The Orthopaedic Recognition of Child Maltreatment
part of a parent or caretaker which results in death, serious physical
or emotional harm, sexual abuse or exploitation; or an act or failure
to act which presents an imminent risk of serious harm.253 Child maltreatment includes all types of abuse and neglect that occur among children under the age of 18 years.202 The four common types of maltreatment include physical, sexual, and emotional abuse as well as child neglect.121 Neglect is the most frequently encountered type of child maltreatment.75
Recent terminology for a battered child, physical abuse, or child abuse
include nonaccidental injury (NAI), inflicted injury, or nonaccidental
trauma (NAT).88
(NCANDS) was initiated in response to Public Law 93-247 to collect and analyze child abuse statistics.254
NCANDS documents that the epidemic of child abuse continues to worsen
in the United States, with approximately 3.6 million reports (47.8 per
1000 children) filed in federal fiscal year 2006 compared to 1.2
million in 1982.253 Approximately
one quarter of these children who received an investigation were
confirmed to have been abused or neglected. This represents a victim
rate of 12.1 per 1000, totaling 905,000 U.S. children in 2006.253 Approximately 60% of confirmed cases are neglect, 16% physical abuse, 10% sexual abuse, and 7% psychologic abuse.202
Reports by professionals are more likely to be confirmed. Whereas
children under the age of 4 years are at greatest risk for
maltreatment, the victim rate is highest for infants, totaling 91,278
(23.2 per 1000 population over the course of less than 1 year).
Newborns in the first week of life may be at the highest risk, with a
total of 29,881 reported cases, 70% of which were reported for neglect.202
with 50% to 80% having evidence of a prior injury. The World Health
Organization estimates that 57,000 children world-wide die from
maltreatment, while more than 1500 die in the United States.149 However, mortality rates are commonly underestimated.65,108
Nineteen percent of maltreatment fatalities occur in infants; whereas,
newborns in the first week of life have greatest risk of death.202
Abuse is second only to sudden infant death syndrome (SIDS) for
mortality in infants 1 to 6 months of age and second only to accidental
injury in children older than 1 year. The incidence of abuse is three
times that of developmental dysplasia of the hip or clubfoot.
Fortunately, there is some evidence that abusive fracture incidence may
be decreasing over the past 24 years, possibly due to a general
increase in recognition of child maltreatment and more preventive
services available to families.158
but additional costs, both direct and indirect, exist. The estimated
national cost of child abuse for the child welfare system is 14 billion
dollars, law enforcement 24 million, and the court system 341 million.201
The long-term social costs of child abuse are substantial: one third of
the victims of child abuse grow up to be seriously dysfunctional,
neglectful, or abusive parents; one third are at high risk for
eventually becoming abusive parents; and only one third do not repeat
the destructive patterns they were exposed to as children.188,234 Exposure to adverse childhood experiences has a high probability of both recent and lifetime depressive disorders.56
Direct and indirect total estimated national costs of child abuse,
including special education for learning disorders of abused children,
maternal mental and health care, legal costs of juvenile delinquency,
lost productivity to society of abused and neglected children as
unemployed adults, and later adult criminality of abused and neglected
children in 2007 is 103.8 billion dollars.
Early recognition by the orthopaedist is critical because children
returned to their homes after an unrecognized episode of child abuse
have a 25% risk of serious reinjury and a 5% risk of death.212 Jenny and Isaac123
have noted a three fold increased mortality rate of children who have
been listed on state abuse registry for all types of abuse. The
mortality rate is highest for those who are physically abused,
especially infants.123
described 6 infants with long-bone fractures, chronic subdural
hematomas, and intraocular bleeding without a history of trauma to
explain the injuries; however, he did not speculate about the etiology
of the children’s injuries. Although his work is cited as the first
report in the English literature of child abuse, it was Ambroise
Tardieu, the prolific French forensic physician, who during the mid
1800s described in great detail the condition of sexual abuse in
children, as well as the battered child syndrome.151 In 1953, Silverman222
characterized the unique metaphyseal fractures found in abused children
and clearly emphasized that these were due to nonaccidental trauma.
Altman and Smith8 published the
first series in the orthopaedic literature of injuries caused by child
abuse in 1960. General public awareness of child abuse increased with
the 1962 publication of a report by Kempe et al.130 characterizing the problems as the battered child syndrome. In 1974, Caffey44
introduced the term “whiplash-shaken infant syndrome” to the literature
to emphasize the etiology of subdural hematomas in infants caused by
shaking episodes. In 1974, Congress acknowledged the national
importance of the prevention of child abuse by the passage of the Child
Abuse Prevention and Treatment Act.254
Since pediatric personnel and hospital-based child protection teams
must be aware of reporting requirements for child maltreatment, there
are published guidelines for the establishment and management of
hospital-based child protection teams.180
turmoil from marital separation, job loss, divorce, family death,
housing difficulties, or financial difficulties are more likely to have
abusive episodes.77 One of the most
important predictors of abuse is the presence of a nonrelated adult
living in the household. Compared to single parent families, death due
to child abuse was noted to be 50 times higher in households that had
unrelated adults; the perpetrator was the unrelated adult in 83.9% of
these cases.213 Families with two
unplanned births are 2.8 times more likely to have an episode of child
abuse than families with no unplanned births.265 Stepparents, babysitters, boyfriends, relatives, and even larger siblings may be abusers.4,109,185
Young, unmarried mothers are more likely to have an infant death from
intentional injury, with a peak incidence of 10.5 intentional deaths
per 10,000 live births.218 In a study of 630 fractures in 194 abused children, the perpetrator was identified in 79% of cases.230
Sixty-eight percent of the perpetrators were male, and 45% of the time
the biologic father was responsible. Abused infants were significantly
younger (4.5 months of age) when a male had abused the child, than when
a female was the abuser (10 months of age). The parents of battered
children may themselves have been abused when they were children.95 High levels of parental stress and belief in corporal punishment are associated with child abuse.64 Parental substance abuse, whether alcohol or other drugs, makes child abuse more likely.105 The risk of physical abuse is fivefold more
likely with maternal cocaine use.255
Violence in the home is not directed solely toward the child. In one
study of families with substantiated child abuse, 30% of the mothers
had also been abused.45 Although the
youngest, poorest, most socially isolated, and economically frustrated
caretakers are the most likely to act violently toward their children,260 any adult from any social or economic level may abuse a child.4
Daycare may be an at-risk environment in situations when there is poor
supervision of the child caregivers. However, in an analysis of 1362
deaths in daycare, home daycare was a much higher risk than was a
formal institutional daycare due to less training and supervision of
the adult caregivers and the absence of adult witnesses.261 Primary parental predictors of child abuse are listed in Table 7-1.
78% of all fractures reported were in children younger than 3 years of
age and 50% of all fractures occurred in children younger than 1 year
of age. Infants younger than 1 year are especially at risk for infant
homicide, the most severe form of child abuse.70,136 The problem may be more widespread than suspected. In one report,33
covert video recordings of adults attending their children who were
hospitalized for suspicious illness documented 14 separate instances of
caretaker attempts to cause upper airway obstruction. An infant may
present to the emergency room dead or near dead after an apparent “life
threatening event.” In these cases, it is important to be open to all
diagnostic possibilities and use a multidisciplinary team approach to
the evaluation.182 Possible
explanations for these events include SIDS, metabolic disease, cardiac
disease, infection, as well as accidental or nonaccidental suffocation.
Up to 11% of infants treated in the emergency room for apparent
life-threatening events are later confirmed to be victims of child
abuse.37 Firstborn children,
premature infants, stepchildren, and disabled children are at a greater
risk for child abuse, as are twins and children of multiple births.29 Benedict et al.,30
in a longitudinal study of 500 disabled children followed from birth to
age 10 years, documented a 4.6% incidence of physical abuse. The most
severely disabled children were less likely to be abused, whereas
marginally functioning children were at greater risk, with parental
frustration considered to be a factor.
|
TABLE 7-1 Parental Predictors of Child Abuse
|
||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||
medical assessment of vague illness and have a history of multiple
diagnostic or therapeutic procedures for unclear reasons are at risk
for having a form of child abuse known as “child abuse that occurs in
the medical setting.”233 This term has replaced the previously used “Münchhausen Syndrome by Proxy,”174
which was named after Baron von Münchhausen, an eighteenthcentury
mercenary whose exaggerated tales of adventure were viewed with great
suspicion. In child abuse that occurs in a medical setting, children
become the victims of this adult behavior when misguided parents
fabricate a wide range of illnesses for their children, often
subjecting them to needless diagnostic workups and treatment.174
Symptoms of the child’s “illness” are based on an imaginary medical
history given by the parent, with signs of the illness either simulated
or induced by the parent. For example, a child may be brought into the
emergency room by a parent with a complaint of vomiting. This complaint
may either be a total fabrication by the parent or the parent may
simulate the complaint by producing “vomitus” from some source as proof
of illness. In one report, bloodstained material was presented by a
caretaker as proof of a child’s “gastrointestinal bleeding,” but DNA
testing revealed that the source was actually from the caretaker.256 Conjunctivitis from a caustic agent placed on an infant by a caretaker has been reported.27 Children have been given clozapine and clonidine by caretakers to simulate illness.26 A parent has caused vomiting in a child by the administration of salt173 or ipecac. In other extreme cases, a rodenticide-induced coagulopathy was seen in a 2-year-old child,17 a deliberate self-induced preterm labor was caused by a parent,93 and another repeatedly gave insulin to a 1-year-old child.174
Over half of reported cases of child abuse in the medical setting
involve induced symptoms, whereas 25% involve a combination of both
simulation and induction of symptoms.37
In less severe cases, the parent’s anxiety can cause them to obtain
unnecessary and harmful or potentially harmful medical care, even
though the parent believes that he or she is acting in the child’s best
interest. Physicians need to be vigilant so as not to be an unwary
participant of this form of child maltreatment.
Caretakers often have a medical background: 35% to 45% are nurses, 5%
are medical office workers, 3% are social workers, and 1% are orderlies.209
The perpetrator of the child’s illness denies the knowledge of its
etiology; however, the acute signs and symptoms of the child’s illness
will resolve if the syndrome is recognized and the child is separated
from the parent.209
Follow-up of families with this disorder is crucial. Failure to
diagnose this condition places a child at risk for either serious
long-term sequelae or death in approximately 9% of cases.
remains difficult. Healthcare workers must have a high degree of
suspicion when children present with repetitive illness with no
physiologic explanation. Physicians need to recognize that their
perseverance in finding an explanation to a child’s illness may
contribute to the inflicted harm to the child. When possible, a
pediatrician with experience in child abuse should become involved in
the evaluation as well as the hospital or community-based
multidisciplinary child protection team. A thorough review of all the
medical care received by the child and communication among team members
is necessary to establish the diagnosis and to recognize patterns of
parental behavior that may harm the child. Covert in-hospital video
surveillance (CVS) of caretakers with their children may be a valuable
means to substantiate or disprove this diagnosis. Hall et al.97
reported that CVS with audio surveillance allowed diagnosis in 56% of
patients monitored and was supportive of the diagnosis in another 22%
of children. The approach is expensive, is not covered by third party
payers, and so is infrequently used. Effective treatment generally
involves assuring the safety of all children in the family and
addressing ongoing dysfunctional family behaviors.
in the context of fractures and other obvious injuries, an increasingly
important situation to recognize is sexual abuse. It is estimated that
25% of abused or neglected children have been sexually abused.150
Physically abused children have a 1 in 6 chance of being sexually
abused, whereas sexually abused children have a 1 in 7 risk of being
physically abused.110 Children
living with nonbiologic parents or with caretakers who are substance
abusers are most at risk. The child usually discloses sexual abuse
under three types of circumstances: the child may have just experienced
an argument with the abuser and may “accidentally” reveal the existence
of the abusive relationship, the child is permanently separated from
the abuser, or the abusive adult is shifting attention to a younger
sibling.259 Up to 25% to 83% of children with a disability have been reported to be abused.239
which is a team effort with the consulting pediatrician, social worker
and other personnel from the hospital’s child protective team, child
protective services worker, law enforcement, and the appropriate
consulting service. The orthopaedic surgeon is involved if the child
has an injury to the musculoskeletal system. The history is usually
taken in the chaotic environment of a busy emergency room, so it is
important to find a quiet area for the interview to be conducted calmly
and with minimal distractions. The orthopaedic surgeon should focus on
the facts of the injury, including the child’s ability to get into the
injury scenario, details of when, where, and what happened, the child’s
position and action before the injury, position after the injury, how
the child reacted, and how promptly the caregiver responded
appropriately. Such detailed interview skills rarely are taught during
residency training. In a survey of pediatric residents, 42% of them had
1 hour or less in training for detection of child abuse, and most
orthopaedic residents likely have even less.76
In a study comparing the documentation of physical abuse between 1980
and 1995 in a teaching hospital, very little improvement was noted.161
Little progress has been made in how frequently physicians inquire
about basic historic information such as the timing of the injury and
who were the witnesses.13 The type of hospital that an injured child visits also influences the likelihood that a diagnosis of abuse will be made.251,252
General hospitals were less likely to diagnose a case of abuse compared
to children’s hospitals. Use of a structured clinical form can increase
the information collected to support the diagnosis of child abuse.21
Having received recent continuing medical education focused on child
abuse was the most important factor for a physician to properly
recognize and report child abuse.84
Precise documentation in child abuse is vital for reasons beyond
medical care. Although most subpoenas for testimony by physicians in
child abuse cases do not result in courtroom appearances,193
all documentation in child abuse cases may become evidence in courtroom
proceedings. Thus, detailed records are helpful to all in courtroom
testimony by physicians.100 The
history needed to document child abuse is termed the investigative
interview, is a team effort, and should be led by members of the child
protective team and the police when potential child abuse is
investigated.
detailed musculoskeletal history and physical examination to
characterize the features and mechanism of the obvious injury and to
discover evidence of additional undocumented injuries. The interview
documents the history (or the lack of history) of the presenting injury
and attempts to uncover enough details about the child’s life so that
plausible scenarios can be evaluated that might explain the injury. The
team should determine how the injured child lives, find out which
family members, friends, or other caretakers have access to the child,
and how likely it is that they might have contributed to the child’s
injuries. A detailed history of injury is obtained individually from
each adult family member in a private setting. If the patient and
siblings can communicate, they should be interviewed separately from
the parents and other members of the family. The location where the
injury occurred and which individuals were actually present are
documented. The interviewer should follow a systematic review of
symptoms: what happened, who was there, when the injury was recognized,
and how long before medical treatment was sought. To avoid provoking
emotions, any additional soft tissue or skeletal trauma discovered
should be brought up at the end of the interview for explanation once
the presentation injury has been thoroughly discussed.
An infant who has sustained abusive head trauma (AHT) typically will
develop immediate neurologic change and will invariably show symptoms
within a few hours.35 For a child
with head trauma, a caregiver’s story that there was a long period
after the injury in which the child had no symptoms is suspect. When
central nervous injury in child abuse is significant or severe, it is
immediately symptomatic; thus, the last caretaker who witnessed the
reported injury or found the child immediately after the injury is
highly suspected
of being the perpetrator.23
Inconsistencies are not challenged during the interview. Leading
questions are avoided in favor of open-end questions. Medical terms
should be explained in plain English, with care taken to avoid medical
jargon. More plausible explanations for the injury are not volunteered.
Open prompts can enhance the interview.190
If the injury was observed, the caregiver should be able to give a
detailed description of the injury mechanism that fits the energy of
the fracture and the clinical picture.198,199
The crucial questions to be answered are not only whether the given
history of trauma is sufficient to explain the severity of injury, but
what other possible scenarios could explain the injury if the
volunteered explanation is not plausible. This requires obtaining a
working knowledge of the child’s environment, which team members can
obtain by asking specific, detailed questions (Table 7-2).
be as gentle as possible, asking how they got hurt rather than who hurt
them. Questions asked should be appropriate for the child’s age. The
child’s account of what he or she was doing at time of injury should be
compared with the accounts of the adult witnesses. If possible, the
siblings of the injured child should be interviewed because they also
are at risk for child abuse. Nonvisual cues during the interview should
be noted (see Table 7-2).
|
TABLE 7-2 Child Abuse: Investigative Interview
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
surgeon or child abuse team must determine if the history of trauma is
adequate to explain the severity of injury.53
This should be based on experience in the care of fractures with
knowledge of their mechanisms of injury and special insight into the
types of trauma most likely to cause significant injury. In addition,
it is extremely important to have knowledge of the developmental
abilities of a child when a caretaker states the child’s injuries are
self-inflicted.125 For example, if
the parents explain that a 4-month-old infant’s femoral fracture
occurred in a fall while the infant was standing alone, this history is
inconsistent with the child’s developmental ability.
carefully considered. Although it is not unusual for a young child to
sustain an accidental fall, it is unusual to sustain a serious injury
from that fall alone. Infants fall from a bed or a raised surface
during a diaper change fairly frequently. In a study of 536 normal
infants,148 nearly 50% of them had
fallen accidentally from an elevated surface, usually after the first 5
months of life, when the children were able to roll over and were more
active. Significant injury in such falls is, however, extremely rare.
