Monteggia Fracture-Dislocation in Children
injury usually involving a fracture of the ulna and dislocation of the
radial head. Unfortunately, despite considerable published awareness of
the risk of failure to diagnose this injury,* Monteggia
fracture-dislocations are still missed acutely by qualified
radiologists, emergency room physicians, and orthopaedic surgeons
amongst others. In addition to failure to recognize the injury pattern,
undertreatment of unstable, acute injuries has also resulted in chronic
Monteggia lesions.30,34,44,53,59,67,71,74,108,110,111,144 A chronic Monteggia lesion is far more complex in terms of surgical decision making and management than an acute injury.18,26,29,39,46,57,63,78,113,117
public health official in Milan, Italy, described a variation of the
injury in 1814 that now bears his name as “a traumatic lesion
distinguished by a fracture of the proximal third of the ulna and an
anterior dislocation of the proximal epiphysis of the radius.”106 In 1967, Jose Luis Bado,8,9
while director of the Orthopedic and Traumatology Institute in
Montevideo, Uruguay, published his classic monograph on classification
of Monteggia lesions. Bado8,9
described a Monteggia lesion as a radial head fracture or dislocation
in association with a fracture of the middle or proximal ulna. For the
last century, numerous authors have made significant contributions on
pathoanatomy, classification, diagnosis, treatment, and complications.* Despite these advances, pediatric Monteggia lesions can still be problematic.
 |
|
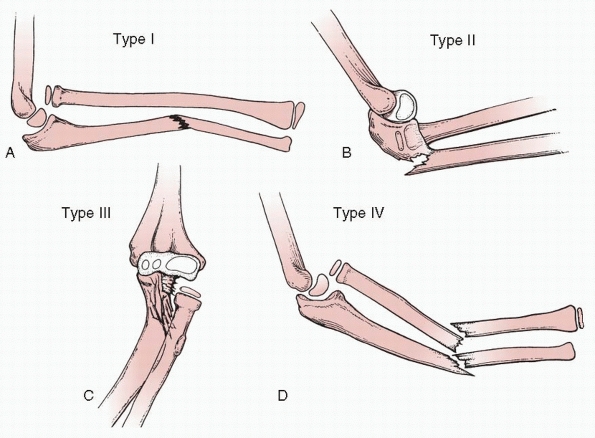
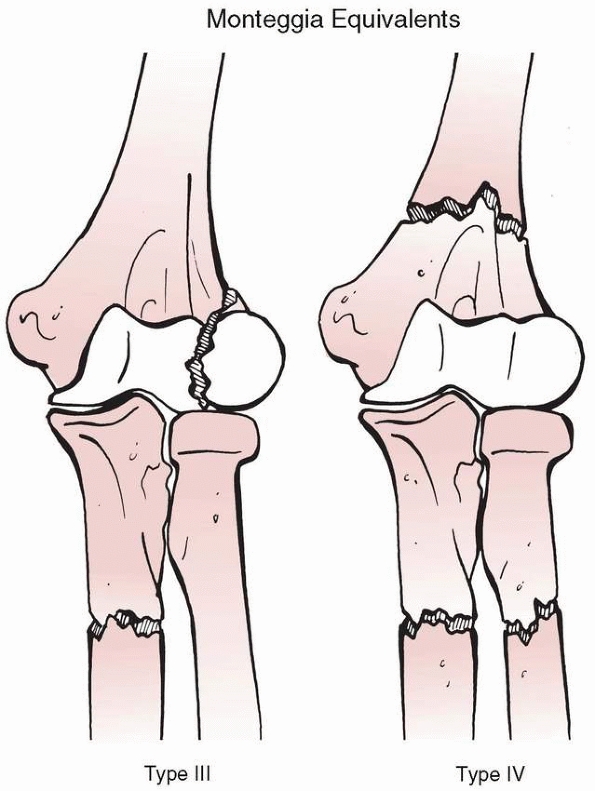
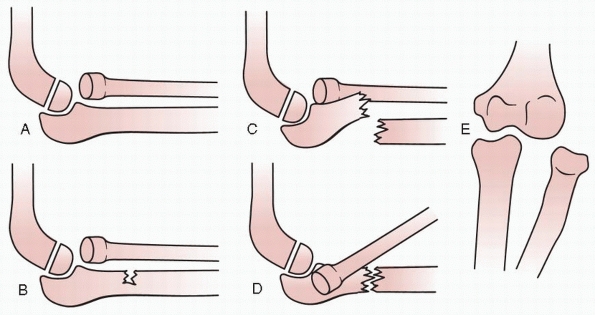
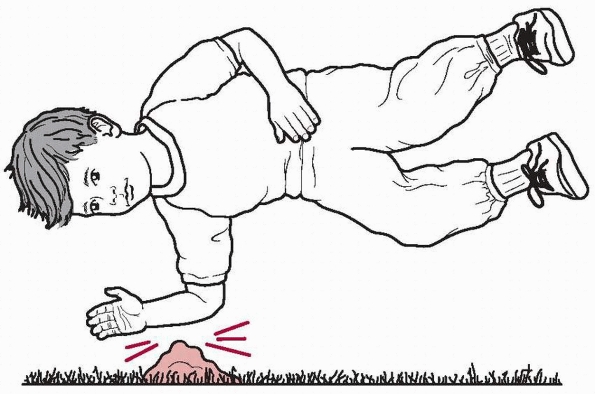
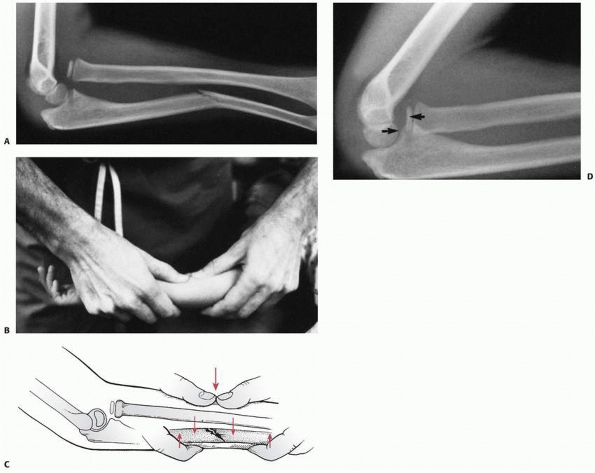
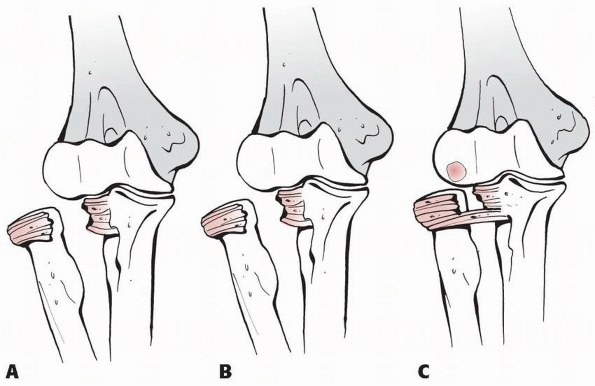
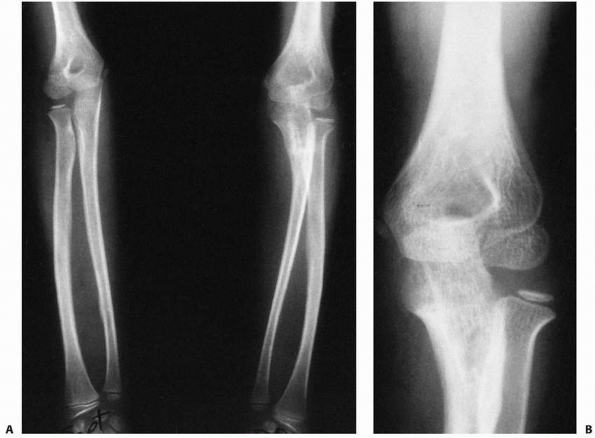
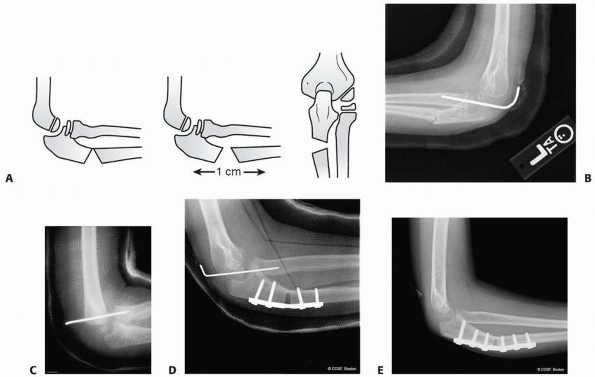
FIGURE 12-1 Bado classification. A.
Type I (anterior dislocation): the radial head is dislocated anteriorly and the ulna has a short oblique or greenstick fracture in the diaphyseal or proximal metaphyseal area. B. Type II (posterior dislocation): the radial head is posteriorly and posterolaterally dislocated; the ulna is usually fractured in the metaphysis in children. C. Type III (lateral dislocation): there is lateral dislocation of the radial head with a greenstick metaphyseal fracture of the ulna. D. Type IV (anterior dislocation with radius shaft fracture): the pattern of injury is the same as with a type I injury, with the inclusion of a radius shaft fracture below the level of the ulnar fracture. |
head associated with an ulnar diaphyseal fracture at any level. This is
the most common Monteggia lesion in children.34,49,75,111
radial head associated with an ulnar diaphyseal or metaphyseal
fracture. This is the most common lesion in adults but very rare in
children.97,98,111
head associated with an ulnar metaphyseal fracture. This is the second
most common pediatric Monteggia lesion.13,44,91,95,143
When associated with an olecranon fracture and a lateral or
anterolateral radiocapitellar dislocation but no radioulnar
dissociation, the injury is not a true Monteggia lesion.60,110,134
the ulna and the radius. The original description was of a radial
fracture at the same level or distal to the ulna fracture. This, too,
is a relatively rare injury.
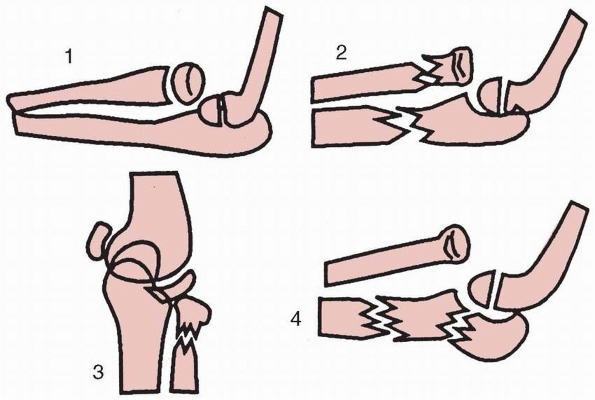
classified certain injuries as equivalents to his true Monteggia
lesions because of their similar mechanisms of injury, radiographic
appearance, or treatment methods. Since his publication, the list of
equivalent lesions has expanded case report by case report (Fig. 12-2).
dislocations of the radial head without ulnar fracture. This
subclassification includes a “pulled elbow” or “nursemaid’s elbow”
because the mechanism of longitudinal traction, pronation, and
hyperextension is similar to a true type I Monteggia lesion. In this
situation, the radiographs are normal. In addition, an isolated
anterior dislocation of the radial head without ulnar fracture is a
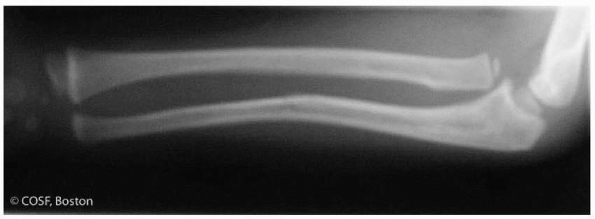
type I equivalent. The ulnar bow sign (Fig. 12-3)
is normal. Subtle plastic deformation of the ulna will have a concave
ulnar bow and could be misdiagnosed as an equivalent lesion when it is
really a true type I lesion. This distinction can be critical in terms
of operative decisions in that the rare but true type I equivalent
lesion requires only open repair of the displaced ligament while the
type I lesion with plastic deformation requires correction of the ulnar
deformity. Other type I equivalencies described thus far include:
anterior dislocation of the radial head with ulnar diaphyseal and
radial neck fractures, anterior dislocation of the radial head with
radial diaphyseal fracture more proximal to ulnar diaphyseal fracture,
anterior radial head dislocation with ulnotrochlear dislocation (Fig. 12-4),111 and anterior dislocation of the radial head with segmental ulna fracture.2.49,60,102,115,134
More case reports will probably expand this subclassification. The type
I equivalent lesions have been shown to have poorer outcomes and
require more operative interventions than other Monteggia lesions.49,91
for subclassification, case reports have emerged over time to include
fractures of the distal humerus (supracondylar, lateral condylar) in
association with proximal forearm fractures (Fig. 12-5).*
 |
|
FIGURE 12-2 Type I Monteggia equivalents. I. Isolated anterior radial head dislocation. II. Ulnar fracture with fracture of the radial neck. III. Isolated radial neck fractures. IV. Elbow (ulnohumeral) dislocation with or without fracture of the proximal radius.
|
classified pediatric Monteggia fracture-dislocations both on direction
of radial head dislocation and type of ulnar fracture. Letts types A,
B, and C were various ulnar fractures associated with anterior
dislocation of the radial head, or Bado type I injuries. A type A is a
plastic deformation fracture; a type B is an incomplete or greenstick
fracture; a type C is a complete fracture of the ulna. Type D injuries
were the same as Bado II or posterior radial head dislocation, and type
E the same as Bado III or lateral radial head dislocations (Fig. 12-6).
defined a Monteggia lesion as a proximal radioulnar joint dislocation
in association with a forearm fracture. It is the character of the
ulnar fracture, more so than the direction of the radial head
dislocation, that is most useful in determining the optimal treatment
of Monteggia fracture-dislocations in both adults and children. Stable
anatomic reduction of the ulnar fracture almost always results in
anatomic, stable reduction of the proximal radius, proximal radioulnar
joint, and radiocapitellar joint in the acute setting. The ulnar
fracture is defined similarly to all pediatric forearm fractures:
plastic deformation, incomplete or greenstick fractures, and complete
fractures. Complete fractures are further subdivided into transverse,
short oblique, long oblique, and comminuted fractures. Treatment
directly relates to the fracture type: closed reduction for plastic
deformation and greenstick fractures, intramedullary fixation for
transverse and short oblique fractures, and open reduction and internal
fixation with plate and screws for long oblique and comminuted
fractures (Table 12-1).
