Fractures of the Humerus
-
General principles.
Epiphyseal fractures are considered separately. Fractures of the
proximal humerus are seen in all age groups but are more common in
older patients. In young adults, they are a result of high-energy
trauma. In older patients, treatment is designed to maintain
glenohumeral motion. Considerable angulation at the fracture site may
be accepted; motion is begun early to avoid shoulder stiffness. -
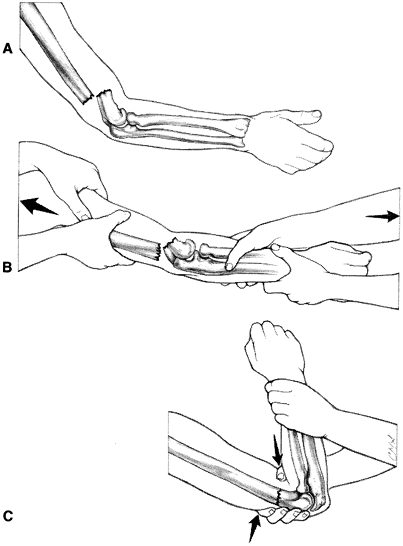
Classification and treatment. Neer divides proximal humeral fractures into six groups, as shown in Fig. 17-1,
and this concept is useful in considering the management of the injury.
There is lack of reliability in interpreting radiographs to accurately
classify proximal humerus fractures. Elderly patients who are too ill
to be considered for surgery are treated as described for the first
group.-
Fractures with minimal displacement and displaced anatomic neck fractures.
Approximately 85% of all fractures of the proximal humerus are in this
category. Any fracture pattern can be seen, but the displacement of all
components must be less than 1 cm, except anatomic neck fractures, to
be considered in this group according to Neer’s concept. Angulatory or
rotatory deformity should not exceed 45 degrees. Stability is usually
afforded by some impaction and the preservation of soft-tissue
attachments. A sling is the preferred treatment. Wrist and hand
exercises are begun immediately. Circumduction exercises should be
started as soon as they can be tolerated, generally within 5 to 7 days.
The patient is instructed to bend to 90 degrees at the waist, allowing
the arm to either hang or swing in a gentle circle and avoid active
contraction of the shoulder muscles (1).
Assisted forward elevation and assisted external rotation exercises in
the supine position can generally be started approximately 10 to 14
days after injury. The fracture site is often completely pain free
after 2 to 3 weeks, and full range of motion is possible in 4 to 6
weeks. Some form of protection may be needed for 6 to 8 weeks; then
more vigorous physical therapy may be prescribed, including wall
climbing, overhead rope-and-pulley, passive range of motion, and
rotator cuff strengthening exercises (2). -
Displaced surgical neck fractures.
The fracture generally occurs with the arm in abduction. The rotator
cuff is usually intact. Undisplaced linear fractures that extend into
the humeral head can occur. The fracture site is often angulated more
than 45 degrees or malrotated. Neurovascular injury can occur in this
type of fracture because the shaft may be displaced into the axilla.
