Ulnohumeral Arthroplasty
The process typically limits extension to a minimal or moderate extent.
Most symptomatic is impingement pain with terminal extension and, less
commonly, terminal flexion with or without ulnar nerve involvement. A
debridement procedure termed ulnohumeral arthroplasty has proven to be effective and reliable for such conditions, especially if ulnar nerve involvement is an issue.
candidate for ulnohumeral arthroplasty. This process occurs
predominantly in males by at least a 5 to 1 ratio (4,11,14).
The mean age of onset is approximately 55 years, range 25 (uncommon) to
65. The chief complaint is terminal extension pain; a painful midarc is
uncommon. Radiohumeral involvement occurs in approximately 50%, and
loose-body formation in approximately 50%. More than half of the
individuals will have an occupation or lifestyle associated with
repetitive use, such as a carpenter, laborer, or person who requires a
wheelchair or crutches for ambulation (11). About one in four will have symptoms of ulnar nerve irritation.
presenting with terminal extension pain, radiographic evidence of
coronoid or olecranon osteophytes, and ossification of the olecranon
foramen. If ulnar nerve symptoms are present, the nerve is inspected.
pain throughout the arc of motion, marked limitation of motion with an
arc of less than 30 to 40 degrees, or severe radiohumeral involvement
indicating an advanced and generalized process. Isolated symptoms of
catching associated with loose bodies are best dealt with by
arthroscopy (12,13). If
motion loss is the principal concern and the ulnar nerve is not
symptomatic, we prefer the column decompression procedure (6) (Chapter 21).
this procedure. This operation is not designed to reliably gain motion
but rather to relieve the pain associated with the impingement
arthritis, especially in terminal extension. If the impingement is
associated with mild osteophyte formation, an arthroscopic debridement
has been effective in the hands of the experienced (12,13).
However, particular attention should be paid to the presence of ulnar
nerve symptoms. This must be addressed at the time of decompression and
prompts this rather than the arthroscopic procedure.
bodies in addition to routine anterior/posterior and lateral
radiographs, it is important to assess this before surgery. Careful
plain films or CT may be useful to define. The precise size of the
osteophytes as well allows identity of any loose bodies. Specific care
is taken not to overlook any loose bodies, as these may cause
mechanical symptoms later. Other imaging studies such as arthrogram or
magnetic resonance imaging (MRI) are worthless.
shoulder, general anesthesia is administered and the elbow is brought
across the chest.
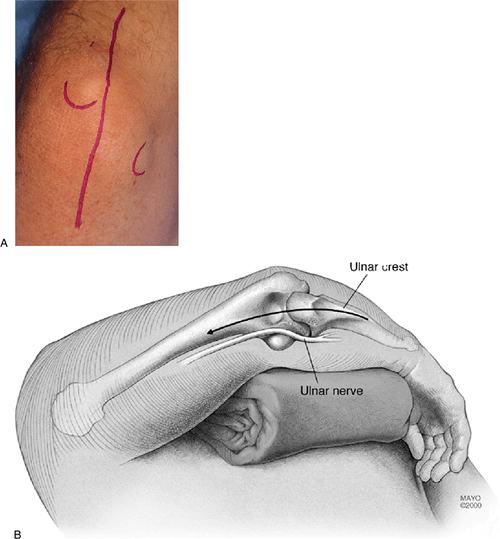
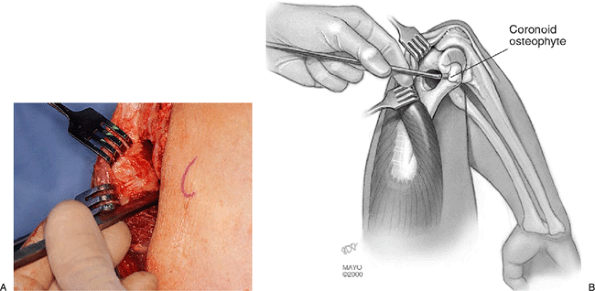
the olecranon. This extends distally about 4 cm and proximally about 6
cm (Fig. 20-1). The subcutaneous tissue is reflected from the medial aspect of the triceps.
