoulder surgery
as opposed to a fracture. If the nonunion is symptomatic, most can be
successfully treated with freshening of the fracture site and internal
fixation with a compression screw. Excision is also possible with
reattachment of the muscles originating from the coracoid to
surrounding soft-tissue structures.
Patients with atrophic nonunions seemed to have fewer symptoms than
those with hypertrophic pseudarthroses. Atrophic nonunions seem to be
much more common than hypertrophic nonunions (39).
ununited fracture at least 16 weeks after injury. The anatomic location
of the fracture affects the union rates; distal clavicular fractures
have a higher rate of nonunion than middle-third fractures. A
displaced, interligamentous distal-third fracture (Neer type II), in
which the proximal fragment is detached from the coracoclavicular
ligament, is unstable and has a higher nonunion rate (68,69,72).
clinically significant problem. Most clavicles heal in a malunited
position, because they are usually treated in a figure-eight sling,
which does not provide adequate enough immobilization to ensure
anatomic position (see Chapter 15). It is very uncommon to require any form of treatment for a malunion of the clavicle, except for a cosmetic deformity (69).
Occasionally, brachial plexus impingement can occur when there is
abundant callus. Shortening of more than 15 mm can produce shoulder
discomfort.
or malunion of the clavicle include significant pain with use of the
ipsilateral shoulder, compromising upper extremity function.
Occasionally, hypertrophic nonunions cause extrinsic compression of the
brachial plexus and the subclavian artery and vein (45). This problem may also be responsible for a thoracic outlet syndrome (16).
Thorough preoperative assessment, including a bone scan, appropriate
angiography, electromyographic studies, and a thoracic or vascular
surgical evaluation, may be indicated. The final indication for
surgical correction of clavicular nonunion or malunion is correction of
unsightly deformities. The patient must be aware that he or she is
exchanging a deformity for a scar. Comparison of radiographs to the
opposite, normal side are useful for planning a repair or osteotomy,
particularly to estimate restoration of length. Operative techniques
most commonly used today include plate fixation and bone graft (6,8,18,51,75,77,92,107), intramedullary Hagie pin and bone graft (4,12,107), and as a last resort, partial or total claviculectomy (59).
-
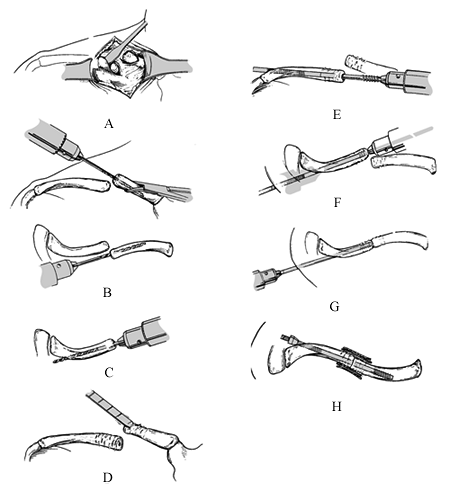
Position the patient in a modified beach-chair position on the operating table (Fig. 27.1).
Because it is difficult to position an x-ray plate beneath the shoulder
once the patient is positioned and draped, place a cassette in position
before the prep and drape. Pad it to protect the patient.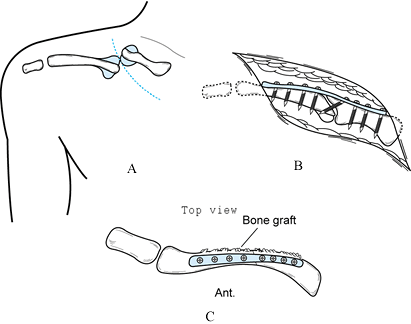 Figure 27.1. Repair of nonunion of the clavicle by plate fixation and bone graft. A: Surgical approach in Langer’s lines. B: Compression plate fixation with an interfragmentary compression screw. C: Top view—note placement of bone graft superiorly and posteriorly.
Figure 27.1. Repair of nonunion of the clavicle by plate fixation and bone graft. A: Surgical approach in Langer’s lines. B: Compression plate fixation with an interfragmentary compression screw. C: Top view—note placement of bone graft superiorly and posteriorly. -
Prepare and drape the patient, with the
involved shoulder and extremity free. Be certain to prep all the way up
to the corner of the mandible and drape widely to ensure adequate
access to the clavicle. -
Make an incision of sufficient length,
usually 10 to 12.5 cm, using Langer lines to minimize scarring. Carry
the incision directly down to the clavicle and expose the superior
surface by subperiosteal dissection. There usually is no need to
develop subcutaneous flaps. In malunions and in hypertrophic nonunions,
the main shaft of the clavicle can be buried and quite difficult to
identify. Palpate the bone carefully as the incision down to bone is
made. Simpson and Jupiter (92) mention
identifying and preserving the cutaneous supraclavicular nerves
crossing the anterior border of the clavicle in order to avoid
dysesthesia postoperatively. I have not found it practical to preserve
these nerves in the midportions of the wound. At the distal and
proximal ends, they can be retracted. In spite of having transected
these nerves in the midportion of the wound routinely, I have never had
a patient complain of postoperative dysesthesia due to neuromas. -
Identify the nonunion. In the case of an
oligotrophic or atrophic nonunion, try to identify the original
fracture ends so that the fracture can be repaired as anatomically as
possible. In most cases, it is worthwhile to plate the clavicle in
anatomic position rather then fix it in malposition, because patients
are much happier and function is better. In most cases, this requires
taking down the nonunion, freshening the bone ends, and drilling the
medullary canal to help revascularization. -
If there is a reasonably stable fibrous union in nearly anatomic position, then occasionally plate fixation in situ is adequate. In my experience, this is rare.
-
In hypertrophic nonunions, it is
worthwhile to shave the hypertrophic callus off the clavicle, taking
care to identify the original clavicle encased in the callus (Fig. 27.1A). Morcelize this bone and use it for bone graft, because this saves harvesting an iliac crest graft. -
A gap may be present owing to bone
resorption, extensive comminution, or bone loss in the case of open
fractures. Plan to restore the full length of the clavicle, placing an
intercalary tricortical bone graft of equal size to the clavicle.
Harvest it from the superior rim of the anterior iliac crest (see Chapter 9). -
Once the nonunion has been reduced, apply
a 3.5 AO limited contact compression plate, Alta 3.7 reconstruction
plate, or equivalent to the superior surface of the
P.890
clavicle,
obtaining eight cortices of solid fixation both proximally and
distally, if possible. Whenever possible, try to obtain
interfragmentary compression across the nonunion site either
independently of the plate or through the plate (Fig. 27.1B). Plates fit best on the superior clavicle and act as a tension band, requiring less molding than plates placed anteriorly (Fig. 27.1C).
Superior plates also have the advantage of protection of the underlying
structures on the inferior aspect of the clavicle by the subclavius
muscle.
-
To ensure proper length of the clavicle, measure the length of the opposite clavicle preoperatively and use this as a guide.
-
Sometimes gaining length can be
difficult. Facilitate this procedure by fixing the plate to one end of
the nonunion first and then using a distractor or other instrument to
distract. Application of a small external fixator with a pin medial and
lateral to the plate to be used as a distractor also works nicely. -
Meticulous closure of the periosteum and
deep fascia with the platysma provides a smooth contour over the
clavicle and may eliminate the need for plate removal later. -
Nonunions in the proximal quarter and in
the distal quarter of the clavicle are difficult to fix because of the
small fragments available. For these nonunions, the Alta 3.7
reconstruction plate is quite useful because of its oval holes, which
give more screws per unit length than in other plates. Augmenting
fixation with a tension band figure-eight wire is useful as well.
-
Petal the superior and posterior surfaces
of the clavicle adjacent to the plate on both sides of the nonunion,
and then apply a cancellous bone graft. -
Do a meticulous layered closure of the
periosteum, deep fascia, and platysma. Use a plastic skin closure to
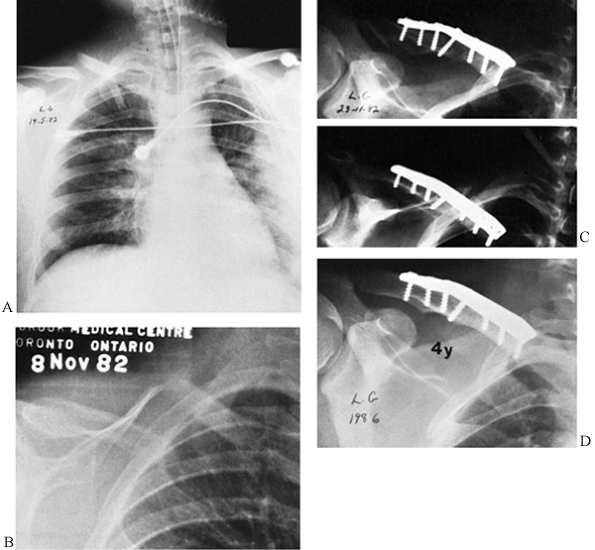
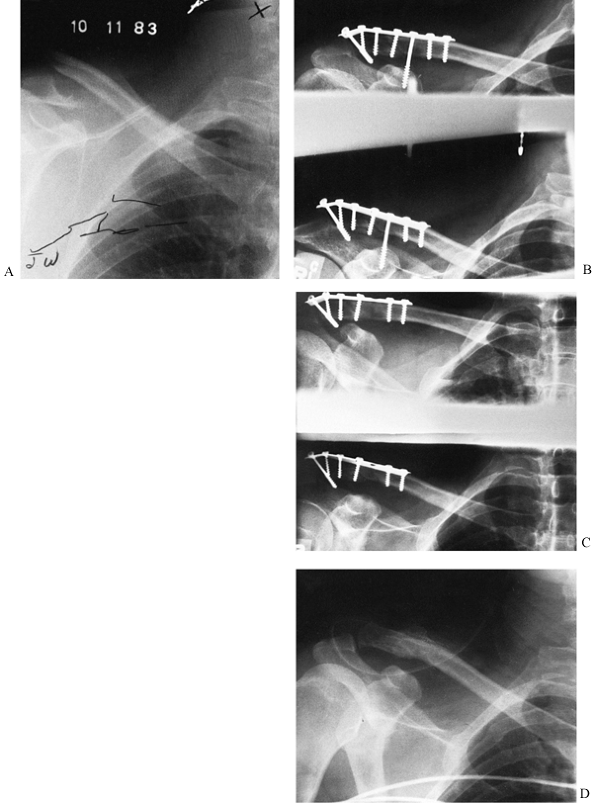
provide the best scar. See Figure 27.2 for a typical case.![]() Figure 27.2. Nonunion of the clavicle. A: A midshaft oblique fracture of the right clavicle at the time of injury. B: Six months after nonoperative treatment, this fracture is still grossly displaced and mobile with no evidence of union. C:
Figure 27.2. Nonunion of the clavicle. A: A midshaft oblique fracture of the right clavicle at the time of injury. B: Six months after nonoperative treatment, this fracture is still grossly displaced and mobile with no evidence of union. C:
Open reduction and internal fixation using a 3.5 mm dynamic compression
plate. Notice the oblique lag screw across the nonunion site. A bone
graft was also added. D: At 4 years,
consolidation has occurred. The patient is asymptomatic and has not
requested that the internal fixation be removed.
