Sternoclavicular Joint Disorders
III – Shoulder Reconstruction > Part B – Evaluation and Treatment of
Shoulder Disorders > 31 – Sternoclavicular Joint Disorders
comparison to other shoulder girdle problems. The sternoclavicular
joint may be affected by traumatic conditions, such as dislocation and
fracture, or atraumatic conditions such as arthritis and infection.
Diseases like sternocostoclavicular hyperostosis, osteitis condensans,
Friedrich disease and spontaneous joint instability also affect the
sternoclavicular joint but are rare. Posterior joint dislocations,
although uncommon, are of particular concern owing to their high risk
of serious complications including respiratory compromise, vascular
compromise, hoarseness, brachial plexus compression, and death. A
thorough understanding of these disorders and the associated clinical
and radiograph findings will allow accurate diagnosis and appropriate
treatment.
a remarkable amount of force, which may be applied directly or
indirectly. A direct force dislocation occurs when a sufficiently
strong posterior directed force is applied to the anterior aspect of
the medial clavicle, and as a result the medial clavicle dislocates
posteriorly toward the mediastinal structures. An indirect force
dislocation, the most common mechanism of injury, may result in
anterior or posterior sternoclavicular joint instability. An anterior
SC joint dislocation occurs when an anterolateral compressive force is
applied to the shoulder creating an external rotatory torque on the
clavicle with resultant anterior displacement of the medial clavicle. A
posterior dislocation results when the opposite occurs, a
posterolateral compressive force results in an internal rotatory torque
on the clavicle with associated posterior dislocation of the medial
clavicle. The two most frequent causes of SC joint subluxation or
dislocation are motor vehicle collisions (40%) and contact sports
(27%), such as rugby or football. Other traumatic causes of injury are
falls, crush injuries and heavy lifting.
affecting the sternoclavicular joint. Its exact cause is unknown;
however, it is thought to be multifactorial in origin (e.g.,
hereditary, trauma, aging, and joint laxity). Sternoclavicular
arthritis has also been associated with spinal accessory nerve palsy
secondary to radical neck surgery. The nerve palsy results in shoulder
ptosis, which increases stresses transmitted across the SC joint
resulting in early degenerative changes. A history of manual labor is
also a risk factor for the development of symptomatic osteoarthritis.
Rheumatoid arthritis involvement of the SC joint is variably reported
in the literature.
bacterial and are commonly associated with intravenous drug use and
immunocompromised states such as acquired immunodeficiency syndrome
(AIDS) or chemotherapy. Other predisposing conditions for SC joint
sepsis include rheumatoid arthritis, alcoholism, bacteremia, and
chronic diseases.
<1% of all joint dislocations. With respect to the shoulder girdle,
they represent only 3% of injuries—compared with 85% for glenohumeral
dislocations and 12% for acromioclavicular joint injuries. Anterior SC
joint dislocations are much more common than posterior dislocations,
with an anterior-to-posterior ratio of 20:1.
is likely underreported as it is very often misdiagnosed and
mistreated. The frequency of SC degenerative arthritis increases with
age, and studies have found degenerative changes in 90% to 100% of
patients over the age of 70 years. Postmenopausal women are more
susceptible than either men or premenopausal women to osteoarthritis;
however, the etiology is unknown. Rheumatoid arthritis (RA) involvement
of the SC joint has been reported in as many as 30% of patients, and
changes were usually present within 1 year of diagnosis.
to have a higher incidence in intravenous drug abusers. Common
causative organisms are Staphylococcus aureus and Streptococcus species. Immunocompromised patients
have other causative organisms, such as Pseudomonas aeruginosa, Neisseria gonorrhoeae, and Candida albicans.
|
TABLE 31-1 Classification of Sternoclavicular Joint Instability
|
|||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
saddle-type joint which is the only true synovial articulation between
the upper extremity and the axial skeleton. The epiphysis of the medial
clavicle is the last to appear and the last to close at 23 to 25 years
of age. The SC joint has limited intrinsic bony stability as less than
half of the medial clavicle articulates with the superolateral
manubrium; therefore, stability is provided by the robust capsular
ligaments and the strong costoclavicular and interclavicular ligaments.
