Fractures of the Shaft of the Tibia and Fibula
pediatric long bone injuries (15%) after radial/ulnar and femoral
fractures.133,142 The prevalence of tibial fractures in both boys and girls has increased since 1950.79 The average age of occurrence is 8 years, and the frequency of occurrence does not change significantly with age.61
Seventy percent of pediatric tibial fractures are isolated injuries;
ipsilateral fibular fractures occur with 30% of tibial fractures.18,142,151
Fifty to 70% of tibial fractures occur in the distal third, and 19% to
39% in the middle third. The least commonly affected portion of the
tibia is the proximal third, yet these may be the most problematic.
Thirty-five percent of pediatric tibial fractures are oblique, 32%
comminuted, 20% transverse, and 13% spiral.133
Tibial fractures in children under 4 years of age usually are isolated
spiral or short oblique fractures in the distal and the middle one
third of the bone. Most tibial fractures in older children and
adolescents are in the distal third.
that present without an associated fibular fracture.10,18,51,100,133
Tibial fractures due to bicycle spoke injuries occur almost exclusively
in children 1 to 4 years of age, whereas most tibial fractures in
children 4 to 14 years of age are the result of sporting or traffic
accidents.10,18,61,79,100,133
More than 50% of ipsilateral tibial and fibular fractures result from
vehicular trauma. Most isolated fibular fractures result from a direct
blow.61,133
The tibia is the second most commonly fractured bone in abused
children. Approximately 16% to 26% of all abused children with a
fracture have an injured tibia.82,95
Nine percent of pediatric tibial fractures are open. Concomitant
fractures of the ankle and foot are the most common injuries associated
with fractures of the tibia and fibula, followed by humeral, femoral,
and radial/ulnar fractures.13 In a
1994 report, the average Injury Severity Score of a child with a tibial
fracture was 10 (range, 0 to 45) with an average hospital stay of 6.5
days (range, 1 to 50 days).13 There
have been no updates of this information in the recent English
literature; however, it would seem certain that the current average
hospital stay is less in 2008.
classified into three major categories based on the combination of
bones fractured and the location of the injuries.
body. There are two concave condyles at the proximal aspect of the
tibia. The medial condyle is larger, deeper, and narrower than the
lateral condyle. An elevated process, the tibial tubercle, located
between the two condyles, is the site of attachment of the patellar
tendon. The shaft of the tibia is prismoid, with a broad proximal
extent that decreases in size until the distal third, where it
gradually increases again in size. The tibial crest is prominent
medially from the tibial tubercle to the tibial plafond and is
subcutaneous without any overlying muscles.51
in the shaft and one in each epiphysis. The tibial diaphysis ossifies
at 7 weeks of gestation and expands both proximally and distally. The
proximal epiphyseal center appears shortly after birth and unites with
the shaft between 14 and 16 years of age. The distal epiphyseal
ossification center appears in the second year of life, and the distal
tibial physis closes between 14 and 15 years of age. Additional
ossification centers are found occasionally in the medial malleolus and
in the tibial tubercle.51
proximally, with the fibula at the knee and the ankle, and with the
talus distally.51 Twelve muscles have either their origin or insertion on the tibia (Table 25-1).
The fibula articulates with the tibia and the talus. The fibular
diaphysis ossifies at about 8 weeks of gestation. The distal epiphysis
is visible at 2 years of age, and the proximal secondary ossification
center at 4 years. The distal fibular physis closes at approximately 16
years; the proximal physis closes later, between the ages of 15 and 18
years.51 Nine muscles have either their origin or insertion on the fibula (Table 25-2).51
|
TABLE 25-1 Muscle Origins and Insertions on the Tibia
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||
condyles of the femur and passes between the medial and lateral heads
of the gastrocnemius muscle. It ends at the distal border of the
popliteus muscle, where it divides into the anterior and posterior
tibial arteries. The anterior tibial artery passes between the tibia
and the fibula over the proximal aspect of the intraosseous membrane.
The posterior tibial artery divides several centimeters distal to this
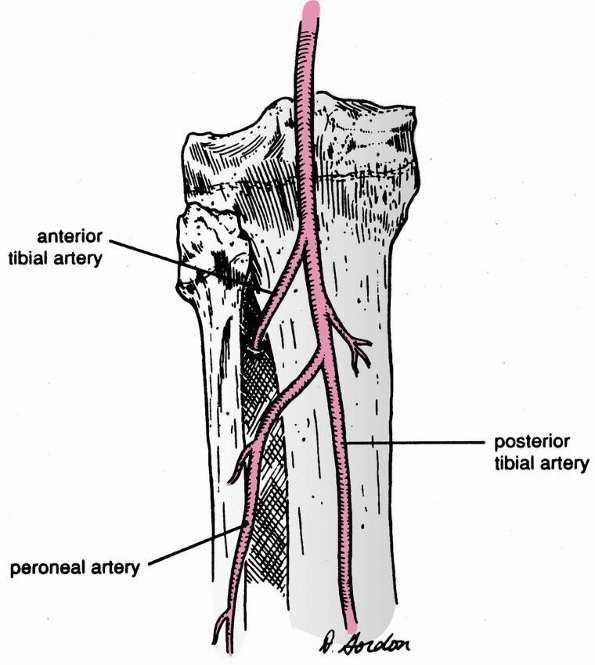
point, giving rise to the peroneal artery (Fig. 25-1).51
|
TABLE 25-2 Muscle Origins and Insertions on the Fibula
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||
 |
|
FIGURE 25-1 Vascular anatomy of the proximal tibia.
|
 |
|
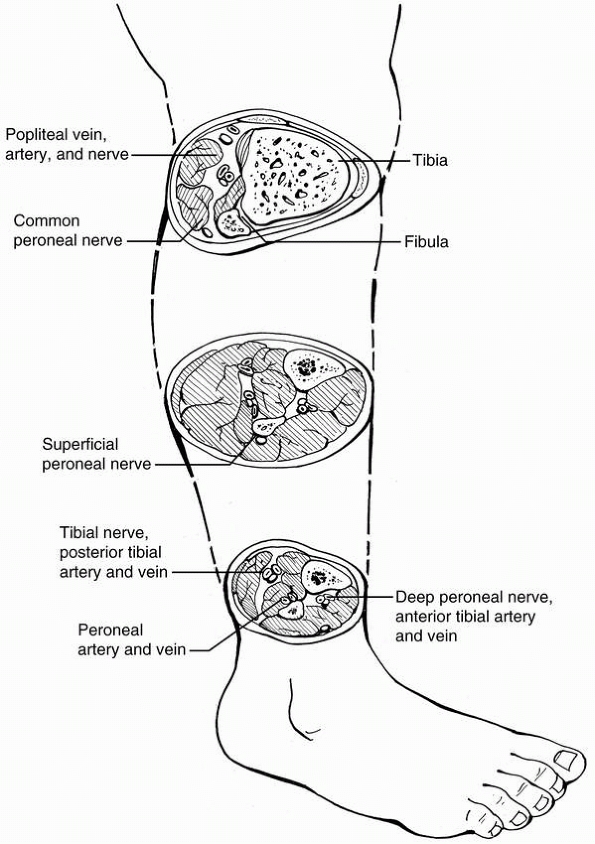
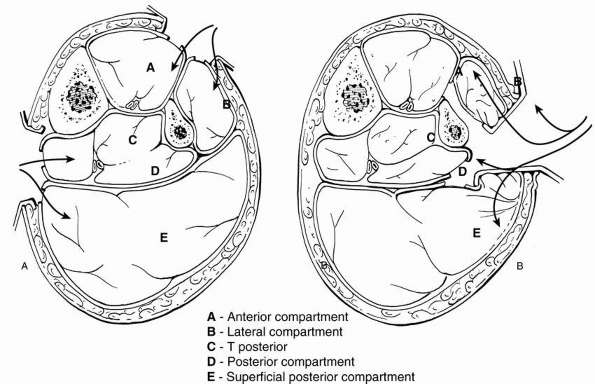
FIGURE 25-2 Fibroosseous compartments of the leg.
|
to the popliteal artery in the popliteal fossa, and then enters the
deep posterior compartment of the leg. This nerve provides innervation
to the muscles of the deep posterior compartment and sensation to the
plantar aspect of the foot. The common peroneal nerve passes around the
proximal neck of the fibula. It divides into the deep and superficial
branches, and then passes into the anterior and the lateral
compartments of the lower leg,51
respectively. Each branch innervates the muscles within its
compartment. The deep peroneal nerve provides sensation to the first
web space. The superficial branch is responsible for sensation across
the dorsal surface of the foot.
The anterior compartment contains the extensor digitorum longus, the
extensor hallucis longus, and the tibialis anterior muscles; the
anterior tibial artery and deep peroneal nerve run in this compartment.
The lateral compartment contains the peroneus longus and brevis
muscles. The superficial peroneal nerve runs through this compartment.
The superficial posterior compartment contains the soleus and
gastrocnemius muscles. The deep posterior compartment contains the
flexor digitorum longus, the flexor hallucis longus, and the tibialis
posterior muscles.
The posterior tibial artery, peroneal artery, and posterior tibial nerve run in this compartment.51
 |
|
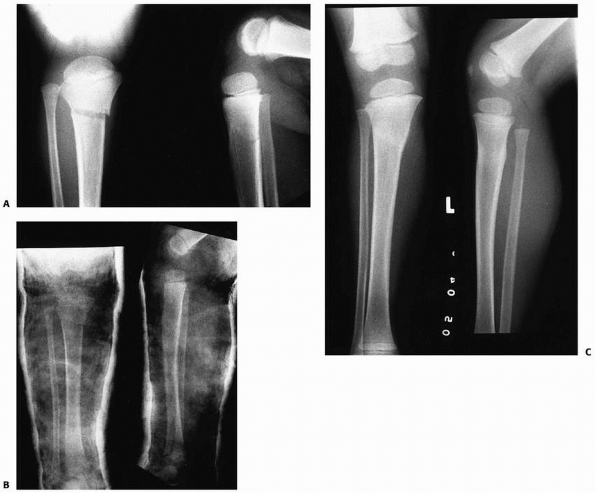
FIGURE 25-3
Anteroposterior radiographs of the knee in a 9-month-old child who was abused show a proximal tibial metaphyseal corner fracture with extension into the physis (right). The follow-up radiograph on the left demonstrates marked new bone function, which suggests the degree of periosteal stripping that occurred at the time of the injury. |
fractures is between the ages of 3 and 6 years. The most common
mechanism of injury is a force applied to the lateral aspect of the
extended knee generating a valgus moment. The cortex of the medial
tibial metaphysis fails in tension, often resulting in an incomplete
fracture. The fibula generally escapes injury, although plastic
deformation may occur.* Occasionally, a proximal tibial metaphyseal fracture may occur as the result of abuse (Fig. 25-3).
present with pain, swelling, and tenderness in the region of the
fracture. Motion of the knee causes moderate pain, and in most cases
the child will not walk. Crepitance is seldom identified on physical
examination, especially if the fracture is incomplete.2,4,21,22,52,71,76,81,110,135,141,146,150,154,155
fracture of the proximal tibial metaphysis. The medial aspect of the
fracture often is widened, producing a valgus deformity.2,4,15,22,52,71,76,126,135,141,146,150,154,155
reported 4 patients with valgus deformities after fractures of the
proximal tibial metaphysis. Since that time, many other investigators4,21,52,71,76,81,92,110,142,146,150
have reported development of tibia valga, even in fractures without any
significant malalignment at the time of initial treatment.
In some cases, proximal tibia valga can be the result of an inadequate
reduction or the loss of satisfactory reduction in the weeks following
the manipulation.135,154 Lehner and Dubas92 suggested that an expanding medial callus produced a valgus deformity, whereas Goff46 and Keret et al.81
believed that the lateral aspect of the proximal tibial physis was
injured at the time of the initial fracture (Salter-Harris type V
injury), resulting in asymmetric growth. Taylor146
believed that the valgus deformity was secondary to postfracture
stimulation of the tibial physis without a corresponding stimulation of
the fibular physis. Pollen115 suggested that premature weight bearing produced an angular deformity of the fracture before union. Rooker and Salter123
believed that the periosteum was trapped in the medial aspect of the
fracture, producing an increase in medial physeal growth and a
developmental valgus deformity.
deformity occurs secondary to an increase in vascular flow to the
medial proximal tibial physis after fracture, producing an asymmetric
physeal response that causes increased medial growth.76
Support for this theory includes quantitative bone scans performed
months after proximal tibial metaphyseal fractures that have shown
increased tracer uptake in the medial aspect of the physis compared
with the lateral aspect.154 Ogden109
identified an increase in the collateral geniculate vascularity to the
medial proximal tibia in a cadaver angiography study of a 5-year-old
child with a previous fracture. This further supports the theory that
medial overgrowth occurs secondary to an increase in the blood flow
supplying the medial aspect of the proximal tibia following injury.101
is the result of an injury to the pes anserinus tendon plate. It is
suggested that the pes anserinus tethers the medial aspect of the
physis, just as the fibula appears to tether the lateral aspect of the
proximal tibial physis. Multiple authors believe that the proximal
tibial fracture disrupts the tendon plate, producing a loss of the
tethering affect. This, then, may lead to medial physeal overgrowth and
a functional hemichondrodiastasis.4,25,26,150,155
Exploration of the fracture, followed by removal and repair of the
infolded periosteum that forms the foundation of the pes anserinus
tendon plate, has been suggested as an approach that may decrease the
risk of a developmental valgus deformity.
Tibia valga deformity can occur after healing of a nondisplaced
fracture, and can recur after corrective tibial osteotomy, further
supporting the premise that asymmetric physeal growth is the cause of
most posttraumatic tibia valga deformities.154
valga is one of slow progression of the deformity, followed by gradual
restoration of normal alignment over time. Zionts and Mac-Ewen155 followed 7 children with progressive valgus deformities of the tibia for an average of 39 months after metaphyseal fractures (Fig. 25-5).
Most of the deformity developed during the first year after injury. The
tibia continued to angulate at a slower rate for up to 17 months after
injury. Six of their 7 patients
had spontaneous clinical corrections. At follow-up, all children had less than a 10-degree deformity.
 |
|
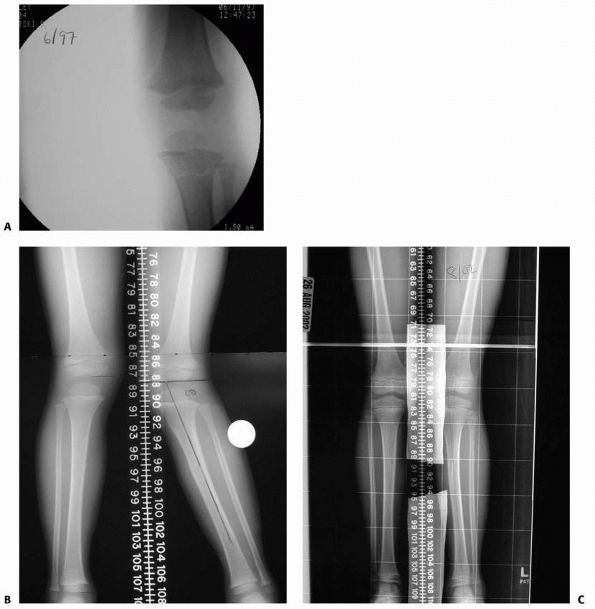
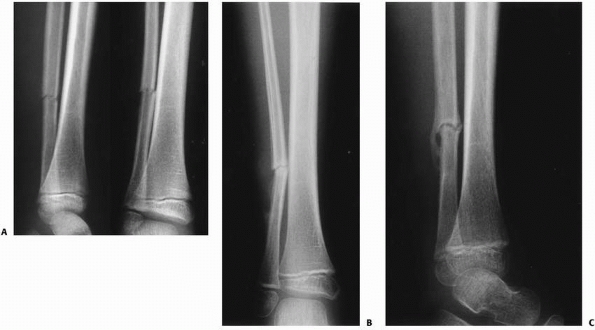
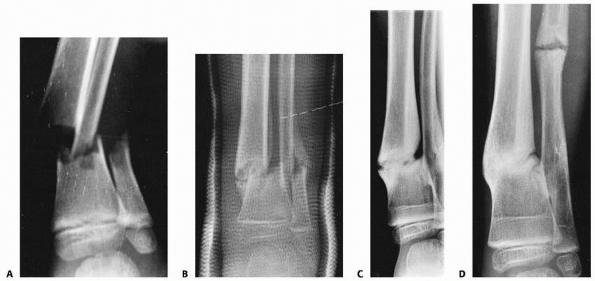
FIGURE 25-4 A.