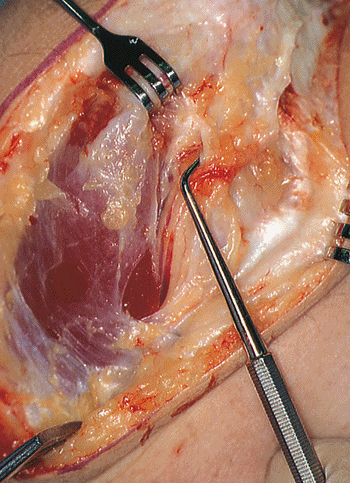
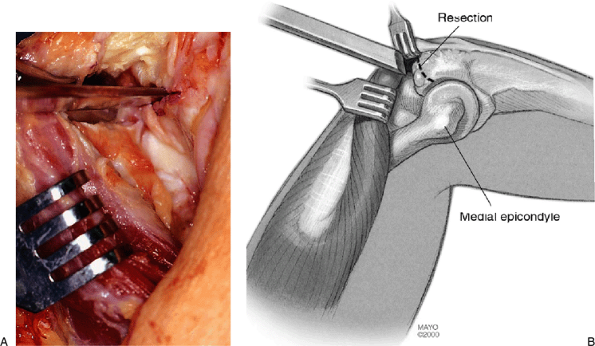
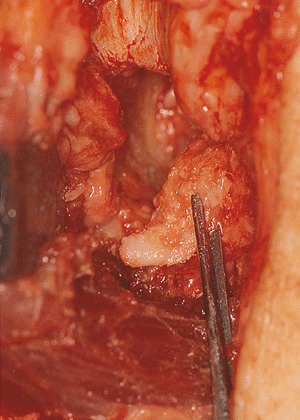
carefully inspected. Its possible involvement with an osteophyte or
from degenerative changes in the medial epicondylar region should be
assessed before surgery (Fig. 20-2). The nerve
has been a source of irritation for a growing number of patients, so we
have a lower threshold to decompress than we once had. The nerve is
carefully inspected. If it appears to be compressed, the cubital tunnel
retinaculum is released.
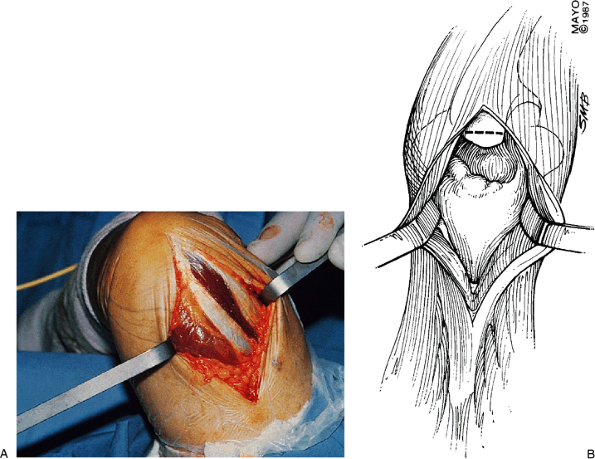
simple triceps-splitting technique was originally described and is
still used in very muscular individuals (Fig. 20-3).
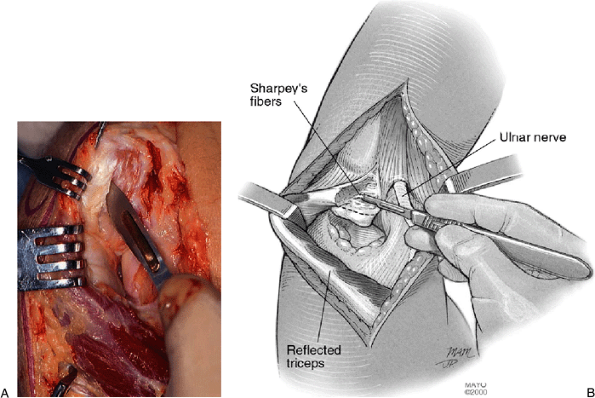
Otherwise, approximately one-third to one-half of the triceps
attachment may be elevated from the tip of the olecranon, releasing
Sharpey’s fibers by sharp dissection (Fig. 20-4).