This is more common in elderly patients with atherosclerotic (less
compliant) arteries.-
Treatment is by closed reduction
under general or supraclavicular regional anesthesia. Align the distal
fragment to the proximal one. This alignment usually requires abduction
and flexion. Reduction of the fracture depends on an intact
posteromedial periosteal sleeve in younger patients. The fracture may
be stable enough to permit immobilization of the arm at the side in a
sling-and-swathe but may require a spica cast or abduction pillow
splint to hold the arm in the reduced position. Fixation can be added
percutaneously to maintain the reduction; this is generally advised in
younger patients. This treatment should be chosen with caution in
patients with significant osteoporosis. As soon as the immobilization
is
P.240
concluded,
generally in 2 to 3 weeks, a program to regain shoulder motion is
started as for fractures with minimal displacement and anatomic neck
fractures. Unstable reductions may necessitate percutaneous pin or
screw fixation. In unreliable patients, the fixation may need to be
protected with a shoulder spica cast for 3 weeks. With reliable
patients, gentle circumduction exercises can be started immediately
after pinning and the exercise program advanced as described at 4 to 6
weeks after surgery for pin removal.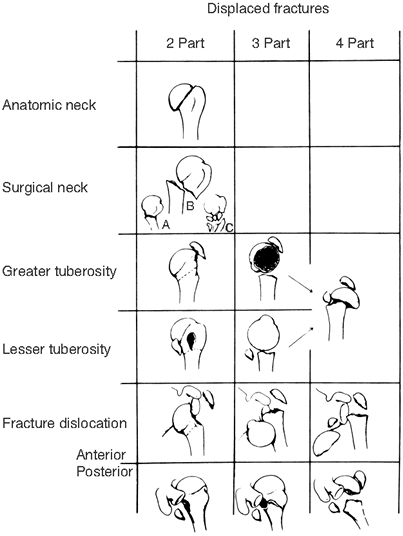 Figure 17-1.
Figure 17-1.
Neer’s anatomic concept for standardizing the terminology of fractures
of the proximal humerus. (From Neer CS. Displaced proximal humeral
fractures. Part I. J Bone Joint Surg (Am) 1970;52:1077, with permission.) -
If closed reduction is impossible,
then consideration is given to open reduction and plate fixation or
tension band wiring. A low profile plate such as the AO/ASIF
(Association for the Study of Internal Fixation) cloverleaf small
fragment plate or proximal humeral locking plate is preferred. The
locking plates are particularly useful in patients with osteopenia.
-
-
Displaced greater or lesser tuberosity fracture, or both.
Rarely, a three-part fracture is encountered involving the lesser or
greater tuberosity as well as the surgical neck. If the fracture is
displaced, then the rotator cuff function is compromised and open
reduction of the fracture is indicated. The fracture should be
anatomically reduced and held firmly with tension band wiring or screw
fixation. It is also possible to fix these fractures percutaneously,
but this
P.241
will
not address a rotator cuff tear. The rotator cuff tear can be addressed
later if pain and weakness remain after the rehabilitation program is
implemented. -
A fracture-dislocation of the shoulder,
whether anterior or posterior, may be reduced by a closed method under
general anesthesia. If closed reduction fails, then open reduction with
internal fixation or prosthetic replacement (in older patients) is
indicated. -
Neer (see Selected Historical Readings) states that open reduction is indicated for any displaced three-part fracture and that prosthetic replacement is preferable treatment for any displaced four-part fracture.
This is because of the high rate of posttraumatic humeral head
osteonecrosis in four-part fractures. We believe that, at best, these
are difficult fractures to treat and that operative treatment should be
undertaken only by surgeons with special expertise in managing shoulder
trauma.
-
-
Complications
-
The most common complication is loss of some glenohumeral motion,
especially of internal rotation and abduction. This often occurs as a
result of malposition of the greater tuberosity. The best way to
rehabilitate the glenohumeral joint is to start motion early and to
achieve primary fracture union. Careful attention to starting an early
physical therapy program can markedly improve the end result. Home
programs where exercises are performed by a motivated patient two to
three times per day with weekly physical therapy monitoring seems to
produce the best results. Open treatment may be indicated to achieve
adequate stability of displaced fractures to allow early motion. -
Delayed union or nonunion
is not uncommon with displaced fractures, especially surgical neck
fractures. When it occurs, some loss of joint motion generally results,
regardless of subsequent treatment. If the patient experiences pain and
loss of motion in association with the nonunion, then the treatment is
either replacement arthroplasty or internal fixation with bone grafting. -
Associated nerve and vascular damage
is not rare with displaced fractures and should be identified early so
that prompt, effective treatment can be instituted. Involvement of the
axillary, median, radial, and ulnar nerves is reported with nearly
equal frequency.
-
-
Examination.
