Femoral Shaft Fractures
shaft fractures continue to evolve on the basis of the improved
understanding of the local anatomy, impact of treatment, and
biomechanics of fixation techniques. Starting with the introduction of
intramedullary nailing by Kuntscher during the years surrounding and
after World War II, patient survival and outcomes have continued to
improve.153,154,155
Improved prevention and management of fracture shortening, angulation,
infection, and nonunion have made intramedullary nailing the primary
treatment for most femoral shaft fractures. Patient mortality and
morbidity from pulmonary dysfunction, open wounds, and the frequently
associated multiple other injuries have continued to improve with a
better understanding of nailing techniques.
60 years. The transition from open nailing techniques to closed
techniques using a remote entry site at the proximal femur paralleled
the availability of image intensification. Intramedullary reaming
allowed placement of larger implants, allowing improved rotational
control and resistance to bending. The introduction and increased
popularity of interlocking nails allowed for improved rotational
control, better maintenance of femoral length, early weight bearing,
the use of smaller implants, and improved control of comminuted and
segmental fractures. Biomechanical improvements in nail designs and
instrumentation have further expanded the indications for nailing.
Cephalomedullary nails and retrograde nails have seen similar
improvements in design and instrumentation, increasing the ease of
insertion and further expanding the use of nailing techniques for some
particularly difficult fractures (Fig. 50-1).
More recently, alternative antegrade intramedullary nail starting
points have been introduced. This includes starting points at, medial
to, and lateral to the tip of the greater trochanter.
impact and timing of different techniques of femoral stabilization has
been gained. The impact of early femoral stabilization
was defined in the landmark prospective and randomized study by Bone and coauthors.25
The beneficial effects of stabilization within 24 hours in the multiply
injured patient included decreased pulmonary complications and
shortened hospital stay. The ill effects of femoral reaming in the
multiply injured patient were largely discounted after the comparative
study of Bosse and coauthors.27 In
this study, mortality and pulmonary dysfunction did not increase with
the use of reamed intramedullary nailing compared with plate fixation
in the multiply injured patient with thoracic trauma. More recently,
several prospective and randomized studies have shown improved rates of
union with a reamed technique compared with unreamed nail insertions.48,61,277
 |
|
FIGURE 50-1
A comminuted, segmental, open femoral shaft fracture with bone loss that occurred after a motorcycle crash. Despite the complexity of the injury, current nail designs and nailing techniques make stabilization of this injury possible. |
and implants for intramedullary nailing are uniformly positive, there
continues to be numerous unanswered questions in the management of
patients with femoral shaft fractures. Intense debate continues
regarding the optimal timing of surgical stabilization, especially in
patients with multiple injuries, associated thoracic trauma, or
associated head injuries. Similarly, the ideal starting point, amount
of reaming, and type of nail all continue to be sources of discussion
and further investigation. Because of the general expectation of
success in every patient treated with intramedullary nailing, the
management of complications must be met with knowledge and planning.
There tends to be an age- and gender-related bimodal distribution of
fractures with injuries occurring most frequently in young males after
high-energy trauma and in elderly females after falls from standing.
The mechanisms in young patients tend to be motor vehicle crashes,
motorcycle crashes, pedestrians struck by vehicles, or falls from
height. The relative distribution of these fractures depends on
multiple factors including the geographic location (urban versus rural)
and country of study. In a review of 515 patients with 551 femoral
shaft fractures in a typical urban U.S. city, the average age was 27.2
years and 70% were males. The mechanisms of injury were motor vehicle
crashes in 78%, motorcycle crashes in 9%, pedestrians struck in 4%,
falls from height in 3%, gunshot wounds in 2%, and other miscellaneous
mechanisms in 3%. Open fractures were identified in 16%, and the
distribution of fracture comminution according to the scheme of
Winquist Hansen was relatively uniform among types 0, 1, 2, 3, and 4.
The fracture patterns that could be identified were oblique in 51%,
transverse in 29%, comminuted in 14%, and spiral in 6%.304
In a very different study, the incidence of femoral shaft fractures in
skeletally mature patients was estimated by Salminen et al. in
semiurban county in Finland reviewed over a 10-year period.241
The incidence of femoral shaft fractures was 9.9 per 100,000
person-years. The bimodal distribution of young males (between the ages
of 15 and 25 years) and elderly females (>75 years) was confirmed.
Most of these fractures (75%) were attributable to high-energy
mechanisms, with the majority being road traffic accidents. The
fracture configuration was either transverse or oblique in 77%.241
The application of these data points to patients injured in North
America may be difficult; no patients in this series from Finland
sustained a fracture caused by a gunshot. Fractures secondary to
low-energy trauma tend to occur more commonly in older female patients.
In a review of 50 femoral shaft fractures caused by low-energy
mechanisms, Salminen et al.240
identified only 13 patients who were younger than 60 years. All
fractures were closed, and none were associated with significant other
injuries. The fracture was spiral in 29 patients, oblique in 11
patients, and transverse in 10 patients. Chronic disease and osteopenia
were commonly identified as contributing to the occurrence of these
fractures.240
fractures of the femoral shaft and are more commonly observed in young
patients after high-energy traumatic injuries. Ipsilateral femoral
fractures can occur at the femoral neck, intertrochanteric, and distal
femoral articular locations and will be discussed in detail later in
this chapter. Other associated musculoskeletal injuries commonly
observed are patellar fractures, tibial fractures, acetabular
fractures, and pelvic ring injuries. Soft tissue trauma to the knee
occurs commonly with femoral shaft fractures and requires a careful
physical examination and further radiologic studies. Associated
abdominal, thoracic, and/or head trauma related to the mechanism
requires evaluation by a team of physicians. The identification and
treatment of these associated injuries will be discussed in further
detail later in this chapter.
shaft fracture is usually obvious. However, a methodical extremity
examination of all patients who sustain injuries from blunt and
penetrating trauma should ensure that the diagnosis is timely and
accurate.
Patients
usually have significant pain localized to the thigh. However, the
presence of associated injuries or other fractures may be distracting,
both for the patient and the examining physician.
evaluation of the traumatized patient and can be obtained from the
patient, family members, emergency personnel, or others. This includes
determination of the injury mechanism, the time elapse from injury to
presentation, the need for a prolonged extrication, the location of the
accident, and any known associated injuries. The mechanism of injury is
an important aspect of the history that may suggest the fracture
location, fracture configuration, and associated soft tissue injury.
The time from injury to presentation gives valuable information
regarding the potential for extensive blood loss into the thigh, the
overall condition of the patient, and the possibility of significant
associated soft tissue injury such as substantial muscle crush that is
occasionally seen with a prolonged extrication. The location of the
accident may give information regarding the potential for specific
organisms contaminating open fractures and the impact of the ambient
temperature on the overall condition of the patient. The identification
of any associated medical comorbidities is similarly an important
aspect of the history. Although this information has little impact on
the actual diagnosis of the femur fracture, it may determine the timing
of treatment, type of fixation, and need for specialized evaluations.
with a femur fracture. However, the examination should not be limited
to sites of obvious pain and deformity. Advanced trauma life support
protocols should be followed in the initial evaluation. The orthopaedic
examination should include visual inspection and palpation of all
extremities, the pelvis, and the spine. In patients with a fractured
femur, there is usually an obvious deformity with gross mobility at the
thigh. The visual inspection should include a circumferential
evaluation of the limb to look for associated open wounds, degloving
injuries, bruising, and abrasions. The ipsilateral knee and hip should
be examined to determine whether there are associated noncontiguous
fractures or ligamentous injuries. A focused examination of the knee
ligaments and associated soft tissues is mandatory, although this is
frequently more accurate in the anesthetized patient at the conclusion
of surgical stabilization of the femur fracture. The association
between femur fractures and concomitant ligamentous and meniscal
injuries of the ipsilateral knee is well documented.287
Investigators evaluated 47 patients with femoral shaft fractures with
arthroscopy and an examination under anesthesia after femoral nailing.
Ligamentous laxity was identified in 49% of patients, medial meniscal
injuries in 26%, and lateral meniscal injuries in 28%. There appeared
to be no relationship between a meniscal injury and the presence of
ligamentous laxity.287
studied 40 patients after femoral stabilization with an examination
under anesthesia and knee arthroscopy. The physical examination
revealed ligamentous laxity in 52.5% of patients. Subsequent
arthroscopic examination identified partial (48%) and complete (5%)
anterior cruciate ligament tears, and partial (5%) and complete (2.5%)
posterior cruciate ligament tears, with lateral and medial meniscus
tears in 20% and 12%, respectively. In total, 55% of patients had
significant arthroscopic findings. A well-defined treatment protocol
for these associated ligamentous findings identified on arthroscopic or
physical examination has not currently been identified. In the majority
of instances, surgical repair or reconstruction is not initially
required. In general the overall approach to these commonly observed
ligamentous findings should parallel the management in a patient
without an associated femoral shaft fracture. Although associated knee
dislocations are uncommon, a cursory examination of the knee or an
examination that is minimized because of the obvious fracture of the
femoral shaft can leave the limb threatened because of vascular injury.
The vascular status of the extremity is determined with palpation
and/or Doppler examination of the distal pulses. Any discrepancy with
the contralateral extremity requires further evaluation. Extremity
traction and limb realignment to a more anatomical position may change
the vascular examination. An expanding hematoma, a bruit, and obvious
bleeding are all indicative of an associated vascular injury. Even the
presence of normal pulses does not completely rule out the possibility
of a vascular injury. In a study of 765 consecutive patients with
closed femoral shaft fractures, Kluger et al.149
identified acute vascular injuries in 10 patients (1.6%). Normal pulses
were identified in a minority of patients with angiographic evidence of
vascular injury, emphasizing the need for continued and repeated
evaluation in these patients. Further, in a study of blunt femoral
fractures with an associated vascular injury, DiChristina et al.72
found that the arterial injury was segmental in 15% of injuries. The
ankle-brachial index has been shown to be a sensitive test for
identifying vascular injuries in a variety of blunt lower extremity
trauma, as well as knee dislocations, and is a simple objective
measurement to supplement the physical examination. An ankle-brachial
index (the Doppler systolic arterial pressure of the injured extremity
divided by that of an uninvolved arm) of less than 0.90 has been found
to have a high sensitivity and specificity for a major arterial injury
of the lower extremity.135
performed in an awake and cooperative patient. Although injuries to the
femoral and obturator nerves are uncommon after a fracture of the
femur, sciatic nerve injury does occur. Accurate documentation of the
sensory and motor function of the tibial and peroneal branches is
therefore a necessity.
determine the presence or absence of communication with the fracture.
Even the smallest of wounds should be viewed with suspicion and any
drainage of fat or blood from the leg should be considered as
indicative of an open fracture until proved otherwise. Although lateral
and anterolateral open wounds are seen most frequently, medial and
posterior open wounds are not infrequent and are worrisome for
associated vascular and neurologic injury, respectively. Open wounds
should be gently irrigated and gross debris or foreign material
removed. Sterile dressings are applied, and repeated examinations are
avoided to minimize further contamination. If possible, the extruded
bone ends should be reduced to minimize further dessication,
contamination, and pressure necrosis of the underlying skin and muscle.
Comfort and hemostasis may also be facilitated. In penetrating
injuries, the entry and exit locations should be determined and can be
marked with radiopaque markers before obtaining radiographs. This can
aid in the intraoperative search for foreign material, debris, or
missile components.
status of the patient, largely because of the potential for blood loss
into the surrounding soft tissues of the thigh. In a study of 53
patients with isolated femur fractures, Lieurance et al.165
found that 21 patients (40%) required blood transfusions averaging 2.5
units of packed red blood cells during their initial hospitalization.
Preoperative hemorrhage as opposed to intraoperative blood loss was
identified as a risk factor for blood transfusion. Interestingly, the
fracture pattern did not correlate with blood loss or the need for
transfusion. Although isolated femur fractures are associated with
blood loss requiring transfusion, the association with hypotensive
shock is less clear. Ostrum et al.205
found that patients with femoral shaft fractures frequently exhibited
hemodynamic changes with blood loss; however, hypotension was not
observed. As a result, the authors recommended that in patients with an
isolated closed femoral shaft fracture with associated hypotensive
shock, alternative sources of blood loss should be investigated.
femur fractures caused by a blunt mechanism. This includes ipsilateral
femoral neck fractures,2,230,263 pelvis and acetabular fractures,195 hip dislocations,311 knee injuries, intercondylar distal femoral fractures,11,44
and ipsilateral distal lower extremity injuries. Associated hip
dislocations occur uncommonly, but this combination of injuries
complicates the initial management. Closed reduction of the hip remains
a priority to protect the femoral head blood supply. However, an
associated femoral shaft fracture complicates the usual reduction
measures and may necessitate placement of an external fixator or a
percutaneous Schanz pin.311 Similarly, associated pelvic and acetabular fractures complicate both the initial evaluation and the subsequent management.
anteroposterior (AP) and lateral radiographs of the entire femur. More
information can be obtained if these are performed with the femur at
length, preferably after traction is applied. Traction can be
accomplished with either a Thomas splint or an appropriately placed
distal femoral or proximal tibial traction pin. Ideally, the entire
femur should be present on a single radiographic cassette. The
radiographs should be critically evaluated to determine the fracture
pattern, bone quality, presence of bone loss, associated comminution,
presence of air in the soft tissues, and amount of shortening. An
actual measurement of the angular deformities is probably of little use
on the initial radiographs. The length of the femur can be estimated
using digital films or with rulers appropriately corrected for
magnification. Contralateral extremity femoral films in two planes are
useful for determining the normal femoral bow and the normal femoral
length. The diameter of the medullary canal at the isthmus can be
measured as part of the preoperative plan if nailing is anticipated.
The presence of osteopenia, metastases, or cortical irregularities in
the region of the fracture or remote in the femur should be identified.
routine evaluation include dedicated films of the hip and knee.
Although an internal rotation radiograph of the hip is ideal for
evaluation of the femoral neck, this may be difficult in a patient with
a femoral shaft fracture. The knee radiographs should be reviewed to
determine whether there is associated joint widening or associated
fractures. If a computed tomography (CT) scan of the abdomen and/or
pelvis is obtained for other reasons, this should be reviewed because
it may provide evidence of injury to the ipsilateral acetabulum or
femoral neck. To minimize the incidence of a missed femoral neck
fracture in association with a fracture of the femoral shaft, a number
of additional radiographic evaluations can be considered including an
internal rotation plain radiograph of the hip, a fine-cut (2-mm) CT
scan of the femoral neck, an intraoperative fluoroscopic lateral of the
femoral neck, and postoperative hip radiographs after femoral
stabilization.273
anatomical location, fracture morphology, degree of comminution, or
combinations thereof. The fracture may be described as proximal third,
middle third, or distal third in location, or at the junctions between
these regions. In addition, fractures may be described on the basis of
the location relative to the isthmus of the femoral canal. Infraisthmal
fractures are important to identify if intramedullary nailing is
planned. In these fractures, the nail will not assist with reduction of
the fracture because the direction of the implant is determined by its
contact fit with the endosteal surface of the femoral isthmus, which is
located proximal to the fracture. Conversely, simple fracture patterns
at the isthmus are predicted to reduce with placement of an
appropriately sized medullary implant. Fractures are often further
described on the basis of the fracture geometry as transverse, oblique,
spiral, or comminuted. This may useful for communication regarding the
injury as well as understanding the mechanism that produced the
fracture.
capabilities. As a result, an appreciation for the amount of fracture
comminution was especially important to recognize. As interlocking
nails became available, predicting which injuries were likely to
subsequently shorten and those patterns that had poor rotational
control was an important part of the decision whether to place
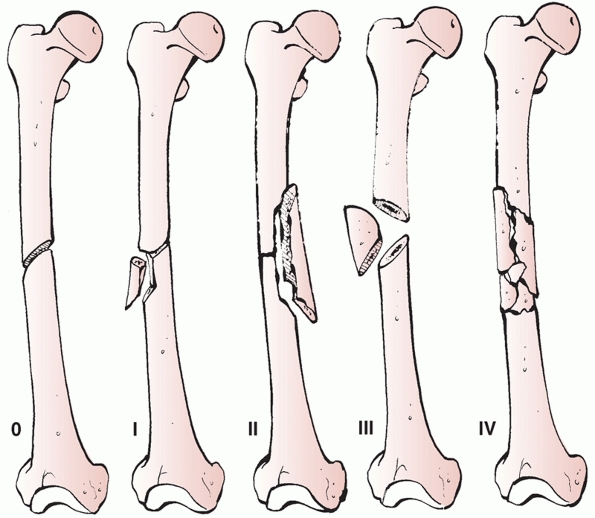
interlocking screws. In the Winquist and Hansen system,297,298 fracture comminution is categorized as from Grade 0 to Grade IV (Table 50-1) based on the percentage of intact
femoral shaft at the fracture site (Fig. 50-2).
Grade 0 fractures have no associated comminution. Grade I fractures
have a small chip or fragment of comminution. Grade II fractures have a
small butterfly fragment, but at least 50% of the cortex remains
intact. Grade III fractures have a larger butterfly fragment with
minimal cortical abutment predicted. Grade IV fractures have no
predicted cortical contact between the fracture fragments and are often
referred to as segmentally comminuted. This was originally used to
determine whether a locking nail should be used and if so, whether it
should be locked statically or dynamically. Grade 0 and I fractures are
stable in length and can theoretically be treated without interlocking;
grade II fractures are at risk for rotational abnormalities and
interlocking is recommended; fractures that are grade III and IV
require interlocking to prevent shortening and rotational malunion.
However, because of the possibility of unrecognized comminution and the
predictable performance of statically locked nails, it is unusual to
consider using an unlocked implant with currently available nailing
systems and techniques.
|
TABLE 50-1 Winquist and Hansen Classification of Fracture Comminution27,28
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
FIGURE 50-2 The Winquist-Hansen classification for diaphyseal femoral comminution. See text and Table 50-1 for explanation.
|
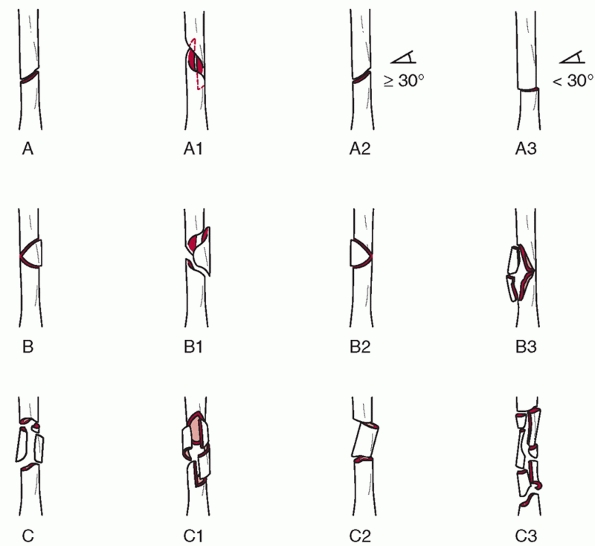
based largely on the fracture morphology and includes the fracture
location as well as the degree and type of comminution (Fig. 50-3).
Type A fractures are considered simple and include spiral, oblique, and
transverse patterns. Type B fractures are wedge fractures and include
spiral wedge, bending wedge, and segmental wedge patterns. Type C
fractures are considered complex patterns that have no predicted
cortical contact between the major proximal and distal fractures. These
fractures are divided on the basis of the same characteristics
described for B fractures. Each of these fractures is further divided
on the basis of location as subtrochanteric, middle, or distal.
Although the precise alphanumeric classification assigned to each
femoral fracture is of limited utility, an understanding of the
fracture pattern and its location assists with surgical planning and
may be useful for documenting and categorizing large numbers of femoral
fractures.
and torsional forces that can exceed three to four times body weight
during normal activities. The commonly observed fracture patterns
are
determined by the magnitude of the applied load, rate of load
application, and strength of the femur. Like all long bones, the femur
is strongest in compression and usually fails in tension as determined
by the direction of the applied load. A purely torsional force results
in the spiral fracture pattern typically seen in elderly patients. In
younger patients, a combination of bending and axial loading produces
the commonly observed transverse and bending wedge fractures. As the
applied force increases, so does the diaphyseal comminution. The
necessary bending force to produce a femoral shaft fracture in the
normal adult has been estimated at 250 Nm.160 However, in purely axial compression, the loads necessary to produce a fracture may exceed 8000 Nm.269
 |
|
FIGURE 50-3
Association for the Study of Internal Fixation classification of fractures of the shaft of the femur. Simple fractures (type A) are distinguished by the degree of obliquity of the fracture line. Wedge fractures (type B) are subclassified according to the anatomy of the wedge fracture. Complex fractures (type C) can be spiral, segmental, or irregular. |
nailing an ideal treatment biomechanically and practically. An
intramedullary nail is a strong device in axial loading and bending
given its centrally located cross-sectional moment and the symmetry in
its design. Thus, a nail can support loads equally in all directions.
Early nail designs were open-sectioned implants that did not have the
capability to accept interlocking screws. As a result, these implants
resisted bending forces only and primarily maintained the angular
alignment of the femur.
and to maintain length was limited. In response to these biomechanical
limitations, nail designs have changed significantly over the past 40
years. Most nails are made of either stainless steel or titanium, each
with its own unique biomechanical properties. The impact on healing of
each material because of its associated modulus of elasticity has not
been clearly elucidated.
an intramedullary nail is determined by a combination of nail
characteristics and fracture characteristics. Important nail
characteristics include the presence or absence of an open section or
slot, the wall thickness, the cross-sectional shape, and the presence
or absence of interlocking screws.246
The presence of a slot, or an open section, significantly decreases the
torsional rigidity of the nail. Similarly, increasing the wall
thickness of the nail will result in an increase in the nail’s
torsional stiffness. Therefore, with slotted and/or thin-walled nails,
torsional loads may result in rotational changes in the fractured
femur-nail construct, despite interlocking. In clinical practice, the
torsional stability of the nail itself is of minor concern, provided
the loads encountered do not exceed the nails elastic deformation
limits. Bending stiffness is primarily determined by the outer diameter
of the implant246 and the material
(stainless steel versus titanium). The modulus of elasticity of 316L
stainless steel is approximately twice that of titanium. The ultimate
strength of titanium is approximately 1.6 times that of stainless
steel. Resistance to axial loading of the implant bone construct is
primarily determined by the presence of interlocking screws and the
bone contact at the fracture if applicable. It becomes obvious that
multiple factors determine the final construct stiffness, all of which
should be understood and considered when choosing a particular
intramedullary nail. In the case of a purely transverse mid-diaphyseal
femur fracture with predicted cortical interdigitation after nailing,
the biomechanical characteristics of the implant are less important
than in a segmentally comminuted fracture that will have no inherent
stability after reestablishment of the length, alignment, and rotation.
The effect on torsional and flexural rigidity of the cross-sectional
shape and wall thickness of intramedullary nails has been studied.270
Implants of the same length and diameter were found to have greater
than a twofold difference in flexural rigidity and greater than a
threefold difference in torsional rigidity depending on these specific
design parameters.270
there is a large mismatch between the radius of curvature of the nail
and the radius of curvature of the femur, which has been estimated to
be between 109 and 120 cm.78,140
From a museum skeleton collection and a hospital biomechanics
laboratory, the femoral bow was determined in 948 femurs from 474
matched pairs using a computer curve-fitting program.78
The average femoral radius of curvature was found to be 120 cm. Age and
femoral length were not found to influence the radius of curvature.
However, race did have an effect on anterior bow: African Americans
donor femurs were noted to have less curvature. The radius of curvature
of eight antegrade nails were measured and found to range from 186 to
300 cm, indicating that the implants were much straighter than the
femurs that they are designed to stabilize. This mismatch could have an
effect on nail entry, femoral bursting, and final femoral alignment in
the sagittal plane. The impact of several parameters and their effect
on femoral bursting and fracture instability were determined by Tencer
et al. and Johnson and Greenberg.141,269,270
The parameters that affect bursting of the femur during antegrade
piriformis nail insertion include mismatch in curvature of the nail and
femur, high bending stiffness, and poor location of the starting hole.
An anterior offset of the starting hole of 6 mm from the centerline of
the femoral canal was found to significantly increase the hoop stresses
of the proximal femur. Factors identified that decrease the force of
femoral nail insertion include overreaming and the use of a nail with a
lower bending rigidity.140
screws are variable, depending on the manufacturer. The number of
distal interlocking screws necessary to maintain the proper length,
alignment, and rotation of the implant bone construct depends on
numerous factors including fracture comminution, fracture location,
implant size, patient size, bone quality, and patient activity.
Although the use of a single distal interlocking screw for femoral
shaft fractures has been shown in a single study to provide equivalent
torsional rigidity and axial load to failure when compared with two
distal screws, these other factors must be considered when determining
the number of screws.112 Distal
fractures, extensive comminution, poor bone quality, and the
expectation of early weight bearing are all variables that suggest the
need for two distal interlocking screws. In addition, interlocking
screws are highly loaded in axial compression during weight bearing.
Although the static stability may be similar with one versus two
screws, constructs with two screws can endure more cyclic loading.
predictable. Closed intramedullary nailing in closed fractures has the
advantage of maintaining both the fracture hematoma and the attached
periosteum. In addition, if reaming is performed, these elements
provide a combination of osteoinductive and osteoconductive materials
to the site of the fracture. Finally, reaming may produce a periosteal
vascular response that increases the local blood flow. As a result,
secondary bone healing with abundant fracture callus formation is
expected in most femur fractures treated with intramedullary nailing.
This leads to the ability to weight bear early after intramedullary
nailing and a low refracture rate after nail removal in clinically
indicated cases.
tubular and has an anterior bow with a radius of curvature of
approximately 120 cm. Proximally, the relevant osseus structures
include the femoral head, femoral neck, calcar femorale, lesser
trochanter, and greater trochanter. Distally, the femur widens into the
metaphysis. The relevant distal osseus structures include the medial
and lateral condyles, medial and lateral epicondyles, and distal
femoral articulation.
medially, and laterally. The thickened posterior cortex of the femur
coalesces into the linea aspera in the central diaphysis of the femur.
The linea aspera divides proximally to the lesser and greater
trochanters, and distally to the medial and lateral femoral condyles.
The linea aspera serves as a muscle attachment site as well as a
buttress along the concavity of the femoral diaphysis.
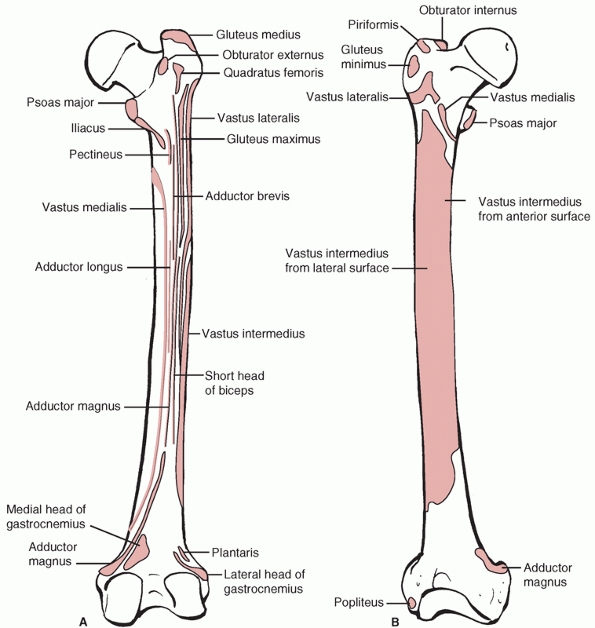
Knowledge of these muscle attachments is important for performing
atraumatic surgical dissections and for understanding the commonly
observed deformity patterns associated with fractures of the femur. The
proximal muscular attachments include the hip abductor and short
external rotator insertions at the greater trochanter, gluteus maximus
osseus insertion at the posterolateral proximal femur, and iliacus and
psoas insertions on the lesser trochanter. The adductors insert on the
posterior and medial aspects of the femur along its length. The vastus
lateralis origin is proximal, just distal to the gluteus medius
insertion. The anterior and lateral femur serves as the origin for the
vastus intermedius along the majority of the diaphysis. On the medial
and posteromedial portions of the femur is the origin of the vastus
medialis. Distally, the gastrocnemius originates from the posterior
aspect of the femoral condyles.
 |
|
FIGURE 50-4 The primary muscular attachments on the anterior (A) and posterior aspects of the femur (B). Anterior view.
|
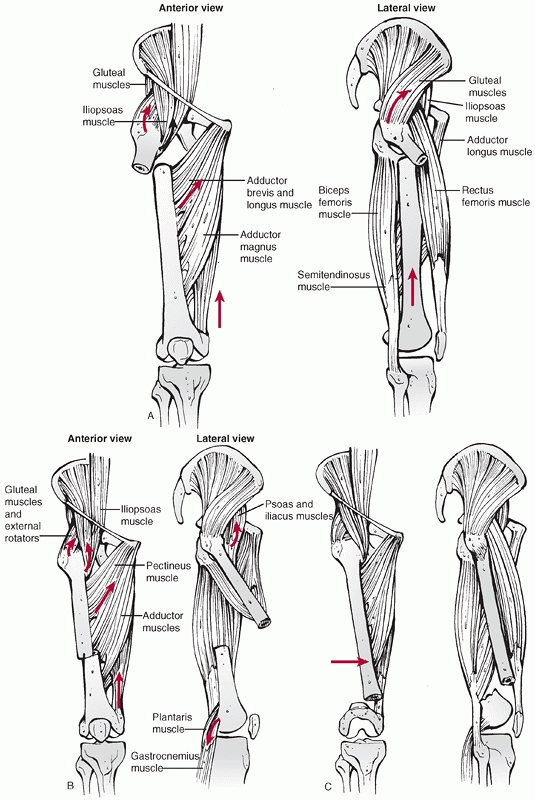
Shortening is universally observed because of the pull of the
hamstrings and quadriceps muscles. In proximal fractures (in the
subtrochanteric region), the proximal segment is typically flexed,
abducted, and externally rotated by the muscular pull of the hip
abductors, external rotators, and iliopsoas.
 |
|
FIGURE 50-5 Muscular attachments and fracture location determine the observed deformities and displacements.
|
pull of the adductors. In distal fractures, the gastrocnemius muscle
origins at the femoral condyles are largely responsible for the
commonly observed fracture extension deformity. The shaft of the femur
is frequently medialized because of the attachments of the adductor
muscles. Because of these largely unopposed muscle forces, the exercise
of attempting to reduce proximal and distal fractures with an
increasing distraction force is typically futile. Limb position,
strategic bumps, and externally applied forces are much more helpful
than brute strength in improving the angulatory and translational
deformities that occur.
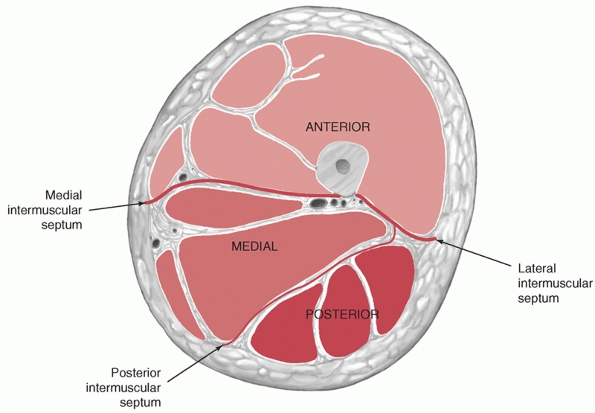
are separated by the medial, lateral, and posterior intermuscular
septae (Fig. 50-6). The anterior compartment of
the thigh contains the quadriceps femoris, iliacus, psoas, sartorius,
and pectineal muscles. The neurovascular structures of the anterior
compartment include the femoral artery and vein, femoral nerve, and
lateral femoral cutaneous nerve. The posterior compartment contains the
biceps femoris, semimembranosus, semitendinosus, and distal portion of
the adductor magnus. The neurovascular structures of the posterior
compartment include branches of the profundus femoris artery, sciatic
nerve, and posterior femoral cutaneous nerve. The medial compartment
contains the adductor brevis, the adductor longus, most of the adductor
magnus, and the gracilis. The neurovascular structures of the medial
compartment include the profundus femoris artery, obturator artery, and
obturator nerve.
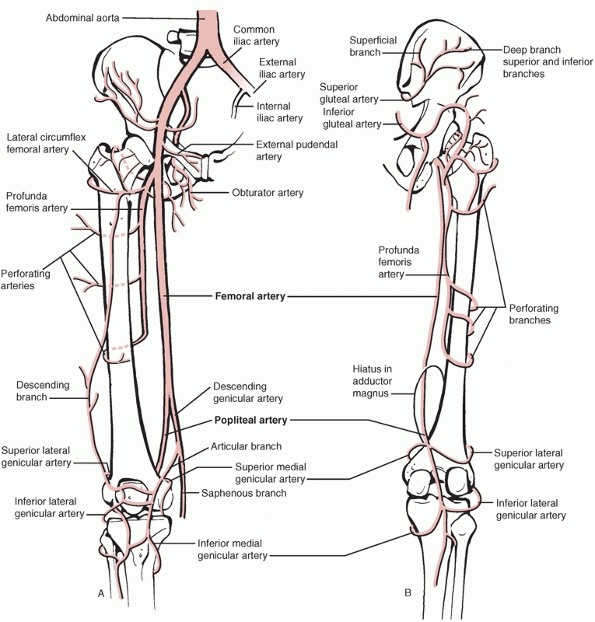
passing through the thigh as well as those perfusing the muscles and
femur (Fig. 50-7). The external iliac artery
becomes the femoral artery as it passes behind the inguinal ligament
and enters the anterior compartment in the femoral triangle. The
profundus femoral artery branches off the femoral artery and gives rise
to the medial and lateral femoral circumflex arteries. The profundus
femoral artery gives off numerous perforating branches along the length
of the femur that pass posteriorly. Distally, the femoral artery passes
through the hiatus of the adductor magus as it becomes the popliteal
artery. Knowledge of the location of these vessels helps make surgical
approaches uneventful.
 |
|
FIGURE 50-6 Cross-sectional diagram of the thigh demonstrates the three major compartments.
|
nutrient vessel(s) and small periosteal vessels. The nutrient arterial
supply to the femur was described in detail by Laing161
in a barium sulphate injection study of 10 adult femurs. The nutrient
arteries were found to arise as branches of the profundus femoris
perforating arteries. In four specimens, two nutrient arteries were
present, similar to that found in pediatric long bones. However, in six
specimens only one nutrient artery supplied the femoral shaft. In all
cases the nutrient artery was found to enter the femur in the region of
the linea aspera and branched proximally and distally to supply the
medullary cavity. In most instances the nutrient artery enters in the
proximal half of the femur; oftentimes it enters in the proximal third.
The location of entry for this vessel has implications during surgical
approaches:
attachments to preserve this nutrient vessel. The periosteal vascular
supply to long bones has been described in detail by Rhinelander225
and was largely based on numerous animal studies and surgical
dissections. He showed that the periosteal arteries are derived from
the blood vessels that also supply the surrounding muscles of the bone.
Anastomoses exist between the medullary and periosteal circulations,
and the normal direction of flow through the entire cortical thickness
is unidirectional from the medullary vessels to the periosteal vessels.