-
The technique is nearly identical to that
described earlier for repair of nonunion. The only difference is that
the old fracture site must be identified and an osteotomy
P.891
made
as much as possible through the old fracture site. I find that this
usually works better than an arbitrary osteotomy, because an arbitrary
osteotomy frequently results in a compensating deformity. -
Even a year or more after a malunion of a
clavicle, the callus surrounding the original bone is more vascular,
pink in appearance, and softer than the hard white native cortical bone
of the clavicle. -
Slide an osteotome along the normal cortex of the clavicle, shaving off the callus until the malunion site is obvious.
-
Use a small water-cooled oscillating saw
to osteotomize through the old fracture site. Refashion the bone ends
to make the clavicle as anatomic as possible, and then plate the
clavicle as described earlier. Bone graft is not usually necessary, but
any callus removed at the fracture site can be morcelized and packed
about the osteotomy site.
 |
|
Figure 27.3. Hagie pin fixation and bone graft of a nonunion of the clavicle. A: A skin incision exposing the nonunion. B: Drilling the medullary canal of the medial fragment. C: Drilling the medullary canal of the lateral fragment. D: Petaling the ends of the clavicle. E: Drilling the Hagie pin out the hole in the lateral fragment. F: Superior view of E. G: Reducing the fracture and driving the Hagie pin retrograde into the medial fragment. H: Superior view. A nut is applied to the Hagie pin to compress the fracture. (Redrawn from Matsen FA, III, and Rockwood CA, Jr. The Shoulder. Philadelphia: W. B. Saunders, 283, with permission.)
|
-
Proceed as described earlier for plate
fixation to the point where the nonunion is ready for internal
fixation. Somewhat more exposure is needed because of the need to have
access to both bone ends at the nonunion site for the intramedullary
pin (Fig. 27.3A). Because a plate will not be
placed, exposure of the entire superior surface is not necessary.
Elevate the periosteum 2.5 cm off of each segment next to the fracture,
trying to maintain the deep soft-tissue attachments to the clavicle. -
Drill the medullary canal of the proximal
(medial) fragment with an appropriately sized drill point for the Hagie
pin to be used (Fig. 27.3B). Be careful not to penetrate the clavicle anteriorly accidentally. -
Drill the medullary canal of the distal
(lateral) fragment, exiting the clavicle medial and posterior to the
acromioclavicular joint. Drill until the bit can be palpated on the
posterolateral aspect of the shoulder where a stab wound is made (Fig. 27.3C). -
Freshen (petal) the ends of the clavicle at the nonunion site (Fig. 27.3D).
-
Select a Hagie pin of the appropriate
length and diameter so that the course threads on the tip of the pin
will lie entirely within the medial fragment. Drill the Hagie
P.892
pin
retrograde with its fine-threaded ends laterally out from the nonunion
site down the medullary canal of the lateral fragment, to bring the tip
to the fracture site (Fig. 27.3E, Fig. 27.3F).
-
Avoid smooth or threaded wire fixation across nonunions because of the risk of wire breakage and wire migration (see Chapter 78) (73,83,106).
-
For distal clavicle nonunions, fixation
in a short distal fragment can be enhanced by the use of a 3.5 mm or
similar T plate, or a 3.5 mm plate with one of the screws in the plate
placed into the base of the coracoid process (see Chapter 78).
With this technique, take care to not excessively narrow the
coracoclavicular interval. Avoid elevation of the arm above 90° until
the coracoclavicular screw is removed after healing of the nonunion. -
Figure-eight tension band wires (without K-wires) are useful for augmenting plate or Hagie pin fixation (Fig. 27.4).
 |
|
Figure 27.4. Nonunion of a distal clavicle fracture. A:
A 25-year-old skier suffered a displaced fracture of the distal third of his clavicle. Nonoperative treatment was unsuccessful. He had pain and an unsightly deformity at 6 months. The atrophic nonunion was completely mobile. B: Internal fixation was performed using a third-tubular plate. There is an interfragmentary screw across the fracture site and a coracoclavicular screw. The most distal screw runs obliquely through the longest portion of the acromion. A cancellous bone graft was applied. C: At 8 weeks, the coracoclavicular screw was removed. Before this, the patient had been allowed pendulum exercises with abduction of his shoulder to only 90°. After screw removal, full range of motion was instituted. D: A radiograph 1.5 years after operative intervention shows that the plate has been removed, and there is solid union of the nonunion. |
-
Reduce the fracture, then drill the Hagie
pin into the medial fragment. When the pin is in place, the fracture
site should be in excellent apposition and compression. If there is a
gap, apply the nut to the lateral end of the pin and compress the
fracture (Fig. 27.3G, Fig. 27.3H). -
Finish petaling the bone ends at the
nonunion site for a distance of 2.5 cm on either side of the nonunion.
Bone graft the fracture on all exposed surfaces except the anterior
subcutaneous border. Boehme et al. (4) use osteal/periosteal rib
grafts, as described by Dineen and Greshman (19); however, cancellous graft from the iliac crest works well also. -
Closure is as described previously.
postoperative care for all three of the above-mentioned procedures is
similar. Protect the shoulder in a sling until the patient is
comfortable. Begin passive circumduction exercises (Codmen’s),
progressing as quickly as the patient can tolerate. Patients can use
the extremity for light activities of daily living but should avoid any
strenuous use of the extremity, lifting of other than very light
objects, and overhead activities until 6 weeks after the surgery.
Between 6 and 12 weeks, depending on the state of union, progress with
gentle overhead pulley exercises but avoid raising the arm against
gravity or any strenuous use until the nonunion is solidly healed,
which generally takes 10 to 12 weeks.
has no pain. The major concern is the bump from the malunion. In these
cases, simple removal of the bump with an osteotome and smoothing of
the clavicle suffices.
the techniques described above are excellent, with success rates of 92%
to 100% after the first operation (4,5,6,8,12,16,18,23,25,39,41,45,51,66,75,77,83,91,92,103,106,107).
Patients usually complain of weakness and early fatigue when working
with the extremity above the head. Some have chronic pain.
Claviculectomy is usually indicated for some infected nonunions, major
bone loss, or a painful nonunion that is unresponsive to surgical
treatment. Sometimes, claviculectomy is necessary to relieve thoracic
outlet syndrome. Claviculectomy may be combined with simultaneous
resection of the first rib, which is usually done through an
independent axillary exposure. To avoid an unsightly, painful, unstable
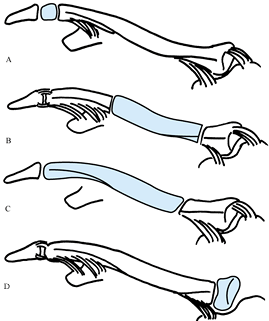
clavicle, resect it only as indicated in Figure 27.5.
 |
|
Figure 27.5.
Partial claviculectomy. Note that the remaining segment is always stabilized by ligaments. Shaded areas indicate resected parts of bone. A: Distal claviculectomy, usually done for acromioclavicular arthritis. This can be part of a Weaver-Dunn procedure (102). B: Resection of the medial intercalary two thirds. The lateral and medial segments are stabilized by their ligamentous attachments. C: Resection of the lateral two thirds, leaving a stable medial fragment. D: Resection of the medial end for arthritis or instability of the sternoclavicular joint. Instability of the remaining clavicle at its medial end may require stabilization to the first rib (see Chapter 78) |
-
Expose the clavicle, as described earlier
for repair of a nonunion. Expose only that portion of the clavicle
planned for resection. -
When resecting the mid two thirds of the
clavicle or the distal two thirds, you can facilitate resection by
entering the nonunion site or making an osteotomy just lateral to the
ligaments, stabilizing the medial end of the clavicle. Expose it with
careful circumferential subperiosteal exposure. -
Grasp this free end of the clavicle with
a bone-holding forceps and then excise the clavicle in a subperiosteal
manner from its bed to the distal resection site. -
Resection of the medial end of the clavicle as illustrated in Figure 27.5D requires special consideration because of the underlying major neurovascular structures. (See Chapter 78 for a description of this exposure and resection.)
-
When resecting the clavicle distal to the
attachments of the coracoclavicular ligaments, it is essential that
these ligaments be intact or reconstructed (see Chapter 78) (102).
-
Resection of a deformed clavicle
surrounded by dense scar can be challenging on occasion because of the
closeness of the underlying neurovascular structures. The best
technique is subperiosteal resection, keeping sharp instruments
directly against the clavicle and avoiding penetration into the
underlying soft tissues. The presence of the subclavius muscle and the
clavipectoral fascia usually provides adequate protection for these
vital structures. -
The major disadvantage of subperiosteal
resection is that occasionally the clavicle partially reforms from the
periosteum. This is particularly true in young adults. If reformation
of a clavicular remnant is a problem, then an extra periosteal
resection is indicated. This requires additional caution. -
Careful repair of the periosteum, deep
fascia, and platysma usually results in the formation of a fibrous
scar, which simulates the excised clavicle and gives a reasonable
cosmetic result. -
Warn all patients that they will
experience less strength and endurance in using the shoulder,
particularly for overhead or pushing activities.
Failure of this fracture to unite within 6 to 8 weeks constitutes a
delayed union. At 12 weeks, an unstable fracture with no evidence of
callus formation is unlikely to heal. Therefore, operative treatment is
usually indicated. Nonunion of the surgical neck of the humerus is rare
(93). Displaced fractures that remain unreduced
owing to muscle forces, interposed deltoid or biceps, or treatment
producing distraction may result in nonunion. In Neer’s series (70,71),
nonunions were more commonly associated with hanging casts or skeletal
traction and displaced four-part fractures. The incidence of proximal
humerus fractures in women is twice that in men. Osteoporosis and a
short proximal fragment covered for the most part by articular
cartilage makes treatment difficult (Fig. 27.6) (35).
Therapeutic alternatives include symptomatic treatment only, open
reduction, and internal fixation combined with a bone graft or
prosthetic replacement. Because of the challenge of obtaining fixation
in the proximal articular fragment, many different approaches have been
used, including simple plate and screw fixation, double plate fixation,
multiple stiff and malleable wires, Rush rods or Ender pins combined
with malleable wires in a figure eight, and various types of blade
plates or specially designed reconstruction plates for the proximal
humerus (30,34,40,48,100).
