The Pediatric Foot
sections: the forefoot, midfoot, and hindfoot. The forefoot consists of
the metatarsals and phalanges. The cuneiform, cuboid, and navicular
bones comprise the midfoot, and the hindfoot consists of the calcaneus
and talus. The three foot segments are linked together by strong
ligaments; because of this linkage, all foot movements occur
concurrently. Supination and pronation are combination movements in the
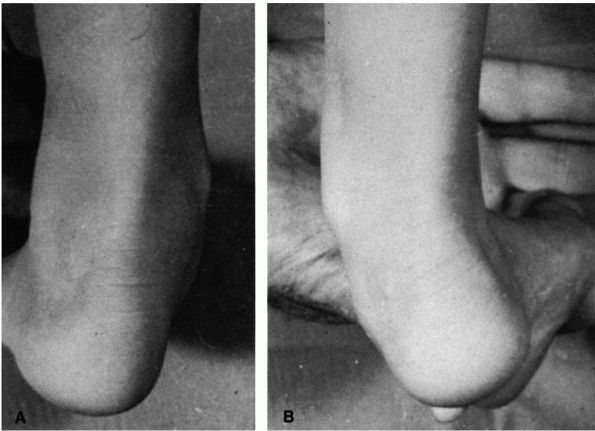
individual foot joints: supination refers to the sole pointing inward, and pronation refers to sole turning outward (Figure 20-1). Varus (inversion) and valgus (eversion) are motions of a foot segment on a theoretic longitudinal axis (Figure 20-2). When the foot is supinated, the heel goes into varus. When the foot is pronated, the heel goes into valgus (Figure 20-3). Adduction and abduction are motions of the foot segment on a theoretic vertical axis (Figure 20-4).
describing any condition of the foot in which the longitudinal arch is
lowered. It is important to distinguish between physiologic pes planus
and pes planus secondary to pathologic conditions.
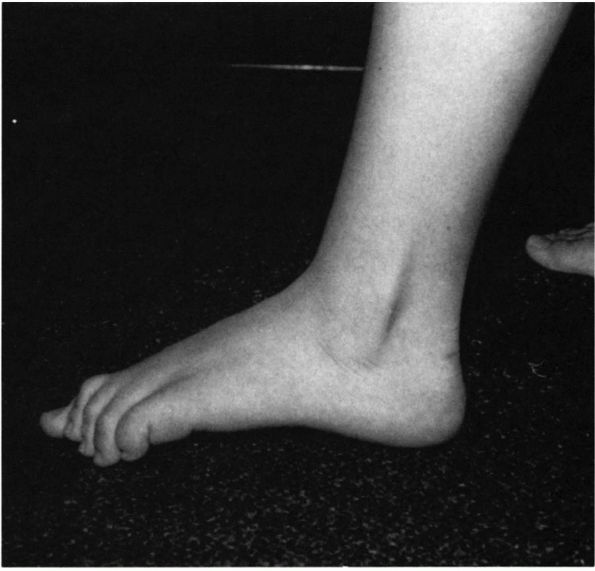
flatfoot) is characterized by varying degrees of loss of the
longitudinal arch of the foot on weight bearing. The foot assumes an
apparent pronated posture with abduction of the forefoot and varying
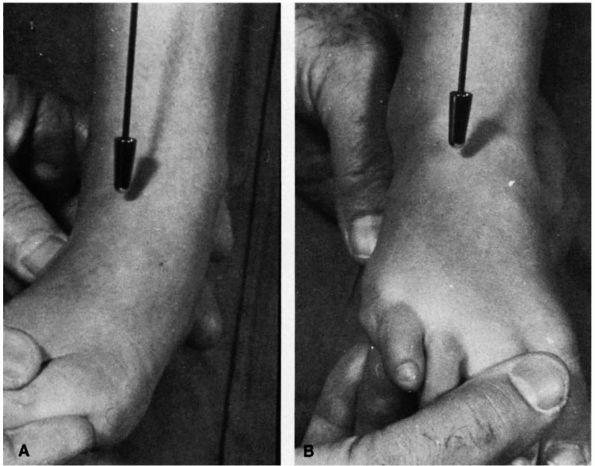
degrees of heel valgus (Figure 20-5). The
important distinguishing characteristic between physiologic and
pathologic pes planus is flexibility. In the physiologic type, the foot
remains flexible.
 |
|
FIGURE 20-1. Foot supination (sole turning inward).
|
have varying degrees of pes planus. This is due to the normal joint
hypermobility in this age group and the normal infant fat pad along the
medial aspect of the foot (Figure 20-6). In
addition, the normal wide-based stance assumed by newly standing or
walking children causes the weight-bearing line to fall medial to first
or second ray, resulting in the hypermobile foot assuming a pes planus
posture.
arch develops in most patients. It is estimated that by age 10 years,
only 4% of the population have persistent pes planus.
 |
|
FIGURE 20-2. Forefoot varus (inversion; A) and forefoot valgus (eversion; B) are motions of a foot segment on a theoretical longitudinal axis.
|
by maintenance of the normal relations between the bones of the foot.
These relations are maintained by the supporting ligamentous and
capsular structures and can be affected by functional stresses applied
to the foot in weight bearing and by muscle contraction. The foot
musculature does not maintain the longitudinal arch. Its purpose is to
maintain balance, adjust the foot to uneven ground, and propel the
body. Biomechanically, when the foot is supinated, the articulations of
the midfoot are “locked,” and the foot is a rigid structure. When the
foot is pronated, however, greater mobility is allowed at the midfoot
joints, and maximal motion can occur at the talonavicular and
calcaneocuboid joints. The position of heel valgus and forefoot
abduction with lowering of the longitudinal arch is often referred to
as a pronated foot, while in actuality,
the forefoot is supinated to varying degrees in relation to the hind
foot. Thus, in true physiologic pes planus, as the calcaneus assumes a
valgus position, the lateral aspect of the forefoot is in contact only
with the ground if the forefoot supinates to some degree in relation to
the hindfoot.
contact with the lateral border of the foot and with the first and
fifth metatarsals. In pes planus, as the calcaneus assumes a more
valgus position, the talar head loses some of its support and assumes a
more vertically oriented position, with
subsequent loss of the normal arch (Figure 20-7).
Body weight shifts medially, altering the normal weight-bearing pattern
and causing increasing ground contact with the medial aspect of the
foot. With time, the Achilles tendon may shorten and act as an everter
of the foot, accentuating the deformity.
 |
|
FIGURE 20-3. (A) Heel valgus (eversion) when foot is pronated. (B) Heel varus (inversion) when foot is supinated.
|
the cause of physiologic pes planus, most centering around abnormal
bone configuration, muscle imbalance, or ligamentous laxity. The origin
of persistent physiologic pes planus, however, remains unknown. Many
patients have a positive family history of a similar condition or
evidence of generalized ligamentous laxity. Physiologic pes planus may
also be associated with obesity. A positive family history should be
sought for conditions associated with joint laxity, such as Marfan and
Ehlers-Danlos syndromes. Physiologic pes planus is occasionally seen as
a residual of the calcaneal valgus foot deformity (discussed later). It
is important to obtain a family history of treatment of similar
conditions because this may have significant bearing on the patient
education necessary in prescribing treatment modalities to the family.
 |
|
FIGURE 20-4. Forefoot adduction (A) and forefoot abduction (B) are motions of a foot segment on a theoretic vertical axis.
|
asymptomatic. They are brought in by their parents because of the
assumption that flatfeet are abnormal and harmful to their child if not
treated. Occasionally, some children may complain of symptoms that are
referable to foot strain after prolonged activity and generally
relieved by rest. Associated leg aches are not uncommon in patients who
present with symptomatic pes planus, but because these are present in a
large portion of normal people, a cause-and-effect relation is
difficult to establish.
 |
|
FIGURE 20-5. (A and B) Physiologic pes planus. Note loss of longitudinal arch and apparent pronated posture with abduction of the forefoot. (C) Physiologic pes planus. Note heel valgus position with loss of longitudinal arch. (D)
Physiologic pes planus. With the leg dangling over the examination table in the nonweight-bearing position, the foot assumes a normal appearance to the arch. (E) Physiologic pes planus tiptoe test. When the patient stands on tiptoes, normal appearance of the arch is apparent. |
 |
|
FIGURE 20-5. (Continued)
|
joint laxity manifested by the ability to hyperextend the metacarpal
phalangeal joints,
appose
the thumb to the forearm, and hyperextend the elbows and knees. The
foot has normal to slightly increased subtalar motion. In weight
bearing, varying degrees of loss of the longitudinal medial arch are
noted. The heel is in valgus and the forefoot in abduction (see Figure 20-5).
With loss of the longitudinal arch on weight bearing, the center of
gravity is shifted medially to the second metatarsal or medially to the
first metatarsal. The patient may have a toe-in gait in an attempt to
shift the weight-bearing axis laterally.
 |
|
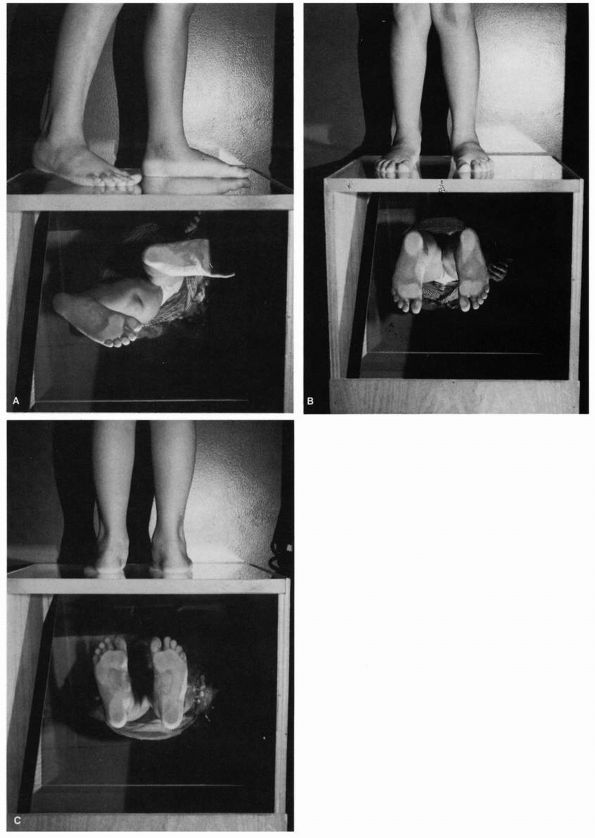
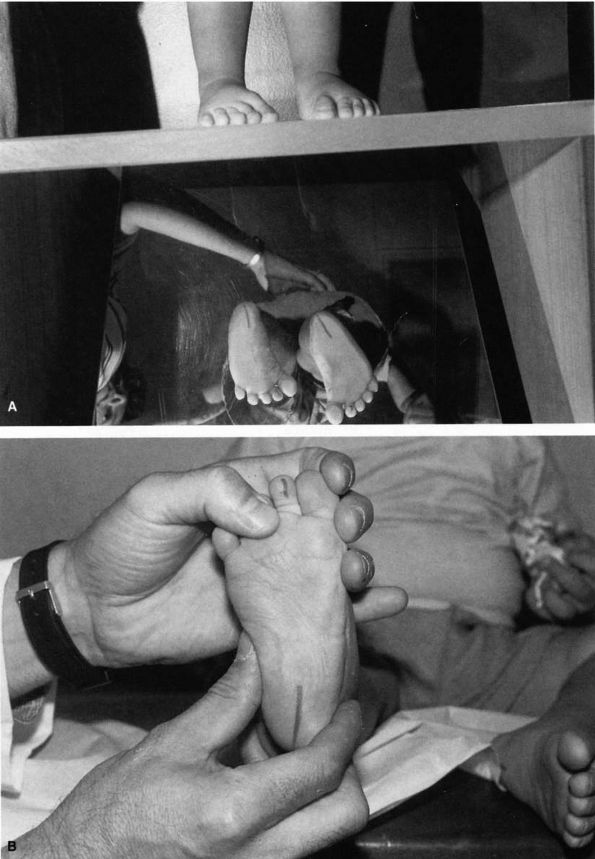
FIGURE 20-6.
Four-month-old infant with physiologic pes planus. Note prominence of the medial fat pad contributing to the appearance of pes planus (fat pad is blanched by finger pressure to emphasize its location). |
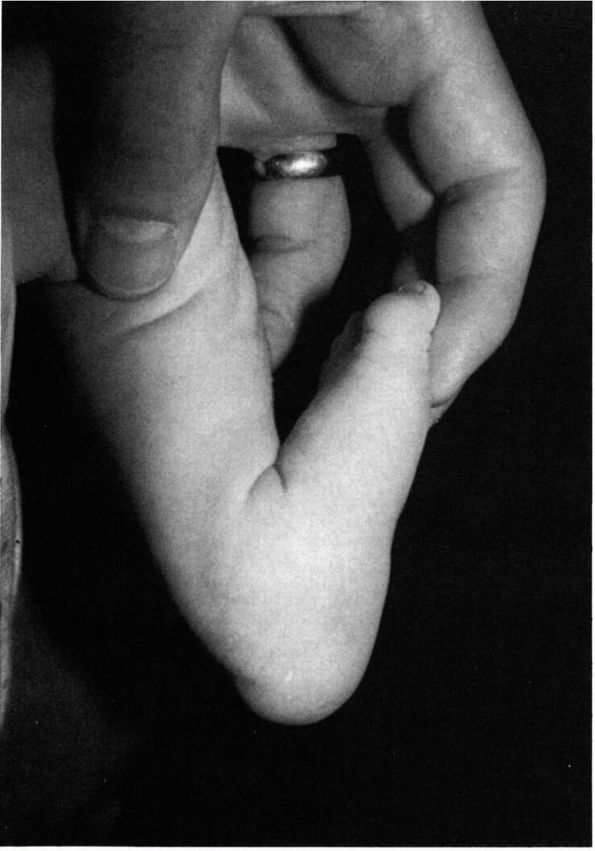
examining the feet in the resting position and by the tiptoe test. The
patient should be examined with legs dangling over the examination
table (see Figure 20-5). In this position, the
physiologic pes planus foot assumes a normal contour to the
longitudinal arch. In the tiptoe test, the patient’s feet are observed
when the patient walks on tiptoes (see Figure 20-5).
In this position, the normal arch is restored, with the heel going to a
neutral or slightly varus position. Muscle strength of the foot should
be normal.
 |
|
FIGURE 20-7.
