Elbow and Forearm Injuries
-
Location.
Rupture of the distal biceps may occur at the muscle tendon junction or
more commonly at its tendinous insertion into the radial tuberosity. -
Mechanism of injury.
Often a chronic case of distal biceps tendinitis has been present,
making the tendon susceptible to failure with forceful supination of
the hand or elbow flexion. -
Examination.
A palpable defect is present at the elbow and the bulk of the biceps
muscle is retracted proximally. Often, this shortened muscle is prone
to spasm for several weeks after the injury occurs. The patient has
minimal weakness to elbow flexion but does have weakness to hand
supination. -
Treatment. If
the rupture occurs at the muscle tendon junction, nonoperative care
with early range-of-motion (ROM) exercises are indicated (1).
Treatment of distal tendon tears is controversial. The biceps functions
as a weak elbow flexor, but it is a strong supinator of the hand.
Individuals who do not like the cosmetic deformity or are involved in
activities that require supination strength should undergo operative
repair. A single curvilinear incision is made that allows exposure to
locate the retracted tendon proximally, and the original biceps tunnel
to the radial tuberosity is used. A repair of the tendon to the
tuberosity with suture anchors is completed. A sling is used for 4
weeks postoperatively with an active assisted ROM program initiated
immediately postoperatively.
-
The mechanism of injury is usually a fall on an hyperextended arm.
-
The history
of an elbow injury must document, if possible, the mechanism of injury;
type and location of pain; amount of immediate sensory, motor, and
circulatory dysfunction; treatment before examination; time when
swelling began; and any history of elbow injuries. -
The examination
of an injured elbow must document, if possible, the degree of effusion,
location of any ecchymosis, ROM, and stability of the joint when
compared with that of the opposite side. In the examination of an
injured elbow, there may be confusion about whether the deformity
arises from a dislocation of the elbow or from a supracondylar
fracture, but this can be resolved clinically by comparing the relative
positions of the two epicondyles and the tip of the olecranon by
palpation. These three bony points form an
isosceles triangle. The two sides remain equal in length in a
supracondylar fracture. If the elbow is dislocated, however, the two
sides become unequal (Fig. 18-1).
The position of the proximal radius should also be palpated on the
lateral surface of the elbow to rule out a radial head dislocation. The
function of the peripheral nerves and the state of the circulation to
the hand, including capillary refill and presence of radial pulse,
should be carefully noted. The anterior interosseous branch of the
median nerve and the radial nerve are most frequently involved. -
Roentgenograms
demonstrate whether the displacement is directly posterior (most
common), posterolateral, or posteromedial. Roentgenograms should
include a lateral view of the elbow, an anteroposterior view of the
humerus, and an anteroposterior view of the forearm. Fractures of the
coranoid process have been identified in 10% to 15% of elbow
dislocations.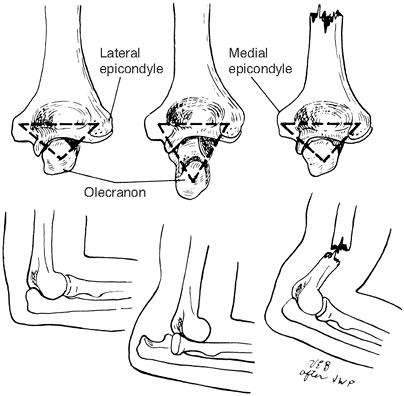 Figure 18-1.
Figure 18-1.
The two epicondyles and the tip of the olecranon form an isosceles
triangle. This triangle is maintained with a supracondylar humeral
fracture, but with an elbow dislocation, the two sides of the triangle
become unequal or distorted. -
Treatment
consists of immediate closed reduction, which is essential, and may
require anesthesia for proper muscle relaxation. Reduction can usually
be achieved by gentle traction on the slightly flexed elbow, applying
countertraction to the humeral shaft. After reduction, motion should be
nearly full, and medial and lateral stability should be assessed. With
a simple posterior elbow dislocation, a portion of the collateral
ligaments are generally intact so the joint is fairly stable and early
motion may be instituted after 3 to 5 days of splinting (2).
