Carpus Fractures and Dislocations
transfers the force and motion of the hand to the supporting forearm
and upper extremity. It allows a wide range of motion in two major
planes and, with its adjacent radioulnar joints, permits a substantial
rotatory arc around the longitudinal axis of the forearm. Unlike a
simple hinge joint such as the elbow, the wrist involves a delicate
interaction between eight carpal bones that are divided into two carpal
rows.39,100,110
While the main motions are flexion-extension and radioulnar deviation,
the primary axis of motion of the carpal bones resides within the head
of the capitate, which is not a singular point, but rather an oblique
screw axis for combined motions of wrist extension/ flexion and
radial/ulnar deviation.38,99,124
To produce this natural movement, individual carpal bones not only turn
up and down and back and forth, but also spin and roll about their own
axes.
The articular surfaces of the joints that make up the wrist have
important roles in subsequent integrated movements of the wrist. The
eight carpal bones are influenced by the shape of the distal radius,
the distal ulna, and the triangular fibrocartilage complex (TFCC).
 |
|
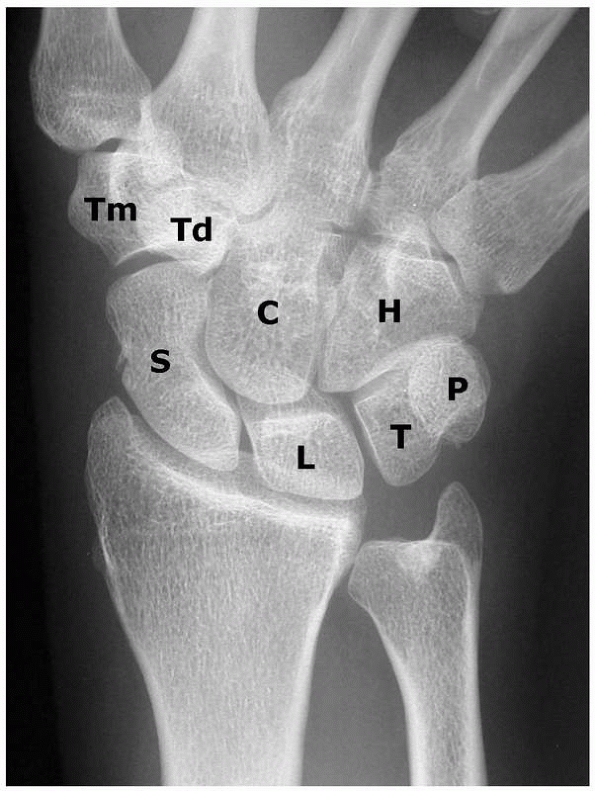
FIGURE 29-1
The wrist is composed of two rows of bones that provide motion and transfer forces. C, capitate; H, hamate; L, lunate; S, scaphoid; T, triquetrum; P, pisiform; Td, trapezoid; Tm, trapezium. |
and the triquetrum. The proximal carpal row is regarded by many authors
as an “intercalated segment” between the radius and the distal row, the
keystone in the coordination of motions of the wrist as well as in the
control of forces that are transmitted from the hand to the forearm and
vice versa. To cope with such an important role, the three proximal row
bones continuously need to adapt their position and orientation to
guarantee the necessary joint congruency between the radius and distal
row. Articular joint congruency depends on joint geometry and the
integrity of the ligaments that connect the three bones to each other
and to the surrounding bones, as the proximal carpal row has no direct
tendon attachments.56,100,110,113
of the flexor carpi ulnaris tendon; accordingly, it does not belong
directly to the proximal carpal row. It may stabilize the proximal
carpal row indirectly by acting on the triquetrum via the
pisotriquetral joint.
unit, consists of the trapezium, the trapezoid, the capitate, and the
hamate. The distal row forms a rigid, supportive transverse arch upon
which the five metacarpals of the hand are supported. The trapezium
articulates with the first metacarpal, the trapezoid with the second,
and the capitate with the third one. The capitate and trapezoid are
tightly connected to the metacarpals, whereas there is 30 to 40 degrees
of flexion-extension and rotation at the metacarpotrapezial joint. The
hamate articulates with the fourth and fifth metacarpal.
ulna, and metacarpals and are attached to roughened areas on the dorsal
and palmar surfaces. The transverse carpal ligament is an extrinsic
ligament that connects the scaphoid tuberosity and trapezial ridge with
the hamate and pisiform to provide structural integrity to the proximal
carpal arch. It also constrains the flexor tendons.
ligaments best observed from within the radiocarpal and midcarpal
joints. From an external view, the ligaments appear as condensations of
the fibrous capsule (Fig. 29-2) and are
difficult to distinguish through the superficial adventitia. They are,
however, quite prominent from the intra-articular aspect of the joint.39
originate laterally from a radial-palmar facet of the radial styloid
and are directed in a distal ulnar direction, where they meet ligaments
originating medially from the TFCC and the distal ulna.
the carpus from translating ulnarly on the medially angulated slope of
the distal radius. The palmar extrinsic ligaments consist of two
V-shaped ligamentous bands: one is proximal and connects the forearm to
the proximal carpal row and one is distal and connects the forearm to
the distal carpal row. The distal limb of the palmar extrinsic
ligaments consists of the radioscaphocapitate ligament laterally and
the ulnocapitate ligament medially
(Fig. 29-3).
The proximal limb consists of the radiolunatotriquetral and
radioscaphoid ligaments laterally and the ulnolunate und ulnotriquetral
ligaments medially.
 |
|
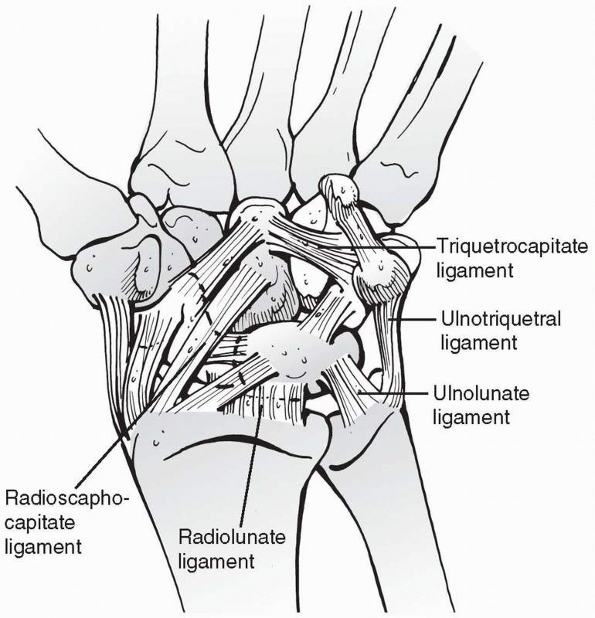
FIGURE 29-2
It is difficult to distinguish the extrinsic ligaments from the fibrous capsule; however, they are quite prominent from the intra-articular aspect of the joint. |
tuberosity of the scaphoid is the radial expansion of the
radioscaphocapitate ligament, which courses over the palmar concavity
of the scaphoid proximal to the tuberosity before inserting on the
palmar aspect of the keel and neck of the capitate.39
It appears to act as a sling across the waist of the scaphoid over
which the scaphoid rotates, and it usually does not have a ligamentous
insertion into the scaphoid itself.
ulnocapitate ligaments do not attach to the head of the capitate, but
form a support sling commonly referred to as the “arcuate ligament.”
Between these two rows of ligaments is a thinned area called the space
of Poirier.144 This area expands
when the wrist is dorsiflexed and disappears in palmarflexion. A rent
develops during dorsal dislocations, and it is through this interval
that the lunate displaces into the carpal canal.
been subdivided into short and long RL ligaments. The radioscapholunate
ligament originates from the palmar aspect of the ridge between the
scaphoid and lunate fossae and inserts into the scapholunate
interosseus ligament.102,178
The radioscapholunate ligament acts as a neurovascular supply to the
scapholunate interosseus membrane and it is not a true extrinsic
ligament of the wrist.
importance are the radiotriquetral and scaphotriquetral (dorsal
intercarpal) ligaments, which describe a V-shape from the dorsal aspect
of the distal radius near Lister’s tubercle to the triquetrum and then
back to the dorsal scaphoid rim. The radial capsule is thickened and
fused with the radioscaphoid ligament, while the ulnodorsal capsule is
augmented by the floors of the fifth and sixth dorsal compartments.
There are no true collateral ligaments.39
 |
|
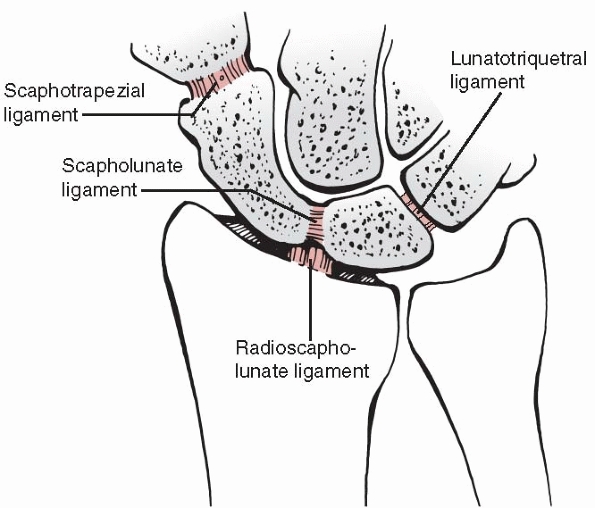
FIGURE 29-3
The palmar capsule consists of two major ligamentous inclusions: the RL ligament is the deeper of the two, which proceeds to the triquetrum and composes in effect the radiolunotriquetral ligament. The more distal and superficial component is often referred to as the arcuate ligament or distal V. The radial component of this ligament is the radioscaphocapitate ligament. The ulnar component of the arcuate ligament is the triquetrocapitate ligament. |
midcarpal joint and couple the distal carpal bones to each other. On
the radial side of the wrist, a V-shaped scaphotrapezial ligament
extends from the scaphoid tuberosity to the palmar tubercle of the
trapezium. Adjacent to it medially are the scaphocapitate and palmar
capitotrapezial ligaments and the capitotrapezoidal ligament. On the
ulnar side of the wrist, the triquetrocapitate and the triquetrohamate
ligaments are a continuation of the ulnotriquetral ligament.39
bones particularly the scaphoid, lunate, and triquetrum. They are
collections of relatively short fibers that bind the bones of either
the proximal or distal rows to each other.108,121,173
In the proximal carpal row, the ligaments are intra-articular,
connecting the scaphoid to the lunate and the lunate to the triquetrum (Fig. 29-4). There is a contiguous blending of the interosseous ligaments with the joint articular cartilage.
(SLIL) has been shown to consist of three components: palmar, central,
and dorsal. The scapholunate (SL) ligament has an important role in
carpal stability. The dorsal SL ligament is the key SL joint
stabilizer. It is formed by a thick collection of fibers
and
is transversely oriented, linking the dorsomedial edge of the scaphoid
to the dorsolateral rim of the lunate. The palmar SL ligament, a
secondary SL stabilizer, is formed by longer, more obliquely oriented
fibers. The long fibers of the palmar portion of the SL interosseous
membrane allow the scaphoid flexibility as it rotates on the lunate.