The triceps is elevated from the posterior aspect of the distal humerus
by blunt dissection using a periosteal elevator, the capsule is
excised, and any loose bodies are removed from the posterior
compartment.
Usually there is a prominent osteophyte present that may extend across
the joint and into the medial and lateral aspect posteriorly. The tip
of the olecranon with the osteophyte is resected first using an
oscillating saw or a 19-mm osteotome to define the exact amount to be
resected. A 13-mm osteotome is used to complete the resection (Fig. 20-6) and the olecranon process with its osteophyte is removed (Fig. 20-7).
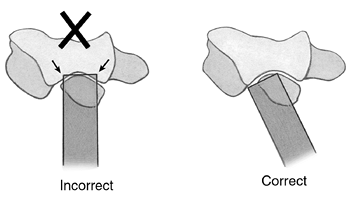
The level should be such that the posterior aspect of the ulna is flush
with the midportion of its articulation. The orientation of the
osteotome should be parallel to each face of the trochlea rather than
directed straight across the olecranon and into the trochlea (Fig. 20-8).
Often there are osteophytes originating from both the medial and the
lateral columns. Proper placement of this foraminectomy is important.
The trephine follows the curvature of the trochlea; the osteophyte may
be removed in part with an osteotome to allow the trephine to be
properly seated. After several turns of the trephine it is removed and
the orientation of the foraminectomy is confirmed to be accurately
placed (Fig. 20-10). The foraminectomy with the trephine is then completed and the core of bone is removed from the
distal humerus. This will frequently include osteophytes from the anterior aspect of the joint (Fig. 20-11).
Inspection through the posterior aspect of the elbow into the anterior
capsule is then possible. Loose bodies are identified and removed (Fig. 20-12).
We then palpate the anterior column and determine whether any
particularly tight bands are present that may need to be released. Any
loose bodies that may be present or have been identified by a
preoperative tomogram are removed and care is taken to be sure that
none are left or overlooked.
 |
|
Figure 20-1. A,B: A straight skin incision is made just medial to the tip of the olecranon.
|
 |
|
Figure 20-2.
The ulnar nerve is identified at the medial margin of the triceps muscle and, if not compressed, is protected in the cubital tunnel (dental probe) but not translocated. |
 |
|
Figure 20-3. A,B: The simplest exposure is that of triceps muscle splitting to expose the posterior joint.
|
 |
|
Figure 20-4. A,B:
The medial aspect of the insertion of the triceps is reflected from the tip of the olecranon. Avoid releasing more than one-half of the Sharpey’s fiber insertion. |
 |
|
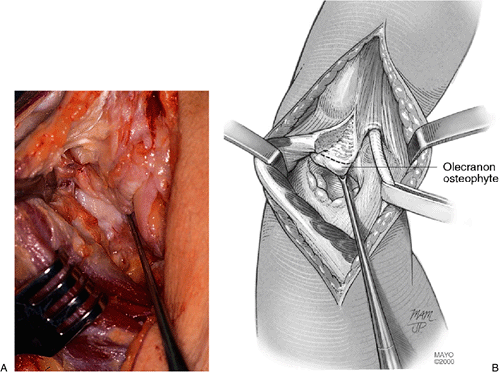
Figure 20-5. A,B: The prominent olecranon osteophyte is identified and the line of olecranon process resection is defined.
|
 |
|
Figure 20-6. A,B:
The osteophyte and process is removed with an osteotome. The initial cut may be made with an oscillating saw to provide optimum orientation. |
 |
|
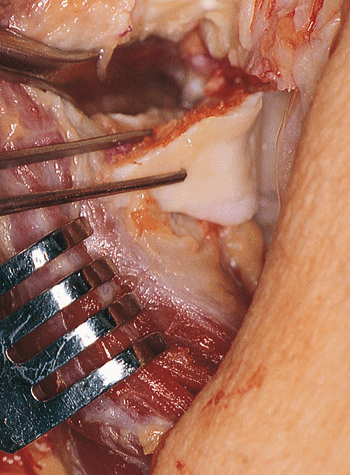
Figure 20-7. Removal of the olecranon process.
|
 |
|
Figure 20-8.
