Nerve Injuries About the Shoulder
III – Shoulder Reconstruction > Part B – Evaluation and Treatment of
Shoulder Disorders > 41 – Nerve Injuries About the Shoulder
neurologic injury about the shoulder is paramount for proper treatment
of a patient’s condition. In a patient presenting with complaints of
shoulder pain or weakness, obtaining a thorough history should be the
first step to establish an accurate diagnosis.
numbness, onset of symptoms, progression, timing of symptomatic
episodes, and any improvement with time. The quality, level, and timing
of pain are important factors to document. A visual scale to have the
patient estimate his or her pain during the day and night, and compare
this with the other noninvolved extremity may, be a useful adjunct.
examination should be attempted. If all or part of the neurologic
examination is unable to be completed, adequate documentation of this
should be made. A cursory exam with documentation of “neurovascularly
intact” may attract future litigation. Diagnosis of nerve injury may be
delayed until the patient regains consciousness and becomes cooperative.
and arm is examining the extremity for muscle atrophy. This can be done
only with the shoulder completely exposed, to be able to view the
shoulder and scapula.
performed on any patient who is coherent, even in the setting of
shoulder trauma. Starting the examination at the level of the fingers
and hand is recommended, for most of this part of the exam should be
able to be done with minimal discomfort to the patient. Assessing
median, ulnar, and radial nerve motor and sensory functions should take
little time and should include two-point discrimination measurements to
both aspects of all fingers and thumb. Elbow flexion and extension can
determine musculocutaneous nerve and high radial nerve function by
testing for biceps, brachialis, brachioradialis, and triceps activity.
Axillary nerve function is determined by testing shoulder abduction,
specifically by looking at deltoid contraction with the arm at the
patient’s side. Loss of motor or sensory function in the distal
extremity can also be helpful in locating the area of injury more
proximally. If radial nerve dysfunction is seen distally in combination
with axillary nerve injury (both nerves being branches of the posterior
cord), this is an indication that the injury may have occurred at the
level of the posterior cord of the brachial plexus.
pectoral nerve (clavicular head) and medial pectoral nerve (sternal
head) function. Latissimus dorsi is innervated by the thoracodorsal
nerve and is tested by extending the arm, or contraction with coughing.
Serratus anterior is supplied by the long thoracic nerve and is tested
for by examining presence of winging while the patient forward flexes
the arm such as in a wall push-up. The rhomboids are tested by scapular
adduction and observing for muscle atrophy. The rhomboids, major and
minor, are innervated by the dorsal scapular nerve.
is some patients with both deltoid and supraspinatus separately.
Supraspinatus and infraspinatus muscles are supplied by the
suprascapular nerve and are tested by looking at external rotation
strength and midrange abduction of the shoulder.
part of any shoulder and upper extremity examination. Just as brachial
plexus injury can affect function of the muscles about the shoulder and
arm, injury of the spinal cord and exiting nerve roots can do the same.
Being able to illicit the patient’s symptoms with flexion, extension of
the neck, or with the Spurling maneuver indicates probable cervical
radiculopathy. In upper motor neuron lesions, deep tendon reflexes may
be hyperreflexic, there may be increased tone, and pathologic reflexes
may be present.
such as gall bladder pain should be excluded as a cause of shoulder
pain.
healthy shoulder joint. It is often difficult to elicit whether the
patient’s pain (and weakness) on testing supraspinatus is caused by
rotator cuff injury, internal joint pathology, or true neurologic
injury. In these cases, lidocaine injection of the subacromial space
may provide some benefit in decreasing pain to the area and obtaining a
better examination.
have nonphysiologic examination findings. However these patients cannot
stop the latissimus from contracting while coughing when testing for
latissimus function.