With other dislocations, the collateral ligaments may be completely
disrupted, creating an unstable joint and necessitating longer
immobilization before active exercises are started. Postreduction
roentgenograms are mandatory because they, too, help determine
postreduction treatment. If the joint space is not congruent, generally
cartilage fragments, bony debris, or ligament is in the joint, and open
reduction and collateral ligament repair are indicated. If significant
articular fragments are displaced, they should be internally fixed with
recessed small or “minifragment” implants at the same time. Coranoid
fractures, unless involving more than 50% of the length, do not require
internal fixation (3). If the elbow is stable
after collateral ligament repair, motion should be initiated as with
stable reductions treated in a closed manner. For an unstable elbow,
following operative repair external fixators, which allow active ROM,
are useful (4). -
Postreduction treatment
-
If the medial and lateral ligaments are intact and are providing a stable elbow joint,
the elbow is placed in a padded posterior splint in 90 degrees of
flexion that extends far enough to support the wrist. The elbow is kept
elevated above the heart until the swelling recedes. Active flexion is
begun in 3 to 5 days to achieve as much ROM as possible. Passive ROM is
contraindicated. Repeat radiographs should be obtained within 3 to 5
days to make certain the
P.253
joint
remains congruent. The elbow is kept in the posterior splint when not
being exercised. As soon as the patient can achieve near full
extension, use of the splint may be discontinued. -
If the elbow is unstable
and the joint is congruent on roentgenograms, it is splinted in 90
degrees of flexion for 2 to 3 weeks with initial elevation to help
control swelling. Radiographs must be obtained in the splint initially
and at 3 to 5 days to ensure that the elbow is congruous. An active
exercise program is then begun to regain ROM. Open reduction is
generally not necessary; there is no documented advantage to open
reduction over closed reduction (2,5,6).
-
-
Complications
-
Up to 15 degrees limitation of full extension as well as some limitation of flexion is common unless an intensive rehabilitation program is instituted.
-
Traumatic peripheral nerve injuries may occur: Ulnar, median, combined ulnar and median, and brachial plexus injury have all been reported.
-
Compromise of circulation can occur as a result of posttraumatic swelling or injury to the brachial artery. See Chap. 2, III, for a discussion of compartmental syndromes.
-
Myositis ossificans can develop, and its treatment should follow the guidelines in Chap. 2, V. Posttraumatic elbow stiffness can be successfully treated by open release (7).
If associated with postresection instability, a hinged external fixator
distractor can be used with good results in motivated patients (8). -
Chronic instability can be difficult to diagnose; when recognized, surgical reconstruction is generally successful (6).
-
-
Fractures of the olecranon may be divided into four groups:
-
Transverse and undisplaced
-
Transverse and displaced
-
Comminuted and minimally displaced with clinical findings suggesting an intact triceps aponeurosis
-
Comminuted and displaced, indicating a disrupted extensor mechanism
-
-
Treatment
-
Undisplaced fractures should be treated
in a posterior splint with the elbow flexed 90 degrees. Pronation and
supination movements are started in 2 to 3 days, and flexion-extension
movements are started at 2 weeks. Protective splinting or a sling is
used until there is evidence of union (usually approximately 6 weeks).
Closed clinical and roentgenographic follow-up is essential to ensure
full ROM and to identify any displacement. -
Displaced fractures should be reduced
anatomically and fixed internally with tension band wiring technique or
by tension band plating via a posterior approach. An olecranon lag
screw should not be used without tension band wire. If used alone, the
screw does not provide maximum stabilization when the elbow flexes
because half of the fracture is placed in compression and the other
half is placed in tension, as shown in Fig. 10-9. Regardless of the type of internal fixation used, motion should be started within the first few days postoperatively.-
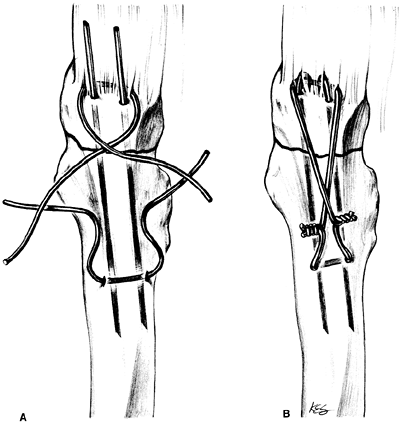
The tension band wiring technique for a transverse displaced fracture
of the olecranon begins with reduction without devitalization of the
fragments. Stabilization of the fragments is accomplished by two
Kirschner wires introduced parallel to each other and to the anterior
cortex of the ulna. Place the drill hole just distal to the fracture,
transversely through the posterior cortex of the ulna. Thread the
1.2-mm (or 16 to 18 gauge) wire through the drill hole, cross the ends
in a figure-8 style, pass the wire around the protruding ends of the
Kirschner wires, and tie the wire under tension, providing two twists,
one on each side of the ulna. This makes the tension even across the
fracture site. The result should be a figure-8 tension band wire with
the crossover point lying over the fracture. Finally, shorten the
projecting ends of the Kirschner wires and bend them to form U-shaped
hooks that are then impacted gently into the bone over the tension wire
(Fig. 18-2) and
P.254
reconstruct the triceps incision over the bent wires. Similar results
can be obtained by inserting a 6.5-mm cancellous screw (with or without
a large washer) across the fracture and using the same figure-8
technique.![]() Figure 18-2.
