Carpal Tunnel Syndrome
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Carpal Tunnel Syndrome
Carpal Tunnel Syndrome
Dawn M. LaPorte MD
Tung B. Le MD
Description
-
CTS is a neuropathy caused by compression of the median nerve within the carpal tunnel.
-
The floor of the tunnel is formed by the volar radiocarpal and intercarpal ligaments.
-
The transverse carpal ligament forms the roof of the tunnel.
-
9 long flexors of the wrist and fingers and 1 nerve (median) run within this spatially limited and relatively rigid tunnel.
-
Thus, any increase in pressure within the tunnel compresses the injury-prone median nerve.
-
A decrease in thenar muscle strength
occurs, along with a numbness or a decrease in the sensibility of the
palmar surface of the radial 3 1/2 digits, especially the middle and
index fingers.
Pregnancy Considerations
-
Occurs more frequently in pregnant than in other individuals
-
Usually resolves postpartum
-
Avoid surgery during pregnancy.
-
Treat with nighttime cockup wrist splint(s) ± corticosteroid injection.
-
Epidemiology
Incidence
-
50% of cases are reported to occur in patients 40–60 years old; average age at carpal tunnel release is 54 years (1).
-
CTS occurs predominantly in females (70%), although the number of males with CTS may be underestimated (1).
Prevalence
-
The prevalence of CTS has been reported to vary between 0.6% and 61% in different occupational groups (2).
-
It is the most commonly diagnosed site of nerve compression in the upper extremity (2,3).
Risk Factors
-
Repetitive hand work
-
Endocrine imbalance
-
History of neuropathy
-
Associated conditions
-
Rheumatoid arthritis
-
Pregnancy
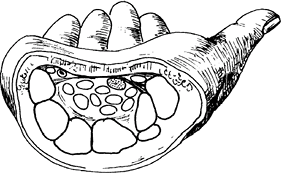 Fig. 1. The median nerve is shown in the carpal tunnel with the finger flexor tendons, under the transverse carpal ligament.
Fig. 1. The median nerve is shown in the carpal tunnel with the finger flexor tendons, under the transverse carpal ligament. -
Thyroid myxedema
-
Acromegaly
-
Amyloidosis
-
Multiple myeloma
-
Diabetes
-
Trauma
-
Alcoholism
-
Gout
-
Space-occupying lesions within carpal tunnel
Genetics
No genetic predisposing factor to CTS has been described.
Pathophysiology
-
Internal fibrosis of the median nerve
-
Epineural scarring and constriction
-
Reduced nerve conduction velocity
Etiology
-
Any factor that increases the pressure within the tunnel compresses the median nerve and leads to CTS.
-
The most common causes include flexor
tenosynovitis; trauma to the carpal bones; ganglion, fibroma, or lipoma
within the tunnel; rheumatoid cyst; gout; and diabetic neuropathy (Fig. 1).
-
CTS can be diagnosed accurately by
careful history and physical examination, inspection for thenar
atrophy, and detection of sensory disturbance via light touch or a
pinwheel. -
Provocative tests, such as the Phalen
test (which consists of placing the affected wrist in hyperflexion in
an attempt to reproduce the numbness in the hand) or tapping over the
course of the nerve in the tunnel to elicit a Tinel sign, also serve to
confirm the diagnosis.
Signs and Symptoms
-
These symptoms can be aggravated with use of the affected hand:
-
Paresthesia in the median nerve distribution in the hand
 Fig.
Fig.
2. The Phalen test for median nerve compression in the carpal tunnel is
performed by holding the wrist flexed 90° for 30 seconds and checking
for paresthesias in the fingers. -
Weakness or clumsiness in the hand
-
Pain in the hand, wrist, or distal forearm
-
Awakening from sleep with pain or numbness in the hand
-
Tinel sign: Tapping the median nerve over the carpal tunnel with resultant paresthesias in the radial 3½ fingers
-
Phalen sign: Paresthesias in the median nerve distribution with full flexion for at least 1 minute
-
Physical Exam
-
The hand should be examined to detect thenar muscle atrophy.