The dorsal third of the ligament is the strongest, while the palmar
ligament has more laxity. The central third appears to be a
fibrocartilaginous membrane which blends with the adjacent cartilage of
scaphoid and lunate. The membrane is thicker palmarly, as it
incorporates a richly vascularized expansion from the radioscapholunate
ligament.17,19,39,115,121
 |
|
FIGURE 29-4 The intra-articular intrinsic ligaments connect adjacent carpal bones.
|
similarly formed from two interosseous ligaments (palmar and dorsal)
connecting the proximal edges of triquetrum and lunate. It
interdigitates with the dorsal radiotriquetral ligament and palmar
ulnotriquetral, ulnolunate, and radiolunatotriquetral insertions. The
palmar third of the lunatotriquetral (LT) ligament is stronger than the
dorsal third being supported by strong palmar ulnocarpal ligaments. Its
fibers are tighter through all ranges of motion than the SL ligaments,
making for a closer kinematic relationship.39,121,173
come from the regional nerves and vessels. Circulation of the wrist is
obtained through the radial, ulnar, and anterior interosseous arteries
and the deep palmar arch. The extraosseous arterial pattern is formed
by an anastomotic network of three dorsal and three palmar arches
connected longitudinally at their medial and lateral borders by the
radial and ulnar arteries (Fig. 29-5). In
addition to transverse and longitudinal anastomoses, there are dorsal
to palmar interconnections between the dorsal and palmar branches of
the anterior interosseous artery.73,137,172
 |
|
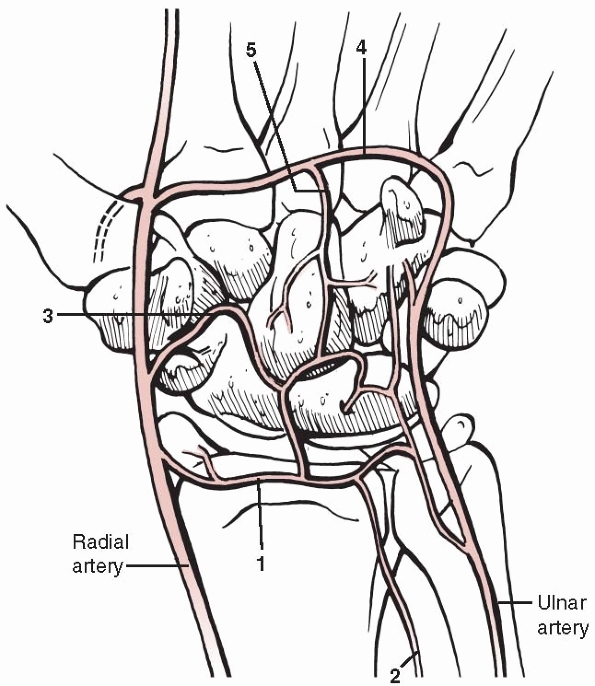
FIGURE 29-5
Schematic drawing of the arterial supply of the palmar aspect of the carpus. Circulation of the wrist is obtained through the radial, ulnar, and anterior interosseous arteries and the deep palmar arch. 1, palmar radiocarpal arch; 2, palmar branch of anterior interosseous artery; 3, palmar intercarpal arch; 4, deep palmar arch; 5, recurrent artery. |
-
The scaphoid, capitate, and about 20% of
all lunates are supplied by a single vessel and thus are at risk for
avascular necrosis. -
The trapezium, triquetrum, pisiform, and
80% of lunates receive nutrient arteries through two nonarticular
surfaces and have consistent intraosseous anastomoses. AVN is therefore
rare. -
The trapezoid and hamate lack an intraosseous anastomosis and, after fracture, can have avascular fragments.
that the blood supply to most carpal bones enters the distal half,
leaving the proximal half at risk. There is no interval, for example,
by which the scaphoid can be approached without endangering some of the
branches that supply its circulation. The lunate blood supply is
constantly endangered by common dorsal approaches to the wrist, but the
blood supply from the palmar radiocarpal arch is usually sufficient to
maintain its blood supply. With fracture-dislocations of the wrist, the
palmar radiocarpal arch usually remains intact, because the dislocation
is distal through the space of Poirier.
compression force applied with the wrist in hyperextension, in which
the palmar ligaments are placed under tension and the dorsal joint
surfaces are compressed and subject to shear stresses.39,111,113
Depending on the degree of radial or ulnar deviation, a ligament, bone
injury, or a combination of both will result. A scaphoid fracture
appears to occur when the wrist is dorsiflexed past 97
degrees
and radially deviated by 10 degrees. In this position, the proximal
pole of the scaphoid is securely held by the radius and the proximal
radioscaphocapitate ligament while the distal pole of the bone is
carried dorsally by the trapeziocapitate complex (Fig. 29-6).
The radioscaphoid ligament is relaxed by the radial deviation and
cannot alleviate the tensile stresses accumulating on the radiopalmar
aspect of the scaphoid. The fracture then propagates dorsally and can
be transverse, oblique, or comminuted depending on the direction of the
applied loads.198
 |
|
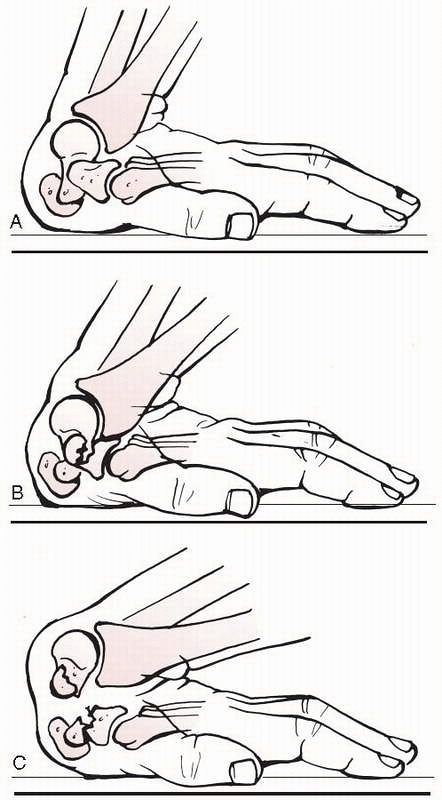
FIGURE 29-6 The most common mechanism of injury is an axial compressive force applied with the wrist in hyperextension. A-C.
The drawings show the fracture mechanism of the scaphoid where the proximal pole of the scaphoid is trapped between the radius and the tense palmar extrinsic ligaments; the full force is concentrated at the waist of the scaphoid. |
hand when an individual straightens the arm for protection and the body
weight and exterior forces are concentrated across the wrist. Other
mechanisms include palmarflexion, as occurs in an over-the-handlebars
motorcycle accident, or twisting injuries in sports where the hand is
forcefully rotated against the stationary body. Ligament tears involve
more substantial force to the hand. High-energy forces result in carpal
bone fractures or ligamentous disruptions of both intrinsic and
extrinsic ligaments and perilunate dislocations. The majority of these
injuries occur around the lunate, which as the carpal keystone is held
most securely to the distal radius. Several authors39,122
have shown that many injuries to the wrist appear to be sequential
variants of perilunate dislocation. Minor injuries, such as sprains,
result from low-energy forces.
flexion-extension, radioulnar deviation at the radiocarpal joint, and
axial rotation around the distal radioulnar joint (DRUJ).110
The radiocarpal articulation acts as a universal joint allowing a small
degree of intercarpal motion around the longitudinal axis related to
the rotation of individual carpal bones. The forearm accounts for about
140 degrees of rotation. Radiocarpal joint motion is primarily
flexion-extension of nearly equal proportions (70 degrees), and radial
and ulnar deviation of 20 and 40 degrees, respectively. This amount of
motion is possible as a result of complex arrangements between the two
carpal rows. During flexion and extension, each carpal row angulates in
the same direction with nearly equal amplitude and in a synchronous
fashion (Fig. 29-7).29,53,110,124
Much of the wrist’s versatility, however, is due to the intercalated
three-bone system of the proximal carpal row. During radioulnar
deviation, the proximal row exhibits a secondary angulation in the
sagittal plane to the synchronous motion occurring in the coronal
plane. Radial deviation induces flexion of the obliquely situated
scaphoid as the trapezium approaches the radius. Through the dorsal
aspect of the SL ligament, this motion is transmitted sequentially to
the lunate and triquetrum, which flex approximately 25 degrees.39,110,115
As the carpus moves back to neutral and onto full ulnar deviation, the
proximal row extends and supinates with respect to the radius.
deviation, but it is the proximal migration of the hamate that forces
the triquetrum to displace palmarly and extend, bringing the lunate
with it. This rotation, by varying the length and contour of the
proximal carpal row, allows for extensive excursion of the wrist while
maintaining stability around a longitudinal axis. This has been
described as the “variable geometry” of the proximal carpal row. When
this mechanism is disrupted by fracture or ligamentous injury, the
wrist becomes destabilized. The usual arcs of motion are no longer
synchronous, and the intercarpal contact patterns change. A snap,
catch, or clunk can be appreciated with motion of the wrist,
particularly when under compressive load. Instability leads, in time,
to degenerative changes as a consequence of increased shear forces and
abnormal contact between individual carpal bones.
of the wrist is located within a small area in the capitate neck. A
line drawn through the axis of rotation parallel with the anatomic axis
of the forearm will, with the hand in neutral position, pass through
the head and base of the third metacarpal, the capitate, the radial
aspect of the lunate, and the center of the lunate fossa of the radius.124
In the sagittal plane with the wrist in neutral flexion-extension, a
line passing through the longitudinal axis of the capitate, lunate, and
radius will show these to be nearly superimposed or colinear. The
scaphoid axis lies at 45 degrees to this line and passes between the
lunate and capitate in a fashion that provides optimal stability to the
midcarpal joint. The scaphoid acts as a stabilizing strut or column to
support the central column. By virtue of its obliquity, the scaphoid
will flex when under compression and exerts a similar force on the
lunate. The lunate, however, is also under the influence of the
triquetrum, which inherently prefers to extend. For this reason, the
lunate may be thought of being in a state of dynamic balance between
two antagonists. It tends to lie in the position of least mechanical
potential energy.39
 |
|
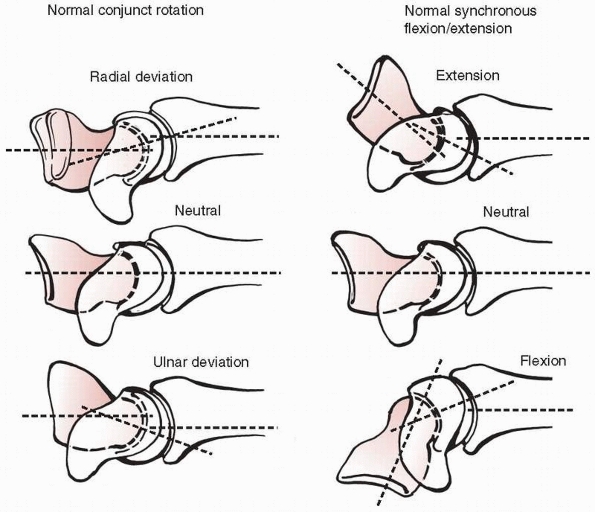
FIGURE 29-7
Conjunct rotation of the entire proximal row occurs in flexion during radial deviation (upper left). The axes of the radius and carpal rows are collinear in neutral (middle left), and the proximal row extends with ulnar deviation (lower left). Angulatory excursions of the proximal and distal rows are essentially equal in amplitude and direction during extension (upper right) and flexion (lower right). This has been described as synchronous angulation. |
When the lunate slips into a statically fixed position of flexion of
more than 15 degrees, volar intercalated segment instability (VISI) is
present. VISI is typical of LT dissociation (LTD), nondissociative
carpal instability, and a carpal instability complex in which
associated instabilities are also present.
10 degrees, dorsal intercalated segment instability (DISI) is present.
The relative alignment of the scaphoid to the lunate, which is usually
about 45 degrees, is important. When this exceeds 70 degrees, the
ligamentous linkage between the scaphoid and lunate is usually
inoperative. The lunate then generally adopts an extended position
(i.e., DISI) and maintains this position even during radial deviation,
thus interrupting the normal rotation and the spatial adaptability of
the proximal row. The same is true when the lunate is fixed in flexion
in a VISI deformity. The wrist will not extend even during ulnar
deviation. A DISI deformity is rarely seen in acute scaphoid fractures,
where it indicates gross carpal instability. It is more often seen in
association with scaphoid pseudarthrosis and scapholunate dissociation,
where it indicates the degree of carpal collapse deformity that has
occurred. In advanced cases, the capitolunate joint becomes subluxed
and may show signs of degenerative arthritis.85
the outstretched hand led to an injury of the wrist or to an injury of
the carpus.
The
four standard views to diagnose an injury are the anteroposterior (AP)
and lateral radiographs, each taken in the exactly neutral position,
and the radial oblique (supinated AP) and ulnar oblique views (Fig. 29-9). These four standard views detect most carpal injuries,67
but the neutral AP view is probably the most misleading as the tubercle
overhangs the waist of the scaphoid in this view and can obscure a
fracture.36 If there is the
suspicion of carpal instability, additional views in maximal radial and
ulnar deviation are recommended. Although most scaphoid fractures will
be detected by the four standard views, further views should be taken
if there is strong clinical suspicion of the presence of an undetected
fracture. Useful views are summarized in Table 29-1.36
 |
|
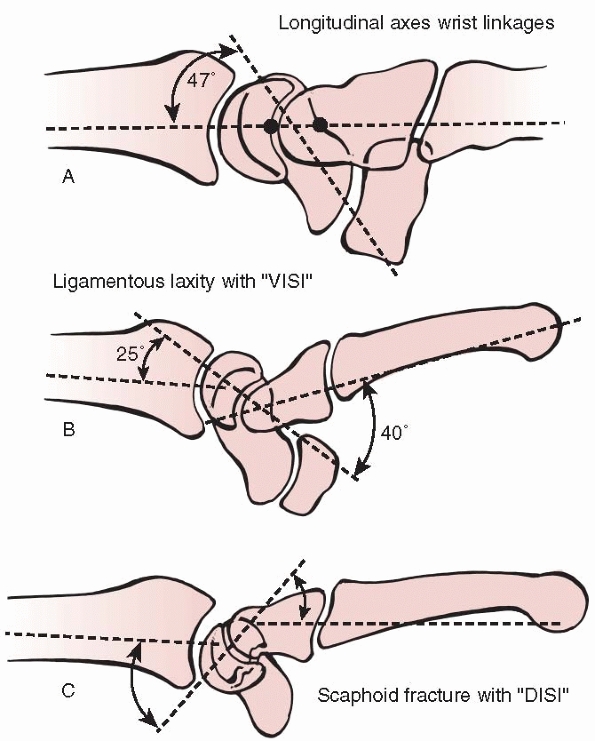
FIGURE 29-8 Schematic drawing of carpal instability. A.