Figure 18-2.
The tension band wiring technique. Two parallel Kirschner wires cross
an olecranon fracture at right angles. One strand of 18-gauge wire has
been inserted within the triceps tendon anterior to the Kirschner
wires. The second wire is inserted through the dorsal ulnar cortex of
the ulna (A). The fixation is secured (B). (JB Lippincott From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven Press, 1993:112, with permission). -
The tension-band wiring technique for comminuted displaced fractures
of the olecranon is much the same except that an anatomic reduction is
more difficult to achieve and small Kirschner wires may be required for
stabilization of minor fracture fragments.
-
-
-
Mechanism of injury. These pediatric injuries occur from a fall on the outstretched hand.
-
Examination.
Pain, occasionally swelling, and tenderness are usually present over
the upper end of the radius. There is also limitation of motion. -
Treatment
-
Fractures with less than 15 degrees of angulation are immobilized in a long-arm splint for 2 weeks. Active exercise is then initiated while the arm is protected in a sling.
-
Angulation of greater then 15 degrees
calls for manipulation under anesthesia. If this fails, operative
reduction is required. After reduction, the fracture is usually stable.
If not, internal fixation is used with a fine, smooth Kirschner wire
introduced from distal to proximal, stopping short of the articular
surface of the radial head. The pin can be removed at 3 weeks and
active motion initiated. The radial head should never be removed in
children.
P.255 -
-
Mechanism of injury.
This injury should be suspected following a fall on the outstretched
hand whenever there is swelling of the elbow joint, tenderness over the
head of the radius, and limitation of elbow function (especially
painful pronation and supination). -
Roentgenograms.
If the fracture is not apparent on the anteroposterior and lateral
roentgenograms, films obtained with the head of the radius in varying
degrees of rotation are helpful. An anterior fat pad sign, indicative
of an elbow effusion, should alert the treating physician to order
these special roentgenograms. -
Treatment
-
Minimally displaced (less than 1 mm) fractures of the head (Mason 1) or impacted fractures of the radial neck
are treated with a posterior splint with active motion exercises
beginning in the first 3 to 5 days. This treatment is followed by the
wearing of a sling and active movement of the elbow. Acutely, it is
helpful to aspirate the elbow effusion and inject 5 mL of 1% lidocaine
to be sure that elbow motion is full and unimpeded. -
Displaced fractures involving less than
one third of the articular surface (Mason 2) are treated by early
motion if the postaspiration and lidocaine injection examination
reveals a full ROM. If motion is blocked or if there is an associated
elbow fracture or dislocation, the fracture is treated by open
reduction with minimal fragment screws and early motion (9,10). The radial head should not be excised. -
Comminuted or displaced fractures of the
head that involve more than one third of the articular surface and
displaced or unstable fractures of the neck are treated by early
excision of the radial head with or without placement of a metal
prosthesis if it is anticipated that after 4 to 5 days pain will
restrict active exercises (5,11).
If adequate movement can be achieved before the fifth day after injury,
excision may be avoided. The end result of excision of the radial head
is good, but a normal elbow motion is generally not achieved. Fifty
percent of the patients have a late complication of subluxation and
pain at the distal radioulnar joint (12,13).
