Upper Limb
when performing manual activities such as buttoning a shirt.
Synchronized interplay occurs between the joints of the upper limb to
coordinate the intervening segments to perform smooth, efficient motion
at the most workable distance or position required for a specific task.
Efficiency of hand function results in large part from the ability to
place it in the proper position by movements at the scapulothoracic,
glenohumeral, elbow, radioulnar, and wrist joints.
-
Shoulder:
proximal segment of the limb that overlaps parts of the trunk (thorax
and back) and lower lateral neck. It includes the pectoral, scapular,
and lateral supra-clavicular regions and is built on half of the
pectoral girdle. The pectoral (shoulder) girdle is a bony ring, incomplete posteriorly, formed by the scapulae and clavicles and completed anteriorly by the manubrium of the sternum (part of the axial skeleton). -
Arm (L. brachium):
first segment of the free upper limb (more mobile part of the upper
limb independent of the trunk) and the longest segment of the limb. It
extends between and connects the shoulder and the elbow and is centered
around the humerus. -
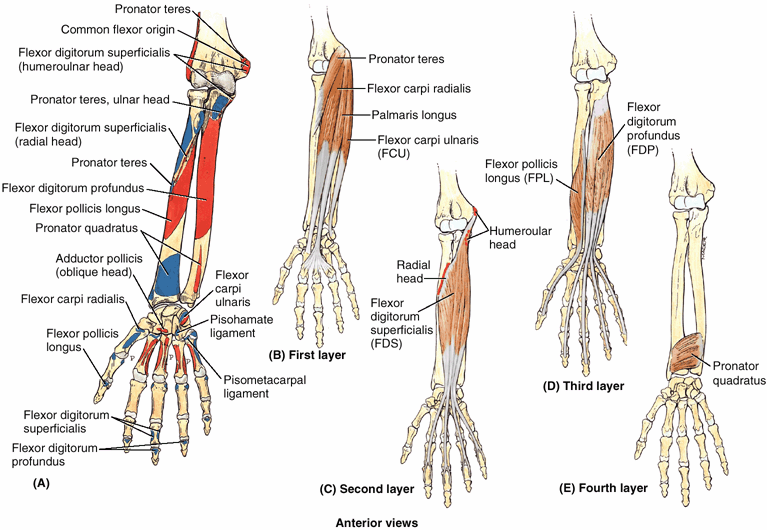
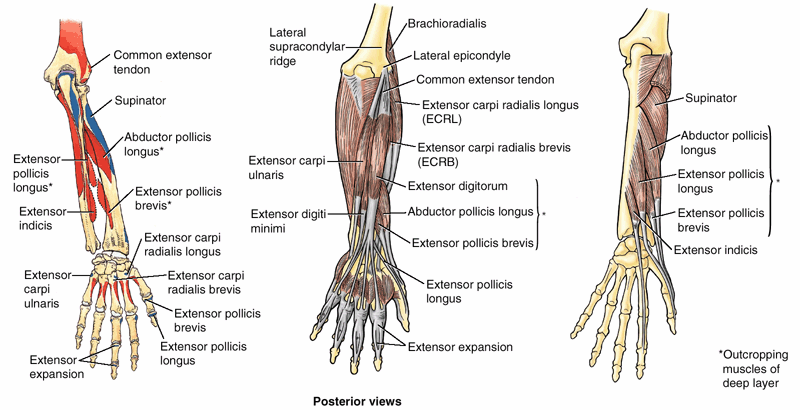
Forearm (L. antebrachium): second longest segment of the limb. It extends between and connects the elbow and the wrist and contains the ulna and radius.
-
Hand (L. manus):
part of the upper limb distal to the forearm that is formed around the
carpus, metacarpus, and phalanges. It is composed of the wrist, palm,
dorsum of hand, and fingers (including an opposable thumb) and is
richly supplied with sensory endings for touch, pain, and temperature.
limb, particularly the hand, are far out of proportion to the extent of
the injury, a sound understanding of the structure and function of the
upper limb is of the highest importance. Knowledge of its structure
without an understanding of its functions is almost useless clinically
because the aim of treating an injured limb is to preserve or restore
its functions.
the upper and lower limbs share many common features. However, they are
sufficiently distinct in structure to enable markedly different
functions and abilities. Because the upper limb is not usually involved
in weight bearing or motility, its stability has been sacrificed to
gain mobility. The upper limb still possesses remarkable strength. And
because of the hand’s ability to conform to a paddle or assume a
gripping or platform configuration, it may assume a role in motility in
certain circumstances.
consists of the scapulae and clavicles, connected to the manubrium of
the sternum. Both girdles possess a large flat bone located
posteriorly, which provides for attachment of proximal muscles and
connects with its contralateral partner anteriorly via small bony
braces, the pubic rami and clavicles.
However,
the flat iliac bones of the pelvic girdle are also connected
posteriorly through their primary attachment to the sacrum via the
essentially rigid, weight-transferring sacroiliac joints. This
posterior connection to the axial skeleton places the lower limbs
inferior to the trunk, enabling them to be supportive as they function
primarily in relation to the line of gravity. Furthermore, because the
two sides are connected both anteriorly and posteriorly, the pelvic
girdle forms a complete rigid ring that limits mobility, making the
movements of one limb markedly affect the movements of the other. The
pectoral girdle, however, is connected to the trunk only anteriorly via
the sternum by flexible joints with 3° of freedom and is an incomplete
ring because the scapulae are not connected with each other
posteriorly. Thus the motion of one upper limb is independent of the
other, and the limbs are able to operate effectively anterior to the
body, at a distance and level that enables precise eye–hand
coordination.
 |
|
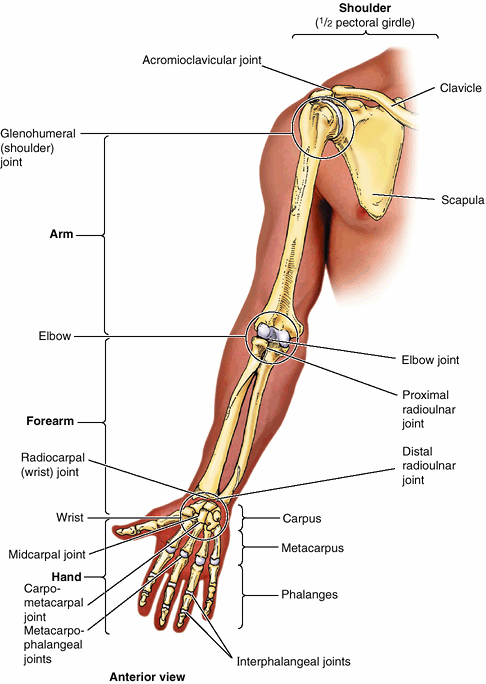
Figure 6.1. Regions and bones of upper limb.
The joints divide the superior appendicular skeleton, and thus the limb itself, into four main regions: shoulder, arm, forearm, and hand. |
the most proximal segment is the largest and is unpaired. The long
bones increase progressively in number but decrease in size in the more
distal segments of the limb. The second most proximal segment of both
limbs (i.e., the leg and forearm) has two parallel bones, although only
in the forearm do both articulate with the bone of the proximal segment
and only in the leg do both articulate directly with the distal
segment. While the paired bones of both the leg and forearm flex and
extend as a unit, only those of the upper limb are able to move
(supinate and pronate) relative to each other, the bones of the leg
being fixed in the pronated position.
(eight and seven, respectively). Both groups of short bones interrupt a
series of long bones that resumes distally with several sets of long
bones of similar lengths, with a similar number of joints of
essentially the same type. The digits of the upper
limb
(fingers including the thumb) are the most mobile parts of either limb,
but all the other parts of the upper limb are more mobile than the
comparable parts of the lower limb.
regarding their development and structure, the upper limb has evolved
into a mobile organ of manipulation that, along with the brain, allows
humans not only to respond to their environments but to manipulate and
control them to a large degree. The upper limb is composed of four
increasingly mobile segments, the proximal three (shoulder, arm, and
forearm) serving primarily to position the fourth (hand), which is for
grasping, manipulation and touch. Four distinctions from the lower
limbs enable the independent operation of the upper limbs, allowing the
hands to be precisely positioned anterior to the body at a distance and
height that enables accurate eye–hand coordination: (1) the upper limbs
are not involved in weight bearing or ambulation, (2) the pectoral
girdle is attached to the axial skeleton only anteriorly via a very
mobile joint, (3) paired bones of the forearm are able to be moved
relative to each other, and (4) the hands have long, mobile fingers and
an opposable thumb.
the inferior appendicular skeleton.
The superior appendicular skeleton articulates with the axial skeleton
only at the sternoclavicular joint, allowing great mobility. The
clavicles and scapulae of the pectoral girdle are supported,
stabilized, and moved by axioappendicular muscles that attach to the relatively fixed ribs, sternum, and vertebrae of the axial skeleton.
 |
|
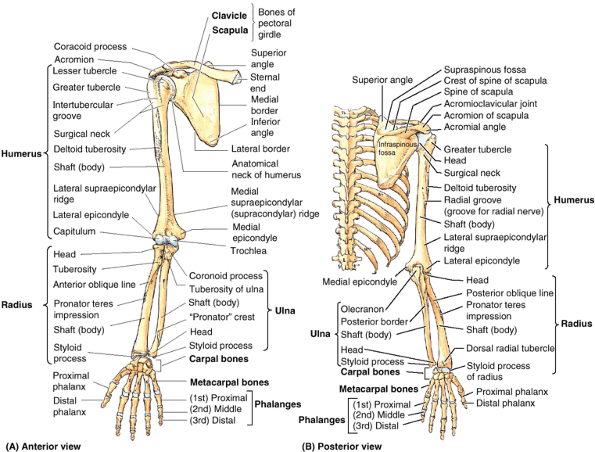
Figure 6.2. Bones of upper limb. A.
The right superior appendicular skeleton includes the right half of the pectoral (shoulder) girdle, composed of the right clavicle and scapula, and the skeleton of the free right upper limb, formed by the remaining bones distal to the scapula. B. The superior appendicular and thoracic parts of the axial skeleton demonstrate that the scapula overlaps parts of the 2nd–7th ribs. Only the thin clavicle links the axial and superior appendicular skeletons. Although not a “true” anatomical joint, the scapula rests and moves on (articulates with) the posterosuperior thoracic wall via the physiological “scapulothoracic joint.” |
 |
|
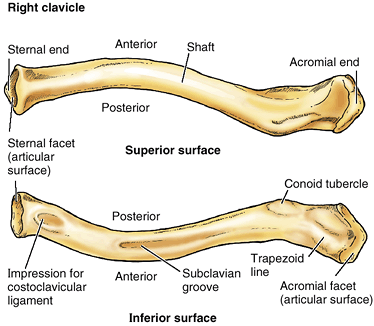
Figure 6.3. Right clavicle.
Prominent features of the superior and inferior surfaces of the clavicle are shown. The bone acts as a mobile strut (supporting brace), connecting the trunk to the upper limb. |
The medial two thirds of the shaft of the clavicle are convex
anteriorly, whereas the lateral third is flattened and concave
anteriorly. These curvatures increase the resilience of the clavicle
and give it the appearance of an elongated capital S.
-
Serves as a moveable, crane-like strut
(rigid support) from which the scapula and free limb are suspended,
keeping them away from the trunk so that the limb has maximum freedom
of motion. The strut is movable and allows the scapula to move on the
thoracic wall at the “scapulothoracic joint,”1
increasing the range of motion of the limb. Fixing the strut in
position, especially after its elevation, enables elevation of the ribs
for deep inspiration. -
Forms one of the bony boundaries of the cervicoaxillary canal (passageway between the neck and the arm), affording protection to the neurovascular bundle supplying the upper limb.
-
Transmits shocks (traumatic impacts) from the upper limb to the axial skeleton.
medullary (marrow) cavity. It consists of spongy (trabecular) bone with
a shell of compact bone.
of the clavicle is rough because strong ligaments bind it to the 1st
rib near its sternal end and suspend the scapula from its acromial end.
The conoid tubercle, near the acromial end of the clavicle (Fig. 6.3), gives attachment to the conoid ligament, the medial part of the coracoclavicular ligament
by which the remainder of the upper limb is passively suspended from
the clavicle. Also, near the acromial end of the clavicle is the trapezoid line, to which the trapezoid ligament attaches; it is the lateral part of the coracoclavicular ligament. The subclavian groove (groove for the subclavius) in the medial third of the shaft of the clavicle is the site of attachment of the subclavius muscle. More medially is the impression for the costoclavicular ligament, a rough, often depressed, oval area that gives attachment to the ligament binding the 1st rib (L. costa) to the clavicle, limiting elevation of the shoulder.
bones. Occasionally, the clavicle is pierced by a branch of the
supraclavicular nerve. The clavicle is thicker and more curved in
manual workers, and the sites of muscular attachments are more marked.
The right clavicle is usually stronger and shorter than the left
clavicle.
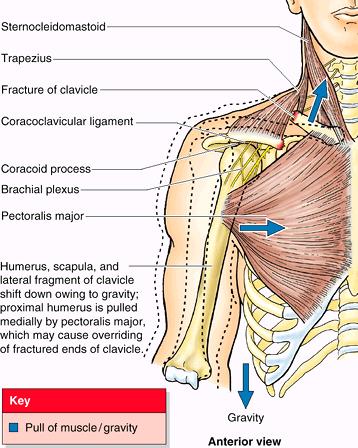
bones. Clavicular fractures are especially common in children and are
often caused by an indirect force transmitted from an outstretched hand
through the bones of the forearm and arm to the shoulder during a fall.
A fracture may also result from a fall directly on the shoulder. The
weakest part of the clavicle is the junction of its middle and lateral
thirds.
Because of the subcutaneous position of the clavicles, the end of the
superiorly directed fragment is prominent—readily palpable and/or
apparent. The trapezius muscle is unable to hold the lateral fragment
up owing to the weight of the upper limb, and thus the shoulder drops.
The strong coracoclavicular ligament usually prevents dislocation of
the AC joint. People with fractured clavicles support the sagging limb
with the other limb. In addition to being depressed, the lateral
fragment of the clavicle may be pulled medially by the adductor muscles
of the arm, such as the pectoralis major. Overriding of the bone
fragments shortens the clavicle.
 |
|
Figure B6.1
|
fractured during delivery if the neonates are broad shouldered;
however, the bones usually heal quickly. A fracture of the clavicle is
often incomplete in younger children—that is, it is a greenstick fracture,
in which one side of a bone is broken and the other is bent. This
fracture was so named because the parts of the bone do not separate;
the bone resembles a tree branch (greenstick) that has been sharply
bent but not disconnected.
beginning during the 5th and 6th embryonic weeks from medial and
lateral primary centers that are close together in the shaft of the
clavicle. The ends of the clavicle later pass through a cartilaginous
phase (endochondral ossification); the
cartilages form growth zones similar to those of other long bones. A
secondary ossification center appears at the sternal end and forms a
scale-like epiphysis that begins to fuse with the shaft (diaphysis)
between 18 and 25 years of age and is completely fused to it between 25
and 31 years of age. This is the last of the epiphyses of long bones to
fuse. An even smaller scale-like epiphysis may be present at the
acromial end of the clavicle; it must not be mistaken for a fracture.
clavicle fails to occur; as a result, a bony defect forms between the
lateral and the medial thirds of the clavicle. Awareness of this
possible congenital defect should prevent diagnosis of a fracture in an
otherwise normal clavicle. When doubt exists, both clavicles are
radiographed because this defect is usually bilateral (Ger et al., 1996).
(superior appendicular skeleton) to the trunk (axial skeleton). It
serves as a movable crane-like strut from which the scapula and free
limb are suspended at a distance from the trunk that enables freedom of
motion. Shocks received by the upper limb (especially the shoulder) are
transmitted through the clavicle, resulting in a fracture that most
commonly occurs between its middle and lateral thirds. The clavicle is
the first long bone to ossify and the last to be fully formed.
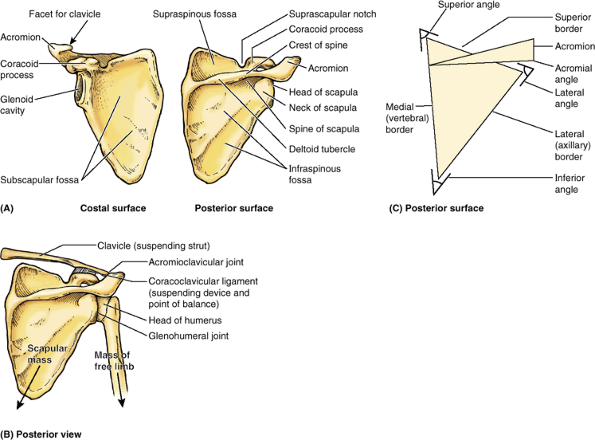
scapula
is thin and translucent superior and inferior to the scapular spine;
although its borders, especially the lateral one, are somewhat thicker.
The spine continues laterally as the flat expanded acromion (G. akros, point), which forms the subcutaneous point of the shoulder and articulates with the acromial end of the clavicle. The deltoid tubercle of the scapular spine
is the prominence indicating the medial point of attachment of the
deltoid. The spine and acromion serve as levers for the attached
muscles, particularly the trapezius.
 |
|
Figure 6.4. Right scapula. A. The bony features of the costal and posterior surfaces of the scapula are demonstrated. B.
The scapula is suspended from the clavicle by the coracoclavicular ligament, at which a balance is achieved among the weight of the scapula, its attached muscles, and the muscular activity medially and the weight of the free limb laterally. C. The borders and angles of the scapula are demonstrated. |
scapula, the AC joint is placed lateral to the mass of the scapula and
its attached muscles (Fig. 6.4B). The glenohumeral (shoulder) joint
on which these muscles operate is almost directly inferior to the AC
joint; thus the scapular mass is balanced with that of the free limb,
and the suspending structure (coracoclavicular ligament) lies between
the two masses.
directed anterolaterally and slightly superiorly, that is considerably
smaller than the ball (head of the humerus) for which it serves as
socket. The beak-like coracoid process (G. korakoédés,
like a crow’s beak) is superior to the glenoid cavity and projects
anterolaterally. This process also resembles in size, shape, and
direction a bent finger pointing to the shoulder, the knuckle of which
provides the inferior attachment for the passively supporting
coracoclavicular ligament.
The lateral border is made up of a thick bar of bone that prevents
buckling of this stress-bearing region of the scapula. The lateral
border terminates in the truncated lateral angle of the scapula, the thickest part of the bone that bears the broadened head of the scapula. The glenoid cavity is the primary feature of the head. The shallow constriction between the head and the body defines the neck of the scapula. The superior border of the scapula is marked near the junction of its medial two thirds and lateral third by the suprascapular notch, which is
located where the superior border joins the base of the coracoid
process. The superior border is the thinnest and shortest of the three
borders.
providing the base from which the upper limb operates. These movements,
enabling the arm to move freely, are discussed later in this chapter
with the muscles that move the scapula.
trauma, as occurs in pedestrian–vehicle accidents. Usually there are
also fractured ribs. Most fractures require little treatment because
the scapula is covered on both sides by muscles. Most fractures involve
the protruding subcutaneous acromion.
upper limb acts. This triangular flat bone is curved to conform to the
thoracic wall and provides large surface areas and edges for attachment
of muscles. These muscles (1) move the scapula on the thoracic wall at
the physiological scapulothoracic joint and (2) extend to the proximal
humerus maintaining the integrity of—and producing motion at—the
glenohumeral joint. Its spine and acromion serve as levers; the
acromion enables the scapula and attached muscles to be located
medially against the trunk with the AC and glenohumeral joints, thereby
allowing movement lateral to the trunk. Its coracoid process is the
site of attachment for the coracoclavicular ligament that passively
supports the upper limb and a site for muscular (tendon) attachment.
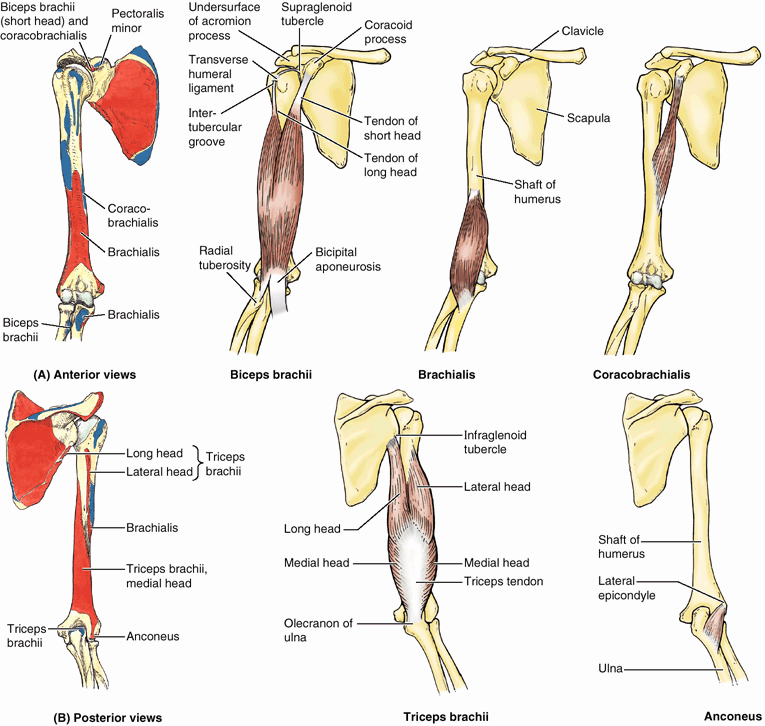
largest bone in the upper limb, articulates with the scapula at the
glenohumeral joint and the radius and ulna at the elbow joint (Figs. 6.1 and 6.2). The proximal end of the humerus has a head, surgical and anatomical necks, and greater and lesser tubercles. The spherical head of the humerus articulates with the glenoid cavity of the scapula. The anatomical neck of the humerus
is formed by the groove circumscribing the head and separating it from
the greater and lesser tubercles. It indicates the line of attachment
of the glenohumeral joint capsule. The surgical neck of the humerus,
a common site of fracture, is the narrow part distal to the head and
tubercles. The junction of the head and neck with the shaft of the
humerus is indicated by the greater and lesser tubercles, which provide
attachment and leverage to some scapulohumeral muscles. The greater tubercle is at the lateral margin of the humerus, whereas the lesser tubercle projects anteriorly from the bone. The intertubercular (bicipital) groove separates the tubercles and provides protected passage for the slender tendon of the long head of the biceps muscle.
spiral groove) posteriorly, in which the radial nerve and deep artery
of the arm lie as they pass anterior to the long and between the medial
and lateral heads of the triceps brachii muscle. The inferior end of
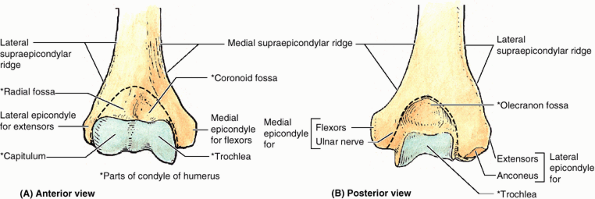
the humeral shaft widens as the sharp medial and lateral supraepicondylar (supracondylar) ridges form and then end distally in the especially prominent medial epicondyle and the lateral epicondyle, providing for muscle attachment.
the capitulum; and the olecranon, coronoid, and radial fossae, makes up
the condyle of the humerus (Fig. 6.5). The condyle has two articular surfaces: a lateral capitulum (L. little
head) for articulation with the head of the radius and a medial, spool-shaped or pulley-like trochlea
(L. pulley) for articulation with the proximal end (trochlear notch) of
the ulna. Two hollows or fossae occur back to back superior to the
trochlea, making the condyle quite thin between the epicondyles.
Anteriorly, the coronoid fossa receives the coronoid process of the ulna during full flexion of the elbow. Posteriorly, the olecranon fossa accommodates the olecranon of the ulna during full extension of the elbow. Superior to the capitulum anteriorly, a shallower radial fossa accommodates the edge of the head of the radius when the forearm is fully flexed.
 |
|
Figure 6.5. Distal end of right humerus. A and B.
Anterior and posterior views illustrate the lateral and medial epicondyles, supraepicondylar ridges, and condyle of the humerus. The condyle (the boundaries of which are indicated by the dashed line) consists of the capitulum; the trochlea; and the radial, coronoid, and olecranon fossae. |
whose demineralized bones are brittle. Humeral fractures are often
result in one fragment being driven into the spongy bone of the other
fragment (impacted fracture). The injuries
usually result from a minor fall on the hand, with the force being
transmitted up the forearm bones of the extended limb. Because of
impaction of the fragments, the fracture site is sometimes stable and
the person is able to move the arm passively with little pain.
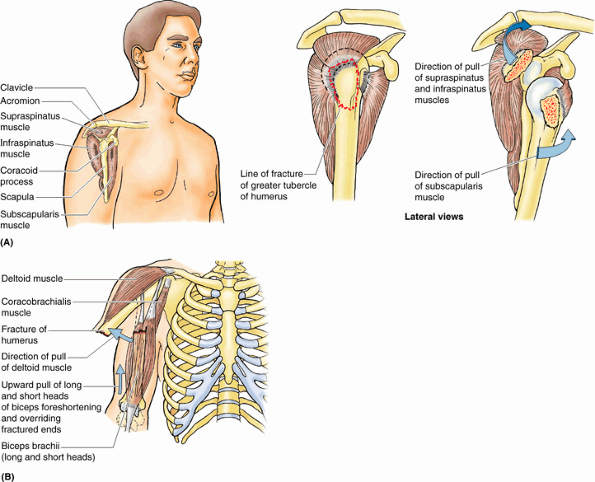
The fracture usually results from a fall on the acromion, the point of
the shoulder. In younger people, an avulsion fracture of the greater
tubercle usually results from a fall on the hand when the arm is
abducted. Muscles (especially the subscapularis) that remain attached
to the humerus pull the limb into medial rotation.
 |
|
Figure B6.2. Humeral fractures. A. An avulsion fracture of the greater tubercle of the humerus is shown. B. A transverse fracture of humeral body is demonstrated.
|
Overriding of the oblique ends of the fractured bone may result in
foreshortening. Because the humerus is surrounded by muscles and has a
well-developed periosteum, the bone fragments usually unite well. An intercondylar fracture of the humerus
results from a severe fall on the flexed elbow. The olecranon of the
ulna is driven like a wedge between the medial and lateral parts of the
condyle, separating one or both parts from the humeral shaft.
-
Surgical neck: axillary nerve.
-
Radial groove: radial nerve.
-
Distal end of humerus: median nerve.
-
Medial epicondyle: ulnar nerve.
the humerus is fractured. These injuries are discussed later in this
chapter.
a series of two—used to position the hand at a height (level) and
distance from the trunk to maximize its efficiency. Its spherical head
enables a great range of motion on the mobile scapular base, and the
trochlea and capitulum at its distal end facilitate the hinge movements
of the elbow and, at the same time, the pivoting of the radius. The
long shaft of the humerus enables reach and makes it an effective lever
for power in lifting as well as providing surface area for attachment
of muscles that act primarily at the elbow. Added surface area for
attachment of flexors and extensors of the wrist is provided by the
epicondyles, the medial and lateral extensions of the shaft.
unit of an articulated mobile strut (the first unit being the humerus),
with a mobile base formed by the shoulder, that positions the hand.
However, because this unit is formed by two parallel bones, one of
which (the radius) can pivot about the other (the ulna), supination and
pronation are possible. This makes it possible to rotate the hand when
the elbow is flexed.
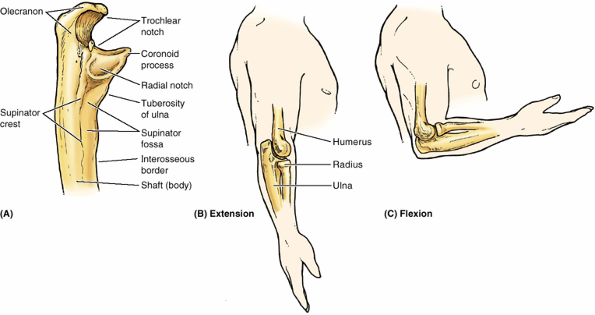
Its more massive proximal end is specialized for articulation with the
humerus proximally and the head of the radius laterally. For
articulation with the humerus, it has two prominent projections: (1)
the olecranon,
which projects proximally from its posterior aspect (forming the point
of the elbow) and serves as a short lever for extension of the elbow,
and (2) the coronoid process, which projects anteriorly. The olecranon and coronoid processes form the walls of the trochlear notch, which in profile resembles the jaws of a crescent wrench as it “grips” (articulates with) the trochlea of the humerus (Fig. 6.6B & C).
The articulation between the ulna and the humerus primarily allows only
flexion and extension of the elbow joint, although a small amount of
abduction–adduction occurs during pronation and supination of the
forearm. Inferior to the coronoid process is the tuberosity of the ulna for attachment of the tendon of the brachialis muscle (Fig. 6.6A).
 |
|
Figure 6.6. Bones of right elbow region. A. The proximal part of the ulna is shown. B.
The bones of the elbow region are shown, demonstrating the relationship of the distal humerus and proximal ulna and radius during extension of the elbow joint. C. The relationship of the humerus and forearm bones during flexion of the elbow joint is demonstrated. |
 |
|
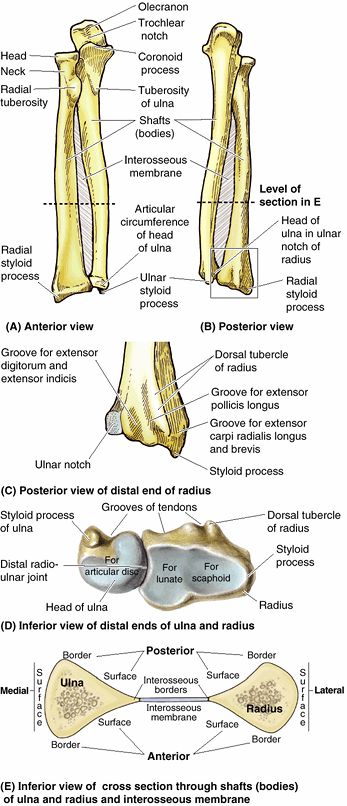
Figure 6.7. Right radius and ulna. A and B. The radius and ulna are shown in the articulated position, connected by the interosseous membrane. C and D.
The features of the distal ends of the forearm bones include grooves for tendons; a dorsal tubercle of the radius (used as a pulley); and articular surfaces for articulation with (1) each other (ulnar notch of radius, articular circumference of head of ulna; see part A), (2) an articular disc (ulna), and (3) the proximal carpal bones (radius). E. In cross section, the shafts of the radius and ulna appear almost as mirror images of one another for much of the middle and distal thirds of their lengths. |
which receives the broad periphery of the head of the radius. Inferior
to the radial notch on the lateral surface of the ulnar shaft is a
prominent ridge, the supinator crest. Between it and the distal part of the coronoid process is a concavity, the supinator fossa. The deep part of the supinator muscle attaches to the supinator crest and fossa.
and shorter of the two forearm bones. Its proximal end includes a short
head, neck, and medially directed tuberosity (Fig. 6.7A). Proximally, the smooth superior aspect of the discoid head of the radius
is concave for articulation with the capitulum of the humerus during
flexion and extension of the elbow joint. The head also articulates
peripherally with the radial notch of the ulna; thus the head is
covered with articular cartilage. The neck of the radius is a constriction distal to the head. The oval radial tuberosity is distal to the medial part of the neck and demarcates the proximal end (head and neck) of the radius from the shaft.
in contrast to that of the ulna, gradually enlarges as it passes
distally. The distal end of the radius is essentially four sided when
sectioned transversely. Its medial aspect forms a concavity, the ulnar notch (Fig. 6.7C & D), which accommodates the head of the ulna. Its lateral aspect becomes increasingly ridge-like, terminating distally in the radial styloid process. Projecting dorsally, the dorsal tubercle of the radius
lies between otherwise shallow grooves for the passage of the tendons
of forearm muscles. The radial styloid process is larger than the ulnar
styloid process and extends farther distally. This relationship
is of clinical importance when the ulna and/or the radius is fractured.
are essentially triangular in cross section, with a rounded,
superficially directed base and an acute, deeply directed apex (Fig. 6.7E). The apex is formed by a section of the sharp interosseous border of the radius or ulna that connects to the thin, fibrous interosseous membrane of the forearm (Fig. 6.7A, B, & E).
The majority of the fibers of the interosseous membrane run an oblique
course, passing inferiorly from the radius as they extend medially to
the ulna (Fig. 6.7A & B).
Thus they are positioned to transmit forces received by the radius (via
the hands) to the ulna for transmission to the humerus.
the result of severe injury. A direct injury usually produces
transverse fractures at the same level, usually in the middle third of
the bones. Isolated fractures of the radius or ulna also occur. Because
the shafts of these bones are firmly bound together by the interosseous
membrane, a fracture of one bone is likely to be associated with
dislocation of the nearest joint.
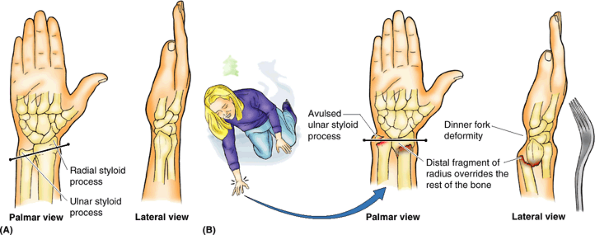
is a common fracture in adults > 50 years of age and occurs more
frequently in women because their bones are more commonly weakened by osteoporosis. A complete transverse fracture of the distal 2 cm of the radius, called a Colles fracture, is the most common fracture of the forearm (Fig. B6.3). The distal fragment is displaced dorsally and is often comminuted
(broken into pieces). The fracture results from forced dorsiflexion of
the hand, usually as the result of trying to ease a fall by
outstretching the upper limb. Often the ulnar styloid process is avulsed (broken off). Normally the radial styloid process projects farther distally than the ulnar styloid (Fig. B6.3A); consequently, when a Colles fracture occurs, this relationship is reversed because of shortening of the radius (Fig. B6.3B). This clinical condition is often referred to as a dinner fork (silver fork) deformity
because a posterior angulation occurs in the forearm just proximal to
the wrist and the normal anterior curvature of the relaxed hand. The
posterior bending is produced by the posterior displacement and tilt of
the distal fragment of the radius.
includes slipping or tripping and, in an attempt to break the fall,
landing on the outstretched limb with the forearm and hand pronated.
Because of the rich blood supply to the distal end of the radius, bony
union is usually good.
are common in older children because of their frequent falls in which
the forces are transmitted from the hand to the radius and ulna. The
healing process may result in malalignment of the epiphysial plate and
disturbance of radial growth.
 |
|
Figure B6.3. Right wrist. A. A normal wrist is shown. B. A Colles fracture with a dinner fork deformity is demonstrated.
|
a two-unit articulated strut (the first unit being the humerus),
projecting from a mobile base (shoulder) that serves to position the
hand. Because the forearm unit is formed by two parallel bones, and the
radius is able to pivot about the ulna, supination and pronation of the
hand are possible during elbow flexion. Proximally, the larger medial
ulna forms the primary articulation with the humerus, whereas distally,
the shorter lateral radius forms the primary articulation with the hand
via the wrist. Because the ulna does not reach the wrist, forces
received by the hand are transmitted from the radius to the ulna via
the interosseous membrane.
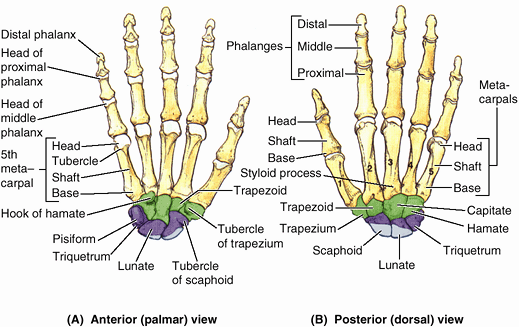
These small bones give flexibility to the wrist. The carpus is markedly
convex from side to side posteriorly and concave anteriorly. Augmenting
movement at the wrist joint, the two rows of carpals glide on each
other; in addition, each bone glides on those adjacent to it.
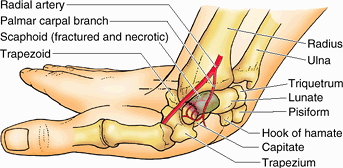
-
Scaphoid (G. skaphé, skiff, boat): a boat-shaped bone that articulates proximally with the radius and has a prominent scaphoid tubercle; it is the largest bone in the proximal row of carpals.
-
Lunate (L. luna,
moon): a moon-shaped bone between the scaphoid and the triquetral
bones; it articulates proximally with the radius and is broader
anteriorly than posteriorly. -
Triquetrum (L. triquetrus,
three-cornered): a pyramidal bone on the medial side of the carpus; it
articulates proximally with the articular disc of the distal radioulnar
joint. -
Pisiform (L. pisum, pea), a small, pea-shaped bone that lies on the palmar surface of the triquetrum.
-
Trapezium (G. trapeze,
table): a four-sided bone on the lateral side of the carpus; it
articulates with the 1st and 2nd metacarpals, scaphoid, and trapezoid
bones. -
Trapezoid: a
wedge-shaped bone that resembles the trapezium; it articulates with the
2nd metacarpal, trapezium, capitate, and scaphoid bones. -
Capitate (L. caput,
head): a head-shaped bone with a rounded extremity and the largest bone
in the carpus; it articulates primarily with the 3rd metacarpal
distally, and with the trapezoid, scaphoid, lunate, and hamate. -
Hamate (L. hamulus,
a little hook): a wedge-shaped bone on the medial side of the hand; it
articulates with the 4th and 5th metacarpal, capitate, and triquetral
bones; it has a distinctive hooked process, the hook of the hamate, that extends anteriorly.
articulate with the proximal row of carpals, and their distal surfaces
articulate with the metacarpals.
of five metacarpal bones (metacarpals). Each metacarpal consists of a base, shaft, and head. The proximal bases of the metacarpals articulate with the carpal bones, and the distal heads of the metacarpals
articulate with the proximal phalanges and form the knuckles. The 1st
metacarpal (of the thumb) is the thickest and shortest of these bones.
The 3rd metacarpal is distinguished by a styloid process on the lateral side of its base.
 |
|
Figure 6.8. Bones of right hand. A and B.
The skeleton of the hand consists of three segments: carpals of the wrist, metacarpals of the palm, and phalanges of the fingers or digits. |
except for the first (the thumb), which has only two; however, the
phalanges of the first digit are stouter than those in the other
fingers. Each phalanx has a base proximally, a shaft (body), and a head distally (Fig. 6.8).
The proximal phalanges are the largest, the middle ones are
intermediate in size, and the distal ones are the smallest. The shafts
of the phalanges taper distally. The terminal phalanges are flattened
and expanded at their distal ends, which underlie the nail beds.
bone. It often results from a fall on the palm when the hand is
abducted, the fracture occurring across the narrow part (“waist”) of
the scaphoid (Fig. B6.4). Pain occurs primarily
on the lateral side of the wrist, especially during dorsiflexion and
abduction of the hand. Initial radiographs of the wrist may not reveal
a fracture; often this injury is (mis-)diagnosed as a severely sprained wrist.
Radiographs taken 10–14 days later reveal a fracture because bone
resorption has occurred there. Owing to the poor blood supply to the
proximal part of the scaphoid, union of the fractured parts may take at
least 3 months. Avascular necrosis of the proximal fragment of the scaphoid (pathological death of bone resulting from inadequate blood supply) may occur and produce degenerative joint disease of the wrist. In some cases, it is necessary to fuse the carpals surgically (arthrodesis).
 |
|
Figure B6.4
|
fractured bony parts because of the traction produced by the attached
muscles. Because the ulnar nerve is close to the hook of the hamate,
the nerve may be injured by this fracture, causing decreased grip
strength of the hand. The ulnar artery may also be damaged when the
hamate is fractured.
together; hence isolated fractures tend to be stable. Furthermore,
these bones have a good blood supply, and fractures usually heal
rapidly. Severe crushing injuries of the hand
may produce multiple metacarpal fractures, resulting in instability of
the hand. Fracture of the 5th metacarpal, often referred to as a boxer’s fracture,
occurs when an unskilled person punches someone with a closed fist. The
head of the bone rotates over the distal end of the shaft, producing a
flexion deformity.
are common (e.g., when a finger is caught in a car door). Because of
the highly developed sensation in the fingers, these injuries are
extremely painful. A fracture of a distal phalanx is usually comminuted, and a painful hematoma
(local collection of blood) soon develops. Fractures of the proximal
and middle phalanges are usually the result of crushing or
hyperextension injuries. Because of the close relationship of
phalangeal fractures to the flexor tendons, the bone fragments must be
carefully realigned to restore normal function of the fingers.
functionality of the end unit, the hand. Located on the free end of a
two-unit articulated strut (arm and forearm) projecting from a mobile
base (shoulder), the hand can be positioned over a wide range relative
to the trunk. Its connection to the flexible strut via the multiple
small bones of the wrist, combined with the pivoting of the forearm,
greatly increases its ability to be placed in a particular position
with the fingers able to flex (push or grip) in the necessary
direction. The carpal bones are organized into two rows of four bones
each, and as a group articulate with the radius proximally and the
metacarpals distally. The highly flexible, elongated fingers—extending
from a semirigid base (the palm)—enable the ability to grip,
manipulate, or perform complex tasks involving multiple and
simultaneous individual motions (e.g., when typing or playing a piano).
surface (notable exceptions being the lunate and trapezoid), enabling
the skilled examiner to discern abnormalities owing to trauma (fracture
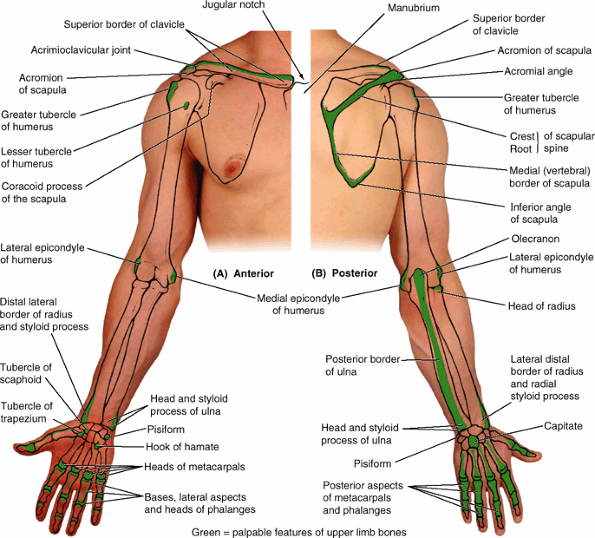
or dislocation) or malformation (Fig. SA6.1).
(suprasternal notch). The acromial end of the clavicle often rises
higher than the acromion, forming a palpable elevation at the acromioclavicular (AC) joint.
The acromial end can be palpated 2–3 cm medial to the lateral border of
the acromion, particularly when the arm is alternately flexed and
extended. Either or both ends of the clavicle may be prominent; when
present, this condition is usually bilateral. Note the elasticity of
the skin over the clavicle and how easily it can be pinched into a
mobile fold. This property of the skin is useful when ligating the
third part of the subclavian artery: the skin lying superior to the
clavicle is pulled down onto the clavicle and then incised; after the
incision is made, the skin is allowed to return to its position
superior to the clavicle, where it overlies the artery (thus not
endangering it during the incision).
is easily felt and often visible. The superior surface of the acromion
is subcutaneous and may be traced medially to the AC joint. The lateral
and posterior borders of the acromion meet to form the acromial angle (Fig. SA6.1B). Inferior to the acromion, the deltoid muscle forms the rounded curve of the shoulder. The crest of the scapular spine is subcutaneous throughout and easily palpated.
 |
|
Figure SA6.1.
|
-
Superior angle of the scapula lies at the level of the T2 vertebra.
-
Medial end of the root of the scapular spine is opposite the spinous process of the T3 vertebra.
-
Inferior angle of the scapula lies at the
level of the T7 vertebra, near the inferior border of the 7th rib and
7th intercostal space.
is palpable inferior to the root of the spine of the scapula as it
crosses the 3rd–7th ribs; the lateral border of the scapula is not
easily palpated because it is covered by the teres major and minor
muscles. When the upper limb is abducted and the hand is placed on the
back of the head, the scapula is rotated, elevating the glenoid cavity
such that the medial border of the scapula parallels the 6th rib and
thus can be used to estimate its position and, deep to the rib, the
oblique fissure of the lung. The inferior angle of the scapula
is easily felt and is often visible. It is grasped when testing
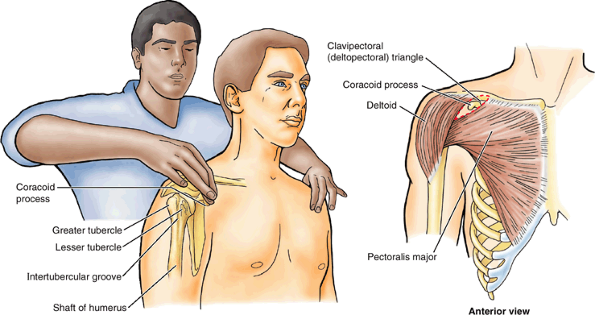
movements of the glenohumeral joint to immobilize the scapula. The coracoid process of the scapula can be felt by palpating deeply at the lateral side of the clavipectoral triangle (Fig. SA6.2).
(armpit). The arm should not be fully abducted, otherwise the fascia in
the axilla will be tense and impede palpation of the humeral head. When
the arm is moved and the scapula is fixed (held in place), the head of
the humerus can be palpated.
may be felt with the person’s arm by the side on deep palpation through
the deltoid, inferior to the lateral border of the acromion. In this
position, the greater tubercle is the most lateral bony point of the
shoulder and, along with the deltoid, gives the shoulder its rounded
contour. When the arm is abducted, the greater tubercle is pulled
beneath the acromion and is no longer palpable. The lesser tubercle of the humerus
may be felt with difficulty by deep palpation through the deltoid on
the anterior aspect of the arm, approximately 1 cm lateral and slightly
inferior to the tip of the coracoid process. Rotation of the arm
facilitates palpation of this tubercle. The location of the intertubercular groove,
between the greater and the lesser tubercles, is identifiable during
flexion and extension of the elbow joint by palpating in an upward
direction along the tendon of the long head of the biceps brachii as it
moves through the intertubercular groove.
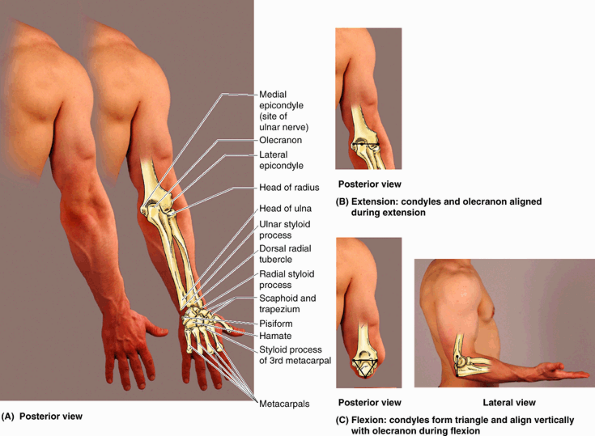
be felt with varying distinctness through the muscles surrounding it.
No part of the proximal part of the humeral shaft is subcutaneous. The
medial and lateral epicondyles of the humerus are subcutaneous and
easily palpated on the medial and lateral aspects of the elbow region.
The knob-like medial epicondyle, projecting posteromedially, is more prominent than the lateral epicondyle. When the elbow joint is partially flexed, the lateral epicondyle
is visible. When the elbow joint is fully extended, the lateral
epicondyle can be palpated but not seen deep to a depression on the
posterolateral aspect of the elbow.
 |
|
Figure SA6.2
|
When the elbow is flexed, the olecranon descends until its tip forms
the apex of an approximately equilateral triangle, of which the
epicondyles form the angles at its base (Fig. SA6.3C).
These normal relationships are important in the diagnosis of certain
elbow injuries (e.g., dislocation of the elbow joint). The posterior border of the ulna,
palpable throughout the length of the forearm, demarcates the
posteromedial boundary between the flexor–pronator and the
extensor–supinator compartments of the forearm. The head of the ulna
forms a large, rounded subcutaneous prominence that can be easily seen
and palpated on the medial side of the dorsal aspect of the wrist,
especially when the hand is pronated. The pointed subcutaneous ulnar styloid process may be felt slightly distal to the rounded ulnar head when the hand is supinated.
be palpated and felt to rotate in the depression on the posterolateral
aspect of the extended elbow joint, just distal to the lateral
epicondyle of the humerus. The radial head can also be palpated as it
rotates during pronation and supination of the forearm. The ulnar nerve
feels like a thick cord where it passes posterior to the medial
epicondyle of the humerus; pressing the nerve here evokes an unpleasant
“crazy bone” sensation.
on the lateral side of the wrist; it is larger and approximately 1 cm
more distal than the ulnar styloid process. The radial styloid process
is easiest to palpate when the thumb is abducted. It is overlaid by the
tendons of the thumb muscles. Because the radial styloid process
extends more distally than the ulnar styloid process, more ulnar
deviation than radial deviation of the wrist is possible. The
relationship of the radial and ulnar processes is important in the
diagnosis of certain wrist injuries (e.g., Colles fracture). Proximal
to the radial styloid process, the anterior, lateral, and posterior surfaces of the radius are palpable for several centimeters. The dorsal radial tubercle
is easily felt around the middle of the dorsal aspect of the distal end
of the radius. The dorsal tubercle acts as a pulley for the long
extensor tendon of the thumb, which passes medial to it.
 |
|
Figure SA6.3
|
the anterior aspect of the medial border of the wrist and can be moved
from side to side when the hand is relaxed. The hook of the hamate can be palpated on deep pressure over the medial side of the palm, approximately 2 cm distal and lateral to the pisiform. The tubercles of the scaphoid and trapezium can be palpated at the base and medial aspect of the thenar eminence (ball of thumb) when the hand is extended.
overlain by the long extensor tendons of the digits, can be palpated on
the dorsum of the hand. The heads of these bones form the knuckles of
the fist; the 3rd metacarpal head is most prominent. The styloid process of the 3rd metacarpal
can be palpated approximately 3.5 cm from the dorsal radial tubercle.
