Anterior Glenohumeral Instability: Pathoanatomy
III – Shoulder Reconstruction > Part B – Evaluation and Treatment of
Shoulder Disorders > 32 – Anterior Glenohumeral Instability:
Pathoanatomy
that, >30 years later, Bankart went on to coin the “essential
lesion.” Since then, a plethora of anatomic and biomechanical studies
have helped to clarify the elements that contribute to anterior
glenohumeral instability (AGI). We now know that the shoulder joint is
the most frequently dislocated joint and that >90% of these
dislocations are anterior. The innate bony anatomy of the glenohumeral
joint makes it particularly prone to instability. It has been likened
to a golf ball on a tee. A small glenoid matched to a large humeral
head allows the joint to be very mobile. The joint is thus quite
dependent on the surrounding soft tissues for stability. When the bony
anatomy is disrupted, or when the soft tissues fail, instability is the
result. The specific pathoanatomy related to AGI is discussed below
under two general categories: static stabilizers and dynamic
stabilizers (Table 32-1).
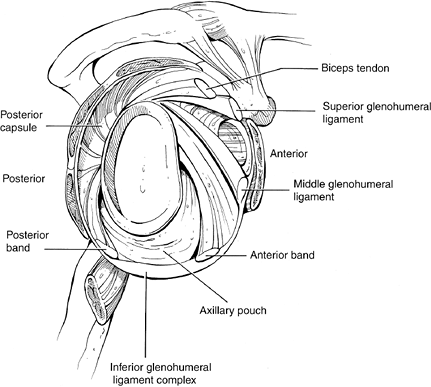
elucidate the structures of the capsule and ligaments of the
glenohumeral joint than any other aspect of the shoulder. It has been
>150 years since investigators first described distinct ligaments
that contributed to the shoulder joint’s stability. Since then, many
others have collaborated in their efforts to arrive at a generally
accepted model of the capsuloligamentous complex. We consider three
major ligaments when discussing anterior glenohumeral instability: the
inferior, middle, and superior (Fig. 32-1).
on the humeral head at the extremes of range of motion. When they
become lax or disrupted, the humeral head translates beyond its normal
boundaries of the glenoid.
universally accepted as the primary static restraint to AGI.
Investigators have conducted cadaveric dissections, histologic
analysis, and biomechanical studies to delineate the individual
components of the complex. The most popular model describes the complex
with an anterior and posterior band with an interposed axillary pouch.
It functions as a sling, or hammock, that changes position and
undergoes reciprocal tightening and loosening with arm rotation. The
anterior band is particularly important at limiting anterior
translation when the arm is externally rotated and abducted to 90
degrees. Injury to this band of the complex is one of the most
significant factors leading to AGI.
anterior dislocation. Traumatic failure of the IGHLC most frequently
occurs when it is avulsed with the anterior labrum, forming a Bankart
lesion. Additionally, it may become stretched out over time by
repetitive microtrauma. Overhead athletes are especially prone to this
type of injury. With either type of injury, the anterior capsule can
undergo plastic deformity as a result of trauma. The capsule becomes
more and more voluminous, causing increased glenohumeral translation.
function as the primary restraint to anterior translation when the arm
is externally rotated and abducted from 60 to 90 degrees. The MGHL can
be absent in ≤30% of individuals, and some feel that this predisposes
to AGI. Additionally, the MGHL can be avulsed along with the IGHLC with
a Bankart lesion.
do with limiting pure anterior translation. But more recently it has
been implicated for its role in the rotator interval laxity. Some
believe that a widened rotator interval as a result of a deficient SGHL
may be implicated in recurrent AGI. Table 32-2 summarizes each of these ligaments’ roles in preventing AGI.
humeral avulsion of the glenohumeral ligament (HAGL) lesion. Unlike the
more commonly seen avulsion of the ligaments from the glenoid/labrum
side, it is possible to detach the ligaments from the humeral side.
This may be caused by either an anterior shoulder dislocation or
hyperabduction.
