Principles of Fractures
shape and structure of the body. Bone provides origin and insertion
sites for muscles and tendons, and is critical for locomotion. Bones
such as the skull, sternum, and ribs protect vital organs. Finally,
bone is a reservoir for minerals, and plays a role in mineral
homeostasis.
cells and matrix that comprise bone are constantly remodeling in
response to changes in loading. Bone is unique in that it is a
self-repairing tissue. As microdamage is accumulated, an infinitely
complex and well-orchestrated cascade of cellular events works to
repair it. Bone can alter its properties and geometry in response to
changes in mechanical load and metabolic demand. Bone is capable
restoring the structural and functional roles of the tissue even after
a catastrophic failure (fracture).
stimuli. The mechanical environment around the bone can induce changes
in structure. Bone responds to increased loads by increasing the amount
and density of tissue, and by changing
shape
in order to optimally withstand applied forces. Similarly, disuse
results in osteopenia. With less force applied to bone, the quantity
and density of bone will diminish to match the perceived demand. Bone
structure and quality is also sensitive to the complex biochemical
cascades that accompany certain metabolic disorders, aging, and
exposure to drugs such as glucocorticoids and bisphosphonates.
amount of collagen, mineral content, and overall density. Bone is like
a two-phase material consisting of a collagenous matrix and a
mineralized crystalline lattice. The collagen matrix is stronger in
tension than in compression. The mineral phase of orderly apatite
crystals is stronger in compression than tension.
different when load is applied in different directions. The tensile
strength of bone is greater when it is loaded along its longitudinal
axis, compared to when it is loaded perpendicular to the longitudinal
axis. Therefore, cortical bone is weak in tension and shear, but tough
under compression. For weight-bearing bones, this appears to be
adaptive.
different when load is applied at different rates. More energy can be
absorbed by bone at higher loading rates than lower loading rates.
Therefore, the more strenuous the activity, the stronger the bone. The
elastic component defines maximum deformity that is achieved prior to
failure. The viscous component determines the time taken to reach the
maximum deformity.
to failure is a reflection of ductility or brittleness. Ductile
substances can undergo a large amount of deformation prior to failure.
Brittle substances have ultimate strains similar to yield strains.
Failure occurs under very small deformations. Cortical bone is ductile
in loading under compression. Cortical bone exhibits a ductile to
brittle transition as the strain rate increases.
to density. Density can vary greatly from area to area. Bone can easily
regulate its strength and stiffness by adjusting density. Subtle
changes in density result in large changes in strength.
absorbed by bone during loading is released within the bone as it
fractures. Extrinsic and intrinsic factors affect bone failure. The
extrinsic factors are the external forces applied to the bone. The
magnitude and area of force distribution, as well as the rate at which
the bone is loaded are important factors in fracture occurrence and
pattern.
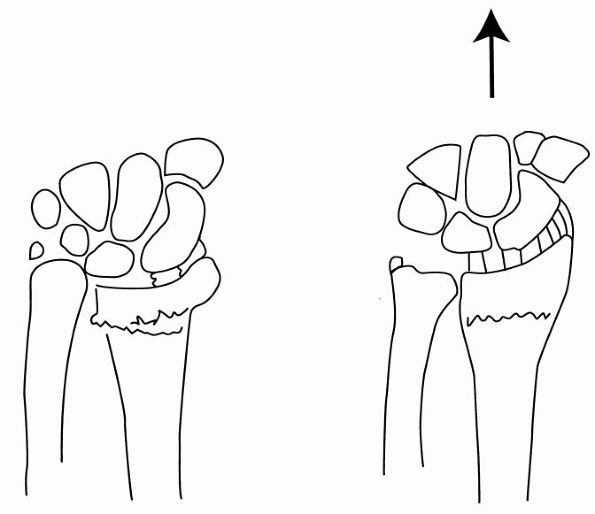
shear, or a combination of forces. Because bone has particular
mechanical characteristics, specific loads applied at specific
directions and rates will produce predictable patterns of failure. A
pure tensile force will produce a transverse fracture. An uneven
bending force results in an oblique fracture. The cortex under
compression breaks before the transverse tension failure is complete.
This results in comminution or a butterfly fragment at the site of
compression. Spiral patterns of fracture are result of torsional load.
With torsion, some bending force coexists, which limits endless
propagation of the spiral. Pure compressive forces result in uniform
impaction. Four-point bending produces two sites of tension, and a
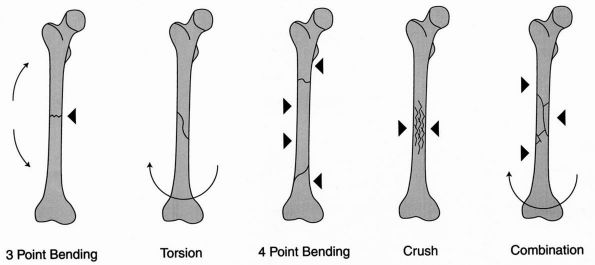
segmental fracture results (Figure 4-1).
biomechanical characteristics, or how much energy the bone can absorb
prior to failure (toughness). Because bone is anisotropic, it absorbs
more energy prior to failure if the load is applied in the longitudinal
axis of the bone. Conversely, it takes less energy to fracture if the
bone is loaded perpendicular to the longitudinal axis. Because bone is
viscoelastic, the rate of loading affects the amount of energy the bone
can absorb. With higher loading speeds, more energy is absorbed, and
failure results in more damage to the bone structure, reflected in the
degree of comminution of the fracture pattern. Lower loading speeds
allow less energy to be absorbed prior to failure, resulting in a
simpler fracture pattern.
three phases: crack initiation, crack propagation, and complete
structural failure. Repetitive loading over long periods results in the
development of microcracks. Irregularities in the microstructure, such
as Haversian canals, lacunae, or canaliculi act as stress risers and
are the sites of crack initiation. The repair response to accumulated
microdamage is termed adaptation. Adaptation is targeted at the repair
of microdamage. If the repair response is insufficient, crack
propagation will proceed, resulting in a slow
but
steady decrease in strength and stiffness of the bone. As microcracks
propagate, larger cracks form in interfaces such as cement lines
between osteons. If crack propagation continues, cracks become larger
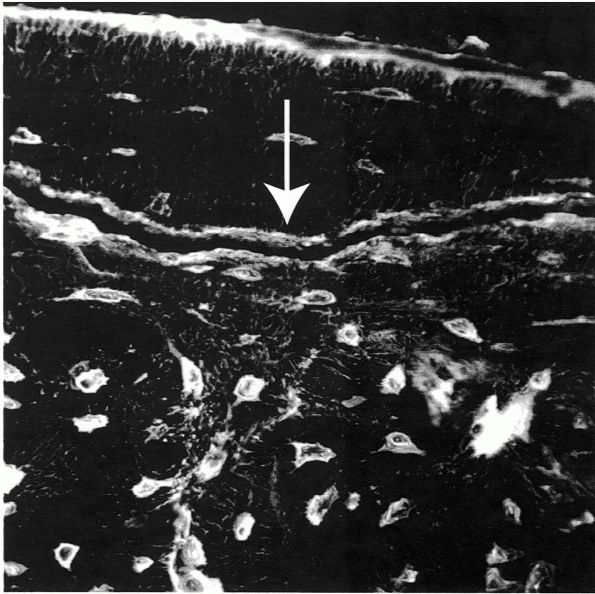
and coalesce (Figure 4-2).
The mechanical properties of the bone cannot support additional load
and a fracture occurs. Areas of the bone experiencing tension forces
have more microdamage than areas under compression. Fatigue damage
increases with increasing strain rate.
 |
|
FIGURE 4-1. Bone fails differently under different loading conditions.
|
 |
|
FIGURE 4-2.
Confocal microscopic image of cortical bone after subcatastrophic fatigue loading. Osteocytes and their canalicular networks are outlined in white. The arrow demonstrates a microcrack. |
application of strain. Fatigue fracture can also occur with fewer
cycles or less strain in pathologic bone. Fatigue fractures are often
not associated with a specific traumatic event and occur in previously
adapted bone. Alterations to peak strain, number of loading cycles, the
quantity of microdamage within bone, and the adaptive response are key
variables that influence the risk of fatigue fracture.
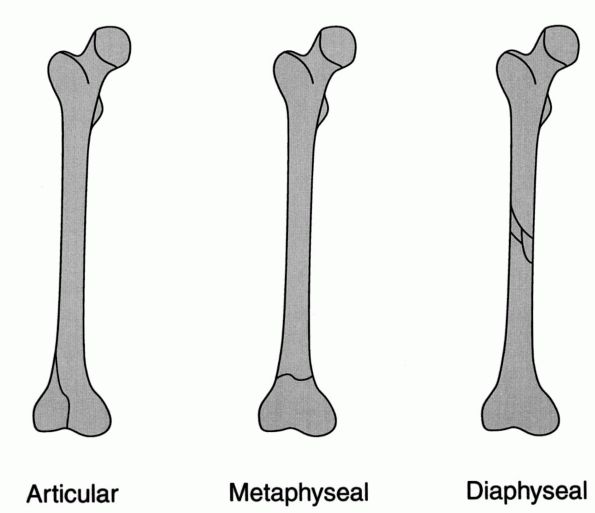
of the bone that is injured. Further descriptive terms can be used that
describe the anatomic location injured, such as diaphyseal or
metaphyseal (Figure 4-3). The morphology of the
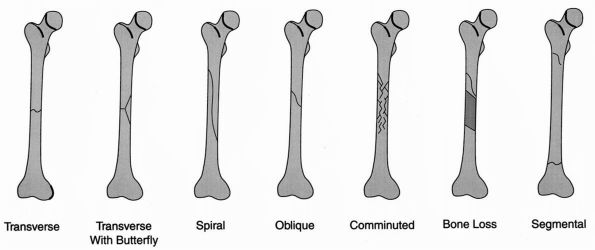
fracture can be described. Common terms include, but are not limited
to, transverse, oblique, spiral, or comminuted (Figure 4-4).
A fracture can be described as intra-articular if it involves a joint
surface. An impacted fracture occurs when the diaphysis is driven into
metaphyseal trabecular bone. A greenstick fracture indicates an
incomplete or bending fracture. A compression fracture of the
metaphyseal region with cortical buckling in a child is a torus
fracture.
of the periosteum, local blood vessels, and muscle always accompany a
fractured bone. Occasionally the soft tissue injury includes major
named arteries or nerves, subcutaneous tissue, and skin. When the skin
is violated, the fracture is termed an open fracture (Figure 4-5).
 |
|
FIGURE 4-3. The anatomic location of a fracture.
|
alignment, they are displaced. Displacement is described by the
position of the distal fragment relative to the proximal fragment.
Alternatively, displacement with angulation can be described by the
direction of the apex of the fracture (Figure 4-6).
systems have been created to organize almost every type of fracture.
The intent of creating a classification system is to highlight
particular variations in a specific type of fracture. These variations
are used either to select a treatment algorithm or assist in predicting
outcome. Several comprehensive fracture classification schemes have
been created to compartmentalize all fractures. The two most frequently
used are the AO/ASIF and Orthopaedic Trauma Association (OTA)
classification systems. These systems are used primarily as research
tools and, to a lesser extent, to communicate between medical
professionals. More often, descriptive terms are used.
 |
|
FIGURE 4-4. The pattern of the fracture.
|
normal bone exceeds its capacity to absorb energy. An example is the
fracture of a humerus in a motor vehicle crash (Figure 4-7).
physiologic forces on abnormal bone. The bone in a pathologic fracture
is weakened by a neoplastic process. Both primary bone tumors and
metastases can cause destruction of the bone structure and impairment
of the adaptation response, rendering it vulnerable to failure under
normal loads (Figure 4-8). Pathologic fractures
have also been associated with osteopenia from abnormal bone
metabolism; these are also referred to as insufficiency fractures (Figure 4-9).
recruits and athletes. Repetitive physiologic load can produce
microcracks that propagate to nondisplaced fractures before significant
repair can occur. It has been theorized that muscle fatigue plays a
role in this mechanism of injury. Skeletal muscle normally diverts some
stress from the bone, but with muscle fatigue, this protective maneuver
is lost (Figure 4-10).
 |
|
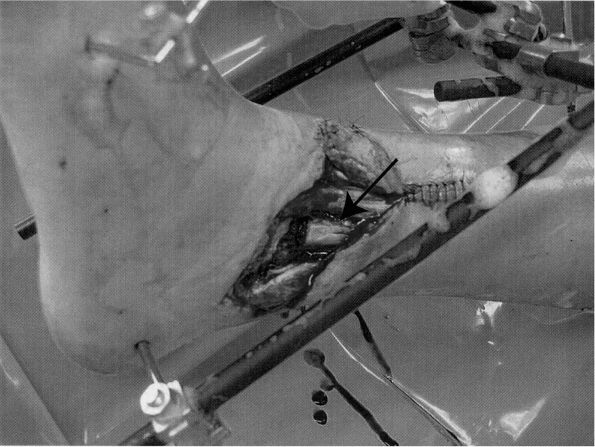
FIGURE 4-5.
