Orif: Humeral Shaft Fracture
for approximately 3% of all fractures; most can be managed
nonoperatively with anticipated good to excellent results. Appropriate
nonoperative and operative treatment of humeral shaft fractures,
however, requires an understanding of humeral anatomy, the fracture
pattern, and the patient’s activity level and expectations. This
chapter illustrates open treatment of a humeral shaft fracture using
plate and screws.
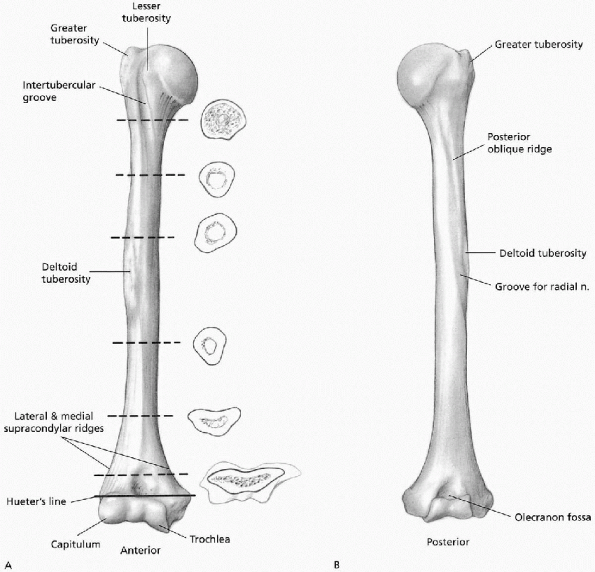
upper border of the pectoralis major insertion to the supracondylar
ridge distally (Fig. 7-1). The proximal aspect
of the humeral shaft is cylindrical on cross section; distally its
anterior-posterior diameter narrows. The anterior border of the humerus
extends from the anterior aspect of the greater tuberosity to the
coronoid fossa. Its medial border extends from the lesser tuberosity to
the medial supracondylar ridge. Its lateral border extends from the
posterior aspect of the greater tuberosity to the lateral supracondylar
ridge. The deltoid muscle inserts onto the deltoid tuberosity, located
on the anterolateral surface of the proximal humeral shaft. The radial
sulcus contains the radial nerve and the profunda artery. The posterior
surface is the origin for the triceps and contains the spiral groove
(see Fig. 6-1).
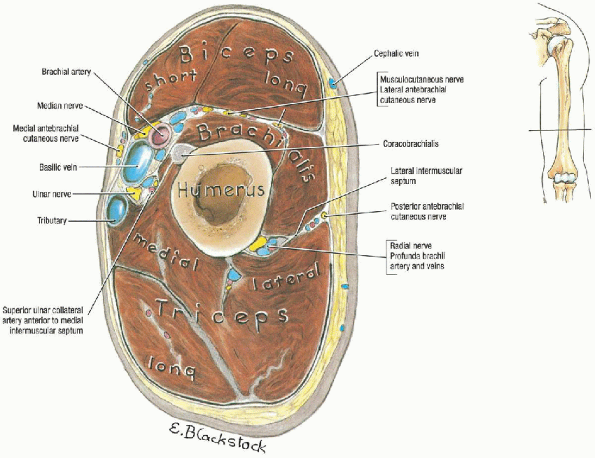
arm into anterior and posterior compartments. The biceps brachii,
coracobrachialis, and brachialis muscles are contained in the anterior
compartment. The brachial artery and vein and the median,
musculocutaneous, and ulnar nerves course along the medial border of
the biceps. The posterior compartment contains the triceps brachii
muscle and radial nerve. The lateral intermuscular septum is perforated
by the radial nerve and the deep branch of the brachial artery. The
medial intermuscular septum is perforated by the ulnar nerve, the
superior ulnar collateral artery, and a posterior branch of the
inferior ulnar collateral artery (Fig. 7-2).