The dorsal aspects of the phalanges can also be easily palpated. The
knuckles of the fingers are formed by the heads of the proximal and
middle phalanges.
comparison with the contralateral limb or with standards for normal
limb growth or size, the acromial angle, lateral epicondyle of the
humerus, styloid process of the radius, and tip of the third finger are
most commonly used as measuring points, with the limb relaxed
(dangling) but with palms directed anteriorly.
that are useful (1) when diagnosing fractures, dislocations, or
malformations; (2) for approximating the position of deeper structures;
and (3) for precisely describing the location of incisions and sites
for therapeutic puncture or of pathology or injury.
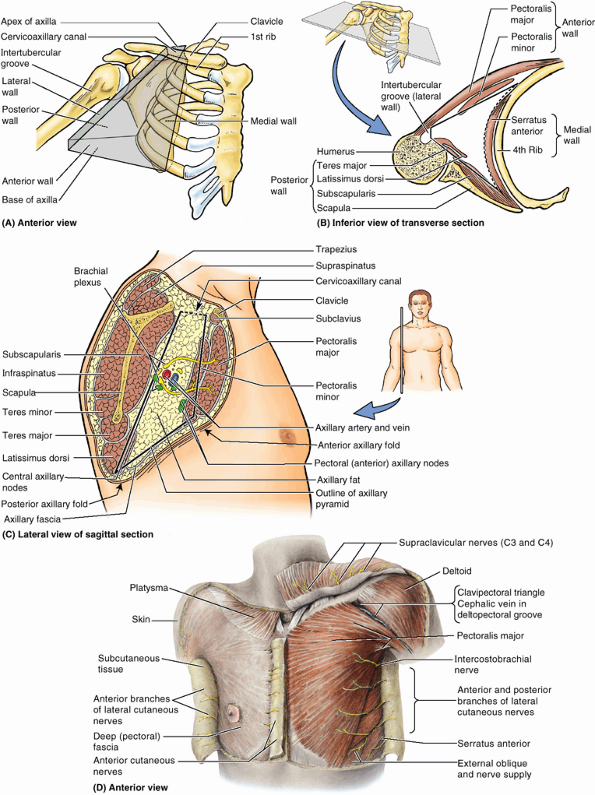
fascia) containing fat and deep fascia surrounding the muscles. If no
structure (no muscle, tendon, or bursa, for example) intervenes between
the skin and the bone, the deep fascia is usually attached to bone.
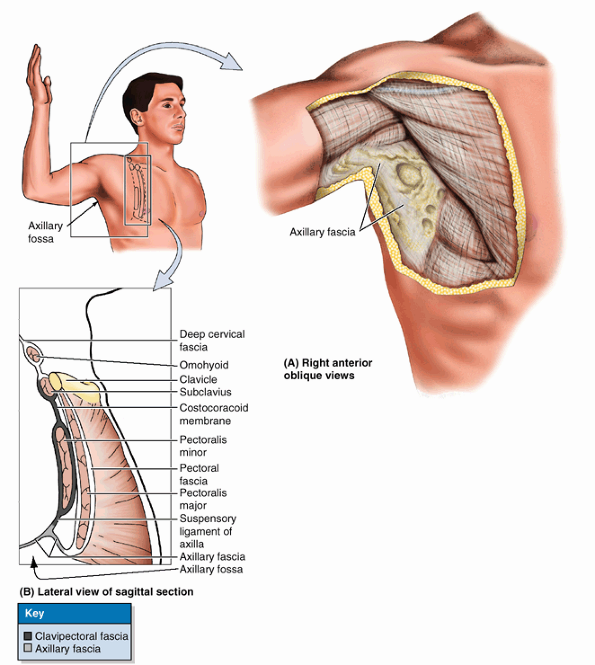
descends from the clavicle, enclosing the subclavius and then the
pectoralis minor, becoming continuous inferiorly with the axillary
fascia. The part of the clavipectoral fascia between the pectoralis
minor and the subclavius, the costocoracoid membrane,
is pierced by the lateral pectoral nerve, which primarily supplies the
pectoralis major. The part of the clavipectoral fascia inferior to the
pectoralis minor, the suspensory ligament of the axilla, supports the axillary fascia and pulls it and the skin inferior to it upward during abduction of the arm, forming the axillary fossa.
descends over the superficial surface of the deltoid from the clavicle,
acromion, and scapular spine. From the deep surface of the deltoid
fascia, numerous septa penetrate between the fascicles (bundles) of the
muscle. Inferiorly, the deltoid fascia is continuous with the pectoral
fascia anteriorly and the dense infraspinous fascia posteriorly. The
muscles that cover the anterior and posterior surfaces of the scapula
are covered superficially with deep fascia, which is attached to the
margins of the scapula and posteriorly to the spine of the scapula.
This arrangement creates osseofibrous subscapular, supraspinous, and infraspinous compartments;
the muscles in each compartment attach to (originate from) the deep
surface of the overlying fascia in part, allowing the muscles to have
greater bulk (mass) than would be the case if only bony attachments
occurred. The supraspinous and infraspinous fascia
overlying the supraspinatus and infraspinatus muscles, respectively, on
the posterior aspect of the scapula are so dense and opaque that they
must be removed during dissection to view the muscles.
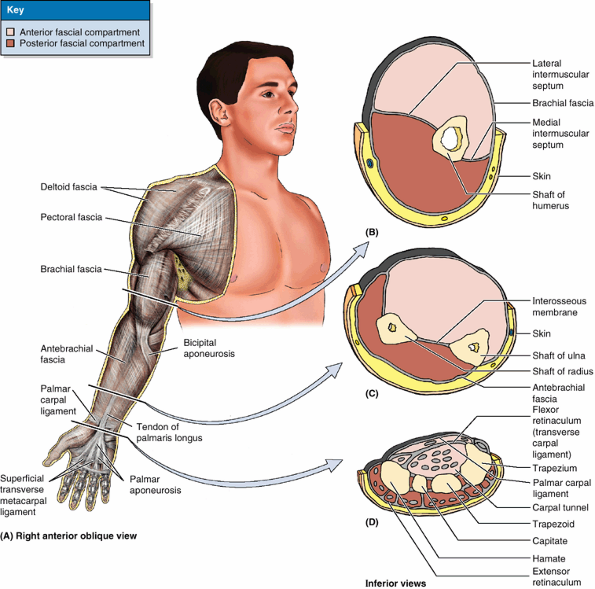
it is continuous superiorly with the deltoid, pectoral, axillary, and
infraspinous fasciae. The brachial fascia is attached inferiorly to the
epicondyles of the humerus and the olecranon of the ulna and is
continuous with the antebrachial fascia, the deep fascia of the
forearm. Two intermuscular septa, the medial and lateral intermuscular septa, extend from the deep surface of the brachial fascia to the central shaft and medial and lateral supraepicondylar ridges of
the humerus (Fig. 6.10B). These septa divide the arm into anterior (flexor) and posterior (extensor) fascial compartments,
each of which contains muscles serving similar functions and sharing
common innervation. As discussed in relation to the fascial
compartments of the lower limb (see Chapter 5),
the fascial compartments of the upper limb are important clinically
because they also contain and direct the spread of infection or
hemorrhage in the limb.
 |
|
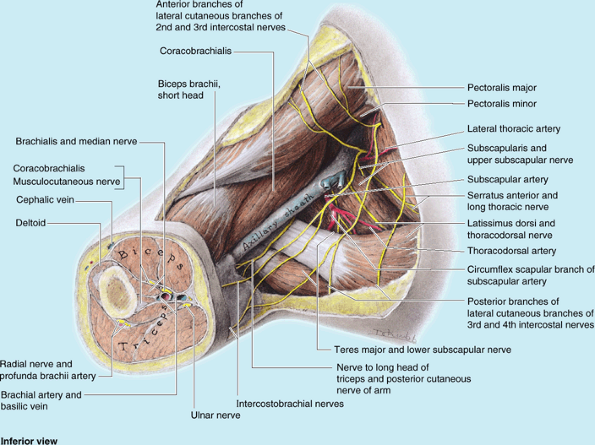
Figure 6.9. Anterior wall and floor of axilla. A. Axillary fascia forms the floor of the axilla and is continuous with the pectoral fascia. B.
The pectoral fascia surrounds the pectoralis major, forming the anterior layer of the anterior axillary wall. The clavipectoral fascia extends between the coracoid process of the scapula, the clavicle, and the axillary fascia, enveloping the subclavius and pectoralis minor muscles and forming the posterior layer of the anterior axillary wall. The suspensory ligament of the axilla is the part of the clavipectoral, which attaches to the axillary fascia; when the arm is abducted, traction by the suspensory ligament pulls the axillary fascia superiorly, producing the hollow of the axillary fossa. |
distal ends of the radius and ulna to form a transverse band, the extensor retinaculum,
which retains the extensor tendons in position. The antebrachial fascia
also forms an anterior thickening, which is continuous with the
extensor retinaculum but is officially unnamed; some authors identify
it as the palmar carpal ligament (Fig. 6.10D). Immediately distal and at a deeper level to the latter, the antebrachial fascia is also continued as the flexor retinaculum (transverse carpal ligament).2
This fibrous band extends between the anterior prominences of the outer
carpal bones and converts the anterior concavity of the carpus into a carpal tunnel, through which the flexor tendons and median nerve pass.
 |
|
Figure 6.10. Fascia and compartments of upper limb. A. Brachial and antebrachial fascia surround the structures of the free upper limb. B.
The intermuscular septa and humerus divide the space inside the brachial fascia into anterior and posterior compartments, each of which contains muscles serving similar functions and the nerves and vessels supplying them. C. The interosseous membrane and the radius and ulna similarly separate the space inside the antebrachial fascia into anterior and posterior compartments. D. Continuing distal to the radius and ulna onto the carpal bones, the deep fascia of the forearm thickens to form the extensor retinaculum posteriorly and a corresponding thickening anteriorly (palmar carpal ligament). At a deeper level to the latter, a ligamentous formation, the flexor retinaculum (transverse carpal ligament) extends between the anterior prominences of the outer carpal bones, converting the anterior concavity of the carpus into an osseofibrous carpal tunnel. |
is thick, tendinous, and triangular and it overlies the central
compartment of the palm. Its apex, located proximally, is continuous
with the tendon of the palmaris longus (when it is present) (Fig. 6.10A).
The aponeurosis forms four distinct thickenings that radiate to the
bases of the fingers and become continuous with the fibrous tendon
sheaths of the digits. The bands are traversed distally by the superficial transverse metacarpal ligament, which forms the base of the palmar aponeurosis. Innumerable minute, strong skin ligaments (L. retinacula cutis) extend from the palmar aponeurosis to the skin (see the Introduction). These ligaments hold the palmar skin close to the aponeurosis, allowing little sliding movement of the skin.
contains the structures of the upper limb as an expansion-limiting
membrane deep to the skin and subcutaneous tissue. Its deep surface,
which occasionally serves to extend the surface area available for
muscular origin, is attached directly or via intermuscular septa to the
enclosed bones. The deep fascia thus forms fascial compartments
containing individual muscles or muscle groups of similar function and
innervation. The compartments also contain or direct the spread of
infection or hemorrhage.
pattern that is easy to understand if it is noted that developmentally
the limbs grow as lateral protrusions of the trunk, with the 1st digit
(thumb or great toe) located on the cranial side (thumb is directed
superiorly). Thus the lateral surface of the upper limb is more cranial
than the medial surface.
gained popular acceptance because of its more intuitive aesthetic
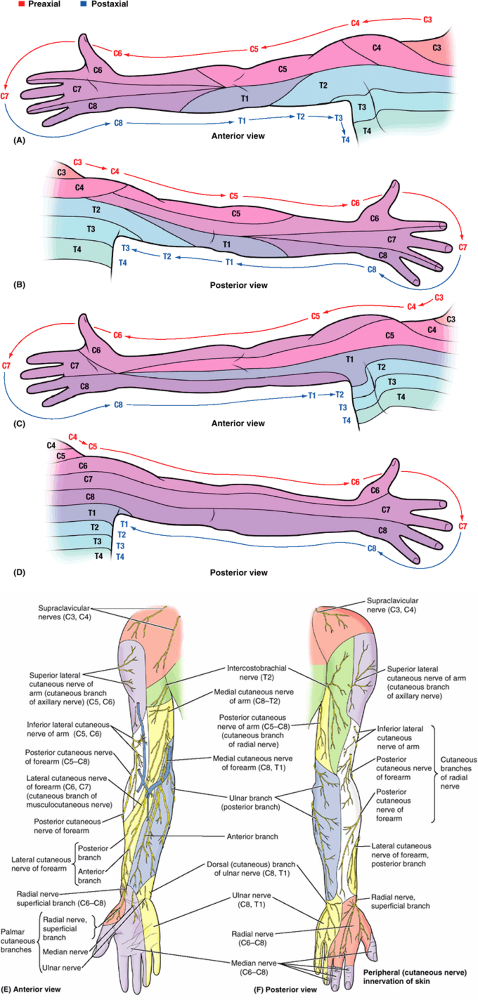
qualities, corresponding to concepts of limb development (Keegan and Garrett, 1948); the other is based on clinical findings and is generally preferred by neurologists (Foerster, 1933).
Both maps are approximations, delineating dermatomes as distinct zones
when actually there is much overlap between adjacent dermatomes and
much variation (even from side to side in the same individual). In both
maps, observe the progression of the segmental innervation of the
various cutaneous areas around the limb when it is placed in its
“initial embryonic position” (abducted with thumb directed superiorly) (Fig. 6.11A–D):
-
C3 and C4 nerves supply the region at the base of the neck extending laterally over the shoulder.
-
C5 nerve supplies the arm laterally (i.e., on the superior aspect of the abducted limb).
-
C6 nerve supplies the forearm laterally and the thumb.
-
C7 nerve supplies the middle and ring fingers (or middle three fingers) and the middle of the posterior surface of the limb.
-
C8 nerve supplies the little finger, the
medial side of the hand, and the forearm (i.e., the inferior aspect of
the outstretched limb). -
T1 nerve supplies the middle of the forearm to the axilla.
-
T2 nerve supplies a small part of the arm
and the skin of the axilla. (This is not indicated on the Keegan and
Garrett map; however, pain experienced during a heart attack,
considered to be mediated by T1 and T2, is commonly described as
“radiating down the medial side of the left arm”).
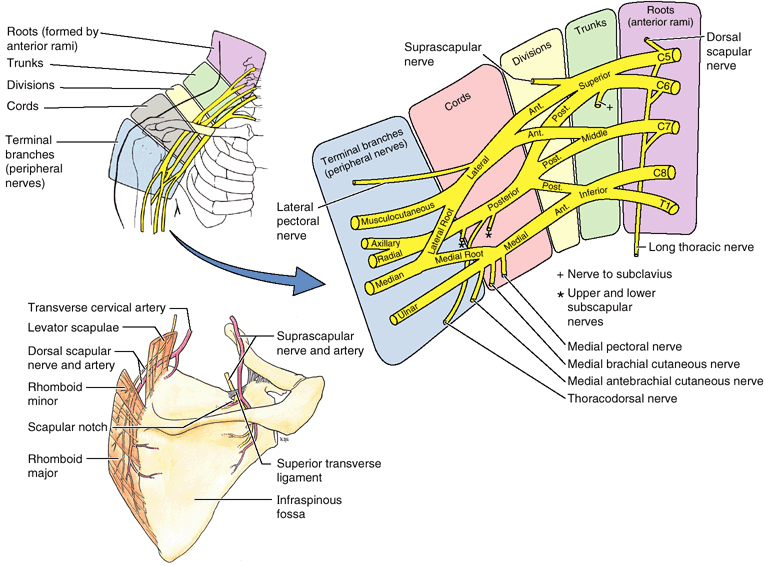
a nerve network consisting of a series of nerve loops formed between
adjacent anterior rami of the first four cervical nerves. The cervical
plexus lies deep to the sternocleidomastoid muscle on the anterolateral
aspect of the neck.
-
The supraclavicular nerves
(C3, C4) pass anterior to the clavicle, immediately deep to the
platysma, and supply the skin over the clavicle and the superolateral
aspect of the pectoralis major.P.746![]() Figure 6.11. Segmental (dermatomal) and peripheral (cutaneous nerve) innervation of upper limb. A and B. The pattern of segmental (dermatomal) innervation of the upper limb proposed by Foerster (1933)
Figure 6.11. Segmental (dermatomal) and peripheral (cutaneous nerve) innervation of upper limb. A and B. The pattern of segmental (dermatomal) innervation of the upper limb proposed by Foerster (1933)
depicts innervation of the medial aspect of the limb by upper thoracic
(T1–T3) spinal cord segments, consistent with the experience of heart
pain (angina pectoris) referred to that area. C and D. The pattern of segmental innervation proposed by Keegan and Garrett (1948)
has gained popular acceptance, perhaps because of the regular
progression of its stripes and correlation with developmental concepts.
In both patterns, the dermatomes progress sequentially around the
periphery of the outstretched limb (with the thumb directed
superiorly), providing a way to approximate the segmental innervation. E and F.
The distribution of the peripheral (named) cutaneous nerves in the
upper limb is demonstrated. Most of the nerves are branches of nerve
plexuses and therefore contain fibers from more than one spinal nerve
or spinal cord segment. -
The posterior cutaneous nerve of the arm (C5–C8), a branch of the radial nerve, supplies the skin on the posterior surface of the arm.
-
The posterior cutaneous nerve of the forearm (C5–C8), also a branch of the radial nerve, supplies the skin on the posterior surface of the forearm.
-
The superior lateral cutaneous nerve of the arm
(C5, C6), the terminal branch of the axillary nerve, emerges from
beneath the posterior margin of the deltoid and supplies skin over the
lower part of this muscle and on the lateral side of the midarm
inferior to its distal attachment to the lateral side of the arm a
little above its middle. -
The inferior lateral cutaneous nerve of the arm
(C5, C6), a branch of the radial nerve, supplies the skin over the
inferolateral aspect of the arm; it is frequently a branch of the
posterior cutaneous nerve of the forearm. -
The lateral cutaneous nerve of the forearm (C6, C7), the terminal cutaneous branch of the musculocutaneous nerve, supplies the skin on the lateral side of the forearm.
-
The medial cutaneous nerve of the arm
(C8–T2) arises from the medial cord of the brachial plexus, often
unites in the axilla with the lateral cutaneous branch of the 2nd
intercostal nerve, and supplies the skin on the medial side of the arm. -
The intercostobrachial nerve
(T2), a lateral cutaneous branch of the 2nd intercostal nerve, also
contributes to the innervation of the skin on the medial surface of the
arm. -
The medial cutaneous nerve of the forearm
(C8, T1) arises from the medial cord of the brachial plexus and
supplies the skin of the anterior and medial surfaces of the forearm.
no anterior) cutaneous nerves of the arm and forearm; as discussed
later in this chapter, this pattern corresponds to that of the cords of
the brachial plexus.
cutaneous innervation occur in the upper limb: (1) segmental
innervation (dermatomes) by spinal nerves and (2) innervation by
multisegmental peripheral (named) nerves. The former pattern is easiest
to visualize if the limb is placed in its initial embryonic position
(abducted with the thumb directed superiorly). The segments then
progress in descending order around the limb (starting with C4
dermatome at the root of the neck, proceeding laterally or distally
along the superior surface and then medially or proximally along the
inferior surface, as the T2 dermatome continues onto the thoracic
wall). Like the brachial plexus, which forms posterior, lateral, and
medial (but no anterior) cords, the arm and forearm have posterior,
lateral, and medial (but no anterior) cutaneous nerves.
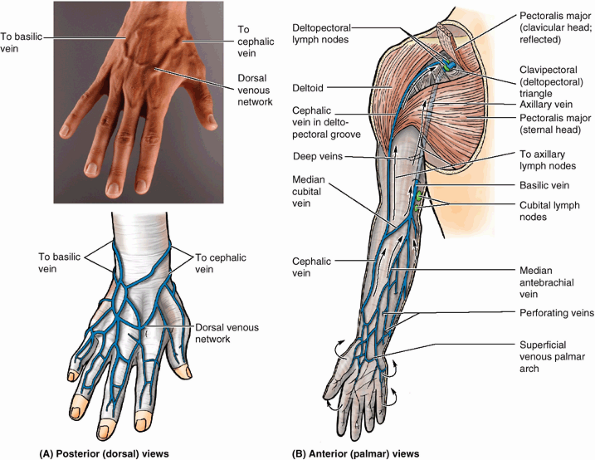
cephalic and basilic veins, originate in the subcutaneous tissue on the
dorsum of the hand from the dorsal venous network (Fig. 6.12). Perforating veins form communications between the superficial and
deep veins. Like the dermatomal pattern, the logic for naming the main
superficial veins of the upper limb cephalic (toward the head) and
basilic (toward the base) becomes apparent when the limb is placed in
its initial embryonic position.
 |
|
Figure 6.12. Superficial veins and lymph nodes of upper limb. A.
The digital veins drain into the dorsal venous network on the dorsum of the hand, which leads to two prominent superficial vessels: the cephalic and basilic veins. B. The basilic and cephalic veins ultimately drain into the origin and termination of the axillary vein, respectively. The median cubital vein is the communication between the basilic and the cephalic veins in the cubital fossa. Perforating veins connect the superficial veins to the deep veins. Arrows indicate the flow of lymph within lymphatic vessels that converge toward the vein and drain into the cubital and axillary lymph nodes. |
head) ascends in the subcutaneous tissue from the lateral aspect of the
dorsal venous network, proceeding along the lateral border of the wrist
and the anterolateral surface of the proximal forearm and arm; it is
often visible through the skin. Anterior to the elbow, the cephalic
vein communicates with the median cubital vein,
which passes obliquely across the anterior aspect of the elbow in the
cubital fossa (a depression in front of the elbow) and joins the
basilic vein. The cephalic vein courses superiorly between the deltoid
and the pectoralis major muscles along the deltopectoral groove and
enters the clavipectoral triangle (Fig. 6.12B).
It then pierces the costocoracoid membrane, part of the clavipectoral
fascia, and joins the terminal part of the axillary vein.
the subcutaneous tissue from the medial end of the dorsal venous
network along the medial side of the forearm and the inferior part of
the arm; it is often visible through the skin. It then passes deeply
near the junction of the middle and inferior thirds of the arm,
piercing the brachial fascia and running superiorly parallel to the
brachial artery and the medial cutaneous nerve of the forearm to the
axilla, where it merges with the accompanying veins (L. venae comitantes) of the axillary artery to form the axillary vein.
begins at the base of the dorsum of the thumb, curves around the
lateral side of the wrist, and ascends in the middle of the anterior
aspect of the forearm between the cephalic and the basilic veins. The
median antebrachial vein sometimes divides into a median basilic vein,
which joins the basilic vein, and a median cephalic vein, which joins
the cephalic vein.
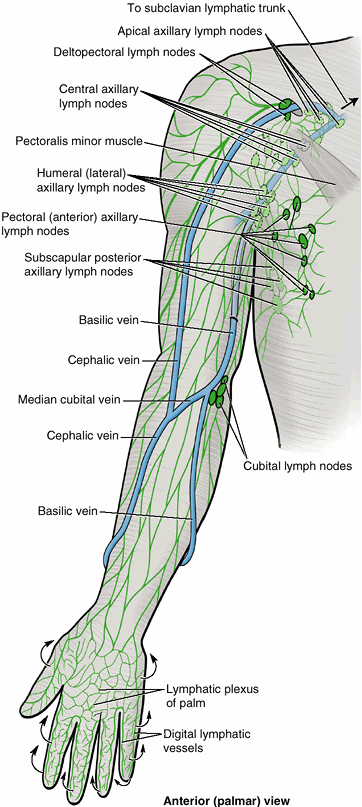
in the skin of the fingers, palm, and dorsum of the hand and ascend
mostly with the superficial veins, such as the cephalic and basilic
veins (Fig. 6.13). Some vessels accompanying the basilic vein enter the cubital (lymph) nodes,
located proximal to the medial epicondyle and medial to the basilic
vein. Efferent vessels from these lymph nodes ascend in the arm and
terminate in the humeral (lateral) axillary lymph nodes (see Chapter 1).
Most superficial lymphatic vessels accompanying the cephalic vein cross
the proximal part of the arm and the anterior aspect of the shoulder to
enter the apical axillary lymph nodes; however, some vessels previously enter the more superficial deltopectoral lymph nodes. Deep lymphatic vessels,
less numerous than superficial vessels, accompany the major deep veins
in the upper limb and terminate in the humeral axillary lymph nodes.
They drain lymph from the joint capsules, periosteum, tendons, nerves,
and muscles and ascend with the deep veins; a few deep lymph nodes may
occur along their
course.
The axillary lymph nodes are drained by the subclavian lymphatic trunk;
both are discussed in greater detail with the axilla, later in this
chapter.
 |
|
Figure 6.13. Lymphatic drainage of upper limb.
Superficial lymphatic vessels originate from the digital lymphatic vessels of the digits and lymphatic plexus of the palm; most drainage from the palm passes to the dorsum of the hand (arrows). The vessels ascend through the forearm and arm, converging toward the cephalic and especially the basilic veins. Some lymph following this superficial route passes through the cubital lymph nodes in the elbow region or deltopectoral nodes in the shoulder region. The superficial and deep lymphatics of the upper limb drain initially to the humeral (lateral) and apical axillary lymph nodes; axillary nodes are drained in turn by the subclavian lymphatic trunk. |
veins is easy to visualize when the limb is placed in its embryonic
position (abducted to 90° with the thumb directed superiorly). The
cephalic vein courses along the cranial (cephalic) margin of the limb,
while the basilic vein courses along the caudal (basic) margin of the
limb. Both veins come from the dorsal venous network on the dorsum of
the hand and drain into the beginning (basilic vein) and end (cephalic
vein) of the axillary vein.
and follow the superficial veins, whereas the deep lymphatics follow
the deep veins. The lymph collected from the upper limb by both
superficial and deep lymphatics drains into the axillary lymph nodes.
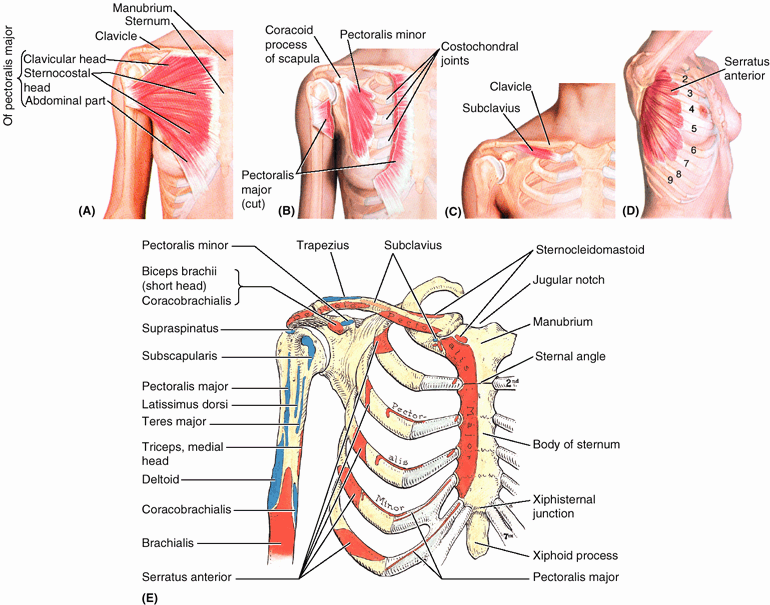
move the pectoral girdle: pectoralis major, pectoralis minor,
subclavius, and serratus anterior. The attachments, nerve supply, and
main actions of these muscles are illustrated in Figure 6.14 and summarized in Table 6.1.
The latter head is much larger and its lateral border forms the
muscular mass that makes up most of the anterior wall of the axilla.
Its inferior border forms the anterior axillary fold (see “Axilla,” later in this chapter). The pectoralis major and adjacent deltoid form the narrow deltopectoral groove, in which the cephalic vein runs (Fig. 6.12B); however, the muscles diverge slightly from each other superiorly and, along with the clavicle, form the clavipectoral (deltopectoral) triangle (Fig. 6.12).
arm when acting together, the two parts of the pectoralis major can
also act independently: the clavicular head flexing the humerus, and
the sternocostal head extending it back from the flexed position.
the arm is abducted 90°; the individual then moves the arm anteriorly
against resistance. If acting normally, the clavicular head can be seen
and palpated. To test the sternocostal head of the pectoralis major,
the arm is abducted 60° and then adducted against resistance. If acting
normally, the sternocostal head can be seen and palpated.
The pectoralis minor is triangular in shape: Its base (proximal
attachment) is formed by fleshy slips attached to the anterior ends of
the 3rd–5th ribs near their costal cartilages; its apex (distal
attachment) is on the coracoid process of the scapula. Variations in
the costal attachments of the muscle are common. The pectoralis minor
stabilizes the scapula and is used when stretching the upper limb
forward to touch an object that is just out of reach. The pectoralis
minor also assists in elevating the ribs for deep inspiration when the
pectoral girdle is fixed or elevated. The pectoralis minor is a useful
anatomical and surgical landmark for structures in the axilla (e.g.,
the axillary artery). With the coracoid process, the pectoralis minor
forms a “bridge” under which vessels and nerves must pass to the arm.
horizontally when the arm is in the anatomical position. This small,
round muscle is located inferior to the clavicle and affords some
protection to the subclavian vessels and the superior trunk of the
brachial plexus if the clavicle fractures. The subclavius anchors and
depresses the clavicle, stabilizing it during movements of the upper
limb. It also helps resist the tendency for the clavicle to dislocate
at the SC joint, for example, when pulling hard during a tug-of-war
game.
overlies the lateral part of the thorax and forms the medial wall of
the axilla. This broad sheet of thick muscle was named because of the
sawtoothed appearance of its fleshy slips or digitations (L. serratus,
a saw). The muscular slips pass posteriorly and then medially to attach
to the whole length of the anterior surface of the medial border of the
scapula, including its inferior angle.
muscles of the pectoral girdle. It is a strong protractor of the
scapula that is used when punching or reaching anteriorly (sometimes
called the “boxer’s muscle”). Its strong inferior part rotates the
scapula, elevating its glenoid cavity so the arm can be raised above
the shoulder. It also anchors the scapula, keeping it closely applied
to the thoracic wall, enabling other muscles to use it as a fixed bone
for movements of the humerus. The serratus anterior holds the scapula
against the thoracic wall when doing push-ups or when pushing against
resistance (e.g., pushing a car).
(or the function of the long thoracic nerve that supplies it), the hand
of the outstretched limb is pushed against a wall. If the muscle is
acting normally, several digitations of the muscle can be seen and
palpated.
sternocostal part, is uncommon, but when it occurs, no disability
usually results. However, the anterior axillary fold, formed by the
skin and fascia overlying the inferior border of the pectoralis major,
is absent on the affected side, and the nipple is more inferior than
usual. In Poland syndrome, both the pectoralis major and minor are absent; breast hypoplasia and absence of two to four rib segments are also seen.
 |
|
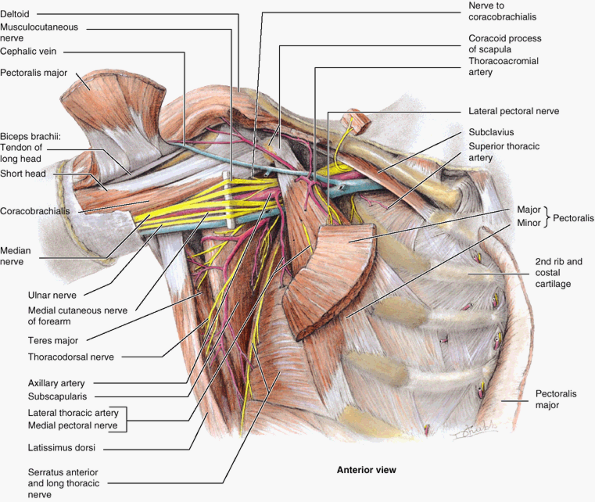
Figure 6.14. Muscular walls of the axilla.
Most of the anterior wall of the axilla and the axillary fat have been removed, revealing the axilla’s medial and posterior walls and neurovascular contents. Of the structures forming the anterior wall, only portions of the pectoralis major (attaching ends, a central part overlying the pectoralis minor, and a cube of muscle reflected superior to the clavicle), the pectoralis minor, and subclavius remain. All the clavipectoral fascia and axillary fat have been removed, as has the axillary sheath surrounding the neurovascular bundle. This enables observation of the medial wall of the axilla, formed by the serratus anterior overlying the lateral thoracic wall, and of the muscles forming the posterior wall. |
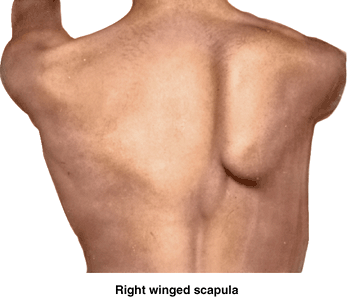
the medial border of the scapula moves laterally and posteriorly away
from the thoracic wall, giving the scapula the appearance of a wing,
especially when the person leans on a hand or presses the upper limb
against a wall. When the arm is raised, the medial border and inferior
angle of the scapula pull markedly away from the posterior thoracic
wall, a deformation known as a winged scapula (Fig. B6.5).
In addition, the upper limb cannot be abducted above the horizontal
position because the serratus anterior is unable to rotate the glenoid
cavity superiorly to allow complete abduction of the limb. Although
protected when the limbs are at one’s sides, the long thoracic nerve is
exceptional in that it courses on the superficial aspect of the
serratus anterior, which it supplies. Thus when the limbs are elevated,
as in a knife fight, the nerve is especially vulnerable. Weapons,
including bullets directed toward the thorax, are a common source
ofinjury.
 |
|
Figure B6.5
|
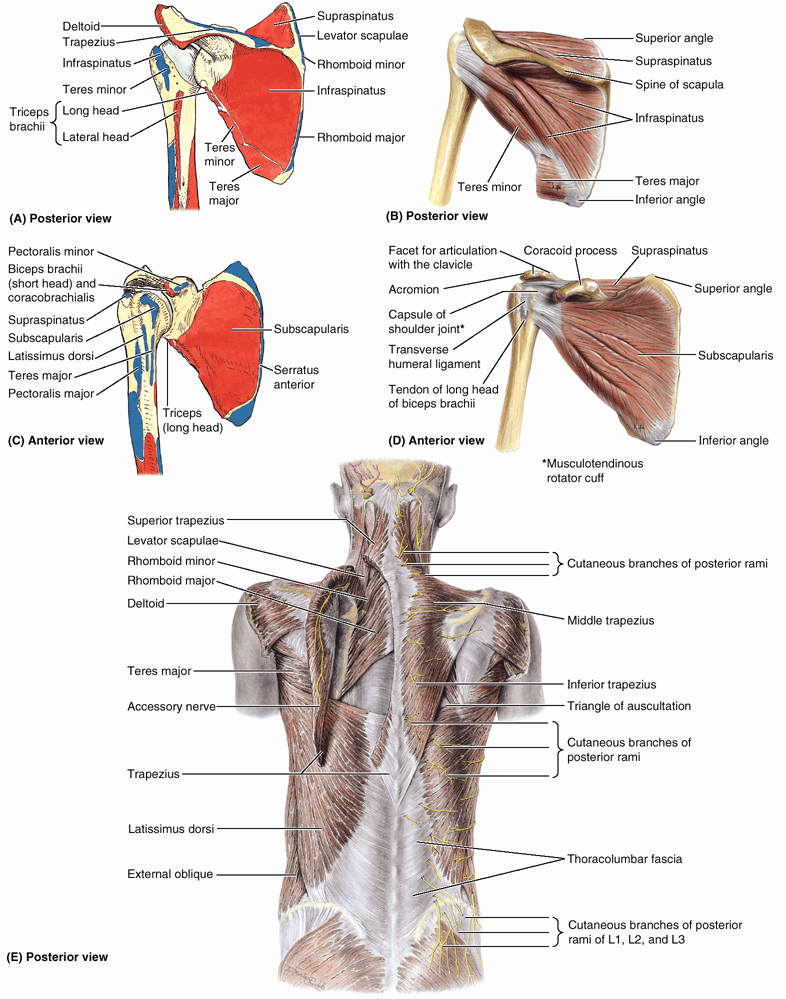
(superficial and intermediate groups of extrinsic back muscles) attach
the superior appendicular skeleton (of the upper limb) to the axial
skeleton (in the trunk). The intrinsic back muscles, which maintain posture and control movements of the vertebral column, are described in Chapter 4. The posterior shoulder muscles are divided into three groups (Table 6.2):
-
Superficial posterior axioappendicular (extrinsic shoulder) muscles: trapezius and latissimus dorsi.
-
Deep posterior axioappendicular (extrinsic shoulder) muscles: levator scapulae and rhomboids.
-
Scapulohumeral (intrinsic shoulder) muscles: deltoid, teres major, and the four rotator cuff muscles (supraspinatus, infraspinatus, teres minor, and subscapularis).
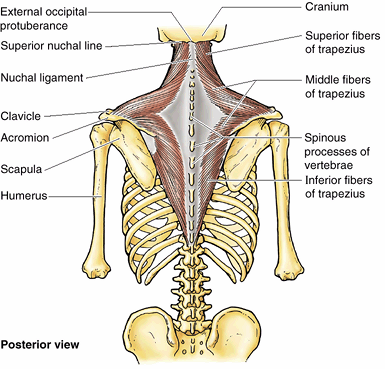
direct attachment of the pectoral girdle to the trunk. This large,
triangular muscle covers the posterior aspect of the neck and the
superior half of the trunk (Fig. 6.15). It was given its name because the muscles of the two sides form a trapezium
(G. irregular four-sided figure). The trapezius attaches the pectoral
girdle to the cranium and vertebral column and assists in suspending
the upper limb. The fibers of the trapezius are divided into three
parts, which have different actions at the physiological
scapulothoracic joint between the scapula and the thoracic wall (Table 6.3):
(1) superior fibers elevate the scapula (e.g., when squaring the
shoulders), (2) middle fibers retract the scapula (i.e., pull it
posteriorly), and (3) inferior fibers depress the scapula and lower the
shoulder.
rotating the scapula on the thoracic wall in different directions,
twisting it like a wing nut. The trapezius also braces the shoulders by
pulling the scapulae posteriorly and superiorly, fixing them in
position on the thoracic wall with tonic contraction; consequently,
weakness of this muscle causes drooping of the shoulders.
the function of the accessory nerve [CN XI] that supplies it), the
shoulder is shrugged against resistance (the person attempts to raise
the shoulders as the examiner presses down on them). If the muscle is
acting normally, the superior border of the muscle can be easily seen
and palpated.
 |
|
Figure 6.15. Trapezius.
This large, superficial, triangular muscle is responsible for the lateral slope between the neck and the shoulder. It assists in suspending the pectoral girdle and elevates, retracts, and rotates the scapula. |
|
Table 6.2. Posterior Axioappendicular and Scapulohumeral Muscles
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 |
|
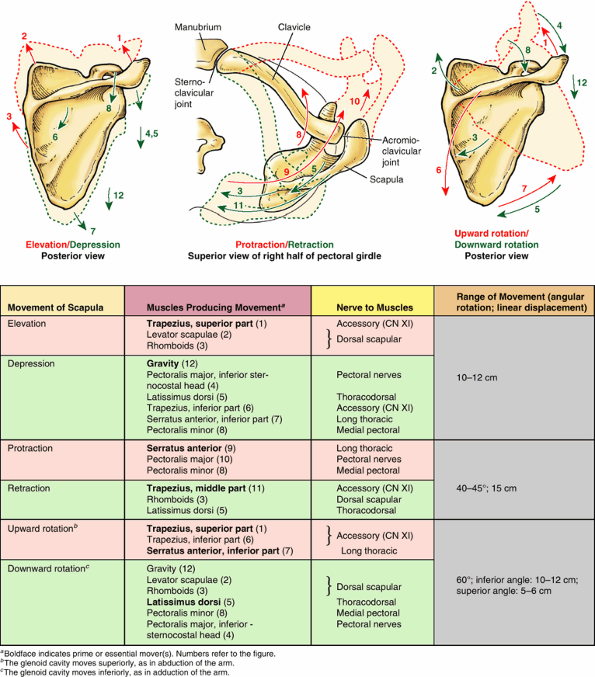
Table 6.3. Movements of the Scapula
|
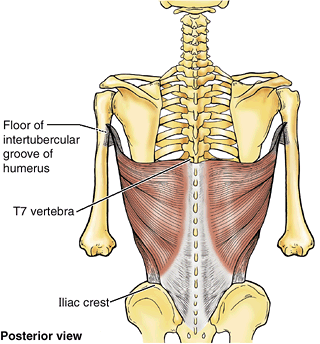
This large, fan-shaped muscle passes from the trunk to the humerus and
acts directly on the glenohumeral joint and indirectly on the pectoral
girdle (scapulothoracic joint). The latissimus dorsi extends, retracts,
and rotates the humerus medially (e.g., when folding the arms behind
the back or scratching the skin over the opposite scapula). In
combination with the pectoralis major, the latissimus dorsi is a
powerful adductor of the humerus, and plays a major role in downward
rotation of the scapula in association with this movement (Table 6.3).
It is also useful in restoring the upper limb from abduction superior
to the shoulder; hence the latissimus dorsi is important in climbing.
In conjunction with the pectoralis major, the latissimus dorsi raises
the trunk to the arm, which occurs when performing chin-ups (hoisting
oneself so the chin touches an overhead bar) or climbing a tree, for
example. These movements are also used when chopping wood, paddling a
canoe, and swimming (particularly during the crawl stroke).
(or the function of the thoracodorsal nerve that supplies it), the arm
is abducted 90° and then adducted against resistance provided by the
examiner. If the muscle is normal, the anterior border of the muscle
can be seen and easily palpated in the posterior axillary fold (see “Axilla,” later in this chapter).
 |
|
Figure 6.16. Latissimus dorsi.
This broad, triangular, mostly superficial muscle extends, adducts, and medially rotates the humerus. It is a powerful adductor and extensor of the arm and raises the body toward the arm during climbing. |
triangular gap in the musculature. The superior horizontal border of
the latissimus dorsi, the medial border of the scapula, and the
inferolateral border of the trapezius form a triangle of auscultation (Table 6.2E).
This gap in the thick back musculature is a good place to examine
posterior segments of the lungs with a stethoscope. When the scapulae
are drawn anteriorly by folding the arms across the chest and the trunk
is flexed, the auscultatory triangle enlarges and parts of the 6th and
7th ribs and 6th intercostal space are subcutaneous.
is a marked ipsilateral weakness when the shoulders are elevated
(shrugged) against resistance. Injury of the accessory nerve is
discussed in greater detail in Chapters 8 and 9.
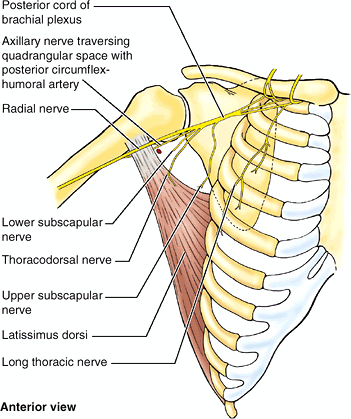
thoracodorsal nerve (C6–C8) supplying the latissimus dorsi at risk of
injury. This nerve passes inferiorly along the posterior wall of the
axilla and enters the medial surface of the latissimus dorsi close to
where it becomes tendinous (Fig. B6.6). The
nerve is also vulnerable to injury during surgery on scapular lymph
nodes because its terminal part lies anterior to them and the
subscapular artery (Fig. B6.7). The latissimus
dorsi and the inferior part of the pectoralis major form an
anteroposterior muscular sling between the trunk and the arm; however,
the latissimus dorsi forms the more powerful part of the sling. With
paralysis of the latissimus dorsi, the person is unable to raise the
trunk with the upper limbs, as occurs during climbing. Furthermore, the
person cannot use an axillary crutch because the shoulder is pushed
superiorly by it. These are the primary activities for which active
depression of the scapula is required; the passive depression provided
by gravity is adequate for most activities.
 |
|
Figure B6.6
|
 |
|
Figure B6.7
|
are the levator scapulae and rhomboids. These muscles provide direct
attachment of the appendicular skeleton to the axial skeleton. The
attachments, nerve supply, and main actions are given in Table 6.2.
lies deep to the sternocleidomastoid; the inferior third is deep to the
trapezius. From the transverse processes of the upper cervical
vertebrae, the fibers of the levator of the scapula pass inferiorly to
the superomedial border of the scapula (Fig. 6.17).
True to its name, the levator scapulae acts with the descending part of
the trapezius to elevate the scapula, or fix it (resists forces that
would
depress
it, as when carrying a load). With the rhomboids and pectoralis minor,
it rotates the scapula, depressing the glenoid cavity (tilting it
inferiorly by rotating the scapula) (Table 6.3).
Acting bilaterally (also with the trapezius), the levators extend the
neck; acting unilaterally, the muscle may contribute to lateral flexion
of the neck (toward the side of the active muscle).
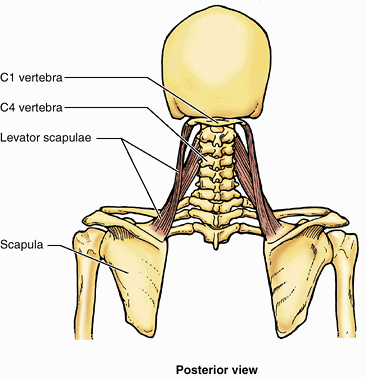 |
|
Figure 6.17. Levator scapulae.
This thick, strap-like muscle descends from the first four cervical vertebrae and attaches to the medial border of the superior angle of the scapula. It elevates and rotates the scapula, tilting the glenoid cavity inferiorly. |
which are not always clearly separated from each other, have a rhomboid
appearance—that is, they form an oblique equilateral parallelogram (Fig. 6.18).
The rhomboids lie deep to the trapezius and form broad parallel bands
that pass inferolaterally from the vertebrae to the medial border of
the scapula. The thin, flat rhomboid major is approximately two times
wider than the thicker rhomboid minor lying superior to it. The
rhomboids retract and rotate the scapula, depressing its glenoid cavity
(Table 6.3). They also assist the serratus
anterior in holding the scapula against the thoracic wall and fixing
the scapula during movements of the upper limb. The rhomboids are used
when forcibly lowering the raised upper limbs (e.g., when driving a
stake with a sledge hammer).
the function of the dorsal scapular nerve that supplies them), the
individual places the hands posteriorly on the hips and pushes the
elbows posteriorly against resistance provided by the examiner. If the
rhomboids are acting normally, they can be palpated along the medial
borders of the scapulae; because they lie deep to the trapezius, they
are unlikely to be visible during testing.
rhomboids, affects the actions of these muscles. If the rhomboids on
one side are paralyzed, the scapula on the affected side is located
farther from the midline than that on the normal side.
proximal upper limb are axioappendicular or scapulothoracic muscles.
The former consist of anterior, superficial posterior, and deep
posterior groups. As a group, the axioappendicular muscles serve to
position the base from which the upper limb will be extended and
function relative to the trunk. The muscles work in antagonistic groups
to elevate–depress and protract–retract the entire scapula or rotate it
to elevate or depress the glenoid cavity and the glenohumeral joint (Table. 6.3).
These movements extend the functional range of movements that occur at
the glenohumeral joint. All of these movements involve both the
clavicle and the scapula; the limits to all movements of the latter are
imposed by the former, which provides the only attachment to the axial
skeleton. Most of these movements involve the cooperation of a number
of muscles with different innervations. Therefore, single nerve
injuries typically weaken but do not eliminate most movements. Notable
exceptions are upward rotation of the lateral angle of the scapula
(superior trapezius/accessory nerve only) and lateral rotation of the
inferior angle of the scapula (inferior serratus anterior/long thoracic
nerve only).
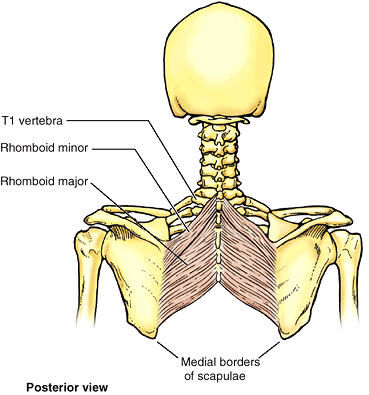 |
|
Figure 6.18. Rhomboids.
The rhomboid muscles (major and minor) retract the scapula and rotate it to depress the glenoid cavity. They also fix the scapula to the thoracic wall. |
(the deltoid, teres major, supraspinatus, infraspinatus, subscapularis,
and teres minor) are relatively short muscles that pass from the
scapula to the humerus and act on the glenohumeral joint. The
attachments, nerve supply, and main actions of these intrinsic shoulder
muscles are summarized in Table 6.2.
As its name indicates, the deltoid is shaped like the inverted Greek
letter delta (Δ). The muscle is divided into unipennate anterior and
posterior parts and a multipennate middle part; the parts of the
deltoid can act separately or as a whole. When all three parts contract
simultaneously, the arm is abducted. The anterior and posterior parts
act like guy ropes to steady the arm as it is abducted. To initiate
movement during the first 15° of abduction, the deltoid is assisted by
the supraspinatus (Table 6.2B).
When the arm is fully adducted, the line of pull of the deltoid
coincides with the axis of the humerus; thus it pulls directly upward
on the bone and cannot initiate or produce abduction. It is, however,
able to act as a shunt muscle, resisting inferior displacement of the
head of the humerus from the glenoid cavity, as when lifting and
carrying suitcases. From the fully adducted position, abduction must be
initiated by the supraspinatus, or by leaning to the side, allowing
gravity to initiate the movement. The deltoid becomes fully effective
as an abductor following the initial 15° of abduction.
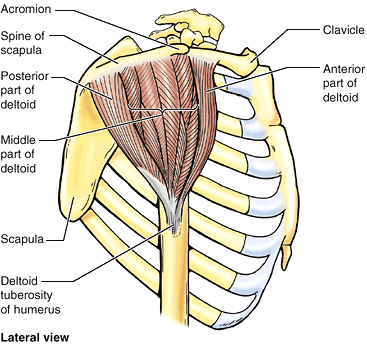 |
|
Figure 6.19. Deltoid.