The photograph demonstrates an open ankle fracture stabilized with a bridging external fixator. Note the exposed fibula in the wound (arrow). |
 |
|
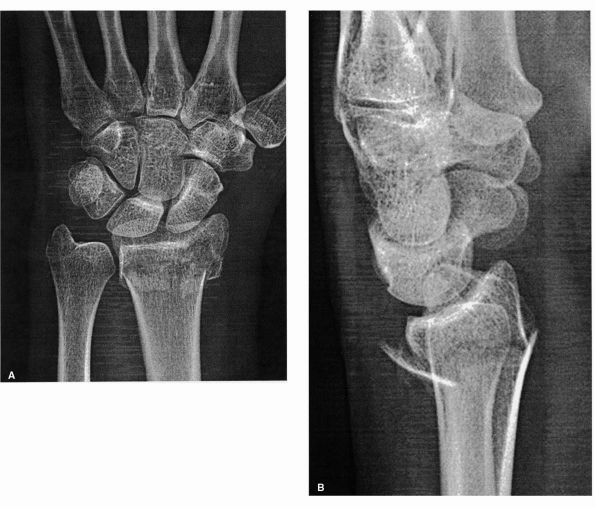
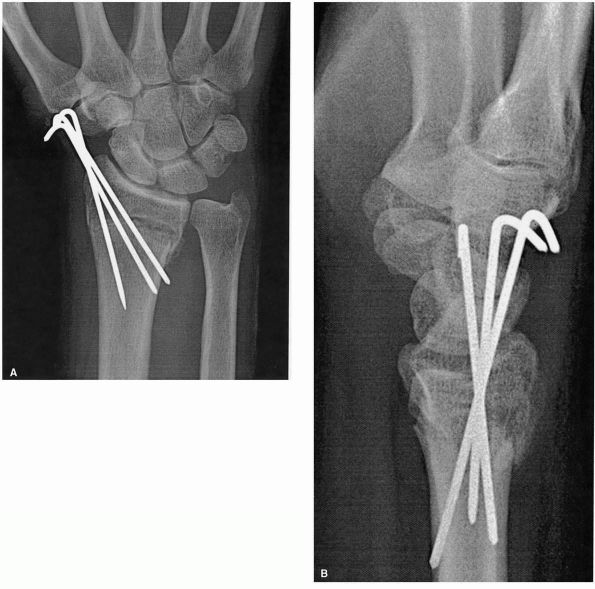
FIGURE 4-6. Posteroanterior (A) and lateral (B)
radiographs of the wrist demonstrate a displaced distal radius fracture. The displacement is posterior, or dorsal. The displacement can also be described as apex anterior angulation. |
 |
|
FIGURE 4-7. Anterioposterior radiograph of the humerus demonstrates a traumatic fracture.
|
them. A single application of force sufficient to cause a fracture can
be applied directly or indirectly. Direct trauma such as the
application of blunt, crush, or penetrating force to the body will
cause soft tissue injury and fracture at the site the force was applied
(Figure 4-11). Indirect trauma includes
tension, angulation, rotation, compression, and a combination of forces
applied at an area remote to the fracture. Transmission of forces
through muscle contractions results in a fracture. An example of an
indirect force causing fracture is the strong contraction of the
triceps with a fixed forearm, resulting in an olecranon fracture (Figure 4-12).
 |
|
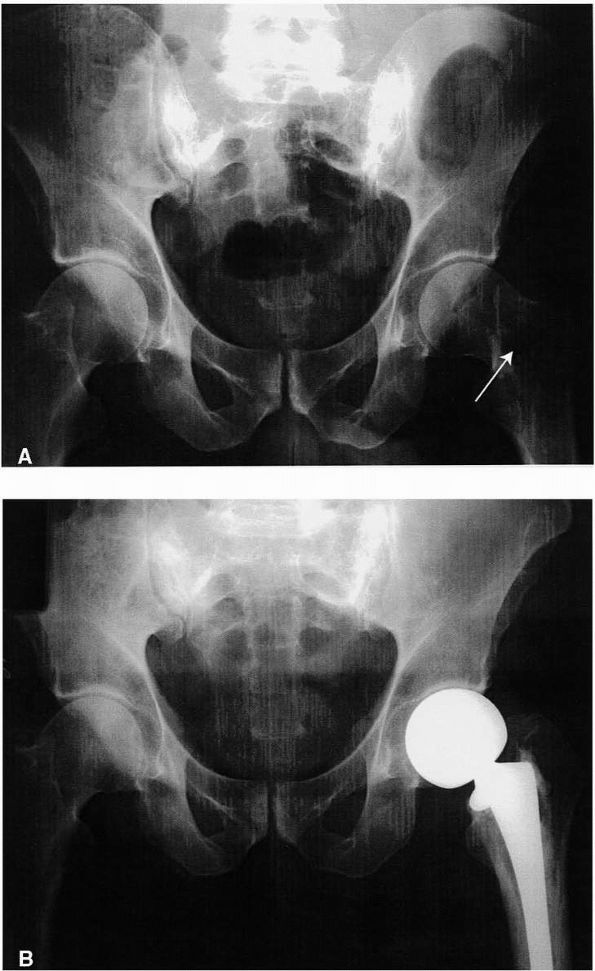
FIGURE 4-8. (A) Anterioposterior radiograph of the pelvis demonstrates multiple myeloma in the femoral neck (arrow). There is a nondisplaced pathological fracture of the basicervical region. (B) This fracture was treated by curettage and cemented hemiarthroplasty. Immediate weight bearing was allowed.
|
triggers a biologic response that starts the repair process. Bleeding
occurs from the ruptured periosteum and surrounding muscle. Bone marrow
contents are released into the vicinity of the fracture and can be
distributed systemically. Inflammatory mediators such as prostaglandins
and leukotrienes are released.
 |
|
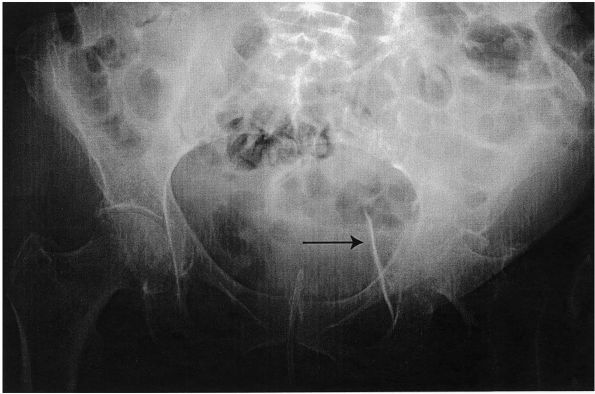
FIGURE 4-9.
An anterior-posterior radiograph of the pelvis demonstrates profound osteopenia in an elderly woman. A fall from a standing height produced a displaced acetabular fracture and central hip dislocation (arrow). This is an insufficiency fracture. |
force has been applied that would cause failure of the bone. A
supraphysiologic load applied to a normal bone, for example during a
motor vehicle accident, is appropriate to cause a tibial shaft
fracture. Passive range of motion of the knee is not an appropriate
force to cause a tibial shaft fracture in a normal ambulatory person,
but is an appropriate mechanism for a paraplegic with severe disuse
osteopenia and spasticity. The absence of an appropriate mechanism of
injury should warrant a search for abnormal bone. Neoplastic
conditions, metabolic disorders of bone, and the clandestine use of
drugs that adversely affect bone metabolism (glucocorticoids) may be
diagnosed by a fracture. An inappropriate mechanism of injury may also
suggest a situation of abuse and should be suspected in those with few
defense mechanisms (children, women, elderly, disabled.)
patient and the area of the body injured. General signs include pain,
swelling, deformity, abnormal mobility, and loss of function. Pain is
caused by bleeding, swelling, abnormal motion on surrounding soft
tissues, and release of inflammatory mediators. Deformity and abnormal
mobility are due to lack of structural support that the bone provides.
Altered function of a limb is a function of pain and lack of normal
structural integrity. Inability to walk or painful ambulation is a
reliable sign of spine or lower extremity fracture in those with poor
communication capacity, such as children and the elderly. Radiographs
confirm the clinical suspicion.
function, both temporarily and permanently. With the diminished ability
to use a limb, the patient experiences functional losses. The injured
patient’s role in the family and society is often altered. The capacity
to earn a living is compromised, and medical bills can be significant,
leading to emotional concerns and financial strains. Patients often
have problems adjusting to their disability and suffer psychological
sequelae related to change in body image and function. Laborers with
fractures that lead to permanent disability often need to retrain and
find more sedentary vocations.
differentiated from multiply injured patients. The effect of multiple
fractures on the systemic physiology is not the same as the sum of the
individual fractures. Bleeding from multiple fractures can produce
shock. Pelvic fractures with displaced sacroiliac dislocations, sacral
fractures, and symphyseal disruptions can be associated with
life-threatening hemorrhage from ruptured pelvic veins. Injuries to
named arteries can also occur with pelvic and acetabular fractures, and
can produce rapid and profound hemorrhage. Fractures with associated
arterial injuries can also be a source of shock. For example,
scapulothoracic dissociation is associated with injury to the
subclavian vessels and can lead to
rapid
and significant blood loss. Thighs with broken femurs can accommodate
one liter of blood. Multiple open fractures can be a source of
significant external blood loss. Multiple skeletal injuries in
combination with visceral injuries can produce significant bleeding and
consumption of platelets and coagulation factors.
 |
|
FIGURE 4-10. Lateral radiograph of the tibia demonstrates a subacute stress fracture of the tibial diaphysis (arrow). Note the sclerosis surrounding the fracture cleft.
|
circulation is increased with multiple fractures. Although this occurs
to some degree with every fracture, certain patients react with a
clinical syndrome known as fat embolism syndrome. Respiratory
insufficiency is the primary clinical sign, ranging from increased
oxygen demands to full-blown acute respiratory distress syndrome
(ARDS), which can be fatal. Other clinical manifestations include
petechiae, anemia, thrombocytopenia, and central nervous system
dysfunction. The cause not completely understood, but hypotheses
include microcirculatory occlusive phenomenon, generalized
inflammation, and cell membrane dysfunction. It is also not understood
what factors make some susceptible to develop fat embolism syndrome,
while the same clinical situation does not produce the syndrome in
others.
 |
|
FIGURE 4-11.
Anterior-posterior radiograph of the forearm demonstrates an injury from direct penetrating trauma. Massive comminution reflects the high energy nature of the injury. |
venous thromboembolism and pulmonary embolus. The factors important in
thrombogenesis are
venous
endothelial injury, venous stasis, and activated coagulation. A
fracture results in diffuse intimal damage in the vessels in the zone
of injury. With immobilization of an injured limb, the forceful muscle
contractions that facilitate venous return to the heart are minimized,
and stasis occurs in the veins. Prolonged recumbency from multiple
injuries increases the risk of venous stasis exponentially. Without
prophylaxis, venous thromboembolism occurs in the majority of injured
patients. Pulmonary embolism is the leading cause of death in those who
survive the initial injury.
 |
|
FIGURE 4-12.
Lateral radiograph of the elbow demonstrates an injury from an indirect source. A nondisplaced fracture of the olecranon was caused by strong contraction of the triceps with a fixed forearm. |
periods in the recumbent position to manage the skeletal instability
and pain. Multiple adverse affects of this position have been observed.
Pulmonary function is compromised due to suboptimal ventilation. Pain
results in poor inspiratory effort and positioning leads to
atelectasis, dependent edema, and aspiration. Narcotic pain medications
decrease the respiratory rate. The sum of these factors leads to
hypoxia and pneumonia. Nutrition is compromised due to the adverse
effects narcotic medication has on gastrointestinal function and
difficulty eating in an atypical position. With pain and decreased
mobility, urinary catheters are needed, which ultimately lead to
urinary tract infections. Immobility leads to skin breakdown and deep
venous thrombosis. In this patient population, early surgical treatment
of multiple fractures, especially pelvic and femur fractures, reduces
time in bed, and greatly improves outcomes.
realignment and splinting. Realignment of a grossly angulated limb will
improve arterial flow and venous drainage distal to the injury.
