Dislocations Of The Elbow
injuries involving three separate articulations: the radiocapitellar,
the ulnohumeral, and the proximal radioulnar joints. Dislocations of
the elbow joint in children are not common. Henrikson52
studied 1579 injuries about the elbow in skeletally immature patients
in Gothenburg, Sweden, in 1966, and found only 45 dislocations, for an
overall incidence of 3%. Peak incidence of pediatric elbow dislocations
typically occurred in the second decade of life, usually between 13 and
14 years of age when the physes begin to close. The same second-decade
peak incidence was reported by Josefsson and Nilsson64 in 1986. In their series, most elbow dislocations occurred in conjunction with sports activities.
be considered as either dynamic or static. Dynamic elbow stabilizers
consist of the elbow musculature, over which the patient has conscious
control, which changes depending on the degree of muscular contraction.
Unlike the shoulder, dynamic stabilizers play only a modest role in
elbow stability. One indirect but important role of the elbow
musculature related to elbow stability is determining elbow position in
space at the time of injury. In general, flexion and supination are
positions of stability, while extension and pronation are positions of
relative instability.
The bone geometry of the elbow creates a relatively constrained hinge.
The coronoid and olecranon form a semicircle of approximately 180
degrees into which the trochlea of the humerus securely articulates.
The concave surface of the radial head matches the convex capitellum
and provides stability to the lateral aspect of the elbow joint. The
bony configuration of the medial and lateral aspects of the elbow
complement each other with the ulnohumeral articulation providing
stability
against medial-lateral or longitudinal translation, while the radiocapitellar joint provides resistance to axial compression.
 |
|
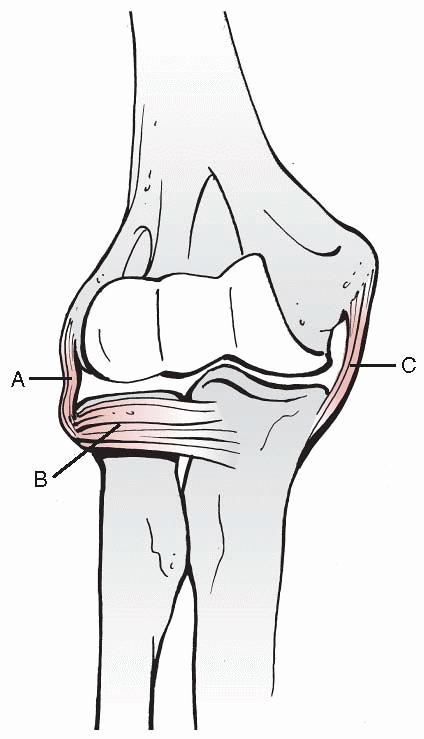
FIGURE 16-1
Anteroposterior view of the elbow illustrates the bone and ligamentous structures which contribute to elbow stability. (A, lateral collateral ligament; B, annular ligament; C, medial collateral ligament.) |
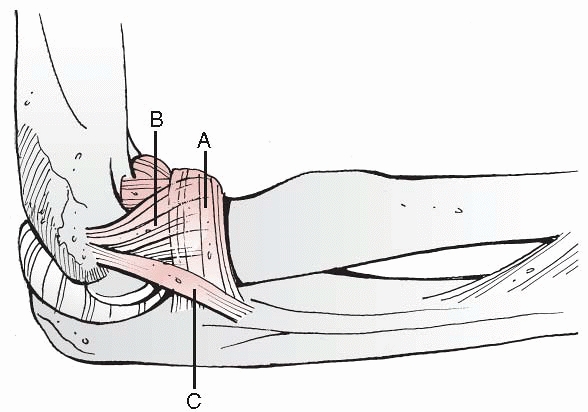
which encircles the radial neck and head, having its origin and
insertion on the proximal ulna. Radial (lateral) collateral ligaments
originate from the lateral epicondyle and insert into the annular
ligament and lateral aspect of the proximal ulna. The primary role of
the annular ligament and lateral collateral ligament complex is to
provide stability to the proximal radiocapitellar and proximal
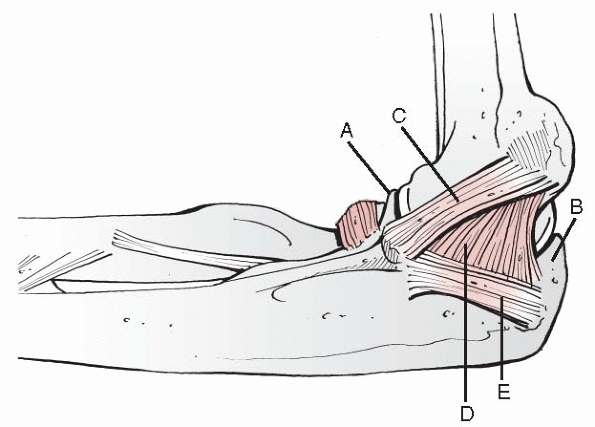
radioulnar joints and to resist varus stress. The ulnar (medial)
collateral ligament resists opening of the medial aspect of the elbow
with valgus stress. Having its origin from the medial epicondyle, the
medial collateral ligament has two primary components that contribute
to elbow stability. The primary stabilizing segment courses from the
medial epicondyle to the coronoid process. A fan-shaped posterior
oblique ligament inserts on the olecranon and functions mainly in
flexion. A small transverse ligament runs from the olecranon to the
coronoid but has little functional importance.
 |
|
FIGURE 16-2
The annular ligament and lateral collateral ligament complex provides stability to the proximal radioulnar joint and radial capitellar articulation. (A, annular ligament; B, lateral collateral ligament insertion on annular ligament; C, lateral collateral ligament inserting on ulna.) |
 |
|
FIGURE 16-3
The medial elbow is stabilized by the hinge articulation between the proximal ulna and the humerus. Three components of the ulnar collateral ligament provide additional elbow stability. (A, coronoid process; B, olecranon process; C, anterior oblique medial collateral ligament; D, posterior oblique medial collateral ligament; E, transverse medial collateral ligament.) |
proximal radioulnar joint relative to the distal humerus: posterior,
anterior, medial, or lateral. Posterior dislocations are further
subdivided into posterolateral and posteromedial displacement.
Occasionally, the proximal radioulnar joint is disrupted. When this
happens, the radius and ulna can diverge from each other. Rarely, the
radius and ulna translocate, with the radius medial and the ulna
lateral. Isolated dislocations of the radial head must be
differentiated from congenital dislocations. Isolated dislocations of
the proximal ulna are exceedingly rare and have not been reported in
children. Included in this chapter is a discussion of the commonly
occurring subluxation of the radial head, or “nursemaid’s elbow.” This
is not a true subluxation but rather a partial entrapment of the
annular ligament in the radiocapitellar joint.
dislocation. The general principles of management include promptly
obtaining a concentric reduction of the elbow joint while identifying
and treating all associated injuries, allowing timely motion and
rehabilitation with the goal of restoring full-elbow motion without
recurrent instability.
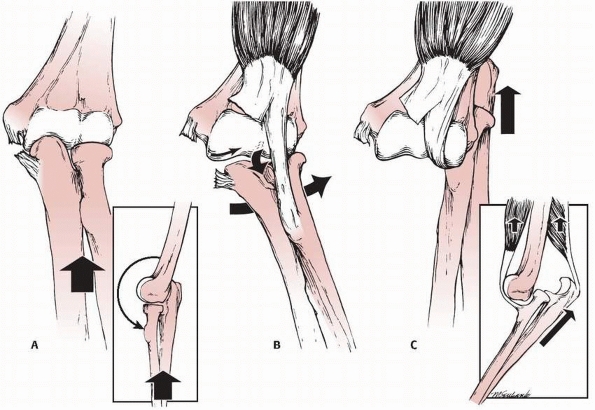
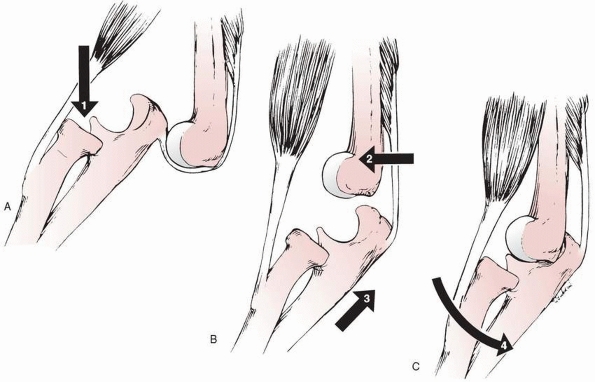
dislocation is a disruption of the ulnar collateral ligaments or
failure of the medial epicondyle apophysis. This produces valgus
instability.
The
proximal radius and ulna displace laterally with the intact biceps
tendon acting as the center of rotation for the displaced forearm (Fig. 16-4).
Application of both abduction and extension forces with anterior soft
tissue disruption results in a posterior or posterolateral elbow
dislocation.100,128
 |
|
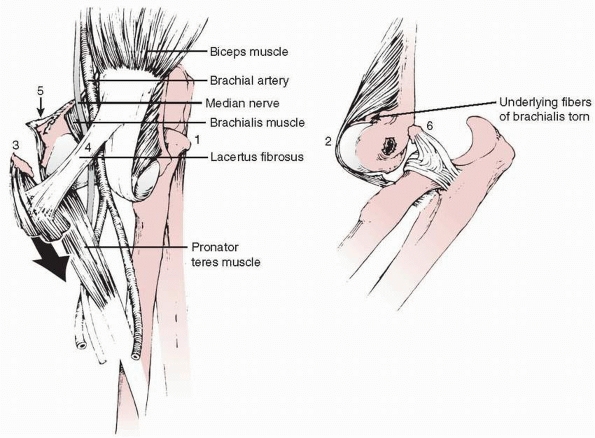
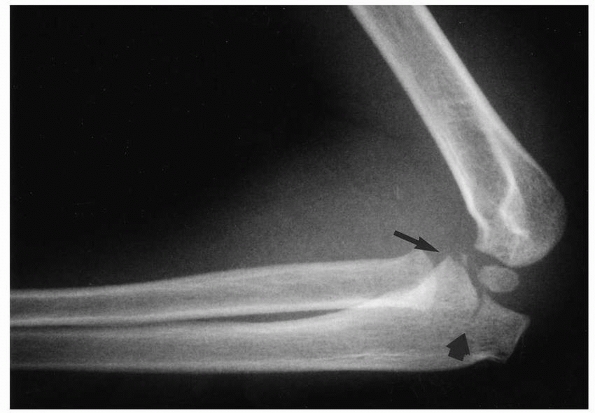
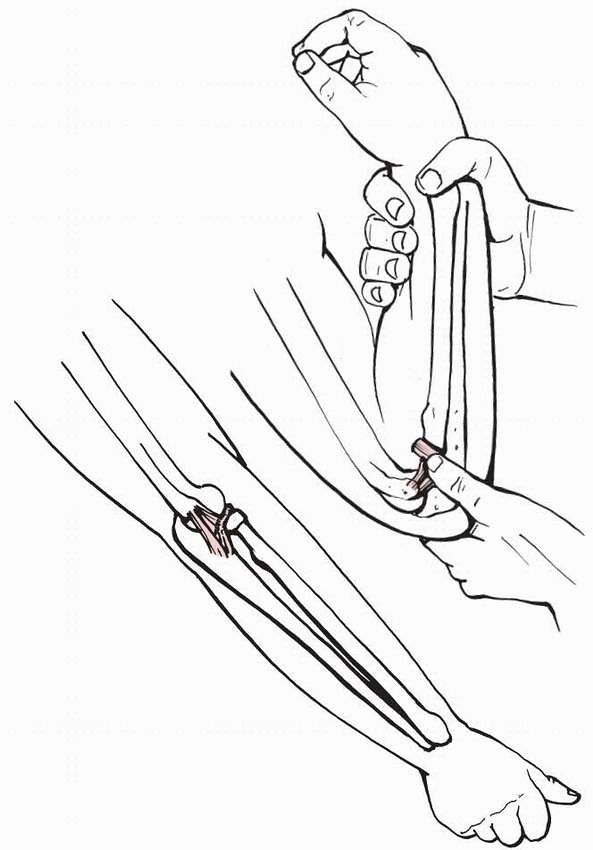
FIGURE 16-4 Mechanism of injury producing a posterior elbow dislocation. A.
