Osteoarthritis and Inflammatory Arthritis of the Hip
– HIP > Part B – Evaluation and Treatment of Hip Disorders > 3 –
Osteoarthritis and Inflammatory Arthritis of the Hip
frequently encountered diseases in orthopaedics. They are the leading
causes of joint disease in the hip, resulting in joint destruction, and
often in the need for hip replacement. Symptomatic osteoarthritis of
the hip is prevalent in 3% to 5% of the adult white population.
Radiographic evidence of osteoarthritis is more common (9% to 10%),
indicating that roughly half of the patients with some radiographic
evidence of osteoarthritis are asymptomatic.
still often used, that implies degenerative changes owing to various
causes. The term DJD can be confusing because it is often used
synonymously for osteoarthritis, but can be applied to any condition
that results in degenerative changes of the joint. A more correct use
of terminology would be to avoid the use of DJD and use the correct
underlying diagnosis instead.
grouped into noninflammatory and inflammatory arthritis. Osteoarthritis
is by far the most common condition of the noninflammatory group.
Osteoarthritis results from a primary failure of the cartilage, whereas
with inflammatory arthritis, the cartilage failure is secondary to the
inflammatory response. Table 3-1 outlines the more common arthritides that can affect the hip joint.
multitude of conditions, with the end result being failure of the
weight-bearing cartilage. Because of its various potential causes, OA
can be thought of as a syndrome rather than a single entity. In the
past, it was felt that most patients who developed osteoarthritis had
primary OA without any identifiable cause, arising as a result of a yet
unidentified weakness of the cartilage. Now, it is more evident that
most patients with OA likely have an underlying mechanical cause that
results in damage and subsequent degeneration of cartilage. However,
still there are patients in whom no cause can be clearly identified,
and these may represent a biologic condition that results in cartilage
failure. These patients represent primary osteoarthritis, which can be
considered a diagnosis of exclusion.
understanding of various mechanical problems, which may be termed
prearthritic conditions, whose natural histories show progression to
osteoarthritis. These conditions include mild hip dysplasia as well as
femoroacetabular impingement (FAI). FAI has become recognized as a
mechanical abnormality of the hip in which the anterior femoral neck
impinges on the acetabulum, leading to shear damage of the articular
cartilage. Two types of impingement have been described: cam type and
pincer type. Originally felt to possibly represent an asymptomatic or
subclinical slipped epiphysis, the cam type of impingement has been
shown to be a developmental abnormality. During development the femoral
head epiphysis and trochanteric apophysis share one physis, which
separates into two distinct growth plates around 4 years of age. A
delayed separation or abnormal, eccentric closure results in an
abnormal morphology typically affecting the anterolateral femoral neck.
The effect is a decreased head/neck offset, reducing the head/neck
ratio in this region and resulting in impingement of the anterior
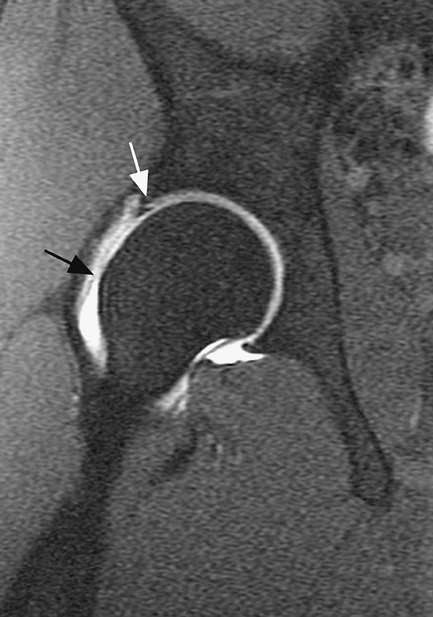
femoral neck with the anterior rim of the acetabulum (Fig. 3-1).
The pincer type of impingement is more a result of an acetabular
abnormality. Approximately 16% of dysplastic acetabula are retroverted.
This retroversion results in a relatively prominent anterior rim, also
causing impingement in flexion. Additionally, a deep acetabulum (coxa
profunda) may result in a prominent acetabular rim, causing
impingement. Both cam and pincer types of impingement may coexist.
|
TABLE 3-1 Arthritides Affecting the HIP
|
||
|---|---|---|
|
types of inflammatory arthritides. Rheumatoid arthritis is the most
common form of inflammatory arthritis. It has a prevalence of 0.3% to
1.5% in North America and is approximately 2.5 times more common in
women. The cause is thought to be an autoimmune cell-mediated response.