Bleeding will diminish as the volume around the fracture is reduced,
and tamponade can occur. Nerve function improves when anatomically
aligned.
techniques. Simple manipulation of an angulated limb into a more
anatomic position is recommended. Longitudinal traction is the simplest
way to reduce a fracture. Generally, the segment that can be controlled
manually is realigned to the less mobile segment. More challenging
techniques include reduction maneuvers where the deformity is
accentuated, then corrected. The maintenance of alignment after the
latter technique depends on an intact soft tissue hinge around the
fracture. Impediments to realignment include interposed soft tissue
between the fracture ends and lack of soft tissue hinge around the
fracture, making the reduction difficult to maintain.
splinting. Gross contamination can be removed, but formal irrigation in
the emergency department is not recommended. Reintroduction of a
contaminated bone end into the wound is tolerated. The entire wound
will be subsequently debrided in the operating room. A sterile dressing
should be applied over the wound and maintained until the patient is in
the operating room.
alignment of a limb with a fracture and decreases motion at the
fracture site. Limitation of excessive fracture motion may prevent
additional injury to vulnerable soft tissues. There is always concern
that an unsplinted closed fracture may be converted into
an
open fracture from the motion of sharp bone ends. Splinting reduces
bleeding and release of marrow elements from the fracture site, and
thus may contribute to resuscitation. By reducing pain, patient
transport and evaluation are facilitated.
variety of fractures. In a hospital, simple materials can be effective
splints. Sheets folded to a swathe or commercially available slings can
help reduce pain for clavicle, scapula, or proximal humerus fractures.
Padded fiberglass or plaster slabs can be customized to splint
fractures of the humerus, forearm, wrist, and hand, as well as
fractures distal to the knee. Prefabricated adjustable knee
immobilizers are helpful in splinting injuries around the knee. A
circumferential sheet can be tied around the pelvis and thighs to
reduce the pelvic volume in an open book pelvic ring injury. Pillows or
sandbags can be used to reduce the motion of a fractured femur.
Philadelphia collars or sandbags can immobilize a cervical spine
fracture. A long rigid board is the method of choice for spine
splinting.
general condition of the patient is optimized, and the patient will
tolerate the process of treatment. The goals of treating the injured
patient are to save life first, then save limb, and limit disability.
The goals of fracture treatment are to obtain stability of the injured
limb, facilitate healing, and accelerate rehabilitation.
important to consider when deciding on a definitive treatment plan. The
overall condition of the patient is of utmost concern. For multiply
injured patients, resuscitation is necessary. Multiple fractures, as
well as visceral injuries, can cause significant hemorrhage. Suboptimal
perfusion of organs can occur from this hemorrhage and is referred to
as shock. Shock can be manifested by tachycardia, hypotension, changes
in mental status, peripheral vasoconstriction, poor urine output, and
ultimately death. Laboratory findings involving shock can include
anemia, thrombocytopenia, and elevated clotting times, which represent
bleeding and consumption of coagulation factors. As perfusion
decreases, cellular metabolism turns from aerobic to anaerobic,
liberating the waste product lactic acid. Lactic acid production
results in metabolic acidosis.
principles are to stop ongoing hemorrhage and replenish lost
circulating volume . This is accomplished with infusions of lactated
Ringer’s or normal saline solution, or blood products, if hemorrhage
has been significant. Transfusion of red blood cells, platelets, and
plasma (containing coagulation factors) may be required to replace lost
circulating volume and replenish consumed factors and cells. Surgical
intervention may be necessary to stop hemorrhage. Surgical removal of
an irreparable bleeding organ (spleen) or ligation of bleeding arteries
may be a necessary component of resuscitation. Restoration and
maintenance of pelvic volume with external devices may be necessary to
promote tamponade of bleeding pelvic vessels after injury.
Alternatively, in some cases, angiographic identification and
intravascular embolization of major bleeding vessels is also in the
algorithm used to control hemorrhage.
patient is hemodynamically stable. Fracture surgery will result in
additional blood loss to an already compromised patient and may
contribute to the patient’s demise. Open fractures can be temporized in
a hemodynamically unstable patient with removal of gross contamination,
limited irrigation of exposed bone, placement of a sterile dressing,
and splinting. Definitive debridement and skeletal stabilization can be
performed when the patient’s condition is compatible with surgery.
Although this step may increase the rate of infection at the fracture
site, it may be a necessary precaution. Fracture surgery can be
considered when the patient’s blood pressure and heart rate have
stabilized, and when end organ perfusion is judged adequate. No active
hemorrhage should be ongoing, and hematologic parameters should be in a
reasonable range. General guidelines are a hematocrit around 30%, INR
< 1.4, and platelets > 80,000/mm3.
treatment of fractures. For patients with a head injury, secondary
brain injury is associated with hypotension and hypoxia. Operative
treatment of fractures in a poorly resuscitated patient may result in a
secondary brain injury. A severe pulmonary injury is a controversial
contraindication to early definitive fracture care.
patients are limited functionally by poor eyesight, diminished hearing,
and limited mobility
from
other medical conditions. Nonoperative treatment of some fractures
requires immobilization in a cast or brace. Casts or braces limit an
elderly person’s mobility and functioning more than similar
restrictions in a younger adult. Weight-bearing restrictions and the
introduction of crutches or a walker can significantly diminish an
elderly patient’s mobility and may contribute to subsequent falls and
injuries. Lack of ability to comply with weight-bearing restrictions
has led to loss of reduction and fixation. Additional problems seen
with external immobilization include skin breakdown, often contributed
to by poor sensation, delicate skin, and other comorbid conditions such
as diabetic neuropathy and vasculopathy. Access to medical care may be
limited, or patients may not want to complain, leading to delayed
diagnosis of pressure areas. After operative treatment of fractures,
mobilization of an elderly patient is much slower than in a young
adult. Irreversible loss of function also happens more frequently in
elderly patients. After hip fractures, only one-third returns to
preinjury function. Perioperative complications and death are more
common due to multiple medical problems and lack of physiologic
reserve. Malnutrition is common in the elderly, which delays wound and
fracture healing.
problems require comprehensive evaluation prior to definitive treatment
of the fracture. The presence or treatment of chronic medical problems
can lead to injuries. Syncope from a new antihypertensive medication or
existing arrhythmia can cause a fall in an elderly patient, producing a
hip fracture. New medical problems can also cause injuries. An acute
myocardial infarction sustained while driving can lead to a crash.
Optimization of the patient’s medical condition prior to surgery is
warranted. Any reversible problems such as dehydration, hypertension,
infections (urinary tract infection, pneumonia) and renal insufficiency
should be reversed. Any anticoagulation requires reversal, as well.
medical problems, extensive preoperative evaluation is often necessary
to understand the patient’s risk for significant perioperative
complications. With this information, a realistic discussion with the
patient and family of the risk-benefit ratio of surgery can be
performed. Chronic renal failure, congestive heart failure, chronic
obstructive pulmonary disease, hip fracture, and an age greater than 70
years have been identified as critical risk factors for inpatient
mortality. Postoperative complications associated with significant
increases in mortality include myocardial infarction, acute renal
failure, pulmonary embolus, pneumonia, and cerebrovascular accident.
Perioperative testing can also provide information that may modify the
perioperative plan. Those with significant pulmonary compromise may
elect to have regional instead of a general anesthesia to prevent
prolonged intubation and ventilation postoperatively. Decisions can be
made about the perioperative management of medical problems, including
the need for postoperative monitoring.
medical problems, fractures usually treated operatively may be treated
nonoperatively if the patient’s overall condition is not favorable.
Often there is a good salvage procedure if the patient has pain or
functional limitations with a malunion. A good example is an elderly
woman in a motor vehicle accident with a depressed tibial plateau
fracture. In isolation, the fracture would require surgical treatment
to correct limb axis deviation and knee instability. However, the
patient also suffered a blunt chest injury and has a pericardial
effusion, which has produced a new arrhythmia. The risks of immediate
surgery may be greater than the risks of reconstructive surgery done at
a later date, with an accepted salvage technique.
important to consider. An elderly nonambulatory patient would not
necessarily need operative treatment for a hip fracture if pain were
well controlled. A dentist would not be able to tolerate nonoperative
treatment for a mallet fracture. The splint required for successful
nonoperative treatment would not be tolerated with frequent hand
washing required by the occupation. A displaced intra-articular lower
extremity fracture in a paraplegic patient would not require operative
reduction and fixation, as it would in an ambulatory patient. However,
an upper extremity injury in a paraplegic patient may be treated
operatively to maximize function and limit disability, when it may be
treated nonoperatively in an ambulatory patient.
attention should be made to the skin condition, vascular inflow, and
innervation. Skin condition is important to observe, for it is a source
of morbidity with either nonoperative or operative
fracture
treatment. Acute changes in the skin from the injury include wounds,
hematomas, degloving injuries, ecchymoses, and blisters. Any wound in
proximity to a fracture should be considered an open fracture until
proven otherwise in the operating room. Degloving injuries are common
with crush or shear mechanisms of injury. The zone of internal injury
is often greatly underestimated by the external appearance of the limb.
The skin and subcutaneous tissue are separated from the underlying
fascia in an open wound, or without break in the skin. Degloved areas
may lead to infected seromas or hematomas. Incisions through a degloved
area are often ill advised. A degloving injury associated with an
acetabular fracture, referred to as a Morel-Lavallee lesion, is
associated with increased rates of surgical wound infection. It is
generally recommended that the degloving injury be treated and healed
before an incision is made in the area to treat the fracture. Areas of
poor skin quality from previous injuries, surgery, burns, grafts, or
ulcers, must be noted. Poor skin quality may affect the decision to
treat operatively, if the tissues can’t tolerate the incisions needed,
or nonoperatively, if the tissues can’t tolerate an immobilization
device.
consideration in treatment decision making. Changes in arterial inflow
of a limb are seen with acute injuries. An injury with an associated
fracture can cause diffuse vascular damage to the bone, periosteum, and
muscle. Fractures with injuries to major named arteries can occur with
penetrating trauma. Injuries to proximal arteries often, but not
always, result in limb ischemia. Injuries to more peripheral arteries
rarely produce ischemia due to the extensive anastamotic system present
between the vessels.
where capillary pressure is overcome. Diffusion of red blood cells and
delivery of oxygen at the cellular level is diminished. This
physiologic process is known as compartment syndrome. Left untreated,
the tissues in the limb become ischemic.
Skeletal muscle can tolerate approximately 6 hours of ischemia before
widespread irreversible myonecrosis occurs. Nerves are also
particularly sensitive to ischemia, although absolute tolerances are
not known. Prolonged ischemia may affect fracture treatment decisions.
Previously treatable fractures in a limb with prolonged ischemia may be
more amenable to amputation.
vessel can diminish vascular inflow to the point where wound and
fracture healing are impaired. Poor wound healing may increase the
chance of infection. Clinical signs of poor arterial inflow include
lack of hair on the ischemic segments, lack of palpable pulses, poor
sensation, and ulcers. Ankle/brachial index is a simple noninvasive
test that can quantify the adequacy of peripheral circulation in the
lower extremities. In patients with suspected vascular disease, a
vascular surgery consultation should be obtained to assess the adequacy
of blood flow to the limb. Reversible forms of ischemia can be
addressed, which may reduce the complications of the fracture
treatment. For those with irreversible ischemia, significant counseling
with the patient and family is necessary to understand the dire
situation. Often, the results of fracture treatment are poor and the
complication rate is high, whether operative or nonoperative treatment
is pursued.
operative and nonoperative treatment methods. An incision through
tortuous dilated veins leads to difficulty in hemostasis, bleeding,
hematoma formation, and occasionally difficulty with wound healing.
Varicosities predispose to venous stasis, especially in an immobilized
limb. The risk of venous thrombosis and pulmonary embolism are
increased.
changes in sensibility or motor strength are attributed to the injury.
Fractures can be associated with neuropraxia, axonotmesis, or
neurotmesis of named peripheral nerves. Loss of sensation in certain
areas of the body can be functionally debilitating. Loss of sensation
in the fingers from an injury to the radial, median, or ulnar nerves
can have adverse effects on dexterity. Loss of sensation to the plantar
aspect of the foot is important in making limb salvage treatment
decisions. Acute changes in strength in the setting of injury can be
attributed to direct musculotendinous injury or associated nerve
injury. These associated injuries will influence treatment decision
making.
most common cause of chronic sensory loss is diabetes mellitus, which
results in a diffuse peripheral neuropathy. Other common causes include
hereditary motor and sensory neuropathies, acquired compressive
neuropathy, radiculopathy, spinal cord pathology, peripheral vascular
disease, and medications. These conditions can also cause chronic motor
weakness. It is important to ask about any preexisting neurovascular
conditions, to fully appreciate the effect of the injury.
affect treatment plan. As aging occurs, there is a diminution in the
bone mineral density. Osteopenia is also seen in patients with
malnutrition, metabolic disorders, and chronic glucocorticoid use
(transplant recipients, systemic inflammatory disease). Cortical
diameters become larger to optimize the toughness of less dense bone.