The elbow is forced into extension that ruptures the medial collateral ligaments. The normal valgus alignment of the elbow accentuates the valgus force at the elbow. B. The lateral slope of the medial crista of the trochlea forces the proximal ulna posterolaterally (small arrow). The biceps tendon serves as a fulcrum for rotation (medium arrow) leading to valgus hinging (large arrow) of the forearm. C. The proximal ulna and radius are then impacted posteriorly and held against the distal articular surface by the contraction of the biceps and triceps (arrows). |
extension-type supracondylar fracture of the distal humerus. With both
injuries, the elbow is held semiflexed, and swelling may be
considerable. Swelling initially is usually less with a dislocation
than with a type III supracondylar humeral fracture. Crepitus is
usually absent in children with a dislocation and the forearm appears
shortened. The prominence produced by the distal humeral articular
surface is more distal and is palpable as a blunt articular surface.
The tip of the olecranon is displaced posteriorly and proximally so
that its triangular relationship with the epicondyles is lost. The skin
may have a dimpled appearance over the olecranon fossa. If the
dislocation is posterolateral, the radial head also may be prominent
and easily palpable in the subcutaneous tissues.
Fractures involving the medial epicondyle, radial head and neck, and
coronoid process are most common. Fractures involving the lateral
epicondyle, lateral condyle, olecranon, capitellum, and trochlea occur
less frequently.21
tissue injury and can be associated with neurovascular injuries and
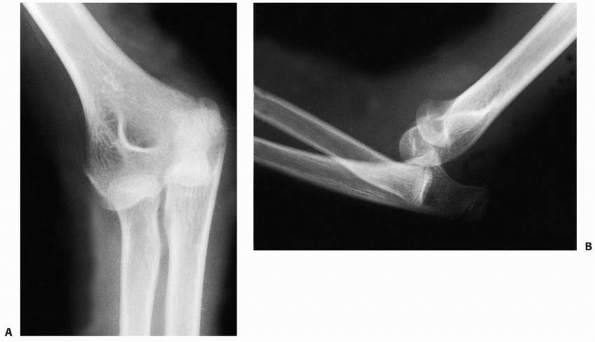
concomitant fractures (Fig. 16-5). The anterior
capsule fails in tension, opening the joint cavity. Radial head
displacement strips the capsule from the posterolateral aspect of the
lateral condyle with the adjacent periosteum. Because of the large
amount of cartilage on the posterolateral aspect of the lateral
condyle, the posterior capsule may not reattach firmly with healing.
This lack of a strong reattachment is believed to be a factor in
recurrent elbow dislocations.101 In a series of 62 adults and adolescents with elbow dislocations requiring surgical treatment, McKee et al.87 reported that disruption of the lateral collateral ligament complex occurred in all 62 elbows.
disrupted either by an avulsion of the medial epicondyle or a direct
tear of the ligament.123,128 Cromack23
found that with medial epicondylar fractures, the origins of the ulnar
collateral ligaments and the medial forearm flexor muscles remain as a
unit, along with most of the pronator teres, which is stripped from its
humeral origin proximal to the epicondyle. These structures are then
displaced posterior to the medial aspect of the distal humerus. The
ulnar collateral ligaments and the muscular origins of the common
flexor muscles tear if the epicondyle remains
attached
to the humerus. With posterolateral displacement of the forearm, the
medial aspect of the distal humerus most often passes into the
intermuscular space between the pronator teres posteriorly and the
brachialis anteriorly. The brachialis, because it has little distal
tendon, is easily ruptured. The rent in the anterior capsule usually is
in this same area.
 |
|
FIGURE 16-5 Injuries associated with elbow dislocation. 1. The radial head and olecranon are displaced posterolaterally. 2. The brachialis muscle is stretched across the articular surface of the distal humerus. 3.
The origins of the medial forearm flexion muscles are either torn or avulsed with the medial epicondyle from the medial condyle. 4. The median nerve and brachial artery are stretched across the medial condyle and held firmly by the lacertus fibrosus. 5. The medial condyle lies in the subcutaneous tissue between the brachialis anteriorly and the pronator teres posteriorly. 6. The lateral (radial) collateral ligaments often avulse a piece of cartilage or bone from the lateral condyle. |
On occasion, the lateral collateral ligament either avulses a small
osteochondral fragment from the lateral epicondyle or tears completely
within its substance.
distal humerus lies subcutaneously between the pronator teres
posteriorly and the brachialis anteriorly. The median nerve and
brachial artery lie directly over the distal humerus in the
subcutaneous tissues. In a cadaver and clinical study by Louis et al.,74
there was a consistent pattern of disruption of the anastomosis between
the inferior ulnar collateral artery and the anterior ulnar recurrent
artery. If the main brachial arterial trunk also is compromised, the
loss of this collateral system can result in the loss of circulation to
the forearm and hand.
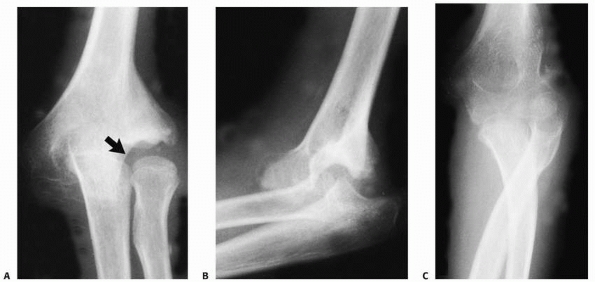
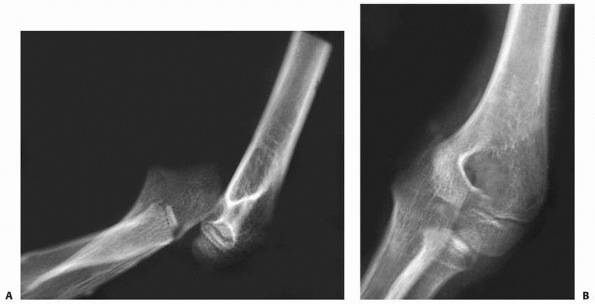
diagnostic of a posterior elbow dislocation. There is a greater
superimposition of the distal humerus on the proximal radius and ulna
in the anteroposterior view. The radial head may be proximally and
laterally displaced, or it may be directly behind the middistal
humerus, depending on whether the dislocation is posterolateral,
posterior, or posteromedial (Fig. 16-6). The
normal valgus angulation between the forearm and the arm usually is
increased. On the lateral view, the coronoid process lies posterior to
the condyles. The x-rays must be examined closely for associated
fractures. Subtle osteochondral fracture fragments can become entrapped
in the joint. If anatomic, congruent reduction is not feasible, and
further evaluation with computerized tomography or magnetic resonance
imaging is utilized to further define complex injury patterns.
dramatic loss of elbow function characterized by loss of motion and
eventually pain (Fig. 16-7). In comparison,
reduction of the dislocated elbow usually achieves marked improvement
of acute pain as well as restoration of long-term function.
reduced spontaneously and closed reduction was successful in 50 cases, but failed in 6 cases (10%). Josefsson et al.63 reported that all 25 dislocations without associated fractures were successfully reduced.
 |
|
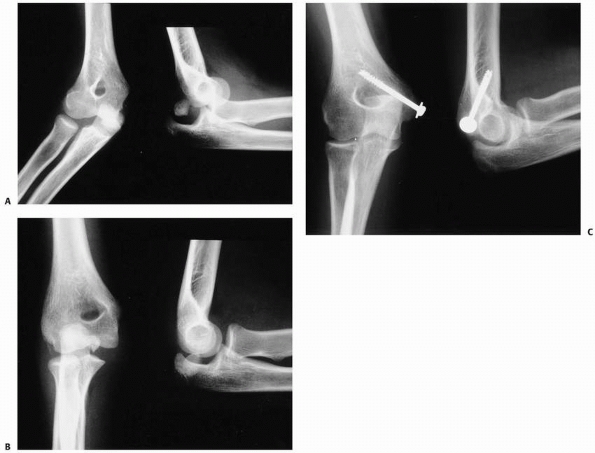
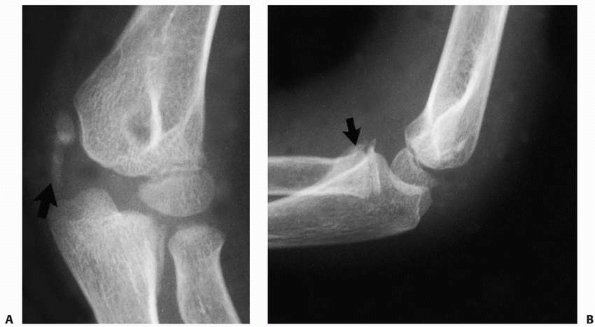
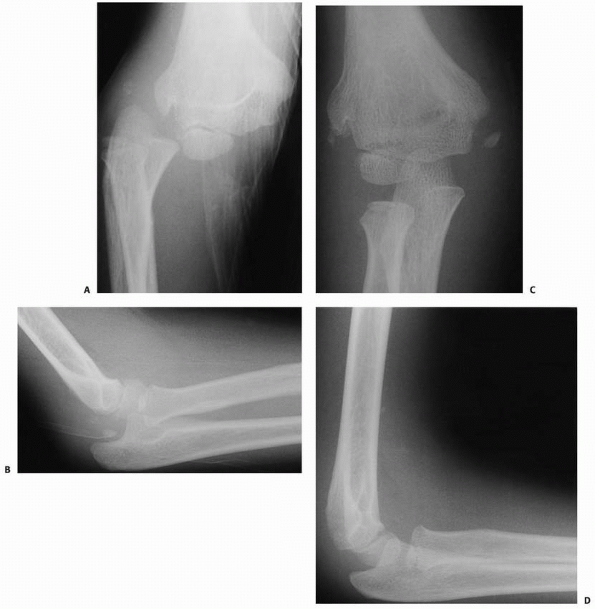
FIGURE 16-6 Radiographic findings. A.
Anteroposterior radiograph. The radial head is superimposed behind the distal humerus. There is increased cubitus valgus. The medial epicondyle has not been avulsed. B. Lateral radiograph demonstrating that the proximal radius and ulna are both displaced posteriorly to the distal humerus. |
injury associated with an elbow dislocation makes it imperative that
the joint be promptly reduced. Royle116 found that dislocations reduced soon after the injury had better outcomes than those in which reduction was delayed.