Physiologic pes planus, standing lateral radiograph. The longitudinal arch is depressed; the talus points directly downward instead of forward in line with the navicular and metatarsals. |
 |
|
FIGURE 20-8. Hypermobile flatfoot associated with short Achilles tendon. Typical appearance is similar to that of physiologic pes planus.
|
This condition, which is often familial, is evidenced by contracture of
the gastrocnemius in association with the same clinical features as
described previously. This condition is usually symptomatic and
associated with long-term disability. These patients can usually
correct the deformity by involuntary muscular effort, as demonstrated
by the patient restoring the arch by standing on tiptoes.
In
addition, in the nonweight-bearing position, the normal arch is
generally present. Contracture of the Achilles tendon is best assessed
with the knee in extension and the talonavicular joint locked in
inversion so that dorsiflexion is measured only at the ankle. The
radiographic features of this condition are characteristic (Figure 20-9).
These patients may also show evidence of hypermobility at the midtarsal
joints, which allows the heel to touch the floor despite a contracted
Achilles tendon. Without treatment, this condition may cause severe
disabling pain.
 |
|
FIGURE 20-9. Hypermobile flatfoot associated with short Achilles tendon. (A) Standing lateral radiographs reveal talus in plantar flexion, calcaneus in equinus indicative of contracted Achilles tendon. (B)
Forced plantar flexion lateral radiograph. The forefoot is collinear with the longitudinal axis of the talus, indicative of passive correctability of this deformity. The patient’s condition resolved with Achilles tendon lengthening. |
pathologic causes of pes planus must be ruled out. These causes include
congenital vertical talus, oblique talus, tarsal coalition, tumor,
foreign body reaction, and Köhler disease of the navicular and
accessory navicular. Accessory navicular bones are seen in about 12% of
the population and are a normal variant. Two patterns are evident. In
one pattern, the accessory navicular is a sesamoid bone within the
posterior tibial tendon (Figure 20-10). It is
anatomically separate from the navicular and usually does not cause
symptoms. In the second form, the accessory navicular is in close
association with the navicular as an ossification center, causing a
change in shape of the navicular. This type may be associated with
pain, particularly during adolescence (Figure 20-11).
Accessory navicular is not a cause of hypermobile flatfoot, but because
both conditions are common, they may present together. Accessory
naviculars may be treated symptomatically, but excision may be required
if conservative measures fail.
 |
|
FIGURE 20-10. Accessory navicular. Note the appearance of sesamoid bone within the posterior tibial tendon.
|
 |
|
FIGURE 20-11.
Accessory navicular. This type of accessory navicular has fused to the primary navicular, altering its shape and leading to prominence of the tuberosity. |
Neuromuscular causes of pes planus, such as cerebral palsy and muscular
dystrophy, can be diagnosed by their typical diagnostic
characteristics. The most severe form of physiologic pes planus is
referred to as an oblique talus because of
its radiologic appearance. It has features similar to vertical talus on
the standing lateral view, but normal alignment is restored on plantar
flexion lateral radiographs. Tarsal coalitions have rigidity of
subtalar motion, may be associated with peroneal spastic flatfoot, and
are diagnosed radiographically (Figures 20-15, 20-16, 20-17 and 20-18).
Other causes of pes planus include the so-called skewfoot or Z-foot
(see metatarsus adductus) and surgically overcorrected clubfeet.
asymptomatic child with a physiologic pes planus. In severe cases,
standing anteroposterior (AP) and lateral radiographs should be
obtained. On the normal standing AP radiograph, the talocalcaneal angle
should be between 15 and 35° (Figure 20-19).
Diversion of the AP talocalcaneal angle to greater than 35° is evidence
of heel valgus. The midtalar line passing medial to the first
metatarsal with the navicular displaced laterally is evidence of
forefoot abduction. On the standing lateral radiograph, the normal
lateral talocalcaneal angle is between 25 and 50°. The talus first
metatarsal angle should be about 0°. On the lateral view, the exact
location of loss of longitudinal arch can be determined. This sag may
occur at the talonavicular joint, first naviculocuneiform joint, and
first metatarsocuneiform joint, or combinations thereof. On the
standing lateral radiograph, the talus is more vertically oriented,
with the metatarsals and the calcaneus in a more horizontal position
than normal because of flattening of the arch (see Figure 20-7).
 |
|
FIGURE 20-12.
Congenital vertical talus. Newborn with sacral agenesis and bilateral congenital vertical talus. The heels are in valgus and the forefoot is abducted. The foot has the characteristic rocker-bottom deformity. |
 |
|
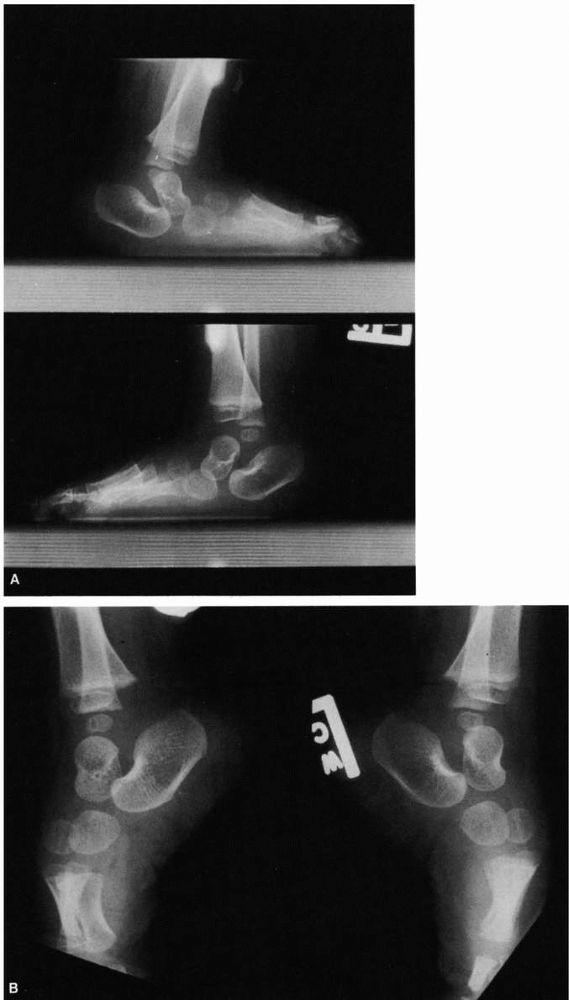
FIGURE 20-13.
Congenital vertical talus of left foot. (Hypermobile flatfoot with contracted Achilles tendon on the right foot.) In the simulated weight-bearing views (upper left and upper right), both feet have the evidence of a rocker-bottom deformity with dorsiflexion occurring at the midfoot, the hindfoot is in equinus, and the forefoot is in dorsiflexion. The talus is more severely plantar flexed on the left than the right. Both calcanea are in equinus, and on the left foot there is disruption of the calcaneal cuboid joint. On the plantar flexion views (bottom), note on the right side the longitudinal axis of the talus is collinear with the forefoot; but on the left (side with congenital vertical talus), the longitudinal axis of the talus is not collinear with the longitudinal axis of the metatarsals, indicative of the rigid nature of the deformity. |
views and Harris views (radiograph taken from behind the foot with the
x-ray beam at a 45° angle) may be helpful in defining a tarsal
coalition or a pathologic process. If tumor, infection, or a stress
fracture is suspected, bone scanning may be helpful. Computed
tomography (CT) is indicated if talocalcaneal tarsal coalition is
suspected (see Figure 20-18). The diagnosis of physiologic pes planus is one of exclusion.
 |
|
FIGURE 20-14. Congenital vertical talus. (A) Standing AP view demonstrates increased angle between talus and calcaneus indicative of the hindfoot valgus. (B) Lateral view of plantar flexion indicates failure of realignment of the metatarsals with the long axis of the talus. (C) Postsurgical realignment of forefoot, midfoot, and hindfoot. (D and E) Standing PA and lateral radiographs 6 years after operation demonstrating restoration of normal anatomic relations.
|
unfortunately clouded by medical and nonmedical mythology. To most
parents and many physicians and paramedical personnel, flatfeet are
considered
a significant health problem. Unfortunately, good natural history data on this condition are lacking.
 |
|
FIGURE 20-14. (Continued)
|
assumption that patients will have problems in the future if the
condition is not treated. In normal children, aged 1 to 3 years, whose
parents bring them in for concerns over flatfeet, reassurance and
explanation of the cause of pes planus are essential. The parents
should be informed about the presence of the normal fat pad, the normal
hyperlaxity of
infancy,
the often familial nature of the condition. They should also be
reassured that, in most children, an arch will develop by 5 years of
age. The parents should be informed of the benign natural history of
the condition. Appropriate literature should be supplied to the family
so they can reassure themselves and other family members who may expect
some treatment because of what they have heard from others, what they
have read, or treatment they underwent as children. Many parents are
under the false assumption that so-called corrective shoes are
responsible for the natural development of the longitudinal arch.
 |
|
FIGURE 20-15. Calcaneal navicular coalition. Forty-five-degree oblique view demonstrates calcaneal navicular coalitions.
|
children with the diagnosis of physiologic pes planus. The educational
aspects of the natural history of the condition cannot be
overemphasized. The parents should be instructed that treatment
modalities offered in the past were offered without any scientific
basis. A recent prospective randomized study of patients with flexible
flatfeet treated by corrective shoes and inserts revealed that all
patients improved moderately after 3 years of treatment, and no greater
improvement was seen in patients who were treated vigorously, even
those treated with custom-made inserts. All treatments in the past,
including exercises, varying shoe modifications, and inserts, have been proved to be ineffective.
 |
|
FIGURE 20-16.
Calcaneal navicular coalition. In a patient with calcaneal navicular bar, standing lateral radiograph demonstrates prominence of the anterior process of the calcaneus and a spur at the superior talonavicular articulation. |
 |
|
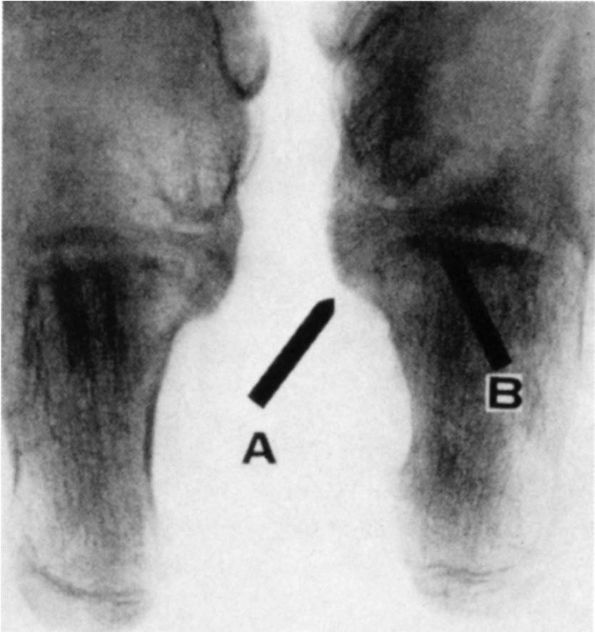
FIGURE 20-17. A talocalcaneal bridge. Harris views of both feet. Note the prominence of the sustentaculum (arrow A); talocalcaneal articulation is obliterated in the medial portion (arrow B).
|
 |
|
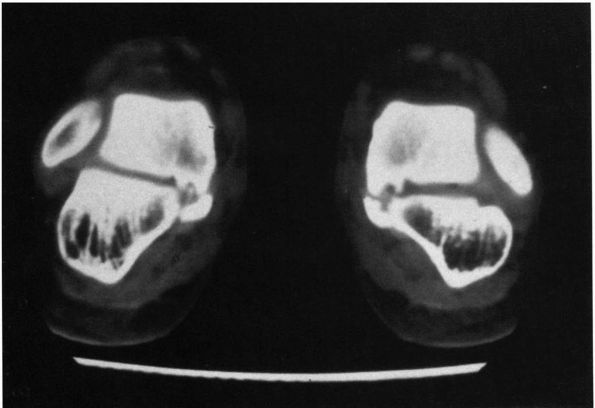
FIGURE 20-18. Talocalcaneal coalition. Frontal section of a CT scan demonstrates tarsal coalition at middle facet joint.
|
diagnosis must be reassessed and sources of painful flatfeet
eliminated. Prophylactic treatment of any type is unwarranted.
Treatment for flexible flatfeet is only indicated if the patient
presents with pain, usually in the foot or calf, or if the patient has
severe excessive shoe wear. The discomfort in the foot and the
associated leg aches, which occur in about 15 to 30% of normal people,
should be treated symptomatically with acetaminophen, local heat, and
massage. If fatigue symptoms or discomfort with increasing activity
persists, shoe modifications can be considered. It is important to
emphasize that these modifications are not corrective. High-top tennis
shoes with a good longitudinal arch can usually be recommended. If
symptoms persist, other noncorrective adaptive measures may be tried,
such as a medial heel wedge, a long shoe counter, or a navicular pad.
that fails to respond to conservative measures, a more formal shoe
orthotic, such as a University of California Biomechanics Lab insert or
custom-made insert, may distribute body weight more evenly across the
sole of the foot and take the pressure off the prominent talar head.