An intra-articular disc ligament exists that divides the joint into two
separate spaces; it functions to reduce incongruities between the
articular surfaces and as a restraint to medial displacement of the
clavicle.
anterior and posterior joint translation (41% and 106%, respectively)
with release of the posterior joint capsule. Anterior capsular release
was found to increase only anterior translation, and sectioning of the
costoclavicular and the interclavicular ligaments resulted in
insignificant joint translation. Therefore, it is thought that the
posterior joint capsule is the most important restraint to anterior and
posterior sternoclavicular joint translations.
anterior to vital superior mediastinal structures. These structures
include the innominate artery and vein, the subclavian artery and vein,
the recurrent laryngeal nerve, the phrenic nerve, the vagus nerve, the
esophagus, and the trachea. Posterior dislocation of the medial
clavicle may compromise any of these structures with potential
life-threatening consequences. These vital structures are also placed
at risk during operative management of sternoclavicular disorders, such
as arthrotomy for infection and open reduction of dislocations.
and span a wide spectrum of orthopedic diseases (trauma, arthritis and
infection). Therefore, a universal classification scheme does not exist.
A formal classification system for degenerative arthritis of the
sternoclavicular does not exist; therefore, standard principles may be
applied. Degenerative changes in the SC joint initiate at the inferior
part of the medial clavicular head, which articulates with the
manubrium. Mild osteoarthritis has radiographic changes consisting of
minimal joint space narrowing and small osteophytes. Moderate
osteoarthritis has further joint space narrowing, subchondral
sclerosis, and larger peripheral osteophytes while severe arthritis has
complete cartilage loss.
result of a motor vehicle collision or a sports-related trauma. A
detailed history will allow determination of the mechanism of injury as
patients may describe a direct blow to the anterior chest or medial
compression to the shoulder girdle with resultant indirect SC joint
injury. Patients may complain of pain, tenderness or deformity around
the SC joint. Symptoms of hoarseness, shortness of breath, difficultly
swallowing, or choking should be elicited as they may indicate
posterior dislocation of the medial clavicle with concomitant
mediastinal compression.
with swelling, tenderness, and severe pain that is exacerbated with arm
movement. The differentiation between anterior and posterior
dislocation can usually be made on physical examination; however, in
cases of severe swelling, accurate diagnosis may be difficult. With an
anterior dislocation, the medial clavicle is prominent and can be
palpated anterior to the manubrium. In patients with a posterior
dislocation, the prominent medial clavicle is absent and the manubrium
is more easily palpated. Patients with posterior dislocations may also
exhibit signs of damage to the pulmonary and vascular systems, such as
stridor, venous congestion, or hemodynamic instability.
may be subtle and consist of only mild pain, tenderness, and swelling.
Joint instability may be tested by translating the medial clavicle
joint in the anteroposterior direction and comparing with the
contralateral side. Patients with atraumatic or spontaneous
sternoclavicular joint instability can usually demonstrate with minimal
discomfort subluxation or dislocation with arm elevation that
spontaneously reduces when the arm is brought down.
activity-related pain and swelling at the sternoclavicular joint.
Symptoms are exacerbated by palpation of the joint and active shoulder
elevation. The medial clavicle may be prominent owing to osteophytes
and may also be in fixed subluxation. Patients with rheumatoid
arthritis usually report similar findings of pain, swelling, and joint
crepitus; however, isolated joint involvement of the SC joint in RA is
rare.
uncommon and is usually associated with immunocompromised states (human
immunodeficiency virus [HIV]), rheumatoid arthritis, renal dialysis, or
intravenous drug abuse. The hallmark features are pain, swelling,
tenderness, and erythema over the SC joint. Constitutional symptoms,
such as fever, chills, and night sweats, are common.