This thick, coarse-textured, triangular muscle covers the glenohumeral joint and forms the rounded contour of the shoulder. The middle, multipennate part of the deltoid is the principal abductor of the arm, the anterior part flexes and medially rotates the arm, and the posterior part extends and laterally rotates the arm. |
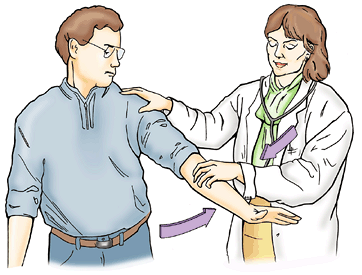 |
|
Figure 6.20. Testing deltoid muscle.
The examiner resists the patient’s abduction of the limb by the deltoid. If the deltoid is acting normally, contraction of the middle part of the muscle can be palpated. |
used to swing the limbs during walking. The anterior part assists the
pectoralis major in flexing the arm, and the posterior part assists the
latissimus dorsi in extending the arm. The deltoid also helps stabilize
the glenohumeral joint and hold the head of the humerus in the glenoid
cavity during movements of the upper limb.
function of the axillary nerve that supplies it), the arm is abducted,
starting from approximately 15°, against resistance (Fig. 6.20).
If acting normally, the deltoid can easily be seen and palpated. The
influence of gravity is avoided when the person is supine.
C6) is severely damaged. Because it passes inferior to the humeral head
and winds around the surgical neck of the humerus, the axillary nerve
is usually injured during fracture of this part of the humerus. It may
also be damaged during dislocation of the glenohumeral joint and by
compression from the incorrect use of crutches. As the deltoid
atrophies, the rounded contour of the shoulder disappears. This gives
the shoulder a flattened appearance and produces a slight hollow
inferior to the acromion. In addition to atrophy of the deltoid, a loss
of sensation may occur over the lateral side of the proximal part of
the arm, the area supplied by the superior lateral cutaneous nerve of the arm (red in Fig. B6.8).
injection of drugs. The axillary nerve runs transversely under cover of
the deltoid at the level of the surgical neck of the humerus. Awareness
of its location avoids injury to it during surgical approaches to the
shoulder.
 |
|
Figure B6.8. Area of anesthesia (red).
|
round) is a thick, rounded muscle that forms a raised oval area on the
inferolateral third of the scapula when the arm is adducted against
resistance (Fig. 6.21A; Table 6.2B & E).
The inferior border of the teres major forms the inferior border of the
lateral part of the posterior wall of the axilla. The teres major
adducts and medially rotates the arm (Fig. 6.21B).
It can also help extend it from the flexed position and is an important
stabilizer of the humeral head in the glenoid cavity—that is, it
steadies the head in its socket.
the lower subscapular nerve that supplies it), the abducted arm is
adducted against resistance. If acting normally, the muscle can be
easily seen and palpated in the posterior axillary fold.
All except the supraspinatus are rotators of the humerus; the
supraspinatus, besides being part of the rotator cuff, initiates and
assists the deltoid in the first 15° of abduction of the arm. The
tendons of the SITS muscles blend with and reinforce the fibrous layer
of the joint capsule of the glenohumeral joint, thus forming the
rotator cuff that protects the joint and gives it stability. The tonic
contraction of the contributing muscles holds the relatively large head
of the humerus in the small, shallow glenoid cavity of the scapula
during arm movements. The attachments, nerve supply, and main actions
of the rotator cuff muscles are given in Table 6.2.
abduction of the arm is attempted from the fully adducted position
against resistance, while the muscle is palpated superior to the spine
of the scapula.
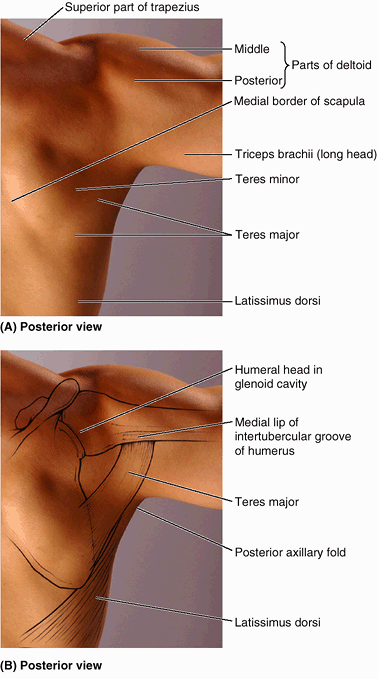 |
|
Figure 6.21. Scapulohumeral muscles. A.
These muscles pass from the scapula to the humerus and act on the glenohumeral joint. The surface anatomy of the scapular muscles and the latissimus dorsi are shown. B. The position of the scapula and humerus when the limb is abducted 90° is shown. The teres major is a thick, rounded muscle that adducts and medially rotates the arm. The latissimus dorsi and teres major form the posterior axillary fold. When the arm is adducted against resistance, this fold is accentuated. |
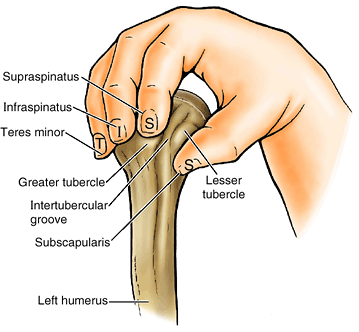 |
|
Figure 6.22. Disposition of rotator cuff muscles.
The primary combined function of the four scapulohumeral (SITS) muscles is to “grasp” and pull the relatively large head of the humerus medially, holding it against the smaller, shallow glenoid cavity of the scapula. The tendons of the muscles (represented by three fingers and the thumb) blend with the fibrous layer of the capsule of the glenohumeral joint to form a musculotendinous rotator cuff, which reinforces the capsule on three sides (anteriorly, superiorly, and posteriorly) as it provides active support for the glenohumeral joint. |
the medial three quarters of the infraspinous fossa and is partly
covered by the deltoid and trapezius. In addition to helping stabilize
the glenohumeral joint, the infraspinatus is a powerful lateral rotator
of the humerus.
the person flexes the elbow and adducts the arm. The arm is then
laterally rotated against resistance. If acting normally, the muscle
can be palpated inferior to the scapular spine. To test the function of the supra-scapular nerve, which supplies the supraspinatus and infraspinatus, both muscles must be tested as described.
elongate muscle that is completely hidden by the deltoid and is often
not clearly delineated from the infraspinatus (Table 6.2B).
The teres minor works with the infraspinatus to rotate the arm
laterally and assist in its adduction. The teres minor is most clearly
distinguished from the infraspinatus by its nerve supply. The teres
minor is supplied by the axillary nerve, whereas the infraspinatus is
supplied by the suprascapular nerve.
thick, triangular muscle that lies on the costal surface of the scapula
and forms part of the posterior wall of the axilla. It crosses the
anterior aspect of the scapulohumeral joint on its way to the humerus.
The subscapularis is the primary medial rotator of the arm and also
adducts it. It joins the other rotator cuff muscles in holding the head
of the humerus in the glenoid cavity during all movements of the
glenohumeral joint (i.e., it helps stabilize this joint during
movements of the elbow, wrist, and hand).
child or adolescent may produce a fracture–dislocation of the proximal
humeral epiphysis because the joint capsule of the glenohumeral joint,
reinforced by the rotator cuff (tendons of the SITS muscles), is
stronger than the epiphysial plate. In severe fractures, the shaft of
the humerus is markedly displaced, but the humeral head retains its
normal relationship with the glenoid cavity of the scapula (Fig. B6.9).
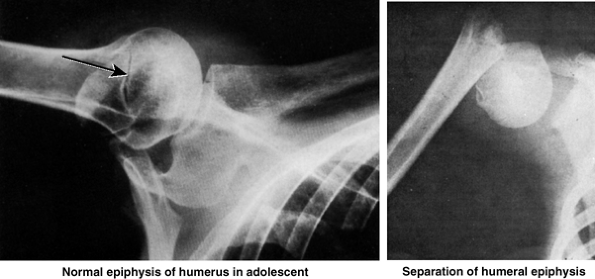 |
|
Figure B6.9
|
rotator cuff, producing instability of the glenohumeral joint. Trauma
may tear or rupture one or more of the tendons of the SITS muscles;
that of the supraspinatus is most commonly involved (Fig. B6.10). Degenerative tendonitis of the rotator cuff
is common, especially in older people. These syndromes are discussed in
detail (later in this chapter) in relationship to the glenohumeral
joint.
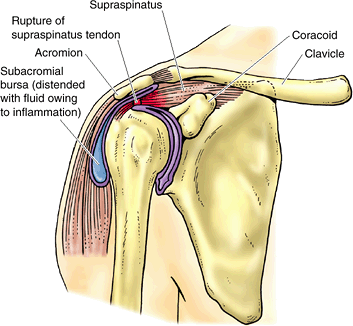 |
|
Figure B6.10
|
SITS muscles), along with certain axioappendicular muscles, act in
opposing groups to position the proximal strut (humerus) of the upper
limb, producing abduction–adduction, flexion–extension, medial–lateral
rotation, and circumduction of the arm. This establishes the height,
distance from the trunk, and direction from which the forearm and hand
will operate. Essentially all movements produced by the scapulohumeral
muscles at the glenohumeral joint are accompanied by movements produced
by axioappendicular muscles at the sternoclavicular and scapulothoracic
joints, especially beyond the initial stages of the movement. A skilled
examiner, knowledgeable in anatomy, can manually fix or position the
limb to isolate and test distinctive portions of specific upper limb
movements. The SITS muscles contribute to the formation of the rotator
cuff, which both rotates the humeral head and holds it firmly against
the shallow socket of the glenoid cavity, increasing the integrity of
the glenohumeral joint capsule.
space inferior to the glenohumeral joint and superior to the axillary
fascia at the junction of the arm and thorax (Fig. 6.23).
The axilla provides a passageway or “distribution center,” usually
protected by the adducted upper limb, for the neurovascular structures
that serve the upper limb. From this distribution center, neurovascular
structures pass (1) superiorly via the cervicoaxillary canal to (or
from) the root of the neck, (2) anteriorly via the clavipectoral
triangle to the pectoral region, (3) inferiorly and laterally into the
limb itself, (4) posteriorly via the quadrangular space to the scapular
region, and (5) inferiorly and medially along the thoracic wall to the
inferiorly placed axioappendicular muscles (serratus anterior and
latissimus dorsi). The shape and size of the axilla varies, depending
on the position of the arm; it almost disappears when the arm is fully
abducted—a position in which its contents are vulnerable. A “tickle”
reflex causes most people to rapidly resume the protected position when
invasion threatens.
-
The apex of axilla is the cervicoaxillary canal,
the passageway between the neck and the axilla, bounded by the 1st rib,
clavicle, and superior edge of the scapula. The arteries, veins,
lymphatics, and nerves traverse this superior opening of the axilla to
pass to or from the arm (Fig. 6.23A). -
The base of axilla
is formed by the concave skin, subcutaneous tissue, and axillary (deep)
fascia extending from the arm to the thoracic wall (approximately the
4th rib level), forming the axillary fossa
(armpit). The base of the axilla or axillary fossa is bounded by the
anterior and posterior axillary folds, the thoracic wall, and the
medial aspect of the arm (Fig. 6.23C). -
The anterior wall of axilla
has two layers, formed by the pectoralis major and pectoralis minor and
the pectoral and clavicopectoral fascia associated with them (Figs. 6.9B and 6.23B & C). The anterior axillary fold
is the inferiormost part of the anterior wall that may be grasped
between the fingers; it is formed by the pectoralis major, as it
bridges from thoracic wall to humerus, and the overlying integument (Fig. 6.23C & D). -
The posterior wall of axilla
is formed chiefly by the scapula and subscapularis on its anterior
surface and inferiorly by the teres major and latissimus dorsi (Fig. 6.23B & C). The posterior axillary fold
is the inferiormost part of the posterior wall that may be grasped. It
extends farther inferiorly than the anterior wall and is formed by
latissimus dorsi, teres major, and overlying integument.P.764![]() Figure 6.23. Location, boundaries, and contents of axilla. A.
Figure 6.23. Location, boundaries, and contents of axilla. A.
The axilla is a pyramidal space inferior to the glenohumeral joint and
superior to the skin of the axillary fossa at the junction of the arm
and thorax. Observe its apex, base, and walls. B.
This transverse section of the axilla illustrates its three muscular
walls. The small, lateral bony wall of the axilla is the
intertubercular groove of the humerus. C.
A sagittal section of the shoulder shows the contents of the axilla and
the scapular and pectoral muscles forming its posterior and anterior
walls, respectively. The axilla is primarily filled with axillary fat (yellow),
forming a matrix in which the neurovascular structures and lymph nodes
are embedded. Inferiorly, the inferior border of the pectoralis major
forms the anterior axillary fold, and the latissimus dorsi and teres
major form the posterior axillary fold. D.
In this superficial dissection of the pectoral region, the subcutaneous
platysma muscle, which descends from the neck to the 2nd or 3rd rib, is
cut short on the right side. The severed muscle is reflected superiorly
on the left side, together with the supraclavicular nerves, so that the
clavicular attachments of the pectoralis major and anterior deltoid can
be observed.P.765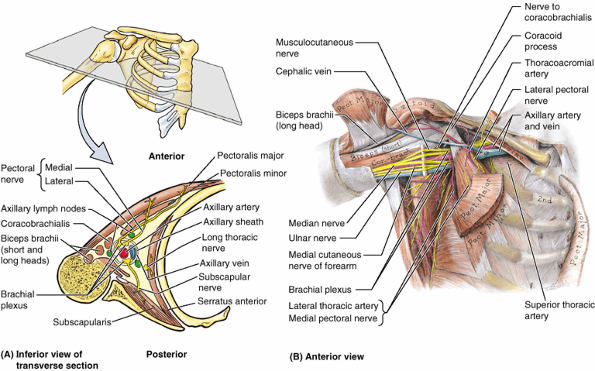 Figure 6.24. Contents of axilla. A.
Figure 6.24. Contents of axilla. A.
This cross section of the axilla demonstrates the contents of the
axilla, including the axillary sheath enclosing the axillary artery and
vein and the three cords of the brachial plexus. The innervation of the
muscular walls of the axilla is also shown. B.
In this dissection, most of the pectoralis major has been removed and
the clavipectoral fascia, axillary fat, and axillary sheath have been
completely removed. The brachial plexus of nerves surrounds the
axillary artery on its lateral and medial aspects (appearing here to be
its superior and inferior aspects because the limb is abducted) and on
its posterior aspect (not visible from this view). -
The medial wall of axilla is formed by the thoracic wall (1st–4th ribs and intercostal muscles) and the overlying serratus anterior (Fig. 6.23A & B).
-
The lateral wall of axilla is a narrow bony wall formed by the intertubercular groove in the humerus.
artery and its branches, axillary vein and its tributaries), lymphatic
vessels, and several groups of axillary lymph nodes, all embedded in a matrix of axillary fat (Fig. 6.23C). The axilla also contains large nerves that make up the cords and branches of the brachial plexus,
a network of interjoining nerves that pass from the neck to the upper
limb. Proximally, these neurovascular structures are ensheathed in a
sleeve-like extension of the cervical fascia, the axillary sheath (Fig. 6.24A).
compartment (distribution center) giving passage to or housing the
major “utilities” serving (supplying, draining, and communicating with)
the upper limb. Although normally protected by the arm, axillary
structures are vulnerable when the arm is abducted. The “tickle” reflex
causes us to recover the protected position rapidly when a threat is
perceived. The structures are ensheathed in a protective wrapping
(axillary sheath), embedded in a cushioning matrix (axillary fat) that
allows flexibility, and are surrounded by musculoskeletal walls. From
the axilla, neurovascular structures pass to and from the entire upper
limb, including the pectoral, scapular, and subscapular regions as well
as the free upper limb.
at the lateral border of the 1st rib as the continuation of the
subclavian artery and ends at the inferior border of the teres major (Table 6.4).
It passes posterior to the pectoralis minor into the arm and becomes
the brachial artery when it passes the inferior border of the teres
major, at which point it usually has reached the humerus. For
descriptive purposes, the axillary artery is divided into three parts
by the pectoralis minor (the part number also indicates the number of
its branches):
-
The first part of the axillary artery is located between the lateral border of the 1st rib and the medial border of the pectoralis minor; it is enclosed in the axillary sheath and has one branch—the superior thoracic artery (Fig. 6.24B; Table 6.4).
-
The second part of the axillary artery
lies posterior to pectoralis minor and has two branches—the
thoracoacromial and lateral thoracic arteries—which pass medial and
lateral to the muscle, respectively. -
The third part of the axillary artery
extends from the lateral border of pectoralis minor to the inferior
border of teres major and has three branches. The subscapular artery is
the largest branch of the axillary artery. Opposite the origin of this
artery, the anterior circumflex humeral and posterior circumflex
humeral arteries arise, sometimes by means of a common trunk.
is a small, highly variable vessel that arises just inferior to the
subclavius. It commonly runs inferomedially posterior to the axillary
vein and supplies the subclavius, muscles in the 1st and 2nd
intercostal spaces, superior slips of the serratus anterior, and
overlying pectoral muscles. It anastomoses with the intercostal and/or
internal thoracic arteries.
a short wide trunk, pierces the costocoracoid membrane and divides into
four branches (acromial, deltoid, pectoral, and clavicular), deep to
the clavicular head of the pectoralis major (Fig. 6.25).
has a variable origin. It usually arises as the second branch of the
second part of the axillary artery and descends along the lateral
border of the pectoralis minor, following it onto the thoracic wall (Fig. 6.24B);
however, it may arise instead from the thoracoacromial, suprascapular,
or subscapular arteries. The lateral thoracic artery supplies the
pectoral, serratus anterior, and intercostal muscles, the axillary
lymph nodes, and the lateral aspect of the breast.
branch of the axillary artery with the greatest diameter but shortest
length descends along the lateral border of the subscapularis on the
posterior axillary wall. It soon terminates by dividing into the
circumflex scapular and thoracodorsal arteries.
often the larger terminal branch of the subscapular artery, curves
posteriorly around the lateral border of the scapula, passing
posteriorly between the subscapularis and the teres major to supply
muscles on the dorsum of the scapula. It participates in the
anastomoses around the scapula.
continues the general course of the subscapular artery to the inferior
angle of the scapula and supplies adjacent muscles, principally the
latissimus dorsi. It also participates in the arterial anastomoses
around the scapula.
passes laterally, deep to the coracobrachialis and biceps brachii. It
gives off an ascending branch that supplies the shoulder. The larger posterior circumflex humeral artery passes medially through the posterior wall of the axilla via the quadrangular space
with the axillary nerve to supply the glenohumeral joint and
surrounding muscles (e.g., the deltoid, teres major and minor, and long
head of the triceps) (Table 6.4).
of the lateral wall of the axilla. Compression of the third part of
this artery against the humerus may be necessary when profuse bleeding
occurs (e.g., resulting from a stab or bullet wound in the axilla). If
compression is required at a more proximal site, the axillary artery
can be compressed at its origin (as the subclavian artery crosses the
1st rib) by exerting downward pressure in the angle between the
clavicle and the inferior attachment of the sternocleidomastoid.
arteries) occur around the scapula. Several vessels join to form
networks on the anterior and posterior surfaces of the scapula: the
dorsal scapular, suprascapular, and (via the circumflex scapular)
subscapular arteries (Fig. B6.11). The importance of the collateral circulation
made possible by these anastomoses becomes apparent when ligation of a
lacerated subclavian or axillary artery is necessary. For example, the
axillary artery may have to be ligated between the 1st rib and
subscapular artery; in other cases, vascular stenosis
(narrowing) of the axillary artery may result from an atherosclerotic
lesion that causes reduced blood flow. In either case, the direction of
blood flow in the subscapular artery is reversed, enabling blood to
reach the third part of the axillary artery. Note that the subscapular
artery receives blood through several anastomoses with the
suprascapular artery, transverse cervical artery, and intercostal
arteries.
Sudden occlusion usually does not allow sufficient time for adequate
collateral circulation to develop; as a result, there is an inadequate
supply of blood to the arm, forearm, and hand. While potential
collateral pathways (periarticular anastomoses) exist around the
shoulder joint proximally and the elbow joint distally, surgical ligation of the axillary artery
between the origins of the subscapular artery and the deep artery of
the arm will cut off the blood supply to the arm because the collateral
circulation is inadequate.
and compress the trunks of the brachial plexus, causing pain and
anesthesia (loss of sensation) in the areas of the skin supplied by the
affected nerves. Aneurysm of the axillary artery may occur in baseball
pitchers because of their rapid and forceful arm movements.
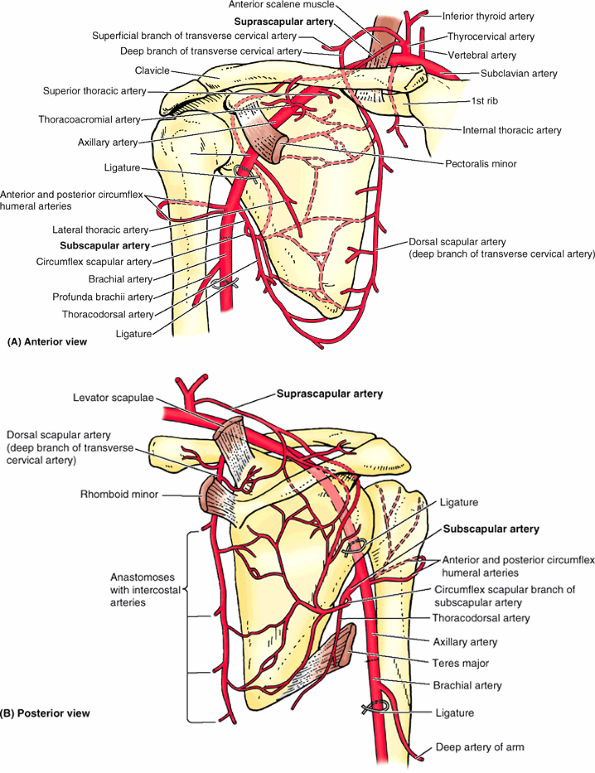 |
|
Figure B6.11
|
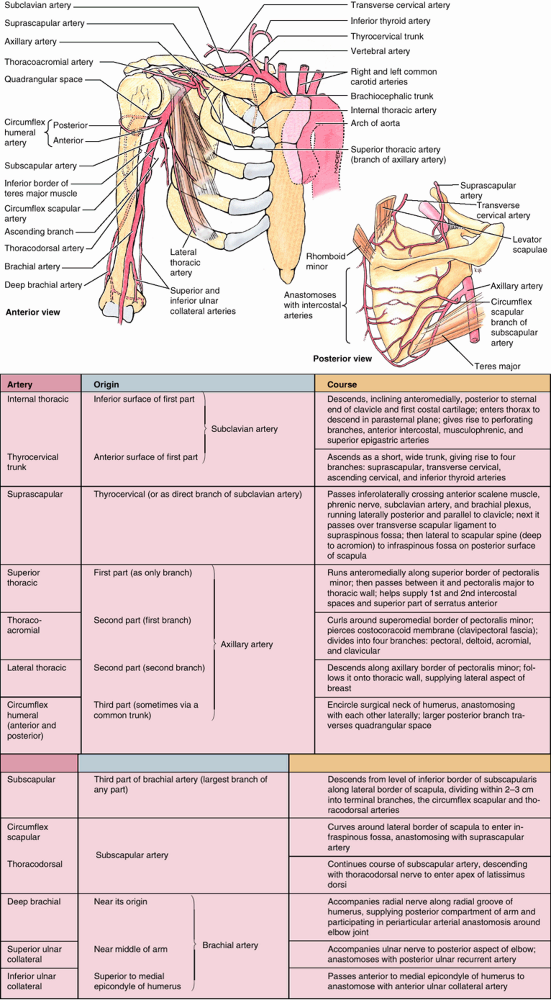 |
|
Table 6.4. Arteries of the Proximal Upper Limb (Shoulder Region and Arm)
|
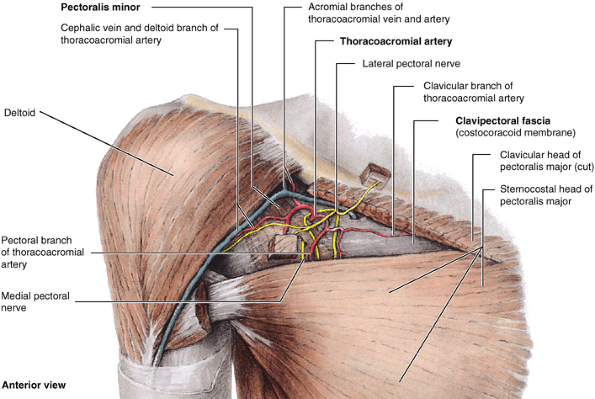 |
|
Figure 6.25. Anterior wall of axilla.
The clavicular head of the pectoralis major is excised except for its clavicular and humeral attaching ends and two cubes, which remain to identify its nerves. The anterior wall of the axilla is formed by the pectoralis major and minor (and the pectoral and clavipectoral fascia that envelops them). The pectoralis major covers the whole of this wall and forms the anterior axillary fold. Extending between the superior border of the pectoralis minor and the clavicle is the costocoracoid membrane (part of the clavipectoral fascia), which is perforated by the thoracoacromial artery and pectoral nerves (both exiting the axilla) and the cephalic vein (entering the axilla). |
initially (distally) on the anteromedial side of the axillary artery,
with its terminal part anteroinferior to the artery (Fig. 6.26). This large vein is formed by the union of the brachial vein (the accompanying veins of the brachial artery) and the basilic vein
at the inferior border of the teres major. The axillary vein is
described as having three parts that correspond to the three parts of
the axillary artery. Thus the initial, distal end is the third part,
whereas the terminal, proximal end is the first part. The axillary vein
(first part) ends at the lateral border of the 1st rib, where it
becomes the subclavian vein. The veins of
the axilla are more abundant than the arteries, are highly variable,
and frequently anastomose. The axillary vein receives tributaries that
generally correspond to branches of the axillary artery with a few
major exceptions:
-
The veins corresponding to the branches
of the thoracoacromial artery do not merge to enter by a common
tributary; some enter independently into the axillary vein, but others
empty into the cephalic vein, which then enters the axillary vein
superior to the pectoralis minor, close to its transition into the
subclavian vein. -
The axillary vein receives, directly or indirectly, the thoracoepigastric vein(s),
which is(are) formed by the anastomoses of superficial veins from the
inguinal region with tributaries of the axillary vein (usually the
lateral thoracic vein). These veins constitute a collateral route that
enables venous return in the presence of obstruction of the inferior
vena cava (see clinical correlation [blue] box “Collateral Routes for Abdominopelvic Venous Blood,” in Chapter 2).
because of its large size and exposed position. When the arm is fully
abducted, the axillary vein overlaps the axillary artery anteriorly. A
wound in the proximal part of the axillary vein is particularly
dangerous, not only because of profuse bleeding but also because of the
risk of air entering it and producing air emboli (air bubbles) in the blood.
The axillary vein becomes the subclavian vein as the first rib is
crossed. Because the needle is advanced medially to enter the vein as
it crosses the rib, the vein actually punctured (the point of entry) in
a “subclavian vein puncture” is the terminal part of the axillary vein.
However, the needle tip proceeds into the lumen of the subclavian vein
almost immediately. Thus it is clinically significant that the axillary
vein lies anterior and inferior (i.e., superficial) to the axillary
artery and the parts of the brachial plexus that begin to surround the
artery at this point.
fat) contains many lymph nodes. The axillary lymph nodes are arranged
in five principal groups: pectoral, subscapular, humeral, central, and
apical. The groups are arranged in a manner that reflects the pyramidal
shape of the axilla (Fig. 6.23A). Three groups of axillary nodes are related to the triangular base, one group at each corner of the pyramid (Fig. 6.27A & B):
consist of three to five nodes that lie along the medial wall of the
axilla, around the lateral thoracic vein and the inferior border of the
pectoralis minor. The pectoral nodes receive lymph mainly from the
anterior thoracic wall, including most of the breast (especially the
superolateral [upper outer] quadrant and subareolar plexus; see Chapter 1).
blood vessels. These nodes receive lymph from the posterior aspect of the thoracic wall and scapular region.
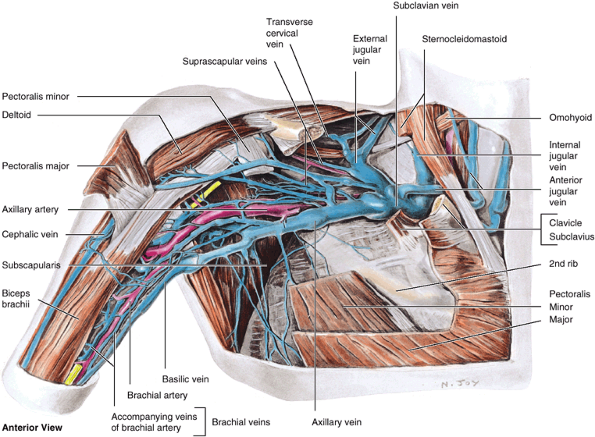 |
|
Figure 6.26. Veins of axilla. Observe that the basilic vein parallels the brachial artery to the axilla, where it merges with the accompanying veins (L. venae comitantes)
of the axillary artery to form the axillary vein. Note the large number of highly variable veins in the axilla, which are also tributaries of the axillary vein. |
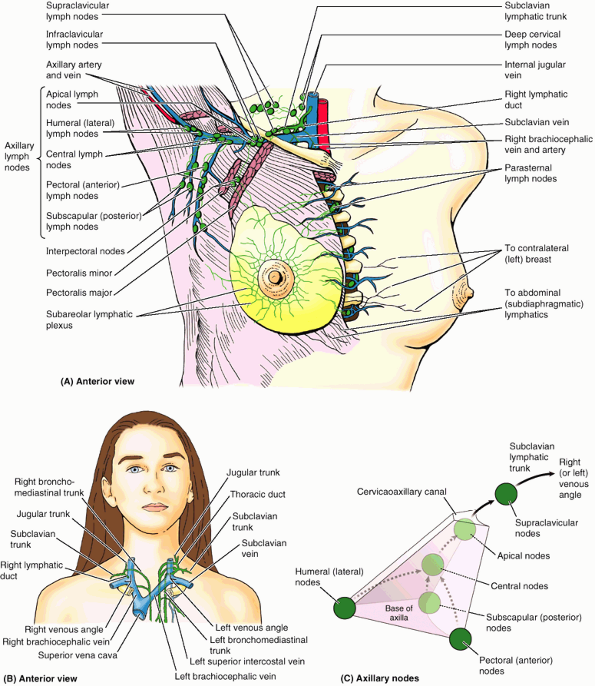 |
|
Figure 6.27. Axillary lymph nodes and lymphatic drainage of right upper limb and breast. A.
Of the five groups of axillary lymph nodes, most lymphatic vessels from the upper limb terminate in the humeral (lateral) and central lymph nodes, but those accompanying the upper part of the cephalic vein terminate in the apical lymph nodes. The lymphatics of the breast are discussed in Chapter 1. B. Lymph passing through the axillary nodes enters efferent lymphatic vessels that form the subclavian lymphatic trunk, which usually empties into the junctions of the internal jugular and subclavian veins (the venous angles). Occasionally, on the right side, this trunk merges with the jugular lymphatic and/or bronchomediastinal trunks to form a short right lymphatic duct; usually on the left side, it enters the termination of the thoracic duct. C. The positions of the five groups of axillary nodes, relative to each other and the pyramidal axilla. The typical pattern of drainage is shown. |
consist of four to six nodes that lie along the lateral wall of the
axilla, medial and posterior to the axillary vein. These nodes receive
nearly all the lymph from the upper limb, except that carried by the
lymphatic vessels accompanying the cephalic vein, which primarily drain
directly to the apical axillary and infraclavicular nodes.
The central nodes are three or four large nodes situated deep to the
pectoralis minor near the base of the axilla, in association with the
second part of the axillary artery. Efferent vessels from the central
nodes pass to the apical nodes. The apical
nodes are located at the apex of the axilla along the medial side of
the axillary vein and the first part of the axillary artery. The apical
nodes receive lymph from all other groups of axillary lymph nodes as
well as from lymphatics accompanying the proximal cephalic vein.
Efferent vessels from the apical group of nodes traverse the cervicoaxillary canal. These efferent vessels ultimately unite to form the subclavian lymphatic trunk, although some vessels may drain en route through the clavicular (infraclavicular and supraclavicular) nodes. Once formed, the subclavian trunk may be joined by the jugular and bronchomediastinal trunks on the right side to form the right lymphatic duct, or it may enter the right venous angle independently. On the left side, the subclavian trunk most commonly joins the thoracic duct (Fig. 6.27A & B).
(inflammation of lymphatic vessels). The humeral group of nodes is
usually the first to be involved. Lymphangitis is characterized by the
development of warm, red, tender streaks in the skin of the limb.
Infections in the pectoral region and breast, including the superior
part of the abdomen, can also produce enlargement of axillary nodes. In
metastatic cancer of the apical group, the nodes often adhere to the
axillary vein, which may necessitate excision of part of this vessel.
Enlargement of the apical nodes may obstruct the cephalic vein superior
to the pectoralis minor.
Because the axillary lymph nodes are arranged and receive lymph (and
therefore metastatic breast cancer cells) in a specific order, removing
and examining the lymph nodes in that order is important in determining
the degree to which the cancer has developed and is likely to have
metastasized. Lymphatic drainage of the upper limb may be impeded after
the removal of the axillary nodes, resulting in lymphedema, swelling as a result of accumulated lymph, especially in the subcutaneous tissue.
of injury. During surgery, the long thoracic nerve to the serratus
anterior is identified and maintained against the thoracic wall. As
discussed earlier in this chapter, cutting the long thoracic nerve
results in a winged scapula. If the thoracodorsal nerve to the
latissimus dorsi is cut, medial rotation and adduction of the arm are
weakened, but deformity does not result. If the nodes around this nerve
are obviously malignant, sometimes the nerve has to be sacrificed as
the nodes are resected to increase the likelihood of complete removal
of all malignant cells.
structures passing between the neck and the upper limb. The axillary
vein lies anterior and slightly inferior to the axillary artery, both
being surrounded by the fascial axillary sheath. For descriptive
purposes, the axillary artery and vein are assigned three parts located
medial, posterior, and lateral to the pectoralis minor. Coincidentally,
the first part of the artery has one branch; the second part, two
branches; and the third part, three branches. The axillary lymph nodes
are embedded in the axillary fat external to the axillary sheath. The
axillary lymph nodes occur in groups that are arranged and receive
lymph in a specific order, which is important in staging and
determining appropriate treatment for breast cancer. In addition to
transporting blood and lymph to and from the upper limb, the vascular
structures of the axilla also serve the scapular and pectoral regions
and lateral thoracic wall. The axillary lymph nodes receive lymph from
the upper limb as well as the entire upper quadrant of the superficial
body wall, from the level of the clavicles to the umbilicus including
most from the breast.
a major nerve network supplying the upper limb; it begins in the neck
and extends into the axilla. Almost all branches of the brachial plexus
arise in the axilla (after the plexus has
crossed
the 1st rib). The brachial plexus is formed by the union of the
anterior rami of the last four cervical (C5–C8) and the first thoracic
(T1) nerves that constitute the roots of the brachial plexus (Fig. 6.28; Table 6.5). The roots usually pass through the gap between the anterior and the middle scalene (L. scalenus anterior and medius) muscles with the subclavian artery (Figs. 6.29 and 6.30).
The sympathetic fibers carried by each root of the plexus are received
from the gray rami of the middle and inferior cervical ganglia as the
roots pass between the scalene muscles.
-
A superior trunk, from the union of the C5 and C6 roots.
-
A middle trunk, which is a continuation of the C7 root.
-
An inferior trunk, from the union of the C8 and T1 roots.
and posterior divisions as the plexus passes through the
cervicoaxillary canal posterior to the clavicle. Anterior divisions of the trunks supply anterior (flexor) compartments of the upper limb, and posterior divisions of the trunks supply posterior (extensor) compartments.
-
Anterior divisions of the superior and middle trunks unite to form the lateral cord.
-
Anterior division of the inferior trunk continues as the medial cord.
-
Posterior divisions of all three trunks unite to form the posterior cord.
the lateral cord is lateral to the axillary artery, although it may
appear to lie superior to the artery because it is most easily seen
when the limb is abducted.
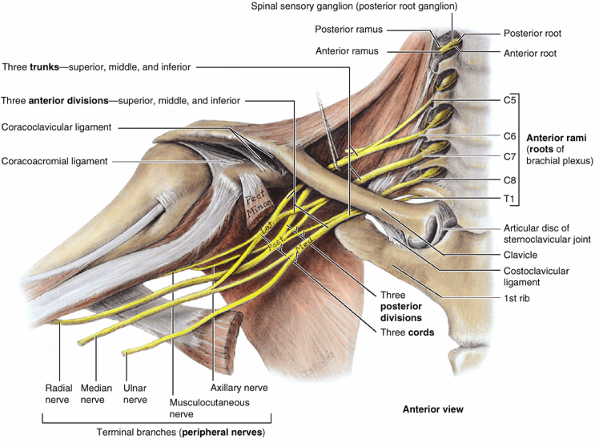 |
|
Figure 6.28. Formation of brachial plexus.
This large nerve network is shown extending from the neck to the upper limb via the cervicoaxillary canal (bound by the clavicle, 1st rib, and superior scapula) to provide innervation to the upper limb and shoulder region. The brachial plexus is typically formed by the anterior rami of the C5–C8 nerves and the greater part of the anterior ramus of the T1 nerve (the roots of the brachial plexus). Observe the merging and continuation of certain roots of the plexus to three trunks, the separation of each trunk into anterior and posterior divisions, the union of the divisions to form three cords, and the derivation of the main terminal branches (peripheral nerves) from the cords as the products of plexus formation. |
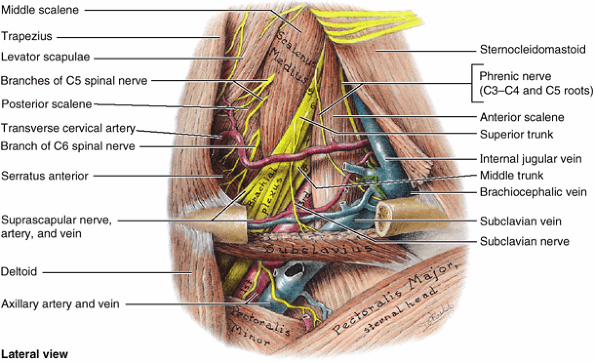 |
|
Figure 6.29. Dissection of right lateral cervical region (posterior triangle).
The brachial plexus and subclavian vessels have been dissected. The anterior rami of spinal nerves C5–C8 (plus T1, concealed here by the third part of the subclavian artery) constitute the roots of the brachial plexus (numbered). Merging and subsequent splitting of the nerve fibers conveyed by the roots form the trunks and divisions at the level shown. The subclavian artery emerges between the middle and anterior scalene muscles with the roots of the plexus. As the neurovascular structures pass posterior to the clavicle, they are traversing the cervicoaxillary canal connecting the neck and axilla. The subclavius, although not of major importance as a muscle, affords some protection to the underlying neurovascular structures when the clavicle is (commonly) fractured in its middle third. |
arise from the roots (anterior rami) and trunks of the brachial plexus
(dorsal scapular nerve, long thoracic nerve, nerve to subclavius, and
suprascapular nerve) and are approachable through the neck. In
addition, officially unnamed muscular branches
arise from all five roots of the plexus (anterior rami C5–T1), which
supply the scaleni and longus colli muscles. The C5 root of the phrenic nerve
(considered a branch of the cervical plexus) arises from the C5 plexus
root, joining the C3–C4 components of the nerve on the anterior surface
of the anterior scalene muscle (Fig 6.29). Branches of the infraclavicular part of the plexus
arise from the cords of the brachial plexus and are approachable
through the axilla. Counting side and terminal branches, three branches
arise from the lateral cord, whereas the medial and posterior cords
each give rise to five branches (counting the roots of the median nerve
as individual branches). The branches of the supra-clavicular and
infraclavicular parts of the brachial plexus are listed in Table 6.5, along with the origin, course and distribution of each branch.
In addition to the five anterior rami (C5–C8 and T1) that form the
roots of the brachial plexus, small contributions may be made by the
anterior rami of C4 or T2. When the superiormost root (anterior ramus)
of the plexus is C4 and the inferiormost root is C8, it is a prefixed brachial plexus. Alternately, when the superior root is C6 and the inferior root is T2, it is a postfixed brachial plexus.
In the latter type, the inferior trunk of the plexus may be compressed
by the 1st rib, producing neurovascular symptoms in the upper limb.
Variations may also occur in the formation of trunks, divisions, and
cords; in the origin and/or combination of branches; and in the
relationship to the axillary artery and scalene muscles. For example,
the lateral or medial cords may receive fibers from anterior rami
inferior or superior to the usual levels, respectively.
may be absent in one or other parts of the plexus; however, the makeup
of the terminal branches is unchanged. Because each peripheral nerve is
a collection of nerve fibers bound together by connective tissue, it is
understandable that the median nerve, for instance, may have two medial
roots instead of one (i.e., the nerve fibers are simply grouped
differently). This results from the fibers of the medial cord of the
brachial plexus dividing into three branches, two forming the median
nerve and the third forming the ulnar nerve. Sometimes it may be more
confusing when the two medial roots are completely separate; however,
understand that although the median nerve may have two medial roots,
the components of the nerve are the same (i.e., the impulses arise from
the same place and reach the same destination whether they go through
one or two roots).
|
Table 6.5. Brachial Plexus and Nerves of the Upper Limb
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
cutaneous sensations in the upper limb. Disease, stretching, and wounds
in the lateral cervical region (posterior triangle) of the neck (see Chapter 8)
or in the axilla may produce brachial plexus injuries. Signs and
symptoms depend on the part of the plexus involved. Injuries to the
brachial plexus result in paralysis and anesthesia. Testing the person’s ability to perform movements assesses the degree of paralysis. In complete paralysis, no movement is detectable. In incomplete paralysis,
not all muscles are paralyzed; therefore, the person can move, but the
movements are weak compared with those on the normal side. Determining
the ability of the person to feel pain (e.g., from a pinprick of the
skin) tests the degree of anesthesia.
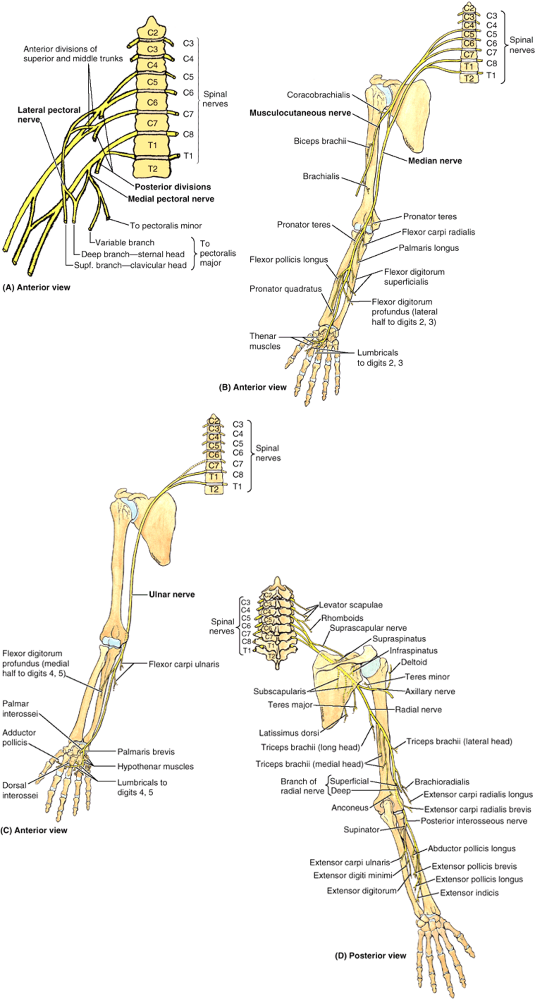 |
|
Figure 6.30. Summary of innervation of upper limb muscles. A.
The medial and lateral pectoral nerves arise from the medial and lateral cords of the brachial plexus, respectively (or from the anterior divisions of the trunks that form them, as shown here for the lateral pectoral nerve). B. The courses of the median and musculocutaneous nerves and the typical pattern of branching of their motor branches are shown. C. The course of the ulnar nerve and the typical pattern of branching of its motor branches are shown. D. The courses of the axillary and radial nerves and the typical pattern of branching of their motor branches are shown. The posterior interosseous nerve is the continuation of the deep branch of the radial nerve, shown here bifurcating into two branches to supply all the muscles with fleshy bellies located entirely in the posterior compartment of the forearm. The dorsum of the hand has no fleshy muscle fibers; therefore, no motor nerves are distributed there. |
(C5 and C6) usually result from an excessive increase in the angle
between the neck and the shoulder. These injuries can occur in a person
who is thrown from a motorcycle or a horse and lands on the shoulder in
a way that widely separates the neck and shoulder (Fig. B6.12A).
When thrown, the person’s shoulder often hits something (e.g., a tree
or the ground) and stops, but the head and trunk continue to move. This
stretches or ruptures superior parts of the brachial plexus or avulses
(tears) the roots of the plexus from the spinal cord. Injury to the
superior trunk of the plexus is apparent by the characteristic position
of the limb (“waiter’s tip position”), in which the limb hangs by the
side in medial rotation (Fig. B6.12B). Upper brachial plexus injuries can also occur in a newborn when excessive stretching of the neck occurs during delivery (Fig. B6.12C).
paralysis of the muscles of the shoulder and arm supplied by the C5 and
C6 spinal nerves occurs: deltoid, biceps, brachialis, and
brachioradialis. The usual clinical appearance is an upper limb with an
adducted shoulder, medially rotated arm, and extended elbow. The
lateral aspect of the upper limb also experiences loss of sensation.
Chronic microtrauma to the superior trunk of the brachial plexus from
carrying a heavy backpack can produce motor and sensory deficits in the
distribution of the musculocutaneous and radial nerves. A superior brachial plexus injury may produce muscle spasms and a severe disability in hikers (backpacker’s palsy) who carry heavy backpacks for long periods.
is a neurologic disorder of unknown cause that is characterized by the
sudden onset of severe pain, usually around the shoulder (Rowland, 2000). Typically, the pain begins at night and is followed by muscle weakness and sometimes muscular atrophy (neurologic amyotrophy). Inflammation of the brachial plexus (brachial neuritis)
is often preceded by some event (e.g., upper respiratory infection,
vaccination, or non-specific trauma). The nerve fibers involved are
usually derived from the superior trunk of the brachial plexus.
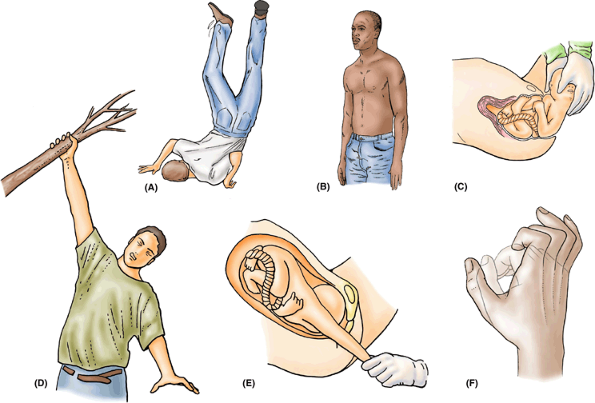 |
|
Figure B6.12. Injuries to brachial plexus. A. Note the excessive increase in the angle between the head and the left shoulder. B. The waiter’s tip position (left upper limb) is demonstrated. C. Observe the excessive increase in the angle between the head and the left shoulder during this delivery. D and E. Excessive increases in the angle between the trunk and the right upper limb are demonstrated. F. A claw hand is shown (person is attempting to assume lightly shaded “fist” position).
|
may result from prolonged hyperabduction of the arm during performance
of manual tasks over the head, such as painting a ceiling. The cords
are impinged or compressed between the coracoid process of the scapula
and the pectoralis minor tendon. Common neurologic symptoms are pain
radiating down the arm, numbness, paresthesia (tingling), erythema
(redness of the skin caused by capillary dilation), and weakness of the
hands. Compression of the axillary artery and vein causes ischemia of
the upper limb and distension of the superficial veins. These signs and
symptoms of hyperabduction syndrome result from compression of the axillary vessels and nerves.
are much less common. Inferior brachial plexus injuries may occur when
the upper limb is suddenly pulled superiorly—for example, when a person
grasps something to break a fall (Fig. B6.12D) or a baby’s upper limb is pulled excessively during delivery (Fig. B6.12E).
These events injure the inferior trunk of the brachial plexus (C8 and
T1) and may avulse the roots of the spinal nerves from the spinal cord.
The short muscles of the hand are affected, and a claw hand results (Fig. B6.12F).
surrounding the axillary sheath interrupts nerve impulses and produces
anesthesia of the structures supplied by the branches of the cords of
the plexus (Fig. 6.24A).
Sensation is blocked in all deep structures of the upper limb and the
skin distal to the middle of the arm. Combined with an occlusive
tourniquet technique to retain the anesthetic agent, this procedure
enables surgeons to operate on the upper limb without using a general
anesthetic. The brachial plexus can be anesthetized using a number of
approaches, including an interscalene, supraclavicular, and axillary
approach or block (Leonard, et al., 1999).
nerve fibers of the five adjacent anterior rami (C5–T1, the roots of
the plexus) innervating the upper limb. Although their segmental
identity is lost in forming the plexus, the original segmental
distribution to skin (dermatomes) and muscles (myotomes) remains,
exhibiting a cranial to caudal distribution for the skin (see “Cutaneous Nerves of the Upper Limb,”
earlier in this chapter) and a proximal to distal distribution for the
muscles. For example, C5 and C6 fibers primarily innervate muscles that
act at the shoulder or flex the elbow; C7 and C8 fibers innervate
muscles that extend the elbow or are part of the forearm; and T1 fibers
innervate the intrinsic muscles of the hand.
merging of the superior and inferior pairs of roots, resulting in three
trunks that each divide into anterior and posterior divisions. The
fibers traversing anterior divisions innervate flexors and pronators of
the anterior compartments of the limb, whereas the fibers traversing
posterior divisions innervate extensors and supinators of the posterior
compartments of the limb. The six divisions merge to form three cords
that surround the axillary artery. Two of the three cords give rise in
turn to 5 nerves, and the third (lateral cord) gives rise to 3 nerves.