These modalities, however, are expensive, must be changed frequently
with foot growth, and have no scientific basis for their use. The use
of shoe modification inserts tends to label the child as having a
problem. The use of these devices to appease parents or grandparents
should be discouraged.
tendo Achilles, heel cord stretching exercises should be instituted. If
symptoms develop or the contracture persists, tendo Achilles
lengthening can be considered. The only operative indications in true
physiologic pes planus flatfoot are severe malalignment problems
causing excessive abnormal shoe wear or pain. Achilles tendon
stretching or casting may be of some benefit. Surgical options for
these indications are rarely indicated. In the past, these options
included soft tissue procedures alone; arthrodeses of the various
tarsal joints; osteotomies; and combined osteotomies, arthrodeses, and
soft tissue procedures, all with the goal of restoring the normal
longitudinal arch, relieving pain, and preserving as much motion as
possible. Results of these procedures have been poor.
because of the high association with contracture of the peroneal
tendons. The most common sites of coalition are between the calcaneus
and the navicular and between the talus and calcaneus. The most common
talocalcaneal coalition is
between
the sustentaculum and the talus, with rare coalitions involving the
anterior or posterior facet. Other tarsal coalitions are much less
common. The coalitions may be complete or partial. When the coalition
is fibrous, it is called a syndesmosis. When the coalition is cartilaginous, it is referred to as synchondroses. A bony union is referred to as a synostosis. Tarsal coalition represents the most common nonneuromuscular cause of pathologic pes planus.
 |
|
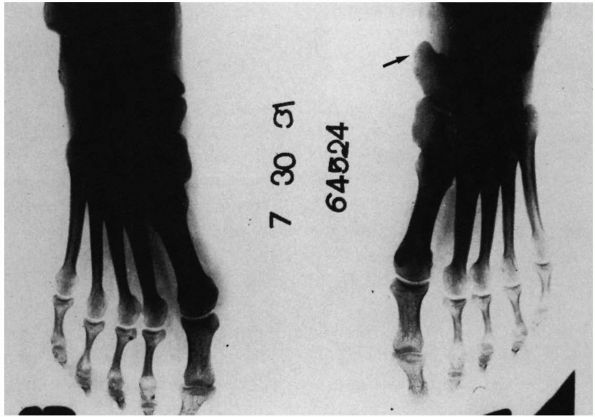
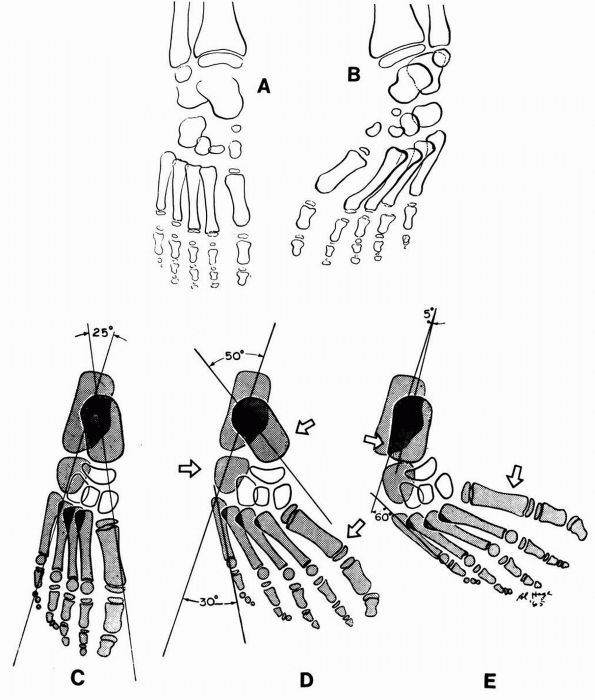
FIGURE 20-19. Congenital metatarsus varus. (A)
The talus, the scaphoid, the first cuneiform, and the first metatarsal form a straight line. The anterior ends of the talus and the calcaneus are separated. (B) The first metatarsal is carried medially and is in line only with the inner cuneiform and the scaphoid, the latter lying lateral to the talar head. The talus and the calcaneus are in the flatfoot position, the anterior ends lying in a divergent relationship. The inversion of the forefoot causes the cuneiforms to overlap and the lateral aspect of the metatarsals to be visualized. The metatarsals normally are bowed dorsalward, and in this view they are wrongly identified as deformed. (C) Diagram of radiograph of a normal foot; (D) a foot with metatarsus adductus; and (E) a clubfoot. Arrows indicate directions and sites of molding during corrective manipulation and plaster-cast application. (Ponseti IV, Becker JR. Congenital metatarsus adductus. J Bone Joint Surg 1966;48A:702) |
estimated, however, that less than 1 to 2% of the population is
affected. Although tarsal coalitions may be multiple, rarely is there
more than one coalition per foot. Bilateralness, however, is common.
support to the theory of failure of segmentation as the origins of
tarsal coalitions (Figure 20-20). This
incomplete segmentation of the mesenchymal anlage of the tarsal bones
gives rise to the fibrous or cartilaginous coalition, which may ossify
later in life. Bilateralness has been reported in up to 70% of
calcaneonavicular coalitions and in 20 to 50% of talocalcaneal
coalitions. Tarsal coalitions are thought to be an inherited condition,
with the most widely accepted pattern being autosomal dominant
inheritance with variable penetrance.
population is unknown, the natural history is uncertain. It is apparent
that many patients with tarsal coalitions have no symptoms, and many
patients with coalitions treated symptomatically can go well into adult
life without persistent pain or disability. Symptoms most commonly
develop when the coalition begins to ossify. Ossification of the
coalition restricts subtalar motion. This alteration in subtalar
mechanics leads to increased stress at adjacent joints, particularly
the ankle and talonavicular joints. If a coalition remains fibrous
(syndesmosis), symptoms may never develop because of the mobility
allowed through the syndesmosis. With increasing ossification of a
cartilaginous (synchondrosis) coalition, decreased mobility ensues,
increasing the likelihood of the patient developing clinical symptoms.
The altered subtalar joint mechanics over time may lead to degenerative
joint disease in adjacent joints, causing persistent pain and
disability. The limited subtalar motion also causes increased laxity in
adjacent joints, particularly the ankle joint, leading to increased
incidence of sprains and secondary joint alterations.
 |
|
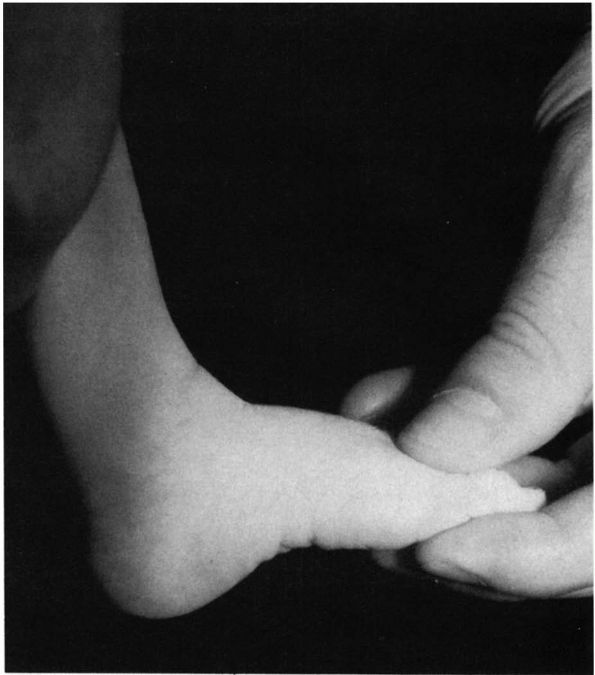
FIGURE 20-20. Tarsal coalition. Fetal specimen demonstrating fibrous tarsal coalition between calcaneus and navicular.
|
during the second decade of life with pain or decreased subtalar
motion. Occasionally, the patient complains of a limp, discomfort in
the calf region, or nonspecific foot pain. The pain is often localized
to the anterior, medial, or lateral aspect of the subtalar joint or to
the talonavicular region. The onset of pain is usually insidious or
associated with a traumatic event such as a nonresolving ankle sprain.
Pain is usually made worse by activities like running and jumping or
prolonged standing; it is usually relieved by rest. The symptom onset
depends on the nature of the coalition (fibrous, cartilaginous, or
bony) and the specific joint involved. Children with the rare
talonavicular coalition may present between 2 and 4 years of age.
Typically, patients with calcaneonavicular coalitions present between 8
and 12 years of age, and those with talocalcaneal coalitions between 12
and 14 years of age. In any child presenting with a painful rigid foot,
tarsal coalition must be ruled out.
 |
|
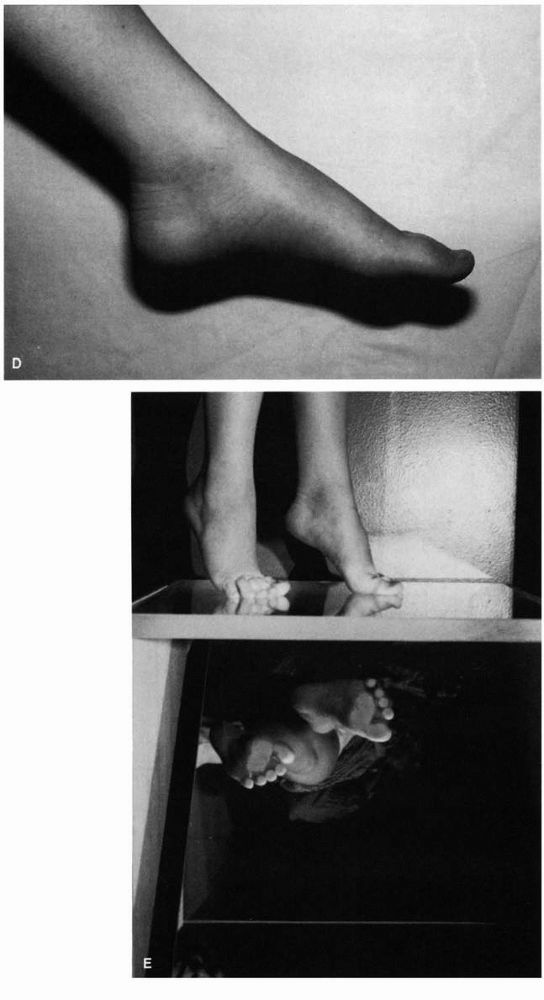
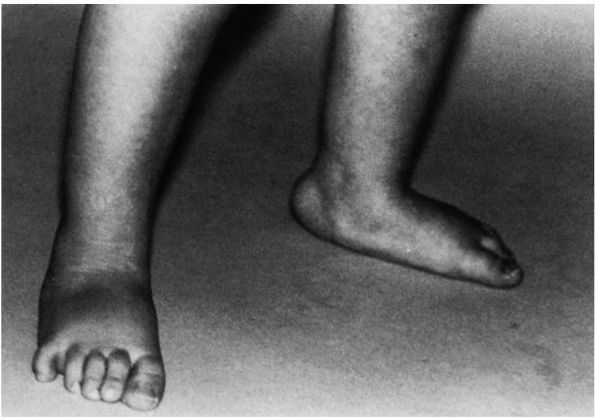
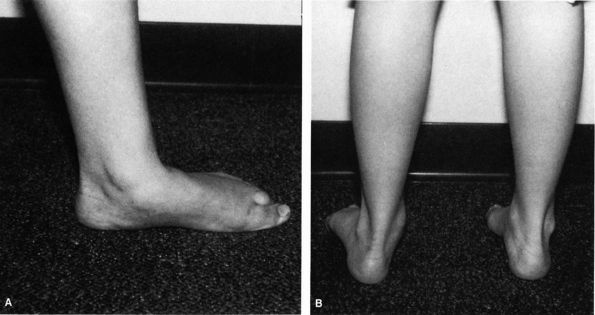
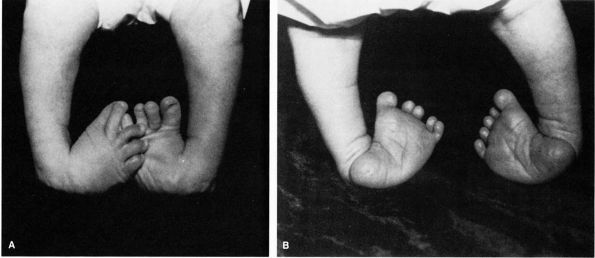
FIGURE 20-21. Tarsal coalition. Note the position of the involved left foot with the forefoot in abduction (A) and heel in valgus (B). Also note the loss of the longitudinal arch.
|
generally reveals decreased hindfoot or midfoot motion, or both. Most
commonly, the heel is in valgus and the forefoot in abduction (Figure 20-21).
The patient may walk with an antalgic gait, and if symptoms are
long-standing and the pain is significant, disuse atrophy may be noted
on calf measurements. In about half of cases, contractures of the
peroneal muscles is present. This is evidenced by prominence of the
peroneal tendons in the lateral aspect of the ankle and foot (Figure 20-22). Attempt at inversion of the deformity causes pain and discomfort along the peroneal region (Figure 20-23).
The peroneal tendons are contracted secondary to prolonged positioning
of the foot in valgus. True muscle spasms of the peroneal tendons are
rare. Increased ankle ligamentous laxity is most commonly seen in
patients with long-standing symptoms, particularly those with
talocalcaneal coalitions. There may also be varying degrees of loss of
the longitudinal arch. Pathologic conditions affecting the subtalar
joint, including tumors, rheumatoid arthritis, and traumatic injuries,
may mimic the physical findings of tarsal coalition.
The diagnosis of a calcaneonavicular coalition can usually be made on
these standard radiographs. The 45° medial oblique radiograph usually
demonstrates this coalition. If the coalition is fibrous or
cartilaginous, however, it may not be obvious on plain radiographs.
Other findings that indicate a possible calcaneonavicular coalition
include elongation at the anterior portion of the calcaneus to a point
of close proximity to the navicular and irregular, sclerotic
margins of the two bones in close approximation (see Figure 20-16).
 |
|
FIGURE 20-22.
Tarsal coalition. Note prominence of the perineal tendons on the lateral aspect of the ankle because of prolonged positioning of the hindfoot in valgus and forefoot in abduction. |
 |
|
FIGURE 20-23.
Tarsal coalition. There is inability to supinate the involved right foot secondary to tarsal coalition with restricted subtalar motion. |
coalitions were often difficult to diagnose. In suspected talocalcaneal
coalitions, Harris views taken from behind the foot at an angle 45°
from the horizontal demonstrate the posterior and medial facets of the
subtalar joint. Normally, these are parallel, but coalitions may be
diagnosed by the loss of the parallel orientation between the two
facets, presence of fusion, or irregular or sclerotic surfaces (see Figure 20-17).
Other types of tomography also have been used to demonstrate
talocalcaneal coalitions; however, CT is the diagnostic method of
choice for demonstrating these coalitions. Coronal sections should be
obtained to document the coalition (see Figure 20-18).
These sections not only document the presence of the coalition but also
clearly define its extent. CT scans are most helpful in planning
surgical management of this condition.
subtalar mechanics may be evident radiographically by secondary
adaptive changes. These changes include dorsal beaking or lipping at
the head or neck of the talus (see Figure 20-16).
This is secondary to stretching of the talonavicular ligaments because
of the navicular impinging on the head of the talus. The lateral aspect
of the talus may appear broadened, with the undersurface of the talar
neck having a concave appearance. There may be apparent narrowing of
the posterior talocalcaneal joint space and inability to determine the
definition of the middle talocalcaneal articulation.
apparent ball-and-socket ankle—manifest by convexity of the dome of the
talus on both the AP and lateral views. In patients presenting with
repeated ankle sprains and radiographic evidence of a ball-and-socket
ankle, tarsal coalition should be sought. In these cases, the
radiographic changes at the ankle joint are secondary to long-standing
ankle instability and adaptive changes of the tibial talar articulation.
should be nonoperative because the natural history indicates that many
patients have no symptoms, and the literature review of various
treatment programs indicates some success with nonoperative treatment.