Trabecular lines become thinner. Remodeling of accumulated microdamage
is diminished. This remodeling offers particular problems with
treatment decision making. Operative treatment of osteopenic fractures
is fraught with problems. Poor purchase of standard implants is
becoming more of a recognized problem. Poor fixation leads to loss of
reduction, resulting in a suboptimal outcome or the need for revision
surgery. Solutions to this problem include using different fixation
strategies in osteopenic bone and modifying existing implants to
strengthen the bone-implant construct. For example, for a patient with
an osteopenic hip fracture, intramedullary hip screws are supplanting
the use of dynamic hip screws. The intramedullary hip screw has the
mass closer to the axis of the bone, creating a stronger construct. New
implants have been developed that are ideally suited for fixation in
osteopenic bone. The traditional plate and screw construct has been
modified so that the threaded screw head engages a complementary
threaded screw hole. This modification creates a fixed angle construct.
Placing several locked screws in the plate creates multiple fixed angle
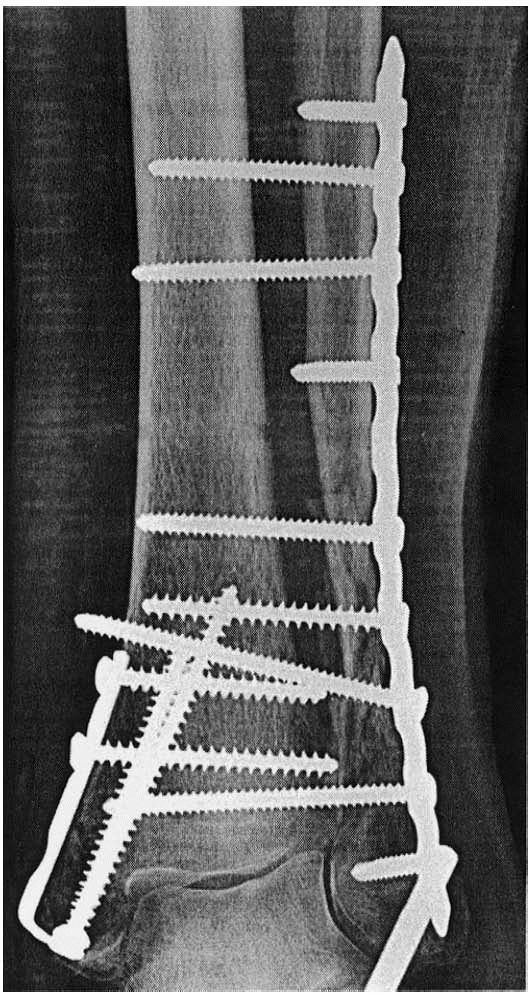
devices (Figure 4-13). This device fails
differently than traditional screw/plate constructs. Instead of
sequential loosening or breaking of screws, the locked construct fails
by catastrophic pullout of the entire device. This type of failure is
rare, even in osteopenic bone. These new implants have improved the
ability to maintain a reduction in osteopenic bone until the fracture
heals.
 |
|
FIGURE 4-13.
The photograph demonstrates a locking plate and screws. Note the threaded heads of the screws, which engage complementary threads in the plate hole. Multiple fixed angle devices are created, which drastically improves fixation in osteopenic bone. |
assessed. Fractures in different bones often require different
treatment plans. For example, metatarsal fractures are most commonly
treated nonoperatively because they heal well with minimal
intervention. Femoral neck fractures are more likely to
be
treated operatively to restore weight bearing immediately. The location
within the bone, pattern of fracture, and the amount of displacement
should be observed. In some bones, the amount of displacement and the
area in which the bone is fractured determines whether the injury is
treated operatively or nonoperatively. A nondisplaced diaphyseal tibia
fracture can be treated nonoperatively, where a displaced proximal
metaphyseal fracture in the same bone usually requires operative
treatment.
obtaining adequate alignment, and maintaining the alignment in an
external immobilization device. For nondisplaced fractures, no change
in alignment is necessary, and this step is skipped. For displaced
fractures, closed reduction improves alignment. Reduction can be
obtained by techniques such as the application of gentle axial
traction. The intact soft tissue hinge guides the fracture to the
correct alignment. The simplest example is having a patient with a
humeral shaft fracture sit up. Gravity provides longitudinal traction
on the arm, and the alignment of the displaced humerus fracture is
improved. When this technique depends on intact ligamentous attachments
around a fracture, it is termed ligamentotaxis (Figure 4-14).
Other times accentuation of the deformity is necessary to unkink a soft
tissue hinge before manipulation into the desired alignment is
performed. Fractures that can be reduced, and reductions maintained in
an external immobilization device are considered stable. Fractures that
cannot be reduced, or lose reduction in an external immobilization
device, are considered unstable.
stability achieved with the reduction of the bone. Common
immobilization devices include splints, casts, and braces. The external
immobilization device contributes a little to the stability of the
fracture by increasing the hydrostatic pressure around the fracture.
They will not prevent displacement of an unstable fracture. They
immobilize the injured part for pain relief and to prevent further
injury. They also position the limb in a way to prevent common
contractures.
 |
|
FIGURE 4-14.
This schematic demonstrates reduction of a displaced distal radius fracture. Longitudinal traction on bone fragments with ligamentous attachments leads to fracture reduction via ligamentotaxis. |
molded around a limb to provide immobilization of a fracture, without
circumferential compression. They are commonly used as the first
treatment of a fracture. The noncircumferential nature accommodates
swelling. Lower extremity splints are either short or long leg,
depending on whether the knee is immobilized. The ankle is always
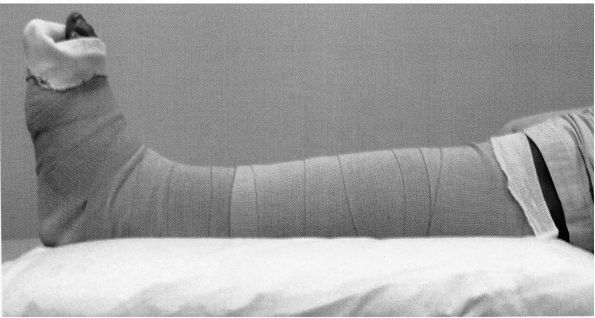
immobilized in a neutral position to prevent an equinus contracture (Figure 4-15).
Upper extremity splints are more varied. A long arm splint is commonly
used to immobilize a radial head fracture, where a short arm splint is
used on a distal radius fracture. Specialized upper extremity splints
include the coaptation, sugar tong, and gutter splints. A coaptation
splint is used to immobilize a proximal or shaft fracture of the
humerus. It consists of a U-shaped slab of padded plaster molded from
the axilla, around the elbow, then up the lateral arm and around the
shoulder. A sugar tong splint is a device used to immobilize a distal
radius fracture. It controls the flexion and extension of the wrist as
well as forearm rotation. A sugar tong splint involves a long slab of
plaster placed from the dorsal metacarpophalangeal joints,
along
the dorsum of the forearm, around the elbow, and to the
metacarpophalangeal joints on the anterior side. Full, unrestricted
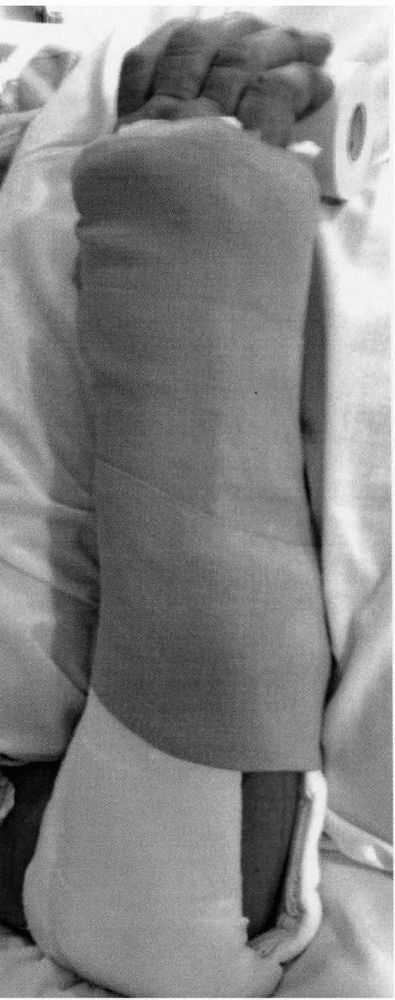
metacarpophalangeal motion should be allowed (Figure 4-16).
A gutter splint is applied to the radial or ulnar border of the hand,
and is commonly used to immobilize metacarpal fractures. The
metacarpophalangeal joints are immobilized in 70° to 90° of flexion, to
prevent contractures of the collateral ligaments (Figure 4-17). Splints are wrapped with ace wraps or other expandable covering to accommodate swelling.
 |
|
FIGURE 4-15.
A padded posterior plaster slab has been used to form a short leg splint. Ace wraps accommodate swelling. The foot is kept in a neutral position to prevent an equinus contracture. |
Plaster casts are moldable and can be shaped to fit the limb. Plaster
casts are applied over a few layers of cotton padding. The plaster
rolls are applied snugly and tucked where free ends are created. The
plaster is molded to the shape of the limb. The forearm and arm are
molded into flattened cylinders. The thigh is molded into a square
shape, and the leg into a triangle. Careful contouring over anatomical
structures such as the concavity of the palm and malleoli is performed
to fit the cast accurately to the complex geometry of the limb.
Three-point pressure can be applied to the cast while it is drying to
create a construct that supports the reduction. If angular alignment of
the fracture in the cast is suboptimal, wedging can be performed to
change the reduction a small degree. Wedging cannot be used to change
malreductions of length or rotation. Casts made of synthetic materials
cannot be molded as well as plaster. Casts made of synthetic materials
should be used when simple immobilization of a stable fracture is
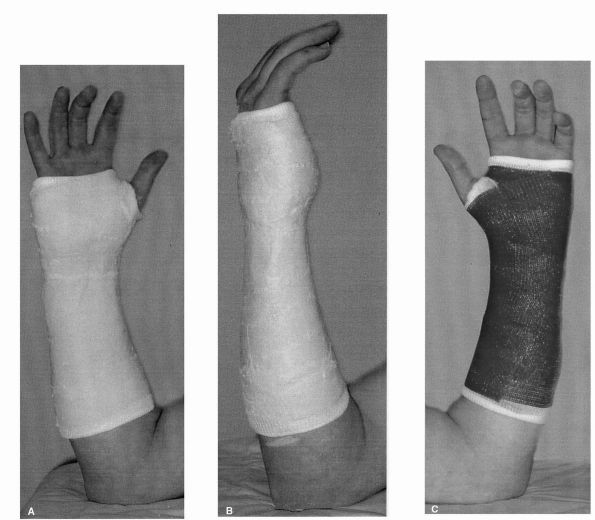
desired, and no maintenance of a reduction is required (Figure 4-18). Synthetic casts are also useful in preventing common contractures after injury.
their success. Patients should be instructed that their splints should
be left on. Many, not knowing this restriction, will remove the splint
if it becomes uncomfortable, and jeopardize the reduction. The
patient’s reapplication of the splint is usually not correct, leading
to pressure necrosis and contractures. Initially after the injury,
volume changes with dependency of the injured limb will manifest with
throbbing pain, tightness, and color change. Patients must be educated
to react to these sensations with elevation of the extremity,
preferably above the heart. Active movement of fingers or toes is also
encouraged to promote venous and lymphatic drainage, and prevent
stiffness of these joints. Pain or the sensation of unrelenting
constriction after a period of elevation should result in the patient’s
seeking medical attention to loosen or replace a too tight splint or
cast. Any complaints of rubbing or burning of the skin should be
investigated immediately for soft tissue injury. Patients should be
instructed not to stick anything into the cast, for it can cause skin
abrasion, laceration, or pressure necrosis. Casts and splints must be
kept clean and dry. Wet cast padding will cause maceration of the skin
and breakdown. Special synthetic liners are available that dry easily,
but are not used routinely.
 |
|
FIGURE 4-16.
A padded plaster slab is fashioned around the elbow and forearm to form a sugar tong splint for a forearm fracture. The metacarpophalangeal joints have unrestricted motion. |
skin breakdown. Focal pressure over a bony prominence or an inadvertent
depressed area caused by the surgeon’s ill-placed fingers may cause
skin and soft tissue pressure necrosis. Areas at risk are those with
little soft tissue covering, such as the ulnar styloid, heel, and
malleoli. Careful attention to padding and cast application will
minimize these problems. Patients’ attempts to soothe itching and
irritation under the casts with the insertion of long and often sharp
objects can also be the source of skin lacerations and abrasions. All
complaints of pain under a splint or cast should be investigated by its
removal and a thorough physical examination. A lost reduction can
always be regained, but an area of pressure necrosis can threaten the
viability of a limb. Extreme caution should be exercised when placing a
splint on a patient that cannot communicate the presence of discomfort.
