Biceps Tendon Injuries
IV – Elbow Reconstruction > Part B – Evaluation and Treatment of
Elbow Disorders > 52 – Biceps Tendon Injuries
insidious partial tears, complete traumatic tears, to chronic neglected
ruptures. Nonoperative treatment was commonly advocated in the past and
still plays a role in the elderly or inactive patient. Many surgeons
now recognize that early surgical reattachment of the torn tendon to
the radial tuberosity will restore function and prevent deformity.
two stages; the first is the partial tear, which can be insidious in
onset, followed by a complete disruption of the remaining tendon with a
sudden traumatic event. Davis and Yassine in 1956 presented two cases,
one a partial and one a complete rupture of the distal biceps tendon,
which illustrated the degenerative changes that occur in the tendon. In
both cases, spurring had occurred at the bicipital tuberosity, which
acted as a knife to separate the tendon with supination and pronation.
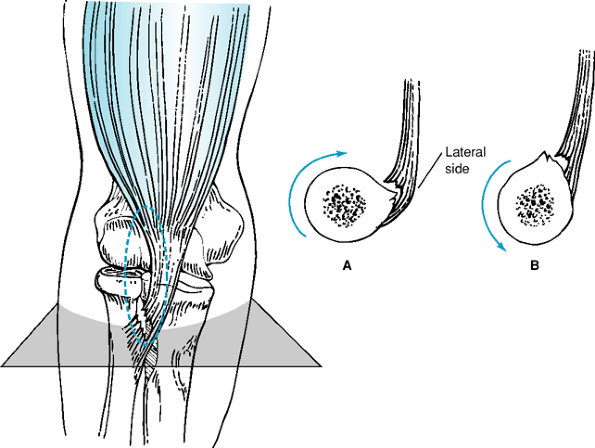
In each case, the disruption occurred in the lateral aspect of the
tendon first and progressed medially (Fig. 52-1).
The tendon avulsion almost always occurs at the insertion site, and at
the time of surgery, the torn tendon end is bulbous and frayed,
confirming the degenerative process of this injury.
whereas women rarely present with this injury. In a review of >100
cases of distal biceps injuries surgically repaired at the Mayo Clinic,
only one patient was a woman, and her tear was only partial. Distal
biceps injuries were once considered uncommon, mostly based on a report
by Gilcrest in 1925 in which he stated that only 3 of 100 patients with
biceps tendon injuries that he reviewed were at the distal insertion.
Currently, greater recognition of this condition has led to more
diagnoses.
complete tears. Complete tears can be further divided into acute
(<10 days from injury), subacute (11 to 21 days), or delayed/chronic
(>21 days). The subclassification of the complete tear is important
when considering surgical management of the torn tendon. On average, if
the patient is operated on ≤10 days of the injury, the retracted tendon
is easily identifiable, the tract to the tuberosity is intact, and the
tendon can be reapproximated to the tuberosity without significant
dissection. If >10 but <21 days have passed since the injury at
the time of surgical repair, the scarring makes the surgery more
difficult and increases the risk of complications, but the tendon can
usually be reapproximated to the tuberosity. At ≥21 days postinjury,
primary repair becomes more difficult and a graft may be necessary to
restore length.
with a sudden traumatic event of forced extension against an actively
flexing elbow. Patients present with ecchymosis, pain, swelling,
weakness, and a palpable defect of the biceps tendon. The ecchymosis is
fairly characteristic, extending along the entire medial aspect of the
arm and forearm. The deformity of the retracted biceps is also
characteristic with the tendon stump retracted proximally and the
Popeye-shaped muscle belly retracted into the upper arm. Initially the
patients may complain of pain, but this often subsides by the time they
present to the orthopaedist. The patients will be tender in the
antecubital fossa and have pain with resisted
supination
and flexion as well as mild to moderate weakness with these resisted
motions. In some cases, the lacertus fibrosis may remain intact, making
it difficult to palpate the tendon defect. In thin individuals, the
diagnosis can be confirmed by comparing the motion of the bicep muscle
belly with the elbow flexed 90 degrees while the forearm is passively
rotated. While moving the forearm from supination to pronation, the
biceps muscle belly should move distally with an intact tendon. In
addition, as the examiner grips a patient’s right injured forearm with
the right arm, he or she should be able to grip the arm above the elbow
and place the left thumb under an intact biceps tendon.