Anteroposterior and lateral radiographs of the proximal tibial metaphyseal fracture with an intact fibula in a 3-year-old child. B. Anteroposterior and lateral radiograph in the initial long-leg cast demonstrate an acceptable alignment. C. Posttraumatic tibia valga is present 1 year after fracture union. (From Sharps CH, Cardea JA. Fractures of the shaft of the tibia and fibula. In: MacEwen GD, Kasser JR, Heinrich SD, eds. Pediatric Fractures: A Practical Approach to Assessment and Treatment. Baltimore: Williams & Wilkins, 1993:321, with permission.) |
analyzed 25 patients with proximal tibial fractures. Twelve children
with a greenstick or a complete fracture developed valgus deformities,
while no child with a torus fracture developed a deformity. Altered
growth at the distal tibial physis appeared to compensate for the
proximal tibia valga in three children. Corrective osteotomies were
performed in four children. The valgus deformity recurred in two of
these four children, and two had iatrogenic compartment syndromes. This
study supports the premise that developmental tibia valga does not
require correction in many patients. If correction is deemed necessary,
it is important to remember that tibial osteotomy is not always a
benign procedure without significant risk of complications. Gradual
correction of the deformity with a proximal medial tibial
hemiepiphysiodesis may be most appropriate treatment for recalcitrant
postfracture tibia valga in a child with significant growth remaining.10,110,119,141,146
|
TABLE 25-3 Proposed Etiologies of Trauma-Induced Tibia Valgus
|
|||||||
|---|---|---|---|---|---|---|---|
|
should be stabilized in a long-leg cast with the knee in 5 to 10
degrees of flexion and with a varus mold (Fig. 25-6).
Displaced proximal tibial fractures require closed reduction with
general anesthesia in the operating room or in an emergency room
setting with adequate sedation. An anatomic reduction or slight varus
positioning should be verified radiographically. If closed reduction to
an anatomic or slight varus position
cannot
be obtained, open reduction is indicated. Open reduction includes
removal of any soft tissue interposed within the fracture site and
repair of the pes anserinus plate if ruptured. The child is placed into
a long-leg, straight-knee cast after reduction, and the alignment is
checked once again radiographically. In rare instances, percutaneous
fixation with smooth pins, or an external fixator, may be required (Fig. 25-7).
The goal is anatomic reduction or slight varus position at the fracture
site. When the child initially presents for treatment of a tibia
fracture at risk of developing genu valgum, it is imperative that the
possibility of this unusual and unpredictable postfracture problem is
discussed with the family. Frequent follow-up visits are required to
verify maintenance of the reduction. The cast is removed approximately
6 weeks after injury. The child may return to normal activities after
recovery of normal knee and ankle range of motion. Long-term follow-up
with a warning to the family of possible growth abnormality is
mandatory.
 |
|
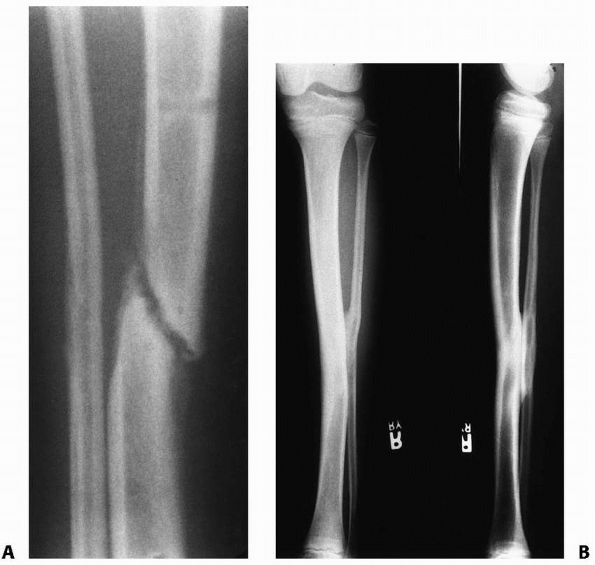
FIGURE 25-5 A-C. Anteroposterior radiographs demonstrating the development and subsequent spontaneous correction of postfracture tibia valga.
|
 |
|
FIGURE 25-6
Anteroposterior and lateral radiographs of the proximal tibia and distal femur in a child who sustained a nondisplaced fracture of the proximal tibial and fibular metaphysis. The knee is casted in extension which facilitates accurate measurements of fracture alignment. |
 |
|
FIGURE 25-7
Anteroposterior radiograph of a 3-year-old female with a severe closed head injury, ipsilateral femur, and proximal tibial metaphyseal fractures. The tibia fracture was stabilized with a modified uniplanar external fixator. |
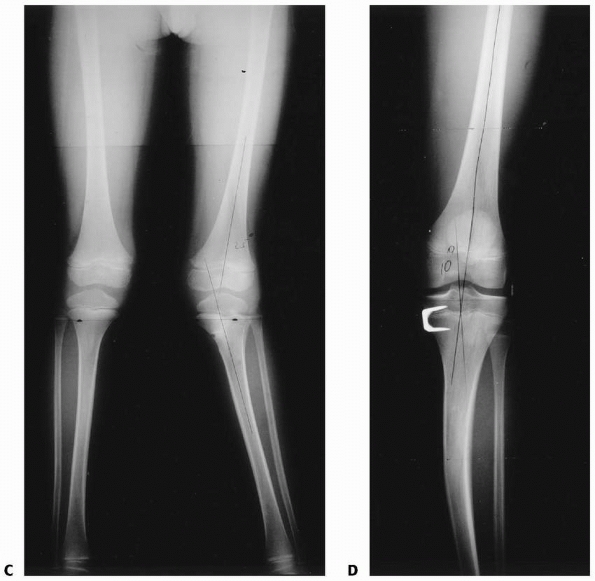
followed until adequate spontaneous correction occurs. This may take 18
to 36 months. Surgical intervention may be indicated in patients more
than 18 months postinjury with a mechanical axis deviation greater than
10 degrees as a result of tibial valgus. Tibial osteotomies are not
indicated in patients with significant growth remaining (Fig. 25-8).
A proximal tibial medial hemiepiphysiodesis can produce more anatomic
alignment without many of the risks of osteotomy. Hemiepiphysiodesis
may be accomplished through a variety of methods utilizing staples,
screws, or newer plate and screw devices (Fig. 25-9A,B).101,141
Orthotic devices do not alter the natural history of posttraumatic
tibia valga and are not recommended. Since the valgus deformity usually
is associated with some element of overgrowth, a contralateral shoe
lift of appropriate size may make the deformity appear less apparent.
 |
|
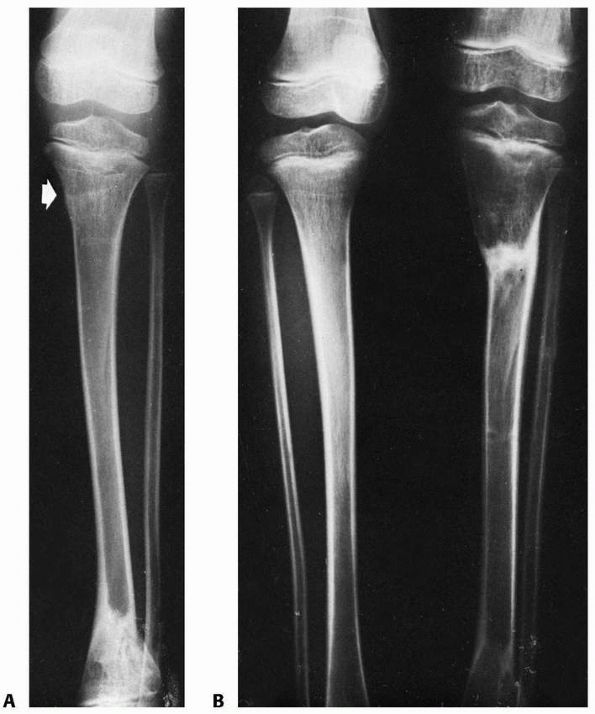
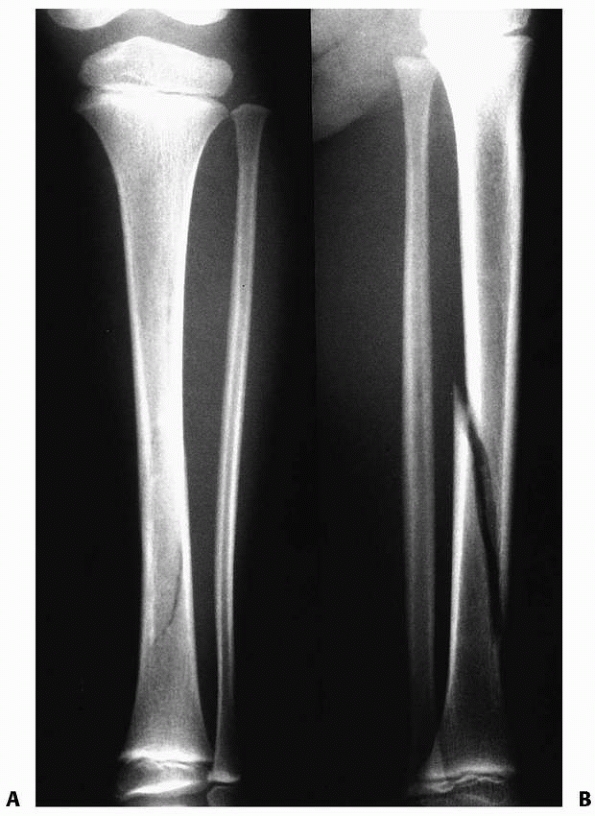
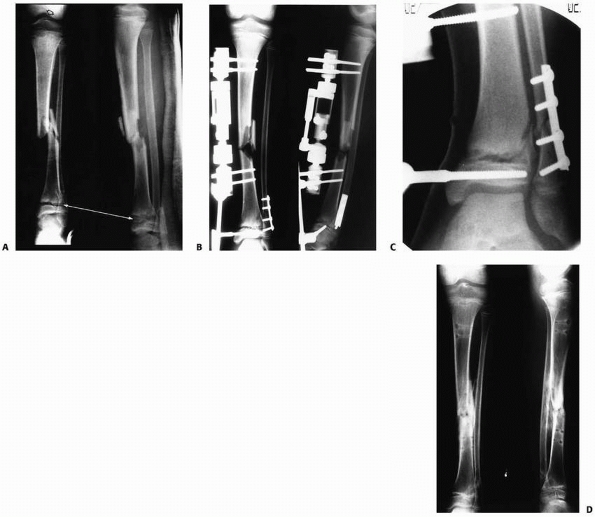
FIGURE 25-8 Developmental valgus after a proximal tibial metaphyseal fracture and subsequent corrective osteotomy. A.
Radiograph taken 6 months after a fracture of the proximal tibia. The injury was nondisplaced. The scar from the initial proximal metaphyseal fracture is still seen (arrow). This child developed a moderate valgus deformity of the tibia within 6 months of fracture. B. A proximal tibial corrective osteotomy was performed. C. Two months postoperatively, the osteotomy was healed and the deformity corrected. D. Five months later, there was a recurrent valgus deformity of 13 degrees. (Courtesy of John J.J. Gugenheim, MD.) |
The fractures can be incomplete (torus, greenstick) or complete. Most
tibial fractures in children under 11 years of age are caused by a
torsional force and occur in the distal third of the tibia. These
oblique and spiral fractures occur when the body rotates with the foot
in a fixed position on the ground. The fracture line generally starts
in the distal anteromedial aspect of the bone and propagates proximally
in a posterolateral direction. If there is not an associated fibula
fracture, the intact fibula prevents significant shortening of the
tibia; however, varus angulation develops in approximately 60% of
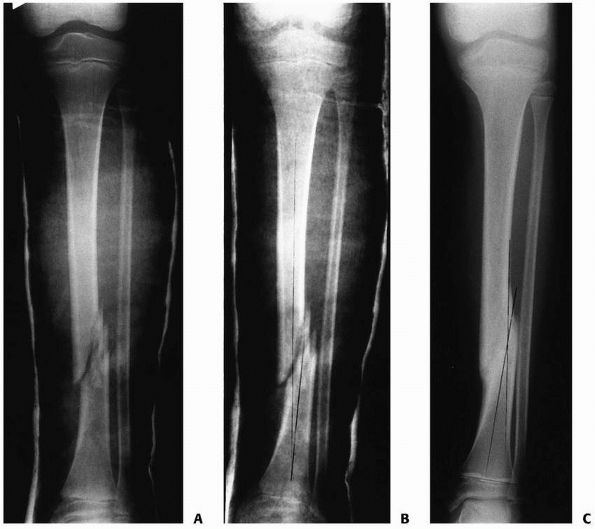
isolated tibial fractures within the first 2 weeks after injury (Fig. 25-10).153
In these cases, the forces of contraction of the long flexor muscles of
the lower leg are converted into an angular moment by the intact fibula
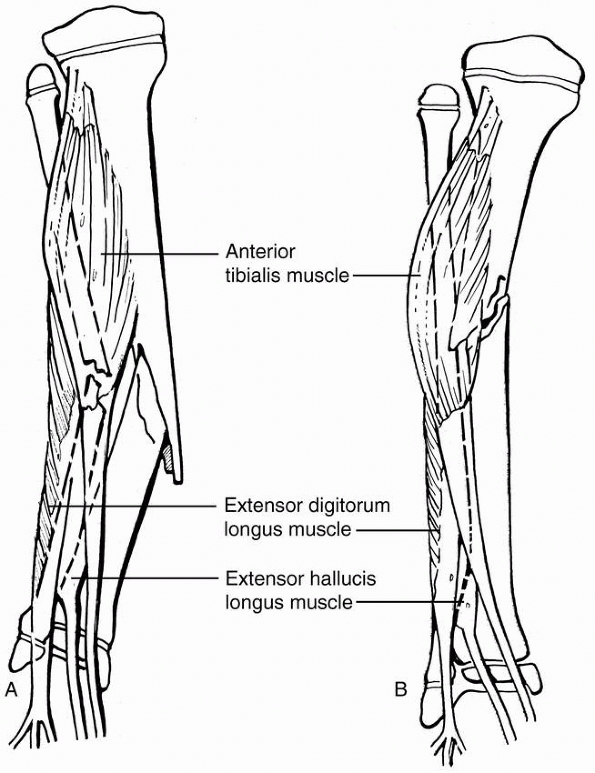
producing varus malalignment (Fig. 25-11A).