 |
|
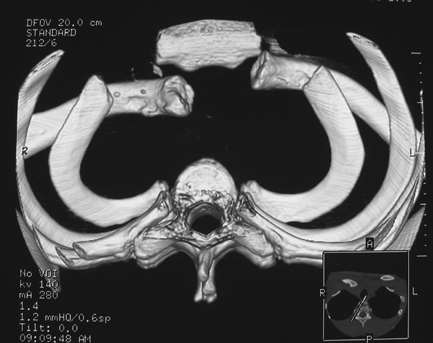
Figure 31-1 Three-dimensional CT reconstruction of a traumatic right posterior sternoclavicular joint dislocation.
|
 |
|
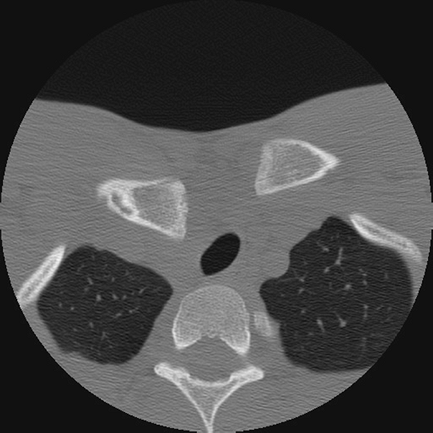
Figure 31-2
Axial CT image of a posterior sternoclavicular joint dislocation with associated compression of the mediastinal structures, notably the trachea. |
interpret for sternoclavicular joint injuries because of overlapping
anatomic structures. Several special projections have been described to
aid in the diagnosis of SC joint pathology, including the serendipity
and Hobb views. The serendipity view is performed with the patient
supine and the radiography tube angled at 40 degrees cephalad, centered
on the manubrium; this image allows a relative axial view of the joint.
The Hobb view approximates a 90-degree lateral view of the SC joint and
is performed with the patient leaning over the radiography table so
that the flexed neck is almost parallel to the table. Radiographs
should be assessed for joint congruity (instability), signs of
arthritis (OA), and erosions with joint destruction (neoplasm, sepsis).
method of assessing the SC joint and has been reported as being the
best imaging modality. It is important to image both sides for
comparison of the pathologic to the normal contralateral side. CT scans
can also be reformatted into three-dimensional images to allow accurate
representation of the SC joint (Fig. 31-1).
When interpreting studies with posterior SC joint dislocations, a
particular benefit is the ability to assess mediastinal structures and
their potential compromise (Fig. 31-2). In patients with such findings, CT with angiography is indicated.
detailed and specific identification of SC joint soft tissues and
mediastinal structures. Coronal MRI images are ideal for evaluation of
the SC joint
articular
surfaces, the intra-articular disc, and the interclavicular and
costoclavicular ligaments. The axial views are useful in assessing the
anterior and posterior sternoclavicular ligaments, joint congruity, and
the relationship between vital mediastinal structures and the SC joint.
that occur in other joints (instability, osteoarthritis, rheumatoid
arthritis, infection, fracture). A detailed history outlining symptom
onset, systemic complaints, family history, and social history will
lead to a provisional diagnosis. Physical examination with a focus on
joint translation, swelling, fluctuance, warmth, and signs of
pulmonary-vascular compromise will further hone the diagnosis. Imaging
with radiographs and CT will be confirmatory and assist with treatment
planning.
generally treated with closed reduction under sedation or general
anesthesia. Anterior dislocations are generally easily reduced;
however, they tend to remain unstable and there is a high redislocation
rate. Because of the high complication rate of surgery and the low rate
of persistent symptoms or functional deficit with nonoperative
treatment, it is recommended that redislocated SC joints be treated
conservatively.
being supine with a moderate-sized bolster placed between the
shoulders. The arm is abducted to 90 degrees with gentle traction
followed by a posterior-directed force applied to the medial clavicle.