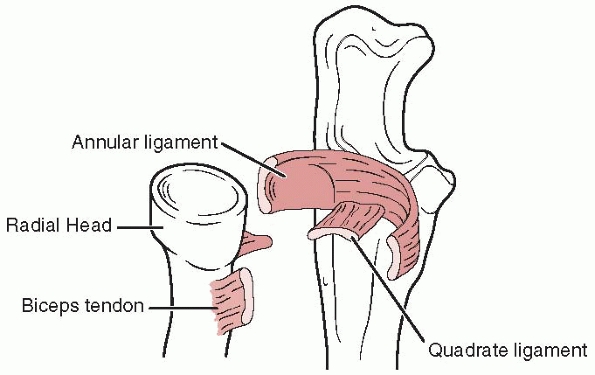
joint, radiocapitellar joint, and proximal forearm is critical to
understanding the treatment of acute and chronic Monteggia lesions. The
ligaments, bony architecture, and joint contours provide stability to
the proximal forearm and elbow. The muscle insertions and origins
affect stability and determine surgical exposure along with neighboring
neurovascular structures.
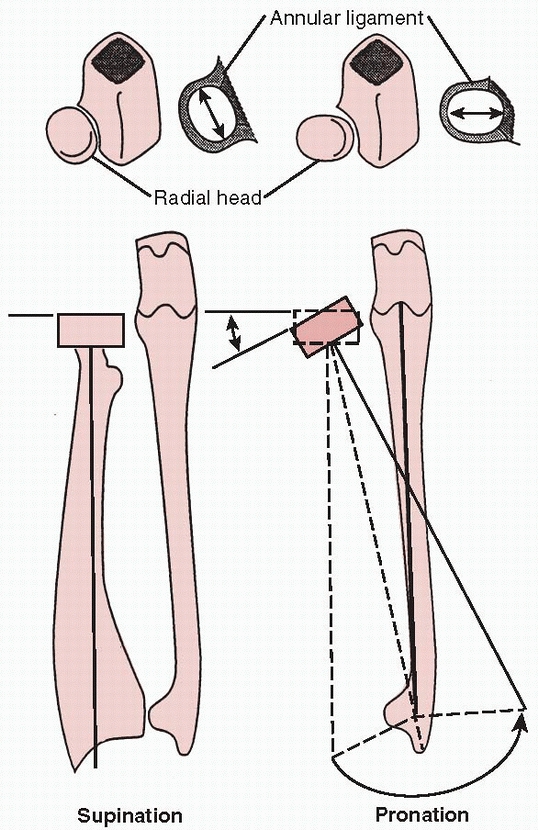
the proximal radioulnar joint during forearm rotation. It surrounds the
radial neck from its origin and insertion on the proximal ulna (Fig. 12-7).
Due to the shape of the radial head, it tightens in supination. It is
part of the lateral collateral ligamentous complex that stabilizes the
distal humerus and proximal forearm. Displacement of the annular
ligament occurs in a Monteggia lesion.
thinner central portion. The quadrate ligament also provides stability
to the proximal radioulnar joint during forearm rotation. The anterior
and posterior borders become taut at the extremes of supination and
pronation respectively.
 |
|
FIGURE 12-3
The ulnar bow line. This line, drawn between the distal ulna and the olecranon, defines the ulna bow. The ulnar bow sign is deviation of the ulnar border from the reference line of more than 1 mm. |
 |
|
FIGURE 12-4 Type I Monteggia equivalent that includes elbow subluxation in addition to the radioulnar dislocation.
|
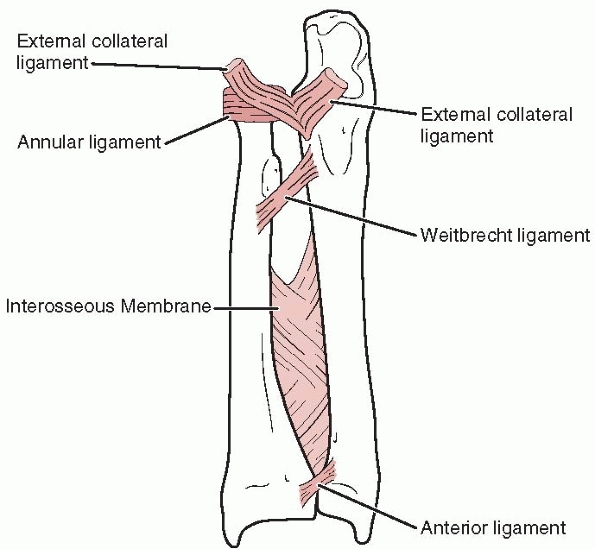
The origin of the oblique ligament is just distal to the radial notch
of the ulna, and its insertion is just distal to the bicipital
tuberosity of the radius. With supination, the oblique ligament
tightens and provides further stability to the proximal radioulnar
joint.
 |
|
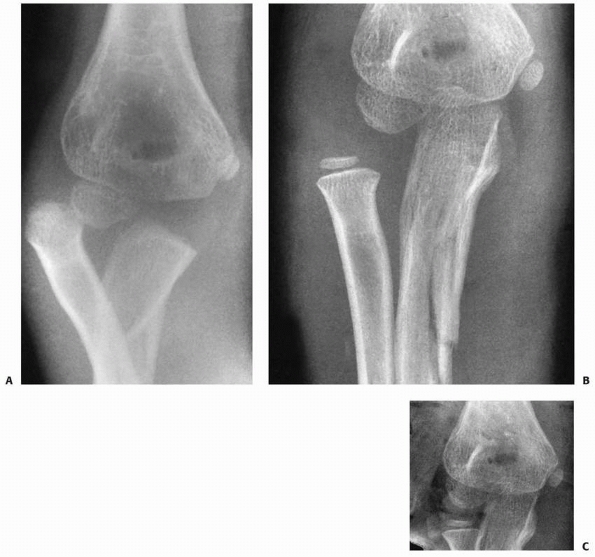
FIGURE 12-5 Type III equivalent described by Ravessoud107:
an oblique fracture of the ulna with varus alignment and a displaced lateral condylar fracture. Type IV equivalent described by Arazi5: fractures of the distal humerus, ulnar diaphysis, and radial neck. |
ligament with its fibers running in the opposite direction (from radius
proximally to ulna distally) to the oblique ligament (see Fig. 12-8).
However, similar to the oblique ligament, it tightens in supination and
provides further stability to the proximal radioulnar joint.
In supination, the long axis of the ellipse is perpendicular to the
proximal ulna, causing the annular ligament and the anterior portion of
the quadrate ligament to tighten and stabilize the proximal radioulnar
joint. In addition, the contact area between the radius and the radial
notch of the ulna increases in supination due to the broadened surface
of the elliptical radial head proximal to distal in that position. This
may provide some additional stability.
anatomic bow in order to achieve full forearm rotation while
maintaining stability in the proximal and distal radioulnar joints (see
Fig. 12-9). With the radius in supination, the
bow tightens the oblique and interosseous ligaments, thereby increasing
proximal radioulnar joint stability.
radius and acts as both a flexor of the elbow and supinator of the
forearm. It is a deforming force in anterior Monteggia
fracture-dislocations, pulling the radius anteriorly as the elbow is
forcibly extended. In treatment, care is taken to maintain the elbow in
flexion to prevent recurrent anterior subluxation of the radial head
while the soft tissues heal.
 |
|
FIGURE 12-6 Pediatric Monteggia fracture classification by Letts et al.75 A. Anterior dislocation of the radial head with plastic deformation of the ulna. B. Anterior dislocation of the radial head with greenstick fracture of the ulna. C. Complete fracture of the ulna with anterior dislocation of the radial head. D. Posterior dislocation of the radial head with fracture of the ulnar metaphysis. E. Lateral dislocation of the radial head and metaphyseal greenstick fracture of the ulna.
|
elbow joint by providing a valgus moment at the joint during extension
and pronation.11,139
It may also act as a deforming force, along with the forearm flexors,
on complete fractures of the ulna in a Monteggia lesion. Surgical
exposure of the proximal radioulnar and radiocapitellar joints is
usually through the anconeus-extensor carpi ulnaris interval.
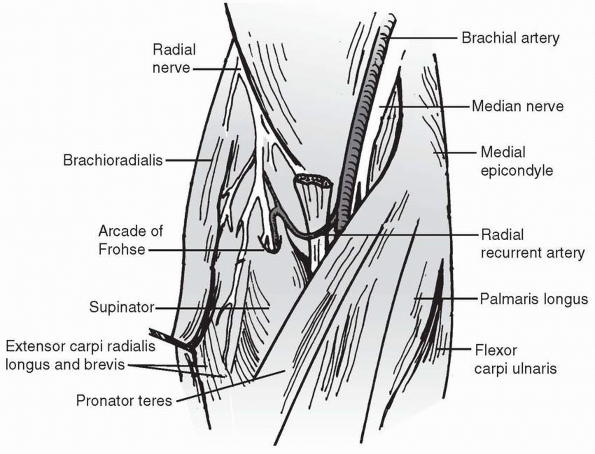
As it descends into the forearm, it divides into the radial sensory
nerve and the posterior interosseous motor branch. The posterior
interosseous nerve passes between the two heads of the supinator, when
present, or beneath the supinator when there is only one head of
supinator. Its close proximity to the proximal radial head and neck
makes it susceptible to injury with Monteggia lesions.67
In chronic Monteggia situations, the posterior interosseous nerve can
become adherent to the dislocated head or, less commonly, entrapped in
the joint.113 Care must be taken with the nerve in surgical reconstructions of the chronic anterior dislocation.
|
TABLE 12-1 Author’s Classification of Monteggia Fracture-Dislocations
|
|||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||
intermuscular septum of the humerus, through the cubital tunnel behind
the medial epicondyle, and then through the flexor carpi ulnaris into
the forearm. It is at risk for injury with type II laterally displaced
Monteggia lesions and with ulnar lengthening in chronic Monteggia
reconstructions.
fusiform swelling about the elbow. The child has significant pain and
has limitations of elbow motion in flexion and extension as well as
pronation and supination. Usually, an angular change in the forearm
itself is evident, with the apex shifted anteriorly and mild valgus
apparent. There may be tenting of the skin or an area of ecchymosis on
the volar aspect of the forearm. It is imperative to check for an open
fracture wound. The child may not be able to extend the digits at the
metacarpophalangeal joint or at the interphalangeal joint of the thumb
because of a paresis of the posterior interosseous nerve. Later, as the
swelling subsides, anterior fullness may remain in the cubital fossa
for the typical Bado type I anterior dislocation. However, this may be
subtle since children will usually have an elbow flexion posture
postinjury. If the injury is seen late, there will be a loss of full
flexion at the elbow and a palpable anterior dislocation of the radial
head. The radial head-distal humerus impingement that occurs may be a
source of pain with activities. There is usually loss of forearm
rotation with late presentation. Progressive valgus may occur if the
anterior radial head dislocation worsens. Lateral dislocations will
generally have a varus bow to the forearm both with acute and chronic
presentations. The laterally displaced radial head will be visible and
palpable.
 |
|
FIGURE 12-7 Ligamentous anatomy of the proximal radioulnar joint.
|
 |
|
FIGURE 12-8
Ligaments of the forearm. In supination, the annular ligament, quadrate ligament, oblique ligament, and interosseous membrane are taut, stabilizing the radial head. |
 |
|
FIGURE 12-9
The radial head is an elliptical structure secured by the annular ligament, which allows movement and gives stability. Because of the shape of the radial head, the stability provided by the annular ligament is maximized in supination. |
includes anteroposterior (AP) and lateral radiographs of the forearm.
Any disruption of the ulna, including subtle changes in ulnar bowing,
should alert the clinician to look for joint disruption at either end
of the forearm.27,28,65,67,77 Unfortunately, the dislocated radial head is all too often missed in the acute setting.