-
2-point discrimination should be checked at the tips of the fingers on the radial and ulnar borders (should be <5–6 mm).
-
Provocative tests such as the Phalen and Tinel tests should be performed (Figs. 2 and 3).
Tests
-
The following basic tests should be ordered to rule out systemic causes of CTS:
-
Sedimentation rate
-
Serum glucose concentration
-
Serum uric acid level
-
Thyroid function test
-
Electromyography/nerve conduction velocity can confirm diagnosis and help determine severity.
-
Imaging
-
Radiography
-
Plain radiographs of the wrist in
patients with previous trauma or in patients with a long history of
inflammatory disease should be performed. -
Cervical spine radiographs also can reveal a cervical rib, if thoracic outlet syndrome is suspected.
-
-
Electromyographic studies can help rule out proximal injury to the median nerve or identify peripheral neuropathy.
Differential Diagnosis
-
TOS
-
Compression of the lower cervical roots by cervical degenerative disc disease or tumors
![]() Fig.
Fig.
3. A Tinel sign indicates an irritated median nerve. It refers to
radiating pain down the fingers after percussion of the carpal tunnel.
P.55
General Measures
-
Nonoperative intervention:
-
Modalities: Cockup wrist splinting,
NSAIDs (not proven effective), diuretics, and cortisone injections
(which must be performed by an experienced physician to avoid direct
injury to the median nerve) -
The patient should wear a wrist splint during sleep (4,5).
-
-
Activity modification in work-related CTS is recommended.
-
Surgical release of the transverse carpal
ligament is performed when nonoperative measures have failed or in
patients with constant numbness, motor weakness, or increased distal
median nerve motor latency noted on electromyography.
Special Therapy
Physical Therapy
-
Occupational or physical therapy should
be consulted for activity modification teaching or for nerve gliding
exercises that might decrease symptoms of nerve compression (6,7). -
Postoperative therapy is aimed at minimizing the development of painful scars and increasing ROM and strength.
Medication (Drugs)
-
No effective medication specifically to treat CTS has been described.
-
Corticosteroid injection into the carpal
tunnel is indicated when the median nerve compression is predicted to
be temporary, as in pregnancy or when the patient’s activity can be
modified.-
Injections must be done with great care to avoid injury to the median nerve.
-
Surgery
-
Open carpal tunnel release is made
through a longitudinal incision that begins on the distal border of the
transverse carpal tunnel ligament and extends proximally to the
proximal wrist crease, in line with the ulnar border of the axis of the
ring finger. -
The incision then is carried through the palmar fascia to the transverse carpal ligament.
-
The ligament then is divided carefully via a combination of scalpel and scissors.
-
Care should be taken to avoid the palmar cutaneous branch or the motor branch of the median nerve.
-
After division of the ligament, the
carpal tunnel and the median nerve should be inspected for any
space-occupying lesion or any signs of chronic inflammation requiring
neurolysis. -
The skin then is reapproximated with nylon sutures.
-
Compared with open carpal tunnel release,
endoscopic carpal tunnel release has equivalent results at 1 year after
surgery but return to work may be faster.
Prognosis
-
Most patients with CTS associated with
the repetitive trauma commonly seen in the workplace respond to a
combination of splinting, cortisone injection into the carpal tunnel,
and activity modification. -
If job modification is not in the
patient’s nonoperative treatment program, splinting and cortisone
injections may provide only temporary relief. -
The maximum return of strength after carpal tunnel release can take 6 months or longer.
Complications
-
Iatrogenic injuries to the median nerve or its branches may occur with open or endoscopic release.
-
Painful surgical scars may ruin the results of a successful decompression procedure.
-
Flexion tendon bowstringing may occur in a few patients.
Patient Monitoring
-
To obtain maximal beneficial results, the
splint should be worn full-time for at least 3–4 months, after which
time use of the splint can be discontinued gradually. -
If symptoms return with removal of the splint, the patient becomes a surgical candidate.
-
The patient usually experiences immediate
pain relief after carpal tunnel release, whereas numbness gradually
improves over the next several months.