In elderly and in middle-aged adults with severe avascular necrosis of
the humeral head, a reasonable alternative is prosthetic replacement of
the proximal humerus. Because the nonunion is typically through the
surgical neck, restoration of the insertion of the rotator cuff is
important. If there is coexisting osteoarthritis of the shoulder joint,
consider total shoulder replacement. In young patients who require a
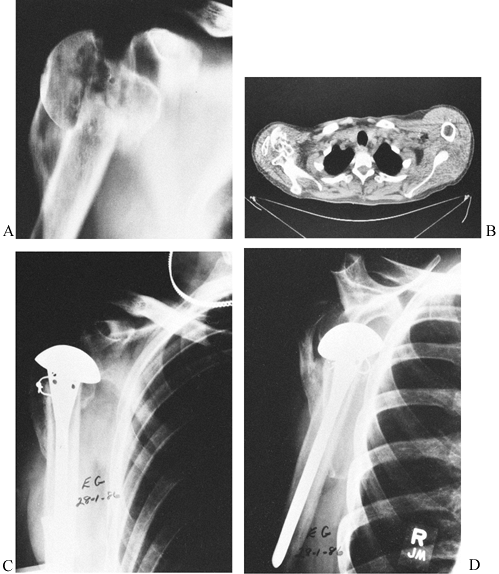
stable pain-free shoulder for heavy labor, consider arthrodesis (see Chapter 103) (Fig. 27.7).
 |
|
Figure 27.6.
Bilateral painless pseudarthrosis of the proximal humerus in a 72-year-old woman. This patient had adequate motion in her shoulders for her activities of daily living. |
 |
|
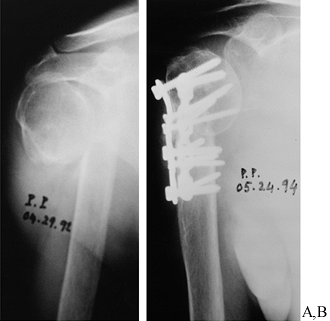
Figure 27.7. Hemiarthroplasty for a malunited fracture of the proximal humerus. A:
Malunion of a displaced four-part proximal humeral fracture. The glenoid is empty, and the humeral head fragment is rotated 180° laterally. This patient had significant pain and limited shoulder function. B: A CT scan of the shoulder shows the malunited humeral head in its rotated position. The greater tuberosity can be seen laterally to the head and appears to be not united in this picture. Notice the sclerotic humeral head, indicating avascular necrosis. C, D: A Neer hemiarthroplasty was inserted for the primary relief of pain. At the time of surgery, the humeral head was osteotomized and excised, and 90° of forward motion was obtainable in the operating room under anesthesia. The patient has done relatively well after surgery; he has mild residual pain with adequate function. |
nonunion are usually accompanied by major ruptures in the rotator cuff.
The most likely avulsion fracture to progress to nonunion is one
involving the posterolateral aspect of the greater tuberosity,
involving the insertions of the infraspinatus and teres minor. On an
anteroposterior (AP) view, these tend to be visualized posterior to the
humeral head and, therefore, are easily missed. The major focus in
repair of these is reconstruction of the rotator cuff, which is
described in Chapter 79. Fixation of the
tuberosity is usually best accomplished by placing it back into its bed
and securing it with multiple figure-eight or horizontal nonabsorbable
sutures interwoven through the insertion of the rotator cuff and the
proximal fragment, and tied through drill holes in the proximal shaft
of the humerus. Screws and other metallic fasteners usually fail
because the avulsed fragment is a thin cortical shell and is usually
full of multiple cracks.
individuals, who, if sedentary, may function reasonably well with a
painless pseudarthrosis or a malunion that does not interfere
significantly with their activities of daily living. Consequently,
premorbid patient activity, age, occupation, and hand dominance play
important roles in the decision whether to surgically repair a proximal
humerus nonunion (Fig. 27.6).
correction are rare, because most patients get along well as long as
the opposite shoulder is normal. Osteotomy to correct a malunion is
most commonly indicated in active patients who are still working and
require full use of their upper extremities for their occupational or
sports activities. The most frequent malunion requiring correction is a
surgical neck or a somewhat more distal fracture that has healed with
apex anterior or lateral angulation, which limits forward flexion and
abduction. Occasionally, this can be painful. Osteotomy has been used
to treat recurrent anterior dislocation of the shoulder as well (104).
osteotomy to correct a malunion requires careful preoperative planning
because of the challenge of obtaining adequate fixation in the proximal
fragment. Rigid fixation is important to allow patients to begin fairly
vigorous circumduction exercises immediately; otherwise, unacceptable
shoulder stiffness may result. It is usually advisable to have a backup
plan with the necessary implants and instrumentation available. In
suitable patients, the backup to reconstruction of the fracture may be
prosthetic replacement. Be certain to discuss this alternative with
your patient, and have the prosthesis and instrumentation available in
the event that repair of the nonunion is not technically feasible.
nonunions of the proximal humerus through the use of small fragment
double plate fixation combined with iliac crest bone graft through a
modified deltopectoral approach, which is described below.
-
Expose the proximal humerus through a Henry’s deltopectoral approach (see Chapter 1).
Do not take down any of the origin of the deltoid or pectoralis major
muscles. If more extensive exposure is required, take down the
insertion of the deltoid in a subperiosteal manner, using a sharp knife
or electrocautery knife. Take this down in continuity with the
brachialis muscle. Identify and coagulate the large bleeders in this
area. This provides ample exposure but does not require direct
reattachment of the deltoid insertion to the humerus, because simple
closure of this musculofascial sleeve restores the continuity of the
deltoid. -
Occasionally, exposure of the joint is
necessary, in which case a partial take down of the origin of the short
head of the biceps and coracobrachialis from the tip of the coracoid
are useful. This step provides excellent
P.896P.897
exposure, making the spiral compression plate described by Gill and Torchia (30) unnecessary. -
Expose the nonunion site laterally and
anteriorly. Try to maintain soft-tissue attachments on the posterior
and medial borders. These nonunions are nearly always pseudoarthroses
or atrophic nonunions. -
Remove soft tissues from the fracture
site and freshen the fracture ends, fashioning them to fit together in
a manner that restores anatomic alignment and maximizes the contact of
the bone surfaces. Open the medullary canal of the distal fragment and
use a 2 mm drill point to drill the sclerotic surface of the nonunion
in multiple places on the proximal fragment. -
Reduce the nonunion and secure the
position with a bone-holding forceps. Often, these nonunions are
oblique, and initial fixation can be done with an interfragmentary
compression screw. -
Fashion two Alta small fragment
reconstruction plates (or another, similar plate) to fit along the
lateral and anterior borders of the fracture, extending up to the
articular surface. The bevelled ends of the plates permit fixation
close to the articular surface without impingement on the acromion or
rotator cuff. Locate these plates as close to 90° to each other as
possible. Secure the plates to the humerus with 3.7 cortical screws,
which are bicortical where there is not articular cartilage. In the
proximal fragment, it is often possible to obtain bicortical fixation
on the proximal fragment through the anterior plate, whereas with the
lateral plate, the direction of the screws is toward the articular
surface; therefore, the screws must be placed short of the subchondral
bone. Cortical screws inserted without tapping tend to get a better
hold than cancellous screws. If they strip out, replace them with the
larger cancellous screws. To improve fixation in osteoporotic bone, try
cross-threading the screws against each other in the proximal fragment
or, as a last resort, inject methacrylate into each screw hole
individually. -
Gently petal the nonunion site up to the
articular surface on the proximal fragment for at least 2.5 cm on the
distal fragment, and apply finely morcelized cancellous bone in a solid
layer along all available bone surfaces. The small, narrow profile of
the Alta plates usually leaves ample room for application of a bone
graft. If space is insufficient, further medial exposure makes a good
location for bone graft (Fig. 27.8) .![]() Figure 27.8. Nonunion in the surgical neck of the humerus. A:
Figure 27.8. Nonunion in the surgical neck of the humerus. A:
An AP radiograph of the right shoulder of an 82-year-old man with a
nonunion of the surgical neck of the humerus of 18 months’ duration
after treatment in a sling. B: An atrophic
nonunion with an interposed biceps tendon was found at surgery and
repaired with two Alta 3.7 plates. The screws were cross-threaded to
improve fixation. An autologous iliac graft was applied. This was
healed by 12 weeks, as seen here. -
Close the deltopectoral interval and the
brachialis-deltoid interval, if necessary, in a single layer with
interrupted resorbable sutures. Perform a plastic closure of the
subcutaneous fat and skin. -
Immobilize the shoulder in a shoulder immobilizer.
-
Alternative methods of internal fixation include blade plates fashioned out of third-tubular or semitubular plates (22).
Although these plates are useful and low profile, I have found them to
be weak. The construct can be reinforced by placing an oblique screw
from the portion of the plate along the shaft up through the tip of the
plate (see Chapter 26), but this is technically tricky. Specialized blade plates and reconstruction plates are now available as well (21,45,51). -
I no longer use large fragment T or L
plates because they are difficult to bend and conform to the proximal
humerus, and they can cause acromial impingement. Their broad surface
area inhibits revascularization of the nonunion site.
gentle pendulum circumduction exercises within a few days. Allow
patients to remove the shoulder immobilizer to shower once the wound is
sealed. Otherwise, have patients wear the shoulder immobilizer both
night and day for the first 6 weeks to protect the repair. If at 6
weeks union seems to be progressing, then a more vigorous circumduction
exercise program to maximize shoulder range of motion can begin. Avoid
resistive exercises and active elevation of the arm until solid union
has occurred, which usually requires 12 weeks. Thereafter, patients can
engage in a full range-of-motion and strengthening program.
Most
patients with nonunions have very stiff shoulders, but I have found
that they reacquire good (although rarely normal) functional range of
motion and strength after about a year of vigorous rehabilitation.
essentially the same techniques except that a closing wedge osteotomy
is made through the nonunion site to correct the deformity.
Nonunion has been associated with inadequate immobilization,
distraction of the fracture, soft-tissue interposition (particularly at
the deltoid tubercle), and use of inappropriate nonrigid internal
fixation (24,29). A
fracture that is mobile and shows no evidence of callus at 12 weeks is
unlikely to heal, particularly if a gap can be seen on radiographs (13,43).
Hypertrophic delayed unions may be worth treating nonoperatively until
6 months, but I tend to intervene soon after 12 weeks to prevent
long-term permanent joint stiffness from prolonged immobilization. As
with nonunions in the proximal humerus, nonunions in the diaphysis are
frequently challenging. Esterhai et al. (26)
found that, in 46 nonunions, 62% were in elderly patients who were
senile and had disuse osteoporosis. Forty-two percent were synovial
pseudoarthroses; 20% were obese; and 5% had osteomyelitis. Of the
patients they elected to treat with electrical stimulation, only 46%
healed despite the fact that their group is the most expert in the
world in electrical stimulation. For that reason, I do not believe that
electrical stimulation is worth using in nonunions of the humerus
unless it is a hypertrophic nonunion, proven by computed tomographic
(CT) scan and bone scan not to be a synovial pseudoarthrosis. It must
be well immobilized. Internal fixation is best for most patients, but
consider electrical stimulation for patients in whom surgery is
contraindicated or risky.
or cosmetic problem. The soft-tissue coverage of the arm can obscure up
to 20° of anterior or posterior angulation and up to 30° of varus.
Shortening of as much as 2.5 cm does not lead to disability, and
rotational malalignment can easily be compensated through the shoulder (24).