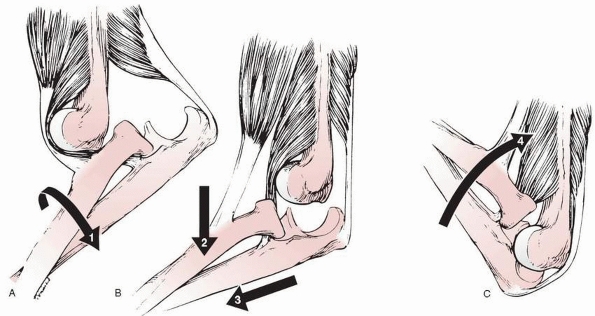
deforming muscle forces so that the coronoid process and the radial
head can slip past the distal end of the humerus. Adequate sedation or
anesthesia is necessary to permit muscle relaxation. Before the primary
reduction forces are applied, the forearm is hypersupinated to dislodge
the coronoid process and radial head from their position behind the
distal humerus and to reduce tension on the biceps tendon.101 The reducing forces are applied in two major directions (Fig. 16-8).
The first reducing force must be along the long axis of the humerus to
overcome the contractions of the biceps and brachialis anteriorly and
the triceps posteriorly. Once these forces are neutralized, the
proximal ulna and radius must be passed from posterior to anterior.
This
requires a second force along the long axis of the forearm. There
appears to be two main philosophies as to the best method of applying
force to counteract the muscles of the arm: the “pullers”10,24,103 (Figs. 16-9, 16-10 and 16-11) and the “pushers”71,91,93 (Fig. 16-12). There also are combined unassisted pusher-puller techniques.46,70
 |
|
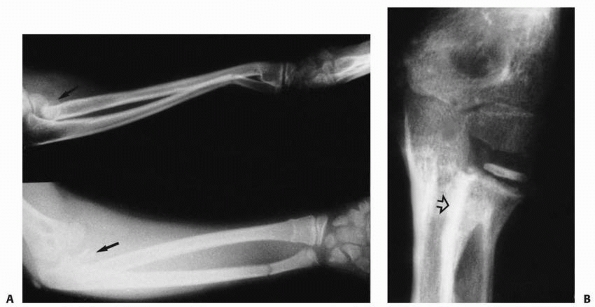
FIGURE 16-7 Unreduced dislocation. A.
Preoperative anteroposterior radiograph. The elbow sustained an injury 3 years before surgery. Elbow motion was extremely limited and painful. The lateral supracondylar ridge had been eroded by the radial head (arrow). B. Lateral radiograph. The posterior position of the olecranon is apparent. C. Anteroposterior radiograph 3 months postoperatively. Total elbow motion was 30 degrees, but there was less pain and more stability. |
 |
|
FIGURE 16-8 Forces required to reduce posterior elbow dislocations. A. The forearm is hypersupinated (arrow 1) to unlock the radial head. B. Simultaneous forces are applied to the proximal forearm along the axis of the humerus (arrow 2) and distally along the axis of the forearm (arrow 3). C. The elbow is then flexed (arrow 4) to stabilize the reduction once the coronoid is manipulated distal to the humerus.
|
 |
|
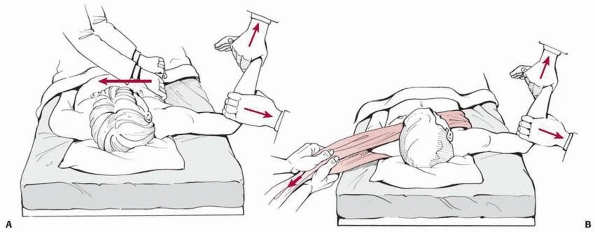
FIGURE 16-9 Reduction by “puller” techniques in a supine position. A.
With the elbow flexed to almost 90 degrees, a force is applied to the anterior portion of the forearm with one hand while the other hand pulls distally along the forearm. A counterforce is applied to offset the manipulating forces by direct stabilization of the patient by a second medical person. B. The counterforce is applied with a sheet around the chest in the ipsilateral axilla. (Redrawn from Parvin RW. Closed reduction of common shoulder and elbow dislocations without anesthesia. Arch Surg 1957;75:972-975, with permission. Copyright 1957, American Medical Association.)15 |
demonstrated that when the coronoid process is locked against the
posterior aspect of the humerus and the elbow is extended, the force
applied to the anterior muscles is multiplied by as much as five times
because of the increased
leverage. This places a marked strain on the injured anterior capsule and the brachialis muscle (Fig. 16-13).
By contrast, when the distal force is applied to the proximal forearm
with the elbow flexed, the force exerted against the muscles across the
elbow is equal to the distracting force. For patients with
posterolateral dislocations, the lateral displacement of the proximal
radius and ulna must first be corrected to prevent the median nerve
from being entrapped or injured during reduction.11,16 Hyperextension reduction puts the median nerve more at risk for entrapment.
 |
|
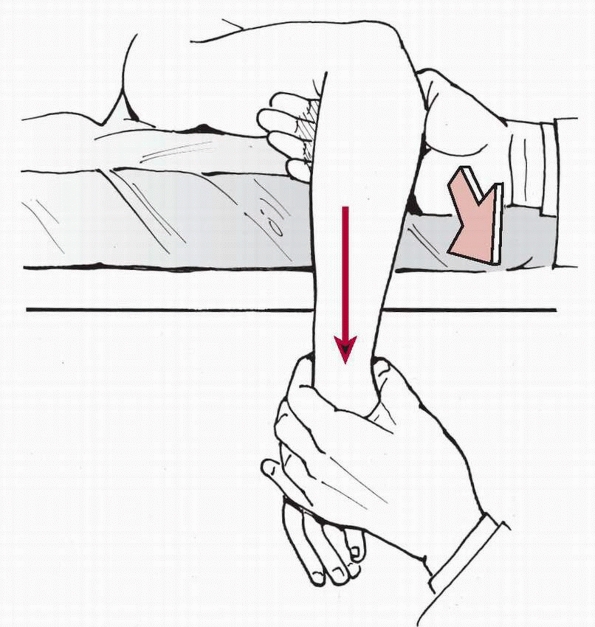
FIGURE 16-10
Reduction by “puller” technique in a prone position. The same forces are applied to the proximal portion of the anterior forearm and distal forearm as in the supine position. The table provides a counterforce against the anterior portion of the distal humerus when the patient is prone. |
determine and document the stability of the elbow by examination while
the patient is under sedation. A concentric reduction must be
documented in all cases. Some type of immobilization, usually a
posterior splint, is advocated by most investigators. A frequently
recommended period of immobilization is 3 weeks,72,73,103,125 although some have advocated early motion.115,116,147
In a recent study of 42 adult patients comparing 2 weeks of cast
immobilization with the use of a simple arm sling and early motion,
Maripuri et al.83 demonstrated
improved early and final functional outcomes in the early mobilization
group compared to the group placed in a cast following reduction.
O’Driscoll et al.100 suggested that
if the elbow was stable in response to valgus stress with the forearm
pronated then the anterior portion of the medial collateral ligament
was intact and the patient could begin early motion. Ninety degrees of
elbow flexion appears to be the standard position of immobilization.
inability to obtain a concentric closed reduction, an open dislocation,
and a displaced osteochondral fracture.
Adults with posterior elbow dislocations without concomitant fracture
have no better function or stability following a primary ligamentous
repair than those treated nonoperatively.61,62 Excellent results have been reported by Josefsson et al.63 in 28 children and adolescents with simple posterior dislocations treated nonoperatively.
Operative intervention is necessary in open posterior dislocations to
irrigate and débride the open wound and elbow and to evaluate the
brachial artery. If there is vascular disruption, most advocate
vascular repair or reconstruction with a vein graft even in the
presence of adequate capillary refill. This lessens the risk of late
cold intolerance, dysesthesias, or dysvascularity.
can have an associated fracture of the coronoid, lateral condyle,
olecranon (Fig. 16-14), or medial epicondyle (Fig. 16-15).
Recently, fracture of the anteromedial facet of the coronoid has been
recognized as an important injury associated with elbow dislocations in
adolescents and adults.31,32 The presence of a concomitant displaced fracture is a common indication for surgical intervention.21,38,142 Surgery for associated fractures produced better results than nonoperative treatment in the series of Carlioz and Abols,21 and similar results were reported by Wheeler and Linscheid.142
Repair of an associated medial epicondylar fracture may also improve
elbow stability in throwing athletes when the injury is in the dominant
arm.123,147
Entrapment of a displaced medial epicondylae fracture within the joint
after reduction is an absolute indication for surgical treatment (see Fig. 16-15).
Ultimately, the of surgical treatment for fractures associated with an
elbow dislocation is based on the circumstances surrounding each
individual patient. Factors favoring operative treatment include older
patient age, instability of the elbow during examination under sedation
at the time of reduction, the presence of a displaced intra-articular
fracture, injury to multiple elbow stabilizers, injury to the patient’s
dominant arm, and anticipated significant sports or activity demands on
the elbow.
on the procedure performed. After open reduction, management is similar
to that after satisfactory closed reduction. The length of
immobilization for fractures is up to 3 to 4 weeks. Protected arc of
motion with a hinged brace or intermittent splinting is utilized
frequently to lessen the risk of posttraumatic contracture.
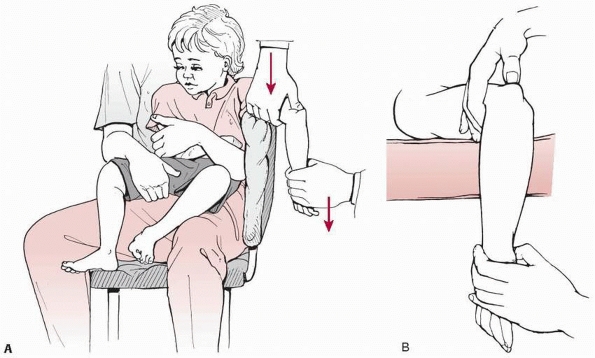
dislocation is preferred in children 9 years of age or younger. In this
age group, the child often can be seated comfortably in the parent’s
lap (see Fig. 16-12). Hanging the arm over the back of a well-padded chair may provide some stabilization.
The forearm must remain supinated during the process of reduction.
Occasionally, it is necessary to hypersupinate the forearm to unlock
the coronoid process and radial head before reduction. Closed reduction
is done with either heavy sedation or general anesthesia. X-rays are
obtained after the manipulation to assess the adequacy of the reduction
(see Fig. 16-11)
and to be certain the joint is congruently reduced. The elbow is
immobilized in a posterior splint with the elbow flexed 90 degrees. If
there is a question of persistent instability, the forearm is held in
full supination. If the elbow is absolutely stable following reduction,
the forearm can be immobilized in midpronation to allow the patient to
be more functional in the splint.
stiffness, the splint is removed after approximately 1 week and the
patient begins intermittent active elbow motion. The patient can
discard the splint and use a sling after 10 to 14 days. The emphasis is
on early active motion to prevent stiffness that often occurs after
this injury. Before reduction, it is important to emphasize to the
parents that there may be some loss of motion, especially extension,
regardless of the treatment. This is usually less than 30 degrees and
not of functional or cosmetic significance.
after the reduction with special attention to the median nerve in terms
of entrapment. This same careful examination must be made at all
follow-up evaluations. Persistent median nerve motor-sensory loss
associated with severe pain and resistance with elbow flexion-extension
arc of motion may be indicative of entrapment. Of note, ulnar
neuropathy is not uncommon and usually resolves spontaneously.
 |
|
FIGURE 16-11 Closed reduction. A. Anteroposterior radiograph of a 9-year-old girl with a posterior dislocation of the right elbow. B. Lateral radiograph shows the proximal radius and ulna posterior to the distal humerus. C. There is a concentric reduction following closed reduction using a puller technique. D. Lateral radiograph.
|
 |
|
FIGURE 16-12 Reduction by “pusher” techniques. A.