Normal longitudinal alignment of the carpal bones with the scaphoid axis at a 47-degree angle to the axes of the capitate, lunate, and radius. B. VISI deformity is usually associated with disruption of the LT ligament. C. DISI deformity is associated with SL ligament disruption or a displaced scaphoid fracture. |
 |
|
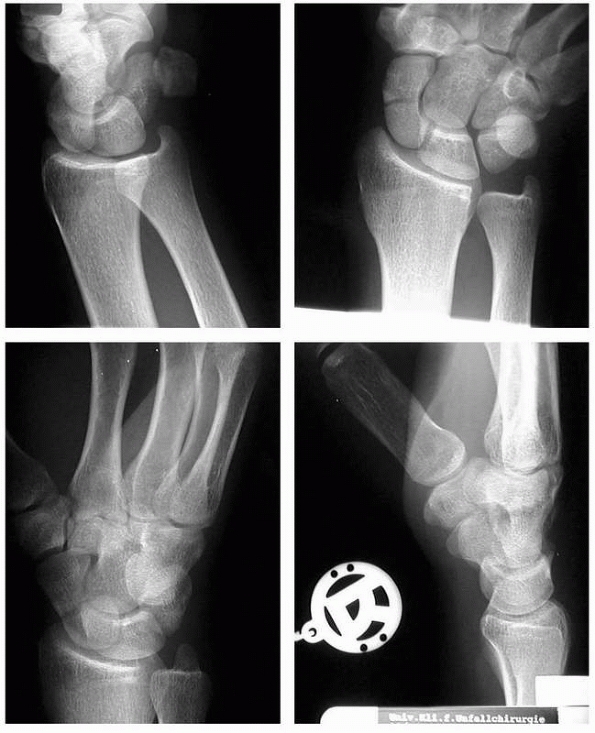
FIGURE 29-9
The four scaphoid views (AP, true lateral, radial oblique, ulnar oblique) detect most of carpal fractures. A fisted AP view can be helpful in detecting scaphoid fractures |
position, the longitudinal axes of the long finger metacarpal,
capitate, lunate, and the radius all fall in the same line. The
longitudinal axis of the scaphoid can be drawn through the midpoints of
its proximal and distal poles. Using these axes, it is possible to
measure angles that define the positions of the carpal bones. For
example, the scapholunate angle averages 45 degrees, and ranges from 30
to 60 degrees in normal wrists. An angle greater than 70 degrees
suggests instability, and one greater than 80 degrees is almost certain
proof of carpal instability or displacement. A capitolunate angle of
more than 20 degrees is also strongly suggestive of carpal instability.
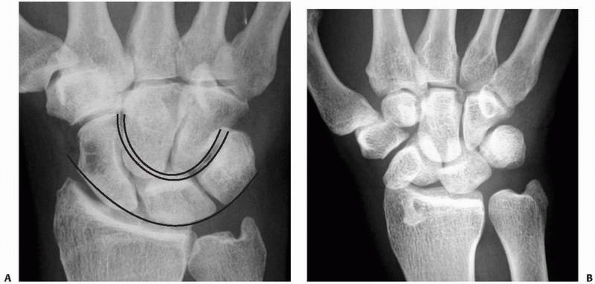
be examined on the AP view. Disruption of these arcs indicates
ligamentous instability.77 The
assessment of Gilula’s line continuity should be a standard in the
evaluation of all AP wrist radiographs to prevent a missed diagnosis of
a perilunate dislocation (Fig. 29-10).
|
TABLE 29-1 Radiologic Views for Detection and Assessment of Scaphoid Fractures
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
radiographs. The DISI pattern is most commonly observed with displaced
scaphoid fractures and scapholunate dissociation (SLD), while the VISI
pattern is more likely to be associated with LTD.
radiograph should show a constant space between scaphoid, lunate, and
triquetrum, which is maintained throughout the range of motion. The
joint space between scaphoid and lunate is usually 1 to 2 mm. With SLD,
an increasing gap appears which may in time be wide enough to accept
proximal migration of the entire capitate head. A spread of more than 3
mm is considered abnormal, and a gap greater than 5 mm is confirmatory
of an SL injury. In addition, the scaphoid flexes palmarward which
gives it less of an elongated profile on the AP view and projects the
cortical waist of the scaphoid as an overlapping ring of bone inside
the scaphoid projection, also known as the “the cortical ring sign.”
The lunate also moves into a DISI position, which can be visualized on
the AP view by the increasing overlap of the capitate silhouette by a
lunate horn producing a wedge shape (Fig 29-10B).
With LTD, a gap between the two bones is not usually evident, but a
break in the normal carpal arc of the proximal carpal row can be seen.
the length of the third metacarpal, is used to quantify carpal
collapse. One method of measuring carpal height is to determine the
distance between the base of the third metacarpal and the articular
surface of the distal radius using a line bisecting the middle of the
radius and metacarpal. The carpal height ratio, however, is of little
significance in assessing ligament damage in wrist hyperextension
injuries.
 |
|
FIGURE 29-10 Gilula’s lines. A.
AP views show three smooth Gilula arcs in a normal wrist. These arcs outline proximal and distal surfaces of the proximal carpal row and the proximal cortical margins of capitate and hamate. B. Arc I is broken, which indicates an abnormal lunotriquetral joint due to a perilunate dislocation. Additional findings are the cortical ring sign produced by the cortical outline of the distal pole of the scaphoid and a trapezoidal shape of the lunate. |
arthrography, videoradiography, and arthroscopy can assist in the
diagnosis of carpal ligament injuries.25,39
Computed tomography (CT) scans are helpful in evaluating carpal
fractures, malunion, nonunion, and bone loss. Three-dimensional imaging
is of use in planning reconstructive procedures for malunions and
nonunions. Macroradiography does not show any advantage in diagnosing
carpal fractures, particularly scaphoid fractures compared to normal
radiographs.50
-
Standard scaphoid views detect most carpal injuries.
-
A DISI pattern is most commonly observed with displaced scaphoid fractures and SLD.
-
A VISI pattern is more likely to be associated with LTD.
-
MRI scans are useful in detecting occult fractures, AVN of the carpal bones, and ligamentous injuries.
-
Perilunate dislocations are easily missed if the continuity of Gilula’s line is not assessed.
1889 by Cousin and Destot before the discovery of radiographs. They
were also well described by Mouchet and Jeanne in 1919. The position of
the scaphoid on the radial side of the wrist, as the proximal extension
of the thumb ray, makes it vulnerable to injury.
the annual incidence of carpal fractures is 39.7 per 100,000 of the
population per year in the United Kingdom. Scaphoid fractures account
for 2.9% of all fractures and for 69% of all carpal injuries (see Table 3-18).
Scaphoid fractures are common among young men with a male to female
ratio of 71:29 and an average age of 35 years. The average time for
healing of a nondisplaced scaphoid fracture in a cast is 8 to 12 weeks,
accounting for a considerable loss of time and productivity in this
young and active population.14,39,65,121,144,152,173,184
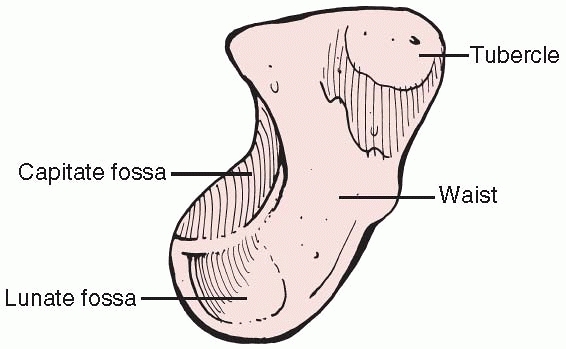
body. It is an irregularly shaped tubular bone, twisted, and bent into
an S-shape (Fig. 29-11). It resembles a
deformed peanut or a boat (in Greek, skaphos means boat). It lies
entirely within the wrist joint, with more than 80% of its surface
being covered by articular cartilage,69
which reduces its capacity for periosteal healing and increases its
tendency to delayed union and nonunion. The scaphoid is located in a
45-degree plane to the longitudinal and horizontal axis of the wrist.
 |
|
FIGURE 29-11 Schematic drawing of the scaphoid.
|
articulates like a socket with the spherical head of the capitate.
Proximally, there is a small, semilunar facet for articulation with the
lunate. The proximal third of the radial surface is convex and
articulates with the radius. Distal to this articulation is the waist,
grooved on its palmar surface by the radioscaphocapitate ligament which
acts as a sling across the waist of the scaphoid although it has no
connection to the bone itself. Taleisnik174
suggested that the radioscaphocapitate ligament provided a fulcrum for
the scaphoid. The scaphoid is ridged across its nonarticular
dorsoradial surface, along which the critical dorsal ridge vessels
traverse. The ridge acts as an insertion point for both the dorsal
component of the SLIL,17 as well as the intercarpal ligament.129
The distal pole is pronated, flexed, and ulnarly angulated with respect
to the proximal pole and presents separate articular surfaces to the
trapezium and trapezoid distally.173
that attach it to the lunate and distally to the trapezium and
trapezoid. Motion in these joints is restricted by the strong
ligaments, which permit a degree of rotation proximally and a degree of
gliding distally.85 These ligaments
merge with the extrinsic ligaments and capsule, which are loose enough
to allow free motion of the scaphoid within the wrist. Otherwise, the
scaphoid has no ligamentous or tendinous attachments and acts with the
rest of the proximal carpal row as an “intercalated segment.”
connecting the proximal and distal carpal rows. Any shear strain that
occurs across the midcarpal joint is transferred through the scaphoid
and may cause fractures and dislocations. Through its stout proximal
and distal ligamentous connections, the scaphoid serves to coordinate
and smooth the motions of the proximal and distal rows, and it has been
likened to a slider-crank mechanism that stabilizes an inherently
unstable dual link system as the midcarpal joint tends to assume a
lunate-extended posture unless constrained by an intact scaphoid.113,207
The kinematic effect of an unstable scaphoid fracture is a dissociation
of the proximal and distal carpal rows that permits the natural
tendency of the two carpal rows to fail by collapsing. This is
demonstrated clinically by the collapse pattern seen with chronic
scaphoid nonunion, a condition called “scaphoid nonunion advanced
collapse” appearing as DISI.56,165,207 Under axial load, the two halves of the scaphoid collapse into a flexed or “humpback” posture.6,154
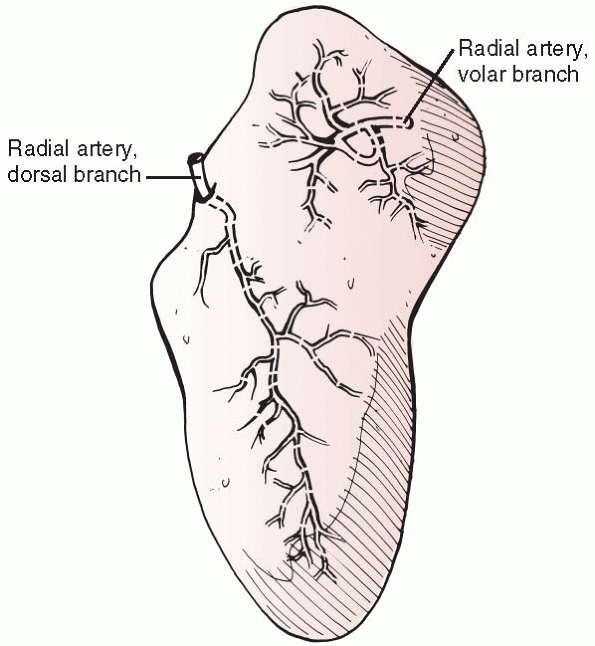
One enters the scaphoid tubercle and supplies its distal 20% to 30% and
the other arises from the dorsal scaphoid branch of the radial artery (Fig. 29-12).