-
An unstable delayed union of the humerus
at approximately 8 weeks after injury, with an obvious gap on
radiographs owing to bone loss or soft-tissue interposition, which
precludes healing. -
An established nonunion of the humerus at
12 weeks that is unstable and painful or, if free of pain, is so mobile
that effective functional use of the extremity is not possible. -
A severe malunion of the humerus, usually
in younger, active patients, that is absolutely cosmetically
unacceptable to the patient (usually severe varus with loss of carrying
angle) or causes a functional deficit sufficient to interfere with
normal activities of daily living, vocational activities, or sports.
function in order to establish appropriate goals for the surgery. The
shoulder and elbow may be quite stiff, and the patient may be using the
nonunion as a false joint, particularly if it is a more distal nonunion
close to the elbow. Stabilization of the nonunion may result in
significant loss of motion, which the patient may find more disabling
than the nonunion. Concomitant soft-tissue procedures and capsular
release to increase elbow and, on occasion, shoulder motion may be
essential to achieve a satisfactory result. The prolonged
immobilization and disuse associated with nonunions of the humerus
frequently lead to osteoporosis, which diminishes the holding power of
screws. Pre-existing hardware with large radiolucent areas around the
fixation device can also destroy bone stock. A thorough preoperative
plan with alternatives is important so that the procedure will be
successful. Operative techniques include the following:
-
When a preexisting intramedullary nail is
in place and alignment is acceptable, closed reamed locked exchange
nailing is a good technique, but the bone stock must be adequate to
provide good fixation for the cross-locking screws. Union is usually
slower and less dependable then plate fixation with bone grafting (57). -
Initial primary intramedullary nailing
with or without bone grafting almost always requires an open reduction,
particularly because the radial nerve is at risk of injury with closed
techniques. Nonlocked nails and the Seidel nail do not give a high
enough success rate to justify their use for nonunions (15,17,78).
Intramedullary techniques do not provide as good fixation as plates and
necessitate opening the humerus proximally, which can lead to rotator
cuff dysfunction and chronic shoulder pain. The loss of the
intramedullary blood supply may slow union. For that reason, I believe
the only role for intramedullary nailing for treatment of nonunions of
the humerus is exchange nailing for a preexisting nail. -
Plate fixation with bone graft is the
most commonly used and most effective method for treating nonunions of
the diaphysis of the humerus. It includes variations such as standard
AO-type compression plating, adjunctive interfragmentary screw
fixation, wave plates, and intramedullary plates (13,66,79,81). -
A fibula split and then fixed on both
sides of the nonunion as “plates” has been successful but, with modern
internal fixation, is not indicated today. When bone stock is a major
problem, however, use of a split fibula to provide a backup to the
plate on the opposite cortex for screw fixation is quite useful and a
good alternative to allograft (28). -
Difficult atrophic nonunions with loss of
bone continuity or nonunions with major bone loss can be treated with
plate fixation and a vascularized fibular graft through a medial
approach (38). -
When osteopenia precludes good screw
fixation, another alternative is the use of adjunctive bone cement,
which must be combined with a copious bone graft, with recognition of
the impact on the blood supply to bone (98). -
External fixation is useful when
osteomyelitis contraindicates the placement of implants at the fracture
site but has the disadvantage of frequent loosening of pins due to
poor-quality bone, pin track infection owing to the mobile soft tissues
in the upper extremity, and interference with shoulder and elbow
rehabilitation owing to tie down of muscles by the external fixation
pins (47).
-
Use Henry’s extensile anterolateral approach to the humerus (see Chapter 1).
The exploration of the radial nerve can be the most challenging part of
this procedure, and bone quality may require a long plate; therefore,
it is essential that the surgical approach be extensile to both ends of
the humerus. Use a posterior approach only for supracondylar nonunions
when exposure beyond the midshaft humerus is not necessary. -
The position of the radial nerve can be
nonanatomic, and it commonly is involved in the soft-tissue scar or
fracture callus. Identify the nerve in the interval between the
brachialis and brachioradialis muscles distally and trace it past the
nonunion site into the spiral grove. If the nerve is embedded in scar,
it is usually necessary to place it in a vascular loop and protect it
during the repair of the nonunion. -
It is rare to be able to fix the nonunion in situ;
therefore, take the nonunion down, remove all fibrous tissue from
between the bone ends, send a specimen for culture, freshen the bone
ends, and open the medullary canals. Sculpt the ends of the bone
fragments as necessary to maximize cortical contact and to ensure good
alignment. -
Shortening up to 2.5 cm in most patients
is acceptable if it is necessary to obtain apposition over the full
width of the cortex. In elderly patients, in whom functional demands
are lower, even more shortening is acceptable. -
Apply a broad plate with 4.5 to 5.0 mm
cortical screws, obtaining at least eight cortices of solid fixation
both proximally and distally. Many of the tricks for obtaining solid
screw fixation are described earlier. Plates usually fit best along the
anterolateral aspect of the humerus. In this location, they are free of
the radial nerve and function as a tension band. Always try to obtain
interfragmentary compression, either through the plate or, better,
independent of the plate. -
After the initial plate and
interfragmentary screw are in place, gently stress the construct,
looking for micromotion in the fracture site. If it is present, or the
hold of the screws is tenuous, I always put a second plate at right
angles to the first plate along the anteromedial cortex. This plate
should be a small fragment plate shorter than the original plate, with
at least six cortices of fixation above and below. The shorter, lighter
plate leaves more humerus exposed for revascularization and bone graft,
and minimizes the risk of a stress riser at the end of the double
plates. -
Petal the available bone surface with a
quarter-inch osteotome for at least 2.5 cm proximal and distal to the
fracture, and lay a morcelized cancellous bone graft along the humerus.
If there is cortical deficiency, cortical cancellous grafts are useful. -
Place a suction drain and meticulously
close the soft tissue. Close the intermuscular interval in which the
radial nerve lies with a layer of sutures deep to the radial nerve to
separate it from the plate and bone graft. This method prevents
reincorporation of the nerve into the scar and fracture callus.
Document this change in location in the dictated operative note. Then
close the muscle envelope around the fracture site to ensure full
muscle coverage, and close the subcutaneous fat and skin in a routine
fashion. A drain is usually advisable. -
Place the arm in a sterile dressing and shoulder immobilizer.
require protection, although I have them wear a shoulder immobilizer
for the first 6 weeks to remind them not to use the arm for anything
but the lightest of activities of daily living. A Sarmiento-type
fracture brace is also useful. Begin gentle, active range-of-motion
exercises for the elbow and shoulder immediately, using circumduction
exercises for the shoulder to avoid bending stresses on the plate. At 6
weeks, if healing is progressing well, overhead pulley exercises for
the shoulder can begin. Avoid resistive exercises or any use of the
extremity for other than light activities of daily living until solid
union is documented, which is
usually
12 or more weeks after surgery. Once solid union occurs, continue a
vigorous range-of-motion and strengthening rehabilitation program to
restore shoulder and elbow function (Fig. 27.9).
 |
|
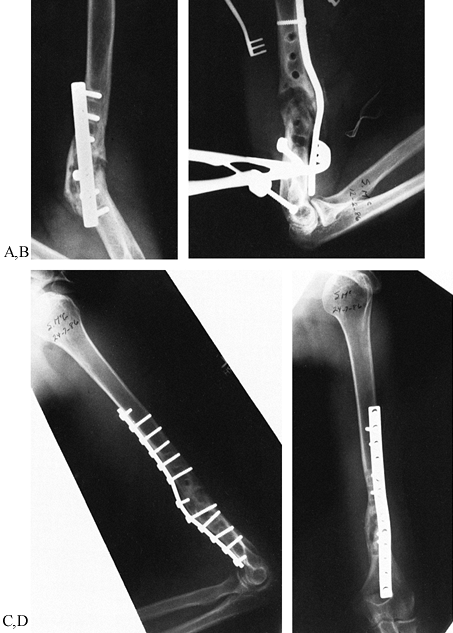
Figure 27.9. A 25-year-old man who had previous plate fixation of a fractured humerus, which resulted in a painful nonunion. A: Notice the inadequate plate and the radiolucencies around the screws, demonstrating looseness of internal fixation. B: The contoured “wave” plate was placed on the tension side of the nonunion. C, D: The nonunion has consolidated. The most distal screw is unicortical, not blocking the olecranon fossa.
|
humerus is very successful, with union rates in various series reported
from 91% in a difficult group of nonunions in elderly patients to 100% (29,38,49,57,66,81,89,103). The results with intramedullary fixation are much less predictable, with union rates reported from 54% to 87% (15,32,78).
nonunions with varus deformity and loss of the carrying angle. (See the
next section.) The surgical technique is nearly identical to that
described earlier for the nonunion. In most cases, a single-plane
osteotomy permits correction of the deformity, and some length can be
regained if the osteotomy is long enough. Stabilize it with an
interfragmentary screw and a broad plate, as described earlier.
nonarticular (that is, supracondylar) or intraarticular (usually
involving the lateral condyle, but involvement of the medial condyle is
possible as well) (56). Nonunions in this
region are exceedingly rare, because acute fractures about the elbow
make up only 2% of all fractures and the cancellous bone in this region
usually leads to union. Malunion is more common. Ackerman and Jupiter (1)
treated only 20 patients with nonunions of the distal humerus during a
16-year period at a major referral center. A general orthopaedic
surgeon may encounter only one of these nonunions in his or her career.
Patients treated nonoperatively and those with neglected fractures
frequently have considerable stiffness in the elbow joint and use the
nonunion as a false joint to gain additional motion at the elbow.
Knowledge of the available range of motion in the elbow is essential
for preoperative planning. Lateral radiographs of the elbow joint in
flexion and extension and the distal humerus usually demonstrate the
true range of motion in the elbow and the instability in the fracture.
In supracondylar nonunions, the cartilage of the joint is usually well
preserved; therefore, a comprehensive soft-tissue release to regain
elbow motion not only greatly enhances function but makes it more
likely that the nonunion will heal by relieving stress on the nonunion
site through the increased motion of the elbow joint. Previously open
supracondylar fractures with nonunion, such as in side-swipe injuries,
may have occurred because of bone loss. In a neglected nonunion that is
functioning as the elbow joint, mechanical erosion of the bone ends
frequently leads to shortening and loss of bone substance (Fig. 27.10 and Fig. 27.11). Reconstruction
of these injuries can be difficult owing to the short articular
fragment and the differential in size between the articular fragment
and the shaft. Although the risk of failure is somewhat higher, use of
a structural intercalary bone graft is sometimes necessary to
reconstruct these difficult nonunions, as illustrated in Figure 27.11.
 |
|
Figure 27.10.