cord. It crosses over the anteroinferior aspect of the subscapularis
muscle near its insertion, then turns posteriorly to cross the
quadrilateral space, where it is in close contact with the inferior
joint capsule. It has been reported to be as close as 10 mm inferior to
the inferior glenoid labrum. When the nerve exits the quadrilateral
space, it branches into two trunks. The posterior trunk branches to
supply teres minor and posterior deltoid, then terminates as the
superior lateral brachial cutaneous nerve. The anterior trunk travels
subfascially, then enters the middle and anterior deltoid to innervate
those muscles. The position of the anterior trunk is reported to be as
close as 4 cm inferior to the anterolateral acromion. Internal
topography studies of the axillary nerve show that on its exit from the
posterior cord, the nerve is monofascicular, but by the time it exits
the quadrangular space, the nerve has distinct fascicles. The deltoid
motor fascicles run superolateral, and the teres minor and sensory
fascicle run inferomedially.
nerve injury to affect the shoulder. It is most commonly seen as a
complication of shoulder dislocation, proximal humerus fracture, or
blunt trauma to the shoulder. The literature reports 5% to 10%
incidence of clear axillary nerve injury with glenohumeral dislocation.
However, at least one study reports electromyography/nerve conduction
study (EMG/NCS) findings in as many as 54% of dislocations, most
patients being subclinical. Fortunately, most patients recover from
their injury spontaneously. Patients who are at a higher risk of
permanent injury are those older than 50 years of age and patients
whose shoulder stays dislocated for >12 hours. The mechanism of
injury is that of direct compression of the dislocated humeral head
against the nerve. Because of the short length of the axillary nerve
from its origin in the posterior cord of the brachial plexus and its
attachment at the deltoid, traction injury may also result at the
infraclavicular brachial plexus.
 |
|
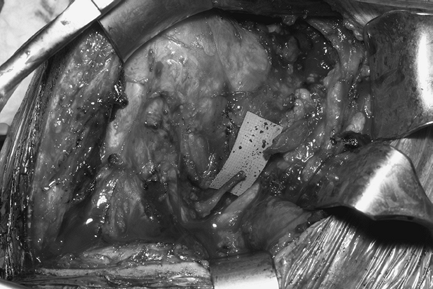
Figure 41-1
An 18-year-old male who dislocated his right shoulder 3 months prior, with no recovery of axillary nerve function. At surgery the axillary nerve was found to be torn. It was repaired with sural nerve grafts. |
to the shoulder without glenohumeral dislocation. Most reports of this
kind of injury show a mechanism of posteriorly directed force from
collisions in football and hockey with similar symptomatology; however,
no isolated axillary nerve ruptures of this type were found reported (Fig. 41-1).
rotator cuff tears associated with neuropathies. Of the 15 patients
evaluated with this combination of injuries, 12 had EMG-demonstrable
axillary nerve injury. Interestingly, only 2 of these 12 patients had
decreased sensation over the lateral shoulder. This study reported that
since the cause of nerve injury was thought to be a traction
neurapraxia, treatment was recommended of rotator cuff repair followed
by a monitored physical therapy protocol. Follow-up EMGs were reported
to have shown significant nerve recovery in the study patients.
compression of the axillary nerve (and posterior humeral circumflex
artery) in the quadrilateral space. Symptoms may present as deltoid
weakness, vague posterior shoulder pain, and tingling and numbness in
lateral shoulder distribution. Compression of the nerve is presumed to
be caused by anomalous fibrous bands, muscle hypertrophy, and mass
effect. Treatment is mostly conservative, with most cases resolving
spontaneously. Exploration and release of impinging structures are
rarely needed.
nerve is also seen as one of many nerves injured in brachial plexus
trauma. In these cases, avulsion or stretch injury of roots, trunks, or
cords of the brachial plexus is the usual site of injury. Isolated
axillary nerve injury in brachial plexus trauma has a reported
incidence between 3% and 6% in the literature.
These procedures include open rotator cuff repair, open and
arthroscopic Bankart procedures, arthroscopic capsular release,
arthroscopic thermal capsulodesis, open reduction internal fixation,
and humeral nail placement for humeral head and neck fractures. The
mechanism of injury varies to include traction injuries, incision or
cautery of the nerve, screw placement through the nerve, and capturing
the nerve with sutures intended to tighten the joint capsule. Incidence
of iatrogenic nerve palsies after plate fixation is reported between 0%
and 5%, whereas incidence of nerve injury after intramedullary nail
placement is between 0% and 4%.