The injury is most often seen in children 8 to 14 years of age. On
examination, the shoulder usually is deformed. Roentgenograms reveal
the correct diagnosis. The epiphyseal fracture is usually a Salter
class 2 or, less commonly, a class 1 fracture (see Chap. 1, VII.B). -
Treatment.
The fracture may usually be reduced by closed methods after appropriate
anesthesia. Reduction requires aligning the distal fragment to the
proximal one, usually by abduction and external rotation of the distal
fragment. Up to the age of 9 years in a girl and 10 years in a boy,
remodeling produces a normal shoulder as long as the rotation of the
two fragments relative to one another is correct. Up to 11 years in a
girl and 12 in a boy, 50% apposition is acceptable, but varus
malalignment should not exceed 45 degrees and rotary deformity must be
minimal. The younger child is placed in a shoulder spica cast with the
arm in the reduced (abducted) position. The cast is maintained for 4 to
6 weeks, at which time it may be removed and the arm brought to the
side. Treatment is then carried out in a sling with circumduction
exercises. Open reduction rarely is indicated, but closed manipulation
and percutaneous pin fixation should be considered if closed reduction
fails to achieve an acceptable degree of correction and stability. The
mature adolescent should be treated as an adult.
-
The diagnosis
is usually self-evident, and the exact fracture pattern is confirmed by
anteroposterior and lateral roentgenographic examination. The incidence
of this fracture is bimodal occurring at the highest rate in young
adults and individuals 60 years of age and older (9). Although the fracture may occur in any part of the diaphyseal bone, the middle third is most commonly involved. -
Physical examination
should be thorough to rule out any nerve or vascular damage. Radial
nerve injury is common with this fracture. The time of onset of any
nerve involvement must be accurately documented. There are three
separate mechanisms by which the nerve may be involved.-
Damage at the time of injury
usually produces a neurapraxia, less commonly an axonotmesis or
traction injury, and rarely a neurotmesis. Neurotmesis is most commonly
associated with open fractures (4). -
During the process of manipulation and immobilization,
neurapraxia can occur, and if the pressure is not relieved, then it can
become an axonotmesis. This usually is a result of the nerve’s becoming
trapped between the fracture fragments. -
During the process of internal fixation, neurapraxia or axonotmesis can develop from manipulation of the nerve.
-
-
Treatment (4,5,6,7,8,9,10)
-
The fracture
should be treated by placing the forearm in a collar and cuff by
immobilizing the arm against the thorax with plaster coaptation
splints, as shown in Fig. 17-2.
The splint can be removed and the patient placed into a snug-fitting
commercial or custom fracture orthoses at 2 to 3 weeks after injury (10,11).
Shoulder and elbow motion is then initiated. Bayonet apposition is
acceptable as long as alignment is good. Distraction should be avoided
and is generally a harbinger of nonunion. Open reduction is indicated
for a vascular injury, for Holstein fracture (an oblique distal third
fracture with radial nerve injury where the nerve can be trapped in the
fracture), for an open fracture (where the nerve should be explored),
for bilateral fractures, for massive obesity (where closed reduction
and orthotic treatment is not possible), and for patients with
polytrauma (3,5).