With displaced fractures, the medullary arteries are disrupted, leaving
the periosteal vessels with the principle role of providing circulation
to the bone. The normal direction of blood flow is reversed with the
loss of the medullary circulation, thus allowing cortical
revascularization.225
interval from the greater trochanter to the knee. A lateral skin
incision centered at the femoral shaft is used. The fascia lata can be
incised along its length exposing the vastus lateralis beneath. The
vastus lateralis can then be carefully dissected off the lateral
intermuscular septum, allowing identification and ligation of the
multiple perforating vessels. The vastus lateralis and underlying
vastus intermedius can then be elevated, taking care to leave the
underlying periosteum intact.
 |
|
FIGURE 50-7 The vascular anatomy of the thigh as viewed from anterior (A) and posterior (B).
|
These techniques have the advantage of sparing significant portions of
the perfusion to the femur. This has been confirmed in a dye injection
cadaver study in which minimally invasive techniques were found to
spare the nutrient and perforating arteries and were associated with a
significant improvement in medullary and periosteal perfusion compared
with open dissection techniques.83
treatment of femoral shaft fractures. These include spica casting,
traction, cast bracing, or combinations thereof. Currently, closed
management as definitive treatment for femoral shaft fractures is
largely limited to instances in which devices for internal fixation are
unavailable or in patients with significant medical comorbidities that
make femoral stabilization impossible. However, the
techniques
of traction are applicable for the temporary stabilization of femur
fractures until definitive fixation can be performed and in cases in
which infection requires removal of all internal stabilizing implants.
Although the use of cast braces is usually unnecessary with modern
techniques for femoral stabilization, these techniques may be useful in
limited circumstances such as in patients who cannot tolerate an
anesthetic or as an augmentative device in patients with distal or
shaft fractures in which adequate internal fixation was not obtained.
to the limb. Skin traction has limited utility because of the inability
to apply sufficient and sustained forces without damaging the skin.
This makes the use of skin traction a poor choice as a definitive
treatment modality. However, in the initial stabilization of a patient
in the field before evaluation at a hospital, some form of noninvasive
traction using a temporarily applied splint may assist with aligning
the limb, providing patient comfort, and limiting additional soft
tissue injury caused by the mobile femoral shaft fracture segment.
placement of an appropriate pin. This can be placed at the distal femur
or the proximal tibia. Small-diameter pins (2-mm) can be optimized with
the use of tensioned bows, obviating the need for large threaded
Steinman pins. A traction pin should be placed with sterile technique
if possible, and knowledge of the location of the relevant anatomical
structures in the region of the pin entry and exit locations should
minimize complications. The entry and exit tracts for the pin should be
appropriately anesthetized with local anesthesia. Safe pin placement is
usually from medial to lateral at the distal femur and from lateral to
medial at the proximal tibia. Placement at the distal femur as opposed
to the proximal tibia for fractures of the femoral shaft allows for
direct traction of the fractured bone and avoids distraction across the
potentially injured knee joint. Distal femoral pins should be placed in
an extra-articular location to avoid septic arthritis. Proximal tibia
pins are typically positioned at the level of the tibial tubercle and
placed in a bicortical location.
operative femoral fracture treatment may consist of the application of
weights attached to pulleys at the end of the bed, or some form of
balanced suspension. Ideally, traction applied to the distal femur or
proximal tibia is balanced against countertraction applied to the
proximal femoral segment. Proximal countertraction can be accomplished
with the weight of the patient or with Trendelenburg positioning. For
definitive treatment of femoral shaft fractures with traction, the
angle of limb, applied weight, and direction of the applied traction
will all require adjustment based on the fracture location.
successfully accomplished with Neufeld roller traction and
modifications thereof.36,91,139,172
The main advantages with Neufeld traction are early knee motion,
enhanced patient mobility, and earlier discharge from the hospital.
Fracture position can be well maintained despite the enhanced knee and
patient mobility. In a study of 30 patients treated with Neufeld roller
traction either temporarily or definitively, Browner et al.36 observed no nonunions and no infections. Similarly, Gates et al.91
reported on their experience with the use of hinged casts and roller
traction in 121 patients in developing countries. In their series,
hospital stay was short and all but one fracture healed.
uncommonly for the treatment of femoral shaft fractures. However, cast
braces can be used successfully, and the techniques of application for
the appropriate indications are important to understand. In unusual
circumstances, they can be used to augment intramedullary fixation if
unlocked implants are used.251 For
distal and femoral shaft fractures, cast braces allow early patient
mobilization and may be used in combination with a period of traction.64,116,186 They are thought to work by converting the thigh into a semi-rigid hydraulic tube that maintains the alignment of the femur.186
Typically, traction is initially used until there is some stability to
the fracture, usually for 6 to 8 weeks. Clinical resolution of fracture
site discomfort, radiographic evidence of callus formation, and lack of
fracture instability on clinical examination are all good indicators of
early healing. Like any form of closed management, success depends on
the technique of application and the proper implementation of weight
bearing. Cast braces cannot be used to correct angulatory or rotational
deformities.
They described the application of a proximal thigh cast and a long leg
cast incorporating the foot combined with a hinge at the knee joint.
The authors reviewed the treatment of 150 patients with femoral shaft
fractures treated with cast braces. The average time in traction was
7.3 weeks, and the average time of casting was 7.2 weeks. There were no
nonunions or refractures. This compares to a group of patients treated
by the same authors with traction followed by spica casting. In these
patients the total treatment time was more than 24 weeks, and more than
10% of patients had either a nonunion or a refracture.186 In another study reviewing an experience with cast braces for femoral fractures, Hardy116
reported acceptable results in106 patients. Union was predictable and
comminuted mid-diaphyseal fractures were observed to shorten more than
distal fractures.116 Similarly, Connolly et al.64
followed 143 patients with femoral shaft fractures treated with
traction followed by cast bracing. Although shortening of up to 2 cm
was observed frequently, nonunion and clinically significant malunion
were uncommon. The conclusions of these studies demonstrate that cast
braces can be successfully used for the treatment of femoral shaft
fractures after a period of traction.
over traction followed by cast bracing or spica casting of femoral
shaft fractures is generally considered obvious. This was studied, and
the improved outcomes with nailing were documented. Locked nailing was
associated with a much shorter hospital stay, decreased time to union,
and improved alignment when compared with traction plus casting.291 Similarly, Johnson et al.139
reported an average hospital stay of 31 days in patients treated with
roller traction compared with 20 days for patients treated with
intramedullary nails. The frequency of failure, defined as an unplanned
reoperation or unacceptable alignment, was reported in 66% of fractures
treated with roller traction compared with 4% of those treated with a
locked intramedullary nail.
Although
these results come as no surprise, they do emphasize the significant
improvements in treatment that have been observed with intramedullary
nailing.
femoral shaft fractures has limited indications. However, temporary
external fixation is used with increasing frequency in some valuable
circumstances. External fixation is most easily accomplished with a
unilateral frame (Fig. 50-8) but circular
frames are designed specifically for the femur. Unfortunately, these
devices are poorly tolerated by the patient over the extensive time
necessary to ensure adequate healing of the femur.
a temporizing measure for the initial stabilization of a fractured
femur. The procedure is rapid, and a temporary external fixator can be
reliably applied in less than 30 minutes. This is particularly
important in the critically ill patient.4,34,199,212,245
The vascular supply to the femur is not damaged to a significant degree
during the application of an external fixator, and this may be
important in high-energy and open injuries with significant damage to
the extraosseous and intraosseous blood supply. No additional foreign
material is introduced in the region of the fracture, which may be
particularly advantageous in open fractures and injuries with
infection. Further, external fixation allows access to the medullary
canal and the surrounding tissues in open fractures with significant
contamination. Dressing changes and local soft tissue care are
maintained with external fixation, although other methods may allow
improved access.
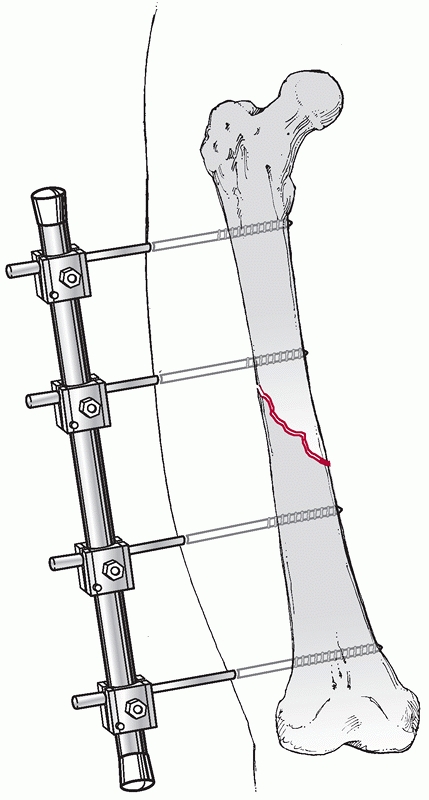 |
|
FIGURE 50-8 Association for the Study of Internal Fixation external half pin fixator used for temporary stabilization of a shaft fracture.
|
are related to this technique as a definitive treatment measure. Pin
tract infections occur commonly and are related to the time the fixator
is in place, the amount of soft tissues that the pins must traverse,
and the sterility at the time of the initial application.117
Loss of knee motion occurs commonly. Angular malunion and femoral
shortening occur more frequently than with other methods. There are
still concerns about the potential increased infection risk associated
with conversion of an external fixator to another definitive treatment
methods. Finally, unilateral external fixation has limited ability to
adequately stabilize the femoral shaft. This is largely because of the
large weight of the leg combined with the distance between the femoral
shaft and the bar of the external fixator.
Initially, extensive comminution and open fractures were considered to
be relative indications for the use of femoral external fixation as a
definitive treatment for femoral shaft fractures. However, as other
treatment methods such as intramedullary nailing have continued to
improve and low complication rates have been demonstrated with nails
even in the most complex injuries, the indications for the use of
external fixation have become more limited. Currently, the primary
indications include use as a temporary bridge to intramedullary nailing
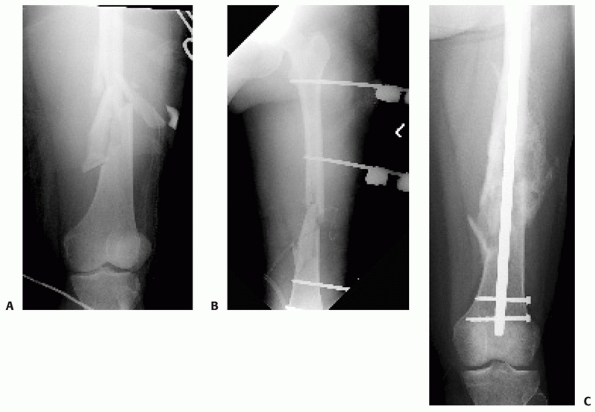
(Fig. 50-9), use in the severely injured
patient who cannot tolerate reaming and/or placement of a medullary
implant as a form of damage control orthopaedics, use in a patient with
an ipsilateral arterial injury that require repair, and in patients
with severe soft tissue contamination in whom a second debridement
would be limited by other devices. Which patients are more suitable for
initial placement of an external fixator followed by secondary
conversion to a medullary implant continues to be better defined but
includes patients with a severe head injury, elevated Injury Severity
Score (ISS), associated thoracic trauma, or multiple extremity
injuries. In patients with an accompanying ipsilateral arterial injury,
an external fixator can be rapidly applied, produces temporary
stability of the limb, and can easily be converted to another form of
stabilization.127
|
TABLE 50-2 Indications for External Fixation
|
|||||
|---|---|---|---|---|---|
|
 |
|
FIGURE 50-9 A comminuted femoral diaphyseal fracture (A)
in a patient with multiple other injuries including a pulmonary contusion, liver laceration, and head injury. Temporary external fixation (B) was rapidly applied initially to provide stability and alignment. Conversion to an antegrade nail 7 days later resulted in uneventful healing (C). |
relatively straightforward and based on the biomechanical principles of
external fixation. For patients requiring rapid application of a
temporary spanning fixator, the goals should be limb realignment,
patient comfort, and prevention of further soft tissue damage. Pins can
be placed anteriorly, anterolaterally, or laterally. Anterior pins
require placement through the extensor mechanism and should be avoided
if possible. Laterally placed pins require placement through the
iliotibial band and may similarly limit knee motion. To minimize this,
the iliotibial band should be incised in line with the leg at the time
of fixator placement. Pins can be placed from an anterolateral
location, anterior to the iliotibial tract. This may minimize knee
stiffness but is technically more difficult because the pins are out of
plane with the typically obtained fluoroscopic images that are used for
their placement.
A minimum of two pins per segment should be placed. A pin should be
placed near the fracture but out of the predicted fracture hematoma.
Another pin should be placed as far away from the fracture in each
segment. If the external fixator is planned as a temporizing measure, a
perfect reduction of the femur may be unnecessary. However, depending
on the original indications for placement of the external fixator, the
device may ultimately remain in position for longer than expected. As a
result, every attempt should be made to realign the limb and
reestablish the femoral length to facilitate the secondary
intramedullary nailing procedure.
femoral shaft fractures with extensive comminution, associated open
wounds, or multiple life-threatening injuries. Several small series
reported fracture union, early mobilization, rare infections, and
limited impact on knee motion.4,68,105,235 Alonso et al.4
treated 24 patients with femoral shaft fractures with external
fixation. This was a temporary treatment in 14 patients, although in 10
patients this was definitive. Healing was ultimately observed in 88%,
but almost half of the patients had significant loss of knee motion.
Shortening was noted in two patients treated definitively with external
fixation. On the basis of their experience, the authors recommended the
use of external fixation in several circumstances including the
aggressive management of soft tissue injuries, for the severely head
injured or traumatized patient, and for infected femoral nonunions. The
limitations of external fixation as a definitive treatment method in
open femoral shaft fractures were further elucidated by Mohr et al.,185
who reported a lengthy treatment period of more than 5 months, early
deep infections in 11%, late deep infections in 11%, shortening in 7%,
and restricted knee motion in 20%. Although all fractures healed, the
high incidence of complications and secondary surgeries in this group
of patients cannot be overlooked.
Of more than 1500 femoral shaft fractures treated with intramedullary
nailing during the same time period, 54 patients were treated with
external fixation followed by planned conversion to an intramedullary
nail. The primary indications for this protocol included critically ill
patients (n = 46) or patients who required expedient femoral fixation
for repair of an ipsilateral vascular injury (n = 8). The average ISS
of these patients was 29, and open injuries were present in 19. The
average period of external fixation was 7 days with a range of 1 to 49
days. The majority of patients underwent conversion from an external
fixation to an intramedullary nail at a single operative procedure (n =
55), but this was done in a staged fashion in four patients who had
significant pin site drainage. In these four patients, traction with
intravenous antibiotics lasting an average of 10 days was instituted to
allow resolution in the intervening time period. Overall,
healing
was observed in 97% of patients within 6 months. One patient developed
an infected nonunion, and one patient had an aseptic nonunion. The
average knee motion was 107 degrees. The authors concluded that
immediate external fixation followed by early conversion to
intramedullary nailing for femoral shaft fracture was safe in selected
multiply injured patients.199
The safety of temporary external fixation with delayed conversion to an
intramedullary implant was further corroborated in a retrospective
study of 173 patients with 192 fractures. The infection rates with
initial external fixation followed by conversion to an intramedullary
device were similar to that in patients treated with primary
intramedullary nailing in multiply injured patients. Pin site
contamination was observed more commonly when the fixator was left in
place for more than two weeks, suggesting a timely conversion to a
medullary implant whenver possible.117
fixation has been investigated to further define the indications in
multiply injured patients. This has led to the concept of “damage
control orthopaedics” in selected patients who may be poor candidates
for early definitive intramedullary nailing of the femur. Scalea et al.245
reported their results with early external fixation followed by
definitive intramedullary nailing in 43 patients with contraindications
to primary nailing. This included patients with associated head injury,
hemodynamic instability, thoracoabdominal trauma, and multiple other
injuries. Similarly, Pape et al.214
reported their conversion from early total care of patients to “damage
control orthopaedics” in the polytraumatized patient. This was
characterized by more frequent use of spanning and temporary external
fixation to treat lower extremity and femoral fractures followed by
delayed conversion to intramedullary nailing. The incidence of multiple
organ system failure was noted to decrease with this change in
treatment philosophy and was believed to be an adequate alternative in
patients at high risk for development of acute respiratory distress
syndrome (ARDS) or multiple organ system failure.213,214
In a prospective, randomized, multicenter study, a sustained
inflammatory response was seen after primary (<24 hours)
intramedullary femoral instrumentation, but not after initial external
fixation or after secondary conversion to an intramedullary implant.
These findings may become clinically relevant in patients at high risk
of developing complications. In addition, it confirms previous studies
that suggest damage control orthopedic surgery minimizes the additional
surgical impact induced by acute stabilization of the femur.213
With time and further study, the indications for early external
fixation followed by delayed conversion to intramedullary nailing will
become better defined.
numerous advantages compared with nonoperative methods and includes
early patient mobilization and early functional rehabilitation of the
injured extremity. The use of plate fixation for the routine treatment
of femoral shaft fractures has decreased with the increased use of
intramedullary nails. Several distinct advantages to plating do exist,
including the ability to obtain an anatomical reduction in appropriate
fracture patterns and the lack of additional trauma to remote locations
such as the femoral neck, acetabulum, and distal femur. The main
disadvantages associated with plate fixation when compared with
intramedullary nailing are the need for an extensive surgical approach
with its associated blood loss, infectious complications, and soft
tissue insult. This can result in associated quadriceps scarring and
its effects on knee motion and quadriceps strength. Further, the impact
of the plate on the femur after fixation cannot be minimized. This
includes the decreased vascularization beneath the plate and the stress
shielding of the bone spanned by the plate. Minimally invasive
techniques of plate application, although not addressing all of the
issues associated with plating, do minimize the additional vascular
insult to the periosteal and medullary blood supply of the femur.83 However, minimally invasive techniques have been associated with an increased incidence of malreduction.315
Finally, because the plate is a load-bearing implant, implant failure
is expected if union does not occur. Although implant failure will
ultimately occur with any orthopaedic device in the case of nonunion, a
load sharing implant of sufficient size will likely have increased
longevity compared with a plate.
plated. However, with the predictable results of intramedullary nails
for both the initial treatment of femoral fractures and the salvage of
other failed fixations, the use of plates as a primary treatment method
is limited (Table 50-3). That being stated,
certain clinical situations and patient factors may make plates
desirable. In most instances, the relative indications for plating are
the same as the relative contraindications for intramedullary nailing.
In patients with an extremely narrow medullary canal in whom
intramedullary nailing is impossible or difficult, plates remain an
excellent option. Plates are useful in fractures that occur adjacent to
or through a previous malunion, or in cases in which there is
obliteration of the canal because of infection or previous closed
management. Plates may be advantageous in fractures that have
associated proximal or distal extension into the pertrochanteric or
condylar regions because fracture reduction and stabilization may be
difficult with a medullary implant.
exposure for the vascular repair frequently involves a wide exposure of
the medial femur. If rapid femoral stabilization is desired, a plate
can be applied quickly through the medial open exposure.
However,
in this circumstance the rate of nonunion is likely increased by the
combination of the injury and surgical exposure. One should consider
that any salvage procedures in this scenario will require a repeat
surgical exposure through a scarred medial approach around a vascular
repair.
|
TABLE 50-3 Indications for Plating
|
||||||||
|---|---|---|---|---|---|---|---|---|
|
completely radiolucent table to allow unimpeded fluoroscopic imaging of
the femur from the hip to the knee. Lateral positioning eases the
retraction of the vastus lateralis in open techniques but may not be
applicable in the polytraumatized patient. In addition, proximal
imaging can be more difficult with the patient positioned laterally.
For supine positioning, the entire limb should be prepped in the
surgical field, including the groin to allow access to femoral vessels
if necessary. A small bump beneath the ipsilateral hip helps to
internally rotate the limb to neutral, simplifying the surgical
approach and making the intraoperative assessment of rotation easier. A
radiolucent ramp or several folded blankets placed beneath the thigh
and leg improves the lateral fluoroscopic imaging by elevating the leg
relative to the contralateral extremity.
submuscular technique may be applicable. For simple fracture patterns
that allow an accurate cortical reduction of the majority of the
femoral shaft, an open technique with compression plating using AO
principles is advisable. However, in fracture patterns that have near
circumferential or segmental comminution, bridge plating techniques are
applicable. This can be accomplished with submuscular plate placement
or an open technique that leaves all the intercalary comminuted
segments undisturbed. No matter what technique is chosen, the
vascularity to the femoral shaft and the associated fracture segments
should be preserved.
patterns, a lateral incision is used. The length of the incision should
be of adequate size to allow placement of a long plate directly on the
lateral femur without traumatic retraction of the muscular envelope.
The iliotibial band is sharply incised along the length of the
incision. The vastus lateralis is then atraumatically elevated from the
posterior limb of its fascia, from distal to proximal. The perforating
vessels should be sequentially identified, isolated, and ligated. The
muscle can then be elevated off the periosteum at the lateral femur. No
periosteal stripping is necessary, and no deep retractors placed over
the anterior femur should be used.
useful adjuncts are available. The patient should be pharmacologically
paralyzed to allow for reestablishment of femoral length. Several
useful intraoperative measures are available to assist with the
indirect reduction of the femoral shaft. A femoral distractor can be
applied to facilitate restoration of length, alignment, and rotation.
Alternatively, a distal femoral traction pin can be applied, allowing
for manual distraction and rotational control. The plate can be applied
and fixed to one end of the femur followed by the use of a push screw
or the articulated tensionerdistractor. Finally, joysticks consisting
of 5-mm Schanz pins can be placed into each femoral segment to assist
with control of the alignment and rotation.
Even in simple patterns, a 10-hole, 4.5-mm plate should be considered a
minimum length. The choice of a broad or a narrow plate depends on the
femoral diameter and the size of the patient. As the fracture
comminution increases, so should the plate length such that at least
five screw holes of plate length are present on each side of the
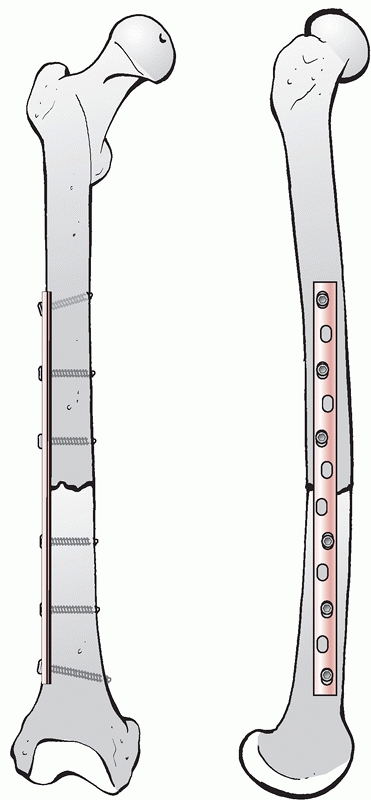
fracture (Fig. 50-10). For transverse
fractures, appropriate over-contouring of the plate should be
performed, and the fracture should be appropriately compressed. This
can be accomplished with a pull screw, the articulated tensioning
device, eccentric screw placement(s) within the holes, or combinations
thereof. For oblique fractures, overcontouring of the plate is
inadvisable and compression should be obtained with standard techniques
using the obliquity of the fracture relative to plate. A lag screw
through the plate increases the construct rigidity and should be used
if appropriate. The number of screws necessary for adequate
stabilization remains unknown, although eight cortices on each side of
the fracture have been recommended in the past.166 The number of screws and the number of cortices are less important than the plate length.261,262 There are very few disadvantages to the use of a longer plate with fewer screws other than the need for a longer incision (Fig. 50-11).
However, screws can be placed percutaneously if a longer implant with a
smaller surgical approach is desired. Three screws in each segment
should maximize the
biomechanical
fixation. This should include a screw at the end of the plate
(preferably directed obliquely) and a screw as close as possible to the
fracture. A third screw in each segment further increases the torsional
stability of the bone implant construct.262
 |
|
FIGURE 50-10 Femoral plating for a simple fracture pattern. Plate length and screw position are more important than screw number.
|
 |
|
FIGURE 50-11 This 74-year-old male sustained a periprosthetic femoral shaft fracture after a motor vehicle crash (A, B). He had no previous problems with his hip prosthesis. The femur was plated using an extensile lateral approach (C-F).
Given the spiral fracture configuration, a direct fracture reduction with lag screw fixation was performed. A long neutralization plate that spanned the entire femur was used. |
The goal is to minimize any associated trauma to the muscular envelope
and the periosteum surrounding the femur. This can be accomplished by
using small incisions at the palpable proximal and distal aspects of
the lateral femur. A plate of appropriate length can be contoured and
slid beneath the vastus lateralis along the length of the femur. A
plate that spans most of the femur exploits the palpable portions of
the femur proximally and distally and is actually easier to apply than
a shorter plate. The lack of an appropriate anterior bow in long plates
can make plate application difficult in simple patterns. However,
incomminuted fractures in which bridging fixation is planned and
submuscular techniques are most applicable, the use of a straight plate
is usually not problematic. After the plate is placed on the midlateral
aspect of the femur, the length, alignment, and rotation of the femur
should
be
restored either manually or with a femoral distractor. Screws can then
be fixed proximally and distally without difficulty. Additional screws
are placed through percutaneous stab incisions along the lateral femur
according to the aforementioned biomechanical principles.
unnecessary after a properly performed plate application for a femoral
fracture. Early active range-of-motion exercises should be encouraged
as soon as wound healing allows. Weight bearing should be limited to
the weight of the leg until there is radiographic evidence of healing
and resolution of fracture site discomfort. Radiographic evaluations at
6-week intervals are usually adequate for following the progression of
healing. If direct reduction and compression plating are used, primary
bone healing is predicted. As a result, radiographic evidence of
healing and, thus, weight bearing are frequently delayed for 4 to 5
months.93,229
If bridge plating and indirect reduction techniques are used, healing
should progress similar to intramedullary nailing with callus formation
evident on radiographs. As a result, weight bearing can usually begin
earlier. Plate removal should be limited to symptomatic patients and
should be delayed for a minimum of 18 to 24 months because of the risk
of refracture.
shaft fractures using AO techniques were relatively consistent. Implant
loosening occurred in 6% to 11% of cases, nonunion in 2% to 8%, and
infection in 0% to 7%. Bone grafting was recommended for defects or in
cases with questionable fixation.56,167,238,271 For the most part, direct reduction and stable fixation of the fracture were recommended. Ruedi and Luscher238
reported on the results of plating 126 comminuted fractures using
Association for the Study of Internal Fixation techniques. Plate
failures and nonunion were observed in less than 10% of cases, yet the
authors still recommended bone grafting in all fractures of the femoral
shaft fixed with a plate. Surprisingly, as early as 1979, bridge
plating of comminuted fractures was recommended in an effort to
maximize the vascularity and healing of these fragments.169
reported on 141 comminuted diaphyseal femur fractures treated with
immediate plate fixation. More than one third of these fractures were
open. Autogenous bone grafting, typically from the ipsilateral proximal
tibial metaphysis, was performed in 95% of patients. Ten plate failures
were observed (7%), and most healed after subsequent treatment with an
intramedullary nail. There was one infection in a patient with an open
fracture. The average time to union was 17 weeks. Similarly, Geissler
et al.93 reported a 93% union rate
at 16 weeks in 71 plated femoral shaft fractures. Cancellous bone
grafting was used in 69% of patients and was recommended as a standard
supplement in this technique.
in plated femoral shaft fractures may be unnecessary if indirect
reduction techniques and a biologically friendly surgical approach are
used.237,286,293,315
Although simple fracture patterns continue to be amenable to direct
reduction and stable fixation, comminuted fractures can be treated by
completely avoiding the fracture fragments. By bridging the fracture
using incisions well away from the fracture, a plate can be slid
beneath the vastus lateralis and applied to the lateral femur with a
combination of percutaneously applied and openly applied screws. The
main goals of this technique are restoration of femoral length,
alignment, and rotation with preservation of blood supply to the
fracture and comminuted fragments. Early reports suggest that this
technique can be safely performed with results similar to other
indirect methods for femoral stabilization.237,286,293,315
plating was retrospectively compared by Zlowodski et al. No bone grafts
were used in either group and a low infection rate was observed and was
unrelated to the surgical approach. However, the submuscular technique
was associated with a higher rate of suboptimal reductions (29%)
compared to a biologically respectful open approach.315
It is the most common treatment for femoral shaft fractures in adults,
and virtually all orthopaedic surgeons have had some exposure and
experience with the techniques necessary to successfully perform a
femoral nailing. However, there are numerous aspects to the procedure
that require emphasis to ensure a good result with minimal
complications. Many of the technical aspects of planning, positioning,
reduction, nailing, and interlocking are appreciated with increasing
experience.
the fracture pattern, which is dependent on an understanding of the
mechanism of injury and the applied force. Good-quality biplaner
radiographic images are necessary and should be reviewed to determine
the canal dimensions, femoral length, presence of comminution, femoral
morphology, and presence of nondisplaced fracture extensions that may
complicate treatment. Contralateral femoral radiographs can be obtained
if there is concern regarding the femoral morphology or in cases with
significant comminution, which makes estimates of femoral length
unreliable. The lateral radiograph should be scrutinized to determine
the femoral bow. Because virtually all femoral nails have a radius of
curvature that is greater (i.e., less curved) than the normal femoral,
increasing femoral bow can make nailing difficult using unmodified
implants. The radiographs should be viewed to determine whether there
is any associated preinjury osseus pathology such as metastatic
disease, primary bone tumor, osteomyelitis, or malunion.
and diameter of a femoral nail should be anticipated before considering
operating on a patient. The femoral length can be determined by several
methods. Radiographs of the contralateral femur can be measured with a
ruler that is corrected for magnification. In fractures without
significant comminution, traction radiographs of the injured femur can
be used to estimate the length. Alternatively, a long ruler can be used
to measure the uninjured femur from the palpable greater trochanter to
the lateral epicondyle. The diameter of the intramedullary canal should
be estimated at the narrowest portion of the femoral canal at the
femoral isthmus. This is usually based on the lateral radiograph.
Although these measures are estimates only and a more accurate
assessment can be obtained intraoperatively, this allows the surgeon to
ensure that an adequate supply of femoral nails with the predicted
lengths and diameters are available.
Patients with small femoral canals (<10-mm) may require special implants specifically designed for these situations.
|
TABLE 50-4 Selected Reports of Femoral Fracture Treatments and Results
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
during the time period extending from identification of the injury to
surgical stabilization. Because delay is unpredictable and frequently
unanticipated, skeletal traction should be placed as early as possible.
Traction maintains femoral length, prevents further soft tissue injury,
provides patient comfort, and may limit the amount of ongoing blood
loss into the thigh. A distal femoral traction pin is preferred to a
proximal tibial pin because of the more direct line of pull and the
high incidence of associated knee ligamentous injuries. A large
traction pin is painful, traumatic to place, and unnecessary. A small
pin (5/64-inch or 2-mm) can be placed from medial to lateral at the
distal femur and tensioned with a traction bow. The ideal location is
anterior in the distal metaphyseal region of the femur, allowing future
passage of the antegrade nail. Approximately 15 to 20 pounds of weight
(or up to 15% of body weight in larger patients) is usually adequate to
maintain femoral length in most patients if traction is applied
acutely. A pulley system at the end of the bed or, ideally, balanced
suspension should be used.
antibiotics consisting of a first generation cephalosporin in patients
without an allergy should be used. Additional antibiotic coverage is
necessary in open fractures and is dependent of the level of
contamination, and the estimated associated soft tissue injury.
fracture depends on numerous factors including the method of
stabilization, associated injuries, and surgeon comfort (Table 50-5).
In a patient with a known spine injury or in a patient who cannot be
adequately evaluated before femoral stabilization, protection of the
spine from further injury is vital. Lateral bending of the spine can be
minimized with supine positioning on a radiolucent table and femoral
stabilization with a retrograde nail, an external fixator, or a plate.
Supine positioning on a radiolucent table with antegrade nailing
requires some degree of lateral bending to allow access to the starting
point. This can be minimized with placement of a trochanteric entry
nail, which allows a more lateral starting point than with piriformis
entry nails.
with the patient lying supine or lateral, each position having specific
advantages and disadvantages. In addition, nailing can be done on a
fracture table or a radiolucent table with or without traction. With
either position on either type of table, the accurate placement of a
distal femoral traction pin assists with the intraoperative assessment
of femoral rotation and attainment of
the
proper length. Even if a pin has been placed in the emergency
department for temporary application of traction, the pin position
should be confirmed fluoroscopically in the operating room and changed
if not in the proper location. An ideal pin should be perfectly
parallel to a condylar overlap lateral of the distal femoral condyles,
ensuring that the rotation of the distal femur is known. This is best
accomplished by placing the pin under fluoroscopic guidance on the
lateral view with the femur properly rotated. In addition, the pin
should be positioned anteriorly to allow passage of the nail posterior
to the pin. This eliminates the time-consuming and frustrating exercise
of trying to remove the traction pin as the femoral nail is passed
later in the procedure. Because of the natural tendency for a valgus
deformity when performing antegrade nailing in the lateral position,
consideration can be given to placing the pin somewhat angulated in the
coronal plane (proximal lateral to distal medial).
|
TABLE 50-5 Lateral versus Supine Positioning for Antegrade Nailing
|
||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||
entire patient by the anesthesiologists, general surgeons,
neurosurgeons, and other physicians involved with ongoing resuscitation
and treatment. This is especially important in patients with multiple
thoracic or abdominal injuries, spine fractures, pelvic ring injuries,
or multiple extremity fractures. Patients with multiple extremity
injuries can undergo simultaneous treatment if positioned supine.
Rotational and angular deformities may be minimized with supine
positioning compared with lateral positioning. The rotation of the leg
is more easily judged with the entire limb accessible. The main
disadvantage with supine positioning is difficulty with identifying the
proper starting point if a first generation antegrade nail is
anticipated. The gluteal muscles and the associated fat on the lateral
thigh make palpation of the greater trochanter difficult. Hip adduction
improves access to the proximal femur. With lateral positioning,
patient access is limited and pulmonary function is suboptimal.
However, identification of the starting point is improved because the
hip is flexed, angulating the torso away from the line of the femoral
shaft. As well, because of the natural adduction of the hip, the soft
tissues of the lateral hip tend to fall away from the anticipated
incision.
Although not necessarily supported in the literature, use of the
fracture table may minimize the number of surgical assistants
necessary. A distal femoral traction pin is preferable to traction
applied to the foot with the fracture table. This allows direct control
of the distal femoral segment, ensuring an accurate assessment of
rotation without distracting across the knee joint. In addition, distal
femoral traction allows the knee to be flexed, minimizing the
intraoperative stretch and tension on the sciatic nerve. Alternatively,
a traction pin can be placed at the proximal tibial metaphysis. This
pin location prevents interference with the medullary implant, however,
traction is applied across the potentially injured knee joint and is
not in direct line with femoral axis. A combination of limb adduction
and tilting of the trunk away from the ipsilateral hip improves access
to the nail entry site. However, this requires that the patient’s
lumbar and thoracic spines are stable to positioning alterations.
Fluoroscopic imaging in the AP and lateral planes is usually without
difficulty. The uninjured leg can be positioned with the hip and knee
flexed to 90 degrees. However, numerous reports of unrecognized
compartmental syndrome in the uninjured leg during lengthy femoral
nailing procedures with the use of a well leg holder that supports the
calf emphasize the need to either check the leg intraoperatively every
hour or abandon this position completely.5,76,179 The relationship between compartmental pressures and time in a well-leg holder was evaluated by Tan et al.266
in a study of 10 patients undergoing femoral nailing procedures. The
authors demonstrated an immediate increase in pressure with positioning
in the well-leg holder that trended upward with time. The pressure
immediately returned to normal when the leg was taken out of the
holder. They further identified a correlation between leg pressure and
body mass index.266 The combination
of decreased perfusion caused by leg elevation and external pressure
from a calf support has been confirmed to cause a decrease in the
difference between diastolic blood pressure and the intramuscular
pressure when the uninjured leg is placed into a well-leg holder on a
fracture table.179 On the basis of their study in healthy volunteers, Meyer et al.179
demonstrated that positioning that leaves the calf free increases the
difference between the diastolic and intramuscular pressure,
potentially decreasing the risk of compartmental syndrome. This can be
accomplished by supporting the leg at the knee and the heel, leaving
the calf free to hang.179
Alternatively, the uninjured leg can placed into a foot holder on the
traction table. The uninjured leg can be “scissored” with the hip and
knee extended. In this position, lateral fluoroscopic imaging of the
proximal femur is compromised but the safety of the uninjured leg is
increased.
