Examination of Palatal Function
– Neurologic Examination > Cranial Nerve Examination > Chapter 19
– Examination of Palatal Function
neurologic examination is to look for evidence of dysfunction of the
vagus (tenth) nerve. In some cases, palatal movement is assessed to
look for evidence of neuromuscular disease causing palatal weakness.
part of a routine neurologic examination. Palatal movement should be
particularly assessed in patients who have complaints of difficulty
swallowing or slurred speech, or in patients who are suspected of
having a severe neuromuscular disorder that may cause palatal weakness.
A gag reflex rarely, if ever, needs to be performed on any awake
patient as part of a standard neurologic examination, however.
vagus (tenth) nerve of the pharyngeal muscles that elevate the palate.
The origin of the vagus nerve is in the medulla. The left vagus nerve
innervates the left palatal muscles, and the right vagus nerve
innervates the right palatal muscles.
-
Ask the patient to open his or her mouth
while you look at the patient’s soft palate and uvula with a
flashlight. If it is difficult to see the palate, gently press down on
the tongue with a tongue depressor. -
Ask the patient to say “ah” (the fancy name for this is phonation).
-
Assess the elevation of both sides of the palate and the uvula to phonation.
symmetrically when the patient says “ah,” and the uvula should remain
primarily in the midline.
-
Limited elevation of one side of the
palate occurs due to unilateral palatal weakness and suggests a lesion
of the tenth nerve on the weak side. Weakness of elevation of one side
of the palate is usually accompanied by deviation of the uvula to the
strong side (Fig. 19-1). True unilateral
palatal weakness is an uncommon finding, most typically seen in
patients with infarctions of the lateral medulla (Wallenberg’s
syndrome) affecting the nucleus of the tenth cranial nerve or in
patients with other disorders
P.61
affecting
the tenth cranial nerve. Vagus nerve lesions causing palatal weakness
may also be associated with hoarseness of the voice due to associated
unilateral vocal cord weakness.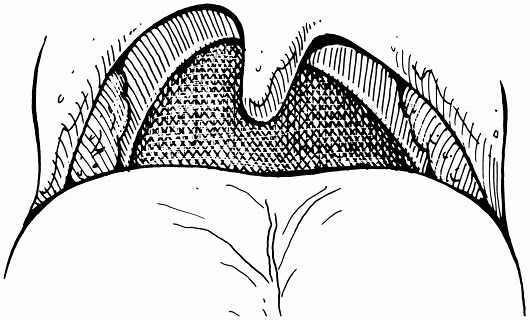 Figure 19-1
Figure 19-1
Weakness of the left side of the palate in a patient with a left vagus
(tenth) nerve lesion. The uvula deviates to the right (strong) side. -
Significant weakness of elevation of both
sides of the palate can be seen in patients with severe generalized
neuromuscular disease, such as myasthenia gravis or Guillain-Barré
syndrome. Symptoms of bilateral palatal weakness include a nasal
quality to the speech and regurgitation of liquids through the nose
when attempting to swallow. -
Palatal myoclonus is a finding that may
rarely be seen when looking at the palate and consists of a continuous,
rapid, rhythmic jerking of both sides of the soft palate. Palatal
myoclonus may be seen due to lesions of the brainstem or as an
idiopathic process, and it is sometimes associated with the clinical
complaint of a clicking sound in the ears.
-
Patients who have had tonsillectomies may
have some asymmetry of their posterior pharynx and soft palate that can
sometimes be confused with unilateral palatal weakness. By looking at
the palates of many normal patients (including patients with previous
tonsillectomies), you’ll have a better feel for the normal variations
in palatal symmetry. -
Use of the gag reflex in the clinical assessment of brain death is described in Chapter 42,
Examination of the Comatose Patient. There is little useful information
to be found by testing the gag reflex of a noncomatose patient. The gag
reflex is a noxious test and should be avoided in routine neurologic
assessment. In those patients in whom swallowing and risk for
aspiration needs to be assessed, formal swallowing assessment by a
speech therapist should be obtained.