Combining two studies of 782 children younger than 5 years of age who
accidentally fell off an elevated surface, such as bed or sofa, reveals
that injuries were limited to three clavicle fractures, six skull
fractures, one humeral fracture, and one subdural hematoma.106,146
In another report, a much higher rate of fracture was seen in falls
from furniture with 98% having fractures, mostly in the upper
extremity, due to the child catapulting during play activity rather
than sustaining a simple short height fall.107
More severe injuries occur in falls from greater heights. Stairway
falls usually result in low-energy injuries, but there is increased
risk of injury if the child is being carried by the caregiver. In a
report of 363 stairway injuries,131
10 were infants who were dropped by their caretakers and four of those
sustained skull fractures. In patients 6 months to 1 year of age, 60%
were using walkers at the time of the stairway injury. Only 4% of
patients had extremity fractures and 1% had skull fractures. Reported
short height falls (<1.5 meters) are rarely documented to cause
death.52 A review of child mortality
in infants and young children in California showed the following causes
of death/l million children/year: prematurity 165, congenital
malformation 316, neoplasms 33, respiratory 38, accidents 121, homicide
22, and short-height falls 0.48 (a total of six cases, all occurring in
the home). Although short-height falls are a rare cause of death, there
has been no reported case of shortfall death in an institution-type
daycare setting, where witnesses are typically present. A fatally
injured child from a reported short-height fall at home must receive
expert postmortem investigation for child abuse.
may be obtained by a review of past medical records or by contacting
the patient’s primary physician and social workers who may have been
involved with the family. The physician or social worker should be
asked if there has been any previous pattern of injury, illness,
ingestion of objects or medications, or noncompliance with healthcare
recommendations; whether the family is receiving counseling or other
support from any community groups; and whether the family has any
previous involvement with child protective services or law enforcement.77
be presented as evidence in court for either custodial hearings or
criminal trial.161 Defending
inaccurate or partial chart notes in court can be extremely
embarrassing as well as placing the child at additional risk. Each
account should be recorded in as much detail as possible, using
quotation marks for exact quotes and specifying who is giving the
history. Particularly with crucial answers, the exact question
preceding the response should be documented. In a study of subsequent
confessions, the initial history, although not consistently true, did
reveal some elements of truth.83 In
addition, the general emotional state of the individual providing the
account, as well as the individual’s reaction to emotionally charged
questions should be documented to assist in later evaluation of the
credibility of the account. If the family wishes to change their story
after the initial account, no changes should be made to the earlier
record, but an addendum should be placed detailing the new account. The
completed record should include several specific items such as the
timing and mechanism of the injury, who found the child, timing of
events, family history of underlying conditions such as osteogenesis
imperfecta, radiographs, and documentation of protective services
involvement.
fracture assessment, a detailed physical examination should follow,
systematically evaluating from head to toes, to detect any signs of
additional acute or chronic injury. Acute and subacute fractures may
cause local tenderness and swelling, whereas chronic fractures may
produce swelling from the presence of callus and clinical deformity
from malunion. Radiographs are obtained to confirm clinically suspected
fractures. A skeletal survey must be performed in children under 2
years of age when there is reasonable suspicion of abuse12:
it should be considered an extension of the physical examination for
this age group. A thorough examination should focus on the body areas
commonly involved in child abuse including the skin, central nervous
system, abdomen, and genitalia. Careful evaluation for signs of
previous injury is useful since 50% of verified abuse cases show
evidence of prior abuse.95
acute fracture site for swelling and bruising, the patient’s entire
body should be systematically evaluated to detect acute and chronic
soft tissue trauma. Deliberate soft tissue injuries are present in 81%
to 92% of abused patients,91,171,241
making them the most common abuse-related physical examination finding.
The types of skin lesions commonly encountered include bruises, welts,
abrasions, lacerations, scars, and burns.
child’s development. Seventeen percent of mobile infants, 53% of
toddlers, and most school children have bruises.166 Young infants have a much lower prevalence of accidental bruising (seen in 1%) compared to mobile toddlers.166 Accidental bruises in babies are also typically noted over bony prominences.47 The toddler may have multiple accidental bruises over bony prominences such as the chin, brow, knees, and shins.4,212,237 Bruises on the back of the head, neck,4
arms, legs, buttocks, abdomen, cheeks, or genitalia may be suspicious
for abuse, although accidental bruises can also occur in all these
locations.8 Accidental bruising of the face is much less common and should be carefully evaluated.166 In the dentistry literature, in a series of 266 children suspected of being abused, Jessee and Rieger124
reported that bruises were the most common soft tissue injury, with the
most common facial. In nonabused children, only 7% had accidental soft
tissue injuries of the face and head, with the peak incidence of 17%
seen in toddlers; whereas, soft tissue injuries were present on the
lower extremities and buttocks in 31% of children and on the upper
extremities in 9%.207 In a study of
1467 patients seen for reasons other than trauma at a medical center
over a 1-year period, 76.6% had at least one skin lesion of recent
onset, 17% had at least five, 4% had at least 10, and fewer than 1% had
more than 15 recent lesions.152 In
children less than 9 months of age, skin lesions were uncommon and were
concentrated on the head and face, while in children over 9 months of
age, the skin lesions were mostly on the lower extremities.152
Although any number of bruises may be present in any child, the
location and configuration of the bruises and the mobility of the
child, taken together with the rest of the medical and social history
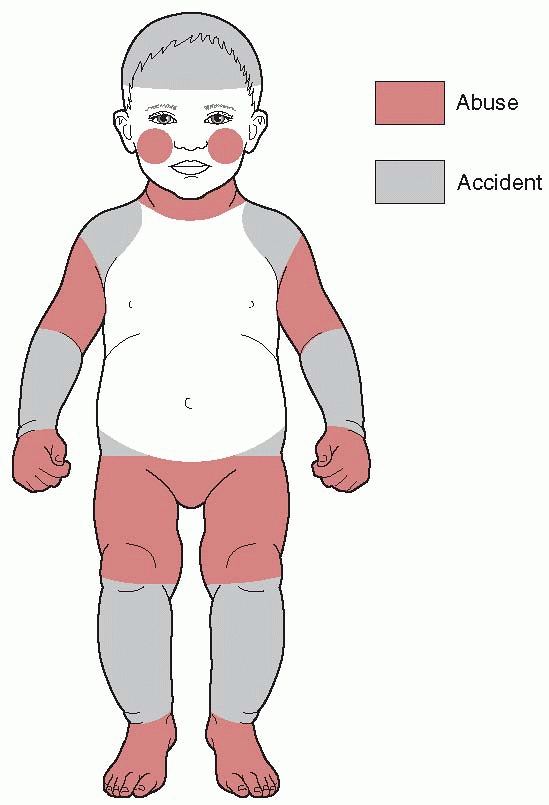
determines the suspicion for abuse (Fig. 7-1 and Table 7-3).
resemble the implement used to inflict the injury, the soft tissue
injuries of abuse are weapon specific in fewer than 10% of patients.171
The weapons used to abuse children often include belt buckles,
staplers, ropes, switches, coat hangers, ironing cords, and the open or
closed human hand.126,240
Bruises inflicted by an open hand may appear on the face or a flat area
of skin and grasp marks may appear as ovoid lesions when the fingertips
are
deeply embedded in the extremities or the shoulders of the child during extreme shaking.115
The injury pattern and the severity of the bruising depend on the
amount of force used, how directly the instrument made contact, and the
specific type of implement used to strike the child.115
 |
|
FIGURE 7-1 Schematic illustrates distribution of abusive versus accidental bruising. (Redrawn from original courtesy of Samir Abedin, MD.)
|
|
TABLE 7-3 Evaluating Bruising in a Child—Implications for Practice
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||
complex skin lesions in which swelling accompanies bruising from injury
through lashing or whipping. Lacerations, scars, and burns are seen in
older abused children, while bruises are seen in all ages.171
Like bruises, the laceration configuration can resemble the weapon used
to inflict the injury on the child. Although minor lacerations around
the eye are fairly common, multiple scars from either lacerations or
burns are suspicious.203,247
Displaced fractures may have associated bruising, with or without
abuse. Deep bruising after abuse can be so extensive that
rhabdomyolysis can occur, detectible by urine dipstick.196
in color over the 2 to 4 weeks following injury, with fading of the
lesions beginning at the periphery. Acute contusions are blue or
reddish purple, gradually changing to green, then to yellow, with final
resolution as a brownish stain as hemoglobin is finally broken down.258 Langlois and Gresham154
noted that a yellowish bruise must be older than 18 hours; a red,
purple, blue, or black coloration of the bruise may be present from 1
hour after injury to resolution; red is always present in bruises
regardless of the age; and bruises of identical age and etiology on the
same person may be of different appearances and may change at different
rates. A deep contusion may take some time to rise to the skin surface
because of intervening fascial planes and thus delay its appearance.
While the color of a bruise may roughly aid in determining the length
of time it has been present, dating bruises based on appearance should
be done with caution.214,232
Mongolian spots, more common in black or Asian infants, are deep-blue
pigmented areas that are present on the lower back at birth, usually
just proximal to the buttocks.16 They do not change in color and gradually resolve as the child matures.115
Cultural differences should be considered when unusual skin lesions are
noted. Vietnamese children may be subjected to the folklore medical
practice known as cao-gio, which places scratches and bruises on the
back of the trunk and may be mistaken for child abuse.43
Other conditions can mimic inflicted bruising: eczema, coagulation
disorders, vasculitis, impetigo, Ehlers-Danlos syndrome, vascular
malformations, dye stains, and others.241
In cases where bruising or bleeding is the only finding of abuse, a
family history for bleeding diathesis, using established protocols for
hematologic evaluation for an underlying bleeding disorder and
involvement of a hematologist, is advised before child maltreatment is
diagnosed.155,244
Burn evaluation should include configuration, approximate percentage of
body surface area, location, distribution, uniformity, length of time
the child was in contact with the burning agent, temperature of the
burning agent, and presence or absence of splash marks when hot liquids
are involved.115
Most accidental pour or spill burns occur on the front of the child,
but accidental burns can also occur on the back as well. In accidental
flowing liquid burns, the injury usually has an arrowhead configuration
in which the burn becomes shallower and more narrow as it moves
downward, and there may be splash marks surrounding the lesion.115
The pattern in accidental burns may also be indicative of flowing water.205
Abuse should be suspected when deep second- or third-degree burns are
well demarcated with circumferential definition. The typical child
abused by scalding burns is an undernourished 2-year-old child with 15%
to 20% of the body involved, usually the buttocks, and has a 10% to 15%
mortality rate from secondary sepsis.205
 |
|
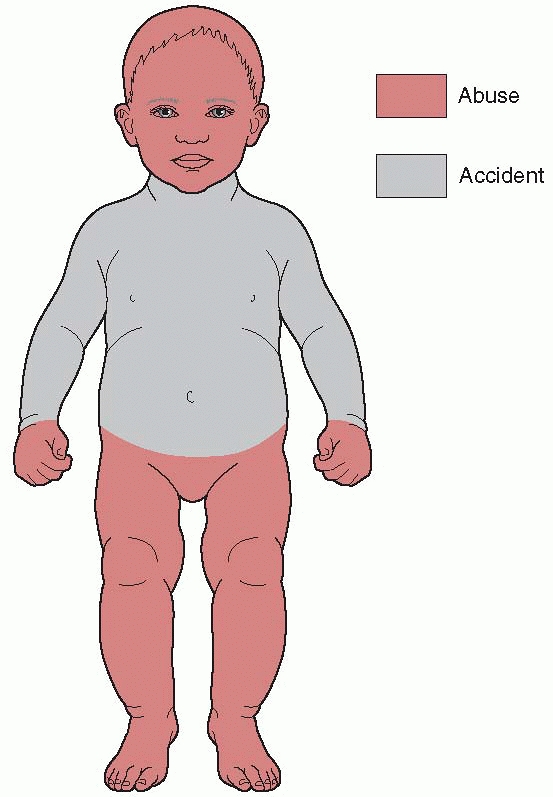
FIGURE 7-2
Schematic illustrates location of accidental versus abusive burns. Note the buttock and lower extremity distribution of nonaccidental immersion burns compared to thoracic distribution accidental burns. (Redrawn from original courtesy of Samir Abedin, MD.) |
stocking or glove configuration may be seen with varying burn depths
and indistinct margins. In deliberate immersion burns such as occurs
when a child’s buttocks are immersed in hot water, the burn demarcation
has uniform depth and a well-demarcated water line.115
The gluteal crease of the buttocks may be spared, giving a
doughnut-like appearance to the burn. In accidental hot water
immersion, the child is uniformly scalded about the lower extremities
as the legs are quickly extended by the child to climb out of the
water, but in deliberate, abusive immersion the child is lowered into
the water and instinctively flexes the hips and knees, thus sparing the
popliteal area.91
the household. Intentional burns by cigarettes are circular, deeply
excavated, and sometimes repetitive, usually about 8 mm in diameter.115
Impetigo may resemble scalds or cigarette burns, but is more
superficial. Severe eczema may mimic burns suspicious for child abuse.104
Contact with heated objects may cause burns of unique shape that allow
identification of their etiology. Children accidentally grasping
curling irons sustain burns of the palms, whereas burns on the dorsum
of the hands are more suspicious for abuse.125
Hair dryers can be used to inflict burns on children, and
full-thickness skin burns can result from the heated air or from
contact with the grill up to 2 minutes after it has been turned off.200 Abuse burns have also been inflicted by stun guns.89
These devices deliver a high-voltage impulse of up to 100,000 volts at
3 to 4 mA, incapacitating the individual and leaving hypopigmented burn
scars on the skin 0.5 cm apart. Circular scars about the wrists may be
due to rope burns when children are restrained for beatings.125 Full-thickness skin burns have been reported in small children who were placed in microwave ovens.7
Certain folklore practices may cause lesions simulating abusive burns.
Round burns on the abdomen, buttock, or between the thumb and
forefinger of Southeast Asian children may be due to a variant on the
Chinese medical practice of moxibustion. Folk medical practitioners’
burn balls of the moxa herb on the surface of the skin for therapeutic
purposes, and both cigarettes and yarn have been similarly used in
refugee camps. The knowledge of these practices may help to avoid
inappropriate accusations of child abuse.81
document all soft tissue injuries that are present before treating
acute fractures. Casts applied in the treatment of fractures,
especially a spica cast, may obscure potentially incriminating skin
lesions and will preclude other members of the child advocacy team from
being able to identify or document them. Photographs taken to document
skin lesions must be done before cast placement.
related to abuse, including the older term shaken baby syndrome (SBS)
and the preferred newer terms AHT,35 inflicted traumatic brain injury
(ITBI), inflicted head trauma (IHT), or nonaccidental head trauma.182
These terms have been used to describe a form of physical nonaccidental
trauma in infants with a triad of subdural hemorrhage, retinal
hemorrhage, and encephalopathy occurring with an inconsistent or
inappropriate history, commonly associated with other inflicted
injuries.101 The American Academy
Committee on Child Abuse and Neglect recommends the term “abusive head
trauma” to be used in the medical record. Recent excellent review
articles discuss fatal AHT90 and the diagnosis of pediatric head trauma in general.116,117
A child under the age of 3 years who suffers head trauma from abuse is
more likely to have sustained a noncontact injury mechanism
(acceleration-deceleration or shaking) resulting in deeper brain
injury, cardiorespiratory compromise with diffuse cerebral
hypoxia-ischemia, and a worse outcome at 6 months than a child who is
accidentally injured.117 Head
injuries can be from indirect noncontact forces such as in shaking or
from direct contact from a blow to the head such as occurs when the
child is thrown against an object. Indirect trauma is felt to be
responsible for the most severe injuries, although the actual injury
may be from both mechanisms. Symptoms typically occur early rather than
later, although secondary or delayed brain injury may occur with edema
and the brain’s neurotoxic injury response.
classic postmortem study of 31 infants with an average age of 3 months,
head trauma was the cause of death in 18. For children less than 2
years of age dying from a traumatic brain injury, 80% of the deaths are
from abuse, with the highest incidence at 6 months.88
For a child with AHT, the mortality rate is approximately 20%, and
survivors have a higher rate of permanent and significant disability
than is seen with accidental trauma.128
reported that 31% of cases of SBS were misdiagnosed on initial
presentation to the emergency room. While early diagnosis of an infant
with AHT is essential, primary prevention is the most important new
development to occur nationally. There is correlation between peak
incidence of infant crying and peak incidence of AHT that occurs 4 to 6
weeks later, suggesting that repeat and prior injuries occur.24
Dias et al.,73 utilizing an early postnatal hospital-based program for
new parents to learn about shaking impact syndrome and how to
appropriately deal with an inconsolable infant, found a 47% decrease in
SBS, whereas intervention programs after abuse is recognized have much
less success.163
is highly unlikely to cause generalized central nervous system (CNS)
injury or subdural or retinal hemorrhage, although isolated skull
fracture or epidural hemorrhage may be seen. The young infant who is
not developmentally mobile enough to cause a fall from a height, having
a relatively large head, immature brain, and weak neck muscles, is very
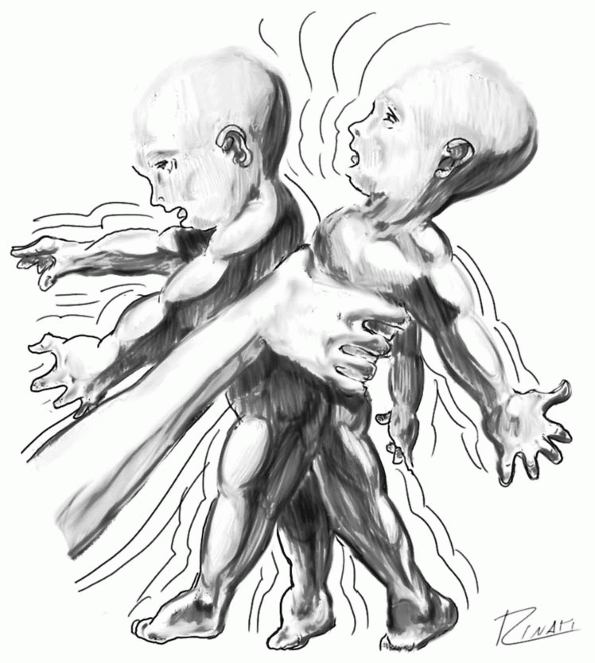
vulnerable to the whiplash effects of inflicted violent shaking (Fig. 7-3).
In 25% to 54% of confirmed cases of AHT, the abuser described an
indirect mechanism by shaking the infant without the head contacting a
surface, with resulting immediate onset of symptoms.34,229
Indirect trauma is responsible for the most severe injuries. There is
sudden angular acceleration and deceleration with associated rotation
of the head and neck in relation to the thorax, producing inertial
shear strain deformation and disruption
leading to diffuse injury.23
Whereas accidental trauma causes subdural hemorrhage from the
translational forces of an impact, inflicted head trauma from
rotational and shearing forces may result in more diffuse subdural or
intrahemispheric hemorrhage.112
|
TABLE 7-4 Criteria for Categorizing the Etiology of Head Injuries
|
||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||
can more easily deform during shaking. This causes vitreo-retinal
traction leading to direct hemorrhage in the retina and in the optic
nerve sheath.262 Fundoscopic examination confirms and documents retinal optic nerve as well as orbital hemorrhage.44
Retinal hemorrhages of abuse classically are multilayered, more
anterior, closer to the ora serrata, and are numerous and bilateral.