Isolated transverse and comminuted fractures of the tibia most commonly
are caused by direct trauma. Transverse fractures of the tibia with an
intact fibula seldom displace significantly.12,77 Comminuted tibial fractures with an intact fibula tend to drift into varus alignment similar to oblique and spiral fractures.12,77,153
may be either complete or incomplete with some element of plastic
deformation. A tibial diaphyseal fracture with an associated complete
fracture of the fibula usually results in valgus malalignment because
of the action of the muscles in the anterolateral aspect of the leg
(see Figs. 25-11B and 25-12). Any fibular injury must be identified and corrected to minimize the risk of recurrence of angulation after reduction (Fig. 25-13A-C).
 |
|
FIGURE 25-8 (continues)
|
 |
|
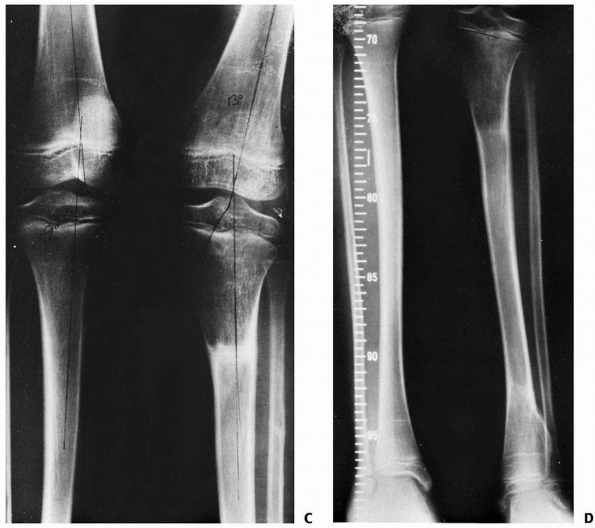
FIGURE 25-9 A. Anteroposterior image of a Salter-Harris type II fracture of the proximal tibia. Notice the valgus alignment. B. This fracture was treated with percutaneous pin fixation after reduction. C. This patient developed tibia valga over a period of approximately 2 years following the injury. D. A medial proximal tibial hemiepiphysiodesis using a staple was performed.
|
 |
|
FIGURE 25-9 (continued)
|
 |
|
FIGURE 25-10 Anteroposterior radiograph of a distal one third tibial fracture without concomitant fibular fracture in a 10-year-old child. A. The alignment in the coronal plane is acceptable (note that the proximal and distal tibial growth physes are parallel). B. A varus angulation developed within the first 2 weeks after injury. C. A 10-degree varus angulation was present after union.
|
 |
|
FIGURE 25-11 A.
Fracture of the middle tibia without an associated fibular fracture tend to shift into varus due to the force created by the anterior compartment musculature of the lower leg and the tethering effect of the intact fibula. B. Fractures involving the middle third of the tibia and fibula may shift into a valgus alignment due to the activity of the muscles in the anterior and the lateral compartments of the lower leg. |
 |
|
FIGURE 25-12 A. Nondisplaced distal tibia fracture with a plastic deformation of the fibula. B. The tibia fracture displaced in a cast 1 week later from the knee exerted by the plastically deformed fibula.
|
children and most commonly results from a direct blow to the lateral
aspect of the leg (Fig. 25-14). Most isolated fractures of the fibular shaft are nondisplaced and heal quickly with symptomatic care and immobilization (Fig. 25-15). Rarely, compartment syndrome may accompany this injury.
fibular diaphyseal fractures vary with the severity of the injury and
the mechanism by which it was produced. Pain is the most common
symptom. Children with fractures of the tibia or fibula have swelling
at the fracture site, and the area is tender to palpation. Almost all
children with a tibia fracture of any type will refuse to ambulate on
that limb. If there is significant injury to the periosteum and
fracture displacement, a bony defect or prominence may be palpable.
Immediate neurologic impairment is rare except with fibular neck
fractures caused by direct trauma.
tibial and fibular diaphyseal fractures, both the dorsalis pedis and
the posterior tibial pulses should be assessed, and a Doppler
examination should be performed if they are not palpable. Capillary
refill, sensation, and pain response patterns, particularly pain with
passive motion, should be monitored. Concomitant soft tissue injuries
must be evaluated carefully. Open fractures must be treated
aggressively to reduce the risk of late complications.
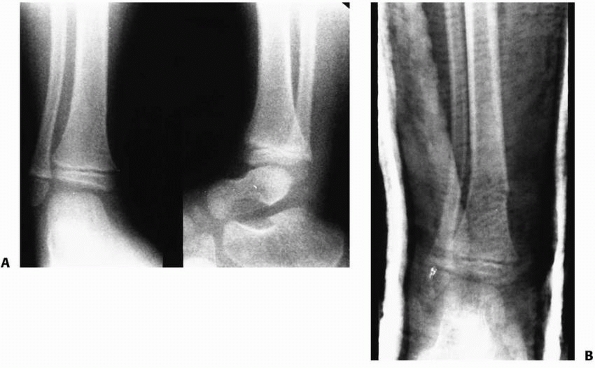
should be obtained whenever a tibial and/or fibular shaft fracture
is/are suspected. While uncommon, tibial shaft fractures may occur in
combination with transitional fractures involving the distal tibial
metaphysis, and as such, close evaluation of the ankle radiographs is
essential (Fig 25-17A-D). Comparison views of the uninvolved leg normally are not indicated. Children with suspected fractures not
apparent on the initial radiographs may need to be treated with
supportive casting to control symptoms associated with the injuries.
Technetium radionuclide scans obtained at least 3 days after injury are
useful to identify fractures that are unapparent on radiographs;
however, in most cases, patients with clinical findings consistent with
a fracture are treated as though a fracture is present. Periosteal new
bone formation on plain radiographs obtained 10 to 14 days after injury
confirms the diagnosis.
 |
|
FIGURE 25-13 A.
Anteroposterior and lateral radiograph of the lower leg in a 12-year-old child showing a comminuted tibial fracture with a concomitant plastic deformation of the fibula. Note the valgus alignment of the tibia. B. This patient had a closed manipulation and casting correcting the valgus alignment in the tibia and partially correcting the plastic deformation of the fibula. C. At union, there is an anatomic alignment of the tibia with a mild residual plastic deformation of the fibula. |
fibular shaft fractures can be treated by manipulation and cast
application.64
Fractures of the tibial shaft without concomitant fibular fracture may
develop varus malalignment. Valgus angulation and shortening can
present a significant problem in children who have complete fractures
of both the tibia and the fibula.
 |
|
FIGURE 25-14 A.
Anteroposterior and lateral radiograph of a 7-year-old child with an isolated open fibula fracture secondary to a bite by a pit bull. B. Anteroposterior radiograph 6 weeks after injury demonstrating consolidation at the fracture site. C. Lateral radiograph showing bridging callus 6 weeks after injury. |
 |
|
FIGURE 25-15
Distal one third fibular fracture in an 8-year-old who was struck on the lateral side of the leg (right). There is moderate new bone formation 6 weeks after injury (left). |
 |
|
FIGURE 25-16 A. Spiral fracture of the distal tibia. The fracture is difficult to identify on the anteroposterior radiograph. B. The fracture is easily identified on the lateral radiograph.
|
 |
|
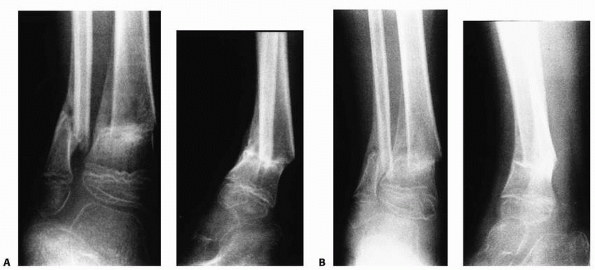
FIGURE 25-17 A. Anteroposterior radiograph of an adolescent patient with a tibial shaft fracture. B-D. Anteroposterior, lateral, and mortise views of the ankle demonstrate an associated triplane fracture.
|
under appropriate sedation, using fluoroscopic assistance when
available. This can be done in the emergency room or in the operating
room. A reduction plan should be made before manipulation based on
review of the deforming forces apparent on the injury radiographs. A
short-leg cast is applied with the foot in the appropriate position
with either a varus or valgus mold, depending on the fracture pattern
and alignment. The cast material is taken to the inferior aspect of the
patella anteriorly and to a point 2 cm distal to the popliteal flexion
crease posteriorly. It may be best to use plaster for the initial cast
because of its ability to mold to the contour of the leg and the ease
with which it can be manipulated while setting. The alignment of the
fracture is reassessed after the short-leg cast has been applied. The
cast is then extended to the proximal thigh with the knee flexed. Most
children with complete, unstable diaphyseal tibial fractures are placed
into a bent-knee (45-degree) long-leg cast to control rotation at the
fracture site and to assist in maintaining
non-weight
bearing status during the initial healing phase. The child’s ankle
initially may be left in some plantar flexion (20 degrees for fractures
of the middle and distal thirds, 10 degrees for fractures of the
proximal third) to prevent apex posterior angulation (recurvatum) at
the fracture site. In a child, there is little risk of developing a
permanent equinus contracture, as any initial plantar-flexion can be
corrected at a cast change once the fracture becomes more stable.
during the first 3 weeks after the cast has been applied. Muscle
atrophy and a reduction in tissue edema may allow the fracture to drift
into unacceptable alignment. Cast wedging may be indicated in an
attempt to improve alignment, and in some cases a second cast
application with remanipulation of the fracture under general
anesthesia may be necessary to obtain acceptable alignment. Acceptable
position is somewhat controversial, and varies based on patient age as
well as location and direction of the deformity.35
Remodeling of angular deformity is limited in the tibia. No absolute
numbers can be given, but the following general principles may be
beneficial in decision making:
-
Varus and valgus deformity in the upper
and midshaft tibia remodel slowly, if at all. Up to 10 degrees of
deformity can be accepted in patients less than 8 years old, and little
more than 5 degrees of angulation in those older than 8 years of age. -
Moderate translation of the shaft of the
tibia in a young child is satisfactory, whereas in an adolescent, at
least 50% apposition is recommended. -
Up to 10 degrees of anterior angulation may be tolerated, although remodeling is slow.
-
Little apex posterior angulation
(recurvatum) can be accepted, as this forces the knee into extension at
heel strike during gait. -
Up to 1 cm of shortening is acceptable.
unacceptable increase in angulation may benefit from remanipulation of
the fracture. This can be attempted in the clinic setting through the
use of cast “wedging.” The fracture alignment in the cast can be
changed by creating a closing wedge, an opening wedge, or a combination
of wedges. Unfortunately, this technique is somewhat labor intensive
and has become something of a lost art. The location for the wedge
manipulation is determined by evaluating the child’s leg under
fluoroscopy and marking the midpoint of the tibial fracture on the
outside of the cast. If fluoroscopy is not available, a series of paper
clips are placed at 2-cm intervals on the cast and anteroposterior and
lateral radiographs are then taken. The paper clips define the location
of the fracture and the location most suitable for cast manipulation.
removed which encompasses 90% of the circumference of the leg with its
base over the apex of the fracture. The exact width of the wedge is
proportional to the amount of correction desired and therefore varies
in each patient. The cast is left intact opposite the apex of the
fracture in the plane of proposed correction. The edges of the cast are
brought together to correct the angulation at the fracture. This
wedging technique may produce mild fracture shortening, and care must
be taken to avoid pinching the skin at the site of cast
reapproximation. Theoretically, the closing wedge technique may
increase exterior constrictive pressure, as the total volume of the
cast is reduced. In light of these concerns, it may be preferable to
use the opening wedge technique whenever possible.
the apex of the fracture is cut perpendicular to the long axis of the
bone. A small segment of the cast is left intact directly over the apex
of the malaligned fracture (~25%). A cast spreader is used to “jack”
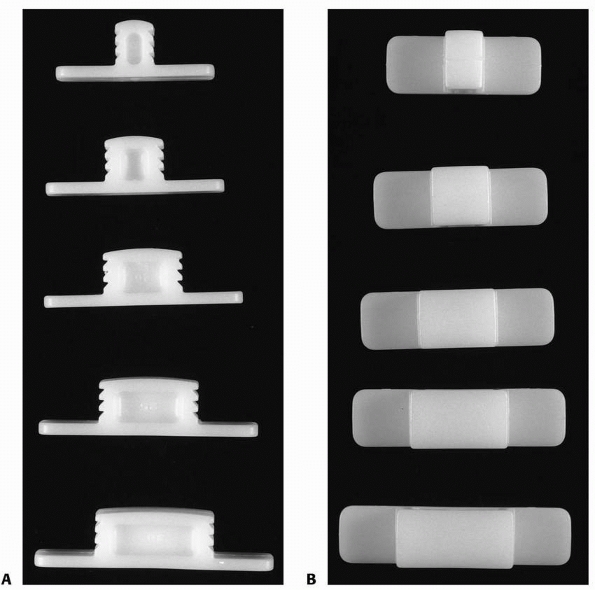
the cast open. Plastic blocks (Fig. 25-18) or a
stack of tongue depressors of the appropriate size are placed into the
open segment to maintain the distraction of the site, and the cast is
wrapped with new casting material after the alignment has been assessed
radiographically (Fig. 25-19). When using any
wedging material, it is imperative that the edges do not protrude into
the cast padding or cause pressure on the underlying skin. This wedging
technique effectively lengthens the tibia while correcting the
malalignment (Figs. 25-20A-D).
opposite the apex of the malaligned fracture is cut perpendicular to
the shaft of the tibia. Two vertical cuts separated by approximately
0.5 cm are made 90 degrees from the first cut in both directions
directly over the fracture. A wedge of casting material is removed from
the apex side of the malaligned fracture and the cast opposite the apex
of the fracture is opened. This closes the defect in the cast over the
apex of the fracture, and produces a change in the angular alignment of
the bone without a significant change in the length of the bone.
reported that only 29 (4.5%) of 638 pediatric tibial fractures in their
study required surgical intervention. However, in the last decade there
has been an increasing interest in surgical stabilization, particularly
for unstable closed tibial shaft fractures as well as open fractures or
those with associated soft tissue injuries. The current indications for
operative treatment include open fractures, some fractures with an
associated compartment syndrome, some fractures in children with
spasticity (head injury or cerebral palsy), fractures in which open
treatment facilitates nursing care (floating knee, multiple long bone
fractures, multiple system injuries), and unstable fractures in which
adequate alignment can not be either attained or maintained.3,9,24,36,40,43,53,68,80
Common methods of fixation for tibial fractures requiring operative
treatment include percutaneous metallic pins, bioabsorbable pins,6 external fixation,28,106,130
and plates with screws, and the use of flexible intramedullary titanium
or stainless steel nails, or in some cases intramedullary Steinmann
pins, is becoming increasingly common.44,48,49,88,106,108,117,125,148 Kubiak et al.88
compared use of titanium flexible nails with external fixation in a
mixed group of patients with open and closed tibia fractures. While the
groups were not matched and were reviewed retrospectively, the authors
reported a clinically significant decrease in time to union with
titanium nails versus external fixation. Gordon et al.49
retrospectively reviewed 60 pediatric patients with open or closed
tibial shaft fractures managed with flexible nails. They found an 18%
complication
rate;
the most common complication was delayed union. In this study, those
patients with delayed time to union tended to be older (mean age 14.1
years) versus the mean age of the study population (11.7 years).
 |
|
FIGURE 25-18 A,B.
Blocks used to hold casts open after wedge corrections of malaligned fractures. The wings on the blocks prevent the blocks from migrating toward the skin. |
 |
|
FIGURE 25-19
Comminuted fracture of the tibia and fibula in a 12-year-old boy struck by a car (left). Notice the extension of the fracture into the metaphysis from the diaphyseal injury. The fracture is in a valgus alignment. The fracture could not be maintained in an acceptable alignment (right). The cast was wedged with excellent result. |
to comparable injuries in adults, and likewise, are classified by the
Gustillo and Anderson System (Table 25-4 and Fig. 25-21).56 Most open fractures of the tibia result from high-velocity/high-energy injuries.
-
Timely débridement, irrigation, and initiation of appropriate antibiotic therapy
-
Fracture reduction followed by stabilization with either an internal or external device
-
Intraoperative angiography (after rapid
fracture stabilization) and management of possible elevation of
compartment pressures when sufficiency of the vascular perfusion is
unclear -
Open wound treatment with loose gauze packing or other methods28,104
-
Staged débridement of necrotic soft
tissue and bone in the operating room as needed until the wounds are
ready for closure or coverage. -
Delayed closure or application of a split
thickness skin graft when possible; use of delayed local or free
vascularized flaps as needed -
Closed cancellous bone grafting for bone defects or delayed union after maturation of soft tissue coverage
 |
|
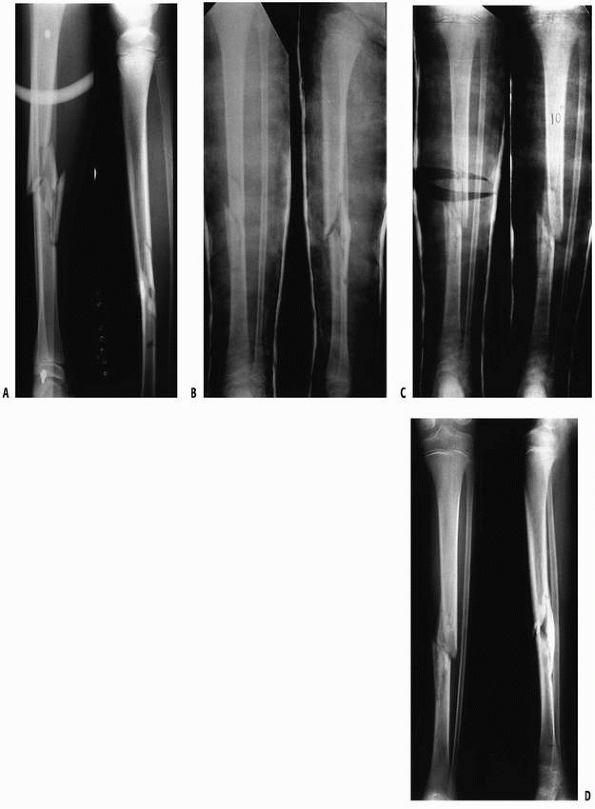
FIGURE 25-20 A.