-
References
1. Trumble
TE. Compressive neuropathies. In: Trumble TE, ed. Principles of Hand
Surgery and Therapy. Philadelphia: WB Saunders, 2000:324–341.
TE. Compressive neuropathies. In: Trumble TE, ed. Principles of Hand
Surgery and Therapy. Philadelphia: WB Saunders, 2000:324–341.
2. Lo SL, Raskin K, Lester H, et al. Carpal tunnel syndrome: a historical perspective. Hand Clin 2002;18:211–217.
3. Amadio PC. The first carpal tunnel release? J Hand Surg. 1995;20B:40–41.
4. Celiker R, Arslan S, Inanici F. Corticosteroid injection vs. NSAID and splinting in carpal tunnel syndrome. Am J Phys Med Rehabil 2002;81:182–186.
5. Chow JCY. Endoscopic carpal tunnel release. Two-portal technique. Hand Clin 1994;10: 637–646.
6. Rozmaryn
LM, Dovelle S, Rothman ER, et al. Nerve and tendon gliding exercises
and the conservative management of carpal tunnel syndrome. J Hand Ther 1998;11:171–179.
LM, Dovelle S, Rothman ER, et al. Nerve and tendon gliding exercises
and the conservative management of carpal tunnel syndrome. J Hand Ther 1998;11:171–179.
7. Seradge H, Parker W, Baer C, et al. Conservative treatment of carpal tunnel syndrome: an outcome study of adjunct exercises. J Okla State Med Assoc 2002;95:7–14.
Additional Reading
Hanel DP. Wrist and hand: reconstruction. In: Kasser JR, ed. Orthopaedic Knowledge Update 5. Home Study Syllabus. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1996:329–347.
Lister G. Compression. In: The Hand, Diagnosis and Indications, 3rd ed. New York: Churchill Livingstone, 1993:283–322.
Mackinnon SE, Novak CB. Compression neuropathies. In: Green DP, Hotchkiss RN, Pederson WC, et al., eds. Green’s Operative Hand Surgery, 5th ed. Philadelphia: Elsevier Churchill Livingstone, 2005;999–1045.
Codes
ICD9-CM
354.0 CTS
Patient Teaching
Activity modification teaching is important to prevent recurrence.
Prevention
The patient should avoid prolonged and repetitive motions of the wrist.
FAQ
Q: If CTS presents during pregnancy, should surgery be considered?
A:
CTS symptoms presenting during pregnancy often resolve after delivery
and therefore treatment should be with nighttime splinting ±
corticosteroid injection if indicated. Ideally, surgery should be
avoided until postpartum to allow for evaluation of resolution of
symptoms after delivery.
CTS symptoms presenting during pregnancy often resolve after delivery
and therefore treatment should be with nighttime splinting ±
corticosteroid injection if indicated. Ideally, surgery should be
avoided until postpartum to allow for evaluation of resolution of
symptoms after delivery.
Q: Does CTS recur after surgical release?
A:
CTS should not recur after surgical release. Persistent or recurrent
symptoms after surgery are most likely secondary to incomplete release,
but they also can be secondary to incorrect diagnosis or untreated
‘double crush’ syndrome with a more proximal etiology or coexisting
peripheral neuropathy.
CTS should not recur after surgical release. Persistent or recurrent
symptoms after surgery are most likely secondary to incomplete release,
but they also can be secondary to incorrect diagnosis or untreated
‘double crush’ syndrome with a more proximal etiology or coexisting
peripheral neuropathy.
Q: What are the symptoms of CTS?
A:
Patients present with complaints of pain, numbness and tingling, and
perhaps difficulty with fine motor tasks. The numbness is typically in
the thumb, index finger, middle finger, and radial 1/2 of the ring
finger. Weakness, when it is present, is in the abductor pollicis
brevis.
Patients present with complaints of pain, numbness and tingling, and
perhaps difficulty with fine motor tasks. The numbness is typically in
the thumb, index finger, middle finger, and radial 1/2 of the ring
finger. Weakness, when it is present, is in the abductor pollicis
brevis.