The dorsal ridge vessels enter through numerous small foramina along
the spiral groove and dorsal ridge. This source accounts for about 80%
of the blood supply. Several studies have shown no vascular supply or
only a single perforator proximal to the waist of the scaphoid.74,134
Because of its unusual retrograde vascular supply, the scaphoid has a
high risk of nonunion and AVN after fracture. Temporary interruption of
the blood supply to the proximal fragment is virtually certain with
proximal pole fractures but, if stabilized, the proximal pole has the
capacity to revascularize and heal.76,118,207
 |
|
FIGURE 29-12 The vascular supply of the scaphoid is provided by two vascular pedicles.
|
reveals that scaphoid fractures are common in young men due to falls
(40.7%) and sporting injuries (32.8%). High-energy injury is much less
common, occurring in just over 10% of cases.
bending with compression dorsally and tension on the palmar surface,
due to forced dorsiflexion of the wrist. When the wrist is extended
beyond 95 degrees, the proximal pole of the scaphoid is tightly held
between the capitate, the dorsal lip of the radius, and the taut palmar
capsule. Fracture of the scaphoid occurs at the waist which is exposed
to the maximal bending movement.198 However, scaphoid fractures can be caused by several other mechanisms.14
The force must be sufficient to produce at least a transient
subluxation of the joint. This is only one step away from the classic
transscaphoid perilunate fracture-dislocation that results from more
severe trauma. Thus, there must be a subtle difference between the
degree of force required to produce an occult fracture, a complete but
stable fracture, or an unstable fracture of the scaphoid. Herbert85
stated that since the line of the midcarpal joint crosses the proximal
pole in radial deviation and the distal pole in ulnar deviation, the
wrist deviation at the time of injury might determine the line of
fracture. Fractures of the waist are usually the result of shear forces
across the scaphoid. Fractures of the tubercle, like radial styloid
fractures, appear to be caused by either compression or avulsion.56,144 Compson36
suggested that the size of a proximal pole fracture depends on the
level of the proximal extent of the joint facet with the capitate,
which is the most variable aspect of scaphoid anatomy and accounts for
the variation in the size of proximal pole fracture. Smaller
proximal pole fractures can also be caused by an avulsion of the attachment of the SL ligament.
 |
|
FIGURE 29-13 A,B. Symptomatic scaphoid nonunion in a 12-year-old boy because of a fall 2 months prior.
|
physis of the distal radius usually fails first. However, scaphoid
fractures can occur in children, and radiographs are mandatory to
diagnose this injury (Fig. 29-13A,B).
Concomitant fractures of the distal radius and scaphoid have been
reported. Most fractures heal with cast at an average of 6 to 8 weeks;
however, nonunion and AVN can occur.50,80,187 In the elderly, the distal radial metaphysis usually fractures before the scaphoid.
functional disability as well as time off work, loss of earnings, and
interference with recreational activities. A common problem with the
fractured scaphoid is diagnosis,65 and posttraumatic complications include pain, dysfunction, malunion, delayed union, and nonunion.
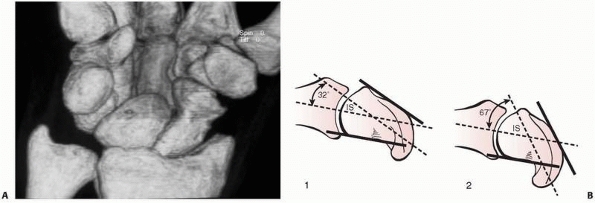
scaphoid tends to flex and the proximal scaphoid extends with the
proximal carpal row, initially causing a dorsal fracture gap followed
by the humpback deformity (Fig. 29-14).56
Despite the lack of direct tendon attachments, joint compressive
forces, trapezium-scaphoid shear stress, and capitolunate rotation
moments all act on the fractured scaphoid. The scaphoid often assumes
an anteverted position, the lunate and triquetrum subluxate forward and
rotate dorsally, and the capitate and hamate subluxate dorsally and
proximally, producing the DISI deformity (see Fig. 29-8C).69
As a consequence of these mechanical factors, as well as the critical
vascularity of the scaphoid bone, scaphoid fractures have a high
tendency to delayed union and nonunion. Nonunion of the scaphoid is a
severe problem, causing arthritis secondary to abnormal loading on the
articular surfaces of the midcarpal joint, pain, and weakness.
 |
|
FIGURE 29-14 A. CT scan of a scaphoid fracture that has healed with a humpback deformity. B.
Schematic drawing of scaphoid: (1) normal scaphoid, (2) humpback deformity. The normal intrascaphoid angle (IS) is 30 degrees ± 5 degrees. The humpback deformity angle measure 67 degrees and the normal scaphoid 32 degrees. |
wrist pain after a fall on the outstretched hand. The diagnosis of a
scaphoid fracture is made from the clinical history with about 90% of
patients recalling a hyperextension injury, the clinical examination
where the index of suspicion is raised, and by proper radiographic
examination which confirms the diagnosis. The importance of obtaining
an accurate history cannot be overestimated because both treatment and
prognosis depend on the type of fracture and fracture mechanism.85 It is important to inquire carefully about previous trauma and not to treat a nonunion as
if it was an acute fracture. Although tenderness in the anatomic
snuffbox has been described as a classic finding in scaphoid fractures,
it is an overly sensitive test that is notoriously inaccurate when used
in isolation.62,141
Swelling and pain are usually apparent in acute fractures; however,
these symptoms can be minimal. After 24 hours, there is often diffuse
pain and swelling. Pain in the anatomic snuff box may be elicited with
longitudinal thumb compression, on either radial or ulnar deviation
with pronation, and using the Kirk-Watson test (see below).
found that any the use of one clinical tests in isolation was
inadequate but that a combination of snuffbox tenderness, scaphoid
tubercle tenderness, and pain with axial compression yielded a
sensitivity of 100% and a specificity of 74%. However, their findings
were only valid in the first 24 hours after fracture.
scaphoid fractures associated with carpal collapse deformity and palmar
capsular contracture. Missed diagnosis is not uncommon and often
results in additional morbidity from secondary changes, including
nonunion, collapse deformity, and degenerative arthritis.
diagnosis of scaphoid fracture is usually made by radiograph.
Radiographic diagnosis of a scaphoid fracture requires four
radiographs: an AP view with the hand in a fist to extend the scaphoid,
a lateral view, a radial oblique (supinated AP) view, and an ulnar
oblique view (see Fig. 29-9). These four views detect most scaphoid fractures.26,67,85,184
Comparative views of the opposite uninjured wrist are often helpful. It
is difficult to diagnose scaphoid fractures on the lateral radiograph,
although this radiograph is essential to diagnose perilunate
fracture-dislocations and to evaluate the overall alignment of the
carpus.
|
TABLE 29-2 Reliability of the Clinical Signs of Scaphoid Fracture
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
-
A dark line may be formed by the dorsal lip of the radius overlapping the scaphoid.
-
The presence of a white line formed by the proximal end of the scaphoid tuberosity
-
The dorsal ridge of the scaphoid may appear bent on the semisupinated view.
radioulnar deviation) may demonstrate fracture displacement, which
indicates an unstable scaphoid fracture. Since the scaphoid flexes in
radial deviation and extends in ulnar deviation, the length of bone
should be assessed by comparing ulnar and radial deviation views in
both wrists. Assuming that the two views are identical, any difference
in length must indicate a scaphoid deformity resulting from either a
fracture or ligament injury.85 When
instability of the scaphoid is suspected, careful analysis of the
lateral radiograph for intrascaphoid angulation or a dorsally tilted
lunate is recommended.
fractures may not be visible on the initial set of radiographs,
although it has been shown that this is rarely the case if they are
evaluated by experienced observers.14,67 Clinical studies7
have shown that scaphoid and pronator fat stripe signs are poor
predictors of the presence or absence of underlying occult fractures.
If there is clinical suspicion but radiographs are negative, a scaphoid
cast is applied and another set of scaphoid views is performed after 10
days (Fig. 29-15).67 As most of the patients with suspected scaphoid fractures are young and active, early diagnosis is important. Macroradiography66 and ultrasound132
have a sensitivity of less than 50% in detecting occult scaphoid
fractures. MRI scans are the most effective way of diagnosing scaphoid
fractures (Fig. 29-16).27,65
It has been shown that an MRI performed as early as 48 hours after the
injury has a sensitivity and specificity approaching 100% and may have
the potential to save as much as $7200 per 100,000 inhabitants by
avoiding loss of productivity due to unnecessary cast immobilization.65 Technetium-99m bone scans28,180
also have a high sensitivity in diagnosing occult fractures of the
carpus. CT scans have the advantage of speed and can produce high
resolution fine-cut
images of the scaphoid in multiple planes.150 Three-dimensional reconstructions of these scans can be helpful for planning operative procedures of scaphoid reconstruction.
 |
|
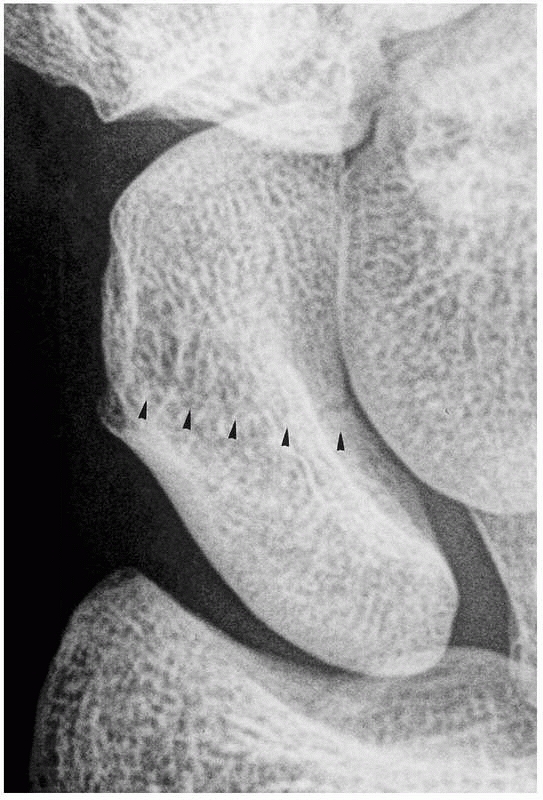
FIGURE 29-15
An occult fracture was detected 10 days after a fall on the outstretched hand. This fracture was not visible on the initial set of radiographs |
scaphoid nonunion is important for planning treatment, and good
radiographs should distinguish between the two,39
although an MRI scan may be helpful. Not uncommonly, a second injury
will draw attention to a minimally symptomatic nonunion which has been
aggravated by the recent event. The acute scaphoid fracture is
represented by a single line through the bone, occasionally with
dorsoradial comminution and dorsal angulation. Late presentation of a
fracture or an established nonunion may show resorption at the fracture
site, subchondral sclerosis, and displacement on both the AP and
lateral radiographs. The longer the time since injury, the greater the
cystic resorption, the denser the sclerosis, the more prominent the
shortening of the scaphoid, and the greater the loss of carpal height.85 Secondary degenerative changes are usually present by 10 to 15 years.
 |
|
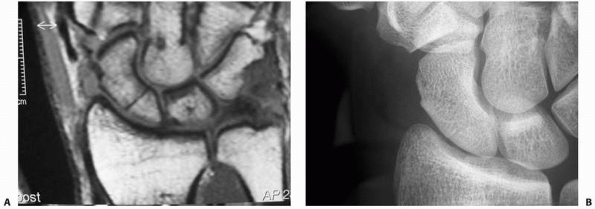
FIGURE 29-16 A. The MRI scan demonstrates a clear fracture line of the scaphoid (proximal pole). B. It is difficult to identify the proximal fracture by native radiographs.
|
 |
|
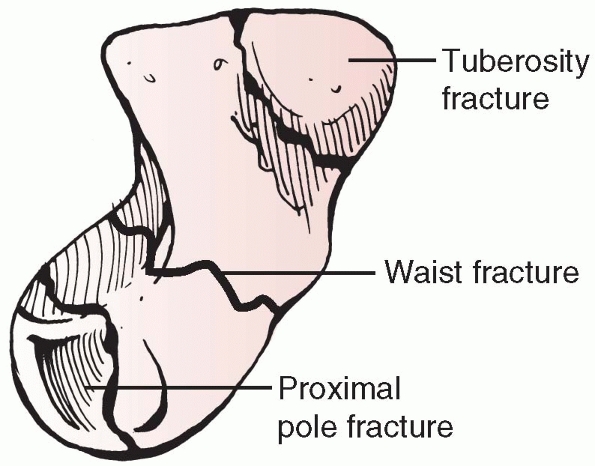
FIGURE 29-17 Classification of scaphoid fractures by anatomic location.
|
injuries such as perilunate dislocation and transscaphoid perilunate
fracture-dislocations may occur. Whatever the mechanism of scaphoid
fracture, it is important to remember that a radiograph never reveals
the true degree of joint and ligament damage that inevitably
accompanies this injury.85
some of whom attempt to correlate fracture union rate with the site of
injury (Fig. 29-17). Waist fractures account
for 65% of scaphoid fractures, with a further 26% being in the proximal
pole with 9% either in the tuberosity or distal articular fractures.
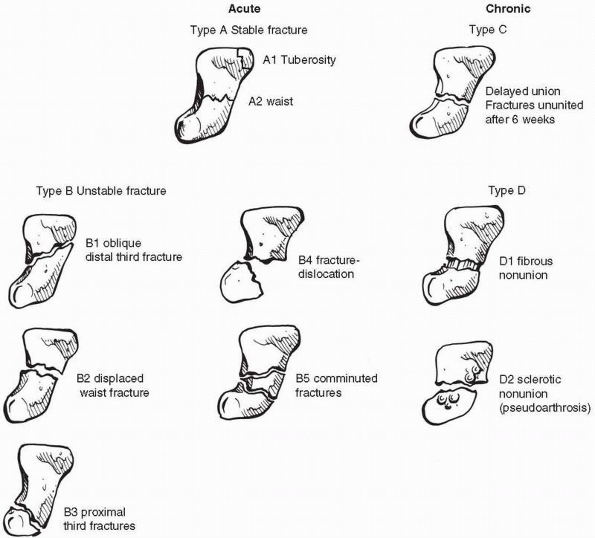
Herbert and Fisher68 proposed a classification intended to identify those fractures most applicable for operative fixation (Table 29-3 and Fig. 29-18).