Anteroposterior and lateral tibial radiographs of an 11-year-old boy who was struck by an automobile, sustaining a markedly comminuted tibial fracture without concomitant fibular fracture. B. Despite the comminution, length and alignment were maintained in a cast. C. The patient’s fracture shifted into a varus malalignment that measured 10 degrees (right). The cast was wedged, resulting in the re-establishment of an acceptable coronal alignment (left). D. The patient’s fracture healed without malunion. |
adults have been modified by the unique characteristics of the
pediatric skeleton. These differences include the following3,24,48,55,138:
-
Comparable soft tissue and bony injuries
heal more reliably in children than in adults, particularly in patients
less than 11 years of age.75 -
Devitalized uncontaminated bone that can
be covered with soft tissue can incorporate into the fracture callus,
and in some cases may be left within the wound. -
External fixation can be maintained, when
necessary, until fracture consolidation with fewer concerns about
delayed or nonunions. -
Retained periosteum can reform bone even after segmental bone loss in younger children.
-
After a thorough irrigation and
débridement, many uncontaminated grade I open wounds may be closed
primarily without an increased risk of infection.
reported 41 children with 42 open fractures of the tibia (18 grade II,
6 grade IIIA, 4 grade IIIB, and 2 grade IIIC). Twenty-two (52%) of the
fractures were comminuted. All wounds were irrigated and débrided, and
antibiotics were administered for at least 48 hours. Twenty-two
fractures were treated with reduction and cast application, and 20 with
external fixation. Three children had early infections, and one of
these patients developed late osteomyelitis. All infections had
resolved at final reported follow-up. The average time to union was 5
months (range, 2 to 21 months). The time to union was directly
proportional to the severity of the soft tissue injury. Fracture
pattern also had an effect on time to union. Segmental bone loss,
infection, and the use of an external fixation device were associated
with delayed union. Four angular malunions of more than 10 degrees
occurred, three of which spontaneously corrected. Four children had
more than 1 cm of overgrowth.
(1 grade I, 10 grade II, and 11 grade III). External fixation was used
for 15 fractures, casting for five, and internal fixation for two. Two
children required early amputation, four required soft tissue flap
coverage, and 13 children had skin grafts. Two additional children with
initially closed injuries required fasciotomy for compartment syndrome
and were included in the group of open tibial fractures. Ten of the 24
injuries healed within 24 weeks. Five children required bone grafting
before healing.
|
TABLE 25-4 Classification of Open Fractures
|
||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||
reported the results of open tibial fractures in 92 children (22 grade
I, 51 grade II, and 19 grade III). Irrigation and débridement were
performed on admission, antibiotics were given for 48 hours, and
tetanus prophylaxis was administered when necessary. Primary closure
was performed in 51 children, and 41 fractures were left open. Eighteen
soft tissue injuries healed secondarily, and 23 required either a split
thickness skin graft or a tissue flap. Sixty-five (71%) of the 92
fractures were reduced and immobilized in an above-the-knee plaster
cast. External fixation was used for unstable fractures, injuries with
significant soft tissue loss, and fractures in patients with multiple
system injuries. Early complications of open tibial fractures in these
children were comparable with those in adults (Table 25-5).9,14,17,20,29,57,63,65,90,107,114,127 Primary closure did not increase the risk of infection if the wound was small and uncontaminated.3,24,65 At reevaluation 1.5 to 9.8 years after injury, the authors23
found that 50% of the patients complained of pain at the fracture site;
23% reported decreased abilities to participate in sports, joint
stiffness, and cosmetic defects; and 64% had leg length inequalities (Table 25-6). Levy et al.93
found comparable late sequelae after open tibial fractures in children,
including a 25% prevalence of nightmares surrounding the events of the
accident. Blasier and Barnes8 and Song et al.138
found that most late complications associated with pediatric open
tibial fractures occurred in children over the age 12 and 11 years,
respectively.
reviewed their experience with open tibial fractures and found no
increased incidence of infection in patients initially débrided more
than 6 hours after injury when compared to children treated similarly
less than 6 hours after fracture. However, it appears that fractures
with more severe soft tissue injuries were more likely to receive more
expedient treatment, thereby complicating the analysis. This apparent
selection bias in some ways limits the overall usefulness of the study.
use of external fixators in tibia fractures in pediatric patients.
Myers et al.106 reviewed 31
consecutive high-energy tibia fractures in children treated with
external fixation. Nineteen of the fractures were open, with mean
follow-up of 15 months. The authors found a high rate of complications
in this patient population, including delayed union (particularly in
patients of at least 12 years of age), malunion, leg-length
discrepancy, and pin track infections. To date, there are no published
studies which directly and prospectively compare use of flexible
intramedullary nails with external fixation for open pediatric tibial
shaft fractures.
Delayed primary closure can be performed if the wound is clean and does
not involve significant muscle loss. In such cases, it is imperative
that closure under tension is avoided. Other options include a wide
variety of local rotational or pedicled myocutaneous flaps.
Vascularized free flaps are viable options in cases for which no other
method of closure is appropriate.
tissue coverage for open tibia fractures involves adult patients, and
as such, must be extrapolated to pediatric fracture management. In a
series of 168 open tibial fractures with late secondary wound closure,
Small and Mollan136 found increased
complications with early pedicled or rotational fasciocutaneous flaps
and late free flaps, but no complications with fasciocutaneous flaps
created more than 1 month after injury. Complications associated with
free flaps were decreased if the procedure was performed within 7 days
of injury. Hallock et al.60 reviewed
11 free flaps for coverage in pediatric patients. They reported a 91%
success rate, which was similar to their rate in adults. However, they
reported a significant rate of complications at both the donor and the
recipient sites.60 Rinker et al.118
reported their experience with free vascularized muscle transfers for
traumatic lower extremity trauma in pediatric patients performed
between 1992 and 2002. At their institution, 26 patients received 28
flaps during that period. The latissimus dorsi was used most commonly
as the origin of the transfer. Twelve of the flaps were performed for
coverage of open tibia fractures. There was a 62% overall complication
rate, with infection and partial skin-graft loss being the most common
problems. The authors concluded that patients receiving free flap
coverage within 7 days of injury had a statistically significant lower
complication rate than those covered later.118
were treated with early broad-spectrum antibiotics, serial
débridements, and the application of an external fixation device.
Tobramycin-impregnated polymethylmethacrylate was placed into the
wounds, and dressings were changed every 48 to 72 hours until the
wounds spontaneously closed, underwent delayed primary closure, or
received flap coverage. No infections occurred in grade I fractures;
approximately 3% of grade II fractures and 8% of grade III fractures
developed infections. No infections occurred in patients who had the
wound closed within 8 days of injury. On the basis of these and other
analyses, it now is recommended that wounds associated with open tibial
fractures be covered within 7 days of injury whenever possible.16,17,19,79,85,111,149
 |
|
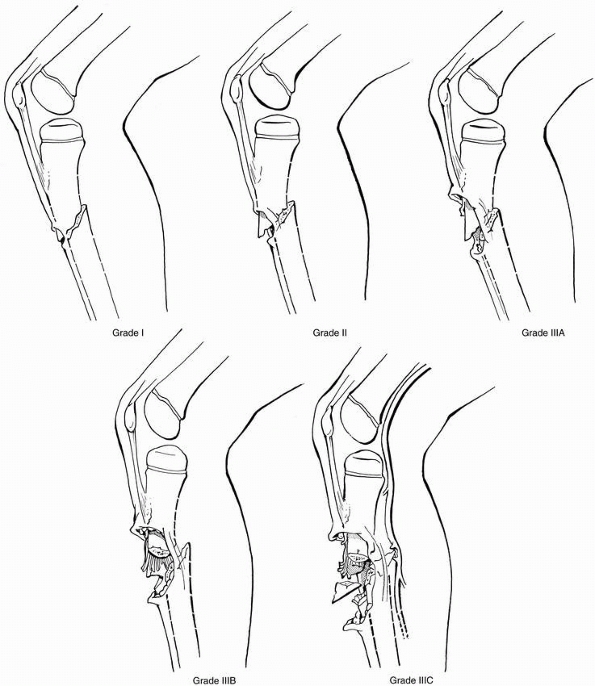
FIGURE 25-21
Gustilo and Anderson classification of open fractures. Grade I: The skin wound measures less than 1 cm long, usually from within, with little or no skin contusion. Grade II: The skin wound measures more than 1 cm long, with skin and soft tissue contusion but no loss of muscle or bone. Grade IIIA: There is a large severe skin wound with extensive soft tissue contusion, muscle crushing or loss, and severe periosteal stripping. Grade IIIB: Like grade IIIA but with bone loss and nerve or tendon injury. Grade IIIC: Like grade IIIA or B with associated vascular injury. (From Alonso JE. The initial management of the injured child: musculoskeletal injuries. In: MacEwen GD, Kasser J, Heinrich SD, eds. Pediatric Fractures: A Practical Approach to Assessment and Treatment. Baltimore: Williams & Wilkins, 1993:32, with permission.) |
|
TABLE 25-5 Early Complications Associated with Open Pediatric Tibial Fractures
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||
subatmospheric pressure dressings in the management of soft tissue
injuries in pediatric patients. Dedmond et al.28
reviewed the Wake Forest experience with negative pressure dressings in
pediatric patients with type 3 open tibia fractures. They found that
use of this device decreased the need for free tissue transfer to
obtain coverage in this patient population.
|
TABLE 25-6 Late Complications Associated with Open Pediatric Tibia Fractures
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
of children with open tibial fractures. Arterial injuries associated
with open tibial fractures include those to the popliteal artery, the
posterior tibial artery, the anterior tibial artery, and the peroneal
artery. Complications are common in patients with open tibial fractures
and associated vascular injuries. Amputation rates as high as 79% have
been reported with grade IIIC fractures. Isolated anterior tibial and
peroneal artery injuries generally have a good prognosis, whereas
injuries of the posterior tibial and popliteal arteries have much less
satisfactory prognoses, and more commonly require vascular repairs or
reconstructions.1,59,65
Patients with open tibial fractures and vascular disruption may benefit
from arterial, and possibly venous, shunting before the bony
reconstruction is performed. This allows meticulous débridement and
repair of the fracture and maintains limb perfusion until the primary
vascular repair is performed.43
However, in most cases, rapid fracture stabilization, usually utilizing
external fixation, can be performed prior to vascular reconstruction
without the need for temporary shunts.
The true incidence of compartment syndrome associated with open
pediatric tibial fractures is unknown. Regardless, it is important to
remember that compartment syndrome may occur in the face of significant
soft tissue injury associated with extensively open fractures, as well
as with closed injuries. Compartment pressures should be measured in
all cases in which history and physical examination findings raise
suspicion. In children, the cardinal initial finding is progressive
pain in the limb, often signaled by increasing narcotic requirements.
Signs such as motor and sensory deficits and loss of pulses are later
findings. Unfortunately, despite physician experience and vigilance,
compartment syndrome may be missed in pediatric patients.
Fasciotomy(ies) is/are indicated for any patient with a significant
elevation of compartment pressures or, more importantly, symptoms
suggestive of a compartment syndrome. A more detailed review of the
pathophysiology, diagnosis, and management of compartment syndrome will
be found in the later section regarding complications of closed,
diaphyseal tibia fractures.
quickly in most cases, and cast immobilization can be used without
affecting the long-term range of motion of the knee and the ankle. A
bent-knee, long-leg cast provides maximal comfort to the patient and
controls rotation of the fractured fragments. Children with
nondisplaced or minimally displaced
fractures
that do not require manipulation generally do not need to be admitted
to the hospital. Children with more extensive injuries should be
admitted for neurovascular observation and instruction in wheelchair,
crutch, or walker use.
|
TABLE 25-7 Acceptable Alignment of a Pediatric Diaphyseal Tibial Fracture
|
|||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
surrounding soft tissues and produce a large hematoma in the fascial
compartments of the lower leg. Circulation, sensation, and both active
and passive movement of the toes should be monitored carefully after
injury. The child should be admitted to the hospital, and reduction
should be performed with adequate sedation and fluoroscopy if
available. Most fractures are casted after reduction, and the cast may
be bivalved or split to allow room for swelling. The fracture must be
evaluated clinically and radiographically within a week of manipulation
to verify maintenance of the reduction. The cast can be wedged to
correct minor alignment problems. Significant loss of reduction
requires repeat reduction with adequate anesthesia (Table 25-7)
and/or utilization of a more rigid fixation method. The long-leg cast
may be changed to a short-leg, weight-bearing cast at 4 to 6 weeks
after injury. Children over 11 years of age may be placed into a
patellar tendon-bearing cast after removal of the long-leg cast.127 Weight-bearing immobilization is maintained until sufficient callus is evident.
 |
|
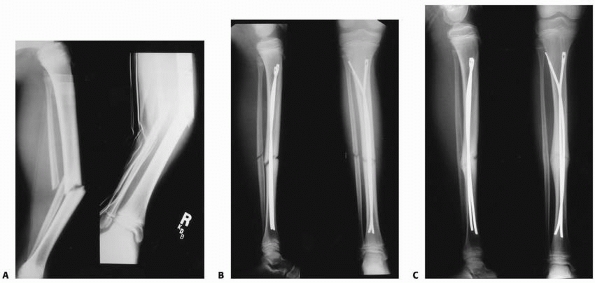
FIGURE 25-22 A.
Anteroposterior and lateral radiographs of a 12-year-old who was involved in a motor vehicle accident sustaining a grade I open middle one third tibial and fibular fractures. B. This injury was treated with intramedullary nail fixation. C. At union, the patient has an anatomic alignment and no evidence of a growth disturbance. |
including spasticity, a floating knee, multiple long-bone fractures, an
associated transitional ankle fracture, extensive soft tissue damage,
multiple system injuries, or an inability to obtain or maintain an
acceptable reduction should be stabilized with a more rigid fixation
method, such as external fixation, percutaneous Kirschner wires, or
flexible intramedullary nails (Figs. 25-22 and 25-23).
thorough and expedient irrigation and débridement of the wound,
although there is some evidence that infection rate is similar in
injuries managed at less than 6 hours after injury and those treated
later.134 The patient’s tetanus
status is determined, and prophylaxis is administered as indicated.
Appropriate intravenous antibiotic treatment is initiated as soon as
possible and maintained as required based on the severity of the open
fracture. The soft tissue wounds should be extended to be certain that
the area is cleansed and débrided of all nonviable tissue and foreign
material. Devitalized bone can be left in place if it is clean and can
be covered by soft tissue. The operative wound extension may be closed
along with the open segment in clean grade I injuries. The wound is
allowed to heal by secondary intention if there is moderate
contamination after irrigation and débridement. Patients with
uncomplicated grade I fractures can be placed in a splint or a cast, or
simple smooth pin fixation will prevent displacement
of many unstable fractures (Fig. 25-24).