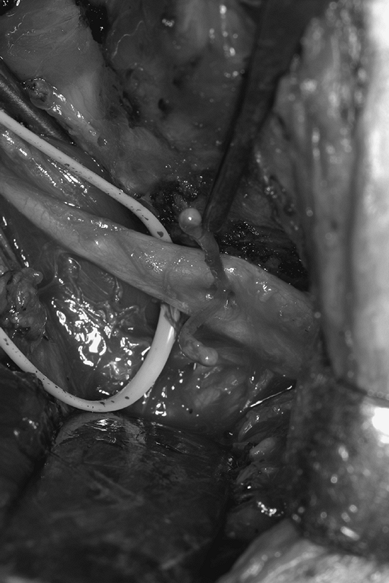 |
|
Figure 41-2
A 21-year-old man underwent prior arthroscopic instability repair. He awoke with severe axillary neuropathy. At surgical exploration, a suture was found compressing the axillary nerve. The suture can be seen dividing the axillary nerve. The suture was removed, and the patient achieved excellent recovery. |
axillary nerve with blind placement of screws for flexible nail
insertion and recommended blunt dissection through the deltoid, direct
visualization of lateral humeral cortex, and use of soft tissue guides
for drilling to protect the nerve.
sharp decline, the close proximity of the axillary nerve to the
inferior glenohumeral joint capsule puts the nerve at a significant
risk of injury owing to high temperatures. These injuries are thought
to be caused by high temperatures in the shoulder joint with the nerve
running as close as 1 cm to the inferior joint capsule. The reported
incidence is 1% to 2% with spontaneous recovery in most cases.
resulting from blunt trauma resolve spontaneously, so in these cases,
it is recommended that nerve recovery should be observed for at least 3
months prior to considering surgical intervention. It is recommended
that a baseline EMG/NCS be obtained at 3 to 4 weeks and repeated at 1
to 2 month intervals to assess nerve recovery. Physical therapy should
be initiated to prevent loss of motion to the shoulder joint. There are
no studies to show that electrical nerve or muscle stimulation speed
recovery. If there are no signs of recovery by 6 months, surgical
exploration with possible nerve grafting is indicated. Because of its
short course through the axilla, cable grafting is the preferred choice
of surgical repair. The axillary nerve is approached via a combined
anterior/posterior incision. The nerve is identified anteriorly at its
origin off the posterior cord and followed posteriorly through the
quadrilateral space. It is then found posteriorly as it branches to
innervate the deltoid and followed anteriorly. Neurolysis is done in
cases where the nerve is shown to conduct with intraoperative direct
electrical stimulation. Nerve grafting is done with preferred use of
sural nerve graft if the nerve is ruptured, retracted, or if neuroma
scarring is too great. Leechavengvongs reported nerve to long head
triceps grafted to axillary nerve deltoid motor branches to reinnervate
an otherwise nonrepairable axillary nerve with excellent results and
rapid recovery.
triceps to very proximal axillary nerve to accomplish the same goal
with inclusion of grafting to the teres minor motor branch.
in neutral abducted position for 2 to 3 weeks, followed by progressive
active and active-assist therapy to regain shoulder range of motion.
Maximal recovery of the nerve is expected at 12 to 18 months from
surgery. One study with 25 patients with axillary nerve repair (most
treated by sural nerve grafting) reported 23 patients obtaining M4 or
M5 strength postoperatively. Neurotization of the nerve is usually done
in massive brachial plexus trauma with thoracodorsal, spinal accessory,
phrenic, and intercostal nerves. These patients have less optimal
recovery.
supplies motor function to the trapezius and sternocleidomastoid
muscles, which is a major scapular stabilizer. It enters the neck
through the jugular foramen and after passing through the
sternocleidomastoid, it crosses the posterior cervical triangle
obliquely to innervate the trapezius on its underside. The posterior
cervical triangle is bordered anteriorly by the sternocleidomastoid,
posteriorly by the trapezius and inferiorly by the clavicle. Although
most motor function to the trapezius is derived from the spinal
accessory nerve, at least some have dual innervation of the upper
portion of the muscle from cervical roots 3 and 4.
ligamentum nuchae superiorly and from the spinous processes of C7–T12.