for humeral shaft fractures. Classically, humeral shaft fractures have
been classified on the basis of various factors that influence
treatment such as (a) fracture location (proximal, middle, or distal
third of the humeral shaft), and in addition whether the fracture is
proximal to the pectoralis major insertion, distal to the pectoralis
major insertion but proximal to the deltoid insertion, or distal to the
deltoid insertion; (b) direction and character of fracture line
(transverse, oblique, spiral, segmental, or comminuted); (c) associated
soft tissue injury (open or closed fracture); (d) associated
periarticular injury involving the glenohumeral or elbow joints; (e)
associated nerve injury involving either the radial, median, or ulnar
nerves; (f) associated vascular injury involving either the brachial
artery or vein; and (g) intrinsic condition of the bone (normal or
pathologic)
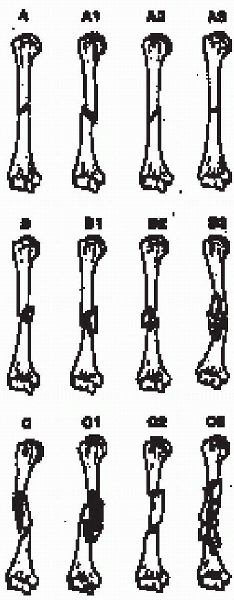
Type A are simple (noncomminuted), type B have a butterfly fragment,
and type C are comminuted. These fracture types are further divided
according to fracture pattern. This alphanumeric classification is used
by both the AO and Orthopaedic Trauma Associations.
-
Open humerus fracture. Open fractures
require emergent débridement; fracture stabilization after soft tissue
and osseous débridement has been reported to reduce the incidence of
infection. -
The humeral shaft fracture with
associated vascular injury is best managed with internal or external
fixation, either before or after vascular repair depending on the
viability of the limb. When vascular repair is needed, nonoperative
management is contraindicated because motion at the fracture may
jeopardize the repair. -
Ipsilateral fracture of the humerus and
radius and ulna (floating elbow). Nonoperative treatment of patients
with a floating elbow has resulted in high rates of nonunion, malunion,
and elbow stiffness. Improved results have been reported after internal
fixation of the humerus and radius and ulna fractures followed by early
range of elbow motion. -
Segmental humerus fracture. Nonoperative
treatment of a segmental humerus fracture is associated with increased
risk of nonunion at one or both fracture sites. -
Pathologic fractures should be internally stabilized to maximize patient comfort and to increase upper extremity function.
-
Operative stabilization of bilateral humerus fractures significantly improves patient self-care.
-
The polytrauma patient is often unable to
remain in the semisitting position necessary to effect fracture
reduction by nonoperative measures. Operative stabilization of the
humerus is necessary to maximize the recovery and rehabilitation
potential of the polytrauma patient. -
Neurologic loss after penetrating injury is an indication for nerve exploration.
-
Fractures that cannot be maintained in
acceptable alignment should be operatively stabilized. In the humeral
shaft, one can accept up to 3 cm shortening, 20 degrees of anterior or
posterior angulation, and 30 degrees of varus. Significant varus can,
however, be cosmetically disfiguring in these individuals; and in those
patients fewer degrees of varus may be accepted. Humeral shaft
fractures in obese patients and women with large pendulous breasts are
at increased risk of
P.76varus angulation. Malrotation is well tolerated secondary to compensatory shoulder motion.