Use of this limited fixation does not preclude supplemental splinting
or casting. Wounds associated with grade II and III fractures are
débrided of devitalized tissue and foreign material. Most children with
grade II and all children with grade III wounds require more rigid
fracture stabilization, usually with external fixation, although
intramedullary nails may be used at the surgeon’s discretion. More
rigid fixation limits the need for significant external splinting,
thereby allowing better access for wound care and sequential
compartment evaluation as needed.
 |
|
FIGURE 25-23
Anteroposterior radiograph of a 14-year-old who was involved in a motor vehicle accident sustaining a distal one third tibial fracture and comminuted distal fibular fracture. This was stabilized with titanium elastic nails. |
 |
|
FIGURE 25-24 A. Anteroposterior radiograph of a grade I open distal one-third tibial fracture in a 7-year-old child. B. Two percutaneous pins were used to stabilize this fracture after irrigation and débridement. C. Good fracture callus was present and the pins were removed 4 weeks after injury.
|
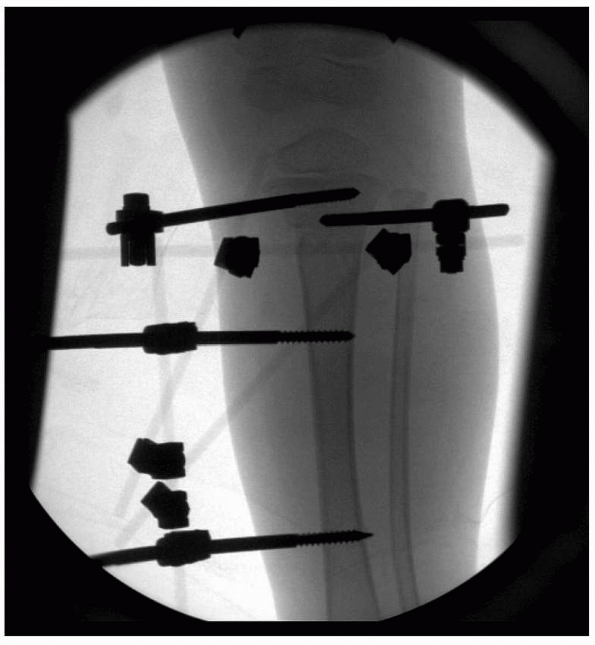
The unilateral frame is easy to apply and allows minor corrections in
angular alignment and length. Secondary pins can be used for added
support (Fig. 25-26); these are connected to
the standard pins or the body of the external fixation device. This
allows control of segmental fragments as needed. Fracture reduction
tools can be applied to the pin clamps to assist in manipulating the
fracture. A small-pin or thin-wire circular frame may be indicated for
complicated fractures adjacent to the joint. Unilateral frames may be
placed to span the joint in question so as to use ligamentotaxis as an
indirect reduction method to establish and maintain alignment (Fig. 25-27).
closer than 1 cm to the physis. The external fixation device is
applied, and a reduction maneuver is performed. All of the connections
in the external fixation device are tightened after reduction has been
obtained. Secondary pins to improve fracture stability are placed at
this time. Limited internal fixation of the fracture can be used to aid
in controlling fracture alignment. A posterior splint may be applied to
prevent the foot from dropping into plantarflexion. This splint should
be easy to remove for subsequent pin care and dressing changes of the
open injury. Splinting of this type can be avoided by external
fixation, be it unilateral or circular, to the forefoot.
children using prebent stainless steel Enders nails or elastic titanium
nails. In almost all cases, the implants are placed in
a
proximal to distal fashion from medial and lateral proximal insertion
points. Fluoroscopy is required for accurate placement. Care must be
taken to avoid injury to the proximal tibial physes, including the
tibial tubercle apophysis. Use of supplemental external splinting is at
the discretion of the treating surgeon.
 |
|
FIGURE 25-25 A,B.
Type II open fracture of the tibia in a 5-year-old boy treated with débridement, unilateral external fixation, and split thickness skin graft. C. Four months after removal of the external fixation. |
 |
|
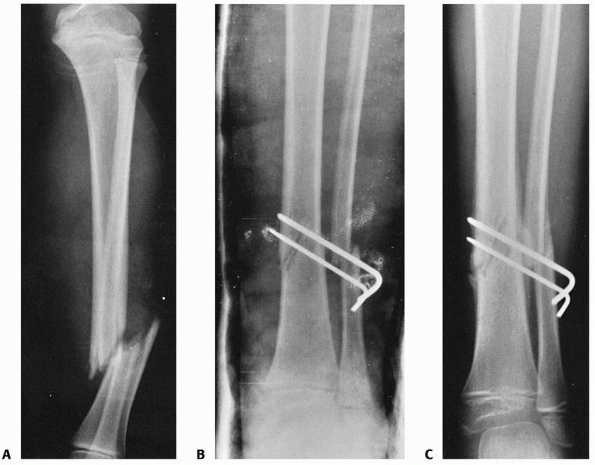
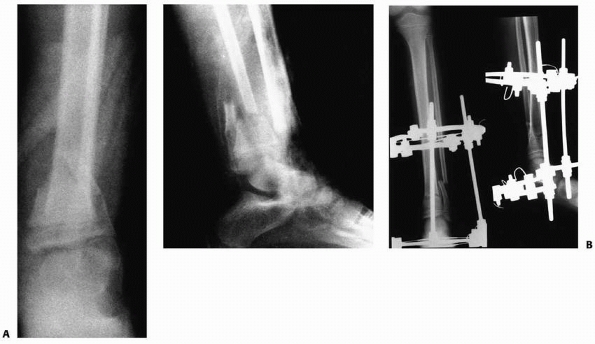
FIGURE 25-26 A.
Anteroposterior and lateral radiographs of the tibia of a 12-year-old boy who was struck by a car. This child sustained a grade IIIB open middle one third tibial fracture, a Salter-Harris type II fracture of the distal tibial physis with associated distal fibular fracture (closed arrows), and a tibial eminence fracture (open arrow). B. Irrigation and débridement and application of an external fixation device were performed. C. The fracture of distal tibial physis was stabilized with a supplemental pin attached to the external fixation device. Open reduction and internal fixation of the fibula was performed to enhance the stability of the external fixator in the distal tibia. D. Anteroposterior and lateral radiogrphs of the tibia approximately 9 months after injury demonstrate healing of the tibial eminence fracture, the comminuted middle one third tibial fracture, and the distal tibial physeal fracture. The distal tibial physis remains open at this time. |
 |
|
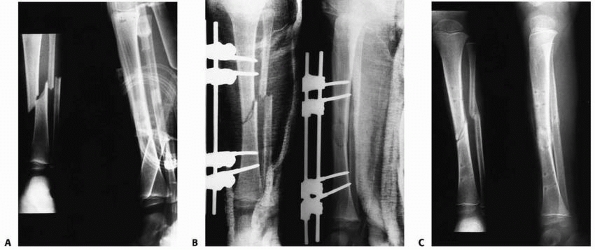
FIGURE 25-27 A. Anteroposterior and lateral radiographs of a grade IIIB open fracture of the distal tibia and fibula. B.
Anteroposterior and lateral radiographs after fracture reduction and stabilization with an Ilizarov circular fixation frame. (From Sharps CH, Cardea JA. Fractures in the shaft of the tibia and fibula. In: MacEwen GD, Kasser J, Heinrich SD, eds. Pediatric Fractures: A Practical Approach to Assessment and Treatment. Baltimore: Williams & Wilkins, 1993:325, with permission.) |
and the type of fracture. The duration of immobilization was 8 to 10
weeks in the Steinert and Bennek series.142 Hansen et al.61
found that healing time ranged from 5 to 8 weeks for “fissures and
infractions” and from 5 to 13 weeks for oblique, transverse, and
comminuted fractures. Hoaglund and States63
reported that in 43 closed fractures in children, the average time in a
cast was 2.5 months (range, 1.5 to 5.5 months), whereas the 5 children
with open fractures were immobilized for 3 months.
found an average time to union of 5.4 months (range, 1.5 to 24.8
months) in a series of 56 open tibial fractures in 55 children. The
factor with the most effect on union time was the age of the patient.
Grimard et al.55 reported that the
age of the patient and the grade of the fracture were significantly
associated with union time. Blasier and Barnes8
found that children under 12 years of age required less aggressive
surgical treatment and healed faster than older children. They also
found that younger children were more resistant to infection and had
fewer complications than older children.
extensive rehabilitation. In the vast majority of cases, normal walking
and running activities serve as therapy. Most children limp with an
out-toeing rotation gait on the involved extremity for several weeks to
a month after the cast is removed. This is secondary to muscle
weakness, joint stiffness, and a tendency to circumduct the limb during
swing phase, rather than a malalignment of the fracture. As the muscle
atrophy and weakness resolve, the limp improves. In very rare
situations, formal physical therapy may be required for some children
after a tibial fracture. Knee range-of-motion exercises and quadriceps
strengthening may be useful in an older child progressing from a
bent-knee cast to weight bearing on a short-leg cast. Progressive
weight bearing on a short-leg cast requires the patient to wean off
crutches or a walker. In some children, this requires supervision. The
child may return to sports when the fracture is healed and the patient
has regained strength and function comparable to that of the uninjured
leg.
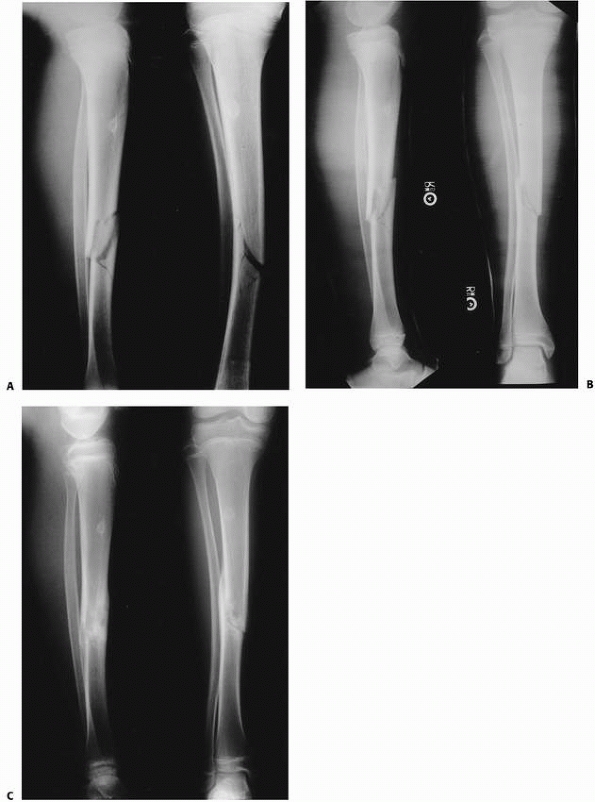
greenstick injuries resulting from increased compressive forces along
the anterior tibial cortex. The anterior cortex is impacted while the
posterior cortex is displaced under tension, with a tear of the
overlying periosteum. A recurvatum deformity may occur (Fig. 25-28).
Reduction of these injuries should be performed with adequate sedation
and maintained with a long-leg cast. The foot should be left in
moderate plantarflexion to prevent recurrence of apex posterior
angulation at the fracture site. The foot is brought up to neutral
after 3 to 4 weeks, and a short-leg walking cast is applied. Unstable
injuries can be treated with percutaneous pins (Fig. 25-29), antegrade flexible nails, or with open reduction and internal fixation as needed (Fig. 25-30).
Open reduction and internal fixation of the distal fibula, if
fractured, may prevent malalignment in an unstable distal tibia
fracture.37
 |
|
FIGURE 25-28 A. Fracture of the distal tibia in a 7-year-old child. The lateral radiograph demonstrates a mild recurvatum deformity. B.
The ankle was initially immobilized in an ankle neutral position, producing an increased recurvatum deformity. The cast was removed and the ankle remanipulated into plantarflexion to reduce the deformity. C. The ankle was then immobilized in plantarflexion, which is the proper position for this type of fracture. |
 |
|
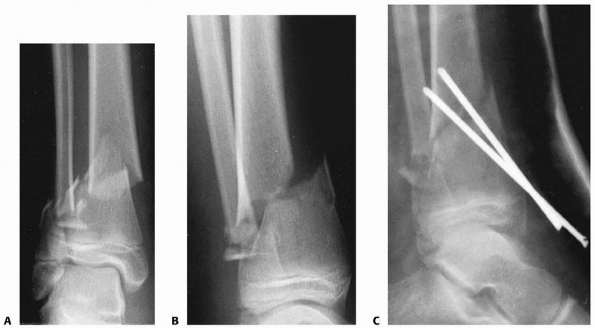
FIGURE 25-29 A,B. Unstable distal metadiaphyseal fractures of the tibia and fibula in a 15-year-old girl. C. This fracture was stabilized with percutaneous pins because of marked swelling and fracture instability.
|
 |
|
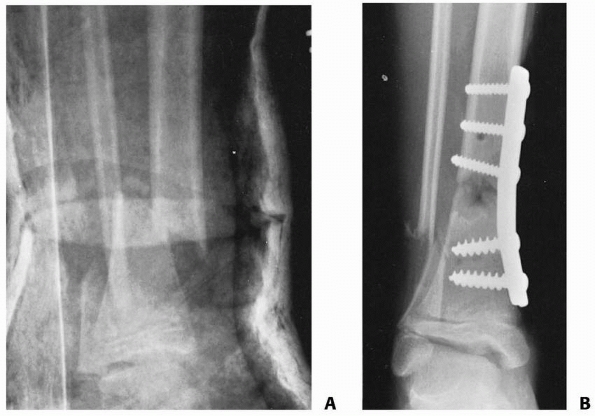
FIGURE 25-30 A.
Anteroposterior radiograph of a distal one-third tibial and fibular fractures in a 9-year-old girl with a closed head injury and severe spasticity. The initial reduction in a cast could not be maintained. B. Open reduction and internal fixation with a medial buttress plate was used to achieve and maintain the alignment. |
fracture, ranging from a seemingly minor closed fracture to a severe,
comminuted fracture.91 Schrock131
described compartment syndromes after derotational osteotomies of the
tibia in children, and compartment syndrome is a well known
complication of tibial osteotomy for angular correction.
four compartments of the lower leg after trauma. Hemorrhage and soft
tissue edema produce an elevation in the pressure within the myofascial
compartment that impairs venous outflow. The small arterioles leading
into the compartment become less efficient in delivering blood as
venous outflow becomes occluded, and the vessels themselves become more
permeable. The arterioles and capillaries close when the pressure in
the compartment exceeds the pressure in the vessels with resultant
ischemia of the surrounding soft tissue. Because tissue pressures can
be elevated enough to produce an ischemic injury, but not high enough
to occlude arterial inflow, the presence of peripheral pulses is
unreliable evidence of adequate tissue perfusion.
pain out of proportion to the apparent severity of the injury. This
increasing pain, often noted as increasing analgesic requirements, is
the most important early sign of potential compartment syndrome in
children. The compartment is firm to palpation. The patient may have a
sensory deficit in the distribution of the nerves that traverse the
compartment. Weakness of the muscles within the involved compartment
and pain on passive motion of those muscles are common. Paralysis of
the muscles in the involved compartment is a late finding. Pain with
passive range of motion appears to be an early and strong clinical
finding. As an example, patients with a compartment syndrome involving
the deep posterior compartment have severe pain that increases with
passive extension of the toes, plantar hyperesthesias, and weakness of
toe flexion.97 Late complications of
untreated lower extremity compartment syndrome include clawed toes, a
dorsal bunion, and limited subtalar motion secondary to necrosis and
subsequent fibrous contracture of the muscles originating in the deep
posterior compartment.78
 |
|
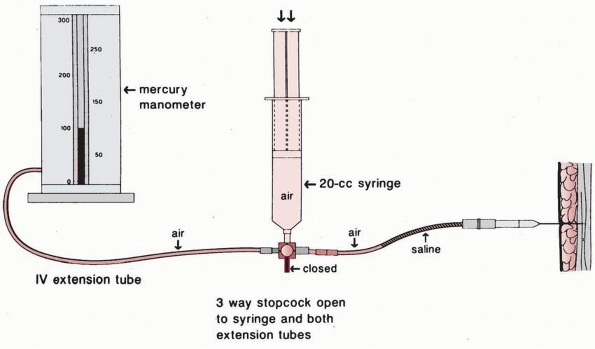
FIGURE 25-31
The Whitesides technique for measuring intracompartmental pressure. (From Whitesides TE, Hanley TC, Morinotok K, et al. Tissue pressure measurement as a determinant for the need for fasciotomy. Clin Orthop Relat Res 1975;113:43, with permission.) |
level of the fracture provide the most accurate assessment of
compartment conditions in those with clinically suspected compartment
syndrome and allow early fasciotomy to reduce the pressure. Whitesides
et al.152 designed an inexpensive apparatus that permitted accurate measurement of compartment tissue pressure (Fig. 25-31).