Circumferential casts should be avoided in this patient population.
Diligent skin checks are required.
 |
|
FIGURE 4-17.
A padded plaster slab is used as an ulnar gutter splints to immobilize a metacarpal neck fracture. The fingers are included with the metacarpophalangeal joints at 70° of flexion and the interphalangeal joints in full extension. This “safe position” prevents contractures. |
contribute to increased pressure in the compartments of the injured
extremity. Because casts are nonyielding, swelling in the underlying
compartments can result in compartment pressures high enough to cause
ischemia to the limb.
All
complaints of unrelenting compression should be investigated. A cast
can be bivalved, and one half removed at a time to inspect the limb. A
reduction maintained by the cast, if lost by removing the cast, can
always be regained. The sequelae of compartment syndrome are
irreversible. Other complications of immobilization devices include
joint stiffness, peripheral nerve palsy, and regional pain syndrome.
 |
|
FIGURE 4-18. (A and B)
A short arm plaster cast is demonstrated. Note the molding of the cast to resemble the shape of the palm. The forearm is molded into a cylinder. (C) A fiberglass short arm cast is shown. Much less molding is allowed with this material. |
alignment and plays some role in reducing fracture motion by restoring
soft tissue tension. Traction can be applied to the skin or through the
skeleton. Skin traction is used in pediatric patients with femur
fractures. Skeletal traction involves placing a transfixion pin through
the distal femur, proximal tibia, or calcaneus. The pin is tensioned
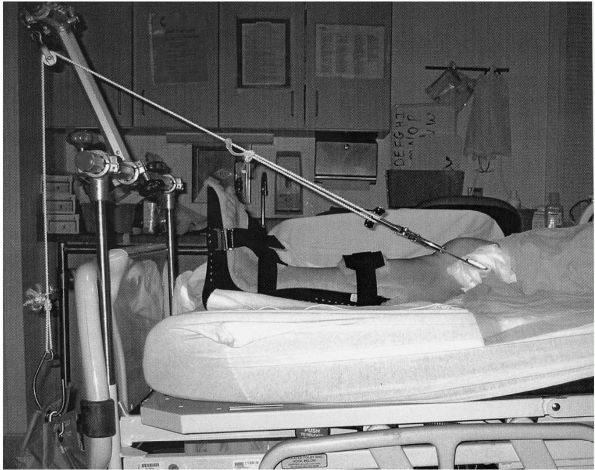
with a bow, and weights applied (Figure 4-19).
The pull of the weights should be executed in line with the femur if
traction is used for pelvic or femoral fractures, and in line with the
longitudinal axis of the tibia if used for tibial fractures. Complex
balanced suspension systems have been erected to suspend the limb;
however, a pillow under the leg is often all that is required to keep
pressure off the heel. Skeletal traction is useful in restoring pelvic
morphology when there is superior migration of a hemipelvis after
fracture. It is also used as a temporizing device in patients with
lower extremity
fractures
when the patient or the limb is not ready for definitive operative
treatment. In a patient with severe head injury, elevated intracranial
pressures, and a femur fracture, definitive treatment of the femur
fracture may result in secondary brain injury. Length and alignment of
the femur fracture can be maintained in traction until the brain injury
improves. Distal tibia fractures are often accompanied by major soft
tissue swelling and blistering. With the foot elevated on a
Braun-Bohler frame, calcaneal traction can maintain limb length and
alignment until the skin is ready for operative treatment.
 |
|
FIGURE 4-19.
A temporary skeletal traction set up is demonstrated in this photograph. A pin is placed in the distal femur. A prefabricated padded splint with heel relief is placed on the foot to prevent equinus contracture and to protect against pressure necrosis. |
treatment. If a patient with a fracture can’t tolerate surgery, or if
the fracture cannot be treated with the resources available, traction
can be used for definitive treatment. This technique is fraught with
complications associated with prolonged bed rest including global
deconditioning and muscular atrophy, skin breakdown, venous
thromboembolism, urinary tract infections, pneumonia, malnutrition, and
the development of psychiatric disorders.
first save life, then limb, joints, and finally to restore function.
Operative treatment of fractures does have a role in resuscitation and
can prevent mortality. Operative reduction of an anterior-posterior
compression type pelvic ring injury with external fixation can reduce
pelvic volume and facilitate tamponade. Judicious early stabilization
of pelvic and femur fractures has been shown to reduce mortality.
However, early definitive operative treatment of all fractures may not
be warranted. For a selected group of severely injured patients,
definitive stabilization of long bone fractures may be detrimental. A
more limited surgical approach with external fixation of pelvic and
long bone fractures to restore length and alignment, or “damage control
orthopedics,” may be a safer approach until the patient’s overall
condition improves. Limb salvage priorities involve debridement of open
fractures to reduce the risk of infection, vascular repair for ischemic
limbs, and soft tissue reconstructive procedures. Joint salvage
involves reconstruction of articular injuries, ligament reconstruction,
and implementation of a rehabilitation exercise program.
stabilization of the injured limb, which reduces pain, facilitates
mobility and rehabilitation, and shortens hospital stay. Operative
restoration of correct limb alignment and articular congruity maximizes
the chances of long-term successful rehabilitation. These benefits are
noted; however, there are risks associated with operative treatment
of
fractures. Bleeding may occur that requires transfusion. Risks
associated with transfusion include transfusion reaction, and the
transmission of bloodborne pathogens. HIV and hepatitis have been
transmitted by transfusion. Donor testing has reduced the risk of
transmitting HIV and hepatitis, but has not eliminated it. Other
bloodborne pathogens likely exist but are currently not identified.
Mutations in currently existing nonpathogens may yield new pathogens.
In addition, transient immunosuppression is seen with blood
transfusions.
factors for surgical site infections in orthopedic patients are related
to increasing age, additional nosocomial infections, wound
contamination, and number of operations. Open fractures have higher
rates of surgical site infections than closed fractures. The infection
rate in open fractures is even higher in the host with an immune
deficiency.
of morbidity and mortality in the United States. The number of
antimicrobial-resistant pathogens infecting wounds is on the rise.
Wound infections almost always require rehospitalization and further
surgery. Surgical debridements carry the risks of additional surgery.
Antibiotic therapy often involves an indwelling central venous catheter
and months of antibiotics. Antibiotics are potentially toxic to bone
marrow, liver, hearing, and kidneys.
of wound infections can be diminished but not eliminated. Factors in
correct prophylactic antibiotic usage include using the correct
antibiotic and redosing after two half-lives during the procedure.
Antibiotics should be infused prior to the start of the procedure, up
to 1 hour before. Prophylaxis should be stopped 24 hours after the
procedure, to prevent the development of antimicrobial-resistant
organisms.
knowledge of the surrounding anatomy. Injuries to nerves, arteries, and
veins have been reported with operative treatment of almost every
fracture. Nerve injuries can include neuropraxia or neurotomesis.
Surgery about the spine runs the risk of spinal cord or nerve root
injury. Vascular injuries can result in significant hemorrhage, and/or
limb ischemia, and often require an intraoperative vascular surgery
consultation. Tendon or ligament injury has also inadvertently occurred
during surgery.
include myocardial infarction, cerebral vascular accident, pulmonary
embolus, anesthesia complications, and nerve palsies and soft tissue
breakdown from positioning and unrelieved pressure. Death can occur
after fracture surgery. The rate of acute mortality after inpatient
orthopedic surgical procedures is approximately 1% for all patients,
and 3.1% for those having surgery for hip fractures.
surgical treatment. Some patient factors contribute to delayed healing.
Protein malnutrition, smoking, and use of nonsteroidal
anti-inflammatory agents all prolong healing times and may predispose
to nonunions. Surgeon-controlled factors include the degree of soft
tissue stripping around the fracture. Every surgical move has its
biological consequence. With every incision, the blood supply to the
fracture is diminished. Careful consideration should be made to
minimize iatrogenic ischemia to the fracture. Diminished blood supply
from aggressive soft tissue stripping leads to longer healing times and
higher infection rates.
include loss of fixation, loss of reduction, regional pain syndrome,
uncosmetic scarring, and stiff joints.
treatment of fractures. If acceptable alignment cannot be obtained, or
if the alignment cannot be maintained by nonoperative means, then
operative treatment is required. In some cases immobilization of a
fracture is morbid to the patient or to the limb. Operative treatment
of certain fractures is required to restore immediate weight bearing.
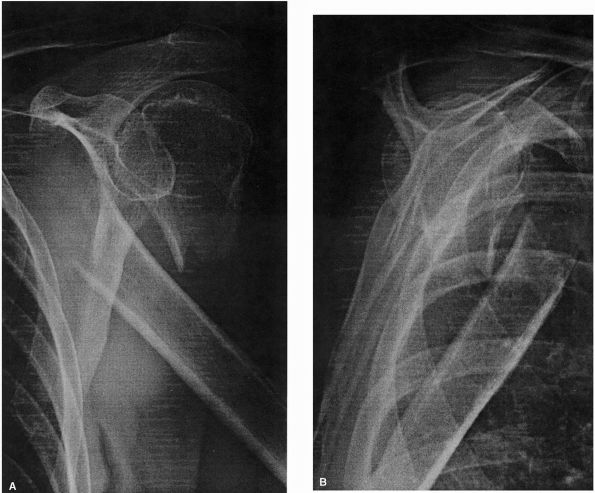
The vast majority of hip fractures fall into this category (Figure 4-20). Irreducible fracture dislocations require operative reduction and internal fixation (Figure 4-21). Some fractures have so much displacement, healing without open reduction is unlikely (Figure 4-22).
Open fractures are always treated operatively. Debridement of
contamination and devitalized tissue reduces the rate of infection.
Fractures associated with arterial injuries are treated operatively, to
restore perfusion. Skeletal stabilization prevents disruption of the
reestablished blood flow. Fractures with compartment syndrome are
treated with fasciotomy and bony stabilization. Stabilization of the
fracture prevents further soft tissue injury. Fractures caused by
pathological processes invading and weakening the bone are treated
operatively (Figure 4-8). Displaced articular fractures are thought to have the best outcome with anatomic reduction and internal fixation (Figure 4-23).
Finally, patients who are multiply injured mobilize better with their
fractures stabilized and have lower rates of morbidity and mortality.
Fractures that, if occurred in isolation, are treated nonoperatively,
such as humeral shaft fractures, can be treated operatively in multiply
injured patients. Certain areas of the body require immediate mobility
of the adjacent joints to prevent stiffness and diminished function.
The upper extremity is extremely sensitive to prolonged immobilization.
Fractures about the elbow and fingers are often treated operatively, so
enough stability can be obtained that immediate range of motion
exercises can be performed in the surrounding joints.
 |
|
FIGURE 4-20. (A)
Anterior-posterior radiograph of the pelvis of an elderly woman demonstrates a right intertrochanteric femur fracture with subtrochanteric extension (arrow). Note the previous left hip fracture treated with internal fixation. (B) The right proximal femur fracture was treated with an intramedullary hip screw. Weight bearing may start immediately postoperatively. |
 |
|
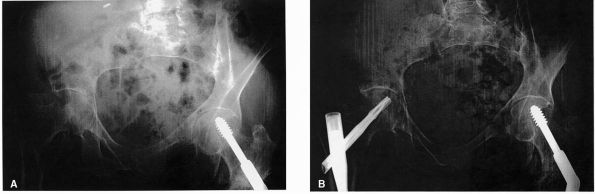
FIGURE 4-21. (A)
Anterior-posterior radiograph of the pelvis demonstrates a symphysis pubis diastasis and a fracture dislocation of the right hip. Reduction of the hip is impossible due to osteochondral fragments in the acetabulum. (B and C) Axial computerized tomography images further demonstrate the posterior dislocation of the hip and intra-articular blocks to reduction. Operative reduction and internal fixation of the fracture were required. (D) Postoperative anterior-posterior radiograph demonstrates a reduced hip and internal fixation of the acetabular fracture. |
 |
|
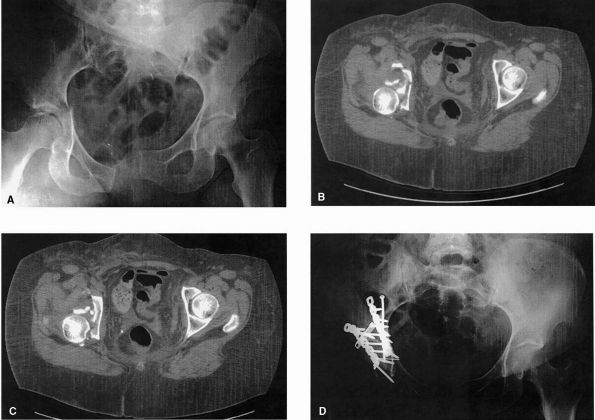
FIGURE 4-22. (A and B)
Anterior-posterior and scapular Y radiographs of the shoulder demonstrate a widely displaced humeral neck fracture. Healing is unlikely with this degree of displacement, and operative reduction and fixation are indicated. (C and D) Neer anterior-posterior and axillary views of the shoulder postoperatively demonstrate better reduction of the fracture and internal fixation with a locked plate. |
 |
|
FIGURE 4-22. (Continued)
|
 |
|
FIGURE 4-23. (A and B)
Mortise and lateral views of the ankle demonstrate a distal tibia fracture with intra-articular extension. Gap and step-off of articular fragments creates an irregular joint surface. (C and D) Postoperative mortise and lateral radiographs reveal reduction of the articular surface maintained by plates and screws. |
stability of a closed reduction. The small diameter wires have some
purchase on both cortices, which supplements the stability of the
construct (Figure 4-24). They have definite
limitations in their ability to hold a reduction in unstable fractures.