In addition to the nerves arising from the cords, 10 more nerves arise
from the various parts of the plexus. Most nerves arising from the
plexus contain fibers from two or more adjacent anterior rami.
demarcating the root of the neck from the thorax. It also indicates the
“divide” between the deep cervical and the axillary “lymph sheds” (like
a mountain range dividing watershed areas): lymph from structures
superior to the clavicles drain via the deep cervical nodes; and lymph
from structures inferior to the clavicles, as far inferiorly as the
umbilicus, drain via the axillary lymph nodes. As the clavicle passes
laterally, its medial part can be felt to be convex anteriorly (Fig. SA6.4).
The large vessels and nerves to the upper limb pass posterior to this
convexity. The flattened acromial end of the clavicle does not reach
the point of the shoulder, formed by the lateral tip of the acromion of the scapula. The acromion is palpable and may be obvious when the deltoid contracts against resistance.
bounded by the clavicle superiorly, the pectoralis major medially, and
the deltoid laterally, which may be evident in the fossa in lean
individuals. The cephalic vein ascending from the upper limb enters the clavipectoral triangle and pierces the clavipectoral fascia to enter the axillary vein. The coracoid process
of the scapula is not subcutaneous; it is covered by the anterior
border of the deltoid; however, the tip of the process can be felt on
deep palpation on the lateral aspect of the clavipectoral triangle. The
coracoid process is used as a bony landmark
when performing a brachial plexus block, and its position is of
importance in diagnosing shoulder dislocations. While lifting a weight,
palpate the anterior sloping border of the trapezius
and where its superior fibers attach to the lateral third of the
clavicle. When the arm is abducted and then adducted against
resistance, the sternocostal part of the pectoralis major can be seen and palpated. If the anterior axillary fold bounding the axilla is grasped between the fingers and thumb, the inferior border of the sternocostal head of the pectoralis major can be felt. Several digitations of the serratus anterior are visible inferior to the anterior axillary fold. The posterior axillary fold is composed of skin and muscular tissue (latissimus dorsi and teres major) bounding the axilla posteriorly.
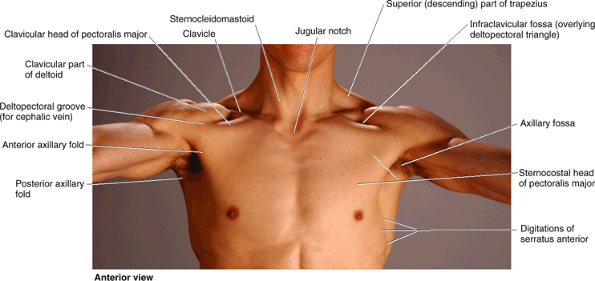 |
|
Figure SA6.4
|
is easily palpated and is usually visible. Grasp the inferior scapular
angle with the thumb and fingers and move the scapula up and down. When
the arm is adducted, the inferior scapular angle is opposite the tip of
the T7 spinous process and lies over the 7th rib or intercostal space.
is the most lateral bony point in the shoulder when the arm is adducted
and may be felt on deep palpation through the deltoid inferior to the
lateral border of the acromion. When the arm is abducted, observe that
the greater tubercle disappears beneath the acromion and is no longer
palpable. The borders and parts of the deltoid are usually visible when
the arm is abducted against resistance. Loss of the rounded muscular
appearance of the shoulder and the appearance of a surface depression
distal to the acromion are characteristic of a dislocated shoulder, or dislocation of the glenohumeral joint. The depression results from displacement of the humeral head. The teres major
is prominent when the abducted arm is adducted and medially rotated
against resistance (as when an acrobat stabilizes or fixes the shoulder
joint during an iron cross maneuver on the ring. [Fig. SA6.7]).
the rhomboids are not always visible. If the rhomboids of one side are
paralyzed, the scapula on the affected side remains farther from the
midline than on the normal side because the paralyzed muscles are
unable to retract it.
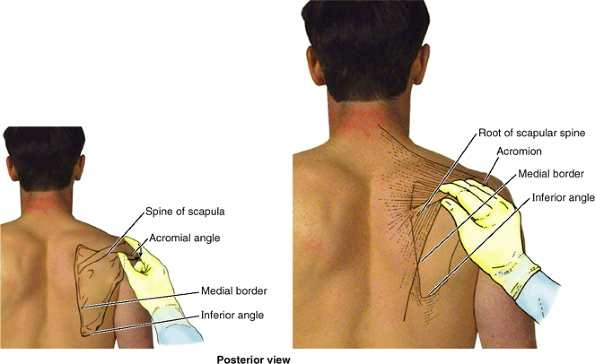 |
|
Figure SA6.5
|
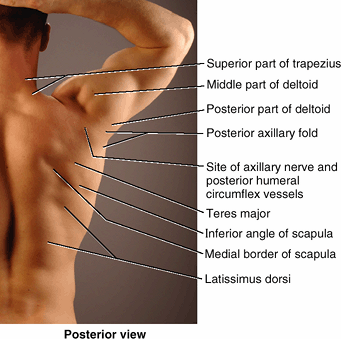 |
|
Figure SA6.6
|
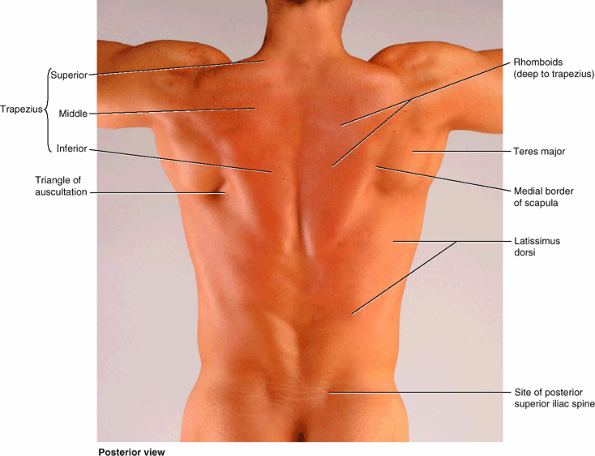 |
|
Figure SA6.7
|
shoulder to the elbow. Two types of movement occur between the arm and
the forearm at the elbow joint: flexion–extension and
pronation–supination. The muscles performing these movements are
clearly divided into anterior and posterior groups. The chief action of
both groups is at the elbow joint, but some muscles also act at the
glenohumeral joint. The superior part of the humerus provides
attachments for tendons of the shoulder muscles.
brachii, brachialis, and coracobrachialis) are in the anterior (flexor)
compartment, supplied by the musculocutaneous nerve (Figs. 6.31 and 6.32),
and one extensor (triceps brachii) is in the posterior compartment,
supplied by the radial nerve. A distally placed assistant to the
triceps, the anconeus, also lies within the posterior compartment. The
flexor muscles of the anterior compartment are almost twice as strong
as the extensors in all positions; consequently, we are better pullers
than pushers. It should be noted, however, that the extensors of the
elbow are particularly important for raising oneself out of a chair and
for wheelchair activity. Therefore, conditioning of the triceps is of
particular importance in elderly or disabled persons.
third head to the biceps. The usual two heads of the biceps arise
proximally by tendinous attachments to processes of the scapula, their
fleshy bellies uniting just distal to the middle of the arm (Fig. 6.31).
When present, the third head extends from the superomedial part of the
brachialis (with which it is blended), usually lying posterior to the
brachial artery. In either case, a single biceps tendon forms distally and attaches primarily to the radius.
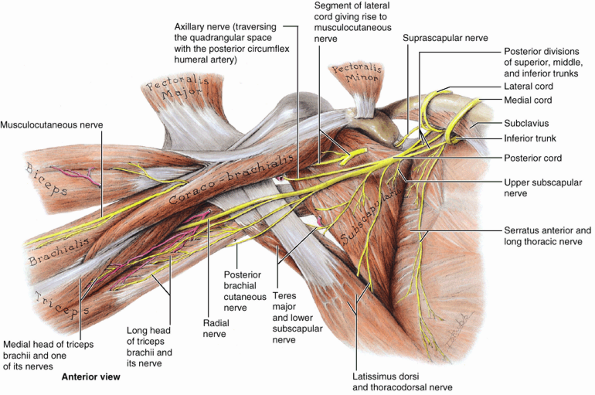 |
|
Figure 6.31. Posterior wall of axilla, musculocutaneous nerve, and posterior cord of brachial plexus.
The pectoralis major and minor muscles are reflected superolaterally, and the lateral and medial cords of the brachial plexus are reflected superomedially. All major vessels and the nerves arising from the medial and lateral cords of the brachial plexus (except for the musculocutaneous nerve from the lateral cord) are removed. The posterior cord, formed by the merging of the posterior divisions of all three trunks of the brachial plexus, gives rise to five nerves: radial, axillary, upper and lower subscapular, and thoracodorsal. Note that the musculocutaneous nerve pierces the coracobrachialis muscle and that the lower subscapular nerve supplies the teres major as well as the subscapularis. |
it has no attachment to the humerus. The biceps is a “three-joint
muscle,” crossing and capable of effecting movement at the
glenohumeral, elbow, and radioulnar joints, although it primarily acts
at the latter two. Its action and effectiveness is markedly affected by
the position of the elbow and forearm. When the elbow is extended, the
biceps is a simple flexor of the forearm; however, as elbow flexion
approaches 90° and more power is needed against resistance, the biceps
is capable of two powerful movements, depending on the position of the
forearm. When the elbow is flexed close to 90° and the forearm is
supinated, the biceps is most efficient in producing flexion.
Alternately, when the forearm is pronated, the biceps is the primary
(most powerful) supinator of the forearm. For example, it is used when
right-handed people drive a screw into hard wood and when inserting a
corkscrew and pulling the cork from a wine bottle. The biceps barely
operates as a flexor when the forearm is pronated, even against
resistance. In the semiprone position, it is active only against
resistance (Hamill and Knutzen, 2003).
glenohumeral joint, the rounded tendon of the long head of the biceps
continues to be surrounded by synovial membrane as it descends in the
intertubercular groove of the humerus. A broad band, the transverse humeral ligament, passes from the lesser to the greater tubercle of the humerus and converts the intertubercular groove into a canal (Table 6.6). The ligament holds the tendon of the long head of the biceps in the groove.
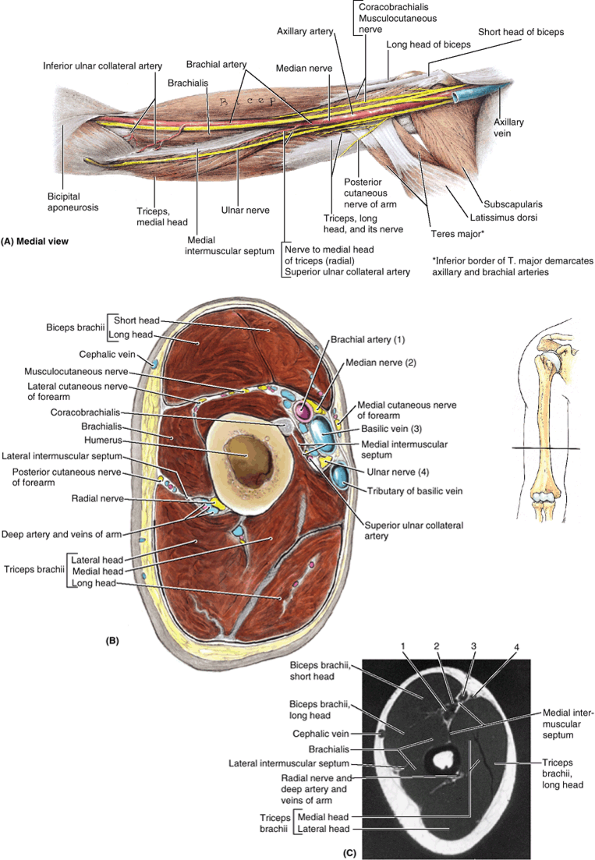 |
|
Figure 6.32. Muscles, neurovascular structures, and compartments of arm. A.
In this dissection of the right arm, the veins have been removed, except for the proximal part of the axillary vein. The courses of the musculocutaneous, median, and ulnar nerves and the brachial artery along the medial (protected) aspect of the arm are demonstrated. Their courses generally parallel the medial intermuscular septum that separates the anterior and posterior compartments in the distal two thirds of the arm. B. In this transverse section of the right arm, the three heads of the triceps and the radial nerve and its companion vessels (in contact with the humerus) lie in the posterior compartment. C. This transverse MRI demonstrates the features shown in part B. The numbered structures are identified in part B. (Courtesy of Dr. W. Kucharczyk, Chair of Medical Imaging and Clinical Director of Tri-Hospital Resonance Centre, Toronto, Ontario, Canada.) |
radial tuberosity via the biceps tendon. However, a triangular
membranous band, called the bicipital aponeurosis,
runs from the biceps tendon across the cubital fossa and merges with
the antebrachial (deep) fascia covering the flexor muscles in the
medial side of the forearm. It attaches indirectly by means of the
fascia to the subcutaneous border of the ulna. The proximal part of the
bicipital aponeurosis can be easily felt where it passes obliquely over
the brachial artery and median nerve (Fig. 6.33A).
The bicipital aponeurosis affords protection for these and other
structures in the cubital fossa. It also helps lessen the pressure of
the biceps tendon on the radial tuberosity during pronation and
supination of the forearm.
the elbow joint is flexed against resistance when the forearm is
supinated. If acting normally, the muscle forms a prominent bulge on
the anterior aspect of the arm that is easily palpated.
that are routinely tested during physical examination. The relaxed limb
is passively pronated and partially extended at the elbow. The
examiner’s thumb is firmly placed on the biceps tendon, and the reflex
hammer is briskly tapped at the base of the nail bed of the examiner’s
thumb (Fig. B6.13). A normal (positive)
response is an involuntary contraction of the biceps, felt as a
momentarily tensed tendon, usually with a brief jerk-like flexion of
the elbow. A positive response confirms the integrity of the
musculocutaneous nerve and the C5 and C6 spinal cord segments.
Excessive, diminished, or prolonged (hung) responses may indicate
central or peripheral nervous system disease or metabolic disorders
(e.g., thyroid disease).
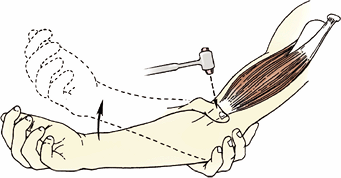 |
|
Figure B6.13. Method of eliciting biceps reflex.
|
a synovial sheath and moves back and forth in the inter-tubercular
groove of the humerus. Wear and tear of this mechanism can cause
shoulder pain. Inflammation of the tendon (biceps tendinitis),
usually the result of repetitive microtrauma, is common in sports
involving throwing (e.g., baseball and cricket) and use of a racquet
(e.g., tennis). A tight, narrow, and/or rough intertubercular groove
may irritate and inflame the tendon, producing tenderness and crepitus (a crackling sound).
partially or completely dislocated from the intertubercular groove in
the humerus. This painful condition may occur in young persons during
traumatic separation of the proximal epiphysis of the humerus. The
injury also occurs in older persons with a history of biceps
tendinitis. Usually a sensation of popping or catching is felt during
arm rotation.
of an inflamed tendon as it moves back and forth in the intertubercular
groove of the humerus. This injury usually occurs in individuals >
35 years of age. Typically, the tendon is torn from its attachment to
the supraglenoid tubercle of the scapula. The rupture is commonly
dramatic and is associated with a snap or pop. The detached muscle
belly forms a ball near the center of the distal part of the anterior
aspect of the arm (Popeye deformity) (Fig. B6.14).
Rupture of the biceps tendon may result from forceful flexion of the
arm against excessive resistance, as occurs in weight lifters (Anderson et al., 2000).
However, the tendon ruptures more often as the result of prolonged
tendinitis that weakens it. The rupture results from repetitive
overhead motions, such as occurs in swimmers and baseball pitchers,
which tear the weakened tendon where it passes through the
intertubercular groove.
 |
|
Figure B6.14
|
|
Table 6.6. Muscles of the Arm
|
|||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||
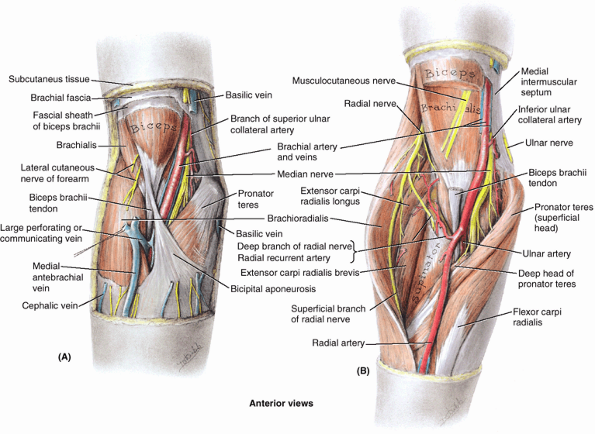 |
|
Figure 6.33. Dissections of cubital fossa. A.
In this superficial dissection, the distal end of the brachial artery lies medial to the biceps tendon. During the measurement of blood pressure, a stethoscope is placed here to listen to pulsations of the brachial artery. At this level, the median nerve lies on the medial aspect of the brachial artery, and both are deep to the bicipital aponeurosis (Fig. 6.38A). B. In this deep dissection, part of the biceps is excised and the cubital fossa is opened widely by retracting the forearm extensor muscles laterally and the flexor muscles medially. The radial nerve, which has just left the posterior compartment of the arm by piercing the lateral intermuscular septum, emerges between the brachialis and the brachioradialis and divides into a superficial (sensory) and a deep (motor) branch (Fig. 6.39A). The superficial branch remains under the protection of the brachioradialis, but the deep branch pierces the supinator to return to the posterior aspect of the limb. The brachial artery is dividing into its terminal branches: the ulnar artery, which runs deeply, and the radial artery, which remains superficial; thus its pulsations are palpable throughout the forearm. |
flattened fusiform muscle that lies posterior (deep) to the biceps. Its
distal attachment covers the anterior part of the elbow joint (Figs. 6.31, 6.32, 6.33 and 6.39A).
The brachialis is the main flexor of the forearm. It is the only pure
flexor, producing the greatest amount of flexion force. It flexes the
forearm in all positions, not being affected by pronation and
supination; during both slow and quick movements; and in the presence
or absence of resistance. When the forearm is extended slowly, the
brachialis steadies the movement by slowly relaxing—that is, eccentric
contraction (you use it to pick up and put down a teacup carefully, for
example). The brachialis always contracts when the elbow is flexed and
is primarily responsible for sustaining the flexed position. Because of
its important and almost constant role, it is regarded as the workhorse
of the elbow flexors.
distal part of its attachment indicates the location of the nutrient
foramen of the humerus. The coracobrachialis helps flex and adduct the
arm and stabilize the glenohumeral joint. With the deltoid and long
head of the triceps, it serves as a shunt muscle,
resisting downward dislocation of the head of the humerus, as when
carrying a heavy suitcase. The median nerve and/or the brachial artery
may run deep to the coracobrachialis and be compressed by it.
As indicated by its name, the triceps has three heads: long, lateral,
and medial. The triceps is the main extensor of the forearm. Because
its long head crosses the glenohumeral
joint, the triceps helps stabilize the adducted glenohumeral joint by
serving as a shunt muscle, resisting inferior displacement of the head
of the humerus. The long head also aids in extension and adduction of
the arm, but it is actually the least active head. The medial head is the workhorse of forearm extension, active at all speeds and in the presence or absence of resistance. The lateral head is strongest but is recruited into activity primarily against resistance. (Hamill and Knutzen, 2003).
Pronation and supination of the forearm do not affect triceps
operation. Just proximal to the distal attachment of the triceps is a
friction-reducing subtendinous olecranon bursa, between the triceps tendon and the olecranon.
determine the level of a radial nerve lesion), the arm is abducted 90°
and then the flexed forearm is extended against resistance provided by
the examiner. If acting normally, the triceps can be seen and palpated.
Its strength should be comparable with the contralateral muscle, given
consideration for lateral dominance (right or left handedness).
relatively unimportant triangular muscle on the posterolateral aspect
of the elbow; it is usually partially blended with the triceps (Table 6.6).
The anconeus helps the triceps extend the forearm and tenses of the
capsule of the elbow joint, preventing its being pinched during
extension. It is also said to abduct the ulna during pronation of the
forearm.
divides into the radial and ulnar arteries (Figs. 6.33B and 6.35).
The brachial artery, relatively superficial and palpable throughout its
course, lies anterior to the triceps and brachialis. At first it lies
medial to the humerus where its pulsations are palpable in the medial bicipital groove (Fig. 6.32B). It then passes anterior to the medial supraepicondylar ridge and trochlea of the humerus (Figs. 6.35 and 6.36). As it passes inferolaterally, the brachial artery accompanies the median nerve, which crosses anterior to the artery (Figs. 6.32A and 6.36). During its course through the arm, the brachial artery gives rise to many unnamed muscular branches and the humeral nutrient artery (Fig. 6.35),
which arise from its lateral aspect. The unnamed muscular branches are
often omitted from illustrations, but they are evident during
dissection.
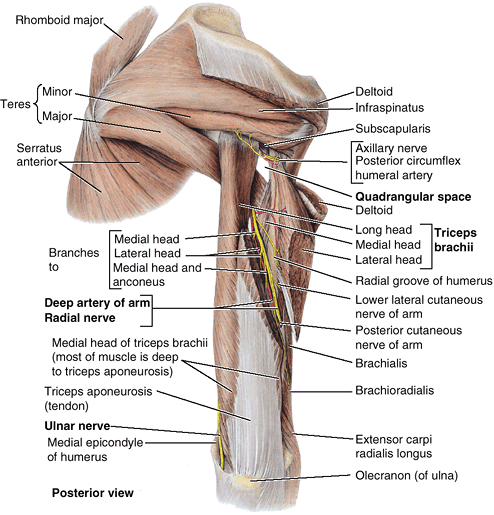 |
|
Figure 6.34. Muscles of scapular region and posterior region of arm.
The lateral head of the triceps brachii is divided and displaced to show the radial nerve and the deep artery of the arm. The exposed bone of the radial groove, which is devoid of muscular attachment, separates the humeral attachments of the lateral and medial heads of the triceps (bony attachments are illustrated in Table 6.6). The structures traversing the quadrangular space and the ulnar nerve passing posterior to the medial epicondyle of the humerus (where the nerve is most commonly injured) are also demonstrated. |
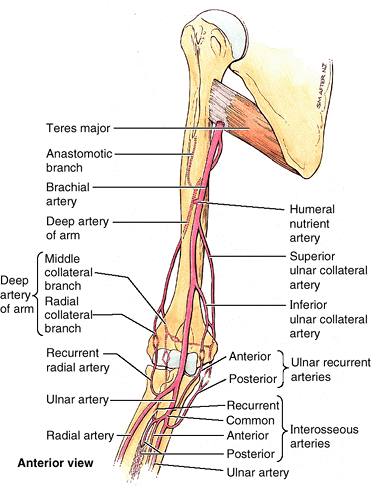 |
|
Figure 6.35. Arterial supply of arm and proximal forearm.
Functionally and clinically important periarticular arterial anastomoses surround the elbow. The resulting collateral circulation allows blood to reach the forearm when flexion of the elbow compromises flow through the terminal part of the brachial artery. |
Other arteries involved are recurrent branches, sometimes double, from
the radial, ulnar, and interosseous arteries, which run superiorly
anterior and posterior to the elbow joint. These arteries anastomose
with descending articular branches of the deep artery of the arm and
the ulnar collateral arteries.
is the largest branch of the brachial artery and has the most superior
origin. The deep artery accompanies the radial nerve along the radial
groove as it passes posteriorly around the shaft of the humerus (Figs. 6.34 and 6.36). The deep artery terminates by dividing into middle and radial collateral arteries that participate in the periarticular arterial anastomoses around the elbow.
nutrient canal on the anteromedial surface
of the humerus. The artery runs distally in the canal toward the elbow.
Other smaller humeral nutrient arteries also occur.
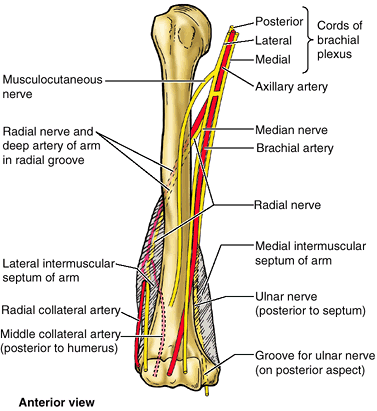 |
|
Figure 6.36. Relationship of the arteries and nerves of the arm to the humerus.
The cords of the brachial plexus surround the axillary artery. The radial nerve and accompanying deep artery of the arm wind posteriorly around, and directly on the surface of, the humerus in the radial groove. The radial nerve and radial collateral artery then pierce the lateral intermuscular septum to enter the anterior compartment. The ulnar nerve pierces the medial intermuscular septum to enter the posterior compartment and then lies in the groove for the ulnar nerve on the posterior aspect of the medial epicondyle of the humerus. The median nerve descends in the arm to the medial side of the cubital fossa, where it is well protected and rarely injured (Figs. 6.33 and 6.39). |
arises from the medial aspect of the brachial artery near the middle of
the arm and accompanies the ulnar nerve posterior to the medial
epicondyle of the humerus (Figs. 6.32A and 6.35).
Here it anastomoses with the posterior ulnar recurrent artery and the
inferior ulnar collateral artery, participating in the periarticular
arterial anastomoses of the elbow.
It then passes inferomedially anterior to the medial epicondyle of the
humerus and joins the anastomoses of the elbow region by anastomosing
with the anterior ulnar recurrent artery.
Because the arterial anastomoses around the elbow provide a
functionally and surgically important collateral circulation, the
brachial artery may be clamped distal to the origin of the deep artery
of the arm without producing tissue damage. The anatomical basis for
this procedure is that the ulnar and radial arteries will still receive
sufficient blood through the anastomoses around the elbow. Although
collateral pathways confer some protection against gradual temporary
and partial occlusion, sudden complete occlusion or laceration of the
brachial artery creates a surgical emergency because paralysis of
muscles results from ischemia of the elbow and forearm within a few hours. Muscles and nerves can tolerate up to 6 hours of ischemia (Salter, 1999);
after this, fibrous scar tissue replaces necrotic tissue and causes the
involved muscles to shorten permanently, producing a flexion deformity,
the ischemic compartment syndrome
(Volkmann or ischemic contracture). Contraction of the fingers and
sometimes the wrist results in loss of hand power as a result of
irreversible necrosis of the forearm flexor muscles.
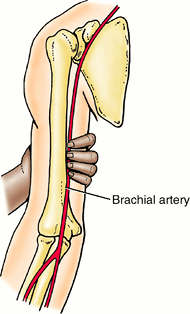 |
|
Figure B6.15. Compression of brachial artery.
|
injure the radial nerve in the radial groove in the humeral shaft. When
this nerve is damaged, the fracture is not likely to paralyze the
triceps because of the high origin of the nerves to two of its three
heads. A fracture of the distal part of the humerus, near the
supraepicondylar ridges, is called a supraepicondylar fracture (Fig. B6.16).
The distal bone fragment may be displaced anteriorly or posteriorly.
The actions of the brachialis and triceps tend to pull the distal
fragment over the proximal fragment, shortening the limb. Any of the
nerves or branches of the brachial vessels related to the humerus may
be injured by a displaced bone fragment.
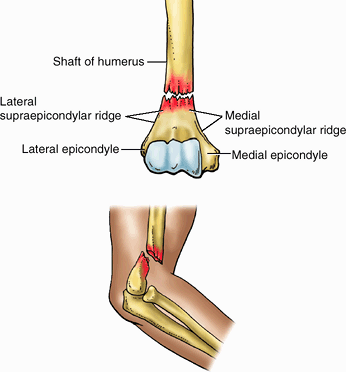 |
|
Figure B6.16. Supraepicondylar fracture.
|
superficial and deep, anastomose freely with each other. The
superficial veins are in the subcutaneous tissue, and the deep veins
accompany the arteries. Both sets of veins have valves, but they are
more numerous in the deep veins than in the superficial veins.
Their frequent connections encompass the artery, forming an anastomotic
network within a common vascular sheath. The pulsations of the brachial
artery help move the blood through this venous network. The brachial
vein begins at the elbow by union of the accompanying veins of the ulnar and radial arteries and end by merging with the basilic vein to form the axillary vein. Not uncommonly, the deep veins join to form one brachial vein during part of their course.
begins opposite the inferior border of the pectoralis minor, pierces
the coracobrachialis, and continues distally between the biceps and
brachialis (Fig. 6.33B). After supplying all three muscles of the anterior compartment of the arm, the nerve emerges lateral to the biceps as the lateral cutaneous nerve of the forearm.
It becomes truly subcutaneous when it pierces the deep fascia proximal
to the cubital fossa to course initially with the cephalic vein in the
subcutaneous tissue. After crossing the anterior aspect of the elbow,
it continues to supply the skin of the lateral aspect of the forearm.
all the muscles in the posterior compartment of the arm (and forearm).
The radial nerve enters the arm posterior to the brachial artery,
medial to the humerus, and anterior to the long head of the triceps,
where it gives branches to the long and medial heads of the triceps (Fig. 6.31).
The radial nerve then descends inferolaterally with the deep brachial
artery and passes around the humeral shaft in the radial groove (Figs. 6.32B, 6.34, and 6.36).
The branch to the lateral head of the triceps arises within the radial
groove. When it reaches the lateral border of the humerus, the radial
nerve pierces the lateral intermuscular septum and continues inferiorly
in the anterior compartment of the arm between the brachialis and the
brachioradialis to the level of the lateral epicondyle of the humerus (Fig. 6.33B). The radial nerve then divides into deep and superficial branches.
-
The deep branch of the radial nerve is entirely muscular and articular in its distribution.
-
The superficial branch of the radial nerve is entirely cutaneous in its distribution, supplying sensation to the dorsum of the hand and fingers.
distally in the arm on the lateral side of the brachial artery until it
reaches the middle of the arm, where it crosses to the medial side and
contacts the brachialis (Fig. 6.36). The median
nerve then descends into the cubital fossa, where it lies deep to the
bicipital aponeurosis and median cubital vein (Fig. 6.33). The median nerve has no branches in the axilla or the arm, but it does supply articular branches to the elbow joint.
distally from the axilla anterior to the insertion of the teres major
and to the long head of the triceps, on the medial side of the brachial
artery (Fig. 6.32). Around the middle of the
arm it pierces the medial intermuscular septum with the superior ulnar
collateral artery and descends between the septum and the medial head
of the triceps (Fig. 6.36). The ulnar nerve passes posterior to the medial epicondyle and medial to the olecranon to enter the forearm (Fig. 6.30C).
Posterior to the medial epicondyle, where the ulnar nerve is referred
to in lay terms as the “crazy bone,” it is superficial, easily
palpable, and vulnerable to injury. Like the median nerve, the ulnar
nerve has no branches in the arm, but it also supplies articular
branches to the elbow joint.
(uncommon in this protected position) is typically inflicted by a
weapon such as a knife. A musculocutaneous nerve injury results in paralysis of the coracobrachialis, biceps, and brachialis.
Consequently, flexion of the elbow joint and supination of the forearm
are greatly weakened but not lost. Weak flexion and supination are
still possible, produced by the brachioradialis and supinator,
respectively, both of which are supplied by the radial nerve. Loss of
sensation may occur on the lateral surface of the forearm supplied by
the lateral antebrachial cutaneous nerve, the continuation of the
musculocutaneous nerve.
Loss of sensation in areas of skin supplied by this nerve also occurs.
When the nerve is injured in the radial groove, the triceps is usually
not completely paralyzed but only weakened because only the medial head
is affected; however, the muscles in the posterior compartment of the
forearm that are supplied by more distal branches of the nerve are
paralyzed. The characteristic clinical sign of radial nerve injury is wrist-drop (inability to extend the wrist and the fingers at the metacarpophalangeal joints (Fig. B6.17A). Instead, the relaxed wrist assumes a partly flexed position owing to unopposed tonus of flexor muscles and gravity (Fig. B6.17B).
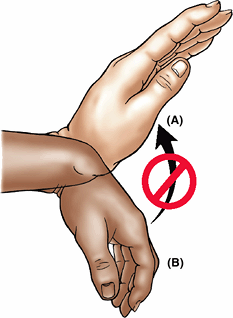 |
|
Figure B6.17. Wrist-drop.
|
The humerus, along with intermuscular septa in its distal two thirds,
divides the arm lengthwise (or more specifically, the space inside the
brachial fascia) into anterior or flexor and posterior or extensor
compartments. The anterior compartment contains three flexor muscles
supplied by the musculocutaneous nerve. The coracobrachialis acts
(weakly) at the shoulder, and the biceps and brachialis act at the
elbow. The biceps is also the primary supinator of the forearm (when
the elbow is flexed). The brachialis is the primary flexor of the
forearm. The posterior compartment contains a three-headed extensor
muscle, the triceps, which is supplied by the radial nerve. One of the
heads (the long head) acts at the shoulder, but mostly the heads work
together to extend the elbow. Both compartments are supplied by the
brachial artery, the posterior compartment primarily via its major
branch, the deep artery of the arm. The primary neurovascular bundle is
located on the medial side of the limb; thus it is usually protected by
the limb it serves.
superficially as a depression on the anterior aspect of the elbow.
Deeply, it is a space filled with a variable amount of fat anterior to
the most distal part of the humerus and the elbow joint. The three
boundaries of the triangular cubital fossa are as follows (Figs. 6.33 and 6.37C):
-
Superiorly, an imaginary line connecting the medial and lateral epicondyles.
-
Medially, the mass of flexor muscles of
the forearm arising from the common flexor attachment on the medial
epicondyle; most specifically, the pronator teres. -
Laterally, the mass of extensor muscles
of the forearm arising from the lateral epicondyle and supraepicondylar
ridge; most specifically, the brachioradialis.
brachialis and supinator muscles of the arm and forearm, respectively.
The roof of the cubital fossa is formed by the continuity of brachial
and antebrachial (deep) fascia reinforced by the bicipital aponeurosis (Figs. 6.38 and 6.39), subcutaneous tissue, and skin.
-
Terminal part of the brachial artery and
the commencement of its terminal branches, the radial and ulnar
arteries. The brachial artery lies between the biceps tendon and the
median nerve. -
(Deep) accompanying veins of the arteries.
-
Biceps brachii tendon.
-
Median nerve.
-
Radial nerve, deep between the muscles
forming lateral boundary of the fossa (the brachioradialis, in
particular) and the brachialis, dividing into its superficial and deep
branches. The muscles must be retracted to expose the nerve.
lying anterior to the brachial artery, and the medial and lateral
antebrachial cutaneous nerves, related to the basilic and cephalic
veins.
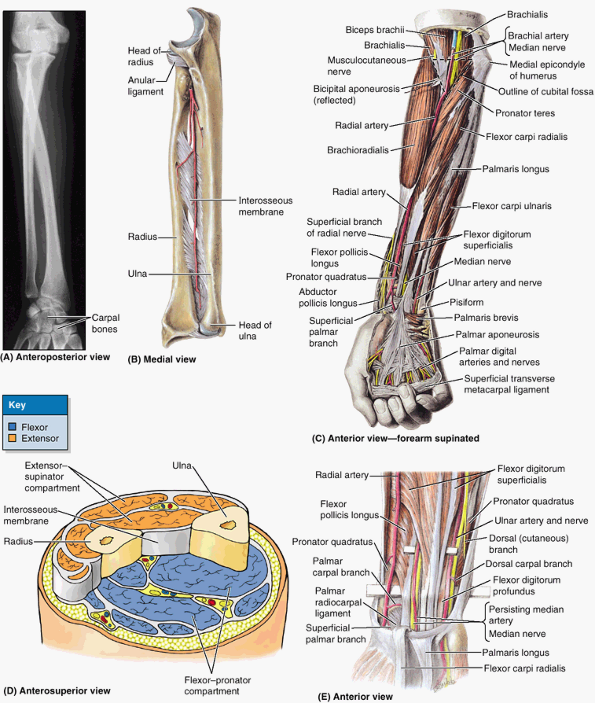 |
|
Figure 6.37. Bones, muscles, and compartments of forearm. A.
An anteroposterior (AP) radiograph of the forearm in pronation is shown. (Courtesy of Dr. J. Heslin, Toronto, Ontario, Canada.) B. The bones of the forearm and the radioulnar ligaments are demonstrated. C. In this dissection the superficial muscles of the forearm and the palmar aponeurosis are revealed. D. This stepped transverse section demonstrates the compartments of the forearm. E. The flexor digitorum superficialis (FDS) and related structures are shown. Observe the ulnar artery descending obliquely posterior to the FDS to meet and accompany the ulnar nerve. |
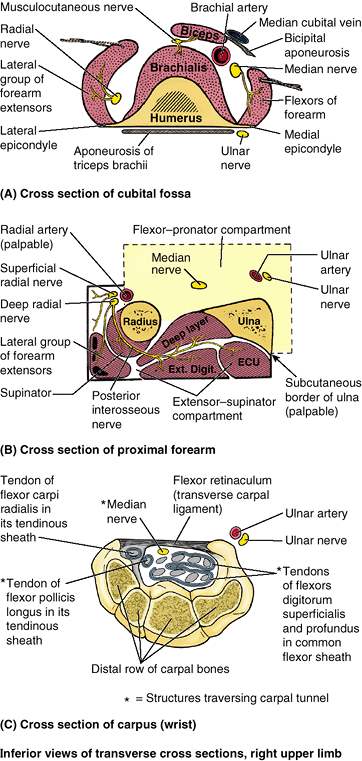 |
|
Figure 6.38. Cross sections demonstrating relationships at level of cubital fossa, proximal forearm, and wrist. A.
At the level of the cubital fossa, the flexors and extensor of the elbow occupy the anterior and posterior aspects of the humerus. Lateral and medial extensions (epicondyles and supraepicondylar ridges) of the humerus provide proximal attachment (origin) for the forearm flexors and extensors. B. Consequently, in the proximal forearm, the “anterior” flexor–pronator compartment actually lies anteromedially, and the “posterior” extensor–supinator compartment lies posterolaterally. The radial artery (laterally) and the sharp, subcutaneous posterior border of the ulna (medially) are palpable features separating the anterior and posterior compartments. No motor nerves cross either demarcation, making them useful for surgical approaches. Ext. digit., extensor digitorum; ECU, extensor carpi ulnaris. C. At the level of the wrist, nine tendons from three muscles (and one nerve) of the anterior compartment of the forearm traverse the carpal tunnel; eight of the tendons share a common synovial flexor sheath. |
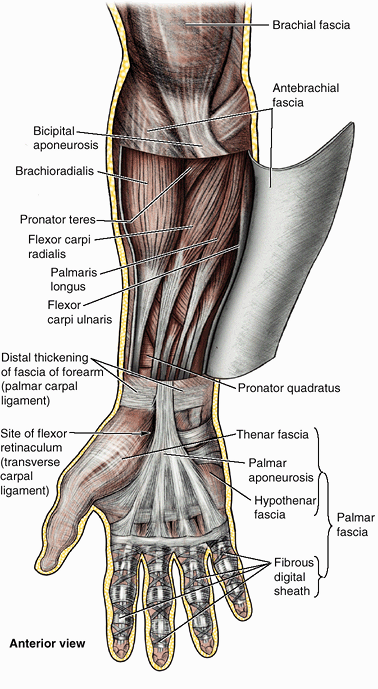 |
|
Figure 6.39. Antebrachial fascia and superficial muscles of forearm.
The brachioradialis, representing the lateral group of muscles, slightly overlaps the radial artery. The four superficial muscles of the anterior (flexor–pronator) compartment of the forearm (pronator teres, flexor carpi radialis, palmaris longus, and flexor carpi ulnaris) radiate from the medial epicondyle of the humerus (Fig. 6.38C). Over the distal ends of the radius and ulna, the antebrachial fascia thickens to form the extensor retinaculum posteriorly and a corresponding thickening, the palmar carpal ligament, anteriorly. Immediately distal and at a deeper level to the latter thickening, the flexor retinaculum (also continuous with the distal part of the antebrachial fascia), retains the tendons of the flexor muscles of the hand and fingers in the carpal tunnel. |
transfusion of blood and intravenous injections because of the
prominence and accessibility of veins. Usually, the median cubital vein
or basilic vein is selected. The median cubital vein lies directly on
the deep fascia, crossing the bicipital aponeurosis, which separates it
from the underlying brachial artery and median nerve and provides some
protection to the latter. Historically, during the days of
bloodletting, the bicipital aponeurosis was known as the grace Deux (Fr. grace of God) tendon,
by the grace of which arterial hemorrhage was usually avoided. A
tourniquet is placed around the midarm to distend the veins in the
cubital fossa. Once the vein is punctured, the tourniquet is removed so
that when the needle is removed the vein will not bleed extensively.
The cubital veins are also a site for the introduction of cardiac
catheters to secure blood samples from the great vessels and chambers
of the heart. These veins may also used for cardioangiography (see Chapter 1).
greatly. In approximately 20% of people, the median antebrachial vein
(median vein of the forearm) divides into a median basilic vein, which joins the basilic vein. and a median cephalic vein, which joins the cephalic vein (Fig. B6.18). In these cases, a clear M
formation is produced by the cubital veins. It is important to observe
and remember that either the median cubital vein or the median basilic
vein, whichever pattern is present, crosses superficial to the brachial
artery, from which it is separated by the bicipital aponeurosis. These
veins are good sites for drawing blood but are not ideal for injecting
an irritating drug because of the danger of injecting it into the
brachial artery. In obese people, a considerable amount of fatty tissue
may overlie the vein.
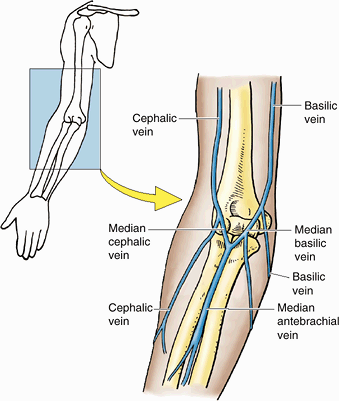 |
|
Figure B6.18
|
form a bulge on the posterior aspect of the arm and are identifiable
when the forearm is extended from the flexed position against
resistance. The olecranon, to which the triceps tendon attaches distally, is easily palpated. It is separated from the skin only by the olecranon bursa, which accounts for the mobility of the overlying skin. The triceps tendon
is easily felt as it descends along the posterior aspect of the arm to
the olecranon. The fingers can be pressed inwards on each side of the
tendon, where the elbow joint is superficial. An abnormal collection of
fluid in the elbow joint or in the triceps bursa or subtendinous olecranon bursa is palpable at these sites; the bursa lies deep to the triceps tendon.
bulge on the anterior aspect of the arm; its belly becomes more
prominent when the elbow is flexed and supinated against resistance (Fig. SA6.9). The biceps brachii tendon
can be palpated in the cubital fossa, immediately lateral to the
midline, especially when the elbow is flexed against resistance. The
proximal part of the bicipital aponeurosis can be palpated where it passes obliquely over the brachial artery and median nerve. Medial and lateral bicipital grooves separate the bulges formed by the biceps and triceps and indicate the location of the medial and lateral intermuscular septa (Fig. SA6.10).
The cephalic vein runs superiorly in the lateral bicipital groove, and
the basilic vein ascends in the medial bicipital groove. Deep to the
latter is the main neurovascular bundle of the limb.
however, it can be palpated with varying distinctness through the
muscles surrounding it, especially in many elderly people. The head of the humerus
is surrounded by muscles on all sides, except inferiorly; thus it can
be palpated by pushing the fingers well up into the axilla. The arm
should be close to the side so the axillary fascia is loose. The
humeral head can be identified by its movements when the arm is moved
and the inferior angle of the scapula is held so the scapula does not
move. The brachial artery may be felt pulsating deep to the medial border of the biceps. The medial and lateral epicondyles of the humerus
are subcutaneous and can be easily palpated at the medial and lateral
aspects of the elbow. The medial epicondyle is more prominent.
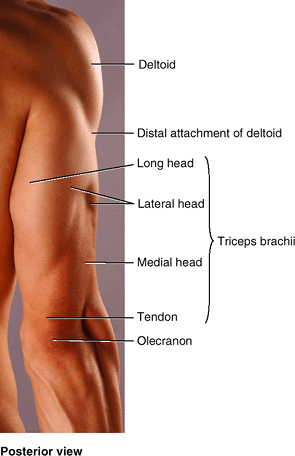 |
|
Figure SA6.8
|
(a soft mass that can be grasped separately), the brachioradialis (most
medial) and the long and short extensors of the wrist, can be grasped
between the fossa and the lateral epicondyle.
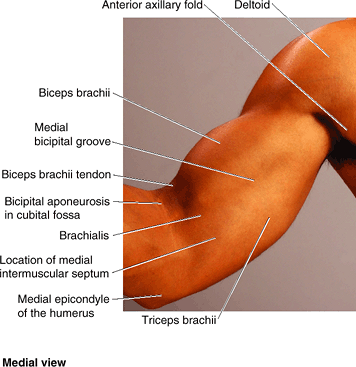 |
|
Figure SA6.9
|
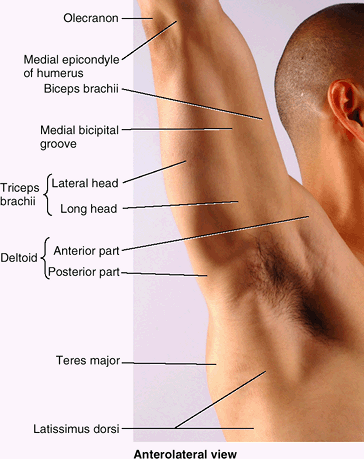 |
|
Figure SA6.10
|
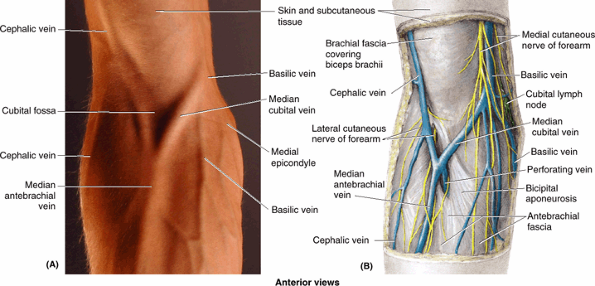 |
|
Figure SA6.11
|
unit of the articulated strut of the upper limb. It extends from the
elbow to the wrist and contains two bones, the radius and ulna (Fig. 6.37A, B, & D),
which are joined by an interosseous membrane. Although thin, this
fibrous membrane is strong. In addition to firmly tying the forearm
bones together while permitting pronation and supination, the interosseous membrane
provides the proximal attachment for some deep forearm muscles. The
head of the ulna is at the distal end of the forearm, whereas the head
of the radius is at its proximal end. The role of forearm movement,
occurring at the elbow and radioulnar joints, is to assist the shoulder
in the application of force and in controlling the placement of the
hand in space.
innervation are grouped within the same fascial compartments in the
forearm. Although the proximal boundary of the forearm per se is
defined by the joint plane of the elbow, functionally the forearm
includes the distal humerus. For the distal forearm, wrist, and hand to
have minimal bulk to maximize their functionality, they are operated by
“remote control” by extrinsic muscles having their bulky, fleshy,
contractile parts located proximally in the forearm, distant from the
site of action. Their long, slender tendons extend distally to the
operative site, like long ropes reaching to distant pulleys.
Furthermore, because the structures on which the muscles and tendons
act (wrist and fingers) have an extensive range of motion, a long range
of contraction is needed, requiring that the muscles have long
contractile parts as well as a long tendon(s).
provide the required length and sufficient area for attachment
proximally, so the proximal attachments (origins) of the muscles must
occur proximal to the elbow—in the arm—and be provided by the humerus.
Generally, flexors lie anteriorly and extensors posteriorly; however,
the anterior and posterior aspects of the distal humerus are occupied
by the chief flexors and extensors of the elbow (Fig. 6.38A).
To provide the required attachment sites for the flexors and extensors
of the wrist and fingers, medial and lateral extensions (epicondyles
and supraepicondylar ridges) have developed from the distal humerus.
The medial epicondyle and supraepicondylar ridge provide attachment for
the forearm flexors, and the lateral formations provide attachment for
the forearm extensors. Thus rather than lying strictly anteriorly and
posteriorly, the proximal parts of the “anterior” (flexor–pronator)
compartment of the forearm lie anteromedially, and the “posterior”
(extensor–supinator) compartment lies posterolaterally (Figs. 6.37D, 6.38B, and 6.40C).
Spiraling gradually over the length of the forearm, the compartments
become truly anterior and posterior in position in the distal forearm
and wrist. These fascial compartments, containing the muscles in
functional groups, are demarcated by the subcutaneous border of the
ulna posteriorly (in the proximal forearm) and then medially (distal
forearm) and by the radial artery anteriorly and then laterally. These
structures are palpable (the artery by its pulsations) throughout the
forearm. Because neither boundary is crossed by motor nerves, they also
provide sites for surgical incision.