Small, portable devices or even an arterial monitoring set-up in the
operating room are available to measure compartment pressures and are
used most commonly at this time. When measuring compartment pressure in
the leg after a tibial fracture, accurate placement of the needle is
essential. Multiple measurements should be performed at different sites
and depths within each compartment, due to apparent variations of
pressure through the compartment.
leg is approximately 0 to 5 mm Hg. A small study of normal children
demonstrated that baseline lower limb compartment pressures are higher
(13 to 16 mm Hg).140 The clinical
application of this information is unclear at this time. Compartment
blood inflow is decreased at 20 mm Hg, and prolonged pressures of 30 to
40 mm Hg, or within 30 mm Hg of diastolic blood pressure, may cause
severe nonreversible injury to the muscles within a fascial compartment
Vascular flow ceases in the microcirculation of an extremity muscular
compartment by the time tissue pressures within the closed compartment
reaches the diastolic blood pressure.
patient with increased or increasing pain. If, after removal of all
encircling wraps, there is no relief, compartment syndrome should be
considered. Any child who has objective or subjective evidence of a
compartment syndrome should undergo an emergent fasciotomy. While there
is some controversy in the literature, symptomatic patients with
compartment pressures greater than 30 mm Hg may benefit from fasciotomy.73,152 In addition, release should be considered strongly if compartment pressures
are within 20 to 30 mm Hg of the diastolic pressure. This is especially
critical in the hypotensive patient or those unable to communicate or
undergo reliable serial examinations for any reason. In a dog model of
ischemia, irreversible injury to muscles and nerves begins after
approximately 5 hours.132
How this animal data relates to children is unclear, but certainly the
surgeon should assure rapid compartment release if muscle ischemia is
suspected. Hyperesthesia, motor defects, and decreased pulses are late
changes and denote significant tissue injury. These signs occur only
after the ischemia has been well established and the injury is
permanent.78,152
fasciotomies, although a single incision, perifibular release is
favored at some centers (Fig. 25-32A,B).98
In the two-incision method, one incision is anterolateral and the
second posteromedial. The fascia surrounding each of the four
compartments should be opened widely. The wounds are left open and a
delayed primary closure is performed when possible. Split thickness
skin grafting of the wounds may be necessary in some cases. Fibulectomy
has been recommended by some as a means by which all four compartments
can be released through a single approach. Most literature does not
support its use, and this procedure should not be performed in
skeletally immature patients. Subsequent shortening of the fibula may
occur, which can produce a valgus deformity at the ankle. Long-term
significant ankle valgus may result in external tibial torsion, gait
impairment, and potentially problematic foot and ankle deformity.22,32
uncommon in children; however, when they do occur, the sequelae can be
devastating. In an evaluation of 14 patients with lower extremity
fractures and concomitant vascular injuries, Allen et al.1
noted that only three children returned to normal function. One factor
leading to a poor outcome was a delay in diagnosis. Evaluation for
vascular compromise is imperative (during the primary and secondary
trauma surveys) in all children with tibial fractures.
 |
|
FIGURE 25-32 A.
Decompressive fasciotomies through a two-incision approach. The anterior lateral incision allows decompression of the anterior and lateral compartments. The medial incision allows decompression of the superficial posterior and the deep posterior compartments. B. A one-incision decompression fasciotomy can be performed through a lateral approach that allows a dissection of all four compartments. |
vascular injury is that of the proximal metaphysis. The anterior tibial
artery is in close proximity to the proximal tibia as it passes between
the fibula and the tibia into the anterior compartment.59,65
Distal tibial fractures also are associated with injuries to the
anterior tibial artery. In these fractures, the vessels are injured
when the distal fragment is translated posteriorly. Posterior tibial
artery injuries are rare, except in fractures associated with crushing
or shearing due to accidents involving heavy machinery, or those
secondary to gunshot wounds involving the lower leg and ankle region.
after a diaphyseal fracture of a child’s forearm or femur is common.
Remodeling of a angulated tibial shaft fracture, however, often is
incomplete (Fig. 25-33).11 As such, the goal of treatment should be to obtain as close to an anatomic alignment as possible. Swaan and Oppers144
evaluated 86 children treated for fractures of the tibia. The original
angulation of the fracture was measured on radiographs in the sagittal
and frontal projections. Girls 1 to 8 years of age and boys 1 to 10
years of age demonstrated moderate spontaneous correction of residual
angulation after union. In girls 9 to 12 years of age and boys 11 to 12
years of age, approximately 50% of the angulation was corrected. No
more than 25% of the deformity was corrected in children over 13 years
of age.
26 of 28 children with varus or valgus deformities at union had
significant residual angular deformities at follow-up. Valgus
deformities had a worse outcome because the tibiotalar joint was left
in a relatively unstable position. Weber et al.151
demonstrated that a fracture with varus malalignment of 5 to 13 degrees
completely corrected at the level of the physis. Most children with
valgus deformities of 5 to 7 degrees did not have a full correction.
 |
|
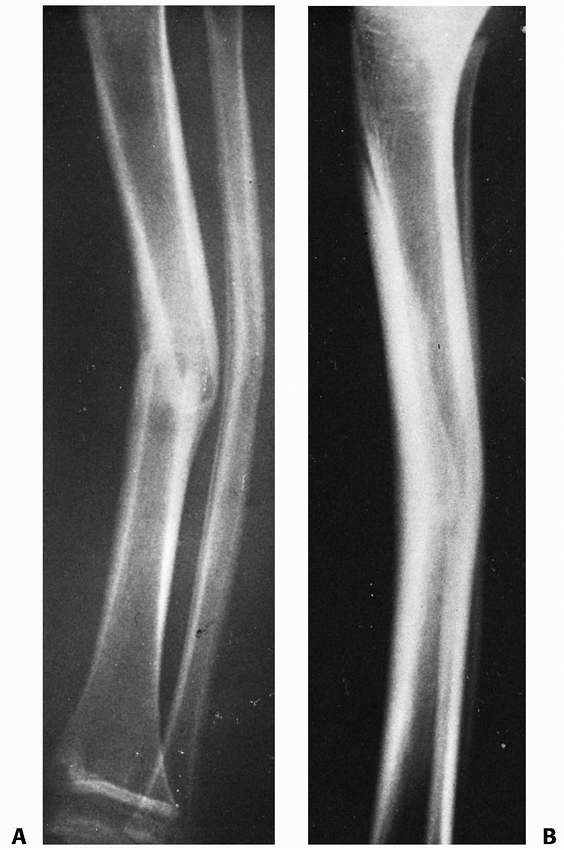
FIGURE 25-33 A 50-month-old child with a middle one-third transverse tibial fracture and a plastically deformed fibular fracture. A. Lateral view shows 20-degree posterior angulation. B. The deformity is still 15 degrees 4 years after the injury.
|
 |
|
FIGURE 25-34 A.
Anteroposterior and lateral radiographs 2 months after injury in a 6-year-old boy reveal a valgus and anterior malunion at the fracture. B. One year later, the child still has a moderate valgus and anterior malalignment of the distal fractured segment. This malalignment produced painful hyperextension of the knee at heel strike during ambulation. |
reported 102 pediatric tibial fractures, 25 of which had malunions of 4
to 19 degrees. Residual angular malunions ranged from 3 to 19 degrees
at final follow-up, without a single patient having a complete
correction. The spontaneous correction was approximately 13.5% of the
total deformity. Shannak133 reviewed
the results of treatment of 117 children with tibial shaft fractures
treated in above-the-knee casts. Deformities in two planes did not
remodel as completely as those in a single plane. The least correction
occurred in apex posterior angulated fractures, followed by fractures
with valgus malalignment (Fig. 25-34). Spontaneous remodeling of malunited tibial fractures in children appears to be limited to the first 18 months after fracture.61
any malrotation should be avoided. A computerized tomographic
evaluation of tibial rotation can be performed if there is any question
about the rotational alignment of the fracture that can not be
determined on clinical examination.
significant functional impairment and necessitate a late derotational
osteotomy of the tibia. Most commonly, derotational osteotomy of the
tibia is performed in the supramalleolar aspect of the distal tibia.
The tibia is osteotomized, rotated, and internally fixed. The fibula
may be left intact, particularly for planned derotation of less than 20
degrees. Maintaining continuity of the fibula adds stability and limits
the possibility of introducing an iatrogenic angular deformity to the
tibia.
the physes in the involved leg, producing growth acceleration. Tibial
growth acceleration after fracture is less than that seen after
femoral fractures in children of comparable ages. Shannak133
showed that the average growth acceleration of a child’s tibia after
fracture is approximately 4.5 mm. Comminuted fractures have the
greatest risk of accelerated growth and overgrowth.
reported that young children have a greater chance for overgrowth than
older children. Accelerated growth after tibial fracture generally
occurs in children under 10 years of age, whereas older children may
have a mild growth inhibition associated with the fracture.61
The amount of fracture shortening also has an effect on growth
stimulation. Fractures with significant shortening have more physeal
growth after fracture union than injuries without shortening at union.100 The presence of angulation at union does not appear to affect the amount of overgrowth.53
reported closure of the anterior tibial physis after fracture in two
children. Both patients sustained a comminuted fracture of the tibial
diaphysis without a concomitant injury of the knee. The fractures were
reduced and stabilized with Kirschner wires reportedly placed distal to
the tibial tubercle. A genu recurvatum deformity developed after
premature closure of the anterior physis. Smillie137
reported one child who had an open tibial fracture complicated by a
second fracture involving the supracondylar aspect of the femur. This
patient also developed a recurvatum deformity secondary to closure of
the anterior proximal tibial physis. At present, no universally
acceptable explanation can be given for this phenomenon. Patients have
demonstrated apparently iatrogenic closure after placement of a
proximal tibial traction pin, the application of pins and plaster, and
after application of an external fixation device. Some children may
have an undiagnosed injury of the tibial physis at the time of the
ipsilateral tibial diaphyseal fracture.84
Regardless of etiology, premature closure of the physis produces a
progressive recurvatum deformity and loss of the normal anterior to
posterior slope of the proximal tibia as the child grows. Management
requires surgical intervention including proximal tibial osteotomy with
all the inherent risks and potential complications of that procedure.
 |
|
FIGURE 25-35 A. Anteroposterior radiograph of the distal tibia and fibula in a 5-year-old boy with an open fracture. B. Early callus formation is seen 1 month after injury. C. The tibia has failed to unite 10 months after injury. D. The patient underwent a fibulectomy 4 cm proximal to the tibial nonunion. The tibial fracture united 8 weeks after surgery.
|
tibial fractures in children. The use of an external fixation device
may lengthen the time to union in some patients, particularly those
with open fractures resulting from high-energy injury.50,94,106
Care must be taken to advance weight bearing appropriately and to
dynamize the frame as soon as possible to maximize bone healing.
Inadequate immobilization that allows patterned micro- or macromotion
also can slow the rate of healing and lead to delayed or nonunion. In
patients with a suspected delayed union or nonunion, a 1-cm fibulectomy
will allow increased compression at the delayed union or nonunion site
with weight bearing and often will induce healing (Fig. 25-35). A posterolateral bone graft also is an excellent technique to produce union in children (Fig. 25-36).
Adolescents near skeletal maturity with a delayed or nonunion can be
managed with a reamed intramedullary nail, concomitant fibular
osteotomy, and correction of any angulation at the nonunion site as
necessary (Fig. 25-37).
infant or toddler can produce a spiral fracture of the tibia without a
concomitant fibular fracture, and is termed a “toddler’s fracture” (Fig. 25-38). This fracture pattern was first reported by Dunbar et al.34
in 1964. The traumatic episode often is unwitnessed by the adult
caretaker. Of those injuries that are witnessed, most caregivers report
a seemingly minor, twisting mechanism. Most
children
with this injury are under 6 years of age, and in one study the average
age was 27 months. Sixty-three of 76 such fractures reported by Dunbar
et al.34
were in children under 2.5 years of age. Toddler’s fractures occur in
boys more often than in girls and in the right leg more often than in
the left. Occasionally, a child may sustain a toddler’s fracture in a
fall from a height.27,147
 |
|
FIGURE 25-36 A. Nonunion of an open tibial fracture. B. After posterolateral tibial bone graft.
|
analyzed the radiographs of 500 acutely limping toddlers and identified
100 in whom a fracture was the etiology of the gait disturbance. The
most common site of fracture was the distal metaphysis of the tibia.
The fibula was fractured with the tibia in only 12 of the 56 tibial
fractures. Only one physeal injury was noted.
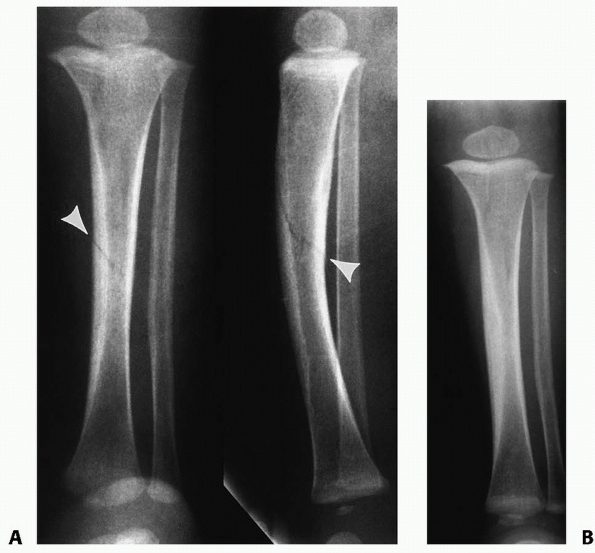 |
|
FIGURE 25-37 A.
Anteroposterior and lateral radiographs of a 14-year-old adolescent who was struck by a car, sustaining a grade IIIB open fracture of the tibia. B. Anteroposterior and lateral radiographs of the tibia after irrigation and débridement, and application of an external fixation device. C. The patient developed a nonunion at the tibia, which progressively deformed into an unacceptable varus alignment. D. The nonunion was treated with a fibular osteotomy followed by a closed angular correction of the deformity and internal fixation with a reamed intramedullary nail. |
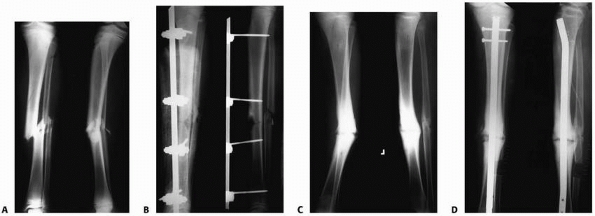 |
|
FIGURE 25-38 A.
Anteroposterior and lateral radiographs of an 18-month-old child who presented with refusal to bear weight on her leg. Note the spiral middle one-third “toddler’s” fracture (arrows). B. This fracture healed uneventfully after 4 weeks of immobilization in a cast. |
with an evaluation of the uninvolved side. This serves as a control for
the symptomatic extremity. The examination begins at the hip and
proceeds to the thigh, knee, lower leg, ankle, and foot. It is
important to note areas of point tenderness, any increase in local or
systemic temperature, and any swelling or bruising of the leg.147
Radiographs of the tibia and fibula should be obtained in both
anteroposterior and lateral projections. An internally rotated oblique
view can be helpful in identifying a nondisplaced toddler’s fracture.
Fluoroscopy also may assist in the identification of subtle fractures.
Occasionally, a fracture line cannot be identified, and the first
radiographic evidence of fracture becomes apparent when periosteal new
bone forms 7
to 14 days after the injury (Fig. 25-39).