 |
|
Figure 52-1 The degenerative tear occurs on the deep side of the tendon. Left: drawing demonstrating the appearance of the lesion at surgery, in which the dotted line represents the enlarged bicipital bursa. Right: A cross section of the area of the arm indicated by the straight line in the left figure. When the arm is pronated (A), the sharp margin of the tuberosity impinges on the tendon; when the arm is supinated (B), the tendon is pulled free. (Reprinted from
Davis WM, Yassine Z. An etiological factor in tear of the distal tendon of the biceps brachii: report of two cases. J Bone Joint Surg A. 1956;39:1365–1368
, with permission.) |
no longer be apparent; however, the muscle belly will remain retracted
and may be atrophic. The retracted tendon is often scarred, fibrosed,
and not palpable, and the patient remains weak in flexion and
supination. These patients complain more of a “cramping” and weakness
rather than a sharp pain with activity.
presentation of complete distal biceps tendon ruptures, patients with
partial tears often fail to describe an acute traumatic event,
describing an insidious onset to their symptoms. The tendon is intact
anteriorly but tender to palpation. In addition, the bicipital
tuberosity is also tender when palpated with the forearm in full
pronation. The patients tend to have weakness with resisted supination
and flexion but not as marked as with complete tears. A local cortisone
and anesthetic injection from a posterior approach to the radial
tuberosity may be both therapeutic and diagnostic in these cases. This
should be done with the arm in full pronation, aiming the needle at the
level of the tuberosity, just between the radius and ulna. The patients
should be warned that temporary posterior interosseous nerve palsy may
result as the anesthetic diffuses through the surrounding tissues.
normal; however, they may occasionally demonstrate osteophytic spurring
at the level of the radial tuberosity. Although occasionally helpful in
the patient with a questionable diagnosis, MRI is often unnecessary. In
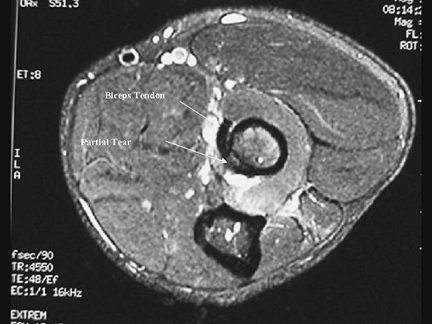
partial tears, however, MRI evaluation is very helpful is assisting in
the diagnosis of these cases. The presence of increased intratendinous
signal intensity and abnormal tendon diameter along with fluid around
the tendon can confirm the diagnosis (Fig. 52-2).
tears may provide acceptable results in older or more sedentary
individuals. The resulting weakness, pain, and deformity, however, have
lead many surgeons to recommend surgical reattachment of the avulsed
tendon to the tuberosity. The issue of surgical approach, however, has
been controversial.
reattach the biceps to the radial tuberosity was associated with
several complications including radial and median nerve palsies. In an
attempt to avoid such complications, Boyd and Anderson advocated a
two-incision technique. They were able to limit the anterior dissection
by exposing the radial tuberosity through a second posterior incision.
Although this technique was thought to decrease the
potential
of nerve injury associated with an anterior approach, it was perceived
to increase the likelihood of radioulnar synostosis.
 |
|
Figure 52-2
Axial MRI image from a patient with a partial distal biceps tendon tear demonstrating increased signal intensity at the tendon insertion site coinciding with the site of the tendon tear on the radial surface of the tendon. (Reprinted from Kelly
EW, Steinmann SP, O’Driscoll SW. Surgical treatment of partial distal biceps tendon ruptures through a single posterior incision. J Shoulder Elbow Surg. 2003;12:456–461 , with permission.) |
occurring with the anterior approach and nerve injury occurring with
the two-incision approach. Firm evidence is lacking attributing either
excess bone formation or nerve injury with either surgical technique.