Lavine’s method. The child is held by the parent while the elbow is draped over the edge of the chair. The olecranon is pushed distally past the humerus by the thumb of the physician while the other arm pulls distally along the axis of the forearm. B. Meyn’s technique with patient lying prone on the table. (Redrawn from Meyn MA, Quigley TB. Reduction of posterior dislocation of the elbow by traction on the dangling arm. Clin Orthop 1974;103:106-107, with permission.) |
always be done with adequate analgesia, sedation, or anesthesia. In
addition to making the experience much less frightening and traumatic
for the child, adequate analgesia, sedation, or anesthesia will achieve
sufficient muscle relaxation for the reduction to be obtained more
effectively with less force, thereby reducing the risk of creating an
iatrogenic fracture (such as fracture of the radial neck) during
reduction.
 |
|
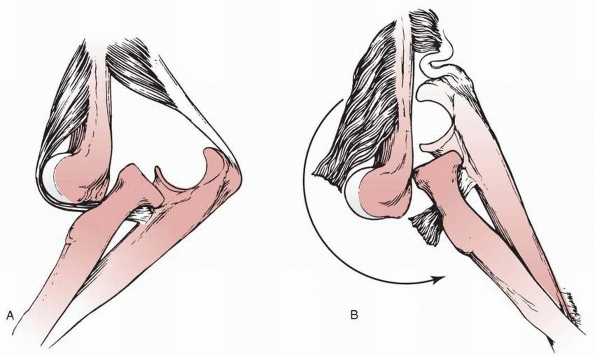
FIGURE 16-13 Hyperextension forces. A. The brachialis is stretched across the distal humerus. B.
Hyperextending the elbow before it is reduced greatly increases the arc of motion and leverage placed across the brachialis. This can result in rupture of large portions of the muscle. (Reprinted from Loomis LK. Reduction and aftertreatment of posterior dislocation of the elbow. Am J Surg 1944;63:56-60, with permission.) |
dislocations can be divided into those occurring early and those
occurring later. Early complications include neurologic and vascular
injuries. Late complications include loss of motion, myositis
ossificans, recurrent dislocations, radioulnar synostosis, and cubitus
recurvatum. The special problems of chronic, unreduced dislocations are
not considered complications of treatment.
 |
|
FIGURE 16-14 Lateral radiograph of a 4–year-old child who sustained an elbow dislocation with a concomitant olecranon fracture (large arrow) and a coronoid fracture (small arrow).
|
the most commonly injured nerve was the ulnar nerve. Of the 32 patients
(10%) who had nerve symptoms after reduction, 21 had isolated ulnar
nerve injuries, 7 had isolated median nerve injuries, and in 4 patients
both the median and ulnar nerves were involved. Linscheid and Wheeler72
recommended ulnar nerve transposition if ulnar nerve symptoms were
present in a patient undergoing open reduction and internal fixation of
a displaced medial epicondylar fracture. Except for the one patient
described by Linscheid and Wheeler,72 the reported ulnar nerve injuries were transient and resolved completely.
 |
|
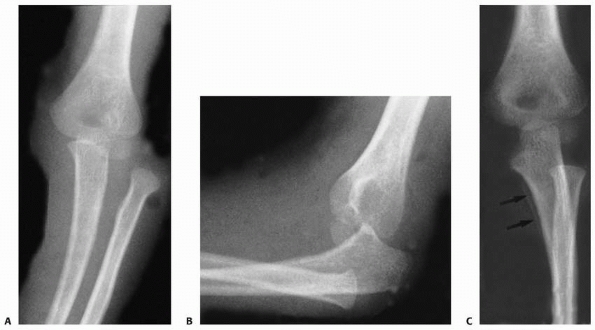
FIGURE 16-15 A.
Anteroposterior and lateral radiograph of a 14-year-old male who sustained an elbow dislocation with an ipsilateral medial epicondyle fracture. B. Anteroposterior radiographs after a closed reduction. Note the entrapment of the medial epicondyle in the joint. C. This patient was treated with an open reduction to extract the medial epicondyle from the joint and an internal fixation using a cannulated screw that allowed rapid mobilization of his elbow. |
reported two radial nerve injuries associated with elbow dislocation;
in both the symptoms rapidly resolved after reduction. Rasool111 reported a third case.
involves the median nerve, which can be damaged directly by the
dislocation or can be entrapped within the joint. Median nerve injuries
occur most commonly in children 5 to 12 years of age. There were seven
median and four median-ulnar nerve injuries (3%) in the combined series.72,97,114,116
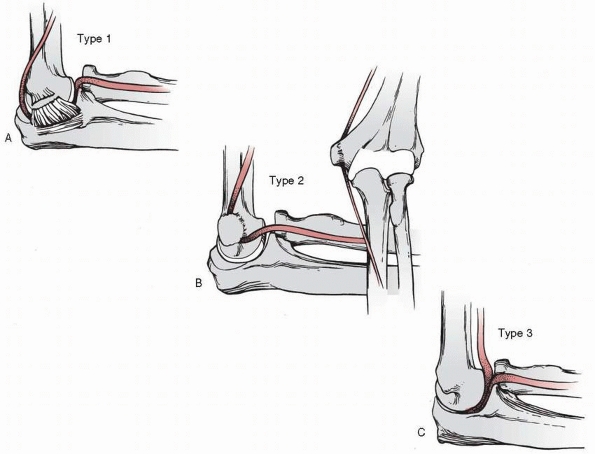 |
|
FIGURE 16-16 Median nerve entrapment. A. Type 1. Entrapment within the elbow joint with the median nerve coursing posterior to the distal humerus. B. Type 2. Entrapment of the nerve between the fracture surfaces of the medial epicondyle and the medial condyle. C.
Type 3. Simple kinking of the nerve into the anterior portion of the elbow joint. (Redrawn from Hallett J. Entrapment of the median nerve after dislocation of the elbow. J Bone Joint Surg Br 1981;63: 408-412, with permission.) |
avulsion of the medial epicondyle or has a rupture of the medial
muscles at their origin and the ulnar collateral ligaments (see Fig. 16-16A).
This allows the median nerve, with or without the brachial artery, to
displace posteriorly. The nerve is especially prone to being entrapped
between the trochlea and the olecranon during the process of reduction
if the lateral displacement of the proximal radius and ulna is not
corrected before reduction. Hallett45
demonstrated in cadavers that pronation of the forearm while the elbow
is hyperextended forces the median nerve posteriorly during the process
of reduction making it vulnerable to entrapment. This type of
entrapment also has been reported by other authors.8,11,16,36,42,84,107,110,132
Delay in diagnosis is common. In some patients with an associated
medial epicondylae fracture, the nerve can be so severely damaged after
being entrapped that neuroma resection and either nerve transposition
and direct repair or grafting is necessary.11,42,84 Good recovery of nerve function has been reported.
This represents a depression on the posterior surface of the medial
epicondylar ridge where the nerve has been pressed against the bone.8,25,42,45,107,110,132 This groove is seen on x-ray as two sclerotic lines parallel to the nerve (Fig. 16-17). This sign disappears when the nerve has been decompressed.
This may or may not be visible on x-ray. The medial epicondyle is
osteomized to free the nerve. Again, decompression alone may be
adequate treatment, although neuroma resection and repair or
reconstruction with nerve grafts may be necessary.
described a fourth type of median nerve entrapment in a 14-year-old boy
who had a posterior elbow dislocation with a medial epicondylar
fracture. The median
nerve
was found entrapped in a healed medial epicondylar fracture (type 2) in
an anterior to posterior direction 18 months after injury. The nerve
then passed through the elbow joint in a posterior to anterior
direction (type 1). The nerve was so severely damaged that it had to be
resected and repaired with sural nerve grafts. A second type 4 median
nerve entrapment also requiring nerve segment resection and grafting
was reported by Ozkoc et al.102
 |
|
FIGURE 16-17
The Matev sign suggesting entrapment of the median nerve in the elbow joint and impingement of the nerve against the posterior surface of the medial condyle. This produces a depression with sclerotic margins. (Redrawn from Matev I. A radiographic sign of entrapment of the median nerve in the elbow joint after posterior dislocation. J Bone Joint Surg Br 1976;58:353-355, with permission.) |
epicondyle and significant median nerve dysfunction was cited by Rao
and Crawford110 as an absolute
indication for surgical exploration of the nerve because of the
frequency of median nerve entrapment with fractures of the medial
epicondyle (types 1 and 2). Magnetic resonance imaging (MRI) may be
helpful in defining the course of the median nerve if entrapment is
suspected.2 Electromyography and
nerve conduction studies have been utilized to assist in operative
decision making. Painful dysesthesias with arc of motion is usually
indicative of entrapment. Once the entrapped nerve is removed from the
joint, neurologic function typically improves. Resection and repair or
nerve grafting are may be necessary.
dislocations in children and adolescents with only eight vascular
injuries (3%) reported in the combined series of 317 patients.72,97,114,116 However, Carlioz and Abols21
reported 4 patients with diminished radial pulses that resolved after
reduction. Arterial injuries have been associated with open
dislocations in which collateral circulation is disrupted.50,66,74,117 In these situations, usually the brachial artery is ruptured,44,50,54,66,74,81 but it also can be thrombosed144 as well as entrapped in the elbow joint.51,104,144 Pearce104
reported an entrapped radial artery in which there was a high
bifurcation of the brachial artery. When there is a complete rupture,
there usually is evidence of ischemia distally. However, the presence
of good capillary circulation to the hand or a Doppler pulse at the
wrist does not always mean the artery is intact.44,54
Arteriograms usually are not necessary because the arterial injury is
at the site of the dislocation. If imaging is indicated to evaluate
possible arterial injury, its minimal risk and invasiveness make
vascular ultrasound an attractive initial imaging choice.
dislocation which returns the displaced brachial vessels to their
normal position51,144
and operative repair of those that are ruptured or severely damaged.
Ligation of the ends has been done in the past with adults, especially
if there was good capillary circulation distally,50,66
but this may predispose to late ischemic changes such as claudication,
cold sensitivity, or even late amputation. Most investigators recommend
direct arterial repair or a vein graft.44,54,74,81,117 Louis et al.74
recommended arterial repair because their cadaver studies demonstrated
that a posterior elbow dislocation usually disrupted the collateral
circulation necessary to maintain distal blood flow.
and usually is no more than 10 degrees of extension. This rarely is of
functional or cosmetic significance. However, this potential for loss
of motion must be explained to the parents before reduction and may be
an indication for a supervised rehabilitation program. If there is
displaced medial epicondylar nonunion, the loss of major range of
motion can be severe and limiting. Similarly, an incongruent elbow
joint will have marked limitations of motion.
heterotopic calcification, which is a dystrophic process. Myositis
ossificans involves ossification within the muscle sheath that can lead
to a significant loss of range of motion of the elbow. Disruption of
the brachialis muscle is believed to be a contributory factor.73 Fortunately, myositis ossificans is rare in children.63,136 Although heterotopic calcification in the ligaments and capsule of the elbow is common,63,114 it rarely results in loss of elbow function (Fig. 16-18).
differentiated true myositis ossificans from heterotopic calcification
in his series of 60 elbow dislocations, and noted that only 3 patients
had true myositis ossificans. Linscheid and Wheeler72
reported that the incidence of some type of heterotopic calcification
was 28%, which was most common around the condyles. Only in five
patients was it anterior to the capsule (which probably represented
true myositis ossificans in the brachialis muscle). Four of these
patients had some decrease in elbow function. Josefsson et al.63
reported that 61% of 28 children with posterior dislocations had
periarticular calcification, but this did not appear to be functionally
significant.