The HAGL lesion must be identified and anatomically repaired to restore stability to the shoulder.
 |
|
Figure 32-1 Glenohumeral capsuloligamentous complex. (From
O’Brien
SJ, Neves MC, Amoczky SP, et al. The anatomy and histology of the inferior glenohumeral ligament complex of the shoulder. Am J Sports Med. 1990;18:449–456 , with permission.) |
 |
|
Figure 32-2 Arthroscopic picture of a Bankart injury viewed from the posterior portal (humeral head on the left and glenoid on the right).
|
|
TABLE 32-1 Static and Dynamic Stabilizers
|
|
|---|---|
|
|
TABLE 32-2 Glenohumeral Ligaments
|
|
|---|---|
|
is the glenoid labrum. It serves as the anterior anchor point for the
capsuloligamentous complex, as well as a chock block during anterior
translation of the humeral head. Additionally, it deepens the glenoid
and increases the surface area contact of the humeral head.
Whether this is truly the “essential lesion,” as Bankart proposed,
remains a topic of debate. Cadaveric studies have shown that simply
detaching the labrum is not sufficient to cause AGI. In contrast,
multiple authors have observed intraoperatively that detachment of the
labrum is quite common after traumatic anterior instability episodes.
One study has demonstrated detachment of the labrum in ≤97% of first
time anterior dislocators without evidence of associated intracapsular
injury. It has also been observed that recurrent anterior subluxers and
dislocators have a fraying of the labrum. The severity of the
deleterious effect on the labrum appears to be additive based on the
number of instability episodes.
periosteal sleeve avulsion, or ALPSA, can result in AGI. This injury
differs from the classic Bankart lesion in that the labrum is
incompletely dissociated from the glenoid. A periosteal sleeve remains
attached to the labrum that allows it to displace medially and rotate
inferiorly. The lesions heal but will lead to recurrent AGI owing to
excessive anterior capsular laxity. The sleeve must be detached,
creating a full Bankart lesion, and then anatomically reattached to
restore the labrum and capsule to proper function.
 |
|
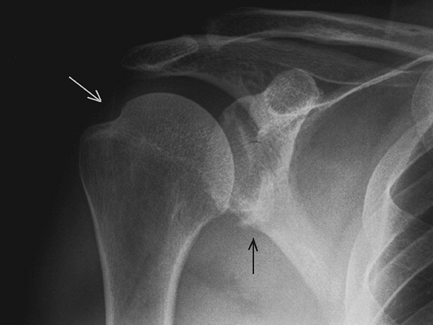
Figure 32-3 Anteroposterior radiograph demonstrating a bony Bankart injury (black arrow) and Hill-Sachs lesion (white arrow).
|
posterolateral margin comes into contact with the anterior glenoid rim.
In the process of dislocating, the portion of the humeral head in
contact with the glenoid can sustain an impression fracture. This
fracture and bone loss is termed a Hill-Sachs lesion (Fig. 32-3).
It can occur in ≤80% of anterior dislocations and may be present in an
even higher percent of recurrent dislocators. Small lesions usually do
not affect stability of the joint, but those >30% of the articular
surface deserve attention. These larger lesions can predispose one to
recurrent AGI, and they require reconstruction to restore stability to
the glenohumeral joint. Despite capsular and labral repairs, large
Hill-Sachs lesion can render the joint unstable.
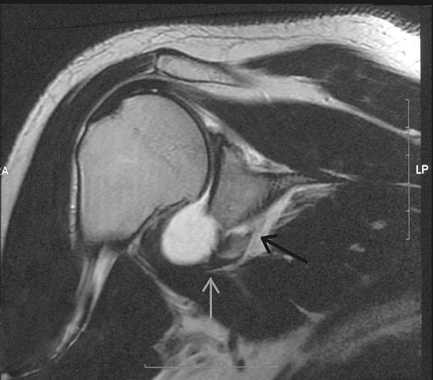
This arises when a portion of the anteroinferior rim of the glenoid is
fractured off with the capsulolabral attachments as the humeral head
dislocates anteriorly (Fig. 32-4). When the
fractured piece contains >20% to 25% of the glenoid surface area, it
should be repaired back to the remaining glenoid.
wear. Recurrent anterior subluxation of the humeral head can cause
gradual deterioration of the glenoid rim. When this defect becomes
large enough, instability may result even after capsulolabral repair.