single anterior or a two-incision approach, the patient is placed
supine on the operating table with the arm out on a hand table. The arm
is then prepped and draped from the wrist to the axilla and a sterile
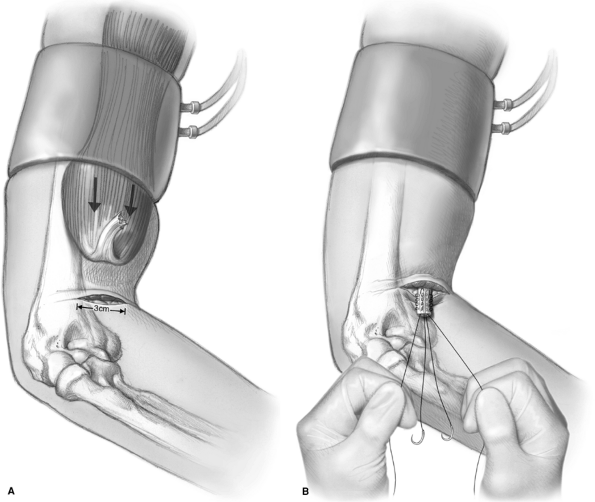
tourniquet is used. The first important task is to milk the muscle
belly distally prior to applying the tourniquet (Fig. 52-3A).
This maneuver pushes the tendon down toward the antecubital fossa where
is can easily be retrieved through the anterior incision.
The incision is centered over the bicipital tract just medial to the
midline. The lateral antebrachial cutaneous nerve lies just to the
lateral aspect of the incision but does not need to be exposed. Just
deep to the subcutaneous tissues lies the fascia of the bicipital
tunnel, which can be incised with scissors longitudinally. In the acute
setting, hemorrhagic fluid is frequently encountered, indicating the
correct plane. Blunt digital dissection can now be used to identify the
radial tuberosity distally in the tunnel, and proximally to identify
the tendon. The tendon may be grasped with an Allis clamp and then
pulled out the anterior incision. The bulbous end is then debrided back
just a few millimeters and the tendon prepared with a running locking
Krackow stitch using a strong nonabsorbable no. 2 suture. This is done
twice to provide four strands of suture (Fig. 52-3B).
from the anterior incision by following the bicipital tunnel. A blunt,
curved hemostat is carefully inserted into the space previously
occupied by the biceps tendon. The instrument slips past the tuberosity
between the radius and ulna and is advanced below the radius past the
ulna while pronating the forearm so that its tip may be palpated on the
dorsal aspect of the proximal forearm (Fig. 52-4).
A second, 4-cm-long incision is made over the instrument, which should
be 1 cm anterolateral to the subcutaneous border of the ulna. The
tuberosity is exposed by a muscle-splitting incision. The ulna is never
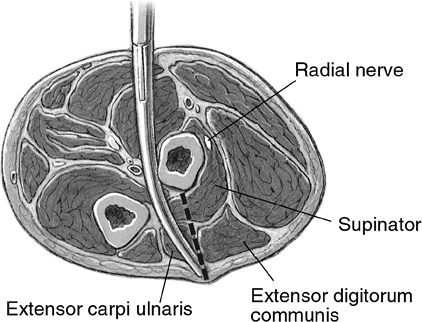
exposed. The supinator fascia is identified after splitting through the
common extensor muscles. Fibers are then split to expose the bicipital
tuberosity, taking care to keep the forearm in maximal pronation to
protect the posterior interosseous nerve. Small Hohmann retractors are
carefully placed underneath the supinator on the radius. A small round
(4 to 5 mm) high-speed burr is used to excavate a trough 1.5 cm long
and 5 mm wide in the radial tuberosity. The trough is taken into the
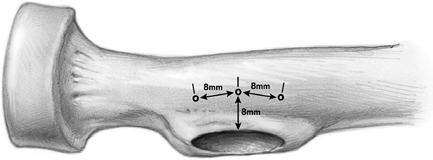
medullary canal of the radius. Two or three drill holes are then placed
7 to 8 mm apart and ≥7 mm from the edge of the excavation using a small
drill bit or 0.062 K-wire (Fig. 52-5). Copious
irrigation is used to remove bone dust at each stage during preparation
of the cavity and the suture holes. The sharp leading edge of the
radial bone trough should be smoothed off to prevent irritation of the
tendon with supination and pronation.
strands of suture through the anterior incision and out the posterior
incision, taking care to be aware of the tendon’s orientation in the
tunnel. The strands of suture are then threaded through the bone trough
and out the drill holes, one at each of the proximal and distal holes
and two out the middle hole (if using three drill holes). A Hewson
suture passer is helpful for this step. The tendon is pulled into the
bone trough by supinating the forearm and pulling on the sutures. The
sutures are tied over the bone bridges. The wound is carefully lavaged
and the wound closed in layers. The patient is placed in a posterior
plaster splint overnight for comfort.