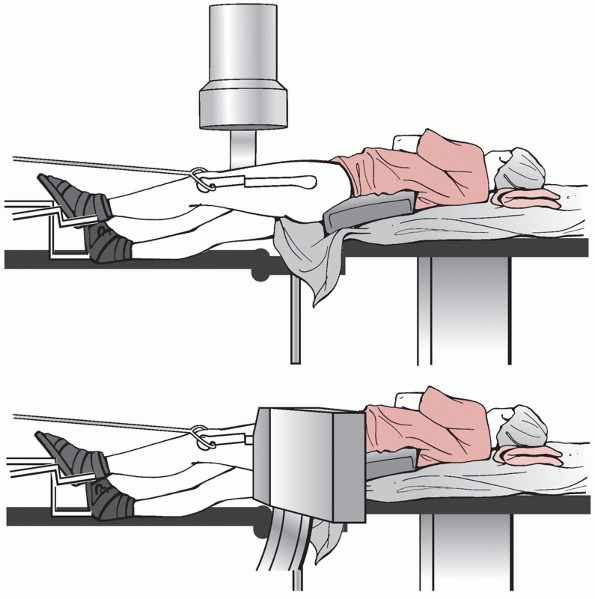 |
|
FIGURE 50-12
Supine position for closed intramedullary nailing using a fracture table. The image intensifier is positioned on the side opposite the injured extremity. In order to obtain intraoperative lateral imaging, the uninjured leg can be extended (as shown). |
The initial positioning is more time consuming and there is limited
access to the patient. This is especially important in the patient with
associated thoracic trauma or pulmonary injury. The natural tendency is
to allow the femur to internally rotate excessively during lateral
nailing, and the initial patient positioning should combat this.
Internal rotation of the distal segment should be limited to 10 or 15
degrees. The uninjured leg is positioned with the knee and hip
extended, allowing unimpeded fluoroscopic imaging in both planes. The
knee height should be appropriately adjusted to resist the commonly
observed valgus deformity.
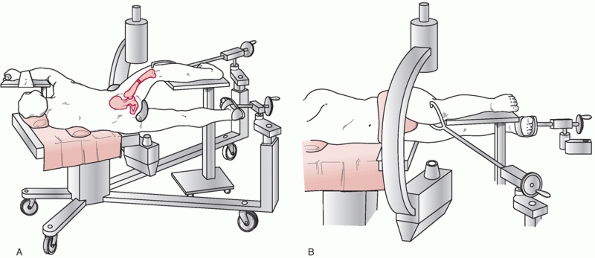 |
|
FIGURE 50-13 Lateral patient position for closed intramedullary nailing. Image intensifier is positioned anterior to patient. A. View from behind patient. B. View from in front of patient.
|
positioning on a radiolucent table with manual traction or intraoperative distraction143,174,254,260 (Fig. 50-14).
This technique has been used successfully and is the standard in most
trauma centers. The main disadvantage to the manual technique is the
need for a trained assistant. However, the strategic use of an
intraoperative femoral distractor or modification of the operating room
table to allow weights to be placed at the end of the bed minimizes the
need for assistance. For supine nailing on a radiolucent table, a bump
is placed medially beneath the hip and the patient is moved as
laterally as possible to maximize access to the lateral hip and flank.
The bump is placed beneath the pelvis and not the greater trochanter,
therefore maximizing access to the hip. The entire leg and ipsilateral
hip are prepped proximally past the level of the iliac crest. A distal
femoral traction pin can be placed as previously described to allow for
application of manual traction and to control rotation. Alternatively,
a femoral distractor can be applied, eliminating the need for a distal
femoral traction pin as well as an assistant.174
Distally, a half pin can be placed anteriorly in the metaphysis from
lateral to medial. Proximally, a half pin can be placed from anterior
to posterior at the level of the lesser trochanter, medial to the
predicted path of the nail. This pin position is at least 2.5 cm from
the femoral nerve and 3.0 cm from the femoral artery based on cadaveric
dissections.174 Alternatively, the
proximal pin can be placed from lateral to medial at the lesser
trochanter, posterior to the predicted path of the nail. The half pin
locations and technique have been described in detail by Baumgaertel
and coauthors.15 The success of femoral nailing without a fracture table has been confirmed in several recent studies. Karpos et al.143
prospectively followed 32 consecutive femoral fractures that were
reduced and stabilized with manual traction. They reported good overall
alignment and decreased operative time compared with comparable femoral
nailing using a fracture table. In addition, more than one third of
patients were able to undergo multiple extremity procedures with the
same operative draping.143 Similarly, Sirkin et al.254
reported similar results with femoral nailing on a radiolucent table
using manual traction only. Compared with the use of a fracture table,
they found the procedure to be more rapid, required fewer table
transfers, allowed accurate reduction, and produced no increased
morbidity.254 In a prospective study
comparing the use of a fracture table with manual traction, Stephen and
colleagues reported an increased incidence of malrotation and increased
operative time with the use of a fracture table.260
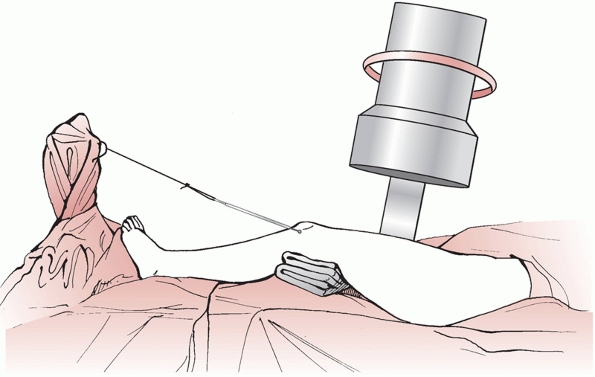 |
|
FIGURE 50-14
Supine positioning on a radiolucent table. A small bump placed centrally combined with lateral placement of the patient allow access to the proximal femur. Intraoperative traction can be used. |
shaft can be difficult and is required during several key stages of
femoral nailing. The fracture must be reduced during guidewire passage,
during reaming, and when the nail is passed. There are a number of
techniques that can facilitate reduction, many or all of which may be
required. Many of these reduction maneuvers are dependent on the
patient’s position and the type of operative table.
by using a femoral distractor, manual traction, or a fracture table.
The use of a femoral distractor has been described in detail as a
useful adjuvant for obtaining length in both acute fractures as well as
delayed nailings15,174 (Fig. 50-15).
Although only one half pin is placed into each of the proximal and
distal segments of the femur, surprisingly good control of alignment
can be obtained. In fractures without segmental comminution, an
accurate assessment of the length after application of a femoral
distractor is easily obtained from fluoroscopic clues. If segmental
comminution exists, the distractor is useful for indirectly
reassembling the intercalary fragments by tensioning the soft tissue
attachments, frequently providing indications regarding length. If the
length cannot be determined fluoroscopically, comparison with the
uninjured femoral length or postoperative CT scanning may be necessary.
with reduction of the femur. Crutches, cooled mallets, large
retractors, and large reduction levers can all be used depending on the
patient position and the primary deformities. If supine nailing
on
a radiolucent table is used, soft bumps of varying heights placed under
the leg near the fracture can be used to correct the angular and
translational deformities seen on the lateral fluoroscopic projection.
In addition, a cannulated nail can be placed into the proximal segment
after it has been prepared with an awl or reamers, thus allowing
control of the proximal segment and passage of the guidewire. A short
small-diameter nail or a specifically designed cannulated device is
available from many nail manufacturers specifically for this purpose.
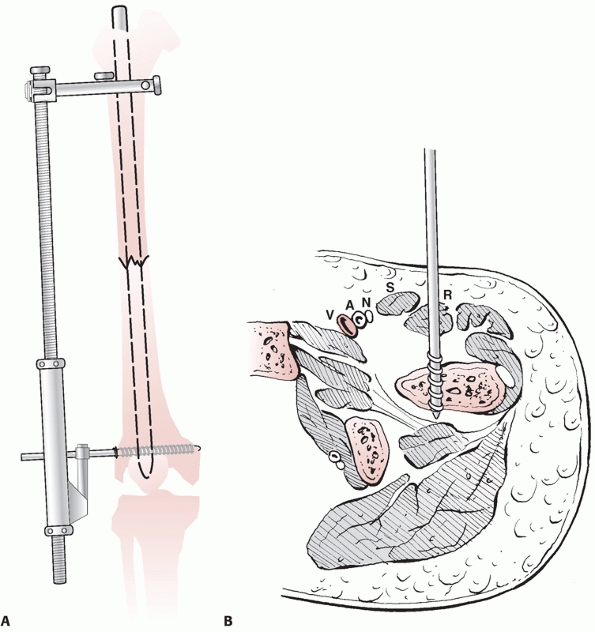 |
|
FIGURE 50-15 A.
A femoral distractor can be placed to allow for restoration of femoral length and rotation. This requires strategic placement of the half pins to ensure that the path of the intramedullary nail is not violated. The distal pin can be placed transversely from lateral to medial in the metaphysis. The proximal pin can be placed from lateral to medial or from anterior to posterior as depicted. B. The location of the relevant soft tissue structures in the vicinity of a pin placed from anterior to posterior at the level of the lesser trochanter. (Redrawn after McFerran MA, Johnson KD. Intramedullary nailing of acute femoral shaft fractures without a fracture table: technique of using a femoral distractor. J Orthop Trauma 1992;6:271-278.) |
This technique allows correction of both angular and rotational
deformities simultaneously. Through small lateral (or anterior) stab
incisions, half pins can be placed either unicortically in the
midlateral aspect of the femur or posteriorly in the thick portion of
the linea aspera. These pins can be used to manipulate the fracture in
the coronal sagittal planes by attaching T-handle chucks to each. If
the sagittal plane translational deformity is largely corrected by
strategically placed bumps, lateral unicortical pins can be used to
correct the coronal translation and angulation with simple
manipulations. The reduction can be maintained while the guidewire is
passed as well as during reaming (Fig. 50-16). To avoid damage to the reamers, the tips of the pins should not be within the intramedullary canal.
Soft Tissue Impact. Current nail designs allow for placement of
antegrade intramedullary implants at the piriformis fossa and in the
region of the greater trochanter. Nails designed to enter at the
trochanteric tip are specifically designed with an additional proximal
lateral bend to facilitate nail placement through this eccentric
starting portal relative to the femoral canal. The piriformis nail
entry location has the advantage of predictably aligning with the
femoral canal in both planes. A trochanteric entry may be easier to
identify given the improved access to the greater trochanter. This may
be especially important in obese patients.228
However, proper placement of the implant requires the surgeon to
accurately match the intraoperative fluoroscopic entry angle with the
lateral bend of the specific nail. A mismatch can be associated with
iatrogentic proximal femoral fracture in shaft fractures, and
malreduction in subtrochanteric fractures.92,141,204
actually a misnomer. The actual location of the ideal entry point for a
medullary implant that is aligned with femoral canal is more accurately
termed the “trochanteric fossa.”208
However, given the general acceptance of the term “piriformis fossa”
when referring to the depression on the inner surface of the greater
trochanter (the “trochanteric fossa”), “piriformis fossa” will be used
in this chapter.
The functional consequences are largely unknown, but the local damage
may contribute to the frequently observed incidence of hip pain (10% to
40%) following antegrade intramedullary nailing. As a result,
alternative entry sites at the proximal femur have been investigated.90,184,220
Patient and limb positioning may have an impact on the local soft
tissue injury during percutaneous antegrade piriformis entry femoral
nailing. In a cadaver study based on retrograde placement of a reamer
proximally to simulate the correct entry site for antegrade nailing,
Ozsoy and coauthors206 measured the
distance to and identified the potential risk of injury to the superior
gluteal nerve. The authors concluded that limited hip flexion and
adduction during nail insertion increases the risk of injury to the
superior gluteal nerve and the gluteus medius muscle. Therefore,
lateral patient positioning or freelegged may allow increased hip
flexion and adduction, thereby limiting these risks.206
 |
|
FIGURE 50-16
The presence of a segmental fracture of the diaphysis of the femur can make reduction and intramedullary nailing more difficult (A). Temporary Schanz pins can be placed percutaneously to allow manipulation, control, and reduction of the fracture (B,C). Initially, the pins can be placed into the medullary canal to optimize control of the fracture segments. During reaming, the pins should be backed out until they are unicortical. The reduction can be maintained with the pins until after the nail is placed across the fractures (D). |
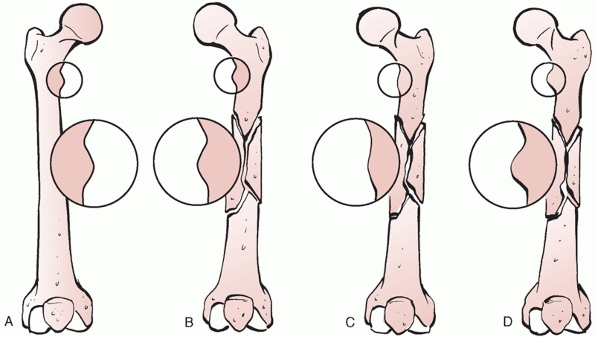 |
|
FIGURE 50-17
The shape of the lesser trochanter can be used to assist with the intraoperative determination of femoral rotation during intramedullary nailing. Before starting the procedure, an anteroposterior (AP) fluoroscopic image of the uninjured proximal femur with the femur in neutral rotation is stored (A). Before interlocking of the injured extremity, the rotation of the proximal segment is adjusted such that the contour and shape of the lesser trochanter are identical to the other side (B). If the proximal segment is internally rotated (external rotation of the entire femur), the lesser trochanter will appear smaller (C). If the proximal segment is externally rotated (internal rotation, of the entire femur), the lesser trochanter will appear larger (D). (Redrawn after Krettek C, Miclau T, Grun O, et al. Intraoperative control of axes, rotation, and length in femoral and tibial fractures. Technical note. Injury 1998;29:C29-C39.) |
Using a cadaver model and three different nail entry portals
(piriformis fossa, in the usual location of a first-generation nail;
anterior to piriformis fossa, in the usual location of a reconstruction
nail; and at the tip of the greater trochanter, in the location of some
trochanteric nails), the authors identified injury to multiple
structures. Specifically, the trochanteric entry portal was associated
with frequent injury to the piriformis tendon (80%) and the obturator
internus (25%), the reconstruction nail entry portal was associated
with less frequent injury to the piriformis tendon (50%) and the
gluteus mimimus (25%), and the piriformis fossa entry portal was
associated with frequent injury to the obturator internus (86%), the
piriformis tendon (71%), the obturator externus (29%) and branches from
the medial femoral circumflex artery.75
In another cadaver study supporting a lateral nail entry point, Moein
et al. found increased injury to branches of the medial femoral
circumflex with a piriformis nail entry.184
The impact of injury to branches of the medial femoral circumflex
during antegrade intramedullary nailing is unknown although the remote
possibility of avascular necrosis of the femoral head exists. However,
since the introduction of antegrade intramedullary nailing, this
complication has been limited to a few recent isolated case reports,106,222 indicating that avascular necrosis is extraordinarily uncommon and the relationship to nail entry is unspecified.
because of the improved ease of starting point identification and nail
insertion (Fig. 50-18). The local soft tissue impact of these
trochanteric entry femoral implants has been investigated with conflicting conclusions.90,173,184,220
Trochanteric entry nails with large screws or helical blades into the
femoral head require a large (usually 17 mm) entry site reamer. In a
study using a cadaver model to investigate the impact of a large entry
portal at the tip of the greater trochanter, McConnell et al.173
reported disruption of an average of 27% of the gluteus medius tendon.
However, a modified medial trochanteric portal placed just medial to
the trochanteric tip (using a 14-mm reamer) was associated with no
visible damage to the tendinous insertion of the gluteus medius in a
different cadaver model.220 Further,
the presence of an alternative entry site lateral and distal to the tip
of the greater trochanter has been demonstrated. This greater
trochanteric bald spot is covered by the subgluteus bursa, is without
tendinous insertion, and may represent an alternative entry site for
specific nail designs.90
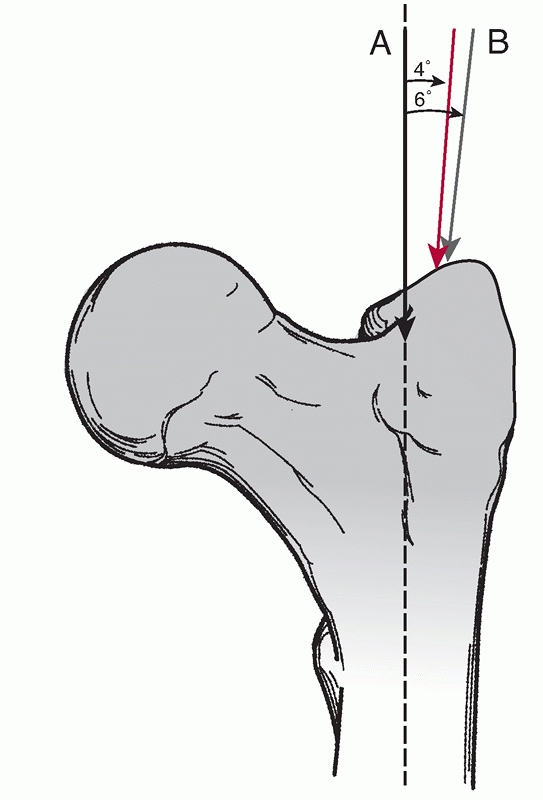 |
|
FIGURE 50-18
On the AP radiographic view, the entry location and direction for a piriformis nail is depicted with the black arrow and is parallel with the femoral shaft on both radiographic views. The entry angle and location for a trochanteric nail depends on the specific design parameters of the implant. Typically, a 4- to 6-degree entry angle is required (red and gray arrows) although some implants use a lateral entry on the proximal femur with a larger entry angle. |
and percutaneous approaches for insertion of an antegrade nail are
possible. The traditional open approach is accomplished through a
longitudinal incision that begins at the proximal tip of the greater
trochanter and extends proximally over a variable distance depending on
the size of the patient. Curving the incision posteriorly in line with
the natural bow of the femur maximizes access to the proper starting
point. The gluteus maximus fascia is incised in line with the incision,
and the muscle fibers can be separated bluntly. The greater trochanter
can be palpated directly, as can the enveloping fascia of the gluteus
medius. The piriformis fossa (or more accurately named, the
trochanteric fossa208) can then be
palpated directly, allowing placement of a curved awl or terminally
threaded pin. Alternatively, a relatively percutaneous approach can be
used (Fig. 50-19). This technique requires
placement of a pin into the piriformis fossa followed by the use of an
appropriately sized cannulated drill with a diameter of 8 to 10 mm.
Frequently this incision (10 to 20 mm in length) is located 10 to 20 cm
proximal and slightly posterior to the palpable greater trochanter.
If the awl appears to be on top of the lateral aspect of the femoral
neck on the AP fluoroscopic projection, the starting point is too
anterior relative to the piriformis fossa. The piriformis fossa is
somewhat posterior to the femoral neck
on
the lateral fluoroscopic image and inferior to the cephalad neck of the
femur on the AP image. The awl can then be advanced in line with the
intramedullary canal on both views. If a cannulated drill is chosen to
initiate the starting portal, the guide pin can be advanced with a
drill or a mallet down the canal of the femur using fluoroscopic
imaging to confirm accurate placement. The starting point is critical
to ensure safe passage of a medullary implant, and a suboptimal
position should not be accepted. A starting point that is too anterior
increases the proximal femoral hoop stresses and increases the
likelihood of femoral bursting. With the patient positioned supine on a
radiolucent table, access to the proper starting point is improved with
maximal adduction of the leg. In more proximal fractures in which
manual adduction of the leg fails to adduct the proximal femoral
segment, a percutaneously placed spike pusher or Schanz pin at the
lateral aspect of the proximal femur can assist with presenting the
starting point.
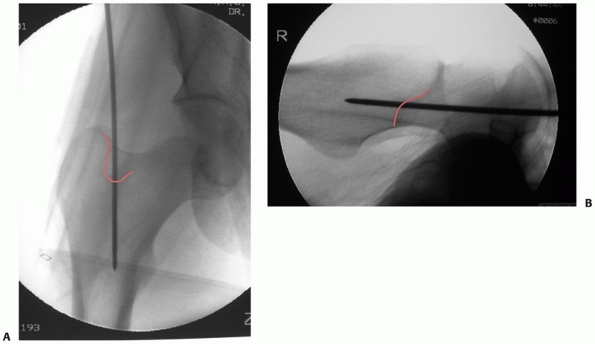 |
|
FIGURE 50-19 The starting point for a femoral nail is shown in the AP (A) and lateral (B)
fluoroscopic images. The lateral image demonstrates the pin position relative to the femoral neck, greater trochanter, and calcar femorale. The outline of the piriformis (trochanteric) fossa should be apparent intraoperatively and is highlighted in red on the AP and lateral views. |
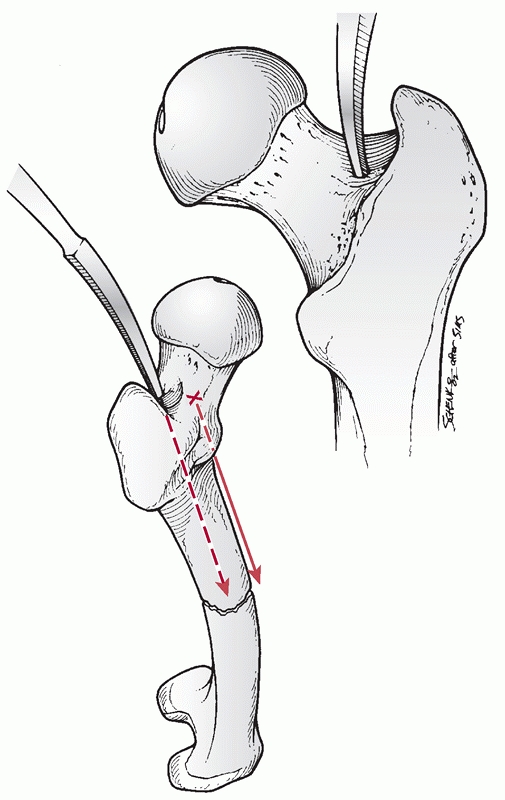 |
|
FIGURE 50-20
Placement of the entrance hole is critical for a successful closed nailing. The tip of the awl should be in line with the longitudinal axis of the medullary canal in both the AP and mediolateral planes. A more anterior placement of the entrance hole can result in inadvertent perforation of the anterior cortex of the proximal femur. |
The medullary cavity proximal exit point was defined in one study using
16 cadaver femora. The location was determined by obtaining radiographs
in 12 sequential planes separated by 15 degrees axially in femurs that
were filled with a radioopaque substance. In 88% of specimens, the
entry point for a straight nail was identified at the medial border of
the greater trochanter, at the tendinous insertion of the piriformis,
and 2.1 cm anterior to the posterior border of the greater trochanter.
For nails with a radius of curvature of 100 cm the nail entry point is
only 0.7 mm anterior to the dorsal edge of the trochanter.92
Because most available antegrade nails have a femoral bow that is
greater than 100 cm, logic suggests that the ideal starting point is
located somewhere between these reported locations.
guidewire can be passed down the canal of the femur and confirmed with
biplanar fluoroscopic imaging. In young patients with dense bone,
T-handled hand reamers may be necessary to define the intramedullary
canal in the pertrochanteric region. This step can be avoided if a
cannulated drill technique is used for initiation of the starting
point, assuming that the drill is passed distally enough in line with
the medullary canal. The guidewire should be bent distally to allow
some directional control. A guidewire without a ball-tip should not be
used if reaming is planned. The guidewire is then advanced down the
canal of the femur to the level of the fracture. With pharmacologic
relaxation, the fracture is then reduced to allow passage of the
guidewire across the fracture and into the distal segment. Numerous
reduction maneuvers as previously outlined are useful for this easily
described yet practically difficult portion of the procedure. The bend
at the end of the guidewire can be exploited to assist with passage of
the guidewire (Fig. 50-21). The guide wire is
then advanced distally and should terminate centrally in the distal
femur. Any residual angulation should be corrected before advancement
of the guidewire distally. This is especially true in fractures that
are distal to the femoral isthmus, especially if the fracture is in the
distal third. A mallet is used to seat the guidewire into the dense
bone of the distal femur to ensure that it remains in position during
reaming. For distal fractures, a true AP and lateral image of the
distal femur should be obtained to ensure central placement of the
guidewire. Femoral length should then be confirmed before determining
the desired nail length. A second guidewire of equal length can be used
to determine the proper length of the nail necessary. Knowledge of the
specific nail characteristics and the normal level of insertion at the
piriformis fossa is necessary to determine the proper length.
 |
|
FIGURE 50-21
A small bend at the end of the bulb-tip guide pin allows for manipulative correction of any residual translation at the fracture site. |
and down the canal of the femur. The fracture should be maintained in a
reduced position during the passage of each reamer to minimize
eccentric bone removal. The process of reaming produces elevated
intramedullary canal pressures and embolism of fat into the venous
system. This is related both to the technique and the design of the
reamers. Reamers should be advanced slowly and incrementally increased
in diameter to minimize the pressure and fat embolism. Reamers should
be sharp, have deep flutes, and have a narrow flexible shaft.24,194,210,218
With the currently available locked intramedullary implants, the
placement of large-diameter nails with an intimate fit along a long
length of the medullary canal is no longer necessary. Depending on the
biomechanical characteristics of the nail, the patient’s size, the
presence of comminution, and the desire for immediate weight bearing, a
minimum nail diameter can be chose by the surgeon. A nail diameter that
is coincident with isthmic cortical chatter felt during reaming is
probably adequate in most cases. The canal is overreamed by 1.0 to 1.5
mm to allow passage of the nail. Failure to enlarge the medullary canal
can result in nail incarceration or iatrogenic femoral comminution,
both of which are avoidable complications.
many currently available nailing systems allow removal of the
ball-tipped guidewire through the nail, eliminating this step in the
procedure. The selected nail dimensions are then confirmed, and the
nail is attached to the proximal locking jig and placed over the
guidewire. The anterior bow of the nail can be used to ease the initial
insertion into the starting hole at the piriformis fossa. By internally
rotating the nail by 90 degrees, the tip of the nail can be placed
around the medial greater trochanter. The rotation of the nail is then
corrected to match the rotation of the femur. The nail is advanced to
the level of the fracture. At this point, the length, alignment, and
rotation of the femur should be corrected accurately. The nail is
advanced across the fracture, and the reduction parameters should be
confirmed. The nail is then driven distally to the appropriate depth (Fig. 50-22).
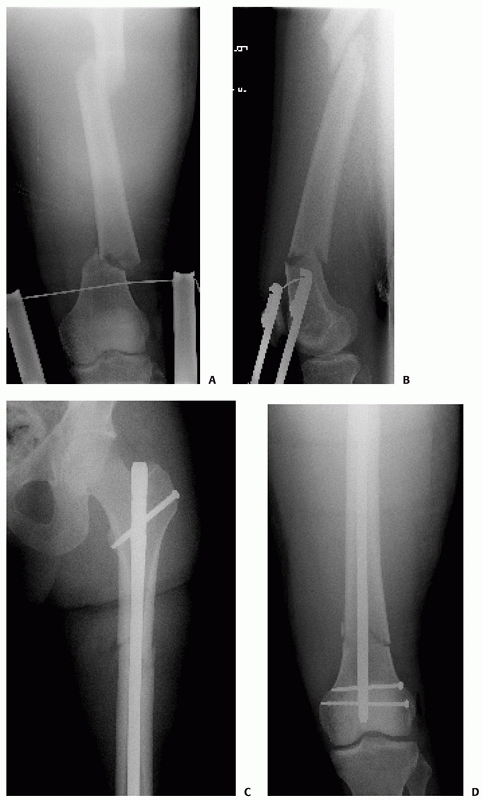 |
|
FIGURE 50-22
An antegrade nail can effectively stabilize a segmental femoral fracture with a proximal isthmic component combined with a distal metaphyseal fracture (A-D). |
simplified with the use of an external jig that allows placement of
screws using multiple sleeves. The configuration and location of these
screws are unique to each nailing system and may be transverse or
oblique
in direction. Static and dynamic screws may be available proximally or
distally. The choice to use one or two proximal interlocking screws
depends on the fracture stability after nailing, fracture location,
patient’s size, nail and screw diameters, and predicted postoperative
activity.
accomplished using a free-hand technique that is highly dependent on
fluoroscopic imaging. External targeting jigs remain under
investigation but have limited applicability because of targeting
inaccuracies. This is because of the long length of the implant and the
deformation that occurs with nail passage. Computer-assisted navigation
systems continue to be explored and will likely increase in popularity
in the near future.
the alignment, especially in rotation, must be maintained until at
least one screw is placed. With supine nailing on a radiolucent table,
the usual error in a rotationally unstable pattern is to externally
rotate the distal segment in an attempt to align the nail with the
image intensifier. To avoid this, the bump should be removed from
beneath the ipsilateral hip and the entire leg should be rotated as a
single unit. There are numerous choices for a free-hand technique.
Radiolucent drills, tapered pins, and radiolucent handles are all
available to assist with distal interlocking. Regardless of the
technique, the goal is to expeditiously place one or two interlocking
screws through the nail with the minimum amount of radiation.
perfectly round circle of the interlocking screw hole. A small
longitudinal skin incision is made followed by an incision through the
iliotibial band in line with the fibers. A sharp drill bit, preferably
with a trochar tip, is angulated obliquely to allow imaging, and the
tip is placed in the exact center of the projected hole as confirmed by
the lateral fluoroscopic image. The drill is then positioned parallel
to the path of the beam and advanced. The drill is then removed,
leaving the drill bit in position to confirm the direction and
placement. Small adjustments can be made on the basis of the
interpretation of the fluoroscopic image. The drill is then advanced
through the nail, a depth gauge is used to determine the screws length,
and an interlocking screw can be placed. The same procedure is repeated
for a second interlocking screw if necessary.
and reamed nails were placed in a closed fashion without interlocking.
These implants relied on the endosteal contact between the nail and the
femur for control of rotation, angulation, and length. The perceived
advantages compared with other techniques included early joint
mobility, early weight bearing, shortened hospital stay, decreased
pain, and predictable union. Fracture comminution and segmental
fractures could be treated with antegrade reamed nails with reports of
100% union and no infections.296,297 In the classic series of 520 femoral fractures in 500 patients treated with reamed intramedullary nailing, Winquist et al.298
reported a union rate of 99.1%. However, shortening of greater than 2
cm occurred in 10 patients and rotation of greater than 20 degrees was
identified in 12 patients.298
antegrade intramedullary nailing continued to expand and the results
have continued to improve. Brumback and coauthors described the
technical decision making, the need for static locking, and the
expected healing in a series of three articles reviewing locked
intramedullary nailing of femoral shaft fractures.37,39,40,42 The previously reported problems with shortening and postoperative loss or rotational alignment were largely eliminated.† Comminuted and rotationally unstable fractures healed in 98% of 112 reamed and interlocked nailings reported by Wiss et al.301 Similar results were reported by Sojbjerg et al.256 and Kempf et al.144
The use of interlocked nails in segmental femoral fractures was
similarly reviewed with healing observed in 97% of patients at an
average of 32 weeks without any additional interventions other than
nail dynamization.300 Brumback et
al. investigated the need for planned conversion from static to dynamic
fixation in a prospective study of 100 femoral shaft fractures treated
with intramedullary nailings.42 They
reported healing in 98% with static interlocking fixation and concluded
that the routine conversion to dynamic fixation was not necessary.42 Complications related to closed interlocked nailing was reported by Benirschke et al.18
in a review of 267 patients evaluated retrospectively and
prospectively. Intraoperative technical complications were observed
uncommonly, but functional outcomes were not as good as previously
appreciated; 37% of patients had pain and 39% had some limitations with
ambulation or standing. More recently, Wolinsky et al.304
reported their results with 551 femoral shaft fractures treated with
closed locked antegrade intramedullary nailing. The authors reported
union in 98.9%, infection in 1%, and no malunions with greater than 10
degrees of angulation.
thought to be from a combination of altered blood flow to the bone and
the local muscles, and the deposition of marrow and cortical elements
at the site of the fracture.‡ The impact of these factors
has been studied in animal models in both the tibia and the femur. More
recent studies suggest that reaming increases a number of growth
factors (platelet-derived growth factor, vascular endothelial growth
factor, insulin-like growth factor I, transforming growth factor
beta-1, and bone morphogenic protein-2) and this is hypothesized to
contribute to the positive healing effects of reaming.101 A potential negative effect of reaming includes injury to the inner two thirds of the bone.145
Animal studies in the tibia suggest that this process is reversed by 12
weeks after reamed nailing and by 6 weeks after unreamed nailing.248
However, reaming has been shown to have a positive influence on the
surrounding muscle perfusion, which may have implications for the
extraosseous blood supply to the bone and the healing fracture.125 In one study, periosteal blood flow was found to increase by a factor of six within 30 minutes of reaming.223 Total blood flow and callus blood flow increases have been similarly demonstrated in animal models.109
The role of unreamed intramedullary nailing for the treatment of
femoral shaft fractures remains unclear. Although the decreased damage
to the endosteal blood flow has been demonstrated in animal studies,
the clinical relevance with respect to infection and union remains
elusive. In addition, the ill effects of reaming on pulmonary function,
especially in the multiply injured patient, have not been definitively
demonstrated.§ The early clinical results of unreamed nailing for femoral shaft fractures reported by Krettek et al.151
were favorable, with only minor implant-related complications reported.
Nonunion was reported in 5.1% of patients in a multicenter review of
unreamed nails reported by Hammacher et al.114
The authors conceded that the use of a small nail inserted without
reaming did not produce a decrease in the number of patients with adult
respiratory distress.114 Herscovici et al.120
reported similar results in 125 fractures treated with unreamed nails.
Although this represented a mixture of antegrade and retrograde
nailings, only 93% healed after the index procedure.
The potentially negative effects of reaming for insertion of
intramedullary nails include elevated intramedullary pressures,
elevated pulmonary artery pressures, increased fat embolism, and
increased pulmonary dysfunction. The potential advantages of reaming
include the ability to place a larger implant, increased union, and
decreased hardware failure. The increased union is believed to be
attributable to both the enhanced biomechanical environment of a larger
implant and the enhanced biologic environment produced during reaming.
Reaming increases the periosteal blood flow and deposits osteoinductive
elements at the fracture, both of which may contribute to improved
healing.109,223
results of treating femoral shaft fractures with intramedullary
interlocked nails with and without intramedullary reaming.* Of interest are the different results observed with the retrospective and prospective studies comparing the two techniques.
treated with reamed (n = 50) and unreamed femoral nails (n = 97),
Giannoudis et al.97 reported union
at an average of 26.9 weeks in the unreamed group compared with 20.5
weeks in the reamed group. The operative time was shorter with the
unreamed technique, and there was no increased risk of infection,
angular deformity, or limb length discrepancy. This led the authors to
conclude that the unreamed technique was more rapid and had no
associated clinical problems of significance. Similarly, Reynders and
Broos224 retrospectively reviewed
107 closed femoral fractures treated with reamed (n = 54) and unreamed
(n = 53) intramedullary nailings. The authors reported no difference in
union time but significantly less operative time with the unreamed
technique. This led to the recommendation that unreamed femoral nailing
should be used to treat acute closed femoral shaft fractures.
presented differing results with contrasting conclusions. In a
prospective and randomized study of 81 patients treated with a
stainless steel statically locked intramedullary nail inserted with and
without reaming, Tornetta and Tiburzi278
reported statistically similar operative times, transfusion
requirements, and time to union when the entire groups were compared.