They usually lose any mechanical advantage within several weeks.
Percutaneously placed pins almost always require supplemental
stabilization with a splint, cast, or external fixator (Figure 4-25C and D).
 |
|
FIGURE 4-24. Posterior-anterior (A) and lateral (B) radiographs of the wrist demonstrate a distal radius fracture. Three Kirschner wires help maintain the reduction.
|
placed bicortically in bone, coupled to external bars and clamps. This
technique provides relative stability. External fixation has several
advantages. It can be quickly applied and is completely modular.
Pins
can be placed at the surgeon’s discretion, and the frame can be custom
built. The fixation construct can also be modified at will. External
fixation is the only fixation method where the surgeon has direct
control over the construct stability. Stability is increased with
anatomic fracture reduction, increased size of pins, increased pin
spread within a fragment, decreased distance of bars to bone, increased
number of bars, and a multiplanar frame. Conversely, the frame can be
destabilized to decrease the stability. It is a good way to maintain
proper length and rotation of the extremity. This is commonly referred
to as “traveling traction.” The technique is tissue friendly. Pins can
be placed around wounds or marginal
quality skin. The technique can also be used for reconstructive tasks such as deformity correction or distraction osteogenesis.
 |
|
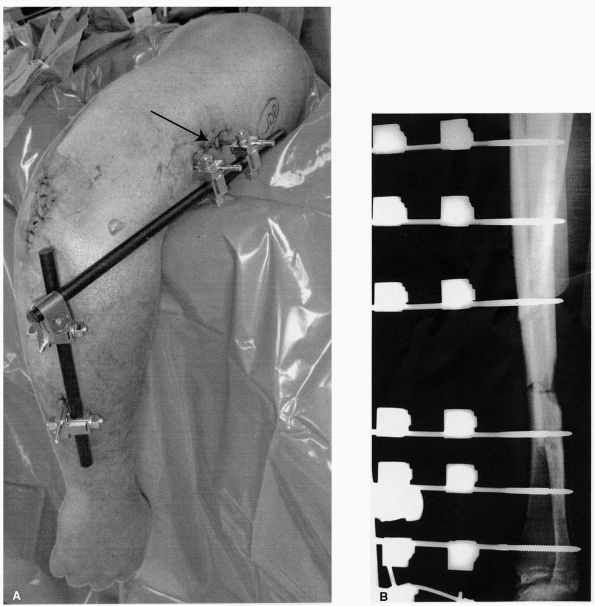
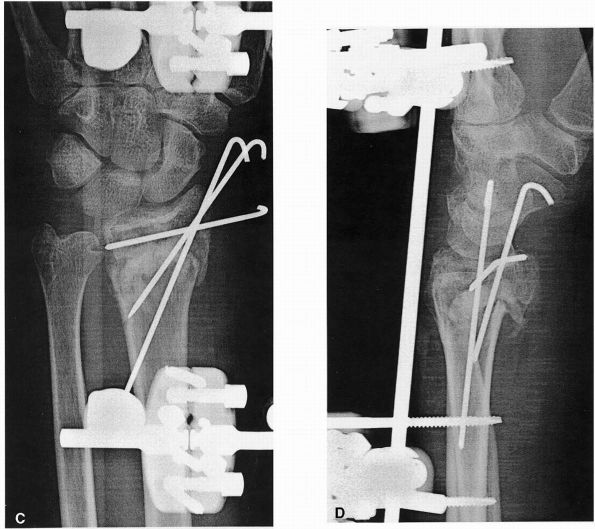
FIGURE 4-25. (A)
This clinical photograph demonstrates a simple external fixator used to stabilize an open distal humerus fracture. A generous incision was created to insert the humeral pins in an effort to avoid injury to the radial nerve. (B) Lateral radiograph of the tibia demonstrates a diaphyseal fracture with posterior bone loss. The reduction is maintained with an external fixator. Two sets of pin-to-bar clamps are seen anterior to the tibia. As the bone heals, the frame can be destabilized by gradually disassembling the construct. (C and D) External fixation is useful for definitive treatment of distal radius fractures. Anterior-posterior and lateral radiographs of the wrist demonstrate this application. The traction provided by the external fixator maintains the metaphyseal reduction with the assistance of Kirschner wires. |
 |
|
FIGURE 4-25. (Continued)
|
into the bone are large threaded pins or small tensioned wires. Pins
can be cylindrical or tapered. The pins are generally coupled to bars
and clamps, and thin wires are tensioned and connected to rings.
External fixation systems can be completely modular, or consist of
prefabricated frames with use directed toward specific regions (wrist,
ankle). New hinged external fixators are used to hold the reduction of
an unstable knee or elbow, while allowing range of motion of the joint.
lower extremity. In the femur, pins are placed into the anterolateral
quadrant. Tibial pins are inserted from the medial border. Talar and
calcaneal pins are inserted from medial to lateral, avoiding the medial
neurovascular bundle. In the upper extremity, pins are inserted through
a generous incision and dissection to avoid nerve injury (Figure 4-25A).
A thorough knowledge of cross-sectional anatomy is required before
placing small transfixion pins. At least two pins or wires should be
inserted into each fragment.
failure is the result of infection and loosening. Pin tract infection
is nearly universal. The incidence of infection varies by site. Fleshy
areas such as the arm, pelvis, and thigh have more pin site infections
than areas with less tissue, such as the tibia. Slight purulent
drainage or localized cellulitis is treated with increased local care
and oral antibiotics. If this fails, or cellulitis becomes regional,
systemic antibiotics are required. With advanced infection, osteolysis
occurs around the pin and can be visualized on radiographs. With the
pins loose, they must be removed, and the tract curetted. Osteomyelitis
or a sequestrum can develop from infected pins. Additional pins in
noninfected area may need to be placed to accommodate for the lost
stability of the construct.
no standard pin care system has been recommended. Physicians vary in
their recommendations from half strength peroxide, peroxide, Betadine,
soap
and
water, chlorhexidine solution, and dilute bleach. The pins should be
covered to prevent external contamination. Fleshy areas should be
compressed with the dressings to prevent pistoning of tissue on the
skin, which contributes to tissue necrosis and infection. Pins should
have complete release of the surrounding soft tissue. Tenting of the
skin causes necrosis, which predisposes the tract to infection. The
threaded portion of the screw should stay below the skin surface. Pin
tract infections will definitely affect future stabilization options.
In the tibia, a pin tract infection is considered a contraindication
for subsequent intramedullary nailing. This scenario is tolerated
somewhat better in the femur.
minimize pin loosening. Mechanical and thermal damage to the bone from
drilling and pin insertion can cause osteonecrosis, which weakens the
critical interface and predisposes to infection. Drills should be sharp
and irrigation cooled, and pins inserted under manual power. As the
rigidity of the construct increases, less strain on the pins occurs.
This also helps preserve the critical interface. Weight bearing on an
unstable fracture should be avoided. Stress overload at the pin-bone
interface puts pin at risk for failure. The bone-pin interface is
stronger in cortical than cancellous bone. Hydroxyapatite coating on
the pins improves osteointegration and the strength of the bone-pin
interface, and prevents loosening. This corresponds to a reduction in
infection of pin tract.
loose, and the frame will become ineffective in maintaining alignment
of the bone. This is why external fixation often leads to nonunion or
malunion when prolonged stabilization is required. Open tibia
fractures, which have long healing times, develop more malunions with
external fixation compared to intramedullary nailing.
Hydroxyapatite-coated pins have been shown to reduce malalignment with
external fixation systems left on for long periods of time, such as for
tibial lengthening.
until the patient or limb is ready for definitive stabilization. Care
must be taken with subsequent intramedullary nailing in the tibia, for
infection rates are higher. External fixation can also be used as
definitive treatment.
treatment for fractures that have an articular injury and metaphyseal
comminution. Distal radius and distal tibial fractures are common
fractures that fit this description. These injuries require precise
articular reduction with maintenance of correct length through the
comminuted metaphyseal segment. External fixation is usually applied to
preserve length of the limb, and articular reduction is performed
through small, directed incisions. Fixation in the metaphyseal and
diaphyseal sections are not required, they will heal with callus (Figure 4-25C and D).
dynamic mechanical environment. The modularity of the frame of an
external fixator allows the surgeon to slowly destabilize the frame as
the fracture heals, gradually applying more load to the bone and less
to the fixator (Figure 4-25B).
play a role in reconstruction. With large areas of bone loss, the
external fixator will allow acute shortening of the limb, followed by
gradual lengthening via distraction osteogenesis. This technique may
obliviate the need for formal soft tissue coverage with local or
rotational muscle flaps.
can be used to describe a variety of devices that are inserted into the
medullary canal of a long bone. These implants are used to stabilize
fractures, osteotomies, impending pathological fractures, and new
regenerate bone after lengthening.
physical characteristics. Flexible nails have small diameters and
uniform curvatures. Fixation is achieved by stacking several into the
medullary canal, or by placing the curved nail to achieve three-point
fixation. Larger diameter rigid nails are solid or hollow. Hollow or
cannulated nails may be inserted over a guide wire. Hollow nails can be
open section (slotted) or closed sectioned. Rigid nails may have
interlocking capabilities. Proximal and distal perforations through the
nail allow placement of screws that pass through bone and nail. Dynamic
locking of the nail is with interlocking screws in one end. This
locking allows some compression and micromotion at the fracture site.
This treatment should be used only with axially stable fractures.
Static locking uses interlocking screws in both fragments and is the
best technique to control length and rotation. Nails are inserted with
or without reaming. Reaming is the process where the intramedullary
canal is enlarged by a motorized rotary curette. This method allows for
the placement of a larger, stronger implant.
exposing the fracture. Traction, manipulation, and fluoroscopy are
required to achieve and maintain reduction. In open nailing, the
fracture site is exposed. Currently, the preference is to avoid open
nailing, except in certain subtrochanteric fractures where closed
reduction almost always fails. By default open fractures are nailed
with an open technique.
evolved over the past decades. Currently two types are used. Small
diameter flexible nails are curved to achieve three-point fixation in
the medullary canal of the bone. Multiple nails are used in the same
bone to achieve many points of contact and interference fit between
each other. These devices hold angulatory alignment well, but are less
proficient in maintaining length and rotation. They are often used in
children’s fractures (Figure 4-26C). Adult
femur and tibia fractures are treated with a cannulated interlocking
nail. The cannulated design allows the use of a smaller guide wire to
obtain the reduction. Reaming and nail insertion are performed over the
guide wire (Figure 4-26A and B). Static interlocking is generally performed.
 |
|
FIGURE 4-26. (A and B)
Anterior-posterior and lateral radiographs of the tibia demonstrate a statically locked intramedullary nail placed to stabilize a diaphyseal tibia fracture. Note the intramedullary nail in the femur as well. (C) Anterior-posterior radiograph of the femur in a child demonstrates multiple small flexible nails stabilizing a femoral shaft fracture. |
nail acts as a splint. Nail contact with the bone occurs at the
insertion site, diaphysis, and interlocking screws. There is some
motion at the
fracture
site. This promotes callus formation. As the bone heals, it gradually
assumes more of the load and less stress is seen by the implant.
Ideally, the bone-nail composite has enough fatigue resistance to allow
fracture healing to occur, yet is not overly rigid to impair the
physiologic stimulus for healing. One advantage of this technique is
that the implant is load sharing, and the construct is strong enough to
allow immediate weight bearing.
good fracture stability through a minimally invasive technique of
insertion. The soft tissue envelope around the fracture is preserved,
minimizing surgical devascularization of the injured bone. The implant
is central in the bone, close to the mechanical axis of the limb, which
is optimally positioned to reduce bending forces. Proximal and distal
locking control length and rotation. Early weight bearing, even in
comminuted fractures, is allowed with this configuration.
for fractures of the diaphyseal femur and tibia. New nail designs with
more peripheral and variable angle interlocking screws, and with
techniques such as blocking screws, can be used for fractures in the
metaphyseal area. Nailing is not always the best treatment method for
all long bones. Intramedullary nailing of humerus fractures results in
more complications, and more secondary surgery. Intramedullary nails
have also been developed for the fibula and forearm, but have limited
indications.
fixation, loss of reduction, and malunion occur, but are usually due to
poor patient selection or poor implant selection. The fracture is
usually too peripheral for the interlocking screws to hold the
reduction, and an alternative fixation scheme may provide more stable
fixation. Another source of healing problems is hardware failure.