of a Henry, S-shaped incision is performed with the transverse aspect
similar to that described above for the mini two-incision procedure,
but with the lateral edge curving distally. The lateral antebrachial
cutaneous nerve is identified in the lateral aspect of the incision and
protected. The brachioradialis is retracted laterally and the pronator
is retracted medially, exposing the radial tuberosity with the forearm
in supination. The posterior interosseous nerve is at risk in this
exposure but can be kept out of the surgical field by supinating the
forearm. The radial tuberosity is debrided of any remaining soft tissue
but is not decorticated. Two suture anchors are then placed in the most
medial aspect of the radial tuberosity. The tendon is identified and
prepared
as
noted above up to the point of placing sutures. One limb of each of the
two sutures is then placed in Krackow fashion up the medial or lateral
edge of the tendon. The two sutures are then tied to each other
proximally. The two free suture ends at the anchors are then tied to
each other pulling the tendon to the tuberosity with the arm in full
supination and 90 degrees of elbow flexion. The wound is closed in
layers and the patient placed in a posterior rigid splint for 7 to 10
days. If using an interference screw, the exposure is the same while
the tuberosity is drilled and the screw inserted per the manufacturer’s
instructions.
 |
|
Figure 52-3 A: The tendon stump is milked distally with the tourniquet applied and then expressed through the anterior incision. B:
Two running, locking stitches are placed in the tendon stump providing four strands of suture to tie to the radius. (Reprinted from Kelly EW, O’Driscoll SW. Mini-incision for acute distal biceps repair. Techniques Shoulder Elbow Surg. 2002;3[2]:57–62
, with permission.) |
days, it is often quite retracted and it is difficult to get the tendon
back to the radius without flexing the elbow. If the tendon can be
reapproximated with the elbow flexed <90 degrees, a primary repair
may be performed with the confidence that the muscle belly will relax
within a few days once tension has been restored. Often, however, in
the chronic setting, the tendon itself is very atrophic or so scarred
that primary repair is not an option. In this situation, a tendon graft
is the best option to restore length and contour. The biceps is first
exposed through a larger, Henry type of anterior incision taking the
smaller transverse incision as described above and carrying it out
laterally, then curving proximally as far as necessary to expose the
muscle. Care is taken to identify and protect the lateral antebrachial
cutaneous nerve. Different types of tendon grafts have been described
including semitendinosus, brachioradialis autografts, and Achilles
tendon allografts. The latter are ideally suited for chronic biceps
reconstructions. The graft has excellent mechanical and physical
properties. The aponeurotic portion of the graft is wide and long
enough to permit secure suturing to the host biceps muscle, while the
distal part of the allograft can be easily trimmed to the appropriate
length.
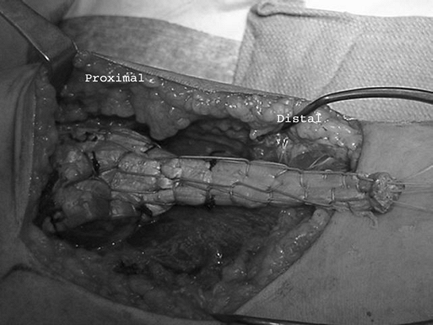
The
wide expansive portion of the Achilles allograft tendon is attached to
the biceps muscle belly and tendon stump with multiple no. 2
nonabsorbable sutures (Fig. 52-6).
The tendon insertion end is then passed through the bicipital tunnel
and out through the posterior incision as described above for the
primary repair. The distal end of the allograft can then be trimmed
back to create the proper length for tensioning prior to inserting the
distal tendon end into the prepared bone trough at the bicipital
tuberosity. The sutures are to be tied with the elbow in 60 to 90
degrees of flexion and full pronation. Once the tendon is trimmed to
the appropriate length, it is prepared as described for the primary
repair above with two no. 2 nonabsorbable sutures in a Krackow fashion
providing four suture stands. The repair is then completed as described
above using the two-incision technique.