Retinoschisis is a splitting of the layers of the macula forming a
cystic cavity caused by shearing and pulling forces of the strong
vitreous attachments to the retinal surface and is classic for AHT.211 Unilateral retinal hemorrhages may occur in 10% to 16% of cases, so unilateral does not rule out SBS.15
Although retinal hemorrhages resulting from normal vaginal birth are
present in 34% of newborns, these resolve by 16 days of age.113
address injury to the cervical spine, so it is not known how frequently
the spine also is injured with this mechanism.20
In very young infants (2 to 3 months of age), forces may be directed to
the upper cervical spine leading to spinal cord injury without obvious
radiographic abnormality (SCIWORA), cervicomedullary junction cord
injury, apnea, and cardiorespiratory arrest.92,117 Direct head injuries may also occur when the child’s head is slammed onto a soft surface such as a mattress.78
On impact, deceleration forces approaching 400 Gs may occur, tearing
the bridging vessels between the skull and the brain and producing
intracranial hemorrhage and cerebral edema. Skull fractures are rare
unless the child is thrown onto a hard object.
suspected of being abused. This should include assessment of the
child’s mental status, motor function, sensation, reflexes, and gait,
if possible. Any abnormal findings warrant further investigation. Also
included should be a dilated fundoscopic examination by an
ophthalmologist looking for retinal hemorrhages. For the child with
acute neurologic findings suspicious for AHT, a
noncontrast
computed tomography (CT) scan is done to evaluate for conditions that
may benefit from prompt medical and neurosurgical treatment, such as
intracranial hemorrhage-acute parenchymal, subarachnoid, subdural, or
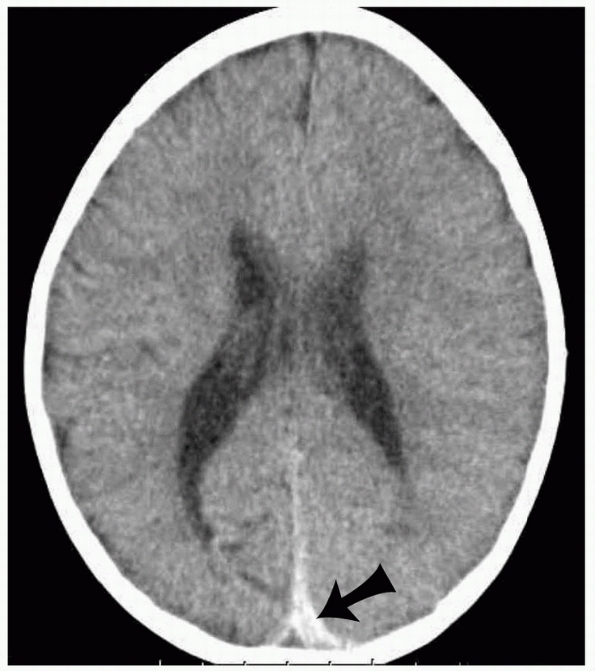
epidural (Fig. 7-4).
If the head CT scan includes upper cervical spine-associated injuries,
pre-existing bony conditions such as Klippel Feil syndrome or occipital
cervical assimilation may be detected.111
Anteroposterior and lateral skull and spinal radiographs are always
included as part of the routine skeletal survey for the child less than
2 years of age and should be performed for any aged child with
suspected AHT (Table 7-5). CT scans alone may
occasionally miss in-plane axial skull fractures. However, these
fractures are usually easily seen on the accompanying skeletal survey.
Although fine-cut three-dimensional CT skull reconstructions may reveal
subtle skull fractures, they may increase delivered radiation by up to
30% over standard head CT. Since the infant is 15 times more sensitive
to the effects of radiation than is an adult, fine-cut CT should not be
the primary imaging modality for detecting skull fractures. Magnetic
resonance imaging (MRI) is best used to fully assess various
intracranial pathology and has become the imaging modality of choice
for evaluating asymptomatic, nonacute parenchymal brain lesions and for
fully documenting the abuse. MRI is also effective for diagnosis of
related conditions in the cervical spine, including ligamentous injury
and intra-spinal injuries such as SCIWORA.
 |
|
FIGURE 7-3
Illustration of acceleration-deceleration injury sustained by a shaken infant. Shaken infants suffer whiplash injuries due in part to their disproportionately large heads in relation to their bodies. This mechanism is believed responsible for the common association of subdural hematomas, retinal hemorrhages, and posterior rib fractures. (Artwork courtesy of Gholamreza Zinati, MD.) |
 |
|
FIGURE 7-4
Interhemispheric subdural hematoma in an 8-month-old female presenting with seizures due to nonaccidental trauma. Axial CT image shows high attenuation blood along the left aspect of the posterior falx (arrow). |
|
TABLE 7-5 Standard Skeletal Survey Radiographic Protocol
|
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||
retinal hemorrhages, occult head injury should always be suspected. At
risk children with obvious neurologic findings should be urgently
screened with head CT for acute pathology. At risk children without
obvious neurologic findings are best imaged initially with MR brain
imaging (ACR guidelines).12 MRI is sensitive for diagnosing small parenchymal hemorrhages78 and offers the highest sensitivity and specificity for the diagnosis of subacute and chronic head injuries.12
Diffusion and susceptibility weighted imaging sequences are extremely
sensitive for detecting subtle hypoxic-ischemic brain injury and
parenchymal hemorrhage194,238
and are routinely included in imaging protocols when available. MR
venography may be used if venous sinus thrombosis is suspected. MR
spectroscopy may detect lactate levels, an indicator of prognosis.82
fontanelles, and macrocephaly. Paresis may be present, and reflexes may
be increased. Older infants and children may have subdural hemorrhages
and musculoskeletal injuries.92
Classic infant AHT with multilayered retinal hemorrhages and acute
subdural hematomas has been noted in an autopsy series of four older
children between 2.5 and 7 years of age.211 Cerebral edema may be lethal,58 so emergency neurosurgical consultation may be needed. Barnes and Krasnokutsky23
reviewed the radiographic evaluation of a young child with a suspected
nonaccidental head injury, including mimicking of conditions, such as
accidental injury from short falls, acute CNS infections,
coagulopathies, venous thrombosis, metabolic abnormalities, and
neoplasms. The diagnosis of these mimics may require
more extensive workup before a diagnosis of AHT is confirmed (Table 7-6).224 Oehmichen et al.186 have presented very practical principles for diagnosing AHT (Table 7-7).
|
TABLE 7-6 Differential Diagnosis of Subdural Hemorrhage in Infants and Children
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||
severe. Common late sequelae after AHT include developmental delays,
sensory and motor deficits, feeding difficulties, recurrent seizures,
attention deficits, and intellectual, educational, and behavioral
dysfunctions.117 In a long-term outcome study, 69% of children had an abnormality and 40% had severe dysfunction.22 Approximately 50% had visual impairment and another 50% had behavior disorder.22
Some children seemed normal until 5 years after the inflicted injury,
then showed learning disorders, so long-term follow-up is essential.
Repeat abuse when AHT is not recognized and the child is returned to
the home is too common.92
|
TABLE 7-7 Principles of Diagnosing Inflicted Traumatic Brain Injury in Children
|
|||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||
In a review of the National Pediatric Trauma Registry, 16% of all blunt
abdominal trauma in children 0 to 4 years of age was attributable to
child abuse.250 The pediatric thorax
and pelvis are very compliant. The abdominal muscles are pliable with
little subcutaneous and omental fat, so there is less protection to the
internal abdominal, chest, and pelvic organs. Whereas shaken infants
sustain head trauma, toddlers receive abdominal injuries as they are
more often punched and beaten. Inflicted abdominal trauma may be due to
beatings with the hand, fist, or when the child is thrown into a fixed
object. The compliant pediatric abdominal wall does not absorb much of
the injury energy, so abdominal bruising is present in only 12% to 15%
of major intra-abdominal injury cases.115
Children with inflicted injuries are more likely to be of a younger
age, malnourished, have a pancreatic or hollow viscous injury, have an
associated traumatic brain injury, and have higher mortality compared
to victims of accidental abdominal injury.251
a wide range of symptoms depending on the organ involved and the
severity of the injury. Fever, vomiting, anemia, abdominal distention,
localized involuntary spasm, and bowel sounds may be absent.185
The liver is the most commonly injured solid organ. With a damaged
liver, right shoulder pain from hemidiaphragm irritation (Kehr sign)
may be associated with abdominal pain and fatal hypovolemic shock.248 Liver function tests may reveal occult liver injury. In one study,60
elevated aspartate aminotransferase, alanine aminotransferase, and
lactic dehydrogenase enzyme levels were useful markers for occult liver
lacerations in abused children who had false-negative abdominal
examinations. Blows to the abdomen often injure the pancreas as it is
violently compressed against the spine. Blunt pancreatic injury due to
nonaccidental injury commonly presents with contusion, transaction, or
laceration, all of which are associated with pancreatitis and elevated
blood amylase. A pancreatic pseudocyst may form, causing obstructive
symptoms several weeks after initial injury.115
Splenic and renal injuries, rare in child abuse, have a 45% risk of
mortality from hemorrhagic or septic shock if care is delayed.63
gastrointestinal tract or bladder are infrequent in accidents but
common in child abuse, particularly in the younger child (mean age 2.5
years).156 Hollow organ abuse
injuries, as is true for most abdominal injuries due to nonaccidental
injury, present for medical attention late, with an inconsistent or
vague history. In a young child with unexplained hollow organ injury,
abuse should be suspected and investigated.
 |
|
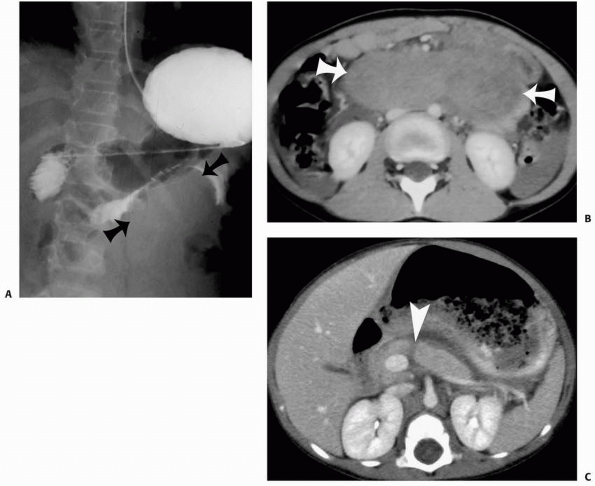
FIGURE 7-5
Duodenal hematoma and pancreatic transection in a 4-year-old male presenting with bilious vomiting due to nonaccidental abdominal trauma. A. Fluoroscopic upper gastrointestinal image reveals a large, well-defined defect within the third portion of the duodenum (arrows). Axial contrast enhanced CT images at the level of the duodenum (B) and pancreas (C) show a large hyperattenuated retroperitoneal duodenal hematoma (arrows) and a linear low attenuation defect (arrowhead) in the pancreatic head. Also noted is peripancreatic fluid. |
Frequently, the radiologist first suggests the possibility of
nonaccidental trauma by finding a duodenal hematoma with no history by
the caregiver of trauma. Blunt trauma to the abdomen may also cause
intestinal perforation, usually involving the small intestine, and the
physical examination may suggest peritonitis. Previously, plain
radiographs were used to search for free air in suspected hollow organ
injuries; however, only 19% of radiographs were diagnostic.39
Today, CT with intravenous contrast enhancement is used for the trauma
evaluation. Hollow organ injuries classically manifested with free air
on the plain radiographs; however, CT imaging better reveals free
fluid, focal bowel wall thickening, inflammation, or ileus. Associated
spine injuries, such as Chance flexion-distraction lumbar spine
fracture, should be evaluated.
recommends CT scans with nonionic intravenous contrast to define injury
to abdominal organs. Contrast should not be used if there is a history
of iodine allergy or renal failure. The use of oral contrast is
debatable with CT scans and may place the patient at risk of
aspiration. Ultrasound and upper gastrointestinal series are most often
used to evaluate duodenal hematoma. When abdominal injury is suspected
in an abused child, the hematocrit and hemoglobin levels are checked,
the child is typed and crossmatched for blood, and two large
intravenous lines are placed in anticipation for surgical treatment.
General surgery consultation is obtained. The overall mortality rate
associated with visceral injury in child abuse is 40% to 50%.60 In fatal cases with liver injury, hepatic glycogen staining may be helpful in establishing time of death for legal reasons.243
Occult abdominal trauma is easily missed, so a high index of suspicion
with serial abdominal examination and liberal use of abdominal CT
should be used in the suspected abused child.112
a physically abused child. Specific guidelines for the evaluation for
sexual abuse were revised and published in 2005.2
Children who have been sexually abused can have symptoms of bed
wetting, fecal incontinence, painful defecation, pelvic pain, abdominal
pain, vaginal itching and bleeding, sexually transmitted diseases, and
pregnancy in postmenarche adolescents. Sexually transmitted diseases
found in abused children include gonorrhea, syphilis, chlamydia,
trichomoniasis, and lymphogranuloma venereum. Although the percentage
of sexually assaulted children with obvious physical trauma to the
genitalia is low,
failure
to document such findings is a serious matter. Sexual abuse is always a
criminal offense and must be reported to legal authorities. The
physical signs of sexual abuse, including genital trauma, sexually
transmitted diseases, or presence of sperm, are present in only 3% to
16% of verified sexual assaults,28,223
but even this minority of patients will be undiagnosed if sexual abuse
is not considered when a child presents with musculoskeletal injury
resulting from abuse.
procedure for handling suspected sexual abuse, but is not expected to
manage this evaluation. When sexual abuse is suspected, consultation
with an experienced medical team will assure competent assessment of
the child’s physical, emotional, and behavioral needs, manage reporting
and legal requirements, and interact with appropriate professionals to
provide comprehensive treatment and follow-up.2
The child’s genitalia should always be examined and documented in a
chaperoned setting by an appropriate physician consultant such as a
pediatrician or a gynecologist in children with physical abuse. If the
sexual assault occurred within 72 hours of evaluation, then a rape kit
must be used by the evaluating physician or nurse examiner to provide
medical evidence of the attack.150 However, detecting semen on examination for forensic evidence decreases markedly after 24 hours.192
for, sexually motivated assault include bruises, scratches, and burns
around the lower trunk, genitalia, thighs, buttocks, and upper legs,
including the knees. Pinch or grip marks may be found where the child
was held. Attempted or achieved penetration may involve the mouth,
vagina, or anus.110 Sexually abused
boys may have poor rectal sphincter tone, perianal scarring, or
urethral discharge. Female genital examination findings that are
consistent with sexual abuse include chafing, abrasion, or bruising of
the inner thighs or genitalia, distortion of the hymen, decreased or
absent hymen, scarring of the external genitalia, and enlargement of
the hymenal opening.9 The size of the transverse hymenal orifice does not correlate as a marker of child abuse.118
The examination of the female genitalia can be normal even when there
has been penetration, because hymen tissue is elastic and there can be
rapid healing. In a study of 36 adolescent pregnant girls evaluated for
sexual abuse, only 2 of 36 had genital changes diagnostic of
penetrating trauma, suggesting that injuries either may not occur or
may heal completely.129 There also is a wide variability of appearance of normal female genitalia,46,58 but posterior hymen disruption is rare and should raise suspicion for abuse.31
physical presentation of abuse. Fractures, documented on plain
radiographs or CT, are present in 11% to 55% of abused children and are
most common in children younger than 3 years of age.4,69,95
The child abuse literature shows varying incidence of abuse-related
fractures, depending on the age of the study population, institution,
study entry criteria, selection bias, and time period when the study
was published.158 The younger the child with a fracture, especially under 18 months of age, the more likely abuse is the cause.61
Fractures resulting from abuse should be suspected in young children if
a caretaker brings the child for evaluation but reports no history of
accidental trauma, especially if the caretaker reports a change in the
child such as extremity swelling or decreased movement of the limb.
Particularly concerning is a bone that fractures under tension with
torsion, rather than the physiologic loading of compression of normal
childhood activity or falls. Pierce and Bertocci199 recommend that the clinician determine if the observed injury of a long bone and the stated mechanism are consistent (Table 7-8).
|
TABLE 7-8 Considerations When Evaluating a Child with a Long Bone Fracture
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||
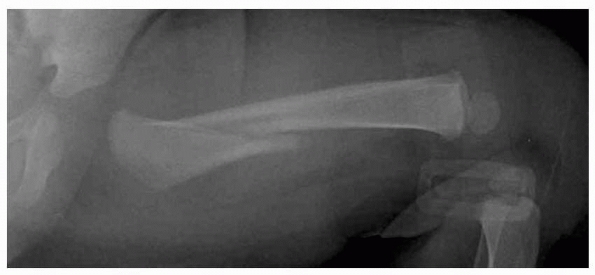
and although nonspecific, are always suspicious for child abuse in
nonambulatory infants (Fig. 7-6).215 Accidental femoral fractures
occur in children old enough to stand or run and who may fall with a
twisting injury to the lower extremities, but femoral fractures in
children younger than 1 year of age are commonly due to abuse.215,246
However, even among nonambulatory children less than 1 year of age with
a femoral fracture, abuse is present in only 42% and other mechanisms
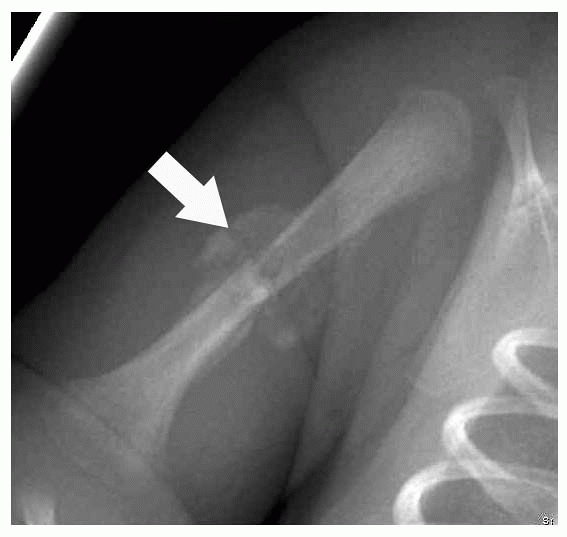
need to be considered.215 Humeral shaft fractures are frequently seen in nonaccidental trauma (Fig. 7-7).