They recommended early operative management of all acute fractures of
the scaphoid waist or proximal pole because of the incidence of
displacement or nonunion.
fracture location. Gelberman’s work74,75,137
confirmed earlier studies by demonstrating that the major blood supply
comes from the scaphoid branches of the radial artery which enter the
dorsal ridge and supply 70% to 80% of the bone, including the proximal
pole. The second major group of vessels enters the scaphoid tubercle,
perfusing only the distal 20% to 30% of the bone. In fractures through
the waist and proximal third, revascularization will occur only with
fracture healing. One can reasonably assume that, with proper
treatment, nearly 100% of tuberosity and distal third scaphoid
fractures will heal, as will 80% to 90% of waist fractures, but only
60% to 70% of proximal pole fractures will heal.39,85
Similarly, union in oblique or shear fractures has been shown to be
delayed in comparison to horizontal fractures. Comminuted or distracted
osteochondral fractures have the poorest rate of union. The healing
time for these different fracture types ranges from 4 to 6 weeks for
tuberosity fractures, 6 to 8 weeks for occult and stable fractures, 10
to 12 weeks for distal third and waist fractures, and 12 to 20 weeks
for comminuted and proximal pole fractures.
|
TABLE 29-3 Classification of Scaphoid Fractures
|
||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||
not be visible on the initial set of radiographs. Patients with wrist
injuries are usually seen in the emergency department by less
experienced doctors who are aware of the dangers of missing a scaphoid
fracture and who know that up to 30% of all scaphoid fractures might
not be detected on initial radiographs.14,67,133
Knowledge of the poor outcome of undiagnosed and untreated scaphoid
fractures ending in pseudarthrosis of the scaphoid and severe
radiocarpal arthritis leads to a tendency to overtreatment. To avoid
missing a few occult fractures of the scaphoid, some patients are
immobilized for prolonged periods of time without a diagnosis being
made before being seen by a senior surgeon.16,146
are reliable methods of diagnosing occult fractures of the scaphoid.
MRI has a higher sensitivity and specificity in the diagnosis of occult
fractures of the scaphoid compared to other methods of diagnosis and
might even be more cost effective than repeated clinical examinations
and radiographs.65 However, most
countries do not have the facilities to refer patients with supposedly
minor injuries for an MRI scan. The literature states that there is low
inter- and intraobserver reliability in diagnosing occult scaphoid
fractures on plain radiographs.179,180
Scaphoid fractures and other injuries to the wrist might not be very
painful initially, although persisting pain clearly indicates an
injury. The diagnosis is usually made by a combination of clinical and
radiologic findings,85 which means that the evaluation of radiographs even by experienced radiologists can lead to poor diagnostic results.179
If an occult fracture of the scaphoid or severe concomitant wrist
injury is suspected but not visible on initial radiographs, the wrist
should be immobilized for 10 days in a forearm cast or splint, and the
patient should be seen by an experienced surgeon and a repeat scaphoid
series should be obtained. However, a prospective study has shown that
70% of all occult scaphoid fractures and 60% of avulsion fractures are
visible on the initial set of radiographs.67
There is little doubt that MRI scans are the most reliable method of
diagnosing occult carpal and wrist fractures at an early stage.27,65
However, it has been shown that that repeated clinical examinations and
radiographs can also detect occult fractures of the scaphoid and
associated wrist injuries in a reasonable time.67 N’Dow et al.133
showed that patients with suspected injuries to the scaphoid and wrist
were often seen for months by junior staff and unnecessarily
immobilized for the same time. It is therefore advised that a protocol
be adopted where senior members of staff see these patients at the
first follow-up and at least once again after 6 weeks.
the criterion standard in the diagnosis of occult fractures of the
wrist. However, if MRI is not available, adequate clinical follow-up
and radiography should lead to the correct diagnosis. It is important
to include the radius and proximal aspects of the
metacarpals
in the scaphoid series to evaluate possible injuries to these bones.
Fractures of the radius, ulna, and the metacarpals occur in 13% of all
cases.67
 |
|
FIGURE 29-18 Schematic drawing of Herbert and Fisher’s classification of fractures of the scaphoid.
|
would seem to be potentially harmful and an unnecessary waste of time
and money. The literature suggests that there may be up to 34% of other
wrist injuries where an occult scaphoid fracture is initially suspected.86,169 However, Gaebler et al.67
found a higher rate of these injuries. Of all the injuries detected,
only 25% were scaphoid fractures. The other 75% consisted of carpal
fractures other than the scaphoid (13%), avulsion fractures of
extrinsic ligaments (12.5%), fractures of the distal radius (12%), bone
bruises (10%), other fractures (26.5%), and soft tissue injuries (26%).
However, many countries provide MRI scans only for emergency situations
or do not have MRI facilities at all. The results of a prospective
study showed that repeat clinical and radiographic examinations are
adequate.67 They will reveal occult
fractures of the scaphoid and other occult fractures of the wrist but
have the disadvantage that soft tissue injury remains undetected except
for ruptures of the SL ligament resulting in SLD.
important. If MRI proves the diagnosis, cast immobilization should be
used. Above-elbow casts and scaphoid casts are not required, and a
simple Colles forearm cast should be used for 4 to 6 weeks. Check
radiographs should be obtained at the time of cast removal. If there
are still clinical and radiologic signs of a scaphoid fracture, another
cast is applied for an additional 2 weeks.
of an occult fracture of the scaphoid, a Colles cast should be applied.
Most nonunions are caused by the patient or surgeon suspecting a simple
wrist sprain and undertaking no further diagnosis or treatment. The
solution is a simple clinic policy. Patients with a suspected occult
scaphoid fracture and negative radiographs are treated by the
application of a Colles cast for 10 to 14 days. After this time, the
cast is removed and a further scaphoid series undertaken. In most
cases, a correct diagnosis is then made and appropriate treatment
commenced.
prefer cast immobilization for 4 weeks. This injury represents a soft
tissue injury and requires time to heal properly. Radiographs can show
persistent displacement and fibrous union causing no disability,
although these findings are more commonly seen in fractures treated
without immobilization.
are usually stable. However, it is not always easy to decide whether
this is the case. Thus, radiologic follow-up is mandatory and surgery
may be necessary if the fracture displaces. If there is doubt about the
fracture type and the presence of displacement, a CT scan is
recommended with the treatment being based on the findings.
method of choice for the primary treatment for undisplaced fractures of
the scaphoid; the important questions to be answered are which joints
should be immobilized and what type of cast should be applied.
authors still advocate the use of above-elbow casts in scaphoid
fractures citing union rates of 95%. However, studies have shown no
advantage to the use of above-elbow casts.4,14 In fact, Kuhlmann et al.,103
in a prospective study, found the above-elbow cast harmful as it
blocked the normal rotation of forearm bones and transferred any
rotational movement to the radiocarpal joint where it caused movement
at the fracture.
proposed the use of an unpadded dorsal backslab, but in 1942 he changed
the cast to include the proximal phalanx of the thumb. This method of
treatment quickly became accepted and is still used in many hospitals.
However, Trojan,184 one of Böhler’s
pupils, assessed most of the patients treated by Böhler and found no
advantage in the use of the scaphoid cast and advocated its use only
for highly unstable and proximal pole fractures.
found that, provided the wrist was not ulnar deviated or extended, the
position of the thumb had no influence on the fracture gap. Clay and
coworkers,34 in a large prospective
randomized study, showed that there was no difference in union rates
whether the thumb was immobilized or not. For this reason, the use of
Colles or forearm casts, rather than scaphoid casts, is advocated.
fractures unite in 6 to 8 weeks with cast immobilization. However, bone
consolidation can take 12 to 16 weeks and some fractures will not have
healed even after this time. Apart from the fact that vertical and
proximal fractures have a worse prognosis than other scaphoid
fractures, there is unfortunately no reliable way of predicting the
outcome in undisplaced fractures.14
believed the incidence of nonunion to be about 50%, and they advocated
internal fixation of scaphoid fractures with a newly designed screw.
However, the idea of internal fixation was not new. McLaughlin123 published the first results of primary open reduction and internal fixation of scaphoid fractures in 1954, followed by Streli169 in 1970. More recently, McQueen et al.125
showed in a randomized study that percutaneous screw fixation of
undisplaced fractures gives significantly better results and a
significantly lower rate of nonunion together with shorter times to
return to work and sports when compared to conservative treatment.
These findings have been corroborated by other surgeons.64,140,212
Percutaneous fixation of the acute undisplaced or minimally displaced
fractures of the scaphoid has become increasingly popular since the
advent of cannulated screw fixation.64,125,146,147,208
The technique is simple and can be performed through either a volar or
dorsal approach. The dorsal approach requires a small open incision as
there is a likely risk to tendons or nerves,1
and the wrist must be in flexion which may displace the fracture and
makes imaging more challenging. With the use of the volar approach, a
potential disadvantage is an increased prevalence of later
scaphotrapezial osteoarthrosis which is usually asymptomatic and has no
impact on the final function.191
Neither approach has been shown to have an advantage in terms of
outcome, although the dorsal approach may improve fixation in proximal
pole fractures.81
trials of percutaneous fixation and cast management in undisplaced or
minimally displaced acute scaphoid waist fractures.3,12,23,125 These show advantages with percutaneous fixation in a more rapid union rate by 4 to 5 weeks,12,23,125 a more rapid return to work and sport, and a more rapid improvement in functional tests.3,12,125 Arora and his colleagues3
also demonstrated a cost benefit of percutaneous fixation, although
this was not statistically significant. However, Davis et al.42
argued compellingly on cost benefit grounds for the surgical treatment
of undisplaced fractures even with open reduction and internal
fixation, which might be expected to be more expensive than
percutaneous fixation.
With the advent and success of percutaneous fixation of the scaphoid,
open reduction and internal fixation is usually reserved for displaced
scaphoid fractures which are irreducible closed. A displaced fracture
is defined as one with more than 1 mm of step-off or more than 60
degrees of SL or 15 degrees of lunatocapitate angulation as observed on
either plain radiographs or CT scans.
did not define whether the fractures studied were displaced or not but
found no differences in union times or complications except for an
increased prevalence of asymptomatic osteoarthrosis of the
scaphotrapezial joint in the operatively managed cases. Return to
function was faster in the operated group and the authors concluded
that open reduction and internal fixation should be comsidered as an
alternative to a cast. The second study46
randomized treatment between open reduction and internal fixation and
cast management in undisplaced or minimally displaced fractures of the
scaphoid waist. There were advantages in the operated group in early
return of movement, better early patient-orientated outcome measures,
and a maintained improvement in grip strength throughout the period of
review. Ten patients in the cast group developed nonunion
compared
to none in the operated group. The disadvantage of open reduction and
internal fixation were minor problems with the scar. Despite these
findings, the authors concluded that scaphoid waist fractures should be
treated in a cast.
scaphoid fractures in low-demand patients, with the wrist in neutral
deviation and neutral flexion-extension for 6 to 12 weeks until there
is radiographic union. If there is doubt about the presence of
displacement, a CT scan will confirm the position of the fracture.
Careful clinical and radiographic follow-up examinations at the time of
cast removal are essential. It is recommended that the patient be
reviewed 6 weeks after cast removal for clinical and radiologic
examination and then every 3 months until the outcome is clear.
 |
|
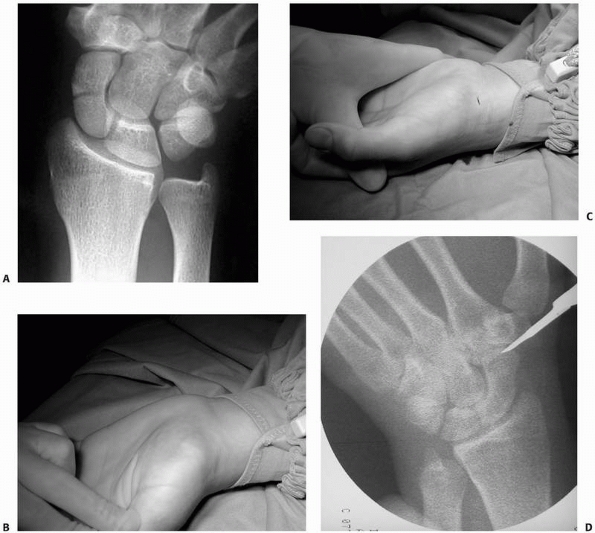
FIGURE 29-19 Percutaneous stabilization of scaphoid fracture. A. AP view of scaphoid fracture in an athlete. B. The wrist should be dorsiflexed prior to insertion of the K-wire. C.