-
Fractures of the humeral shaft associated with intraarticular fracture extension require operative treatment.
 |
|
FIGURE 7-1. Anterior (A) and posterior (B) views of humerus. (From Doyle JR. Arm. In: Doyle JR, Botte MJ, eds. Surgical anatomy of the hand and upper extremity. Philadelphia: Lippincott Williams & Wilkins, 2003:315-364, with permission.)
|
 |
|
FIGURE 7-2. Transverse section through arm. (From Agur AMR, Lee MJ. Grant’s atlas of anatomy, 10th ed. Philadelphia: Lippincott Williams & Wilkins, 1999, with permission.)
|
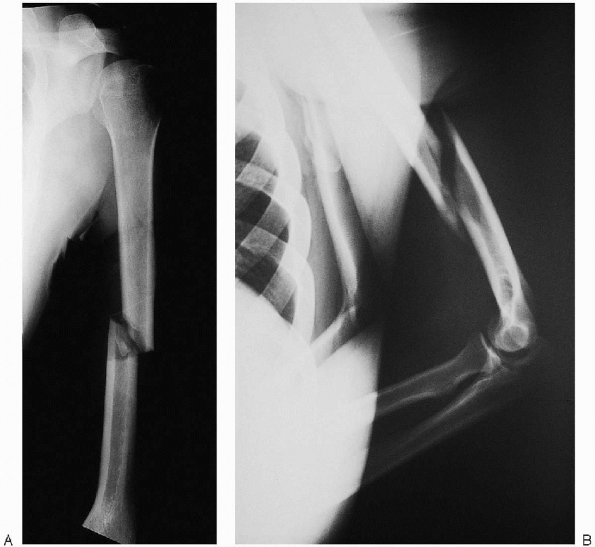
anteroposterior (AP) and lateral radiographs, taken at 90 degrees to
one another. The shoulder and elbow joint should be included in each
view.
rather than simply rotating the injured extremity. In highly comminuted
or displaced fractures, traction radiographs may allow better fracture
definition. Comparison radiographs of the contralateral humerus are
helpful for preoperative planning. Tomograms and computed tomography
are rarely indicated. In pathologic fractures, additional studies
(technetium bone scan, computed tomography, and magnetic resonance
imaging) may be necessary to delineate the extent of disease before
fracture treatment.
major fracture fragments, should be determined before one attempts
definitive surgical intervention. Identification of the individual
fragments is often facilitated with traction radiographs. Radiographs
of the opposite, uninjured extremity serve as a template for
preoperative planning; the individual fracture fragments, chosen
implant, and surgical tactic can be drawn on the intact humeral
template. This requires the surgeon to understand the “personality of
the fracture” and to mentally prepare for the operative procedure.
 |
|
FIGURE 7-3.
The AO/ASIF classification of humeral shaft fractures. (From Zuckerman JD, Koval KJ. Fractures of the shaft of the humerus. In Rockwood CA Jr, Green DP, Bucholz RW, et al., eds. Rockwood and Green’s fractures in adults, 4th ed, vol 1. Philadelphia: Lippincott Williams & Wilkins, 1996:1025-1053, with permission.) |
 |
|
FIGURE 7-4. Anteroposterior (A) and lateral (B) radiographs demonstrating a displaced humeral shaft fracture.
|
 |
|
FIGURE 7-5.
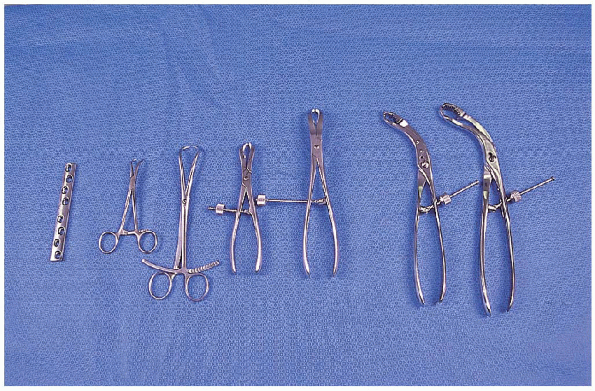
The instruments necessary for open reduction and internal fixation of the humeral shaft: 4.5-mm broad dynamic companion peak (DCP), small and large reduction clamps (2), Verbrugge clamps (4). |
internal fixation of a humeral shaft fracture plate and screws include
the following (Fig. 7-5):
 |
|
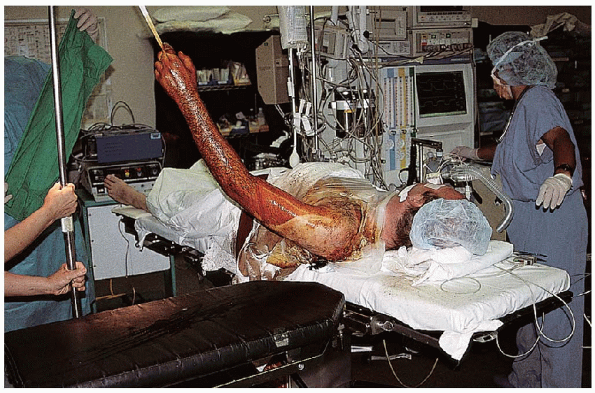
FIGURE 7-6. Supine patient positioning with use of a hand table. The upper extremity is elevated for the surgical prep.