Nonoperative treatment measures are based on immobilizing the subtalar
joint. Shoe orthotics, ankle-foot orthoses, nonsteroidal
anti-inflammatory agents, and activity restriction may be tried as a
first line of treatment. If these fail, a period of cast immobilization
with a short-leg walking cast for 3 to 6 weeks should be tried. If
symptoms recur or are not alleviated by conservative measures, surgical
excision is indicated. The most commonly used surgical technique is
wide excision of the bar and interposition of either extensor digitorum
brevis tendons or fat. Patients are immobilized in a cast for about 7
to 10 days, followed by range of motion exercise and protected weight
bearing. Full weight bearing is allowed in 4 to 6 weeks. The main
indication for surgery is pain relief, not restoration of joint motion,
although with calcaneonavicular bar excisions, restoration and
maintenance of joint motion can be expected if the patient does not
have secondary degenerative joint disease changes. If symptoms persist
and secondary degenerative joint disease is present in the adjacent
joints, triple arthrodesis remains the only option for relief of the
patient’s symptoms. Success rates of surgery in calcaneonavicular
coalitions are best in young patients
with
cartilaginous bars and no evidence of degenerative joint disease at the
talonavicular joint. Talar beaking is not a contraindication for
surgery because it does not necessarily represent degenerative changes.
more difficult. Usual treatment should center around nonoperative
measures as indicated previously for calcaneonavicular coalitions. If
these nonoperative measures fail to provide lasting relief of the
patient’s symptoms, resection of the coalition with interposition of
fat or bone wax should be considered. Specific criteria for
resectability of these coalitions are lacking. Long-term series with
large numbers of patients are unavailable. Contraindications to
resection, however, are an extensive coalition and degenerative joint
disease at the adjacent joints. In these circumstances, subtalar fusion
or triple arthrodesis should be considered. The most common cause of
failure in surgical management of tarsal coalitions is incomplete
resection.
foot. It is characterized by a rigid flatfoot deformity, with the
plantar aspect of the foot having a convex contour. The heel is in
valgus, and the forefoot is abducted (see Figure 20-12). This entity has also been called congenital convex pes planus, congenital convex pes valgus, and congenital flatfoot with talonavicular dislocation. All these terms are descriptive either of the clinical or radiographic appearance of the foot.
usually associated with other congenital abnormalities, musculoskeletal
defects, or disorders of the central nervous system. There is a high
incidence of congenital vertical talus in children with
myelomeningocele (10% having congenital vertical talus), congenital hip
dysplasia, and several trisomies (13 to 15%, 18%). This entity is more
common in boys than girls, and there appears to be a familial tendency.
It may be bilateral, but if unilateral, it may be associated with a
pathologic condition of the opposite foot, including clubfoot,
metatarsus adductus, or calcaneal valgus deformity.
involved foot is usually smaller than the opposite side with decreased
circumference of the calf. In the newborn, the dorsal aspect of the
foot may be in close approximation to the distal aspect of the tibia,
similar to the foot position in the calcaneal valgus deformity. Unlike
calcaneal valgus, however, this position is rigid, and the foot cannot
be flexed in a plantar direction. The sole of the foot has a convex
appearance, the rocker-bottom deformity. The hindfoot is in the
equinovalgus position with the Achilles tendon contracted. The forefoot
is in the abducted dorsiflexed position. The head of the talus is
easily palpable on the plantar medial aspect of the foot at the apex of
the foot convexity. The deformity is rigid; it cannot be manipulated
into the normal position. The head of the talus is covered
dorsolaterally by the displaced navicular. Attempts at manipulation
fail to reduce the talonavicular joint. The clinical appearance may
mimic a hypermobile flatfoot or calcaneal valgus deformity. In both
these conditions, however, normal relations, particularly the
talonavicular relation, can be restored by plantar flexion.
radiographs should be obtained. Standing or simulated standing lateral
radiographs reveal the calcaneus to be in equinus and talus to be
vertically oriented parallel to the long axis of the tibia (see Figure 20-13).
Because of the extreme plantar flexion of the talus, only the posterior
aspect of dome articulates with the distal aspect of the tibia. In
children younger than 3 to 5 years of age, the navicular is not
ossified, and hence the talonavicular dislocation can only be inferred
by noting that the forefoot is displaced dorsally in relation to the
talus. Occasionally, a concave depression may be noted on the talar
neck induced by the dorsolateral subluxation of the navicular. Once the
navicular is ossified, the talonavicular dislocation is easily
demonstrated. Radiographs may also demonstrate disruption of the
calcaneocuboid joint with dorsolateral displacement of the cuboid. The
diagnosis can be confirmed radiographically by a forced plantar flexion
lateral view.
are not restored on the plantar flexion lateral view. The long axis of
the talus is plantar to the cuboid, as opposed to dorsal, and the long
axis of the metatarsals cannot be brought into collinear alignment with
the long axis of the talus (see Figure 20-13).
vertical talus confirm the anatomic distortions evident by the clinical
and radiographic presentation. The specimens reported are similar in
their clinical features, all demonstrating hindfoot valgus, equinus
deformity, and the dorsolateral subluxation of the navicular on the
talus. The talus itself may be hypoplastic with a facet joint on the
dorsal neck at the point of articulation with the
navicular.
The sustentaculum talus is hypoplastic and the anterior facet joint
absent. The peroneal and posterior tibialis tendons are displaced
dorsally, resulting in muscle imbalance. The cause of this condition is
unknown.
not only on the foot deformity but also on any associated
musculoskeletal or central nervous system disorder. In general, without
treatment the ambulatory patient develops significant callosities over
the head of the talus. This results in pain and skin breakdown over the
talar head. The gait of these children is awkward, and shoeing may be a
significant problem.
whether associated conditions are present. In the isolated deformity,
surgical correction is almost always necessary. The foot should be
manipulated to try to stretch the dorsolateral soft tissues. The
manipulations are followed by casting with a long-leg cast changed at
weekly intervals. The purpose of the manipulation and casting is to
stretch the dorsolateral constricted soft tissues to minimize surgical
complications, particularly skin necrosis. Manipulation and casting
should be begun immediately at birth and continued for 6 to 10 weeks.
Surgical correction is then performed either as a single or multistage
procedure. The surgical correction involves lengthening the contracted
dorsolateral structures, reducing the talonavicular or calcaneocuboid
(or both) joint subluxations, and correcting of the equinus deformity
through a posterior capsulotomy of the ankle and subtalar joint and
Achilles tendon lengthening. Reinforcement of the soft tissue
structures on the plantar aspect of the navicular by use of the
posterior tibial tendon is generally indicated (see Figure 20-14).
In older children (over 2.5 years of age), surgical correction is often
accompanied by an extra-articular subtalar arthrodesis at the time of
surgical correction or as an adjunctive procedure at a later time.
Surgical corrections are aimed at restoring normal bony alignment and
muscle balance. Complication rates of surgery are high and include
aseptic necrosis of the talus, loss of reduction, and stiffness,
particularly of the subtalar joint. Success rates are better in
children treated surgically when younger than 1 year of age. Tendon
transfers may be needed at a later date to restore muscle balance. In
the adolescent or adult with untreated or recurrent congenital vertical
talus, triple arthrodesis may be the only way to restore normal bony
alignment.
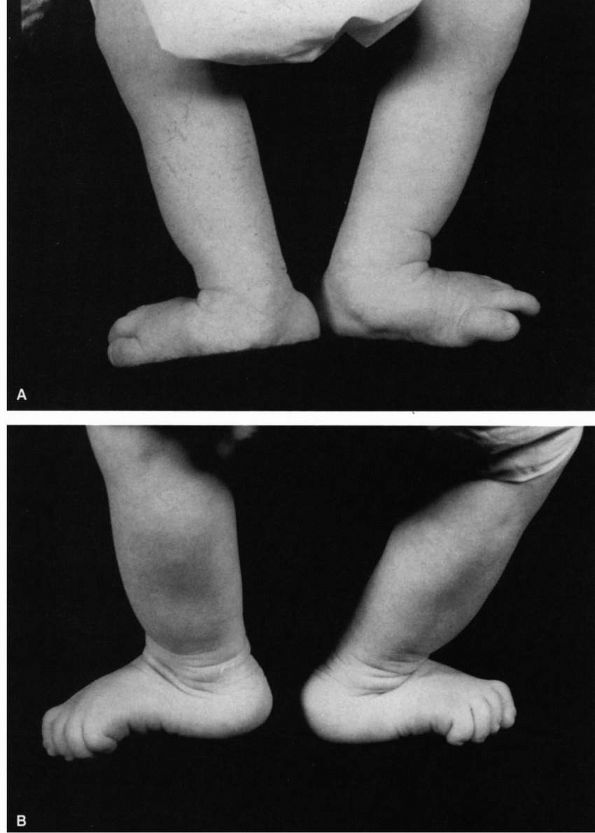
calcaneal valgus, congenital talipes calcaneal valgus) is one of the
most common foot deformities seen at birth. The entire foot is held in
the dorsiflexed everted position, and in its most severe form, the foot
lies adjacent to the anterior border of the tibia (Figure 20-24).
Calcaneal valgus is thought to be secondary to intrauterine molding. It
is most common in firstborn children and in children of young mothers.
It has a female predominance of 1:0.6 and is estimated to occur in 1 of
every 1,000 live births.
tibia with the forefoot in varying degrees of abduction and the heel in
varying degrees of valgus. The peroneal tendons may be subluxated
anterior to the lateral malleolus. The soft tissues on the dorsal and
lateral aspect of the foot are contracted and restrict plantar flexion
and inversion. There may be
a
transverse crease just distal to the ankle joint on the dorsal aspect
of the foot. The foot can generally be manipulated to neutral or just
short of the neutral position and, occasionally in mild cases, just
beyond this position (Figure 20-25).
The deformity may be accompanied by a mild abduction of the forefoot in
varying degrees of heel valgus. There is an occasional association of
this deformity with external rotation contractures in the hip and with
other conditions thought to be secondary to intrauterine molding
deformities (e.g., congenital hip dysplasia and torticollis).
 |
|
FIGURE 20-24. Calcaneal valgus deformity. There is close approximation of the dorsum of the foot to the anterior aspect of the distal tibia.
|
calcaneal valgus deformity, such as myelomeningocele and
arthrogryposis, as well as congenital vertical talus. In congenital
vertical talus, the Achilles tendon is contracted, the hindfoot is in
equinus, and there is a rocker-bottom deformity. Half the cases of
vertical talus are associated with a neuromuscular deformity. All cases
of posteromedial bowing of the tibia are associated with a calcaneal
valgus deformity of the foot.
pes calcaneal valgus. The foot can be palpated to show normal alignment
with no subluxation at the talonavicular joint. Radiographs are only
necessary when the diagnosis is in question. It is important to
stimulate the foot to make certain that the plantar flexors are present.
 |
|
FIGURE 20-25. Calcaneal valgus deformity. The foot can easily be manipulated to or just short of the neutral position.
|
spontaneous correction. Persistence of some of the deformity may lead
to a flexible flatfoot. Casting is rarely necessary. Treatment should
be directed at instructing the parents in stretching exercises. The
foot should be gently manipulated into plantar flexion and inversion.
In general, the deformity is corrected by 2 to 4 months of age. If it
is persistent, however, manipulation and casting can be considered.
tarsal navicular. It is a self-limited condition characterized by pain
or swelling in the area of the tarsal navicular in association with
certain radiographic features. It occurs in the age range of 4 to 7
years, with 80% of cases occurring in boys. One-fourth to one-third of
cases are bilateral.
thought to be related to repetitive trauma and interruption of blood
supply to the tarsal navicular. The tarsal navicular is the last bone
of the foot to ossify. The appearance of the ossification center varies
and is gender related. In girls, the tarsal navicular ossifies between
18 months and 2 years of age. In boys, the ossification occurs between
2.5 and 3 years of age. The normal ossification center has a smooth
contour and uniform density. In otherwise normal children who have
delay in appearance of the ossification center of the navicular,
however, it may appear flat or fragmented with multiple ossification
centers of increased density and irregular contour. Several
ossification centers may eventually coalesce to form the navicular.
Postmortem studies of the navicular in children reveal that the blood
supply is tenuous, being supplied by only a single vessel until age 6
years.
female) in whom ossification is delayed. The pathogenesis may be
secondary to traumatic interruption of the vasculature to the tarsal
navicular at a crucial stage in ossification.
complaints of pain and tenderness to palpation over the tarsal
navicular. Localized swelling is occasionally evident. There may be
palpable thickening of the soft tissues around the tarsal navicular.
Many affected children walk with an antalgic gait and bear
weight
on the lateral aspect of the foot to avoid pressure over the medial
aspect and the tarsal navicular. Active and passive range of motion are
normal.
On the standing lateral view, the navicular has a decreased AP diameter
with evidence of varying amounts of flattening. Multiple centers of
ossification may be present. As mentioned previously, these
radiographic features may be a normal variation in as many as one-third
of children, particularly those who have late-onset ossification.
Therefore, the diagnosis of Köhler disease is made only with the
combination of the clinical signs, symptoms, and the radiographic
features.
radiographic changes in the opposite navicular and be totally
asymptomatic. In the normal child, the radiographic appearance is
assumed to be secondary to coalescence of multiple ossification
centers, while in the child with Köhler disease, the radiographic
features represent the changes of avascular necrosis, with invasion by
granulation tissue, resorption of necrotic trabeculae, and deposition
of new bone.
benign. No long-term disabilities have been reported in patients who
have Köhler disease despite lack of treatment. In most cases, the
navicular assumes a relatively normal appearance within 1 to 3 years
after symptom onset.
 |
|
FIGURE 20-26. Köhler disease or osteochondrosis of the tarsal navicular.
|
symptoms and not to hasten the reparative process. Treatment for Köhler
disease is nonsurgical and depends on the magnitude of symptoms. In
patients with mild symptoms, restriction of activities may be all that
is necessary. In children with more severe symptoms, a longitudinal
arch support can be considered to more evenly distribute the patient’s
body weight in weight bearing. These measures, in conjunction with
avoidance of strenuous activities such as jumping and running, usually
relieve symptoms. In patients with more severe symptoms, immobilization
in a short-leg cast for 3 to 4 weeks usually provides good relief of
symptoms. The patient may need to use crutches with touch weight
bearing for a short time but then may bear full weight on the cast as
long as symptoms do not recur. Cast treatment should be continued until
the patient is asymptomatic. In severe cases, the use of a short-leg
walking cast improves the natural history of symptoms dramatically but
has no effect on the radiographic course of the disease. Without
treatment, most patients have intermittent symptoms for 1 to 3 years
that is activity related and relieved by rest.