Plates and screws, reamed intramedullary nails, and flexible
intramedullary nails seem to be equally efficacious. Intramedullary
nails can be placed without opening the fracture site, but they do
result in a 20% to 30% incidence of postoperative shoulder pain (4,5,6,7,8). For
P.243
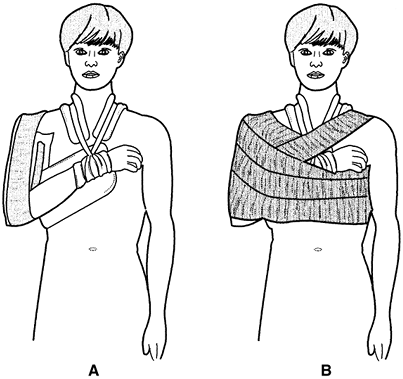
this reason, plate fixation is the preferred method of operative stabilization in most settings.![]() Figure 17-2. Treatment of the humeral shaft fractures. A:
Figure 17-2. Treatment of the humeral shaft fractures. A:
The first step is to apply coaptation splints to the arm and then to
apply a commercial collar and cuff or one made of muslin. Stockinet
should not be used because it stretches. The neck and wrist are padded
beneath the collar and cuff with felt. B:
After adequate padding in the axilla and beneath the forearm, the arm
and forearm can be immobilized against the thorax with a swathe. -
Treatment of an associated radial nerve injury
-
Nerve involvement at the time of injury calls for passive range-of-motion exercises of the wrist and fingers and for use of a radial nerve splint for the wrist and fingers if return of function is not beginning at 2 to 3 weeks. Follow up the patient for nerve recovery as outlined in Chap. 1, V.E for nerve injuries. The prognosis for recovery is excellent, with 90% or more patients regaining full function.
-
Nerve involvement at the time of closed reduction should be treated with nerve exploration and fixation as soon as possible.
-
Late nerve involvement is also an indication for exploration and neurolysis.
-
-
-
Complications.
Delayed unions and nonunions do occur. They are best treated with
compression plating and a cancellous bone graft. Longer plates and the
use of methyl methacrylate in screw holes may be necessary in
osteoporotic patients. If nonunion occurs after intramedullary nailing,
plate fixation with bone grafting results in healing in approximately
90% of cases; repeat IM nailing is generally not advisable.
-
A supracondylar fracture is most common in children and elderly patients, but it may occur at any age (12). The mechanism of injury
is extension or flexion, or a direct blow as a result of high-energy
trauma. The extension type of injury is produced by a fall on the
extended arm and is stable only in significant flexion. Such a fracture
may have an intracondylar or intracapsular component. The flexion type
is produced by a fall on the flexed elbow and is relatively stable in
extension. -
Examination.
The elbow injury is obvious clinically, but the full extent of the
damage must be demonstrated with good roentgenograms. Because of the
potential for associated vascular and nerve injury, it is essential to
conduct a careful assessment for such injuries. Vascular damage, nerve
damage, or marked displacement constitutes a surgical emergency. At
times, it is possible to bring about relief by reducing the fracture
with sedation and applying a splint. -
Treatment
-
Children
-
Because of the seriousness of the potential complication of Volkmann’s contracture with a supracondylar fracture,
nearly all children with a displaced fracture are admitted to the
hospital as close monitoring of the neurovascular status is required.
As soon as the condition of the patient allows, a definitive reduction
under general anesthesia is attempted. The technique of reduction is
illustrated in Figs. 17-3 and 17-4.
The authors prefer percutaneous or open cross–Kirschner-wire fixation
after reduction. If the patient is seen late and the swelling is
massive, an alternative is the use of Dunlop traction until the
swelling resolves (see Fig. 9-5).