AP and lateral radiographs of a 42-year-old man with a supracondylar nonunion of the humerus. He had only a 40° arc of motion in the elbow joint and had been using this pseudarthrosis for motion. Note the resorption of the proximal fragment and the size mismatch at the fracture site. See Figure 27-11 for management of this problem. |
 |
|
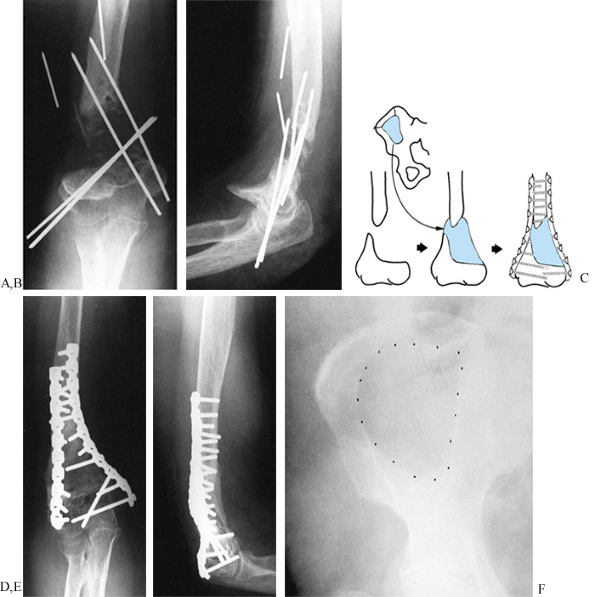
Figure 27.11. A:
Nonunion of a supracondylar fracture of the humerus in a 50-year-old woman. AP view shows 2.5 inches (7.5 cm) of bone loss. This fracture was open and was initially fixed with K-wires. No infection occurred, but it did not heal. A second operation at another institution, using bone graft and the K-wire fixation seen in this radiograph, was unsuccessful. B: Lateral view. C: The nonunion was treated with bone grafting and internal fixation in the following manner: •Through a posterior approach, the hardware was removed, fracture ends curetted, and length restored.
•A bicortical graft from the ilium was harvested.
•The graft was shaped and fitted into the defect with
some tension in the surrounding soft tissues to produce compression across the graft. •Internal fixation with two AO 4.5 mm reconstruction plates, one on each pillar of the distal humerus was achieved.
D: Anteroposterior view 12
weeks after surgery, at which time union appears to have occurred. The plates stop at different levels proximally to reduce the stress-riser effect, and six screws were placed in the short distal fragment. E: Lateral view. F: AP view of the pelvis showing the bone graft donor site. |
most commonly in the lateral condyle of the humerus. More commonly,
fractures of the lateral condyle heal in malposition with cubitus
valgus and continue to function fairly well throughout life. Patients
with symptoms that require surgery usually present with tardy ulnar
nerve palsy, decreased range of motion, and pain and apprehension with
use of the elbow (53). Sometimes, corrective
osteotomy must be performed at the time of repair of the nonunion to
improve position using a tricortical graft in the nonunion site (53). Intraarticular debridement and release and balancing of the soft tissues may be necessary to improve or maintain motion.
-
Intolerable pain from the nonunion.
-
Deformity that is not compatible with the level of function the patient expects or is cosmetically unacceptable.
-
Enough instability in the nonunion that the patient can no longer function at the level needed.
-
Cubitus valgus with progressive ulnar nerve palsy. Treatment alternatives include
-
Nonoperative treatment with supportive bracing.
-
Surgical treatment, with repair of the nonunion through double plate fixation and bone graft.
-
For cubitus valgus with a healed malunion
of the lateral condyle or a stable fibrous union, a closing-wedge or
opening-wedge osteotomy with plate fixation and a structural bone
graft, if an opening wedge is performed. Anterior transfer of the ulnar
nerve for tardy ulnar nerve palsy is usually necessary. -
In some cases, direct repair of a
nonunion of the lateral condyle is possible, but usually there is
sufficient remodeling that a satisfactory intraarticular contour is
exceedingly difficult to obtain.
-
Position the patient in a lateral
decubitus position on a regular operating table, with the operated
extremity uppermost. Support the arm on a well-padded obstetrics and
gynecology leg holder or similar device, permitting gravity to allow
the forearm to dangle at an angle of 90°. -
Prepare and drape the extremity free up to the shoulder, and prepare the iliac crest for bone graft harvest as well.
-
Approach the distal humerus and elbow joint through a straight midline incision just off the tip of the olecranon.
-
Dissect along the deep fascia medially to
the medial epicondyle, and identify the ulnar nerve. If tardy ulnar
nerve palsy is present or if the nerve will be at risk because of the
type of internal fixation to be done, perform an anterior transfer of
the ulnar nerve. I prefer to place it in a subcutaneous pocket, taking
care to release the medial intermuscular septum. Be certain that the
nerve has no tension or impingement upon it. -
From here, the approach varies according
to the needs of the particular situation. In a nonarticular
supracondylar nonunion that is at least 4 cm proximal to the joint
line, a midline triceps splitting approach often suffices for the
procedure. If the nonunion is closer to the joint, or if there are
significant intraarticular adhesions requiring a soft-tissue release,
then full exposure of the articular surface of the humerus and the
elbow joint is required. Do this through either an extended triceps
splitting approach, as described in Chapter 1,
or a chevron-type olecranon osteotomy. I prefer the triceps-splitting
approach. For this approach to be successful, the joint capsule,
triceps, and origins of the flexor and extensor muscle groups of the
forearm are reflected to beyond the epicondyles in medial and lateral
full-thickness flaps. Take care to preserve the triceps aponeurosis as
it crosses the tip of the olecranon to avoid disrupting the continuity
of the triceps mechanism. -
Now take down the nonunion, freshen the
bone ends, and reshape them to obtain maximum cortical apposition and
to correct deformity. Open the medullary canal proximally, and multiply
drill the face of the distal fragment distally with a 2 mm drill point. -
Now internally fix with double plates,
one on the posterior aspect of the lateral condyle and another along
the medial supracondylar ridge at right angles to the posterolateral
plate. Molding the plates to the bone is challenging; therefore, use
3.5 mm reconstruction plates or their equivalent. -
On the lateral side, fashion the plate to
fit down to the articular surface of the lateral condyle, taking care
to be certain that there is no impingement with the radial head when
the elbow is in full extension. Try to obtain at least three cortical
screws of fixation in the distal fragment. The most distal screws
running from posterior to anterior are opposite the articular surface
and therefore cannot be bicortical. I prefer to use nontapped cortical
screws, because this seems to provide better
P.904
purchase
than cancellous screws. Approximately four bicortical screws of solid
fixation in the proximal fragment are usually adequate. On the medial
side, usually the plate does not need to extend around the medial
curvature of the medial epicondyle unless the distal fragment is quite
small. This plate normally provides excellent fixation, because the
distal screws can extend transversely across the condyles in a
bicortical fashion. Try to place a similar number of screws in both
fragments medially as well. -
If an intercalary defeat is present that
cannot be handled by direct apposition of the two fragments, use a
technique similar to that described in Figure 27.11. -
Examine the elbow to determine the range
of motion. A range of -20° of extension to 120° of flexion provides
reasonably good function. If this is not present, consider a
soft-tissue release (60,63). -
Excise all intraarticular adhesions.
-
Inspect the olecranon and remove any osteophytes that are preventing full extension.
-
Inspect the olecranon fossa and remove
any osteophytes that are blocking full extension. If there is a block
to flexion, make a window in the olecranon fossa to provide access to
the coronoid fossa and permit removal of anterior osteophytes that may
be blocking motion. This should provide extension to within 10° of
neutral. -
If extension appears to be limited owing
to a tight anterior capsule, then dissect carefully along the anterior
aspect of the capsule from lateral to medial, isolating the capsule
from the anterior soft-tissue structures. Then carefully excise the
anterior capsule, taking care to avoid injury to the anterior
neurovascular structures. This also provides excellent exposure for
removal of any anterior osteophytes that might be impeding full flexion. -
When carrying the elbow through range of
motion, be certain that the articular surface of the olecranon remains
completely congruent with the distal end of the humerus rather than
hinging open, which gives a false measurement of the available motion
in flexion. -
Apply cancellous bone graft along the edges of the nonunion, taking care to not encroach on the joint.
-
If a tourniquet is used, deflate it now
and ensure good hemostasis. Drain the elbow. Meticulously close the
posterior longitudinal wound. In the case of a triceps-splitting
approach, close the deep capsule and deep triceps in a separate layer
and then close the triceps aponeurosis and approximate the fascia of
the extensor and flexor compartments of the forearm in a single layer
with interrupted #0 resorbable sutures. Close the subcutaneous fat and
skin in the usual manner. Take care to be certain that the ulnar nerve
remains in good position. -
Most patients tolerate immobilization
better in a position of about 20° of flexion than in one of 90°. Apply
a bulky dressing and medial and lateral splints to support the elbow
just short of full extension. Elevate the arm 10 cm above the heart.
-
Considerable swelling and occasionally
even skin blistering or compartment syndrome can occur after extensive
reconstructive procedures about the elbow. Monitor the patient
carefully during the first 48 hours postoperatively. If the patient has
pain beyond that expected, be certain to release the dressing fully and
inspect the arm carefully. If swelling is excessive or compartment
syndrome threatens, early release of the surgical incision down to the
deep fascia, and occasionally even deeper, may be necessary. After
swelling subsides, the wound is usually easily reapproximated. -
As soon as swelling subsides and the
patient becomes comfortable, remove the bulky dressing and splint,
apply a lightweight Bledsoe-type brace, and immediately begin active
range-of-motion exercises. With this procedure, it is absolutely
essential that the patient begin early aggressive, active motion under
the supervision of a therapist. The goal is to achieve the full motion
expected by 6 weeks after surgery. On the operative table, before
awakening the patient, it is possible to examine the elbow under
anesthesia to establish what the safe range of motion is before
excessive stress is placed on the reconstruction of the nonunion. A
brace can be set for this range of motion to protect the nonunion
during this rehabilitation. When bone-to-bone apposition has been
achieved, reasonably good stability is present at 6 weeks, but full
union usually requires 12 to 16 weeks. Do not allow resistive exercises
or use of the extremity for other than light activities of daily living
until full union has occurred. I have not found continuous passive
motion for the elbow to be of value.
-
Position the patient in the supine
position on an operating table, and prepare and drape the operated
extremity free as well as the iliac crest for bone graft. -
Make a longitudinal incision, beginning
over the radial head and extending proximally along the midlateral
aspect of the humerus. Dissect directly down to the lateral
supracondylar ridge of the humerus, and expose the distal humerus down
to the joint capsule by subperiosteal dissection. Place a sharp-tipped
Hohmann retractor posteriorly and anteriorly to expose the distal
humerus. Take care to avoid injury to the radial nerve. Under
fluoroscope control, drill a 2 mm K-wire transversely
P.905
across the humerus just proximal to the olecranon fascia and parallel to the elbow joint. -
While protecting the soft tissues, make a
transverse osteotomy to but not through the medial cortex. Open the
osteotomy by manipulation, which results in a greenstick fracture of
the opposite cortex. Confirm restoration of the anatomic position on
fluoroscopy. -
Harvest a tricortical iliac graft from
the anterior ilium. Insert this into the defect, compress the defect,
and internally fix it with a 3.5 reconstruction plate along the
posterolateral supracondylar ridge. Try to place at least one screw in
an interfragmentary fashion. -
An alternative is to perform an oblique
osteotomy in the frontal plane, which then permits correction of the
deformity by simply rotating through the osteotomy site. Fix it with an
anterior-to-posterior interfragmentary screw and a lateral
neutralization plate. Although this technique is technically more
difficult, I prefer it because union is faster and it eliminates the
need to harvest a bone graft. -
Postoperative treatment is as described earlier.
achieved union in five of five patients, and in my personal series of
12 patients, I achieved union in 100%. Those who required a soft-tissue
release to achieve elbow motion or who have intraarticular fractures do
less well from the standpoint of regaining elbow motion. Usually,
pronation and supination are nearly normal. In some patients, we have
had astoundingly good results, with gains in total motion of over 100°,
and in others we have seen no improvement from the preoperative range
of motion. The determining factors appear to be the degree of
intraarticular adhesion and arthritis, and the ability of the patient
to exercise in the face of discomfort during the postoperative recovery.
patients with a painful flail extremity with which they are unable to
perform even the minimal activities of daily living. In these patients,
particularly if they are elderly, total elbow arthroplasty provides a
method for salvage (27,64). Morrey and Adams (64)
reported on 36 consecutive patients with an average age of 68 years who
underwent semiconstrained elbow replacement for distal humeral
nonunion, with an average follow-up of somewhat more than 4 years. Of
these patients, 86% had a satisfactory result and only two had a poor
result. Patients showed a marked decrease in pain and an improvement in
the overall mean arc of motion from 74° to 111°. This is a challenging
procedure, however, as evidenced by the fact that seven patients had
complications and five of these required reoperation.
the original fracture (such as in alcoholics who fail to seek
treatment) or failed internal fixation (usually a tension band wire),
or is secondary to major bone loss such as in side-swipe injuries.