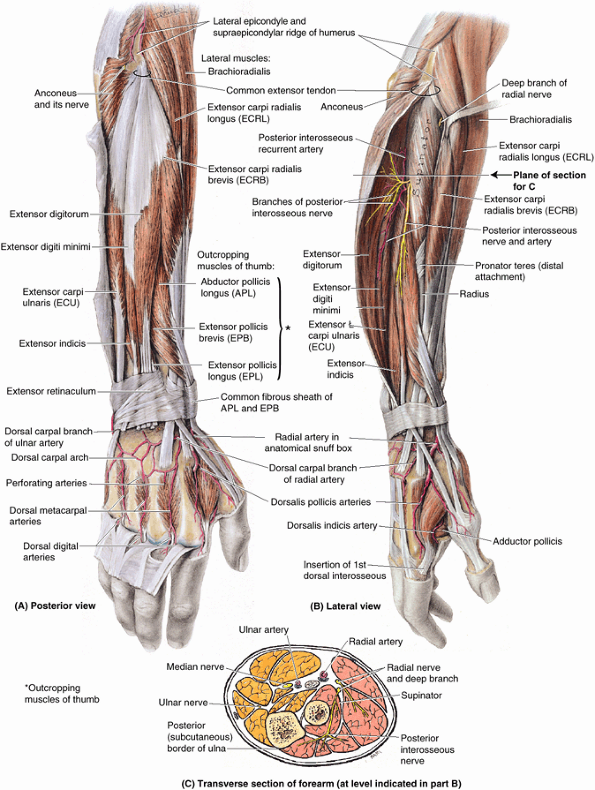 |
|
Figure 6.40. Extensor muscles of right forearm. A.
The superficial layer of extensor muscles is shown. The distal extensor tendons have been removed from the dorsum of the hand without disturbing the arteries because they lie on the skeletal plane. The fascia on the posterior aspect of the forearm is thickened to form the extensor retinaculum, which is anchored on its deep aspect to the radius and ulna. B. The deep layer of extensor muscles is shown. Three outcropping muscles of the thumb* emerge from between the extensor carpi radialis brevis and the extensor digitorum: abductor pollicis longus, extensor pollicis brevis, and extensor pollicis longus. The furrow from which the three muscles emerge has been opened proximally to the lateral epicondyle, exposing the supinator muscle. C. This transverse section of the forearm shows the superficial and deep layers of muscles in the posterior compartment (pink), supplied by the radial nerve, and the anterior compartment (gold), supplied by the ulnar and median nerves. Figure 6.38B also demonstrates these concepts. |
The extensors and supinators of the forearm are in the posterior
compartment and are all served by the radial nerve (directly or by its
deep branch). The fascial compartments of the limbs generally end at
the joints; therefore, fluids and infections in compartments are
usually contained and cannot readily spread to other compartments. The
anterior compartment is exceptional in this regard because it
communicates with the central compartment of the palm through the
carpal tunnel (Fig. 6.38C).
which act on the elbow joint exclusively, whereas others act at the
wrist and fingers. In the proximal part of the forearm, the muscles
form fleshy masses extending inferiorly from the medial and lateral
epicondyles of the humerus (Figs. 6.37C and 6.38A). The tendons of these muscles pass through the distal part of the forearm and continue into the wrist, hand, and fingers (Figs. 6.37C & E and 6.38C).
The flexor muscles of the anterior compartment have approximately twice
the bulk and strength of the extensor muscles of the posterior
compartment.
-
A superficial layer or group
of four muscles (pronator teres, flexor carpi radialis, palmaris
longus, and flexor carpi ulnaris). These muscles are all attached
proximally by a common flexor tendon to the medial epicondyle of the humerus, the common flexor attachment. -
An intermediate layer, consisting of one muscle (flexor digitorum superficialis).
-
A deep layer or group of three muscles (flexor digitorum profundus, flexor pollicis longus, and pronator quadratus).
are supplied by the median and/or ulnar nerves (most by the median;
only one and a half exceptions are supplied by the ulnar).
Functionally, the brachioradialis is a flexor of the forearm, but it is
located in the posterior (posterolateral) or extensor compartment and
is thus supplied by the radial nerve. Therefore, the brachioradialis is
a major exception to the rule that (1) the radial nerve supplies only
extensor muscles and (2) that all flexors lie in the anterior (flexor)
compartment.
(flexor digitorum superficialis and flexor digitorum profundus) also
flex the metacarpophalangeal and wrist joints. The flexor digitorum
profundus flexes the fingers in slow action; this action is reinforced
by the flexor digitorum superficialis when speed and flexion against
resistance are required. When the wrist is flexed at the same time that
the metacarpophalangeal and interphalangeal joints are flexed, the long
flexor muscles of the fingers are operating over a shortened distance
between attachments, and the action resulting from their contraction is
consequently weaker. Extending the wrist increases their operating
distance, and thus their contraction is more efficient in producing a
strong grip (Fig. 6.48). Tendons of the long
flexors of the digits pass through the distal part of the forearm,
wrist, and palm and continue to the medial four fingers. The flexor
digitorum superficialis flexes the middle phalanges, and the flexor
digitorum profundus flexes the distal phalanges.
muscles of the anterior compartment of the forearm are listed by
layers, in Table 6.7. The following discussion provides additional details, beginning with the muscles of the superficial and intermediate layers.
fusiform muscle, is the most lateral of the superficial forearm
flexors. Its lateral border forms the medial boundary of the cubital
fossa.
the person’s forearm is flexed at the elbow and pronated from the
supine position against resistance provided by the examiner. If acting
normally, the muscle is prominent and can be palpated at the medial
margin of the cubital fossa.
(FCR) is a long fusiform muscle located medial to the pronator teres.
In the middle of the forearm, its fleshy belly is replaced by a long,
flattened tendon that becomes cord-like as it approaches the wrist. The
FCR produces flexion (when acting with the flexor carpi ulnaris) and
abduction of the wrist (when acting with the extensors carpi radialis
longus and brevis). When acting alone, the FCR produces a combination
of flexion and abduction simultaneously at the wrist so that the hand
moves anterolaterally. To reach its distal attachment, the FCR tendon
passes through a canal in the lateral part of the flexor retinaculum
and through a vertical groove in the trapezium in its own synovial tendinous sheath of the flexor carpi radialis (Fig. 6.38C). The FCR tendon is a good guide to the radial artery, which lies just lateral to it (Fig. 6.37C).
|
Table 6.7. Muscles of the Anterior Compartment of the Forearm
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
fusiform muscle, is absent on one or both sides (usually the left) in
approximately 14% of people, but its actions are not missed. It has a
short belly and a long, cord-like tendon that passes superficial to the
flexor retinaculum and attaches to it and the apex of the palmar
aponeurosis (Figs. 6.37C and 6.39).
The palmaris longus tendon is a useful guide to the median nerve at the
wrist. The tendon lies deep and slightly medial to this nerve before it
passes deep to the flexor retinaculum.
the wrist is flexed and the pads of the little finger and thumb are
tightly pinched together. If present and acting normally, the tendon
can be easily seen and palpated.
(FCU) is the most medial of the superficial flexor muscles. The FCU
simultaneously flexes and adducts the hand at the wrist if acting
alone. It flexes the wrist when it acts with the FCR and adducts it
when acting with the extensor carpi ulnaris. The ulnar nerve enters the
forearm by passing between the humeral and the ulnar heads of its
proximal attachment (Fig. 6.37C).
This muscle is exceptional among muscles of the anterior compartment,
being fully innervated by the ulnar nerve. The tendon of the FCU is a
guide to the ulnar nerve and artery, which are on its lateral side at
the wrist (Fig. 6.37C & E).
the person puts the posterior aspect of the forearm and hand on a flat
table and is then asked to flex the wrist against resistance while the
examiner palpates the muscle and its tendon.
(FDS) is often included with the superficial muscles of the forearm,
which attach to the common flexor origin and therefore cross the elbow (Table 6.7).
When considered this way, it is the largest superficial muscle in the
forearm. However, the FDS actually forms an intermediate layer between
the superficial and the deep groups of forearm muscles (Fig. 6.37C & E). The median nerve and ulnar artery enter the forearm by passing between its humeroulnar and radial heads (Table 6.7A & C).
Near the wrist, the FDS gives rise to four tendons, which pass deep to
the flexor retinaculum through the carpal tunnel to the fingers. The
four tendons are enclosed (along with the four tendons of the flexor
digitorum profundus) in a synovial common flexor sheath (Fig. 6.38C).
The FDS flexes the middle phalanges of the medial four fingers at the
proximal interphalangeal joints. In continued action, the FDS also
flexes the proximal phalanges at the metacarpophalangeal joints and the
wrist joint. The FDS is capable of flexing each finger it serves
independently.
one finger is flexed at the proximal interphalangeal joint against
resistance and the other three fingers are held in an extended position
to inactivate the flexor digitorum profundus.
layers of muscles makes up the primary neurovascular plane of the
anterior (flexor–pronator) compartment; the main neurovascular bundles
exclusive to this compartment course within it.
This thick muscle “clothes” the anterior aspect of the ulna. The FDP
flexes the distal phalanges of the medial four fingers after the FDS
has flexed their middle phalanges (i.e., it curls the fingers and
assists with flexion of the hand, making a fist). Each tendon is
capable of flexing two interphalangeal joints, the metacarpophalangeal
joint and the wrist joint. The FDP divides into four parts, which end
in four tendons that pass posterior to the FDS tendons and the flexor
retinaculum within
the common flexor sheath (Fig. 6.38C).
The part of the muscle going to the index finger usually separates from
the rest of the muscle relatively early in the distal part of the
forearm and is capable of independent contraction. Each tendon enters
the fibrous sheath of its digit, posterior to the FDS tendons. Unlike
the FDS, the FDP can flex only the index finger independently; thus the
fingers can be independently flexed at the proximal but not the distal
interphalangeal joints.
the proximal interphalangeal joint is held in the extended position
while the person attempts to flex the distal interphalangeal joint. The
integrity of the median nerve in the proximal forearm can be tested by
performing this test using the index finger, and that of the ulnar
nerve can be assessed by using the little finger.
thumb), lies lateral to the FDP, where it clothes the anterior aspect
of the radius distal to the attachment of the supinator (Fig. 6.37C & E; Table 6.7A & D). The flat FPL tendon passes deep to the flexor retinaculum, enveloped in its own synovial tendinous sheath of the flexor pollicis longus on the lateral side of the common flexor sheath (Fig. 6.38C).
The FPL primarily flexes the distal phalanx of the thumb at the
interphalangeal joint and, secondarily, the proximal phalanx and 1st
metacarpal at the metacarpophalangeal and carpometacarpal joints,
respectively. The FPL is the only muscle that flexes the
interphalangeal joint of the thumb. It also may assist in flexion of
the wrist joint.
It cannot be palpated or observed, except in dissections, because it is
the deepest muscle in the anterior aspect of the forearm. Sometimes it
is considered to constitute a fourth muscle layer. The pronator
quadratus clothes the distal fourth of the radius and ulna and the
interosseous membrane between them (Table 6.7A & E).
The pronator quadratus is the only muscle that attaches only to the
ulna at one end and only to the radius at the other end. The pronator
quadratus is the prime mover for pronation. The muscle initiates
pronation; it is assisted by the pronator teres when more speed and
power are needed. The pronator quadratus also helps the interosseous
membrane hold the radius and ulna together, particularly when upward
thrusts are transmitted through the wrist (e.g., during a fall on the
hand).
(flexor–pronator) compartment of the forearm are located anteromedially
because they arise mainly from the common flexor attachment (medial
epicondyle and supraepicondylar ridge) of the humerus. Muscles in
superficial layer “bend” the wrist to position the hand (i.e., flex the
wrist when acting exclusively and abduct or adduct the wrist when
working with their extensor counterparts) and assist pronation. The
only muscle of the intermediate layer (FDS) primarily flexes the
proximal joints of 2nd–5th fingers. Muscles of the deep layer attach to
the anterior aspects of the radius and ulna, flex all (but especially
the distal) joints of all five digits, and pronate the forearm. The
muscles of the anterior compartment are innervated mostly by the median
nerve, but one and a half muscles (the FCU and ulnar half of the FDP)
are innervated by the ulnar nerve. The nerves and the ulnar artery
traverse the compartment in the fascial plane between the intermediate
and the deep layers of muscles. Flexion of the wrist and hand is used
for grasping, gripping, and drawing things toward one self. Pronation
is used for positioning the hand to manipulate or pick things up. Both
movements are basic protective (defensive) movements.
-
Muscles that extend and abduct or adduct
the hand at the wrist joint (extensor carpi radialis longus, extensor
carpi radialis brevis, and extensor carpi ulnaris). -
Muscles that extend the medial four fingers (extensor digitorum, extensor indicis, and extensor digiti minimi).
-
Muscles that extend or abduct the thumb (abductor pollicis longus, extensor pollicis brevis, and extensor pollicis longus).
which prevents bowstringing of the tendons when the hand is extended at
the wrist joint. As the tendons pass over the dorsum of the wrist, they
are provided with synovial tendon sheaths
that reduce friction for the extensor tendons as they traverse the
osseofibrous tunnels formed by the attachment of the extensor
retinaculum to the distal radius and ulna (Fig. 6.41).
(extensor carpi radialis brevis, extensor digitorum, extensor digiti
minimi, and extensor carpi ulnaris) are attached proximally by a common extensor tendon to the lateral epicondyle (Fig. 6.40; Table 6.8).
The proximal attachment of the other two muscles in the superficial
group (brachioradialis and extensor carpi radialis longus) is to the
lateral supraepicondylar ridge of the humerus and adjacent lateral
intermuscular septum. The four flat tendons of the extensor digitorum
pass deep to the extensor retinaculum to the medial four fingers. The
common tendons of the index and little fingers are joined on their
medial sides near the knuckles by the respective tendons of the
extensor indicis and extensor digiti minimi (extensors of the index and
little fingers, respectively).
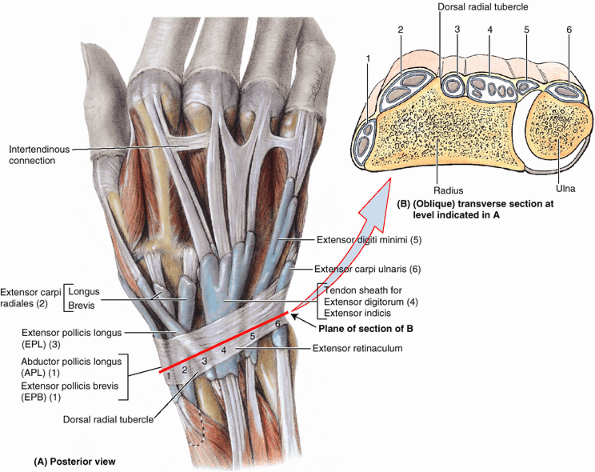 |
|
Figure 6.41. Synovial sheaths and tendons on distal forearm and dorsum of hand. A. Observe that the six synovial tendon sheaths (blue)
occupy six osseofibrous tunnels formed by attachments of the extensor retinaculum to the ulna and especially the radius, which give passage to 12 tendons of nine extensor muscles. Numbers refer to the labeled osseofibrous tunnels. B. This slightly oblique transverse section of the distal end of the forearm shows the extensor tendons traversing the six osseofibrous tunnels deep to the extensor retinaculum. |
muscles of the posterior compartment of the forearm are provided, by
layer, in Table 6.8. The following discussion provides additional details.
As mentioned previously, the brachioradialis is exceptional among
muscles of the posterior (extensor) compartment in that it has rotated
to the anterior aspect of the humerus and thus flexes the forearm at
the elbow. It is especially active during quick movements or in the
presence of resistance during flexion of the forearm (e.g., when a
weight is lifted), acting as a shunt muscle resisting subluxation of
the head of the radius. The brachioradialis and the supinator are the
only muscles of the compartment that do not cross and therefore are
incapable of acting at the wrist. As it descends, the brachioradialis
overlies the radial nerve and artery where they lie together on the
supinator, pronator teres tendon, FDS, and FPL. The distal part of the
tendon is covered by the abductors pollicis longus and brevis as they
pass to the thumb (Fig. 6.40).
the elbow joint is flexed against resistance with the forearm in the
midprone position. If the brachioradialis is acting normally, the
muscle can be seen and palpated.
As it passes distally, posterior to the brachioradialis, its tendon is
crossed by the abductor pollicis brevis and extensor pollicis brevis.
The ECRL is indispensable when clenching the fist.
|
Table 6.8. Muscles of the Posterior Compartment of the Forearm
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
the wrist is extended and abducted with the forearm pronated. If acting
normally, the muscle can be palpated inferoposterior to the lateral
side of the elbow. Its tendon can be palpated proximal to the wrist.
(ECRB), as its name indicates, is a shorter muscle than the ECRL
because it arises distally in the limb, yet it attaches adjacent to the
ECRL in the hand (but to the base of the 3rd metacarpal rather than the
2nd). As it passes distally, it is covered by the ECRL. The ECRB and
ECRL pass under the extensor retinaculum together within the tendinous sheath of the extensor carpi radiales (Fig. 6.41).
The two muscles act together to various degrees, usually as synergists
to other muscles. When the two muscles act by themselves, they abduct
the hand as they extend it. Acting with the extensor carpi ulnaris,
they extend the hand (the brevis is more involved in this action);
acting with the FCR they produce pure abduction. Their synergistic
action with the extensor carpi ulnaris is important in steadying the
wrist during tight flexion of the medial four fingers (clenching a
fist), a function in which the longus is more active.
On the dorsum of the hand, the tendons spread out as they run toward
the fingers. Adjacent tendons are linked proximal to the knuckles
(metacarpophalangeal joints) by three oblique intertendinous connections
that restrict independent extension of the fingers (especially the ring
finger). Consequently, normally no finger can remain fully flexed as
the other ones are fully extended. Commonly, the fourth tendon is fused
initially with the tendon to the ring finger and reaches the little
finger by a tendinous band.
Each extensor digital expansion (dorsal expansion or hood) is a
triangular, tendinous aponeurosis that wraps around the dorsum and
sides of a head of the metacarpal and proximal phalanx. The visor-like
“hood” formed by the extensor expansion over the head of the
metacarpal, holding the extensor tendon in the middle of the digit, is
anchored on each side to the palmar ligament (a reinforced portion of the fibrous layer of the joint capsule of the metacarpophalangeal joints) (Fig. 6.42B & D). In forming the extensor expansion, each flexor digitorum tendon divides into a median band, which passes to the base of the middle phalanx, and two lateral bands, which pass to the base of the distal phalanx (Fig. 6.42D & E). The tendons of the interosseous and lumbrical muscles of the hand join the lateral bands of the extensor expansion (Fig. 6.42).
a delicate fibrous band that runs from the proximal phalanx and fibrous
digital sheath obliquely across the middle phalanx and two
interphalangeal joints (Fig. 6.42C).
It joins the extensor expansion to the distal phalanx. During flexion
of the distal interphalangeal joint, the retinacular ligament becomes
taut and pulls the proximal joint into flexion. Similarly, on extending
the proximal joint, the distal joint is pulled by the retinacular
ligament into nearly complete extension.
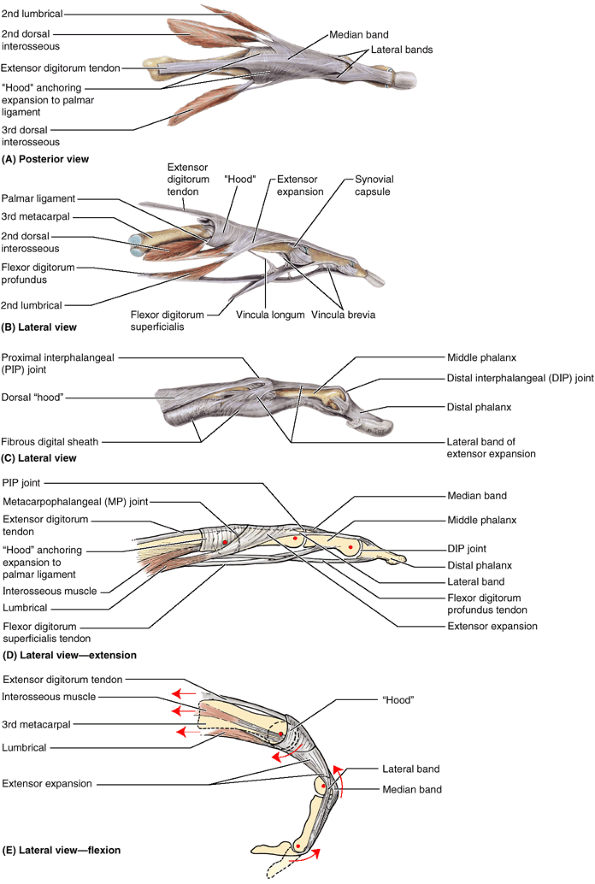 |
|
Figure 6.42. Dorsal digital (extensor) apparatus of 3rd digit. The metacarpal bone and all three phalanges are shown in parts A, B, D, and E; only the phalanges are shown in part C. A.
This posterior view shows the extensor digitorum tendon trifurcating (expanding) into three bands: two lateral bands that unite over the middle phalanx to insert into the base of the distal phalanx, and one median band that inserts into the base of the middle phalanx. B. Part of the tendon of the interosseous muscles attaches to the base of the proximal phalanx; the other part contributes to the extensor expansion, attaching primarily to the lateral bands, but also fans out into an aponeurosis. Some of the aponeurotic fibers fuse with the median band, and other fibers arch over it to blend with the aponeurosis arising from the other side. On the radial side of each digit, a lumbrical muscle attaches to the radial lateral band. The dorsal hood consists of a broad band of transversely oriented fibers attached anteriorly to the palmar ligaments of the metacarpophalangeal (MP) joints that encircle the metacarpal head and MP joint, blending with the extensor expansion to keep the apparatus centered over the dorsal aspect of the digit. C. Distally, retinacular ligaments extending from the fibrous digital sheath to the lateral bands also help keep the apparatus centered and coordinate movements at the proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints. D. Contraction of the extensor digitorum alone results in extension at all joints (including the MP joint in the absence of action by the interossei and lumbricals). E. Because of the relationship of the tendons and the lateral bands to the rotational centers of the joints (red dots in parts D and E), simultaneous contraction of the interossei and lumbricals produces flexion at the MP joint but extension at the PIP and DIP joints (the so-called Z-movement). |
phalanges and, through its collateral reinforcements, it secondarily
extends the middle and distal phalanges as well. After exerting its
traction on the digits, or in the presence of resistance to digital
extension, it helps extend the hand at the wrist joint.
the forearm is pronated and the fingers are extended. The person
attempts to keep the fingers extended at the metacarpophalangeal joints
as the examiner exerts pressure on the proximal phalanges by attempting
to flex them. If acting normally, the extensor digitorum can be
palpated in the forearm, and its tendons can be seen and palpated on
the dorsum of the hand.
The tendon of this extensor of the little finger runs through a
separate compartment of the extensor retinaculum, posterior to the
distal radioulnar joint, within the tendinous sheath of the extensor digiti minimi.
The tendon then divides into two slips; the lateral one is joined to
the tendon of the extensor digitorum, with all three tendons attaching
to the dorsal digital expansion of the little finger. After exerting
its traction primarily on the 5th finger, it contributes to extension
of the hand.
(ECU), a long fusiform muscle located on the medial border of the
forearm, has two heads: a humeral head from the common extensor tendon
and an ulnar head that arises by a common aponeurosis attached to the
posterior border of the ulna and shared by the FCU, FDP, and deep
fascia of the forearm. Distally, its tendon runs in a groove between
the ulnar head and its styloid process, through a separate compartment
of the extensor retinaculum within the tendinous sheath of the extensor carpi ulnaris.
Acting with the ECRL and ECRB, it extends the hand; acting with the
FCU, it adducts the hand. Like the ECRL, it is indispensable when
clenching the fist.
the forearm is pronated and the fingers are extended. The extended
wrist is then adducted against resistance. If acting normally, the
muscle can be seen and palpated in the proximal part of the forearm and
its tendon can be felt proximal to the head of the ulna.
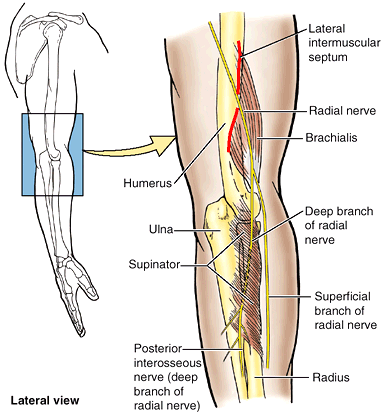 |
|
Figure 6.43. Relationship of radial nerve to brachialis and supinator muscles.
In the cubital fossa, lateral to the brachialis, the radial nerve divides into deep (motor) and superficial (sensory) branches. The deep branch penetrates the supinator muscle and emerges in the posterior compartment of the forearm as the posterior interosseous nerve. It joins the artery of the same name to run in the plane between the superficial and the deep extensors of the forearm. |
Spiraling medially and distally from its continuous, osseofibrous
origin, this sheet-like muscle envelops the neck and proximal part of
the shaft of the radius. The deep branch
of
the radial nerve passes between its muscle fibers, separating them into
superficial and deep parts, as it passes from the cubital fossa to the
posterior part of the arm. As it exits the muscle and joins the
posterior interosseous artery, it may be referred to as the posterior
interosseous nerve. The supinator is the prime mover for slow,
unopposed supination, especially when the forearm is extended. The
biceps brachii also supinates the forearm and is the prime mover during
rapid and forceful supination against resistance when the forearm is
flexed (e.g., when a right-handed person drives a screw).
act on the thumb (abductor pollicis longus, extensor pollicis longus,
and extensor pollicis brevis) and the index finger (extensor indicis) (Figs. 6.40 and 6.41; Table 6.8).
The three muscles acting on the thumb are deep to the superficial
extensors and “crop out” (emerge) from the furrow in the lateral part
of the forearm that divides the extensors. Because of this
characteristic, they are referred to as outcropping muscles (Fig. 6.40A).
(APL) has a long, fusiform belly that lies just distal to the supinator
and is closely related to the extensor pollicis brevis. Its tendon, and
sometimes its belly, is commonly split into two parts, one of which may
attach to the trapezium instead of the usual site at the base of the
1st metacarpal. The APL acts with the abductor pollicis brevis during
abduction of the thumb and with the extensor pollicis muscles during
extension of this digit. Although deeply situated, the APL emerges at
the wrist as one of the outcropping muscles. Its tendon passes deep to
the extensor retinaculum with the tendon of the extensor pollicis
brevis in the common synovial tendinous sheath of the abductor pollicis longus and extensor pollicis brevis.
the thumb is abducted against resistance at the metacarpophalangeal
joint. If acting normally, the tendon of the muscle can be seen and
palpated at the lateral side of the anatomical snuff box and on the lateral side of the adjacent extensor pollicis brevis tendon.
(EPB), the fusiform short extensor of the thumb, lies distal to the APL
and is partly covered by it. Its tendon lies parallel and immediately
medial to that of the APL but extends farther, reaching the base of the
proximal phalanx (Fig. 6.41). In continued
action after acting to flex the proximal phalanx of the thumb, or
acting when that joint is fixed by its antagonists, it helps extend the
1st metacarpal and extend and abduct the hand. When the thumb is fully
extended, a hollow called the anatomical snuff box, can be seen on the radial aspect of the wrist (Fig. 6.44).
the thumb is extended against resistance at the metacarpophalangeal
joint. If the EPB is acting normally, the tendon of the muscle can be
seen and palpated at the lateral side of the anatomical snuff box and
on the medial side of the adjacent APL tendon (Figs. 6.40 and 6.41).
medial to the dorsal tubercle of the radius. It uses the tubercle as a
trochlea (pulley) to change its line of pull as it proceeds to the base
of the distal phalanx of the thumb. The gap thus created between the
long extensor tendons of the thumb is the anatomical snuff box. In addition to its main actions (Table 6.8), the EPL also adducts the extended thumb and rotates it laterally.
the thumb is extended against resistance at the interphalangeal joint.
If the EPL is acting normally, the tendon of the muscle can be seen and
palpated on the medial side of the anatomical snuff box.
The snuff box is visible when the thumb is fully extended; this draws
the tendons up and produces a triangular hollow between them. Observe
that the:
-
Radial artery lies in the floor of the snuff box.
-
Radial styloid process can be palpated proximally and the
P.813P.814
base of the 1st metacarpal can be palpated distally in the snuff box.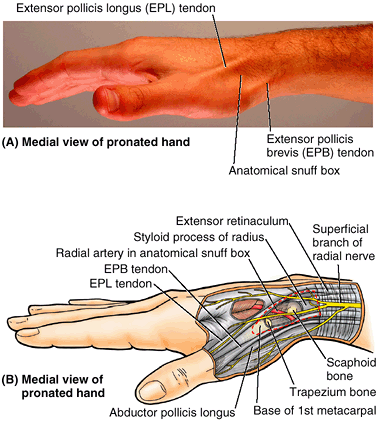 Figure 6.44. Anatomical snuff box. A.
Figure 6.44. Anatomical snuff box. A.
When the thumb is extended, a triangular hollow appears between the
tendon of the extensor pollicis longus (EPL) medially and the tendons
of the extensor pollicis brevis (EPB) and abductor pollicis longus
(APL) laterally. B. The floor of the snuff
box, formed by the scaphoid and trapezium bones, is crossed by the
radial artery as it passes diagonally from the anterior surface of the
radius to the dorsal surface of the hand. -
Scaphoid and trapezium can be felt in the floor of the snuff box between the radial styloid process and the 1st metacarpal (see clinical correlation [blue] box “Fracture of the Scaphoid,” earlier in this chapter).
musculoskeletal condition that may follow repetitive use of the
superficial extensor muscles of the forearm. Pain is felt over the
lateral epicondyle and radiates down the posterior surface of the
forearm. People with elbow tendinitis often feel pain when they open a
door or lift a glass. Repeated forceful flexion and extension of the
wrist strain the attachment of the common extensor tendon, producing
inflammation of the periosteum of the lateral epicondyle (lateral epicondylitis).
avulse part of its attachment to the phalanx. The most common result of
the injury is a mallet or baseball finger (Fig. B6.19A).
This deformity results from the distal interphalangeal joint suddenly
being forced into extreme flexion (hyperflexion when, for example, a
baseball is miscaught or a finger is jammed into the base pad (Fig. B6.19B).
These actions avulse the attachment of the tendon to the base of the
distal phalanx. As a result, the person cannot extend the distal
interphalangeal joint. The resultant deformity bears some resemblance
to a mallet.
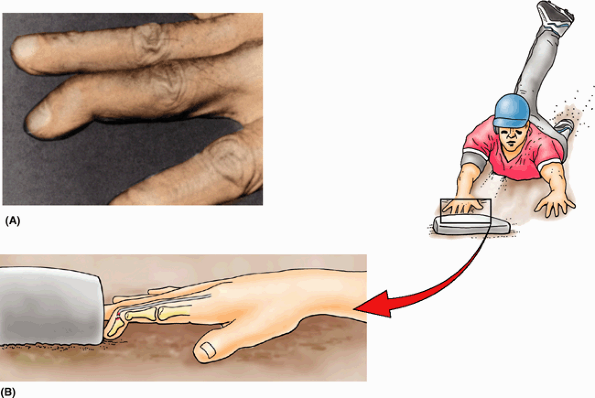 |
|
Figure B6.19. Mallet finger. The clinical appearance (A) and mechanism of injury (B) are shown.
|
laypersons, is common because the olecranon is subcutaneous and
protrusive. The typical mechanism of injury is a fall on the elbow
combined with sudden powerful contraction of the triceps. The fractured
olecranon is pulled away by the active and tonic contraction of the
triceps (Fig. B6.20), and the injury is often considered to be an avulsion fracture (Salter, 1999).
This is a serious fracture requiring the services of an orthopedic
surgeon. Because of the traction produced by the tonus of the triceps
on the olecranon fragment, pinning is usually required. Healing occurs
slowly, and often a cast must be worn for nearly a year.
Usually the cyst is the size of a small grape, but it varies and may be
as large as a plum. The thin-walled cyst contains clear mucinous fluid.
The cause of the cyst is unknown, but it may result from mucoid
degeneration (Salter, 1999). Flexion of the
wrist makes the cyst enlarge, and it may be painful. Clinically, this
type of swelling is called a “ganglion” (G. swelling or knot).
Anatomically, a ganglion refers to a collection of nerve cells (e.g., a
spinal ganglion). These synovial cysts are close to and often
communicate with the synovial sheaths on the dorsum of the wrist. The
distal attachment of the ECRB tendon to the base of the 3rd metacarpal
is another common site for such a cyst. A cystic swelling of the common
flexor synovial sheath on the anterior aspect of the wrist can enlarge
enough to produce compression of the median nerve by narrowing the
carpal tunnel (carpal tunnel syndrome).
This syndrome produces pain and paresthesia in the sensory distribution
of the median nerve and clumsiness of finger movements (see clinical correlation [blue] box “Carpal Tunnel Syndrome,” earlier in this chapter.
 |
|
Figure B6.20
|
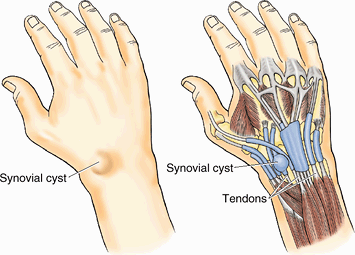 |
|
Figure B6.21
|
This muscle confers independence to the index finger in that the
extensor indicis may act alone or together with the extensor digitorum
to extend the index finger at the proximal interphalangeal joint, as in
pointing. It also helps extend the hand.
posterolaterally. Generally, the more distal their distal attachment
(insertion) the more distal and more deeply placed is their proximal
attachment (origin). Thus the most proximal muscle (brachioradialis)
does not cross and thus cannot act at the wrist (true also of the
supinator). The next most proximal muscles act to “bend” the wrist
(extend or act with their flexor counterparts to abduct and adduct).
The most distal muscles, which make up the deep layer, act at the thumb
and index finger. The extensors of the wrist and hand enable reach
(extension), opening of the hand in preparation for grasping, and
pushing; supination enables the holding of objects and feeding.
Extension is an aggressive movement (hitting, striking, pushing).
Extension of the wrist, however, is also an important component of
tight grip (clenching).
radial arteries, which usually arise opposite the neck of the radius in
the inferior part of the cubital fossa as terminal branches of the
brachial artery (Fig. 6.45). The origins and courses of the named arteries of the forearm are described in Table 6.9. The following discussion provides additional details.
can be palpated on the lateral side of the FCU tendon, where it lies
anterior to the ulnar head. The ulnar nerve is on the medial side of
the ulnar artery. Branches of the ulnar artery arising in the forearm
participate in the periarticular anastomosis of the elbow and supply
muscles of the medial and central forearm, the common flexor sheath,
and the ulnar and median nerves.
-
The anterior and posterior ulnar recurrent arteries
anastomose with the inferior and superior ulnar collateral arteries,
respectively, thereby participating in the periarticular arterial
anastomoses of the elbow. The anterior and posterior
P.815P.816P.817
arteries may be present as anterior and posterior branches of a (common) ulnar recurrent artery.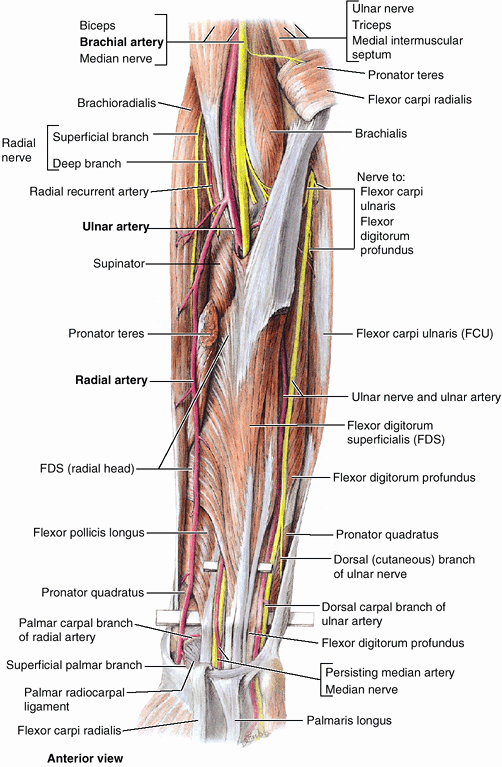 Figure 6.45. Flexor digitorum superficialis and related vasculature.
Figure 6.45. Flexor digitorum superficialis and related vasculature.
Three muscles of the superficial layer (pronator teres, flexor carpi
radialis, and palmaris longus) have been removed, leaving only their
attaching ends; the fourth muscle of the layer (the flexor carpi
ulnaris) has been retracted medially. The tendinous humeral attachment
of the FDS to the medial epicondyle is thick; and the linear attachment
to the radius, immediately distal to the radial attachments of the
supinator and pronator teres, is thin (Table 6.7).
The ulnar artery and median nerve pass between the humeral and the
radial heads of the FDS. The artery descends obliquely deep to the FDS
to join the ulnar nerve, which descends vertically near the medial
border of the FDS (exposed here by splitting a fusion of the FDS and
the FCU). A (proximal) probe is elevating the FDS tendons (and median
nerve and persisting median artery). A second (distal) probe is
elevating all the remaining structures that cross the wrist
(radiocarpal) joint anteriorly.Table 6.9. Arteries of the Forearm and Wrist![image]()
Artery Origin Course in Forearm Ulnar As larger terminal branch of brachial artery in cubital fossa Descends inferomedially and
then directly inferiorly, deep to superficial (pronator teres and
palmaris longus) and intermediate (flexor digitorum superficialis)
layers of flexor muscles to reach medial side of forearm; passes
superficial to flexor retinaculum at wrist in ulnar (Guyon) canal to
enter handAnterior ulnar recurrent artery Ulnar artery just distal to elbow joint Passes superiorly between
brachialis and pronator teres, supplying both; then anastomoses with
inferior ulnar collateral artery anterior to medial epicondylePosterior ulnar recurrent artery Ulnar artery distal to anterior ulnar recurrent artery Passes superiorly, posterior
to medial epicondyle and deep to tendon of flexor carpi ulnaris; then
anastomoses with superior ulnar collateral arteryCommon interosseous Ulnar artery in cubital fossa, distal to bifurcation of brachial artery Passes laterally and deeply, terminating quickly by dividing into anterior and posterior interosseous arteries Anterior interosseous As terminal branches of common interosseous artery, between radius and ulna Passes distally on anterior
aspect of interosseous membrane to proximal border of pronator
quadratus; pierces membrane and continues distally to join dorsal
carpal arch on posterior aspect of interosseous membranePosterior interosseous Passes to posterior aspect of
interosseous membrane, giving rise to recurrent interosseous artery;
runs distally between superficial and deep extensor muscles, supplying
both; replaced distally by anterior interosseous arteryRecurrent interosseous Posterior interosseous artery, between radius and ulna Passes superiorly, posterior
to proximal radioulnar joint and capitulum, to anastomose with middle
collateral artery (from deep brachial artery)Palmar carpal branch Ulnar artery in distal forearm Runs across anterior aspect of
wrist, deep to tendons of flexor digitorum profundus, to anastomose
with the palmar carpal branch of the radial artery, forming palmar
carpal archDorsal carpal branch Ulnar artery, proximal to pisiform Passes across dorsal surface
of wrist, deep to extensor tendons, to anastomose with dorsal carpal
branch of radial artery, forming dorsal carpal archRadial As smaller terminal branch of brachial artery in cubital fossa Runs inferolaterally under
cover of brachioradialis; lies lateral to flexor carpi radialis tendon
in distal forearm; winds around lateral aspect of radius and crosses
floor of anatomical snuff box to pierce first dorsal interosseous muscleRadial recurrent Lateral side of radial artery, just distal to brachial artery bifurcation Ascends between
brachioradialis and brachialis, supplying both (and elbow joint); then
anastomoses with radial collateral artery (from deep brachial artery)Palmar carpal branch Distal radial artery near distal border of pronator quadratus Runs across anterior wrist
deep to flexor tendons to anastomose with the palmar carpal branch of
ulnar artery to form palmar carpal archDorsal carpal branch Distal radial artery in proximal part of snuff box Runs medially across wrist
deep to pollicis and extensor radialis tendons, anastomoses with ulnar
dorsal carpal branch forming dorsal carpal arch -
The common interosseous artery,
a short branch of the ulnar artery, arises in the distal part of the
cubital fossa and divides almost immediately into anterior and
posterior interosseous arteries. -
The anterior interosseous artery
passes distally, running directly on the anterior aspect of the
interosseous membrane with the anterior interosseous nerve, whereas the
posterior interosseous artery courses
between the superficial and the deep layers of the extensor muscles in
the company of the posterior interosseous nerve. The relatively small
posterior interosseous artery is the principal artery serving the
structures of the middle third of the posterior compartment. Thus it is
mostly exhausted in the distal forearm and is replaced by the anterior
interosseous artery, which pierces the interosseous membrane near the
proximal border of the pronator quadratus. -
Unnamed muscular branches of the ulnar artery supply muscles on the medial side of the forearm, mainly those in the flexor–pronator group.
can be felt throughout the forearm, making it useful as an
anterolateral demarcation of the flexor and extensor compartments of
the forearm. When the brachioradialis is pulled laterally, the entire
length of the artery is visible (Fig. 6.45; Table 6.9).
The radial artery lies on muscle until it reaches the distal part of
the forearm. Here it lies on the anterior surface of the radius and is
covered by only skin and fascia, making this an ideal location for
checking the radial pulse. The course of the radial artery in the
forearm is represented by a line joining the midpoint of the cubital
fossa to a point just medial to the radial styloid process. The radial
artery leaves the forearm by winding around the lateral aspect of the
wrist and crosses the floor of the anatomical snuff box (Figs. 6.44 and 6.45).
-
The radial recurrent artery participates in the periarticular arterial anastomoses around the elbow by anastomosing with the radial collateral artery, a branch of the deep artery of the arm.
-
The palmar and dorsal carpal branches of the radial artery
participate in the periarticular arterial anastomosis around the wrist
by anastomosing with the corresponding branches of the ulnar artery and
terminal branches of the anterior and posterior interosseous arteries,
forming the palmar and dorsal carpal arches. -
The unnamed muscular branches of the radial artery
supply muscles in the adjacent (anterolateral) aspects of both the
flexor and the extensor compartments because the radial artery runs
along (and demarcates) the anterolateral boundary between the
compartments.
level than usual. In this case, the ulnar and radial arteries begin in
the superior or middle part of the arm, and the median nerve passes
between them (Fig. B6.22). The musculocutaneous and median nerves commonly communicate as shown in this illustration.
Pulsations of a superficial ulnar artery can be felt and may be
visible. This variation must be kept in mind when performing
venesections for withdrawing blood or making intravenous injections. If
an aberrant ulnar artery is mistaken for a vein, it may be damaged and
produce bleeding. If certain drugs are injected into the aberrant
artery, the result could be fatal.
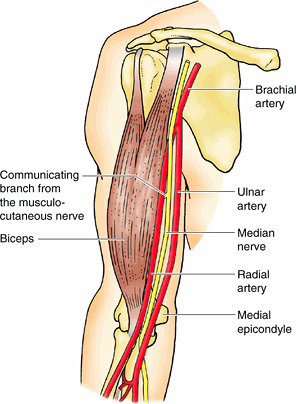 |
|
Figure B6.22
|
the radial artery lies on the anterior surface of the distal end of the
radius, lateral to the tendon of the FCR. Here the artery is covered by
only fascia and skin. The artery can be compressed against the distal
end of the radius, where it lies between the tendons of the FCR and
APL. When measuring the radial pulse rate, the pulp of the thumb should
not be used because it has its own pulse, which could obscure the
patient’s pulse. If a pulse cannot be felt, try the other wrist because
an aberrant radial artery on one side may
make the pulse difficult to palpate. A radial pulse may also be felt by
pressing lightly in the anatomical snuff box.
than usual; it may be a branch of the axillary artery or the brachial
artery. Sometimes the radial artery is superficial to the deep fascia
instead of deep to it. When a superficial vessel is pulsating near the
wrist, it is probably a superficial radial artery. The aberrant vessel
is vulnerable to laceration.
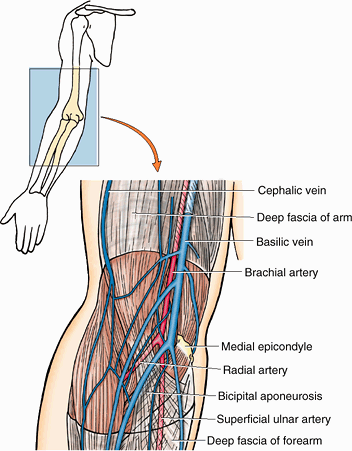 |
|
Figure B6.23
|
deep veins. The superficial veins ascend in the subcutaneous tissue.
The deep veins accompany the deep arteries of the forearm.
significance of the superficial veins of the upper limb were discussed
earlier in this chapter.
arise and accompany the ulnar artery. The veins accompanying each
artery anastomose freely with each other. The radial and ulnar veins
drain the forearm but carry
relatively
little blood from the hand. The deep veins ascend in the forearm along
the sides of the corresponding arteries, receiving tributaries from
veins leaving the muscles with which they are related. Deep veins
communicate with the superficial veins. The deep interosseous veins,
which accompany the interosseous arteries, unite with the accompanying
veins of the radial and ulnar arteries. In the cubital fossa the deep
veins are connected to the median cubital vein, a superficial vein. These deep cubital veins also unite with the accompanying veins of the brachial artery.
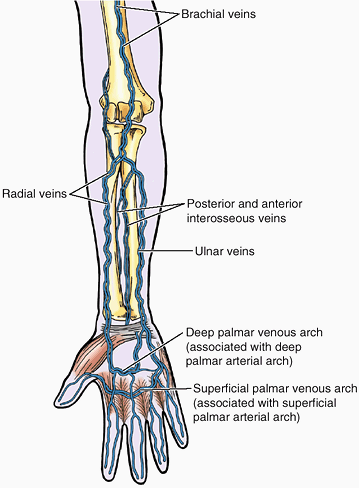 |
|
Figure 6.46. Deep venous drainage of upper limb.
The deep accompanying veins surround the arteries as their companions, with which they share names. They are relatively small, usually paired, and interconnected at intervals by transverse branches. |
radial. The median nerve is the principal nerve of the anterior
(flexor–pronator) compartment of the forearm (Figs. 6.38B and 6.48).
Although the radial nerve appears in the cubital region, it soon enters
the posterior (extensor–supinator) compartment of the forearm. Besides
the cutaneous branches, there are only two nerves of the anterior
aspect of the forearm: the median and ulnar nerves. The named nerves of
the forearm are illustrated and their origins and courses are described
in Table 6.10. The following discussion provides additional details and discusses unnamed branches.
It supplies muscular branches directly to the muscles of the
superficial and intermediate layers of forearm flexors (except the
FCU), and deep muscles (except for the medial [ulnar] half of the FDP)
via its branch, the anterior interosseous nerve.
small twigs to the brachial artery. Its major named nerve in the
forearm is the anterior interosseous nerve (Table 6.10). In addition, the following unnamed branches of the median nerve arise in the forearm:
-
Articular branches. These branches pass to the elbow joint as the median nerve passes it.
-
Muscular branches. The nerve to the pronator teres
usually arises at the elbow and enters the lateral border of the
muscle. A broad bundle of nerves pierces the superficial flexor group
of muscles and innervates the FCR, the palmaris longus, and the FDS. -
Anterior interosseous nerve.
This branch runs distally on the interosseous membrane with the
anterior interosseous branch of the ulnar artery. After supplying the
deep forearm flexors (except the ulnar part of the FDP, which sends
tendons to 4th and 5th fingers), it passes deep to and supplies the
pronator quadratus, then ends by sending articular branches to the
wrist joint. -
Palmar cutaneous branch of the median nerve.
This branch arises in the forearm, just proximal to the flexor
retinaculum, but is distributed to skin of the central part of the palm.
flexion of the proximal interphalangeal joints of the 1st–3rd fingers
is lost and flexion of the 4th and 5th fingers is weakened. Flexion of
the distal interphalangeal joints of the 2nd and 3rd fingers is also
lost. Flexion of the distal interphalangeal joints of the 4th and 5th
fingers is not affected because the medial part of the FDP, which
produces these movements, is supplied by the ulnar nerve. The ability
to flex the metacarpophalangeal joints of the 2nd and 3rd fingers is
affected because the digital branches of the median nerve supply the
1st and 2nd lumbricals. Thus, when the person attempts to make a fist,
the 2nd and 3rd fingers remain partially extended (“hand of
benediction”) (Fig. B6.24). Thenar muscle function (function of the muscles at the base of the thumb) is also lost, as in carpal tunnel syndrome (see clinical correlation [blue] box “Carpal Tunnel Syndrome,” later in this chapter).
 |
|
Figure B6.24. Pronator syndrome. A. Testing the flexion of the distal interphalangeal joint of the index finger is shown. B. The hand of benediction is demonstrated.
|
caused by compression of the median nerve near the elbow. The nerve may
be compressed between the heads of the pronator teres as a result of
trauma, muscular hypertrophy, or fibrous bands. Individuals with this
syndrome are first seen clinically with pain and tenderness in the
proximal aspect of the anterior forearm. Symptoms often follow
activities that involve repeated elbow movements.
|
Table 6.10. Nerves of the Forearm
|
||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||
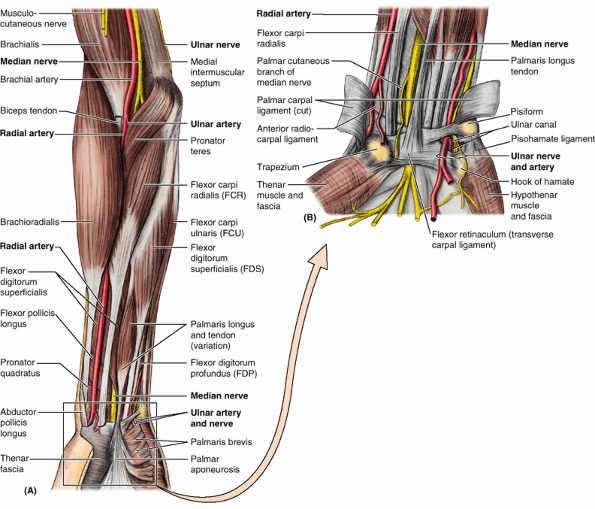 |
|
Figure 6.47. Neurovascular structures in anterior aspect of forearm and wrist. A.