The muscle can be divided into three portions: upper, middle, and
inferior. It is the upper portion of the muscle that originates from
the ligamentum nuchae, rotating around to become the posterior border
of the posterior cervical triangle, and finally attaching to the
posterior aspect of the lateral third of the clavicle. This part of the
muscle may have alternate innervation from cranial nerves 3 and 4 and
may still remain functional after spinal accessory nerve injury. The
upper portion elevates and upwardly rotates scapula. The middle portion
of the muscle inserts on the medial acromion and the lateral aspect of
the scapular spine and adducts and retracts the scapula. The most
inferior portion of the muscle’s origin is mostly thoracic spinous
processes as far inferior as T12, and insertion is on the medial spine
of the scapula. This portion mainly depresses and rotates the scapula
downward. The spinal accessory nerve gives off branches to innervate
these
different
parts sequentially, which is important in brachial plexus
reconstruction for using the lower branches to neurotize injured
nerves, without losing the elevating function of the upper trapezius
and while preserving neck contour. In this situation, the rhomboids and
serratus can partly compensate for the lost inferior sections with
continued retraction of the scapula.
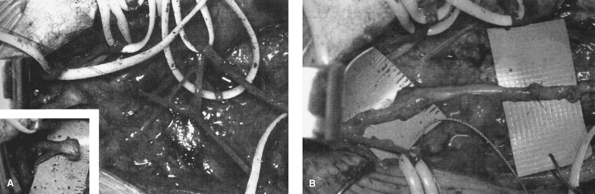 |
|
Figure 41-3 Spinal accessory nerve. (From
Steinmann SP, Spinner RJ. Nerve problems about the shoulder. In: Rockwood CA Jr, ed. The Shoulder. Vol. 2. 3rd ed. Philadelphia: WB Saunders; 2004:1015
, with permission.) |
the scapula, with its action of elevating, rotating, and retracting the
shoulder blade. Loss of this function causes the shoulder to droop and
allows the scapula to rotate downward, outward, and away from the
midline. This causes winging of the scapula and decreases strength and
range of motion in the planes of abduction and forward flexion. As the
shoulder assumes this new position, subacromial impingement now becomes
more likely, as does development of rotator cuff tendinopathy. Other
shoulder stabilizers are overworked, which causes pain and spasm. The
decreased range of motion can also result in a stiff shoulder and may
advance to frank adhesive capsulitis. This, in turn, causes still
active shoulder stabilizers and rotator cuff muscles to work even
harder to compensate, worsening the patient’s pain and spasm. In
addition to the drooping shoulder, atrophy of upper trapezius fibers
may cause a considerable change in the contours of the patient’s
neckline, which usually results in significant self-image problems.
seemingly benign, has significant morbidity, resulting in pain,
disability, and a significantly altered physical appearance. Injury to
the spinal accessory nerve can occur after penetrating trauma to the
shoulder. Blunt trauma to the shoulder and neck region may also injure
the nerve, causing trapezius palsy. However, the most common cause is
iatrogenic laceration after cervical lymph node biopsy, which is
reported to be as high as 3% to 8% in the literature.
the cervical lymph nodes in the posterior triangle of the neck. During
lymph node dissection, the nerve can easily be injured because of sharp
laceration, clipping of nerve thought to be a vessel, or cautery of
fibers.
to the spinal accessory nerve is usually a painful shoulder with some
decreased shoulder range of motion. Patients and treating physicians
may attribute these complaints to postoperative pain. Initially the
trapezius may show minimal wasting, and winging may not be appreciated.
The levator scapulae muscle may be able to compensate and produce a
normal-appearing shoulder shrug. Also, the possibility of a secondary
innervation of the trapezius from upper cervical nerves may confuse the
initial physical examination. As the trapezius becomes more atrophied,
the appearance of the shoulder becomes more obvious, as discussed above.
history of the above symptoms should make the astute physician think of
the possibility of spinal accessory nerve injury. The condition is best
diagnosed by EMG/NCS done, at the earliest, 3 to 4 weeks after injury.