Reaming was associated with more rapid callus formation yet higher
blood loss. Further analysis of the data revealed faster union in the
subpopulation of patients with distal fractures when reaming was used.
Intraoperative technical complications occurred more commonly with the
unreamed technique.278 In a subsequent study by the same authors,277
172 patients were prospectively randomized and their results were
compared. With the larger data set available, the authors were able to
show a significant improvement in the time to union with reaming (80
days) compared with those nails placed without reaming (109 days). This
led to the conclusion that there is no advantage to the routine use of
nailing without reaming.277 Clatworthy and coauthors61
reported their results of a prospective and randomized trial comparing
reamed and unreamed nails in 45 patients with femoral shaft fractures.
Of note, the study was stopped early because of the high rate of
implant failure in the unreamed group. They reported more significantly
more rapid union (28.5 versus 39.4 weeks) and a much lower proportion
of nonunions at 9 months (18% versus 57% nonunion) in patients treated
with reamed nails compared with those treated with unreamed nails.
Secondary procedures to achieve union were more common in the unreamed
group. Finally, in a multicenter, prospective, randomized clinical
trial from seven level-I trauma centers sponsored by the Canadian
Orthopaedic Trauma Society, 224 patients were enrolled to compare the
rate of nonunion after intramedullary nailing with and without reaming.
The authors reported nonunions in 7.5% of patients treated without
reaming compared with 1.7% of patients treated with reaming. They
determined the relative risk of nonunion was 4.5 times greater without
reaming and with the use of a relatively small-diameter nail.48
attempted to determine the effects of reaming on the rates of nonunion,
implant failure, malunion, compartmental syndrome, pulmonary embolus,
and infection. Only prospective and randomized trials were used as part
of the analysis. Although the data represented both tibias and femurs
treated with intramedullary nails, the evidence suggests that reamed
nailing significantly reduces the rates of nonunion and implant failure
compared with unreamed nailing.21
Trochanteric entry nails have been used with success for the treatment
of intertrochanteric, subtrochanteric, pertrochanteric, and combination
fractures of the proximal femur. Some of the potential advantages of
the trochanteric tip as a starting portal for placement of a medullary
implant include less operative time and less intraoperative
fluoroscopy, largely because of ease of identification of the
trochanter as a starting point. If a nail designed for placement into
the piriformis fossa is placed through the more readily accessible
trochanteric tip, the complications of iatrogenic fracture comminution
and varus malreduction are increased.92,141,204
However, newer nail designs with appropriate proximal bends have
allowed for placement of a medullary implant through the trochanteric
tip. However, the initial nail designs used for stabilization of these
proximal injuries were characterized by a large proximal segment,
typically requiring a 17-mm
reamer
at the entry site. In a cadaver model designed to investigate the
impact of this large entry portal in the tip of the greater trochanter,
a significant portion (average of 27%) of the gluteus medius tendon
insertion was found to be disrupted.173 The clinical significance of this is currently unknown.
diaphyseal femur fractures is a relatively contemporary approach. Newer
nail design characteristics including a smaller proximal diameter of
the implant and multiple bends have allowed placement through the
trochanteric tip. The smaller entry portal has the theoretic advantage
of minimizing any additional soft tissue damage at the gluteus medius
tendon. Ricci et al.,228 in a
prospective nonrandomized study, compared the results after treatment
with antegrade nails placed either through the piriformis fossa or the
greater trochanter. In both techniques, alignment was maintained and no
iatrogenic fracture comminution occurred. The average fluoroscopy time
was significantly greater in the piriformis insertion group, and a
longer average operative time was required in these patients. These
differences were amplified in obese patients in whom identification of
the piriformis starting portal is difficult. Patient outcomes were
similar between the two groups. The authors suggested that a
specifically designed trochanteric entry nail represents a viable
alternative for the management of femoral shaft fractures.228
A variety of techniques and implants were subsequently described
including flexible implants introduced through extra-articular distal
femoral portals with and without distal femoral locking capabilities.
These implants were used to treat both distal and proximal femoral
fractures, as well as to prophylactically stabilize proximal femoral
metastases.81,243,314
An extra-articular medial condylar starting portal was suggested by
Swiontkowski et al. for the treatment of ipsilateral femoral neck and
shaft fractures, using antegrade femoral implants.264 Sanders et al.242
expanded the indications to include the multiply injured patient, other
ipsilateral fractures, and pregnancy. Insertion of both femoral nails
and tibial nails was possible using a medial condylar distal femoral
entry site, enabling fracture healing in difficult situations.
intercondylar distal femoral starting portal was introduced in 1991
with the genucephalic nail.119 This
implant was initially used to treat distal femoral fractures and as an
alternative for revision of failed fixations in the distal femur. The
use of this implant expanded to include treatment of intercondylar
fractures and periprosthetic fractures of the distal femur. Because of
the short length of the implant, the initial application to diaphyseal
injuries was limited.119,168,247
Experience and difficulties with the shorter nails, combined with the
success of longer retrograde femoral implants placed through various
starting portals, ultimately led to the development of retrograde
femoral nails specifically designed to span the entire femur.108,121,182,202,217
The major implant design changes that have facilitated the expansion of
indications include a more appropriate anterior bow, multiple distal
interlocking options, anterior to posterior proximal interlocking
options, and variable nail dimensions. These implants can now be used
in certain circumstances to treat femoral diaphyseal fractures.
|
TABLE 50-6 Indications for Retrograde Nails
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
with the use of retrograde nails has produced a number of clinical
circumstances in which the implants may offer an advantage over other
techniques of femoral shaft stabilization.121,242 However, these remain relative indications (Table 50-6, Fig. 50-23).
The major advantage with a retrograde entry portal is the ease in
properly identifying the starting point. In addition, distraction of
the fracture site is decreased with retrograde nailing compared with
the antegrade technique. In situations in which surgical time and
repositioning cannot be tolerated by the patient, retrograde nailing
may be more suitable than the antegrade technique. Ipsilateral injuries
such as femoral neck, pertrochanteric, acetabular, patellar, or tibial
shaft fractures may make retrograde nailing a desirable option. In the
case of an ipsilateral intracapsular femoral neck fracture, proper
fixation of the femoral neck should remain a priority and is best
accomplished with multiple cannulated screws, a sliding hip screw, or
combinations thereof. The femoral shaft fracture can be treated with a
retrograde nail or plate fixation, both of which have been shown to
predictably produce fracture union (Fig. 50-24).
Depending on the surgical technique and the planned operative approach
in a patient with an ipsilateral acetabular fracture, retrograde
nailing remains a consideration. This is most relevant if a planned
extensile or posterior approach to the acetabulum is planned because
the antegrade nail insertion site may be within the subsequent surgical
exposure. This is probably not a large clinical concern for most
surgeons experienced in the treatment of acetabular fractures. If a
retrograde technique is used in this situation, consideration should be
given to over-reaming the femoral canal significantly to allow for
atraumatic retrograde nail placement, avoiding further surgical impact
on the already injured acetabulum. In patients with ipsilateral tibial
shaft
fractures (i.e., a “floating knee”), a single percutaneous incision for
the placement of a retrograde femoral nail and an antegrade tibial nail
has been advocated and accomplished with good results. However, the
length of the incision for the percutaneous placement of an antegrade
femoral nail is limited, and the advantage of avoiding this remains
unknown. The presence of an ipsilateral patellar fracture requiring
surgical fixation certainly allows for easy identification of the
starting point for a retrograde femoral nail. However, similar to the
situation in patients with an ipsilateral tibial fracture, the
morbidity associated with the introduction of an additional surgical
incision at the hip is probably minimal.
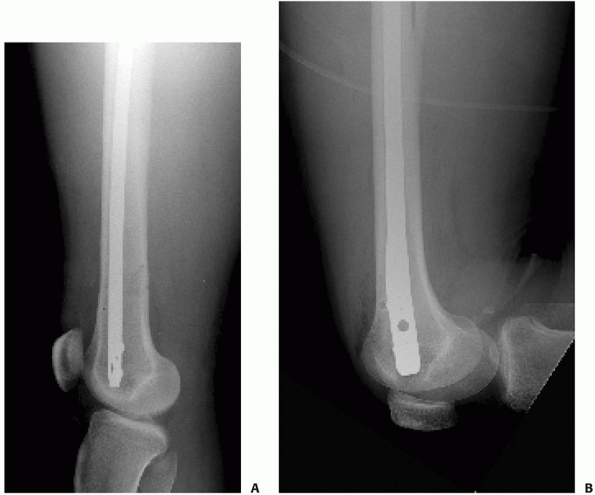 |
|
FIGURE 50-23 An antegrade nail can be placed quite distally (A). This closely approximates the normal location of an appropriately placed retrograde nail (B).
|
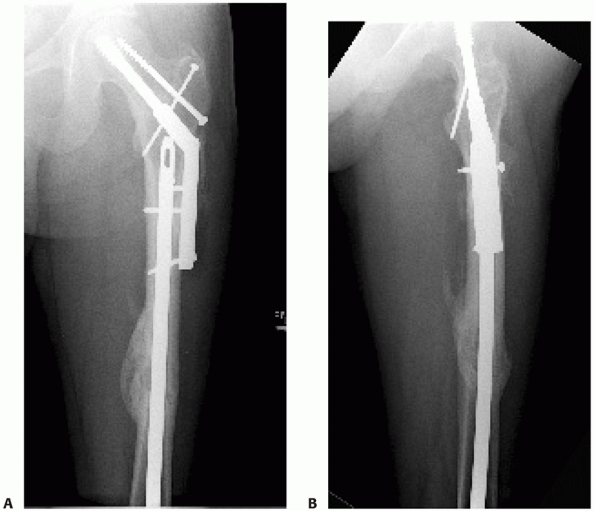 |
|
FIGURE 50-24
A retrograde nail was used to stabilize the femoral shaft fracture in a patient with an ipsilateral intertrochanteric fracture. The nail can be placed proximally to the level of the sliding hip screw barrel (A,B). |
have been suggested. The presence of multiple other fractures and
multiple other organ system injuries suggest that rapid stabilization
of a patient in the supine position may be optimal. Although femoral
nailing certainly can be quickly accomplished with an antegrade
technique, the retrograde entry site may be performed more rapidly in
some circumstances. The rapid placement of a small-diameter unreamed
retrograde nail in the multiply injured patient as an alternative to
temporary external fixation has been described as “Damage Control
Nailing” and can be considered.122
Bilateral femoral fractures can be treated with retrograde nails
without repositioning the patient, potentially decreasing the total
operative time in a critically injured patient. In patients with an
associated vascular injury, rapid treatment with an initially unlocked
retrograde implant can be performed, allowing fracture stabilization to
facilitate the subsequent vascular repair. In the morbidly obese
patient in whom the entry site for antegrade nailing is particularly
difficult, a retrograde nail may be a reasonable alternative and has
been associated with decrease operative time and radiation exposure.282
Similarly in pregnant patients, retrograde nails may be easier to place
and have the advantage of potentially decreased radiation exposure
around the hip. In patients with distal femoral periprosthetic
fractures above a total knee arthroplasty, a retrograde femoral nail
may offer a reasonable fixation option. The design of the femoral
component and the available space for placement of the retrograde
implant are necessary before consideration of retrograde medullary
fixation. The fixation of the medullary implant in the stress-shielded
distal femoral metaphysis may be poor, making consideration of other
strategies necessary. Finally, an ipsilateral through knee amputation
in a patient with an associated femoral shaft fracture is a good
indication for a retrograde nail.
nails exist. Because of the need for knee flexion that allows nail
placement,279 patients with
restricted knee motion may be poor candidates for retrograde femoral
nailing. Similarly, patients with patellar baja may not have adequate
room for placement of a retrograde nail between the patella and
anterior tibial plateau with the knee flexed. Subtrochanteric
fractures, although successfully treated with retrograde nails in some
instances, may be difficult to control unless the nail is placed to an
extremely cephalad location. The presence of an associated open
traumatic wound may make retrograde nailing less desirable because
these injuries are associated with an increased risk of infection with
the potential for subsequent septic arthritis of the knee.
a radiolucent table that allows unimpeded fluoroscopy from the knee to
the hip. A small bump beneath the ipsilateral flank may help avoid
external rotation of the leg. The entire leg and hip are prepped to the
iliac crest and medially to allow access to the femoral artery if
needed. Pharmacologic relaxation is necessary in all cases, especially
if manual traction is the primary reductive force. The C-arm is
positioned perpendicular to the long axis of the table on the
contralateral side to allow for ease with imaging and placement of
interlocking screws. Knee flexion of 34 to 52 degrees279
is necessary to allow identification of the proper entry portal and
placement of the nail. This can easily be accomplished with several
bolsters or a large radiolucent triangle. Femoral length and fracture
reduction can be accomplished manually, with a femoral distractor183 or with percutaneous and unicortical Schanz pins used as joysticks.95
A femoral distractor can be used to maintain length, alignment, and
rotation during the entire procedure. The proximal pin can be placed
from anterior to posterior, medial to the predicted nail path. Distally
the pin is placed from lateral to medial, anterior to the predicted
nail path. Percutaneous Schanz pins for manipulative reduction can be
placed from lateral to medial, unicortically, and close to the
fracture. As with any nailing procedure, the fracture should be reduced
during reaming and nail placement, and until interlocking is complete.
pole of the patella and the tibial tubercle is optimal. A smaller
incision of 2 to 3 cm at the location of the perfect starting portal is
certainly possible and preferred by many surgeons. The approach can be
accomplished medial to or through the central portion of the
infrapatellar tendon. The starting point can be palpated or identified
radiographically. The location for the proper starting point is
anterior to the posterior cruciate ligament origin and at or slightly
medial to the intercondylar sulcus in line with the canal of the femur.
This has been identified as 6.2 to 12 mm anterior to the posterior
cruciate ligament femoral attachment and through the articular
cartilage of the posterior intercondylar sulcus.52,152
Alternatively, the entry site can be identified radiographically on the
basis of the lateral fluoroscopic image. With the femur rotated into a
perfect condylar overlap lateral view, the proper entry site is at the
apex of Blumensaat’s line (Fig. 50-25).
However, the optimal entry side based on the lateral radiographic
projection is dependent on the implant design and may be more anterior
than previously suggested.191 Given
the anatomical valgus of the distal femur the entry angle should not be
perpendicular to the femoral articulation because this can produce a
varus reduction if the fracture is located distal to the femoral
isthmus. Instead, the entry angle should be in 5 to 9 degrees of valgus
as confirmed on the intraoperative AP fluoroscopic image, coincident
with the axis of the femoral canal. The starting point can be initiated
with either a sharp awl or a cannulated drill. Use of a cannulated
drill has the advantage of allowing for minor corrections in the entry
angle before committing with a large opening in the distal femoral
articular surface. Both reamed and unreamed techniques have been
described, and the relative advantages of each are probably similar to
those of antegrade techniques. For placement of a reamed nail, a
ball-tipped guidewire is placed across the fracture and into the
medullary canal of the opposite segment. The guidewire should be
advanced proximal to the lesser trochanter to ensure placement of a
long implant. Reaming is performed with the fracture reduced and the
knee flexed to the proper degree that minimizes damage to the inferior
pole of the patella, the proximal tibia, and the distal femoral
articulation. The canal should be overreamed by at least 1 mm greater
than the desired nail diameter. If a proximal femoral or ipsilateral
acetabular fracture is present, consideration should be given to
over-reaming by 1.5 to 2.0 mm to allow for atraumatic nail passage.
radius of curvature that is greater than that of the normal human
femur. As a result, extension of the fracture may occur despite a
proper entry portal for the implant. A more posterior entry site, in
addition
to potentially damaging the femoral posterior cruciate ligament origin,
can result in accentuation of fracture site extension. In contrast, a
more anterior starting point will produce fracture site flexion and be
located in the patellofemoral articulation. The nail should be recessed
beneath the cartilage surface distally and above the lesser trochanter
proximally (Fig. 50-26).
In a study using a cadaveric femoral model tested with pressure
sensitive film, Morgan et al. demonstrated that placement of the nail 1
mm prominent at the knee joint resulted in significant increases in
patellofemoral joint contact pressures at 90 and 120 degrees of knee
flexion when compared with nails placed flush or recessed.190
Distal interlocking is typically facilitated with a targeting jig that
allows placement of a variable number of screws from lateral to medial.
For some nail designs, endcaps are available that contact the ultimate
distal interlocking screw, preventing toggle of the screw-nail
junction. Locking of the distal interlocking bolts to the nail may be
beneficial for decreasing fracture site motion.268
In addition, bolts are available that can be placed on the medial ends
of the screws as they exit the medial metaphyseal femoral cortex,
potentially increasing the fixation in osteoporotic bone. The knee
joint should be vigorously irrigated after nail placement to remove any
debris that has accumulated from reaming. Proximal interlocking can be
performed from anterior to posterior or from lateral to medial
depending on the design of the nail. Given the need to maintain the
proper femoral rotation throughout the procedure, anterior to posterior
proximal interlocking is usually easier. Because of the potential for
injury to the neurovascular structures located medially, internal
rotation of the nail relative to the femur should be avoided. The major
structures at risk during placement of anterior to posterior
interlocking screws include the femoral artery and branches of the
profundus artery medially, and the sciatic nerve posteriorly. The
relative safe zone for placement of anterior to posterior interlocking
screws has been described at the level of the lesser trochanter. In
this location, the safe corridor was identified from 7 degrees medial
to 20 degrees lateral relative to the sagittal axis. This safe zone
decreased by 52% in patients with an ipsilateral acetabular fracture,
according to examination of CT scans.35
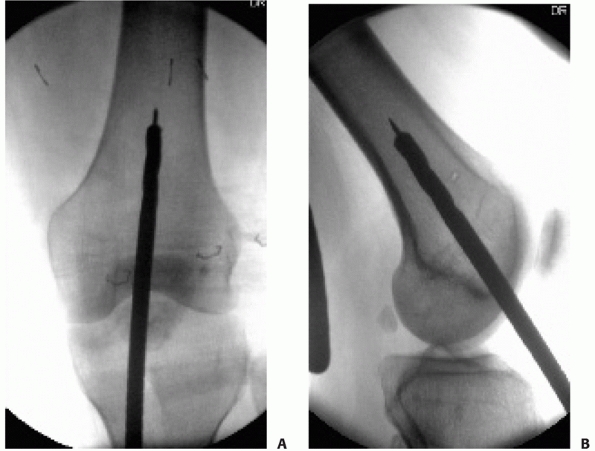 |
|
FIGURE 50-25
The proper starting point for a retrograde nail can be confirmed intraoperatively with image intensification. On the AP view, the starting point should be in line with the femoral shaft, at an angle of 5 to 9 degrees relative to the distal femoral articular surface (A). On the lateral view, the starting point should be at the apex of the Blumensaat line, slightly posterior to the location in (B). |
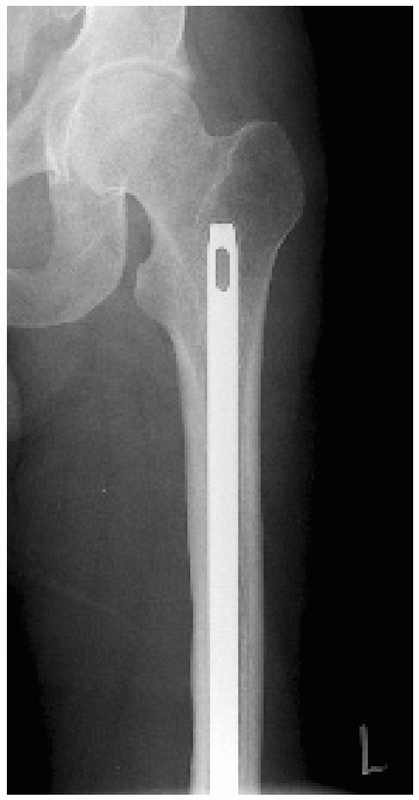 |
|
FIGURE 50-26 A retrograde nail is ideally placed proximal to the level of the lesser trochanter.
|
retrograde nailing. Injury to the local neurovascular structures with
proximal interlocking is possible and has been reported, including
injury to a branch of the profunda femoris artery.66
An incision that allows direct palpation of the anterior femur combined
with avoidance of internal rotation of the nail minimizes this risk.
In
addition, locking performed above the level of the lesser trochanter
further minimizes the risk of injury to the local neurovascular
structures.231
Although injury to the popliteal artery has been reported with
retrograde nailing, this complication appears to be more related to the
injury than to the implant or the retrograde technique.12
Heterotopic ossification in intra-articular and periarticular locations
has been reported after retrograde nailing, and this should remain a
concern in patients with associated risk factors.123 Synovial metallosis has been observed after retrograde medullary nailing, but the impact of this is unknown.136
The negative impact of the retrograde femoral reaming on the blood flow
to the distal femur and the cruciate ligaments has been demonstrated in
an animal model, but the clinical impact is unclear.79
The use of retrograde nails for the treatment of proximal fractures
remains controversial. In a review of 17 subtrochanteric femur
fractures treated with retrograde nails, DiCicco et al.73 reported healing with greater than 5 degrees of varus malalignment in 35% of patients. Similarly, Ricci et al.226
reported more problems with angular malalignment of proximal third
femoral fractures treated with intramedullary nailing when compared
with middle third fractures. The exact distance between the proximal
extension of the fracture and the interlocking screws is unknown, but 5
cm is probably advisable as a minimum length of intact femoral
diaphysis.
early clinical experience with the use of long retrograde nails placed
through an intercondylar starting point for the treatment of femoral
shaft fractures was largely limited to the multiply injured patient and
those patients with severe ipsilateral lower extremity injuries.108,121,182,217 Patterson et al.217
reported on 17 femur fractures in 16 patients treated with retrograde
nails and followed for an average of almost 2 years. Medullary nails
normally designed for antegrade implantation were used in these
patients. The indications for the use of a retrograde nail was an
ipsilateral femoral neck fracture in eight patients, an ipsilateral
through or above knee amputation in five patients, and other associated
injuries including a traumatic arthrotomy and anipsilateral acetabular
fracture. Fourteen of these 17 injuries were open fractures.
Complications were observed commonly and were likely related to the
severity of the initial injuries. The poor results were due to
nonunions, loss of knee motion, and infection; hardware removal was
required commonly. Despite this, the authors believed that knee
function was not adversely affected and that the intercondylar starting
point could be used successfully in difficult injuries.217 Moed and Watson182
described their experience with 22 femoral shaft fractures treated with
unreamed retrograde nails placed through the intercondylar starting
point. Union occurred in less than 4 months in 19 cases, and the major
complications were three nonunions and a rotational malunion.
Restriction of knee motion was not observed. Herscovici and Whiteman121
further described the indications for the use of retrograde nails based
on their experience with 45 fractures. They observed a rotational
abnormality in one patient and two nonunions that both healed after a
revision procedure. Knee motion averaged 129 degrees; however,
decreased flexion and an extensor lag were observed in a minority of
patients. The authors suggested that the relative indications for this
procedure may include ipsilateral proximal femoral fractures,
ipsilateral acetabular fractures, ipsilateral tibial fractures, morbid
obesity, and bilateral femoral shaft fractures. These initial studies,
although promising, suggest that knee-related morbidity does exist with
these implants and that union rates may be lower than in patients
treated with antegrade, statically locked, reamed medullary nailing.
However, the complexity of these injuries and the use of antegrade
nails placed in a retrograde fashion in the most severe injuries likely
have contributed to these observations.
retrograde applications became more readily available, prospective
studies evaluating their use in all femoral fractures as well as in
comparison with antegrade techniques became possible. Early reports
demonstrated an increased number of nonunions and delayed unions
compared with historical reports of antegrade, reamed medullary nailing
techniques.183,202 Moed et al.183
prospectively reported on a consecutive series of patients with femoral
shaft fractures treated with unreamed retrograde nails placed through a
patellar tendon splitting approach. Early nail dynamizations were
performed at 6 to 12 weeks. The authors observed a decrease rate of
nonunion (6%) and time to union (12.6 weeks) when compared with their
earlier study. There were minimal complaints of knee pain, and knee
function was rated as excellent using a clinical rating system. Ostrum
et al.202 similarly reported on a
prospective and consecutive series of 61 fractures treated with a
reamed 10-mm retrograde nail placed through a medial parapatellar
incision. More than half of these fractures had significant (Winquist
type 3 or 4) comminution, and 26% were open injuries. The authors
observed a union rate of 95% when they included one planned bone
grafting for traumatic bone loss and five nail dynamizations. One case
of knee sepsis was observed, leading the authors to recommend caution
in patients with open fractures. Associated knee problems were not
encountered.
directly compared and reported in one retrospective study, one
prospective, and two prospective and randomized studies.201,226,277,282
In a retrospective study comparing 134 femoral fractures treated with a
retrograde technique and 147 fractures treated with an antegrade
technique, Ricci et al.226 compared
the rates of delayed union, nonunion, malunion, and complications at an
average of 23 months. Union occurred after the initial procedure in 89%
of the fractures treated with antegrade nails and 88% of those treated
with retrograde nails. The final rate of union after additional
interventions and the rate of malunions were the same between the two
groups. After excluding patients with ipsilateral hip or knee injuries,
the authors reported a significantly higher rate of pain at the
associated entry site for each group. In patients treated with
retrograde nails, 36% had knee pain compared with 9% of those treated
with antegrade nails. Ipsilateral hip pain was reported in 10% of
patients treated with antegrade nails compared with 4% of patients
treated with retrograde nails. This led the authors to conclude that
although union rates between the two treatment approaches are
comparable, complications related to the knee and hip are related to
the nail insertional site. Ostrum et al.201
compared femoral fractures treated with antegrade and retrograde nails
in a prospective and randomized study of 100 patients. Small-diameter
(10-mm) nails were inserted after reaming in both groups. The authors
reported fewer nail dynamizations and more rapid healing with the
antegrade technique by almost
4
weeks. Knee pain was found to be equal in both groups, but thigh pain
was observed to be associated with antegrade nails. Final healing after
secondary procedures was similar between the two groups. In another
prospective and randomized study comparing antegrade and retrograde
femoral nailing for femoral shaft fractures, Tornetta and Tiburzi277
found no difference in operating time, blood loss, technical
complications, nail size, or the need for blood transfusions in 69
fractures. Reamed nails were used with both insertional techniques. The
authors reported an increased rate of rotational and length
discrepancies with the retrograde technique. In their study, the
antegrade procedures were performed using a fracture table, whereas the
retrograde procedures were accomplished with manual traction on a
radiolucent table. The time to union and the rate of union (100%) were
the same for both surgical approaches. Because of the limited length of
follow-up, no conclusions could be drawn regarding long-term knee
function or complications. In a more recent follow-up presentation,
Tornetta and coauthors reported similar results in knee range of
motion, stair-climbing ability, pain medication requirements, and Short
Form-36 outcomes in patients prospectively randomized to treatment with
either an antegrade or retrograde nail.280 In a prospective and nonrandomized multicenter study, Tucker and coauthors282
demonstrated similar outcomes in patients treated with an antegrade or
a retrograde technique. The emphasis of their study was primarily on
the difference in patients who were obese (defined as body mass index
greater than or equal to 30 kg/m2).
In obese patients, the retrograde technique was associated with
significantly decreased operative and radiation exposure times,
supporting the use of this technique in some obese patients.282
allows early patient mobilization, decreases pain, facilitates nursing
care, minimizes joint stiffness, and allows early functional
rehabilitation. Early mobilization avoids many of the complications
associated with prolonged recumbency such as pulmonary compromise,
pressure sores, and muscle deconditioning.
pain after femoral stabilization. As a result, they should be
encouraged to sit up and get out of bed immediately after fixation.
Because of the strength of a femur treated with a statically locked
intramedullary nail, there should be virtually no concern by the
patient or the physician regarding the stability of the mechanical
construct. This applies to femurs stabilized with both antegrade and
retrograde nailing techniques. Quadriceps and hamstrings exercises can
proceed according to the patient’s comfort. Unrestricted active and
passive range-of-motion exercises of the knee and hip can similarly be
instituted immediately after surgery. Restoration of motor strength is
dependent on the traumatic injury to the muscles, any associated
injuries, and the patient’s motivation. In patients with isolated
femoral shaft fractures, supervised outpatient physical therapy is
frequently unnecessary.
factors including the patient’s associated injuries, the soft tissue
injury, and the location of the fracture. For fractures treated with
the currently manufactured intramedullary nails, immediate weight
bearing is safe from a mechanical standpoint. Brumback et al.41
reported the biomechanical and clinical results of simulated and actual
early weight bearing using commonly available implants. They found that
immediate weight bearing of segmentally comminuted midisthmal fractures
treated with a statically locked intramedullary nail using two distal
interlocking screws was safe and allowed healing without shortening or
nail fatigue failure. Similarly, Arazi et al.7
followed 24 patients with comminuted diaphyseal femur fractures for a
minimum of 1 year. Unrestricted weight bearing was allowed, and most
patients were able to bear weight between 2 and 4 weeks after surgery.
No nail-related mechanical failures occurred, and all fractures healed
without complications. An interlocking screw in each of two patients
demonstrated some bending, but this was without consequence. The
experience reported in these two studies supports the contention that
early weight bearing after reamed statically locked antegrade
intramedullary nailing is safe. Early weight bearing may encourage
callus formation and should be encouraged in applicable patterns.
Fractures with proximal or distal extension and associated ipsilateral
femoral fractures require individual modification to the weight-bearing
progression. If weight bearing is limited during the first 6 to 12
weeks, an ankle dorsiflexion splint or orthosis should be used to avoid
an equinus contracture.
weeks, 12 weeks, and 6 months and should include two views of the
entire femur to include the proximal and distal interlocking screws as
well as the hip and knee joints. Groin pain in a patient who has
sustained a femoral shaft fracture should be evaluated at any point in
the postoperative course given the possibility of an associated
clandestine or iatrogenic femoral neck fracture. However, clandestine
femoral neck fracture has been observed in asymptomatic patients as
well.230 A femoral neck fracture was
ultimately identified in 10 patients without radiographic evidence
before plating of an ipsilateral diaphyseal femoral fracture. This
review emphasizes the need for dedicated hip radiographs
postoperatively and at any time a patient becomes symptomatic.230
injured patient, especially those patients with associated chest
trauma, remains a topic of some contention. Early retrospective studies
suggested that immediate internal fixation of long bone fractures was
beneficial in patients with multiple injuries, and this included the
use of reamed intramedullary nails.103,137,233,234,265
Although the risk of fat embolism was recognized, most series suggested
that early femoral stabilization actually decreased the incidence of
severe fat embolism and pulmonary complications. Talucci et al.
reported five cases of fat embolism syndrome in patients treated with
delayed intramedullary nailing and no cases in patients treated with
immediate nailing.265 Johnson et al.137
retrospectively evaluated 132 patients with multiple musculoskeletal
injuries with an ISS of 18 or higher. They found that early operative
stabilization of the majority of fractures was associated with a
decreased incidence of ARDS. Because of the retrospective nature of the
study, however, firm conclusions could not be determined. In a landmark
article, Bone et al.25 addressed the impact of early stabilization of long bone fractures
on pulmonary complications, hospital stay, and the number of days in the intensive care unit.
treated with either early (<24 hours) or delayed femoral
stabilization. The patients were divided on the basis of the number of
associated injuries as either isolated or multiply injured. The
incidence of pulmonary complications including ARDS, fat embolism, and
pneumonia was lower in both groups of patients treated with immediate
femoral stabilization.
appears to be clearly important in the multiply injured patient, the
impact of femoral nailing and especially reaming is less clear. This
has been especially contentious in the patient with a concomitant
pulmonary injury. Several investigators have therefore looked
specifically at the effects of reaming and intramedullary nailing on
pulmonary function in animal models.77,211,302,306,307 In a hemorrhagic shock and lung contusion model, Pape et al.211
found increased pulmonary artery pressure and increased lung capillary
permeability in animals treated with reamed nails compared with
unreamed nails. In contrast, Wolinsky et al.302
found that femoral reaming did not affect pulmonary shunt or pulmonary
compliance in an ARDS sheep model if appropriately resuscitated.
Similarly, Duwelius et al.77 found that pulmonary dysfunction did not increase in a pulmonary contusion model.
investigations, several clinical studies sought to address the issue of
reaming and intramedullary nailing on pulmonary function and mortality
in patients with an associated thoracic injury.27,29,51,53,209,285 Pape et al.209
investigated whether early intramedullary stabilization of femoral
shaft fractures in multiply injured patients may be detrimental in the
subpopulation of patients with an associated thoracic injury. In a
retrospective review of 766 patients, 106 met the inclusion criteria
and all were multiply injured (ISS >18). The authors reported an
increased incidence of ARDS and mortality in the patients who had
associated severe chest trauma and were treated with immediate nailing.
However, this is in contradistinction to the study by Charash et al.,
who arrived at a different conclusion.53
That is, pulmonary complications were decreased in all patients who
underwent early femoral stabilization with reamed nailing, including
those with thoracic trauma.
reamed femoral nailing on the multiply injured patient and the patient
with thoracic trauma, Bosse et al.27
designed a study looking at patients treated at two different centers.
Although the patient populations and the protocols for trauma care were
similar at the two centers, reamed intramedullary nailing was used in
95% of patients at one institution, whereas plating was used in 92% of
patients at the other institution. This allowed for comparison of the
effects of reamed nailing and not necessarily the impact of a femoral
fracture on outcomes. The overall incidence of ARDS was only 2% in
patients with a femoral fracture compared with 6% to 8% in patients
without a femur fracture but with a thoracic injury. The occurrence of
ARDS, pneumonia, pulmonary embolism, multiple organ system failure, and
death were similar regardless of the type of treatment or the presence
of a thoracic injury. This led to the conclusion that nailing with
reaming for the acute stabilization of femoral fractures in the
multiply injured patient with a thoracic injury did not increase the
occurrence of the aforementioned complications.
the impact of intramedullary instrumentation on the pulmonary
complications and mortality in the multiply injured patient.*
In a prospective and randomized evaluation of patients treated with
early intramedullary nailing for their femoral fractures, no difference
was found in the incidence of ARDS in patients treated with reamed or
unreamed nails. The authors observed a low overall incidence of ARDS
and could not detect a difference given the small sample size of
multiply injured patients.48
However, there continues to be a significant body of evidence that
suggests that in a specific subpopulation of patients, early
intramedullary nailing may be deleterious and is associated with
elevation of certain proinflammatory markers, especially interleukin
(IL)-6.† Both the femoral fracture and the process of
reaming has been shown to increase IL-6 levels, which may indicate an
increase in the inflammatory response and the presence of an additional
insult due to the surgical treatment.192
This IL-6 increase has been shown to be closely correlated with injury
severity and the development of a systemic inflammatory response state.98,216
This has led to the recommendation that early external fixation of long
bone fractures followed by delayed intramedullary nailing may minimize
the additional surgical impact in patients at high risk for developing
complications (see Chapter 9).
high-energy trauma. These patients frequently have multiple other
orthopaedic injuries and involvement of several organ systems. Vascular
injuries are commonly observed in association with open femoral shaft
fractures.
femoral shaft, an associated open traumatic wound suggests significant
initial displacement and associated soft tissue disruption. Unlike the
tibia, which is entirely subcutaneous over its anteromedial face, the
femur is completely covered in muscle except at the palpable proximal
and distal aspects. For that reason, a small skin disruption is usually
indicative of a much larger soft tissue injury. As a result, the usual
classification system of Gustilo and Anderson for open fractures cannot
necessarily be accurately applied.111 Although previous articles have used this system for open femoral shaft fractures,‡ no studies exist that compare its reliability and reproducibility.
similar to that of other open long bone fractures and includes
antibiotics, debridement, and stabilization. Repeated examinations of
the open wound outside of the operating room should be avoided.
Antibiotics and tetanus prophylaxis should be administered immediately.