 |
|
Figure 52-4
A large blunt curved hemostat is placed through the anterior incision, down the tunnel of the biceps tendon, and between the radius and ulna to identify the site for the posterior incision. (Reprinted from Kelly EW, O’Driscoll SW. Mini-incision for acute distal biceps repair. Techniques Shoulder Elbow Surg. 2002;3[2]:57–62
, with permission.) |
 |
|
Figure 52-5
Illustration of the proximal radius describing the position of the holes placed to pass the suture and tie over the bone bridge. The holes should be 7 to 10 mm from the trough edge and 7 to 8 mm apart, creating a very stable bone bridge over which to tie the suture. (Reprinted from Kelly EW, O’Driscoll SW. Mini-incision for acute distal biceps repair. Techniques Shoulder Elbow Surg. 2002;3[2]:57–62
, with permission.) |
 |
|
Figure 52-6
The aponeurosis of the Achilles allograft is secured proximally to the muscle belly and remaining tendon stump of the biceps while distally it is prepared with two running, locking sutures to secure the allograft to the radius. |
repair can be accomplished through a single posterior incision avoiding
any anterior dissection. The radial tuberosity is located by palpating
the lateral forearm in full pronation, or by measuring down from the
olecranon on the lateral preoperative x-ray view. A 4-cm incision is
then made centered over the radial tuberosity, 1 cm anterolateral to
the subcutaneous border of the ulna. The fascia of the extensor
digitorum communis is identified and split longitudinally in line with
the skin incision, avoiding the subcutaneous border of the ulna. With
the forearm fully pronated to protect the posterior interosseous nerve,
the supinator fascia is identified and split longitudinally over the
radial tuberosity, exposing the underlying biceps tendon at its
insertion on the radius. As the partial tear and pathology occurs on
the undersurface of the tendon, which is not exposed, the tendon in the
wound often appears normal.
tendon needs to be pulled out of the wound and probed. To accomplish
this, a stay suture is placed in the most proximal portion of the
biceps that is visible in the wound and the tendon pulled down and out
of the wound. This same maneuver is repeated two or three times with
the elbow flexed, each time placing a new stay suture more proximal in
the tendon to pull more tendon out of the wound. With 2 to 3 cm of
biceps tendon pulled out through the posterior wound, the undersurface
of the tendon can be inspected and probed to reveal the defect in the
undersurface of the tendon. Once the pathology has been confirmed, the
remaining portion of the intact tendon can be detached while the tendon
is held securely with the stay sutures to prevent retraction into the
wound. The degenerative and frayed end of the tendon is sharply
debrided, cutting back a few millimeters into healthier tendon. The
tendon is then made to retract between the radius and ulna by extending
the elbow while the stay sutures permit it to be brought back
posteriorly after preparation of the bicipital tuberosity. The trough
in
the radial tuberosity is created and the tendon prepared and secured to
the radius as described above in the two-incision technique.
tendon in the acute or subacute setting (<30 days) are uniformly
excellent. Numerous reports, regardless of the technique used, have
demonstrated return of function, contour, and strength by 6 months. The
results from partial repairs are similar but much less commonly
reported. Pain relief can be achieved in 90% of patients with the
posterior-only incision. The results from chronic repairs using a
tendon graft are also limited in number but similarly acceptable with
90% of patients satisfied and few complaints of pain. The restoration
of objective strength, however, has not been well documented.
a bone trough and transosseous sutures, immobilization of the elbow can
be limited to only the first night and rehabilitation of the tendon can
be started the day after surgery in the setting of acute, chronic, or
partial repairs. The patients are instructed to begin gravity-assisted
extension exercises with active-assisted and passive flexion the day
they are removed from the postoperative dressing. The sling is worn for
comfort the first 6 weeks to prevent a constant gravitational pull on
the tendon. As their initial postoperative pain subsides, they are
instructed to “use no more force than would be required to lift a glass
of water or a telephone receiver” for 6 weeks, then to “use common
sense” and avoid heavy force (e.g., getting a window unstuck, and so
on) until 3 months. From 3 to 6 months postoperatively, they are simply
advised to avoid violent force such as occurs in contact sports but can
work against unlimited resistance. They can begin a self-directed
strengthening program with light weights. Formal physical therapy is
rarely indicated. Unlimited activities are permitted after 6 months in
all patients.
JM, Amadio PC, Morrey BF, et al. Proximal radioulnar synostosis after
repair of distal biceps brachii rupture by the two-incision technique.
Report of four cases. Clin Orthop. 1990;253:133–136.
EW, Steinmann S, O’Driscoll SW. Surgical treatment of partial distal
biceps tendon ruptures through a single posterior incision. J Shoulder Elbow Surg. 2003;12:456–461.
Huec JC, Moinard M, Liquois F, et al. Distal rupture of the tendon of
biceps brachii. Evaluation by MRI and the results of repair. J Bone Joint Surg. 1996;78B:767–770.