If the nerve injury is recognized within 6 months of the injury, the
recommended plan is exploration with planned neurolysis versus repair
of the nerve, either in primary fashion or with the use of (sural)
nerve graft, depending on intraoperative findings. It is recommended to
have intraoperative electrophysiologic testing available during the
procedure. The preferred timing for surgery is as soon as possible
after injury to the spinal accessory nerve for preservation of best
nerve function; however, successful recovery of trapezius function has
been reported as far out as 1 year.
resulting from blunt trauma, initial EMG/NCS should be done 3 to 4
weeks after injury as a baseline and the patient followed up every 2 to
3 months, looking for resolution of symptoms or improved EMG/NCS
results. If no sign of recovery occurs by the 4- to 6-month time frame,
surgical exploration is an option (Fig. 41-3).
injury) with a history of multiple consultations without a clear
diagnosis. After 12 months, primary repair of the nerve is generally
not useful because of motor end plates degeneration. If the patient
compensated well for his or
her
condition, continued observation is a reasonable option. Some patients,
however, have severe disability and are unable to function with their
resultant level of function. Braces may be offered to these patients,
but they tend to be cumbersome.
in the past with modest results, for the large torsion forces on the
scapula usually tend to stretch and tear such repairs. The current
standard for trapezius reconstruction is the Eden-Lange procedure. This
procedure involves dynamic transfer of the levator scapulae, rhomboid
major, and rhomboid minor muscles. The levator is transferred to the
lateral scapular spine, the rhomboid major as lateral as possible onto
the infraspinatus fossa, and the rhomboid minor either to the scapular
spine or the supraspinatus fossa. Multiple authors reported good
results with this procedure. The salvage operations such as
scapulothoracic fusion should be reserved for patients who either have
failed all the above attempts at stabilization or have
fascioscapulohumeral dystrophy with global loss of shoulder function.
This is an operation with potentially very high complication rates.
rotator cuff function. Its injury causes significant morbidity with
loss of abduction and external rotation of the involved shoulder.
trunk of the brachial plexus; it courses through the posterior triangle
of the neck following the omohyoid under the anterior border of the
trapezius. The nerve enters the supraspinatus fossa through the
suprascapular notch (under the superior transverse scapular ligament),
where it gives off branches to innervate the supraspinatus muscle. Upon
exiting the supraspinatus fossa through the spinoglenoid notch, the
nerve splits off a sensory branch to innervate the posterior joint
capsule and turns medial to innervate the infraspinatus muscle.
tethered are its origin off the upper trunk (the Erb point) and at the
suprascapular notch, where it is noted to be relatively fixed. It may
also be compressed at the level the spinoglenoid ligament as the nerve
courses around the spine of the scapula. It is also here that the nerve
may be as close as 20 mm to the superoposterior glenoid edge.
 |
|
Figure 41-4
Suprascapular nerve compression. Nerve loop holds the suprascapular nerve being compressed by a large ganglion at the suprascapular notch in a 50-year-old man. The cyst was resected, and he achieved excellent recovery. |
blunt trauma sustained to the shoulder, often in occasional with a
fracture of the scapula. A common cause of compression of the nerve is
a ganglion cyst either at the suprascapular notch or at the
spinoglenoid notch. The presumptive origin of these cysts is from
degenerative glenoid labral tears (Fig. 41-4).
The literature also cites many sports as potential predisposing factors
for repetitive-type injury to the suprascapular nerve. The literature
often cites volleyball players as the most commonly affected patients,
but reports have also implicated baseball, tennis, and weight lifting
as possible activities aggravating chronic injury. Parsonage-Turner
syndrome is also a cause of idiopathic supraspinatus palsy. This
condition has certain identifying characteristics and will be discussed
later in the chapter.
nearly identical to those of a rotator cuff tear initially. However,
specific symptoms are dependent on the location of the injury or
compression. When the injury level is at the suprascapular notch or
proximally, patients complain of pain over the posterior and lateral
aspects of the shoulder. They also note significant weakness of
abduction and external rotation. When the site of injury is more
distal, such as the spinoglenoid notch, there is usually less pain
(owing to the fact that the sensory nerve may have split off the main
nerve) and only loss of external rotation strength may be found. Later
as significant muscle atrophy develops, the condition declares itself
more clearly. Even then, supraspinatus atrophy is never observed owing
to the bulk of the overlying trapezius.