If a stable reduction ensues, the patient may be immobilized in a
figure-of-eight bandage, a Velpeau bandage, a clavicle strap harness,
or a bulky pressure pad taped over the medial clavicle for 6 weeks. If
the SC joint redislocates, the patient may be placed in a shoulder
sling for comfort until symptoms subside.
instability should be considered only in patients who have failed
nonoperative treatment. Patients may complain of pain, deformity, and
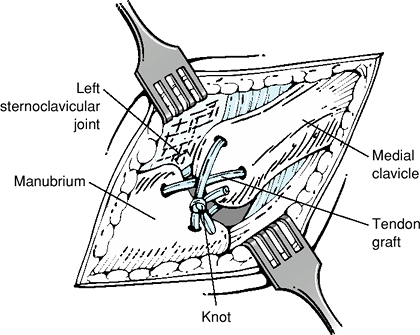
crepitus. Various procedures have been described to stabilize the
medial clavicle or reconstruct the SC joint. The author’s preferred
technique is reconstruction of the anterior and posterior SC joint
capsule and sternoclavicular ligaments with tendon graft woven through
the manubrium and medial clavicle (Fig. 31-3).
The patient is positioned in a 40-degree upright beach-chair position.
The surgical approach involves an oblique 6- to 8-cm incision centered
over the medial clavicle extending over the manubrium. The platysma
muscle is divided, and the medial clavicle and SC joint are exposed.
Drill tunnels (3 to 4 mm in diameter) are created in the medial
clavicle, and the manubrium followed by passage of the tendon graft.
The joint is reduced, and the tendon graft is secured. This is followed
by suture repair of the costoclavicular ligaments and remaining soft
tissues to augment the reconstruction. Other surgical options include
the Burrow procedure (subclavius tendon tenodesis to medial clavicle),
sternal head of sternocleidomastoid muscle transfer, costoclavicular
ligament reconstruction with tendon graft, and distal clavicle
resection with soft tissue stabilization.
 |
|
Figure 31-3
Tendon-weave reconstruction of the anterior and posterior sternoclavicular joint capsule and sternoclavicular ligaments. The tendon graft is passed through drill tunnels created in the medial clavicle and manubrium. |
undergo a thorough history and physical examination assessing for
associated mediastinal injuries. Mediastinal injuries, if present,
should be completely investigated and the appropriate referrals made to
vascular, cardiothoracic, or general surgery.
within 7 to 10 days should be treated with an attempted closed
reduction. Once reduced, unlike anterior dislocations, posterior
dislocations tend to remain stable. Closed reduction should be
conducted in the operating room with appropriate anesthesia and with
vascular or thoracic surgery available. The most commonly described
reduction maneuver is the abduction-traction technique, in which the
patient is positioned supine with a medium-sized bolster placed between
the shoulders. The arm is abducted to 90 degrees with traction; as the
arm is gently extended, the medial clavicle is levered forward with a
reduction occurring usually with an audible snap. If the reduction is
unsuccessful, the medial clavicle may be manually manipulated to bring
it forward, and if this is also unsuccessful, a sterile towel clip may
be used to grasp the clavicle to pull it forward. Resistant posterior
SC joint dislocations have also been reduced by another maneuver termed
the adduction-traction technique. This
technique involves gentle traction to the adducted arm with a
posterior-directed force applied to both shoulders, which levels the
medial clavicle over the first rib and into its normal position.
dislocations include an unsuccessful or unstable closed reduction,
chronic posterior instability, or chronic posterior dislocations.