Insertion of a Silastic prosthesis to prevent late complication appears
warranted, but complications from the prosthesis itself are not
uncommon (synovitis, prosthesis fracture); therefore, the authors
recommend a metal prosthesis when indicated (11).
-
-
This is a dislocation of the radial head and a fracture of the proximal ulna. There are four types, as described by Bado (see Selected Historical Readings), depending on the direction of radial head dislocation and associated radial fracture.
-
The mechanism of injury
may be a “failed” posterior dislocation of the elbow, that is, the ulna
fractures instead of dislocating because of an axial loading force.
Alternatively, the injury may occur as a result of an anteriorly or
posteriorly directed blow. -
Treatment
-
Children.
Closed reduction of the ulna is carried out. If the radial head has not
been indirectly reduced by realigning the ulna, reduction of the radial
head is attempted by supination of the forearm and direct pressure on
the radial head, which usually is successful. When the radial head
cannot be anatomically reduced, removal of the interposing joint
capsule with repair of the anular ligament is advisable. -
Adults. Operative treatment is recommended (14,15,16).
Open reduction with compression plate fixation of the ulna is generally
followed by indirect reduction of the radius. If reduction of the
radius is not obtained, an open reduction
P.256
must
be done. If the radial head is unstable, cast for approximately 6 weeks
in supination, then start active exercises. If the radial head is
stable after closed reduction or open repair, start early active motion
with a hinged elbow orthosis, maintaining the forearm in supination.
Protect the arm until the fracture is healed. With anterior dislocation
and an unstable closed reduction, the arm may be immobilized in 100
degrees to 110 degrees of elbow flexion, which relaxes the biceps and
helps maintain reduction of the radial head. If the radial head remains
subluxed after ulnar fixation, the forearm should be supinated while
applying pressure over the radial head.
-
-
Roentgenograms.
Of all fractures, this type best exemplifies the need for visualizing
the joint above and below fractures of long bones (elbow and wrist). -
Treatment
-
Children. The
fractures are usually of the greenstick type, and even with
considerable displacement, a dense periosteal sleeve ordinarily
remains. This sleeve is usually sufficient to make satisfactory closed
reduction possible. Greenstick fractures tend to redisplace unless the
fracture is overreduced, that is, unless the opposite cortex has been
fractured with the reduction. For the closed reduction in which
angulation is the only deformity to be corrected, conscious sedation
and hematoma block may be adequate. Where there is total displacement
with shortening of either of both bones, a brief general anesthetic
enhances a traumatic reduction. In the child, operative treatment is
generally unnecessary because remodeling with growth is excellent and
there is an increased likelihood that cross-union will develop after
operative treatment. In the mature adolescent, failure to obtain a
satisfactory closed reduction is an indication for open reduction and
treatment as for the adult. Bone grafting of operatively reduced
fractures in the adolescent is not necessary. -
Adults. (16,17,20,21,22)
-
Principles.
It is difficult to achieve a satisfactory closed reduction of displaced
fractures of the forearm bones, and, if achieved, it is hard to
maintain. Unsatisfactory results of closed treatment have been reported
to range from 38% to 74% (19). For this reason, open reduction with internal fixation is routine except in cases of undisplaced fractures. -
Undisplaced single bone fractures should be treated in a long-arm cast until there is roentgenographic evidence of union or definitive evidence or delayed union.
-
Fractures of both bones or a displaced isolated fracture
of the radius or ulna should be treated by open reduction, plate
fixation, and cancellous bone grafting whenever there is bone loss.
Bone grafting should not be performed routinely (21,22).
This treatment is carried out as a semielective procedure as soon as
the patient’s condition warrants; reduction is easiest when the
fracture is treated within the first 48 hours. At a minimum, there must
be screws engaging six cortices above and below the fracture site.
Great care must be exercised to restore the length and curvature of the
radius relative to the ulna to prevent loss of pronation and supination
(19,20). The use of a 3.5-mm plate system has nearly eliminated the problem of refracture after plate removal (16,24).
Previously, this problem was thought to be related to
“stress-protection” of the underlying cortical bone but is now
understood to be related to cortical bone ischemia (16).