|
 |
|
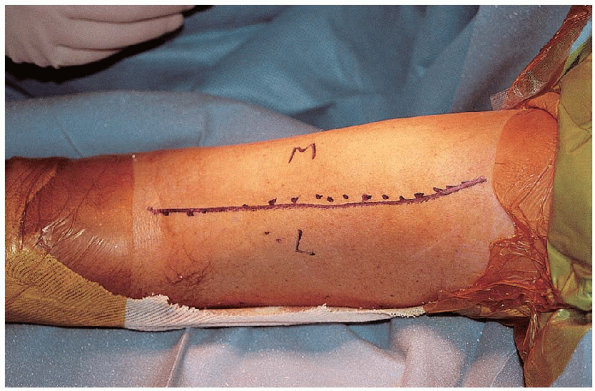
FIGURE 7-7. The incision is made along the lateral border of the biceps, ending just proximal to the elbow flexion crease.
|
-
Small fragment plate and screws
-
Large fragment plate and screws
-
Large and small reduction clamps
-
Verbrugge clamps
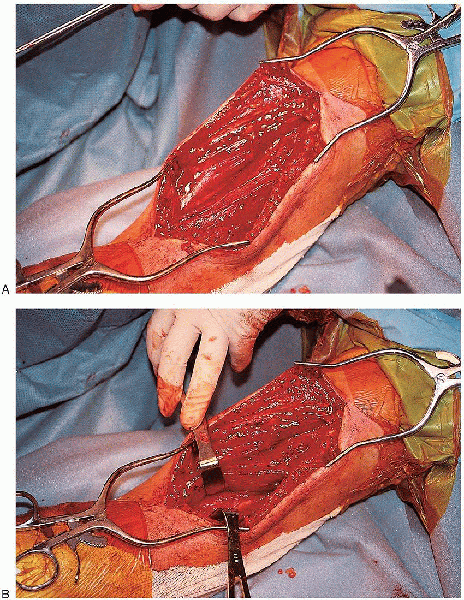
most fractures, I prefer an anterolateral approach to the humerus. An
incision is made along the lateral border of the biceps, ending just
proximal to the elbow flexion crease (Fig. 7-7). The lateral border of the biceps is identified,
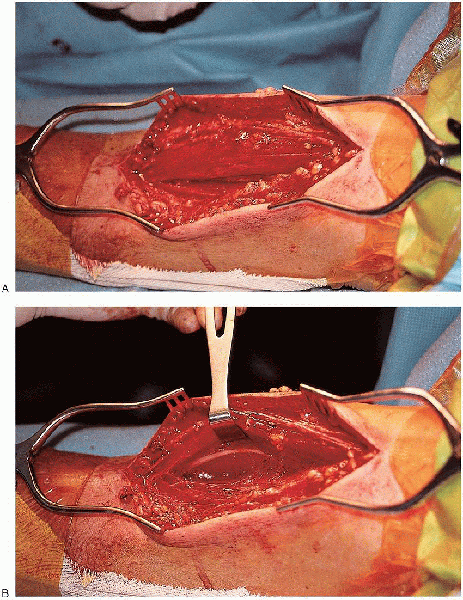
 and the muscle retracted medially (Fig. 7-8).