Fractures in unusual locations such as the distal clavicle, scapula,
acromial tip, proximal humeral metaphysis, or distal humeral physis may
result from violent blows or upper extremity traction injury and are
suggestive of abuse in young children.10 Infants may normally have a separate ossification center adjacent to the tip of the acromion, simulating a fracture,144
but a true fracture has sharp, demarcated edges, may be positive on
bone scan, and will show callus or healing. Although fractures of the
sternum are believed to be specific for child abuse by Kleinmann,133 accidental midsternal fractures in children have been reported.103
 |
|
FIGURE 7-6
Femoral fracture in a 3-month-old male victim of nonaccidental trauma. Radiograph of the femur demonstrates an oblique diaphyseal fracture without evidence of periosteal reaction or healing. |
 |
|
FIGURE 7-7
Humeral fracture in a 3-week-old male after a difficult delivery. Radiograph shows a transverse middiaphyseal fracture with extensive callus (arrow). |
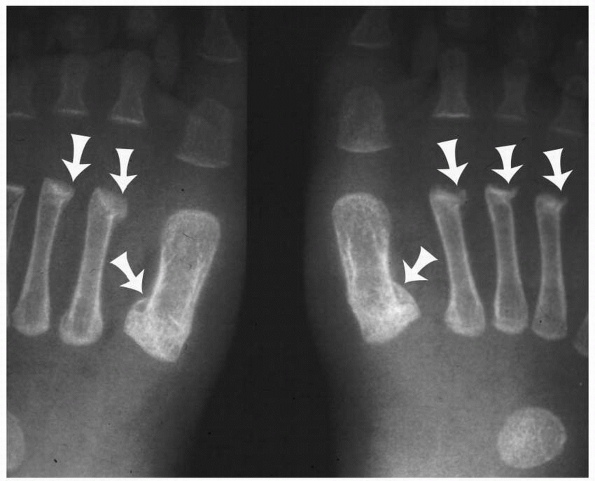
reviewed 11 hand and foot fractures in abused children younger than 10
months of age and found mostly torus fractures either of the
metacarpals or the proximal phalanges of the hand and similar fractures
of the first metatarsals of the feet (Fig. 7-8).
Clinical signs of fracture were present in only one patient, and bones
scans were insensitive to the presence of the fractures in all
patients. These injuries are best seen on the oblique views standard in
the skeletal survey.
 |
|
FIGURE 7-8
Metatarsal fractures in a 2-month-old female victim of nonaccidental trauma. Radiographic image from a skeletal survey shows multiple healing, bilateral, and symmetric proximal and distal metatarsal fractures (arrows). |
abuse literature, and it is often the presence of multiple fractures
that indicates nonaccidental trauma (Fig. 7-9). In one of the largest series, King et al.132
reported 429 fractures in 189 abused children. Fifty percent of these
patients had a single fracture, and 17% had more than three fractures.
Approximately 60% of fractures were found in roughly equal numbers in
the humerus, femur, and tibia. Fractures also occurred in the radius,
skull, spine, ribs, ulna, and fibula, in order of decreasing frequency.
Another study185 found a similar
incidence of fractures of the humerus, femur, and tibia in abused
children, with skull fractures seen in 14%. In contrast, Akbarnia et al.3
found that rib fractures in abused patients were twice as prevalent as
fractures of any one long bone; the next most frequently fractured bone
was the humerus, followed by the femur and the tibia. Nearly a third of
these patients had skull fractures. Loder and Bookout162
reported the tibia to be the bone most commonly fractured in their
series of abused children, followed by the humerus, the femur, the
radius, and the ulna. In a classic study of 31 postmortem infants, the
fracture pattern was very different from clinical studies in living
children.139 Highly detailed
skeletal, specimen, and histopathologic analysis revealed 165 total
fractures, most commonly ribs, distal femur, the ends of the tibia, and
skull (Fig. 7-10). The fact that 29 of the 31
infants had evidence of a healing fracture provides sobering evidence
of the need to aggressively diagnose nonaccidental trauma before an
infant is killed. Physician education in child abuse is necessary to
properly identify and report child abuse,153 as there are many pitfalls to avoid (Table 7-9).
There are several medical conditions that result in weakened bone and
predisposition to fracture, such as osteogenesis imperfecta, that
should be considered in the evaluation of a young child with multiple
fractures.120
The orthopaedist often is asked to determine the age of fractures with
some certainty to corroborate a history of injury given by caretakers.
Experienced orthopaedists and radiologists can roughly estimate the age
range of fractures by their radiographic appearance and their
experience reading many radiographs of known dated injuries. Although
specific guidelines have been established for estimating the age of
fractures in children,74 there is not good evidence-based data for accurately predicting the age of healing fractures.202
In general, fractures seen on radiographs are considered acute until
callus appears. Classic metaphyseal lesions (CML) are acute until
periosteal reaction appears at about 14 days; however, not all CML
develop visible callous, so dating in the absence of callous should be
done with caution. Skull fractures generally cannot be dated.
inclusion criteria, the following conclusions were reached: the science
of fracture dating is inexact and periosteal reaction is seen as early
as 4 days and is present in at least 50% of cases by 2 weeks with
remodeling peaking at 8 weeks after the fracture.202
In dating fractures in infants younger than 6 months, one must be aware
of the normal physiologic diaphyseal periosteal reaction
that is frequently present.197
This is typically symmetric, diaphyseal only, and seen on the long
bones of the extremities. The most difficult fractures to date are
those that are completely healed, with substantial remodeling, and
often the only sign of a healed fracture is a thickened cortex.
 |
|
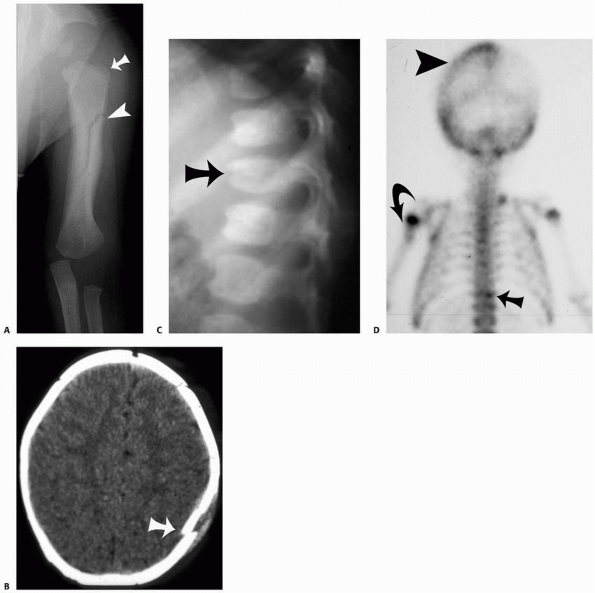
FIGURE 7-9 Multiple fractures in a 3-month-old female victim of inflicted injury. A. Frontal radiograph of the humerus shows proximal metaphyseal irregularity consistent with a corner fracture (arrow) and an oblique diaphyseal fracture with extensive periosteal reaction and healing (arrowhead). B. Axial CT image reveals a depressed left calvarial fracture (arrow). C. Lateral thoracolumbar radiograph suggests a T12 compression fracture (arrow), which is confirmed on nuclear bone scintigraphy (D) as a region of increased uptake (arrow). Bone scan also confirms left parietal (arrowhead) and humeral (curved arrow) fractures.
|
acute injury, a complete skeletal survey should be used to screen for
additional fractures in all children younger than age 2 years when
abuse is suspected.12,130 The standard views obtained on a skeletal survey recommended by the American College of Radiology11 are listed in Table 7-5.
Abnormalities of the limbs detected on one view should undergo
additional orthogonal views for completeness. Lateral views of the
entire spine must always be included in the skeletal survey. Bilateral
oblique views of the thorax are helpful, and some authors insist
mandatory, in the diagnosis of subtle rib fractures.130
Oblique thoracic films obtained on 2-week follow-up skeletal survey
increased diagnostic yield, with 46% of repeat surveys revealing
additional fractures.141,264
Oblique radiographs of the hands are standard, since they may detect
subtle torus fractures of the metacarpals and the phalanges not seen on
a plain anteroposterior images.184 The American Academy of Pediatrics Section on Radiology12
cautioned that a “baby gram” has no place in diagnosing fractures of
child abuse because the obliquity of the angle at which the radiographs
transverse the skeleton may obscure many subtle
fractures.62 Imaging systems should have a spatial resolution of at least 10 line pairs per millimeter and should be used without a grid.11
 |
|
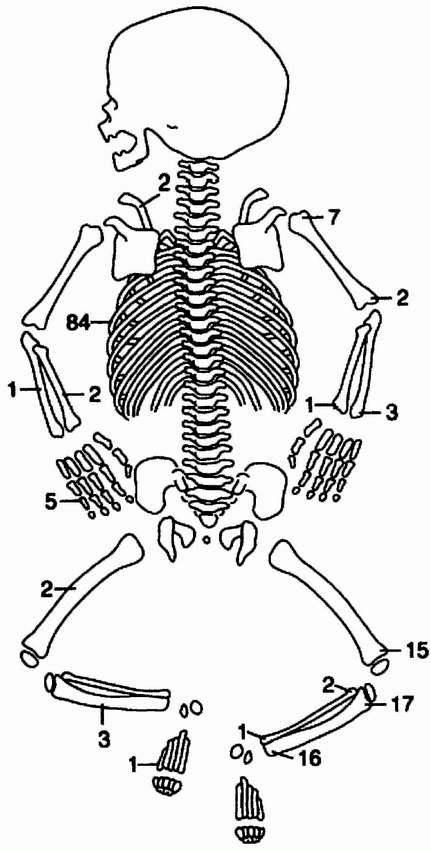
FIGURE 7-10
Schematic representation of the distribution 165 fractures in 31 infant fatalities. Single vertebral fracture and 13 skull fractures in this case series are not shown. (Image reprinted with permission from Kleinmann PK, Marks SC Jr, Richmond JM, et al. Inflicted skeletal injury: a postmortem radiologic-histologic study in 31 infants. AJR September 1995;165(3):647-650). |
patients older than 2 years of age. They have less value for children
older than age 5 years since the older child can describe where the
pain is located. For children between the ages of 2 and 5 years, the
test should be individualized.12 The
cost-effectiveness of skeletal surveys in the older child appears to be
low, but may be helpful for the child with a disability who cannot
cooperate with the physical examination. In one study of 331 children,
only eight patients without overt physical signs of child abuse had
occult fractures revealed by the survey80; however, the use of the skeletal survey in these few patients possibly prevented both reinjury and death.
is the standard of care for imaging suspected child abuse in children
less than 2 years of age. A radionucleotide bone rarely is used as a
complementary and confirmatory test for problem solving some difficult
cases.62 Neither a skeletal survey or a technetium bone scan alone will detect all occult fractures.130 In Kleinman’s postmortem infant study of fractures diagnosed by detailed histopathology,
58% of these fractures were seen on skeletal survey and 92% were seen
by specimen radiographs. Because of a false-negative rate of 12% with
skeletal surveys, Sty and Starshak236
suggested that a technetium bone scan be used as an initial screening
test. Technetium bone scintigraphy is very useful in the diagnosis of
occult rib fractures62; however,
there is inconsistent interpretation in children younger than 18 months
of age. Bone scintigraphy is not useful for areas that are normally
active such as the physis and metaphysis, but is very good when imaging
areas away from the physis, such as the shaft of a long bone.
Scintigraphy is not reliable to detect skull fractures.177
Bone scan and skeletal survey may be considered complementary rather
than competing imaging modalities; however, the skeletal survey is
performed first. Jaudes119 found
that when results of either a bone scan or a skeletal survey were
normal in a known abused child, the use of both tests often revealed
additional occult fractures. Technetium scans are not useful for dating
fractures because increased isotope uptake may occur at a fracture as
early as 24 hours after injury and scan abnormalities may persist for
years.87
|
TABLE 7-9 Pearls and Pitfalls of Nonaccidental Trauma
|
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
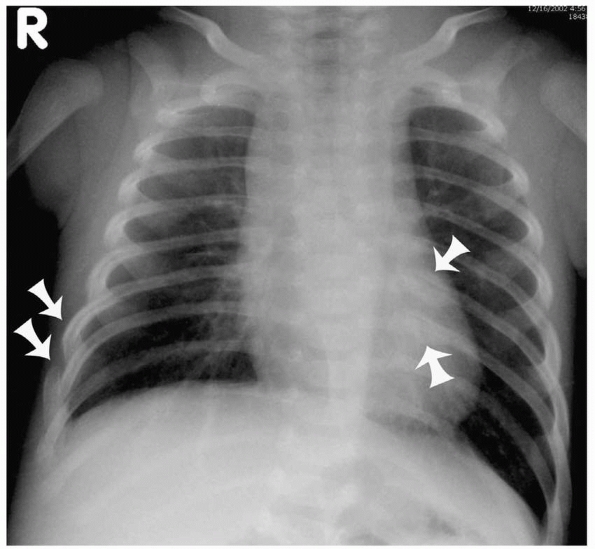
FIGURE 7-11
Rib fractures in multiple stages of healing in a 4-month-old female victim of nonaccidental injury. Frontal chest radiograph reveals acute (no periosteal reaction or healing) and subacute/healing (positive periosteal reaction) rib fractures (arrows). |
diagnosis of occult fractures, since some fractures, especially of the
ribs, may not be seen until callus appears at 10 to 14 days. The second
look skeletal survey better defines the fracture seen on the original
survey and may help determine the age of the fracture.130 Kleinman et al.141
reported that a follow-up skeletal survey 2 weeks after the initial
series detected 27% more fractures and provided assistance in dating
20% of previously detected fractures.
communication system has replaced standard film-screen imaging in most
hospitals; however, its role in the detection of the subtle fractures
of child abuse needs further study. Child abuse fractures can be missed
on digitalized images.263 Kleinman et al.142
noted that digital imaging of child abuse fractures had a spatial
resolution lower than film-screen imaging, but the difference was not
appreciable in detecting rib fractures in a postmortem evaluation.
High-quality image screens are necessary for optimal image
interpretation.
skull or the extremities have an equal risk of the etiology being
either accident or abuse.169
However, 80% of skull fractures from abuse are seen in infants less
than 1 year of age. Skull fractures were the most commonly reported
fracture in one series.171 Detailed postmortem analysis of 31 abused infants, with an average age of 3 months, observed confirmed skull fractures in 13.139 Skeletal surveys missed 26% of skull fractures confirmed on CT scan.211
Bone scintography is even less sensitive and is notably poor in
detection of skull fractures. Skull fractures are nonspecific and the
morphology of the fracture does not distinguish accidental from
inflicted trauma.23 Simple linear skull fractures are usually accidental; however, 80% of inflicted skull fractures are also linear.157
Complex skull fractures without a history of significant trauma,
including comminuted, diastatic (separated sutures), displaced
fractures, and fractures crossing suture lines, are suspicious, but not
diagnostic for abuse.37 Skull fractures cannot be dated.
in child abuse. Traditionally, a midshaft spiral fracture was believed
to be uniquely caused by a violent abusive twisting injury of the
extremity of the child. However, it is now known that this is not true.
In a study of 23 long-bone fractures in abused children, spiral
fractures were found in 78%.109 However, others found that 71% of diaphyseal fractures were transverse in abused children.91 Loder and Bookout162
reviewed 69 long-bone fractures in abused children and noted that 56%
were transverse, 36% oblique, and only 8% spiral. In another study of
429 fractures,81 48% of fractures
were transverse and 26% were spiral. Most of these long-bone fractures
were in either the middle or distal third of the shaft. Transverse
fractures are most commonly associated with either a violent bending
force or a direct blow to the extremities, whereas spiral or oblique
fractures of the long bones are due to axial-loaded, twisting injuries,
such as in a fall. Humeral shaft fractures in children under 3 years of
age have an 18% risk of being due to probable abuse.216
In delayed follow-up, long-bone fractures may show exuberant callus
because of a lack of immobilization, and multiple fractures may be
present in different stages of healing.6
Juxtacortical calcification may be seen without fracture when there is
diaphyseal periosteal separation resulting from tractional or torsional
force when the limb is grasped or pulled along the shaft of the bone.176
for nonaccidental trauma; whereas children old enough to run can fall
and accidentally fracture their femurs if there is a significant
twisting motion at the time of injury.246
Despite a high likelihood of nonaccidental trauma in an infant with a
femoral fracture, an infant with a femur fracture may have accidental
trauma as the cause, if the parent’s reported mechanism is consistent
with the injury. In a recent case series from Alberta, Canada, only 17%
of femoral fractures in infants less than 1 year of age were from
abuse, while the author’s review of eight previous reports showed that
nonaccidental trauma was the cause for 42% to 93% of cases.114 Scherl et al.206
reported that there was equal risk of having a spiral or transverse
femoral fracture as a result of abuse. As children get older and more
active, a femoral fracture is more likely to be from accidental injury
than from abuse. Schwend et al.215
reported that while 42% of femoral fractures in infants not walking
were related to nonaccidental injury, only 2.6% of femoral fractures in
ambulatory toddlers were. Blakemore et al.36
noted that only 2% of femoral fractures from age 1 to 5 years were due
to abuse. Risk factors for abuse were age younger than 12 months, the
child not yet walking, a questionable mechanism, and other associated
injuries.