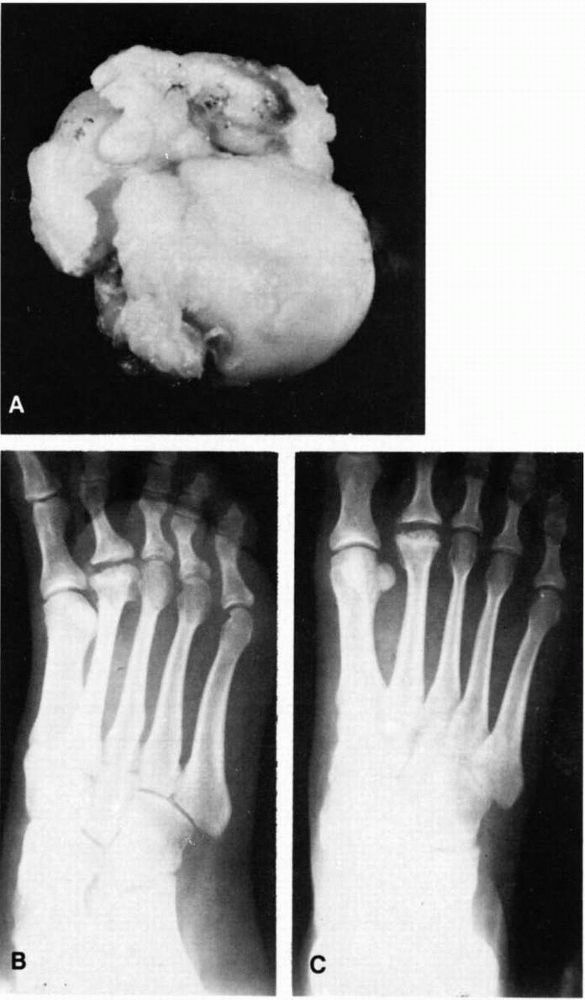
Specifically, it is an aseptic necrosis of the metatarsal head.
Three-fourths of cases occur in girls, and the second metatarsal head
is the most commonly involved, although the disease may affect the
third or fourth metatarsal head. Freiberg disease rarely occurs before
the age of 13 or 14 years.
thought to be similar to that of osteochondritis dissecans of the knee.
The second metatarsal is the longest and the most rigid metatarsal. It
is subjected to the greatest amount of stress in walking. Freiberg
infarction is sometimes seen with an accompanying stress fracture of
the metatarsal.
around the second metatarsophalangeal joint. They may complain of
stiffness and have a limp secondary to the pain. On physical
examination, the discomfort is well localized. There may be palpable
swelling at the second metatarsophalangeal joint. Pain may be elicited
on passive range of motion.
Motion
may be limited and painful. The history may be one of exacerbations and
remissions, with pain aggravated by activity and relieved by rest.
flattened, enlarged appearance with areas of increased sclerosis and
fragmentation. The affected metatarsophalangeal joint may be narrowed,
and in long-standing disease, secondary degenerative changes may be
evident (Figure 20-27).
In many cases, the condition is self-limited, with revascularization of
the affected metatarsal head. The disease process may leave the
metatarsal head deformed. Many patients have no pain or discomfort and
good range of motion. In some cases, however, the disease course
involves exacerbations and remissions. Significant deformity may ensue,
and secondary degenerative changes may occur at the metatarsophalangeal
joint.
 |
|
FIGURE 20-27. Freiberg infarction (osteochondrosis of the metatarsal head). (A)
Frontal view of the resected metatarsal head. The articular cartilage is irregular with areas of loss of articular surface. There are multiple indentations about the head. The capsule about the periphery is thickened, and secondary osteoarthritic spurs are present. A cleft at the margin suggests formation of a loose body by separation. (B and C) Radiographs of the second metatarsal head before resection showing sclerosis, irregularity, widening, and spurring with flattening. |
aseptic necrosis. Initial treatment should be symptomatic. Symptomatic
treatment includes decreasing activities and using metatarsal pads
inserted in the shoe or metatarsal bars on the sole of the shoe. These
two measures are designed to allow for weight bearing on the metatarsal
neck as opposed to the metatarsal head to decrease the stresses applied
to the metatarsal head. In patients who have more acute symptoms, a
short-leg walking cast with or without crutches may provide relief. If
the joint is free of degenerative changes and symptoms persist, removal
of the necrotic fragment alone may provide symptomatic relief. A foot
orthosis designed to provide pressure relief over the second metatarsal
head may be used on a long-term basis once the acute symptoms have
subsided or after surgical removal of the necrotic segment. Mild
symptoms may be treated by an orthosis alone.
nonoperative treatment, surgical treatment may be offered. This may
include removal of the loose fragment and resection of the base of the
proximal phalanx. Alternatively, resection of the metatarsophalangeal
joint may be required, with syndactylization of the second and third
toe to avoid significant shortening that may follow resection of the
metatarsophalangeal joint. This usually provides good relief of
symptoms.
most common overuse syndromes seen in growing children. It most
commonly occurs in the age range of 6 to 12 years and is thought to be
due to repeated microtrauma. Most affected children are extremely
active. This condition may thus represent chronic strain at the
insertion of the tendo Achilles.
over the posterior aspect of the calcaneus. Physical examination
reveals tenderness to compression over the calcaneal apophysis.
Symptoms may cause discomfort with passive ankle dorsiflexion. The
condition must be differentiated from other sources of heel pain in
young children (Table 20-1).
3 to 8.5 years) and 7.9 years of age in boys (range, 6 to 10 years). In
many normal children, the calcaneal apophysis may appear fragmented and
then coalesce from two to three separate ossification centers. This
normal ossification variant, in combination with symptomatology, is
considered diagnostic of Sever disease (Figure 20-28).
If patients have bilateral symptoms, radiographs are often not
necessary. In unilateral cases, however, radiographs of both feet
should be obtained to rule out other causes of heel pain, such as
retrocalcaneal bursitis, stress fractures, infection, rheumatologic
conditions, and neoplastic lesions.
|
TABLE 20-1. Sources of Heel Pain in Childhood
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
severe symptoms, activity restriction may be necessary. If this alone
does not relieve symptoms or if symptoms are acute, a short-leg walking
cast may be applied for 3 to 4 weeks. This usually is adequate to
curtail symptoms. Longer periods of casting or activity restriction of
up to 1 to 3 months may be necessary in some cases. No long-term
disability or deformity has been reported from Sever disease.
adductus, metatarsus varus, skew foot, serpentine foot, pes adductus,
metatarsus adductovarus, hooked forefoot, metatarsus internus, and congenital metatarsus varus.
These terms unfortunately are used inconsistently throughout the
medical literature. The two most widely used terms are metatarsus
adductus and metatarsus varus, which describe slightly different
forefoot variations but are synonymous. In this condition, the forefoot
is generally adducted and occasionally inverted (varus) at the
tarsometatarsal joint, and the hindfoot is generally neutral to valgus (Figure 20-29; see Figure 20-19).
Metatarsus adductus is present at birth but often is overlooked by the
family until the child is between 3 months and 1 year of age.
deformity. Its incidence is 1 in 1,000 live births. It has a female
predominance of 4:3 and a 5% incidence of the condition in first-degree
relatives. There is no known pattern of inheritance, but the risk of a
second sibling being affected is 1 in 20. Two-thirds of patients have
involvement of both feet. There is a strong association between
metatarsus adductus and congenital hip dysplasia and dislocation.
thought to be secondary to intrauterine molding because 59% of patients
are firstborn children. Other etiologic theories include peroneal
muscle weakness with overactive anterior tibialis and posterior
tibialis; abnormal insertion of the tibialis posterior tendons on the
first cuneiform rather than their usual site on the navicular; and
posture habits caused by prone, sleeping with the buttocks elevated,
hips
and knees in complete flexion, feet adducted and tucked beneath the
buttocks, and sitting on the adducted feet. Persistent soft tissue
contractures may lead to secondary tarsal changes, making the deformity
rigid with time.
 |
|
FIGURE 20-28. Severe disease of the calcaneal apophysis. (A) Standing lateral radiograph. (B)
Calcaneal views. Note sclerotic fragmented appearance of the right symptomatic calcaneus as opposed to the sclerotic semifragmented appearance of the asymptomatic left side. (Ponseti IV, Becker JR. Congenital metatarsus adductus. J Bone Joint Surg 1966; 48A:702) |
usually not noticed by the parents until the child begins to crawl or
walk. Occasionally, patients present to a physician in the toddler
years when the parents complain of the child in-toeing or having
difficulty wearing shoes. On physical examination, all the metatarsals
are adducted and the forefoot is occasionally in varus (see Figure 20-29).
The heel is in neutral to slight valgus. The great toe is often widely
separated from the second toe, and the base of the fifth metatarsal and
the cuboid are prominent on the lateral aspect of the foot. The medial
border of the foot is concave, and the lateral border is convex. Medial
tibial torsion often accompanies metatarsus adductus. The Achilles
tendon is not tight, and the foot can be fully dorsiflexed at the ankle
joint. The deformity is often accentuated by overactivity in the
abductor hallucis and the short toe flexors.
moderate, or severe, depending on whether the forefoot can be passively
corrected to neutral or to an overcorrected position. Severe
deformities are rigid and not passively correctable. The ratio of
supple to rigid deformity is about 10:1. The term serpentine foot is often used for a rigid adducted forefoot with an accompanying heel valgus.
a mild deformity, the bisector passes through the third toe; in a
moderate deformity, it passes between the third and fourth toes or just
the fourth toe; and in a severe deformity, the heel bisector passes
between the fourth and fifth toes. The deformity is said to be flexible
or passively correctable if the forefoot (second toe) can be passively
abducted beyond the heel bisector (see Figure 20-29).
Many patients exhibit dynamic hallux varus, whereby the great toe
deviates medially during stance phase but the metatarsals are normally
aligned.
 |
|
FIGURE 20-29. (A)
Thirteen-month-old boy with bilateral metatarsus adductus. The left foot is abducted and the right forefoot is adducted and in slight varus. The heel bisector is at the fourth toe on the left foot and between the third and fourth toes on the right foot. (B) Note passive correctability of deformity. Forefoot can be passively abducted beyond the heel bisector. |
metatarsus adductus. Radiographs can, however, document deformity and
are used by some to classify the deformity. Radiographs, if taken,
should be in the standing position or with the foot resting in a
simulated standing position on the radiograph cassette. Radiographs
demonstrate sharp medial angulation of the tarsometatarsal joints, with
the first metatarsal being more severely adducted than the fifth (see Figure 20-19).
Normally, a line drawn through the longitudinal axis of the first
metatarsal is parallel or diverges laterally from a line drawn through
the longitudinal axis of the talus. In metatarsus adductus, the first
metatarsal line falls medial to the talar line. In the weight-bearing
or simulated weight-bearing film, the calcaneal line should bisect the
cuboid and the base of the fourth metatarsal. In metatarsus adductus,
the calcaneal line passes through the lateral portion of the cuboid and
through the base of the fifth metatarsal. Heel valgus is evidenced by a
greater than 35° AP talocalcaneal angle and by medial and forward
displacement of the head of the talus in relation to the anterior
portion of the calcaneus. The navicular
(generally not seen on radiographs in this age group) is neutral or displaced laterally on the talar head (see Figure 20-19).
benign. It is estimated that 85 to 90% of cases resolve spontaneously
without treatment. In childhood, persistent metatarsus adductus leads
to an in-toeing gait and occasional complaints of stumbling or
tripping. Adults with uncorrected metatarsus adductus rarely complain
of pain but may have hallux valgus and bunions. Shoe wear may be a
problem in patients with uncorrected metatarsus adductus. Patients may
complain of pain in the lateral foot and in the tarsometatarsal joints.
Shoes may irritate this area. It is thus important in infancy to select
patients who require treatment.
the passive correctability of the deformity. In patients in whom the
deformity corrects by stimulation of the lateral border of the foot or
in those in whom the heel is stabilized, the deformity can be passively
corrected or overcorrected, and only observation is necessary. Most
cases correct spontaneously. In most large series, if the foot remained
passively correctable, the deformity had corrected spontaneously by the
age of 3 years. Parents should not be encouraged to do manipulations.
Manipulations by parents are generally poorly done and may accentuate
heel valgus and only minimally correct forefoot adduction. There is no
scientific validity for the use of straight-last or reverse-last shoes
in the treatment of metatarsus adductus. Denis Browne splints should
not be used because they may accentuate heel valgus.
metatarsus adductus, manipulation and casting are indicated. Two main
components of the deformity, adduction of the metatarsals and varying
degrees of valgus of the heel, must be corrected simultaneously.