Early operative débridement, preferably within 6 to 8 hours, should be
performed depending on the patient’s other associated injuries. In the
operating room, any planned incisions for surgical stabilization of the
femur should be drawn on the skin to allow for intelligent surgical
extensions of the open wound for definitive debridement. If
appropriate, the traumatic wounds should be extended to allow a
complete examination of the bone ends and medullary canal. A separate
surgical incision for the purposes of debridement can be used if the
traumatic wound is located in a poorly extensile location.
All
devitalized cortical fragments should be removed with the intention of
not routinely reimplanting these segments. The bone ends should be
débrided and cleaned of any foreign material while avoiding further
soft tissue devitalization. Multiple liters of saline should be used to
clean the contaminated fragments. A thorough débridement should be
performed to decrease the overall risk of early and late infection. In
circumstances in which gross contamination has occurred and the initial
débridement is questionable, a second débridement at 48 hours should be
planned.
and was performed in a timely fashion, definitive stabilization of the
femoral shaft can proceed, usually with reamed intramedullary nailing.
Historically, traction and external fixation have been used to
definitively treat open femoral shaft fractures. However, these methods
have numerous disadvantages that have precluded their routine use.
Specifically, traction requires a period of immobilization and supine
positioning that is undesirable in the polytraumatized patient. The
delay in stabilization of the femoral shaft has been shown to be
associated with increased mortality, and every effort should be made to
stabilize the limb within 24 hours.25
In addition, length and alignment are poorly controlled and fracture
instability contributes to early patient discomfort. Nursing care is
difficult, because patients must remain in a relatively fixed position.
Management of other associated injuries is further jeopardized by the
need for constant traction on the extremity. External fixation is a
reasonable temporizing measure in specific circumstances but is
associated with multiple difficulties as a definitive treatment method.
In patients with multiple injuries that preclude early operative
stabilization of their open femur fractures and in patients with severe
soft tissue injuries that require a second débridement, temporary
external fixation is a reasonable and rapid initial management approach
that allows delayed conversion to a medullary implant at 5 to 10 days.
External fixation as a definitive treatment is associated with pin
tract infections, shortening, and loss of knee motion.
including type III open wounds, has been found to have an acceptable
complication rate in several studies and remains the treatment of
choice in most instances.37,164,200,239,295 Lhowe and Hansen164
reported on 42 patients after immediate reamed intramedullary nailing
of open femoral diaphyseal fractures who were followed for a minimum of
12 months. Union occurred in all patients, and infection, angular
malunion, and limb length inequality were observed infrequently.
Brumback et al.37 retrospectively
identified 89 open femoral fractures, the majority of which were type
III open fractures. Immediate reamed nailing was performed in 56
patients, whereas 33 patients underwent delayed stabilization at 5 to 7
days. Fractures that had a delay in the initial debridement of more
than 8 hours were typically treated with staged nailing. All fractures
healed and no infections were observed in type I, II, and IIIA open
fractures. In the type IIIB injuries, infections were observed in 11%
and occurred in injuries treated immediately and those treated delayed.
Whether early nailing resulted in a higher infection rate was further
investigated by Williams et al., who prospectively assigned 42 patients
with open femoral fractures to immediate versus delayed intramedullary
nailing. They observed a low rate of infection and nonunion, and found
no relationship with timing or the associated soft tissue injury.295
The initial treatment of open femoral shaft fractures with immediate,
reamed intramedullary nailing has been confirmed by multiple other
studies.200,239
low-velocity missiles are observed relatively commonly in most urban
trauma centers. They are typically the result of handgun injuries, and
four classic types of fractures have been described in the femur. These
include the “drill-hole,” incomplete, butterfly, and spiral fractures.
The former is result of a metaphyseal injury in which the bullet passes
through the bone, producing minimal comminution and maintaining the
integrity of the remaining femur. Incomplete fractures occur when the
bullet grazes the cortex of the femur with a subcritical force.
Fracture comminution occurs when the missile impacts the diaphyseal
bone, resulting in the commonly observed butterfly fragmentations.
Spiral fractures typically occur in a slightly remote location relative
to the path of the bullet and likely represent an associated torsional
force caused by weight bearing at the time of impact.255
This has led to significant cost savings and early patient mobilization
compared with the traditional approach of traction, antibiotics, and
delayed intramedullary fixation.163,299,308
For fractures caused by low and midvelocity gunshots, treatment with
immediate nailing without a formal debridement of the comminuted
diaphyseal fragments and bullet particles has resulted in predictable
union with acceptable complications20 (Fig. 50-28). Nowotarski and Brumback198
retrospectively reviewed 39 femoral fractures caused by handgun
missiles, which were treated with early (<24 hours) intramedullary
nailing at an average follow-up of more than 1 year. Complications
included one delayed union, one nonunion, and one infection, all of
which healed with a single additional operative procedure. Similarly,
Tornetta and Tiburzi276 reported on
the results of antegrade intramedullary nailing of distal femur
fractures caused by gunshots. Despite close proximity to the distal
interlocking screws in all cases, fractures healed predictably and no
secondary bone grafting procedures were required. Because of the good
results in these and other studies combined with the cost savings by
decreasing the length of hospitalization, immediate intramedullary
nailing of gunshot femoral fractures is recommended.20,163,198,276,299,308
and shotgun blasts are an entirely different injury than those caused
by handguns. Shotgun injuries are characterized by significant
contamination, devitalization, and soft tissue injury. Occasionally if
the injury occurred at close range, the wadding may be present within
the wound and represents a foreign body. These injuries frequently
require multiple débridements to decrease the rate of infection.
Similarly, high-velocity missile injuries caused by hunting and assault
rifles produce massive tissue injuries that require an aggressive and
radical débridement of all devitalized fragments, and serial
debridements are frequently necessary.
shaft fracture and an ipsilateral vascular injury requires
communication and coordination between the vascular surgeon and the
orthopaedic surgeon. The goal of treatment should be skeletal
stabilization
combined with expeditious lower-extremity revascularization. In many
cases, management should include fasciotomies of the leg to avoid
time-dependent reperfusion compartmental syndrome. Prophylactic
compartment releases distal to the site of vascular injury should be
considered if there is greater than 3 hours of ischemia. Vascular flow
to the extremity should be reestablished within 6 hours if possible to
maximize limb salvage rates. Therefore, the orthopaedic management is
largely based on the time from injury to surgery. If stabilization can
proceed expeditiously and allows enough time for vascular repair,
definitive treatment with a nail or a plate can be performed primarily.
If the time from injury to presentation is unknown or lengthy, then
limb perfusion should be reestablished first. This can be accomplished
with either temporary shunting or definitive vascular repair. A
temporary shunt provides restoration of blood flow, which can then be
followed with definitive skeletal stabilization. This allows a stable
skeleton to simplify the definitive vascular repair. In addition, if a
definitive vascular repair precedes orthopaedic stabilization, there is
always the risk of injuring the vascular repair as the limb length is
reestablished. If vascular repair with a saphenous interposition graft
is performed before skeletal stabilization, some redundancy of length
is recommended to prevent disruption during re-establishment of femoral
length.
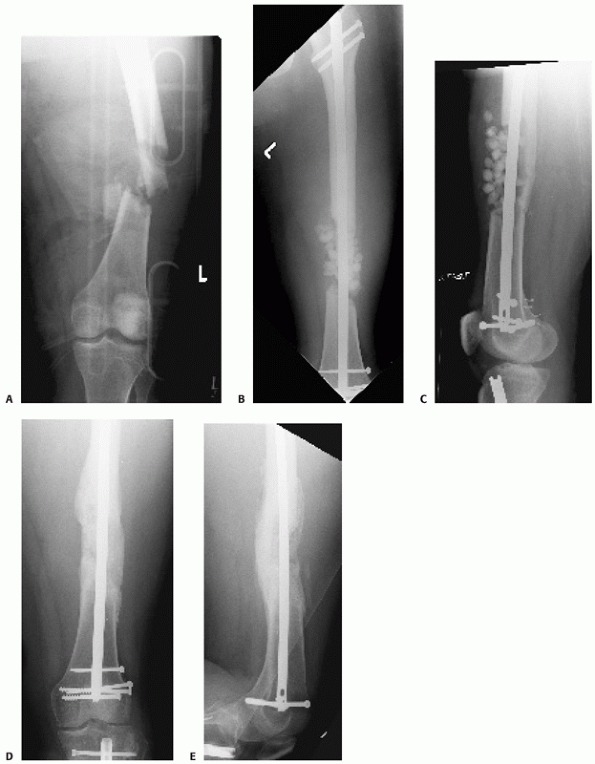 |
|
FIGURE 50-27 This patient sustained a contaminated open femur fracture with bone loss after a motorcycle crash (A). An antegrade nail was used to stabilize the femur, and antibiotic beads were used to fill the dead space (B,C). Iliac crest bone grafting was performed at 6 weeks. Healing proceeded uneventfully (D,E).
|
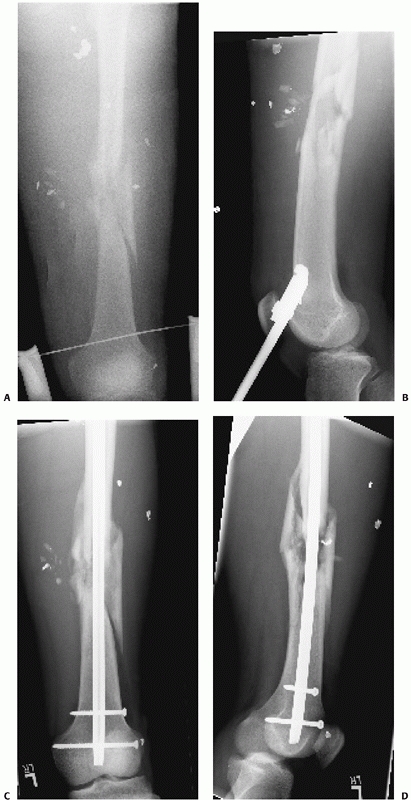 |
|
FIGURE 50-28 This patient sustained a gunshot wound to the leg with an associated femoral shaft fracture (A,B). An antegrade, statically locked, reamed nail allowed early weight bearing and healing (C,D).
|
This can be useful in cases in which definitive stabilization with a
plate or nail cannot be performed because of time constraints or other
injuries of the patient. Early exchange to an intramedullary nail can
then be performed as the patient’s overall clinical condition allows.127
In most instances, definitive internal femoral stabilization can be
performed during the same surgical procedure as the vascular repair.
The choice of a plate or a nail depends on the surgical exposure, the
fracture location, and the associated injuries. In open femoral
fractures with an associated vascular injury, the surgical approach for
medial plating is usually accomplished by a combination of the
traumatic injury and vascular approach. A plate can usually be applied
quickly. Because of the potentially increased risk of nonunion and
infection in these patients, the surgeon must consider the possibility
that a repeat procedure in this location may be necessary.
Intramedullary nailing can be performed with the same indications and
concerns as any closed or open femoral fractures as applicable.
retrospectively evaluated 19 patients with femoral fractures requiring
stabilization and an associated vascular injury that required repair.
Internal fixation preceded vascular repair in 10 patients, whereas in
nine patients femoral stabilization followed vascular repair. Their
favorable results led them to conclude that internal fixation could
safely precede vascular repair, and vascular shunts should be used in
cases of prolonged ischemic time. Despite skeletal stabilization and
limb revascularization, open femur fractures with associated vascular
injuries have significant complications. The long-term results of 13
blunt femoral fractures with associated arterial injuries were reviewed
by DiChristina et al.72 In two
patients, double level arterial injuries were identified. In the eight
open fractures, two patients had above knee amputation, three patients
had persistent drainage, and no patients regained more than 90 degrees
of knee motion. In contrast, in five patients with closed fractures,
all regained full function and full knee motion. The authors again
stressed that femoral stabilization can be performed before arterial
repair if sufficient time is available for the vascular procedure. As
with most injuries, the outcomes were dependent on the associated soft
tissue injury, specifically the presence of an open fracture.72
patients with associated craniocerebral trauma remains controversial.
Patients with significant head trauma are at risk for secondary brain
injury as a result of surgical management of any injury including their
femoral shaft fracture. Transient hypotension is frequently implicated
as a potential cause of further cerebral insult. This may be because of
the inability of these patients with a head injury to adequately
autoregulate their cerebral perfusion pressure. However, these patients
are frequently multiply injured and at risk for pulmonary complications
related to a delay in fixation of their femoral shaft fracture. As a
result, the management of patients with complicated injuries requires
coordination between the relevant surgical services including the
general, neurologic, and orthopaedic surgeons.
stabilization in patients with an associated head injury are difficult
to interpret. The retrospective nature of all of these studies
introduces significant selection biases and limits definitive
conclusions.6,133,175,257,281
However, some useful information can be obtained from these studies.
Sixty-one patients with severe or moderate closed head injuries
(Glasgow Coma Scale score <9) with femur fractures were
retrospectively reviewed by Townsend et al.281
They found that patients treated for their femur fractures within 2
hours were eight times more likely to experience a hypotensive event
than those patients treated after 24 hours. The majority (74%) of
patients with intracranial monitoring experienced cerebral perfusion of
less than 70 mm Hg. Similarly, Jaicks et al.133
found a trend toward increasing intraoperative hypotension and hypoxia
in patients treated with early femoral stabilization. Although the
neurologic complication rate was similar between patients undergoing
early versus delayed femoral stabilization, the average discharge
Glasgow Coma Scale score was significantly lower in the early fixation
group. In a study of 17 patients with an average ISS of 35, Anglen et
al.6 monitored intracranial pressure
during reamed intramedullary nailing. The average cerebral perfusion
pressure decreased by 17 mm Hg, and 70% of patients had an average
intraoperative cerebral perfusion pressure of less than 75 mm Hg.
However, the impact of transient hypotension on neurologic outcome is
not known.
were unable to identify a statistically significant predictor or
central nervous system complications in 32 patients with combined head
injuries and femoral fractures. They did find that a delay in femur
stabilization was a strong predictor of pulmonary complications,
concluding that a delay made pulmonary complications 45 times more
likely. McKee et al.175 used a
retrospective, case control study to determine the effect of a femoral
shaft fracture treated with intramedullary nailing on the neurologic
disability and mortality in patients with associated head injuries.
They identified 46 patients with closed head injuries with femur
fractures and matched these with 99 patients with a similar ISS and
Glasgow Coma Scale score yet no femur fracture. The authors found no
significant difference in early mortality, length of hospital stay,
level of neurologic disability, or the results of cognitive testing.
However, the small number of patients may limit the conclusions of this
study. In a detailed cohort study evaluating the effect of timing of
nonneurological operative interventions, Wang et al.288
compared early (≤24 hours) and late (>24 hours) surgical treatment
on functional outcomes, morbidity, and mortality. At 6 months following
injury, patients treated early had significantly improved
neuropsychological scores. Additionally, a higher incidence of
pneumonia and a longer hospital stay was associated with a delay in
surgical treatment. This led the authors to conclude that in patients
with combined multisystem trauma and non-operative traumatic brain
injury, early treatment of orthopaedic injuries under general
anesthesia was not associated with worse neuropsychological or
functional outcomes.288
femoral neck and shaft fractures have been a source of controversy
since the first descriptions of the injury pattern. Concomitant femoral
neck fractures occur in 3% to 10% of patients with femoral shaft
fractures.2,290,303,313 Many of the associated femoral neck
fractures are nondisplaced, and missed injuries have been reported in 30% to 57% of cases (Table 50-7).
|
TABLE 50-7 Percentage of Missed, Delayed, or Occult Femoral Neck Fractures in Patients with Combined Injuries
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
identified the commonly observed fracture patterns and results of
treatment. The median age of the patients in the review was 34 years,
and men were injured in 78% of cases. The hip fracture diagnosis was
delayed in 30% of cases. Hip fracture treatment was uniformly
successful with 99% healing and only 5.1% complicated by aseptic
necrosis. Locked intramedullary nailing for treatment of the femoral
shaft yielded the most predictable result when compared with unlocked
nailing and plate fixations. There were no reported cases of infection
or nonunion with locked nailing of the femoral shaft in this systematic
review.
femoral fracture patterns appear to be associated with ipsilateral
femoral shaft fractures. In his systematic review, Alho reported the
locations of the associated hip fracture as subcapital in 2%,
midcervical in 21%, basicervical in 39%, pertrochanteric in 14%, and
intertrochanteric in 24%.2 In a
review of 52 patients with ipsilateral proximal femoral and shaft
fractures, the fracture line inferior exit point was observed to be at
the inferomedial femoral neck and proximal to the lesser trochanter.
Only three fracture configurations were seen. The most common pattern
was a basicervical neck fracture (AO 31-B2.1) in 55% followed by a
vertical midcervical intracapsular shear pattern (AO 31-B2.3) in 35%
and an intertrochanteric fracture through the greater trochanter (AO
31-A1.2) in 10%. This indicates that the majority of these proximal
femoral fractures are extracapsular in location. All of the observed
intracapsular femoral neck fractures were vertically oriented, making
fixation particularly difficult in displaced patterns. Of the fractures
that were initially missed, none were intertochanteric in location.252
nonunion and aseptic necrosis are lower in patients with combined
femoral neck and shaft fractures than in young patients with
high-energy femoral neck fractures in isolation.1,2,19
This may be because of the commonly observed extracapsular location of
the neck fracture, the tendency for these fractures to be minimally or
nondisplaced, or a combination of the two. The delay in diagnosis of
the femoral neck fracture and treatment of the femoral neck after
stabilization of the femoral shaft fracture (i.e., in cases of
iatrogenic or occult femoral neck fractures) have not necessarily
produced complications.2,19
intertrochanteric fracture is the result of several concurrent factors.
Because of the presence of an ipsilateral fracture of the femoral
shaft, AP imaging of the injured extremity before stabilization of the
femoral shaft fracture is typically hampered by external rotation of
the proximal femoral segment.69
Because these patients are frequently in severe discomfort as a result
of their shaft fracture, suboptimal imaging of the hip may
unfortunately be accepted. Even with careful positioning of the lower
extremity for quality images of the hip as a part of the routine
radiographic evaluation of a femoral shaft fracture, proximal segment
control is inadequate because of the shaft fracture. It has been noted
serendipitously that in patients with known or suspected ipsilateral
acetabular fractures, the obturator oblique radiograph frequently
demonstrates the femoral neck along its longest axis, assisting with
the radiologic evaluation.
fractures in patients with femoral shaft fractures, review of all
available imaging studies at multiple time points in the patient’s
evaluation and treatment is recommended (Table 50-7).
First, dedicated hip radiographs should be obtained as a part of the
initial radiologic evaluation of any patient with a femoral neck
fracture. Second, if pelvic oblique radiographs are obtained because of
a suspected or known ipsilateral acetabular fracture, these should be
scrutinized for the presence of a femoral neck fracture. Third, if a CT
scan is obtained for evaluation of abdominal or pelvic trauma, this
should be reviewed because occult fractures are frequently demonstrated
on the relevant axial images (Fig. 50-29).
Fourth, intraoperative fluoroscopic images before initiating antegrade
nailing of a femoral shaft fracture should be obtained. Fifth, hip
fluoroscopic images and/or radiographs should be obtained after femoral
shaft stabilization with the hip in 10 to 15 degrees of internal
rotation. Finally, dedicated postoperative hip radiographs should be
obtained before leaving the operating room to confirm the integrity of
the femoral neck. By using a best-practice protocol consisting of a
dedicated internal rotation plain radiograph of the hip, a 2-mm CT scan
through the femoral neck, a fluoroscopic lateral of the femoral neck
before fixation, and postoperative orthogonal hip radiographs in the
operative room, Tornetta et al. demonstrated a substantial improvement
in the rate of missed femoral neck
fractures
in patients with femoral shaft fractures. The delay in femoral neck
fracture diagnosis was reduced by 91% by using these consistent
radiographic evaluations.273
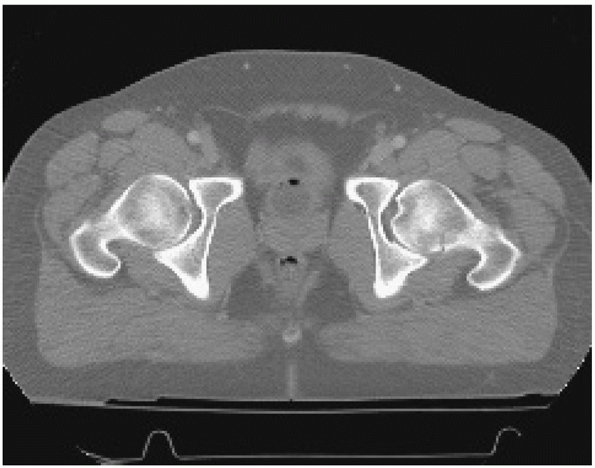 |
|
FIGURE 50-29
Computed tomography (CT) scan of the pelvis and abdomen was obtained in this patient with multiple injuries, including a femoral shaft fracture. The femoral neck fracture was demonstrated on the axial images, despite normal radiographs of the pelvis and hip. |
reviewed the impact of abdominal CT scan evaluations on the ability to
demonstrate nondisplaced fractures of the femoral neck. In a series of
152 femoral shaft nailings, 14 femoral neck fractures were ultimately
identified. Of these, eight were not visible on the initial screening
pelvic radiographs. On retrospective review of the abdominal CT scans,
six of these eight femoral neck fractures were shown to be present but
nondisplaced. The remaining two femoral neck fractures were not visible
on preoperative CT scans and were thus believed to be iatrogenic
according to the authors.
may be accentuated if the fracture is truly nondisplaced. However,
there is always the possibility that the fracture is iatrogenically
produced during the manipulation, reduction, and placement of an
antegrade intramedullary nail. It has been suggested that iatrogenic
fractures do occur as evidenced by normal preoperative CT scans in
patients later found to have a nondisplaced fracture of the femoral
neck after intramedullary nailing.313 This was investigated by Simonian et al.,253
who compared the proximal femoral anatomy and nail insertion depths in
four patients with iatrogenic femoral neck fractures with 311 patients
without this complication. They found a higher neck shaft angle of 139
degrees in the patients with femoral neck fractures than in those
without (125 degrees). Further, in the four patients with femoral neck
fractures, the nails were inserted below the tip of the greater
trochanter. This was not observed in patients with similarly elevated
neck shaft angles but without femoral neck fractures. This led the
authors to recommend avoiding deep insertion of the femoral nail beyond
the tip of the greater trochanter in patients with a valgus femoral
neck. Although these findings may be specific to the nail insertional
jig used, an awareness of this potential complication is necessary.
However, the majority of femoral neck fractures that are diagnosed
after femoral nailing are likely missed injuries. This is emphasized in
a report of “clandestine” femoral neck fractures in a group of patients
treated with plate fixations for their femoral shaft fractures. Riemer
et al. reported delayed identification of a femoral neck fracture in
31% of patients treated with plating of their femoral shaft fracture, a
procedure unlikely to produce significant associated proximal femoral
injury.230
to be controversial. Experience has led many authors to suggest that
these two noncontiguous fractures should each be treated with an
implant that optimizes fracture healing while simultaneously
prioritizing the femoral neck fracture fixation (Fig. 50-30).
This is in large part because of the increased difficulty observed with
managing complications associated with inadequate or suboptimal femoral
neck fixation such as aseptic necrosis, nonunion, malunion, and failure
of fixation. The major complications associated with failure of the
available methods for treating the femoral shaft component of this
injury combination are generally familiar and more straightforward.
This has led to the recommendation that the femoral neck or
intertrochanteric fracture should be treated with multiple lag screws
or a sliding hip screw, with or without capsulotomy, as appropriate.
The femoral shaft component can be treated with whichever method is
most familiar and reliable, typically a retrograde femoral nail or
lateral plate fixation.263,264,290
Femoral plating combined with multiple screws or a sliding hip screw
for the femoral neck fracture has yielded good results in several
series.55,94
emphasis. The type of fixation for the femoral neck fracture should not
differ from isolated injuries in this location. Typically, multiple lag
screws are used to stabilize subcapital and transcervical fractures,
whereas a sliding hip screw is used for basicervical and
intertrochanteric fractures. The order of fixation is influenced by the
two treatment methods chosen combined with the urgency of early
reduction and stabilization of an intracapsular femoral neck fracture.
If the proximal femoral fracture is intracapsular in location and
displaced, consideration should be given to completing this portion of
the procedure first if the patient’s overall medical condition allows.
This is largely to allow for urgent preservation of the femoral head
blood supply. In cases in which a retrograde nail is desired for
stabilization of the femoral shaft fracture, the canal should be
overreamed to allow for atraumatic passage of the nail to avoid any
additional stress on the femoral neck. If a basicervical femoral neck
fracture is stabilized with a sliding hip screw, unicortical screws can
be initially placed in the side plate and exchanged for longer screws
that avoid the retrograde nail. This will allow for placement of a
retrograde nail as proximally as possible.
neck fracture is identified after antegrade femoral nailing, strategic
lag screw fixations anterior to the nail can be successfully performed.
An additional hip joint capsulotomy can be performed to relieve any
intracapsular tamponade if the fracture location warrants. In cases in
which a displaced femoral neck fracture is identified after placement
of an antegrade nail, the ultimate treatment depends largely on the
fracture location. If the fracture communicates with the nail entry
site, it is unlikely that an anatomical reduction of the femoral neck
can be obtained with the nail still in position. Nail removal,
anatomical fixation of the femoral neck, and alternative fixation of
the femoral shaft should be performed.
cephalomedullary (reconstruction) nail has been used to treat combined
femoral neck and shaft fractures. This has been associated with good
results in several small series and has been recommended as an option.
However, in a retrospective review of ipsilateral neck and shaft
fractures treated with multiple different methods, Watson and Moed290
found that 75% of the femoral neck nonunions that occurred at their
institution developed after the use of a reconstruction nail. Jain et
al.134 reported on 23 cases of
ipsilateral hip and shaft fractures treated with a single implant over
a 4-year period. Complications of the femoral neck fixation included
one nonunion, one varus malunion, and one aseptic necrosis, for an
overall rate of 13%. There are a number of technical and conceptual
difficulties with the use of a reconstruction nail for the treatment of
combined neck and shaft fractures. First, a medullary implant is
unlikely to be the treatment of choice for fractures of the femoral
neck. Second, the entry site for the reconstruction nail is frequently
in the same location as the femoral neck fracture. Even with an open
reduction of the femoral neck, there is the potential for further
displacement during nail placement. Third, it can be technically
challenging to seat the nail properly with the correct anteversion to
allow placement of two screws accurately into the femoral head and
parallel to the femoral neck. By avoiding a nail entry site that is
through or near the femoral neck fracture, a trochanteric entry
cephalomedullary implant to treat this combination of fractures may
alleviate some of these technical challenges.
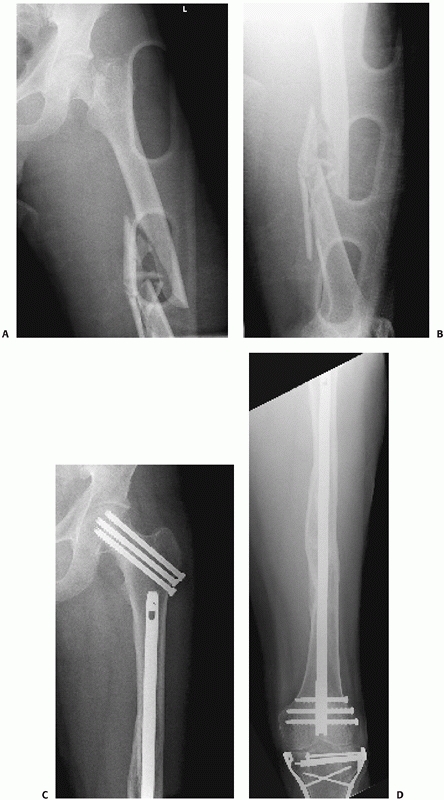 |
|
FIGURE 50-30 This patient sustained displaced ipsilateral femoral shaft and femoral neck fractures after a motor vehicle crash (A,B).
Treatment consisted of open reduction and internal fixation of the femoral neck fracture followed by retrograde intramedullary nailing of the femoral shaft fracture. Healing of both injuries proceeded without complications (C,D). |
associated ipsilateral fracture patterns can further complicate the
management of femoral shaft fractures (Fig. 50-31).
Segmental comminution, characterized by circumferential loss of
cortical contact even after reduction, can be successfully managed with
closed intramedullary nailing.300 In a series of 33 segmental femur fractures treated with reamed antegrade nailing, Wiss et al.300
identified infrequent complications that included one nonunion and two
malunions. This led the authors to conclude that virtually all
fractures between the lesser trochanter and the femoral condyles can be
successfully managed with intramedullary nailing. Technical
difficulties with nailing segmentally comminuted fractures include the
intraoperative determination of the proper length and rotation of the
femur, as the visual clues at the fracture itself are less helpful.
Preoperative assessment of the contralateral femoral length can be used
as a guide to judge the length of the injured extremity. Segmental
femoral injuries characterized by multiple noncontiguous fractures
should be differentiated from fractures with segmental comminution and
deserve special mention. These fractures are particularly difficult to
treat with intramedullary nailing because of the need to simultaneously
maintain two reductions. Percutaneous Schanz pins placed as joysticks
into each segment can greatly assist with maintenance of reduction
during reaming and nail placement. For fractures with a “napkin ring”
segment of diaphyseal bone, the free segment should be stabilized with
either a percutaneous pin or a percutaneous clamp during reaming to
avoid spinning the fragment on its soft tissue attachments.
combination with femoral shaft fractures, posing additional challenges.
The articular fracture should be prioritized from an implant
standpoint, but not necessarily from a timing standpoint. The
stabilization of femoral shaft fractures in a critically ill patient
still takes priority over the operative fixation of periarticular
fractures. However, a thoughtful preoperative plan can ensure that an
accurate articular reduction of the distal femur can be accomplished as
well. If the patient can tolerate a longer procedure, the articular
injury should be reduced and stabilized first with whatever implants
are necessary, because there is more flexibility with stabilization of
the femoral shaft fracture. Screw fixations alone are frequently
adequate for coronal plane articular fractures of the distal femur and
will not interfere with passage of an antegrade nail. For medial and
lateral femoral condyle fractures, a combination of strategically
placed lag screws and plates will usually not interfere with nail
placement. For a supracondylar intercondylar distal femoral fracture
combined with a noncontiguous femoral shaft fracture, the articular
surface of the intercondylar component must first be reduced and
stabilized followed by stabilization of the remaining supracondylar and
shaft fractures. Depending on the locations of the distal and shaft
fractures, single (plate or nail) or multiple (plate and plate or plate
and nail) implants may be necessary. In general, combined plate and
screw fixations of the distal articular fracture should be performed.
Reasonable results have also been obtained by using a combination of
lag screws to reduce the distal articular injury with a nail to
stabilize both the femoral shaft and the distal supracondylar
components. However, in their review of 10 patients with intercondylar
distal femoral fractures combined with a femoral shaft fracture, Butler
et al. reported some articular displacement in 40% of cases in which
screws alone were used to stabilize the intercondylar component.44
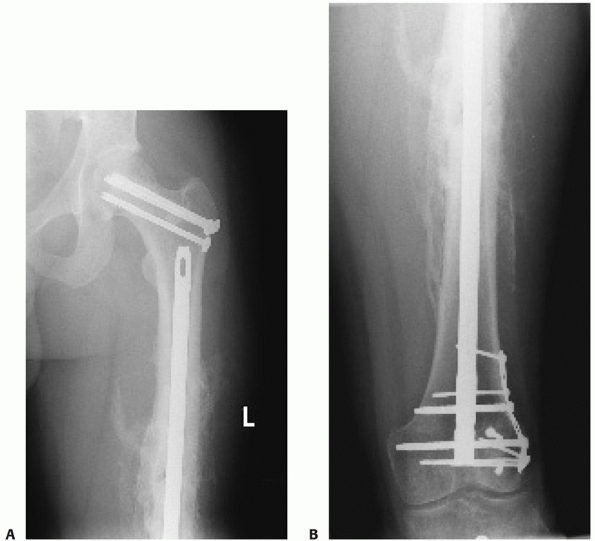 |
|
FIGURE 50-31
This patient sustained combined fractures of the femoral neck, femoral shaft, and distal femoral lateral condyle. The femoral neck was first stabilized. The lateral condyle was then treated with open reduction and internal fixation. Finally, the femoral shaft was stabilized with a retrograde nail (A,B). |
neck, femoral shaft, and distal femur have been reported. This
combination of injuries occurs in less than 0.5% of femoral fractures.
All femoral neck fractures in one series were vertical in orientation
and all distal femoral articular injuries were unicondylar. A
recommended treatment algorithm was presented by Barei et al.11
and was based on their experience with seven patients. Open reduction
and internal fixation of the displaced femoral neck fracture should be
prioritized followed by fixation of the displaced distal articular
fracture. Finally, the diaphyseal fracture can be treated with a
technique that does not jeopardize either of the other two fixations.
Specifically, this can be with either a plate or an intramedullary nail
(antegrade or retrograde).
hip joint, and femoral shaft, although rare, do occur. These are
frequently caused by a dashboard injury with direct impact on the knee
with the hip joint flexed. The extensor mechanism disruption may be a
patellar fracture, an infrapatellar tendon injury or a quadriceps
tendon rupture. A treatment protocol based on their experience with
managing 10 patients with this combination of injuries was reported by
Mosheiff et al.193 They recommended
intramedullary nailing of the femur, followed by open reduction and
internal fixation of the acetabular fracture, followed by extensor
mechanism repair. Frequently, multiple stages were required, but this
protocol simplified each surgical episode and maximized patient
recovery.
known to have a worse overall prognosis and a higher mortality than
patients with unilateral femur fractures.65,197
Several factors may contribute to this including increased associated
injuries, increased blood loss, a higher risk of adult respiratory
distress syndrome, or the increased systemic effects of multiple long
bone fractures. In addition, the presence of bilateral femur fractures
is associated with other complications including compartmental
syndrome, peroneal nerve palsy, and delayed union. The incidence of
bilateral femoral shaft fractures in patients treated at tertiary
referral trauma centers ranges from 7.3% to 9.6%. These patients tend
to have a higher ISS and a lower Glasgow Coma Scale score than patients
with unilateral femoral shaft fractures.65,197
reported increased ISS, mortality, and ARDS in 85 patients with
bilateral injuries. The mortality rate in patients with bilateral femur
fractures was 25.9% compared with 11.7% in patients with unilateral
injuries. Similarly, ARDS was diagnosed in 15.7% of patients with
bilateral fractures compared with 7.3% of patients with unilateral
fractures. The increase in mortality was found to be related to the
associated injuries and various physiologic parameters as opposed to
the presence of bilateral fractures.65
The increased mortality in patients with bilateral fractures was
confirmed in another study reviewing 689 patients with unilateral
injuries and 54 patients with bilateral injuries treated with reamed
intramedullary nailing for their femoral shaft fractures.197
Patients with bilateral femur fractures were found to have a higher
average ISS and a longer length of stay than patients with unilateral
fractures. Mortality in patients with bilateral femur fractures was
5.6% compared with 1.5% in patients with unilateral femur fractures.
The relative risk of death in patients with bilateral fractures was 3.8
times higher than in patients with unilateral fractures. Multiple
linear regression and logistic regression with age and ISS as
covariants were used to compare patients with a similar degree of
trauma. This revealed an odds ratio of 3.3 for mortality in patients
with bilateral femur fractures compared with patients with unilateral
femur fractures. Because the ISS does not increase with the presence of
a second femoral shaft fracture, the ISS may not accurately reflect
mortality in patients with bilateral femur fractures.197
fractures is the same as that for unilateral femoral shaft fractures.