In infants and toddlers, these fractures can occur when the child is
violently shaken by the extremities with direct violent traction or
rotation of the extremity (see Fig. 7-7).177
Buckle fractures may occur at multiple sites, seldom producing
exuberant callus. Repeated injury may cause irregular metaphyseal
deformities. Periosteal avulsion typically produces new bone formation
within 2 to 3 weeks of injury and may be confused with osteomyelitis.6
New bone formation may be delayed, particularly in children with
malnutrition or rickets. Metaphyseal fractures constituted 40% of
fractures in one series,91 but fewer than 15% in another.146
Distinguishing between an accident and child abuse is based on the
location and the type of fracture. He emphasized that both moderate-
and low-specificity radiographic
findings
of child abuse become much more specific when there is an inadequate
explanation for the injury. The presence of multiple injuries,
particularly in the young child, is especially concerning for abuse.
|
TABLE 7-10 Specificity of Skeletal Trauma for Abuse
|
||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||
more susceptible to fractures, both related to their prematurity and to
increased risk of child abuse.49
They may have underlying genetic, metabolic, and nutritional deficiency
that predispose to fractures. Underlying osteopenia may lead to
insufficiency fractures, both acute and chronic, in various stages of
healing. Higher parental stress from caring for a sick or disabled
infant may result in higher risk of nonaccidental trauma. In the
premature infant with multiple fractures, investigation of the bone
health as well as for child abuse is necessary, depending on the
clinical context and findings.
These fractures are almost exclusively seen in nonaccidental injury,
but are not the most common fractures in abused children. The incidence
of CML in large series ranges from 15% to 32%.91,132,146,162 Radiographs show a corner fracture at the edge of the ossified portion of the zone of provisional calcification, which is the metaphyseal side of the physis as opposed to the epiphyseal side.
If a significant portion of the metaphyseal rim is involved, a
bucket-handle fracture pattern is produced. Based on their
histopathologic autopsy study of metaphyseal fractures in abused
infants, Kleinman et al.136,138
found that bucket-handle and corner fractures are actually a
full-thickness metaphyseal fracture extending through the primary
spongiosa of bone just above the zone of provisional calcification (Fig. 7-12).
Centrally, the amount of metaphysis remaining attached to the physis
was thin, but peripherally the fracture line curved away from the
physis so that a substantial metaphyseal rim remained attached to the
physis (Fig. 7-13). On radiographic study, this
metaphyseal rim formed the basis for both corner and bucket-handle
fractures. In healing fractures, biopsy specimens showed metaphyseal
extension of hypertrophied chondrocytes.191 Metaphyseal corner fractures are most likely caused by either violent shaking or traction injuries to the extremity.4
Subepiphyseal-metaphyseal lucency can also be caused by systematic
disease such as rickets and leukemia. Corner fractures of the distal
radius, ulna, tibia, and proximal humerus also have been reported with
developmental coxa vara associated with spondylometaphyseal dysplasia.68
Since fracture callus does not reliably occur, dating the CML lesion is
always unreliable. The presence of callus does indicate that the
fracture is greater than 10 to 14 days.
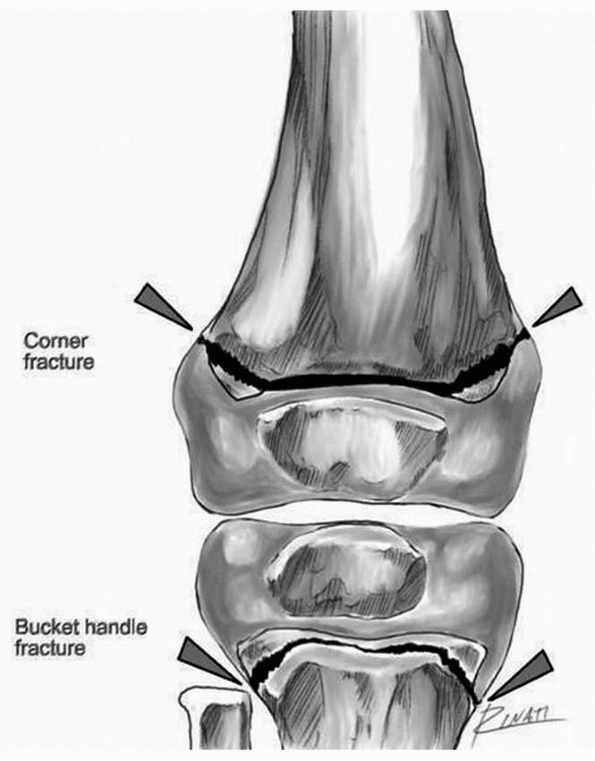 |
|
FIGURE 7-12
Schematic representation of classic metaphyseal lesions (CML). Illustration demonstrates the path of the CML. Depending upon the angle at which the CML is viewed from, it may appear to extend across the width of the ossified physis (tibia illustrating a bucket handle fracture) or only the margins of the physis (femur, illustrating a corner fracture). (Artwork courtesy of Gholamreza Zinati, MD.) |
especially when located posterior and associated with other long-bone
fractures. Abusive rib fractures may be caused by squeezing of the
chest by a caretaker,44 hitting the child from behind, or stepping on the chest.141,226 Kleinman et al.140
postulated that severe shaking of an infant can cause front-to-back
chest compression, which levers the posterior rib over the transverse
process of the vertebral body, causing fractures of the posterior rib
shaft at the transverse process and of the rib head adjacent to the
vertebra (Fig. 7-14). One series showed that fractures of the first rib in children were only seen in abuse.235 Barsness et al.25
reported that rib fractures had a positive predictive value of
nonaccidental injury of 95% in children younger than 3 years of age. In
this study, rib fracture(s) were the only skeletal manifestation of
nonaccidental injury in 29% of the children. Posterior rib fractures
are difficult to diagnose acutely because they lack callus and are
rarely displaced. Even with healing, the callus
on radiography may be obscured by the overlying transverse process.136
Oblique views of the chest are often included in skeletal surveys
because they may better show these fractures. Posterior rib fractures
are the most common location in child abuse, but fractures may occur
anywhere along the arc of the rib, including disruption of the anterior
costochondral junction (Fig. 7-15). Posterior
rib fractures tend to occur between T4 and T9. Acute anterior
costochondral separations of the ribs may be difficult to see on chest
radiographs,225 and with healing, the anterior end of the osseous rib becomes widened and
club shaped.146,185
Anterior rib fractures are commonly associated with abdominal injury
and can be detected on CT scan. Healing fractures show callus, but
healed fractures may be subtle, with only a fusiform thickening of the
rib. Older fractures of the ribs in nonaccidental trauma may form
lytic, expansile lesions.164
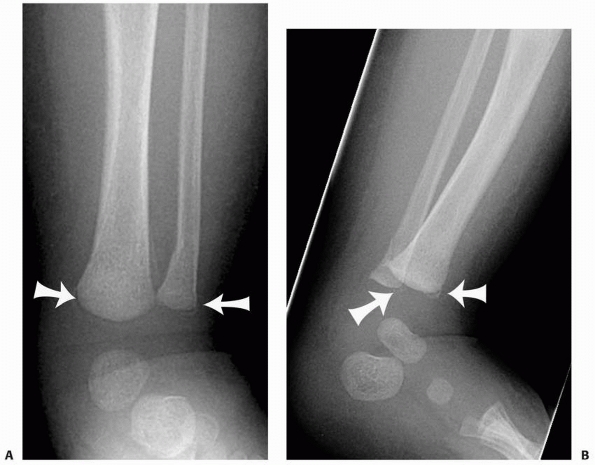 |
|
FIGURE 7-13 Classic metaphyseal fracture in a 2.5-month-old male victim of nonaccidental injury. A. Frontal radiograph of the tibia and fibula demonstrate transmetaphyseal lucencies, or bucket handle fractures (arrows). B. A lateral ankle radiograph reveals lucency at the tibial and fibular metaphyseal margins indicating corner fractures (arrows).
|
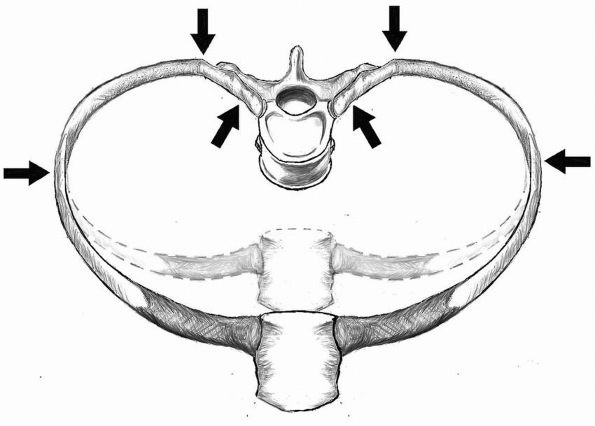 |
|
FIGURE 7-14
Schematic representation of rib fracture mechanism. Anterior chest compression causes the posterior ribs to be levered over the transverse processes of the vertebra causing posterior and lateral rib fractures. (Artwork courtesy of Samir Abedin, MD.) |
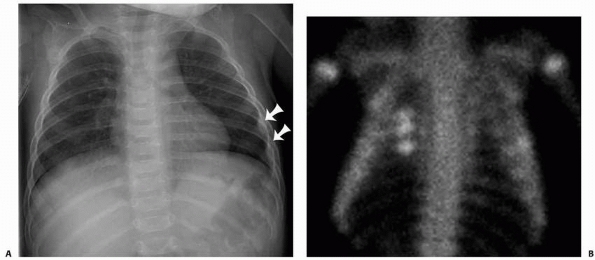 |
|
FIGURE 7-15 Rib fractures in a 9-month-old male victim of nonaccidental trauma. A. Chest radiograph reveals left lateral sixth and seventh rib fractures (arrows). B.
Nuclear medicine bone scan confirms foci of increased uptake within the left lateral ribs as well as revealing additional hot foci in multiple right posterior lateral ribs. |
who have undergone resuscitation for cardiac arrest; in which case,
there may be confusion about the etiology of the fractures. However,
the elasticity of the infant chest allows a high tolerance to
compression, having low reported rates of rib fractures from
cardiopulmonary resuscitation between 0.3% and 2%, with none being
posterior rib fractures.165
Cardiopulmonary resuscitation is therefore a very rare cause of rib
fractures and seldom causes classic posterior rib fractures. Death from
cardiac arrhythmia from a blow to the chest has been reported in a
7-week-old abused infant whose rib fractures at autopsy were initially
thought to be due to resuscitation efforts.18 In addition to rib fractures, abused infants can sustain severe lung contusion and respiratory distress from chest wall trauma,170 with fatal fat embolus reported.183
highdetailed preautopsy skeletal surveys and specimen radiographs are
helpful in fully evaluating and diagnosing child abuse.134 In a postmortem study of 31 infants who died of inflicted skeletal injury,139
there were a total of 165 fractures (51% rib fractures, 39% metaphyseal
long bone fractures, 5% long-bone shaft fractures, 4% fractures of the
hands and feet, 1% clavicular fractures, and less than 1% spinal
fractures).
spinal fractures of fatally abused children generally involve 25% or
less compression of the vertebrae. In a report of 103 children with
cervical spine injury, only three patients had injury due to abuse and
all had spinal cord injury without radiographic abnormality (SCIWORA).40
In another study of fractures of the cervical spine, prevertebral soft
tissue edema on radiographs was the only sign of cervical injury, since
spontaneous reduction of the cervical vertebrae after dislocation was
common.242 Thomas et al.245
reported a 9-week-old boy with spinal cord injury resulting from
cervical spine fracture who presented as a floppy infant. Although
routine cervical radiographs were normal, MRI studies showed
retropulsion of a fragment of the primarily cartilaginous C3 vertebrae
into the spinal canal. Hangman’s type fractures of the posterior
elements have been described in infants as a result of child abuse.143
This must be distinguished from C2 primary spondylolysis which may be
associated with pyknodysostosis, both of which are rare disorders
associated with wormian bones and pencil pointing of the distal
phalanges.67
reported a compression fracture of C5 with anterior subluxation of C4
on C5 in a 3-month-old abused premature twin requiring decompression
and cervical fusion. The other twin had a C5 on C6 fracture-subluxation
treated with casting, but later required surgery to reduce and fuse the
subluxation. MRI was very helpful in showing spinal cord compression in
both cases. Oral189 reported on an inflicted avulsion fracture of C2 and interspinous ligament injury in a 4-year-old child.
buttocks are forcibly slammed onto a flat surface with hyperflexion of
the spine.4,5
Half of these fractures involved the anterosuperior end plate
associated with a compression deformity, 30% had pure compression
fractures, and 20% had fractures of the superior end plate without
significant compression. Positioning premature infants in extreme
hyperflexion for lumbar puncture has been reported to cause iatrogenic
lumbar spine fracture.96 Carrion et al.48 reported circumferential physeal fractures
of the thoracolumbar spine associated with child abuse that required
open reduction. Thoracolumbar fracture dislocations may occur in abused
children with or without neurologic injury.159,219 Flexion-distraction Chance fractures and synchondroses injuries (Fig. 7-16)
may also be seen in nonaccidental trauma. Although neurologic injury in
spinal fractures resulting from child abuse is uncommon,66 any patient with abusive spinal injury should undergo thorough neurologic examination (see Fig. 7-16).
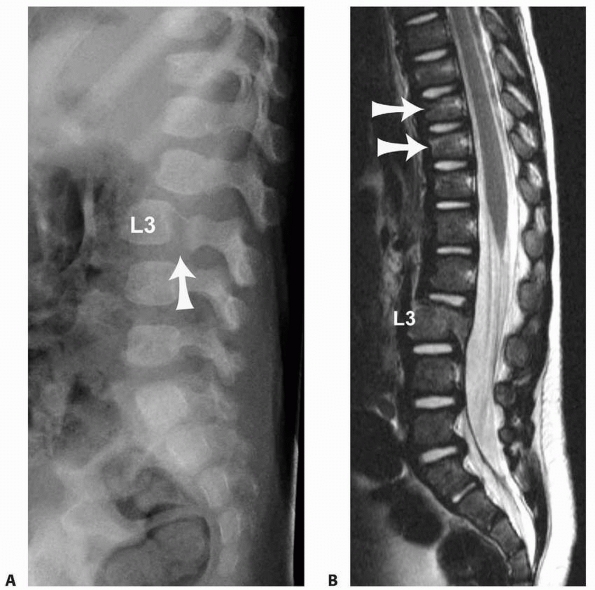 |
|
FIGURE 7-16 Lumbar spine fracture in a 16-month-old male victim of nonaccidental trauma. A. Lateral lumbar radiograph shows lucency through the L3 synchondrosis (arrow) with anterolisthesis of L3 body on L4. B.
Sagittal T2-weighted MRI reveals hyperintense signal within the bone marrow of the fractured L3. Slight compression fractures of T10 and T11 are also noted (arrows). |
with sedimentation rate, liver function studies, and urinalysis.
Clotting studies, including prothrombin time and activated partial
thromboplastin time, thrombin time, fibrinogen, factor VIII, factor IX,
and von Willebrand factor antigen and activity should be performed in
patients with bleeding or ecchymosis to evaluate for bleeding
diathesis. If bruising is the only finding of possible abuse,
consultation with a hematologist may be necessary to fully evaluate for
an unusual bleeding disorder.244
Infants born prematurely are at risk for rickets and low bone density.
Therefore, evaluation of calcium, phosphorous, alkaline phosphatase,
and 25-OH vitamin D may be useful in such infants.
neuron-specific enolase S100B and myelin-basic protein, have been found
to be released into the peripheral circulation, analogous to cardiac
enzyme release after myocardial injury. These two markers when used
together are 79% sensitive and 100% specific in diagnosing traumatic
brain injury, making them potentially very promising for evaluating
suspected mild head trauma.32 If there is suspicion of substance abuse by any family member, a toxicology screen should also be performed on the patient.91
with suspected inflicted injury is the child protective services team.
In a study by Banaszkiewicz et al.,19 three tiers of physicians
reviewed the medical records of 74 children under the age of 1 year
presenting to the emergency department with fractures: staff
clinicians, orthopaedic attendings, and a child protective team
pediatrician. In over one fourth of cases of abuse, the possibility was
underestimated during the original evaluation. Any suspected abuse
should initiate a minimum evaluation that includes an appropriate
radiographic evaluation with a skeletal survey in the younger child,
dilated fundoscopic examination by an ophthalmologist, and consultation
by a child abuse specialist. Any significant nonorthopaedic injury
should prompt consultation by the appropriate subspecialty:
neurosurgery, general surgery, plastic surgery, ophthalmology, or
urology.6 In cases of suspected
sexual abuse, a thorough genital examination will be required,
including a gynecologic consultation for girls. This is typically
initiated by the child protective services team.
diagnosis of child abuse, it is equally important to maintain an
objective, critical view and not to make the diagnosis in error.120
Overdiagnosing child abuse can be harmful to the family, with the
parents being placed at risk of losing custody of their children and
also facing criminal charges.127
Even direct allegations of child abuse may turn out to be false.