At the elbow, the brachial artery lies between the biceps tendon and the median nerve. It bifurcates into the radial and ulnar arteries. In the forearm, the radial artery courses between the extensor and the flexor muscle groups. B. This deep dissection of the distal part of the forearm and proximal part of the hand shows the course of the arteries and nerves. |
does not give rise to branches during its passage through the arm. In
the forearm it supplies only one and a half muscles, the FCU (as it
enters the forearm by passing between its two heads of proximal
attachment) and the ulnar part of the FDP, which sends tendons to the
4th and 5th fingers. The ulnar nerve and artery emerge from beneath the
FCU tendon and become superficial just proximal to the wrist. They pass
superficial to the flexor retinaculum and enter the hand by passing
through a groove between the pisiform and the hook of the hamate. A
band of fibrous tissue from the flexor retinaculum bridges the groove
to form the small ulnar canal (Guyon canal) (Fig. 6.47B).
The branches of the ulnar nerve arising in the forearm include unnamed
muscular and articular branches, and cutaneous branches that pass to
the hand:
-
Articular branches pass to the elbow joint while the nerve is between the olecranon and medial epicondyle.
-
Muscular branches supply the FCU and the medial half of the FDP.
-
The palmar and dorsal cutaneous branches arise from the ulnar nerve in the forearm, but their sensory fibers are distributed to the skin of the hand.
and the ulnar nerves in the forearm. These branches are usually
represented by slender nerves, but the communications are important
clinically because even with a complete lesion of the median nerve,
some muscles may not be paralyzed. This may lead to an erroneous
conclusion that the median nerve has not been damaged.
Ulnar nerve injuries usually occur in four places: (1) posterior to the
medial epicondyle of the humerus, (2) in the cubital tunnel formed by
the tendinous arch connecting the humeral and ulnar heads of the FCU,
(3) at the wrist, and (4) in the hand.
The injury results when the medial part of the elbow hits a hard
surface, fracturing the medial epicondyle (“funny bone”). Compression
of the ulnar nerve at the elbow (cubital tunnel syndrome) is also common (see clinical correlation [blue] box “Cubital Tunnel Syndrome,” later in this chapter). Ulnar nerve injury usually produces numbness and tingling (paresthesia) of the medial part of the palm and the medial one and a half fingers (Fig. B6.26).
Pluck your ulnar nerve at the posterior aspect of your elbow with your
index finger and you may feel tingling in these fingers. Severe
compression may also produce elbow pain that radiates distally.
Uncommonly, the ulnar nerve is compressed as it passes through the
ulnar canal (see clinical correlation [blue] box “Ulnar Canal Syndrome (Guyon Tunnel Syndrome),” later in this chapter).
sensory loss to the hand. An injury to the nerve in the distal part of
the forearm denervates most intrinsic hand muscles. Power of wrist
adduction is impaired, and when an attempt is made to flex the wrist
joint, the hand is drawn to the lateral side by the FCR (supplied by
the median nerve) in the absence of the “balance” provided by the FCU.
After ulnar nerve injury, the person has difficulty making a fist
because, in the absence of opposition, the metacarpophalangeal joints
become hyperextended, and he or she cannot flex the 4th and 5th fingers
at the distal interphalangeal joints when trying to make a fist.
Furthermore, the person cannot extend the interphalangeal joints when
trying to straighten the fingers. This characteristic appearance of the
hand, resulting from a distal lesion of the ulnar nerve, is known as claw hand (main en griffe).
The deformity results from atrophy of the interosseous muscles of the
hand supplied by the ulnar nerve. The claw is produced by the unopposed
action of the extensors and FDP.
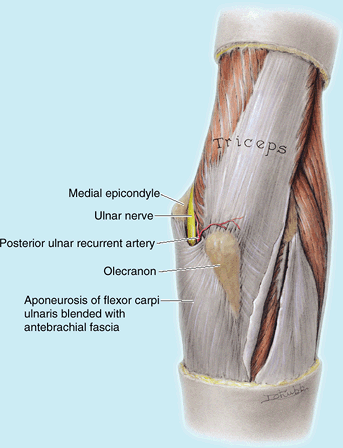 |
|
Figure B6.25. Vulnerable position of ulnar nerve.
|
The signs and symptoms of cubital tunnel syndrome are the same as an
ulnar nerve lesion in the ulnar groove on the posterior aspect of the
medial epicondyle of the humerus.
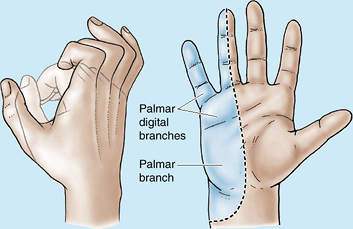 |
|
Figure B6.26. Claw hand and sensory distribution of ulnar nerve.
|
serves motor and sensory functions in both the arm and the forearm (but
only sensory functions in the hand). However, its sensory and motor
fibers are distributed in the forearm by two separate branches, the
superficial (sensory or cutaneous) and deep radial/posterior
interosseous nerve (motor). It divides into these terminal branches as
it appears in the cubital fossa, anterior to the lateral epicondyle of
the humerus, between the brachialis and the brachioradialis (Fig. 6.43).
The two branches immediately part company, the deep branch winding
laterally around the radius, piercing the supinator enroute to the
posterior compartment.
arises from the radial nerve in the posterior compartment of the arm,
as it runs along the radial groove of the humerus. Thus it reaches the
forearm independent of the radial nerve, descending in the subcutaneous
tissue of the posterior aspect of the forearm to the wrist, supplying
the skin.
is also a cutaneous nerve, but it gives rise to articular branches as
well. It is distributed to skin on the dorsum of the hand and to a
number of joints in the hand, branching soon after it emerges from the
overlying brachioradialis and crosses the roof of the anatomical snuff
box (Fig. 6.44).
runs in the fascial plane between superficial and deep extensor muscles
in close proximity to the posterior interosseous artery; it is usually
referred to as the posterior interosseous nerve (Fig. 6.43).
It supplies motor innervation to all the muscles with fleshy bellies
located entirely in the posterior compartment of the forearm (distal to
the lateral epicondyle of the humerus).
fracture of the humeral shaft. This injury is proximal to the branches
to the extensors of the wrist, and so wrist-drop is the primary clinical manifestation of an injury at this level (see clinical correlation [blue] box “Injury to the Radial Nerve in the Arm,”
earlier in this chapter). Injury to the deep branch of the radial nerve
may occur when wounds of the forearm are deep (penetrating). Severance
of the deep branch of the radial nerve results in an inability to
extend the thumb and the metacarpophalangeal (MP) joints of the other
digits. Thus the integrity of the deep radial nerve may be tested by
asking the person to extend the MP joints while the examiner provides
resistance (Fig. B6.27). If the nerve is
intact, the long extensor tendons should appear prominently on the
dorsum of the hand, confirming that the extension is occurring at the
MP joints rather than at the interphalangeal joints (movements under
the control of other nerves). Loss of sensation does not occur because
the deep branch of the radial nerve is entirely muscular and articular
in distribution. See Table 6.8 to determine the muscles that are paralyzed (e.g., extensor digitorum) when this nerve is severed.
cutaneous nerve, is severed, sensory loss is usually minimal. Commonly,
a coin-shaped area of anesthesia occurs distal to the bases of the 1st
and 2nd metacarpals. The reason the area of sensory loss is less than
expected, given the areas highlighted in Table 6.10, is the result of the considerable overlap from cutaneous branches of the median and ulnar nerves.
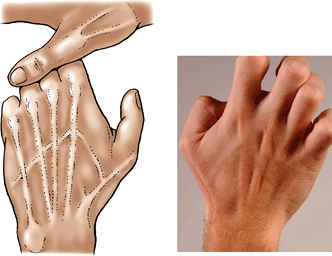 |
|
Figure B6.27. Testing the radial nerve.
|
of the forearm (lateral antebrachial cutaneous nerve) is the
continuation of the musculocutaneous nerve after its motor branches
have all been given off to the muscles of the anterior compartment of
the arm. The medial cutaneous nerve of the forearm (medial antebrachial cutaneous nerve) is an independent branch of the medial cord of the brachial plexus. With the posterior cutaneous nerve of the forearm
from the radial nerve, each supplying the area of skin indicated by its
name, these three nerves provide all the cutaneous innervation of the
forearm. There is no “anterior cutaneous nerve of the forearm.” (Memory device: This is similar to the brachial plexus, which has lateral, medial and posterior cords, but no anterior cord.)
have been considered separately, it is important to place them into
their anatomical context. Except for the superficial veins, which often
course independently in the subcutaneous tissue, these neurovascular
structures usually exist as components of neurovascular bundles. These
bundles are composed of arteries, veins (in the limbs, usually in the
form of accompanying veins), and nerves as well as lymphatic vessels,
which are usually surrounded by a neurovascular sheath of varying
density.
subcutaneous tissue of the forearm. These veins are subject to great
variation. Once they have penetrated the deep fascia, cutaneous nerves
run independently of the veins in the subcutaneous tissue where they
remain constant in location and size, with lateral, medial, and
posterior cutaneous nerves of the forearm supplying the aspects of the
forearm described by their names. Three major (radial, median or
middle, and ulnar) and two minor (anterior and posterior interosseous)
neurovascular bundles occur deep to the antebrachial fascia.
accompanying veins, and superficial radial nerve—course along and
define the border between the anterior and the posterior forearm
compartments (the vascular structures serving both) deep to the
brachioradialis. The middle (median nerve and variable median artery
and veins) and ulnar (ulnar nerve, artery, and accompanying veins)
bundles course in a fascial plane between the intermediate and the deep
flexor muscles. The median nerve supplies most muscles in the anterior
compartment, many via its anterior interosseous branch, which courses
on the interosseous membrane. The ulnar nerve supplies the one and a
half exceptions (FCU and ulnar half of the FDP). The deep radial nerve
penetrates the supinator to join the posterior interosseous artery in
the plane between the superficial and the deep extensors. This nerve
supplies all the muscles arising in the posterior compartment. The
flexor muscles of the anterior compartment have approximately twice the
bulk and strength of the extensor muscles of the posterior compartment.
This, and the fact that the flexor aspect of the limb is the more
protected aspect, accounts for the major neurovascular structures being
located in the anterior compartment, with only the relatively small
posterior interosseous vessels and nerve in the posterior compartment.
can be palpated distal to the lateral epicondyle. Supinate and pronate
your forearm and feel the movement of the radial head. The posterior border of the ulna
is subcutaneous and can be palpated distally from the olecranon along
the entire length of the bone. This landmark demarcates the
posteromedial boundary separating the flexor–pronator (anterior) and
extensor–supinator (posterior) compartments of the forearm.
that are attached to the medial epicondyle. To estimate the position of
these muscles, put your thumb posterior to your medial epicondyle and
then place your fingers on your forearm as shown in Figure SA6.13. The black dot
on the dorsum of the hand indicates the position of the medial
epicondyle. The cubital fossa is bounded laterally by the prominence of
the extensor–supinator group of muscles attached to the lateral epicondyle (Fig. SA6.14). The pulsations of the radial artery
can be palpated throughout the forearm as it runs its superficial
course from the cubital fossa to the wrist (anterior to the radial
styloid process), demarcating the anterolateral boundary separating the
flexor–pronator and extensor–supinator compartments of the forearm.
its distal end and is easily seen and palpated. It appears as a rounded
prominence at the wrist when the hand is pronated. The ulnar styloid process can be palpated just distal to the ulnar head. The larger radial styloid process
can be easily palpated on the lateral side of the wrist when the hand
is supinated, particularly when the tendons covering it are relaxed.
The radial styloid process is located approximately 1 cm more distal
than the ulnar styloid process. This relationship of the styloid
processes is important in the diagnosis of certain injuries in the
wrist region (e.g., fracture of the distal end of the radius). Proximal
to the radial styloid process, the surfaces of the radius are palpable for a few centimeters. The lateral surface of the distal half of the radius is easy to palpate.
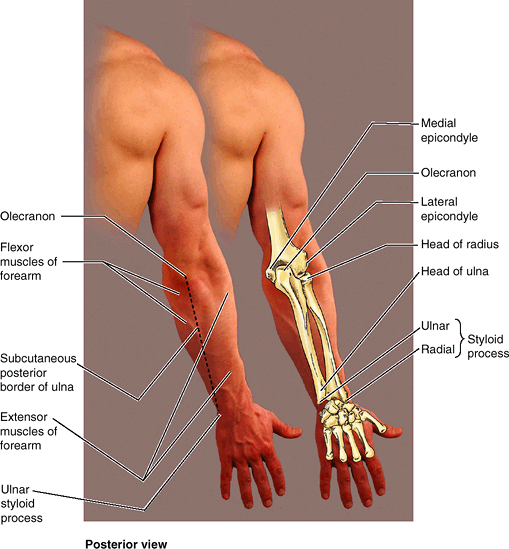 |
|
Figure SA6.12
|
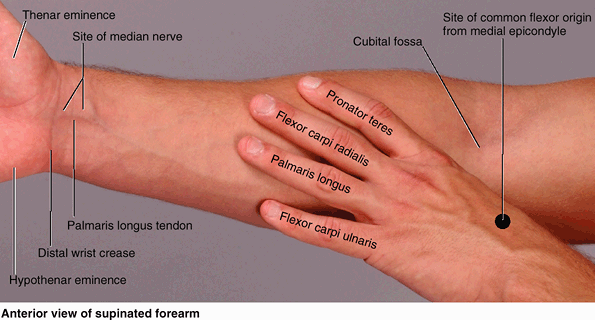 |
|
Figure SA6.13
|
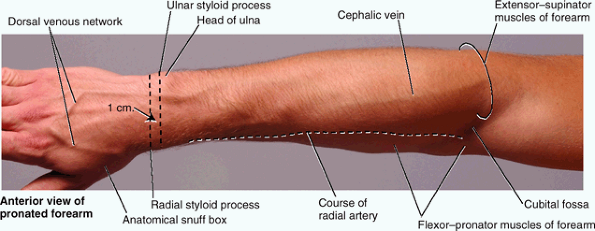 |
|
Figure SA6.14
|
is the manual part of the upper limb distal to the forearm. Once
positioned at the desired height and location relative to the body by
movements at the shoulder and elbow, and the direction of action is
established by pronation and supination of the forearm, the working
position or attitude (tilt) of the hand is adjusted by movement at the
wrist joint. The skeleton of the hand consists of carpals in the wrist, metacarpals in the hand proper, and phalanges
in the digits. The digits are numbered from one to five, beginning with
the thumb and ending with the little finger. The palmar aspect of the
hand features a central concavity that, with the crease proximal to it
(over the wrist bones) separates two eminences: a lateral, larger and
more prominent thenar eminence at the base of the thumb, and a medial, smaller hypothenar eminence proximal to the base of the 5th finger (Fig SA6.13).
structure and function of the hand is essential for all persons
involved in maintaining or restoring its activities: free motion, power
grasping, precision handling, and pinching.
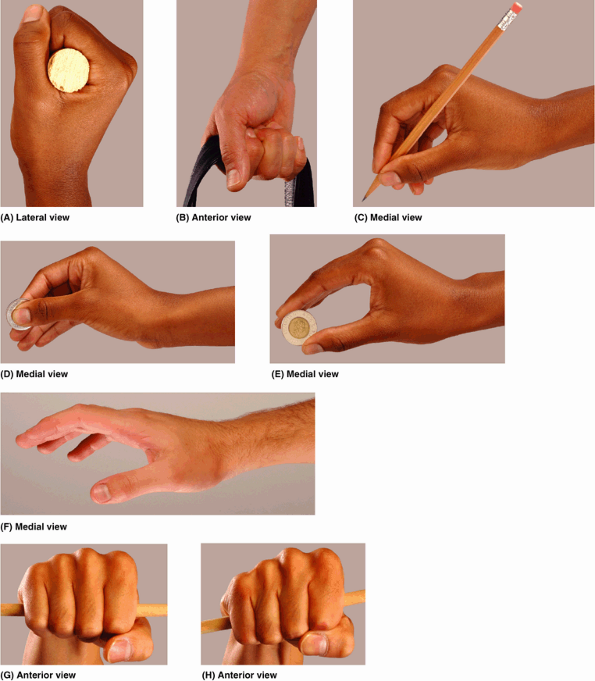 |
|
Figure 6.48. Functional positions of hand. A.
In the power grip, when grasping an object, the metacarpophalangeal (MP) and interphalangeal (IP) joints are flexed, but the radiocarpal and midcarpal joints are extended. “Cocking” (extension of) the wrist increases the distance over which the flexor tendons act, increasing tension of the long flexor tendons beyond that produced by maximal contraction of the muscles alone. B. The hook grip (flexion of the IP joints of the 2nd–4th digits) resists gravitational (downward) pull with only digital flexion. C. The precision grip is used when writing. D and E. One uses the precision grip to hold a coin to enable manipulation (D) and when pinching an object (E). F. Casts for fractures are applied with the hand and wrist in the resting position. Note the mild extension of the wrist. G and H. When gripping an unattached rod loosely (G) or firmly (H), the 2nd and 3rd carpometacarpal joints are rigid and stable, but the 4th and 5th are saddle joints permitting flexion and extension. The increased flexion changes the angle of the rod during the firm grip. |
refers to forcible motions of the digits acting against the palm; the
fingers are wrapped around an object with counterpressure from the
thumb—for example, when grasping a cylindrical structure (Fig. 6.48A).
The power grip involves the long flexor muscles to the fingers (acting
at the interphalangeal joints), the intrinsic muscles in the palm
(acting at the metacarpophalangeal joints), and the
extensors
of the wrist (acting at the radiocarpal and midcarpal joints). The
“cocking” of the wrist by the extensors increases the distance over
which the flexors of the fingers act, producing the same result as a
more complete muscular contraction. Conversely, as flexion increases at
the wrist, the grip becomes weaker and more insecure.
This grip consumes less energy, involving mainly the long flexors of
the fingers, which are flexed to a varying degree, depending on the
size of the object that is grasped.
involves a change in the position of a handled object that requires
fine control of the movements of the fingers and thumb—for example,
holding a pencil, manipulating a coin, threading a needle, or buttoning
a shirt (Fig. 6.48C & D).
In a precision grip, the wrist and fingers are held firmly by the long
flexor and extensor muscles, and the intrinsic hand muscles perform
fine movements of the digits.
compression of something between the thumb and the index finger—for
example, handling a teacup or holding a coin on edge (Fig. 6.48E)—or between the thumb and the adjacent two fingers—for example, snapping the fingers. The position of rest is assumed by an inactive hand—for example, when the forearm and hand are laid on a table (Fig. 6.48F). This position is often used when it is necessary to immobilize the wrist and hand in a cast to stabilize a fracture.
is thin over the thenar and hypothenar eminences, but it is thick
centrally where it forms the fibrous palmar aponeurosis and in the
fingers where it forms the digital sheaths (Figs. 6.39 and 6.49). The palmar
aponeurosis
a strong, well-defined part of the deep fascia of the palm, covers the
soft tissues and overlies the long flexor tendons. The proximal end or
apex of the triangular palmar aponeurosis is continuous with the flexor
retinaculum and the palmaris longus tendon. When the palmaris longus is
present, the palmar aponeurosis is the expanded tendon of the palmaris
longus. Distal to the apex, the palmar aponeurosis forms four
longitudinal digital bands or rays that radiate from the apex and
attach distally to the bases of the proximal phalanges and become
continuous with the fibrous digital sheaths.
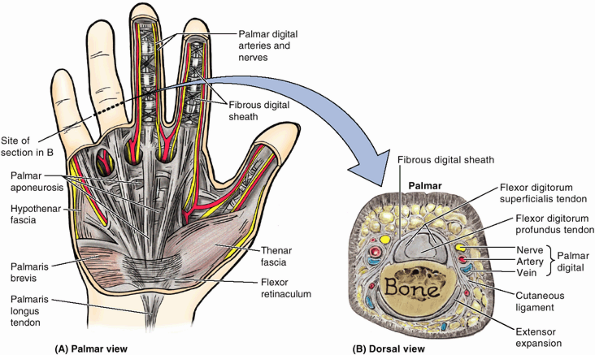 |
|
Figure 6.49. Palmar fascia and fibrous digital sheaths. A.
The palmar fascia is continuous with the antebrachial fascia. The thin thenar and hypothenar fascia covers the intrinsic muscles of the thenar and hypothenar eminences, respectively. Between the thenar and the hypothenar muscle masses, the central compartment of the palm is roofed by the thick palmar aponeurosis. When present (approximately 80% of the time), the distal end of the palmaris longus tendon blends with the aponeurosis superficial to the flexor retinaculum. Fibrous digital sheaths (shown here for the middle and index fingers), continuous with the longitudinal fiber bundles of the palmar aponeurosis, form the coverings of the digital portions of the tendons of the FDS and FDP. B. A transverse section of the 4th finger (proximal phalanx level) is shown. Within the fibrous digital sheath and proximal to its attachment to the base of the middle phalanx, the FDS tendon has split into two parts to allow continued central passage of the FDP tendon to the distal phalanx. The palmar digital nerve, artery, and vein are adjacent to the sheath, not to the phalanx (Bone). The dorsal digital neurovascular structures become exhausted near the midpoint of the middle phalanges; thus the palmar nerves, arteries, and veins serve all (palmar and dorsal aspects) of the digits distally. |
are ligamentous tubes that enclose the synovial sheaths, the
superficial and deep flexor tendons, and the tendon of the FPL in their
passage along the palmar aspect of their respective fingers (Figs. 6.39, 6.42C, and 6.49). The flexor digital sheaths are composed of five anular and four cruciform (cross-shaped) parts or “pulleys.”
extends deeply from the lateral border of the palmar aponeurosis to the
3rd metacarpal. Lateral to this septum is the lateral or thenar compartment containing the thenar muscles. Between the hypothenar and the thenar compartments is the central compartment
containing the flexor tendons and their sheaths, the lumbricals, the
superficial palmar arterial arch, and the digital vessels and nerves.
The deepest muscular plane of the palm is the adductor compartment containing the adductor pollicis.
The spaces are bounded by fibrous septa passing from the edges of the
palmar aponeurosis to the metacarpals. Between the two spaces is the
especially strong lateral fibrous septum, which is attached to the 3rd
metacarpal. Although most fascial compartments end at the joints, the
midpalmar space is continuous with the anterior compartment of the
forearm via the carpal tunnel.
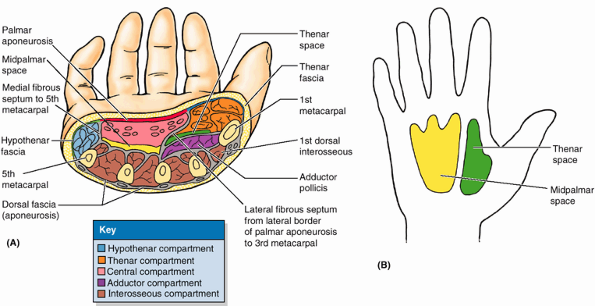 |
|
Figure 6.50. Compartments, spaces, and fascia of palm. A.
This transverse section through the middle of the palm illustrates the fascial compartments of the hand. The hypothenar fascia, attached to the lateral side of the 5th metacarpal, bounds the hypothenar compartment. Similarly, the thenar fascia, attached to the palmar aspect of the 1st metacarpal, bounds (with the metacarpal) the thenar compartment. The central compartment of the palm is covered by the palmar aponeurosis and separated from the thenar and hypothenar compartments by medial and lateral fibrous septa attaching to the 5th and 3rd metacarpals, respectively. The septum attached to the 3rd metacarpal also separates the midpalmar and thenar spaces The adductor compartment contains the adductor pollicis muscle. B. The midpalmar space underlies the central compartment of the palm and is related distally to the synovial tendon sheaths of the 3rd–5th digits and proximally to the common flexor sheath as it emerges from the carpal tunnel. The thenar space underlies the thenar compartment and is related distally to the synovial tendon sheath of the index finger and proximally to the common flexor sheath distal to the carpal tunnel. |
disease of the palmar fascia resulting in progressive shortening,
thickening, and fibrosis of the palmar fascia and aponeurosis. The
fibrous degeneration of the longitudinal bands of the palmar
aponeurosis on the medial side of the hand pulls the 4th and 5th
fingers into partial flexion at the metacarpophalangeal and proximal
interphalangeal joints (Fig. B6.28A).
The contracture is frequently bilateral and is seen in some men >50
years of age. Its cause is unknown, but evidence points to a hereditary
predisposition. The disease first manifests as painless nodular
thickenings of the palmar aponeurosis that adhere to the skin.
Gradually, progressive contracture of the longitudinal bands produces
raised ridges in the palmar skin that extend from the proximal part of
the hand to the base of the 4th and 5th fingers (Fig. B6.28B).
Treatment of Dupuytren contracture usually involves surgical excision
of all fibrotic parts of the palmar fascia to free the fingers (Salter, 1999).
resulting from hand infections usually appear on the dorsum of the
hand, where the fascia is thinner. The potential fascial spaces of the
palm are important because they may become infected. The fascial spaces
determine the extent and direction of the spread of pus formed by these
infections. Depending on the site of infection, pus will accumulate in
the thenar, hypothenar, or adductor compartments. Antibiotic therapy
has made infections that spread beyond one of these fascial
compartments rare; however, an untreated infection can spread
proximally through the carpal tunnel into the forearm, anterior to the
pronator quadratus and its fascia.
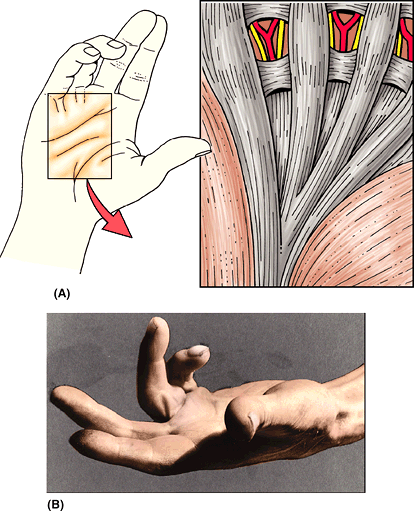 |
|
Figure B6.28. Dupuytren contracture.
|
-
Thenar muscles in the thenar compartment: abductor pollicis brevis, flexor pollicis brevis, and opponens pollicis.
-
Adductor pollicis in the adductor compartment.
-
Hypothenar muscles in the hypothenar compartment: abductor digiti minimi, flexor digiti minimi brevis, and opponens digiti minimi.
-
Short muscles of the hand, the lumbricals, are in the central compartment with the long flexor tendons.
-
The interossei lie in separate interosseous compartments between the metacarpals.
on the lateral surface of the palm and are chiefly responsible for
opposition of the thumb. Normal movement of the thumb is important for
the precise activities of the hand. The high degree of freedom of
movements of the thumb results from the 1st metacarpal being
independent, with mobile joints at both ends. Thus several muscles are
required to control its freedom of movement:
-
Extension: extensor pollicis longus, extensor pollicis brevis, and abductor pollicis longus.
-
Flexion: flexor pollicis longus and flexor pollicis brevis.
-
Abduction: abductor pollicis longus and abductor pollicis brevis.
-
Adduction: adductor pollicis and 1st dorsal interosseous.
-
Opposition:
opponens pollicis. This movement occurs at the carpometacarpal joint
and results in a “cupping” of the palm. Bringing the tip of the thumb
into contact with the 5th finger or any of the other fingers involves
considerably more movement than can be produced by the opponens
pollicis alone. This complex movement begins with the thumb in the
extended position and initially involves abduction and medial rotation
of the 1st metacarpal (cupping the palm) produced by the action of the
opponens pollicis at the carpometacarpal joint and then flexion at the
metacarpophalangeal joint (Fig. 6.51). The
reinforcing action of the adductor pollicis and FPL increases the
pressure that the opposed thumb can exert on the fingertips. In
pulp-to-pulp opposition, movements of the finger opposing the thumb are
also involved.
(APB), the short abductor of the thumb, forms the anterolateral part of
the thenar eminence. In addition to abducting the thumb, the APB
assists the opponens pollicis during the early stages of opposition by
rotating its proximal phalanx slightly medially.
tendon of the FPL, share (with each other and often with the APB) a
common, sesamoid-containing tendon at their distal attachment. The
bellies usually differ in their innervation: The larger superficial
head of the FPB is innervated by the recurrent branch of the median
nerve, whereas the smaller deep head is usually innervated by the deep
palmar branch of the ulnar nerve. The FPB flexes the thumb at the
carpometacarpal and metacarpophalangeal joints and aids in opposition
of the thumb.
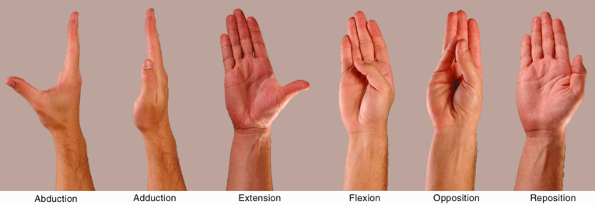 |
|
Figure 6.51. Movements of thumb.
The thumb is rotated 90° to the other digits. (This can be confirmed by noting the direction the nail of the thumb faces compared with the nails of the other fingers.) Thus abduction and adduction occur in a sagittal plane and flexion and extension occur in a coronal plane. Opposition, the action bringing the tip of the thumb in contact with the pads of the other fingers (e.g., with the little finger), is the most complex movement. The components of opposition are abduction and medial rotation at the carpometacarpal joint and flexion of the metacarpophalangeal joint. |
|
Table 6.11. Intrinsic Muscles of the Hand
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
flex the thumb against resistance. If acting normally, the muscle can
be seen and palpated; however, keep in mind that the FPL also flexes
the thumb.
The opponens pollicis opposes the thumb, the most important thumb
movement. It flexes and rotates the 1st metacarpal medially at the
carpometacarpal joint during opposition; this movement occurs when
picking up an object. During opposition, the tip of the thumb is
brought into contact with the pad of the little finger, as shown in Figure 6.51.
The adductor pollicis has two heads of origin, which are separated by
the radial artery as it enters the palm to form the deep palmar arch.
Its tendon usually contains a sesamoid bone. The adductor pollicis
adducts the thumb, moving the thumb to the palm of the hand (Fig. 6.51), thereby giving power to the grip (Fig. 6.48G & H).
on the medial side of the palm and move the little finger. These
muscles are in the hypothenar compartment with the 5th metacarpal (Figs. 6.50A and 6.52). The attachments, innervations, and main actions of the hypothenar muscles are summarized in Table 6.11.
is the most superficial of the three muscles forming the hypothenar
eminence. The abductor digiti minimi abducts the 5th finger and helps
flex its proximal phalanx.
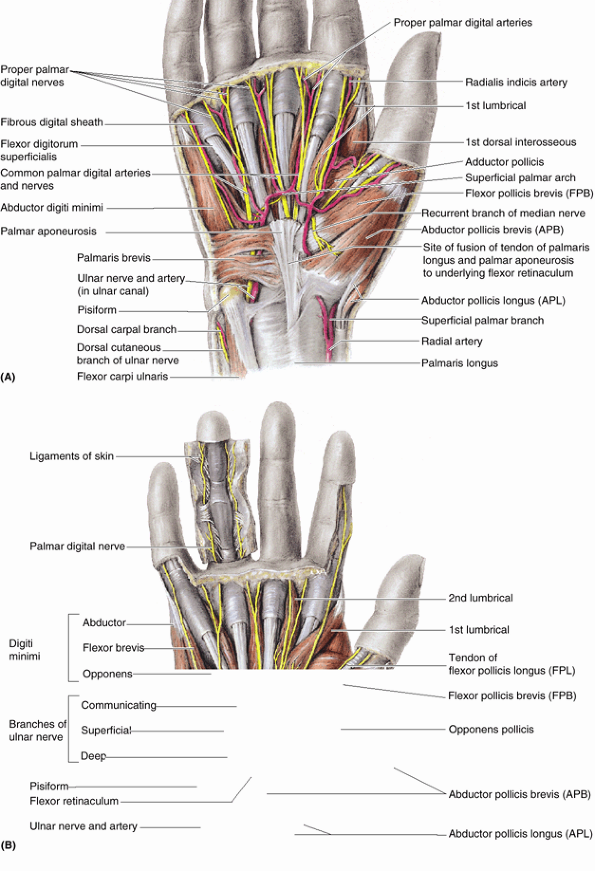 |
|
Figure 6.52. Superficial dissections of right palm.
The skin and subcutaneous tissue have been removed, as have most of the palmar aponeurosis and the thenar and hypothenar fasciae. A. The superficial palmar arch is located immediately deep to the palmar aponeurosis, superficial to the long flexor tendons. This arterial arch gives rise to the common palmar digital arteries. In the digits, a digital artery (e.g., radialis indicis) and nerve lie on the medial and lateral sides of the fibrous digital sheath. The pisiform bone protects the ulnar nerve and artery as they pass into the palm. B. Three thenar and three hypothenar muscles attach to the flexor retinaculum and to the four marginal carpal bones united by the retinaculum. |
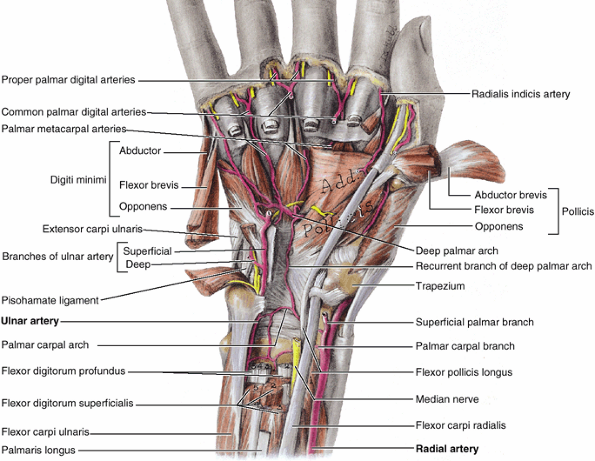 |
|
Figure 6.53. Muscles and arteries of distal forearm and deep palm.
This deep dissection of the palm reveals the anastomosis of the palmar carpal branch of the radial artery with the palmar carpal branch of the ulnar artery to form the palmar carpal arch, and the deep palmar arch. The deep palmar arch lies at the level of the bases of the metacarpal bones, 1.5–2 cm proximal to the superficial palmar arch. |
is variable in size; it lies lateral to the abductor digiti minimi. The
flexor digiti minimi brevis flexes the proximal phalanx of the 5th
finger at the metacarpophalangeal joint.
is a quadrangular muscle that lies deep to the abductor and flexor
muscles of the 5th finger. The opponens digiti minimi draws the 5th
metacarpal anteriorly and rotates it laterally, thereby deepening the
hollow of the palm and bringing the 5th finger into opposition with the
thumb (Fig. 6.51). Like the opponens pollicis, the opponens digiti minimi acts exclusively at the carpometacarpal joint.
it is not in the hypothenar compartment. The palmaris brevis wrinkles
the skin of the hypothenar eminence and deepens the hollow of the palm,
thereby aiding the palmar grip. The palmaris brevis covers and protects
the ulnar nerve and artery. It is attached proximally to the medial
border of the palmar aponeurosis and to the skin on the medial border
of the hand.
The 1st dorsal interosseous muscle is easy to palpate; oppose the thumb
firmly against the index finger and it can be easily felt. (Some
authors describe four palmar interossei; in so doing, they are
including the deep head of the FPB because of its similar innervation
and placement on the thumb; Table 6.11). The four dorsal interossei abduct the fingers, and the three palmar interossei adduct them. A mnemonic device is
to make acronyms of Dorsal ABduct (DAB) and Palmar ADuct
(PAD). Acting together, the dorsal and palmar interossei and the
lumbricals produce flexion at the metacarpophalangeal joints and
extension of the interphalangeal joints (the so-called Z-movement).
This occurs because of their attachment to the lateral bands of the
extensor expansions (Fig. 6.42B).
Understanding the Z-movement is useful because it is the opposite of
claw hand, which occurs in ulnar paralysis when the interossei and the
3rd and 4th lumbricals are incapable of acting together to produce the
Z-movement (see clinical correlation [blue] box “Ulnar Nerve Injury,” earlier in this chapter).
The flexor and digital sheaths enable the tendons to slide freely over
each other during movements of the fingers. Near the base of the
proximal phalanx, the tendon of FDS splits and surrounds the tendon of
FDP (Figs. 6.49B and 6.54B). The halves of the FDS tendon are attached to the margins of the anterior aspect of the base of the middle phalanx (Fig. 6.42D). The tendon of FDP, after passing through the split in the FDS tendon, the tendinous chiasm, passes distally to attach to the anterior aspect of the base of the distal phalanx.
The sheaths extend from the heads of the metacarpals to the bases of
the distal phalanges. These sheaths prevent the tendons from pulling
away from the digits (bowstringing). The fibrous digital sheaths
combine with the bones to form osseofibrous tunnels through which the tendons pass to reach the digits. The anular and cruciform parts (often referred to clinically as “pulleys”) are thickened reinforcements of the fibrous digital sheaths (Fig. 6.54B).
The tendon of the FPL passes deep to the flexor retinaculum to the
thumb within its own synovial sheath. At the head of the metacarpal,
the tendon runs between two sesamoid bones, one in the combined tendon of the FPB and APB and the other in the tendon of the adductor pollicis.
hand and fingers (grasping, pinching, pointing, etc.) are produced by
extrinsic muscles with fleshy bellies located distant from the hand
(near the elbow) and long tendons passing into the hand and fingers.
The shorter, more delicate and weaker movements (typing, playing
musical instruments, and writing) and positioning of the fingers for
the more powerful movements are accomplished largely by the intrinsic
muscles. The muscles and tendons of the hand are organized into five
fascial compartments: two radial compartments (thenar and adductor)
that serve the thumb; an ulnar (hypothenar) compartment that serves the
little finger; and two more central compartments that serve the medial
four fingers (a palmar one for the long flexor tendons and lumbricals,
and a deep one between the metacarpals for the interossei).
the highly mobile thumb. Indeed, when extrinsic muscles are also
considered, the thumb has eight muscles producing and controlling the
wide array of movements that distinguish the human hand. The interossei
produce multiple movements: the dorsal interossei (and abductors
pollicis and digiti minimi) abduct the fingers, whereas the palmar
interossei (and adductor pollicis) adduct them. Both movements occur at
the metacarpophalangeal joints. Acting together with the lumbricals,
the interossei flex the metacarpophalangeal and extend the
interphalangeal joints of the medial four fingers (the Z-movement).
can cause infection of the digital synovial sheaths. When inflammation
of the tendon and synovial sheath occurs (tenosynovitis),
the digit swells and movement becomes painful. Because the tendons of
the 2nd, 3rd, and 4th fingers nearly always have separate synovial
sheaths, the infection is usually confined to the infected finger. If
the infection is untreated, however, the proximal ends of these sheaths
may rupture, allowing the infection to spread to the midpalmar space (Fig. 6.51B). Because the synovial sheath of the little finger is usually continuous with the common flexor sheath (Fig. 6.54B),
tenosynovitis in this finger may spread to the common sheath and thus
through the palm and carpal tunnel to the anterior forearm, draining
into the space between the pronator quadratus and the overlying flexor
tendons (Parona space). Likewise,
tenosynovitis in the thumb may spread via the continuous synovial
sheath of the FPL (radial bursa). How far an infection spreads from the
fingers depends on variations in their connections with the common
flexor sheath.
sheath on the dorsum of the wrist. Excessive friction of these tendons
on their common sheath results in fibrous thickening of the sheath and
stenosis of the osseofibrous tunnel. The excessive friction is caused
by repetitive forceful use of the hands during gripping and wringing
(e.g., squeezing water out of clothes). This condition, called Quervain tenovaginitis stenosans,
causes pain in the wrist that radiates proximally to the forearm and
distally toward the thumb. Local tenderness is felt over the common
fibrous sheath on the lateral side of the wrist.
aspect of the digit produces stenosis of the osseofibrous tunnel, the
result of repetitive forceful use of the fingers. If the tendons of the
FDS and FDP enlarge proximal to the tunnel, the person is unable to
extend the finger. When the finger is extended passively, a snap is
audible. Flexion produces another snap as the thickened tendon moves.
This condition is called digital tenovaginitis stenosans (trigger finger or snapping finger).
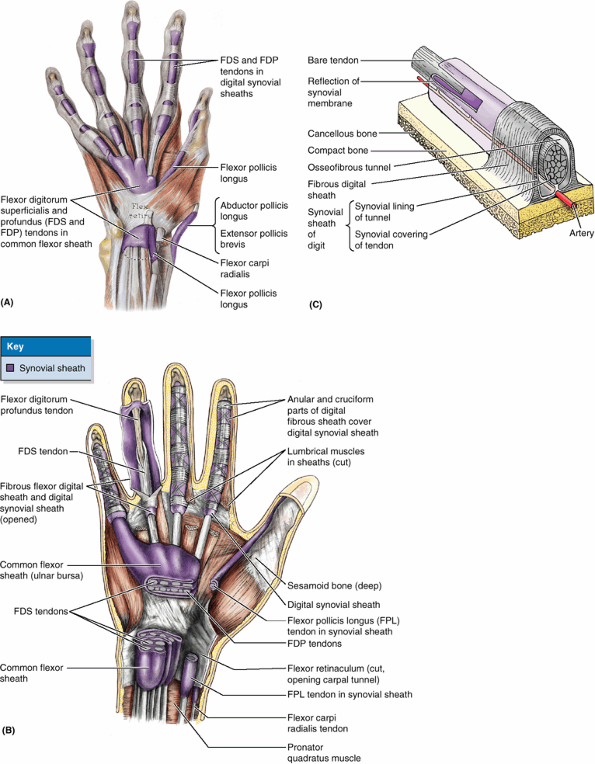 |
|
Figure 6.54. Flexor tendons, common flexor sheath, fibrous digital sheaths, and synovial sheaths of digits. A.
This dissection of the anterior aspect of the distal forearm and hand shows the synovial sheaths of the long flexor tendons to the digits. Observe the two sets: (1) proximal or carpal, posterior to the flexor retinaculum, and (2) distal or digital, within the fibrous sheaths of the digital flexors. B. This dissection of the palm illustrates the tendons and fibrous digital sheaths. The fibrous sheaths of the digits attach along the borders of the proximal and middle phalanges to capsules (palmar ligaments) of the interphalangeal joints and to the surface of the distal phalanx. C. The structure of an osseo-fibrous tunnel of a finger, containing a tendon, is shown. Within the fibrous sheath, the synovial sheath consists of the (parietal) synovial lining of the tunnel and the (visceral) synovial covering of the tendon. These layers of the synovial sheath are actually separated by only a capillary layer of synovial fluid, which lubricates the synovial surfaces to facilitate gliding of the tendon (see Introduction). |
in many different positions, often while grasping or applying pressure,
the hand is supplied with an abundance of highly branched and
anastomosing arteries so that oxygenated blood is generally available
to all parts in all positions. Furthermore, the arteries or their
derivatives are relatively superficial, underlying skin capable of
sweating, so that excess heat can be released. To prevent undesirable
heat loss in a cold environment, the arterioles of the hands are
capable of reducing blood flow to the surface and to the ends of the
fingers. The ulnar and radial arteries and their branches provide all
the blood to the hand. The arteries of the hand are illustrated and
their origins and courses are described in Table 6.12.
It enters the palm by passing between the heads of the 1st dorsal
interosseous muscle and then turns medially, passing between the heads
of the adductor pollicis. The radial artery ends by anastomosing with
the deep branch of the ulnar artery to form the deep palmar arch, which is formed mainly by the radial artery. This arch lies across the metacarpals just distal to their bases (Fig. 6.53). The deep palmar arch gives rise to three palmar metacarpal arteries and the princeps pollicis artery. The radialis indicis
artery passes along the lateral side of the index finger. It usually
arises from the radial artery, but it may originate from the princeps
pollicis.
arches are lacerated. It may not be sufficient to ligate only one
forearm artery when the arches are lacerated, because these vessels
usually have numerous communications in the forearm and hand and thus
bleed from both ends. To obtain a bloodless surgical operating field
for treating complicated hand injuries, it may be necessary to compress
the brachial artery and its branches proximal to the elbow (e.g., using
a pneumatic tourniquet). This procedure prevents blood from reaching
the ulnar and radial arteries through the anastomoses around the elbow.
marked by cyanosis and often accompanied by paresthesia and pain, is
characteristically brought on by cold and emotional stimuli. The
condition may result from an anatomical abnormality or an underlying
disease. When the cause of the condition is idiopathic (unknown) or
primary, it is called Raynaud syndrome
(disease). The arteries of the upper limb are innervated by sympathetic
nerves. Postsynaptic fibers from the sympathetic ganglia enter nerves
that form the brachial plexus and are distributed to the digital
arteries through branches arising from the plexus. When treating
ischemia resulting from Raynaud syndrome, it may be necessary to
perform a cervicodorsal presynaptic sympathectomy (excision of a segment of a sympathetic nerve) to dilate the digital arteries.
are provided in Table 6.13.
In addition, branches or communications from the lateral and posterior
cutaneous nerves may contribute some fibers that supply the skin of the
dorsum of the hand.
|
Table 6.12. Arteries of the Hand
|
|||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||
hand through the carpal tunnel, deep to the flexor retinaculum, along
with the nine tendons of the FDS, FDP, and FPL (Fig. 6.55). The carpal tunnel
is the passageway deep to the flexor retinaculum between the tubercles
of the scaphoid and trapezoid bones on the lateral side and the
pisiform and hook of the hamate on the medial side. Distal to the
carpal tunnel, the median nerve supplies two and a half thenar muscles
and the 1st and 2nd lumbricals (Table 6.13). It
also sends sensory fibers to the skin on the entire palmar surface, the
sides of the first three digits, the lateral half of the 4th digit, and
the dorsum of the distal halves of these digits. Note, however, that
the palmar cutaneous branch of the median nerve,
which supplies the central palm, arises proximal to the flexor
retinaculum and passes superficial to it (i.e., it does not pass
through the carpal tunnel).
the forearm and the wrist. The most common site is where the nerve
passes through the carpal tunnel.
or, more commonly, increases the size of some of the nine structures
(or their coverings) that pass through it (e.g., inflammation of
synovial sheaths). Fluid retention, infection, and excessive exercise
of the fingers may cause swelling of the tendons or their synovial
sheaths. The median nerve is the most sensitive structure in the carpal
tunnel (Fig. B6.29B–D) and therefore is the most affected. This nerve has two terminal sensory branches that supply the skin of the hand; hence, paresthesia (tingling), hypoesthesia (diminished sensation), or anesthesia
(absence of sensation) may occur in the lateral three and a half
digits. Recall, however, that the palmar cutaneous branch of the median
nerve arises proximal to and does not pass through the carpal tunnel;
thus sensation in the central palm remains unaffected. The nerve also
has one terminal motor branch, the recurrent branch, which serves the
three thenar muscles (Table 6.11).
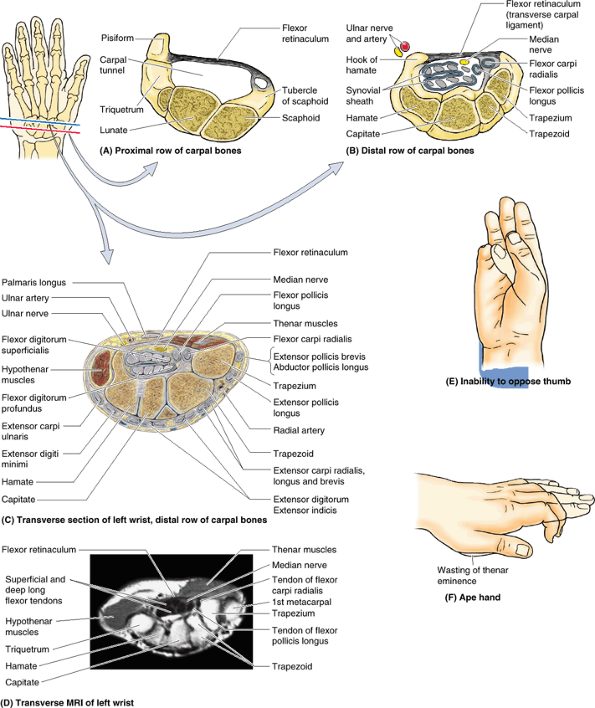 |
|
Figure B6.29
|
thumb (owing to weakness of the APB and opponens pollicis) may occur if
the cause of compression is not alleviated. Individuals with carpal
tunnel syndrome are unable to oppose the thumb (Fig. B6.29E)
and have difficulty buttoning a shirt or blouse as well as gripping
things such as a comb. As the condition progresses, sensory changes
radiate into the forearm and axilla. Symptoms of compression can be
reproduced by compression of the median nerve with your finger at the
wrist for approximately 30 s. To relieve both the compression and the
resulting symptoms, partial or complete surgical division of the flexor
retinaculum, a procedure called carpal tunnel release,
may be necessary. The incision for carpal tunnel release is made toward
the medial side of the wrist and flexor retinaculum to avoid possible
injury to the recurrent branch of the median nerve.
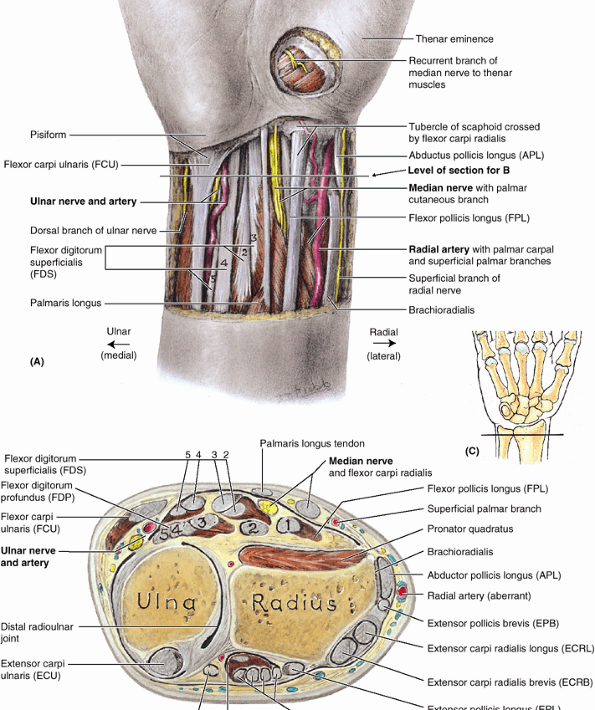 |
|
Figure 6.55. Structures in distal forearm (wrist region). A.