Reamed intramedullary nailing, whether antegrade or retrograde, can be
expected to produce similar rates of union compared with treatment in
unilateral injuries. Retrograde nails have been used successfully and
mortality appears to be similar to other studies using predominanly
antegrade nails.49 The use of
temporary external fixation consistent with damage control orthopaedics
may be considered in these patients depending on their associated
injuries.
likely to decrease in the near future. There are several technical
aspects of antegrade intramedullary nailing that make the procedure
more difficult in obese patients. Osseous landmarks are difficult to
palpate, and femoral adduction is usually somewhat limited. In
addition, the common locations of excess adipose tissue usually limit
the surgeon’s ability to align a guide pin or an awl with the femoral
canal when attempting to localize the correct starting point. This
frequently leads to the need for a large surgical approach to simply
identify the osseous anatomy proximally. Although lateral positioning
greatly assists with identifying the starting point, this may not be a
practical position depending on the size of the patient. Reduction of
the femoral shaft is increasingly difficult with increasing patient
size, and the usual techniques may be impractical. As well, the
external jig that is used for proximal interlocking may not clear the
lateral thigh tissues. Because of the difficulties associated with
identifying the piriformis antegrade starting point, alternative nail
entry sites have been recommended in obese patients.228,282 Ricci et al.228
demonstrated decreased surgical time and radiation exposure yet similar
functional outcomes in obese patients treated with a trochanteric entry
nail compared to a piriformis entry nail. Similar results have been
demonstrated using retrograde nailing as an alternative in obese
patients.282 The authors found
similar decreases in operative and fluoroscopy time when a retrograde
nail was used compared to an antegrade nail placement. Although the
retrograde starting point may be easier to identify in obese patients,
proximal interlocking can be a lengthy experience given the distance
between the anterior skin of the thigh and the anterior femoral cortex.
Long drill bits, long screwdrivers, and a suture tied to the
interlocking screw may assist with proximal interlocking of a
retrograde nail.
morbidly obese patients treated with reamed antegrade nailings were
reported by McKee and Waddell.176
The patients had an average weight of more than 300 pounds with an
average body mass index of 49.2. The surgical procedures averaged 3.8
hours in duration with an average blood loss of 1100 mL. Numerous
complications were noted including two iatrogenic trochanteric
fractures, two wound infections, four deep venous thromboses, and one
fatal pulmonary embolism.
high-energy mechanisms. More frequently, they are the result of falls
from standing. However, motor vehicle accidents and pedestrians hit by
cars occur in this patient demographic as well. Particular challenges
in this group of patients include fixation in relatively osteopenic
bone and management of the multiple associated medical problems
frequently observed.
bone mineral density occur and are more commonly observed in females.
As a result, fixation becomes particularly difficult. In addition,
preexisting arthritic conditions frequently limit the excursion of the
knee and hip joints, potentially prohibiting specific fixation options.
Of particular importance is the identification and treatment of
preexisting medical diseases that occur frequently in this patient
population. In a cohort of 102 elderly (average age of 81 years)
patients who sustained a femur fracture, Sartoretti et al.244
identified commonly observed comorbid conditions that included
cardiovascular disease in 80%, musculoskeletal disease in 75%,
gastrointestinal disease in 67%, psychiatric disease in 61%, urologic
disease in 55%, and pulmonary disease in 41%. The postoperative
mortality was 11%, and the mean hospitalization was 30 days.
elderly patients is uniformly associated with high union rates yet a
high incidence of complications including mortality. In a series of 138
patients aged more than 65 years with femoral shaft fractures,
complications were observed in 46% and mortality in 20%.28 Other authors have reported mortality rates that are similar to those in elderly patients with hip fractures.3,30,189 The mental status of the patient has been found to be a significant predictor of survival,28 and the development of a new medical problem after injury has been associated with a poor result.30
In surviving patients, fracture union can be expected after
intramedullary nailing for fractures of the femoral shaft. In a review
of 12 femoral fractures treated with statically locked intramedullary
nails, union was observed in all patients.
specific to elderly patients must be observed. Because of the
relatively thin cortices, care must be taken to accurately identify the
starting portal. Iatrogenic comminution can occur with manipulation of
the femoral shaft despite relatively low applied forces. Interlocking
screws frequently have poor purchase. If a mismatch between the
sagittal bow of the femur and the nail, an iatrogenic distal femoral
fracture may occur if a long antegrade nail is chosen.203
A careful preoperative evaluation of the shape of the femur on both the
AP and lateral views is necessary before deciding on a medullary
implant in elderly patients. Because of the capacious canal, a
large-diameter implant may be necessary.
osteopenic bone, many manufacturers have made specific design changes
in medullary implants. Some interlocking screws are designed with a
large washer on the lateral side and a large nut with washer that can
be threaded on the leading (medial) side of the screw. Some retrograde
nails allow placement of a locking bolt that prevents coronal plane
toggling of the most distal interlocking screw. Multiplanar distal
metaphyseal locking screws and spiral blades are available with some
nails and may assist with purchase in the capacious metaphysis.
Knowledge of the specific implant characteristics is important when
deciding the treatment plan in these challenging fractures.
Because the proximal femur is the most commonly affected site of
metastases in the appendicular skeleton, the relevant management will
be discussed. The diagnosis of metastases should not be assumed despite
clinical suggestions and a history of carcinoma in another location.
Discussion with an orthopaedic oncologist will help to avoid the
complications associated with treatment of an unknown femoral lesion.132
to provide femoral stability, thereby decreasing pain, allowing
mobilization, and facilitating nursing care. Fracture healing depends
on the type of tumor. Osseous healing may not occur in many of these
injuries despite stabilization. In 129 pathologic fractures of long
bones, Gainor and Buchert89 observed
healing in 67% of fractures from multiple myeloma, 44% from renal
carcinoma, 37% from breast carcinoma, and in no fractures secondary to
lung carcinoma. Overall, the fracture healing rate was 35%, but this
increased to 74% in patients who survived longer than 6 months.
Although a significant percentage of these fractures were treated
without internal fixation, this emphasizes the difficulty with
obtaining union in these patients.
nail, for metastatic lesions of the femoral shaft is based loosely on
clinical symptoms, expected length of survival, and lesion size.
Guidelines for the size of a metastatic lesion that requires
prophylactic internal fixation has been suggested by Menck et al.178
in a radiographic study of 69 patients. They recommended stabilization
if the ratio between the width of the metastasis and the bone diameter
was greater than 0.6, if the axial cortical destruction in the femoral
shaft was greater than 30 mm, or if the cortical destruction of the
femoral circumference was greater than or equal to 50%.
If plate fixation is chosen, cement should be used to augment the
fixation in most instances. Locked implants can be considered given the
frequently present poor bone quality. Intramedullary nailing is optimal
in most femoral fractures resulting from metastatic disease because of
the biomechanical properties of the load-sharing implant. To span the
entire femur including the femoral neck, a cephalomedullary nail should
be used in pathologic fractures. Patients can safely bear weight after
stabilization. However, intramedullary nailing for metastatic disease
is associated with increased perioperative complications including fat
embolism and mortality. Barwood et al.14
observed intraoperative oxygen desaturation in 24% of patients with
death in 7% of patients treated with intramedullary nail fixation for
their overt or impending femoral fractures. Cole et al.63
reported their experience with reamed and unreamed intramedullary
nailing in 73 femurs with metastatic disease. Both techniques were
found to sufficiently stabilize the femur, and implant failures were
uncommon. Death associated with the nailing procedure occurred in one
patient treated with a reamed nail and in one patient treated with an
unreamed nail. In general, second-generation reconstruction nails or
other cephalomedullary implants should be used for the treatment of
metastatic femoral fractures. Although a standard femoral nail is
adequate for lesions confined to the femoral diaphysis, minimization of
the need for future stabilization procedure can be
accomplished with the use of an implant that effectively protects the entire femur.
proximal femoral shaft or subtrochanteric region has been described.
This fracture has been associated with the use of alendronate and is
thought to be associated with the prolonged suppression of bone
remodeling with this medication.102,159,162,196
Alendronate is a bisphosphonate that inhibits bone resorption by
osteoclastic suppression. Decreased bone turnover and impaired repair
of microscopic damage has been implicated in the propogation of these
subtrochanteric or proximal femoral shaft fractures. Several
characteristics were common to these fractures based on a review of 17
patients with low energy subtrochanteric and proximal femoral fractures
by Kwek et al.158 and included:
cortical thickening on the lateral side of the subtrochanteric region,
a transverse fracture, and a medial cortical spike (Fig. 50-32). The majority of patients (76%) had prodromal pain and bilateral involvement (53%).158
Given the potential for bilateral involvement, it is generally
recommended that contralateral femur radiographs be obtained to look
for early signs prior to fracture.
 |
|
FIGURE 50-32
This elderly woman sustained a subtrochanteric fracture after a fall from standing. She had been treated with alendronate for a number of years and had a several month history of proximal thigh pain prior to her fracture. The fracture is relatively transverse and there is associated cortical hypertrophy in the subtrochanteric region (A). Treatment consisted of placement of a cephalomedullary nail with a helical blade (B,C). Healing progressed uneventfully as demonstrated at 5 years (D,E). (Case courtesy of Dean Lorich, MD, New York, NY.) |
additionally demonstrated this relationship between chronic alendronate
use, the presence of a simple transverse fracture, and unicortical
beaking in the area of cortical hypertrophy. Although the exact causal
relationship between alendronate therapy and these atypical fractures
has yet to be
confirmed,
recognition of this pattern is important especially given the prodromal
symptoms and consistency of bilateral involvement.102,159,162,196
treatment in the majority of cases is immediate closed, statically
locked, reamed, antegrade intramedullary nailing using a piriformis
starting portal. We tend to use a percutaneous approach with the
patient positioned supine on a radiolucent table with the leg draped
free. A guide pin with a cannulated drill allows for a precise
determination of the starting point. An intraoperative distal femoral
traction accurately placed allows for distraction and reduction of the
fracture as well as assessment of rotation.
threatening injuries, early treatment with nailing leads to union and
allows early patient mobilization. Appropriate patient selection and
careful attention to the numerous technical aspects of the procedure
can minimize the potential complications. Early treatment of femur
fractures with reamed nailing in polytraumatized patients decreases
patient mortality.25 Static locking prevents shortening, maintains femoral rotation, and does not have a deleterious effect on union.42,304
Reaming allows for placement of an appropriately sized implant,
increases the rate of union, and decreases the incidence of hardware
failure.21,47,277 The potential negative impacts of reaming on the patient with multiple or thoracic injuries have not been confirmed clinically.27 Overall, union can be expected in 97% to 99% of cases.47,297,300,304
portal for nail placement is largely based on the preference of the
surgeon. At our institution, an antegrade nail is chosen if at all
possible mainly because of the ease and predictability of future or
secondary procedures. If the patient develops a complication that
requires either an exchange nail or implant removal, our preference is
to do that procedure at an extraarticular location (the trochanteric
fossa) as opposed to an intra-articular location (the knee). As well,
the same “relative indications” for retrograde nails can be interpreted
as “relative contraindications.” For instance, an ipsilateral patellar
or articular injury at the knee suggests local trauma; the iatrogenic
trauma of then going through the knee with reamers and a medullary
implant seems unjustified. The situations that make a retrograde nail
more attractive include ipsilateral femoral neck fractures, morbid
obesity, and bilateral injuries in a critically ill patient. With an
ipsilateral femoral neck fracture, I prefer to prioritize the femoral
neck because of the lack of good salvage procedures for complications
related to that injury. A retrograde nail can be placed after the
femoral neck is stabilized; however, a plate can be used as well. In
morbidly obese patients (BMI > 35), in whom the extensive surgical
approach for an antegrade nail is associated with an increased risk of
infection, a retrograde nail may be desirable. For bilateral injuries
in the critically ill patient, the ability to rapidly stabilize both
femurs without the need to reposition the patient can make retrograde
nailing a good option in rare circumstances. These nails can be placed
and locked distally using the attached external jig, saving the
proximal interlocking for a time when the patient can undergo a more
extensive procedure. However, external fixation with conversion to
antegrade intramedullary nails after the patient has stabilized is a
reasonable option as well.212,213
is generally reserved for unusual circumstances given the excellent
results with intramedullary nailing. Primarily, this procedure is used
only in patients with an extremely narrow medullary canal, previously
placed hardware, an associated vascular injury, proximal or distal
fracture extensions, lack of fluoroscopy, or an associated femoral neck
fracture. Submuscular and/or open techniques that maintain maximal
femoral vascularity are used.
used as a definitive treatment for a femoral shaft fracture in an
adult. However, this technique may be used as a temporary form of
stabilization until femoral nailing is deemed safe. This includes
patients with an associated vascular injury, patients with multiple
injuries, and patients with massive medullary canal contamination. Even
in these circumstances, primary treatment reamed nailing is still
usually preferred in the majority of circumstances.
intramedullary nailing. The primary nerves at risk are the femoral,
sciatic, peroneal, and pudendal. Patient positioning and intraoperative
traction are usually implicated as causal. A careful preoperative
neurologic examination should be performed and documented to avoid
unnecessary confusion if a patient is discovered to have nerve
dysfunction after femur stabilization.
dysfunction are complications of femoral nailing and are likely related
to the use of traction table with a perineal post.38,85,170
prospectively studied 106 patients treated with static antegrade
nailing to determine the duration and magnitude of intraoperative
traction that was associated with development of a pudendal nerve
palsy. Pudendal nerve palsies occurred in 10 patients, six of whom were
male. Sensory changes were present in nine instances, and one patient
had erectile dysfunction. Symptoms resolved in all but one patient. The
magnitude of the traction was noted to be significantly higher in those
patients who developed a pudendal nerve injury. Patients who developed
a postoperative pudendal nerve palsy had slightly longer procedure
times, although this is not statistically significant. The association
of a pudendal nerve palsy and the use of a fracture table were further
emphasized in a combined retrospective and prospective study by France
and Aurori.85 Retrospectively,
pudendal palsies were identified in 1.9% of patients, and only 1
patient of 36 developed this complication during the prospective
portion of their study. Erectile dysfuction has been shown to be highly
prevalent after intramedullary nailing of femoral shaft fractures. In
one study, more than 40% of patients had some erectile dysfunction and
was postulated to
be related to direct pressure on the pudendal nerves by the perineal post.170
process of femoral nailing. This complication is likely caused by
stretching of the nerve during various reduction maneuvers. It is
important to avoid any prolonged over distraction of the limb during
the procedure. Although this is unlikely if manual traction is used, it
is possible if a femoral distractor or the fracture table is used to
maintain femoral length during nailing. Knee flexion during surgery can
relax the sciatic nerve and its terminal branches; knee extension
should be avoided. In addition, circumferential dressings, especially
at the knee, should be avoided postoperatively. Although a case report
exists,33 suggesting that a
postoperative sciatic nerve injury was caused by bow-stringing of the
nerve between the fracture surfaces in a displaced proximal femoral
fracture, this is unlikely given the large numbers of reported femoral
nailings without this complication.297,304 Assuming all other causes of sciatic nerve injury are excluded, a stretch injury can usually be observed with expected return.
antegrade intramedullary nailing are of particular concern. In four
patients with bilateral femur fractures, Carlson et al.50
reported four peroneal nerve palsies and two compartmental syndromes in
the leg that was stabilized second. In each case, the injured leg was
initially placed into a calf-supported leg holder. On the basis of
their experience the authors cautioned against this type of positioning
in patients with bilateral lower extremity injuries. The incidence of
contralateral leg compartmental syndrome is a well-documented
complication even in patients without bilateral injuries.
to the surrounding muscles in addition to the obvious and treatable
osseus injury. In addition, surgical treatment is associated with a
further insult to the lower extremity musculature. In the case of open
plating, this usually involves a lateral approach to the femur with
associated dissection of the vastus lateralis. In antegrade femoral
nailing, injury to the hip abductors and external rotators may occur as
a result of the surgical approach, nail insertion, or both.10,75,173,184,206 The approach for antegrade femoral nailing, whether percutaneous or open, may have an effect on subsequent muscle function.
reviewed 29 patients at a minimum of 16 months from injury. The
patients were treated with both open and closed methods including spica
casting, cast bracing, open plating, and intramedullary nailing.
Quadriceps impairment was identified in 83% of patients. Prompt
healing, young age, and fracture location at the midshaft level were
found to predict better function. Patients treated with a plate or an
intramedullary nail were found to have a better overall functional
result but did not have a measurable increase in quadriceps strength.181 In a study of hip abductor function after femoral nailing, Bain et al.10
reviewed 32 patients clinically and radiographically. In addition to
trochanteric pain, thigh pain, and a limp, the authors found a
significant difference in abductor strength and the abduction ratio
compared with asymptomatic controls. A correlation between abductor
weakness and patient complaints was also noted. In contrast, other
authors found no difference in hip abduction strength at greater than 2
years from injury in 23 patients with femoral fractures treated with
intramedullary nailing. However, a significant decrease in knee
extension strength when compared with the contralateral extremity was
found.70 This was subsequently
confirmed in a study of 17 patients with healed femoral fractures
evaluated at least 18 months after surgery. The authors evaluated the
bone mineral density of the medial and lateral femoral cortices and the
isometric strength of six separate muscle groups, which included the
quadriceps, hamstrings, hip extensors, hip flexors, hip abductors, and
hip adductors. They found a significant reduction in quadriceps
strength but no difference in the remaining five muscle groups when
compared with the contralateral extremity as a control. A decrease in
the bone mineral density of the femoral cortices was found, but this
could not be attributed to the implant or the change in muscle strength
observed.142 Finsen et al.84
compared the quadriceps strength in 14 patients treated with
intramedullary nails and 12 patients treated with open plating.
Isokinetic thigh muscle function was fully restored in nailed patients,
but there was a decrease in strength in plated patients. The authors
noted a moderate flexion strength deficit in both groups.
the effects of antegrade femoral nailing on patient function and
outcomes.8,118
Eight patients were evaluated for hip abductor weakness following
antegrade femoral nailing of isolated femoral shaft fracrures. The
authors identified significant time dependent gait abnormalities and
dynamic hip abductor weakness in the two- and six-month evaluations.
Patients did improve with time and their functional outcomes were found
to correlate with ipsilateral trunk leaning.8,118
However, in a cohort of 21 patients evaluated at a minimum of 1 year
after piriformis entry antegrade femoral nailing, normal gait patterns
were observed. Although the authors observed lower peak torque by the
hip abductors and extensors compared to the contralateral side,
functional questionnaires demonstrated no significant disability.118
greater than 5 degrees of angulation in either the coronal
(varus-valgus) or sagittal (flexion-extension) planes. Although the
effects of an angular deformity and its impact on ipsilateral joint
mechanics and contact pressures have been defined for the tibia, the
same is not true for the femur. Periarticular angular deformities are
more likely to have an increased effect on the proximate joint than
malunions in the mid-diaphyseal portion of the femur. Fortunately, with
the use of operative fixation for most femoral diaphyseal fractures,
malunion is less common.
the femur occurs infrequently after intramedullary nailing, largely
because of the intimate fit between the medullary implant and the
cortical bone of the femoral isthmus. However, in the proximal and
distal thirds of the femur, the more voluminous medullary canal ensures
that cortical contact with the nail will not occur, allowing for
angular deformities to occur. As well, fractures located proximally or
distally have angular reductions that are more dependent on the
starting points than those fractures located in the middle third.
Overall, the rate of angular malalignment after medullary nailing is
between 7% and 11%.143,227,304 In an investigation looking at the factors associated with angular
deformities after femoral nailing, Ricci et al.227
found the highest rate of malalignment in proximal third fractures
(30%) compared with fractures in the distal third (10%) or middle third
(2%). Increased malalignment was seen in unstable fracture patterns
(12%) as compared with stable fracture patterns (7%). They found no
relationship between angular deformity and either the nail diameter or
the direction of the nail insertion (i.e., retrograde or antegrade).
Wolinsky et al.304 reported an
increased rate of angular deformity in distal femoral fractures treated
with reamed, locked, antegrade nailing. The use of manual traction as
opposed to the fracture table has not been found to affect angular
alignment.143,304
medullary implant in the proximal or distal thirds of the femur
requires attention to detail during reduction, reaming, nail passage,
and interlocking. In all femoral fractures, the sagittal plane
alignment can be maintained with strategically placed bumps if manual
traction is used. This assumes, however, that the proper femoral length
is restored to prevent overlapping of the fractured bone ends. In
proximal fractures, a properly aligned starting point will greatly
assist with minimizing angular deformities. Percutaneous clamps,
pushers, and joysticks can be used to control the proximal segment
during the remaining portions of the nailing procedure. For distal
fractures, it is important to ensure that reaming is accomplished over
a well-centered guidewire to avoid eccentric bone removal. Similar to
proximal fractures, percutaneously placed reduction tools can greatly
assist with obtaining and maintaining the reduction and alignment in
distal fractures.
two distal interlocking screws should be strongly considered in
fractures located distal to the isthmus. Because the diameter of the
transverse hole in the nail is larger than the interlocking bolt that
it accommodates, a certain amount of coronal plane deformation of the
femur can occur. This is related to the specific nail design and
tolerances, as well as the bone quality. Similarly, rotation around the
interlocking bolt in the sagittal plane is possible with a single
locking screw. Although a large distance between the proximal
interlocking bolt and the fracture is desirable, Tornetta and Tiburzi276
demonstrated good maintenance of reduction in extremely distal femoral
fractures treated with antegrade intramedullary nailing, despite having
all proximal interlocking screws within 5 cm of the fracture.
with fixation. Unlike in the tibia, femoral diaphyseal osteotomies may
not require placement or removal of a wedged-shaped intercalary graft
to allow the correction to occur. Depending on the deformity and the
preoperative plan, a single or double-level osteotomy may be required.
Standing films from the hips to the ankles are necessary to plan for a
correction that accurately restores the mechanical axis. Stabilization
with an intramedullary nail offers a number of advantages including
early weight bearing and predictable healing. If a medullary implant is
chosen for stabilization, the osteotomy can be performed with an
intramedullary saw or through a limited incision. Plate fixation
requires a more extensive exposure, and weight bearing must be
restricted until healing occurs. However, plate fixation allows for a
more accurate correction of angular and rotational deformities (Fig. 50-33).
method of femoral stabilization. It is unlikely in compression plating
of the femur, but does occur with antegrade nailing, retrograde
nailing, external fixation, traction, and bridge plating. The amount of
femoral rotation that can be well tolerated by the patient is largely
unknown, but there appears to be increased symptoms and the need for
operative correction in patients with more than 15 degrees of
rotational malalignment.32,131,146,312
This has been confirmed by a review of 21 patients with 15-degree
rotational deformities demonstrated on CT scans. These patients were
found to have functional limitations and difficulties with demanding
activities such as sports, running, and climbing stairs. Surprisingly,
an external torsional deformity was associated with increasing symptoms
compared with an internal torsional deformity.130,131
This may be due to the observation of decreased compensation and more
physical complaints in patients with an external rotation malalignment.130
nailing, 19% of patients were found to have a rotational deformity of
15 degrees or more. This was symptomatic in 38% of patients, compared
with 12% of patients with deformities between 10 and 15 degrees. In
contrast, no patient with less than 10 degrees of a rotational
malalignment had relevant symptoms.32
The overall incidence of a rotational malalignment exceeding 15 degrees
after antegrade intramedullary nailing using a statically locked
implant ranges from 9% to 28%.32,131,312
However, in unstable fractures with Winquist type 3 and 4 comminution,
rotational malalignment was identified in almost half of the patients
independent of fracture location and patient position at the time of
nailing.274
postoperatively using several methods including clinical examination
and radiologic evaluations. Clinically, rotation of the contralateral
extremity can be confirmed by flexing the hip and knee to 90 degrees
and recording the internal and external rotation of the leg. This can
then be compared with the injured side after intramedullary nailing.
There are several limitations to this method.150
First, there is some toggle between the interlocking bolts and the nail
that allows some rotation of the femur around the implant. Second, if a
slotted and relatively thin walled nail is used, the implant itself can
rotate around its long axis, making the clinical measurement
inaccurate. Third, these measurements rely on measuring rotation
relative to the pelvis. The pelvis is usually tilted to allow for nail
placement, making this measurement inaccurate. Finally, clinical
examination is only useful after the nail and interlocking bolts have
been placed. If a perceived difference is confirmed, revision is
required. Although clinical measurement is the easiest and most readily
available method for determining rotation, its accuracy is questionable
at best. In a study using CT scans to confirm the final rotational
alignment in 76 femurs treated with medullary nails, clinical
examination failed to identify almost half of the patients with
20-degree deformities.131
for determining femoral rotation, most of which can be accomplished
easily during intramedullary nailing. Normally, the cortical thickness
of the femur in the AP and lateral planes can be assessed
fluoroscopically, helping to judge the proper rotation. Because the
femoral canal is not perfectly cylindrical and the cortical thickness
is not uniform around the diameter of the bone, small rotational
differences will be reflected by a change in the apparent cortical
thickness. Although this has not been shown to be accurate in a
published study, it is useful clinically. In segmentally comminuted
femur fractures, the lack of osseus apposition at the fracture makes
this radiologic clue relatively useless. Another method is the
determination of the femoral anteversion based on a lateral
fluoroscopic image of the femoral neck. After confirming a true neutral
rotation of the distal femur, a lateral hip fluoroscopic image can be
obtained with the image intensifier in the same rotation, allowing for
an accurate measurement of the femoral neck anteversion. This can be
used to compare with the known femoral anteversion of the uninjured
femur, which is obtained preoperatively.157,274
An alternative method for determining intraoperative femoral rotation
is accomplished by comparing the shape and appearance of the lesser
trochanter, a surprisingly sensitive sign.146,150
Before prepping the affected limb, the image intensifier is positioned
laterally and a true condylar overlap lateral of the unaffected distal
femur is obtained, thereby ensuring the rotation of the leg. The image
intensifier is then rotated 90 degrees, and an AP view of the lesser
trochanter is obtained and stored for comparison. Then, at the time of
surgery, the distal femoral segment can similarly be rotated into a
perfect lateral position. The proximal segment can then be rotated with
a percutaneous Schanz pin or external jig to match the lesser
trochanteric profile to the stored image of the unaffected leg. This
method has been demonstrated to reproduce the proper rotation to within
4 degrees in 87% of cases, and to within 15 degrees in all cases146 (see Fig. 50-17).
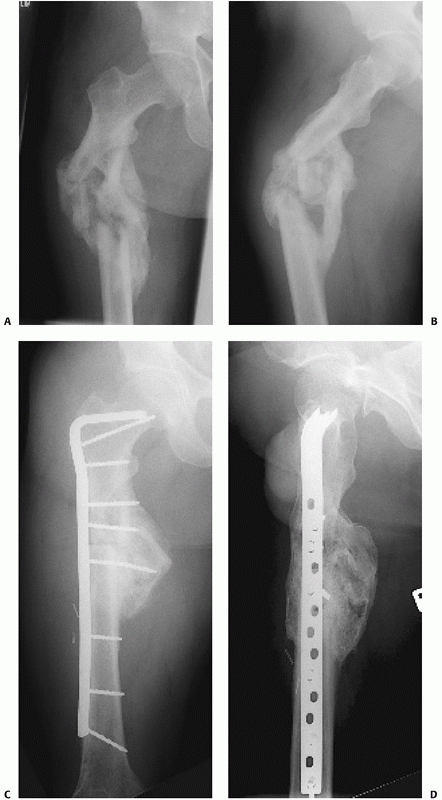 |
|
FIGURE 50-33 Nonoperative treatment of this patient’s femoral shaft fracture resulted in a significant malunion with varus and extension (A,B). An osteotomy with plate stabilization was required to restore the mechanical axis of the limb (C,D).
|
assessed at the time of nail passage, after interlocking, and before
leaving the operating room. If there is any doubt or clinical
suggestion of abnormality, a CT scan should be obtained to document the
difference. CT can be used to assess the femoral anteversion (and thus,
the femoral rotation) by comparing similar axial cuts of the injured
and uninjured femurs at the levels of the femoral neck and distal femur
(Fig. 50-34). By comparing the relative angles
of the posterior femoral condyles and the long axis of the femoral
neck, the femoral torsion can be assessed.31,32
However, poor intraobserved reliability due to inaccuracy of
identification of the femoral neck axis has been previously
demonstated. Consideration should be given to taking multiple
measurements as the intra- and inter-observer variance has been shown
to be approximately 4 degrees.129 It
is important to strictly maintain the position and rotation of the legs
between the tomographic cuts to ensure an accurate assessment. This can
usually be accomplished by simply taping the legs down during the
evaluation. Although this method has limited utility in the
intraoperative assessment of femoral rotation, it can be used to judge
rotation in suspected cases after surgery. If the deformity exceeds 15
degrees, consideration should be given to correcting the malalignment
acutely. Acute correction of a rotational deformity can usually be
accomplished by removing the distal interlocking screws and rotating
the distal segment of the femur around the nail. Pins placed into the
femur can be used to judge the rotation before and after correction.
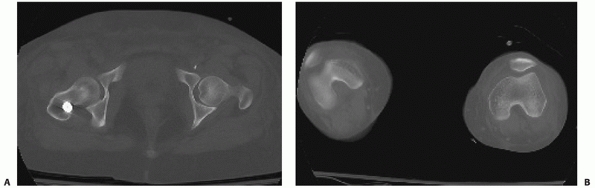 |
|
FIGURE 50-34 CT scan with axial cuts of the femoral neck (A) and distal femur (B)
can be used to determine the relative rotation of the femur. Comparison with the opposite femur indicates a 25-degree external rotational deformity of the right femur. |
observed after a fractured femoral shaft. Stiffness is thought to be
related to the type of treatment, fracture location, and associated
injuries. An associated head injury and the formation of ectopic bone
can both contribute to limited knee motion. High-energy mechanisms such
as a motor vehicle crash, multiple procedures, and a delay in union
were also associated with persistent knee stiffness after treatment in
one study.128 Although treatment with a plate has been suggested to contribute to some knee stiffness,58 larger studies have failed to identify this relationship.56,93,229
Further, a trend toward improved knee motion was shown after treatment
with an antegrade femoral nail compared with a retrograde femoral nail
in a prospective and randomized evaluation comparing the two techniques.280
However, most studies have failed to report an association between
retrograde nailing and knee stiffness. Both knee flexion and extension
may be limited after a femoral fracture. Most typical is a combination
of limited passive knee flexion and limited active knee extension (knee
extension lag). Limited knee flexion is typically caused by scarring of
the quadriceps muscles, especially the vastus intermedius, anteriorly
in the region of the fracture. In these cases, treatment consists of an
aggressive rehabilitation program including active knee flexion. If
left untreated, scarring at the knee joint may occur, further
complicating
management.
Knee stiffness usually improves in the first 6 to 12 weeks after
surgical stabilization of a femoral shaft. If there is a lack of
continued improvement clinically at 3 to 6 months, a knee manipulation
and/or a surgical release can be considered. However, this is necessary
in the minority of cases. The results of a Judet quadricepsplasty for
the management of the posttraumatic stiff knee have been demonstrated
in several studies and reports.128,188,289
In certain circumstances, the presence of an anteriorly displaced
cortical fragment, anterior ectopic bone, and reduction in extension
may further be associated with or contribute to a loss of knee flexion.
Treatment of the underlying cause may be necessary in some
circumstances. Knee and hip pain are reported commonly after the
treatment of femoral shaft fractures. The relative incidence of each is
associated with the method of treatment. Ricci et al.,226
in a comparison study of antegrade and retrograde femoral nails,
reported an increased rate of knee pain with retrograde nails (36%
versus 9%) and an increased rate of hip pain with antegrade nails (10%
versus 4%). The incidence of hip pain after antegrade nailing ranges
from 10% to 40%.74,226
This may be related to the formation of heterotopic bone in the region
of the greater trochanter, although hip pain without radiographic
evidence of nail prominence or ectopic bone does occur. Femoral nail
removal23,104,126,180,272
should be restricted to symptomatic patients with hip pain. Partial
resolution of symptoms can be expected in the majority of these
patients.
this chapter in the sections on antegrade nailing, retrograde nailing,
femoral nail removal, and heterotopic ossification.
intramedullary nailing may be related to the surgical procedure, the
fracture, muscle weakness, or the presence of heterotopic ossification.
Formation of ectopic bone at the entry site and overlying the starting
point for an intramedullary nail is observed commonly, especially after
reamed nailing (Fig. 50-35). Fortunately, the majority of heterotopic ossification is not associated with pain or limitations in motion.43,88,171,259
Further, surgical excision is rarely required. Overall, the incidence
of heterotopic ossification ranges from 9% to 60%. Clinically
significant heterotopic ossification occurs in only 5% to 10% of
patients. The origin of proximal thigh pain and its relationship to
heterotopic bone formation was investigated by Dodenhoff et al.74
in their review of 80 patients treated with antegrade intramedullary
nailing. More than 40% of patients were found to have residual proximal
thigh pain almost 2 years from surgery. The usual location was in the
region of the greater trochanter. No correlation was found between the
nail prominence and the incidence of pain. However, a strong
relationship was found between the formation of heterotopic
ossification and the presence of pain.
patient factors, injury patterns, or technical factors has been
inconsistent. Several studies have confirmed the lack of association
between nail prominence and ectopic bone formation.74,171
Heterotopic ossification formation has been found to be increased in
association with male gender, a delay to surgery, and prolonged
intubation.171,259 The most commonly identified risk factor is an associated head injury,171,259 although the Glasgow Coma Scale has not been consistent in predicting excessive bone formation.43
Reamed antegrade nails have been correlated to increased ectopic bone
formation compared with unreamed nails, suggesting that the osteogenic
reaming debris is primarily responsible. In this study, heterotopic
bone was identified in 36% of patients treated with reamed nails
compared with 9% of patients treated with undreamed nails. As well, the
volume extent of bone formation was uniformly increased after reamed
nailing.88
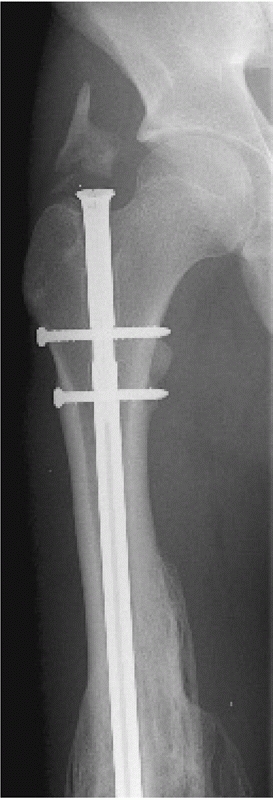 |
|
FIGURE 50-35 Heterotopic ossification at nail entry site.
|
description, and causes of heterotopic bone formation associated with
antegrade nailing was that by Brumback et al.43
They reviewed the results of 80 intramedullary nails placed in an equal
number of patients who were either treated with small volume bulb
syringe irrigation or large volume pulsatile irrigation after nailing.
The size of the ectopic bone was determined for comparison. Overall, no
heterotopic bone was observed in 40% of patients, whereas 34% had mild,
15% had moderate, and 11% had severe bone formation. They observed a
lack of correlation between bone formation and age, gender, delay to
surgery, or ISS. The use of pulsatile irrigation did not decrease the
incidence and volume of heterotopic bone formation.43
after antegrade reamed intramedullary nailing of femoral shaft
fractures. However, clinically significant bone formation that requires
operative excision or nail removal is infrequent. Although
a
correlation has been identified between bone formation and proximal
thigh pain, a significant number of patients have completely normal
radiographs and discomfort at the thigh and lateral hip. Further, it is
unclear whether heterotopic bone formation is indicative of surgical
trauma to the abductors, reaming with osteogenic elements, or patient
factors that are not well defined. It is likely that heterotopic bone
formation is a combination of these numerous patient, injury, and
surgical factors.
or intramedullary nail is rarely encountered. If the fracture is truly
healed, refracture of the femur through the implant would suggest
additional trauma capable of injuring both the femur and the implant.