Plates should not be routinely removed from healed adult diaphyseal
forearm fractures. Eight-hole plates are used most often. If bone
grafting is indicated because of significant bone loss, the graft
should be taken without disturbing either table of iliac bone or its
muscle attachments, as described in Chap. 10, II.K;
postoperatively, morbidity from the graft site is minimized. Reliable
patients may be placed in a removable splint and early motion started
as soon as wound healing is complete.
-
-
-
Description.
This fracture is at the junction of the middle and distal third of the
radius and is combined with a subluxation of the distal radioulnar
joint (said to represent approximately 5% of forearm fractures). -
Treatment.
The treatment of choice is the same as for an isolated displaced
fracture of the radius with forearm immobilization in supination for 6
weeks. The radius is fixed anatomically with a volar approach and plate
fixation as for bone forearm fractures. If the distal radioulnar joint
remains stable in supination as documented radiographically, a long-arm
splint is applied to this position. In a reliable patient, elbow motion
can be started with the forearm in supination using a hinged orthoses
or Munster cast as soon as wound healing is confirmed. Occasionally, an
open reduction of the distal radioulnar joint is necessary because of
inability to reduce the joint. If the reduction is unstable, fixation
with two Kirschner wires from the ulna to the radius is advisable; the
wires are removed in 4 weeks. The Kirschner wire should be a minimum
size of .062 in. or larger to avoid breaking. The distal radioulnar
joint must be confirmed to be reduced by roentgenograms during the
immobilization period.
-
Mechanism.
This fracture frequently occurs as the result of a blow across the
subcutaneous surface of the bone, thus the term “nightstick fracture.” -
Treatment. If
the fracture is displaced and not associated with radial head
subluxation, it can be well treated conservatively. Functional bracing
or treatment with casting yields 95% to 98% union rates with good
fixation (26,27,28).
-
This extraarticular fracture of the
distal radius was first described by Abraham Colles in 1814. In this
important paper, he differentiated this injury from the rare
dislocation of the wrist on clinical grounds without the aid of
roentgenograms. -
Examination. The wrist and hand are displaced dorsally in relation to the shaft of the radius (Fig. 18-3) to form the classic silver-fork deformity. Tenderness is found over the distal radius and over the ulnar styloid.
-
Roentgenograms. Anteroposterior and lateral films are essential and often show the following:
-
Comminution of the dorsal cortex
-
The following displacements, in varying degrees, of the distal fragments:
-
Dorsal displacement
-
Dorsal angulation
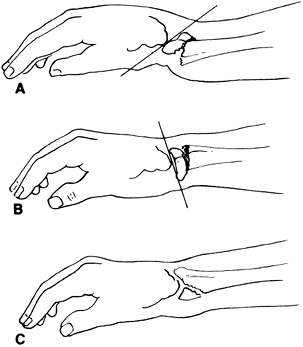 Figure 18-3. A: Colles’ fracture. B: Smith fracture (reversed Colles’ fracture). C: Barton fracture (causes displacement of the anterior portion of the articular surface).
Figure 18-3. A: Colles’ fracture. B: Smith fracture (reversed Colles’ fracture). C: Barton fracture (causes displacement of the anterior portion of the articular surface). -
Proximal displacement
-
Radial displacement
-
Articular extension. If the articular fractures are displaced, treatment is different.
P.258 -
-
-
Treatment
must be directed as vigorously toward maintaining hand, elbow, and
shoulder function as toward obtaining an acceptable cosmetic result.-
The radiocarpal joint normally faces palmarward
anywhere from 0 degrees to 18 degrees, so any amount of dorsal
angulation is usually unacceptable, and better alignment should be
attempted. Reduction of extraarticular fractures that are angulated
palmarward between 1 degrees and 15 degrees depends on the age of the
patient and the activity level desired; ordinarily, no reduction is
necessary. If the palmar tilt is between 10 degrees and 20 degrees, the
fracture should be immobilized with no attempt at reduction. The normal
radial deviation of the radiocarpal joint ranges from 16 degrees to 28
degrees. -
Reduction of
this fracture usually is easy to achieve but difficult to maintain. It
may be performed under a hematoma block, a Bier block (intravenous
regional anesthetic), or an axillary block. Reducing the deformities
that have been described previously involves the following steps:-
Fingertrap traction with a 10-lb weight
hung from a strap across the arm is used, and the elbow is flexed 90
degrees in the line of the forearm to disimpact the fracture. Manual traction is an equally effective alternative. -
While traction is maintained, pressure is
applied to the dorsal aspect of the distal fragment and to the palmar
aspect of the proximal fragment to correct dorsal displacement and rotation. -
Pressure is applied on the radial aspect of the distal fragment to correct radial deviation.