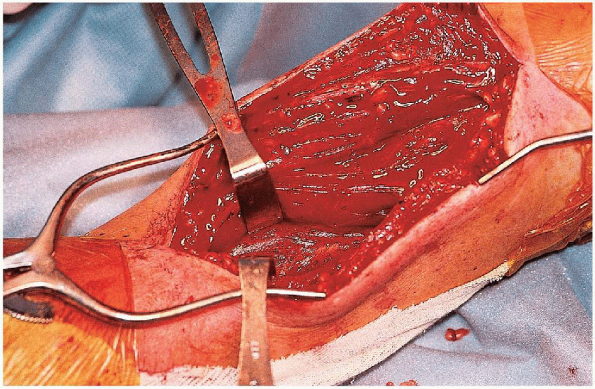
and the muscle retracted medially (Fig. 7-8).  The interval between the brachialis and brachioradialis is identified proximal to the elbow and the two muscles separated (Fig. 7-9).
The interval between the brachialis and brachioradialis is identified proximal to the elbow and the two muscles separated (Fig. 7-9). 
The brachioradialis is retracted laterally, and the brachialis and
biceps muscles are retracted medially. The radial nerve lies between
the brachialis and brachioradialis and must be identified (Fig. 7-10).

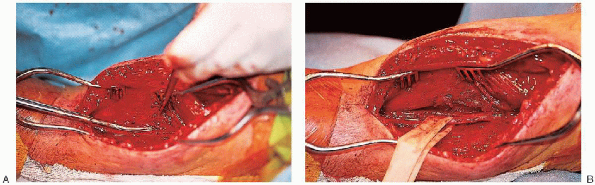
The radial nerve is traced proximally through the lateral intermuscular
septum and protected throughout the remainder of the procedure (Fig. 7-11).
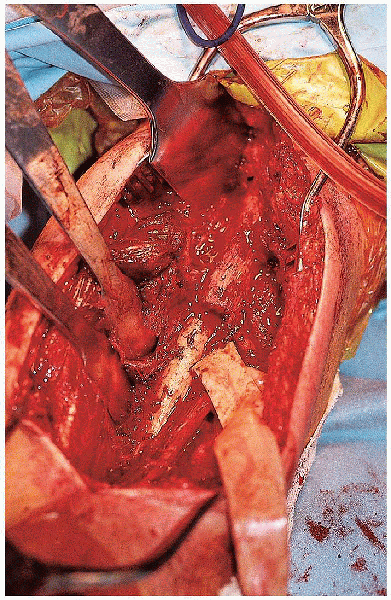
The periosteum is incised longitudinally at the lateral border of the
brachialis muscle, and the humerus is dissected subperiosteally (Fig. 7-12).

The anterolateral approach can be extended proximally into an anterior
approach to the shoulder and distally to an anterior approach to the
elbow.
 |
|
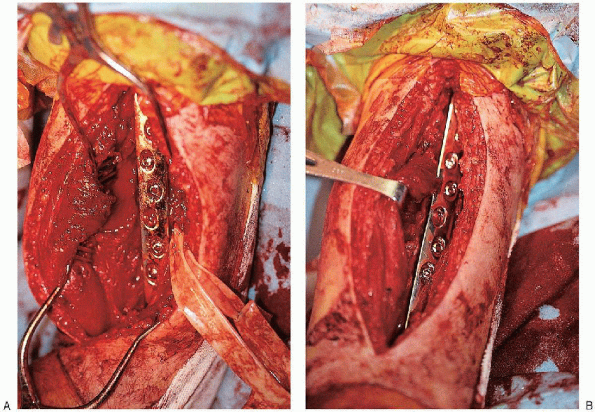
FIGURE 7-8. The lateral border of the biceps is identified, and the muscles are retracted medially (A and B).