Further pathogenesis is discussed later. The inciting event that begins
the inflammatory response has yet to be identified, but is likely an
extrinsic factor (e.g., infectious, environmental) in a genetically
susceptible host. A genetic predisposition (HLA-B27) has also been
shown in seronegative (defined as rheumatoid factor–negative)
arthropathies; however, an infectious cause has been more closely
linked to certain types. Reactive and enteric spondyloarthropathies
have been associated with various gastrointestinal and genitourinary
infections.
factor responsible for most osteoarthritis, there are epidemiologic
factors as well. These epidemiologic factors may result in a
predisposition of the joint to osteoarthritis as a result of altered
mechanics or other yet to be defined biologic factors. Family and twin
studies have shown an increased prevalence of osteoarthritis within
families. Familial studies have documented an increased incidence in
first degree relatives, with 8% to 13% requiring hip replacement or
having symptoms of coxarthrosis. Twin studies further underscore the
hereditary component of osteoarthritis. Monozygotic female twins older
than 50 years of age have been shown to have an approximately 60%
heritability or genetic factor for the development of hip
osteoarthritis. Additional risk factors for the development of
osteoarthritis include increased age (older), race (whites [3% to 5%
prevalence] greater than in Asians), as well as gender. In those
younger than 50 years of age, men have a higher risk of developing hip
osteoarthritis; in those older than 50 years of age, women have a
greater incidence of the disease.
 |
|
Figure 3-1 Coronal oblique view of patient with cam type femoroacetabular impingement. Note the prominence of bone anteriorly (black arrow) resulting in poor head–neck offset and reduced head/neck ratio. Note also anterior labral tear (white arrow).
|
associated with osteoarthritis of the knee, the literature linking
obesity to hip disease is less well defined. Nevertheless, a growing
body of evidence now more strongly supports the relationship of obesity
to hip osteoarthritis. This relationship seems to be important even at
a younger age; increased body mass index (BMI) earlier in life (age 18)
is a stronger predictor for the development of osteoarthritis than
increases in BMI later in life and is associated with increased risk
for requiring hip replacement. Increased BMI is also associated with
changes in gait patterns. When comparing gait patterns of nonobese and
obese persons, changes in gait symmetry, stride width, and hip
abduction angles were noted,
suggesting
that a mechanical effect in obese patients could also result in the
development of OA. Yet other studies suggest that patients who are
obese suffer more hip complaints at the same radiographic stage than
nonobese patients, therefore making them more likely to seek hip
replacement at an earlier stage than nonobese patients. Possibly
therefore, the incidence of radiographic OA is similar in obese and
nonobese populations; however, obese populations are more symptomatic
and seek treatment sooner for a given stage of osteoarthritis. In
summary, studies have shown that obesity is a risk factor in the
development of hip osteoarthritis. This association is stronger for
women, in whom increased BMI early in life has been shown to be
associated with an increased incidence of OA.
 |
|
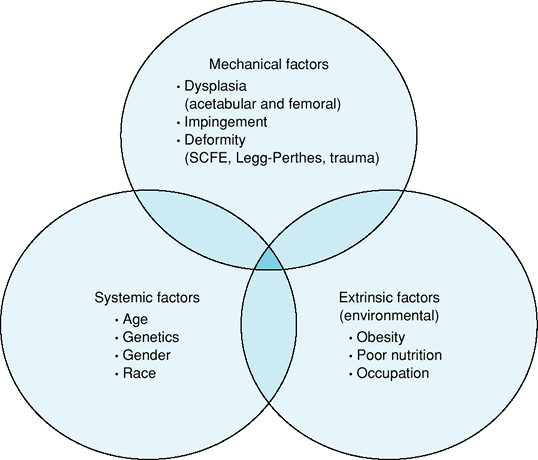
Figure 3-2 Etiologic factors associated with the development of osteoarthritis.
|
with osteoarthritis of the hip than that of the knee. However, some
population studies do suggest that occupation may have some influence
on the development of hip osteoarthritis such as the higher prevalence
of hip osteoarthritis in European farmers. Other studies have suggested
that high-demand recreational activities (professional soccer, track
and field, racket sports) may also contribute to hip arthritis. Figure 3-2 outlines various factors that contribute to the development of osteoarthritis.
times more common in women). A genetic predisposition is supported by
studies that show familial clustering and a higher prevalence in
monozygotic twins versus dizygotic twins, with monozygotes having a 3.5
greater chance of developing the disease. Further genetic
predisposition is supported by the higher prevalence in Native American
populations (5% to 6%). Seronegative arthropathies have a genetic
predisposition that is dependent on the prevalence of HLA-B27 in a
given population. Generally, the greater the prevalence of HLA-B27 in a
given population, the higher the prevalence of spondyloarthropathies.