Improper manipulation and casting treatment of metatarsus adductus lead
to a pronation deformity of the foot. A flatfoot with residuals of
metatarsus adductus and severe heel valgus is a significantly worse
problem than the original deformity.
calcaneus underneath the talus. With the calcaneus supinated, the
cuneiform, navicular, and cuboid bones are inverted, bringing the bases
of the metatarsals in proper alignment with the talus and calcaneus
(see Figure 20-19). The metatarsals are then
abducted, with counterpressure applied over the cuboid bone. It is
important not to pronate the forefoot because a cavus deformity will
result. The manipulations of the foot are sustained for several
minutes, and this is followed by the application of a thinly padded,
well-molded, toe-to-groin plaster cast changed at biweekly intervals
until the foot is in the slightly overcorrected position. Complete
correction usually requires 3 to 4 long-leg plaster applications. The
casting treatment is complete when the lateral aspect of the foot is no
longer convex, the heel is in a neutral to slight valgus position, and
the forefoot has been completely corrected past neutral. Successful
treatment of metatarsus adductus by manipulations and casting in
patients older than 8 months of age is not likely, and surgical
correction may be necessary.
only in patients with significant cosmetic or shoe-wearing problems. In
patients younger than 2 years of age with rigid metatarsus adductus,
first metatarsal cuneiform capsulotomy and release of the abductor
hallucis, followed by casting, is usually successful. In older
children, corrective bone surgery may be necessary.
is sometimes used to denote the varying amounts of cavus of the
forefoot evident in patients with clubfeet. In the clubfoot, the heel
is in varus, and the first metatarsal is in severe plantar flexion,
while the fifth metatarsal is normally aligned with the cuboid and
calcaneus (Figures 20-30 and 20-31; see Figure 20-19). Cavus is caused by eversion of the forefoot in relation to the hindfoot.
apparent at birth. All clubfeet are not of the same severity, although
all have the basic components of adduction and inversion of the
forefoot and midfoot, heel varus, and fixed equinus. The soft tissue
changes vary from mild to severe. Clubfoot should best be thought of as
a spectrum of deformities. Clubfoot may occur as an isolated disorder
or in combination with various syndromes and other associated
anomalies, such as arthrogryposis, sacral agenesis, amniotic bands,
Larsen syndrome, diastrophic dwarfism, Freeman-Sheldon syndrome, and
myelodysplasia.
 |
|
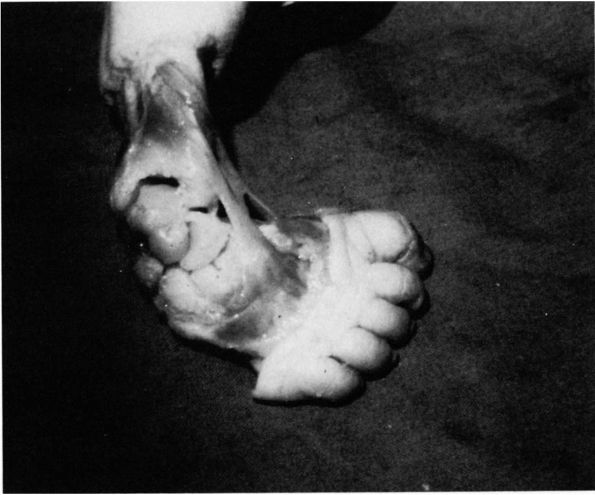
FIGURE 20-30.
Severe clubfoot deformity. The heel is in severe varus, and the forefoot is adducted and inverted. The cavus deformity results from the slightly pronated position of the forefoot in relation to the hindfoot. |
1 to 2 per 1,000 live births. It has a male predominance of 2:1 and an
incidence of bilateralness estimated to be about 50%. There is an
increased incidence in certain racial and ethnic groups, such as
Polynesians, Maoris, and South African blacks, with a much higher
incidence if the patient has a positive family history for clubfoot.
 |
|
FIGURE 20-31.
Clubfoot in a 3-day-old infant. The navicular is medially displaced and articulates only with the medial aspect of the head of the talus. The cuneiforms are seen to the right of the navicular, and the cuboid is underneath it. The calcaneocuboid joint is directed posteromedially. The anterior two-thirds of the os calcis is seen underneath the talus. The tendons of the anterior tibialis extensor hallucis longus and the extensor digitorum longus are medially displaced. (Ponseti IV, Campos J. Observations on pathogenesis and treatment of congenital clubfoot. Corr 1972;84:50-60) |
patients remains unknown. Many theories have been advanced, including
intrauterine molding defect, blastemic defect of the tarsal cartilage,
primary nerve lesion with secondary muscle dysfunction, vascular
abnormalities, arrested embryonic development, abnormal tendon
insertions, and primary fibrotic contracture. The most widely accepted
theory is that of polygenic inheritance modified by environmental
factors.
The child presents with the foot in severe supination with a fixed
equinus deformity, heel varus, forefoot and midfoot adduction, and
varying amounts of cavus. The involved foot is generally smaller than
the opposite side with varying amounts of calf atrophy.
on the dorsolateral aspect of the foot. Depending on the severity of
the cavus deformity, there may be a deep skin crease across the plantar
medial aspect of the midfoot. The foot cannot be passively manipulated
into the neutral position.
deformity. The calcaneus, talus, and cuboid are usually ossified at
birth. The navicular does not ossify until about 3 years of age. The
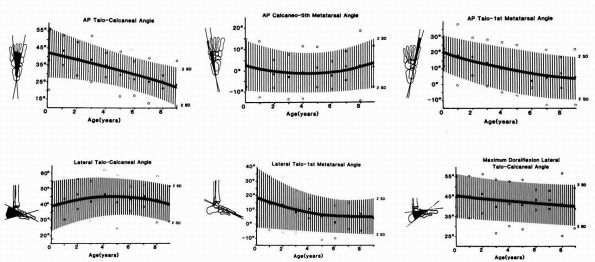
normal values of
bony relations on standing AP and lateral views of the foot are somewhat variable and age dependent (Figure 20-32).
(photographs are also useful for this purpose), for follow-up, in
assessing the results of nonoperative treatment, and in planning for
operative correction of the deformity if necessary. It is best to
obtain the initial radiographs in the maximally corrected position.
This position varies depending on the flexibility of the individual
clubfoot.
exhibit parallelism on both the AP and lateral radiographs, indicating
hindfoot varus and equinus (see Figure 20-31).
The talus first metatarsal angle is negative, indicating adduction of
the forefoot. Because of the inversion of the forefoot, the metatarsals
appear overlapped. The cuboid is medially displaced on the AP view,
indicating the adduction at the midfoot; and on the lateral view, the
first metatarsal is in plantar flexion to a greater degree than the
fifth metatarsal, indicating cavus deformity.
In the clubfoot, the talar body is in plantar flexion with the neck
angulated medially. The navicular articulates with the medial aspect of
the talar neck, and the navicular tuberosity is in close approximation
with the medial malleolus. The calcaneus is directly underneath the
talus, and the cuboid is medially displaced beneath the navicular. The
midfoot is thus adducted and inverted in relation to the talus. The
dorsal tendons are medially displaced, and the head of the talus is
prominent laterally.
 |
|
FIGURE 20-32. Normal radiographic values for various foot measurements. (Vanderwilde
R, Staheli LT, Chew DE et al. Measurements on radiographs of the foot in normal infants and children. J Bone Joint Surg 1988;70A:407-415) |
than the noninvolved side, with the neck in varying degrees of medial
deviation. The navicular is wedged-shaped laterally, with a prominent
tuberosity. The calcaneus is small, often with an absent anterior
facet. The posterior facet shows varying degrees of hypoplasia and may
be linked directly to the middle facet. In unilateral deformities, the
foot is always smaller than the noninvolved side, and the calf has
varying degrees of atrophy. The tuberosity of the navicular is held in
close approximation to the talar neck, the sustentaculum and the medial
malleolus by the shortened, thickened tibionavicular ligament,
calcaneonavicular ligament, and sheath of the posterior tibial tendon.
clinical problems, results in a severe handicap unless corrected. The
surface area for weight bearing is the lateral aspect of the foot;
without treatment, even an otherwise normal patient develops pressure
sores and sinuses by the fourth or fifth decade of life (Figure 20-33).
deformity vary in the orthopaedic literature. Some judge success only
by radiographic criteria, others by function, and others by certain
clinical criteria. Thus, the literature on treatment is difficult to
compare.
 |
|
FIGURE 20-33. Four-year-old girl with bilateral untreated clubfeet.
|
and maintain the foot in plantargrade position. Treatment should be
initiated immediately on diagnosis, preferably within the first week of
life. Treatment for the newborn with clubfoot is by manipulation and
then casting to maintain the correction obtained through manipulation.
Corrections begun at a later age may be more difficult owing to
ligamentous contracture and joint deformity. Toe-to-groin plaster casts
are used to maintain the corrections obtained through manipulation. The
equinus deformity is the last deformity corrected to prevent
development of a rocker-bottom foot. Casts are changed at weekly
intervals, and most deformities are corrected in 5 to 7 casts.
Successful treatment rates by casting regimens alone vary in the
literature from 85 to 95%. Night splinting is often used for prolonged
periods (several years) to maintain correction.
natural tendency to recur. The more severe and rigid the initial
deformity, the greater the risk of recurrence. Recurrences may be
treated by serial manipulations and casting followed by occasional
tendon transfers to correct for any muscle imbalance.
to manipulation and casting or that recur may require extensive
posterior, medial, and lateral soft tissue releases. The releases are
best done at a young age but can be done satisfactorily in children
until 5 years of age.
shortening procedures (decancellation of the cuboid or wedge resection
of the cuboid in excision of the anterior end of the calcaneus) are
often performed in conjunction with posteromedial releases. This is
because the greater length of the lateral foot column compared with the
medial foot column is thought to be secondary to the medial soft tissue
contractures.
medial, subtalar, and lateral releases performed for residual,
resistant, or recurrent clubfoot include skin sloughing on
posteromedial aspect of the foot, overcorrection of the deformity,
residual forefoot adductus, stiffness, and incomplete correction of the
deformity.
persistent clubfoot deformity in older children. These procedures are
best offered to the patient at 10 to 12 years of age, when foot growth
is complete.
Parents notice that the child is walking on the toes either all or most
of the time. Idiopathic toe-walking is thought to be an inherited
condition because up to 70% of patients have a positive family history.
The condition is bilateral and predominantly affects boys (3:1). About
20% of these children have evidence of a learning disability, and an
occasional child carries the diagnosis of hyperkinesia with minimal
brain dysfunction.
normal gait variation. Generally, within the first 6 months after
walking, the gait may progress from the toe-toe gait or an occasional
toe-toe gait to a toe-heel gait and eventually to a heel-toe gait. The
mature heel-toe gait pattern is generally established by the time a
child is 3 years of age. Careful history of gait development should be
obtained in each patient who presents with a chief complaint of
toe-walking. Patients with the diagnosis of idiopathic toe-walking have
nearly always walked on their toes.
upper and lower extremities as well as a careful neurologic examination
and observation of the patient’s gait. Variable amounts of contracture
and restriction of ankle dorsiflexion are noted. The amount of
contracture or restriction of motion may not be symmetric. These
patients have normal sensory examinations and no evidence of muscle
weakness. Deep tendon reflexes should be intact
without
evidence of hyperactivity. The spine should be evaluated for evidence
of hair patches, dimpling, hyperpigmentation, or nevi, which are
suggestive of spinal dysraphism. There should be minimal or no
contracture of the hamstrings, and the patient should have good control
of the upper extremities.
patients with idiopathic toe-walking can walk on their heels and have a
heel-toe gait periodically, but the observed gait pattern usually is
toe-toe. Idiopathic toe-walkers with heel cord contractures can
generally get their heels down in standing only through knee
hyperextension (Figure 20-34).
All conditions that may be associated with an equinus deformity and
contracture of the tendo Achilles must be ruled out. Cerebral palsy can
be ruled out by the absence of increased deep tendon reflexes,
hypertonicity, hamstring contractures, and the lack of posturing
abnormalities of the upper extremity during gait. Gait analysis may be
of help in differentiating the idiopathic toe-walker from the cerebral
palsy patient. Other conditions, such as spinal dysraphism, muscular
dystrophy, tethered spinal cord, or other central nervous system
dysfunctions, must be ruled out. Electromyographs, motor nerve
conduction studies, spine films, CT scan of the brain, or MRI may be
necessary. Muscle biopsy to rule out muscular dystrophy is also
warranted on occasion. Any child with a unilateral deformity,
particularly of recent onset, should have an etiologic source sought. A
neurologic consultation is often in order.
 |
|
FIGURE 20-34. Three-year-old male idiopathic toe-walker. The heels can be brought to the floor by knee hyperextension.
|
abnormal findings other than those referable to the equinus deformity
with varying degrees of contracture of the Achilles tendon. They have
normal sensation, no pain, and no muscle dysfunction.
of the patient and the degree of contracture of the Achilles tendon. In
patients who are younger than 3 to 4 years of age and have no or
minimal contracture of the Achilles tendon, passive range of motion and
stretching exercises are indicated. The child’s progress should be
monitored carefully. If ankle dorsiflexion to at least 10° cannot be
restored by this method in 3 to 4 months, serial casts should be
applied. If, however, the ankle can be passively dorsiflexed to neutral
or beyond, but the child habitually toe-walks, use of a hinged or
nonhinged ankle foot orthosis is an option to prevent plantar flexion.
These orthoses can be used for a period of weeks to months, depending
on the clinical situation. The patient should be continually
reevaluated and progress reassessed. In most cases, serial casting in
dorsiflexion for 4 to 6 weeks is usually sufficient to resolve the
problem. Many patients require postcasting ankle-foot orthoses, passive
range of motion, and careful follow-up to ensure that the condition
does not recur. In most cases, these noninvasive procedures provide
resolution of the problem. For the child who fails to respond to serial
casting or is otherwise not a candidate for this procedure, Achilles
tendon lengthening provides uniformly good results. Surgical Achilles
tendon lengthening is followed by 3 weeks in a nonweight-bearing
short-leg cast, then 3 weeks in a weight-bearing short-leg cast.
Recurrences after this procedure are rare.
position of the legs of an infant or the way a child walks frequently
results in medical consultation.
Unfortunately, these concerns often result in unnecessary, costly treatment.
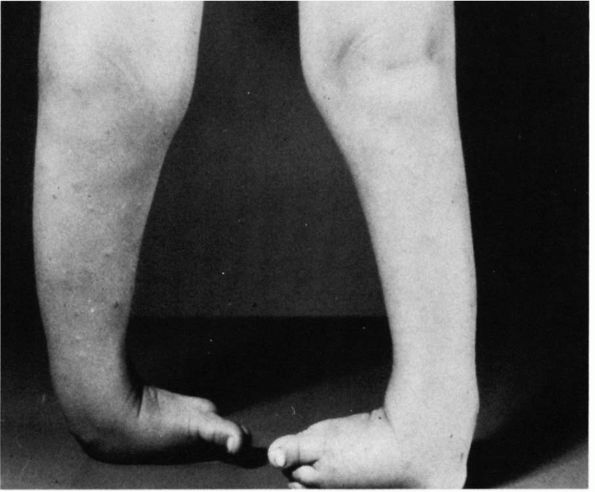
and trochanter) is usually anteverted about 40° in relation to the
transcondylar axis of the distal femur. The intermalleolar axis of the
distal tibia in relation to the interplateau axis of the proximal tibia
is in about 3° of lateral rotation. During the first year of life,
femoral anteversion decreases by about 8° and thereafter decreases by
about 1° per year until the adult configuration of about 10 to 15° of
anteversion is reached at maturity. Tibial version also increases
throughout life until the adult lateral version of 15 to 20° is reached
at maturity. Version of more than two standard deviations beyond the
mean is referred to as torsion.
parents perceive an abnormality should be carefully checked to see
whether the child is merely in the normal stages of development or has
a torsional problem. The most common torsional problems are femoral
antetorsion and medial tibial torsion. The normal values for version
vary according to the age of the patient (Figure 20-35).