A distal skin incision was made along the transverse wrist crease, crossing the pisiform bone. The skin and fasciae are removed proximally, revealing the tendons and neurovascular structures. A circular incision and removal of the skin and thenar fascia reveals the recurrent branch of the median nerve to the thenar muscles, vulnerable to injury when this area is lacerated because of its subcutaneous location. B. This transverse section of the distal forearm demonstrates the long flexor and extensor tendons and neurovascular structures en route from forearm to hand. The ulnar nerve and artery are under cover of the flexor carpi ulnaris; therefore, the pulse of the artery cannot be easily detected here. C. Orientation drawing indicating the plane of the section shown in part B. |
|
Table 6.13. Nerves of the Hand
|
|||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||
because this nerve is relatively close to the surface. In attempted
suicides by wrist slashing, the median nerve is commonly injured just
proximal to the flexor retinaculum. This results in paralysis of the
thenar muscles and the first two lumbricals. Hence, opposition of the
thumb is not possible and fine control movements of the 2nd and 3rd
digits are impaired. Sensation is also lost over the thumb and adjacent
two and a half fingers.
of the thumb. Undoubtedly, injuries to the nerves supplying the
intrinsic muscles of the hand, especially the median nerve, have the
most severe effects on this complex movement. If the median nerve is
severed in the forearm or at the wrist, the thumb cannot be opposed;
however, the APL and adductor pollicis (supplied by the posterior
interosseous and ulnar nerves, respectively) may imitate opposition.
in the elbow region results in loss of flexion of the proximal and
distal interphalangeal joints of the 2nd and 3rd digits. The ability to
flex the metacarpophalangeal joints of these fingers is also affected
because digital branches of the median nerve supply the 1st and 2nd
lumbricals. Ape hand (Fig. B6.29F)
refers to a deformity in which thumb movements are limited to flexion
and extension of the thumb in the plane of the palm. This condition is
caused by the inability to oppose and by limited abduction of the
thumb. The recurrent branch of the median nerve to the thenar muscles (Fig. 6.55A)
lies subcutaneously and may be severed by relatively minor lacerations
of the thenar eminence. Severance of this nerve paralyzes the thenar
muscles and the thumb loses much of its usefulness.
Here the ulnar nerve is bound by fascia to the anterior surface of the
flexor retinaculum as it passes between the pisiform (medially) and the
ulnar artery (laterally). Just proximal to the wrist, the ulnar nerve
gives off a palmar cutaneous branch that passes superficial to the flexor retinaculum and palmar aponeurosis and supplies skin on the medial side of the palm (Table 6.13). The dorsal cutaneous branch of the ulnar nerve supplies the medial half of the dorsum of the hand, the 5th finger, and the medial half of the 4th finger (Fig. 6.55B). The ulnar nerve ends at the distal border of the flexor retinaculum by dividing into superficial and deep branches (Fig. 6.52B). The superficial branch of the ulnar nerve supplies cutaneous branches to the anterior surfaces of the medial one and a half fingers. The deep branch of the ulnar nerve
supplies the hypothenar muscles, the medial two lumbricals, the
adductor pollicis, the deep head of the FPB, and all the interossei.
The deep branch also supplies several joints (wrist, intercarpal,
carpometacarpal, and intermetacarpal). The ulnar nerve is often
referred to as the nerve of fine movements because it innervates most of the intrinsic muscles that are concerned with intricate hand movements (Table 6.13).
may occur at the wrist where it passes between the pisiform and the
hook of the hamate. The depression between these bones is converted by
the pisohamate ligament into an osseofibrous tunnel, the ulnar canal
(Guyon tunnel; Fig. 6.47B). Ulnar canal syndrome
is manifest by hypoesthesia in the medial one and a half fingers and
weakness of the intrinsic muscles of the hand. “Clawing” of the 4th and
5th fingers (hyperextension at the metacarpophalangeal joint with
flexion at the proximal interphalangeal joint) may occur, but—in
contradistinction to proximal ulnar nerve injury—their ability to flex
is unaffected and there is no radial deviation of the hand.
hands in an extended position against the hand grips put pressure on
the hooks of their hamates, which compresses their ulnar nerves. This
type of nerve compression, which has been called handlebar neuropathy, results in sensory loss on the medial side of the hand and weakness of the intrinsic hand muscles.
It pierces the deep fascia near the dorsum of the wrist to supply the
skin and fascia over the lateral two thirds of the dorsum of the hand,
the dorsum of the thumb, and proximal parts of the lateral one and a
half digits (Table 6.10).
hand, radial nerve injury in the arm can produce serious hand
disability. The characteristic handicap is inability to extend the
wrist resulting from paralysis of extensor muscles of the forearm, all of which are innervated by the radial nerve (Fig. 6.40B; Table 6.8). The hand is flexed at the wrist and lies flaccid, a condition known as wrist-drop (see clinical correlation [blue] box “Injury to the Radial Nerve in the Arm,”
earlier in this chapter). The fingers of the relaxed hand also remain
in the flexed position at the metacarpophalangeal joints. The
interphalangeal joints can be extended weakly through the action of the
intact lumbricals and interossei, which are supplied by the median and
ulnar nerves (Table 6.11). The radial nerve has
only a small area of exclusive cutaneous supply onthe hand. Thus the
extent of anesthesia is minimal, even in serious radial nerve injuries,
and is usually confined to a small area on the lateral part of the
dorsum of the hand.
anastomoses between both radial and ulnar vessels and palmar and dorsal
vessels. The arteries of the hand collectively constitute a
periarticular arterial anastomosis around the collective joints of the
wrist and hand. Thus blood is generally available to all parts of the
hand in all positions as well as while performing functions (gripping
or pressing) that might otherwise compromise especially the palmar
structures. The arteries to the digits are also characterized by their
ability to vasoconstrict during exposure to cold to conserve heat and
to dilate (while the hand becomes sweaty) to radiate excess heat.
the zones of cutaneous innervation and the roles of motor innervation
are well defined, as are functional deficits. In terms of intrinsic
structure, the radial nerve is only sensory via its superficial branch
to the dorsum of the hand. The median nerve is most important to the
function of the thumb and sensation from the lateral three and half
digits and adjacent palm, whereas the ulnar nerve supplies the
remainder. The intrinsic muscles of the hand constitute the T1 myotome.
not only the more sensitive and functional palmar aspect but also the
dorsal aspect of the distal part of the digits (nail beds). The
superficial dorsal venous network is commonly used for administering
intravenous fluids.
like other palpable pulses, is a peripheral reflection of cardiac
action. The radial pulse rate is measured where the radial artery lies
on the anterior surface of the distal end of the radius, lateral to the
FCR tendon, which serves as a guide to the artery (Fig. SA6.15).
Here the artery can be felt pulsating between the tendons of the FCR
and the APL and where it can be compressed against the radius. The tendons of FCR and palmaris longus
can be palpated anterior to the wrist, a little lateral to its middle,
and are usually observed by flexing the closed fist against resistance.
The palmaris longus tendon is smaller than the FCR tendon and is not
always present. The palmaris longus tendon serves as a guide to the
median nerve, which lies deep to it (Fig. 6.55B). The FCU tendon
can be palpated as it crosses the anterior aspect of the wrist near the
medial side and inserts into the pisiform. The FCU tendon serves as a
guide to the ulnar nerve and artery. The tendons of the FDS can be palpated as the fingers are alternately flexed and extended. The ulnar pulse is often difficult to palpate. The tendons of the APL and EPB indicate the anterior boundary of the anatomical snuff box (Fig. SA6.16). The tendon of the EPL
indicates the posterior boundary of the box. The radial artery crosses
the floor of the snuff box, where its pulsations may be felt. The scaphoid and, less distinctly, the trapezium are palpable in the floor of the snuff box.
loose when the hand is relaxed. Prove this by pinching and pulling
folds of your skin here. The looseness of the skin results from the
mobility of the subcutaneous tissue and from the relatively few fibrous
skin ligaments that are present. Hair is present in this region and on
the proximal parts of the digits, especially in men. If the dorsum of
the hand is examined with the wrist extended against resistance and the
digits abducted, the tendons of the extensor digitorum
to the fingers stand out, particularly in thin individuals. These
tendons are not visible far beyond the knuckles because they flatten
here to form the extensor expansions of the fingers (Fig. 6.42B). The knuckles that become visible when a fist is made are produced by the heads of the metacarpals.
Under the loose subcutaneous tissue and extensor tendons on the dorsum
of the hand, the metacarpals can be palpated. A prominent feature of
the dorsum of the hand is the dorsal venous network (Fig. 6.12A).
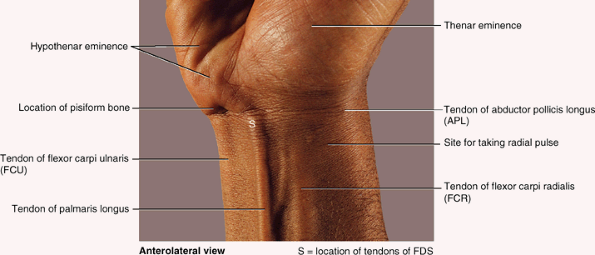 |
|
Figure SA6.15
|
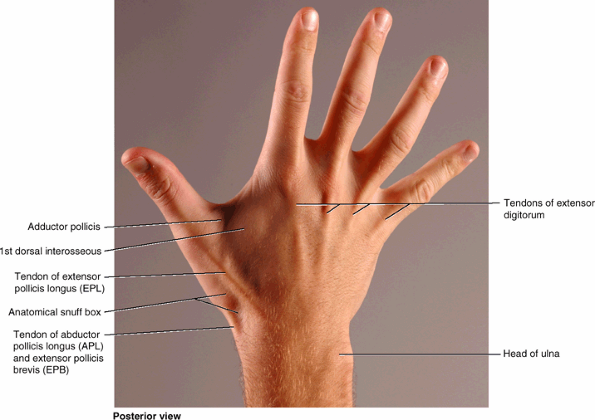 |
|
Figure SA6.16
|
lies across the center of the palm, level with the distal border of the
fully extended thumb. The main part of the arch ends at the thenar eminence. The deep palmar arch lies approximately 1 cm proximal to the superficial palmar arch. The palmar skin presents several more or less constant flexion creases, where the skin is firmly bound to the deep fascia, that help locate palmar wounds and underlying structures:
-
Wrist creases, proximal, middle, distal: The distal wrist crease indicates the proximal border of the flexor retinaculum.
-
Palmar creases, transverse, longitudinal:
The longitudinal creases deepen when the thumb is opposed; the
transverse creases deepen when the metacarpophalangeal joints are
flexed.-
Radial longitudinal crease (the “life line” of palmistry): partially encircles the thenar eminence, formed by the short muscles of the thumb.
-
Proximal (transverse) palmar crease:
commences on the lateral border of the palm, superficial to the head of
the 2nd metacarpal; extends medially and slightly proximally across the
palm, superficial to the bodies of the 3rd–5th metacarpals.
-
-
Distal (transverse) palmar crease:
begins at or near the cleft between the index and the middle fingers;
crosses the palm with a slight convexity, superficial to the head of
the 3rd metacarpal and then proximal to the heads of the 4th and 5th
metacarpals.
-
Proximal digital crease: located at the root of the finger, approximately 2 cm distal to the metacarpophalangeal joint.
-
Middle digital crease: lies over the proximal interphalangeal joint.
-
Distal digital crease: lies over or just proximal to the distal interphalangeal joint.
creases. The proximal digital crease of the thumb crosses obliquely, at
or proximal to the 1st metacarpophalangeal joint. The skin ridges on the pads of the digits, forming the fingerprints,
are used for identification because of their unique patterns. The
physiological function of the skin ridges is to reduce slippage when
grasping objects.
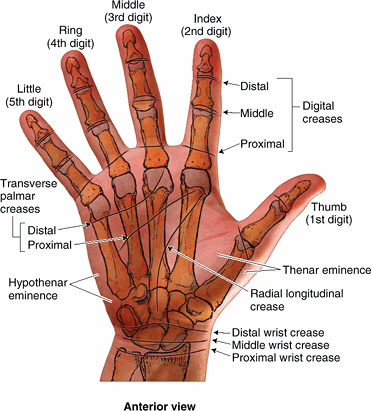 |
|
Figure SA6.17
|
is a valuable extension of the conventional physical examination of
people with certain congenital anomalies and genetic diseases (Nussbaum et al., 2004).
For example, people with trisomy 21 (Down syndrome) have
dermatoglyphics that are highly characteristic. In addition, they often
have a single transverse palmar crease (simian crease); however,
approximately 1% of the general population has this crease with no
other clinical features of the syndrome.
should be kept in mind when examining wounds of the palm and when
making palmar incisions. Furthermore, it is important to know that the
superficial palmar arch is at the same level as the distal extremity of
the common flexor sheath (Figs. 6.52 and 6.54).
As mentioned previously, incisions or wounds along the medial surface
of the thenar eminence may injure the recurrent branch of the median
nerve to the thenar muscles (see clinical correlation [blue] box “Trauma to the Median Nerve,” earlier in this chapter).
usually all moving simultaneously. Functional defects in any of the
joints impair movements of the pectoral girdle. Mobility of the scapula
is essential for free movement of the upper limb. The clavicle forms a
strut that holds the scapula, and hence the glenohumeral joint, away
from the thorax so it can move freely. The clavicle establishes the
radius at which the shoulder (half of the pectoral girdle and
glenohumeral joint) rotates at the SC joint. The 15–20° of movement at
the AC joint permits positioning of the glenoid cavity that is
necessary for arm movements.
both scapulothoracic (movement of the scapula on the thoracic wall) and
glenohumeral movements must be considered. Although the initial 30° of
abduction may occur without scapular motion, in the overall movement of
fully elevating the arm, the movement occurs in a 2:1 ratio: For every
3° of elevation, approximately 2° occurs at the glenohumeral joint and
1° at the physiological scapulothoracic joint. In other words, when the
upper limb has been elevated so that the arm is vertical at the side of
the head (180° of arm abduction or flexion), 120° occurred at the
glenohumeral joint and 60° occurred at the scapulothoracic joint. This
is known as scapulohumeral rhythm. The important movements of the pectoral girdle are scapular movements (Table 6.3):
elevation and depression, protraction (lateral or forward movement of
the scapula) and retraction (medial or backward movement of the
scapula), and rotation of the scapula.
is a saddle type of synovial joint but functions as a ball-and-socket
joint. The SC joint is divided into two compartments by an articular disc. The disc is firmly attached to the anterior and posterior sternoclavicular ligaments, thickenings of the fibrous layer of the joint capsule, as well as the interclavicular ligament.
The great strength of the SC joint is a consequence of these
attachments. Thus, although the articular disc serves as a shock
absorber of forces transmitted along the clavicle from the upper limb,
dislocation of the clavicle is rare, whereas fracture of the clavicle
is common. The SC joint is the only articulation between the upper limb
and the axial skeleton, and it can be readily palpated because the
sternal end of the clavicle lies superior to the manubrium of the
sternum.
manubrium and the 1st costal cartilage. The articular surfaces are
covered with fibrocartilage.
the SC joint, including the epiphysis at the sternal end of the
clavicle. It is attached to the margins of the articular surfaces,
including the periphery of the articular disc. A synovial membrane lines the internal surface of the fibrous layer of the joint capsule, extending to the edges of the articular surfaces.
strengthens the capsule superiorly. It extends from the sternal end of
one clavicle to the sternal end of the other clavicle. In between, it
is also attached to the superior border of the manubrium. The costoclavicular ligament
anchors the inferior surface of the sternal end of the clavicle to the
1st rib and its costal cartilage, limiting elevation of the pectoral
girdle.
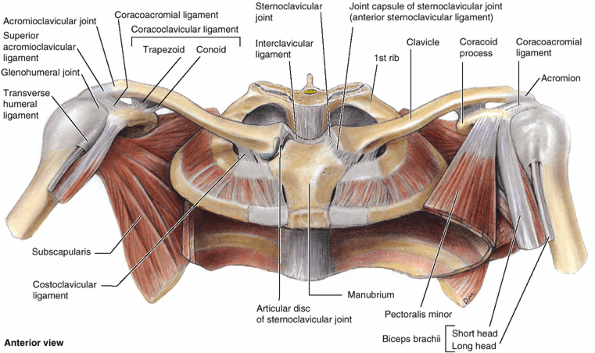 |
|
Figure 6.56. Pectoral girdle and associated tendons and ligaments.
The pectoral (shoulder) girdle is a partial bony ring (incomplete posteriorly) formed by the manubrium of the sternum, the clavicle, and the scapulae. Joints associated with these bones are the sternoclavicular, acromioclavicular, and glenohumeral (shoulder). The girdle provides for attachment of the superior appendicular skeleton to the axial skeleton and provides the mobile base from which the upper limb operates. |
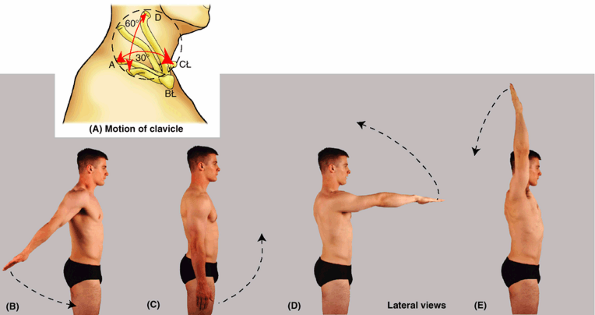 |
|
Figure 6.57. Movements of upper limb at joints of pectoral girdle. A. Range of motion of lateral end of clavicle permitted by movements at the sternoclavicular joint. A↔C = protraction/retraction; A↔D = elevation/depression. B–E. Circumduction of upper limb requires coordinated movements of the pectoral girdle and glenohumeral joint. B. Beginning with extended limb, retracted girdle; C. Neutral position. D. Flexed limb, protracted girdle; E. Elevated limb and girdle.
|
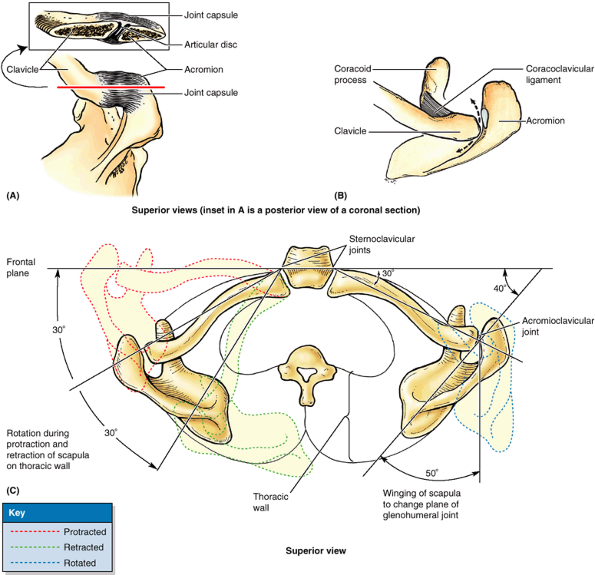 |
|
Figure 6.58. Acromioclavicular and sternoclavicular joints. A. This view of the right AC joint shows the joint capsule and partial disc (inset). B.
The function of the coracoclavicular ligament is demonstrated. As long as this ligament is intact with the clavicle tethered to the coronoid process, the acromion cannot be driven inferior to the clavicle. The ligament, however, does permit protraction and retraction of the acromion. C. Clavicular movements at the SC and AC joints permit protraction and retraction of the scapula on the thoracic wall (red and green lines) and winging of the scapula (blue line). Movements of a similar scale occur during elevation, depression, and rotation of the scapula. The latter movements are shown in Table 6.3, which also indicate the muscles specifically responsible for these movements. |
accompanied by rotation of the clavicle around its longitudinal axis.
The SC joint can also be moved anteriorly or posteriorly over a range
of up to 25–30°. Although not a typical movement, except perhaps during
calisthenics, it is capable of performing these movements sequentially,
moving the acromial end along a circular path—a form of circumduction.
strength, which depends on its ligaments, its disc, and the way forces
are generally transmitted along the clavicle. When a blow is received
to the acromion of the scapula, or when a force is transmitted to the
pectoral girdle during a fall on the outstretched hand, the force of
the blow is usually transmitted along the length of the clavicle, i.e.,
along its long axis. The clavicle may fracture near the junction of its
middle and lateral thirds, but it is rare for the SC joint to
dislocate. Most dislocations of the SC joint in persons < 25 years
of age result from fractures through the epiphysial plate because the
epiphysis at the sternal end of the clavicle does not close until 23–25
years of age.
(stiffening or fixation) of the joint occurs, or is necessary
surgically, a section of the center of the clavicle is removed,
creating a pseudojoint or “flail” joint to permit scapular movement.
(AC joint) is a plane type of synovial joint, which is located 2–3 cm
from the “point” of the shoulder formed by the lateral part of the
acromion (Figs. 6.56 and 6.58).
acromion of the scapula. The articular surfaces, covered with
fibrocartilage, are separated by an incomplete wedge-shaped articular disc.
is a strong pair of bands that unite the coracoid process of the
scapula to the clavicle, anchoring the clavicle to the coracoid
process. The coracoclavicular ligament consists of two ligaments, the
conoid and trapezoid ligaments, which are often separated by a bursa. The vertical conoid ligament is an inverted triangle (cone), which has its apex inferiorly where it is attached to the root of the coracoid process. Its wide attachment (base of the triangle) is to the conoid tubercle on the inferior surface of the clavicle. The nearly horizontal trapezoid ligament
is attached to the superior surface of the coracoid process and extends
laterally to the trapezoid line on the inferior surface of the
clavicle. In addition to augmenting the AC joint, the coracoclavicular
ligament provides the means by which the scapula and free limb are
(passively) suspended from the clavicular strut.
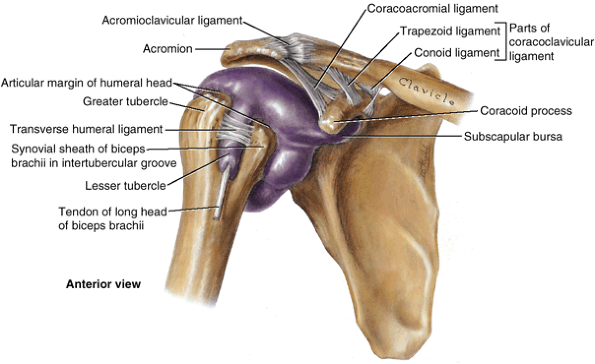 |
|
Figure 6.59. Glenohumeral joint.
The extent of the synovial membrane of the glenohumeral (shoulder) joint is demonstrated in this specimen in which the articular cavity has been injected with blue latex and the fibrous layer of the joint capsule has been removed. The articular cavity has two extensions: one where it forms a synovial sheath for the tendon of the long head of the biceps brachii in the intertubercular groove of the humerus, and the other inferior to the coracoid process where it is continuous with the subscapular bursa between the subscapularis tendon and the margin of the glenoid cavity. The joint capsule and intrinsic ligaments of the AC joint are also demonstrated. |
of the clavicle. These movements are associated with motion at the
physiological scapulothoracic joint (Figs. 6.57 and 6.58; Table 6.3).
No muscles connect the articulating bones to move the AC joint; the
axioappendicular muscles that attach to and move the scapula cause the
acromion to move on the clavicle.
articular branches of the nerves supplying the muscles that act on the
joint), the lateral pectoral and axillary nerves supply the AC joint (Table 6.5).
However, consistent with the joint’s subcutaneous location and the fact
that no muscles connect the articulating bones, innervation is also
provided to the AC joint by the subcutaneous lateral supraclavicular
nerve, an occurrence more typical of the distal limb.
to result from a hard fall on the shoulder or on the outstretched upper
limb. Dislocation of the AC joint can also occur when a hockey player
is driven into the boards or when a person receives a severe blow to
the superolateral part of the back. An AC joint dislocation, often
called a “shoulder separation,” is severe when both the AC and the
coracoclavicular ligaments are torn. When the coracoclavicular ligament
tears, the shoulder separates from the clavicle and falls because of
the weight of the upper limb. Rupture of the coracoclavicular ligament
allows the fibrous layer of the joint capsule to be torn so that the
acromion can pass inferior to the acromial end of the clavicle.
Dislocation of the AC joint makes the acromion more prominent, and the
clavicle may move superior to this process.
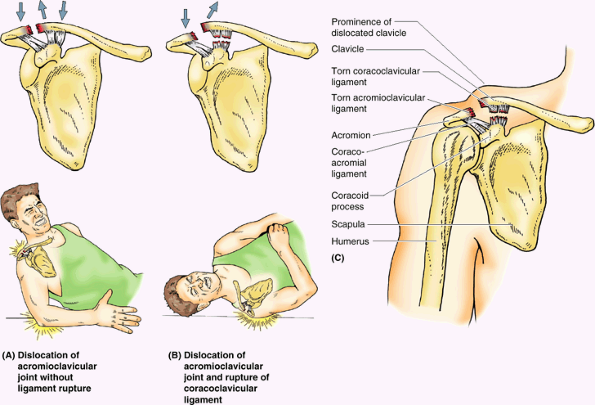 |
|
Figure B6.30
|
is a ball-and-socket type of synovial joint that permits a wide range
of movement; however, its mobility makes the joint relatively unstable.
(L. lip). Both articular surfaces are covered with hyaline cartilage.
The glenoid cavity accepts little more than a third of the humeral
head, which is
held
in the cavity by the tonus of the musculotendinous rotator cuff, or
SITS, muscles (supraspinatus, infraspinatus, teres minor, and
subscapularis) (Table 6.2).
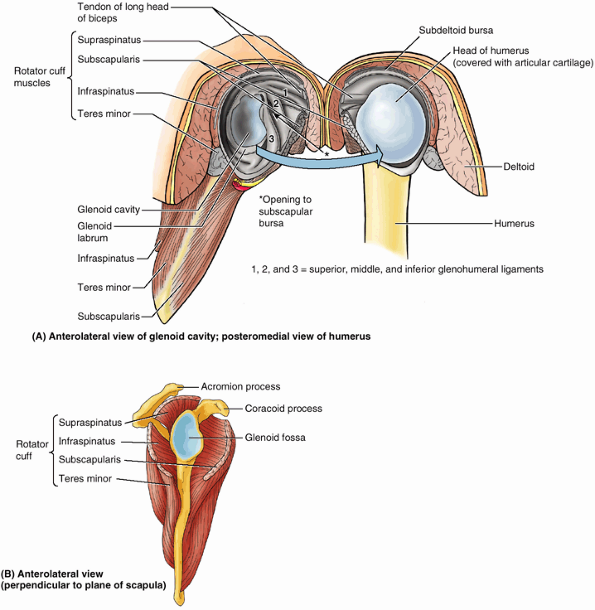 |
|
Figure 6.60. Rotator cuff and glenohumeral joint. A.
In this dissection of the glenohumeral joint, the joint capsule was sectioned and the joint opened from its posterior aspect as if it were a book. Four short SITS muscles (supraspinatus, infraspinatus, teres minor, and subscapularis) cross and surround the joint, blending with its capsule. The anterior, internal surface demonstrates the glenohumeral ligaments, which were incised to open the joint. B. The SITS muscles of the left rotator cuff are shown as they relate to the scapula and its glenoid cavity. The prime function of these muscles and the musculotendinous rotator cuff is to hold the relatively large head of the humerus in the much smaller and shallow glenoid cavity of the scapula. |
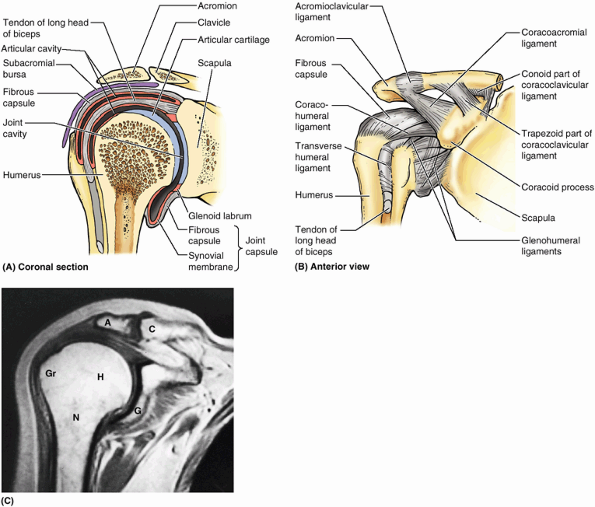 |
|
Figure 6.61. Capsules and ligaments of glenohumeral and acromioclavicular joints. A. The bones, articular surfaces, joint capsule, cavity of the joints, the subacromial bursa are shown. B.
The acromioclavicular, coracohumeral, and glenohumeral ligaments are demonstrated. Although shown on the external aspect of the joint capsule, the glenohumeral ligaments are actually a feature observed from the internal aspect of the joint (as in Fig. 6.60A). These ligaments strengthen the anterior aspect of the capsule of the glenohumeral joint, and the coracohumeral ligament strengthens the capsule superiorly. C. This coronal MRI shows the right glenohumeral and AC joints. A, acromion; C, clavicle; G, glenoid cavity; Gr, greater tubercle of humerus; H, head of humerus; N, surgical neck of humerus. (Courtesy of Dr. W. Kucharczyk, Chair of Medical Imaging and Clinical Director of Tri-Hospital Resonance Centre, Toronto, Ontario, Canada.) |
the glenohumeral joint and is attached medially to the margin of the
glenoid cavity and laterally to the anatomical neck of the humerus (Fig. 6.61A & B).
Superiorly, this part of the joint capsule encroaches on the root of
the coracoid process so that the fibrous layer of the joint capsule
encloses the proximal attachment of the long head of the biceps brachii
to the supraglenoid tubercle of scapula within the joint. The joint
capsule has two apertures: (1) an opening between the tubercles of the
humerus for passage of the tendon of the long head of the biceps
brachii (Fig. 6.59) and (2) an opening situated anteriorly, inferior to the coracoid process that allows communication between the subscapular bursa
and the synovial cavity of the joint. The inferior part of the joint
capsule, the only part not reinforced by the rotator cuff muscles, is
its weakest area. Here the capsule is particularly lax and lies in
folds when the arm is adducted; however, it becomes taut when the arm
is abducted.
the internal surface of the fibrous layer of the joint capsule and
reflects from it onto the glenoid labrum and the humerus, as far as the
articular margin of the head (Figs. 6.59, 6.60A, and 6.61).
The synovial membrane also forms a tubular sheath for the tendon of the
long head of the biceps brachii, where it lies in the intertubercular
groove of the humerus and passes into the joint cavity, extending as
far as the surgical neck of the humerus (Fig. 6.59).
ligament, which strengthens the capsule superiorly, are intrinsic
ligaments—that is, part of the fibrous layer of the joint capsule (Figs. 6.60A and 6.61B). The glenohumeral ligaments
are three fibrous bands, evident only on the internal aspect of the
capsule, that reinforce the anterior part of the joint capsule. These
ligaments radiate laterally and inferiorly from the glenoid labrum at
the supraglenoid tubercle of the scapula and blend distally with the
fibrous layer of the capsule as it attaches to the anatomical neck of
the humerus. The coracohumeral ligament is
a strong broad band that passes from the base of the coracoid process
to the anterior aspect of the greater tubercle of the humerus (Fig. 6.61B). The transverse humeral ligament
is a broad fibrous band that runs more or less obliquely from the
greater to the lesser tubercle of the humerus, bridging over the
intertubercular groove (Figs. 6.59 and 6.62B).
The ligament converts the groove into a canal, which holds the synovial
sheath and tendon of the biceps brachii in place during movements of
the glenohumeral joint.
This osseo-ligamentous structure forms a protective arch that overlies
the humeral head, preventing its superior displacement from the glenoid
cavity. The coracoacromial arch is so strong that a forceful superior
thrust of the humerus will not fracture it; the humeral shaft or
clavicle fractures first. Transmitting force superiorly along the
humerus (e.g., when standing at a desk and partly supporting the body
with the outstretched limbs), the humeral head presses against the
coracoacromial arch. The supraspinatus muscle passes under this arch
and lies deep to the deltoid as its tendon blends with the joint
capsule of the glenohumeral joint as part of the rotator cuff (Fig. 6.60A & B).
Movement of the supraspinatus tendon, passing to the greater tubercle
of the humerus, is facilitated as it passes under the arch by the subacromial bursa (Fig. 6.61A), which lies between the arch superiorly and the tendon and tubercle inferiorly.
any other joint in the body. This freedom results from the laxity of
its joint capsule and the large size of the humeral head compared with
the small size of the glenoid cavity. The glenohumeral joint allows
movements around three axes and permits flexion–extension,
abduction–adduction, rotation (medial and lateral) of the humerus, and
circumduction. Lateral rotation of the humerus increases the range of
abduction. When the arm is abducted without rotation, available
articular surface is exhausted and the greater tubercle contacts the coracoacromial arch,
preventing further abduction. If the arm is then laterally rotated
180°, the tubercles are rotated posteriorly and more articular surface
becomes available to continue elevation. Circumduction at the glenohumeral joint is an orderly sequence of flexion, abduction, extension, and adduction—or the reverse (Fig. 6.57).
Unless performed over a small range, these movements do not occur at
the glenohumeral joint in isolation; they are accompanied by movements
at the two other joints of the pectoral girdle (SC and AC). Stiffening
or fixation of the joints of the pectoral girdle (ankylosis) results in a much more restricted range of movement, even if the glenohumeral joint is normal.
Other muscles that serve the glenohumeral joint as shunt muscles,
acting to resist dislocation without producing movement at the joint
(e.g., when carrying a heavy suitcase), or that maintain the large head
of the humerus in the relatively shallow glenoid cavity are also listed.
(secreted by the synovial membrane) are situated near the glenohumeral
joint. Bursae are located where tendons rub against bone, ligaments, or
other tendons and where skin moves over a bony prominence. The bursae
around the glenohumeral joint are of special clinical importance
because some of them communicate with the articular (joint) cavity
(e.g., the subscapular bursa). Consequently, opening a bursa may mean
entering the cavity of the glenohumeral joint.
The bursa protects the tendon where it passes inferior to the root of
the coracoid process and over the neck of the scapula. It usually
communicates with the cavity of the glenohumeral joint through an
opening in the fibrous layer of the joint capsule (Fig. 6.60A); thus it is really an extension of the glenohumeral joint cavity.
is located between the acromion, coracoacromial ligament and deltoid
superiorly and the supraspinatus tendon and joint capsule of the
glenohumeral joint inferiorly (Fig. 6.61A).
Thus it facilitates movement of the supraspinatus tendon under the
coracoacromial arch and of the deltoid over the joint capsule of the
glenohumeral joint and the greater tubercle of the humerus. Its size
varies, but it does not normally communicate with the cavity of the
glenohumeral joint.
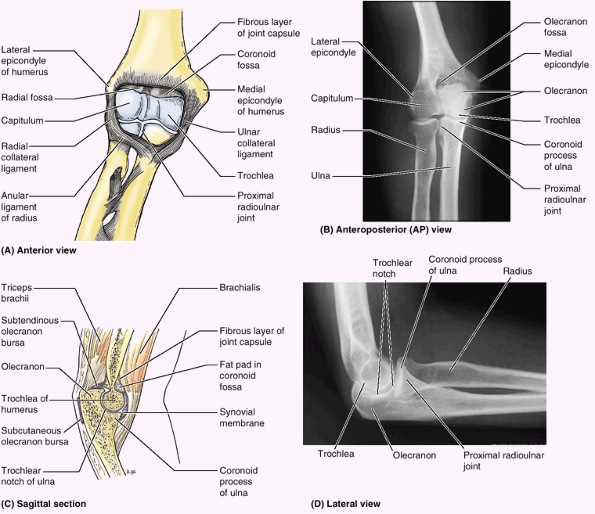 |
|
Figure 6.62. Elbow and proximal radioulnar joints. A.
The thin anterior aspect of the joint capsule has been removed to reveal the articulating surfaces of the bones inside. The strong collateral ligaments were left intact. B. This anteroposterior radiograph shows the extended elbow joint. C. The fibrous layer and synovial membrane of the joint capsule, the subtendinous and subcutaneous olecranon bursae, and humeroulnar articulation of the elbow joint are demonstrated. D. This lateral radiograph shows the flexed elbow joint. (Parts B and D courtesy of Dr. E. Becker, Associate Professor of Medical Imaging, University of Toronto, Toronto, Ontario, Canada.) |
result in pain, tenderness, and limitation of movement of the
glenohumeral joint. This condition is also known as calcific scapulohumeral bursitis.
Deposition of calcium in the supraspinatus tendon is common. This
causes increased local pressure that often causes excruciating pain
during abduction of the arm; the pain may radiate as far as the hand.
The calcium deposit may irritate the overlying subacromial bursa,
producing an inflammatory reaction known as subacromial bursitis.
As long as the glenohumeral joint is adducted, no pain usually results
because in this position the painful lesion is away from the inferior
surface of the acromion. In most people, the pain occurs during 50–130°
of abduction (painful arc syndrome) because
during this arc the supraspinatus tendon is in intimate contact with
the inferior surface of the acromion. The pain usually develops in
males 50 years of age and older after unusual or excessive use of the
glenohumeral joint.
|
Table 6.14 Movements of the Glenohumeral (Shoulder) Joint
|
|||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
during repetitive use of the upper limb above the horizontal (e.g.,
during throwing and racquet sports, swimming, and weightlifting).
Recurrent inflammation of the rotator cuff, especially the relatively
avascular area of the supraspinatus tendon, is a common cause of
shoulder pain and results in tears of the musculotendinous rotator
cuff. Repetitive use of the rotator cuff muscles (e.g., by baseball
pitchers) may allow the humeral head and rotator cuff to impinge on the
coracoacromial arch, producing irritation of the arch and inflammation
of the rotator cuff. As a result, degenerative tendonitis of the rotator cuff develops. Attrition of the supraspinatus tendon also occurs (Fig. B6.31).
the person is asked to lower the fully abducted limb slowly and
smoothly. From approximately 90° abduction, the limb will suddenly drop
to the side in an uncontrolled manner if the rotator cuff (especially
the supraspinatus part) is diseased and/or torn.
strain of the muscles, for example, when an older person strains to
lift something, such as a window sash that is stuck, a previously
degenerated musculotendinous rotator cuff may rupture. A fall on the
shoulder may also tear a previously degenerated rotator cuff. Often the
intracapsular part of the tendon of the long head of the biceps brachii
becomes frayed (even worn away) leaving it adherent to the
intertubercular groove. As a result, shoulder stiffness occurs. Because
they fuse, the integrity of the fibrous layer of the joint capsule of
the glenohumeral joint is usually compromised when the rotator cuff is
injured. As a result, the articular cavity communicates with the
subacromial bursa. Because the supraspinatus muscle is no longer
functional with a complete tear of the rotator cuff, the person cannot
initiate abduction of the upper limb. If the arm is passively abducted
15° or more, the person can usually maintain or continue the abduction
using the deltoid.
glenohumeral joint is commonly dislocated by direct or indirect injury.
Because the presence of the coracoacromial arch and the support of the
rotator cuff are effective in preventing upward dislocation, most
dislocations of the humeral head occur in the downward (inferior)
direction. However, they are described clinically as anterior or (more
rarely) posterior dislocations, indicating whether the humeral head has
descended anterior or posterior to the infraglenoid tubercle and the
long head of the triceps. The head ends up lying anterior or posterior
to the glenoid cavity.
occurs most often in young adults, particularly athletes. It is usually
caused by excessive extension and lateral rotation of the humerus (Fig. B6.32).
The head of the humerus is driven inferoanteriorly, and the fibrous
layer of the joint capsule and glenoid labrum may be stripped from the
anterior aspect of the glenoid cavity in the process. A hard blow to
the humerus when the glenohumeral joint is fully abducted tilts the
head of the humerus inferiorly onto the inferior weak part of the joint
capsule. This may tear the capsule and dislocate the shoulder so that
the humeral head comes to lie inferior to the glenoid cavity and
anterior to the infraglenoid tubercle. The strong flexor and adductor
muscles of the glenohumeral joint usually subsequently pull the humeral
head anterosuperiorly into a subcoracoid position. Unable to use the
arm, the person commonly supports it with the other hand. Inferior dislocation of the glenohumeral joint
often occurs after an avulsion fracture of the greater tubercle, owing
to the absence of the upward and medial pull produced by the muscles
attaching to the tubercle.
joint dislocates because of its close relation to the inferior part of
the joint capsule of this joint. The subglenoid displacement of the
head of the humerus into the quadrangular space damages the axillary
nerve. Axillary nerve injury is indicated by paralysis of the deltoid
(manifest as an inability to abduct the arm to or above the horizontal
level) and loss of sensation in a small area of skin covering the
central part of the deltoid.
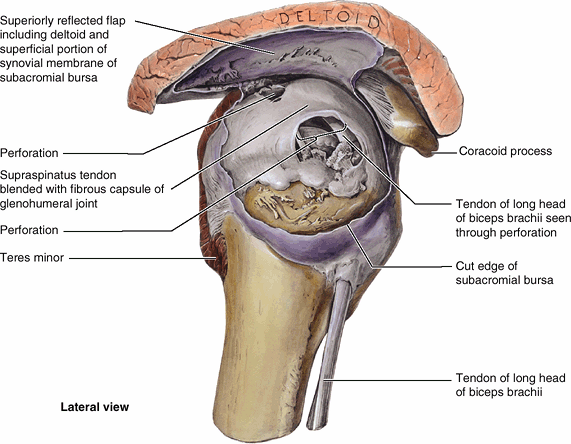 |
|
Figure B6.31. Attrition of the supraspinatus tendon.
|
commonly occurs in athletes who throw a baseball or football and in
those who have shoulder instability and subluxation (partial
dislocation) of the glenohumeral joint. The tear often results from
sudden contraction of the biceps or forceful subluxation of the humeral
head over the glenoid labrum. Usually a tear occurs in the
anterosuperior part of the labrum. The typical symptom is pain while
throwing, especially during the acceleration phase, but a sense of
popping or snapping may be felt in the glenohumeral joint during
abduction and lateral rotation of the arm.
joint capsule of the glenohumeral joint, rotator cuff, subacromial
bursa, and deltoid usually cause adhesive capsulitis
(“frozen shoulder”), a condition seen in individuals 40–60 years of
age. A person with this condition has difficulty abducting the arm and
can obtain an apparent abduction of up to 45° by elevating and rotating
the scapula. Because of the lack of movement of the glenohumeral joint,
strain is placed on the AC joint, which may be painful during other
movements (e.g., elevation, or shrugging, of the shoulder). Injuries
that may initiate acute capsulitis are glenohumeral dislocations,
calcific supraspinatus tendinitis, partial tearing of the rotator cuff,
and bicipital tendinitis (Salter, 1999).
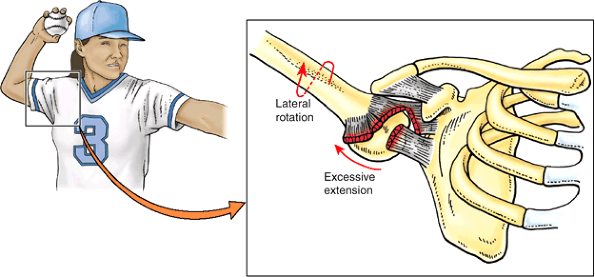 |
|
Figure B6.32. Dislocation of glenohumeral joint.
|
glenohumeral joint in positioning the upper limb. The SC joint links
the appendicular skeleton to the axial skeleton. The SC and AC joints
enable the movement at the physiological scapulothoracic joint, where
approximately 1° of movement occurs for every 3° of arm movement
(scapulohumeral rhythm). In turn, approximately two thirds of the
movement at the scapulothoracic joint result from motion at the SC
joint, and one third is from motion at the AC joint. The strength and
integrity of the joints of the shoulder complex do not depend on
congruity of the articular surfaces. The integrity of the SC and AC
joints results from intrinsic and extrinsic ligaments and the SC
articular disc, whereas that of the glenohumeral joint is maintained by
the tonic and active contraction of the muscles acting across it,
particularly the SITS (rotator cuff) muscles.
respectively; therefore, there are humeroulnar and humeroradial
articulations. The articular surfaces, covered with hyaline cartilage,
are most fully congruent (in contact) when the forearm is in a position
midway between pronation and supination and is flexed to a right angle.
It is attached to the humerus at the margins of the lateral and medial
ends of the articular surfaces of the capitulum and trochlea.
Anteriorly and posteriorly it is carried superiorly, proximal to the
coronoid and olecranon fossae. The synovial membrane
lines the internal surface of the fibrous layer of the capsule and the
intracapsular non-articular parts of the humerus. It is also continuous
inferiorly with the synovial membrane of the proximal radioulnar joint.
The joint capsule is weak anteriorly and posteriorly but is
strengthened on each side by collateral ligaments.
triangular bands that are medial and lateral thickenings of the fibrous
layer of the joint capsule (Figs. 6.62A and 6.63). The lateral, fan-like radial collateral ligament extends from the lateral epicondyle of the humerus and blends distally with the anular ligament of the radius,
which encircles and holds the head of the radius in the radial notch of
the ulna, forming the proximal radioulnar joint and permitting
pronation and supination of the forearm. The medial, triangular ulnar collateral ligament
extends from the medial epicondyle of the humerus to the coronoid
process and olecranon of the ulna and consists of three bands: (1) the anterior cord-like band is the strongest, (2) the posterior fan-like band is the weakest, and (3) the slender oblique band deepens the socket for the trochlea of the humerus.
axis of the fully extended ulna makes an angle of approximately 170°
with the long axis of the humerus. This angle, called the carrying angle (Fig. 6.64),
is named for the way the forearm angles away from the body when
something is carried, such as a pail of water. The obliquity of the
ulna and thus of the carrying angle is more pronounced (the angle is
approximately 10° more acute) in women than in men. It is
teleologically said to enable the swinging limbs to clear the wide
female pelvis when walking. In the anatomical position, the elbow is
against the waist. The carrying angle disappears when the forearm is
pronated.
forearm and hand, most of which have some potential to affect elbow
movement. In turn, their function and efficiency in the other movements
they produce are affected by elbow position. However, the chief flexors of the elbow joint are the brachialis and biceps brachii (Fig. 6.65).
The brachioradialis can produce rapid flexion in the absence of
resistance (even when the chief flexors are paralyzed). Normally, in
the presence
of resistance, the brachioradialis and pronator teres assist the chief flexors in producing slower flexion. The chief extensor of the elbow joint is the triceps brachii, especially the medial head, weakly assisted by the anconeus.
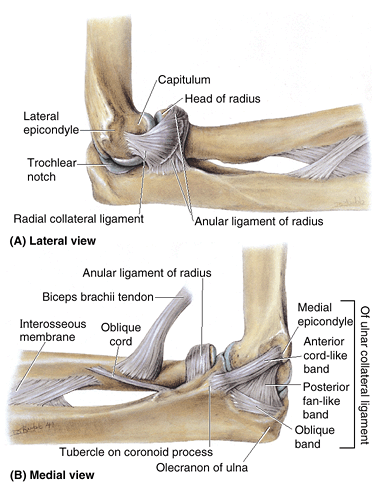 |
|
Figure 6.63. Collateral ligaments of elbow joint A.
The fan-like radial collateral is attached to the anular ligament of the radius, but its superficial fibers continue on to the ulna. B. The ulnar collateral ligament has a strong, round, cord-like anterior band (part), which is taut when the elbow joint is extended, and a weak, fan-like posterior band, which is taut when the joint is flexed. The oblique fibers merely deepen the socket for the trochlea of the humerus. |
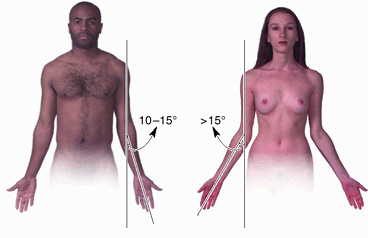 |
|
Figure 6.64. Carrying angle of elbow joint.
This angle is made by the axes of the arm and forearm when the elbow is fully extended. Note that the forearm diverges laterally, forming an angle that is greater in the woman. Teleologically, this is said to allow for clearance of the wider female pelvis as the limbs swing during walking; however, no significant difference exists regarding the function of the elbow. |
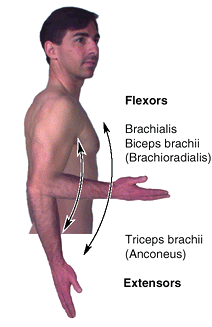 |
|
Figure 6.65. Flexor and extensor muscles of elbow joint.
During slow flexion or maintenance of flexion against gravity, the brachialis and biceps brachii are mainly involved. With increasing speed, the brachioradialis becomes involved. In the absence of resistance, the brachioradialis can flex the elbow when the other flexors are paralyzed. The triceps brachii is the main extensor of the forearm at the elbow joint. The anconeus muscle and gravity assist the triceps in extending the elbow joint. |
-
Intratendinous olecranon bursa, which is sometimes present in the tendon of triceps brachii.
-
Subtendinous olecranon bursa, which is located between the olecranon and the triceps tendon, just proximal to its attachment to the olecranon.
-
Subcutaneous olecranon bursa, which is located in the subcutaneous connective tissue over the olecranon.
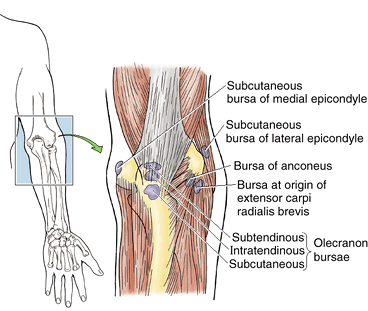 |
|
Figure 6.66. Bursae around elbow joint.
Of the several bursae around the elbow joint, the olecranon bursae are most important clinically. Trauma of these bursae may produce bursitis (inflammation of the bursae). |
 |
|
Figure B6.33
|
during falls on the elbow and to infection from abrasions of the skin
covering the olecranon. Repeated excessive pressure and friction, as
occurs in wrestling, for example, may cause this bursa to become
inflamed, producing a friction subcutaneous olecranon bursitis (e.g., “student’s elbow”) (Fig. B6.33).