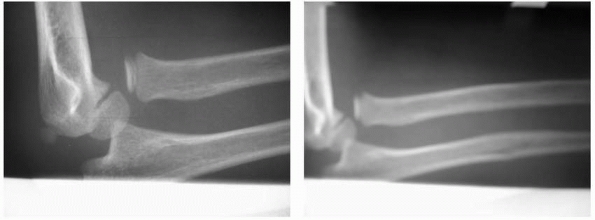
capitellum is particularly important and is best defined by a true
lateral view of the elbow. In a type I Monteggia fracture-dislocation,
the radiocapitellar relationship may appear normal on an AP radiograph
despite obvious disruption on the lateral view (Fig. 12-11). If there is doubt regarding the radiocapitellar alignment, further radiographic evaluation must be obtained. Smith118 and later Storen128
noted that a line drawn through the center of the radial neck and head
should extend directly through the center of the capitellum. This
alignment should remain intact regardless of the degree of flexion or
extension of the elbow (Fig. 12-12). In some instances, there is disruption of the radiocapitellar line in a normal elbow. Miles and Finlay84
pointed out that the radiocapitellar line passes through the center of
the capitellum only on a true lateral projection. They reported five
patients in whom the elbow was clinically normal but the
radiocapitellar line appeared disrupted. In analyzing the radiographs,
they found that the radiographic projection of the elbow was usually an
oblique view or that the forearm was pronated in the radiograph. If
this disruption appears on radiographs in a child with an acute injury,
however, it is the treating surgeon’s responsibility to ensure that it
is an insignificant finding. As Dr. John Hall55
often said, “Monteggia lesions are not like throwing horse shoes; being
close does not count.” It is still too frequent an occurrence that a
highly qualified, distraught, orthopaedic surgeon will call for
referral of a chronic Monteggia lesion that was missed acutely.
magnetic resonance imaging (MRI) scan may be useful to determine the
congruency of the radial head and capitellum. If the radial head is no
longer centrally concave or the capitellum is no
longer symmetrically convex, surgical reduction may fail or produce pain and limited motion.
 |
|
FIGURE 12-10 Dissection of the forearm at the level of the elbow.
|
radiocapitellar relation is disrupted radiographically, evaluation of
the shape of the radial head and neck helps determine the cause of the
disruption, especially if there is no history of trauma or the
significance of the trauma is questioned. Bucknill23 suggested that McFarland’s81
classic description of congenital radial head dislocation with an
atypical deformed radial head, dysplastic capitellum, concavity of the
posterior border of the proximal ulna, and periarticular ossifications
probably represented old traumatic dislocations. Lloyd-Roberts and
Bucknill78 noted that many
unilateral anterior dislocations were most likely old traumatic
dislocations rather than congenital dislocations. Caravias24
recognized that the existence of a congenital anterior dislocation as a
separate entity was doubtful and that true anterior congenital
dislocation of the radial head was rare. True congenital dislocations
are usually posterior, may be bilateral, and can be associated with
various syndromes such as Ehlers-Danlos, nail-patella, and Silver
syndromes (Fig. 12-13).3,78
Therefore, all isolated anterior and anterolateral dislocations of the
radial head, regardless of symptoms, should be suspected as having a
traumatic origin unless there is evidence of congenital or systemic
differences, such as proximal radioulnar synostosis.
 |
|
FIGURE 12-11 The AP view (A) demonstrates an apparently located radial head, but the lateral view (B) shows an anterior dislocation of the radial head. Note the disruption of the radiocapitellar line.
|
 |
|
FIGURE 12-12
Composite drawing with the elbow in various degrees of flexion. A line drawn down the long axis of the radius bisects the capitellum of the humerus regardless of the degree of flexion or extension of the elbow. |
who noted that the fracture occurs when a direct blow on the posterior
aspect of the forearm first produces a fracture through the ulna. Then,
either by continued deformation or direct pressure, the radial head is
forced anteriorly with respect to the capitellum, causing the radial
head to dislocate. Monteggia99 explained that these injuries sometimes resulted from a blow by a staff or cudgel on the forearm raised to protect the head.
fracture-dislocation, has been mentioned in the literature. During the
American Civil War, Monteggia fractures were frequent because of direct
blows on the forearm received while attempting to parry the butt of a
rifle during hand-to-hand combat. The major argument against this
theory as the mechanism is that in the usual clinical situation there
rarely is evidence of a direct blow to the posterior aspect of the
forearm, such as a contusion or laceration.38,139
published his observations regarding anterior Monteggia fractures.
Previous investigators had based their direct blow theory on hypothesis
and clinical observation, but Evans38
used cadaver experiments to support his hypothesis. He demonstrated
that hyperpronation of the forearm produced a fracture of the ulna with
a subsequent dislocation of the radial head. He postulated that during
a fall, the outstretched hand, initially in pronation, is forced into
further pronation as the body twists above the planted hand and forearm
(Fig. 12-15). This hyperpronation causes the
radius to be crossed over the midulna, resulting in anterior
dislocation of the radial head or fracture of the proximal third of the
radius along with fracture of the ulna. In the patients reported in
Evans’38 article, the ulnar
fractures demonstrated a pattern consistent with anterior tension and
shear or longitudinal compression. His cadaver studies, however, showed
the ulna fracture pattern to be consistent with a spiral or torsional
force. This theory was also supported by Bado.10
First, the ulnar fracture rarely presents clinically in a spiral
pattern; it is often oblique, indicating an initial force in tension
with propagation in shear rather than rotation. Second, Evans’38
experiments, which were done on totally dissected forearms, did not
take into consideration the dynamic muscle forces at play during a fall
on an outstretched hand.
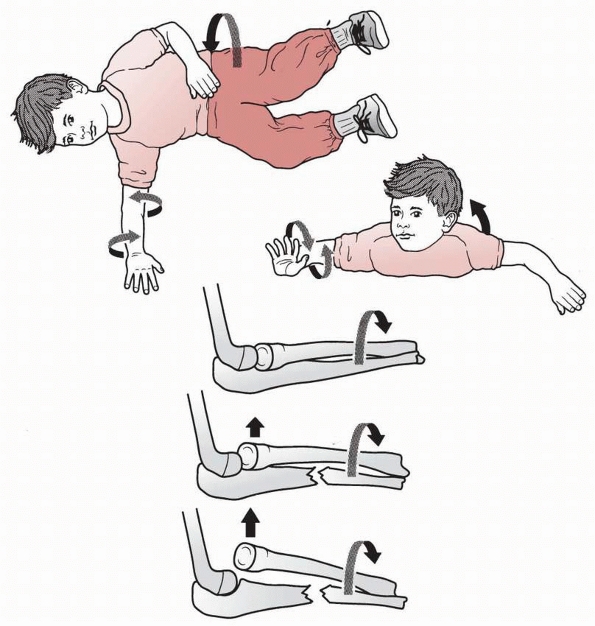
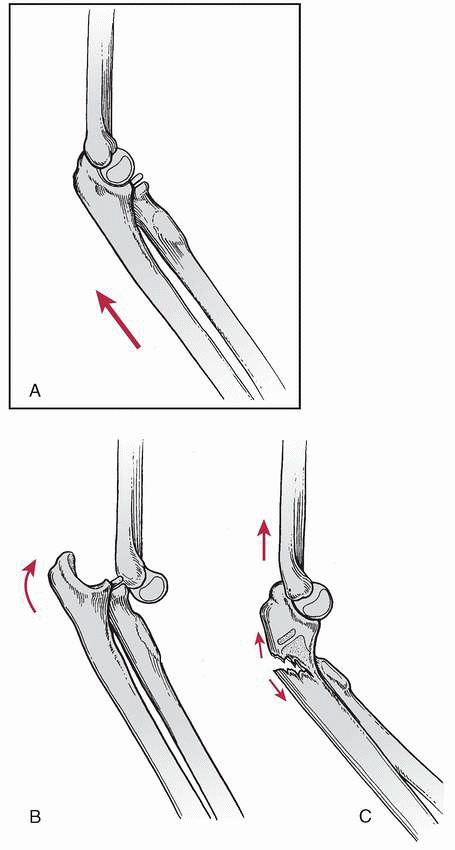
analyzed both theories and presented good clinical evidence that type I
Monteggia fractures were caused by a combination of dynamic and static
forces. His study postulated three steps in the fracture mechanism:
hyperextension, radial head dislocation, and ulnar fracture (Fig. 12-16).
The patient falls on an outstretched arm with forward momentum, forcing
the elbow joint into hyperextension. The radius is first dislocated
anteriorly by the violent reflexive contracture of the biceps, forcing
the radius away from the capitellum. Once the proximal radius
dislocates, the weight of the body is transferred to the ulna. Because
the radius is usually the main load-bearing bone in the forearm, the
ulna cannot handle the transmitted longitudinal force and weight and,
subsequently, fails in tension. This tension force produces an oblique
fracture line or a greenstick fracture in the ulnar diaphysis or
diaphyseal-metaphyseal junction. In addition to the momentum of the
injury, the anterior angulation of the ulna results from the pull of
the intact interosseous membrane on the distal fragment, causing it to
follow the radius. The brachialis muscle causes the proximal ulnar
fragment to flex at the elbow.
the three proposed mechanisms, but the most common mechanism is a fall
on an outstretched hand that forces the elbow into complete extension,
locking the olecranon into the humerus. The forearm is in a rotational
position of neutral to midpronation. As the proximal ulna locks into
the distal humerus, the bending force stresses the proximal radioulnar
joint. Because of the relatively pronated position of the joint, the
ligamentous restraints are lax, providing only tenuous stability for
the radial head. The anterior bending force, combined with a reflexive
contraction of the biceps, violently dislocates the radial head
anteriorly. The radioulnar joint and its ligamentous complex are at
risk because of the ligamentous laxity and the decreased contact area
between the proximal radius and ulna created by the rotation of the
forearm. At midrotation, the short axis of the elliptical radial head
is perpendicular to the ulna, causing the annular ligament and the
dense anterior portion of the quadrate ligament to be relaxed. The
contact area of the proximal radioulnar joint, because of the shape of
the radial head, is also decreased, further reducing the stability of
the joint. The ulna, now the main weight-bearing structure of the
forearm, is loaded by a continued bending moment, causing tension on
the anterior cortex and producing failure. The force at the site of
failure is propagated in shear at approximately 45 degrees to the long
axis
of the ulna. This mechanism may produce plastic deformation with an
anterior bow, a greenstick fracture, or an oblique fracture pattern,
all of which are seen clinically. As the anterior bending movement
continues, the vector of the biceps changes and acts as a tether and
resists any further advance of the proximal radius. The distal fragment
of the ulna continues to advance, acting as a fulcrum against the
radial shaft. The anteriorly directed force of the distal ulnar
fragment, combined with the retrograde resistance of the biceps, may
create a fracture of the radius, or a type IV Monteggia lesion.
 |
|
FIGURE 12-13 Congenital versus traumatic dislocation. A. AP view of the elbow of a 7-year-old who presented with limited forearm rotation. B.
Lateral radiograph of the same child. Note dysplastic radial head, anterior dislocation, and a hypoplastic capitellum. This is congenital. C. AP radiograph of congenital synostosis. D. Lateral radiograph of congenital synostosis and posterior dislocation. Note posterior bow of the ulna and hypoplasia of the capitellum. This is also congenital. |
based their treatment choices on the type of ulnar fracture rather than
on the Bado type. Plastic deformation of the ulna is treated with
closed reduction of the ulnar bow to obtain stable reduction of the
radioulnar joint. Incomplete (greenstick or buckle) fractures of the
ulna are similarly treated with closed reduction and casting. Most
Monteggia injuries that are plastic deformation or greenstick fractures
in children are stable when immobilized in 100
to 110 degrees of flexion and full supination. In all series,4,9,21,22,34,44,75,91,108,113,118,143
anterior Monteggia lesions in children have uniformly good results when
treated by manipulative closed reduction, if the radial head is
properly aligned and the ulna fracture is reduced with length
preserved. These results most clearly apply to plastic deformation and
incomplete fractures, which make up the majority of anterior Monteggia
lesions. However, complete fractures can be unstable after closed
reduction. Therefore, with complete short oblique and transverse ulna
fractures or ones associated with a radial fracture (type IV),
intramedullary Kirschner wire (K-wire) fixation is recommended. At
times, this may involve use of the intramedullary K-wire in the
proximal fragment to joystick the reduction under fluoroscopic
guidance. Long oblique or comminuted fractures, which may develop
shortening and malalignment even with intramedullary fixation, are best
stabilized with plate and screw fixation. Using this treatment
protocol, Ring and Waters111 reported excellent results in all 28 patients treated within 24 hours of injury (Table 12-2). Poor results occurred in two patients who were referred late with persistent radial head dislocations.
 |
|
FIGURE 12-14
The fracture-dislocation is sustained by direct contact on the posterior aspect of the forearm, either by falling onto an object or by the object striking the forearm. The continued motion of the object forward dislocates the radial head after fracturing the ulna. |
 |
|
FIGURE 12-15 Hyperpronation theory (Evans).38
Rotation of the body externally forces the forearm into pronation. The ulnar shaft fractures with further rotation, forcibly dislocating the radial head. |
 |
|
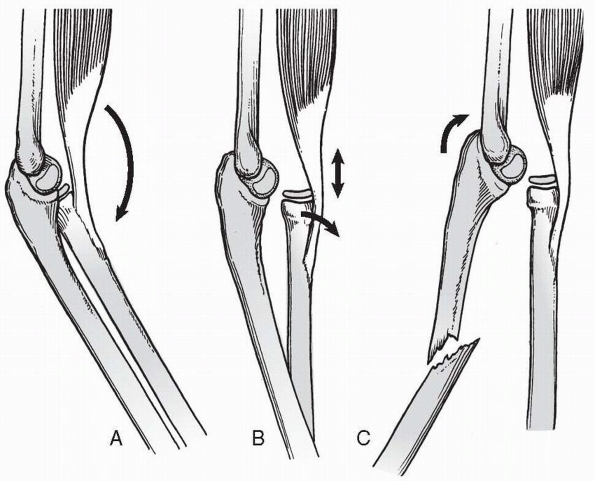
FIGURE 12-16 Hyperextension theory. A. Hyperextension: forward momentum caused by a fall on an outstretched hand forces the elbow into extension. B. Radial head dislocation: the biceps contracts, forcibly dislocating the radial head. C. Ulnar fracture: forward momentum causes the ulna to fracture because of tension on the anterior surface.
|
three steps: correcting the ulnar deformity, providing a stable
reduction of the radial head, and maintaining ulnar length and fracture
stability (Fig. 12-17). For plastic deformation
and incomplete fractures, this can usually be achieved with closed
reduction and cast immobilization. For complete fractures, fracture
instability after closed reduction may lead to
loss of anatomic ulnar length and redislocation of the radial head.
|
TABLE 12-2 Treatment of Monteggia Fracture-Dislocations in Children According to Ulnar Injury
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||
 |
|
FIGURE 12-17 Reduction of a type I Monteggia fracture-dislocation.
|
The first step is to re-establish the length of the ulna by
longitudinal traction and manual correction of any angular deformity.
The forearm is held in relaxed supination as longitudinal traction is
applied with manual pressure directed over the apex of the deformity
until the malangulation is corrected clinically and radiographically (Fig. 12-18).
With plastic deformation fractures, this may necessitate significant
force that requires general anesthesia. With greenstick fractures, the
correction of the ulnar deformity and radial head reduction can often
be achieved with conscious sedation in the emergency room.
Monteggia lesions (defined as maintenance of the radial head reduction)
with nonanatomic alignment of the ulnar fracture (Fig. 12-19).44,103,105 However, anatomic reduction and healing of the ulna fracture is strongly advocated.
Once ulnar length and alignment have been reestablished, the radial
head can be relocated. This is often accomplished by simply flexing the
elbow to 90 degrees or more, thus producing spontaneous reduction (see Fig. 12-19).
Occasionally, posteriorly directed pressure over the anterior aspect of
the radial head is necessary for reduction of the radial head. Flexion
of the elbow to 110 to 120 degrees stabilizes the reduction. Once the
radial head position is established, it should be scrutinized
radiographically in numerous views to ensure a concentric reduction.
With a type I fracture, the optimal radiographic view is a true lateral
of the elbow with the forearm held in supination. The longitudinal axis
of the radius should pass directly through the center of the capitellum
(Fig. 12-20).