radial neck, the incidence of a secondary proximal radioulnar
synostosis is increased (Fig. 16-19). This can occur regardless of whether the radial neck fracture is treated operatively or nonoperatively.16,21,100 Carlioz and Abols21 reported a synostosis in 1 of 3 patients with posterior elbow dislocations associated with radial neck fractures.
significant tearing of the anterior capsule. As a result, after
reduction, when all the stiffness created by the dislocation has
subsided, the patient may have some hyperextension (cubitus recurvatum)
of the elbow. This usually is minimally symptomatic but if asymmetric,
may be cosmetically disturbing to the parents and adolescent.
combined series of dislocations, only 2 of 317 patients (0.6%)
experienced recurrent dislocations.72,97,114,116 Approximately 80% of recurrent dislocations are in males. Three investigators have reported bilateral cases.65,92,112
all of collateral ligament instability, capsular laxity, and bone and
articular cartilage defects.
 |
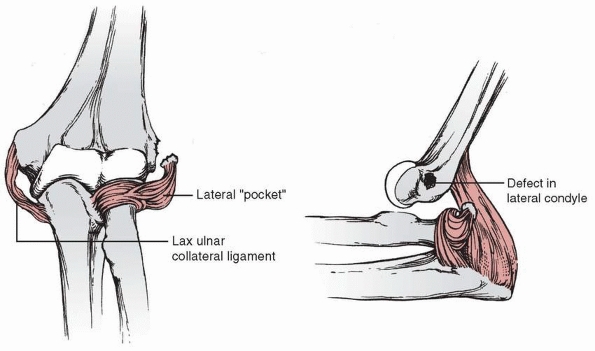
|
FIGURE 16-18 A. Heterotopic calcification of the ulnar collateral ligaments in an elbow that had been dislocated for 2 months (arrow). B.
Lateral view of the same elbow. Some myositis ossification has occurred where the brachialis inserts into the coronoid process (arrow). |
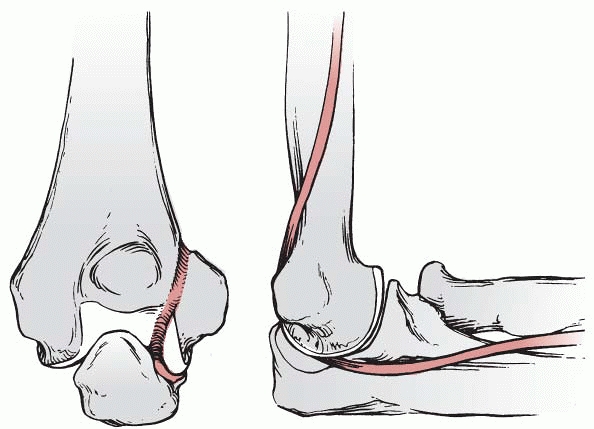
suggested that articular changes are secondary and that the primary
defect is a failure of the posterolateral ligamentous and capsular
structures to become reattached after reduction (Fig. 16-20). Osborne and Cotterill101
proposed that the extensive articular cartilage covering the surface of
the distal humerus leaves little surface area for soft tissue
reattachment and the presence of synovial fluid further inhibits soft
tissue healing. With recurrent dislocations, the radial head impinges
against the posterolateral margin of the capitellum, creating an
osteochondral defect (Fig. 16-21). In addition
to the defect in the capitellar articular surface, a similar defect
develops in the anterior articular margin of the radial head. When
these two defects oppose each other, recurrence of the dislocation is
more likely. Subsequent studies have confirmed these findings in almost
all recurrent dislocations, especially in children.33,49,99,133,138,146
 |
|
FIGURE 16-19 Radioulnar synostosis. A.
Injury radiographs demonstrating a posterolateral dislocation associated with a Salter-Harris type II proximal radius fracture (arrow). Open reduction of the proximal radial fracture was performed. B. Six months later, the patient developed a proximal radioulnar synostosis (arrow). (Courtesy of Ruben Pachero, MD.) |
described posterolateral instability in 5 patients, including 2
children, in whom laxity of the ulnar part of the radial collateral
ligament allowed a transitory rotary subluxation of the ulnohumeral
joint and a secondary dislocation of the radiohumeral joint. Patients
with posterolateral instability often describe a history of recurrent
temporary dislocation of the elbow but, when examined, exhibit no
unusual clinical findings. The instability is diagnosed with a
posterolateral rotary instability test. In some patients,
posterolateral rotary instability can be detected only with the patient
completely relaxed under general
anesthesia.
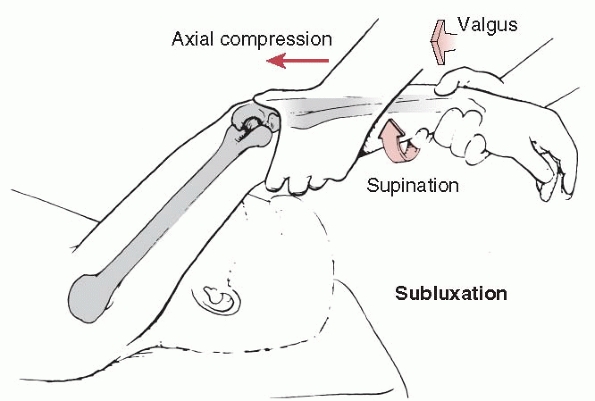
This test is done by holding the patient’s arm over the head while
applying proximal axial compression plus a valgus and supination force
to the forearm with the elbow flexed to 20 to 30 degrees (Fig. 16-22). O’Driscoll et al.99
reported that surgical repair of the lax ulnar portion of the radial
collateral ligament eliminated the posterolateral rotary instability.
In children and adolescents, the same instability can occur from
cartilage nonunion of the origin of the radial collateral ligament.
 |
|
FIGURE 16-20
Pathology associated with recurrent elbow dislocations. The three components that allow the elbow to dislocate: a lax ulnar collateral ligament, a “pocket” in the radial collateral ligament, and a defect in the lateral condyle. (Reprinted from Osborne G, Cotterill P. Recurrent dislocation of the elbow. J Bone Joint Surg Br 1966;48: 340-346, with permission.) |
 |
|
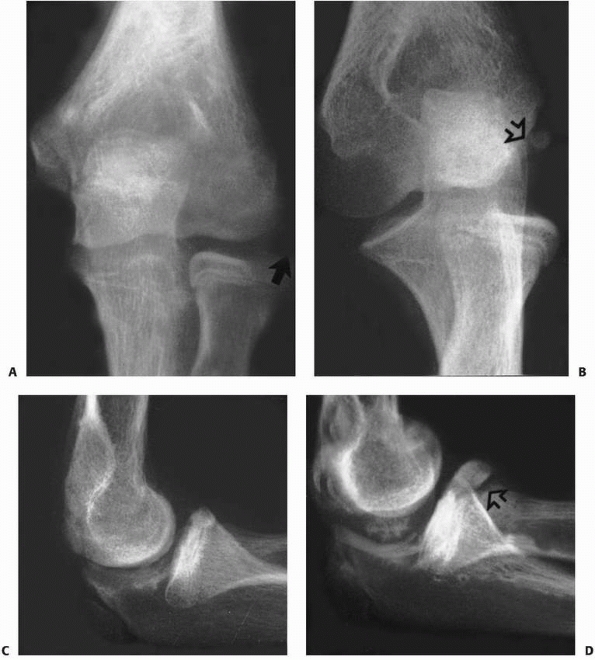
FIGURE 16-21 Radiographic changes associated with recurrent elbow dislocation. A. Anteroposterior radiograph of a 13-year-old who had recurrent dislocations. An osteochondral fragment (arrow) is attached to the lateral ligament. B. An oblique radiograph shows the defect (arrow) in the posterolateral condylar surface. C. Radiographs of an 11-year-old after his first dislocation. D. One year later, after recurrent dislocation and subluxations, blunting of the radial head has developed (arrow). (Courtesy of Marvin E. Mumme, MD.)
|
 |
|
FIGURE 16-22
Posterolateral rotary instability. Posterolateral rotational instability is best demonstrated with the upper extremity over the head with the patient supine. The radial head can be subluxated or dislocated by applying a valgus and supination force to the forearm at the same time proximal axial compression is applied along the forearm. (Reprinted from O’Driscoll SW, Bell DF, Morrey BF. Posterolateral rotary instability of the elbow. J Bone Joint Surg Am 1991;73:441, with permission.) |
 |
|
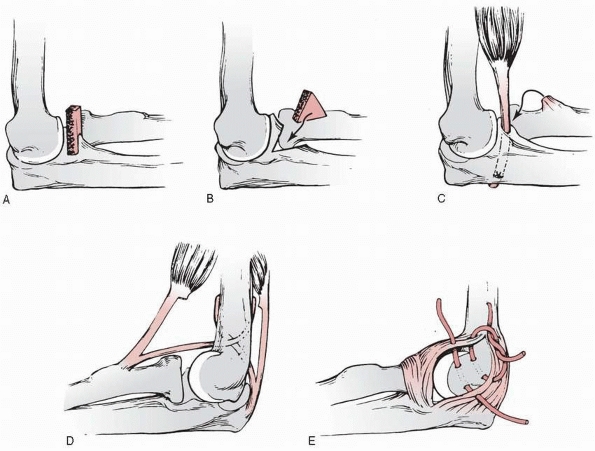
FIGURE 16-23 Surgical procedures for recurrent dislocation. A. Simple coronoid bone block. B. Open wedge coronoid osteotomy. C. Biceps tendon transfer to coronoid process. D. Cruciate ligament reconstruction. E. Lateral capsular reattachment of Osborne and Cotterill.101
|
in the capitellum and radial head, bone defects may include a shallow
semilunar notch resulting from a coronoid fossa process fracture or
multiple recurrent dislocations.
used an orthosis that blocked the last 15 degrees of extension. After
his patient wore this orthosis constantly for 2 years and with vigorous
activities for another 6 months, there were no further dislocations,
but the follow-up period was only 1 year. Beaty and Donati9 emphasized that physical therapy and the use of an orthosis should be tried before surgery is considered.
posterior elbow dislocations is predominately surgical. Various
surgical procedures have been described to correct bone and soft tissue
abnormalities (Fig. 16-23).
reinforce it (Fig. 16-23C). Kapel65
developed a cruciate ligament reconstruction in which distally based
strips of the biceps and triceps tendon were passed through the distal
humerus (Fig. 16-23D). Beaty and Donati9
modified this technique by transferring a central slip of the triceps
through the humerus posterior to anterior and attaching it to the
proximal ulna.
 |
|
FIGURE 16-24 Effects of recurrent dislocation. This girl began to have recurrent dislocations of her elbow at age 9. A. The ease at which the elbow redislocates is shown in this radiograph. B,C. Radiographs taken at the beginning of episodes of dislocation. Her dislocation continued. D,E. Four years later, the elbow demonstrated marked changes in its architecture. (Courtesy of David J. Mallams, MD.)
|
in which the lateral capsule is reattached to the posterolateral aspect
of the capitellum with sutures passing through holes drilled in the
bone (Fig. 16-23E). The joint should be inspected at surgery because osteocartilaginous loose bodies may be present.49,80,133 Since Osborne and Cotterill’s101 initial report of eight patients, successful use of this technique has been reported in numerous others.33,49,80,99,133,138,146 Zeier148 and O’Driscoll et al.99 reinforced the lateral repair with strips of fascia lata, triceps fascia, or palmaris longus tendon.
the arm is immobilized in a long arm cast with the elbow flexed 90
degrees for 4 to 6 weeks. Protected active range of motion exercises
are performed for an additional 4 to 6 weeks. Strenuous activities are
avoided for 12 weeks postoperative.
dislocations include loose osteocartilaginous fragments and destruction
of the articular surface of the joint (Fig. 16-24), elbow stiffness, or recurrent instability.
children are extremely rare in North America. Most reported series are
from other countries.37
Pathologically, there is usually subperiosteal new bone formation that
produces a radiohumeral horn, myositis ossificans of the brachialis
muscle, capsular contractures, shortening of the triceps muscle,
contractures of the medial and lateral collateral ligaments, and
compression of the ulnar nerve.36,37 These factors have to be considered when planning treatment.
reduction is achieved within 3 months of the initial dislocation.4 Results after surgical reconstruction decline thereafter but still may produce some improvement in function.30,37,78,90,94
Fixation of the elbow joint to maintain reduction with one or two large
smooth pins for 2 to 4 weeks followed by vigorous but protected
physical therapy has been recommended.37,94
reported improved extension and better functional results 1 to 3 months
after injury in 34 patients with chronic elbow dislocation
reconstruction in whom the triceps tendon was not lengthened compared
with 38 patients who had the triceps lengthened at surgery.