Patients or family friends may make false statements about an abuse
situation through misinterpretation, confabulation, fantasy, delusions,
and other situations.33 The American Academy of Child and Adolescent
Psychiatry43
has published guidelines for the evaluation of abuse, stating that the
possibility of false allegations needs to be considered, particularly
if the charges are coming from the parent rather than the child, the
parents are engaged in a dispute over custody or visitation, or the
child is a preschooler.
should not be confused with corner fractures of child abuse. These
variants are seen most commonly in the proximal tibia, distal femur,
proximal fibula, distal radius, and distal ulna. A bony beak may be
seen medially in the proximal humerus or tibia, and is usually
bilateral. Cortical irregularity in the medial proximal tibia may also
be seen in 4% of normal infants and young toddlers and is bilateral in
25%. Beaks may extend beyond the metaphyseal margins in both the distal
radius and the lateral aspect of the distal femur, with bilateral
normal variants in 25% of infants and young toddlers.187
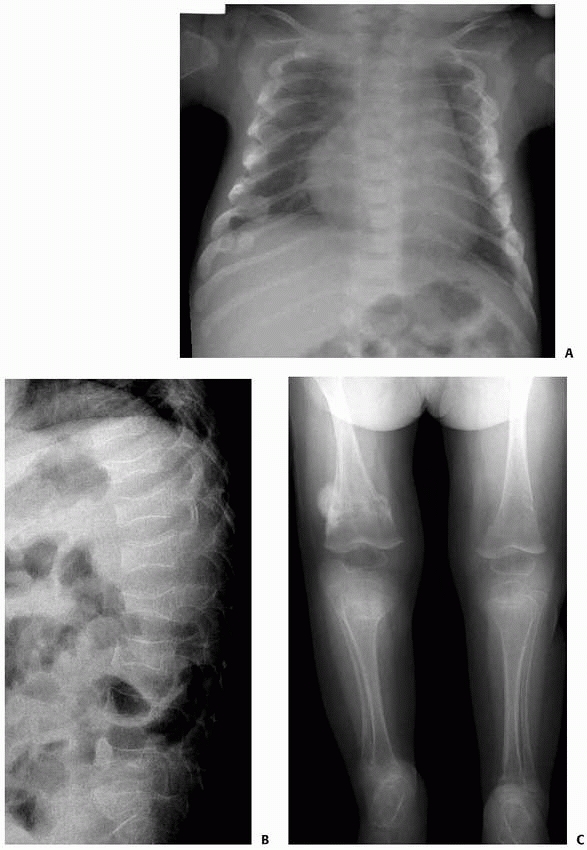 |
|
FIGURE 7-17 Hypophosphatasia in a 2-month-old female with multiple fractures. A. Chest radiograph shows severe osteopenia and multiple bilateral healing rib fractures. B. Lateral spine radiograph reveals multiple compressed vertebra. C. Lower extremity radiographs demonstrate multiple, bilateral healing femoral and lower leg fractures.
|
overlap with the findings of systemic diseases such as Caffey disease
(infantile cortical hyperostosis), osteomyelitis, septic arthritis,
insufficiency fracture, hypophosphatasia (Fig. 7-17), leukemia (Fig. 7-18), metastatic neuroblastoma, osteogenesis imperfecta (OI) (Fig. 7-19), scurvy (Fig. 7-20), vitamin D deficient and drug-induced rickets (Fig. 7-21),
congenital insensitivity to pain, osteopetrosis, kinky hair syndrome,
prostaglandin therapy, osteoid osteoma, and other benign bone tumors.6 Children with biliary atresia may present with osteopenia and fractures
without history of significant injury, which should not be mistaken for child abuse.72
There has been an increase in the incidence of syphilis in females of
childbearing age, and, although extremely rare, congenital syphilis can
mimic fractures of child abuse with diaphysitis, metaphysitis, and
multiple pathologic fractures in different stages of healing.160
Physiologic periostitis, in contrast to lesions from child abuse, is
seen in young infants of about 6 months of age, is usually bilateral,
symmetric, diaphyseal, located on the long bones—humerus, femur, and
tibia—and has no periostitis of the metaphysis.62
Insufficiency rib fractures may be seen in rickets of prematurity as
well as rickets of low birth weight and also have been reported after
chest physiotherapy.53 The presence of metabolic disease and pathologic fractures does not exclude the possibility of child abuse. Duncan and Chandry79
reported a 3-month-old girl with multiple fractures associated with
rickets who died suddenly at 5 months of age. Child abuse was suspected
but not proven. Three years later, evidence of child abuse was found in
a subsequent sibling in the same family.
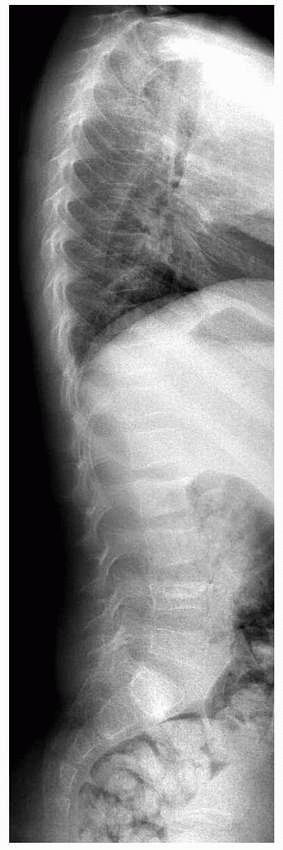 |
|
FIGURE 7-18
Leukemia in a 4-year-old boy presenting with back pain. Lateral spine radiograph shows osteopenia and multiple spine compression fractures. |
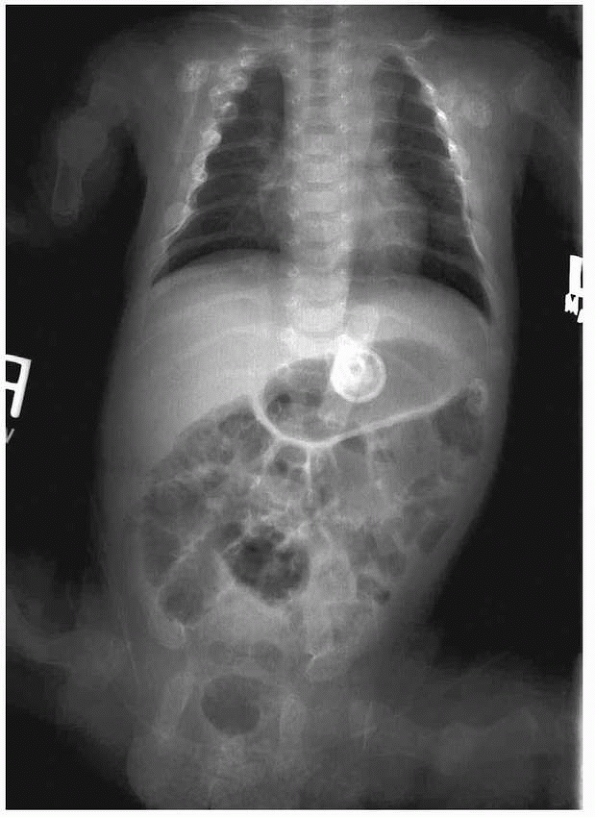 |
|
FIGURE 7-19
Osteogenesis imperfecta in a 2-month-old female with multiple rib and extremity fractures. Frontal radiograph of the chest and abdomen reveals diffuse osteopenia as well as multiple bilateral rib and proximal extremity fractures in various stages of healing. |
hearings as alternative possibilities to nonaccidental traumatic
injuries, and these diseases should be objectively considered in the
differential diagnosis. Linear lucencies of the proximal tibia noted
after intraosseous vascular access needles may mimic fractures, but
careful analysis of the imaging studies can determine the actual cause
of the lucency.102 Metaphyseal
corner fractures of the distal tibia and fibula were seen in eight
children treated with likely forceful serial casting for clubfoot, with
only one potentially related to nonaccidental trauma.94 Leukemia should always be considered in a child with diffuse osteopenia or metaphyseal lucencies. McClain et al.168
reported a 2-year-old child who died of undiagnosed acute lymphoblastic
leukemia, having been earlier reported as a possible victim of child
abuse. Ecchymosis on the back and extremities did not initiate an
appropriate evaluation for leukemia or bleeding disorder. Clinical
signs of leukemia, including fever, pallor, petechia, purpura,
adenopathy, hepatosplenomegaly, and bone pain, should be sought in
children with bruising of unknown origin. Factor XIII deficiency may
cause unexplained bleeding from minor trauma and be mistaken for child
abuse because the standard coagulation profile may be negative and
factor-specific tests may be negative if performed posttransfusion.181
presents with multiple fractures of unknown etiology, but may be a
difficult diagnosis to make. OI caused by spontaneous mutation can
occur without a family history.195
The so-called hallmark of OI is an intensely blue sclerae, but this
feature is consistently present only in Sillence type I,220 may be
completely absent in patients with type IV, and is less obvious in type
III.195 Sillence and Butler221
noted that patients with either type II or III OI may have blue sclerae
at birth, but the sclerae can become normal by adolescence. The rare
Sillence type II OI, termed Congenta A in the Shapiro classification,
has normal sclerae, but bone abnormalities and osteopenia are severe
and early death is likely.195 Blue
sclerae may be present in normal young infants and can be
misinterpreted as a sign of OI. The presence of abnormal teeth, known
as dentinogenesis imperfecta, may be helpful in a diagnosis if the
child is old enough
for
teeth to have erupted. Plain radiographs may show long bones of normal
density in both types I and IV OI. Another radiographic sign of OI,
wormian bones of the skull, is consistently present only in type III
and is often absent in types I and IV.195
Since type IV OI does not have blue sclera or wormian bones and is a
milder form of OI than type III, diagnosis may be initially delayed or
confused with nonaccidental trauma. Other rare types of OI have been
described, which further confounds the medical and legal evaluation.
Some authors believe that the presence of metaphyseal fracture is
pathognomonic for child abuse and, therefore, helpful to distinguish
abuse from OI,1,14 but others71,195
believe that there is no particular fracture pattern that renders the
diagnosis of OI likely. Children with OI tend to bruise excessively,
which overlaps with child abuse.217 SIDS has also been described in infants with undiagnosed OI.187
 |
|
FIGURE 7-20 Scurvy in a 3-year-old male with bruising and petechia (A), bleeding and infected appearing gums, poorly healing biopsy incision (B), and bilateral distal femoral fractures. C. Lateral radiographs of the lower extremities show bilateral subperiosteal hematomas seen as uplifting of the periosteum (arrows). D.
Follow-up frontal radiograph of the lower extremities after treatment with vitamin C demonstrates calcification of subperiosteal hematomas, as well as metaphyseal irregularity similar to classic metaphyseal lesions (arrowheads). |
and Rimsza90
reported that 87% of children with OI have abnormal procollagen that
can be detected by a skin biopsy with fibroblast culture. Fibroblasts
are assayed for abnormally low levels of procollagen as well as primary
abnormal procollagen.42 Steiner et al.231
reported that over a 4-year period, 48 patients were referred for
collagen analysis to diagnose OI in cases of suspected child abuse.
Only 6 of these 48 children had abnormal collagen test results, and in
five of the six patients, the diagnosis of OI could have been made on
clinical and radiologic findings. More recently, Malowe et al.166
found 11 of 262 samples submitted to rule out OI had alterations in the
amount or structure of type I collagen synthesized, consistent with the
diagnosis of OI. In 11 others, OI could not be excluded. Referring
physicians correctly diagnosed children with OI in six of the 11
patients clinically. Four children believed to have OI by physical
examination had normal biochemical studies, representing a
false-positive clinical diagnosis, attributed mostly to the use of
sclera hue as a major diagnostic criterion.167
The authors concluded that laboratory testing for OI remains a valuable
adjunct when determining the etiology of fractures in children. Even
when a child has OI or other metabolic bone disorders, fractures may be
due to comorbid nonaccidental trauma. Knight and Bennett.145
reported a young child with OI whose abuse could not be proved until
linear bruising of the face from being slapped was documented.
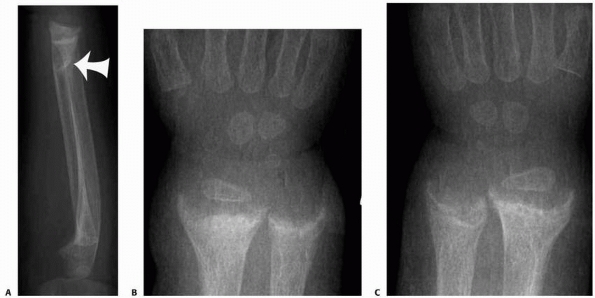 |
|
FIGURE 7-21 Rickets in a 16-month-old male who was breast fed. A. Lateral forearm radiograph shows osteopenia and a distal radial fracture (arrow) with some dorsal angulation (B,C). Metaphyseal cupping and fraying of the distal radius and ulna bilaterally are also noted.
|
described 39 patients with a variant of OI that they described as a
temporary brittle bone disease in which fractures were limited to the
first year of life followed by spontaneous improvement. However, an
extensive review by the Society for Pediatric Radiology175
concluded that the entity of temporary brittle bone disease has
insufficient scientific evidence to warrant this as a plausible
diagnosis.
handled appropriately with the medical and the legal systems
cooperatively involved.123 SIDS is a
subset of sudden unexpected death in infancy (SUDI) and refers to the
death of an infant less than 1 year of age with the onset of the fatal
episode apparently occurring during sleep that remains unexplained
after a thorough review of the circumstances of death and clinical
history.123,258
Since SIDS is more common than infanticide, death by abuse intentional
suffocation is very commonly initially attributed to SIDS before the
correct diagnosis is made.116a However, other causes of sudden death such as intracranial bleeds must be excluded. Byard et al.41
reported a 5-month-old girl who died suddenly from spontaneous
subarachnoid hemorrhage from undiagnosed Ehlers-Danlos syndrome. They
recommended collagen analysis in patients with unexplained multifocal
spontaneous hemorrhages to exclude this rare syndrome. Sperry and
Pfalzgraf228 reported a 9-month-old
infant whose diagnosis of SIDS became uncertain when postmortem
radiographs showed healing symmetric clavicle fractures and a healing
left medial humeral condyle fracture. Subsequent investigation showed
that the child had undergone “chiropractic” manipulation 4 weeks before
death by an unlicensed therapist to correct “shoulder dislocations,”
with the parents exonerated of abuse charges. When abuse is suspected
in an infant fatality, combined radiology, CT scan, detailed forensic
autopsy, and osteologic investigation is required to detect all
fractures that are present.50 Detailed examination of organs, such as the orbit, are also becoming the standard in autopsy protocols.178
in treatment is hospital admission. This is therapeutic in that it
places the child in a safe, protected environment, provides the
opportunity for additional diagnostic workup, and, more importantly,
investigation of the family’s social situation by appropriate
personnel. In tertiary centers, multidisciplinary teams often are
available to evaluate and treat such children, but in other
circumstances the orthopaedist may be primarily responsible for
coordinating both evaluation and treatment. Court custody may be
required for children of uncooperative families who refuse admission,
and hospitalization should be continued until a full investigation is
completed by the appropriate child protective services and a safe
disposition is established. In the United States, the physician is
required by law to report all suspected abuse to appropriate child
protective services or legal authorities. Although physicians have
better reporting rates than most other professionals, 27% of injuries
considered likely to be caused by abuse and 76% of injuries that were
considered possibly related to child abuse were not reported.85
When the reporting is done in good faith, the physician has immunity
against criminal or civil liability for these actions, but in only
three states—Ohio, California, and Alabama—does this protection include
absolute immunity.59 The distinction
is critical. Absolute immunity means that the physician who reports
suspected child abuse cannot ever be held for damages sought by
families for allegedly inappropriate reports of child abuse or neglect.
The granting of absolute immunity, even for physicians, is not
encouraged by the American legal system because in theory it would
protect individuals who make false reports of child abuse in order to
harass families and would deprive the injured parties their legal right
to seek damages for harmful actions. In contrast, physician immunity
based on good faith reporting of suspected child abuse is contingent on
the physician having a reasonable belief that abuse or neglect has
occurred. Although in theory this protection seems to be quite
adequate, recently there has been a dramatic rise in the number of
lawsuits filed by families seeking damages for alleged, unfounded
reports of child abuse and neglect. Although it is true that by the
time these lawsuits are eventually resolved, physicians have almost
never been held liable for good faith reports of child abuse, in a
substantial number of these cases, the physicians first lost at trial
level before eventually prevailing at appeal. Considerable expense,
frustration, and loss of time can be experienced by the physician in
defending against such allegations as the families and their attorneys
pursue multiple forms of legal theories in court and attempt to evade
the immunity provisions.59 On the
other hand, the stakes for failure to report suspected child abuse are
likely much higher, potentially exposing the physician to charges of
malpractice.4
of definitive child abuse or neglect but also cases when abuse is just
suspected or is considered a possibility. Physicians have been held
liable for damages for their negligence in failing to diagnose child
abuse when the child subsequently was reinjured by further abuse, and,
ironically, the parents also may be able to collect additional
compensation for losses resulting from medical expenses. For families
to be successful in these lawsuits, they must be able to prove that the
failure to make the diagnosis of child abuse was negligent and that,
had the diagnosis been made, steps would have been taken to protect the
child from additional abuse. Although the probability of a physician
being held liable under such circumstances is low, the amount of
damages can be high if the family does prevail when the child has
suffered permanent sequelae.59
the child’s musculoskeletal injuries and facilitates various medical
consultations. Recommendations for disposition of the child after
completion of medical treatment may be a group decision through a
multidisciplinary team or, more often, the decision of the primary
physician, who may be the orthopaedist. Final disposition choices may
include return to the family, return to a family member who does not
live in the child’s home, or placement in a shelter or a foster home
setting. The risk of reinjury and death is significant if the abused
child is returned to the unsafe home, so the orthopaedist must strongly
support child protective services in custodial actions when it is
believed that a child’s injury truly occurred from abuse at home. Not
only must the definitive diagnosis of child abuse be documented in the
chart, but a separate notarized affidavit may be necessary. Commonly,
custodial actions by child protective services are reviewed in a court
hearing in a matter of weeks, and the physician may be called to
testify in the hearing. Criminal charges also may be brought against
the perpetrator of the child abuse, and the physician likely also
serves as a witness in these proceedings.
child abuse proceedings. First, he or she serves as a material witness
whose testimony is confined to the physician’s personal involvement in
the legal matter of the child’s evaluation and treatment. The testimony
may include clarification to the court of information contained in
progress notes in the chart or of other past documentation. As a
material witness, the physician cannot render opinions about the facts
as stated during his or her testimony. In addition, however, the
physician may also be sworn in as an expert witness.98
This is an individual considered by the court to have special knowledge
and experience that qualifies him or her to render opinions about
certain facts presented in the courtroom. The limits of the physician’s
expertise usually are defined by the attorneys in court before the
testimony of the expert witness.
reasons. The courtroom is an unfamiliar setting for most physicians and
the adversarial nature of the American legal system may be perceived as
a hostile environment. In the courtroom, opposing attorneys are likely
to search for inconsistencies in the testimony or unfamiliarity with
the record to discredit the physician witness.