Once the concentric reduction of the radial head is confirmed, the
elbow should be placed at approximately 110 to 120 degrees of flexion
to alleviate the force of the biceps, which could redislocate the
radial head (see Figs. 12-20 and 12-21).
The forearm is placed in a position of midsupination to neutral
rotation to alleviate the forces of the supinator muscle and the
anconeus, as well as the forearm flexors, which tend to produce radial
angulation of the ulna.
fracture is reduced and the neutralization position is established, a
molded long-arm splint or cast is applied to hold the elbow joint in
the appropriate amount of flexion, usually 110 to 120 degrees. Once the
cast is completed, careful radiographic assessment should establish the
concentric reduction of the radial head with respect to the capitellum,
as well as satisfactory alignment of the ulna.
patient is followed at 7 to 10 day intervals to confirm continued
satisfactory reduction by radiography. At 4 to 6 weeks after the
initial reduction, if there is radiographic evidence of consolidation
of the ulnar fracture and stability of the radial head, the long-arm
cast can be removed, with progressive guarded return to full activity.
indications for operative treatment of type I fracture-dislocations:
failure to obtain and maintain ulnar fracture reduction and failure of
radial head reduction. The fractures most at risk are complete ulnar
fractures. On rare occasions, there will be an entrapped annular
ligament that prevents anatomic radial head reduction.
If the ulnar fracture cannot be reduced or held in satisfactory
alignment by closed treatment, operative intervention is indicated. The
quality of the ulnar reduction affects the ability to reduce the radial
head, which is of primary importance. If the ulnar fracture can be
reduced but not maintained because of the obliquity of the fracture,
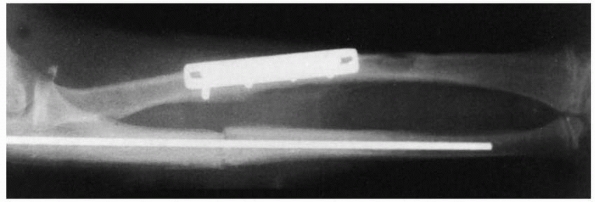
internal fixation is indicated.44,91 Intramedullary fixation is standard in most series of Monteggia fracture-dislocations in children (Fig. 12-22).8,9,34,43,44,72,74,79,91,104,111,114,128,143
This method of fixation can be accomplished percutaneously, using image
intensification and flexible nails or K-wires. Entry can be through the
apophysis or proximal metaphysis of the ulna, depending on the level of
the fracture and surgeon’s preference. Intramedullary fixation is
preferred for transverse and short oblique fractures. Long oblique and
comminuted fractures may redisplace even with intramedullary fixation.
Plate and screw fixation is preferred with these rarer fractures.74,96,101,136,140,145
The second indication is failure to reduce the radial head
satisfactorily by closed means. This is more common in type III
Monteggia lesions, but it can also occur in type I lesions. It results
from soft tissue interposition, including entrapped capsule or an
orbicular ligament pulled over the radial head.139,145 Interposed cartilaginous or
osteochondral fractures (Fig. 12-23) in the radiocapitellar joint or proximal radioulnar joint may also prevent complete reduction of the radial head.139 Morris86
described a patient in whom reduction of the radial head was obstructed
by radial nerve entrapment between the radial head and ulna.
 |
|
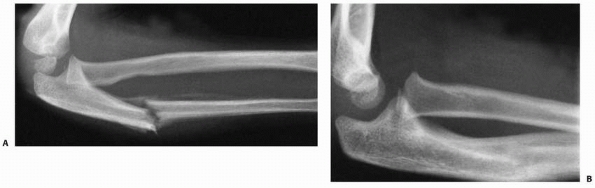
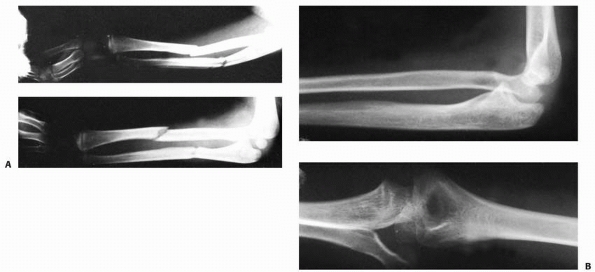
FIGURE 12-18 Closed reduction, type I lesion. A. Typical type I lesion in a 7-year-old. B.
Correction of plastic deformation. Plastic deformation of the ulna must be corrected to prevent recurrence of the angular deformity. C. This allows reduction of the radial head and prevents its late subluxation. (From Wilkins KE, ed. Operative Management of Upper Extremity Fractures in Children. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1994, with permission.) D. The deformity of the ulna is corrected first, and then the elbow is hyperflexed. However, the radial head is still anteriorly subluxed (arrows), and the ulna still has some anterior plastic deformation. This is not acceptable. |
 |
|
FIGURE 12-19 A. Malaligned ulnar fracture with radial head reduced. B. Subsequent apex posterior angulation healing of ulna fracture while maintaining radial head reduction.
|
 |
|
FIGURE 12-20
Reduction of the radial head. Flexing the elbow spontaneously reduces the radial head. Occasionally, manual pressure is required in combination with flexion. |
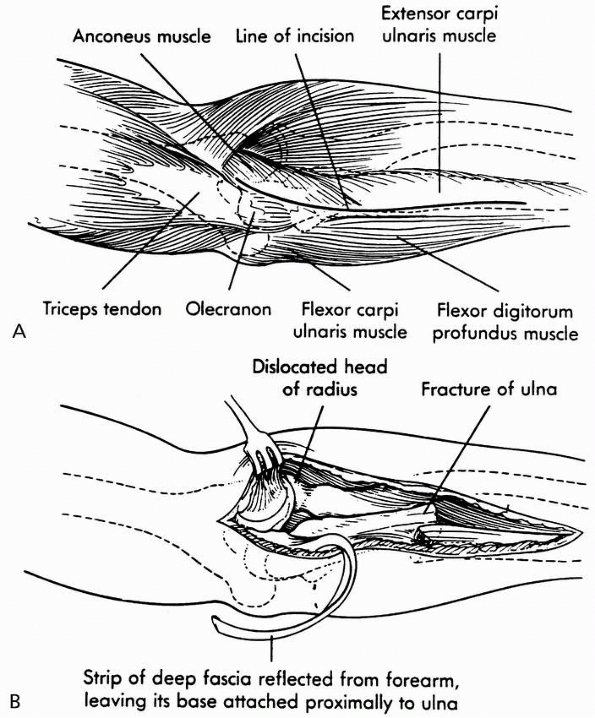
The interval between the anconeus and the extensor carpi ulnaris, using
the distal portion of a Kocher incision, provides sufficient exposure
of the radial head and the interposed structures.52,129
This approach protects the posterior interosseous nerve when the
forearm is pronated. A more extensile approach was described by Boyd.20
This exposure is begun by making an incision following the lateral
border of the triceps posteriorly to the lateral condyle and extending
it along the radial side of the ulna (see Fig. 12-24).
The incision is carried under the anconeus and extensor carpi ulnaris
in an extraperiosteal manner, elevating the fibers of the supinator
from the ulna. This carries the approach down to the interosseous
membrane, allowing exposure of the radiocapitellar joint, excellent
visualization of the orbicular ligament, access to the proximal fourth
of the entire radius, and approach to the ulnar fracture all through
the same incision.20,21,121
In addition, elevation of the extensor-supinator mass from the lateral
epicondyle allows more proximal exposure of the dislocated radial head
if entrapped behind the capsule.
 |
|
FIGURE 12-21 Once the reduction is complete, radiographs should be analyzed for re-establishment of the radiocapitellar line (arrows) and ulnar alignment on both the lateral (A) and Jones (B) views.
|
almost always leads to a stable reduction of the radial head. This in
turn leads to an excellent long-term outcome. Failure to obtain and
maintain ulnar fracture and radial head reduction will lead to a
chronic Monteggia lesion, which is a complex clinical and surgical
problem with risk of a suboptimum outcome. Therefore, I am very
aggressive in my treatment of acute Monteggia fracture-dislocations.
Percutaneous intramedullary fixation of complete transverse and short
oblique ulna fractures is standard. Open reduction and internal
fixation with plate and screws of the rarer long oblique and comminuted
fracture is also standard. Any irreducible or unstable radial head
after fracture reduction and stabilization is approached surgically to
define and correct the cause.
This usually involves repairing entrapped soft tissues. This aggressive approach avoids late complications.
 |
|
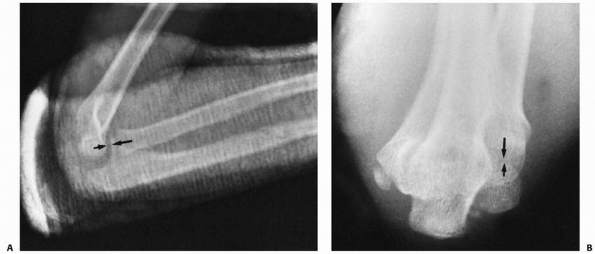
FIGURE 12-22 Lateral (A) and AP (B) views of long oblique ulnar fracture with anterior dislocated radial head. C. Percutaneous reduction and fixation of ulnar fracture through apophysis.
|
bivalved long-arm cast is used for 4 to 6 weeks with the forearm in
slight supination and the elbow flexed 90 to 110 degrees depending on
the degree of swelling. Radiographs are obtained every 1 to 2 weeks
until fracture healing. Intramedullary hardware is removed with
fracture healing. Plate and screw fixation is removed after 6 months
only if it is irritating. Home rehabilitation is begun at 6 weeks and
return-to-sports is dependent on restoration of motion and strength.
 |
|
FIGURE 12-23 A. Radial head dislocation and complete annular ligament tear. B. Radial head dislocation and partial ligament tear. C. Radial head dislocation and partial or complete annular ligament tear and osteochondral fragment.
|
swollen but exhibits posterior angulation of the proximal forearm and a
marked prominence in the area posterolateral to the normal location of
the radial head. The entire upper extremity should be examined because
of the frequency of associated fractures.71,97
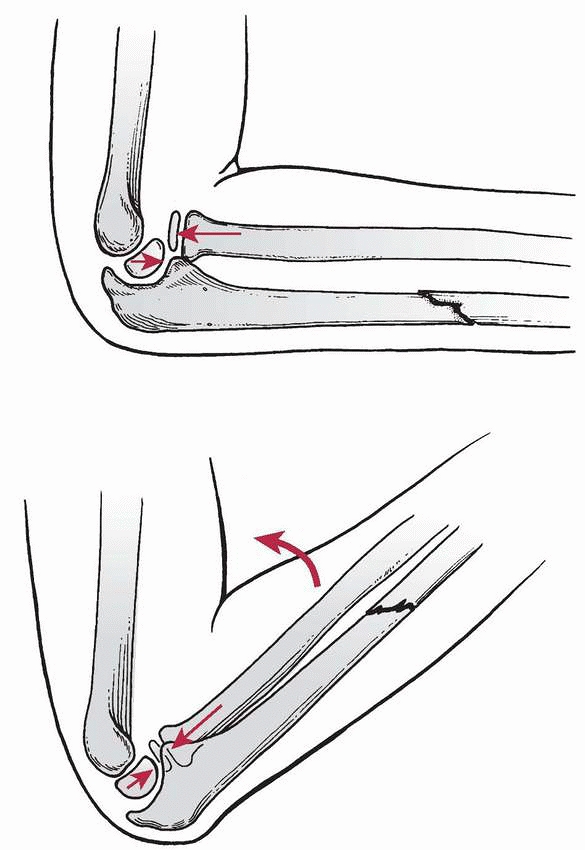
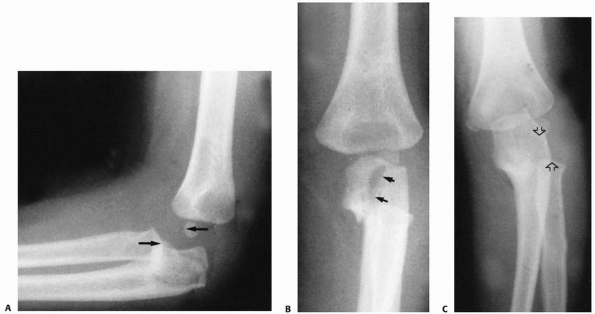
the pertinent features for classifying this fracture. The typical
finding is a proximal metaphyseal fracture of the ulna with possible
extension into the olecranon (Fig. 12-25).37,91,135 Midshaft fractures also occur, with an oblique fracture pattern.8,37,91 The radial head is dislocated posteriorly or posterolaterally9
and should be carefully examined for other injuries. Accompanying
fractures of the anterior margin of the radial head have been noted.37,97 Initially,
these are subtle in children but can lead to progressive subluxation and make late reconstruction difficult (Fig. 12-26).
 |
|
FIGURE 12-24 Surgical approach. A. The incision is carried under the anconeus and extensor carpi ulnaris to expose the radial head and orbicular ligament. B.