This type of bursitis is also known as “dart thrower’s elbow” and
“miner’s elbow.” Occasionally, the bursa becomes infected and the area
over the bursa becomes inflamed.
is much less common. It results from excessive friction between the
triceps tendon and olecranon, for example, resulting from repeated
flexion–extension of the forearm as occurs during certain assembly-line
jobs. The pain is most severe during flexion of the forearm because of
pressure exerted on the inflamed subtendinous olecranon bursa by the
triceps tendon.
results in pain when the forearm is pronated because this action
compresses the bicipitoradial bursa against the anterior half of the
tuberosity of the radius.
from a fall that causes severe abduction of the extended elbow, an
abnormal movement of this articulation. The resulting traction on the
ulnar collateral ligament pulls the medial epicondyle distally (Fig. B6.34).
The anatomical basis of avulsion of the epicondyle is that the
epiphysis for the medial epicondyle may not fuse with the distal end of
the humerus until up to age 20. Usually fusion is complete
radiographically at age 14 in females and age 16 in males. Traction injury of the ulnar nerve
is a frequent complication of the abduction type of avulsion of the
medial epicondyle. The anatomical basis for this stretching of the
ulnar nerve is that it passes posterior to the medial epicondyle before
entering the forearm.
may occur when children fall on their hands with their elbows flexed.
Dislocations of the elbow may result from hyperextension or a blow that
drives the ulna posterior or posterolateral (Anderson et al., 2000).
The distal end of the humerus is driven through the weak anterior part
of the fibrous layer of the joint capsule as the radius and ulna
dislocate posteriorly (Fig. B6.35). The ulnar
collateral ligament is often torn, and an associated fracture of the
head of the radius, coronoid process, or olecranon process of the ulna
may occur. Injury to the ulnar nerve may occur, resulting in numbness
of the little finger and weakness of flexion and adduction of the wrist.
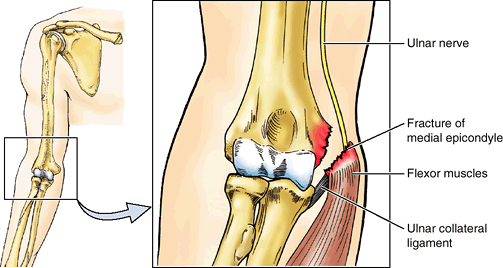 |
|
Figure B6.34
|
 |
|
Figure B6.35 Dislocation of elbow.
|
lines the deep surface of the fibrous layer and non-articulating
aspects of the bones. The synovial membrane is an inferior prolongation
of the synovial membrane of the elbow joint.
attached to the ulna anterior and posterior to its radial notch,
surrounds the articulating bony surfaces and forms a collar that, with
the radial notch, creates a ring that completely encircles the head of
the radius (Figs. 6.67, 6.68 and 6.69). The deep surface of the anular ligament is lined with synovial membrane, which continues distally as a sacciform recess of the proximal radioulnar joint
on the neck of the radius. This arrangement allows the radius to rotate
within the anular ligament without binding, stretching, or tearing the
synovial membrane.
of the radius rotates within the collar formed by the anular ligament
and the radial notch of the ulna. Supination turns the palm anteriorly, or superiorly when the forearm is flexed (Figs. 6.37A & C, 6.68 and 6.70). Pronation
turns the palm posteriorly, or inferiorly when the forearm is flexed.
The axis for these movements passes proximally through the center of
the head of the radius and distally through the site of attachment of
the apex of the articular disc to the head (styloid process) of the
ulna. During pronation and supination, it is the radius that rotates;
its head rotates within the cup-shaped collar formed by the anular
ligament and the radial notch on the ulna. Distally, the end of the
radius rotates around the head of the ulna. Almost always, supination
and pronation are accompanied by synergistic movements of the
glenohumeral and elbow joints that produce simultaneous movement of the
ulna, except when the elbow is flexed.
the supinator (when resistance is absent) and biceps brachii (when
power is required because of resistance), with some assistance from the
EPL and ECRL (Fig. 6.68C). Pronation
is produced by the pronator quadratus (primarily) and pronator teres
(secondarily), with some assistance from the FCR, palmaris longus, and
brachioradialis (when the forearm is in the midpronated position).
radial and recurrent interosseous arteries, respectively) (Fig. 6.34; Table 6.9).
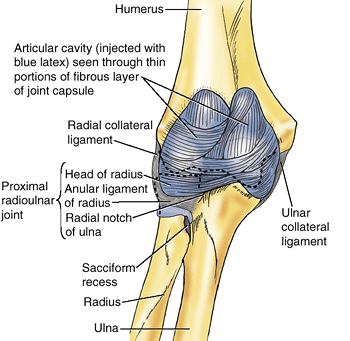 |
|
Figure 6.67. Proximal radioulnar joint The anular ligament attaches to the radial notch of the ulna, forming a collar around the head of the radius (Fig. 6.68A),
creating a pivot type of synovial joint. The articular cavity of the joint is continuous with that of the elbow joint, as demonstrated by the blue latex injected into that space and seen through the thin parts of the fibrous layer of the capsule. |
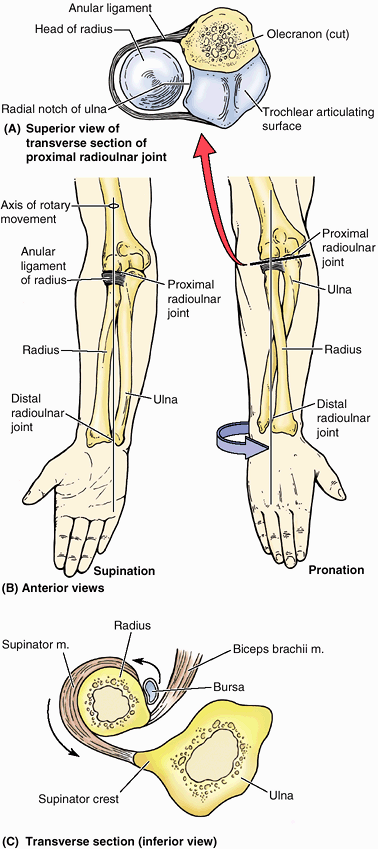 |
|
Figure 6.68. Supination and pronation of forearm. A. The head of the radius rotates in the “socket” formed by the anular ligament and radial notch of the ulna. B.
Supination is the movement of the forearm that rotates the radius laterally around its longitudinal axis so that the dorsum of the hand faces posteriorly and the palm faces anteriorly. Pronation is the movement of the forearm that rotates the radius medially around its longitudinal axis so that the palm of the hand faces posteriorly and its dorsum faces anteriorly (Fig. 6.77). C. The actions of the biceps brachii and supinator in producing supination from the pronated position at the radioulnar joints are shown. |
musculocutaneous, median, and radial nerves. Pronation is essentially a
function of the median nerve, whereas supination is a function of the
musculocutaneous and radial nerves.
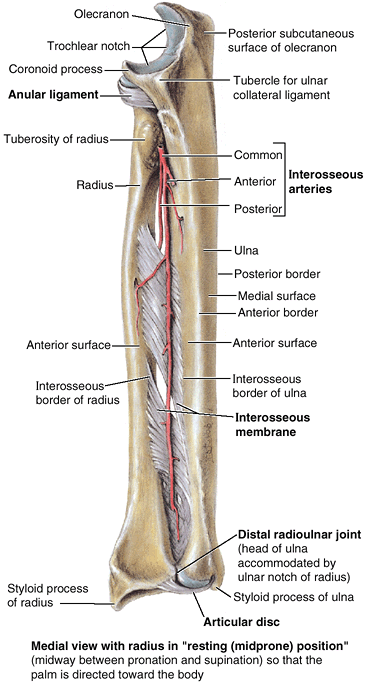 |
|
Figure 6.69. Radioulnar ligaments and interosseous arteries.
The ligament of the proximal radioulnar joint is the anular ligament. The ligament of the distal radioulnar joint is the articular disc. The interosseous membrane connects the interosseous margins of the radius and ulna, forming the radioulnar syndesmosis. The general direction of the fibers of the interosseous membrane is such that a superior thrust to the hand is received by the radius and is transmitted to the ulna. |
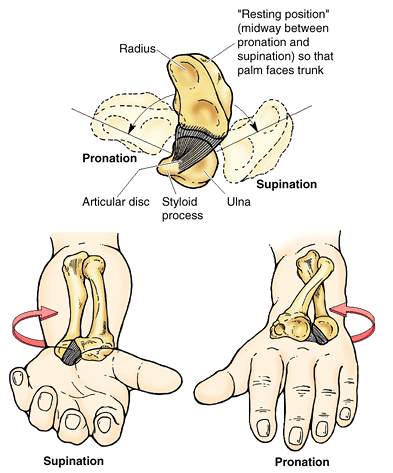 |
|
Figure 6.70. Movements of distal radioulnar joint during supination and pronation of forearm.
The distal radioulnar joint is the pivot type of synovial joint between the head of the ulna and the ulnar notch of the radius. The inferior end of the radius moves around the relatively fixed end of the ulna during supination and pronation of the hand. The two bones are firmly united distally by the articular disc, referred to clinically as the triangular ligament of the distal radioulnar joint. It has a broad attachment to the radius but a narrow attachment to the styloid process of the ulna, which serves as the pivot point for the rotary movement. |
to transient subluxation (incomplete temporary dislocation) of the head
of the radius (also called “nursemaid’s elbow” and “pulled elbow”). The
history of these cases is typical. The child is suddenly lifted
(jerked) by the upper limb while the forearm is pronated (e.g., lifting
a child into a bus) (Fig. B6.36). The child may
cry out, refuse to use the limb, protects the limb by holding it with
the elbow flexed and the forearm pronated. The sudden pulling of the
upper limb tears the distal attachment of the anular ligament, where it
is loosely attached to the neck of the radius. The radial head then
moves distally, partially out of the anular ligament. The proximal part
of the torn ligament may become trapped between the head of the radius
and the capitulum of the humerus. The source of pain is the pinched
anular ligament. Treatment of the subluxation consists of supination of
the child’s forearm while the elbow is flexed (Salter, 1999). The tear in the anular ligament soon heals when the limb is placed in a sling for 2 weeks.
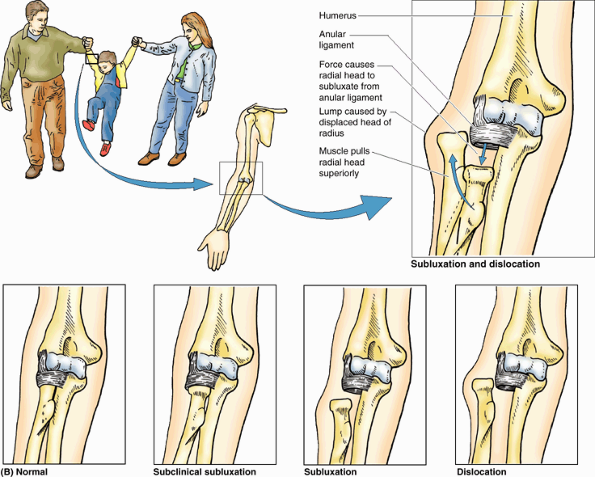 |
|
Figure B6.36
|
notch on the medial side of the distal end of the radius. A
fibrocartilaginous articular disc of the distal radioulnar joint
(sometimes referred to by clinicians as the “triangular ligament”)
binds the ends of the ulna and radius together and is the main uniting
structure of the joint (Figs. 6.70, 6.71 and 6.72B).
The base of the articular disc is attached to the medial edge of the
ulnar notch of the radius, and its apex is attached to the lateral side
of the base of the styloid process of the ulna. The proximal surface of
this triangular disc articulates with the distal aspect of the head of
the ulna. Hence, the joint cavity is L-shaped in a coronal section; the
vertical bar of the L is between the radius and the ulna, and the horizontal bar is between the ulna and the articular disc (Figs. 6.71B & C and 6.72A).
The articular disc separates the cavity of the distal radioulnar joint from the cavity of the wrist joint.
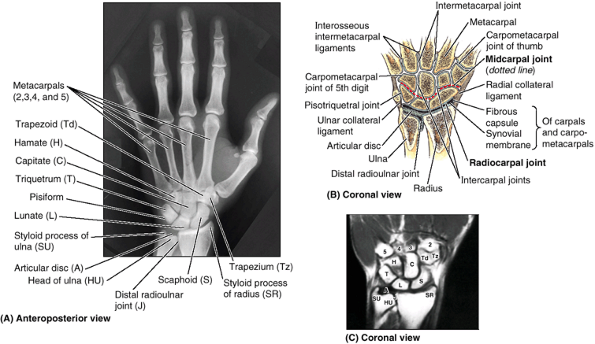 |
|
Figure 6.71. Bones of wrist and hand. A.
In radiographs of the wrist and hand the “joint space” at the distal end of the ulna appears wide because of the radiolucent articular disc. (Courtesy of Dr. E. L. Lansdown, Professor of Medical Imaging, University of Toronto, Toronto, Ontario, Canada.) B. This coronal section of the right hand demonstrates the distal radioulnar, wrist, intercarpal, carpometacarpal, and intermetacarpal joints. Although they appear to be continuous when viewed radiographically in parts A and C, the articular cavities of the distal radioulnar and wrist joints are separated by the articular disc of the distal radioulnar joint. C. This coronal MRI shows the wrist. Structures are identified in part A. (Courtesy of Dr. W. Kucharczyk, Chair of Medical Imaging and Clinical Director of Tri-Hospital Magnetic Resonance Centre, Toronto, Ontario, Canada.) |
This redundancy of the synovial capsule accommodates the twisting of
the capsule that occurs when the distal end of the radius travels
around the relatively fixed distal end of the ulna during pronation of
the forearm.
layer of the joint capsule of the distal radioulnar joint. These
relatively weak transverse bands extend from the radius to the ulna
across the anterior and posterior surfaces of the joint.
of the radius moves (rotates) anteriorly and medially, crossing over
the ulna anteriorly (Fig. 6.70). During
supination, the radius uncrosses from the ulna, its distal end moving
(rotating) laterally and posteriorly so the bones become parallel.
primary function as a hinge joint, the fact that it involves the
articulation of a single bone proximally with two bones distally, one
of which rotates, confers surprising complexity on this compound
(three-part) joint. The hinge movement, the ability to transmit forces,
and the high degree of stability of the joint primarily result from the
conformation of the articular surfaces of the humeroulnar joint (i.e.,
of the trochlear notch of the ulna to the trochlea of the humerus). The
integrity and functions of the humeroradial joint–proximal radioulnar
joint complex depends primarily on the combined radial collateral and
anular ligaments. The combined synovial proximal and distal radioulnar
joints plus the interosseous membrane enable pronation and supination
of the forearm. The anular ligament of the proximal joint, articular
disc of the distal joint, and interosseous membrane not only hold the
two bones together while permitting the necessary motion between them,
but they (especially the membrane) also transmit forces received from
the hand by the radius to the ulna for subsequent transmission to the
humerus and pectoral girdle.
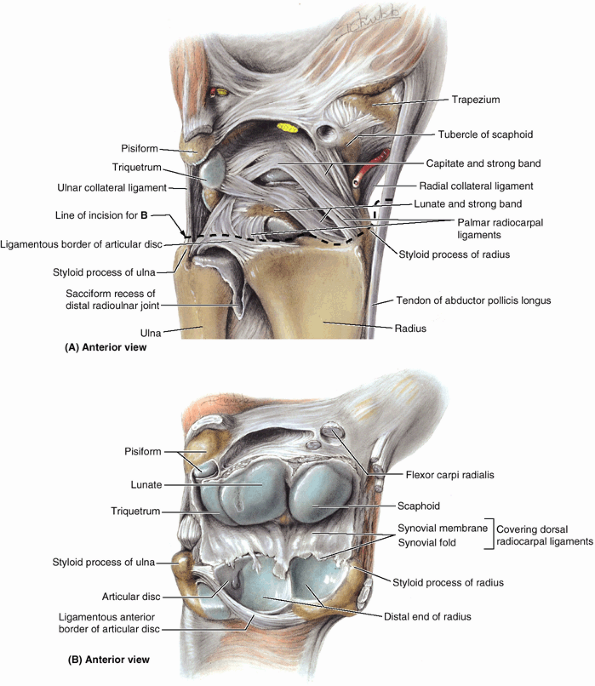 |
|
Figure 6.72. Dissection of distal radioulnar, radiocarpal, and intercarpal joints. A.
The ligaments of these joints are shown. The hand is forcibly extended but the joint is intact. Observe the palmar radiocarpal ligaments, passing from the radius to the two rows of carpal bones. These strong ligaments are directed so that the hand follows the radius during supination. B. The joint is opened anteriorly, with the dorsal radiocarpal ligaments serving as a hinge. Observe the nearly equal proximal articular surfaces of the scaphoid and lunate and that the lunate articulates with both the radius and the articular disc. Only during adduction of the wrist does the triquetrum articulate with the disc. |
the proximal segment of the hand, is a complex of eight carpal bones,
articulating proximally with the forearm via the wrist joint and
distally with the five metacarpals. The wrist (radiocarpal) joint
is a condyloid (ellipsoid) type of synovial joint. The position of the
joint is indicated approximately by a line joining the styloid
processes of the radius and ulna, or by the proximal wrist crease (Figs. 6.71, 6.72A & B, and SA6.17).
distal end of the radius and the articular disc of the distal
radioulnar joint articulate with the proximal row of carpal bones,
except for the pisiform. The latter bone acts primarily as a sesamoid
bone, increasing the leverage of the FCU. It lies in a plane anterior
to the other carpal bones, articulating with only the triquetrum.
surrounds the wrist joint and is attached to the distal ends of the
radius and ulna and the proximal row of carpals (scaphoid, lunate, and
triquetrum). The synovial membrane lines the internal surface of the fibrous layer of the joint capsule and is attached to the margins of the articular surfaces (Fig. 6.72B). Numerous synovial folds are present.
take the same direction so that the hand follows the radius during
pronation of the forearm. The joint capsule is also strengthened
medially by the ulnar collateral ligament, which is attached to the ulnar styloid process and triquetrum (Figs. 6.71B and 6.72A). The joint capsule is also strengthened laterally by the radial collateral ligament, which is attached to the radial styloid process and scaphoid.
The movements are flexion–extension, abduction–adduction (radial
deviation–ulnar deviation), and circumduction. The hand can be flexed
on the forearm more than it can be extended; these movements are
accompanied (actually, are initiated) by similar movements at the
midcarpal joint between the proximal and the distal rows of carpal
bones. Adduction of the hand is greater than abduction (Fig. 6.73B).
Most adduction occurs at the wrist joint. Abduction from the neutral
position occurs at the midcarpal joint. Circumduction of the hand
consists of successive flexion, adduction, extension, and abduction.
“carpi” muscles of the forearm, the tendons of which extend along the
four corners of the wrist (comparing a cross-section of the wrist to a
rectangle [Fig. 6.73C]) to attach to the bases of the metacarpals. The FCU does so via the pisohamate ligament, a continuation of the FCU tendon if the pisiform is considered a sesamoid bone within the continuous tendon.
-
Flexion of the wrist is produced by the FCR and FCU, with assistance from the flexors of the fingers and thumb, the palmaris longus and the APL.
-
Extension of the wrist is produced by the ECRL, ECRB, and ECU, with assistance from the extensors of the fingers and thumb.
-
Abduction of the wrist
is produced by the APL, FCR, ECRL, and ECRB; it is limited to
approximately 15° because of the projecting radial styloid process. -
Adduction of the wrist is produced by simultaneous contraction of the ECU and FCU.
however, tight grip (clenching of the fist) requires extension at the
wrist. The mildly extended position is also the most stable and the
“resting position.”
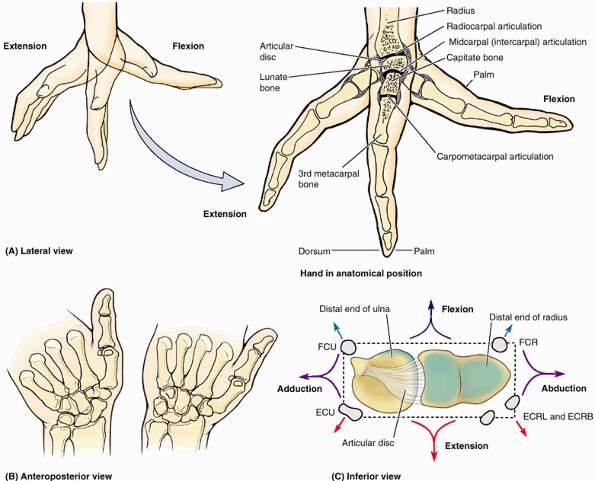 |
|
Figure 6.73. Movements of wrist. A.
In this sagittal section of the wrist and hand during extension and flexion, observe the radiocarpal, midcarpal, and carpometacarpal articulations. Most movement occurs at the radiocarpal joint, with additional movement taking place at the midcarpal joint during full flexion and extension. B. Movement at the radiocarpal and midcarpal joints during adduction and abduction is demonstrated as seen in posteroanterior radiography. C. This view of the proximal articular surface of the radiocarpal joint indicates the position of the tendons of the primary (“carpi”) muscles acting at the (“four corners” of the) joint and the movements produced by their combined activity. The carpi muscles include the flexor carpi ulnaris (FCU), extensor carpi ulnaris (ECU), flexor carpi radialis (FCR), extensor carpi radialis longus (ECRL), and extensor carpi radialis brevis (ECRB). |
the most common fracture in people >50 years of age, is discussed in
the clinical correlation (blue) box “Fractures of the Radius and Ulna,”
earlier in this chapter. Fracture of the scaphoid,
relatively common in young adults, is discussed in the clinical
correlation (blue) box “Fracture of the Scaphoid,” earlier in this
chapter.
The lunate is pushed out of its place in the floor of the carpal tunnel
toward the palmar surface of the wrist. The displaced lunate may
compress the median nerve and lead to carpal tunnel syndrome (discussed earlier in this chapter). Because of its poor blood supply, avascular necrosis of the lunate may occur. In some cases, excision of the lunate may be required. In degenerative joint disease of the wrist, surgical fusion of carpals (arthrodesis) may be necessary to relieve the severe pain.
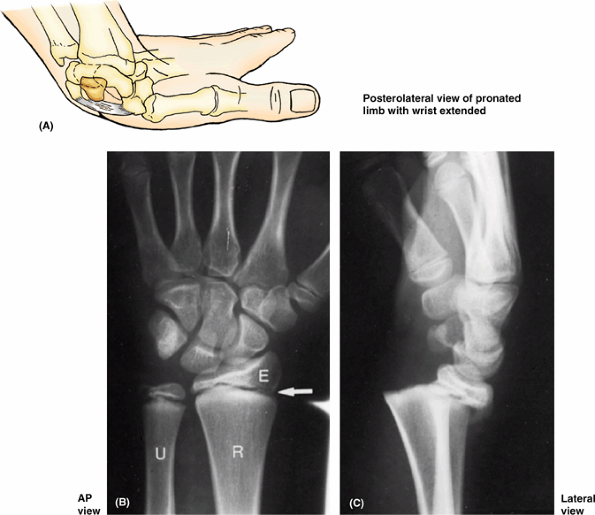 |
|
Figure B6.37. Wrist fractures. A. Dislocation of lunate is shown. B. This radiograph of a young person shows a normal epiphyseal plate (arrow). E, distal radial epiphysis (R); U, ulna. C. A fracture-separation of the distal radial epiphysis is shown.
|
A small fracture of the shaft of the radius is also visible (not
obvious). When the epiphysis is placed in its normal position during
reduction, the prognosis for normal bone growth is good.
-
Joints between the carpal bones of the proximal row.
-
Joints between the carpal bones of the distal row.
-
The midcarpal joint, a complex joint between the proximal and distal rows of carpal bones.
-
The pisotriquetral joint, formed from the articulation of the pisiform with the palmar surface of the triquetrum.
carpometacarpal joint of the thumb, which
is independent. The wrist joint is also independent. The continuity of
the articular cavities, or the lack of it, is significant in relation
to the spread of infection and to arthroscopy, in which a flexible
fiberoptic scope is inserted into the articular cavity to view its
internal surfaces and features. The fibrous layer of the joint capsule surrounds these joints, which helps unite the carpals. The synovial membrane lines the fibrous layer and is attached to the margins of the articular surfaces of the carpals.
concomitantly with movements at the wrist (radiocarpal) joint,
augmenting them and increasing the overall range of movement. Flexion
and extension of the hand are actually initiated at the midcarpal joint, between the proximal and the distal rows of carpals (Figs. 6.71B and 6.73).
Investigators disagree regarding the amount of movement occurring at
the wrist vs. the midcarpal joints. Most state that flexion and
adduction occur mainly at the wrist joint whereas extension and
abduction occur primarily at the midcarpal joint. Movements at the
other IC joints are small, with the proximal row being more mobile than
the distal row.
branch of the median nerve and the dorsal and deep branches of the
ulnar nerve.
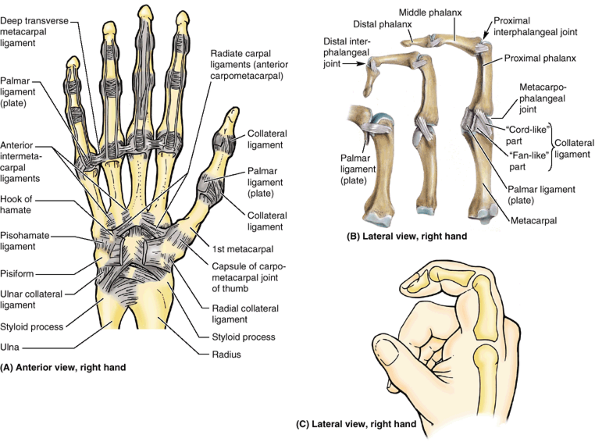 |
|
Figure 6.74. Joints of hand. A.
This dissection of the hand shows the palmar ligaments of the radioulnar, radiocarpal, intercarpal, carpometacarpal, and interphalangeal joints. B. A dissection showing the metacarpophalangeal and interphalangeal joints. The palmar ligaments (plates) are modifications of the anterior aspect of the MP and IP joint capsules. C. The flexed index finger demonstrates its phalanges and the position of the MP and IP joints. The knuckles are formed by the heads of the bones, with the joint plane lying distally. |
articulate with the carpal surfaces of the bases of the metacarpals at
the CMC joints. The important CMC joint of the thumb is between the
trapezium and the base of the 1st metacarpal and has a separate
articular cavity. Like the carpals, adjacent metacarpals articulate
with each other; IM joints occur between the radial and the ulnar
aspects of the bases of the metacarpals.
enclosed by a common joint capsule on the palmar and dorsal surfaces. A
common synovial membrane lines the internal surface of the fibrous
layer of the joint capsule, surrounding a common articular cavity.
surrounds the joint and is attached to the margins of the articular
surfaces. The synovial membrane lines the internal surface of the
fibrous layer. The looseness of the capsule facilitates free movement
of the joint.
(the former part of the palmar aponeurosis), associated with the distal
ends of the metacarpals, play a role in limiting movement at the CMC
and IM joints as they limit separation of the metacarpal heads.
any plane (flexion–extension, abduction–adduction, or circumduction)
and a restricted amount of axial rotation. Most important, the movement
essential to opposition of the thumb occurs here. Although the opponens
pollicis is the prime mover, all of the hypothenar muscles contribute
to opposition. Almost no movement occurs at the CMC joints of the 2nd
and 3rd fingers, that of the 4th finger is slightly mobile, and that of
the 5th finger is moderately mobile, flexing and rotating slightly
during a tight grasp (Fig. 6.48G & H).
When the palm of the hand is “cupped,” (as during pad-to-pad opposition
of thumb and little finger), two thirds of the movement occur at the
CMC joint of the thumb, and one third occurs at the CMC and IC joints
of the 4th and 5th fingers.
of the proximal phalanges in the MP joints, and the heads of the
phalanges articulate with the bases of more distally located phalanges
in the IP joints.
(plates), which form the palmar aspect of the joint capsule. The
fan-like parts of the collateral ligaments cause the palmar ligaments
to move like a visor over the underlying metacarpal or phalangeal
heads. The strong cord-like parts of the collateral ligaments of the MP
joint, being eccentrically attached to the metacarpal heads are slack
during extension and taut during flexion. As a result, the fingers
cannot usually be spread (abducted) when the MP joints are fully
flexed. The interphalangeal joints have corresponding ligaments but the
distal ends of the proximal and middle phalanges, being flattened
anteroposteriorly and having two small condyles, permit neither
adduction or abduction.
the long flexor ligaments to glide and remain centrally placed as they
cross the convexities of the joints. The palmar ligaments of the
2nd–5th MP joints are united by deep transverse metacarpal ligaments
that hold the heads of the metacarpals together. In addition, the
dorsal hood of each extensor apparatus attaches anteriorly to the sides
of the palmar plates of the MP joints.
circumduction of the 2nd–5th digits occur at the 2nd–5th MP joints.
Movement at the MP joint of the thumb is limited to flexion–extension.
Only flexion and extension occur at the IP joints.
dynamic contribution to a skill or movement, or allowing it to be
stabilized in a particular position to maximize the effectiveness of
the hand and fingers in manipulating and holding objects. Complexity as
well as flexibility of the wrist results from the number of bones
involved. Extension–flexion, abduction–adduction, and circumduction
occur. Overall, most wrist movement occurs at the wrist (radiocarpal)
joint between the radius and articular disc of the distal radioulnar
joint and the proximal row of carpal bones (primarily the scaphoid and
lunate). However, concomitant movement at the IC joints (especially the
midcarpal IC joint) augments these movements. The CMC joints of the
four medial fingers, which share a common articular cavity, have
limited motion (especially those of the 2nd and 3rd digits),
contributing to the stability of the palm as a base from and against
which the fingers operate. Motion occurs at the CMC joints for the 3rd
and 4th digits, mostly in association with a tight grip or cupping of
the palm, as during opposition. However, the great mobility of the CMC
joint of the thumb, a saddle joint, provides the digit with the major
portion of its range of motion and specifically enables opposition.
Therefore it is key to the effectiveness of the human hand. In contrast
to the CMC joints, the MP joints of the medial four fingers offer
considerable freedom of movement (flexion–extension and
abduction–adduction), whereas that of the thumb is limited to
flexion–extension, as are all IP joints.
a sprain of the radial collateral ligament and an avulsion fracture of
the lateral part of the proximal phalanx of the thumb. This injury is
common in individuals who ride mechanical bulls.
to the rupture or chronic laxity of the collateral ligament of the 1st
MP joint (Fig. B6.38). The injury results from
hyperabduction of the MP joint of the thumb, which occurs when the
thumb is held by the ski pole while the rest of the hand hits the
ground or enters the snow. In severe injuries, the head of the
metacarpal has an avulsion fracture.
 |
|
Figure B6.38
|
tenderness, angulation, rotation, or instability. Anteroposterior (AP),
lateral, axial, and oblique views are usually sufficient to detect bony
and other injuries. Radiological examinations of the upper limb focus
mainly on bony structures, because muscles, tendons, and nerves are not
well visualized. When examining radiographs of the upper limb, it is
essential to know the median times of appearance of postnatal
ossification centers and when fusion of epiphyses is radiographically
complete in males and females. Without such knowledge, an epiphysial
line could be mistaken for a fracture.
laterally rotated so that its epicondyles are parallel with the X-ray
film cassette (Figs. 6.77A and 6.76A).
Because some obliquity of the glenoid cavity occurs normally, it
appears oval in shape. In this view, the lateral two thirds of the
clavicle is visible. The articulation of the acromial end of the
clavicle with the acromion of the scapula at the AC joint
is apparent. This is a frequent site of subluxation of the joint. The
surgical neck of the humerus, approximately 2.5 cm distal to the
greater and lesser tubercles, is a common site of fracture. The
axillary nerve is in contact with the surgical neck and vulnerable to
injury. Examination of the humerus reveals dense cortical bone along
the shaft, which thins out proximally and becomes extremely thin over
the head of the bone. The radial nerve runs inferolaterally in the
radial groove on the posterior surface of the humerus and is vulnerable
to injury in a midhumeral fracture.
essential additional view of the AC and glenohumeral joints. To obtain
an axial projection, the person is asked to abduct the arm and extend
the shoulder over the X-ray film cassette. In Figure 6.75B, the acromion, glenoid cavity, humeral head, coracoid process, and suprascapular notch are visible.
X-ray film cassette with the forearm supinated. The X-ray beam is
directed perpendicular to the cassette and at the elbow joint. Figure 6.76A
shows the distal end of the humerus as it flares out and ends as the
prominent medial epicondyle and the more flattened lateral epicondyle.
The ulnar nerve is in contact with the medial epicondyle and may be
injured when it is fractured or its epiphysis is dislocated. Distal to
the epicondyles are the convex capitulum and pulley-shaped trochlea.
Between the epicondyles is a radiolucent area representing the
superimposed olecranon and coronoid fossae. The disc-shaped radial head
and its concave articular surface, distal to the capitulum, is apparent.
young adults after a fall on the hand. The radial notch in the ulna is
overlapped by the medial aspect of the radial head where they are in
contact, forming the proximal radioulnar joint. The olecranon of the
ulna is superimposed on the distal end of the humerus where it lies in
the olecranon fossa. Just distal to the trochlea of the humerus is the
coronoid process of the ulna.
the elbow is flexed 90°, and the arm and forearm are placed on the
X-ray film cassette with the thumb extended. In this projection, the
epicondyles, capitulum, and trochlea are superimposed. The superimposed
supraepicondylar ridges form a dense radiopaque shadow. The coronoid
process of the ulna is partly obscured by the radial head.
the forearm is positioned so that it is supinated and the elbow joint
is fully extended. Note that both the elbow and wrist joints are shown.
Observe the translucent area between the capitulum and the radial head
and between the trochlea and the coronoid process. This area is where
the articular cartilages of the articulating bones are located. The
radius and ulna bow (are outwardly convex) as they extend distally from
the elbow. The bones become increasingly separated from each other in
their distal two thirds, coming into contact more abruptly distally.
The interosseous membrane is radiolucent (invisible to radiographic study). To detect fractures and verify their correct reduction
(restoration to the normal position), keep in mind that the radial
styloid process normally ends 1 cm distal to the ulnar styloid process.
In Figure 6.77B, the way in which the radius crosses the ulna during forearm pronation is demonstrated.
assess skeletal age. For clinical studies, the radiographs are compared
with a series of standards in a radiographic atlas of skeletal
development to determine the age of the child. Epiphysial fractures
are more common in young children than in adolescents because tight
fusion of the epiphyses with the bodies of the bones has not occurred.
Fusion of the distal radial and ulnar epiphyses is complete
radiographically at age 16 in females and at age 18 in males. The
carpal bones are superimposed on each other; however, when compared
with a skeleton of the wrist and hand, the bones can be identified. A
lateral projection of the wrist and hand is of great importance because
certain fractures may be revealed only in this projection (Fig. 6.78A).
generally across its narrow part. A radiologist looks for a scaphoid
fracture if the physician reported tenderness over the scaphoid in the
anatomical snuff box; however, it may not be detectable even in several
oblique views until approximately 2 weeks after the injury (see clinical correlation [blue] box “Fracture of the Scaphoid.” earlier in this chapter).
postnatally. The centers for the capitate and hamate appear first.
Ossification centers are usually obvious during the 1st year; however,
they may appear before birth. Accessory ossicles
(small bones) are sometimes observed between the usual carpals; their
possible occurrence should be kept in mind when examining radiographs
of the carpus. Carpal fusions (e.g., between the lunate and the triquetrum) may occur and should be regarded as variations.
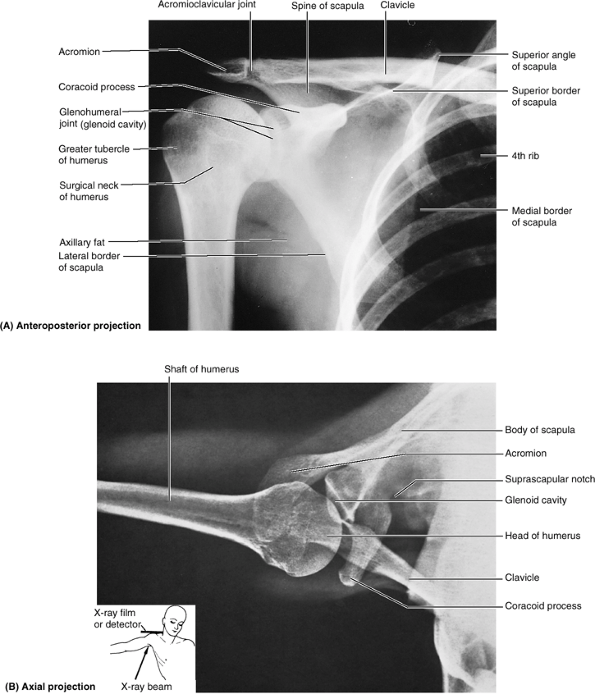 |
|
Figure 6.75. Radiographs of glenohumeral joint. A.
The head of the humerus and the glenoid cavity overlap, obscuring the joint plane because the scapula does not lie in the coronal plane (therefore the glenoid cavity is oblique, not in a sagittal plane, which is especially evident in part B). (Courtesy of Dr. E. L. Lansdown, Professor of Medical Imaging, University of Toronto, Toronto, Ontario, Canada) B. The orientation drawing shows how the axial projection radiograph was taken. |
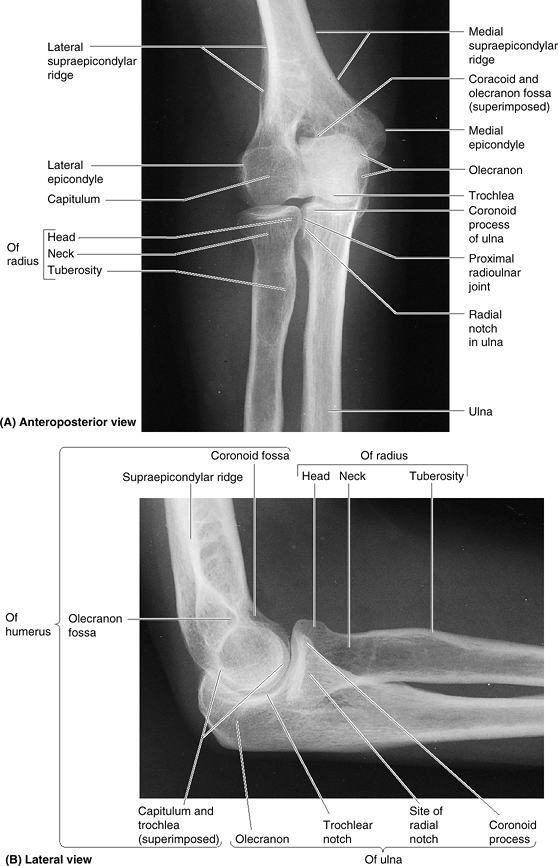 |
|
Figure 6.76. Radiographs of elbow joint. A. The joint planes (occupied by radiolucent articular cartilage) are especially evident in the extended joint. B.
The elbow is flexed to a 90° angle. The spherical nature of the capitulum, around which the superior surface of the radius glides, is especially evident. The head of the radius and the radial notch of the ulna overlap at the proximal radioulnar joint. (Courtesy of Dr. E. Becker, Associate Professor of Medical Imaging, University of Toronto, Toronto, Ontario, Canada.) |
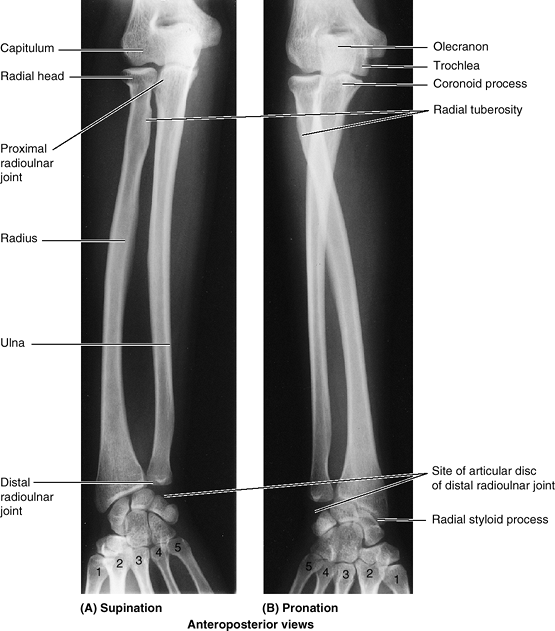 |
|
Figure 6.77. Radiographs of radioulnar joints. A. In the supinated position, the radius and ulna are parallel. B.
During pronation, the inferior end of the radius moves anteriorly and medially around the inferior end of the ulna, carrying the hand with it; thus in the pronated position, the radius crosses the ulna anteriorly. 1–5, the metacarpals. (Courtesy of Dr. J. Heslin, Toronto, Ontario, Canada.) |
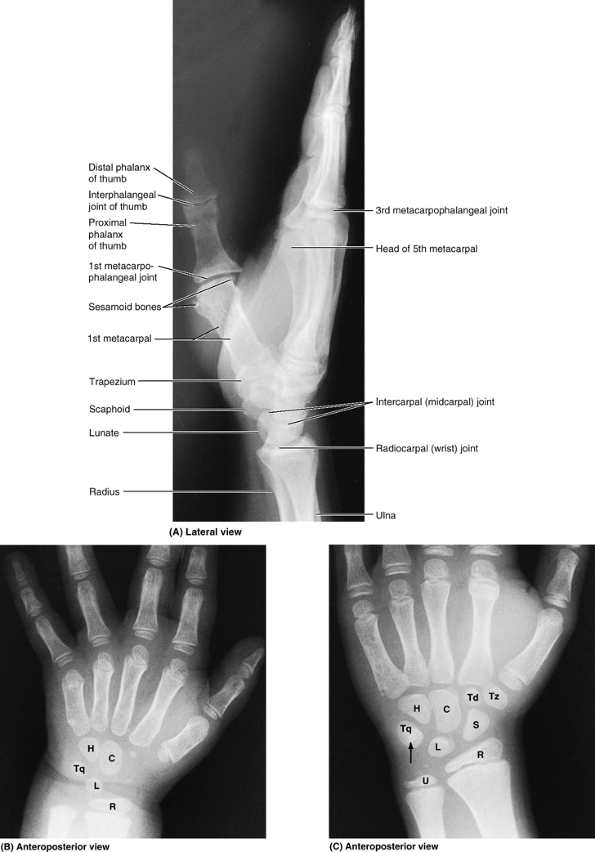 |
|
Figure 6.78. Radiographs of right wrist and hand. A.
This lateral view shows the adult hand. (Courtesy of Dr. E. L. Lansdown, Professor of Medical Imaging, University of Toronto, Toronto, Ontario, Canada.) B. The distal end of the forearm and the hand of a 2.5-year-old child are shown. Ossification centers of only four carpal bones are visible. Observe the distal radial epiphysis (R). C, capitate; H, hamate; L, lunate; Tq, triquetrum. C. The inferior end of the forearm and hand of an 11-year-old child are shown. Ossification centers of all carpal bones are visible. The arrow indicates the pisiform lying on the anterior surface of the triquetrum. The distal epiphysis of the ulna (U) has ossified but all epiphyseal plates (lines) “remain open” (i.e., they are still unossified). S, scaphoid; Td, trapezoid; Tz, trapezium. (Courtesy of Dr. D. Armstrong, Associate Professor of Medical Imaging, University of Toronto, Toronto, Ontario, Canada.) |
the fingers are superimposed, and little information can be obtained by
examining them in this view (Fig. 6.78A).
If a particular finger is injured and suspected of having a fracture,
it is viewed laterally with the other fingers flexed. The shaft of each
metacarpal begins to ossify during fetal life, and ossification centers
appear postnatally in the heads of the four medial metacarpals and in
the base of the 1st metacarpal (Fig. 6.78B). By age 11, ossification centers of all carpal bones are visible (Fig. 6.78C). Pseudoepiphyses (accessory centers) are occasionally seen in the head of the 1st metacarpal and in the base of the 2nd metacarpal.
When interest is in a specific artery, the dye is injected directly
into it, usually through a catheter. Arteriography may be used to
determine the patency of arteries before and after surgical procedures
in the upper limb to repair injuries resulting from trauma.
the anatomical images are created by computer reconstructions of the
electronic data. The reconstructed images look like cross sections of
the limb, and they can be reconstructed in the coronal and sagittal
planes. Because the person must be in the CT scanner for only brief
periods, fast (2-s) scans can be produced; consequently, involuntary
movement produces minimal distortion of the images. For example, arthrotomography
enhanced by CT is able to demonstrate subtle fractures (e.g., of the
rim of the glenoid cavity) and reactive bone changes around a
recurrently dislocating glenohumeral joint (Halpern, 2004).
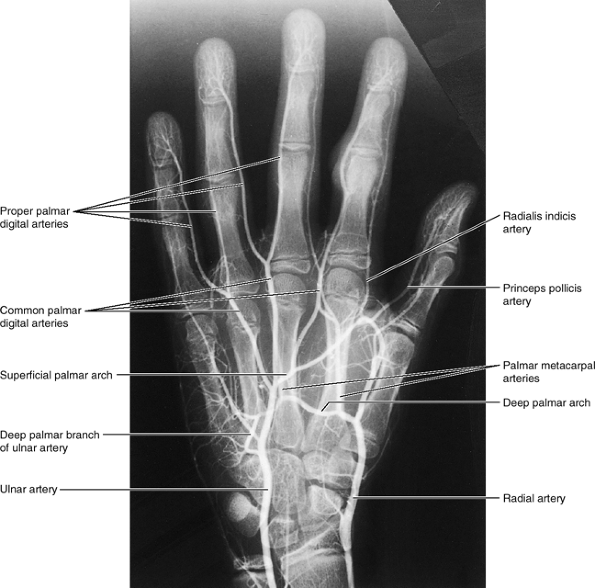 |
|
Figure 6.79. Angiogram of hand.
The superficial palmar arch, formed primarily by the ulnar artery, is usually completed by the superficial palmar branch of the radial artery. In this teenage hand, the carpal bones are fully ossified, but the epiphyseal lines of the long bones (e.g., radius and ulna) are still open. Closure occurs when growth is complete, usually at the end of the teenage years. (Courtesy of Dr. D. Armstrong, University of Toronto, Toronto, Ontario, Canada) |
soft tissues of the limbs because adults can keep their limbs
motionless for the 5–10 min required for scanning. This technique
produces cross-sectional, coronal, and sagittal images and has the
advantage that it does not involve the use of X-rays. Because MRI
requires the person to remain still for several minutes, this technique
is difficult to use with children. In Figure 6.80,
observe the good resolution of the muscles, bones, and joints. MRI is
helpful in the diagnosis of subluxation, dislocation, impingement of
nerves, cartilage tears, and rotator cuff tears of the glenohumeral
joint (Halpern, 2004). Coronal MRIs are helpful in demonstrating ruptured tendons in the shoulder, elbow, hand, and wrist regions.
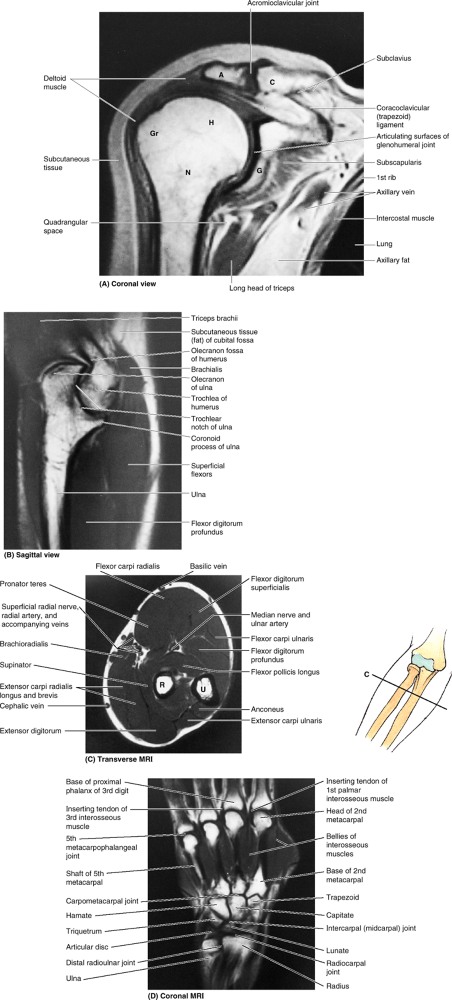 |
|
Figure 6.80. MRI studies of upper limb. A.
The glenohumeral and acromioclavicular joints are shown. The “white” (signal-intense) parts of the identified bones are the fatty matrix of cancellous bone; the thin black outlines (absence of signal) of the bones are the compact bone that forms their outer surfaces. A, acromion; C, clavicle; G, glenoid cavity; Gr, greater tubercle of humerus; H, head of humerus; N, surgical neck of humerus. B. The elbow region is shown. C. The proximal part of the forearm is shown. The orientation drawing shows the plane of the MRI. The subcutaneous border of the ulna (U) and the radial artery demarcate the anteromedial flexor and posterolateral extensor compartments. R, radius. D. In this image of the wrist and hand, the bones, joints, and interosseous muscles can be observed. (Courtesy of Dr. W. Kucharczyk, Professor and Chair of Medical Imaging, University of Toronto, and Clinical Director of Tri-Hospital Magnetic Resonance Centre, Toronto, Ontario, Canada.) |
is a physiological “joint,” in which movement occurs between
musculoskeletal structures (between the scapula and associated muscles
and the thoracic wall), rather than an anatomical joint, in which
movement occurs between directly articulating skeletal elements. The
scapulothoracic joint is where the scapular movements of
elevation–depression, protraction–retraction, and rotation occur.
It is awkward that the structure officially identified as the flexor
retinaculum does not correspond in position and structure to the
extensor retinaculum when there is another structure (the palmar carpal
ligament, currently unrecognized by Terminologia Anatomica) that does. The clinical community has proposed and widely adopted the use of the more structurally based term transverse carpal ligament to replace the term flexor retinaculum. The authors urge FICAT to adopt this terminology in future editions of Terminologia Anatomica.
LJ (Chair), Educational Affairs Committee, American Association of
Clinical Anatomists: The clinical anatomy of several invasive
procedures. Clin Anat 12:43, 1999.