Altered anatomy and limited motion predispose these patients to injury.
The key to differentiating a congenital from an acute traumatic elbow
dislocation is examination of the x-ray architecture of the
articulating surfaces. In a congenitally dislocated elbow, there is
atrophy of the humeral condyles and the semilunar notch of the
olecranon. The radial head and neck may be hypoplastic, and the
articular surface of the radial head may be dome-shaped instead of
concave. Unfortunately, these same changes can result from chronic
recurrent dislocation after trauma, making the differentiation between
congenital and chronic traumatic dislocation difficult. If other
congenital anomalies are present or the child has an underlying
syndrome, such as Ehlers-Danlos or Larsen syndrome, the dislocation is
likely to be congenital. Obtaining comparison x-rays of the
asymptomatic, contralateral elbow often reveals identical anatomy,
confirming the etiology of the dislocation as congenital.
only five were anterior, for an incidence of slightly over 1%. They are
associated with an increased incidence of complications, such as
brachial artery disruption and associated fractures, compared with
posterior dislocations.59,143
 |
|
FIGURE 16-25 Anterior dislocation of the elbow. A. Initial anteroposterior radiograph. The olecranon lies anterior to the distal humerus. B.
Initial lateral radiograph. The proximal ulna and radial head lie anteromedial, and the elbow carrying angle is in varus. (Courtesy of Hilario Trevino, MD.) |
is a fullness in the antecubital fossa. Swelling usually is marked
because of the soft tissue disruption associated with this type of
dislocation. There is severe pain with attempted motion. A careful
neurovascular examination is mandatory.
diagnostic. In most cases, the proximal radius and ulna dislocate in an
anteromedial direction (Fig. 16-25). Associated
fractures are common. In children, the triceps insertion may be avulsed
from the olecranon with a small piece of cortical bone.145 This fragment usually reduces to the olecranon after reduction. Wilkerson143 reported an anterior dislocation associated with a displaced olecranon fracture in a 7-year-old boy. Inoue and Horii57
reported an 11-year-old girl with an anterior elbow dislocation with
displaced fractures of the trochlea, capitellum, and lateral
epicondyle. These were repaired with open reduction and internal
fixation using Herbert bone screws.
time.145
As with posterior dislocations, a force must first be applied
longitudinally along the axis of the humerus with the elbow semiflexed
to overcome the forces of the biceps and triceps. The longitudinal
force along the axis of the forearm is directed toward the elbow (Fig. 16-26).
To make reduction easier, the distal humerus can be forced in an
anterior direction by pushing on the posterior aspect of the distal arm.
 |
|
FIGURE 16-26 Reduction of anterior dislocation. A. With the elbow semiflexed, a longitudinal force is applied along the long axis of the humerus (arrow 1). Pulling distally on the forearm may be necessary to initially dislodge the olecranon. B. Once the olecranon is distal to the humerus, the distal humerus is pushed anteriorly (arrow 2) while a proximally directed force is applied along the long axis of the forearm (arrow 3). C. Finally, the elbow is immobilized in some extension (arrow 4).
|
is open, there is a brachial artery injury, or there is an associated
fracture that does not realign satisfactorily after closed reduction.
Open reduction and internal fixation of the fracture may then be
necessary.57,143
elbow should be immobilized in some extension for 1 to 3 weeks,
followed by protected active range-of-motion exercises. Early motion
after open reduction and internal fixation of an associated olecranon
fracture usually can be allowed.57,143
is the initial procedure of choice. A distal force must be applied in
line with and parallel to the long axis of the humerus first. Once the
length has been re-established, a posteriorly directed force along the
axis of the forearm is applied until the elbow is reduced.
either incomplete or complete, are more common than medial dislocations
in adults. There are no recent reports of medial dislocations in
children.
notch articulates with the captilulo-trochlear groove, and the radial
head appears more prominent laterally. There often is good flexion and
extension of the elbow, increasing the likelihood that a lateral
dislocation will be overlooked. In a complete lateral dislocation, the
olecranon is displaced lateral to the capitellum. This gives the elbow
a markedly widened appearance.
 |
|
FIGURE 16-27 Lateral elbow dislocation. A. Initial anteroposterior radiograph in this 6-year-old with a lateral dislocation and displaced medial epicondyle fracture. B. Lateral radiograph shows slight posterior dislocation. C,D. Postreduction radiographs demonstrate anatomic reduction of the dislocation. The medial epicondyle is satisfactorily aligned.
|
A longitudinal force is applied along the axis of the humerus to
distract the elbow, and then direct medial or lateral pressure
(opposite the direction of the dislocation) is applied over the
proximal forearm (Fig. 16-27).
dislocation with disruption of the interosseous membrane between the
proximal radius and ulna with the radial head displaced laterally and
the proximal ulna medially (Fig. 16-28). These dislocations are extremely rare.7,19,29,56,55,86,95,125,129,139
trauma. Associated fractures of the radial neck, proximal ulna, and
coronoid process are common.1,19,35,139
It has been speculated that, in addition to the hyperextension of the
elbow that produces the dislocation, a strong proximally directed force
is applied parallel to the long axis of the forearm, disrupting the
annular ligament and interosseous membrane and allowing the divergence
of the proximal radius and ulna. In a cadaveric study, Altuntas et al.5
confirmed that only after release of all the ligamentous stabilizers of
the elbow and release of the intraosseous membrane from the elbow to
the distal third of the forearm could a divergent dislocation be
replicated.
 |
|
FIGURE 16-28 Medial-lateral divergent dislocation. A. Anteroposterior view demonstrating disruption of the proximal radioulnar joint with the radius lateral and the ulna medial. B. Lateral radiograph confirms that the radius and ulna are both posterior to the distal humerus. C. A radiograph taken 4 weeks after injury shows periosteal new bone formation (arrows), indicating where the soft tissues were extensively torn away from the proximal ulna.
|
using closed reduction under general anesthesia. Reduction is achieved
by applying longitudinal traction with the elbow semiextended and at
the same time compressing the proximal radius and ulna together.
In the third child, after attempted closed reduction was unsuccessful,
surgical exploration found the avulsed anterior band of the medial
collateral ligament complex of the elbow was found to be interposed
between the medial condyle of the humerus and the olecranon.96 After removing and repairing the interposed ligament, stable reduction was achieved.
immobilized in 90 degrees of flexion and the forearm in neutral for
approximately 1 to 3 weeks. Active range-of-motion exercises are then
begun. Most patients typically regain full elbow motion, including
forearm pronation and supination.
extremely rare injury with fewer than 10 cases having been reported in
the English literature.19,20,34,40,47,58,76
Radioulnar translocation is commonly missed on the anteroposterior
x-ray unless the proximal radius and ulna are noted to be completely
reversed in relation to the distal humerus.
the pronated hand with the elbow in full or nearly full extension,
producing an axial force on the proximal radius. The anterior radial
head dislocation occurs first, followed by the posterior dislocation of
the olecranon. The radial head, depending on the degree of pronation,
can be lodged in the coronoid fossa or dislocated posteriorly. As a
consequence, fractures of the radial head, radial neck, or coronoid
process may occur.19,20,34,76 Harvey and Tchelebi 47
reported a case in which the cause of radioulnar translocation may have
been iatrogenic: the result of inappropriate technique used to reduce a
posterior elbow dislocation.
and minimal deformity may be apparent. Once pain has been adequately
managed with analgesics, the most consistent finding on clinical
examination is limited elbow range of motion, especially in supination.
also reported one patient who sustained a fracture of the tip of the
coronoid. Proposed soft tissue injuries include radial collateral
ligament, medial collateral ligament, annular ligament, and
interosseous ligament injury.34,58 Isbister58 described transient
ulnar nerve paresthesia that resolved after reduction of the
translocation. Osteonecrosis of the radial head was noted in one
patient after open reduction of a proximal radioulnar translocation.47
The patient must be completely relaxed under general anesthesia, as
sedation or regional anesthesia is unlikely to provide sufficient
relaxation. With the elbow flexed approximately 90 degrees,
longitudinal traction is applied to the elbow while the forearm is
supinated (Fig. 16-29). If the radial head can
be palpated, gentle anterior-directed pressure may help slide the
radial head and neck over the coronoid process, allowing the proximal
radius and ulna to resume their normal configuration. As always, just
the right amount of force should be used; excessive force risks
iatrogenic fracture to the proximal radius. Successful closed reduction
should be confirmed on x-ray, and the elbow should be immobilized for
approximately 3 to 4 weeks with the forearm supinated and the elbow
flexed 90 to 100 degrees.
A lateral approach provides adequate exposure to the translocation and
radial neck fracture if present. At surgery, the radial head and neck
are typically found trapped beneath the trochlea of the distal humerus.
Elbow extension tightens the biceps tendon, making reduction more
difficult. With the elbow flexed, a freer or joker elevator can be
placed beneath the radial head and neck facilitating delivery over the
coronoid process as the forearm is supinated. If present, a radial neck
fracture may now be treated in standard fashion. Internal fixation also
may be necessary for an unstable displaced fracture.
 |
|
FIGURE 16-29 Proximal radioulnar translocation. A. Position of the proximal radius and ulna with a proximal radioulnar translocation. B.
Closed reduction is rarely successful, but may be attempted under general anesthesia using gentle longitudinal traction while supinating the forearm. (Redrawn from Harvey S, Tchelebi H. Proximal radioulnar translocation. J Bone Joint Surg 1979;61:447-449, with permission.) |
used an osteotomy of the proximal ulna to expose and reduce the radius
that was complicated by a postoperative ulnar nerve paralysis that
recovered completely over 2 months.
is immobilized for approximately 3 to 4 weeks with the forearm
supinated and the elbow flexed 90 to 100 degrees, followed by active
elbow range-of-motion exercises.
contracture impede reduction, the patient is brought to the operating
room where as little as possible but as much as necessary is done to
obtain and maintain a stable reduction of the elbow. With the patient
completely relaxed under general anesthesia and pharmacologic
paralysis, closed reduction is attempted by applying longitudinal
traction to the flexed elbow while the forearm is gently but firmly
supinated. If the radial head can be palpated, gentle anterior-directed
pressure may help slide the radial head and neck over the coronoid
process, allowing the proximal radius and ulna to resume their normal
configuration.
reduction is done through a lateral approach as described above. Once
closed or open reduction is achieved, stability of the elbow is
assessed. The elbow is immobilized in the position of maximal
stability, which typically involves flexion of 90 to 100 degrees and
forearm supination. If the elbow remains unstable, radiocapitellar pin
placement may be considered. A pin of adequate size must be selected
and the elbow must be immobilized the entire time the pin is in place
(typically 3 weeks) to avoid pin breakage. Annular ligament
reconstruction or ulnar osteotomy has not been necessary, but might be
considered if a stable reduction can not be achieved by other means.