meticulously prepare to give testimony by conducting a thorough review
of the child’s medical records and a review of recent medical
literature on the subject of child abuse.98
Often, there is a pretestimony discussion with child protective
services counsel in family court cases or the district attorney’s
office in criminal cases. Such meetings should preferably be in person,
and the orthopaedist’s professional training and expertise are examined
to determine whether he or she may serve as a material witness, an
expert witness, or both. The attorney should be provided the
orthopaedist’s curriculum vitae, and another copy
should
be made available to the court. If the orthopaedist is to serve as a
material witness, the factual information of the case as well as the
limitations of the physician’s knowledge are discussed, as are
questions that may be posed during testimony. Orthopaedists functioning
as expert witnesses should indicate relevant information that should be
provided through questioning during testimony. In addition, anticipated
testimony from any opposing expert witness and cross-examination
questions from the opposing attorney should be discussed. The opposing
attorney also may request an informal pretestimony meeting. The
orthopaedist should request a list of questions that will be asked in
this session ahead of time and request that both the prosecution
attorney and the opposing attorney be present during the session, which
often is recorded.
attorneys question the witness under oath to “discover” the testimony
that the witness will provide in court. The primary purpose for a
deposition in the discovery process is to keep attorneys from later
being surprised in court by testimony of witnesses.52
Any testimony the physician gives during the deposition will be
recorded, and later in court any inconsistencies between testimony and
prior depositions will be vigorously attacked by attorneys in
cross-examination. Depositions are rarely used in criminal prosecutions98;
instead, a subpoena is issued requiring a physician witness to appear
at the courtroom at a certain time. Often, there may be hours of delay
before the testimony actually begins. Through prior arrangements with
the attorneys, the orthopaedist may be placed “on call” if he or she
works within a reasonable distance of the courtroom and can be
available a short time before the actual testimony is needed. The
physician has no legal right to such treatment and must be prepared to
honor the exact conditions of the subpoena if alternative arrangements
cannot be made. If significant delays are encountered to giving
testimony and the attorneys are not responsive to physician hardship,
then the orthopaedist should contact the judge directly to remedy the
situation.52 In the courtroom, the orthopaedist should be conservatively dressed and appear attentive, competent, poised, and at ease.52,98
and identified. Next follows qualification, direct examination, and
then cross-examination. In the qualification process, the attorney asks
the physician fairly detailed questions about the orthopaedist’s
training and background to establish whether he or she is a credible
witness.98 The attorney wishes to
impress the judge or jury with the orthopaedist’s qualifications as a
witness, whereas the opposing attorney may challenge the witness with
questions to cast doubt on his or her expertise.52
During this phase, the attorneys also may establish the limits of the
physician’s expertise as an expert medical witness. Next, the attorney
will proceed with direct examination. A series of questions are asked
that aim at developing a logical and progressive line of thought
leading to a conclusion.52 In child
abuse cases, in particular, the testimony will lead to the fact that
the abuse has occurred and that it has been appropriately diagnosed. In
addition, the physician expert witness may be asked to give an opinion
of the risk for subsequent abuse if the child returns to the home where
the alleged abuse occurred. The physician witness will almost never be
asked about the guilt or innocence of the caretaker accused of abuse,
but the orthopaedist in certain circumstances will come close to
answering the “ultimate question”52
by testifying about a child’s statement of history if it identifies the
abuser. Some states, however, restrict such testimony. In Maryland, a
physician may not testify regarding any disclosures made by a child
abuse victim unless the disclosure is admissible under a recognized
exception to the rule prohibiting hearsay evidence.237
The orthopaedist should ask about any possible restrictions on his or
her testimony with the attorney in pretrial discussion. In testimony,
the orthopaedist will want to use the courtroom setting to advocate for
the safety and well-being of the child.98
Questions regarding medical findings often will be prefaced in the
courtroom by the words “reasonable medical certainty,” a term that is
poorly understood by most physicians. Chadwick52
offered a definition of reasonable medical certainty as “certain as a
physician should be in order to recommend and carry out treatment for a
given medical condition.” He offered an example that the certainty for
the diagnosis and treatment of leukemia must be much higher than that
for diagnosis and treatment of a viral upper respiratory tract
infection.
carefully chosen and should be understandable by a lay jury. Testimony
should be objective, honest, and thorough.98
Attorneys may frame questions in ways that are difficult to understand,
and the orthopaedist should not hesitate to ask the attorney to clarify
a question.52 Answers should be
brief, without volunteering extra information, but the perception
listeners will have of the answers should be carefully considered by
the orthopaedist. In particular, attorneys may phrase yes or no
questions that could place misleading words in the mouth of the
orthopaedist. In such situations, when neither response is appropriate,
the orthopaedist should answer in a sentence that provides an accurate
answer.98 Language should be
straightforward, and visual aids may be used in providing clear
testimony. The expert should use testimony as an educational process
for the court, in which the common experience and knowledge of the jury
is used to build understanding with common sense explanations of
medical findings.52
direct examination. The opposing attorney’s role is to challenge the
material presented by the physician witness to protect the defendant.98
This may involve an attempt to bring into question the physician’s
credibility, the medical record, the physician’s training or expertise,
or the physician’s objectivity or composure and clarity of thought
before the jury.98 Attorneys may
accomplish this by finding inconsistencies with prior statements,
asking leading questions as well as questions that allow only certain
desired answers, and minimizing physician qualifications.52
The attorney may frame a question that contains certain elements that
the physician agrees with and others that are misleading, and often the
question will end with “Isn’t that so, doctor?” or “Is that true?” The
physician witness should be firm in answering such questions, clearly
stating what in the question he or she agrees with and what he or she
does not. It is also common to encounter questions from attorneys based
on hypotheses that are extremely unlikely, and the physician needs to
point out that unlikelihood.52 Part
of the strategy of aggressive cross-examination is to provoke the
physician into arguments or unprofessional behavior that could
discredit the physician or his or her testimony before the court. In
particular, juries will allow aggression on the part of an attorney,
but they expect physician witnesses to respond professionally, even
under extreme duress.69 Inexperienced potential physician witnesses can prepare
themselves by either watching trials or participating in mock trials.52 Brent38
assembled an excellent series of vignettes of expert medical witness
case studies in court and provided detailed instructions with regard to
the responsibilities of such experts. Both redirect examination and
recross-examination may follow cross-examination at the discretion of
attorneys, but usually these procedures are very short.52
remains in the protective custody of the state or was returned to the
home, but the danger of further abuse exists in both situations. In a
study of recurrent maltreatment in 10 states based on the National
Child Abuse and Neglect Data System, Fluke et al.86
found that the recurrence rate was 13% by 6 months after the first
episode of reported abuse and return to the home, increasing to 17% by
12 months. In a report of 206 care and protection petitions brought to
the Boston juvenile courts,179 31
were dismissed with return of the child to the parents. During a 2-year
follow-up of these dismissed cases, 29 had reports of further
mistreatment, and 16 were returned to court under another care and
protection petition. One risk factor identified by the study was a
previous appearance in court; half of dismissed cases with this risk
factor returned to court again. Children ordered permanently removed
from parental custody by the court may still suffer further abuse by a
new caretaker. Another alternative pathway of custody is gaining
popularity with the court systems in which the abused child is released
to the custody of a relative of the family with consideration given to
the wishes of the parents or other prior custodians of the child.
Although in theory this approach may help preserve the integrity of the
family unit, the child may still be in danger in this sort of
arrangement. Handy et al.99 of the
Pediatric Forensic Medicine Program of the Kentucky State Medical
Examiner’s Office noted evidence of recurrent abuse 2 to 9 months after
the original injury in six patients out of 316 referrals (1.8%) to the
program. They emphasized that in two of these cases, the child was in
protective custody of a family relative when the original perpetrator
was allowed unsupervised access to the child in violation of court
order. It is possible that such reinjuries occur because either the
close relatives of the child abuser may not believe that the caretaker
committed the original abuse or the relatives are under emotional
pressure to allow the caretaker to have access to the child in spite of
court order. It is hoped that the court systems can strike a balance
between the need to preserve the family unit and the need to protect
the child from further abuse.
Home visitor programs can contact a mother immediately after the birth
of her child and arrange for a visit in which the mother’s parenting
strengths are assessed. Parents requiring additional support are linked
to community agencies and family resources.10,227
Practicing Safety, a project sponsored by the American Academy of
Pediatrics (AAP) and funded by the Doris Duke Charitable Foundation,
works to decrease child abuse and neglect by expanding anticipatory
guidance and increasing screening by pediatric practices to parents of
children aged 0 to 3 years. The AAP website
(www.aap.org/practicingsafety) also lists resources for physicians and
parents.
parenting skills such as discipline methods, basic childcare, infant
stimulation, child development, education, and familiarity with local
support services. Such support seems to enhance parent and child
interactions, and mothers report a diminished need to punish or
restrict their children. Antivictimization programs teach children
certain concepts believed to facilitate self-protection, such as
identification of strangers, types of touching, saying “no” to
inappropriate advances, and telling someone about inappropriate
behavior.
and trauma team’s prompt recognition of child abuse in the emergency
department or clinic and appropriate intervention.55
After protecting the welfare of the child, the most important issue in
dealing with child abuse is to help both the child and the family
through early recognition of the problem and appropriate therapeutic
measures by all health personnel.
Sheppard for technical assistance with the manuscript and to Drs. Sami
Abedin and Reza Zinati for their medical illustrations.
DS, Greenspan A, Reinhart M, et al. Differentiation of child abuse from
osteogenesis imperfecta. AJR Am J Roentgenol 1990;154(5):1035-1046.
JA, Kaplan RA, Starling SP, et al. Guidelines for medical care of
children who may have been sexually abused. J Pediatr Adolesc Gynecol
2007;20(3):163-172.
B, Torg JS, Kirkpatrick J, et al. Manifestations of the battered-child
syndrome. J Bone Joint Surg Am 1974;56(6):1159-1166.
RC, Surrell JA, Cohle SD. Microwave oven burns to children: an unusual
manifestation of child abuse. Pediatrics 1987;79(2):255-260.
Academy of Pediatrics Committee on Child Abuse and Neglect: Guidelines
for the evaluation of sexual abuse of children. Pediatrics
1991;87(2):254-260.
Academy of Pediatrics. A guide to references and resources in child
abuse and neglect. In: AAP, ed. American Academy of Pediatrics: Section
on Child Abuse and Neglect. Elk Grove Village, IL; Author; 1994:107-190.
JD. Assessment of factors resulting in abuse evaluations in young
children with minor head trauma. Child Abuse Negl 2008;32(3):405-413.
A, Friedman JE, Warner WC Jr, et al. Complete distal femoral
metaphyseal fractures: a harbinger of child abuse before walking age. J
Pediatr Orthop 2007;27(7): 751-753.
J, Hartman K, Pedersen A, et al. Rodenticide-induced coagulopathy in a
young child. A case of Munchausen syndrome by proxy. Am J Pediatr
Hematol Oncol 1993; 15(1):126-130.
AM, Craig BR, Lonergan GJ. Homicidal commotio cordis: the final blow in
a battered infant. Child Abuse Negl 2003;27(1):125-130.
PA, Scotland TR, Myerscough EJ. Fractures in children younger than age
1 year: importance of collaboration with child protection services. J
Pediatr Orthop 2002;22(6):740-744.
KM, Thomson E, Johnson D, et al. Late neurologic and cognitive sequelae
of inflicted traumatic brain injury in infancy. Pediatrics
2005;116(2):e174-185.
PD, Krasnokutsky M. Imaging of the central nervous system in suspected
or alleged nonaccidental injury, including the mimics. Top Magn Reson
Imaging 2007; 18(1):53-74.
RG, Trent RB, Cross J. Age-related incidence curve of hospitalized
Shaken Baby Syndrome cases: convergent evidence for crying as a trigger
to shaking. Child Abuse Negl 2006;30(1):7-16.
KA, Cha ES, Bensard DD, et al. The positive predictive value of rib
fractures as an indicator of nonaccidental trauma in children. J Trauma
2003;54(6):1107-1110.
C, Risse M, Schutz H, et al. Munchausen syndrome by proxy (MSBP): an
extreme form of child abuse with a special forensic challenge. Forensic
Sci Int 2003; 137(2-3):147-151.
DE, Stein F, Coats DK, et al. Recurrent conjunctivitis as a
presentation of Münchhausen syndrome by proxy. Ophthalmology
2003;110(8):1582-1584.
MI, White RB, Wulff LM, et al. Reported maltreatment in children with
multiple disabilities. Child Abuse Negl 1990;14(2):207-217.
RP, Dulani T, Adelson PD, et al. Identification of inflicted traumatic
brain injury in well-appearing infants using serum and cerebrospinal
markers: a possible screening tool. Pediatrics 2006;117(2):325-332.
W. False statements and the differential diagnosis of abuse
allegations. J Am Acad Child Adolesc Psychiatry 1993;32(5):903-910.
D, Shelton D. Perpetrator accounts in infant abusive head trauma
brought about by a shaking event. Child Abuse Negl
2005;29(12):1347-1358.
DL, Shelton D. Functional time limit and onset of symptoms in infant
abusive head trauma. J Paediatr Child Health 2007;43(1-2):60-65.
LC, Loder RT, Hensinger RN. Role of intentional abuse in children 1 to
5 years old with isolated femoral shaft fractures. J Pediatr Orthop
1996;16(5):585-588.
JL, Guenther E, Filloux FM, et al. Death, child abuse, and adverse
neurological outcome of infants after an apparent life-threatening
event. Pediatrics 2008;122(1): 125-131.
RL. The irresponsible expert witness: a failure of biomedical graduate
education and professional accountability. Pediatrics
1982;70(5):754-762.
RA, Bass DH, Rode H, et al. Gastrointestinal tract perforation in
children due to blunt abdominal trauma. Br J Surg 1992;79(6):522-524.
RL, Brunn MA, Garcia VF. Cervical spine injuries in children: a review
of 103 patients treated consecutively at a level 1 pediatric trauma
center. J Pediatr Surg 2001; 36(8):1107-1114.
RW, Keeley FW, Smith CR. Type IV Ehlers-Danlos syndrome presenting as
sudden infant death. Am J Clin Pathol 1990;93(4):579-582.
J. The whiplash shaken infant syndrome: manual shaking by the
extremities with whiplash-induced intracranial and intraocular
bleedings, linked with residual permanent brain damage and mental
retardation. Pediatrics 1974;54(4):396-403.
WV, Dormans JP, Drummond DS, et al. Circumferential growth plate
fracture of the thoracolumbar spine from child abuse. J Pediatr Orthop
1996;16(2):210-214.
DM, Doria AS, Paul BS. Clinical-radiological features of fractures in
premature infants—a review. J Perinat Med 2007;35(5):366-375.
C, Marinelli E, Di Giancamillo A, et al. Sensitivity of autopsy and
radiological examination in detecting bone fractures in an animal
model: implications for the assessment of fatal child physical abuse.
Forensic Sci Int 2006;164(2-3):131-137.
for Disease Control and Prevention. Nonfatal maltreatment on infants.
United States, October 2005 to September 2006. Morb Mortal Wkly Rep
2008;27:338-339.
DL, Bertocci G, Castillo E, et al. Annual risk of death resulting from
short falls among young children: less than 1 in 1 million. Pediatrics
2008;121(6):1213-1224.
M, Foix-L’Helias L, Scheinmann P, et al. Rib fractures after chest
physiotherapy for bronchiolitis or pneumonia in infants. Pediatr Radiol
2002;32(9):644-647.
DC, Knight V, Ziegfeld S, et al. The tip of the iceberg for child
abuse: the critical roles of the pediatric trauma service and its
registry. J Trauma 2004;57(6):1189-1198; discussion 1198.
PN, Kornberg AE, Brody AS, et al. Markers for occult liver injury in
cases of physical abuse in children. Pediatrics 1992;89(2):274-278.
C, Haley K, Hayes J, et al. The risk of child abuse in infants and
toddlers with lower extremity injuries. J Pediatr Surg
2005;40(1):120-123.
JL, Behl LE. Relationships among parental beliefs in corporal
punishment, reported stress, and physical child abuse potential. Child
Abuse Negl 2001;25(3): 413-419.
TL, DiGuiseppi C, Byers T, et al. Underascertainment of child
maltreatment fatalities by death certificates, 1990 to 1998. Pediatrics
2002;110(2 Pt 1):e18.
G. Primary spondylolysis of the axis vertebra (C2) in three children,
including one with pyknodysostosis. Pediatr Radiol 1989;19(8):535-538.
G, Birch JG, Herring JA. Developmental coxa vara associated with
spondylometaphyseal dysplasia (DCV/SMD): “SMD-corner fracture type”
(DCV/SMD-CF) demonstrated in most reported cases. Pediatr Radiol
2000;30(1):14-24.
HJ, Slovis T, Helfer RE, et al. Undiagnosed abuse in children younger
than 3 years with femoral fracture. Am J Dis Child 1990;144(8):875-878.
PA, Spevak MR, Schwarz KB. Fractures in biliary atresia misinterpreted
as child abuse. Pediatrics 2003;112(1 Pt 1):185-188.
MS, Smith K, DeGuehery K, et al. Preventing abusive head trauma among
infants and young children: a hospital-based, parent education program.
Pediatrics 2005; 115(4):e470-477.
S, Spirakis CN, Stone RE. The influence of age and nutritional status
on “bone scar” formation in the distal end of the growing radius. Am J
Phys Anthropol 1964; 22:295-305.
AC, Gennarelli TA, Thibault LE, et al. The shaken baby syndrome. A
clinical, pathological, and biomechanical study. J Neurosurg
1987;66(3):409-415.
S, Obaldo RE, Walsh IR, et al. Neuroimaging of nonaccidental head
trauma: pitfalls and controversies. Pediatr Radiol 2008;38(8):827-838.
EG. Analysis of caretaker histories in abuse: comparing initial
histories with subsequent confessions. Child Abuse Negl
2006;30(7):789-798.
EG, Sege R, Mattson CL, et al. Assessment of suspicion of abuse in the
primary care setting. Ambul Pediatr 2002;2(2):120-126.
EG, Sege RD, Griffith J, et al. From suspicion of physical child abuse
to reporting: primary care clinician decision-making. Pediatrics
2008;122(3):611-619.