show fatty degeneration and atrophy of the involved muscles in the
absence of massive RCT. Although acutely denervated muscles may not
show any significant changes, MRI findings of subacute denervation are
characterized by high signal intensity distributed homogeneously
throughout the denervated muscle on T2-weighed images.
compressive mass of the nerve is known, surgical exploration is
recommended. Most ganglions at the spinoglenoid notch can be reached
and debrided via shoulder arthroscopy, at which time the labral tear
may also be debrided or repaired. A single ganglion noted on MRI with
no neurologic involvement does not need operative resection. Repair of
any associated symptomatic labral tear may be considered, but the
ganglion itself does not need to be debrided. Repair of the labral tear
will often cause the ganglion to resorb over time.
cord of the brachial plexus. It courses through the coracobrachialis in
an oblique medial to lateral direction, entering the coracobrachialis
approximately 5 cm below the coracoid. The nerve then travels in a
lateral direction to send motor branches to first the biceps and then
to the brachialis muscles. Distal to these branches, the nerve becomes
the lateral antebrachial cutaneous nerve to supply the lateral forearm.
glenohumeral dislocations and is occasionally seen as a result of
penetrating trauma (such as knife wounds).
motor and sensory situation with symptoms of weakness of elbow flexion
and with pain and numbness along the radial forearm. However, a pure
sensory syndrome of lateral antebrachial nerve compression may also be
seen, with symptoms exacerbated by vigorous activity and elbow
extension. The sensory nerve is thought to be compressed between the
biceps and brachialis on its exit just lateral to the distal biceps
tendon or by fascial bands in the antebrachial fossa. Treatment is
usually conservative with rest, nonsteroidal anti-inflammatories, and
posterior splint to limit hyperextension of the elbow.
resulting from traumatic or from iatrogenic origin, and no recovery is
seen by the 3 to 4-week mark postinjury, an EMG/NCS can be performed
both for diagnostic purposes and to establish a baseline for following
recovery of the nerve. Since most musculocutaneous nerve injuries are
traction related versus sharp lacerations of the nerve, spontaneous
recovery is expected within the first 3 to 6 months after initial
injury. If no biceps recovery is seen by 6 months, or if initial injury
is suspected to be a frank division of the nerve, surgical exploration
should be performed. After exploration and neurolysis of the involved
nerve segment where the nerve appears to be intact and intraoperative
EMG shows conduction across the nerve segment involved, a further
period of observation for recovery is recommended. If, however, neuroma
scarring or complete laceration of the nerve is found, excision of
scarred nerve segments with interpositional nerve grafting is the
preferred treatment option.
part of brachial plexus injury, or there may be no proximal segment to
graft the nerve into, other reconstructive options for recovery of
biceps function exist. The Oberlin transfer, which transfers one or two
ulnar nerve (wrist flexion) fascicles to the motor branch to the
biceps, is an excellent choice for rapid recovery of biceps function,
owing to the short distance of reinnervation. Recovery of the biceps
has been reported as soon as 3 months from the procedure, with ultimate
biceps strength of M4 in >90% of patients. For patients who do not
have the ulnar or median nerve available because of more extensive
brachial plexus trauma, neurotization procedures from intercostals,
spinal accessory, phrenic, and medial pectoral nerves may be an
available option.
injury, the chance of successful muscle function recovery with nerve
repairs and transfers is significantly decreased. For these patients,
tendon transfer such as the Steindler flexorplasty is recommended. This
procedure requires a functioning brachioradialis (radial nerve), which
is transferred more proximally on the humerus with the plan of
improving elbow flexion. Tendon transfers such as triceps, latissimus,
and pectoralis major and minor are have also been described.