In the younger child, there is some latitude in anteroposterior
angulation or displacement. The direction of the initial displacement
provides a clue for the proper forearm position after reduction. If the
initial displacement is medial, then placing the forearm into pronation
tightens the medial hinge, closes any lateral gap in the fracture line,
and helps prevent subsequent cubitus varus. If the initial displacement
is lateral, then placing the forearm in supination tightens the lateral
soft-tissue hinge, closes the medial aspect of the fracture line, and
helps prevent cubitus deformity. The use of Baumann angle
to guide treatment was described in the German literature in 1929. To
use this technique, bilateral roentgenograms of the distal humerus are
necessary. A line is drawn down the center of the diaphysis of the
humerus, and another is drawn across the epiphyseal plate of the
capitellum. If the angle is 5 degrees different from the unaffected
side, the reduction is not complete and a significant abnormality in
the carrying angle, such as cubitus varus, may result. The reduction is
generally off in rotation. On the lateral radiograph, the anterior
humeral line must pass through the capitellum to ensure that there is
not a malreduction with rotation or extension.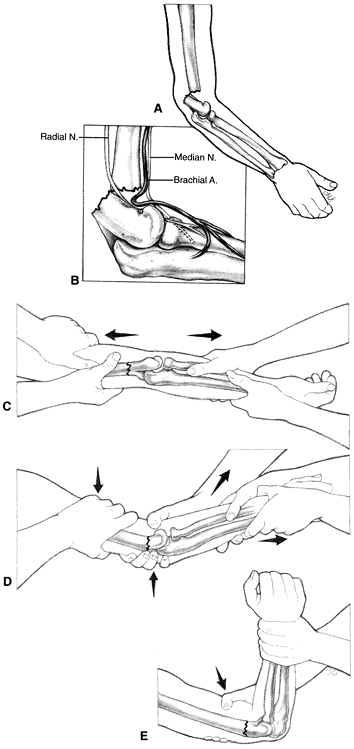 Figure 17-3. Reduction technique for supracondylar humeral fractures that occur with the elbow in flexion. A: Distal fragment is displaced posteriorly. B: The brachial artery may become entrapped at the fracture site. C: Restore length by applying traction against countertraction. D: With pressure directed anteriorly on the distal fragment, provide reduction. E: The reduction is generally stable with the elbow in flexion with the forearm pronated.
Figure 17-3. Reduction technique for supracondylar humeral fractures that occur with the elbow in flexion. A: Distal fragment is displaced posteriorly. B: The brachial artery may become entrapped at the fracture site. C: Restore length by applying traction against countertraction. D: With pressure directed anteriorly on the distal fragment, provide reduction. E: The reduction is generally stable with the elbow in flexion with the forearm pronated.![]() Figure 17-4. Reduction technique for supracondylar fractures that occur with the elbow in extension. A: The distal fragment is displaced anteriorly relative to the proximal fragment. B: Restore length by applying traction against countertraction. C:
Figure 17-4. Reduction technique for supracondylar fractures that occur with the elbow in extension. A: The distal fragment is displaced anteriorly relative to the proximal fragment. B: Restore length by applying traction against countertraction. C:
With pressure directed posteriorly on the distal fragment, the fracture
is reduced. The elbow is then extended to enhance stability of the
reduction in most circumstances.P.244P.245Open reduction may be necessary if repeated attempts at
closed reduction fail. Small incisions are recommended to place the pin
starting from the medial side to be sure the ulnar nerve is not injured
(12). An anterior or lateral incision may be
used to expose the fracture. The anterior incision may provide the
easiest direct exposure because of the generally extensive damage to
the brachial muscle by the fracture displacement. Internal fixation or
percutaneous smooth pins are often required to maintain a satisfactory
reduction. Because there is the serious possibility of causing nerve
and vascular damage in this region, repeated manipulation should be
infrequent and the rule “one doctor, one manipulation” applies. Splint
the elbow in 20 to 30 degrees of flexion after pinning the fracture to
allow for swelling. This is only possible when the fracture has been
stabilized by pin fixation. The patient must be observed for at least
24 hours for the signs and symptoms of compartment syndrome. Frequent
checks of the radial pulse by palpation and Doppler are recorded in the
chart, and the patient is closely observed for the signs of
compartmental syndrome (see Chap. 2, III).
The pins are removed after 3 to 4 weeks, and intermittent active motion
is started out of cast or splint. The splint is discarded 6 weeks after
the
P.246
injury.
Stiffness may result from overzealous attempts of family, friends, and
therapists to aid the child in regaining motion quickly. The child
should be allowed to use the elbow, and the family should be reassured
that he or she will gain extension of the joint with time and growth. -
Distal humeral epiphyseal slips in younger children are rare, but when they occur, they should be treated as supracondylar fractures.