-
-
The following are useful clinical tests of reduction:
-
Palpation of
the normal wrist shows that the radial styloid lies 1 cm distal to the
ulnar styloid, and this relationship should be restored on the injured
side. -
There should be no tendency toward recurrence of the deformity;
that is, when one holds the elbow with the forearm parallel to the
ground, the wrist contour appears normal. This may be difficult to
assess with severe swelling.
-
-
Methods of immobilization
-
The wrist usually is immobilized
with the hand in ulnar deviation, the wrist neutral to no more than 15
degrees of volar flexion, and the anterior splints or single posterior
splint extending over the first and second metacarpals to maintain the
full ulnar deviation. Splints should be placed over a single layer of
Webril applied with an adherent. Splints are wrapped in place by
bias-cut stockinet or by an elastic bandage. Because of the potential
for swelling, a circular cast is not advisable as initial treatment.
The splints may be incorporated into a circular cast after all
adjustments for swelling have been made. It is essential to allow full
(90-degree) flexion of all metacarpophalangeal joints. -
Short-arm versus long-arm casting.
If the surgeon wishes to maintain an accurate reduction, the elbow
joint should be immobilized. A forearm splint-cast is appropriate,
however, in the following situations:-
When the individual is debilitated or elderly
-
When an incomplete reduction is to be accepted
-
When no reduction is attempted, and the impacted position of the fragments is accepted
-
-
In the younger individual with a severely comminuted and displaced extraarticular fracture, consider external skeletal fixation through the radius and the second metacarpal to maintain proper position and length (21).
Immobilization in the fixator for at least 6 weeks is usually
necessary, followed by mobilization of the wrist. In the older patient
with badly comminuted fractures, early excision of the distal ulna and
acceptance of radial
P.259
shortening may also be considered (29). See Chap. 10, II.J, for a discussion of external skeletal fixation. -
The presence of intraarticular extension
changes the treatment paradigm in all but the most debilitated
patients. A displacement of more than 3 to 4 mm mandates an attempt at
closed reduction. Displacement of more than 2 mm warrants reduction in
an adult because of the association of residual displacement with
degenerative joint disease of the radiocarpal joint (30).
Closed reduction of articular displacement is rarely successful.
Therefore, an open reduction through a dorsal approach; Kirschner wire
fixation; bone graft for the dorsal defect; and pins, external
fixation, or small fragment plates for neutralization are generally
recommended. There has been increased interest in open reduction in the
internal fixation over the last decade to improve functional outcomes
of these fractures in adults younger than 65 to 70 years of age where
functional decrease is high (18,31).
-
-
-
Aftercare
-
Frequent active movements of the fingers and elevation of the hand are both essential to reduce swelling and relieve pain. Full movement of the shoulder joint also must be maintained.
-
Within 1 week of treatment, the following criteria should be met:
-
There is full, active movement of the fingers and the shoulder.
-
Pain is minimal and readily controlled with minimal analgesics.
-
The immobilization is satisfactory and comfortable.
-
-
Follow-up roentgenograms obtained through the splint should be obtained:
-
After reduction
-
On the third day or when the swelling subsides
-
After 10 to 14 days
-
At 6 and 12 weeks after injury
-
-
Duration of immobilization.
If the fracture is unreduced, it should be immobilized for 4 to 6
weeks. If the fracture is reduced, it should be immobilized for 6 to 8
weeks. Diminishing of tenderness over the site of fracture is evidence
of progressive union. The wearing of a removable dorsal splint for
several weeks after cast removal can improve patient comfort while
allowing mobilization of the extremity.
-
-
Complications
-
The most frequent complication is stiffness of the finger joints and shoulder.
-
Pain with finger movement or numbness in the radial three digits often can signify a carpal tunnel syndrome.