As with traumatic bone loss, large defects require bone grafting. Many
procedures have been described to augment glenoid bone stock including
the transfer of the coracoid process (Bristow procedure or Latarjet
procedure) and the use of autograft bone block.
some influence on posterior glenohumeral instability, it most likely
has little or no effect on anterior instability. Clinical studies and
sophisticated CT analyses have failed to show any significant
relationship between version and AGI. However, one must be sure that
apparent changes in glenoid version are not the result of glenoid bone
loss.
 |
|
Figure 32-4 Coronal plane MRI demonstrating fracture of the anteroinferior glenoid (black arrow) and maintenance of the labral attachment to the glenoid rim (gray arrow).
|
than static stabilizer, but passive tension within the cuff appears to
play some role in preventing AGI. Specifically, the subscapularis has
been shown to limit anterior translation of the humeral head at low
ranges of shoulder abduction. When the subscapularis becomes injured or
ruptured, as such is the case particularly in older individuals who
suffer traumatic anterior dislocations, its static block to anterior
translation is lost.
shoulder joint because of the relatively higher osmotic pressure in the
surrounding interstitial tissue that causes water to be drawn out of
the joint. This effect appears to be important when dynamic stabilizers
are not functioning properly. A defect in the capsule or labrum, or
degenerative changes in the glenohumeral joint, eliminate the effect.
The importance of this negative pressure is probably negligible,
though, when dynamic stabilizers are functioning properly.
have received less attention than static stabilizers. Most early
stabilization procedures were nonanatomic reconstructions,
which
resulted in altered biomechanics of the joint. This subsequently led to
secondary problems, such as decreased range of motion and glenohumeral
arthritis. But with advancements in laboratory and surgical techniques,
we have been able to understand better the dynamic factors that affect
shoulder stability.
rotator cuff as a dynamic stabilizer of the shoulder. The coordinated
contracture of the rotator cuff causes a force coupling of the muscles
and a joint reaction force vector toward the center of the glenoid. The
net result is a joint compression force that keeps the humeral head
located within the glenoid fossa. Dysfunction of the rotator cuff
muscles owing to poor neuromuscular control, injury, atrophy,
contracture, or tendon deficiency can result in uncoupling of the
muscles and a net force vector directed away from the center of the
glenoid. Consequently, excessive translation of the humerus occurs and
undue strain is placed on the capsuloligamentous structures and the
labrum. The net result of rotator cuff dysfunction is instability.
important factor in glenohumeral joint stability. Dysfunction of the
coordinated timing and positioning of the glenoid and humeral head can
be caused by dyskinesis of the scapular rotators. Most often, this is
caused by fatigue of the serratus anterior and trapezius muscles. Less
commonly, dysfunction may be caused by long thoracic nerve palsy.
serves an important function in dynamic shoulder stabilization,
especially when the rotator cuff or capsuloligamentous structures are
overwhelmed. It serves its greatest role in preventing anterior
displacement when the arm is in internal rotation at the middle and
lower levels of elevation. When there is a Bankart lesion, the function
of the biceps in preventing humeral head displacement may be even more
important than the rotator cuff muscles. Indeed, in patients with
rotator cuff weakness, the biceps tendon may become hypertrophied.
the shoulder capsule and ligaments. These receptors are thought to
provide feedback information about the joint position and motion. This
enables a coordinated interaction of the dynamic shoulder stabilizers.
Individuals with a history of AGI appear to have a higher threshold for
detecting passive motion of their shoulder. Whether or not these
feedback loops function at speeds fast enough to prevent instability
episodes remains a topic of debate.
RA, Wheeler JH, Ryan JB, et al. Arthroscopic Bankart repair versus
nonoperative treatment for acute, initial anterior shoulder
dislocation. Am J Sports Med. 1994;22:589–594.
SJ, Neves MC, Arnoczky SP, et al. The anatomy and histology of the
inferior glenohumeral ligament complex of the shoulder. Am J Sports Med. 1990;18:449–456.
SJ, Schwartz RS, Warren RF, et al. Capsular restraints to
anterior-posterior motion of the abducted shoulder: a biomechanical
study. J Shoulder Elbow Surg. 1995;4:298–308.
DC, Arciero RA. Pathologic changes associated with shoulder
dislocations. Arthroscopic and physical examination findings in
first-time traumatic anterior dislocations. Am J Sports Med. 1997;25:306–311.