Neglected nonunions can do surprisingly well. They generally are free
of pain with a 2- to 4-cm gap, and the only functional deficit is
weakness in extension, which causes functional limitations but is
compatible with light activities of daily living. In my experience,
failure of internal fixation is most common when lightweight wires are
used to fashion a tension band repair that is then subjected to
repetitive heavy use by an uncooperative patient. It also occurs in
patients who have been victims of multiple trauma, are on enforced bed
rest, and tend to use their elbows for moving themselves in bed.
Failure tends to occur early before these become established nonunions
and can usually be treated by repeated internal fixation with stronger
devices. Nonunions due to bone loss are much more challenging because
they often involve a segment of the articular surface. Indications for
surgery include pain and functional loss. Alternative methods of
treatment in addition to bone graft include compression-plate fixation
with a 3.5 reconstruction plate placed on either the medial or lateral
surfaces of the olecranon and ulnar shaft; tension band plating with a
hook plate, as illustrated in Figure 27.12; or repeat tension band wiring, using a combination of screws and 18-gauge wire for the tension band.
 |
|
Figure 27.12. Nonunion of the olecranon. A: Inadequate tension band fixation of an olecranon fracture resulted in a nonunion. B:
Fixation has been removed, and a one third tubular plate has been fashioned as a hook plate, using the end hole as two sharp prongs. The tensioning device was applied after fixation of the plate to the olecranon fragment by a lag screw across the fracture site. Tensioning was then applied and supplemented by a long interfragmental fully threaded 3.5 mm screw. C: At 9 months, consolidation of the nonunion was occurring. This view also demonstrates the hook plate with its firm attachment into the olecranon. |
-
Expose the olecranon by subperiosteal dissection. If there is a stable fibrous nonunion in good position, internal fixation in situ is indicated.
-
Otherwise, excise the fibrous tissue from
the nonunion site, freshen the bone ends and open the medullary canal
of the distal fragment, and reduce the fracture. -
Take care to not reduce the diameter of
the olecranon fossa because this will produce incongruence in the elbow
joint, which can lead to loss of motion, pain, instability, and
precocious arthritis. -
Place a reconstruction plate along the
medial or lateral border of the olecranon, and mold it carefully to
maintain anatomic position. -
Apply a cancellous bone graft.
-
After completion of the fixation, examine
the elbow under anesthesia to determine the safe range of motion that
can be used postoperatively without excessively stressing the construct. -
Close the wounds and apply a bulky soft dressing, splinting the elbow just short of full extension.
-
After swelling has subsided, apply a
Bledsoe-type brace with the locks set to permit a safe range of motion,
and immediately begin active gentle motion. Avoid use of the extremity
for anything but light activities of daily living until union occurs,
which is generally no earlier than 8 weeks. Most heal by 12 weeks, but
some take as long as 16 weeks if an intercalary bone graft has been
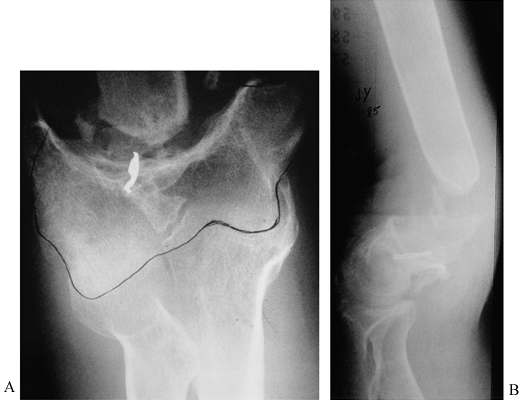
used (Fig. 27.13). Figure 27.13. Nonunion of the olecranon. A: AP and lateral radiographs showing failure of a third tubular plate, resulting in nonunion. B:
Figure 27.13. Nonunion of the olecranon. A: AP and lateral radiographs showing failure of a third tubular plate, resulting in nonunion. B:
AP and lateral radiographs. This fibrous nonunion was in an acceptable
position and, therefore, was treated with compression plate fixation
and an interfragmentary compression screw in situ, resulting in rapid healing.
This was treated with an inlay cancellous iliac crest bone graft,
followed by long-arm cast immobilization for 4 weeks, resulting in
radiographic union by 10 weeks. Surprisingly, full pronation and
supination returned.
of the diaphysis of the radius and ulna, whether both or only one is
involved, has generally been considered mandatory in adults (3,7,10,14,20,31,36,37,44,46,65,67,76,85,86,94,95,97).
Nearly anatomic reduction and early motion are necessary to avoid
restriction of pronation and supination. Although the ulna may be
treated with a closed reduction and functional bracing (87), plate fixation of the ulna and, on occasion, intramedullary nailing are necessary in significantly displaced fractures.
fractures are 98% or better, with good to excellent functional results
and less than 30% loss of total pronation and supination (3,10,14,20,31,43,80). At least six to eight cortices of fixation, with a 3.5 mm system and compression techniques, should be used (65,94).
Nonunions of the fractures of the shafts of the radius and ulna are now
most commonly due to segmental bone loss, infection, or inadequate
internal fixation with mechanical failure. Poor surgical technique with
excessive soft-tissue striping can also lead to nonunion because of the
devascularization of the bone ends (61,62).
-
Treatment of nonunions of the diaphysis
of the radius and ulna does not differ significantly from primary
internal fixation. Approach the ulna through a longitudinal incision
along the subcutaneous border and the radius through a modified
Thompson’s dorsal radial approach. Making the skin incision on a line
drawn from the tip of the radial styloid to the lateral epicondyle of
the humerus, using the appropriate intermuscular interval, allows
exposure of the radius from radial head to radial styloid (see Chapter 1). -
In most cases, loose screws or broken
plates, or both, are present. Remove these and identify the nonunion
site. If the overall alignment is acceptable and there is a stable
fibrous nonunion, then simple plate fixation and compression usually
suffice. -
In most cases, however, deformity is
present. Most likely you will have to deal with shortening and
angulation, and possibly intercalary bone loss. Restoring alignment in
the ulna is not too difficult because, other than in the area of the
olecranon, the bone for the most part is straight. Restoring the radial
bow of the radius, however, can be difficult, and intraoperative
radiographic guidance with either a fluoroscope or plain radiographs is
very important. Occasionally, nonunions or malunions are complicated by
synostosis or collapse of the interosseous membrane. This requires take
down of the synostosis and shaving of the bone to restore the normal
contour, as well as soft-tissue release in the area of the interosseous
membrane. This can be quite challenging because of the presence of the
neurovascular bundles in this area. -
Restore normal alignment and length. A
temporary distractor or an external fixator may be necessary to hold
the radius out to length. Place cancellous bone or a structural
tricortical iliac crest bone graft into any bone deficiency, and apply
a 3.5 mm or equivalent plate, using interfragmentary compression and
longitudinal compression where possible. Try to obtain at least eight
cortices of fixation proximal and distal to the fracture. In some cases
in which there is no bone loss, the internal fixation can be carried
out first and the bone graft applied second. -
Apply plates to the dorsal lateral aspect
of the radius, where they act as a tension band, and on the ulna they
can be placed on the subcutaneous border or slipped off to the side so
that they are less prominent beneath the skin. When applying bone
graft, do not impinge on the interosseous membrane because this may
lead to synostosis or restriction in motion. -
After internal fixation, determine the
safe range of motion in flexion and extension of the wrist and elbow,
and in pronation and supination. This will be useful in instructing the
patient about postoperative exercises. -
Close the muscle envelope over the
fracture sites but leave the deep fascia open because of the
predilection for swelling after these extensive procedures. Close the
skin in a routine manner and place the arm in a bulky long arm splint
with the elbow at 20° or so of flexion and the forearm in neutral
supination and pronation. After swelling has abated, a lightweight
brace or molded orthotic cuff is useful to remind the patient to be
careful with the forearm. Have the patient begin active motion
immediately, using the extremity only for light activities of daily
living until union occurs. In the forearm, nonunions usually require at
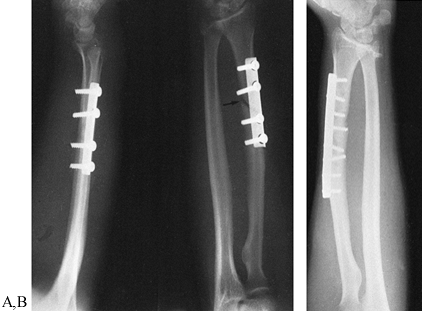
least 16 weeks and may require up to 6 months to heal solidly (Fig. 27.14 and Fig. 27.15).![]() Figure 27.14. Delayed union of a Galeazzi fracture. A:
Figure 27.14. Delayed union of a Galeazzi fracture. A:
An oblique fracture has been internally fixed using a semitubular plate
with inadequate cortical purchase. There is no interfragmentary screw
across the fracture. B: Union after
fixation with a 3.5 mm dynamic compression plate placed on the dorsal
radial surface with an interfragmentary screw, along with a cancellous
bone graft. Figure 27.15. Atrophic nonunion of the ulna in a Monteggia fracture dislocation. A, B: Atrophic nonunion of the fracture of the ulna treated previously by cerclage wire and intramedullary fixation. C: A 3.5 mm dynamic compression plate and cortical cancellous bone grafting were used to stabilize the ulnar fracture. D:
Figure 27.15. Atrophic nonunion of the ulna in a Monteggia fracture dislocation. A, B: Atrophic nonunion of the fracture of the ulna treated previously by cerclage wire and intramedullary fixation. C: A 3.5 mm dynamic compression plate and cortical cancellous bone grafting were used to stabilize the ulnar fracture. D:
After 1 year, union had occurred. Restoration of the alignment and
length of the ulna resulted in satisfactory position of the radius and
functional forearm rotation.
malposition; loss of the normal arc and spacing between the radius and
ulna due to collapse of the bones toward the interosseous membrane; or
to subluxation or internal derangements in the proximal radioulnar
joint or the distal radioulnar joint. The latter problems in the joints
are addressed in Chapter 43.