JD, Yuan YY, Edwards M. Recurrence of maltreatment: an application of
the National Child Abuse and Neglect Data System (NCANDS). Child Abuse
Negl 1999; 23(7):633-650.
L Rauth-Farley K, Alexander R, et al. Abusive Head Trauma in Infants
and Children: A Medical, Legal, and Forensic Reference. St. Louis, MO:
GW Medical Publishing; 2006.
AM, Boal DK, Wallach DM, et al. Metaphyseal fractures mimicking abuse
during treatment for clubfoot. Pediatr Radiol 2001;31(8):559-563.
J, Haller JO. Iatrogenic vertebral body compression fracture in a
premature infant caused by extreme flexion during positioning for a
lumbar puncture. Pediatr Radiol 2000;30(6):410-411.
DE, Eubanks L, Meyyazhagan LS, et al. Evaluation of covert video
surveillance in the diagnosis of munchausen syndrome by proxy: lessons
from 41 cases. Pediatrics 2000;105(6):1305-1312.
M, McAuliff T. Preparation for child abuse litigation: perspectives of
the prosecutor and the pediatrician. Pediatr Ann 1997;26(5):288-295.
MP, Kao SC. Intraosseous vascular access defect: fracture mimic in the
skeletal survey for child abuse. Pediatr Radiol 2002;32(3):188-190.
S, Huyer D, Manson D. Sternal fractures as a manifestation of abusive
injury in children. Pediatr Radiol 2002;32(12):902-906.
TR, Priolo D, Hultman CS, et al. Eczema mimicking child abuse: a case
of mistaken identity. J Burn Care Rehabil 2002;23(5):357-359;
discussion 357.
WL, Shaw BA, Gerardi JA. Injuries when children reportedly fall from a
bed or couch. Clin Orthop Relat Res 2003(407):148-151.
ME, Brown G, Verbiest S, et al. Underascertainment of child abuse
mortality in the United States. JAMA 1999;282(5):463-467.
HS, Sankar WN, Wills BP, et al. Congenital osseous anomalies of the
upper cervical spine. J Bone Joint Surg Am 2008;90(2):337-348.
LA, May K, Talbot JF, et al. Incidence, distribution, and duration of
birthrelated retinal hemorrhages: a prospective study. J AAPOS
2006;10(2):102-106.
C, Joughin E, Goldstein S, et al. Femoral fractures in children younger
than three years: the role of nonaccidental injury. J Pediatr Orthop
2008;28(3):297-302.
PW, Gallagher TA. Child abuse intervention in the emergency room.
Pediatr Clin North Am 1992;39(5):1053-1081. 116a. Hymel KP, and the
Committee on Child abuse and Neglect and National Association of
Medical Examiners. Distinguishing sudden infant death syndrome from
child abuse fatalities. Pediatrics 2006;118:421-427.
KP, Makoroff KL, Laskey AL, et al. Mechanisms, clinical presentations,
injuries, and outcomes from inflicted versus noninflicted head trauma
during infancy: results of a prospective, multicentered, comparative
study. Pediatrics 2007;119(5):922-929.
DM, Everett VD, Ingram DL. The relationship between the transverse
hymenal orifice diameter by the separation technique and other possible
markers of sexual abuse. Child Abuse Negl 2001;25(8):1109-1120.
PK. Comparison of radiography and radionuclide bone scanning in the
detection of child abuse. Pediatrics 1984;73(2):166-168.
HT, Runyan DK, Marshall SW, et al. A population-based study of
inflicted traumatic brain injury in young children. JAMA
2003;290(5):621-626.
ND, Menard SW, Santos A. Genital anatomy in pregnant adolescents:
“normal” does not mean “nothing happened.” Pediatrics 2004;113(1 Pt
1):e67-69.
AM, Butler A, Morris S, et al. Which radiological investigations should
be performed to identify fractures in suspected child abuse? Clin
Radiol 2006;61(9):723-736.
PK, Blackbourne BD, Marks SC, et al. Radiologic contributions to the
investigation and prosecution of cases of fatal infant abuse. N Engl J
Med 1989;320(8): 507-511.
PK, Marks SC. Vertebral body fractures in child abuse.
Radiologic-histopathologic correlates. Invest Radiol 1992;27(9):715-722.
PK, Marks SC Jr. Relationship of the subperiosteal bone collar to
metaphyseal lesions in abused infants. J Bone Joint Surg Am
1995;77(10):1471-1476.
PK, Marks SC Jr, Adams VI, et al. Factors affecting visualization of
posterior rib fractures in abused infants. AJR Am J Roentgenol
1988;150(3):635-638.
PK, Marks SC Jr, Blackbourne B. The metaphyseal lesion in abused
infants: a radiologic-histopathologic study. AJR Am J Roentgenol
1986;146(5):895-905.
PK, Marks SC Jr, Richmond JM, et al. Inflicted skeletal injury: a
postmortem radiologic-histopathologic study in 31 infants. AJR Am J
Roentgenol 1995;165(3): 647-650.
PK, Nimkin K, Spevak MR, et al. Follow-up skeletal surveys in suspected
child abuse. AJR Am J Roentgenol 1996;167(4):893-896.
PK, O’Connor B, Nimkin K, et al. Detection of rib fractures in an
abused infant using digital radiography: a laboratory study. Pediatr
Radiol 2002;32(12): 896-901.
PK, Spevak MR. Variations in acromial ossification simulating infant
abuse in victims of sudden infant death syndrome. Radiology
1991;180(1):185-187.
MS, Swischuk LE, Fagan CJ. Patterns of injury and significance of
uncommon fractures in the battered child syndrome. Am J Roentgenol
Radium Ther Nucl Med 1974;121(1):143-149.
H, Driessen G, Gomberg R, et al. Accidental falls from elevated
surfaces in infants from birth to 1 year of age. Pediatrics
1969;44(5):869-876.
J. Ambroise Tardieu: the man and his work on child maltreatment a
century before Kempe. Child Abuse Negl 2005;29(4):311-324.
WG, Dubowitz H. What factors affect the identification and reporting of
child abuse-related fractures? Clin Orthop Relat Res 2007;461:219-225.
NE, Gresham GA. The aging of bruises: a review and study of the color
changes with time. Forensic Sci Int 1991;50(2):227-238.
DJ, Hatch EI Jr, Feldman KW, et al. Diagnostic and surgical
implications of child abuse. Arch Surg 1988;123(9):1101-1105.
JM, Thomas SA, Rosenfield SN, et al. Fractures in young children:
distinguishing child abuse from unintentional injuries. Am Dis Child
1993;147(1):87-92.
JM, Larson IA, Abdoo D, et al. Are abusive fractures in young children
becoming less common? Changes over 24 years. Child Abuse Negl
2007;31(3): 311-322.
TL, Berdon WE, Cassell I, et al. Thoracolumbar fracture with
listhesis—an uncommon manifestation of child abuse. Pediatr Radiol
2003;33(5):305-310.
HL, Thomas BH, Jamieson E, et al. Effectiveness of home visitation by
public-health nurses in prevention of the recurrence of child physical
abuse and neglect: a randomised controlled trial. Lancet
2005;365(9473):1786-1793.
S, Mann MK, John N, Ellaway B, et al. Does cardiopulmonary
resuscitation cause rib fractures in children? A systematic review.
Child Abuse Negl 2006;30(7): 739-751.
S, Mann MK, Sibert J, et al. Are there patterns of bruising in
childhood which are diagnostic or suggestive of abuse? A systematic
review. Arch Dis Child 2005;90(2): 182-186.
A, Pepin MG, Byers PH. Testing for osteogenesis imperfecta in cases of
suspected nonaccidental injury. J Med Genet 2002;39(6):382-386.
JL, Clark MA, Sandusky GE. Undiagnosed, untreated acute lymphoblastic
leukemia presenting as suspected child abuse. J Forensic Sci
1990;35(3):735-739.
J, Hanson R, Grigor W, et al. Lung injury resulting from a
nonaccidental crush injury to the chest. Pediatr Emerg Care
1991;7(3):166-168.
P, Grossman W, Gaffney M, et al. Soft-tissue injury as an indication of
child abuse. J Bone Joint Surg Am 1995;77(8):1179-1183.
DF, Carpenter BL. Radiologic imaging of inflicted injury in the child
abuse syndrome. Pediatr Clin North Am 1990;37(4):815-837.
JM, Bishop SJ, Jellinek MS, et al. What happens after the care and
protection petition? Reabuse in a court sample. Child Abuse Negl
1992;16(4):485-493.
Association of Children’s Hospital and Related Institutions. Defining
the Children’s Hospital Role in Child Maltreatment. Alexandria, VA:
Author; 2006.
RS, Jalili M, Kolls BJ, et al. Factor XIII deficiency mistaken for
battered child syndrome: case of “correct” test ordering negated by a
commonly accepted qualitative test with limited negative predictive
value. Am J Hematol 2002;71(4):328-330.
AW, Vandeven AM. Unexplained infant and child death: a review of sudden
infant death syndrome, sudden unexplained infant death, and child
maltreatment fatalities including shaken baby syndrome. Curr Opin
Pediatr 2006;18(2):196-200.
GR II, Corey TS, Davis GJ. Nonfracture-associated fatal fat embolism in
a case of child abuse. J Forensic Sci 1990;35(2):493-499.
K, Spevak MR, Kleinman PK. Fractures of the hands and feet in child
abuse: imaging and pathologic features. Radiology 1997;203(1):233-236.
M, Meissner C, Saternus KS. Fall or shaken: traumatic brain injury in
children caused by falls or abuse at home—a review on biomechanics and
diagnosis. Neuropediatrics 2005;36(4):240-245.
K, Matsumoto H, Hayase T, et al. An autopsy case of osteogenesis
imperfecta initially suspected as child abuse. Forensic Sci Int
1994;65(2):97-104.
JE. Intergenerational transmission of child abuse: rates, research, and
clinical implications. Am J Psychiatry 1993;150(9):1315-1324.
R, Rahhal R, Elshershari H, et al. Intentional avulsion fracture of the
second cervical vertebra in a hypotonic child. Pediatr Emerg Care
2006;22(5):352-354.
LK, Marks SC Jr, Kleinman PK. Metaphyseal extensions of hypertrophied
chondrocytes in abused infants indicate healing fractures. J Pediatr
Orthop 1993;13(2): 249-254.
VJ, Hicks RA, Vandervort FE. “You are hereby commanded to appear”:
pediatrician subpoena and court appearance in child maltreatment.
Pediatrics 2001;107(6): 1427-1430.
PM, Ceulemans B, Laridon A, et al. Cortical hypoxic-ischemic brain
damage in shaken-baby (shaken impact) syndrome: value of
diffusion-weighted MRI. Pediatr Radiol 2003;33(12):868-871.
CR, Burns J, McAllion SJ. Osteogenesis imperfecta: the distinction from
child abuse and the recognition of a variant form. Am J Med Genet
1993;45(2):187-192.
J, Losek JD. Child physical abuse and rhabdomyolysis: case report and
literature review. Pediatr Emerg Care 2007;23(7):474-477.
MC, Bertocci GE, Janosky JE, et al. Femur fractures resulting from
stair falls among children: an injury plausibility model. Pediatrics
2005;115(6):1712-1722.
MC, Bertocci GE, Vogeley E, et al. Evaluating long bone fractures in
children: a biomechanical approach with illustrative cases. Child Abuse
Negl 2004;28(5): 505-524.
CT, Holton J. The total estimated cost of child abuse and neglect in
the United States. Chicago: Prevent Child Abuse America. Available at:
http://member.preventchildabuse.org/site/DocServer/cost_analysis.pdf?docID=144.
Accessed August 25, 2009.
I, Maguire S, Harrison SK, et al. How old is this fracture? Radiologic
dating of fractures in children: a systematic review. AJR Am J
Roentgenol 2005;184(4): 1282-1286.
D, Barbor, P. Unusual Injury? Recent injury in normal children and
children with suspected nonaccidental trauma. Br Med J (Clin Res Ed)
1982;285:1399-1401.
DM, Christian CW, Bilaniuk LT, et al. Occult head injury in high-risk
abused children. Pediatrics 2003;111(6 Pt 1):1382-1386.
H, Brandt JD, Rosas AJ, et al. Findings in older children with abusive
head injury: does shaken-child syndrome exist? Pediatrics
2006;117(5):e1039-1044.
P. Child deaths resulting from inflected injuries: household risk
factors and perpetrator characteristics. Pediatrics 2005;116:687-693.
AJ, Ricci LR. How accurately can bruises be aged in abused children?
Literature review and synthesis. Pediatrics 1996;97(2):254-257.
RM, Werth C, Johnston A. Femur shaft fractures in toddlers and young
children: rarely from child abuse. J Pediatr Orthop 2000;20(4):475-481.
BA, Murphy KM, Shaw A, et al. Humerus shaft fractures in young
children: accident or abuse? J Pediatr Orthop 1997;17(3):293-297.
Y. Osteogenesis imperfecta. Review of the literature with presentation
of 29 cases. Am J Dis Child 1975;129(6):679-687.
CD, Graves P, Maloney K, et al. Mortality from intentional and
unintentional injury among infants of young mothers in Colorado, 1986
to 1992. Arch Pediatr Adolesc Med 1996;150(10):1077-1083.
JP, Sarwark JF. Thoracolumbar fracture-dislocation in child abuse: case
report, closed reduction technique and review of the literature.
Pediatr Neurosurg 2008; 44(3):253-257.
D, Butler B, Latham M, et al. Natural history of blue sclerae in
osteogenesis imperfecta. Am J Med Genet 1993;45(2):183-186.
FN. The roentgen manifestations of unrecognized skeletal trauma in
infants. Am J Roentgenol Radium Ther Nucl Med 1953;69(3):413-427.
AJ, Robben SG, Meradji M. Sonographically detected costo-chondral
dislocation in an abused child. A new sonographic sign to the
radiological spectrum of child abuse. Pediatr Radiol 1990;20(7):566-567.
FW, Gilday DL, Ash JM, et al. Unsuspected costo-vertebral fractures
demonstrated by bone scanning in the child abuse syndrome. Pediatr
Radiol 1980;10(2): 103-106.
K, Pfalzgraf R. Inadvertent clavicular fractures caused by
“chiropractic” manipulations in an infant: an unusual form of
pseudoabuse. J Forensic Sci 1990;35(5): 1211-1216.
SP, Patel S, Burke BL, et al. Analysis of perpetrator admissions to
inflicted traumatic brain injury in children. Arch Pediatr Adolesc Med
2004;158(5):454-458.
SP, Sirotnak AP, Heisler KW, et al. Inflicted skeletal trauma: the
relationship of perpetrators to their victims. Child Abuse Negl
2007;31(9):993-999.
RD, Pepin M, Byers PH. Studies of collagen synthesis and structure in
the differentiation of child abuse from osteogenesis imperfecta. J
Pediatr 1996;128(4): 542-547.
J Jr. Beyond Munchausen syndrome by proxy: identification and treatment
of child abuse in a medical setting. Pediatrics 2007;119(5):1026-1030.
J Jr, Amaya-Jackson L. Understanding the behavioral and emotional
consequences of child abuse. Pediatrics 2008;122(3):667-673.
JR, Starshak RJ. The role of bone scintigraphy in the evaluation of the
suspected abused child. Radiology 1983;146(2):369-375.
NF, Taylor JA, Feldman KW. Bruises in infants and toddlers: those who
don’t cruise rarely bruise. Puget Sound Pediatric Research Network.
Arch Pediatr Adolesc Med 1999;153(4):399-403.
DY, Davis PC, Hopkins KL, et al. Nonaccidental pediatric head injury:
diffusion-weighted imaging findings. Neurosurgery 2001;49(2):309-318;
discussion 318-320.
PM, Brookhouser PE, Scanlan JM, et al. Patterns of physical and sexual
abuse of communicatively handicapped children. Ann Otol Rhinol Laryngol
1991;100(3): 188-194.
JR, England D, Siebert CF Jr. Hepatic glycogen staining. Applications
in injury survival time and child abuse. Am J Forensic Med Pathol
2001;22(3):313-318.
NH, Robinson L, Evans A, et al. The floppy infant: a new manifestation
of nonaccidental injury. Pediatr Neurosurg 1995;23(4):188-191.
SA, Rosenfield NS, Leventhal JM, et al. Long-bone fractures in young
children: distinguishing accidental injuries from child abuse.
Pediatrics 1991;88(3):471-476.
M, DiScala C, Terrin NC, et al. Blunt abdominal injury in the young
pediatric patient: child abuse and patient outcomes. Child Maltreat
2004;9(1):111-117.
M, Discala C, Terrin NC, et al. Patient and injury characteristics in
abusive abdominal injuries. Pediatr Emerg Care 2006;22(10):700-704.
M, Waddimba A, Griffith J, et al. Variation in the diagnosis of child
abuse in severely injured infants. Pediatrics 2006;117(3):722-728.
Department of Health and Human Services. The Child Abuse Prevention and
Treatment Act (CAPTA). Washington, DC: Author; 2003.
M, James LS, Catz C. Defining the sudden infant death syndrome (SIDS):
deliberations of an expert panel convened by the National Institute of
Child Health and Human Development. Pediatr Pathol 1991;11(5):677-684.
J, Dreby J. Fatalities and the organization of child care in the United
States, 1985-2003. Am Sociol Rev 2005;70:729-757.
T, Levin AV, Shafiq A, et al. Postmortem orbital findings in shaken
baby syndrome. Am J Ophthalmol 2006;142(2):233-240.
DC, Don S, Hildebolt C, et al. Skeletal surveys for child abuse:
comparison of interpretation using digitized images and screen-film
radiographs. AJR Am J Roentgenol 1998;171(5):1415-1419.
S, Makoroff K, Care M, et al. Utility of follow-up skeletal surveys in
suspected child physical abuse evaluations. Child Abuse Negl
2005;29(10):1075-1083.
SJ. Unplanned childbearing and family size: their relationship to child
neglect and abuse. Fam Plann Perspect 1991;23(4):155-161.
JF, Cohen J. Dating fractures. In: Kleinman PK, ed. Diagnostic Imaging
of Child Abuse. Baltimore: Williams & Wilkins; 1987:168-177.