Smaller interlocking screws used with smaller nails in tibia fractures
tend to break more often, however, hardware failure is not always
associated with nonunion or malunion.
patient, particularly the timing of femoral nailing, is often
controversial. For the vast majority of patients, fixation of long bone
(particularly femur fractures) within the first 1 to 2 days is
beneficial. Shorter duration of ventilator dependence, shortened length
of stay in the hospital, and lower rates of acute respiratory distress
syndrome, pneumonia, and other pulmonary problems has been reported. It
is thought that some multiply injured patients cannot tolerate early
intramedullary nailing of the femur or tibia. It has been proposed that
those patients with significant pulmonary injuries have higher rates of
adult respiratory distress syndrome and mortality after this procedure,
but others have disputed this conclusion.
of femur fractures in patients with closed head injuries and elevated
intracranial pressures. The fear is that the femur stabilization will
cause secondary brain injury. Factors associated with secondary brain
injury are hypotension, hypoxia, and subsequent decreased cerebral
blood flow. Cerebral perfusion pressure has been found to decrease
intraoperatively during reamed intramedullary nailing of the femur.
Early fixation of femur fractures in patients with head injury is
thought to be safe; however there is no clear-cut guidance from the
literature and treatment should be tailored to the individual patient.
fractures with unacceptable alignment after closed reduction and
immobilization, lower extremity limb malalignment, and articular
incongruity. In some cases open reduction and internal fixation is
warranted to allow immediate weight bearing, or because the patient’s
outcome will be better than nonoperative treatment.
is very important. Articular fractures are thought to require perfect
anatomic reduction for best outcome. Gaps or step-offs in the articular
surface produce areas of stress concentration, which is thought to lead
to posttraumatic arthrosis. However, not all joints require perfect
articular reduction for good results. The outcome of acetabular
fractures is dependent on the quality of reduction. However, there is
little proof that accurate articular reduction of tibial plateau
fractures is important for a good clinical outcome. The results in
intra-articular fractures about the proximal interphalangeal joint
depend more on maintaining joint reduction than articular reduction.
Other factors such as age and infection also affect the outcome after
articular fracture.
significant affect on function. The radius morphology must be
anatomically reduced to allow full
forearm rotation (Figure 4-27).
Metacarpal and phalangeal fractures must have no malrotation or the
fingers will not be parallel, which is functionally disabling. Apex
anterior angulation of a metatarsal neck fracture will lead to plantar
prominence of the metatarsal head, producing a painful prominence with
weight bearing.
correct axial alignment of the limb is just as important as the quality
of articular reduction. If a fracture malreduction leads to varus or
valgus alignment of the knee or ankle relative to the floor, ambulation
becomes awkward and painful, deformity results with subsequent
degenerative changes in the affected joints. For the femur and tibia,
varus and valgus tolerances approach 5°. Malrotation in the lower
extremities is poorly tolerated if the difference between limbs exceeds
10°. Shortening of the lower limb greater than 1 cm results in
symptomatic leg length discrepancy, and often requires orthotic
management.
 |
|
FIGURE 4-27. Anterior-posterior (A) and lateral (B)
radiographs of the forearm demonstrate anatomic reduction of the radius and ulna. The reduction is maintained by 3.5 mm low contact dynamic compression plates and cortical screws. Perfect reduction of the radius is critical in restoring full forearm rotation. |
Different fractures require different types of stability. Screws are
usually considered to be cortical or cancellous. Cancellous screws have
a larger outer diameter, a deeper thread, and a larger pitch than
cortical screws. Screws used to obtain compression across a fracture
site are termed lag screws. Compression occurs between the screw head
on one cortex, and thread purchase on the far cortex. Screws are also
used to secure a plate to the bone. Locked screws have threaded heads
that fit into a corresponding thread on the plate hole, creating a
fixed angle device (Figures 4-13, 4-28). Screws range in size from 1.1 mm to 7.3 mm. Screws can be solid or cannulated. Cannulated screws are placed over a smaller
guide wire, which may improve the accuracy of implant placement in critical areas.
 |
|
FIGURE 4-28.
Anterior-posterior radiograph of the ankle in an elderly woman. Note the profound osteopenia. This difficult fracture is stabilized using a locking fibular plate. Several screws are passed from the fibula into the tibia to improve purchase of the implants. |
Minifragment implants include cortical screws from 1.1 mm to 2.7 mm.
Small fragment screws are 3.5 mm cortical screws and 4.0 mm cancellous
screws. Large fragment implants use 4.5 mm cortical and 6.5 mm
cancellous screws. Cannulated 7.3 mm cancellous screws are available as
a separate set. The size of the screw needed depends on the size of the
bone, size of the fragment, and surgeon preference.
plate affect the plate’s strength and contourability. Plates vary from
1.5 mm wafers in the minifragment set to stout, broad 4.5 mm dynamic
compression plates. Tubular plates are thin, moldable, and placed in
areas with little subcutaneous tissue. Dynamic compression plates allow
variable placement of screws in the holes. With eccentric screw
placement, compression can be achieved indirectly across the fracture.
Limited contact dynamic compression plates have a lesser footprint to
lessen the deleterious effect plates have on the underlying cortical
circulation. Reconstruction plates have deep grooves between holes to
allow more complex contouring. Periarticular plates are designed to fit
on a certain portion of a certain bone. The plate shape and type
transitions as the needs differ in various areas of the bone.
screws provide compression across a fracture site, but the lever arm is
too limited to resist functional loading. Lag screws are often
supplemented with a plate that resists these forces. This is a
neutralization plate. A plate functions as a tension band when applied
to the tension side of a fracture. Compression plating can be performed
to compress a fracture without lag screws. A buttress plate has a
supporting role. A locked plate acts as an internal external fixator,
stabilizing the fracture with multiple fixed angle devices.
stability. Absolute stability is achieved with lag screws and a
neutralization plate. Motion is reduced to such an extent at the
fracture site that primary bone healing occurs. Relative stability
confers that all motion is not eliminated, but enough stability exists
to allow bone healing and rehabilitation. A bridge plate is an example
of relative stability. The screws couple the plate to the bone proximal
and distal to the fracture, leaving this area alone.
alignment of the bone until the fracture heals. Unlike intramedullary
nails, these implants are less load sharing, and weight bearing is
usually not allowed until the bone heals.
patient. When the fracture is fresh or unstable, pain limits activity.
Problems with limited activity include global deconditioning, muscle
atrophy, joint stiffness, and disuse osteopenia. However, as the
fracture heals, pain lessens, and activity level should slowly
increase. Treatment modalities such as casts or braces will immobilize
joints, producing stiffness. Immobilization also decreases cartilage
nutrition, further insulting the joint. Some lower extremity fractures
require physician-imposed restrictions on weight bearing, which makes
locomotion with a walker or crutches unnatural and cumbersome.
patient to his or her vocational and recreational activities. Every
injury is different, but each patient can tolerate some exercise.
Patients should be encouraged to participate in joint range of motion
exercises and
muscle
strengthening or maintenance exercises. An exercise program for all
limbs should be established. For example, upper extremity strengthening
exercises will improve crutch-walking endurance in the patient with a
lower extremity injury.
helpful as the patient transitions from wheelchair to independent
ambulation. Balance and proprioception training are important factors
in regaining normal function. Water exercise may be beneficial in
maintaining strength and endurance in those who have restrictions on
weight bearing, or are not quite comfortable exercising on land.
providing instruction and feedback to the patient. The therapist also
monitors the patient’s progress, alerting the physician if no
improvement or regression occurs. It should be made clear, however,
that it is the patient’s responsibility to perform all exercises as
instructed, every day. Exercise should not be limited to physical
therapy sessions only. The consequences of noncompliance should be
emphasized.
difficult. The emphasis in the upper extremity is early joint range of
motion to prevent stiffness. Again, a licensed physical or hand
therapist is part of the methodology, but should not be the sole source
of exercise for the injured patient.
team consists of not only physicians, nurses, and therapists, but also
dieticians, social workers, and vocational counselors. The
psychological impact of injury tends to be under-recognized by the
medical team. The inclusion of a health psychologist to the team may
benefit the injured patient. Considerable psychological distress has
been identified in patients up to 2 years after severe lower extremity
injury, and few get any mental health services.
MPG, Boskey A, Kaufman JK, et al. Form and Function of Bone. In:
Buckwalter JA, Einhorn TA, Simon SA, eds. Orthopaedic Basic Science.
2nd Ed. Aurora, IL American Academy of Orthopedic Surgeons, 2000:
320-369. This comprehensive chapter reviews the
structure and function of bone. Topics covered include bone morphology,
cellular mechanisms of bone remodeling, bone matrix composition, bone
blood flow, biomechanics of bone, material properties of bone, bone
metabolism and mineral homeostasis, age-related changes in bone mass
and morphology, and metabolic bone disease.
SM, Ostrum RF, Chao EYS, et al. Bone injury, regeneration, and repair.
In: Buckwalter JA, Einhorn TA, Simon SA, eds. Orthopaedic Basic
Science. 2nd Ed. Aurora IL American Academy of Orthopedic Surgeons,
2000:371-400. This comprehensive chapter is a
definitive source of information on all aspects of bone injury and
repair. The effects of bone repair after surgical intervention are well
presented.
JW, Ramsey WC, Harkess JW. Principles of fractures and dislocations.
In: Rockwood CA, Green DP, Bucholz RW, et al., eds. Rockwood and
Green’s Fractures in Adults. 4th Ed. Philadelphia: Lippincott-Raven,
1996:3-120. This chapter in this classic fracture
textbook provides a comprehensive review of important concepts related
to fractures and dislocations.
SM, Claes L. Biology and biomechanics in fracture management. In: Ruedi
TP and Murphy WM, eds. AO Principles of Fracture Management. New York:
Thieme, 2000:7-32. This chapter is a
well-illustrated and succinct summary of the biology of fracture
healing, and how the process is altered by surgical stabilization.
WH, Code KI, Jay RM, et al. A prospective study of venous
thromboembolism after major trauma. N Engl J Med 1994;331:1601-1606. This
study reported the prevalence of thromboembolic disease in injured
patients with no prophylaxis. Fifty-eight percent of patients had deep
venous thrombosis (DVT), detected by screening venography and impedance
plethysmography. Three of the 716 patients died of pulmonary embolism
prior to screening. Five independent risk factors were determined for
the development of DVT: older age, blood transfusion, surgery, fracture
of femur or tibia, and spinal cord injury.
HC, Giannoudis P, Krettek C. The timing of fracture treatment in
polytrauma patients: relevance of damage control orthopedic surgery. Am
J Surg 2002;183:622-629. A historical overview of
treatment philosophies for multiply injured patients with fractures is
presented. The authors favor a “damage control orthopedics” philosophy
when treating those multiply injured patients at high risk of
developing systemic complications. This involves temporary
stabilization, followed by definitive treatment when the patient’s
condition allows.
and rapid reduction in pelvic volume can be achieved in patients with
pelvic ring injuries using simple methods of external compression.
DJ, Olson SA, Matta JM. Diagnosis and management of closed internal
degloving injuries associated with pelvic and acetabular fractures: the
Morel-Lavallee lesion. J Trauma 1997;42:1046-1051. This
is a review of the authors’ experience with 34 patients with closed
degloving injuries. Positive cultures were obtained in 46% of the
patients and were related to time from injury to debridement. The
authors recommend early debridement of the degloving injury, either
before or at the time of fracture fixation, and leaving the wound open.
MM, and Court-Brown CM. Compartment monitoring in tibial fractures. The
pressure threshold for decompression. J Bone Joint Surg Br
1996;78-B:99-104. The authors determined the
differential pressure measurement (diastolic pressure—compartment
pressure) of 30 mm Hg to be a reliable threshold for fasciotomy. Using
this criterion led to no missed cases of compartment syndrome in this
group.
T, Iorio R, Healy WL. Rate of and risk factors for acute inpatient
mortality after orthopaedic surgery. J Bone Joint Surg Am
2002;84-A:562-572. Overall mortality for
inpatient orthopedic procedures was 0.92%. The mortality rate was 3.1%
for patients with hip fractures, and 0.5% for patients without hip
fractures. Five critical risk factors were identified as most helpful
in identifying patients at risk for death: chronic renal failure,
congestive heart failure, chronic obstructive pulmonary disease, hip
fracture, and age of greater than 70 years. A linear increase in
mortality was seen with increasing numbers of critical risk factors.