-
-
Adults. These
injuries occur rarely and generally in elderly individuals. Stiffness
in the elbow develops rapidly in the older patient when the elbow is
immobilized for any length of time. One of the requirements for any
method of treatment is to allow early mobilization. Therefore,
treatment should be as follows:-
If the fracture is minimally displaced and stable,
then supination-pronation exercises are begun within 2 to 3 days
without removal of the posterior splint. After 2 weeks, the splint may
be removed during these sessions to allow some active flexion and
extension. -
If the fracture is displaced, the percutaneous pins may be used for stability to allow early motion as outlined in 1.a (above).
-
Open reduction and internal fixation should be considered if steps a and b do not produce satisfactory alignment and stability (13,14).
-
If the elbow is grossly swollen and
difficult to treat by the aforementioned methods or if marked
comminution precludes stable fixation, then olecranon pin traction with early movement is an option; it is rarely indicated.
-
-
-
Complications
-
Cubitus varus and valgus (varus is far more common)
-
Loss of elbow motion
-
Tardy ulnar nerve palsy
-
-
Type of injury.
“T” and “Y” fractures are typically supracondylar fractures of the
lower end of the humerus with a vertical component running into the
elbow joint, but any combination of fractures in this area (e.g.,
comminuted fractures, fractures of the capitulum) are included in this
category. Some comminution usually is present. -
Roentgenograms.
Films must be of excellent quality to assess the fracture pattern
adequately. Intraoperative traction films may be helpful in defining
the fracture pattern. -
Treatment. If
the fracture is one in which reduction and firm fixation can be
achieved by open reduction and internal fixation, then this is
performed (14). Highly comminuted fractures
should be referred to experienced fracture surgeons to prevent the
situation of open reduction and unstable fixation. Optimum exposure for
anatomic reduction of the joint surface often requires an olecranon
osteotomy; patients undergoing internal fixation should be started on
active range-of-motion exercises within 3 to 5 days of the procedure.
If the degree of comminution is so great that the internal fixation
cannot be satisfactorily achieved and referral is not an option, then
the fracture may rarely be treated by olecranon pin traction and early
motion. Begin movement of the hand and fingers, and commence shoulder
movements after 2 weeks. If traction is not used, active flexion from
the position of immobilization is encouraged if it does not cause pain.
Tenderness usually disappears in 4 to 6 weeks; the splint is then
discarded, and further active elbow movement is encouraged. This injury
commonly results in significant loss of elbow extension. In the most
comminuted fractures in elderly individuals, total elbow replacement is
an excellent option. This requires referral to an experienced elbow
surgeon.
-
Type of injury. These are nearly always seen in children and are a serious injury type of the disruption of the joint surface.
-
Roentgenograms.
Routine anteroposterior and lateral films are obtained, but oblique
films and films of the uninjured elbow often are needed to define the
injury accurately. -
Treatment. If
displacement is present, then open reduction and pin (two small
Kirschner wires) fixation are essential. If no displacement is evident,
then additional
P.247
roentgenograms
should be obtained in 5 to 7 days to check position. Open reduction is
done through a lateral approach with minimal stripping of the bony
fragment. Rotation of the fragment must be accurately assessed. The
pins are removed at 3 weeks; gentle exercises are started at 6 weeks. -
Complications
-
Failure to achieve accurate reduction of the fracture results in cubitus valgus, late arthritic changes, nonunion, or a tardy ulnar nerve palsy.
-
When the epiphysis is open, overgrowth of the lateral condyle occasionally occurs, with a resulting cubitus varus.
-
-
Mechanism of injury.
The center of ossification of the medial epicondyle of the humerus
appears at 5 to 7 years of age. Displacement of the medial epicondyle
as an isolated injury is uncommon. The common mechanism is the result
of an elbow dislocation with avulsion of the fragment. This is most
common in children but can occur in adults. The medial ligament of the
elbow maintains its inferior attachment and pulls the medial epicondyle
from the humerus. -
The diagnosis
may be made clinically in a great majority of cases. When the medial
epicondyle has been avulsed, there is a surprisingly large defect,
which is easily palpated even in a swollen elbow. -
Roentgenograms are used to identify the position of the medial epicondyle. Roentgenograms of the normal elbow are helpful.