free muscle transfer. Many of these procedures have been performed with
reasonable success, primarily using gracilis to supplement biceps
function. This muscle has a proximal neurovascular pedicle and shape
that is optimal for restoring biceps function. The proximal vessels are
usually connected to the thoracoacromial trunk, with the obturator
nerve branch connected to the spinal accessory nerve with sural graft
extension. The proximal muscle is usually attached through bone sutures
to the distal clavicle and acromion, while distally it is woven into
biceps tendon.
from proximal contributions from cervical roots 5, 6, and 7. The nerve
has a long course along the lateral thorax (26 cm) to its insertion on
the serratus anterior. This muscle originates from the lateral aspect
of the upper nine ribs and inserts along anteromedial scapula, with the
inferior component of the muscle being the most important, inserting
over the inferomedial corner of the scapula. This insertion is
important in stabilizing the scapula on the chest wall and protracting
the scapula in forward flexion and abduction. If this function is lost,
scapular winging is seen with actions such as wall push-ups and
overhead activities (Fig. 41-5). This winging
is different than that caused by spinal accessory nerve injury in that,
with the loss of serratus stabilization, the vertebral border and
inferior pole of the scapula become more prominent This deformity
becomes accentuated with forced forward flexion of the arm.
forward flexion and abduction as well as pain and weakness about the
shoulder. The pain is usually posterior and may result from spasm and
overuse of other scapular stabilizers such as the rhomboids and levator
scapulae. Complaints of initial severe pain followed by atrophy and
winging is commonly seen in Parsonage-Turner syndrome.
the diagnostic workup for any patient who presents with scapular
winging, the best diagnostic test for long thoracic nerve injury is
EMG/NCS. Radiographs, however, may detect the occasional osteochondroma
that may cause compression of the nerve as well as other neoplasms
inside and outside the thoracic cavity. CT scan and MRI are seldom
useful except in cases of neoplasm or cervical disk herniation to make
or refine the diagnosis.
injury, resolve spontaneously. Physical therapy is initiated to
preserve motion and for shoulder-strengthening exercises. Braces are
not considered effective. If there is no improvement seen clinically or
with EMG/NCS after 9 months, and the patient is severely affected by
his or her loss of scapular protraction or by pain, operative
intervention in the form of muscle transfers is a potential option.
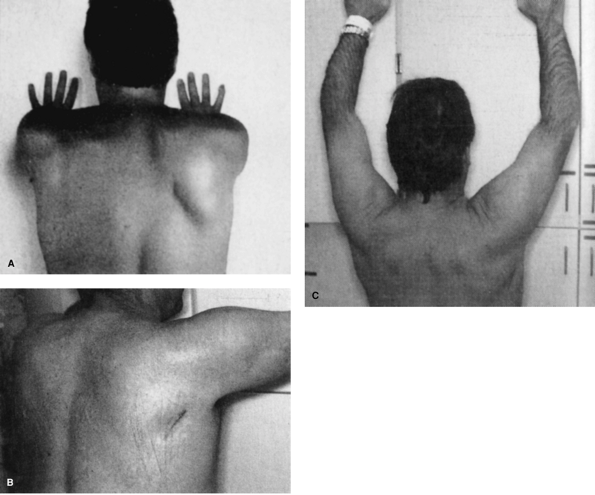 |
|
Figure 41-5
Long thoracic nerve palsy. A complete long thoracic nerve paralysis from Parsonage-Turner syndrome developed in this 36-year-old man. His winged scapula did not improve after 3 years. He had persistent pain in his shoulder and disability when performing overhead maneuvers. A: Prominent right scapula winging is noted preoperatively. B: Postoperatively, the winging has disappeared after pectoralis major transfer. The posterior incision has healed well. C: Postoperatively, his shoulder arc of motion has improved as well. (From Steinmann SP, Spinner RJ. Nerve problems about the shoulder. In: Rockwood CA Jr, ed. The Shoulder. Vol. 2. 3rd ed. Philadelphia: WB Saunders; 2004:1016
, with permission.) |
muscle transfer via tendon interposition graft to the scapula. Graft
choices are autograft or allograft and include fascia lata or hamstring
tendons. Allograft Achilles tendon is a great option, as its proximal
portion drapes over the pectoralis muscle and tendon and its distal
tendon portion provides strong attachment to the scapula.