HLA-B27 is common in certain Native American populations (up to 50%
positive), relatively common in Europeans (7% to 20%), less prevalent
in Asians and North American whites (7%), and uncommon in African
Americans (1% to 2%). Spondyloarthropathies occur in approximately 5%
to 14% of HLA-B27–positive individuals. Seronegative
spondyloarthropathies can also occur, less commonly, in individuals who
are HLA-B27–negative.
overload of the cartilage. In rare situations there is a true genetic
basis to joint destruction in which a generalized joint destruction
occurs as a result of a mutation that codes for type II collagen. Much
more commonly, the cartilage may be predisposed to damage because of
various mechanical conditions in the joint that result in a gradual
destruction of the cartilage. There is a failure of the chondrocytes to
maintain or repair damaged cartilage. Although chondrocytes are
metabolically more active in osteoarthritis, it is postulated that the
increased response is inadequate against the increased degradation of
products synthesized by the chondrocytes. Characteristic changes occur
within the cartilage structure, including changes in water content
(increased) and changes in proteoglycan concentrations (overall
decrease with shorter chains and increased chondroitin/keratin sulfate
ratio). Another characteristic change is collagen destruction:
Interleukin 1 (IL-1) from various cells (chondrocytes, synovial cells,
neutrophils)
regulates
the production of catabolic enzymes, e.g., metalloproteinases that
degrade the core protein of proteoglycans and collagenase resulting in
collagen destruction. IL-1 also influences the cartilage matrix by
causing a decreased synthesis of types II and IX collagen and an
increase in types I and III collagen.
is secondary to the inflammatory response, which begins in the
synovium. In early rheumatoid arthritis (RA), a microvascular synovial
injury appears to occur, resulting in edema and synovial cell
proliferation. Lymphocytes and macrophages infiltrate the synovium
early on, forming organized lymphoid tissue. Plasma cells are found in
more advanced disease. With synovial hyperplasia, the pannus of
synovium that extends to the edge of cartilage and bone begins to
invade and destroy the bone and cartilage. Synovial macrophages produce
cytokines (interleukin 1, tumor necrosis factor [TNF]-α and -β), which
in turn regulate the production of various degradative enzymes
(metalloproteinases, collagenase, stromelysin) by synovial fibroblasts
and chondrocytes, resulting in cartilage destruction. Bony erosions
result from multinucleated giant cells, which may originate from the
pannus, which is rich in macrophages. Rheumatoid synovial T cells have
been shown to produce osteoclast differentiation factor, which may be
responsible for the transformation of synovial macrophages into
multinucleated giant cells and the subsequent erosion of bone.
regardless of the cause. Occasionally, there are symptoms that may
differentiate osteoarthritis from inflammatory arthritis; however, both
may present with similar symptoms of hip pathology.
mechanical with activity-related pain or pain with certain motions
resulting from mechanical irritation or impingement. As the disease
progresses and becomes more severe, symptoms may also become more
constant and may include pain at rest.
involvement, either polyarticular or oligoarticular. It is rarely
monoarticular involving the hip. Although patients with inflammatory
disease may have hip symptoms that are mechanical in nature, these
patients tend to have a higher occurrence of constant hip pain or rest
pain because of chronic synovitis and hip joint effusion.
proximal anterior thigh (roughly 80% to 90% of patients). Pain often
radiates down the anterior thigh toward the knee. Buttock and lateral
thigh symptoms also occur in many patients, but these symptoms in
isolation are less common. The lateral proximal thigh pain is usually
felt more deeply and often more proximally (over the abductor muscles),
than symptoms of trochanteric bursitis, which are typically over the
posterolateral aspect of the greater trochanter and somewhat more
superficial. Occasionally patients present with isolated knee pain;
however, this pain tends to be more diffuse and slightly more proximal
than pain that originates from the knee.
Loss of motion, typically internal rotation, is one of the initial
findings. As the arthritis progresses, motion usually becomes more
restricted and may eventually result in a nearly ankylosed hip.