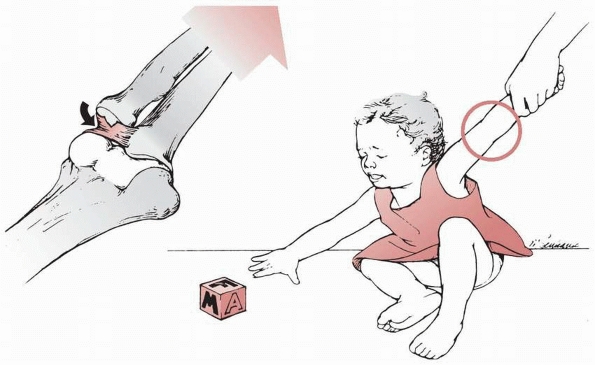
The term “nursemaid’s elbow” and other synonyms have been used to
describe this condition. The demographics associated with subluxation
of the radial head have been well described.6,22,56,60,126
The mean age at injury is 2 to 3 years, with the youngest reported
patient 2 months of age. It rarely occurs after 7 years of age. Sixty
to 65% of the children affected are
girls,
and the left elbow is involved in approximately 70%. It is difficult to
determine the actual incidence because many subluxations are treated in
primary care physician’s offices, by parents, or resolve spontaneously
before being seen by a physician.
Cadaver studies have shown that longitudinal traction on the extended
elbow can produce a partial slippage of the annular ligament over the
head of the radius and into the radiocapitellar joint, sometimes
tearing the subannular membrane. Displacement of the annular ligament
occurs most easily with the forearm in pronation. In this position, the
lateral edge of the radial head, which opposes the main portion of the
annular ligament, is narrow and round at its margin.77,85
In supination, the lateral edge of the radial head is wider and more
square at its margin, thereby restricting slippage of the annular
ligament. McRae and Freeman89 demonstrated that forearm pronation maintained the displacement of the annular ligament.
partially over the radial head in this condition. This anatomic finding
has been confirmed in numerous cadaver experiments.85,89,120
After 5 years of age, the distal attachments of the subannular membrane
and annular ligament to the neck of the radius have strengthened
sufficiently to prevent its tearing and subsequent displacement.120
Previously, the theory was proposed that the radial head diameter was
less in children than in adults and this contributed to subluxation of
the annular ligament. However, cadaver studies of infants, children,
and adults have shown that the ratio of the head and neck diameters is
essentially the same.118,120 Griffin43
suggested that the lack of ossification of the proximal radial
epiphysis in children less than 5 years of age made it more pliable,
thereby facilitating slippage of the annular ligament.
 |
|
FIGURE 16-30
The injury most commonly occurs when a longitudinal pull is applied to the upper extremity. Usually the forearm is pronated. There may be a partial tear in the subannular membrane, allowing the annular ligament to subluxate into the radiocapitellar joint. |
performed a controlled study comparing 30 normal children with 100 who
had pulled elbow syndrome. They found an increased frequency of
hypermobility or ligamentous laxity among children with pulled elbows.
Also, there was an increased frequency of hypermobility in one or both
parents of the involved children compared with noninvolved children,
suggesting that hypermobility could be a factor predisposing children
to this condition.
injury occurs when the forearm is pronated, the elbow extended, and
longitudinal traction is applied to the patient’s wrist or hand (see Fig. 16-30).85,89,122
Such an injury typically occurs when a young child is lifted or swung
by the forearm or when the child suddenly steps down from a step or off
a curb while one of the parents is holding the hand or wrist.
reported that 5 of 6 infants under 6 months of age with a pulled elbow
sustained the injury when rolling over in bed with the extended elbow
trapped under the body. It was believed that this maneuver, especially
if the infant was given a quick push to turn over by an older sibling
or a parent, provided enough longitudinal traction to displace the
annular ligament proximally.
longitudinal pull on the elbow of the young child. The initial pain
usually subsides rapidly, and the child does not appear to be in
distress except that he or she is reluctant to use the involved
extremity. The upper extremity is typically held at the side with the
forearm pronated. A limited painless arc of flexion and extension may
be present; however, any attempt to supinate the forearm produces
pain
and is met with resistance. Although there is no evidence of an elbow
effusion, local tenderness may be present over the radial head and
annular ligament. In some patients, the pain may be referred proximally
to the shoulder but most complain of pain distally toward the wrist.6,56
In patients without a witnessed longitudinal traction injury, other
causes, such as occult fracture or early septic arthritis, must be
carefully ruled out.
condition because there is essentially only one type of pulled elbow
syndrome.
manipulation is attempted? If there is a reliable history of traction
to the elbow, the child is 5 years of age or younger, and the clinical
findings strongly support the diagnosis, x-rays are not necessary.6,22,108,120,137
If, however, there is an atypical history or clinical examination,
x-rays should be obtained to be certain there is not a fracture before
manipulation is attempted.
but subtle abnormalities may be present. Normally, the line down the
center of the proximal radial shaft should pass through the center of
the ossification center of the capitellum (radiocapitellar line).39,127
Careful review of x-rays may demonstrate the radial capitellar line to
be lateral to the center of the capitellum in up to 25% of patients.39,127
Determination of this subtle change requires a direct measurement on
the x-ray. Interestingly, the pulled elbow can be reduced by the
radiology technician because the elbow x-rays are usually taken with
the forearm supinated. The subluxation is reduced inadvertently when
the technician places the forearm into supination to position it for
the x-ray. Bretland13 suggested that
if the best x-ray that can be obtained is an oblique view with the
forearm in pronation, pulled elbow syndrome is the likely diagnosis.
The diagnosis is made by demonstrating an increase in the echonegative
area between the articular surfaces of the capitellum and the radial
head and increased radial capitellar distance. Kosuwon et al.118
found that this distance is normally about 3.8 mm with forearm
pronated. With a subluxated radial head, this measured 7.2 mm. A
difference of 3 mm between the normal and affected sides, therefore,
suggests radial head subluxation.
successfully treated by closed reduction. This is usually best done by
forearm supination.22,43,56,75,108,122,126
Some have recommended that supination be done with the elbow flexed,
and others have found that supination alone with the elbow extended can
effect a reduction. In many patients, a snapping sensation can be both
heard and palpated when the annular ligament reduces (Fig. 16-31). Macias et al.75
reported that hyperpronation was more successful than supination in a
randomized study. Reduction was successful in 40 of 41 patients (98%)
in the hyperpronation group, compared with 38 of 44 patients (86%) in
the supination group. They concluded that the hyperpronation technique
was more successful, required fewer attempts, and was often successful
when supination failed. Generally, a full arc of supination to
pronation of the forearm, with elbow flexion and extension, will reduce
all pulled elbows.
 |
|
FIGURE 16-31 Reduction technique for nursemaid’s elbow. Left: The forearm is first supinated. Right:
The elbow is then hyperflexed. The surgeon’s thumb is placed laterally over the radial head to feel the characteristic snapping as the ligament is reduced. |
reported a decreased rate of recurrence during the 10 days following
reduction if the elbow was splinted in a flexed supinated position for
2 days following reduction. Salter and Zaltz120 recommended the use of a sling, mainly to prevent the elbow from being pulled a second time. Kohlhaas and Roeder68
recommended a T-shirt technique for flexed elbow stabilization in very
young children. This provided adequate immobilization without the use
of a sling by pinning the sleeve of the long sleeve T-shirt to the
opposite chest. In general, after a successful closed reduction of a
first time annular ligament
subluxation,
immobilization of the extremity is not necessary if the child is
comfortable and using the arm normally. After the reduction, it is
important to explain to the parents the mechanism of injury and to
emphasize the need to prevent longitudinal pulling on the upper
extremities. Picking the child up under the axillae and avoiding games
such as “ring around the roses” and involve longitudinal traction to
the arm are stressed. However, recurrence rate is high even with the
most diligent parents. Therefore, instruction in home reduction of the
pulled elbow is very useful and lessens visits to the emergency room
and primary care physician.
reduce spontaneously. There are no reported cases of long-term sequelae
of untreated annular ligament subluxation. Therefore, open reduction is
rarely if ever indicated for annular ligament subluxation. An
indication for surgery might be the chronic, symptomatic, irreducible
subluxation.137 In such a circumstance, the annular ligament must be partially transected to achieve reduction.
whether or not the child had a traction force applied across the
extended elbow. The entire extremity is then carefully examined. Focal
tenderness should be present directly over the radiocapitellar joint.
If the history or physical examination is not entirely consistent with
annular ligament subluxation, then x-rays of the upper extremity are
obtained to assess for other injuries before manipulating the elbow.
clearly established, manipulation is performed. It is first explained
to the parents that there will be a brief episode of pain followed by
relief of the symptoms. The patient usually is seated on the parent’s
lap. The patient’s forearm is grasped with the elbow semiflexed while
the thumb of the surgeon’s opposite hand is placed over the lateral
aspect of the elbow. The forearm is first supinated. If this fails to
produce the characteristic snap of reduction, then the elbow is gently
flexed maximally until the snap occurs (see Fig. 16-31).
Just before reaching maximal flexion, there often is an increase in the
resistance to flexion. At this point, a little extra pressure toward
flexion is applied, which usually produces the characteristic snap as
the annular ligament suddenly returns to its normal position. If this
fails, then the hyperpronation technique of Macias et al.75
is used. Full flexion-extension elbow motion and forearm
pronation-supination motion is performed to the extremes, and this
usually resolves the “outliers” which do not reduce with the usual
mechanisms.
felt or if the patient fails to use the extremity after manipulation?
In a few patients, discomfort may persist despite successful annular
ligament reduction. If the subluxation has occurred more than 12 to 24
hours before the child is seen, there often is a mild secondary
synovitis, and recovery may not be immediate and dramatic. One must
confirm that the initial diagnosis was correct. If not taken before the
manipulation, x-rays should be obtained and the entire extremity
careful re-examined. If the x-ray results are normal and the elbow can
be fully flexed with free supination and pronation, the physician can
be assured that the subluxated annular ligament has been reduced. In
this circumstance, the patient’s arm may be placed in a splint or sling
for a few days to 1 week and re-examined clinically and by x-ray if
needed.
resulted in annular ligament subluxation. Such an injury mechanism is
much more likely to result in a fracture (possibly occult) about the
elbow.
unrecognized and unreduced subluxations. Almost all subluxations reduce
spontaneously. The only problem seems to be discomfort to the patient
until the annular ligament reduces.
Recurrent subluxations usually respond to the same manipulative
procedure as the initial injury. They eventually cease after 4 to 5
years when the annular ligament strengthens and ligament laxity
lessens. Recurrences do not lead to any long-term sequelae. If
recurrent annular ligament subluxation significantly impacts a
patient’s quality of life because of pain or limited activity,
immobilization in an above-elbow cast with the forearm in supination or
neutral position for 2 to 3 weeks is usually effective at preventing
recurrence.
Wilkins, and George Thompson for their contributions to this chapter.
The information presented in this chapter is based on their efforts in
previous editions.
G, Dalbayrak S, Yilmaz M, et al. MRI demonstration of intra-articular
median nerve entrapment after elbow dislocation. Skeletal Radiol
2003;32:537-541.