It can be corrected by osteotomy to place forearm motion in a more
functional range. It is difficult to increase the total range of motion
because of intraosseous membrane contraction and soft-tissue scarring.
cross-unions may occur. Rotational problems are best managed at the
time of acute fracture care. Radioulnar synostosis (3,5,50)
may follow closed or open treatment. It appears to be related directly
to the extent of injury to the interosseous membrane, because it is
more common in fractures that are at the same level, in open fractures,
and after internal fixation. Early motion can significantly reduce the
incidence of this problem in internally fixed fractures.
indicated. As long as the hand can be used appropriately and can be
placed in the appropriate positions to perform day-to-day activities,
no additional treatment is required. This usually is in the neutral or
somewhat pronated position, allowing shoulder and elbow motion to
compensate.
the forearm has been elusive, but recent work provides reasonably good
guidelines (54,90,96).
This is particularly an issue when one considers the need for open
reduction and internal fixation in adolescents, in whom the amount of
remolding that is possible following healing in a nonanatomic position
can be somewhat unpredictable. Matthews et al. (54)
showed that with 10° of angulation in the radius, there was minimal
functional loss in pronation and supination, whereas over 20° of
angulation functional loss occurred. Tarr et al. (96)
provided more specific information, in that they demonstrated in a
cadaver study that greater than 10° of angulation in both bones located
in the distal third of the forearm resulted in an average loss of range
of motion of 12.5% ±pm 4.5%. If this same angulation was present in the
middle third of the forearm, this loss increased to 16% ±pm 5.7%;
therefore, angulation in the middle third of the forearm is tolerated
less well than in the distal third. They found that the loss in
supination and pronation secondary to rotational malposition was
directly proportional to the degree of malrotation. Schemitsch and
Richards (90), in a retrospective review of 55
patients with forearm fractures who underwent plate fixation at 6 years
of follow-up, provided a new method of assessing radial bow and
relating this to loss of motion. Although angulation over 10° in both
bones has adverse functional effects, it appears that preservation of
the normal bow of the radius is the more critical factor. In their
patients, they compared the radial bow on comparison x-ray studies to
the normal side and measured this according to the maximum distance
between the radius and the ulna at the interosseous membrane. Their
overall results in this group of patients were excellent, in that 54 or
55 fractures in the radius and ulna healed and 84% of the patients had
satisfactory functional results. They demonstrated that restoration of
the radial bow was directly correlated with the functional outcome and
that completely normal motion
required
restoration of the radial bow to normal. In spite of the efforts made
in their series to achieve anatomic reduction of both bones, their
results show that this is difficult; the mean outcomes in their series
were 64° in pronation and 74° in supination. The normal maximum radial
bow, as measured at the interosseous membrane, in their series was 15
mm. To get 80% of normal range of motion, this had to be within 1.5 mm
of normal. They found the same direct relationship to grip strength.
Stated another way, if the maximum radial bow was within 4% to 5% of
normal, then 80% of forearm range of motion and grip strength could be
expected. As emphasized in the study conducted by Tarr et al. (96),
both the location and the amount of the loss of radial bow were
important. The overall results in their series were somewhat less good
than previously reported; the unsatisfactory functional outcomes in
their study were 16%, as compared to 15% for Anderson et al (3) and 9% for Chapman et al (14).
They attributed this to the fact that the severity of injury was
greater in their series in that all of their patients had fractures of
both bones and greater numbers of fractures were open.
reported on 27 osteotomies for malunion of the forearm, including 20 in
the radius, two in the ulna, and five in both. Their indications were
loss of motion in 20 (average loss 74°, range 20° to 120°), a painful
distal radioulnar joint in six, and poor cosmesis in one. One of the
most important findings in their study was that time had a significant
effect on the improvement in range of motion. Patients operated on
sooner than 12 months after the original injury gained an average of
29° of supination and pronation (range 20° to 160°, and in those
operated on more than 12 months after injury the gains were less than
half, averaging 30° (range -25° to 95°). Of the six patients operated
on for distal radioulnar joint pain, three experienced marked
improvement of their pain and achieved a stable joint, but the average
loss of range of motion in the six patients was 7° (range -25° to 25°).
The patient operated on for cosmetic problems was pleased with the
appearance of the forearm but lost 10° of rotation. Their outcomes
point out that it is possible to achieve significant improvement in
patients with forearm malunions, but the surgery is better done earlier
than later and does not have consistent results, and the fact that
Trousdale and Linscheid had complications in 11 of their 27 patients
demonstrates that the surgery is challenging.
-
Interoperative radiographic evaluation of
the correction achieved is important; therefore, use a radiolucent hand
table and fluoroscopy or plain radiographs, or both. -
Depending on whether osteotomies are
planned for an isolated forearm bone or both bones, use the surgical
approaches described earlier. Expose the site for osteotomy in a
subperiosteal fashion. This should be at the maximum point of
deformity. Use gentle technique to minimize soft-tissue injury and to
avoid invading the interosseous space. When performing osteotomies of
both the radius and ulna at the same level, it is important to try to
prevent communication of the hematomas from the two operative sites
because this could lead to synostosis. -
Perform an appropriate osteotomy,
depending on the deformity to be corrected. In many cases, it is
possible to identify the old fracture site and reassemble the fracture
in anatomic position after removing excess callus and refashioning the
bone ends. In more mature malunions, it is necessary to perform a
formal osteotomy. Often this must be in an oblique plane to allow
correction of angulation and rotary deformity, which are frequently
combined. This can be challenging because the rotational component of
the deformity is difficult to assess by radiography preoperatively.
Some repeat shaping of the osteotomy site after intraoperative
radiographs and examination for range of motion are usually necessary. -
Internally fix the osteotomy, taking care
to place an appropriate bow in the plate on the radius to restore fully
the radial bow. Obtain eight cortices of fixation proximal and distal
to the osteotomy site with an interfragmentary screw across the
osteotomy, if possible. The plates are best located just off the
subcutaneous border of the ulna and on the dorsal radial aspect of the
radius. You may make an exception for a very distal radius osteotomy,
where the plate might be better placed palmerly. -
If the patient has pathology in the
interosseous membrane or at the distal radioulnar joint (DRUJ),
additional procedures to release contractures of the interosseous
membrane or to address problems in the DRUJ may be necessary. See the
discussion of treatment of synostosis below; see Chapter 43 for DRUJ problems. -
Perform a meticulous soft-tissue closure,
leaving the deep fascia open. Initially immobilize the extremity in a
well-padded long-arm splint, with the elbow at 90° and the forearm in
neutral pronation and supination. As soon as pain subsides and the
swelling is controlled, begin a supervised range-of-motion exercise
program under the supervision of a hand therapist. Solid stability of
the internal fixation is obviously necessary to obtain an optimal
result, the latter requiring fairly vigorous early active range of
motion without resistance.
reconstructed with an osteotomy, but in most cases, assuming that the
radius and ulna are longitudinally stable and there are no major DRUJ
problems, the easiest procedure producing the best results is radial
head excision.
-
Approach the radial head through a Kocher incision (see Chapter 1).
Expose the radial head and proximal neck as far as the annular
ligament. Take care to avoid injury to the posterior interosseous nerve. -
With a water-cooled mini-oscillating saw
or high-speed burr, transect the radial neck just proximal to the
radial head and smooth the edges to remove any osteophytes or malunited
fragments. -
Leave the annular ligament intact. If it is disrupted and the proximal radius is unstable, reconstruct it.
-
Close the wound in a routine fashion,
apply a bulky sterile dressing and splint, and begin elbow and forearm
exercises as soon as the patient will tolerate them.
the upper extremity are similar to those of all major surgery in the
upper extremity, including infection, neurovascular injury, failure of
the fixation, loss of joint motion, and others. The risk of these
problems can be minimized by careful attention to patient selection and
details of the surgery. The outcome depends strongly on a fully
cooperative patient who is capable of performing exercises in the face
of discomfort and who is completely compliant with postoperative
instructions.
is most common after severe proximal forearm fractures. It can be
managed by radial head resection with excision of the synostosis, as
described earlier. Restoration of forearm motion through excision of a
synostosis is challenging because soft-tissue contracture and scarring
frequently compromise the motion that can be gained, and avoiding
injury to the anterior and posterior interosseous neurovascular bundles
can be challenging. To prevent reformation of the synostosis, fat,
muscle, and Silastic membranes have been used to fill the space between
the radius and the ulna (9,50,74,101,108,109).
If large raw areas of bone are left after excision of the synostosis, I
find that coating these with a thin layer of bone wax and then filling
the gap where the synostosis was present with autologous fat helps
prevent reformation (Fig. 27.16).
 |
|
Figure 27.16. Synostosis of both bones of the forearm. A:
A 25-year-old man sustained an open fracture of both bones of the forearm, which was treated with plate fixation. He developed a synostosis of his forearm in a nonfunctional position. B: This postoperative radiograph shows excision of the synostosis with a free fat graft packed in the area of the synostosis. At 9 months, he had functional forearm rotation, lacking the last 20° of supination and pronation. |
for a detailed discussion. For most activities of daily living, an
elbow flexion and extension arc of motion from 30° to 130° is
necessary. A marked impairment of the ability to position the hand in
space occurs when a flexion contracture exceeds 45° and flexion is less
then 110°. These are indications for operative treatment of contracture
of the elbow. Lesser degrees of loss of motion may be an indication,
depending on the patient’s functional needs. Loss of motion can be
caused by extrinsic contractures involving the joint capsule,
ligaments, and osseous structures, and intrinsic contractures can be
caused by intra-articular incongruity or malunions and adhesions. If
there is significant loss of articular cartilage or if posttraumatic
degenerative arthritis is present, fascial interposition arthroplasty
may be necessary to gain a satisfactory outcome. This usually requires
use of distraction with a specialized external fixator.
contracture, with and without distraction, are available. Morrey’s
technique (63) is utilitarian and is commonly used for treatment of contractures (Fig. 27.17).