Adduction and flexion contractures typically occur. Patients may limp,
with a decreased stance phase on the affected side, and may show a
positive Duchenne sign because of pain and/or weakness. Patients with
inflammatory disease usually have less restriction in range of motion
unless the disease has caused severe erosion of the femoral head or a
significant protrusio deformity of the acetabulum resulting in a
captured femoral head.
loss is the general radiographic feature of arthritis. Specific
radiographic characteristics help differentiate osteoarthritis from
inflammatory arthritis. However, differentiation between these two
conditions occasionally can be difficult, and both may be present
radiographically.
are joint space narrowing, subchondral sclerosis, degenerative
subchondral cysts, and peripheral osteophytes. Occasionally the joint
space may still be well maintained, but the appearance is somewhat
irregular and other features such as peripheral osteophytes or evidence
of prearthritic conditions such as femoroacetabular impingement may be
present. Initially, the joint space narrowing is often asymmetrical
with either a superomedial or superolateral wear pattern. Eventually
the entire joint space may disappear. Radiographic features are more
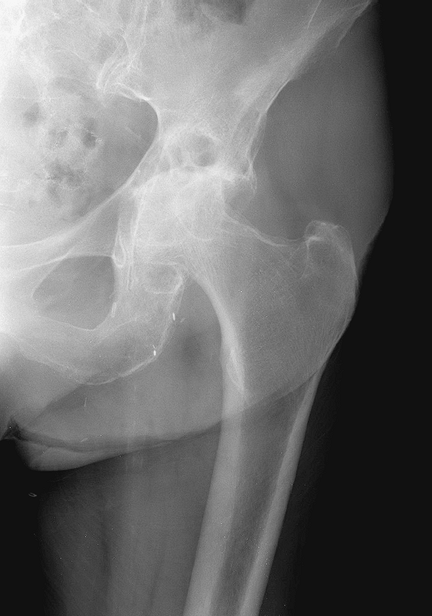
hypertrophic than those seen with inflammatory arthritis (Fig. 3-3).
symmetrical joint space narrowing with fewer hypertrophic changes.
Peripheral osteophytes, although often visible, are usually small.
Cystic changes are more evident than with osteoarthritis. Diffuse
osteopenia is characteristic of inflammatory changes. The wear pattern
is often symmetrical at onset, but may eventually lead to a more medial
wear pattern with a protrusio deformity of the acetabulum and
superomedial migration of the femoral head (Fig. 3-4).
described. It must be remembered that approximately 40% to 50% of
patients with radiographic changes of osteoarthritis are asymptomatic.
Joint space narrowing has been shown to correlate most strongly with
clinical symptoms. A number of grading systems are presented in Table 3-2.
with hip pain is to obtain good quality, properly exposed and oriented
radiographs with the appropriate views. In a properly oriented
anteroposterior pelvis radiograph, the
obturator
foramina appear symmetrical and the coccyx projects approximately 1 cm
above the pubicsymphysis. A true lateral radiograph also should be
obtained with attention focused on the contour of the anterior femoral
head/neck junction and also the anterior acetabulum. Together with a
thorough history, the large majority of conditions can be diagnosed
with the use of plain radiographs.
 |
|
Figure 3-3
Radiographic example of patient with osteoarthritis. Note the superolateral joint space narrowing, bony sclerosis, and large osteophytes. The changes are much more hypertrophic than that seen in inflammatory arthritis. |
 |
|
Figure 3-4
Radiographic example of patient with rheumatoid arthritis. Note the symmetrical joint space narrowing with an early protrusio deformity, and cystic changes. Large osteophytes are not present. |
 |
|
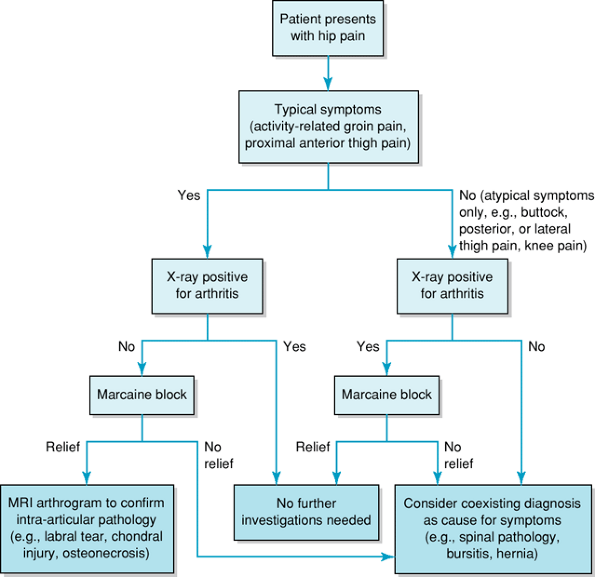
Figure 3-5 Diagnostic algorithm for patients presenting with hip pain.