The completion of the osteotomy of the olecranon is with the osteotome parallel to each face of the trochlea. Direct transection will injure the trochlea. |
 |
|
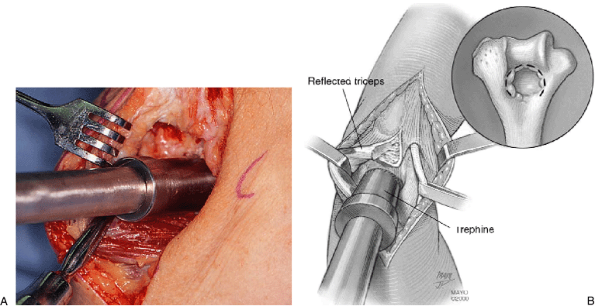
Figure 20-9. A,B: With the triceps reflected laterally a trephine is used to remove the ossified olecranon fossa.
|
 |
|
Figure 20-10.
The contour of the trephine follows that of the trochlea, and inspection of the initial cut should be made before its completion. |
removing the coronoid osteophyte and a portion of the coronoid process.
By fully flexing the elbow the coronoid appears in the orifice created
by the trephine. This can only be done with the elbow flexed. This is
usually easily accomplished if the triceps has been split (Fig. 20-13A), but if the triceps has been reflected, it must be retracted laterally at the same time as the elbow is being flexed, which
is done with difficulty in the heavily muscled patient (Fig. 20-13).
A curved 7-mm osteotome follows the distal aspect of the
foraminectomized distal humerus. The tip of the olecranon is palpated
and with a curvature directed toward the ulna; the coronoid with its
osteophyte is resected and removed through the foramen (Fig. 20-14).
The anterior aspect of the joint is again palpated with elbow flexion
and extension to ensure that this has been adequately resected. A final
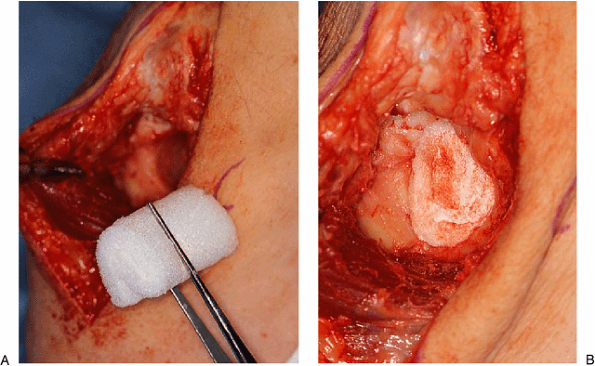
check for any residual loose bodies or impingement is followed by
placing a portion of rolled Gelfoam into the defect to fill the dead
space to minimize the chance of hematoma and possibly recalcification (Fig. 20-15).
 |
|
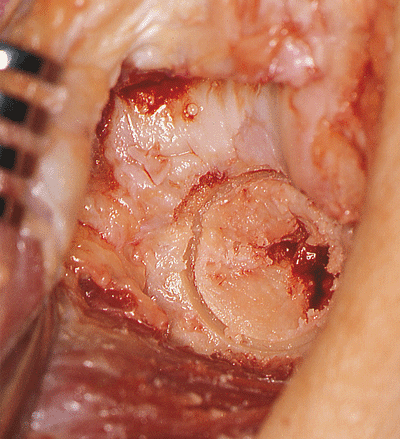
Figure 20-11. The foraminectomized portion of the distal humerus is removed. Note the anterior osteophytes present on this specimen.
|
 |
|
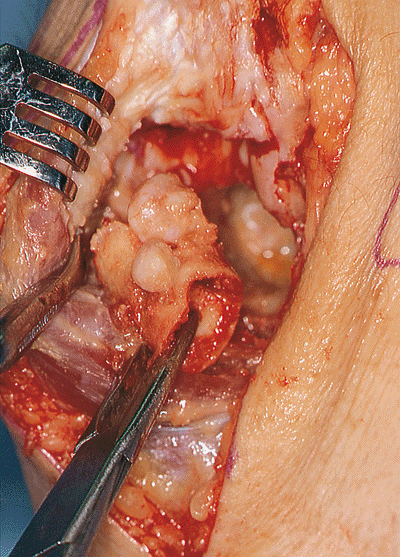
Figure 20-12. Anterior compartment loose bodies then may be identified and removed through the foramen.