A 4 to 5 mm incision is sufficient for insertion of the screw. The incision should be placed in skin crease to avoid visible scars. D. The joint space between scaphoid and trapezium is opened under flouroscopy. (continues) |
prefer percutaneous screw fixation. This includes the majority of young
high-demand patients. The method is relatively easy and, if the patient
is compliant, it allows postoperative treatment without cast
immobilization. The advantage of this minimally invasive method is
early return to sports and work in a population which is usually young
and active.82,121
No serious complications are expected when the surgical procedure is
performed carefully. Of all the screws available, the authors prefer
the Acutrak screw (Acumed, Inc., Beaverton, OR), which has some key
features that make it different from other cannulated screws (Fig 29-19J).
It was developed to produce interfragmentary compression with a
headless screw. The thread pitch varies at a constant rate along the
length of the screw. This accumulation of pitch differentials results
in gradual compression at the fracture site. The taper on the outer
profile of the screw causes the threads to constantly purchase new
bone. This minimizes thread damage and improves pull-out strength.
Biomechanic studies
have
shown that the Acutrak variable pitch, tapered, headless, compression
screw performed significantly better and provided superior fixation
than did the Herbert compression screw, and it was often better than
the AO lag screw.16,68,93,181,202
 |
|
FIGURE 29-19 (continued) E. The K-wire is inserted in a 45-degree angle at both planes. F,G. The position of the K-wire is checked by fluoroscopy. H. A second K-wire is required in unstable scaphoid fractures to prevent rotation of the fracture fragments. I. The drill is inserted. J. A variable pitch scaphoid screw. (continues)
|
 |
|
FIGURE 29-19 (continued) K. Insertion of scaphoid screw. L. Check insertion of screw by flouroscopy to avoid rotation of fracture fragments. M. Closure of wound with one suture. N. Postoperative radiograph shows a good compression of the fragments; the fracture gap is no longer visible.
|
three-dimensional understanding of the anatomy of the scaphoid is
required (Fig. 29-19). There are no major
vessels, nerves, or tendons endangered by the minimal invasive approach
to the scaphoid. The hand is placed on a radiolucent table with the
shoulder abducted and the forearm in supination. The wrist is extended
over a roll. The correct placement of the guide wire is crucial to the
success of the procedure. It helps to remember that the scaphoid lies
in a 45-degree plane to both the longitudinal and horizontal axes of
the wrist. A 4 to 5 mm skin incision is made about 1 cm distal and
radial to the scaphoid tubercle and the tip of the guidewire placed on
the scaphoid tubercle. The correct entry point is one that will allow
central placement of the screw in the scaphoid in both the AP and
lateral planes. In a few cases with an overhanging trapezium, it may be
necessary to insert the guidewire through the trapezium, which does not
seem to result in added morbidity.126
The guidewire is inserted at a 45-degree angle in both planes,
visualizing the AP plane with a fluoroscope. Unstable scaphoid
fractures have a tendency to rotate when the screw is inserted. If so,
a second wire is inserted to support the fracture site and avoid
rotational deformity. The length of the screw is then measured and
approximately 3 mm subtracted from the length to avoid prominence at
either end. The Acutrak screw, which is selfdrilling and self-tapping,
is then inserted. Screw progress should be monitored with the
fluoroscope to ensure that no rotation or distraction occurs at the
fracture site. If distraction occurs, the screw should be removed and
the track drilled. A central position of the screw without joint
penetration at the radiocarpal joint or prominence at the
scaphotrapezial
joint
should be confirmed with AP, lateral, and supinated and pronated views
of the wrist. Postoperatively, a bandage is applied with no cast being
required. Noncontact sports are allowed immediately. Contact sports,
heavy lifting, or weight bearing through the wrist are allowed 6 weeks
after surgery.
pole and oblique fractures require different treatment from that of
nondisplaced fractures. Unstable or displaced fractures of the scaphoid
have a high incidence of delayed union and nonunion, and the routine
use of cast immobilization is not generally recommended. However, there
are a few indications for closed reduction and cast management of
displaced scaphoid fracture. Patients who undergo conservative
treatment have to be carefully selected and will include patients with
metabolic diseases, noncompliant patients, and those patients with
significant medical comorbidities. Closed reduction involves
three-point pressure on the tubercle of the distal scaphoid in a palmar
direction combined with dorsal pressure over the capitate and dorsal
support of the distal radius, which helps reduce and maintain the
dorsolunate angulation. An acceptable reduction includes alignment with
less than 1 mm of displacement and a SL angle of not more than 60
degrees.
the efficacy of closed treatment as he was convinced, as are most
orthopaedic surgeons, that for sound bone union to take place, the
fracture fragments must be in close apposition so that soft tissue
interposition or synovial fluid cannot affect healing. He believed that
if closed treatment is used for complete fractures, osseous union may
be the result more of luck than skill.85
active population, proper stabilization should be performed. We prefer
percutaneous screw fixation as described above (see Fig. 29-19).
If reduction cannot be achieved, two pins should be inserted, one in
each fragment, and these pins are used as joysticks to reduce the
fracture. A temporary Kirschnerwire (K-wire) can be inserted to
maintain the reduction, and the guidewire for the screw is then
introduced. For acute displaced fractures that cannot be reduced
percutaneously, we recommend open reduction and compression screw
fixation of the scaphoid as soft tissue interposition is not uncommon
and often results in fibrous instead of osseous union.85,104,135,205
If there is a humpback deformity as a result of comminution, then bone
grafting is required. K-wire fixation alone is not advisable as the
rate of nonunion is high. Cast immobilization is not usually required
unless there is associated ligamentous injury.
or a volar approach, driving the guidewire through the proximal pole
and inserting the screw from the dorsal aspect. With this technique, it
is much easier to get a proper purchase on the small proximal fragment.162
displaced small proximal pole fractures, nonunions of the proximal
pole, and for exposure of injuries to the SL ligament. We prefer a
straight 3 to 4 cm incision centered over the back of the wrist after
checking the level of the SL junction with the fluoroscope. The
extensor pollicis longus tendon is mobilized radially after incision of
the retinaculum. The dorsal capsule is then incised and the scaphoid
exposed. Care is taken to avoid injury to the dorsal ridge vasculature
during the approach. The fragments are reduced manually or with the
assistance of K-wire joysticks. Bone grafting may be used to stimulate
union. A compression screw is then used after inserting a temporary
K-wire to prevent rotation. The dorsal wrist capsule should always be
repaired. The use of postoperative immobilization depends on the screw
purchase in bone and the stability of the fragment after fixation.
but the risk is probably greater in unstable fractures and
correspondingly less in stable fractures. The natural history of a
scaphoid nonunion depends on the stability of the nonunion with
progressive degenerative changes correlating with increasing
displacement of the nonunion.118
few will have had percutaneous fixation of their fracture. If initial
nonoperative treatment is chosen for the stable undisplaced fracture,
careful clinical and radiologic follow-up is required to identify a
developing nonunion. If there are no signs of union after 12 weeks,
operative intervention should be considered. If conservative treatment
is continued and there are still no signs of union after 16 weeks, the
patient has to understand that union is unlikely.
 |
|
FIGURE 29-20 Healed proximal pole fracture 6 months after dorsal approach.
|
unstable scaphoid nonunions. The stable scaphoid nonunion is
characterized by a firm fibrous nonunion that prevents deformity from
occurring. The length and shape of the scaphoid remain well preserved,
and the risk of osteoarthritis is small. Radiographs show an indistinct
fracture line with variable cystic changes affecting the adjacent bone
fragments. The patients are usually relatively symptom-free unless the
wrist is subjected to further trauma, which often leads to an unstable
nonunion with all of the associated problems of carpal collapse,
osteoarthritis, pain, and weakness.85
Although there are patients who seem to have an asymptomatic, stable
nonunion of the scaphoid for many years, most patients will become
symptomatic if the stable nonunion progresses to an unstable one and
osteoarthritis occurs. This has been reported as occurring in the
majority of cases,118 but it must be
appreciated that studies relate to symptomatic nonunion as asymptomatic
cases do not present frequently to the orthopaedic surgeon.
is to prevent progression to an unstable nonunion and the development
of degenerative changes. Treating fibrous nonunions is usually
straightforward and gives good results, whereas patients with unstable
nonunions often have persistent postoperative problems due to the
osteoarthritic changes of the radiocarpal joint. The earlier the
surgery, the lower the incidence of secondary osteoarthritis. The
standard palmar approach should be used for all reconstructions, except
those involving small proximal pole fractures.85
reported a series of stable scaphoid nonunions that were treated by
percutaneous screw fixation with good results. Their indications were
nonunions that were well aligned and without extensive sclerosis or
bone resorption at the nonunion site. It seems that selected nonunions
might require only rigid fixation, preferably undertaken percutaneously
to minimize devascularization.
The incision is based over or radial to the flexor carpi radialis from
the scaphoid tubercle to the distal radius. The sheath of the flexor
carpi radialis tendon is incised and the tendon retracted ulnarly.
Directly beneath the tendon lies the palmar capsule of the wrist, just
above the scaphoid. The capsule should be incised longitudinally. There
are no neurovascular structures at risk as the radial neurovascular
bundle lies radially. The superficial palmar branch of the radial
artery is distal at the end of incision and needs to be ligated in
cases of wider exposure of the distal scaphoid. It is important to
prepare the nonunion surfaces by removing any fibrous tissue and
sclerotic bone. We usually leave the dorsal cartilage in place. This
provides a hinge and facilitates assessment of scaphoid length. In most
cases of stable nonunion, cancellous bone graft from the distal radius
usually provides sufficient volume, although iliac crest bone graft can
be used if necessary. Screw fixation of the scaphoid is then used.
Immobilization in a cast or splint is not required postoperatively
except in occasional cases for pain relief.
sclerotic bone surfaces, with synovial erosion, fibrous cysts, and
continuous bone wear at the fracture leading to a marked discrepancy
between the sizes of the two bone fragments. Unstable scaphoid nonunion
leads to instability and progressive collapse and deformity.56,57,118,152 Fisk56
was the first to describe the humpback deformity of the scaphoid that
results from established nonunion where the proximal scaphoid rotates
dorsally into extension and the distal part faces downward in flexion.
Impingement between the palmarflexed distal pole of the scaphoid and
the styloid process of the radius results in radiocarpal osteoarthritis.195
At the same time, the unsupported carpus collapses into a DISI
deformity with increasing subluxation and secondary arthritis of the
midcarpal joint.85 Techniques of
palmar and radiopalmar bone grafting have been developed to correct
scaphoid malalignment and to restore normal scaphoid length. Failure to
correct the humpback deformity results in intraoperative problems
because the screw cannot be adequately placed and will cut out, leaving
residual instability. Even if the nonunion heals, the malunited
scaphoid has a twofold increase in degenerative arthritis compared with
a scaphoid that has healed with correct alignment.185
usually excellent whereas in D2 fractures the result depends on the
viability of the bone fragments and the extent to which secondary
changes have developed. The quoted success rates of achieving union
with internal fixation and bone grafting range from 60% to 95%.48,183
The differing rates may be explained by differences in the type of
fractures, differences in the demographics of the patients, or the
acknowledged difficulty in defining union. Recently, smoking has been
implicated as a reason for failure of nonunion surgery.48,114
relieve pain, increase function, and prevent the development or
progression of osteoarthritis. In the treatment of nonunion of the
scaphoid, it is essential to maintain the important principles of
fracture healing and at the same time secure correct scaphoid
alignment. The major principles to follow are early diagnosis, complete
resection of the nonunion, correction of deformity secondary to carpal
collapse and carpal instability, preservation of blood supply, bone
apposition by an inlay graft, and screw fixation for fracture stability.
required to determine the degree of correction that one may expect to
achieve. Radiographs should be compared with films of the opposite
uninjured wrist. Sagittal images from CT scans provide the best method
of evaluating the location of the nonunion and the degree of collapse.
The lateral intrascaphoid
angle6 and the height-to-length ratio of the bone help identify angulation and collapse of the scaphoid.185
The lateral intrascaphoid angle is formed by the intersection of the
perpendicular lines to the diameters of the proximal and distal poles.
An angle of more than 35 degrees has been shown to be associated with
an increased incidence of arthrosis even in fractures that went on to
unite.7 The collapse of the scaphoid
in the sagittal plane causes DISI pathology and increases the chances
of wrist arthrosis even if the scaphoid finally heals.6
Restoration of normal scaphoid anatomy in the treatment of nonunion
therefore aims to reduce or postpone the incidence of osteoarthritis
and to improve the function of the wrist.55
healing potential of a scaphoid, diminished vascularity of the proximal
scaphoid is not a contraindication to a palmar inlay bone graft.39
If fracture union can be achieved, the relative avascularity will
improve. It is advantageous to confirm AVN of proximal pole fragments
to determine the prognosis for successful treatment. Methods of
assessing AVN include bone scan, CT scans, and MRI. The latter
technique is undoubtedly the most sensitive and is preferred. However,
the only definitive test for confirming AVN is the observation at
surgery of the presence or absence of bleeding from bone. Green78
reported that the number of punctuate bleeding points is a good
indicator of vascularity of the bone. When the proximal pole was
completely avascular, the likelihood of successful healing with a graft
was virtually nil and an alternative procedure such as intercarpal
fusion, excision of the proximal scaphoid, interposition arthroplasty,
proximal row carpectomy, or scaphoid allograft should be considered.