AS, Mintjes-de Groot AJ, Severijnen AJ, et al. Risk assessment for
surgical-site infections in orthopedic patients. Infect Control Hosp
Epidemiol 1999;20:402-407. Age, additional
nocosomial infections, wound contamination class, preoperative stay,
and numbers of operations were identified as important risk factors for
orthopedic surgical-site infections in Dutch patients.
O, Krettek C, Miclau T, et al. Minimally invasive plate osteosynthesis:
does percutaneous plating disrupt femoral blood supply less than the
traditional technique? J Orthop Trauma 1999;13:401-406. A
cadaver vascular injection study demonstrated that a percutaneous
submuscular plating technique preserved more blood supply to the bone
than traditional open methods of plate application.
PV, MacDonald DA, Matthews SJ, et al. Nonunion of the femoral
diaphysis: the influence of reaming and nonsteroidal anti-inflammatory
drugs. J Bone Joint Surg Br 2000; 82-B:655-658. A
group of patients with femoral nonunions was compared to a group of
patients with healed femur fractures. Fewer nonunions were noted in
comminuted femoral fractures and in patients allowed early weight
bearing. Nonsteroidal anti-inflammatory use after injury was
significantly associated with femoral nonunion.
EJ, Agel J, Selznick HS, et al. Deleterious effect of smoking on
healing of open tibia-shaft fractures. Am J Orthop 2002;31: 518-521. A
retrospective review of tibial fractures treated with either external
fixation or intramedullary nailing demonstrated patients who smoked had
decreased rates of union, slowed healing, and increased complications.
GD, Hymes RA, LaDouceur MS, et al. Postoperative infections in
asymptomatic HIV-seropositive orthopedic trauma patients. J Trauma
1994;37:545-550. A retrospective review of
patients with orthopedic injuries demonstrated a higher infection rate
among asymptomatic HIV seropositive patients (16.7%) compared to HIV
seronegative patients (5.4%). Differences in infection rate after open
fractures were also significant, and became more significant as the
severity of the open fracture increased.
SJ, Keating JF, Meek RN. Fat embolism syndrome in isolated femoral
fractures: does timing of nailing influence incidence? Injury
1998;29:131-133. The incidence of fat embolism
syndrome was reviewed in a consecutive series of 274 patients with
isolated femur fractures. No fat embolism syndrome was seen in patients
older than 35 years. In those <35, if nailing of femoral fracture
was performed early (<10 hours from injury), no fat embolism
syndrome was observed. If femoral fracture stabilization was delayed, a
10% incidence of fat embolism syndrome was observed.
DP, Kuehnert MJ, Sawyer RG. CDC/SIS Position Paper. Preventing
antimicrobial-resistant bacterial infections in surgical patients. Surg
Infect (Larchmt) 2002;3:375-385. The authors
developed a multistep approach to help surgeons prevent
antibiotic-resistant bacterial infections in their patients. The focus
of the recommendations includes steps to prevent infection, diagnose
and treat infection effectively, use antibiotics appropriately, and
prevent transmission of organisms.
AM, Manigrasso MP, O’Connor JP. Cyclo-oxygenase-2 function is essential
for bone fracture healing. J Bone Miner Res 2002;17:963-976. Fracture
healing failed in rats given COX-2 inhibitors and in COX-2 knockout
mice. COX-2 is required for normal endochondral ossification.
F, and Johnson W. Unilateral external fixation: methods to increase and
reduce frame stiffness. Clin Orthop 1989;241: 48-56. This is a review of the mechanical properties of different external fixator constructs.
A, Vannini F, Mosca M, et al. State of the art review: techniques to
avoid pin loosening and infection in external fixation. J Orthop Trauma
2002;16:189-195. Hydroxyapatite coating of
external fixator pins was the most effective technique to improve
bone-pin interface. The effect was most evident with the use of tapered
pins.
P III, Bergman M, Watnik N, et al: Treatment of grade-IIIb open tibial
fractures: a prospective randomised comparison of external fixation and
non-reamed locked nailing. J Bone Joint Surg Br 1994;76-B:13-19. This
study demonstrated no advantage of external fixation in treating severe
open tibia fractures. The rate of malunion was less in the group
treated with intramedullary nailing. The authors feel the soft tissue
management was improved with stabilization by intramedullary nails.
JO, Luber, K, Park T. The effect of femoral nailing on cerebral
perfusion pressure in head-injured patients. J Trauma
2003;54:1166-1170. Seventeen patients with an
intracranial pressure monitor underwent femoral nailing. A decrease in
the cerebral perfusion pressure occurs nearly universally
intraoperatively. The authors suggest careful management of the mean
arterial pressure intraoperatively is critical to maintain cerebral
perfusion pressure.
LB, Johnson KD, Weigelt J, et al. Early versus delayed stabilization of
femoral fractures: a prospective randomized study. J Bone Joint Surg Am
1989;71-A:336-340. This prospective randomized
study found that delayed stabilization of femur fractures in multiply
injured patients resulted in increased rates of pulmonary complications
and longer hospital stays.
LB, Sucato D, Stegemann PM, et al. Displaced isolated fractures of the
tibial shaft treated with either a cast or intramedullary nailing: an
outcome analysis of matched pairs of patients. J Bone Joint Surg Am
1997;79-A:1336-1341. This study examined the
outcomes of operative versus nonoperative treatment of displaced tibial
shaft fractures. Those treated with intramedullary nailing had shorter
times to union. This group also had better knee, ankle, and SF-36
scores.
MJ, MacKenzie EJ, Riemer BL, et al. Adult respiratory distress
syndrome, pneumonia, and mortality following thoracic injury and a
femoral fracture treated either with intramedullary nailing with
reaming or with a plate. J Bone Joint Surg Am 1997;79-A:799-809. Patients
with femoral fractures were treated with early reamed intramedullary
nailing or plating, depending on the institution they were at. Groups
included those with and without a significant chest injury. For
patients without a chest injury, no difference in the rates of ARDS,
pneumonia, pulmonary embolus, multi-organ failure, or death was seen
between the two groups. Similarly, no differences in these
complications were seen between the groups with a chest injury, when
the two stabilization techniques were
compared. The authors concluded the use of reamed intramedullary
nailing for acute stabilization of femur fractures in multiply injured
patients who have a thoracic injury does not increase the occurrence of
pulmonary complications or death.
RJ, Toal TR Jr., Murphy-Zane MS, et al. Immediate weight-bearing after
treatment of a comminuted fracture of the femoral shaft with a
statically locked intramedullary nail. J Bone Joint Surg
1999;81:1538-1544. In patients with femur
fractures treated with reamed statically locked intramedullary nails,
immediate weight bearing is safe, even if the fracture is comminuted.
WE, Fabian TC, Croce MA. Delayed surgical fixation of femur fractures
is a risk factor for pulmonary failure independent of thoracic trauma.
J Trauma 1994;37:667-672. This duplication of
Pape’s study yielded different results. Delayed surgical fixation was
associated with higher pulmonary complication rates, independent of the
severity of thoracic injury.
SM, Rutledge R, Dahners LE, et al. Incidence, management, and outcome
of femoral shaft fracture: a state-wide population-based analysis of
2,805 adult patients in a rural state. J Trauma 1994;37:255-261. Nonsurgical
treatment of femoral shaft fractures resulted in increased mortality.
For multiply injured patients (ISS > 15) skeletal stabilization at 2
to 4 days was associated with the lowest mortality. In this group a
trend toward higher mortality was observed with stabilization in the
first day. The authors suggest further study warranted in the multiply
injured patients, and an individualized approach is warranted.
PV, Veysi VT, Pape HC, et al. When should we operate on major fractures
in patients with severe head injuries? Am J Surg 2002;183:261-267. This
review determines the available literature does not give definite
guidance in the management of patients with fractures associated with
brain injuries. The authors feel that treatment of the skeletal
injuries should be tailored to the individual patient.
KD, Cadambi A, Seibert GB. Incidence of adult respiratory distress
syndrome in patients with multiple musculoskeletal injuries: effect of
early operative stabilization of fractures. J Trauma 1985;25:375-384. This
retrospective study demonstrated a significant increase in ARDS
associated with a delay (>24 hours) in operative stabilization of
major fractures in multiply injured patients. This was more apparent
with the more severely injured patients (Injury Severity Scores >
40).
JF, O’Brien PJ, Blachut PA, et al. Locking intramedullary nailing with
and without reaming for open fractures of the tibial shaft: a
prospective randomized study. J Bone Joint Surg Am 1997;79-A:334-341. This
study compared the outcomes of nails inserted with and without reaming
in open tibial fractures. Equivalent outcomes were observed, with a
higher rate of hardware failure in the unreamed group. Reamed
intramedullary nailing is safe for open tibia fractures.
HC, Auf’m’Kolk M, Paffrath T, et al. Primary intramedullary femur
fixation in multiple trauma patients with associated lung contusion—a
cause of post traumatic ARDS? J Trauma 1993;34:540-548. In
the presence of significant pulmonary injury, early intramedullary
nailing causes additional pulmonary damage and may trigger ARDS. In the
absence of chest trauma, early definitive stabilization of femoral
fractures is beneficial to the patient.
PA, O’Brien PJ, Meck RN et al. Interlocking intramedullary nailing with
and without reaming for the treatment of closed fractures of the tibial
shaft. J Bone Joint Surg Am 1997;79-A: 640-646. This
study compared the outcomes of nails with and without reaming in closed
tibia fractures. Increased rates of delayed union and hardware failure
were seen in the unreamed group.
TM, Scott JD, Brumback RJ, et al. Early fracture fixation may be “just
fine” after head injury: No difference in central nervous system
outcomes. J Trauma 1999;46:839-846. A review of
patients with head injuries and associated pelvic or lower extremity
injuries was performed looking for differences between early versus
delayed skeletal fixation. Early fracture fixation was not found to
negatively influence brain injury outcome or mortality.
JM. Fractures of the acetabulum: accuracy of reduction and clinical
results in patients managed operatively within three weeks after the
injury. J Bone Joint Surg Am 1996;78-A: 1632-1645. This
review of operative treatment of acetabular fractures demonstrated the
quality of reduction was related to the postoperative clinical results.
Anatomic reduction and avoidance of complications resulted in the best
clinical results.
JL, Buckwalter J, Gelberman R, et al. Articular fractures: does an
anatomic reduction really change the result? J Bone Joint Surg Am
2002;84-A:1259-1271. The authors review the data
available on articular reduction and patient outcome. Topics covered
include the effects of articular injury, articular step-off, accuracy
of the measurement of articular displacement, and the effects on the
accuracy of reduction on outcomes of specific fractures.
RG, Brien D, Buckley RE, et al. Fixation of fractures of the shaft of
the humerus by dynamic compression plate or intramedullary nail: A
prospective, randomised trial. J Bone Joint Surg Br 2000;82-B:336-339. A
prospective randomized trial of intramedullary nailing versus dynamic
compression plating for unstable humerus fractures demonstrated higher
rate of complications with the use of intramedullary nails. The authors
feel that intramedullary nails may have specific indications, but
dynamic compression plating is the standard of care.
SM, Frigg R, Hehli M, et al. Lag Screw. In: Ruedi TP and Murphy WM,
eds. AO Principles of Fracture Management. New York: Thieme, 157-168. This well-illustrated chapter provides a concise review of the mechanics and applications of lag screws.
B, and Holz U. Plates. In: Ruedi TP and Murphy WM, eds. AO Principles
of Fracture Management. New York: Thieme, 2000:169-186. This
well-illustrated chapter provides a concise review of the mechanics and
use of different types of plates in fracture surgery.
EA, Magaziner J, Wang J, et al. Patients with hip fracture: subgroups
and their outcomes. J Am Geriatric Soc 2002;50:1240-1249. In
this review of 571 patients with hip fractures, 33 to 37% returned to
prior levels of function 6 months after fracture. Only 25% were
independent ambulators at that time. The authors developed five
subgroups with 6 month outcomes that clinicians may use to predict
functional recovery for patients.
ML, MacKenzie EJ, Edwin D, et al. Psychological distress associated
with severe lower-limb injury. J Bone Joint Surg Am
2003;85-A:1689-1697. Two years after severe lower
extremity injury, almost one-fifth of patients had severe phobic
anxiety and/or depression (versus 2 to 3% rate in general population).
Factors associated with psychological disorders in these patients
include poorer physical function, younger age, nonwhite race, poverty,
a likely drinking problem, neuroticism, poor sense of self-efficacy,
and limited social support.