Patients with chronic posterior SC joint dislocations without initial
symptoms of mediastinal compromise have experienced significant late
complications such as vascular compromise, thoracic outlet syndrome,
and erosion of the medial clavicle into vital mediastinal structures
(arteries and veins). The operative technique of open reduction and
stabilization is identical as for anterior SC joint dislocations, and
the reader is referred to the previous section.
sternoclavicular joint are best managed with nonoperative treatment,
such as anti-inflammatory medications, local steroid injections, and
activity modification. Patients with rheumatoid arthritis should also
be managed medically in conjunction with a rheumatologist.
arthritis include persistent pain and functional limitation despite
maximized nonoperative treatment. Operative treatment involves excision
of the medial end of the clavicle with preservation of the posterior
sternoclavicular and costoclavicular ligaments. On average, 8 to 10 mm
of medial clavicle is excised; if too much is excised or if damage to
the stabilizing ligaments occurs, clavicular instability may occur.
organism-specific parenteral antibiotics, along with surgical
irrigation and debridement. In subacute and chronic cases with delayed
diagnosis, abscess formation with bone destruction may necessitate
partial SC joint resection and first rib debridement. Untreated or
partially treated infections may progress to extrapleural or
intrathoracic abscess with potentially life-threatening complications.
In severe cases with extensive debridement, patients may require
transposition of the ipsilateral pectoralis major muscle to obliterate
residual space and to reconstruct the chest wall.
usually mild. Patients may complain of a noncosmetic bump at the medial
end of the clavicle or symptoms consistent with late degenerative
arthritis.
dislocations has been associated with a wide variety of complications
owing to the proximity of the joint to the mediastinal structures.
Documented complications include pneumothorax, respiratory distress,
venous congestions, laceration of the superior vena cava, compression
of the subclavian artery, brachial plexopathy, esophageal rupture,
tracheoesophageal fistula, and hoarseness. Although the rate of
complications has been documented at 25%, the reported fatality rate is
low.
disorders vary depending on the type of surgical procedure.
Complications of medial clavicle resection usually relate to damage of
the stabilizing ligaments leading to instability and pain. Most
complications associated with past operative stabilization procedures
for traumatic SC joint injuries related to hardware migration.
Kirschner wires, Steinmann pins, and Hagie pins used to transfix the SC
joint have migrated and punctured vital structures; therefore,
alternative means of joint stabilization are recommended such as
autograft or allograft tendon reconstruction.
disorders, there are few good outcomes studies. Studies in the
literature are limited by their retrospective design, few patient
numbers, and variable clinical follow-up.
anterior sternoclavicular joint dislocations states a 70% to 80%
satisfaction rate (return to normal activities and no SC joint pain).
Posterior SC joint dislocations that are successfully managed with
closed reduction appear universally to do well in the literature, with
minimal pain and disability, no recurrences, and minimal crepitus.
outcomes of surgically treated posterior SC joint dislocations.
Analysis of the few studies available shows the results are highly
variable and may depend on the type of operative procedure. Procedures
involving resection of the medial clavicle without stabilization appear
to have poor outcomes owing to residual instability. Medial clavicle
resection procedures with maintenance or reconstruction of the
supporting ligaments have a 70% good to excellent outcome. Outcomes
with open reduction and ligament reconstruction are also variable and
range from 42% to 90% good to excellent results.
clavicle resection with preservation of the stabilizing joint
structures provides a 70% to 90% good to excellent outcome at medium-
to long-term follow-up. Once again, the studies available are few,
retrospective, with low patient numbers, and use variable outcome
measures.
surgery involves protection of the shoulder and SC joint with a
shoulder immobilizer and limited motion consisting of pendulum
exercises for 6 weeks. Patients may then progress to passive range of
motion, active assisted motion, and then to active range of motion.
Shoulder-strengthening exercises are initiated at 3 months.
resection for arthritis is similar to the postoperative management of
SC joint instability surgery. The rehabilitation goals are to allow
adequate healing of the sternoclavicular soft tissues to prevent late
instability while allowing protected shoulder motion.
debridement should be managed in a shoulder immobilizer for comfort.
Patients requiring aggressive debridement with medial clavicle excision
should be managed similarly to patients with medial clavicle resections
for arthritis.
A, Patsalis T, Michiels I. Resection arthroplasty of the
sternoclavicular joint for the treatment of primary degenerative
sternoclavicular arthritis. J Bone Joint Surg Br. 2002;84:513–517.