The incision can be extended distally to allow exposure of the ulnar fracture and proximally to facilitate harvesting of the tendinous strip for orbicular ligament reconstruction, if necessary. |
analyzed seven fractures in adults and noted that a proximal ulnar
fracture was the typical pattern. He postulated that the injury
occurred by longitudinal loading rather than direct trauma.121 Olney and Menelaus91 reported four type II lesions in their series of children’s Monteggia fractures. Three of these patients had proximal ulnar
fractures and one an oblique midshaft fracture, suggesting two different mechanisms of injury.
 |
|
FIGURE 12-25 Type II Monteggia fracture-dislocation. The typical radiographic findings include (A) a posterior dislocation of the radial head (arrows) and (B) a proximal metaphyseal fracture, which may extend into the olecranon (arrows). The radial head also may be posterolateral (arrows) (C).
|
 |
|
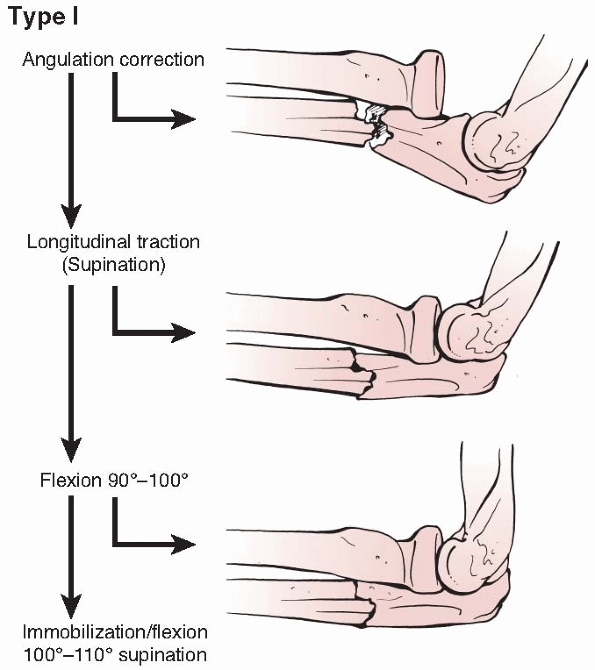
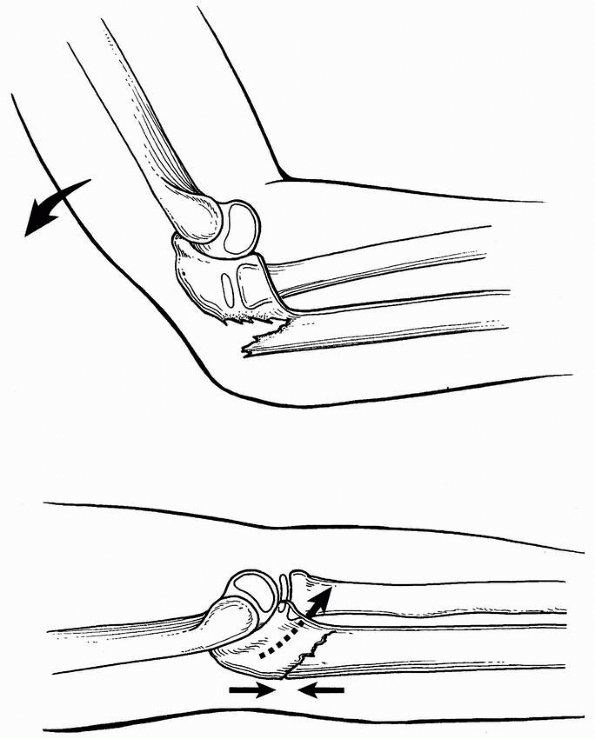
FIGURE 12-26 Mechanism of injury for type II Monteggia fracture-dislocation. A. The elbow is flexed approximately 60 degrees; a force is applied longitudinally, parallel to the long axis of the forearm. B. A posterior elbow dislocation may occur. C. If the integrity of the anterior cortex of the ulna is compromised, a type II fracture-dislocation occurs.
|
was that type II lesions occur when the forearm is suddenly loaded in a
longitudinal direction with the elbow flexed 60 degrees. He showed that
a type II lesion occurred consistently if the ulna fractured;
otherwise, a posterior elbow dislocation was produced (see Fig. 12-26).
A possible difference in bony strength of the ulna suggested a reason
for the high incidence of type II Monteggia fractures in older adults
and their rarity in children. Penrose100 further noted that the rotational position of the forearm did not seem to affect the type of fracture produced.
described type II Monteggia injuries caused by low-velocity injuries in
six adults, five of whom were on long-term corticosteroid therapy. They
suggested that this supports the theory that the type II (posterior)
Monteggia injury is a variant of posterior elbow dislocation, in that
it occurs when the ulna is weaker than the ligaments surrounding the
elbow joint, resulting in an ulnar fracture before the ligament
disruption associated with dislocation occurs.
 |
|
FIGURE 12-27 Longitudinal traction and pronation of the forearm and immobilization in 60 degrees flexion or complete extension.
|
incomplete type II fractures usually have a satisfactory result after
closed reduction.75,91,98,105,143
The ulnar fracture is reduced by longitudinal traction in line with the
long axis of the forearm while the elbow is held at 60 degrees of
flexion (Fig. 12-27). The radial head may
reduce spontaneously or may require gentle, anteriorly directed
pressure applied to its posterior aspect. The elbow is extended once
the radial head is reduced and is immobilized in that position to
stabilize the radial head and allow molding posteriorly to maintain the
ulnar reduction.34,98,141 If the ulnar alignment cannot be maintained, an intramedullary K-wire should be used.
concentric reduction of the radial head and alignment of the ulnar
fracture. When there is an unstable, complete ulnar fracture,
percutaneous intramedullary fixation or open reduction and internal
fixation with plate and screws are used similar to type I
fracture-dislocations.96,101
The radial head should be reduced by open technique if there is
interposed tissue or if it is accompanied by a fractured capitellum or
radial head.
re-established by applying longitudinal traction and straightening the
angular deformity. The radial head may reduce spontaneously or
with
gentle, anteriorly directed force over the radial head. Once reduced,
the position of the head can be stabilized by holding the elbow in
extension. If the ulnar fracture is stable, it can be maintained by
cast immobilization with the elbow in extension. However, if there is
any doubt, percutaneous intramedullary fixation is preferred.
Comminuted or very proximal fractures may require open reduction and
internal fixation with plate and screws or tension band fixation.
Postoperative radiographs are obtained approximately every 7 to 10 days
to confirm continued reduction of the radial head.
radial head if it cannot be obtained through closed manipulation.
Management of the annular ligament is the same as described for type I
Monteggia lesions.
require early detection to avoid late loss of alignment. Open reduction
and internal fixation may be required to maintain radiocapitellar joint
stability. Osteonecrosis and nonunion are complications of this injury.
tissue healing, usually 6 weeks. Home rehabilitation is performed until
restoration of motion and strength.98
significant limitation of motion, especially supination, are the
hallmarks of lateral (type III) Monteggia fracture-dislocations. Again,
these signs can be subtle and missed by harried clinicians.
Open reduction of the radial head may be necessary because of
interposition of soft tissue between it and the ulna or capitellum.13,60,111,133,145,147
Radial angulation at the fracture site is common to all lesions,
regardless of the level. Radiographs of the entire forearm should be
obtained because of the association of distal radial and ulnar
fractures with this complex elbow injury.135
As with all Monteggia injuries, the acute lesion can be missed if
proper radiographs are not obtained and appropriate close examination
of the studies are not performed.
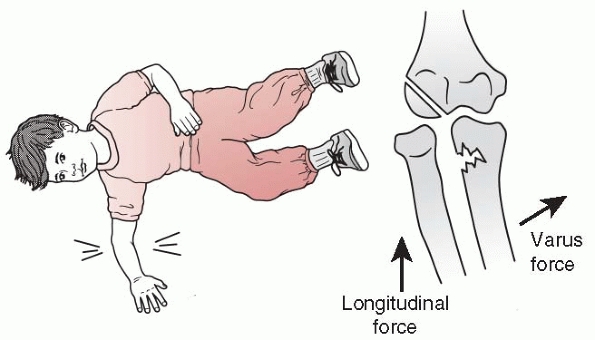
fractures of the proximal ulna with lateral and anterolateral
dislocations of the radial head and concluded that the mechanism of
injury was varus stress at the level of the elbow, in combination with
an outstretched hand planted firmly against a fixed surface (Fig. 12-28).
This usually produces a greenstick ulnar fracture with tension failure
radially and compression medially. The radial head dislocates
laterally, rupturing the annular ligament. Hume60
suggested that the injury may be the result of hyperextension of the
elbow combined with pronation of the forearm. Other authors confirmed
the mechanism of varus force at the elbow as the cause of these
injuries.9,34,87,98,134
The direction of the radial head dislocation is probably determined by
the rotation and angulation force applied simultaneously with the varus
moment at the elbow.87
 |
|
FIGURE 12-28
Mechanism of injury for type III lesions. A forced varus stress causes a greenstick fracture of the proximal ulna and a true lateral or anterolateral radial head dislocation. |
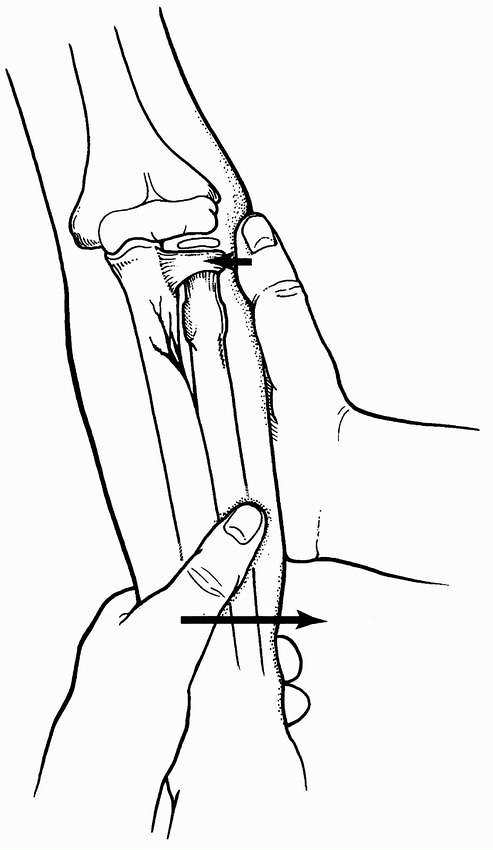
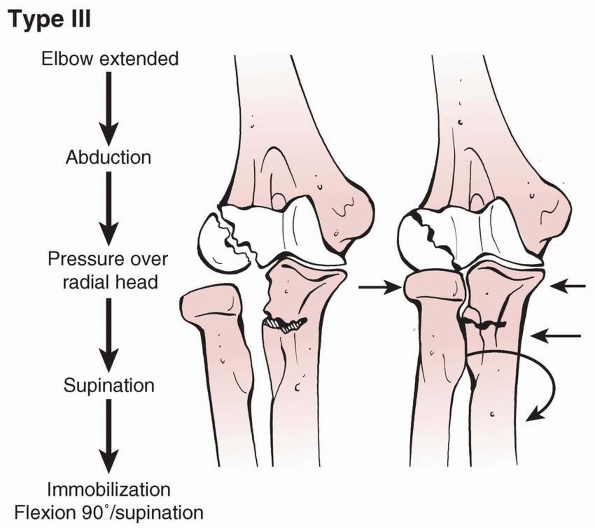
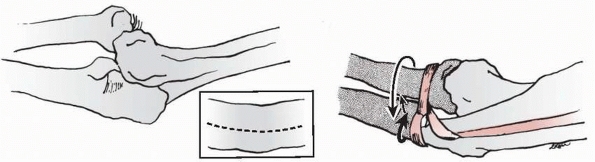
manipulative closed reduction is usually effective in pediatric
patients with metaphyseal, incomplete, or plastic deformation fractures.9,34,46,60,75,87,91,98,134,143,147 However, the rate of operative treatment has been reported to be as high as 12%.91 The reduction maneuver for nonoperative type III lesions is shown in Fig. 12-29.
The elbow is held in extension with longitudinal traction. Valgus
stress is placed on the ulna at the site of the fracture, producing
clinical realignment (Fig. 12-30). The radial head may spontaneously reduce or need assistance with gentle pressure applied laterally (see Fig. 12-29). Reduction sometimes produces a palpable click.135
Ulnar length and alignment must be maintained to ensure a stable radial
head. Fluoroscopic radiographs are obtained to confirm radial head
reduction.84 Any malalignment of the
radiocapitellar joint in any view implies the possibility of interposed
tissue or persistent malalignment of the ulna fracture. The angular
alignment of the ulna must be anatomic to allow and maintain reduction
of the radial head.44
elbow in flexion. The degree of flexion varies depending on the
direction of the radial head dislocation. When the radius is in a
straight lateral or anterolateral position, flexion to 110 to 120
degrees improves stability.37,87,105,143 If there is a posterolateral component to the dislocation, apposition of only 70 to 80 degrees of flexion has been recommended.135
Of note, it can be difficult to assess continued reduction of the
radial head on the AP view radiographically in a cast with the elbow
flexed.
 |
|
FIGURE 12-29 Reduction of type III lesion. Valgus stress is placed on the ulna at the fracture site (arrows), producing clinical realignment. The radial head may spontaneously reduce.
|
which tightens the interosseous membrane and further stabilizes the
reduction.9,34,87,143 Some have suggested positions of immobilization from pronation134 to slight supination.135 Ramsey and Pedersen105
recommended neutral as the best position of rotation to avoid loss of
motion; their patients showed no loss of reduction using this position.
 |
|
FIGURE 12-30 Schematic reduction maneuvers for type III Monteggia fracture.
|
and lateral planes to confirm the reduction of the radial head and
assess the ulnar alignment. Up to 10 degrees of ulnar angulation is
acceptable in younger children, provided the radial head reduction is
concentric and stable. Range-of-motion testing of stability is
appropriate and necessary with plastic deformation fractures since AP
radiographs in the cast will be difficult to assess.
mold over the fracture site. Immobilization is usually in 90 to 100
degrees of flexion for lateral Monteggia lesions and 60 to 80 degrees
of flexion for posterolateral dislocations. The fracture and radial
head reduction need to be truly stable for cast immobilization since
postreduction radiographs are hard to interpret accurately.
until fracture and soft tissue healing, usually by 6 weeks. Home
rehabilitation is performed until restoration of motion and strength.
Final radiographs are obtained with full restoration of motion and
strength to be certain there is anatomic reduction of the proximal
radioulnar and radiocapitellar joints.
goals: reduction and stabilization of both the ulnar fracture and the
radial head. If there is an inability to obtain and maintain anatomic
alignment of the ulnar fracture, proximal radioulnar, and
radiocapitellar joints, then operative treatment is indicated.
malalignment may prevent anatomic relocation of the radial head. The
ulnar fracture can usually be reduced closed, but open reduction may be
necessary because of interposed tissue.
recurrent lateral dislocation of the radial head. Persistent varus
alignment or radial bow, particularly with oblique fractures, may lead
to recurrent subluxation of the proximal radius (Fig. 12-31).44,91 Anatomic reduction of the ulna and fixation with plates and screws44 or intramedullary wires8 will yield excellent results.