The pain usually is associated with complaints or abnormal neurologic
findings in the median nerve distribution. If the abnormal findings
persist for 3 days or increase in severity over 4 to 12 weeks, the
carpal tunnel should be surgically released. If the patient has severe
median nerve deficit, carpal tunnel release should be part of the
initial management, which generally involves percutaneous pinning,
external fixation, or open reduction. -
Pain over the distal radioulnar joint
on supination of the forearm is a common complaint when immobilization
is discontinued. The symptoms usually disappear within 6 months. Warn
the patient of this problem in advance; if symptoms persist after full
mobilization of the hand, excision of the distal ulna should be
considered. -
Some recurrence of deformity
is common. It is rare for the fractured wrist to have the same
appearance as a normal wrist. Give the patient advance warning about
this discrepancy and stress the desirability of good function rather
than cosmesis. -
If rupture by attrition of the extensor pollicis longus
is diagnosed, early repair is indicated. This may occur even with
nondisplaced fractures. This is thought to be due to damage to the
blood supply to the paratenon.
-
-
Description. These fractures are often referred to incorrectly as Colles’ fractures because the deformity of the wrist is similar.
-
Roentgenograms.
Roentgenographic examination is diagnostic. Be certain that the
fracture is not one of the types of epiphyseal slips described below in
XIII. -
Treatment.
When completely displaced, these fractures can be difficult to reduce.
Manipulation should be done with the patient anesthetized or under
conscious sedation, and the rule “one doctor, one manipulation”
applies. Direct traction alone is rarely successful and should not be
attempted, especially without complete patient relaxation under an
anesthetic.-
Manipulative reduction consists of either
-
Traction in line with the deformity until the bone ends can be “locked on,” followed by correction of the deformity.
-
Increasing the angulation of the distal fragments by manipulation (re-creating the deformity)
until the bone ends can be “locked on,” followed by alignment of the
distal fragment to the proximal fragment to correct the deformity.
-
-
If reduction can be achieved,
it is usually stable, and treatment then consists of immobilization as
for a Colles’ fracture in a long-arm splint with the elbow at 90
degrees. -
The fracture infrequently requires open reduction.
-
-
Smith fracture
is a fracture of the distal radius with the distal fragment and
accompanying carpal row displaced volarly (reversed Colles’ fracture; Fig. 18-3B).
The articular surface of the radius is not involved. This injury is
usually secondary to a blow on the dorsum of the wrist or distal radius
with the forearm in pronation.-
Treatment may
initially consist of a closed reduction under anesthesia. Longitudinal
treatment is applied in a line with the deformity (pronation and
flexion) until the fragments are distracted. Supination and pushing
dorsally on the distal fragment reduce the fracture. The fracture
should be immobilized with the forearm positioned in supination and the
wrist in extension. These fractures are highly unstable and the patient
should be informed that this may occur and that open reduction with
pins or small fragment plates is generally necessary. -
Postmanipulative care is the same as for a Colles’ fracture.
-
-
Barton fracture is a fracture-dislocation in that the triangular fragment of the volar surface of the distal radius is sheared off (Fig. 18-3C). This fragment along with the carpus is displaced volarly and proximally.
-
The mechanism of injury is usually forced pronation under the axial load.
-
Treatment of
this fracture by closed methods is difficult. Unless there is
significant comminution, open reduction and fixation with a volar
buttress plate is recommended.
-
-
The usual mechanism of injury
is a fall on the outstretched hand with a forced rotation of the wrist
into dorsiflexion, resulting in dorsal displacement of the distal
radius through the epiphyseal plate. -
This fracture follows the rule of epiphyseal injuries (see Chap. 1, VIII.B). It is usually a Salter class 1 or 2 fracture of the epiphysis; hence, growth arrests may occur. The parents of an injured child must be gently acquainted with this fact.
-
Good-quality roentgenograms are essential in determining the type of epiphyseal separation.
-
Treatment.
The younger the child, the more angulation and displacement can be
accepted with assurance of normal subsequent function and cosmesis. In
a child of any age, angulation exceeding 25 degrees or displacement exceeding 25% of the radial height should be reduced.