Technetium radionuclide bone scan can assist in the diagnosis of
unapparent fractures, but is used rarely. A bone scan of a patient with
such a spiral fracture of the tibia will demonstrate diffuse increased
uptake of tracer throughout the affected bone (“black tibia”). This can
be differentiated from infection as infection tends to produce a more
localized area of increased tracer uptake.34
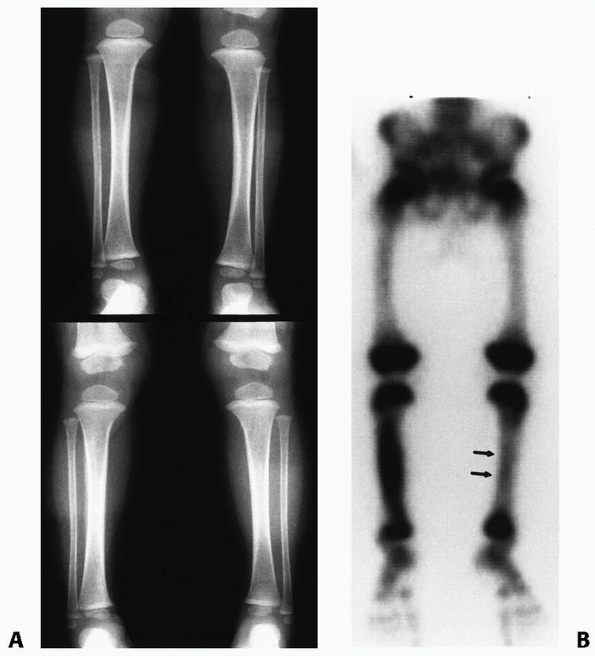 |
|
FIGURE 25-39 A.
Anteroposterior radiograph of the tibia in a 3-year-old child who refused to bear weight on the right leg 3 weeks before presentation. The history of obvious trauma was absent. The radiographs revealed periosteal new bone formation in the midshaft of the right tibia. There was also tenderness to palpation in the midleft tibia as well despite normal radiographs. B. A bone scan showed increased uptake in both the left and right tibia. There was significantly less uptake on the left side, the more recent injury. |
in a bent-knee, long-leg cast for approximately 3 to 4 weeks. Some
children may require an additional 2 weeks of immobilization in a
below-the-knee walking cast once the above-the-knee cast is removed,
but this is uncommon.
foot is caught between the spokes of a turning bicycle wheel. This
produces a severe compression or crushing injury to the soft tissues of
the foot and ankle and occurs most commonly when two children are
riding a bicycle designed for one, with the injured passenger riding on
the handlebars, or over the rear wheel.41,99
An oblique or spiral fracture of the tibia also can occur secondary to
the torsional forces on the limb. The injury to the foot, ankle, and
lower leg can be exacerbated when the child’s foot is extracted
forcibly from the spokes of the bicycle.
a bicycle spoke injury may be deceiving. The foot often appears normal
or may show only minor skin abrasions. The patient often presents 24 to
48 hours after the accident complaining of a painful swollen foot and
leg. This injury is similar to a “wringer” injury of the arm in that
the initial examination may not reveal the true extent of the injury.
Izant et al.70 reviewed 60 bicycle
spoke injuries in children under 14 years of age. The most common age
range of injury was 2 to 8 years. Three components were identified to
this trauma: (i) a laceration of the tissue from the knifelike action
of the spoke, (ii) a crushing injury from the impingement between the
wheel and the frame of the bicycle, and (iii) a shearing injury from
the coefficient of these two forces. The laceration created by this
injury often involves the malleoli, the Achilles tendon area of the
heel, and the dorsum of the foot.
admitted to the hospital because the extent of the damage may not be
identified initially. Initial therapy consists of a mild compression
dressing with a multilayered cotton bandage. The extremity is elevated
and the child is kept at bedrest during the first 24 hours. A long-leg
splint is applied if a tibial fracture is present. After this period of
bedrest and elevation, the child may ambulate nonweight bearing with
crutches. Frequent inspection of the extremity must be made during the
subsequent 48 hours. Débridement of devitalized tissue is performed as
any necrosis becomes apparent. Large areas of hematoma formation may be
treated with aspiration to prevent further elevation of the overlying
skin. Multiple débridements may be required, and definitive treatment
must await complete delineation of the necrotic area. Delayed wound
closure, sometimes requiring skin grafting, may be necessary if
full-thickness skin loss occurs. Occasionally, a free flap may be
required, however this is rare.41,70,99
A child with a concomitant tibial fracture is placed in an
above-the-knee nonweight-bearing cast at the completion of care for the
foot injury, particularly if the soft tissue injury is fairly minor.41
The tibial fracture may require stabilization with an external fixator
if the soft tissue loss on the foot and ankle is severe, and in these
cases the external fixation device may be extended to include the foot
and ankle.
involving both the femur and the tibia. In the past, these injuries
often were treated with traction and casting (Fig. 25-40). The extent of the injuries often left permanent functional deficits when not managed aggressively.11,33
fractures are treated most appropriately with operative stabilization
of the femur and either cast immobilization of the tibia after
reduction or operative fixation. In pediatric patients, the femoral
fracture can be stabilized with a unilateral external fixator, plate
and screw constructs, or flexible nails. Patients near skeletal
maturity may be candidates for lateral entry reamed femoral nails,
although the other options remain viable as well plate fixation, either
open or percutaneous, is useful for fractures in the subtrochanteric or
supracondylar area of the femur in adolescents, while external fixation
may be useful in these areas as well. The tibial fracture is reduced
and stabilized after the femoral fracture has been stabilized. Closed
tibia fractures in these situations may be treated with cast
immobilization or operative intervention. Open tibial fractures
associated with an ipsilateral femoral fracture should be stabilized
with an external fixator or flexible intramedullary nails whenever
possible (Fig. 25-41).
common cause of lower extremity weakness in children. Because these
patients had sensation, fractures were identified early. Disease
trends
have changed over time. As late as 1958, 90% to 95% of children with
myelomeningocele died in the first year of life, usually from a
neurologic complication. Advances in neurosurgery and urology have
lengthened the lifespan of children with myelomeningocele
significantly. The mortality rate in the first year of life for these
children is now approximately 3% to 5%. Currently, pediatric
orthopaedic surgeons manage a large number of paraplegic children who
have sensory and/or motor deficits associated with myelomeningocele.33,42,45
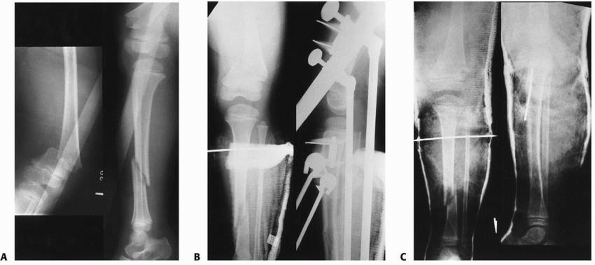 |
|
FIGURE 25-40 A. Ipsilateral fractures of the distal femur and tibia without an ipsilateral fibular fracture in a 5-year-old. B.
The child was treated with tibial pin traction for the femoral injury (pin applied below the tibial tubercle) and a short-leg splint for the tibial fracture initially. C. The child was placed into a spica cast after 2 weeks of traction. The tibial traction pin was used to help stabilize both fractures. |
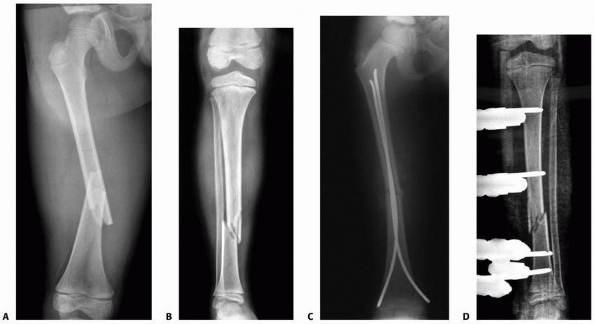 |
|
FIGURE 25-41 A,B. Floating knee injury in a 7-year-old boy. C. Femoral fracture was fixed with flexible intramedullary nails. D. Tibial fracture was stabilized with external fixation.
|
were the first to publish a report on children with myelomeningocele
who sustained pathologic fractures of the proximal tibia. These two
children had tense hyperemic skin and radiographic evidence of
exuberant new bone formation, suggesting a malignant tumor (Fig. 25-42). Both children underwent a biopsy because of these radiographic findings.
warmth, and erythema are common in paraplegic children with a fracture.
He stated that “fractures to the growth plate in paraplegic children
often resemble osteomyelitis.”139 Golding47 reported one physeal injury to the distal tibia in a child with myelomeningocele. Gyepes et al.47 reported seven metaphyseal and physeal injuries in patients with myelomeningocele. Stern et al.143
reported bilateral distal tibial and fibular physeal injuries in a
child with myelomeningocele. In most cases, these physeal fractures are
chronic physeal injuries, which are characterized by an irregular,
dense, widened physis and adjacent subperiosteal new bone formation.
 |
|
FIGURE 25-42
An undisplaced fracture of the proximal tibial metaphysis in a child with myelodysplasia. Note the exuberant new bone formation. |
reported 44 fractures in 22 children in a population of 122 children
with myelomeningocele. The most common age range for fracture was 3 to
6 years. These fractures were more common in a flail limb. Only 6.6% of
the patients with quadriceps activity had fractures, whereas 19% of
those with no active muscle contraction (flail limb) had fractures.
This incidence decreased to 12.5% in a group of children with spastic
paralysis. The tibia and femur were the most common bones affected. The
most common locations for tibial fractures were the distal diaphysis
and distal metaphysis. Drennan and Freehafer33
reported 58 fractures in 25 patients among 84 children with
myelomeningocele. Ten fractures were of the tibia. Eleven of the 58
fractures occurred after the removal of a spica cast, suggesting that
immobilization worsened osteopenia and increased the risk of subsequent
fracture.
producing the complex findings associated with a tibial fracture in a
paralytic child.58 Repeated
microtrauma can lead to a metaphyseal infarction, subperiosteal
hemorrhage, and, perhaps, physeal hemorrhage. Subsequent healing
produces endosteal and periosteal callus formation and further
generalized osteopenia secondary to the immobilization. The widening of
the physis most likely is secondary to a disturbance of the normal
reabsorption mechanism during bone development at the metaphysis. This
results from frequent subclinical metaphyseal infarctions and could be
the result of hemorrhage into the physis itself.
therapy is indicated. Displaced fractures are reduced closed and
immobilized for 3 to 4 weeks in a bulky dressing or a posterior,
molded, well-padded splint. As the underlying skin is insensate, care
must be taken to avoid pressure areas which may lead to sores or skin
breakdown. Healing is determined by the absence of local warmth and
swelling and the reconstitution of the width of the physis on
radiographs.89 The child should be
fitted with an orthosis or placed back into his or her prefracture
orthosis soon after the immobilization is discontinued so as to return
to prefracture activity level as soon as possible. Parsch and Rossak113
reported 31 fractures in 120 patients with myelomeningocele. They
emphasized treatment with a wrap and splint until early fracture
consolidation. To prevent “fracture disease,” they stressed early
standing and walking to help minimize any further increases in existing
osteopenia. Physeal injuries may require prolonged periods of
immobilization and very rarely may be treated surgically to gain
maximal stabilization. Complications in patients with paralysis and a
tibial fracture are relatively uncommon, and usually are related to
pressure sores produced by poorly padded casts. Early physeal arrest
can occur, producing a leg-length discrepancy or angular deformity.139
in 1939 reported an “unusual type of lesion” in the tibia of 12
children. All were determined to be stress fractures involving the
proximal third of the tibial shaft. Since then, numerous reports of
stress fractures involving the tibia and the fibula have been published.7,31,36,39,62,69,86,96,102,103,116,124,128,145
In adults, the fibula is involved in stress fractures twice as often as
the tibia; in children, the tibia is affected more often than the
fibula (Fig. 25-43). The prevalence of stress fractures in boys and girls is equal.
 |
|
FIGURE 25-43 Bilateral midtibial stress fractures in an adolescent with genu varus.
|
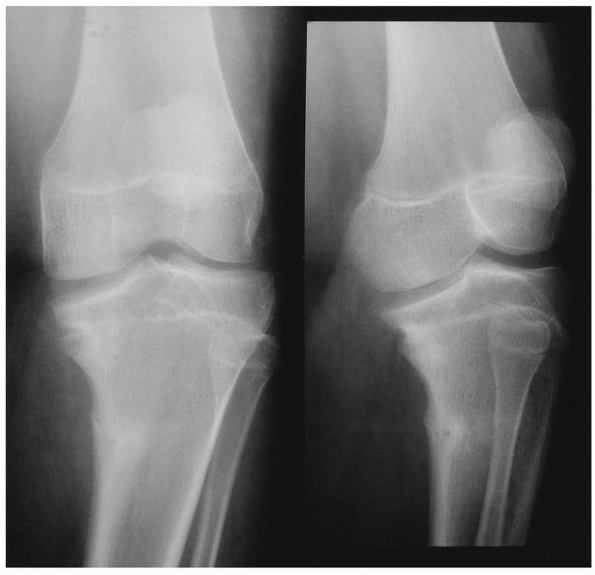 |
|
FIGURE 25-44
Anteroposterior and lateral radiographs of the knee of a 15-year-old with adolescent onset tibia vara. Note the posteromedial stress fracture. |
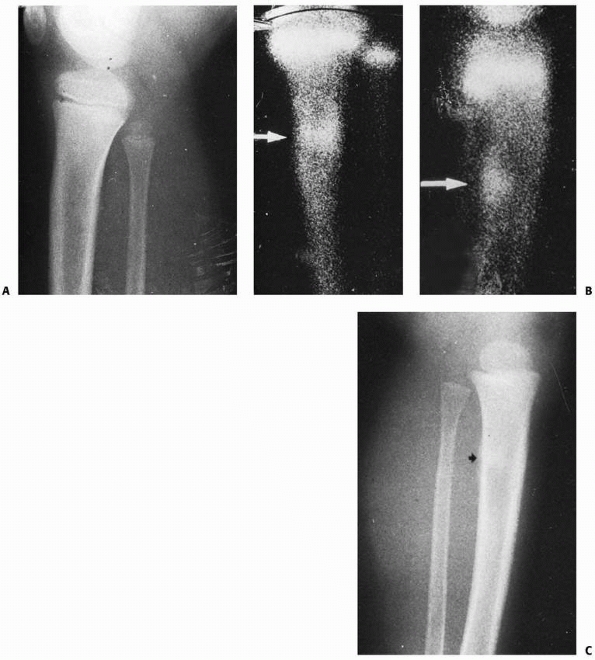 |
|
FIGURE 25-45 A.
Lateral radiograph of the proximal tibia in a 9-year-old who complained of pain in the right leg. There was no history of trauma, and the radiographs were unremarkable. B. A bone scan 2 days after the onset of symptoms demonstrates increased tracer uptake in the proximal one third of the tibia in both the anteroposterior and lateral projections (arrows). C. Increased bone density and subtle periosteal new bone formation was identified in the proximal tibia 3 weeks later (arrows). (Courtesy of James Conway, MD.) |
to a bone is exceeded by the bone’s capacity to withstand it.