|
radiographic features of arthritis. If the clinical presentation
correlates with the radiographs, then no further investigations are
necessary. Patients who present with radiographic changes of arthritis
but whose symptoms are atypical (isolated buttock, lateral hip or knee
pain) may be further evaluated with an intra-articular local anesthetic
injection placed under fluoroscopic guidance. If the symptoms are
temporarily relieved by the injection, then hip pathology is highly
likely. Patients who present with symptoms of hip pathology but whose
radiographs appear normal, despite close scrutiny for conditions such
as mild dysplasia, femoroacetabular impingement, or retroverted
acetabulum, may require further investigation, usually with an MRI
scan. If intra-articular pathology such as a labral tear is suspected,
then a gadolinium arthrogram MRI is most valuable. Figure 3-5 outlines a diagnostic algorithm for patients presenting with hip pain.
total hip replacement. However, various other procedures are indicated
for certain conditions. A more detailed discussion of specific
management will be presented in subsequent chapters. For an overview,
see Table 3-3.
the usual indication for surgery. Occasionally patients complain more
of restricted function and less of pain, but it is generally the pain
that results in the restricted function and is the reason why patients
seek hip replacement surgery. Prior to surgery, patients should receive
an appropriate coarse of nonoperative management. For osteoarthritis,
this includes activity modification, weight control if feasible, the
use of walking aids, and medications (nonnarcotic analgesics and
nonsteroidal anti-inflammatory medications). Presently, the routine use
of corticosteroid or hyaluronate hip injections cannot be recommended.
Patients with inflammatory arthritis are generally under the care of a
rheumatologist or internist for nonoperative
management. However, when considering surgery, certain considerations must be addressed; these are discussed below.
|
TABLE 3-3 Surgical Options for Patients with Osteoarthritis or Prearthritic Conditions
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||
rarely a disadvantage in delaying surgery as long as the patient is
able to maintain function. However, for conditions that may be
considered prearthritic (e.g., femoroacetabular impingement, dysplasia
without arthritic changes) there may be some merit in recommending
joint-sparing surgery when symptoms initially begin or are relatively
mild, rather than have the patient undergo a protracted coarse of
nonoperative treatment. Symptoms should still be significant enough to
justify the risks of surgery, but a long extensive coarse of
nonoperative management may be counterproductive because further
cartilage damage may occur during this time period. The goal of
nonarthroplasty joint-preservation surgery is to relieve symptoms and
if possible, also to alter the natural history and prevent or delay the
onset of arthritic changes; hence there may be an optimum window of
time in which such surgery is most successful. Unfortunately,
definitive data on altering of the natural history by
joint-preservation surgery is still lacking.
inflammatory arthritis should be counseled as to the risks, possible
complications, and usual recovery related to the procedure. Patients
should be medically stable, and any chronic medical conditions should
be assessed preoperatively and optimized prior to surgery. This
includes maintaining proper nutrition and also eliminating potential
sources of infection by specifically asking about their dental history
or any urinary problems. A careful skin evaluation is also necessary.
concerns that require consideration before surgery. These concerns
include polyarticular disease, medication used for management of
inflammatory disease, as well as unique reconstructive challenges
because of bone deformity or loss. Patients with inflammatory
arthritis, particularly rheumatoid disease, generally have
polyarticular involvement. Prior to surgery, C-spine lateral flexion
and extension views are necessary to exclude C1-C2 instability.
Additionally, in most circumstances, lower extremity surgery should be
planned prior to upper extremity surgery and hip replacement prior to
knee replacement when both are needed. It is more difficult for the
patient to regain knee motion if there is significant hip disease.
Patients with inflammatory disease are often on immunosuppressive
agents (corticosteroids, disease-modifying antirheumatic drugs—e.g.,
methotrexate, TNF-α antagonists). The use of these before surgery
should be reduced if possible or temporarily discontinued. This is
particularly true for TNF-α antagonists, which are potent immune
suppressors; continued use during the perioperative period may increase
the risk of infection. Last, patients with rheumatoid arthritis often
have osteopenic bone, which is at increased risk of intraoperative
fracture. These patients may also have acetabular bone loss related to
a protrusio deformity, which may require bone grafting or the use of
special implants (e.g., deep profile cup or in severe cases an
acetabular reconstruction cage). As in all reconstructive cases,
appropriate surgical planning is necessary to anticipate and have
available any special implants, instruments, or bone graft that may be
required.
WH, Bourne RB, Oh I. Intra-articular acetabular labrum: a possible
etiological factor in certain cases of osteoarthritis of the hip. J Bone Joint Surg. 1979;61A:510–514.
EW, Mandl LA, Aweh GN, et al. Total hip replacement due to
osteoarthritis: the importance of age, obesity and other modifiable
risk factors. Am J Med. 2003;114:93–98.