|
 |
|
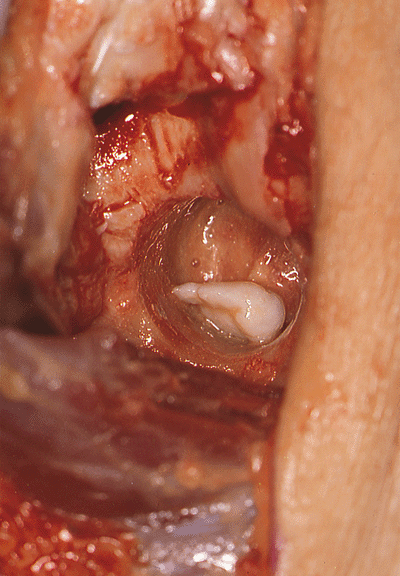
Figure 20-13. A,B:
With the triceps reflected laterally and the elbow flexed as much as possible, an osteotome is introduced through the foramen. The instrument follows the distal surface of the foramen, and the coronoid process with its osteophyte is then osteotomized. |
 |
|
Figure 20-14. The osteophyte and a portion of the coronoid are removed.
|
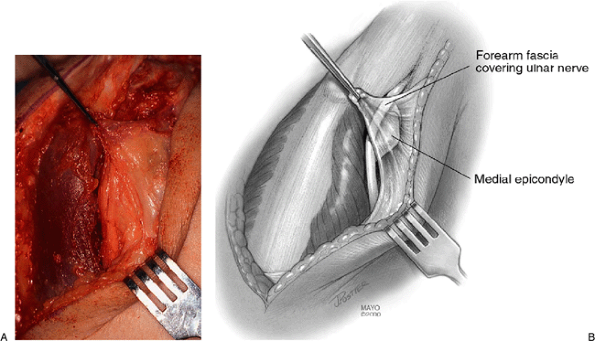
normal position if partially reflected. Reattachment is not necessary
since adequate insertion strength persists. The forearm and brachial
fascia are brought back to the medial margin of the triceps and secured
with absorbable suture (Fig. 20-16). The remainder of the closure is routine and is the choice of the surgeon.
 |
|
Figure 20-15. Gelfoam is then rolled in a cylinder-type fashion (A) and placed in the foramen (B).
|
 |
|
Figure 20-16. A,B:
The triceps is allowed to resume its normal position. Reattachment is not considered necessary unless more than half of the triceps has been reflected. Forearm fascia is brought to the margin of the triceps to prevent any subluxation of the ulnar nerve. |
A continuous passive motion (CPM) machine is then used, beginning the
day of surgery for approximately 24 to 36 hours, at which time the
axillary catheter is discontinued and a portable CPM is provided. The
patient is dismissed at day 2 or 3. If significant loss of extension or
flexion was observed before surgery and it is felt that this may be
improved after the procedure, then flexion and extension braces, again
similar to those described for the surgical release of the stiff elbow,
are prescribed. Reassessment is made at 3 weeks. At that time the use
of the splints is decreased to approximately 2 to 3 hours in the
morning and 2 to 3 hours in the evening, with the patient continuing to
sleep in the splints. The CPM machine is generally discontinued after
the third week as well. The patient is seen again at 6 weeks and at 3
months. It is uncommon to gain or to lose any significant motion after
3 months, but this may still occur up to 6 months or possibly even a
year. The exact period of time during which these patients are followed
must be individualized.
by Outerbridge and Kashiwagi in a series of patients in the Japanese
literature in 1977 (5). The experience was updated by Minimi et al. in 1996 (8).
With longer surveillance, recurrence of both pain and motion loss was
observed in about 40%. The original report revealed greater than 90%
satisfactory results, but it was recognized that the osteophytes may
recur, and the underlying disease process is of course still present. A
more recent experience, again from Japan, tends to confirm these
findings (7). At the Mayo Clinic the procedure
was modified by preserving the triceps, decompressing the ulnar nerve,
and using a trephine for decompression. The results of the first 13
patients reveal that approximately 85% were considered satisfactory at
an average of 3 years following the surgery. Pain relief is seen in
approximately 90%. Improved motion is observed in 80% and averages
about 10 to 15 degrees of improved extension and approximately 10
degrees of improved flexion for an overall improvement arc of about 20
to 25 degrees. There has been no instance of instability. The
experience is currently being updated (1).