However, fractures at the ends of plates can occur. Although this is
uncommon and should not be a strong indication for the routine removal
of plates in adults, patients with plates should be counseled regarding
this possibility.
impact on the time-related strength of the bone. If bridge plating is
used to span a comminuted diaphyseal femur fracture, this indirect
method of reduction should ensure that secondary bone healing occurs
with abundant callus formation. Guidelines for timing of hardware
removal are similar to that with intramedullary nails. If the plate is
subsequently removed, the screw holes are a potential source of stress
concentration that could lead to a refracture if a critical torsional
force is applied. Although this is unlikely, patients should avoid high
impact and torsional activities after plate removal. If an open plating
procedure is used with direct compression of the fracture, the femur
would be expected to heal with primary bone healing. As a result,
callus formation would not be expected and plate removal should be
delayed for at least 12 to 24 months to allow for maximal remodeling
and maturation of fracture healing. Refracture is still unlikely;
however, potential sites include the screw holes as well as the
previous fracture.
diaphyseal fracture is similarly uncommon. In 214 patients treated with
static interlocking nailing, only one refracture was identified. This
occurred through the site of the original fracture 6 weeks after nail
removal. There were no secondary fractures at the site of the proximal
or distal interlocking screw holes.39 In a number of subsequent studies reviewing nail removal, no cases of refracture or secondary fracture have been reported.23,104,272
retrograde intramedullary nailing procedures are broken implants. With
advances in nail design and an appreciation for the biomechanics of
these implants, fatigue failure of the implant occurs much less
frequently. Broken nails are indicative of femoral nonunion. If a
fracture fails to heal, the nail will eventually fatigue and break. The
timing of nail failure is dependent on numerous factors including the
size of the implant, type of metal, location of the nonunion, fracture
pattern, patient’s weight, and patient’s activity level. In a review of
60 broken nails in 56 patients, Franklin et al. identified the commonly
observed sites of nail failure.86
The usual location for fatigue failure of the nail is at the site of
the nonunion, where the implant deformation is maximal with motion.
Other locations include transitional sites in the implant and locations
where metal has been removed such as at the interlocking screw holes.
Transitional sites of the nail are the proximal portion of the slot and
the proximal nail waist in implants with an enlarged insertional
diameter.
straightforward; however, difficulties are frequently encountered. If
the femur and the broken implant are well aligned, implant extraction
can proceed in a closed fashion from the antegrade entry site. The
proximal portion of the nail can be removed using an extraction
attachment or conical bolt. If necessary, the proximal segment can be
over-reamed slightly to facilitate removal of the distal segment of the
nail. A long hook can then be placed down the cannulated portion of the
nail as previously described.86 This
frequently requires the use of a straight awl placed down the length of
the cannulated nail to remove any bone that is present distal to the
nail tip. If a hook fails to engage the distal nail segment, multiple
guide wires can be stacked in the distal nail segment to produce an
interference fit at the nail tip. In cases in which significant
displacement of the nonunion has occurred since the time of nail
breakage, an open procedure may be necessary to extract the distal
portion of the nail.
more frequently if small-diameter bolts and nails are used. The screws
typically break at either the medial or lateral aspects of the nail.
This location is important to determine before attempting removal. If
the screw has broken at the medial aspect of the nail, removal of the
broken portion of the screw before nail removal may not be necessary.
However, if the screw breaks at the lateral aspect of the nail, the
entire screw must be removed before attempting to back the nail out.
Broken distal interlocking screws can usually be removed by first
extracting the lateral screw section with an appropriate screwdriver. A
large Steinmann pin with a diameter that approximates the minor
diameter of the locking screw can then be used to push the medial
segment of the locking screw into the soft tissues on the medial thigh.
This can then be extracted through a separate incision. If the nail has
migrated distally and the medial portion of the broken screw does not
align well with the proximal portion, the nail can be extracted
slightly to realign the screw before attempted removal.
current nail designs. However, even in a healed fracture, if enough
force is applied the nail can bend. If the bend in the nail and the
nail diameter are both small, the nail can be extracted without
difficulty. However, significant bends usually require an open
procedure for removal. The nail may need to be cut at the site of the
new fracture or nonunion, and the proximal segment can then be removed
in the usual fashion. The distal segment can be removed as described or
directly from the site of the fracture or nonunion.
fracture healing remains unknown. The initial recommendations of
waiting at least 24 months before nail removal have been shown to be
unnecessary in several studies. Nails removed in less than
1 year have not been associated with refracture in properly selected patients.104,126,180
Complete radiographic fracture consolidation and a lack of associated
clinical symptoms are likely adequate to ensure that fracture healing
is adequate in closed fractures.
complications. For that reason, nail removal in skeletally mature
individuals should be restricted to symptomatic patients only.23,104,126,180,272
In a retrospective review of 164 femoral nails removed after fracture
consolidation, the time interval between nail implantation and nail
removal had no effect on operative time or the incidence of
complications. In the 109 patients available for follow-up at a minimum
of 2 years after nail removal, many were found to have persistent local
symptoms. In the 53% of patients who underwent nail removal for
symptoms, 78% were improved, 16% were no different, and 7% were worse.
In the 47% of patients who were asymptomatic before nail removal, 20%
had increased local symptoms after nail removal. Overall, 41% of
patients were better, 40% were unchanged, and 13% were worse.104
symptomatic patients is the potential for wound complications, which
have been reported in 4% to 10% of patients.23,126,180
This has been shown to be independent of the operative time, nail
depth, heterotopic ossification, and experience of the surgeon.104 No difference has been observed in complications or operative time when removing titanium and steel implants.126
removed in either the supine or lateral position depending on the
surgeon comfort and size of the patient. The radiographs should be
carefully scrutinized for implant identification and fatigue fracture
in anticipation of all necessary removal equipment. Obviously, all
interlocking bolts must be removed before backing out the nail.
However, the extraction jig should be attached to the proximal aspect
of the nail before removing all interlocking bolts to avoid advancing
the nail down the canal and spinning the nail with tightening of the
device. The presence or absence of an end-cap should be anticipated. Of
note, on the basis of experience in 164 nail removals in one study,
end-cap removal was found to be equally time consuming and as difficult
as removal of ingrown bone at the top of the nail, leading to the
authors’ recommendation that an end-cap should be avoided at nail
insertion.104
The diagnosis requires suspicion and frequent examination, especially
given the amount of swelling that is commonly observed after a femoral
shaft fracture. Intense thigh pain and tense swelling should alert the
physician to the possibility of a thigh compartmental syndrome in the
awake and cooperative patient. Pain with passive stretching of the
involved muscles corresponding to the anterior, posterior, and medial
compartments is consistent with the diagnosis. Loss of sensation in the
distribution of the sensory nerves passing through the thigh provides
further evidence. Thigh muscle weakness further supports the diagnosis.
Although it is appreciated that most of these clinical signs are
present in all patients with a femoral shaft fracture, the alerted
physician is obliged to consider the diagnosis of a thigh compartmental
syndrome in any patient with a femur fracture. The use of compartmental
pressure monitoring in the awake patient is usually reserved for
confirmation only because the diagnosis is usually made clinically. In
the unconscious patient, the diagnosis may be more difficult and a high
index of suspicion is similarly required. A tensely swollen thigh can
be evaluated early in the unconscious patient with compartment pressure
monitoring. The threshold for diagnosis in the thigh has not been
firmly established but probably parallels the leg. Exact pressures of
30 or 40 mm Hg or a pressure threshold based on the patient’s diastolic
blood pressure has been suggested.177,250,267
Morbidity was reported in 47% of patients with thigh compartmental
syndrome in one study. Therefore, if the diagnosis is in question or if
pressure monitoring equipment is unavailable to confirm the diagnosis,
one should err on the side of early intervention.
as follows: systemic hypotension, coagulopathy, vascular injury, a
history of external thigh compression, and trauma to the thigh with or
without a fracture of the femur. In their review of 21 thigh
compartmental syndromes, 10 had an associated femur fracture, half of
which were open injuries. This suggests that an open fracture does not
adequately decompress the thigh compartments, similar to the situation
in the tibia. The relationship between intramedullary nailing and the
development of a thigh compartmental syndrome has not been firmly
established. It has been speculated, based on Schwartz and colleagues’
experience with five thigh compartmental syndromes after closed
nailings, that the combination of the decreased thigh volume after
fracture reduction and the normally associated bleeding associated with
the injury is largely responsible.250
The impact of reaming with the associated deposition of additional
volume in the thigh is unknown. However, according to knowledge of
intramedullary nailing of tibia fractures, fracture reduction is
thought to be largely responsible for the increase in pressure.
other ipsilateral extremity fractures after intramedullary nailing of a
femoral shaft fracture has been suggested as a potential cause of a
thigh compartmental syndrome. In the event that multiple procedures are
planned followed intramedullary nailing, a thigh tourniquet should be
avoided to minimize this mitigating circumstance.187
emergency decompressive fasciotomy. As described by several authors,
this can be accomplished through an extensile lateral incision that
gives access to the anterior and posterior compartments. The medial
compartment pressures can then be reassessed to determine whether an
additional medial approach is required. Because of the universally
present significant associated swelling, delayed primary closure or
skin grafting of the fasciotomy is usually delayed for at least 5 days.250,267
femoral shaft fractures. The largest series of antegrade reamed
interlocked nailings report final nonunion rates of 0.9%297 and 1.1%.304 These high rates of union with statically interlocked nails have been confirmed in multiple other studies of femoral
diaphyseal fractures including those with segmental comminution.41,42,256,300,301
However, the incidence of nonunion is probably more frequent than these
reports indicate. In the series of 551 fractures reported by Wolinsky
et al.,304 healing after the index
intramedullary nailing procedure was 94%. In a study of 280 femoral
fractures treated with intramedullary nailing, Pihlajamaki and coauthors221
identified delayed and nonunions that required further surgical
intervention in 12.5%. Although their definition included patients with
no radiographic progression of healing as early as 4 months, the
incidence of further surgery in 35 fractures suggests that delayed and
nonunion may be more common than predicted by some reports.
Injuryrelated risk factors that would be expected to be associated with
an increased incidence of nonunion include the presence of associated
open wounds. However, several studies confirm that open fractures
treated with immediate nailing unite predictably.37,107,239,295
The major identifiable treatment-related risk factor for delayed or
nonunion appears to be treatment with an unreamed intramedullary nail
based on several randomized studies.47,61,277
vascularity, lack of mechanical stability, fracture site distraction,
bone loss, and/or soft tissue interposition. Recently, the use of
anti-inflammatory medications after injury was shown to be a
significant risk factor for delayed and nonunion.100
Impaired vascularity may be related to the initial injury or to the
treatment. Open fractures and excessive soft tissue stripping may
contribute to nonunion by affecting the local bone blood supply.
Mechanical stability may be inadequate if a small nail is used.
Fracture distraction should be avoided to maximize healing. If a
nonunion occurs in a closed fracture treated with an appropriately
sized implant, a metabolic evaluation should be considered to help
identify the underlying cause.
controversial. Most femoral fractures treated with reamed nails heal in
3 to 6 months. In the prospective and randomized study by Tornetta and
Tiburzi,277 union was observed in 80
days in patients treated with reamed nails. In contrast, almost 200
days were reported for union in the series by Clatworthy et al.61
Given the disparity in reported rates of healing, nonunion is probably
best defined by a lack of progression of healing combined with clinical
symptoms of discomfort at a minimum of 6 months from the time of
treatment. Further, nonunion implies that healing is considered
unlikely without further intervention. A broken nail in association
with pain indicates a nonunion.
diaphyseal nonunions that were initially treated with an intramedullary
nail. This includes nail dynamization, exchange nailing, plate
fixations, bone grafting, and combinations thereof. Nail dynamization
is an attractive option for treatment of a femoral nonunion because it
involves the simple removal of one or two interlocking bolts depending
on the nail design and the location of the nonunion. Most current nail
designs have a dynamic slot that limits the potential shortening that
can occur after removal of a single static interlocking screw.
Alternatively, both of the proximal or distal interlocking screws can
be removed in selected cases that are believed to be rotationally
stable and in which significant shortening is not expected. The results
of nail dynamization for the conversion of a femoral nonunion to a
union are questionable. Several large series by experienced surgeons
have demonstrated little effect by routinely dynamizing statically
locked intramedullary nails.42,256,300,301
In a series of 24 patients with statically locked nails, dynamizations
at 4 to 12 months because of delayed healing failed to produce union in
42% of cases. Further, in the 10 cases of persistent nonunion after
dynamization, shortening of greater than 2 cm was present in half of
these patients.309 Nail dynamization in segmental fractures has been reported with similar results.310 In 12 patients who underwent nail dynamization at 5 to 10 months, seven failed to unite and required a bone grafting procedure.310
Although dynamization may be effective in some cases, there is only
retrospective literature suggesting some success in patients who may
have otherwise healed.
by several authors, and mixed results have been reported. Because all
studies reviewing the success of exchange nailing are retrospective,
the types of nonunions, length of time from the initial treatment to
the exchange nailing procedure, and use of bone graft in addition to
nail replacement are all confounding variables.87,113,221,292,294
An early study reported 96% success in treating delayed unions and
nonunions of the femur with reaming and implantation of a larger nail.292 Furlong et al.87
reviewed their success with exchange nailing in 25 patients, almost
half of whom had autologous bone grafting at the same time. Healing was
observed in all but one patient at an average of 30 weeks. Union
occurred more rapidly in patients undergoing a simultaneous bone
grafting procedure. Hak and colleagues113
identified 23 patients treated with reamed intramedullary nails who had
a lack of progression to healing for at least 4 months. The patients
were treated with exchange nailing using an implant with a diameter 1
to 3 mm larger. All eight of the nonsmokers healed after exchange
reamed nailing, whereas only 10 of 15 patients who smoked healed. Their
overall success rate was 78%. Positive intraoperative cultures did not
preclude healing after exchange nailing in five patients. Weresh et al.294
retrospectively reviewed their experience with 19 patients with femoral
nonunions defined as a lack of progressive healing for at least 3
months, clinical signs, and at least 6 months since the initial
treatment. Exchange reamed nailing using an implant at least 2mm larger
in diameter was used as the primary treatment. Supplemental bone
grafting was performed in four patients. Healing was observed in only
53% of patients.
has also been shown to be successful in the management of aseptic
femoral nonunions that have been initially treated with intramedullary
nailing16,283 (Fig. 50-36). Bellabarba and coauthors16
reported their results in treating a consecutive series of 23 patients
with established femoral nonunions. The nonunions were classified as
atrophic in 22%, oligotrophic in 48%, and hypertrophic in 30%. After
nail removal, indirect reduction and plating techniques were used to
correct the deformities and compress the nonunions. Supplemental
autologous bone grafting was used in all of the atrophic nonunions and
in 73% of the oligotrophic nonunions. Healing was observed in 91% of
cases after the initial plating procedure. The two patients with
persistent nonunions healed after a revision plating procedure. The
main disadvantage to this method is the need for a period of protected
weight bearing after the plating procedure. Augmentative plating for
nonunions following intramedullary nailing has been associated with
high success rates and could be considered as another alternative.57,283 Ueng et al. reported 100% union in 17 patients treated with augmentative plating for nonunions
after femoral nailing.57,283
The patients in their series all had persistent rotational instability
after intramedullary nailing, and the plates were applied in attempt to
control this. Early weight bearing was allowed, and bony union was
observed at an average of 7 months after treatment.283
Similarly, in a series of 15 paitents with femoral nonuions following
intramedullary nailing, treatment with plate augmentation and bone
grafting resulted in fracture union in all cases57 (Fig. 50-37).
 |
|
FIGURE 50-36
This 21-year-old man sustained injuries after a motorcycle crash including a distal femoral fracture with an associated sciatic nerve palsy (A,B). The fracture displacement produced vascular embarrassment that was relieved after open reduction of the femur. Retrograde nailing resulted in nonunion at 12 months (C,D), (continues) |
treated with plate fixations are less commonly observed, largely due to
the relative infrequency with which plates are used as a primary
treatment for femoral shaft fractures given the success of
intramedullary devices. The principles for treatment in a previously
plated femoral shaft fracture are similar to that for other diaphyseal
nonunions. Treatment is largely dictated by the combined goals of
achieving mechanical stability in a biologically attractive environment
that maximizes healing. In most cases, removal of the plate and
placement of a reamed intramedullary nail achieves these goals and is
the most reliable method of treatment.80 In a prospective and randomized study of 40 patients
with nonunions following plate fixation, treatment consisted of
interlocked reamed nailing with or without autogenous bone grafting.
Treatment with a reamed nail without bone grafting resulted in similar
results with less operating time and blood loss.80
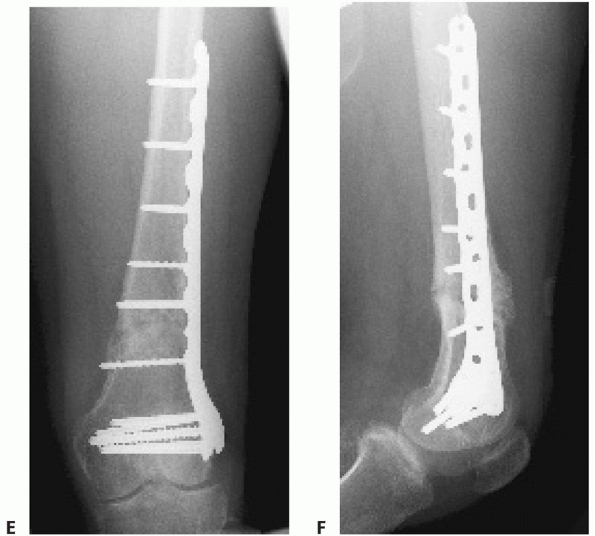 |
|
FIGURE 50-36 (continued) which was treated with compression plating (E,F).
|
femoral shaft fractures. The reported incidence of infection
complicating reamed intramedullary nailing is less than 1% in most
large series.* The reported infection rates in patients
treated with intramedullary nailing for open femoral fractures ranges
from 2.4% to 4.8%.37,164,200,295
The increased infection risk is likely related to the extent of soft
tissue stripping, amount of contamination, and adequacy of debridement.
The diagnosis should be suspected in any patient with a femoral
nonunion, regardless of whether the original injury was open or closed.
intramedullary nailing make the diagnosis fairly obvious. Pain,
swelling, and erythema may be present. More commonly, purulent drainage
is present. This may be located at the site of a previous open wound,
from a sinus tract that has formed in a remote location, at the nail
entry site, or from one of the interlocking screw insertion sites.
Purulent drainage from one of these locations is usually consistent
with a deep infection and not a localized abscess in a coincidental
location. Increasing pain, fevers, or constitutional symptoms may be
present. Further laboratory studies should include a sedimentation rate
and C-reactive protein. These studies may be less important for the
diagnosis than for their value with following treatment in the future.
Plain radiographs should be obtained in an attempt to determine
fracture healing, the stability of the implant, and the presence of any
obvious nonviable bone. Increased density is often consistent with a
sequestrum, whereas periosteal new bone formation may indicate repair
or attempts to heal around a segment of dead bone.
is surgical. All infected and necrotic tissue should be removed, and
the bone should be assessed for viability. This requires an open
surgical approach. Bone viability can be assessed visually or with a
laser Doppler. Any dead or infected tissue should be removed.
Intraoperatively, the stability of the nail should be assessed. If the
implant fits tightly and is providing adequate stability, the nail can
potentially be left in position. Antibiotic selection should be based
on the intraoperative cultures. If adequate stability is present, an
infected femur can heal. After healing, the nail can be removed and the
canal reamed to remove any residual infection.
débridement, the nail should be removed and the canal should be reamed
to remove the contaminated membrane and any residual medullary
purulence. Replacement of the nail is desirable whenever possible.
Fracture (or nonunion) stability must be obtained and maintained during
treatment, because the implant itself is not the source of infection.305
Instead, the infection is likely perpetuated by mechanical and/or
biologic inadequacies. There are several choices for maintaining
stability at this juncture including external fixation, plate fixation,
locked intramedullary nailing, and temporary placement of an antibiotic
nail.13,54,148,207,232,284
External fixation has been used with success after an adequate
intramedullary débridement. In a series of 15 infected femoral
nonunions, Ueng et al.284 presented
a two stage protocol. Initial management consisted of a radical
débridement, local antibiotic bead placement, and external fixation.
The second stage consisted of bead removal, bone grafting, and
continued external fixation. Despite a long period of external
fixation, healing occurred. Barquet et al.13
successfully treated 11 of 13 infected femoral nonunions with a similar
protocol. Alternatively, plate fixation can be used to maintain
stability after nail removal and debridement of the intramedullary and
extramedullary infection. Wave plating with bone grafting was used
successfully to obtain union in 12 of 13 patients with infected
nonunions in a series reported by Ring and colleagues.232
The wave plate was specifically contoured to decrease the contact in
the region of the nonunion and to allow placement of large quantities
of bone graft at the site of the nonunion.
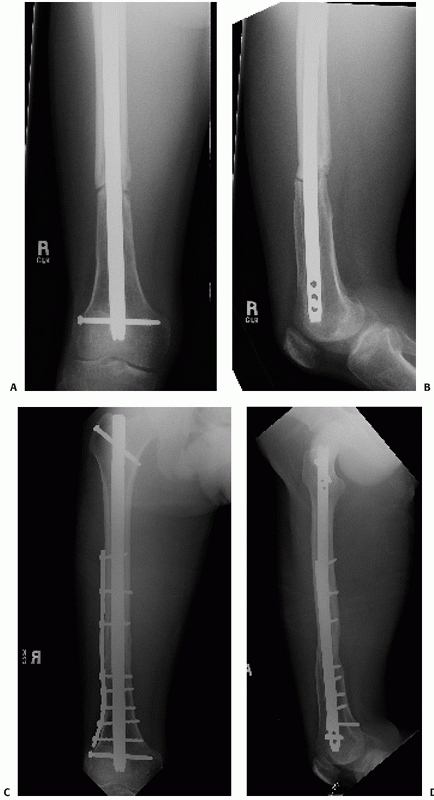 |
|
FIGURE 50-37
This 28-year-old man sustained a femoral shaft fracture following a motor vehicle crash. He underwent exchange nailing using a dynamically locked implant for his aseptic femoral nonunion 1 year following his original injury. Radiographs 6 months later demonstrated persistence of the atrophic nonunion (A,B). Treatment consisted of an open approach, placement of autograft bone obtained from the ipsilateral proximal tibia, and compression plating around the nail. Healing progressed uneventfully as demonstrated at 6 months (C,D). (Case courtesy of Lisa Taitsman, MD, Harborview Medical Center, Seattle, WA.) |
after a thorough debridement of the canal and any associated
devitalized bone has been used successfully to manage infected femoral
nonunions as well.148 In a series of 38 infected femoral pseudarthroses, Klemm148
obtained fracture union in 34 patients after placement of an
interlocking nail. He used a combination of debridement, antibiotic
beads, insertion of an intramedullary nail, and an irrigation system to
successfully treat these infected nonunions. Unlike plating and
external fixation, exchange nailing after reaming allows early weight
bearing. Finally, the use of a temporary antibiotic cement rod was
demonstrated by Paley and Herzenberg.207
They were able to eradicate intramedullary infections in six femurs.
Although four of the infections were caused by transports over nails
and only two were infected pseudarthroses, the local delivery of high
concentrations of antibiotics while maintaining some stability may be
useful and merits further investigation.
evolve. Although statically locked, reamed femoral nailing is generally
accepted as the optimal treatment for the adult with a femoral shaft
fracture; investigations continue to elucidate the appropriateness in
several circumstances. The choice of entry portal for placement of a
femoral nail remains an area of continued study. In fractures of the
femoral shaft, it is unlikely that the actual entry portal has a
significant bearing on healing. More important are the techniques
(reamed versus unreamed) and the biomechanical properties of the
medullary implant. If these are equal, it is unlikely that the rates of
union, malalignment, infection, fat embolism, or compartmental syndrome
will change solely on the basis of the choice of entry portal. The main
advantages of alternative starting points appear to be the technical
ease of identifying the starting point, the potential reduced time of
the procedure, and the reduced radiation exposure. These factors may be
amplified in obese patients. Therefore, the choice to use a starting
point at the greater trochanter, the trochanteric fossa, or the
intercondylar distal femur should be mainly based on the entry site
related complications, the anticipated need for secondary surgical
procedures at those locations, and any relevant patient related
concerns. Continued investigations will hopefully better define the
indications for the use of different starting points for intramedullary
femoral nailing.
nailing has evolved into a viable option for antegrade nailing of
femoral shaft fractures. Although the use of trochanteric entry nails
has been advocated with success for pertrochanteric and subtrochanteric
fractures for more than a decade, their use for femoral shaft fractures
has only recently been advocated. Improvements in implant design and
instrumentation have minimized the size of the entry portal, minimizing
the damage to the abductor insertion. In addition, implant design
changes have reduced the implant related complication of fracture
propagation previously observed with these devices. As the impact of
this entry site for nail placement continues to be better defined, so
will the relative indications.
investigated in an attempt to minimize the radiation exposure and
surgical time associated with this portion of the procedure.
Computer-assisted techniques and external jigs that allow rapid and
predictable placement of interlocking bolts continue to evolve.
orthopaedic procedure, particularly reamed femoral nailing, on the
overall morbidity and mortality of the multiply injured patients
continues to be investigated. Especially critical is the treatment of
patients with an associated head injury, a thoracic injury, or multiple
extremity fractures. Timing of surgical treatment in patients with head
injuries remains poorly understood. The impact of early operative
stabilization to decrease mortality is balanced with the potentially
yet unknown impact of decreased cerebral perfusion in patients who do
not adequately autoregulate or have sustained hypotension. The balance
of early operative intervention of all long bone fractures and “damage
control orthopaedics” in the multiply injured patient, especially those
with associated thoracic trauma, continues to be studied with vigor. It
is expected that the roles of these treatment approaches will be better
defined in the near future.
A. Concurrent ipsilateral fractures of the hip and femoral shaft: a
meta-analysis of 659 cases. Acta Orthop Scand 1996;67:19-28.
A. Concurrent ipsilateral fractures of the hip and shaft of the femur.
A systematic review of 722 cases. Ann Chir Gynaecol 1997;86:326-336.
A, Ekeland A, Stromsoe K. Femoral shaft fractures in the elderly
treated with Grosse-Kempf slotted locked intramedullary nail. Ann Chir
Gynaecol 1992;81: 366-371.
J, Geissler W, Hughes JL. External fixation of femoral fractures.
Indications and limitations. Clin Orthop 1989;241:83-88.
JO, Luber K, Park T. The effect of femoral nailing on cerebral
perfusion pressure in head-injured patients. J Trauma 2003;54:1166-1170.
M, Ogun TC, Oktar MN, et al. Early weight-bearing after statically
locked reamed intramedullary nailing of comminuted femoral fractures:
is it a safe procedure? J Trauma 2001;50:711-716.
M, Ford KR, Wyrick J, et al. A prospective functional outcome and
motion analysis evaluation of the hip abductors after femur fracture
and antegrade nailing. J Orthop Trauma 2008;22:3-9.
TJ, Melton LJ 3rd, Lewallen DG, et al. Epidemiology of diaphyseal and
distal femoral fractures in Rochester, Minnesota. 1965-1984; Clin
Orthop 1988;188-194.
GI, Zacest AC, Paterson DC, et al. Abduction strength following
intramedullary nailing of the femur. J Orthop Trauma 1997;11:93-97.
DP, Schildhauer TA, Nork SE. Noncontiguous fractures of the femoral
neck, femoral shaft, and distal femur. J Trauma 2003;55:80-86.
CJ, Higgins LD. Vascular compromise after insertion of a retrograde
femoral nail: case report and review of the literature. J Orthop Trauma
2002;16:201-204.
A, Silva R, Massaferro J, et al. The AO tubular external fixator in the
treatment of open fractures and infected nonunions of the shaft of the
femur. Injury. 1988;19: 415-420.
SA, Wilson JL, Molnar RR, et al. The incidence of acute
cardiorespiratory and vascular dysfunction following intramedullary
nail fixation of femoral metastasis. Acta Orthop Scand, 2000;71:147-152.
F, Dahlen C, Stiletto R, et al. Technique of using the AO-femoral
distractor for femoral intramedullary nailing. J Orthop Trauma
1994;8:315-321.
C, Ricci WM, Bolhofner BR. Results of indirect reduction and plating of
femoral shaft nonunions after intramedullary nailing. J Orthop Trauma
2001;15: 254-263.
U, Ekbom T, Johnell O, et al. Incidence of femoral and tibial shaft
fractures. Epidemiology 1950-1983 in Malmo, Sweden. Acta Orthop Scand
1990;61:251-254.
SK, Melder I, Henley MB, et al. Closed interlocking nailing of femoral
shaft fractures: assessment of technical complications and functional
outcomes by comparison of a prospective database with retrospective
review. J Orthop Trauma 1993;7: 118-122.
M, Tornetta P, Kerina M, et al. Femur fractures caused by gunshots:
treatment by immediate reamed intramedullary nailing. J Trauma
1993;34:783-785.
M, Guyatt GH, Tong D, et al. Reamed versus nonreamed intramedullary
nailing of lower extremity long bone fractures: a systematic overview
and meta-analysis. J Orthop Trauma 2000;14:2-9.
M, Schemitsch EH. Bone formation following intramedullary femoral
reaming is decreased by indomethacin and antibodies to insulin-like
growth factors. J Orthop Trauma 2002;16:717-722.
LB, Babikian G, Stegemann PM. Femoral canal reaming in the polytrauma
patient with chest injury. A clinical perspective. Clin Orthop
1995;91-94.
LB, Johnson KD, Weigelt J, et al. Early versus delayed stabilization of
femoral fractures. A prospective randomized study. J Bone Joint Surg Am
1989;71:336-340.
LB, McNamara K, Shine B, et al. Mortality in multiple trauma patients
with fractures. J Trauma 1994;37:262-264; discussion 264-265.
MJ, MacKenzie EJ, Riemer BL et al. Adult respiratory distress syndrome,
pneumonia, and mortality following thoracic injury and a femoral
fracture treated either with intramedullary nailing with reaming or
with a plate. A comparative study. J Bone Joint Surg Am
1997;79A:799-809.
BR, Stephen D, Brenneman FD. Thoracic trauma and early intramedullary
nailing of femur fractures: are we doing harm? J Trauma 1997;43:24-28.
AD Jr, Wilber JH. Patterns and complications of femur fractures below
the hip in patients over 65 years of age. J Orthop Trauma
1992;6:167-174.
M, Terjesen T, Rossvoll I. Femoral shaft fractures treated by
intramedullary nailing. A follow-up study focusing on problems related
to the method. Injury 1995; 26:379-383.
M, Terjesen T, Rossvoll I. Torsional deformity after intramedullary
nailing of femoral shaft fractures. Measurement of anteversion angles
in 110 patients. J Bone Joint Surg Br 1993;75:799-803.
JM, Dunkerley DR. Closed nailing of a femoral fracture followed by
sciatic nerve palsy. J Bone Joint Surg Br 1990;72:318.
PL, Miserez MJ, Rommens PM. The monofixator in the primary
stabilization of femoral shaft fractures in multiply-injured patients.
Injury 1992;23:525-528.
GA, Firoozbakhsh K, Summa CD. Potential of increased risk of
neurovascular injury using proximal interlocking screws of retrograde
femoral nails in patients with acetabular fractures. J Orthop Trauma
2001;15:433-437.
BD, Kenzora JE, Edwards CC. The use of modified Neufeld traction in the
management of femoral fractures in polytrauma. J Trauma 1981;21:779-787.
RJ, Ellison PS Jr, Poka A, et al. Intramedullary nailing of open
fractures of the femoral shaft. J Bone Joint Surg Am 1989;71A:1324-1331.
RJ, Ellison TS, Molligan H, et al. Pudendal nerve palsy complicating
intramedullary nailing of the femur. J Bone Joint Surg Am
1992;74A:1450-1455.
RJ, Ellison TS, Poka A, et al. Intramedullary nailing of femoral shaft
fractures. Part III: Long-term effects of static interlocking fixation.
J Bone Joint Surg Am 1992; 74:106-112.
RJ, Reilly JP, Poka A, et al. Intramedullary nailing of femoral shaft
fractures. Part I: Decision-making errors with interlocking fixation. J
Bone Joint Surg Am 1988; 70A:1441-1452.
RJ, Toal TR Jr, Murphy-Zane MS, et al. Immediate weight-bearing after
treatment of a comminuted fracture of the femoral shaft with a
statically locked intramedullary nail. J Bone Joint Surg Am
1999;81A:1538-1544.
RJ, Uwagie-Ero S, Lakatos RP, et al. Intramedullary nailing of femoral
shaft fractures. Part II: Fracture-healing with static interlocking
fixation. J Bone Joint Surg Am 1988;70A:1453-1462.
RJ, Wells JD, Lakatos R, et al. Heterotopic ossification about the hip
after intramedullary nailing for fractures of the femur. J Bone Joint
Surg Am 1990;72A: 1067-1073.
MS, Brumback RJ, Ellison TS, et al. Interlocking intramedullary nailing
for ipsilateral fractures of the femoral shaft and distal part of the
femur. J Bone Joint Surg Am 1991;73A:1492-1502.
M, Mocetti E, Alfie V, et al. Fat embolism and related effects during
reamed and unreamed intramedullary nailing in a pig model. J Orthop
Trauma 2002;16:239-244.
CD, Meek RN, Blachut PA, et al. Intramedullary nailing of the femoral
shaft: a prospective, randomized study. J Orthop Trauma 1992;6:448-451.
Study Group. Nonunion following intramedullary nailing of the femur
with and without reaming. Results of a multicenter randomized clinical
trial. J Bone Joint Surg Am 2003;85A:2093-2096.
Study Group. Reamed versus unreamed intramedullary nailing of the
femur: comparison of the rate of ARDS in multiple injured patients. J
Orthop Trauma 2006; 20:384-387.
LK, Taghizadeh S, Murali J, et al. Retrograde intramedullary nailing in
treatment of bilateral femur fractures. J Orthop Trauma 2008;22:530-534.
DA, Dobozi WR, Rabin S. Peroneal nerve palsy and compartment syndrome
in bilateral femoral fractures. Clin Orthop 1995;115-118.
DW, Rodman GH Jr, Kaehr D, et al. Femur fractures in chest-injured
patients: is reaming contraindicated? J Orthop Trauma 1998;12:164-168.
DB, Moed BR, Kingston C, et al. Identification of the optimal
intercondylar starting point for retrograde femoral nailing: an
anatomical study. J Trauma 2003;55: 692-695.
WE, Fabian TC, Croce MA. Delayed surgical fixation of femur fractures
is a risk factor for pulmonary failure independent of thoracic trauma.
J Trauma 1994;37: 667-672.
YS, Kim KS. Plate augmentation leaving the nail in situ and bone
grafting for non-union of femoral shaft fractures. Int Orthop
2005;29:287-290.
JP, Xenakis T, Papakostides KG, et al. Bridge plating osteosynthesis of
20 comminuted fractures of the femur. Acta Orthop Scand Suppl
1997;275:72-76.
J, Court-Brown C, Kinninmonth AW, et al. Intramedullary locking nails
in the management of femoral shaft fractures. J Bone Joint Surg Br
1988;70B:206-210.
MG, Clark DI, Gray DH, et al. Reamed versus unreamed femoral nails. A
randomised, prospective trial. J Bone Joint Surg Br 1998;80B:485-489.
AS, Hill GA, Theologis TN, et al. Femoral nailing for metastatic
disease of the femur: a comparison of reamed and unreamed femoral
nailing. Injury 2000;31:25-31.
JF, Dehne E, Lafollette B. Closed reduction and early cast-brace
ambulation in the treatment of femoral fractures. II. Results in 143
fractures. J Bone Joint Surg Am 1973;55A:1581-1599.
CE, Mitchell KA, Brumback RJ, et al. Mortality in patients with
bilateral femoral fractures. J Orthop Trauma 1998;12:315-319.