AO, Balakumar J, Howells RJ, et al. Posterior divergent dislocation of
the elbow in children and adolescents: a report of three cases and
review of the literature. J Pediatr Orthop 2005;25:317-321.
K, Mortensen AC, Gron P. Transverse divergent dislocation of the elbow.
A report of two cases. Acta Orthop Scand 1985;56:442-443.
H, De Pablos J, Gonzalez J, et al. Entrapment of the median nerve after
posterior dislocation of the elbow. Microsurgery 1983;4:215-220.
JH, Donati NL. Recurrent dislocation of the elbow in a child. A case
report and review of the literature. J Pediatr Orthop 1991;11:392-396.
S, Holst-Nielsen F. Intra-articular entrapment of the median nerve
after dislocation of the elbow. J Hand Surg Br 1897;12(3):356-358.
JM, Bollini G, Jacquemrier M, et al. The treatment of old dislocations
of the radial head in children by osteotomy of the upper end of the
ulna. Apropos of 15 cases [Article in French]. Rev Chir Orthop
Reparatrice Appar Mot 1988;74:173-182.
SR, Tito AV, Cuesta FJG, et al. Median nerve paralysis following elbow
fractures and dislocations. Apropos of a series of 12 cases [Article in
French]. Ann Chir 1984;38:270-273.
A, Wolfe SW, Marsh JS. Use of a modified Bell Tawse procedure for
chronic acquired dislocation of the radial head. J Pediatr Orthop
1998;18:410-414.
A, Prada S, Teixeira K. Case report and review of the literature.
Proximal radioulnar transposition in an elbow dislocation. J Orthop
Trauma 1992;6:106-109.
W, Heinrich SD. Acute annular ligament interposition into the
radiocapitellar joint in children (nursemaid’s elbow). J Pediatr Orthop
1995;15:454-456.
PI. The mechanism and nature of the injury in dislocations of the elbow
and a method of treatment. Aust N Z J Surg 1960;30:212-216.
AS. Outcome of longstanding dislocated elbows treated by open reduction
and excision of collateral ligaments. Singapore Med J 2004;45:14-19.
JN, Ring DC. Fracture of the anteromedial facet of the coronoid
process. Surgical Technique. J Bone Joint Surg Am 2007;89(Suppl
2):267-283.
M, Gauer EF, Muller W. Die Operative Behandlung der Rezidivierenden und
Traumatischen Luxation des Ellenbogengelenkes nach Osborne une
Cotterill. Arch Orthop Unfall Chir 1976;86:141-156.
O, Nybonde T, Karlsson G. Luxation of the elbow complicated by proximal
radio ulnar translocation. Acta Radiol 1990;31:145-146.
Bardouni A, Mahfoud M, Ouadghiri M, et al. Divergent dislocation of the
elbow. A case report [Article in French]. Rev Chir Orthop Reparatrice
Appar Mot 1994;80:150-152.
P, Levai JP, Collin JPH. Median nerve entrapment in elbow dislocation
[Article in French]. Rev Chir Orthop Reparatrice Appar Mot
1977;63:13-16.
JV, Kassab MT, Douik M. Untreated posterior dislocation of the elbow in
children. J Bone Joint Surg Am 1984;66(6):921-926.
JV, Slimane N, Kassab MT. Elbow dislocation with avulsion of the medial
humeral epicondyle. J Bone Joint Surg Br 1990;72(1):102-104.
RJ, Brooks S. Brachial artery damage accompanying closed posterior
dislocation of the elbow. J Bone Joint Surg Br 1985;67(3):378-381.
H. Entrapment of the median nerve after dislocation of the elbow. A
case report. J Bone Joint Surg Br 1981;63B(3):408-412.
CC, Von Laer L, Hell AK. Open reduction, ulnar osteotomy and external
fixation for chronic anterior dislocation of the head of the radius. J
Bone Joint Surg Br 2005;87(1):88-94.
RS, Roberston IM. Open dislocation of the elbow with rupture of the
brachial artery. J Bone Joint Surg Br 1952;34B(4):636-637.
III KE, Moneim MS, Omer GE, et al. Brachial artery disruption following
closed posterior elbow dislocation in a child. A case report with
review of the literature. Clin Orthop Relat Res 1984;184:145-149.
G, Horii E. Case report. Combined shear fractures of the trochlea and
capitellum associated with the anterior fracture-dislocation of the
elbow. J Orthop Trauma 1992;6:373-375.
JA. Simple anterior dislocation of the elbow joint with rupture of the
brachial artery. Case report. Am J Surg 1940;47:479-486.
HCN, Youngson GG, Beattie TF. The epidemiology of radial head
subluxation (“pulled elbow”) in the Aberdeen City area. Health Bull
(Edinb) 1990;48:58-61.
P, Gentz CF, Johnell O, et al. Surgical versus nonsurgical treatment of
ligamentous injuries following dislocations of the elbow joint. Clin
Orthop Relat Res 1987;214:165-169.
PO, Gentz CF, Johnell O, et al. Surgical versus nonsurgical treatment
of ligamentous injuries following dislocations of the elbow joint. A
prospective randomized study. J Bone Joint Surg Am 1987;69(4):605-608.
PO, Johnell O, Gentz CF. Long-term sequelae of simple dislocation of
the elbow. J Bone Joint Surg Am 1984;66(6):927-930.
P, Sweeney JG, Silk FF. Three cases of compound posterior dislocation
of the elbow with rupture of the brachial artery. J Bone Joint Surg Br
1962;44B:119-121.
A, Ahmed M. Technical tricks. Closed reduction of posterior dislocation
of the elbow: a simple technique. J Orthop Trauma 1999;13:58-59.
LK. Reeducation and after-treatment of posterior dislocation of the
elbow. With special attention to the brachialis muscle and myositis
ossificans. Am J Surg. 1944;63:56-60.
DS, Ricciardi JE, Spengler DM. Arterial injury: a complication of
posterior elbow dislocation. A clinical and anatomical study. J Bone
Joint Surg Am 1974;56(8):1631-1636.
CG, Bothner J, Wiebe R. A comparison of supination/flexion to
hyperpronation in the reduction of radial head subluxations. Pediatrics
1998;102:10.
B, Laupattarakasem W, Supachutikul A, et al. Late reduction of
dislocated elbow. Need triceps be lengthened? J Bone Joint Surg Br
1992;75(3):426-428.
H. Recurrent dislocation of the elbow accompanied by ulnar neuropathy.
A case report and review of the literature. Clin Orthop Relat Res
1981;161:270-274.
M, Minkowitz B, Shimotsu G, et al. Brachial artery laceration with
closed posterior elbow dislocation in an eight-year-old. Clin Orthop
Relat Res 1993;296:109-112.
SN, Debnath UK, Rao P, Mohanty K. Simple elbow dislocation among
adults: A comparative study of two different methods of treatment.
Injury 2007;38:1254-1258.
I. A radiological sign of entrapment of the median nerve in the elbow
joint after posterior dislocation. A report of two cases. J Bone Joint
Surg Br 1976;58(3):353-355.
MD, Schemitsch EH, Sala MJ, et al. The pathoanatomy of lateral
ligamentous disruption in complex elbow instability. J Shoulder Elbow
Surg 2003;12:391-396.
Hall R. Recurrent posterior dislocation of the elbow joint in a boy.
Report of a case. J Bone Joint Surg Br 1953;35B:56.
S, Sud A, Tiwari A, et al. Open reduction for late-presenting posterior
dislocation of the elbow. J Orthop Surg 2007;15:15-21.
MA, Quigley TB. Reduction of posterior dislocation of the elbow by
traction on the dangling arm. Clin Orthop Relat Res 1974;103:106-108.
A, Tanaka S, Hirofuji E, et al. Transverse divergent dislocation of the
elbow in a six-year-old boy: case report. J Trauma 1992;32:118-119.
M, Sawaizumi T, Ito H. Transverse divergent dislocation of the elbow
with ipsilateral distal radius fracture in a child. J Orthop Trauma
2007;21:145-149.
SW, Morrey BF, Korinek S, et al. Elbow subluxation and dislocation. A
spectrum of instability. Clin Orthop Relat Res 1992;280:186-197.
G, Akpinar S, Hersekli MA, et al. Type 4 median nerve entrapment in a
child after elbow dislocation. Arch Orthop Trauma Surg 2003;123:555-557.
P, Gharib M. Traumatic subluxation of the head of the radius [Article
in German]. Deutsch Med Wochenschr 1976;101:1520-1523.
DJ, Linscheid RL, Svien HJ. Intra-articular median nerve entrapment
with dislocation of the elbow. Clin Orthop Relat Res 1973;90:100-103.
NA, Kenwright J, Taylor RG, et al. Complete lesion of the median nerve
associated with dislocation of the elbow. Acta Orthop Scand
1974;45:365-369.
SB, Crawford AH. Median nerve entrapment after dislocation of the elbow
in children. A report of 2 cases and review of the literature. Clin
Orthop Relat Res 1995;312:232-237.
PP. Transplantation of the biceps tendon as a treatment for recurrent
dislocation of the elbow. Br J Surg 1947;35:201-204.
G, McDevitt ER, Chronister R, et al. Treatment of simple elbow
dislocation using an immediate motion protocol. Am J Sports Med
1999;27:308-311.
MK, Auliciano PL. Open elbow dislocation with brachial artery
disruption: case report and review of the literature. Orthopedics
1986;9:539-542.
JR. The relationship of the radial head to radial neck diameters in
fetuses and adults with reference to radial head subluxation in
children. J Bone Joint Surg Am 1969;51(4):781-783.
RB, Zaltz C. Anatomic investigations of the mechanism of injury and
pathologic anatomy of pulled elbow in young children. Clin Orthop Relat
Res 1971;77:134-143.
GH, Bennett JB, Woods GW, et al. A biomechanics of elbow instability:
the role of the medial collateral ligament. Clin Orthop Relat Res
1980;146:42-52.
YK, Tello E, D. FB. Transverse divergent dislocation of the elbow with
ipsilateral distal radius epiphyseal injury in a seven-year-old. Injury
1998;29:798-802.
JO, Helmig P, Kjaersgaard-Andersen P. Dislocation of the elbow: an
experimental study of the ligamentous injuries. Orthopedics
1987;12:461-463.
HC, Jones JM. Rupture of the brachial artery accompanying dislocation
of the elbow or supracondylar fracture. J Bone Joint Surg Am
1951;33A:889-894.
RN, Larrick RB, Meyer TL. Median nerve entrapment following elbow
dislocation in children. A report of two cases. J Bone Joint Surg Am
1969;51(2):381-385.
PO, Paschaloglou C, Stavrou Z, et al. Recurrent dislocation of the
elbow. Report of three cases. J Bone Joint Surg Am 1975;57A:1084-1086.
SJ, Wilson SC, Rychak J. Irreducible pulled elbow in a child. A case
report. Clin Orthop Relat Res 1992;284:153-155.
P, Orduna M. Transverse divergent dislocation of the elbow in a child.
A case report. Clin Orthop Relat Res 1993;294:312-313.
RD. Anterior elbow dislocation associated with olecranon fractures.
Review of the literature and case report. Iowa Orthop J 1993;13:223-225.
R. A case of complete anterior dislocation of both bones of the forearm
at the elbow. Surg Gynecol Obstet 1913;16:570-571.
J, Tayon B. Recurrent dislocation of the elbow. Apropos of 6 cases
[Article in French]. Rev Chir Orthop Reparatrice Appar Mot
1974;60:485-495.