Preliminary results reveal that approximately 20% note some ulnar nerve
symptoms, which has prompted the current recommendation regarding
preoperative ulnar nerve assessment and decompression. Nonetheless,
approximately 80% are satisfied a mean of 7 years from surgery. The
procedure has been redone in one patient.
patient population, that of a severe ulnar neuropathy. It is felt that
a retractor may have compressed this nerve during the surgical
procedure. This experience in part prompted the recommended exposure in
which the ulnar nerve is identified and protected throughout the
surgical procedure. Recurrence of the disease process is a function of
time (8). Within the first 5 years, less than
10% symptomatic recurrence has been observed, which is consistent with
what is reported in the literature.
columns, improper placement of the foraminectomy may lead to a column
fracture. Hence the need for adequate visualization of the margins of
the columns.
elbow. He indicated that he had particular difficulty holding objects
overhead for any period of time, and this was limiting his
ability
to do his job. This process had been noticed approximately 2 years
earlier, with the first abnormality noticed being loss of full
extension and forearm rotation. He had a radial head excision with only
modest impairment limited to forearm rotation. He had little pain
through the midarc of flexion and extension. The examination revealed a
range of elbow flexion of 30 to 125 degrees, pronation of 70 degrees,
and supination of 75 degrees. The ulnar nerve was painless to
palpation. Radiographs revealed a prominent osteophyte in the anterior
coronoid, less so in the tip of the olecranon (Fig. 20-17). The olecranon foramen was ossified, as was the resected radial head (Fig. 20-18),
as demonstrated on the anteroposterior radiograph. Debridement included
the olecranon, coronoid, foramen osteophytes, and a loose body (Fig. 20-19). Five years after the surgical procedure the patient has an arc
of motion of 18 to 130 degrees, and pronation-supination is unchanged.
He has essentially no pain and is well pleased with the result (Fig. 20-20).
 |
|
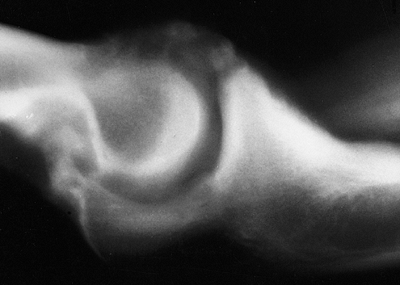
Figure 20-17.
A 46-year-old laborer has extensor pain and motion of 40 to 120 degrees. The lateral roentgenograph reveals osteophytes of the olecranon and of the coronoid. |
 |
|
Figure 20-18. The olecranon and coronoid foramen are ossified on the anteroposterior view.
|
 |
|
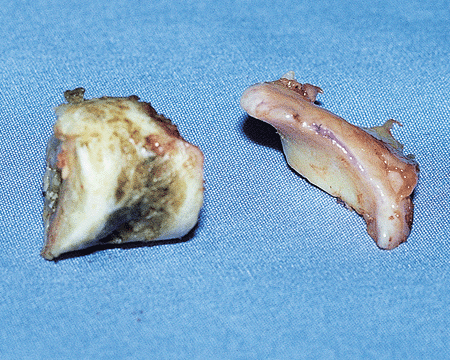
Figure 20-19.
The debridement consists of a large olecranon osteophyte and of the foramen resection. The coronoid osteophyte was also removed. |
 |
|
Figure 20-20. A,B: Five years after removal the motion is from 20 to 130 degrees. There is no pain and the foramen osteophytes have not recurred.
|
S, Morrey BF, O’Driscoll S. Primary osteoarthritis of the elbow treated
by ulnohumeral arthroplasty: a long term follow-up study. J Bone Joint Surg 2001 (accepted).
M, Kato S, Kashiwagi D. Outerbridge-Kashiwagi’s method for arthroplasty
of osteoarthritis of the elbow: 44 elbows followed for 8–16 years. J Orthop Sci 1996;1:11.