|
 |
|
FIGURE 7-9. The interval between the brachialis and brachioradialis is identified proximal to the elbow and the two muscles are separated (A and B).
|
 |
|
FIGURE 7-10. Identification of the radial nerve between the brachialis and brachioradialis muscles.
|
 |
|
FIGURE 7-11. A: The radial nerve is traced proximally through the lateral intermuscular septum. B: A Penrose drain is then placed around the nerve.
|
 |
|
FIGURE 7-12. Exposure of the humeral shaft fracture.
|
fracture is exposed, evaluated, débrided of hematoma, and anatomically
reduced. Minimal soft tissue stripping should be performed; butterfly
fragments must not be devitalized. Provisional stabilization is
performed using reduction clamps or Kirschner wires. A 4.5-mm broad
dynamic compression plate is usually selected for midshaft fractures (Fig. 7-13).

In smaller patients, a 4.5-mm narrow dynamic compression plate may be
used. If the fracture pattern permits, the plate should be applied in
compression.
 Lag screws should be inserted through the plate whenever possible (Fig. 7-14). Eight to ten cortices fixation proximal and distal to the fracture should be obtained (Fig. 7-15).
Lag screws should be inserted through the plate whenever possible (Fig. 7-14). Eight to ten cortices fixation proximal and distal to the fracture should be obtained (Fig. 7-15).  Fixation stability must be assessed before closure (Fig. 7-16).
Fixation stability must be assessed before closure (Fig. 7-16). 
The need to bone graft is determined by the amount of comminution and
soft tissue stripping. In general, one should have a low threshold for
cancellous bone grafting of these fractures when plates and screws are
used. One should obtain final radiographs once surgery is completed (Fig. 7-17).
 |
|
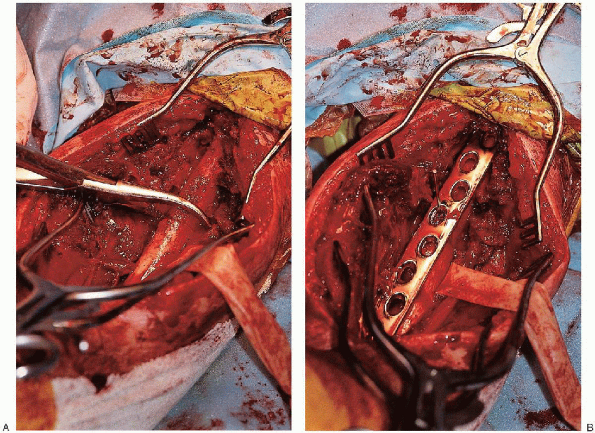
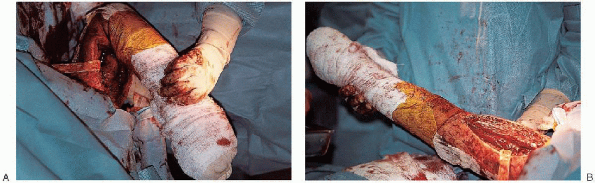
FIGURE 7-13. Provisional fracture fixation first using a reduction clamp (A) and then a broad compression plate (B and C). (continued)
|
to achieve maximal functional outcome after both operative and
nonoperative humeral shaft fracture management. Early and vigorous
postsurgical range of motion exercises of the hand and wrist should be
strongly urged. As shoulder pain diminishes, range of motion exercises
for the shoulder and elbow are initiated. As union progresses,
supervised exercises
to
recover upper extremity strength are started. Caution is warranted
relative to management of the elbow; it should not be passively
stretched. Myositis ossificans, which has been reported around the
elbow following humeral shaft fracture, can be prevented by exclusively
using active range of motion exercises.