Failed closed reduction of the radial head with anatomic alignment of
the ulna fracture implies interposition of soft tissue, which is
repaired through a Boyd approach (see Fig. 12-24).20,145 This allows removal of the interposed tissues139,145 and repair or reconstruction of the annular ligament and the periosteum of the ulna, if necessary (Fig. 12-32),14,23,44,46,121,133 The surgical technique is essentially the same as previously described for a type I Monteggia fracture-dislocation.
open or closed technique. This is usually performed by anatomic, stable
reduction of the ulnar fracture that in turn leads to a stable
reduction of the proximal radioulnar and radiocapitellar joints.
 |
|
FIGURE 12-31 Varus deformity of the ulna. A.
AP views of both elbows showing residual radial bow of the proximal ulna after an incompletely reduced Monteggia type III lesion. B. This bow has produced a symptomatic lateral subluxation of the radial head. |
similar to that of a type I lesion. More swelling and pain are present
because of the magnitude of force required to create this complex
injury. Particular attention should be given to the neurovascular
status of the limb, anticipating the possible increased risk for a
compartment syndrome. Although this injury is uncommon in general and
rare in children, the radiocapitellar joint should be examined in all
midshaft forearm fractures to avoid missing the proximal radioulnar
joint disruption (Fig. 12-33). Failure to recognize the radial head dislocation is the major complication of this fracture.12
type IV lesion is caused by hyperpronation. Of the case reports
discussing the mechanism of injury, both hyperpronation44 and a direct blow112 have been postulated. Olney and Menelaus91
reported a single type IV lesion in their series but did not discuss
the mechanism. Type IV lesions appear to be caused by the mechanism
described for type I lesions.
techniques. Percutaneous intramedullary fixation of the radial and
ulnar fractures with flexible pins and closed reduction of the radial
head also have been described.47,112
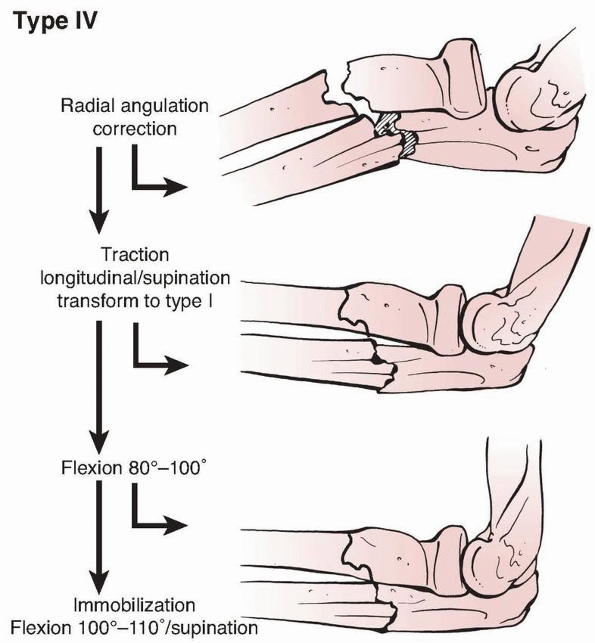
are similar to those of other types. The presence of the free-floating
proximal radial fragment hampers the ability to reduce the radial head.
Stabilization of the radial fracture converts a type IV lesion to a
type I lesion, making treatment easier.
attempted initially, with the aim of transforming the type IV lesion to
a type I lesion (Fig. 12-35), especially if the
radial and ulnar fractures have greenstick patterns. Use of the image
intensifier allows immediate confirmation of reduction, especially
of
the radial head. Closed treatment of unstable ulnar lesions should not
be attempted. If the initial reduction cannot be obtained, anatomic,
stable reduction with either intramedullary or plate fixation is
performed (Fig. 12-36).
unstable and the reduction of the radial head is easier to obtain and
maintain after stable fixation of the radius. In young patients, this
may be achieved by intramedullary fixation. In children older than 12
years, plating of the radius through a Henry extensile approach56 provides more rigid stabilization (see Fig. 12-36).
Once stability is achieved, a closed reduction of the radial head is
attempted. This is usually successful, but any intra-articular
obstruction can be removed through a Boyd approach.
long-arm cast for 4 to 6 weeks in 110 to 120 degrees of flexion with
the forearm in neutral rotation. A short-arm cast is used thereafter if
additional fracture protection is necessary. Home rehabilitation is
performed until restoration of motion and strength. Final radiographs
are obtained with full restoration of motion and strength to be certain
there is anatomic reduction of the proximal radioulnar and
radiocapitellar joints.
 |
|
FIGURE 12-32 Irreducible type III lesion. A. Injury films showing typical greenstick olecranon fracture and lateral dislocation of a type III Monteggia lesion. B. After manipulation and correction of the ulnar deformity, the radial head still was not reduced. C. Open reduction was performed to extract the interposed torn orbicular ligament.
|
 |
|
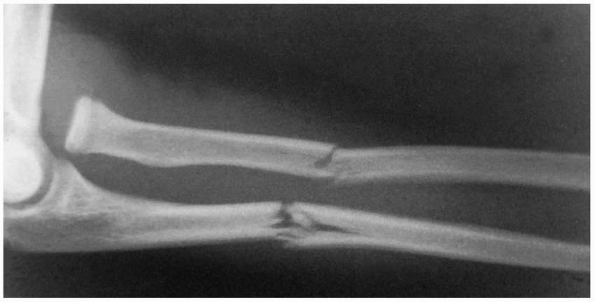
FIGURE 12-33 Type IV Monteggia lesion. A.
Anterior dislocation of the head of the radius with fracture of the upper third of the radial shaft with the ulna fracture angulated anteriorly. The dislocation of the radial head was not recognized. B. Five years later, the radial head was still dislocated, misshapen, and prominent. A full range of motion was present, with the exception of a loss of 10 degrees of full supination. The patient had no pain, but generalized weakness was noted in this extremity, especially in throwing motions. |
 |
|
FIGURE 12-34
Type IV lesion. There is an anterior dislocation of the radial head. The radial and ulnar fractures are usually in the middle third of the shaft, with the radial fracture distal to the ulnar fracture. |
 |
|
FIGURE 12-35 Reduction schematic for type IV Monteggia fracture.
|
 |
|
FIGURE 12-36
Operative treatment, type IV lesion. The initial goal is to stabilize the radius. In older children, a plate may be indicated. Intramedullary pinning usually is adequate. |
corresponding Bado lesion, with the common triad of pain, swelling, and
deformity.
should be made with at least two orthogonal views of the elbow in
addition to views of the forearm. Special views such as obliques should
be obtained to clearly delineate the associated injuries (e.g., radial
head or neck fractures, lateral humeral condyle fractures) and allow
adequate pretreatment planning.
helps define its equivalent type and is discussed in the sections on
the relevant Bado type.
general components of the lesion: ulnar fracture alignment and radial
head reduction. Associated injuries must be dealt with appropriately.
Bado types. The method is dictated by the fracture pattern and location
and its stability after reduction.
dislocations are evaluated and treated using principles based on the
particular injury. They are discussed thoroughly in other sections of
this chapter and book.
The shape of the ulna in patients with a seemingly isolated dislocation
of the radial head usually indicates persistent plastic deformation or
malunion of the ulna and a traumatic etiology to the radial head
dislocation (see Figs. 12-3 and 12-37).77,84,118,128
Chronic Monteggia radial head dislocations have been diagnosed as early
as several weeks after injury during cast changes for a misdiagnosed,
isolated ulnar fracture or years later due to pain, restriction of
motion, and/or arm malalignment. Even a few weeks after injury,
treatment becomes much more complicated than acute recognition and
intervention. Recognition of a dislocated radial head at the time of
injury can prevent the difficult problem of an untreated, chronic
Monteggia lesion.
 |
|
FIGURE 12-37 Ulnar bow line. A. The injury film of an 8-year-old girl who fell, spraining her arm. Note anterior bow of the ulna (black arrows) and loss of the radiocapitellar relation (open arrow). B. Film at time of diagnosis. Note the persistent ulnar bow and overgrowth of radius.
|
 |
|
FIGURE 12-38 Late presenting anterior radial head dislocation with ossification of displaced annular ligament.
|
there is controversy regarding subsequent care. At present there are
limited levels of evidence and conflicting retrospective literature on
this problem. Some reports indicate that the natural history of the
untreated lesion is not problematic.89,116,126 Fahey40
suggested that, although in the short term persistent dislocations do
well, they cause problems later. Other reports support the view that
the natural history of persistent dislocation is not benign and is
associated with restricted motion, deformity, functional impairment,
pain, potential degenerative arthritis, and late neuropathy.1,6,15,18,24,46,49,60,61,63,64,77 Kalamchi63 reported
pain, progressive valgus deformity, and restricted motion, especially
loss of forearm rotation and elbow flexion. Tardy nerve palsies have
been reported subsequent to long-standing, unrecognized Monteggia
lesions.1,6,58,78
chronic Monteggia lesion at anytime postinjury to only when there is
pain, restricted motion, and functional disability. That wide spectrum
of expert opinion makes individual case decision making difficult for
patients, parents, and clinicians. Blount19 and Fowles et al.44
suggested that reconstruction provides the best results in patients who
have had a dislocation for 3 to 6 months or less. Fowles et al.44 reported successful relocations up to 3 years after injury; Freedman et al.,46
up to 6 years after injury. Throughout the literature, the appropriate
age for radial head reduction seems to be younger than 10 years.127 Hirayama et al.57
suggested that the procedure not be performed if there is significant
deformity of the radial head, flattening of the capitellum, or valgus
deformity of the neck of the radius. Seel and Peterson117
suggested that the age of the patient and the duration of the
dislocation are unimportant. Their criteria for surgical repair were
(i) normal concave radial head articular surface and (ii) normal shape
and contour of the ulna and radius (deformity of either correctable by
osteotomy). They treated seven patients ranging in age from 5 to 13
years for chronic dislocations that had been present from 3 months to 7
years. All seven were fully active with no elbow pain or instability at
an average of 4 years after surgery.
Monteggia lesions in children because of the long-term sequelae,
Rodgers et al.112 cautioned that the
results of reconstructive procedures are unpredictable and associated
with a number of complications including malunion of the ulnar shaft,
recurrent radiocapitellar subluxation, and radial and ulnar neuropathy.
reconstruction of a chronic Monteggia when (i) the diagnosis is made
early, (ii) there is preservation of the normal concave radial head and
convex capitellum, (iii) especially when there is progressive deformity
(i.e., valgus), loss of motion, and pain, and, (iv) the patient and
family are well aware of the concerns with operative reconstruction.
chronic Monteggia lesions have been variable in terms of (i) annular
ligament repair or reconstruction,53 (ii) ulnar osteotomy alone62 or in combination with ligament reconstruction,30,59 and (iii) radial osteotomy.29 The technique for delayed reduction of the radial head in a Monteggia fracture-dislocation is attributed to Bell-Tawse,14 who used the surgical approach described by Boyd.20 Other surgical approaches have been developed.52,129
 |
|
FIGURE 12-39
The central slip of the triceps is used to reconstruct an annular ligament in Bell-Tawse reconstruction. The direction of stability is posterior (large arrow). |
all authors advocate surgical repair or reconstruction of the annular
ligament in conjunction with an ulnar osteotomy for a pediatric chronic
Monteggia lesion. Ligament repair or reconstruction without an
osteotomy is very rarely indicated.146 Kalamchi63 restored stability after open reduction and osteotomy by utilizing the native annular ligament. Bell-Tawse14 used a strip of triceps tendon to reconstruct the annular ligament, as did Lloyd-Roberts78 and Hurst.61 Bell-Tawse14
used the central portion of the triceps tendon passed through a drill
hole in the ulna and around the radial neck to stabilize the reduction
and immobilized the elbow in a long-arm cast in extension. Bucknill23 and Lloyd-Roberts78
modified the Bell-Tawse procedure by using the lateral portion of the
triceps tendon, with a transcapitellar pin for stability. The elbow was
immobilized in flexion. Hurst and Dubrow61
used the central portion of the triceps tendon but carried the
dissection of the periosteum distally along the ulna to the level of
the radial neck, which provided more stable fixation than stopping
dissection at the olecranon as described by Bell-Tawse.14
They also used a periosteal tunnel rather than a drill hole for
fixation of the tendinous strip to the ulna. Other authors have used
other soft tissues for reconstruction, including the lacertus fibrous,26 a strip of the forearm fascia,120 palmaris longus free tendon graft,142 and free fascia lata graft.138 Seel and Peterson117
described the use of two holes drilled in the proximal ulna. The holes
are placed at the original attachments of the annular ligament and
allow repair of the annular ligament (frequently avulsed from one
attachment and trapped within the joint) or reconstruction of the
annular ligament with triceps tendon. This technique secures the radial
head in its normal position from any dislocated position and allows
osteotomy for correction of any accompanying deformity of the ulna or
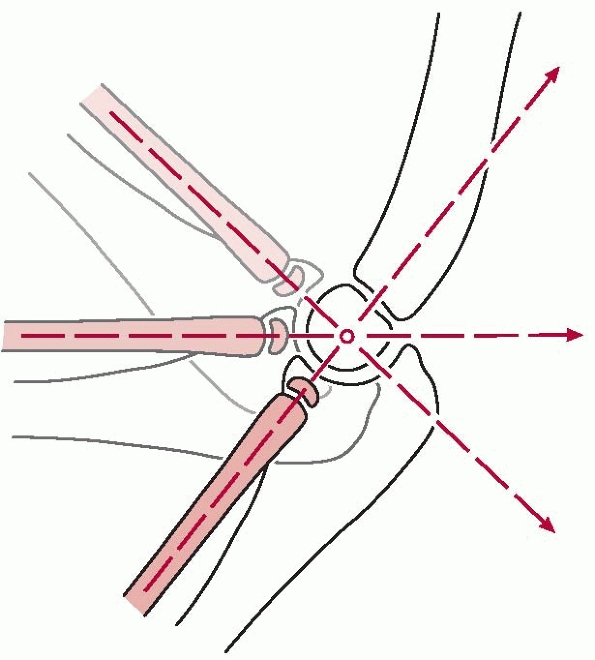
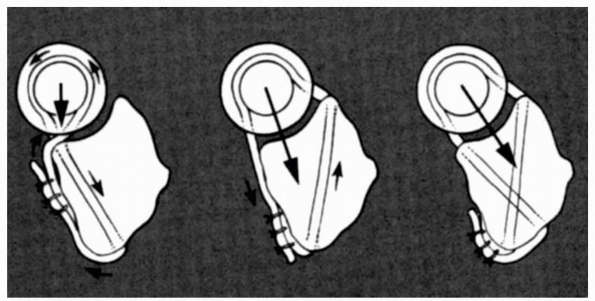
radius. Seel and Peterson117 noted that the Bell-Tawse procedure tends to pull the radius posterolaterally (Fig. 12-39)
and possibly constricts the neck of the radius, thereby potentially
limiting the growth of the radial neck (“notching”) and reducing
forearm rotation. Seel and Peterson117
placed a single drill hole obliquely across the ulna to exit medially
at the site of the medial attachment of the annular ligament on
the coronoid process of the ulna (Fig. 12-40).