who failed tendon transfer procedures and continue to be severely
disabled by their condition and for patients with multimuscle atrophy
and weakness such as patients with fascioscapulohumeral dystrophy. This
procedure has a high reported complication rate and may be disabling in
itself owing to severely decreased shoulder motion and variable pain
relief.
neuritis, is thought to be an uncommon condition. Men are more likely
to be affected, with a reported male-to-female ratio ranging between
2:1 and 11:1. Age of presentation is variable, but most patients
present in the third to seventh decades of life.
thought to be inflammatory or immune mediated. Brachial neuritis is
described following a viral illness, immunization, surgery, extreme
exercise, and pregnancy. There is also thought to be an inherited form
of the syndrome known as hereditary neuralgic amyotrophy. Patients
affected with this disorder usually present at an earlier age and may
have
recurrent episodes of what typically appears to be Parsonage-Turner syndrome.
patients describe an initial onset of severe shoulder pain with no
apparent cause. The pain is commonly described as intense and burning
in quality and may last from days to weeks. This painful episode is
followed by progressive muscle atrophy with accompanying weakness and
sensory loss. Fewer patients with atypical presentation complain of
motor and sensory loss but are fortunate enough not to have the initial
painful onset. Muscles innervated by C5 and C6 are most commonly
involved, and the most typically affected nerves include the
suprascapular, axillary, long thoracic, anterior interosseous, and
radial nerves. Brachial neuritis can affect individual nerves or
involve many nerves of the brachial plexus and the cervical region
(such as the spinal accessory nerve) at the same time. Approximately
10% of the cases have bilateral presentation.
made on history, a thorough physical examination, and ruling out other
conditions that may be responsible for the patient’s symptoms. Some
orthopaedic conditions that may have similar presentations and symptoms
include herniated cervical disk, perilabral ganglia, rotator cuff tear,
impingement syndrome, shoulder bursitis, calcific tendonitis, and
adhesive capsulitis. Neurologic conditions that may mimic this
condition include entrapment syndromes also known as inflammatory
demyelinating polyneuropathy, transverse myelitis, and mononeuritis
multiplex. EMG/NCS will identify nerves and muscles involved and will
initially show acute denervation, with fibrillation and positive waves
seen at the 3- to 4-week mark. MRI is useful more to exclude other
diagnoses and will typically show a picture of selective involved
muscle atrophy with increased signal on T2-weighed scans.
as Bell palsy, most patients show spontaneous improvement with time.
However, recovery can be variable, with most patients having residual
effects such as winging. Most patients recover within 3 to 6 months,
but complete recovery may take >12 months. Treatment is supportive,
with nonsteroidal anti-inflammatory medications and other analgesics.
The use of steroids and immunoglobulin therapy has not been shown to be
effective. Physical therapy is recommended to regain range of motion
and to strengthen shoulder girdle muscles. As in all other cases of
permanent deficits described earlier in this chapter, tendon transfers
may be of use to treat long-term disability.
LU, Compito CA, Duralde XA, et al. Transfer of the levator scapulae,
rhomboid major, and rhomboid minor for paralysis of the trapezius. J Bone Joint Surg. 1996;78A:1534–1540.
DC, Yeh MC, Wei PC. Intercostal nerve transfer of the musculocutaneous
nerve in avulsed brachial plexus injuries: Evaluation of 66 patients. J Hand Surg. 1992;17A:822–828.
S, Witoonchart K, Uerpairojkit C, et al. Nerve transfer to biceps
muscle using a part of the ulnar nerve in brachial plexus injury (upper
arm type): a report of 32 cases. J Hand Surg. 1998;23A:711–716.
L. Paralysis of the serratus anterior due to electric shock relieved by
transplantation of the pectoralis major muscle. A case report. J Bone Joint Surg. 1983;45A:156–160.
C, Beal D, Leerhavengvongs S, et al. Nerve transfer to biceps muscle
using part of ulnar nerve for C5-C6 avulsion of the brachial plexus:
anatomical study and report of four cases. J Hand Surg. 1994;19A:232–237.