The cause of the torsional problems is unknown but may be due to
persistent version or genetic factors. Postnatal sitting and sleeping
postures have been implicated as mechanisms that either cause torsional
abnormalities or contribute to their lack of resolution, but no
conclusive proof exists. Excessive ligament laxity on a genetic basis
has been thought by some investigators to contribute to persistent
femoral antetorsion in that many children with femoral antetorsion have
accompanying physiologic pes planus, genu recurvatum, and excessive
lumbar lordosis. The latter two may actually be compensatory measures
for femoral antetorsion.
in-toeing should have a careful history and physical examination. The
history should include the age at which the parents first noted the
deformity, how they think it affects the child’s function, and any
perceived disability because of the deformity. Sleeping and sitting
postures should be assessed and a complete history of normal growth and
development obtained. The age at onset of walking should be evaluated.
Any delay in development of walking beyond 18 months of age may be
suggestive of a neuromuscular abnormality such as cerebral palsy. A
family history of similar problems should be sought.
neurologic examination and a torsional profile of the patient. The most
common abnormalities seen are those of femoral antetorsion, medial
tibial torsion, and metatarsus adductus. Other conditions, such as an
overactive abductor hallucis, clubfoot deformity, or dynamic in-toeing
because of muscle imbalance, must be ruled out.
worse at the end of the day or when tired, which may indicate failure
of compensatory mechanisms. The problem may be of great concern to
parents, who often scold the child for walking in a way that is more
comfortable because of the child’s rotational profile.
unobstructed area. The position of the patella and the feet should be
noted. The physician should assess the foot progression angle. The foot
progression angle is the axis of the foot as the child walks along an
imaginary line of progression. This can be estimated or special paper
(footprint paper) can be used to assess the foot progression angle.
Negative foot progression angles designate in-toeing; positive foot
progression angles designating outtoeing. The normal foot progression
angle is usually positive.
extension in the prone position. The knee is flexed to 90°, and
rotation is assessed medially and laterally in relation to the gluteal
cleft. The pelvis should be stabilized, and no force should be exerted
on the limb. Internal and external rotation are assessed and compared
with normal, age-matched values (Figures 20-36 and 20-37).
In most cases, the thigh-foot axis is sufficient. Tibial rotation can
be assessed in several ways. With the patient in the prone position and
the knees flexed to 90°, the thigh-foot axis can easily be assessed and
compared with normal, age-matched values. If the patient has a foot
deformity, the transmalleolar axis should be used. The transmalleolar
axis is assessed by placing the thumb and index finger on the medial
and lateral malleoli, respectively, to define the intermalleolar axis;
a perpendicular axis is then defined, and the angles between the
perpendicular and intermalleolar axis and the long axis of the thigh
are assessed. A simpler assessment of the intermalleolar axis is done
with the patient sitting with the legs hanging free over the table and
the knees at 90°. The thumb and index finger can be placed on the
medial and lateral malleoli, respectively, and the intermalleolar axis
can be assessed in relation to the tibial tubercle, determining the
degree of tibial rotation.
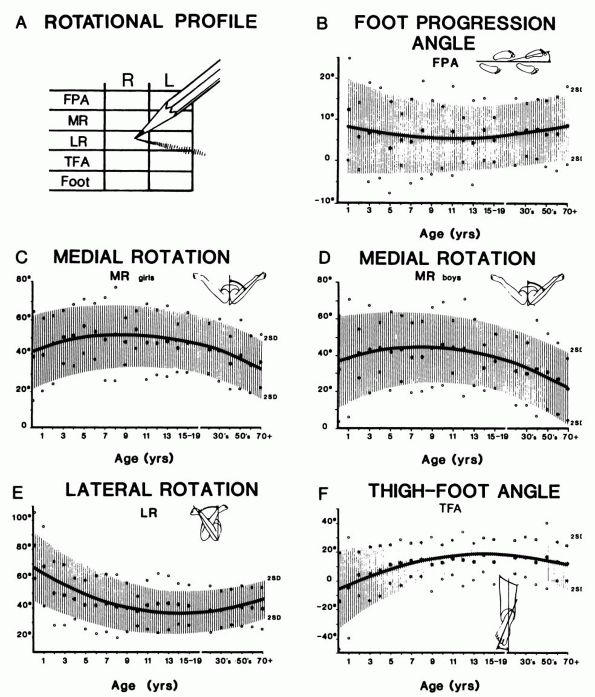 |
|
FIGURE 20-35. The rotational profile. (A)
The method of recording and the degree of measurement for each element of the profile are depicted. This simple chart includes the vital information necessary to establish the diagnosis and to document deformity. (B through F) Normal values with the profile based on 1,000 normal limbs are shown. In each figure, the age is listed on the abscissa on a logarithmic scale, and the degrees are shown on the ordinate scale. The mean values are shown in the solid line with a ±2 standard deviation normal range shown in the shaded areas. A gender difference was found from medial rotation, so values are shown independently. (Staheli LT. The lower limb. In: Morrissy RT, ed. Lovell and Winter’s Pediatric Orthopedics, 3rd Ed, vol. 2. Philadelphia: JB Lippincott, 1990:742) |
metatarsus adductus and residual deformity secondary to previous
clubfoot treatment. The cause of the patient’s in-toeing gait may be
one or more abnormalities in the lower extremity. Occasionally, a
rotational profile of the parent may reveal a torsional problem that
explains the torsional problem in the child or lack of resolution of
the problem in the older child.
children with torsional problems. In the infant, congenital hip
dysplasia must be ruled out, and if clinical examination warrants,
radiographs may be necessary. Determination of version is best done by
CT or MRI with cuts through the axis of the femoral neck and the
femoral condyles. Torsion of the tibia is easily measured clinically,
and hence radiographs or special studies are rarely necessary.
 |
|
FIGURE 20-36. Femoral antetorsion. (A)
Four-year-old girl with femoral antetorsion. In the standing view, the patella points inward. In the prone position, excessive femoral antetorsion indicated by internal rotation to about 90° (B) and by restricted external rotation (C). |
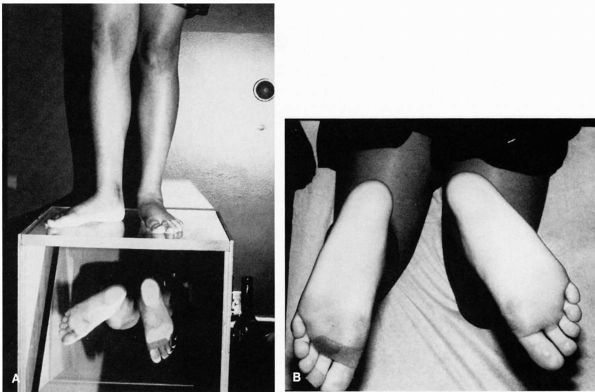 |
|
FIGURE 20-37. Lateral tibial torsion. (A) Twelve-year-old girl with lateral tibial torsion. (B) Unilateral abnormality in the thigh-foot axis is seen.
|
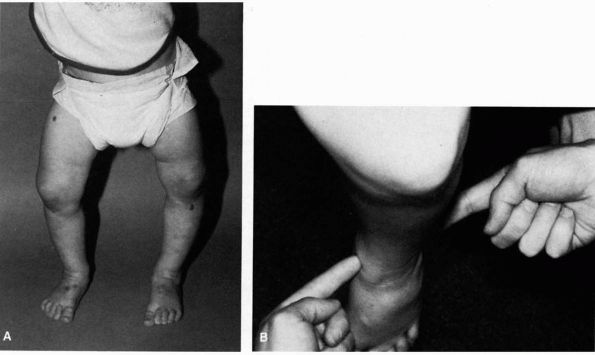 |
|
FIGURE 20-38. Medial tibial torsion. (A) Eighteen-month-old boy with medial tibial torsion and physiologic bowing. (B)
Tibial rotation is assessed by visualizing relation of intermalleolar axis in reference to the tibial tubercle with patient sitting with leg over the edge of the examination table. |
gradual resolution, and hence treatment of these conditions is rarely
necessary. Treatment by devices such as corrective shoes, twister
cables, and alteration of sleeping or sitting habits have never been
shown to affect the natural history of these conditions and should
therefore be avoided. Education of the family regarding the natural
history of these conditions is important. The family should be
reassured that most torsional problems resolve spontaneously in the
course of normal growth. The parents should also be reassured that if
there is a positive family history of torsional problems, complete
resolution may not occur, but in most cases, no functional disability
ensues.
in by parents for complaints of the feet pointing out. Careful
examination of the hips should be done to rule out congenital hip
dysplasia. External rotation contractures are normal in the infant and
gradually resolve with time. Treatment is never indicated.
the parents complaining of one foot turning out, a careful hip
examination should be performed to rule out any associated congenital
hip dysplasia. In general, the out-turned foot is the more normal foot
because this condition usually coexists with metatarsus adductus or
medial tibial torsion on the opposite side. The natural history should
be explained to the parents and observation recommended.
in-turning of the lower extremities is metatarsus adductus. Congenital
hip dysplasia must, however, be ruled out.
most common cause of in-toeing is medial tibial torsion, which may or
may not be accompanied by metatarsus adductus. Reassurance and
observation is the treatment of choice.
medial femoral torsion is a common cause of an in-toeing gait. Natural
history studies indicate that medial femoral torsion is not associated
with degenerative joint disease over the long term, and hence
observation is the only treatment warranted. Radiographs or special
studies are not indicated unless there is asymmetry.
femoral torsion is rarely indicated. Surgical correction can be
considered in cases of medial tibial torsion if the child is older than
8 years of age (when spontaneous correction is no longer possible),
if
the discrepancy is more than three to four standard deviations from the
mean, and if the deformity is causing the child significant functional
or cosmetic problems. Supramalleolar osteotomy is usually the treatment
of choice when surgical correction is contemplated.
usually does not resolve with age. Lateral tibial torsion can be
considered for correction if it is greater than 30° and causes
significant functional or cosmetic deformity to the child (see Figure 20-37).
if the child is older than 8 years of age and has more than three
standard deviations from the mean of torsional deformity (medial
rotation greater than 85°, lateral rotation less than 10°, or
anteversion greater than 50°). Consideration can be given for
correction either at the intertrochanteric level or the supracondylar
region; most surgeons prefer the intertrochanteric region. In
teenagers, closed intramedullary rotational osteotomy can be considered.
antetorsion, lateral tibial torsion compensates for the deformity.
Surgical treatment should be avoided because the rotational osteotomies
would need to be performed in the femur and the tibia, and subsequent
patellofemoral malalignment problems could ensue.
authors present a review of 22 skeletally immature patients with 39
accessory navicular bones seen during a 4-year period. Twenty-five of
the feet were treated surgically after failure of conservative
treatment. Symptoms were relieved in all surgically treated patients.
Detailed histologic studies of the excised specimens are presented. The
changes were consistent with the theory that chronic chondro-osseous
tensile failure could occur and that this condition is responsible for
the clinical findings.
is a classic study of flatfeet in 3,600 Canadian army recruits. The
authors found that flexible flatfoot produces disability only when it
occurs in combination with a contracted tendo Achilles.
article reports on a radiographic study of 10 children with flexible
flatfeet. Radiographs were taken barefoot, with a Thomas heel, with an
over-the-counter insert, and with two specially molded plastic foot
orthoses. The study showed no difference between the barefoot
radiographs and those in which an appliance was used.
LT, Chew DE, Corbett M. The longitudinal arch: a survey of eight
hundred and eighty-two feet in normal children and adults. J Bone Joint
Surg 1987;69A:426. This article reports on a
study of 441 normal subjects (1 to 80 years old) that was conducted to
determine the configuration of the longitudinal arch. The authors found
that flatfeet are usual in infants, common in children, and within the
normal range of observations in adults.
DR, Mauldin D, Speck G et al. Corrective shoes and inserts as treatment
for flexible flat foot in infants and children. J Bone Joint Surg
1989;71A:800. This article reports on a
randomized prospective study of 98 patients treated by various
“accepted” methods for flexible flatfoot. The authors demonstrated that
flexible flatfoot improved naturally over the 3 years of the study and
that the degree of improvement was not affected by wearing of a
corrective shoe or a shoe with an insert.
author recommended that CT evaluation of both feet in transaxial and
coronal planes be obtained in patients with suspected tarsal coalition.
This was based on a study where 6 of 30 children with symptomatic
tarsal coalition were found to have multiple coalitions in the same
foot, which is a higher percentage than had previously been reported.
and axial CT and MRI studies were obtained for 40 feet in 20 patients
with symptoms suggesting tarsal coalition. The authors concluded that
CT is the gold standard and the more cost-effective imaging study for
detecting tarsal coalition. MRI is also very good for detecting tarsal
coalition, particularly if other causes for ankle or foot pain are
being considered.
P, Kumar SJ. Calcaneonavicular coalition treated by resection and
interposition of the extensor digitorum brevis muscle. J Bone Joint
Surg 1990;72A:71. The authors present a 2- to
20-year follow-up of 75 calcaneonavicular coalitions treated by
resection and interposition of the extensor digitorum brevis muscle.
Good or excellent long-term results were reported in 77% of the cases.
The best results were reported in patients between 11 and 15 years of
age who had a cartilaginous coalition. Talar beaking was not a
contraindication to surgery.
author evaluated 31 index patients with tarsal coalitions and peroneal
spastic flatfoot and 90 of their first-degree relatives. Thirty-nine
percent of the first-degree relatives were found to have some type of
tarsal coalition, but none was ever symptomatic. The study demonstrates
that tarsal coalitions are inherited probably as an autosomal dominant
disorder and that tarsal coalition is probably not a rare phenomenon.
subtalar arthrodesis was performed on 44 feet with hindfoot pathology
on which 10 of the feet had a talocalcaneal coalition. The average age
at surgery for this subgroup was 26 years. At an average follow-up of
91 months, the AOFAS score was 93 of a possible 100 points, and 88% of
the patients were satisfied or very satisfied with their results.
authors present a superb review of the history, origin, hereditary
evidence, incidence, clinical presentations, pathomechanics, radiologic
diagnosis, differential diagnosis, and treatment of tarsal coalitions.