A less-than-automatic reduction is preferable to repeated
manipulations. The reduction is accomplished after adequate anesthesia
to ensure complete muscle relaxation. Traction is applied in the line
of deformity. The manipulation and postreduction treatment are the same
as for a Colles’ fracture. The patient should be immobilized in a
long-arm cast for 3 to 4 weeks, followed by a short-arm cast for 2 to 4
weeks. Parents should be reassured that remodeling of the plate and
joint motion will occur.
sedation in the emergency department longitudinal traction with the
elbow slightly flexed postreduction stability examination and
radiographs are essential for planning. If the elbow has good
stability, start ROM exercises at 7 to 10 days.
Unstable elbow after reduction, intraarticular fragments, associated
fractures, especially of the coronoid process or radial head/neck.
Repair of the collateral ligaments, joint irrigation, fixation of
sassociated fractures, particularly coronoid fractures of any
significant size. Splint for 7 to 10 days and then start active
range-of-motion (AROM) exercises.
Displacement of fracture of more than 2 mm or any persistent
angulation, especially when associated with radial head dislocation.
Posterior approach, ORIF with tension band wire loop (figure-8) around
K wires. ORIF with small fragment plates for more complicated fractures.
intraarticular hematoma, injection of lidocaine followed by ROM
(especially pronation and supination) of the elbow.
wherever technically possible using minifragment screws (or mini plates
for Mason 3). Excision of radial head where reduction is not possible
using metallic spacer where there is an ipsilateral wrist injury.
plates and screws for any displaced forearm shaft fracture in an adult.
The exception is the isolated ulna fracture with minimal shortening
(<1–2 mm) and at least 50% apposition of bone fragments. Generally
use eight-hole plate length or longer; plates should be left in
wherever possible.
-
Galeazzi variant—fixation of radius as
described, with examination of distal radioulnar joint. If stable in
supinated position, hold forearm in supinated position for 6 weeks; if
joint is unstable, apply temporary K wire fixation. -
Monteggia variant—fixation of ulna
fracture as described, examination (radiographic and clinical) of
radiocapitellar joint. If not reduced, check ulna reduction for
anatomicity and, if perfect, undertake open reduction of radius. -
Isolated ulna—ORIF with technique described for fractures with significant displacement and shortening.
-
Isolated radius—ORIF with technique
described for fractures with significant displacement (>2–3 mm of
shortening) or loss of radial bow.
and lateral radiographs of the forearm, physical examination. Computed
tomography scan can be helpful for intraarticular fractures.
-
Extraarticular variant—closed reduction
under intravenous regional or hematoma block. Follow up radiographs in
3 to 7 days to be sure that reduction is maintained. Comminution at the
fracture site makes redisplacement likely. The reduction must be
neutral on the lateral with >4 mm loss of radial length on
anteroposterior view this is age dependent. External fixation is also
an option. -
ORIF or closed reduction with percutaneous pinning for intraarticular fractures with greater than 2-mm displacement.
with K wires or small fragment specialized plates. Volar approach with
small T plate for Barton (volar, partial articular fractures).
DM, Wild LM, Schemitsch EH, et al. Standard surgical protocol to treat
elbow dislocations with radial head and coronoid fractures. J Bone Joint Surg (Am) 2004;86:1122–1130.
PO, Gentz CF, Johnell O, et al. Surgical versus nonsurgical treatment
of ligamentous injuries following dislocations of the elbow. J Bone Joint Surg (Am) 1987;69:605–608.
JP, Werier J, MacDermid JC, et al. Arthroplasty with a metal radial
head for unreconstructible fractures of the radial head. J Bone Joint Surg (Am) 2001;83:1201–1211.
D, Prommersberger K, Jupiter JB. Combined dorsal and volar plate
fixation of complex fractures of the distal part of the radius. J Bone Joint Surg (Am) 2004;86:1616–1652.
EH, Richards RR. The effect of malunion on functional outcome after
plate fixation of both bones of the forearm in adults. J Bone Joint Surg (Am) 1992;74:1068–1078.
RR, Schmeling GL, Schwab JP. The necessity of acute bone grafting in
diaphyseal forearm fractures: a retrospective review. J Orthop Trauma 1997;11:288–294.
P, Holmich P, Orsnes T, et al. Isolated ulnar shaft fractures:
comparison of treatment by a functional brace and long-arm cast. J Bone Joint Surg (Br) 1992;74:757–759.