The tendon was routed through the tunnel, brought around the neck, and
sutured to the lateral side of the ulna. With this construct, the
direction of stability was posteromedial. The use of two drill holes to
secure the annular ligament or other reconstructive tendon at both
normal attachments of the annular ligament on the ulna achieved a more
normal posteromedial holding force on the neck of the radius.
Alternatives to holes drilled in the bone are small bone staples or
bone-anchoring devices.
 |
|
FIGURE 12-40 Drawings of transverse cuts of the proximal right radius and ulna (viewed distally) at the level of the radial head. Left. Route of the triceps tendon in Bell-Tawse reconstruction. The direction of stability is posterior (large arrow). Center.
Drill hole placed obliquely to exit the ulna at the site of the medial annular ligament attachment. The direction of stability is posteromedial (large arrow). Right. Two drill holes exit the ulna at sites of medial and lateral annular ligament attachments. The direction of stability is anatomic (arrow). |
with or without ligament repair/reconstruction, for a pediatric chronic
Monteggia lesion. Various types of osteotomies have been used to
facilitate reduction of the radial head and prevent recurrent
subluxation after annular ligament reconstruction (Fig. 12-41). Kalamchi63
reported using a “drill hole” ulnar osteotomy to obtain reduction of
the radial head in two patients. Minimal periosteal stripping with this
technique allowed the osteotomy to heal rapidly. Hirayama et al.57
used a 1-cm distraction ulnar osteotomy approximately 5 cm distal to
the tip of the olecranon with plate-and-screw fixation, but
complications with loosening and plate breakage occurred. Mehta82,83
used an osteotomy of the proximal ulna stabilized with bone graft. In
neither series was annular ligament repair done. Oner and Diepstraten92
suggested that ulnar osteotomy is not necessary in type I lesions
(anterior dislocation), but in type III lesions (anterolateral
dislocation) recurrent subluxation is likely without osteotomy.
Freedman et al.46 reported a delayed
open reduction of a type I Monteggia lesion without annular ligament
reconstruction but with ulnar osteotomy, radial shortening, and
deepening of the radial notch of the ulna.
 |
|
FIGURE 12-41 A. Diagram of floating open osteotomy without fixation or bone graft. B. Similar osteotomy with radiocapitellar pin fixation. C. Unfortunately in this case, the radial head was never reduced and the pin was placed without anatomic alignment. D. In this situation, the osteotomy was plated without bone graft, the radiocapitellar joint pinned anatomically for 4 weeks. E. Long-term-follow up with anatomic healing.
|
compared the results of simple corrective ulnar osteotomy in six
patients with those of posterior angular (overcorrected) osteotomy in
six others, and found that better clinical outcomes were obtained with
the overcorrected, angular osteotomy. Tajima and Yoshizu,132
in a series of 23 neglected Monteggia fractures, found that the best
results were obtained by opening wedge osteotomy of the proximal ulna
without ligament reconstruction.
in patients with chronic dislocation of the radial head after missed
type I Monteggia lesions, reduction was successfully obtained with
ulnar corticotomy and gradual lengthening and angulation of the ulna
using an external fixator. Another option for type IV old Monteggia
fracture is a shortening
osteotomy of the radius, usually indicated for angulation of the radius without angulation of the ulna.
diagnosis of a Monteggia lesion, reduction and stabilization of the
radial head in its appropriate relation with the capitellum are
indicated. Even though the child may do well in the short term without
reduction of the radial head, problems usually develop in adolescence
or adulthood when progressive instability, pain, weakness of the
forearm, and restriction of motion are likely to occur. There is also a
risk of tardy radial or ulnar nerve palsies. The concavity of the
radial head and convexity of the capitellum are assessed
preoperatively, usually by MRI scan. Appropriate discussion with the
patient and family regarding the risks and complications of surgery is
performed. This is not an operation for the inexperienced surgeon or
uninformed patient and family.
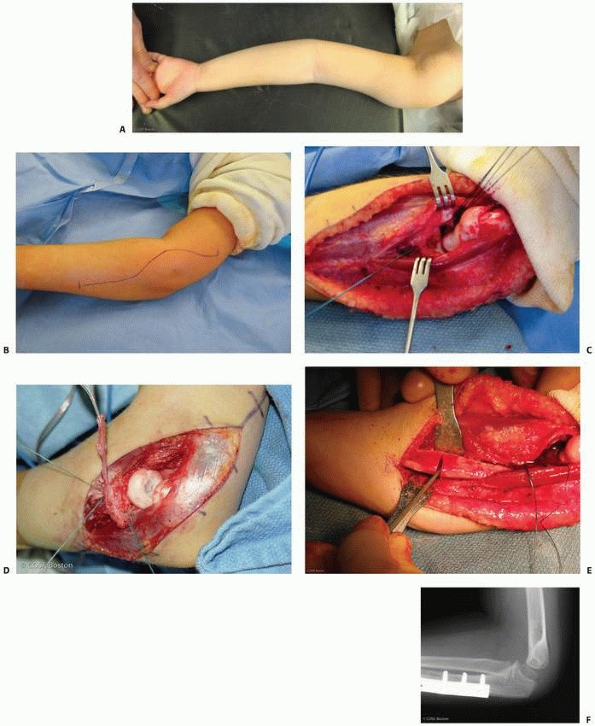
The skin incision is curvilinear to allow for proximal triceps tendon
harvesting, if necessary, and distally for an ulnar opening wedge
osteotomy. Initially, only the central portion is opened. The radial
nerve is identified between the brachialis and brachioradialis in the
distal humerus. Dissection of the nerve is performed distally to its
branching into motor (posterior interosseous nerve) and sensory nerves.
Generally the posterior interosseous nerve is adherent to the
dislocated radial head. The nerves are mobilized and protected
throughout the remainder of the reconstruction.
utilized to expose the joint. The joint exposure is carried proximal
with elevation of the extensor-supinator mass and capsule as a single
tissue plane off the distal humerus. This gives complete exposure of
the elbow joint. The radial head is usually dislocated anteriorly and
superiorly with a wall of interposed capsule and ligament blocking
reduction. Pulvinar and synovitis are thoroughly débrided from the
elbow joint. Particular attention is paid to a thorough débridement of
the proximal radioulnar joint to allow the radial head to fit
anatomically into place once reduced. At this stage, a decision needs
to be made if the native annular ligament can be used for
reconstruction. There is usually a central perforation in the capsular
wall that separates the dislocated radial head from the joint. This
perforation indicates the site of the opening of the original ligament.
Dilatation and radial incisions extending from the center outward are
made to enlarge this opening. This usually enables the native annular
ligament to be reduced over the radial neck. Capsular adhesions are
removed from the radial head to assist in reduction of the radial head
and neck back into the joint. The native ligament usually detaches from
the ulna with a large periosteal sleeve (the site of ossification on
the radiographs of a chronic Monteggia lesion), and this can be the
site for suture reattachment to the ulna of the native ligament. If the
native ligament cannot be used, and most of the time it can, then it is
thoroughly débrided in preparation for harvesting of triceps fascia for
ligament reconstruction.
accomplished, it is scrutinized for congruity between the radial head
and the capitellum. If this is satisfactory, ligamentous repair or
reconstruction alone can be done. This is exceedingly unusual. If the
radius cannot be reduced atraumatically, an ulnar osteotomy is made at
the site of maximal deformity. This involves a more distal exposure to
the ulna. Subperiosteal dissection is performed with fluoroscopic
assistance at the site of maximal deformity. An opening wedge osteotomy
is made with a laminar spreader to allow the radial head to align
itself with the capitellum without pressure. Partial overcorrection of
the ulnar alignment is the goal. When reduced anatomically, the ulnar
osteotomy is then fixed partially proximally and distally with a plate
and screws. Further testing of a complete stable arc of rotation of the
radial head is performed to be certain the correct level and degree of
osteotomy were obtained to maintain radiocapitellar and radioulnar
alignment. If correct, the fixation is completed. No bone graft is
used, and the periosteum is repaired.
reconstruction is completed. If the native ligament is used, and it
usually is in situations that are a year or less out from injury, then
Ethibond mattress sutures (Ethicon, Somerville, NJ) are placed in the
annular ligament and the ligament is repaired through ulnar periosteal
tunnels. None of the radial sutures are tightened until all are placed.
If reconstruction is necessary, a 6 to 8 cm strip of triceps fascia is
developed from proximal to distal, carefully elevating the periosteum
from the proximal ulna down to the level of the radial neck. Over the
olecranon apophysis, this dissection will be delicate so as to not
inadvertently amputate the fascia. The strip of tendon is then passed
through the periosteum, around the radial neck, and then brought back
and sutured to itself and the ulnar periosteum. The passage and
securing in the periosteum is similar in design to the drill holes
advocated by Seel and Peterson.117
At this stage, the radial head and capitellum alignment should be
anatomic throughout full rotation. Final closure involves repair of the
capsule and extensor-supinator origin back to the lateral epicondylar
region of the humerus. Final radiographs and fluoroscopic testing of a
stable arc of motion in both flexion-extension and pronation-supination
planes are gently tested before completion of closure. Prophylactic
volar and dorsal forearm fasciotomies are carefully performed through
the original incision with elevation of the skin and subcutaneous
tissues and a long tenotomy scissors. Final inspection of the radial
nerve is performed before subcutaneous and skin closure.
needed if the osteotomy and soft tissue repair tension are correct. At
times, it is used intraoperatively for temporary stability to get the
osteotomy and repair right; it is then removed to test range of motion.
If there is radial head deformity in very chronic reconstructions,
pinning the joint is sometimes useful for 3 to 4 weeks postoperatively.
In my experience, this has been occasionally necessary in repeat
surgery for a chronic Monteggia lesion in which options are limited and
the patient has pain and marked limitation of motion. Then, the
radiocapitellar joint is secured by passing a smooth,
transcapitellar
pin through the posterior aspect of the capitellum into the radial head
and neck with the elbow at 90 degrees and the forearm in supination. A
pin of sufficient size is mandatory to avoid pin failure68;
a small pin may fatigue and break. An alternative technique to secure
the reduction of the radius is transversely pinning the radius to the
ulna.75
 |
|
FIGURE 12-42 A. Clinical deformity of chronic Monteggia injury with increased cubitus valgus. B. Extensile incision for annular ligament reconstruction and ulnar osteotomy. C.
Exposure of radiocapitellar and radioulnar joint with elevation of extensor-supinator origin from lateral epicondyle, protection of radial nerve, and thorough joint débridement. D. Radial head with osteochondral change from chronic dislocation. Annular ligament has been reduced around radial neck and sutures are in place for construction to annular ligament. E. Ulnar opening wedge osteotomy at site of maximum deformity. F. Long-term follow-up of ulnar osteotomy and the anatomic reduction of proximal radioulnar joint and radiocapitellar joint. |
[Kimberly Clark, Chantilly, VA]) long-arm cast is applied with the
forearm in 60 to 90 degrees of supination and the elbow flexed 80 to 90
degrees. The cast is maintained for 4 to 6 weeks and is then changed to
a removable bivalve to allow active motion, especially pronation and
supination. Elbow flexion and extension return more rapidly than rotary
motion of the forearm which may take up to 6 months to improve, with
pronation possibly limited, though minimally, permanently.112 Final desired result is not determined until radiographs are anatomic with full restoration of motion.
nerve injury, making it the most common complication associated with
Monteggia fractures.60 It is most commonly associated with types I and III injuries.14,89,118
The posterior interosseous nerve is most commonly injured because of
its proximity to the radial head and its intimate relation to the
arcade of Frohse. The arcade may be thinner and therefore more pliable
in children than in adults.122 In
addition, the periosteum is much thicker in pediatric patients. This
may account in part for the rapid resolution of the nerve injury in
children.
Nerve function usually returns by 12 weeks after reduction, if not
sooner.123,125 A review of a series of children’s Monteggia lesions91
recommends waiting 6 months before intervention for a posterior
interosseous nerve injury. Most series report 100% resolution in both
fractures treated promptly and those treated late.1,6,76
of irreducible Monteggia fractures caused by interposition of the
radial nerve posterior to the radial head documented return of function
approximately 4 months after the nerve was replaced to its normal
anatomic position and the radial head was reduced. Morris,86
in cadaver studies, showed that significant anterior dislocation of the
radial head and varus angulation of the elbow allowed the radial nerve
to slide posterior to the radial head and, with subsequent reduction of
the radial head, become entrapped. If a chronic reconstruction is
undertaken in the presence of a persistent radial nerve lesion, it is
highly recommended that radial nerve exploration and decompression be
performed before joint débridement. Rodgers et al.113 cited a partial nerve injury during similar circumstances that was then microscopically repaired with full recovery. Rang106 acknowledged the same experience to the author in an open educational forum.
adult with an ulnar nerve lesion associated with a type II Monteggia
lesion with spontaneous resolution. Stein et al.125
reported three combined radial and ulnar nerve injuries, two of which
underwent exploration and decompression for functional return of the
nerve.
in their report specifically examining nerve injuries in Monteggia
lesions, reported no median nerve deficits. Watson and Singer142
reported entrapment of the main trunk of the median nerve in a
greenstick ulnar fracture in a 6-year-old girl. Completion of the
fracture was necessary for release of the nerve. At 6 months after
surgery, there was full motor recovery but sensation was slightly
reduced in the tips of the index finger and thumb.