Herbert85 stated that carpal
collapse and secondary arthritis are rarely associated with proximal
pole nonunion. He therefore argued against the use of interposition
bone grafts and suggested screw fixation by a dorsal approach, with or
without cancellous bone grafting, depending on the findings at the time
of surgery. Although the fracture may not unite, the patient’s own bone
should be better than any implant. Another alternative is a
vascularized bone graft.
 |
|
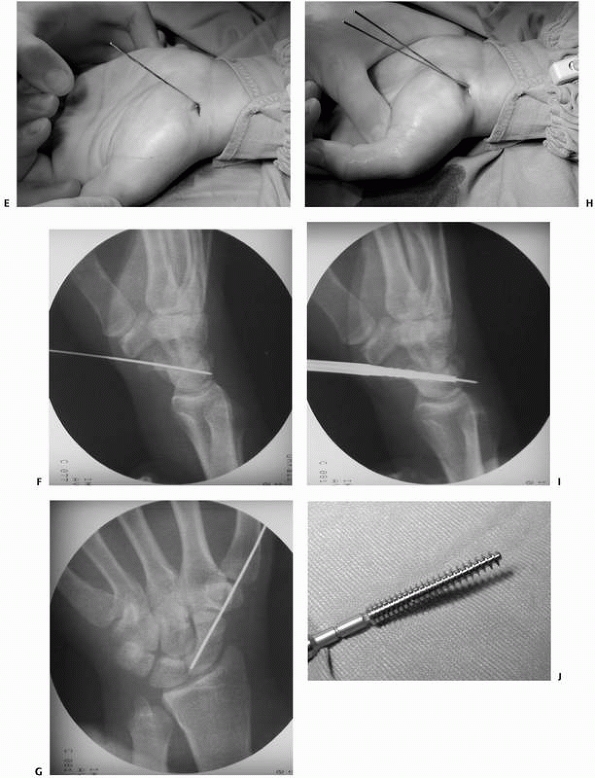
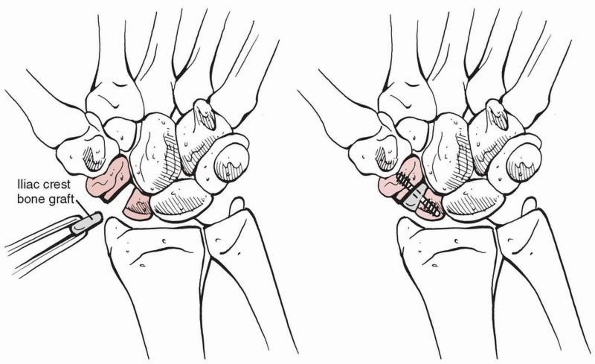
FIGURE 29-21 Standard Russe153
bone graft (top). His technique relied on packing a corticocancellous bone graft into a trough curretted through the volar cortex of both fragments. Because the volar cortex is often foreshortened by erosion of the fragments, loss of length is difficult to correct without introducing a cortical graft (center). Modified Russe winged graft that is impacted into a volar trough to lengthen the scaphoid (bottom). |
reconstructions of unstable scaphoid nonunions to avoid damaging the
dorsal blood supply. Scaphoid nonunions might not be visible
macroscopically and often need sharp division with the knife. It is
useful to check the site of a nonunion as fusion of the proximal pole
of the scaphoid with the lunate has been undertaken assuming that this
joint was the site of nonunion!
but this technique does not usually correct volar shortening. Anterior
wedge grafting procedures are now in common use as humpback deformities
can be corrected with this technique.51,182 Initial reduction of the lunate and temporary pin fixation to the radius can facilitate accurate reduction.182
deformity. The nonunion gap is exposed and débrided, and the fracture
fragments are mobilized. It is best to leave a cartilage hinge
posteriorly to provide a fulcrum around which the fragments may be
hinged open although this is often not possible in older, unstable
scaphoid fractures. If the hinge is released in an effort to regain all
of the scaphoid length, the fracture fragments will become extremely
unstable and difficult to align. Furthermore, the gap between the two
fragments may be too great for the scaphoid to revascularize the
proximal pole.185
distracted with small spreaders. This maneuver usually achieves
adequate correction of the carpal deformity and a satisfactory
improvement in wrist extension. Provided that reasonable correction is
achieved and that the wrist extends to at least 45 degrees, most
patients achieve satisfactory clinical results.69
The fracture surfaces are excised with a small osteotome, burr, or
curette. We prefer a corticocancellous wedge graft from the iliac
crest. This is an interposition graft, which is inserted on the palmar
surface and serves to bridge the fracture gap and correct any
displacement or angulation of the scaphoid that has occurred. To
correct angular deformity and restore normal scaphoid length, the
amount of resection and size of the graft can be calculated
preoperatively by CT scans. The indications for interposition grafting
include gross motion at the nonunion site, scaphoid resorption, and
loss of carpal height. Most commonly, the operative procedure involves
an anterior interposition bone graft, with the size based on
comparative scaphoid views of the opposite wrist and intraoperative
measurements.
graft of the exact size is removed from the iliac crest with an
osteotome. Oscillating saws should not be used, as thermal necrosis of
the graft can occur. With the wedge graft in place and the scaphoid
reduced and held with a K-wire, a compression screw is inserted (Fig. 29-22).
Internal fixation with K-wires alone is usually not successful as
compression is required to achieve union. However, if the graft shows a
tendency to rotate, additional fixation with a K-wire may be required.
If there is a severe or longstanding DISI deformity with a RL angle
greater than 20 degrees, additional pinning of the lunate to radius for
6 to 8 weeks is advised.55 It may be
difficult to completely correct carpal instability in long-standing
cases, and these patients may be better served by various salvage
procedures.
usually not required but a Colles cast can be used if there is doubt
about stability or pins have been used across the radiocarpal joint.
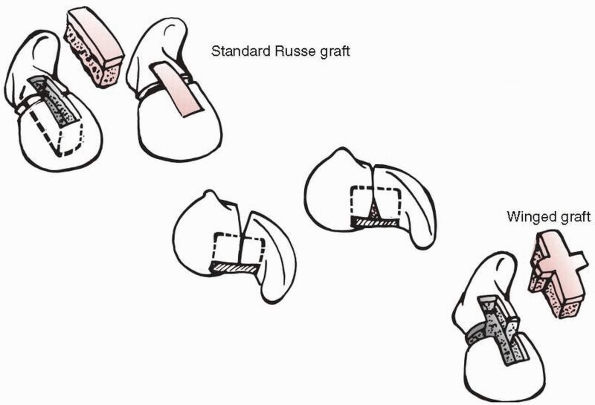 |
|
FIGURE 29-22
Insertion of an iliac crest bone graft and stabilization with a screw for treatment of scaphoid nonunions. The bone graft is wedged to correct the angulation deformity that often occurs. |
 |
|
FIGURE 29-23 Pronator quadratus graft.
|
can be performed in patients with radiologic signs of stage I
radioscaphoid arthritis, this being arthritis that is limited to the
scaphoid and radial styloid. This is undertaken to relieve pain arising
from arthritic joints or osteophyte impingement. If there are no
radiologic signs of arthritis, a styloidectomy should not be undertaken
at the same time as a scaphoid reconstruction often relieves symptoms.
 |
|
FIGURE 29-24 Radial styloidectomy for pain relief in a patient who showed arthritic changes due to scaphoid nonunion.
|
fragment can be excised with impunity. However, most surgeons are aware
that if it is more than 8 mm long, the results are poor and the wrist
feels weak.14
panscaphoid osteoarthritis, total replacement of the scaphoid is worth
considering.189 If the scaphoid must
be excised, it seems reasonable to replace it with something! Silicone
implants induced progressive silicone arthritis in many cases,84
and the technique was abandoned 20 years ago. Other methods of
replacement such as cadaveric bones and titanium implants are currently
in clinical trials. However, unless the midcarpal joint is stable and
painless, this procedure should be combined with a fusion across the
midcarpal joint.85 Without this
fusion, progressive carpal subluxation is likely to occur. The fusion
is unlikely to trouble patients as most have long-standing carpal
collapse deformity with secondary osteoarthritis. It is important to
correct the midcarpal subluxation as much as possible in order to
improve the range of dorsiflexion. Unless at least 30 degrees of
extension is maintained after surgery, the patient will almost
certainly continue to experience pain when the wrist is loaded.85
Young and active patients are likely to complain of continued pain
after this procedure, and wrist arthrodesis is therefore preferable in
these patients.
lead to increasing midcarpal and radiocarpal osteoarthritis secondary
to increasing carpus collapse. If this is not treated, there is
increasing pain and weakness, and wrist motion becomes restricted to
the extent that reconstructive surgery is no longer feasible and wrist
fusion is required. Pain is the main factor to be taken into
consideration when deciding for or against wrist arthrodesis.
Arthrodesis is an accepted surgical treatment option for patients with
markedly restricted and painful wrist motion. Instability and deformity
of the wrist affect hand function significantly but pain diminishes
both strength and dexterity. Wrist arthrodesis achieves good pain
relief,85,92
especially in younger patients with high functional demands. It can be
difficult to convince patients with severe pain but good wrist movement
that the optimal treatment might be a wrist fusion. However, the pain
relief associated with a successful fusion results in significant
improvement of hand function and grip strength. Preoperatively, it is
easy to supply the patient with a dorsal splint to simulate arthrodesis
to see if this helps wrist function and symptoms.
to the joint compressive forces at the scaphotrapezial and
radioscaphoid joints. The proximal fragment has a tendency to extend,
deviate radially, and supinate relative to the distal fragment. The
collapse of the scaphoid in the sagittal plane causes DISI pathology
and increases the chances of wrist arthrosis even if the scaphoid
finally heals.6
entity that causes altered carpal kinematics and abnormal load
distribution which may cause premature wrist arthrosis, the reported
number of patients treated with early osteotomy is surprisingly small.
Indications for osteotomy are pain, weakness, limited range of motion,
and deformity of the scaphoid detected on radiographs and evaluated by
CT scans. Restoration of normal scaphoid anatomy in malunion aims to
reduce or postpone the incidence of osteoarthritis and to improve
function of the wrist.52,55 Lynch et al.117
reported a technique of corrective osteotomy that corrects the
intrascaphoid angles, restores palmar length to the scaphoid, and
reduces DISI deformity of the carpus. This method seems to have a role
in the prevention or slowing of the onset of arthritis in young
patients with high functional demands.117
scaphoid fractures, especially those involving the proximal pole.
Occasionally, AVN may occur without a fracture, either as a
complication of SL ligament injury or as an idiopathic condition known
as Preiser’s disease.143 The term
Preiser disease is associated with AVN of the scaphoid without fracture
or trauma, although it should be noted that the AVN described by
Preiser probably occurred in fractured scaphoids as all of his patients
had a well-documented history of trauma. The typical symptoms of AVN
are increasing pain and stiffness of the wrist. Radiographs usually
show a small, deformed proximal pole fragment with cystic changes and
areas of sclerosis. It is mandatory in all cases of scaphoid nonunion
to exclude AVN by MRI scans before surgery is undertaken as the
diagnosis of AVN alters the treatment options.
The bone graft can be harvested dorsally through the second dorsal
compartment of the distal radius, anteriorly in the form of a pronator
quadratus graft, or from
the
second metacarpal. It is important to adhere to the basic principles of
nonunion treatment with meticulous preparation and stabilization of the
nonunion site.
-
Occult scaphoid fractures are easily detected by MRI scans.
-
Percutaneous stabilization of scaphoid
fractures significantly reduces time lost from work and sports and
increases the rate of union. -
Proximal pole fractures can also be stabilized percutaneously by a dorsal approach.
-
Malalignment of scaphoid fractures is often undiagnosed. CT scans are helpful.