Initially, osteoclastic tunnel formation increases. These tunnels
normally fill with mature bone. With continued force, cortical
reabsorption accelerates. Woven bone is produced to splint the weakened
cortex. This bone is disorganized, however, and does not have the
strength of the bone it replaces. A fracture occurs when bone
reabsorption outstrips bone production. When the offending force is
reduced or eliminated, bone production exceeds bone reabsorption. This
produces cortical and endosteal widening with dense repair bone that
later remodels to mature bone.38,74,112
There is evidence of local tenderness that worsens with activity. The
child may have a painful limp, while a toddler with a stress fracture
will not bear weight on the involved extremity. The pain tends to be
worse in the day and to improve at night and with rest. The knee and
the ankle have full ranges of motion. Usually, there is minimal, if
any, swelling at the fracture site.15,30,39,67,85,120
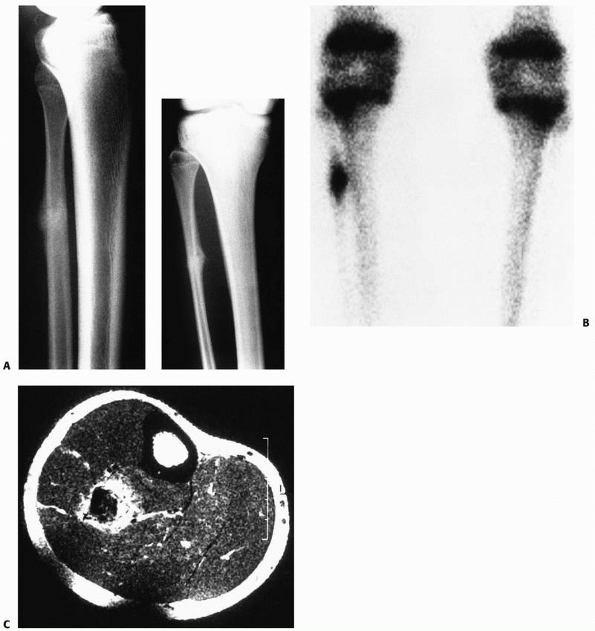 |
|
FIGURE 25-46 A. Stress fracture of the diaphysis of the fibula in a 14-year-old girl with mild genu varum. B. Bone scan of stress fracture showing marked increased tracer uptake. C.
MR image demonstrates new central bone formation and an inflammatory zone around the fibular cortex. (From Sharps CH, Cardea JA. Fractures of the shaft of the tibia and fibula. In: MacEwen GD, Kasser JR, Heinrich SD, eds. Pediatric Fractures: A Practical Approach to Assessment and Treatment. Baltimore: Williams & Wilkins, 1993:324, with permission.) |
fracture and generally become evident approximately 2 weeks after the
onset of symptoms.31 Radiographic
findings consistent with fracture repair can manifest in one of three
ways: localized periosteal new bone formation, endosteal thickening,
or, rarely, a radiolucent cortical fracture line (Fig. 25-44).30,31,33,85,128
bone scanning reveals a local area of increased tracer uptake at the
site of the fracture (Fig. 25-45). Computerized
tomography rarely demonstrates the fracture line, but often delineates
increased marrow density, endosteal and periosteal new bone formation,
and may show soft tissue edema within the area of concern. Magnetic
resonance (MR) imaging67,85 shows a localized band of very low signal intensity continuous with the cortex.
These MR findings can be diagnostic for a stress fracture, and will
differentiate such lesions from malignancy, thereby obviating the need
for biopsy.
in the upper third. The child normally has a painful limp of gradual
onset with no history of a specific injury. The pain is described as
dull, occurring in the calf near the upper end of the tibia on its
medial aspect, and occasionally is bilateral. Physical findings include
local tenderness on one or both sides of the tibial crest with a
varying degree of swelling.
tibia begins with activity modification. An active child can rest in a
long-leg walking cast for 4 to 6 weeks followed by gradual increase in
activity. Nonunions of stress fractures of the tibia have been
described. Green52 reported six
nonunions, three of which were in children. Two required excision of
the nonunion site with iliac crest bone grafting. The third was treated
by electromagnetic stimulation. In all three, the stress fractures
occurred in the middle third of the tibia.
The fractures are normally localized to the distal third of the fibula.
The child presents with a limp and may complain of pain. Tenderness is
localized to the distal half of the fibular shaft. Swelling normally is
not present. The obvious bony mass commonly seen in a stress fracture
of the fibula in an adult is normally not seen in a comparable fracture
in a child.
first 10 days to 2 weeks after the symptoms begin. The earliest sign of
a stress fracture of the fibula is the presence of “eggshell” callus
along the shaft of the fibula.15 The
fracture itself cannot always be seen because the periosteal callus may
obscure the changes in the narrow canal. Radionuclide bone imaging can
help to identify stress fractures before the presence of radiographic
changes (Fig. 25-46).
osteomyelitis, and a soft tissue injury without accompanying bony
injury. Treatment consists of rest or, in the very active child, a
short leg-walking cast for 4 to 6 weeks.
MJ, Nash JR, Ioannidies TT, et al. Major vascular surgeries associated
with orthopaedic injuries to the lower limb. Ann R Coll Surg Engl
1984;66:101-104.
GS III, Weiner LS, Yang EC. Treatment of type II and type III open
tibia fractures in children. J Orthop Trauma 1997;11:357-362.
LO. Valgus deformity following proximal metaphyseal fractures in
children: experiences in the African tropics. J Trauma 1990;30:102-107.
G, Kallieris D, Seebock T, et al. Bioreabsorbable pins and screws in
pediatric traumatology. Eur J Pediatr Surg 1994;4:103-107.
WW, Durbin RA. Ipsilateral fractures of the femur and tibia in children
and adolescents. J Bone Joint Surg Am 1991;73:429-439.
SL, Gotschall C, Robertson W, et al. The relationship of skeletal
injuries with trauma score, injury severity score, length of hospital
stay, hospital charges, and mortality in children admitted to a
regional pediatric trauma center. J Pediatr Orthop 1994; 14:449-453.
JCY, Shen WY. Limb fracture pattern in different pediatric age groups:
a study of 3350 children. J Orthop Trauma 1993;7:15-22.
G, Byrd HS, Jones RE. Primary versus delayed tissue coverage for severe
open tibial fractures: a comparison of results. Clin Orthop Relat Res
1983;178:54-63.
L. Fracture of the proximal portion of the tibia in children followed
by valgus deformity. Surg Gynecol Obstet 1953;97:183-188.
KE, Limbird TJ, Green NE. Open fractures of the diaphysis of the lower
extremity in children. J Bone Joint Surg Am 1992;74:218-232.
G, Aldegheiri R, Renzi-Brivio LR, et al. Chondrodiastasis-controlled
symmetrical distraction of the epiphyseal plate. Limb lengthening in
children. J Bone Joint Surg Br 1986;68:550-556.
G, Aldegheiri R, Renzi-Brivio L, et al. Limb lengthening by distraction
of the epiphyseal plate. A comparison of two techniques in the rabbit.
J Bone Joint Surg Br 1986;68:545-549.
BT, Kortesis B, Punger K, et al. Subatmospheric pressure dressing in
temporary treatment of soft tissue injuries associated with type III
open tibial shaft fractures in children. J Pediatr Ortho.
2006;26:728-732.
JS, Owen HF, Nogrady MB, et al. Obscure tibial fracture of infants—the
toddler’s fracture. J Can Assoc Radiol 1964;25:136-144.
CC. Staged reconstruction of complex open tibial fractures using
Hoffmann external fixation. Clin Orthop Relat Res 1983;178:130-161.
KA, Weisz R, Hiebert R, et al. Does fibular plating improve alignment
after intramedullary nailing of distal metaphyseal tibia fractures? J
Orthop Trauma 2006;20: 94-103.
M, Strong ML, MacIntosh R. External fixation maintained until fracture
consolidation in the skeletally immature. J Pediatr Orthop
1983;13:98-101.
P, Giacomelli MC, Basic B, et al. Problems of operative and
nonoperative treatment and healing in tibial fractures. Injury
2005;26(Suppl 1):A44-50.
RC, Gaynor T, Mahar A, et al. Intramedullary flexible nail fixation of
unstable pediatric tibial diaphyseal fractures. J Pediatr Orthop
2005;25:570-576.
JE, Gregush RV, Schoenecker PL, et al. Complications after titanium
elastic nailing of pediatric tibial fractures. J Pediatr Orthop
2007;27:442-446.
JE, Schoenecker PL, Oda JE, et al. A comparison of monolateral and
circular external fixation of unstable diaphyseal tibial fractures in
children. J Pediatr Orthop 2003;12:338-345.
H. Anatomy: descriptive and surgical. In: Pick TP, Howden R, eds.
Anatomy: Descriptive and Surgical. New York: Bounty Books, 1977:182.
NE. Tibia valga caused by asymmetrical overgrowth following a
nondisplaced fracture of the proximal tibia metaphysis. J Pediatr
Orthop 1983;3:235-237.
RB, Anderson JT. Prevention of infection in the treatment of 1025
fractures of long bones: retrospective and prospective analyses. J Bone
Joint Surg Am 1976;58: 453-458.
RB, Mendoza RM, Williams PN. Problems in the management of type III
(severe) open fractures: a new classification of type III open
fractures. J Trauma 1984;24: 742-746.
MT, Newbern DH, Neuhauser EBD. Metaphyseal and physeal injuries in
children with spina bifida and meningomyeloceles. Am J Roentgenol
Radium Ther Nucl Med 1965;95:168-177
LM, Staple TW. Arterial injuries associated with fractures of the
proximal tibia following blunt trauma. South Med J 1969;62:1439-1448.
G, Korenreich L, Ziv N, et al. The enigma of stress fractures in the
pediatric age: clarification or confusion through the new imaging
modalities. Pediatr Radiol 1990;20:469-471.
JB, Sanderson PL, Rickman M, et al. External fixation of children’s
fractures: use of the Orthofix Dynamic Axial Fixator. J Pediatr Orthop
1997;6:203-206.
RJ, Rothman BF, Frankel V. Bicycle spoke injuries of the foot and ankle
in children: an underestimated “minor” injury. J Pediatr Surg
1969;4:654-656.
DW, Cozen L. Genu valgum as a complication of proximal tibial
metaphyseal fractures in children. J Bone Joint Surg Am
1971;53:1571-1578.
CCM. Fractures of the lower limbs in spina bifida cystica: a survey of
44 fractures in 122 children. Dev Med Child Neurol Suppl 1970;22(Suppl
22):88.
HMJ, Boaos PLO. Routine monitoring of compartment pressures in patients
with tibial fractures: beware of over treatment. Injury 2001;32:415-421.
SE, Alonso JE, Cook FF. The etiology of valgus angulation after
metaphyseal fractures of the tibia in children. J Pediatr Orthop
1987;7:450-457.
MK, Nilsson BE, Obrant KJ. Fracture incidence after tibial shaft
fractures: a 30-year follow-up study. Clin Orthop Relat Res
1993;287:87-89.
G, Lönnerholm T, Olerud S. Cavus deformity of the foot after fracture
of the tibial shaft. J Bone Joint Surg Am 1975;57:893-900.
J, Hansson LI, Svensson K. Incidence of tibiofibular shaft and ankle
fractures in children. J Pediatr Orthop 1982;2:386-396.
SS, Dickson K. Determining the prognosis for limb salvage in major
vascular injuries with associated open tibial fractures. Orthop Rev
1992;21:195-199.
DM, Caligiuri DA, Katzman BM. Local-advancement soft-tissue coverage in
a child with ipsilateral grade IIIB open tibial and ankle fractures. J
Orthop Trauma 1996; 10:577-580.
K, Urbonaviciene A. Stress fracture of the fibula in the first few
years of life (report of six cases). Aust Radiol 1996;40:261-263.
EM, Egal KA, Scher D, et al. Operative treatment of tibial fractures in
children: are elastic stable intramedullary nails an improvement over
external fixation? J Bone Joint Surg Am 2005;87:1761-1768.
SJ, Lowell HR, Townsend P. Physeal, metaphyseal, and diaphyseal
injuries of the lower extremities in children with myelomeningocele. J
Pediatr Orthop 1984;4: 25-27.
A, Dubas J. Sekundare Deformierungen nach Epiphysenlosungen und
Epiphysenliniennahen Fraktunen. Helv Chir Acta 1954;21:388-410.
AS, Wetzlan M, Lewars M, et.al. The orthopaedic and social outcome of
open tibia fractures in children. Orthopaedics 1997;20:593-598.
RU, Montgomery RJ. Treatment of established and anticipated nonunion of
the tibia in childhood. J Pediatr Orthop 2002;22:754-760.
P. The appearance of bone scans following fractures, including
immediate and long-term studies. J Nucl Med 1979;20:1227-1231.
FA III, Winquist RA, Krugmire RTS. Diagnosis and management of
compartment syndromes. J Bone Joint Surg Am 1980;62:286-291.
LB, Reesor K. Spiral tibial fractures of children: a commonly
accidental spiral long bone fracture. Am J Emerg Med 1990;8:234-237.
JP, Wong-Chung J, Bertrand H, et al. Percutaneous epiphysiodesis using
transphyseal screws (PETS). J Pediatric Ortho 1998;18:363-369.
LJ, Gerbino PG. Etiologic assessment of stress fractures of the lower
extremity in young athletes. Orthop Trans 1980;4:1.
JF III, Argenta LC, Marks MW, et al. Treatment of soft tissue defects
in pediatric patients using the VAC system. CORR 2000;376:26-31.
KS, Starr DE. Closure of the anterior portion of the upper tibial
epiphysis as a complication of tibial-shaft fracture. J Bone Joint Surg
Am 1964;46:570-574.
T, Weisman DS, Ronchetti P, et al. Flexible titanium nailing for the
treatment of the unstable pediatric tibial fracture. J Pediatr Orthop
2004;24:601-609.
JA, Ogden DA, Pugh L, et al. Tibia valga after proximal metaphyseal
fracture in childhood: a normal biologic response. J Pediatr Orthop
1995;15:489-494.
B, Valerio IL, Stewart DH, et al. Microvascular free flap
reconstruction in pediatric lower extremity trauma: a 10-year review.
Plast Reconstr Surg 2006;118:570-571.
M, Khouri N, Carlioz H, et al. Fractures of the proximal tibial
metaphysis in children: review of a series of 25 cases. J Pediatr
Orthop 1987;7:444-449.
G, Salter R. Presentation of valgus deformity following fracture of the
proximal metaphysis of the tibia in children. J Bone Joint Surg Br
1980;62:527.
KH, Lindemann I, Keppler P. Flexible intramedullary nailing in
pediatric lower limb fractures. J Pediatr Orthop 2006;26:505-509.
RB, Best T. The pathogenesis and prevention of valgus deformity
following fractures of the proximal metaphyseal region in the tibia in
children. J Bone Joint Surg Am 1973;55:1324.
MJ. Taylor spatial frame in the treatment of pediatric and adolescent
tibial shaft fractures. J Pediatr Orthop 2006;26:164-170.
RE, Shannon JM, Dickerson JR. Factors involved in recovery from
experimental skeletal muscle ischemia in dogs. Am J Pathol
1961;39:721-737.
DL, Kautz SM, Kay RM, et al. Effects of delay on surgical treatment on
rate of infection in open fractures in children. J Pediatric Ortho
2000;20:19-22.
JM, Smeulders MJ, van der Horst CM. Normal compartment pressures of the
lower leg in children. J Bone Joint Surg Br 2008;90(2):215-219.
HH, Sandrow RE, Sullivan PD. Complications of tibial osteotomy in
children for genu varum or valgum. Evidence that neurological changes
are due to ischemia. J Bone Joint Surg Am 1971;53:1629-1635.
MB, Grant SS, Isaacson AS. Bilateral distal tibial and fibular
epiphyseal separation associated with spina bifida. Clin Orthop Relat
Res 1967;50:191-196.
JW, Oppers VM. Crural fractures in children. A study of the incidence
of changes of the axial position and of enhanced longitudinal growth of
the tibia after the healing of crural fractures. Arch Chir Neerl
1971;23:259-272.
VR, De Silva U, Bache CE, et al. Flexible intramedullary nails for
unstable fractures of the tibia in children. An 8-year experience. J
Bone Joint Surg 2006;88: 536-540.
der Werkon C, Meevwis JD, et al. The simple fix: external fixation of
displaced isolated tibial fractures. Injury 1993;24:46-48.
BG. Fibrous interposition causing valgus deformity after fracture of
the upper tibial metaphysis in children. J Bone Joint Surg Br
1977;59:290-292.
TE Jr, Haney TC, Morimoto K, et al. Tissue pressure measurements as a
determinant for the need of fasciotomy. Clin Orthop Relat Res
1975;113:43-51.
J, Letts M. Isolated fractures of the tibia with intact fibula in
children: a review of 95 patients. J Pediatr Orthop 1997;17:347-351.
LE, Harcke HT, Brooks KM, et al. Posttraumatic tibia valga: a case
demonstrating asymmetric activity at the proximal growth plate on
technetium bone scan. J Pediatr Orthop 1977;7:458-462.