KJ, Beaver RL. Arterial injury during retrograde femoral nailing: a
case report of injury to a branch of the profunda femoris artery. J
Orthop Trauma 2001;15:140-143.
EJ, D’Ambrosia R, Shoji H, et al. Fractures of the femoral shaft
treated by external fixation with the Wagner device. J Bone Joint Surg
Am 1984;66A:360-364.
RH, Riemer BL, Butterfield SL. Ipsilateral femoral neck and shaft
fractures: an overlooked association. Skeletal Radiol 1991;20:251-254.
G, Sjogren S. Postoperative restoration of muscle strength after
intramedullary nailing of fractures of the femoral shaft. Acta Orthop
Scand 1976;47: 101-107.
Campos J, Vangsness CT Jr, Merritt PO, et al. Ipsilateral knee injury
with femoral fracture. Examination under anesthesia and arthroscopic
evaluation. Clin Orthop 1994; 178-182.
DG, Riemer BL, Butterfield SL, et al. Femur fractures with femoral or
popliteal artery injuries in blunt trauma. J Orthop Trauma
1994;8:494-503.
RM, Dainton JN, Hutchins PM. Proximal thigh pain after femoral nailing.
Causes and treatment. J Bone Joint Surg Br 1997;79B:738-741.
C, Leunig M, Beck M, et al. Entry point soft tissue damage in antegrade
femoral nailing: a cadaver study. J Orthop Trauma 2001;15:488-493.
TW, Schutzer SF, Deafenbaugh MK, et al. Compartment syndrome
complicating use of the hemi-lithotomy position during femoral nailing.
A report of two cases. J Bone Joint Surg Am 1989;71A:1556-1557.
PJ, Huckfeldt R, Mullins RJ, et al. The effects of femoral
intramedullary reaming on pulmonary function in a sheep lung model. J
Bone Joint Surg Am 1997; 79A:194-202.
KA, Chang EY, Cvitkovic J, et al. Mismatch of current intramedullary
nails with the anterior bow of the femur. J Orthop Trauma
2004;18:410-415.
AW, Schemitsch EH, Richards RR. Femoral and cruciate blood flow after
retrograde femoral reaming: a canine study using laser Doppler
flowmetry. J Orthop Trauma 1998;12:253-258.
KM, Allam MF. Intramedullary fixation of failed plated femoral
diaphyseal fractures: are bone grafts necessary? J Trauma
2008;65:692-697.
J, Simon-Wiedner R. Die Fixierung der trochanteren Bruche mit runden,
elastichen Codylennagein. Acta Chirurgica, Austriaca, 1970:40.
O, Krettek C, Miclau T, et al. Minimally invasive plate osteosynthesis:
does percutaneous plating disrupt femoral blood supply less than the
traditional technique? J Orthop Trauma 1999;13:401-406.
AJ, Giannoudis PV, Smith RM. Heterotopic ossification: a comparison
between reamed and unreamed femoral nailing. Injury 1997;28:9-14.
MJ, Robertson WJ, Boraiah S, et al. Anatomy of the greater trochanteric
“bald spot”: a potential portal for abductor sparing femoral nailing?
Clin Orthop Relat Res 2008;466:2196-2200.
DJ, Alms M, Cruz MM. Hinged cast and roller traction for fractured
femur. A system of treatment for the Third World. J Bone Joint Surg Br
1985;67B:750-756.
T, Pennig D, Koebke J, et al. Antegrade femoral nailing: an anatomical
determination of the correct entry point. Injury 2002;33:701-705.
WB, Powell TE, Blickenstaff KR, et al. Compression plating of acute
femoral shaft fractures. Orthopedics 1995;18:655-660.
WB, Savoie FH, Culpepper RD, et al. Operative management of ipsilateral
fractures of the hip and femur. J Orthop Trauma 1988;2:297-302.
GM, Burgar AM. Percutaneous skeletal joysticks for closed reduction of
femoral shaft fractures during intramedullary nailing. J Orthop Trauma
2001;15: 570-571.
PV, Furlong AJ, Macdonald DA, et al. Reamed against unreamed nailing of
the femoral diaphysis: a retrospective study of healing time. Injury
1997;28:15-18.
PV, Harwood PJ, Loughenbury P, et al. Correlation Between IL-6 Levels
and the Systemic Inflammatory Response Score: Can an IL-6 Cutoff
Predict a SIRS State? J Trauma 2008;65:646-652.
PV, Hildebrand F, Pape HC. Inflammatory serum markers in patients with
multiple trauma. Can they predict outcome? J Bone Joint Surg Br
2004;86B:313-323.
PV, MacDonald DA, Matthews SJ, et al. Nonunion of the femoral
diaphysis. The influence of reaming and non-steroidal anti-inflammatory
drugs. J Bone Joint Surg Br 2000;82B:655-658.
SK, Yang KY, Koh JS, et al. Subtrochanteric insufficiency fractures in
patients on alendronate therapy: a caution. J Bone Joint Surg Br
2007;89B:349-353.
RJ, Gimbrere JS, van Niekerk JL, et al. Early osteosynthesis and
prophylactic mechanical ventilation in the multitrauma patient. J
Trauma 1982;22:895-903.
T, Hufner T, Hankemeier S, et al. Femoral nail removal should be
restricted in asymptomatic patients. Clin Orthop 2004;222-226.
FA, Graham AJ, Morein G. The management of severely comminuted
fractures of the femoral shaft, using the external fixator. Injury
1985;16:377-381.
RM, Sands KC. Avascular necrosis of the femoral head following
intramedullary nailing of the femur in a skeletally mature young adult:
a case report. Am J Orthop 2008;37:319-322.
A, Trafton PG. Early complications in the management of open femur
fractures: a retrospective study. J Orthop Trauma 1991;5:51-56.
P, DiCicco J, Karpik K, et al. Ipsilateral fractures of the femur and
tibia: treatment with retrograde femoral nailing and unreamed tibial
nailing. J Orthop Trauma 1996;10:309-316.
O, Utvag SE, Reikeras O. Effects of graded reaming on fracture healing.
Blood flow and healing studied in rat femurs. Acta Orthop Scand
1994;65:32-36.
O, Utvag SE, Reikeras O. Restoration of bone flow following fracture
and reaming in rat femora. Acta Orthop Scand 1994;65:185-190.
RB, Anderson JT. Prevention of infection in the treatment of 1025 open
fractures of long bones: retrospective and prospective analyses. J Bone
Joint Surg Am 1976;58A: 453-458.
PD, Bicknell HR Jr, Bronson WE, et al. The use of one compared with two
distal screws in the treatment of femoral shaft fractures with
interlocking intramedullary nailing. A clinical and biomechanical
analysis. J Bone Joint Surg Am 1993;75A: 519-525.
DJ, Lee SS, Goulet JA. Success of exchange reamed intramedullary
nailing for femoral shaft nonunion or delayed union. J Orthop Trauma
2000;14:178-182.
ER, van Meeteren MC, van der Werken C. Improved results in treatment of
femoral shaft fractures with the unreamed femoral nail? A multicenter
experience. J Trauma 1998;45:517-521.
AE. The treatment of femoral fractures by cast-brace application and
early ambulation. A prospective review of one hundred and six patients.
J Bone Joint Surg Am 1983;65:56-65.
PJ, Giannoudis PV, Probst C, et al. The risk of local infective
complications after damage control procedures for femoral shaft
fracture. J Orthop Trauma 2006;20: 181-189.
N, Jando VT, Lu T, et al. Muscle function and functional outcome
following standard antegrade reamed intramedullary nailing of isolated
femoral shaft fractures. J Orthop Trauma 2008;22:10-15.
SL, Trager S, Green S, et al. Management of supracondylar fractures of
the femur with the GSH intramedullary nail: preliminary report. Contemp
Orthop 1991; 22:631-640.
D Jr, Ricci WM, McAndrews P, et al. Treatment of femoral shaft fracture
using unreamed interlocked nails. J Orthop Trauma 2000;14:10-14.
LT, Blue BA. Intraarticular heterotopic ossification in the knee
following intramedullary nailing of the fractured femur using a
retrograde method. J Orthop Trauma 1999;13:385-388.
TM, Aksenov SA, Schemitsch EH. Cortical bone blood flow in loose and
tight fitting locked unreamed intramedullary nailing: a canine
segmental tibia fracture model. J Orthop Trauma 1998;12:127-135.
TM, Aksenov SA, Schemitsch EH. Muscle perfusion after intramedullary
nailing of the canine tibia. J Trauma 1998;45:256-622.
A, Pollak AN, Moehring HD, et al. Removal of intramedullary nails from
the femur: a review of 45 cases. J Orthop Trauma 1996;10:560-562.
WM, Taffet R, DeLong WG Jr, et al. Early exchange intramedullary
nailing of distal femoral fractures with vascular injury initially
stabilized with external fixation. J Trauma 1994;37:446-451.
RL, Bruggeman AW, Pakvis DF, et al. Computed tomography determined
femoral torsion is not accurate. Arch Orthop Trauma Surg
2004;124:552-554.
RL, Ongkiehong BF, Gruneberg C, et al. Compensation for rotational
malalignment after intramedullary nailing for femoral shaft fractures.
An analysis by plantar pressure measurements during gait. Injury
2004;35:1270-1278.
RL, Pakvis DF, Verdonschot N, et al. Rotational malalignment after
intramedullary nailing of femoral fractures. J Orthop Trauma
2004;18:403-409.
DJ, Haidukewych GJ. Management of pathologic fractures of the proximal
femur: state of the art. J Orthop Trauma 2004;18:459-469.
RR, Cohn SM, Moller BA. Early fracture fixation may be deleterious
after head injury. J Trauma 1997;42:1-5; discussion 5-6.
P, Maini L, Mishra P, Upadhyay A, Agarwal A. Cephalomedullary
interlocked nail for ipsilateral hip and femoral shaft fractures.
Injury 2004; 35;1031-1038.
K, Lynch K, Paun M, et al. Noninvasive vascular tests reliably exclude
occult arterial trauma in injured extremities. J Trauma
1991;31:515-519; discussion 519-522.
EE, Marroquin CE, Kossovsky N. Synovial metallosis resulting from
intraarticular intramedullary nailing of a distal femoral nonunion. J
Orthop Trauma 1993;7: 320-324.
KD, Cadambi A, Seibert GB. Incidence of adult respiratory distress
syndrome in patients with multiple musculoskeletal injuries: effect of
early operative stabilization of fractures. J Trauma 1985;25:375-384.
KD, Johnston DW, Parker B. Comminuted femoral-shaft fractures:
treatment by roller traction, cerclage wires, and an intramedullary
nail, or an interlocking intramedullary nail. J Bone Joint Surg Am
1984;66A:1222-1235.
KD, Tencer AF, Sherman MC. Biomechanical factors affecting fracture
stability and femoral bursting in closed intramedullary nailing of
femoral shaft fractures, with illustrative case presentations. J Orthop
Trauma 1987;1:1-11.
W, Lindsey RW, Noble PC, et al. Long-term residual musculoskeletal
deficits after femoral shaft fractures treated with intramedullary
nailing. J Trauma 2000;49: 446-449.
PA, McFerran MA, Johnson KD. Intramedullary nailing of acute femoral
shaft fractures using manual traction without a fracture table. J
Orthop Trauma 1995;9: 57-62.
I, Grosse A, Beck G. Closed locked intramedullary nailing. Its
application to comminuted fractures of the femur. J Bone Joint Surg Am
1985;67:709-720.
SB, Hallfeldt KK, Perren SM, et al. The effects of reaming and
intramedullary nailing on fracture healing. Clin Orthop 1986;18-25.
JJ, Kim E, Kim KY. Predicting the rotationally neutral state of the
femur by comparing the shape of the contralateral lesser trochanter.
Orthopedics 2001;24:1069-1070.
KF, Rush J. Closed intramedullary nailing of femoral shaft fractures. A
review of 112 cases treated by the Kuntscher technique. J Bone Joint
Surg Am 1981;63A: 1319-1323.
Y, Gonze MD, Paul DB, et al. Blunt vascular injury associated with
closed midshaft femur fracture: a plea for concern. J Trauma
1994;36:222-225.
C, Miclau T, Grun O, et al. Intraoperative control of axes, rotation,
and length in femoral and tibial fractures. Technical note. Injury
1998;29(suppl 3):C29-C39.
C, Rudolf J, Schandelmaier P, et al. Unreamed intramedullary nailing of
femoral shaft fractures: operative technique and early clinical
experience with the standard locking option. Injury 1996;27:233-254.
TY, Skedros JG, Bloebaum RD. Measurement of femoral anteversion by
biplane radiography and computed tomography imaging: comparison with an
anatomical reference. Invest Radiol 2003;38:221-229.
EB, Goh SK, Koh JS, et al. An emerging pattern of subtrochanteric
stress fractures: a long-term complication of alendronate therapy?
Injury 2008;39:224-231.
EB, Koh JS, Howe TS. More on atypical fractures of the femoral
diaphysis. N Engl J Med 2008;359:316-317; author reply 317-318.
BA, Lorich DG, Lane JM. Atypical fractures of the femoral diaphysis in
postmenopausal women taking alendronate. N Engl J Med
2008;358:1304-1306.
AS, Wetzler MJ, Guttman G, et al. Treating gunshot femoral shaft
fractures with immediate reamed intramedullary nailing. Orthop Rev
1993;22:805-809.
R, Benjamin JB, Rappaport WD. Blood loss and transfusion in patients
with isolated femur fractures. J Orthop Trauma 1992;6:175-179.
SE, Seligson D, Henry SL. Intramedullary supracondylar nailing of
femoral fractures. A preliminary report of the GSH supracondylar nail.
Clin Orthop 1993;200-206.
F, Wyss A, Brunner C, et al. Plate osteosynthesis of femoral shaft
fractures in adults. A follow-up study. Clin Orthop 1979;62-73.
R, Tricoire JL, Rischmann P, et al. High prevalence of erectile
dysfunction in young male patients after intramedullary femoral
nailing. Urology 2005;65:559-563.
PH, Paley D, Kellam JF. Heterotopic ossification around the hip with
intramedullary nailing of the femur. J Trauma 1988;28:1207-1213.
T, Tornetta P 3rd, Benson E, et al. Gluteus medius tendon injury during
reaming for gamma nail insertion. Clin Orthop 2003;199-202.
MA, Johnson KD. Intramedullary nailing of acute femoral shaft fractures
without a fracture table: technique of using a femoral distractor. J
Orthop Trauma 1992;6:271-278.
MD, Schemitsch EH, Vincent LO, et al. The effect of a femoral fracture
on concomitant closed head injury in patients with multiple injuries. J
Trauma 1997;42: 1041-1045.
RS, White KK, Smith JM, et al. Intramuscular and blood pressures in
legs positioned in the hemilithotomy position: clarification of risk
factors for well-leg acute compartment syndrome. J Bone Joint Surg Am
2002;84A:1829-1835.
R, Renwick SE, DeCoster TA, et al. Removal of intramedullary rods after
femoral shaft fracture. J Orthop Trauma 1992;6:460-463.
AJ, Markley K, Greer RB 3rd. A critical analysis of quadriceps function
after femoral shaft fracture in adults. J Bone Joint Surg Am
1980;62A:61-67.
BR, Watson JT. Retrograde intramedullary nailing, without reaming, of
fractures of the femoral shaft in multiply injured patients. J Bone
Joint Surg Am 1995;77A: 1520-1527.
BR, Watson JT, Cramer KE, et al. Unreamed retrograde intramedullary
nailing of fractures of the femoral shaft. J Orthop Trauma
1998;12:334-342.
CM, Verhofstad MH, Bleys RL, et al. Soft tissue injury related to
choice of entry point in antegrade femoral nailing: piriform fossa or
greater trochanter tip. Injury 2005; 36:1337-1342.
V, Nickel VL, Harvey JP Jr, et al. Cast-brace treatment for fractures
of the distal part of the femur. A prospective controlled study of 150
patients. J Bone Joint Surg Am 1970;52A:1563-1578.
MR, Garfin SR, Hargens AR. Compartment syndrome of the thigh
complicating surgical treatment of ipsilateral femur and ankle
fractures. J Orthop Trauma 1987;1: 71-73.
TJ, Harwin C, Green SA, et al. The results of quadricepsplasty on knee
motion following femoral fractures. J Trauma 1987;27:49-51.
CG, Gibson MJ, Cross AT. Intramedullary locking nails for femoral shaft
fractures in elderly patients. J Bone Joint Surg Br 1990;72B:19-22.
E, Ostrum RF, DiCicco J, et al. Effects of retrograde femoral
intramedullary nailing on the patellofemoral articulation. J Orthop
Trauma 1999;13:13-16.
SJ, Hurley D, Agudelo JF, et al. Retrograde femoral nailing: an
understanding of the intercondylar insertion site. J Trauma
2008;64:151-154.
JR, Smith RM, Pape HC, et al. Stimulation of the local femoral
inflammatory response to fracture and intramedullary reaming: a
preliminary study of the source of the second hit phenomenon. J Bone
Joint Surg Br 2008;90B:393-399.
R, Segal D, Wollstein R, et al. Midshaft femoral fracture, concomitant
ipsilateral hip joint injury, and disruption of the knee extensor
mechanism: a unique triad of dashboard injury. Am J Orthop
1998;27:465-473.
CA, Schavan R, Frigg R, et al. Intramedullary pressure increase for
different commercial and experimental reaming systems: an experimental
investigation. J Orthop Trauma 1998;12:540-546.
EJ, Siebenrock K, Ekkernkamp A, et al. Ipsilateral fractures of the
pelvis and the femur—floating hip? A retrospective analysis of 42
cases. Arch Orthop Trauma Surg 1999;119(3-4):179-182.
AS, Lane JM, Lenart BA, et al. Low-energy femoral shaft fractures
associated with alendronate use. J Orthop Trauma 2008;22:346-350.
SE, Agel J, Russell GV, et al. Mortality after reamed intramedullary
nailing of bilateral femur fractures. Clin Orthop 2003;272-278.
P, Brumback RJ. Immediate interlocking nailing of fractures of the
femur caused by low- to mid-velocity gunshots. J Orthop Trauma
1994;8:134-141.
PJ, Turen CH, Brumback RJ, et al. Conversion of external fixation to
intramedullary nailing for fractures of the shaft of the femur in
multiply injured patients. J Bone Joint Surg Am 2000;82A:781-788.
RF, Agarwal A, Lakatos R, et al. Prospective comparison of retrograde
and antegrade femoral intramedullary nailing. J Orthop Trauma
2000;14:496-501.
RF, DiCicco J, Lakatos R, et al. Retrograde intramedullary nailing of
femoral diaphyseal fractures. J Orthop Trauma 1998;12:464-468.
RF, Levy MS. Penetration of the distal femoral anterior cortex during
intramedullary nailing for subtrochanteric fractures: a report of three
cases. J Orthop Trauma 2005;19:656-660.
RF, Marcantonio A, Marburger R. A critical analysis of the eccentric
starting point for trochanteric intramedullary femoral nailing. J
Orthop Trauma 2005;19: 681-686.
RF, Verghese GB, Santner TJ. The lack of association between femoral
shaft fractures and hypotensive shock. J Orthop Trauma 1993;7:338-342.
MH, Basarir K, Bayramoglu A, et al. Risk of superior gluteal nerve and
gluteus medius muscle injury during femoral nail insertion. J Bone
Joint Surg Am 2007;89A: 829-834.
D, Herzenberg JE. Intramedullary infections treated with antibiotic
cement rods: preliminary results in nine cases. J Orthop Trauma
2002;16:723-729.
SA, Shepherd L, Babourda EC, et al. Piriform and trochanteric fossae. A
drawing mismatch or a terminology error? A review. Surg Radiol Anat
2005;27: 223-226.
HC, Auf’m’Kolk M, Paffrath T, et al. Primary intramedullary femur
fixation in multiple trauma patients with associated lung contusion—a
cause of posttraumatic ARDS? J Trauma 1993;34:540-547; discussion
547-548.
HC, Dwenger A, Grotz M, et al. Does the reamer type influence the
degree of lung dysfunction after femoral nailing following severe
trauma? An animal study. J Orthop Trauma 1994;8:300-309.
HC, Dwenger A, Regel G, et al. Pulmonary damage after intramedullary
femoral nailing in traumatized sheep: is there an effect from different
nailing methods? J Trauma 1992;33:574-581.
HC, Giannoudis PV, Grimme K, et al. Effects of intramedullary femoral
fracture fixation: what is the impact of experimental studies in
regards to the clinical knowledge? Shock 2002;18:291-300.
HC, Grimme K, Van Griensven M, et al. Impact of intramedullary
instrumentation versus damage control for femoral fractures on
immunoinflammatory parameters: prospective randomized analysis by the
EPOFF Study Group. J Trauma 2003;55:7-13.
HC, Hildebrand F, Pertschy S, et al. Changes in the management of
femoral shaft fractures in polytrauma patients: from early total care
to damage control orthopedic surgery. J Trauma 2002;53:452-461;
discussion 461-462.
HC, Regel G, Dwenger A, et al. Influences of different methods of
intramedullary femoral nailing on lung function in patients with
multiple trauma. J Trauma 1993;35: 709-716.
HC, Rixen D, Morley J, et al. Impact of the method of initial
stabilization for femoral shaft fractures in patients with multiple
injuries at risk for complications (borderline patients). Ann Surg
2007;246:491-499; discussion 499-501.
RD, Harrow ME, Banks DM, et al. Comparison of mechanical loads produced
by current intramedullary reamer systems. J Orthop Trauma
1998;12:531-539.
AC, Christie J, Keating JF, et al. The detection of fat embolism by
transoesophageal echocardiography during reamed intramedullary nailing.
A study of 24 patients with femoral and tibial fractures. J Bone Joint
Surg Br 1993;75B:921-925.
EA, Jahangir AA, Mashru RP, et al. Is there a gluteus medius tendon
injury during reaming through a modified medial trochanteric portal? A
cadaver study. J Orthop Trauma 2007;21:617-620.
HK, Salminen ST, Bostman OM. The treatment of nonunions following
intramedullary nailing of femoral shaft fractures. J Orthop Trauma
2002;16:394-402.
A, Little K, Chappell A. Osteonecrosis of the femoral head following
medullary nailing of the femur in an adult. Acta Orthop Belg
2007;73:258-262.
IL, McCarthy ID, Hughes SP. The acute vascular response to
intramedullary reaming. Microsphere estimation of blood flow in the
intact ovine tibia. J Bone Joint Surg Br 1995;77B:490-493.
PA, Broos PL. Healing of closed femoral shaft fractures treated with
the AO unreamed femoral nail. A comparative study with the AO reamed
femoral nail. Injury 2000;31:367-371.
FW. The normal microcirculation of diaphyseal cortex and its response
to fracture. J Bone Joint Surg Am 1968;50A:784-800.
WM, Bellabarba C, Evanoff B, et al. Retrograde versus antegrade nailing
of femoral shaft fractures. J Orthop Trauma 2001;15:161-169.
WM, Bellabarba C, Lewis R, et al. Angular malalignment after
intramedullary nailing of femoral shaft fractures. J Orthop Trauma
2001;15:90-95.
WM, Schwappach J, Tucker M, et al. Trochanteric versus piriformis entry
portal for the treatment of femoral shaft fractures. J Orthop Trauma
2006;20:663-667.
BL, Butterfield SL, Burke CJ 3rd, et al. Immediate plate fixation of
highly comminuted femoral diaphyseal fractures in blunt polytrauma
patients. Orthopedics 1992;15:907-916.
BL, Butterfield SL, Ray RL, et al. Clandestine femoral neck fractures
with ipsilateral diaphyseal fractures. J Orthop Trauma 1993;7:443-449.
J, Tornetta P 3rd, Ritter C, et al. Neurologic and vascular structures
at risk during anterior-posterior locking of retrograde femoral nails.
J Orthop Trauma 1998;12: 379-381.
D, Jupiter JB, Sanders RA, et al. Complex nonunion of fractures of the
femoral shaft treated by wave-plate osteosynthesis. J Bone Joint Surg
Br 1997;79B:289-294.
EB, von Bonsdorff H, Hakkinen S, et al. Prevention of fat embolism by
early internal fixation of fractures in patients with multiple
injuries. Injury 1976;8:110-116.
B, Bengtson S, Herrlin K, et al. External fixation of femoral
fractures: experience with 15 cases. J Orthop Trauma 1990;4:70-74.
AG, Fitzpatrick CB. Closed Kuntscher nailing of femoral shaft
fractures. A series of 100 consecutive patients. J Bone Joint Surg Br
1978;60B:504-509.
TP, Luscher JN. Results after internal fixation of comminuted fractures
of the femoral shaft with DC plates. Clin Orthop 1979;74-76.
S, Pihlajamaki H, Avikainen V, et al. Specific features associated with
femoral shaft fractures caused by low-energy trauma. J Trauma
1997;43:117-122.
ST, Pihlajamaki HK, Avikainen VJ, et al. Population based epidemiologic
and morphologic study of femoral shaft fractures. Clin Orthop
2000;241-249.
BJ, Ryan JR, Salciccioli GG. Prophylactic femoral stabilization with
the Zickel nail by closed technique. J Bone Joint Surg Am
1986;68A:991-999.
C, Sartoretti-Schefer S, Ruckert R, et al. Comorbid conditions in old
patients with femur fractures. J Trauma 1997;43:570-577.
TM, Boswell SA, Scott JD, et al. External fixation as a bridge to
intramedullary nailing for patients with multiple injuries and with
femur fractures: damage control orthopedics. J Trauma 2000;48:613-621;
discussion 621-623.
T, Krallis P, Descamps PY, et al. The femoral supracondylar nail:
preliminary experience. Acta Orthop Belg 1998;64:385-392.
EH, Kowalski MJ, Swiontkowski MF, et al. Cortical bone blood flow in
reamed and unreamed locked intramedullary nailing: a fractured tibia
model in sheep. J Orthop Trauma 1994;8:373-382.
EH, Turchin DC, Kowalski MJ, et al. Quantitative assessment of bone
injury and repair after reamed and unreamed locked intramedullary
nailing. J Trauma 1998; 45:250-255.
JT Jr, Brumback RJ, Lakatos R, et al. Acute compartment syndrome of the
thigh. A spectrum of injury. J Bone Joint Surg Am 1989;71A:392-400.
JC, Gupta SP, Mathur NC, et al. Comminuted femoral shaft fractures
treated by closed intramedullary nailing and functional cast bracing. J
Trauma 1993;34:786-791.
TE, Gruen GS, DiTano O, et al. Ipsilateral proximal and shaft femoral
fractures: spectrum of injury involving the femoral neck. Injury
1997;28:293-297.
PT, Chapman JR, Selznick HS, et al. Iatrogenic fractures of the femoral
neck during closed nailing of the femoral shaft. J Bone Joint Surg Br
1994;76B:293-296.
JO, Eiskjaer S, Moller-Larsen F. Locked nailing of comminuted and
unstable fractures of the femur. J Bone Joint Surg Br 1990;72B:23-25.
DJ, Kreder HJ, Schemitsch EH, et al. Femoral intramedullary nailing:
comparison of fracture-table and manual traction. a prospective,
randomized study. J Bone Joint Surg Am 2002;84A:1514-1521.
K, Dieter U, Stachowiak G, et al. Biomechanical testing of the LCP—how
can stability in locked internal fixators be controlled? Injury
2003;34(suppl 2):B11-B19.
K, Stachowiak G, Forster T, et al. Oblique screws at the plate ends
increase the fixation strength in synthetic bone test medium. J Orthop
Trauma 2004;18:611-6.
MF, Hansen ST Jr, Kellam J. Ipsilateral fractures of the femoral neck
and shaft. A treatment protocol. J Bone Joint Surg Am 1984;66A:260-268.
RC, Manning J, Lampard S, et al. Early intramedullary nailing of
femoral shaft fractures: a cause of fat embolism syndrome. Am J Surg
1983;146:107-111.
V, Pepe MD, Glaser DL, et al. Well-leg compartment pressures during
hemilithotomy position for fracture fixation. J Orthop Trauma
2000;14:157-161.
SD, Achterman CA, Hayhurst J, et al. Acute compartment syndrome in the
thigh complicating fracture of the femur. A report of three cases. J
Bone Joint Surg Am 1986;68A:1439-1443.
NC, Park S, Iesaka K, et al. The effect of locked distal screws in
retrograde nailing of osteoporotic distal femur fractures: a laboratory
study using cadaver femurs. J Orthop Trauma 2005;19:380-383.
AF, Kaufman R, Ryan K, et al. Femur fractures in relatively low-speed
frontal crashes: the possible role of muscle forces. Accid Anal Prev
2002;34:1-11.
AF, Sherman MC, Johnson KD. Biomechanical factors affecting fracture
stability and femoral bursting in closed intramedullary rod fixation of
femur fractures. J Biomech Eng 1985;107:104-111.
AD, Morgan-Jones RL, Spencer-Jones R. Intramedullary femoral nailing:
removing the nail improves subjective outcome. Injury 2002;33:247-249.
P 3rd, Kain MS, Creevy WR. Diagnosis of femoral neck fractures in
patients with a femoral shaft fracture. Improvement with a standard
protocol. J Bone Joint Surg Am 2007;89A:39-43.
P 3rd, Ritz G, Kantor A. Femoral torsion after interlocked nailing of
unstable femoral fractures. J Trauma 1995;38:213-219.
P 3rd, Tiburzi D. Antegrade or retrograde reamed femoral nailing. A
prospective, randomised trial. J Bone Joint Surg Br 2000;82B:652-654.
P 3rd, Tiburzi D. Anterograde interlocked nailing of distal femoral
fractures after gunshot wounds. J Orthop Trauma 1994;8:220-227.
P 3rd, Tiburzi D. The treatment of femoral shaft fractures using
intramedullary interlocked nails with and without intramedullary
reaming: a preliminary report. J Orthop Trauma 1997;11:89-92.
P, Bonenberger EG, Reynolds F. Retrograde femoral nail placement:
quantiifying the limits of knee flexion and extension. Presented at the
Orthopaedic Trauma Association Annual Meeting, 2002.
P, Kain M, Brown D. Antegrade versus retrograde femoral nailing: a
prospective randomized evaluation. Presented at the Orthopaedic Trauma
Association Annual Meeting, 2004.
RN, Lheureau T, Protech J, et al. Timing fracture repair in patients
with severe brain injury (Glasgow Coma Scale score <9). J Trauma
1998;44:977-982; discussion 982-983.
MC, Schwappach JR, Leighton RK, et al. Results of femoral
intramedullary nailing in patients who are obese versus those who are
not obese: a prospective multicenter comparison study. J Orthop Trauma
2007;21:523-529.
SW, Chao EK, Lee SS, et al. Augmentative plate fixation for the
management of femoral nonunion after intramedullary nailing. J Trauma
1997;43:640-644.
SW, Wei FC, Shih CH. Management of femoral diaphyseal infected nonunion
with antibiotic beads local therapy, external skeletal fixation, and
staged bone grafting. J Trauma 1999;46:97-103.
der Made WJ, Smit EJ, van Luyt PA, et al. Intramedullary femoral
osteosynthesis: an additional cause of ARDS in multiply injured
patients? Injury 1996;27:391-393.
Riet YE, van der Werken C, Marti RK. Subfascial plate fixation of
comminuted diaphyseal femoral fractures: a report of three cases
utilizing biological osteosynthesis. J Orthop Trauma 1997;11:57-60.
CT Jr, DeCampos J, Merritt PO, et al. Meniscal injury associated with
femoral shaft fractures. An arthroscopic evaluation of incidence. J
Bone Joint Surg Br 1993; 75B:207-209.
MC, Temkin NR, Deyo RA, et al. Timing of surgery after multisystem
injury with traumatic brain injury: effect on neuropsychological and
functional outcome. J Trauma 2007;62:1250-1258.
JJ. The Judet quadricepsplasty for management of severe posttraumatic
extension contracture of the knee. A report of a bilateral case and
review of the literature. Clin Orthop Relat Res 1990;169-173.
LX, Gristina AG, Fowler HL. Unstable femoral shaft fractures: a
comparison of interlocking nailing versus traction and casting methods.
J Orthop Trauma 1988;2: 10-12.
LX, Winquist RA, Hansen ST. Intramedullary nailing and reaming for
delayed union or nonunion of the femoral shaft. A report of 105
consecutive cases. Clin Orthop 1986;133-141.
K, Runkel M, Degreif J, et al. Minimally invasive plate fixation in
femoral shaft fractures. Injury 1997;28(suppl 1):A13-A19.
MJ, Hakanson R, Stover MD, et al. Failure of exchange reamed
intramedullary nails for ununited femoral shaft fractures. J Orthop
Trauma 2000;14:335-338.
MM, Askins V, Hinkes EW, et al. Primary reamed intramedullary nailing
of open femoral shaft fractures. Clin Orthop 1995;182-190.
RA, Hansen ST. Segmental fractures of the femur treated by closed
intramedullary nailing. J Bone Joint Surg Am 1978;60A:934-939.
RA, Hansen ST Jr. Comminuted fractures of the femoral shaft treated by
intramedullary nailing. Othop Clin North Am 1980;11:633-647.
RA, Hansen ST Jr, Clawson DK. Closed intramedullary nailing of femoral
fractures. A report of 520 cases. J Bone Joint Surg Am 1984;66A:529-539.
DA, Brien WW, Becker V Jr. Interlocking nailing for the treatment of
femoral fractures due to gunshot wounds. J Bone Joint Surg Am
1991;73A:598-606.
DA, Brien WW, Stetson WB. Interlocked nailing for treatment of
segmental fractures of the femur. J Bone Joint Surg Am 1990;72A:724-728.
DA, Fleming CH, Matta JM, et al. Comminuted and rotationally unstable
fractures of the femur treated with an interlocking nail. Clin Orthop
1986;35-47.
PR, Banit D, Parker RE, et al. Reamed intramedullary femoral nailing
after induction of an “ARDS-like” state in sheep: effect on clinically
applicable markers of pulmonary function. J Orthop Trauma
1998;12:169-175; discussion 175-176.
P, Slack R, Harvey L, et al. The prevention of infection in open
fractures: an experimental study of the effect of fracture stability.
Injury 1994;25:31-38.
GE, Simon P, Redl H, et al. Intramedullary pressure changes and fat
intravasation during intramedullary nailing: an experimental study in
sheep. J Trauma 1994; 36:202-207.
GE, Thurnher M, Redl H, et al. Pulmonary reaction during intramedullary
fracture management in traumatic shock: an experimental study. J Trauma
1994;37: 249-254.
DG, Levin JS, Esterhai JL, et al. Immediate internal fixation of
low-velocity gunshot-related femoral fractures. J Trauma
1993;35:678-681; discussion 681-682.
CC. The effect of dynamization on slowing the healing of femur shaft
fractures after interlocking nailing. J Trauma 1997;43:263-267.
CC, Chen WJ. Healing of 56 segmental femoral shaft fractures after
locked nailing. Poor results of dynamization. Acta Orthop Scand
1997;68:537-540.
CC, Shih CH, Chen LH. Femoral shaft fractures complicated by
fracture-dislocations of the ipsilateral hip. J Trauma 1993;34:70-75.
KH, Han DY, Jahng JS, et al. Prevention of malrotation deformity in
femoral shaft fracture. J Orthop Trauma 1998;12:558-562.
KH, Han DY, Park HW, et al. Fracture of the ipsilateral neck of the
femur in shaft nailing. The role of CT in diagnosis. J Bone Joint Surg
Br 1998;80B:673-678.
RE, Fietti VG Jr, Lawsing JF, et al. A new intramedullary fixation
device for the distal third of the femur. Clin Orthop 1977;185-191.
M, Vogt D, Cole PA, et al. Plating of femoral shaft fractures: open
reduction and internal fixation versus submuscular fixation. J Trauma
2007;63:1061-1065.