This article was published before the use of CT scanning in
diagnosis and also before several long-term reviews of treatment. The
background information and bibliography on tarsal coalition are superb.
BW, Asher MA. Excision of symptomatic coalition of the middle facet of
the talocalcaneal joint. J Bone Joint Surg 1987;69A:539. The
authors report excision of the middle facet of the talocalcaneal joint
and autogenous fat grafting in nine patients with 10 symptomatic
coalitions. Eight of 10 feet had satisfactory results.
S, Cooperman DR, Thompson GH. Interposition of the split flexor
hallucis longus tendon after resection of a coalition of the middle
facet of the talocalcaneal joint. J Bone Joint Surg 1999;81A:11. Fourteen
feet in 10 patients with painful middle facet talocalcaneal coalitions
that had failed conservative management underwent resection of the
coalition and interposition of a split portion of the flexor hallucis
longus tendon. At a mean follow-up of 51 months (range 32 to 60
months), 12 of the feet were rated as excellent and good using the
AOFAS rating system. None of the patients had symptoms of functional
impairment of the great toe.
MF, Scranton PE, Hansen S. Tarsal coalitions: long-term results of
surgical treatment. J Pediatr Orthop 1983;3:287. The
authors reviewed 40 patients who underwent 57 operations for tarsal
coalition. Poor results were correlated with inadequate resection or
advanced degenerative joint disease. Talar beaking does not necessarily
represent early degenerative joint disease but does represent
talonavicular ligament traction spurs, which are not necessarily
associated with articular degeneration but are caused by increased
stress across the talonavicular joint. This beaking is not a
contraindication to bar resection.
authors present a classification of congenital vertical talus, discuss
the pathophysiology, and present a surgical method of management. This
remains the classic article on the subject.
single-stage surgical correction procedure was performed on 41 patients
with 55 congenital vertical tali. At follow-up (average 7 years), there
were 31 good and 11 fair results. The authors cautioned that underlying
diagnoses are common and should be identified to minimize the risk of
recurrence.
K, Shoenecker PL, Sheridan J. Congenital vertical talus and its
familial occurrence: an analysis of 36 patients. Clin Orthop
1979;139:128. The authors report the follow-up of
36 patients with 57 feet with congenital vertical talus. A high
incidence of associated congenital hip dislocation, arthrogryposis,
congenital hypoplasia of the tibia, and central nervous system
abnormalities was noted. Half of the patients with a primary isolated
form of congenital vertical talus had a positive family history of foot
deformities in first-degree relatives. A method of surgical correction
is presented.
authors present a series of 15 congenital vertical tali in 12 patients.
They found that the best result was obtained with early subtalar
arthrodesis (Grice operation) and plantar K-wire fixations. Attempts to
augment push-off power with tendon transfers were unrewarding. Casting
alone revealed the worst results. Half of patients had associated
abnormalities.
this article, 125 cases of congenital calcaneal valgus are presented.
Forty-nine percent were treated with manipulation and taping; 51% were
treated with observation alone. The authors demonstrate no significant
difference in the outcome between the two groups. The follow-up was
between 3 and 11 years, and most feet were normal. Pronation of the
feet was often seen when the patients began to walk, and many had
slight residual valgus compared with the other side.
H. The significance of congenital pes calcaneo-valgus in the origin of
pes palno-valgus in childhood. Acta Orthop Scand 1960;30:64. The
authors reviewed 2,735 consecutive newborns and followed the patients
for 2 years. One-hundred and forty-seven of the patients had more than
20° of heel valgus; 333 had 10 to 15°; 759 had 0 to 5°; and 1,496 had
0°. When seen at 2 years of age, 43% of the 147 patients with at least
20° of valgus had flatfeet. Twenty-three percent of the group with
normal valgus had flatfeet. The authors conclude that severe
calcaneo-valgus is associated with a flatfoot deformity in later life.
R. Family studies and the cause of congenital clubfoot: talipes
equinovarus, talipes calcaneo-valgus, and metatarsus varus. J Bone
Joint Surg 1964;46B:445. This article deals with
family history, associated abnormalities, and causes of clubfoot,
metatarsus varus, and calcaneal valgus deformity. This is an excellent
review article on the epidemiology and origin of these three foot
conditions.
E, Ricciardi Pollni PT, Falez’ F. Köhler’s disease of the tarsal
navicular: long-term follow-up of 12 cases. J Pediatr Orthop
1984;4:416. The authors report an average 33-year
follow-up of 12 patients with Köhler disease of the tarsal navicular.
Complete restoration of normal navicular anatomy averaged 8 months.
Treatment did not affect the radiographic course of the disease. All
patients reconstituted normal navicular shape, were asymptomatic, and
had no evidence of degenerative joint disease.
author reports 45 cases of Köhler disease of the tarsal navicular (39
boys, 6 girls). Treatment had no effect on the radiographic course of
the disease. The radiographs of 50 normal children (25 boys, 25 girls)
were evaluated for scaphoid development with radiographs taken every 6
months from age 9 months to 4 years. In over half the female patients,
a well-developed ossific nucleus of the scaphoid was apparent at 2
years of age; it was apparent by 3.5 years of age in all the patients.
More than one-third of the male patients were older than 3.5 years of
age before the scaphoid appeared. The average age of appearance of the
ossific nucleus for girls is 18 months to 2 years and for boys, 2.5 to
3 years of age. The author also discussed ossification patterns of the
scaphoid in relation to time of appearance. The radiographic appearance
is unrelated to the duration of symptoms or to treatment. Normal
delayed development of the appearance of the ossific nucleus to the
scaphoid may simulate a radiographic picture similar to that seen in
Köhler disease.
W. The ossification and vascularization of the tarsal navicular and
their relation to Köhler’s disease. J Bone Joint Surg 1958;40B:765. This
article reports on an excellent study of the vascular supply to the
tarsal navicular and a radiographic study of 52 normal children’s feet.
Radiographs were taken at 6-month intervals between the ages of 2 and 5
years to assess normal ossification patterns in the navicular. On the
basis of the vascular injection studies and the clinical follow-up, the
author proposes that Köhler disease of the navicular is caused by compression of the bony nucleus at a critical phase during the growth of a navicular whose appearance is delayed.
authors reviewed 20 patients with Köhler disease of the tarsal
navicular with an average follow-up of 9.5 years. All patients were
asymptomatic and had reconstituted the navicular to the normal
radiographic appearance. Short-leg casting significantly affected the
morbidity in patients, reducing the symptomatic period from 15 months
(untreated patients) to less than 3 months.
author, who described the origin of the condition in 1913, discusses
Köhler’s opinion that the cause of the condition is probably not
traumatic. This is a classic paper.
this review of 41 cases, female patients predominated. The author
proposes a traumatic origin (i.e., stress fracture) for the disease.
Treatment options at various disease stages are discussed.
A, Lieberson S, Mendes DG et al. Remodeling of the calcaneus apophysis
in the growing child. J Pediatr Orthop 1995;4B:74. The
authors used radiographs and CT scans to compare the heels of 36
children with symptoms of calcaneal apophysis and 52 control children.
On lateral radiographs, increased density of the calcaneal apophysis
was noted in all heels. One or two radiolucent lines (fragmentation)
were noted in all of the painful heels but in only 27% of the heels in
the control group. CT demonstrated normal increased density with growth.
LJ, Ireland ML. Prevention and management of calcaneal apophysitis in
children: an overuse syndrome. J Pediatr Orthop 1987;7:34. The
authors present an excellent historical review and extensive discussion
on the differential diagnosis of heel pain in the child and adolescent.
The authors present a large series (85 children, 137 heels) of
calcaneal apophysitis (Sever disease) treated by a physical therapy
program of lower-extremity stretching, particularly the Achilles
tendon, ankle dorsiflexion strengthening, and orthotics. All patients
were able to return to their sport of choice 2 months after the
diagnosis. The authors proposed that the cause of the condition is an
overuse syndrome.
author describes a radiographic classification in 84 patients with 124
feet with a minimal follow-up of 2 years. The study was devised to
determine prospectively whether radiographic evaluation can provide
better prognostic information than the usual clinical criteria. The
author proposes a four-group classification based on the
anteroposterior radiographs: simple metatarsus adductus, complex
metatarsus adductus, simple skewfoot, and complex skewfoot. The author
reports that all patients with complex skewfoot had flatfoot at
follow-up and that there was a strong association with the use of Denis
Browne splints and flatfoot deformity at follow-up. Ninety-seven
percent of untreated feet responded favorably. The period of cast
treatment for patients with complex skewfoot deformity was required
twice as long as for those with simple metatarsus adductus, and all had
flatfoot at follow-up. This article includes an extensive bibliography.
was a retrospective study of the results of treatment of 160 children
(265 feet) classified by flexibility according to the extent of passive
abduction of the forefoot against the stabilized hindfoot with
reference to the heel bisector. Results of treatment were statistically
significantly better when treatment was begun between the ages of 1 day
and 8 months. The only significant predictor of a good outcome was the
age of the patient. The recurrence rate was 12%. Severity and
flexibility did not appear to affect the treatment outcome. This is an
excellent review of the subject with an extensive bibliography.
P, Weinstein SL, Ponseti IV. The long-term functional and radiographic
outcomes of untreated and nonoperatively treated metatarsus adductus. J
Bone Joint Surg 1994;76A: 257. Thirty-one
patients (45 feet) who had metatarsus adductus were evaluated and
followed for an average of 32 years and 6 months. Twelve patients (16
feet) who had a passively correctable deformity (mild or moderate) at
the time of the initial presentation had no treatment. Twenty patients
(29 feet) who had a partly flexible or rigid deformity (moderate or
severe) at the time of the initial presentation were managed with
serial manipulation and application of plaster holding casts. (One
patient who had a bilateral deformity had no treatment on one side and
conservative management on the other). The results were good in all 16
of the untreated feet and in 26 (90%) of the 29 feet that had been
conservatively treated. There were no poor results. The passively
correctable deformities resolved spontaneously. Radiographs showed an
obliquity of the medial cuneiform-metatarsal joint in 21 (68%) of the
31 feet that were examined clinically and radiographically. Similar
findings were observed in four of 11 contralateral, normal feet. Hallux
valgus was not a common outcome. No patient had operative correction.
patients who had 71 congenital clubfeet were evaluated at an average
age of 34 years (range, 25 to 42 years). With the use of pain and
functional limitations as the outcome criteria, 35 (78%) of the 45
patients had an excellent or good outcome compared with 82 (85%) of 97
individuals who did not have congenital deformity of the foot. The
technique of treatment led to good long-term results in patients who
had clubfoot. The data suggest that a sedentary occupation and
avoidance of excessive weight gain may improve the overall long-term
result. Excessive weakening of the triceps surae may predispose
patients to a poor result. Therefore, it is prudent to avoid
overlengthening of this muscle. The outcome could not be predicted from
the radiographic result.
authors present a superb review of the pathologic anatomy of clubfoot,
comparing five clubfeet with three normal control feet in subjects of
the same ages. The authors propose a retracting fibrosis as the primary
etiologic factor of clubfoot deformity.
good general review of the theory behind and the treatment procedure
for the correction of clubfoot by a method used at the University of
Iowa for over 40 years.
VJ. Resistant congenital clubfoot:—one-stage posteromedial release with
internal fixation. J Bone Joint Surg 1979;61A:805. The
author reports modifications of his original technique (most widely
used technique with surgical treatment of clubfoot) and end results in
149 feet. The author reports that the best results and fewest
complications occurred in patients operated on between 1 and 2 years of
age.
R, Staheli LT, Chew DE et al. Measurements on radiographs of the foot
in normal infants and children. J Bone Joint Surg 1988;70A:407. The
authors present a radiographic review of feet of 74 normal infants and
children ranging in age from 6 to 127 months. The authors present their
results and compare these to results gleaned from the literature in
other studies of normal feet.
review article on the epidemiologic and etiologic theories on
idiopathic clubfoot should be read in conjunction with this author’s
article listed under Calcaneal Valgus.
PTP, Wheelhouse WW, Shiavi R et al. Habitual toe-walkers: clinical and
electromyographic gait analysis. J Bone Joint Surg 1977;59A:97. The
authors report a clinical and electromyographic study of six children
who are habitual toe-walkers compared to six otherwise normal children
walking on their toes. The abnormalities noted on dynamic
electromyograms reverted to normal in the habitual toe-walkers after
plaster cast treatment.
authors reported on 20 patients with an average follow-up of 3 years
(range, 1.5 to 7 years), all treated by Achilles tendon lengthening.
All children were otherwise normal. The surgical outcome was good in
every patient.
authors report dynamic electromyograms in 18 patients with idiopathic
toe-walking as compared with normal children walking on their toes and
cerebral palsy children with equinus deformities. Significant
differences in phasic time were demonstrated between cerebral palsy and
idiopathic toe-walking patients versus controls, but no significant
differences were noted between idiopathic toe-walkers and the cerebral
palsy patients. Because of these gait abnormalities, the authors
conclude that idiopathic toe-walking may be due to an unknown nervous
system deficiency.
excellent review article covers not only torsional abnormalities but
also angular deformities of the lower extremity. It includes excellent
references.
authors measured anteversion in 44 hips in 32 patients with idiopathic
osteoarthritis of the hip and compared this with measurements in 98
normal adult hips. The differences in the two groups were not
significant. The authors did not find medial femoral torsion associated
with osteoarthritis of the hip.
HB, Weiner DS, Cook AJ et al. Relationship between femoral anteversion
and osteoarthritis of the hip. J Pediatr Orthop 1989;9:396. In
a CT scanning study, the authors demonstrated no difference in
anteversion between osteoarthritis subjects and controls with reference
to anteversion. They concluded that rotational femoral osteotomies to
prevent osteoarthritis are not warranted.
author briefly discusses rotational problems in infants and children
and presents the indications and methods of surgical treatment in the
rare cases that require operative intervention.
LT, Corbett M, Wyss C et al. Lower-extremity rotational problems in
children: normal values to guide in management. J Bone Joint Surg
1985;67A:39. The authors present the rotational
profile and the normal values for progression angle, medial rotation,
lateral rotation, and thigh-foot angle. This is a classic reference
article for torsional deformities of the lower extremity.