-
Treatment.
Reduce any elbow dislocation by linear traction with sedation and
assess the position of the fragment roentgenographically. The medial
epicondyle may be trapped within the joint, causing incomplete motion.
If the epicondyle is in the joint, then open reduction is required. The
medial epicondyle fracture can be reduced and held by pin fixation. In
adults, consider small fragment screws. If open reduction is
undertaken, the ulnar nerve must be protected but need not be transpositioned anteriorly. -
Complications
are largely those of an elbow dislocation. If the medial epicondyle
remains displaced, ulnar nerve problems are not uncommon. If the
epicondyle is anatomically reduced and the elbow joint space is
roentgenographically sound, then the injury can be treated by splinting
for 7 to 10 days followed by early active motion exercises (earlier in
adults).
shoulder radiograph with axillary view and transscapular lateral
(shoulder trauma series) view. Consider computed tomography scan with
reconstructions if a displaced three- or four-part fracture is noted on
plain radiographs and the patient is a surgical candidate.
humeral head is located. If the fracture is impacted or minimally
displaced, apply sling for comfort and begin assisted range-of-motion
exercises at 7–14 days.
Marked (greater than 1 cm) displacement of tuberosity fragments, varus
angulation of head, dislocated humeral head, head-splitting fracture,
or open fractures.
-
Greater tuberosity fractures: open reduction and screw or tension band fixation
-
Two-part surgical neck fractures: closed
reduction and percutaneous pinning. In pediatric fractures, plate or
intramedullary nail fixation in adults -
Three-part fractures: closed reduction and pinning versus open reduction with internal fixation with tension band technique
-
Four-part fractures, head-splitting
fractures: prosthetic replacement is advisable for elderly patients
with markedly comminuted fractures or those associated with humeral
head dislocation.
and application of coaptation splints convert splints to functional
brace and begin range-of-motion exercises for shoulder and elbow 2
weeks following injury.
4.5-mm large fragment low contact dynamic compression plate (LCDCP),
explore and protect radial nerve. Alternatively, use an antegrade
interlocking humeral nail but expect shoulder pain in 20% to 30% of
individuals.
Posterior approach with olecranon osteotomy where articular
displacement is severe. Fixation with two 3.5-mm reconstruction plates
at right angles. Olecranon osteotomy fixed with 6.5-mm cancellous
screws with tension band wire.
AJ, Roolker W, Patt TW, et al. Open reduction and internal fixation of
three and four part fractures of the promimal part of the humerus. J Bone Joint Surg (Am) 2002;84:1919–1925.
MJ, Beauchamp CG, Kellam JK, et al. The results of plating humeral
shaft fractures in patients with multiple injuries: the sunnybrook
experience. J Bone Joint Surg (Br) 1985;67:293–296.
DL, Hale JM, Bassett J, et al. Operative treatment of supracondylar
fractures of the humerus in children. The consequences of pin
placement. J Bone Joint Surg (Am) 2001;83:735–740.
TR, Koval ICJ, Gallagher M, et al. Open reduction and internal fixation
of the distal humerus. Functional outcome in the elderly. J Trauma 1997;43:578–584.
E. Beiträge zur Kenntnis der Frakturen an Ellbogengellenk unter
besonderer Berücksichtigung der Spätfolgen. I. Allgemeines und Fractura
supra condylica. Beitr f Klin Chir 1929;146:1–50.
JL, Ecker ML, Chung SM, et al. Supracondylar fractures of the humerus
in children treated by closed reduction and percutaneous pinning. Clin Orthop 1983;177: 203–209.
EJ, Radin EL. Intercondylar T fractures of the humerus in the adult. A
comparison of operative and nonoperative treatment in twenty-nine
cases. J Bone Joint Surg (Am) 1969;51:130–131.