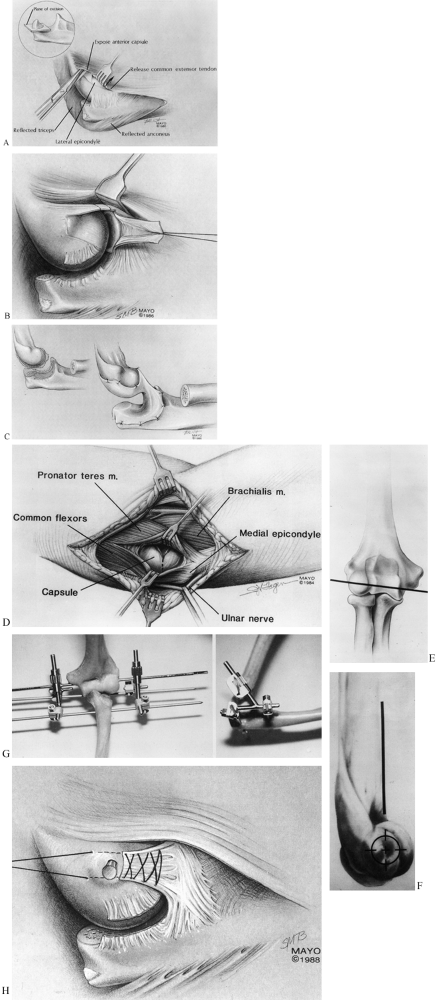 |
|
Figure 27.17. Morrey fascial arthroplasty of the elbow. A: The reflected extensor mechanism, resected tip of the olecranon, released forearm extensors, and exposed anterior capsule. B: The reflected lateral collateral ligament and the anterior capsule resected to the medial side (broken lines). C: Joint surfaces to be smoothed with a burr (dotted areas). A fascial graft attached to the humerus and ulna, with sutures through bone. D: Medial approach. E: Location of the anatomic axis of rotation of the elbow in the frontal plane. F: Lateral view of the axis of rotation of the elbow. G: Mayo Clinic distraction device. H: Repair of the lateral collateral ligament to the humerus. (From Morrey BF. Post-traumatic Contracture of the Elbow. J Bone Joint Surg 1990;72-A:601.)
|
-
Place the patient supine on an operating table with a sandbag under the operated side. Drape the upper extremity free.
-
Prep and drape the ipsilateral lateral thigh for possible harvest of a fascial graft.
-
Make an extensile posterolateral approach, using the interval between the anconeus and extensor carpi ulnaris (see Chapter 1).
Expose as much of the elbow joint as necessary to achieve an adequate
release by elevating the triceps from the posterior aspect of the
humerus in continuity with the lateral forearm musculature and triceps
aponeurosis. Dissect medially along the anterior aspect of the humerus
joint capsule to expose the anterior structures (Fig. 27.17A). -
Excise the posterior tip of the olecranon
process and any osteophytes, and remove the posterior capsule. Excise
or release anterior capsular adhesions and structures as necessary.
Lyse all intracapsular adhesions. -
If possible, preserve the lateral
collateral ligament. If release is necessary, reflect it distally,
releasing its humeral origin. Resect the anterior capsule (Fig. 27.17B). If anterior impingement is found, excise any bony osteophytes. -
If 50% or more of the articular surface
of the elbow is not covered by hyalin cartilage, or if a significant
malunion is present, recontour the joint and perform an interpositional
fascial arthroplasty. Smooth the joint surfaces of the humerus and ulna
with a burr (Fig. 27.17C). -
Trim the fascial graft to the appropriate
size and shape, and attach it to the articular surface of the distal
humerus through sutures along the edges of the humeral joint surface.
This can be aided by front-to-back drill holes. Then double the fascial
membrane back on itself to form a continuous double layer covering the
olecranon. Secure the graft to the olecranon in a similar manner (Fig. 27.17C). -
Try to preserve the radial head, but excise it if it presents problems.
-
If an external fixator will be applied or
there is a need to complete the soft-tissue release, make a medial
approach over the medial epicondyle. Split the flexor-pronator muscles
in line with their fibers and complete the medial part of the
capsulectomy. If necessary, perform an anterior transfer of the ulnar
nerve (Fig. 27.17D). -
Apply a distraction or dial-compass external fixator.
-
Under fluoroscopic control, insert a
guide pin through the center of the capitellum, transversely across the
condyles of the humerus, to exit the trochlea dead center. It is
important that this be directly in line with the instant center of
rotation of the elbow (Fig. 27.17E, Fig. 27.17F). -
Mount the external fixator on this pin,
and then place two or more half pins into the distal humerus and two in
the proximal ulna according to the directions of the manufacturer.
Adjust the frame to ensure appropriate motion and to separate the joint
surfaces 4 to 5 mm in all positions of the elbow. Remove the guide pin (Fig. 27.17G). -
Repair the lateral collateral ligament, using a Bunnell stitch placed through the drill holes in the humerus (Fig. 27.17H).
-
Place a small suction drain and close the wounds in layers.
-
Apply a sterile dressing and a bulky compression dressing.
-
Begin motion as soon as possible. Morrey uses continuous passive motion.
removes the external fixator under anesthesia, gently examines the
elbow (avoiding manipulation) to assess the end points of motion, and
then uses turnbuckle splints, one for extension and one for flexion, to
help the patient gain range of motion while continuing on an active
daily exercise program. He uses the turnbuckle splints regularly for as
long as 6 months following the routine outlined in Table 27.1.
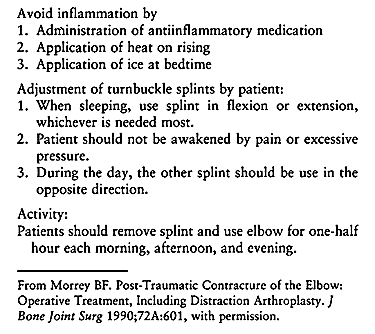 |
|
Table
27.1. General Guidelines for Use of Turnbuckle Splints for the First Three Postoperative Months in the Treatment of a Stiff Elbow |
treated by release without distraction external fixation, the
preoperative arc of total motion was 32°. Postoperatively, it increased
to 74°. In those treated with distraction arthroplasty without
interposition, total motion before operation was 32° and increased to a
total average arc of motion of 99°. In the six treated with
interpositional arthroplasty and distraction, motion increased from a
total of 27° to 107°. The increases in pronation and supination were
modest and were best in the interposition-distraction group.
treatment of nonunions and malunions in the upper extremity, because
these are uncommon problems that may appear only one or two times in
the lifetime of an average surgeon. Large series are rare even in the
hands of surgeons working in major referral centers. In addition, each
patient’s problem is unique and requires an individualized approach.
Recognizing these limitations, my recommendations for the treatment of
nonunions and malunions in the upper extremity are as follows:
-
Use a careful soft-tissue technique with
as limited exposure of bone as possible (usually two of the four
quartiles of circumference available) in an effort to maintain the
blood supply to the bone. -
Take down the nonunion site in most cases
by fashioning of the bone ends to correct deformity and maximize
surface area, opening the medullary canal and placing multiple shallow
drill holes on metaphyseal fragments to encourage revascularization. -
Use solid internal fixation, eliminating
any micromotion; try to obtain fixation in two planes, usually with a
plate in one plane and an interfragmentary screw in the other, followed
by autologous bone graft laid on a petaled cortical surface. -
During surgery under anesthesia,
establish the safe range of motion possible for early rehabilitation.
Institute early motion and then progress the rehabilitation program as
the fracture consolidates. -
For nonunions of the surgical neck of the
humerus, use 3.5 mm reconstruction double plate fixation combined with
iliac crest bone graft. -
For mid-diaphyseal nonunions of the
humerus, use broad plate fixation with interfragmentary screws combined
with autologous bone graft. -
For supracondylar humerus nonunions, use
double plate fixation with 3.5 mm or equivalent reconstruction plates,
placing one plate on the posterior aspect of the lateral column and one
on the medial aspect of the medial column combined with iliac crest
bone graft. -
For elbow arthroplasty, I follow the tenets advocated by Morrey (63,64)
as outlined earlier; using a straight posterior approach when
accompanying bony reconstruction makes this a more convenient approach. -
For olecranon nonunion, use single and
occasionally double plate fixation with small reconstruction plates
combined with iliac crest bone graft (tricortical graft for bone
deficiency). -
For malunions, I try to use oblique
single plane oblique osteotomies with interfragmentary screw fixation
and neutralization plates. -
Using these techniques, between 1980 and
1995 I was able to achieve union in 36 of 37 nonunions of the humerus
and 100% healing of five nonunions in the radius and ulna.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
D, Curtis RJ, DeHaan JT, et al. Treatment of Nonunion of Fractures of
the Midshaft of the Clavicle with a Modified Intramedullary Hagie Pin
and Autogenous Bone Grafting. J Bone Joint Surg 1991;73A:1219.
PN, Kingsbury GH, Wilbur JH. Midshaft Clavicle Nonunions Treated with
Intramedullary Steinmann Pin Fixation and Onlay Bone Graft. J Orthop Trauma 1994;8:88.
M, Petriccioli D, Panno B, Marenghi P. Seidel Locked Nailing for the
Treatment of Unstable Fractures and Nonunion of the Humerus. Chirurgia Degli Organi di Movimento 1996;81:189.
PH, Luitse JS, Strating RP, van der Hart CP. Operative Treatment for
Delayed Union and Nonunion of Midshaft Clavicular Fracture: AO
Reconstruction Plate Fixation and Early Mobilization. J Trauma 1996;40:985.
JR, Greshman RB. Osteoperiosteal Grafts: A Preliminary Report of the
Treatment of Fresh and Ununited Fractures of the Long Bones. J Bone Joint Surg 1962;44A:1653.
DRJ, Torchia ME. The Spiral Compression Plate for Proximal Humeral
Shaft Nonunion: A Case Report and Description of the New Technique. J Orthop Trauma 1999;13:141.
JB. Complex Non-union of the Humeral Diaphysis. Treatment with a Medial
Approach, an Anterior Plate, and a Vascularized Fibular Graft. J Bone Joint Surg 1990;72A:701.
SD, Goitz HT, Redler MR, Whitehill R. Nonunion of a Midshaft Clavicle
Fracture Associated with Subclavian Vein Compression. Orthopaedic Review 1989;18:431.
LS, Kaufer H, Garver DF, Sonstegard DA. The Effect on
Supination-pronation of Angular Malalignment of Fractures of Both Bones
of the Forearm. An Experimental Study. J Bone Joint Surg 1982;64A:14.
M, Jupiter J, Toh CL, et al. Reconstruction after Malunion and Nonunion
of Intra-articular Fractures of the Distal Humerus. Methods and Results
in 13 Adults. J Bone Joint Surg 1994;76:614.
A, Caja VJ, Sabato C, et al. Composite Bone Grafting and Plate Fixation
for the Treatment of Nonunions of the Forearm with Segmental Bone Loss:
A Report of Eight Cases. J Orthop Trauma 1995;9:419.
D, Perey BH, Jupiter JB. The Functional Outcome of Operative Treatment
of Ununited Fractures of the Humeral Diaphysis in Older Patients. J Bone Joint Surg 1999;81A:177.
EH, Richards RR. The Effect of Malunion on Functional Outcome after
Plate Fixation of Fractures of Both Bones of the Forearm in Adults. J Bone Joint Surg 1992;74A:1068.
RR, Garfinekl AI, Sarmiento A. The Effects of Angular and Rotational
Deformities of Both Bones of the Forearm. An In Vitro Study. J Bone Joint Surg 1984;66A:65.
BG, Simpson LA, Hardegger F. Rotational Osteotomy for Recurrent
Anterior Dislocation of the Shoulder Associated with a Large Hill-Sachs
Lesion. J Bone Joint Surg 1984;66-A:1443.
CC, Shih CH, Chen WJ, Tai CL. Treatment of Clavicular Aseptic Nonunion:
Comparison of Plating and Intramedullary Nailing Techniques. J Trauma 1998;45:512.