 |
|
FIGURE 7-13. (Continued)
|
 |
|
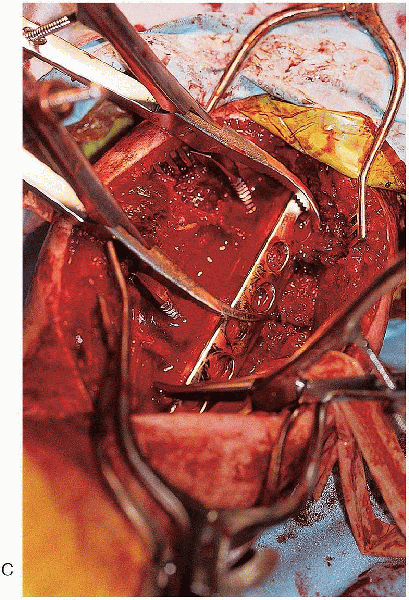
FIGURE 7-14. Placement of a lag screw through the plate (A to C). (continued)
|
 |
|
FIGURE 7-14. (Continued)
|
 |
|
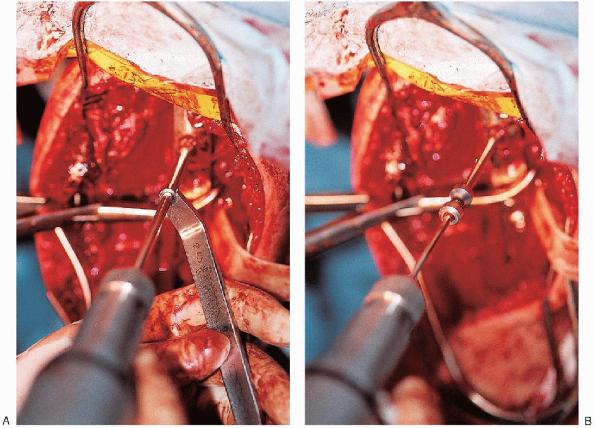
FIGURE 7-15. Final fracture fixation with insertion of the remaining screws (A and B).
|
 |
|
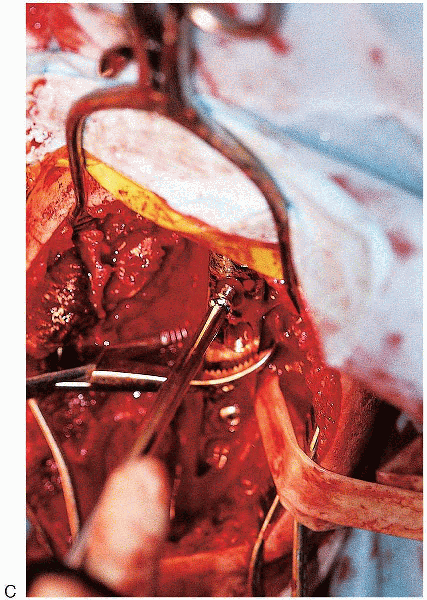
FIGURE 7-16. Placement of the arm through a range of motion to assess fracture stability.
|
 |
|
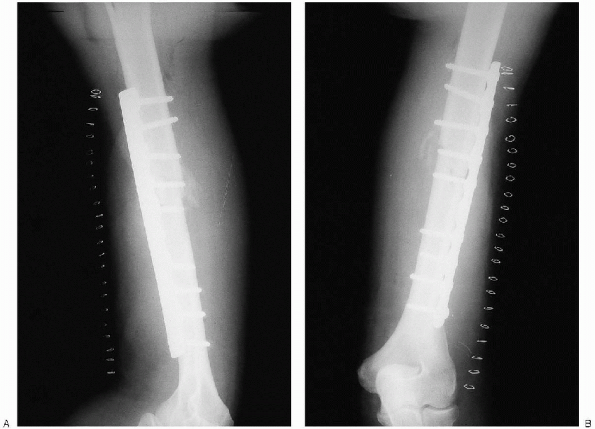
FIGURE 7-17. Final intraoperative radiographs (A and B).
|