Although reported treatment has varied, excision of the radial head
with exploration and neurolysis of the nerve generally produced good
results,1,6 while exploration of the nerve alone produced variable results.58,76 Yamamoto et al.148 combined radial head resection and nerve exploration with tendon transfers, producing good results in two patients.
reported two type I equivalent lesions consisting of a fractured radial
neck and midshaft ulnar fracture. This injury was unique because of
significant medial displacement of the distal radial fragment.
Obtaining and maintaining reduction of the radius was difficult with a
closed technique.
reported an ipsilateral ulnar shaft lesion and a lateral condylar
fracture without loss of the radiocapitellar relation, suggesting a
Monteggia type II equivalent. Kloen et al.69
reported an unusual bilateral Monteggia fracture and described the
operative technique for this treatment. Despite surgical and
rehabilitative challenges, excellent results were obtained in both
elbows. In essence, any fracture about the elbow and forearm should be
inspected for an associated Monteggia lesion.
fracture-dislocations have been noted radiographically: around the
radial head and myositis ossificans. Ossification around the radial
head and neck14,60,76,78,126,128
appears as a thin ridge of bone in a cap-like distribution and may be
accompanied by other areas resembling sesamoid bones; they resorb with
time. Ossification may also occur in the area of the annular ligament,36
including in a chronic Monteggia with a displaced annular ligament.
Elbow function generally is not affected by the formation of these
lesions14,60,78,126,128
as long as the radial head and neck are anatomically reduced.
ossificans, reported to occur in approximately 3% of elbow injuries and
7% of Monteggia lesions in adults and children.90
Myositis ossificans has a good prognosis in patients younger than 15
years of age, appearing at 3 to 4 weeks after injury and resolving in 6
to 8 months. Its occurrence is related to the severity of the initial
injury, association with a fractured radial head, the number of
remanipulations during treatment, and passive motion of the elbow
during the postoperative period.90,137
-
Evaluation of the radial head location
requires an AP view of the proximal forearm and a true lateral view of
the elbow. All forearm injuries require careful inspection of the
proximal radioulnar joint and the radiocapitellar joint before
treatment. -
The radiocapitellar line must be anatomic in all views.
-
If the radial head is dislocated, always
look for ulnar fracture or plastic deformation. Conversely, if the ulna
is fractured, always look for a radial head subluxation or dislocation. -
Stability of the ulnar reduction is
required to maintain reduction of the radial head. Stability may be
inherent to the fracture pattern (plastic deformation or incomplete
fractures) or achieved by internal fixation (intramedullary fixation
for short oblique and transverse fractures; plate and screw fixation
for long oblique and comminuted fractures). -
Radial head reduction confirmed by an intact radiocapitellar line must be achieved by open or closed means.
-
If the radial head is irreducible or
unstable, reconstruction of the annular ligament and/or removal of
interposed soft tissue is required. -
Treatment of an acute Monteggia lesion is much easier and more successful than reconstruction of a chronic Monteggia lesion.
-
Reconstruction of a chronic Monteggia lesion is not an operation for the uninitiated.
contributions of the authors of previous editions of this chapter, Drs.
Earl Stanley and Jose de la Garza, as well as the outstanding
assistance of Ms. Bonnie Kaufman in our hand research unit.
M, Oĝün TC, Kapicioĝlu MI. The Monteggia lesion and ipsilateral
supracondylar humerus and distal radius fractures. J Orthop Trauma
1999;13(1):60-63.
JH. Fractures and dislocations about the elbow in children: section on
Monteggia fractures. AAOS Instr Course Lect 1991;40:373-384.
FH, Corkery PH. Lateral dislocation of the radiohumeral joint with
greenstick fracture of the upper end of the ulna. J Bone Joint Surg Br
1960;42:782-784.
N, Jindal P. Monteggia lesion in a child: variant of a Bado type-IV
lesion. A case report. J Bone Joint Surg Am 1996;78(8):1252-1255.
A. Ipsilateral Monteggia equivalent injury and distal radial and ulnar
fracture in a child. J Orthop Trauma 1994;8(5):431-433.
D, Trussell A. Ipsilateral radial head dislocation and distal fractures
of both forearm bones in a child. Am J Orthop 1995;24:498-500.
HB. Surgical exposure of the ulna and proximal one third of the radius
through one incision. Surg Gynecol Obstet 1940;71:86-88.
I, De Smet L. Missed radial head dislocations in children associated
with ulnar deformation: treatment by open reduction and ulnar
osteotomy. J Orthop Trauma 2004;18(6):375-378.
S, O’Doherty D. Type I Monteggia fracture dislocation associated with
ipsilateral distal radial epiphyseal injury. J Orthop Trauma
2001;15(5):373-375.
GU. Missed chronic anterior Monteggia lesion. Closed reduction by
gradual lengthening and angulation of the ulna. J Bone Joint Surg Br
2001;83(4):547-550.
AA, Ceroni D, Kaelin A. An unusual Monteggia type-I equivalent fracture
in a child. J Bone Joint Surg Br 2003;85(4):584-586.
FF, Egenolf M, Carsten C, et al. Unstable diaphyseal fractures of both
bones of the forearm in children: plate fixation versus intramedullary
nailing. Injury 2005; 36(10):1210-1216.
JV, Sliman N, Kassah MT. The Monteggia lesion in children. Fracture of
the ulna and dislocation of the radial head. J Bone Joint Surg Am
1983;65:1276-1282.
JL, Buschmann WR, Insler HP. Monteggia type I equivalent lesion:
diaphyseal ulna and proximal radius fracture with a posterior elbow
dislocation in a child. J Orthop Trauma 1991;5:373-375.
L, Luk K, Leong JC. Radial head reduction after a missed Monteggia
fracture: brief report. J Bone Joint Surg Br 1988;70:846-847.
WK, Timperlake RW. Orthopedic treatment of 4 type IV Monteggia
fracture-dislocations in a child. J Bone Joint Surg Br 1992;74:780-781.
U, Pritsch M, Levy O, et al. Monteggia and equivalent lesions: a study
of 41 cases. Clin Orthop Relat Res 1997;337:208-215.
U, Pritsch M, Yosepovich A. Monteggia lesion in a child: variant of a
Bado type-IV lesion. A case report. J Bone Joint Surg Am
1997;79(11):1753-1754.
ML. Monteggia fracture: a combined surgical approach employing a single
lateral incision. Clin Orthop Relat Res 1967;50:87-93.
BM, Stevens PM, Smith JT. Chronic Monteggia fractures in children:
outcome after treatment with the Bell-Tawse procedure. J Pediatr Orthop
B 2004;13(6):402-406.
T, Takemitsu Y, Yagihara K, et al. Operation for chronic dislocation of
the radial head in children. J Bone Joint Surg Br 1987;69:639-642.
F, Jensen V. Tardy posterior interosseus nerve palsy as a result of an
unreduced radial head dislocation in Monteggia fractures: a report of
two cases. J Hand Surg Am 1984;9:572-575.
JH, Sulaiman AR, Lee HC, et al. Open reduction and annular ligament
reconstruction with fascia of the forearm in chronic monteggia lesions
in children. J Pediatr Orthop 2005;25(4):501-506.
AC. Anterior dislocation of the head of the radius associated with
undisplaced fracture of olecranon in children. J Bone Joint Surg Br
1957;39:508-512.
LC, Dubrow EN. Surgical treatment of symptomatic chronic radial head
dislocation: a neglected Monteggia fracture. J Pediatr Orthop
1983;3:227-230.
G, Shionoya K. Corrective ulnar osteotomy for malunited anterior
Monteggia lesions in children: 12 patients followed for 1 to 12 years.
Acta Orthop Scand 1998; 69:73-76.
S, De Schrijver F, De Smet L. Radial head dislocation with plastic
deformation of the ulna in children. A rare and frequently missed
condition. Acta Orthop Belg 2000;66(4):359-362.
TC, Mader K, Wulke AP, et al. Operative treatment of chronic Monteggia
lesion in younger children: a report of three cases. J Shoulder Elbow
Surg 2006;15(1): 119-121.
B, Eriksen AF. Simultaneous type II Monteggia lesion and fracture
separation of the lower radial epiphysis. Injury 1986;17:51-62.
P, Prevot J, Ligen JN, et al. Elastic stable intramedullary nailing in
forearm shaft fractures in children: 85 cases. J Pediatr Orthop
1990;10:167-171.
RL, Jacksen T. Tardy palsy of posterior interosseous nerve with
Monteggia fracture. J Bone Joint Surg Am 1975;57:124-125.
GC, Bucknill TM. Anterior dislocation of the radial head in children:
aetiology, natural history, and management. J Bone Joint Surg Br
1977;59:402-407.
SJ, Gordon JE, Schoenecker PL. Intramedullary fixation of unstable
bothbone forearm fractures in children. J Pediatr Orthop
1998;18(4):451-456.
H, Yoshida K, Doi R, et al. Combined Monteggia and Galeazzi fractures
in a child: a case report and review of the literature. J Orthop Trauma
2003;17(2):128-131.
H, Kondo K, Saka K. Type II Monteggia lesion with fracture-separation
of the distal physis of the radius. Am J Orthop 2000 Sep;29(9):717-719.
RJ, LeFevre GW. Irreducible isolated dislocation of the radial head: a
case report. Clin Orthop Relat Res 1971;80:72-74.
FC, Diepstraten AF. Treatment of chronic posttraumatic dislocation of
the radial head in children. J Bone Joint Surg Br 1993;75:577-581.
N, Ikeda K, Hagiwara N, et al. Posterior interosseous nerve injury
complicating ulnar osteotomy for a missed Monteggia fracture. Scand J
Plast Reconstr Surg Hand Surg 2004;38(6):376-378.
R, Waters PM. Posttraumatic reconstruction of the elbow in the
pediatric patient. Clin Orthop Relat Res 2000;(370):115-126.
KD. Die Morote-Drahtung bei proximalen und mittleren Unterarm Schaft
Frakturen des Kindes. Operat Orthop Traumatol 1990;2:245-255.
Sicialia JE, Morote Jurado JL, Corbach Gironés JM, et al. Osteosíntesis
percuntánea en fracturas diafisaris de ante brazo en niños y
adolescentes. Rev Esp Cir Ost 1977; 12:321-334.
RS, Bowe JA. Ipsilateral supracondylar humerus fracture and Monteggia
lesion: a case report. J Orthop Trauma 2002;16(10):737-740.
DM, Galpin RD, Carey TP. Intramedullary Steinmann pin fixation of
forearm fractures in children. Long-term results. Clin Orthop Relat Res
2000;(376):39-48.
RH, Pedersen HE. The Monteggia fracture-dislocation in children. Study
of 15 cases of ulnar-shaft fracture with radial-head involvement. JAMA
1962;82:1091-1093.
FA. Lateral condyle fracture and ipsilateral ulnar shaft fracture:
Monteggia equivalent lesions. J Pediatr Orthop 1985;5:364-366.
F. Unstable fracture-dislocations of the forearm (Monteggia and
Galeazzi lesions). J Bone Joint Surg Am 1982;64:857-863.
FW, Cordell LD. Unstable fracture-dislocations of the forearm. The
Monteggia and Galeazzi lesions. Arch Surg 1968;96:999-1007.
WB, Smith BG. A type IV Monteggia injury with a distal diaphyseal
radius fracture in a child. J Orthop Trauma 1993;7:84-86.
WB, Waters PM, Hall JE. Chronic Monteggia lesions in children:
complications and results of reconstruction. J Bone Joint Surg Am
1996;78:1322-1329.
DE, Klugman JA, Madan SS, et al. Anterior dislocation of the radial
head with fractures of the olecranon and radial neck in a young child:
a Monteggia equivalent fracture-dislocation variant. J Orthop Trauma
2005;19(6):425-428.
RB, Zaltz C. Anatomic investigations of the mechanism of injury and
pathologic anatomy of “pulled elbow” in young children. Clin Orthop
Relat Res 1971;77:134-143.
A, Khan O, Bagga T. Simultaneous monteggia type I fracture equivalent
with ipsilateral fracture of the distal radius and ulna in a child: a
case report. J Med Case Reports 2008;2:190.
M. The arcade of Frohse and its relationship to posterior interosseous
nerve paralysis. J Bone Joint Surg Br 1968;50:809-812.
M, Freundlich BD, Teicher J. Posterior interosseous nerve palsy as a
complication of Monteggia fracture in children. Clin Orthop Relat Res
1968;58:141-145.
M, Kaplan EB. The quadrate ligament of the elbow—its relationship to
the stability of the proximal radioulnar joint. Acta Orthop Scand 1970;
41:632-647.
JCH, Ellis BW. Vulnerability of the posterior interosseous nerve during
radial head reduction. J Bone Joint Surg Br 1971;53:320-332.
ML, Kopp M, Gillespie R. Fracture of the radial neck and proximal ulna
with medial displacement of the radial shaft. Orthopedics
1989;12:1577-1579.
T, Yoshizu T. Treatment of long-standing dislocation of the radial head
in neglected Monteggia fractures. J Hand Surg Am 1995;20:S91-S94.
SD. Dislocation of the head of the radius associated with fracture of
the upper end of ulna in children. J Bone Joint Surg Br 1969;51:700-706.
SD, Ierodiaconou MD, Rousis N. Fracture of the upper end of the ulna
associated with dislocation of the head of the radius in children. Clin
Orthop Relat Res 1988; 228:240-249.
GH, Wilber JH, Marcus RE. Internal fixation of fractures in children
and adolescents. Clin Orthop Relat Res 1984;188:10-20.
JD, Lipscomb AB. Recurrent radial head subluxation treated with annular
ligament reconstruction. Clin Orthop Relat Res 1989;246:131-135.
L, Delronge G, Lamoureux J. Shaft forearm fractures in children.
intramedullary nailing with immediate motion: a preliminary report. J
Pediatr Orthop 1988;8: 450-453.
A, Wolfe SW, Marsh JS. Use of a modified Bell Tawse procedure for
chronic acquired dislocation of the radial head. J Pediatr Orthop
1998;18(3):410-414.
PR. Greenstick fracture of the upper end of the ulna with dislocation
of the radio-humeral joint or displacement of the superior radial
epiphysis. J Bone Joint Surg Br 1963;45:727-731.
K, Yoshiaki Y, Tomihara M. Posterior interosseous nerve palsy as a
complication of Monteggia fractures. Nippon Geka Hokan 1977;46:46-56.