-
Conservative treatment often ends in delayed healing. An aggressive operative approach is recommended.
and some authors believe that unrecognized and untreated fractures of
the lunate lead to Kienböck disease. This opinion was based on the work
of Verdan,190 who applied strong
forces to cadaver bones and observed that the resulting fractures were
not visible on standard radiographs but only on histology. A major
argument against this hypothesis are the MRI findings of Schiltenwolf
et al.,157 who postulated that early
venous congestion of the lunate was responsible for the pathogenesis of
Kienböck disease but found no fractures. The lunate necrosis after
perilunate dislocation is probably due to impairment of the arterial
vasculature.160
osteonecrosis of the lunate. It usually has an insidious onset without
a history of injury; however, diagnosis is sometimes made after a
simple fall that fractures the necrotic bone (Fig. 29-25). Osteonecrosis may be the result of interruption of the vascular supply to the lunate,157
which shows no radiographic evidence of injury until sclerosis and
osteochondral collapse are seen. The condition is more common in
patients with an ulnar minus variant.
row in the well-protected concavity of the lunate fossa of the radius,
anchored on either side by the interosseous ligaments to the scaphoid
and triquetrum with which it articulates. Distally, the convex capitate
head fits into the concavity of the lunate. The joint reaction force
from the capitate and radius squeezes the lunate ulnarly. The proximal
pole of the hamate has a variable articular facet on the distal ulnar
surface of the lunate, and ulnar deviation increases the degree of
contact of these two bones. The vascular supply of the lunate is
primarily through the proximal carpal arcade both dorsally and
palmarly. However, the literature suggests that 7% to 26% of lunates
may have a single volar or dorsal blood supply and are therefore
vulnerable to AVN because of disruption of extraosseous blood supply.58 Several authors.39,75,137 have shown the intralunate anastomoses to be of three main types. The degree of cross flow between the systems is variable.
history of a hyperextension injury such as a fall on the outstretched
hand. Occasionally, repetitive stresses of the wrist or a strenuous
push will give rise to a “snap” in the wrist.39
In extension, the lunate is displaced onto the palmar aspect of the
lunate fossa and rotated dorsally. The capitate drives against the
palmar aspect of the lunate and at the same time pushes it in an ulnar
direction. This is resisted by the RL ligament, which exerts tension at
its lunate insertion. If there is an ulnar minus variant, the support
offered by the TFCC and ulnar head will be minimal, and even less when
the hand is pronated. The compressive stresses over the proximal
convexity of the lunate shift dramatically at the interface between the
TFCC and radial articular surface. The lack of ulnar support may also
allow proximal displacement of the triquetrum placing further tensile
stress on the lunate surface through the LT ligament. This appears to
provide a reasonable scenario for the transverse fractures that occur
in the sagittal plane.
tension that develops in the SL ligament, because these are frequently
seen with SLD. Avulsion fractures of the ulnar aspect of the palmar
pole are usually associated with a perilunate dislocation. It is also
possible that sufficient stress develops, where the arteries penetrate
the bone, to induce devascularization. In this situation, avascularity
would precede fracture, rather than vice versa. Indeed, there is
considerable evidence that both mechanisms can be responsible for
Kienböck disease and that several contributing factors such as trauma,
ulnar variance, and impaired vascularity interact to produce Kienböck
disease.
of the difficulty is that the fragmentation that occurs in Kienböck
disease can be confused with fractures (Fig. 29-25A). However, acute fractures of the lunate are classified into five groups177:
-
Frontal fractures of the palmar pole with involvement of the palmar nutrient arteries.
-
Osteochondral fractures of the proximal articular surface without substantial damage to the nutrient vessels.
-
Frontal fractures of the dorsal pole.
-
Transverse fractures of the body.
-
Transarticular frontal fractures of the body of the lunate.
horn avulsion fractures that occur more often in the radial corner than
in the ulnar corner. Fractures of the body are usually transverse in
the coronal plane. The more common of these is between the middle and
palmar thirds of the body.
because a nondisplaced crack is often obscured by superimposed
structures. The best example of this problem is the palmar cortical
line of the radial styloid which is aligned with the division between
the dorsal and palmar thirds of the lunate where a transverse fracture
often occurs.39 The AP view of this
is in a plane almost perpendicular to the fracture, which is overlapped
by the rims of the distal radius and is therefore not apparent. The
palmar horn of the lunate may also be hidden by the pisiform
and
scaphoid shadows. For these reasons, clinical suspicion must take
precedence over the findings on plain films. A technetium-99m bone scan
will be positive within 24 hours of injury. Oblique films sometimes
help to visualise fracture lines, but CT scans provide more precise
detail. Osteonecrotic changes are also more easily seen on CT scans
than on radiographs, and it is also often possible to differentiate the
primary fracture from the secondary fractures associated with
fragmentation.
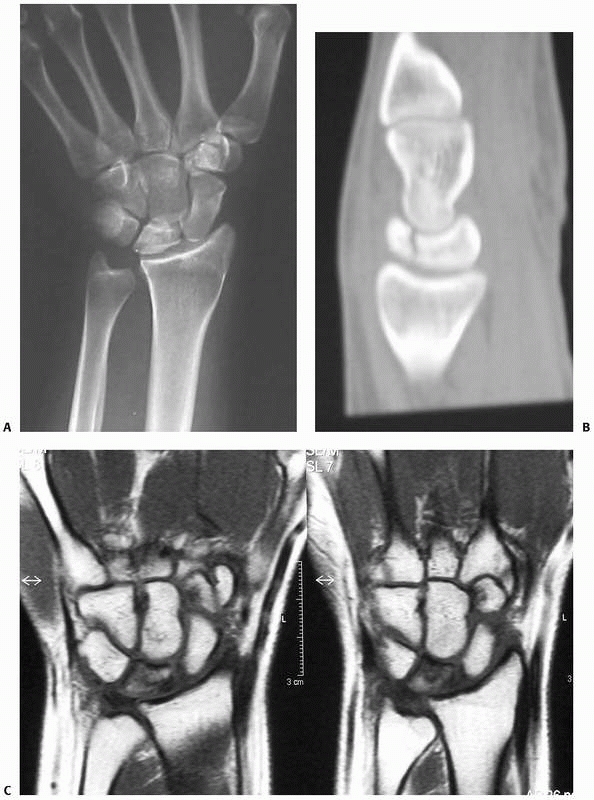 |
|
FIGURE 29-25 A. AP radiograph of a 25-year-old woman after a skiing accident. It shows a sclerotic lunate and an ulnar negative variance. B. A CT scan demonstrates a fracture of the sclerotic lunate. C. An MRI scan demonstrates decreased vascularity of the lunate.
|
the early stages of lunate AVN, and to demonstrate revascularization as
well as healing. MRI will show evidence of diminished vascularity
before changes are apparent on radiograph, and this modality is now the
imaging procedure of choice for early evaluation of Kienböck’s disease.
Gadolinium enhancement allows a more accurate assessment of lunate
vascularity and revascularization. Arthroscopic examination permits a
direct assessment of the articular surfaces and the integrity of the
intrinsic ligaments.
immobilization for 4 weeks. Healing of nondisplaced lunate fractures,
especially
of
avulsion injuries of the dorsal or palmar horns, is relatively good. A
transverse fracture of the body will heal if it remains nondisplaced,
particularly in adolescents. However, it is important to recognize
that, especially with high-energy injury, a lunate fracture may be
associated with carpal dislocation or subluxation and the fracture may
progress to carpal instability, nonunion, or AVN.39
Indications for open reduction and internal fixation include
displacement or associated carpal instability. Imaging can be very
helpful and ideally should include MRI scans. If there is evidence of
separation of the lunate fragments by the capitate, union will not
occur and the risk of AVN is markedly increased. Although the efficacy
of internal fixation of the lunate is unproven and the obstacles to
successful reduction and fixation are substantial, the consequences of
inaction are quite predictable. Distraction with an external fixator
may facilitate reduction of the lunate fragments.39
progress to Kienböck disease. If this occurs, the treatment includes
radial shortening, radial wedge osteotomy, or ulnar lengthening in the
early stages and carpal arthodeses if the condition is advanced.
The triquetrum may sustain a transverse fracture in a perilunate
dislocation, but it usually displaces dorsally with the distal carpal
row away from the lunate. The most common triquetral fracture is
probably the impingement shear fracture of the ulnar styloid against
the dorsal triquetrum which occurs with the wrist in extension and
ulnar deviation, particularly when a long ulnar styloid is present.70
Shear impingement by the hamate against the posteroradial projection of
the triquetrum, the triquetrohamate impaction syndrome, occurs through
compression of the wrist, when the body weight is supported by the hand
placed in forced dorsal and ulnar extension while the forearm is
pronated.112 The triquetrum is rarely dislocated alone because of its strong ligamentous connections.
localized to the appropriate area. Dorsal chip fractures of the
triquetrum are easily overlooked on the AP radiograph because of the
normal superimposition of the dorsal lip on the lunate. Such fractures
are usually seen in one of the views of the normal scaphoid series. If
not, a slightly oblique, pronated lateral radiograph will project the
triquetrum even more dorsal to the lunate. Transverse fractures of the
triquetral body are usually easily identified on the standard AP view.
CT scans may be required to detect the extent of injury. If occult
fractures are suspected, MRI scans should be considered.65,67
until symptoms subside is sufficient for avulsion injuries. Triquetral
body fractures in association with carpal disruption require internal
fixation.
The pisiform is generally injured during a fall on the dorsiflexed,
outstretched hand. Most fractures are sports-related and easily missed.105
A direct blow while the pisiform is held firmly against the triquetrum
under tension from the flexor carpi ulnaris leads to either avulsion of
its distal portion with a vertical fracture or an osteochondral
compression fracture at the pisotriquetral joint. Based on the findings
of Arner and Hagberg,11 the fractured bone should be excised.148,160
This avoids pisotriquetral incongruity. The type of fracture pattern is
therefore irrelevant as excision eliminates any impact of fracture
pattern on clinical outcome. The small amount of loss of grip strength
associated with excision is not of functional significance.160
However, absence of the pisiform exposes the ulnar artery and nerve to
more trauma and may increase the possibility of hammer syndrome and
neuropathy. We prefer conservative therapy primarily and undertake
secondary resection if there are any problems with nonunion and
incongruity.
although some patients may present with ulnar nerve symptoms as the
nerve divides into its terminal branches beside the pisiform bone.
Special views are required to see pisiform injuries. A lateral view of
the wrist with the forearm in 20 to 45 degrees supination and carpal
tunnel views are useful. If subluxation of the pisotriquetral joint is
suspected, the diagnosis is made when one or more of the following are
present: a joint space of less than 4 mm in width, loss of parallelism
of the joint surfaces greater than 20 degrees, and proximal or distal
overriding of the pisiform amounting to more than 15% of the width of
the joint surfaces.39
usually sufficient. Rarely painful nonunion may occur when excision of
the pisiform is usually effective.
The majority of trapezial fractures are ridge avulsion fractures or
vertical fractures of the body. Fracture through the articular surface
of the trapezium is produced by the base of the first metacarpal being
driven into the articular surface of the trapezium by the adducted
thumb. There might also be an anvil mechanism related to the radial
styloid. These fractures may be associated with dislocation of the
first carpometacarpal joint. Avulsion fractures caused by the capsular
ligaments can occur during forceful deviation, traction, or rotation.
Direct blows to the palmar arch area or forceful distraction of the
proximal palmar arch may result in avulsion of the ridge of the
trapezium by the transverse carpal ligament.39 Fractures of the tuberosity of the trapezium may be associated with fractures of the hook of the hamate or with dislocation of
the hamate because the flexor retinaculum is fixed to the ridges of both bones.160
fracture of the trapezium. Fractures of the tuberosity are projected by
carpal tunnel views.
sufficient for undisplaced fractures. If displacement or dislocation is
present, open reduction and internal fixation is indicated in most
cases. Painful nonunion sometimes occurs with trapezial ridge fractures
when excision is usually successful in eliminating symptoms.
as are isolated trapezoid dislocations, although palmar dislocations
have been reported. The trapezoid is located between the first and
second ray, which might explain why this bone may be exposed to fewer
forces able to cause fracture or dislocation.160
Injury to the trapezoid is generally associated with forces applied
through the second metacarpal. Ligamentous instability produced by a
similar injury or osteochondral injuries to the trapezoid-second
metacarpal, capitate-third metacarpal, or metacarpohamate joints often
escape detection.
metacarpal. A trapezoid dislocation or fracture-dislocation is seen on
the AP radiograph as a loss of the normal relationship between the
second metacarpal base and the trapezoid. The trapezoid may be
superimposed over the trapezium or the capitate, and the second
metacarpal may be proximally displaced. Oblique views and CT scans may
be helpful.
for trapezoid fractures. Displacement of up to 2 mm has been treated
successfully nonoperatively. Open reduction and internal fixation or
excision of smaller fragments can be used for displaced fractures.155
whether capitate fractures are rare or frequent. It is likely that
capitate fractures are more common than was previously thought.31,65,67
However, diagnosis may be difficult without an MRI scan, and the
capitate obviously heals even without immobilization, as nonunion is
rare.
-
Direct blow or crushing injuries. These are usually associated with injuries to the metacarpals and other carpal bones.
-
The scaphocapitate syndrome, described by Fenton,54
in which a violent blow directed to the radial styloid would first
fracture the scaphoid and then the capitate but produce no dislocation.
However, because fractures of the scaphoid and the capitate are only
stage 1 or stage 2 of the spectrum of injury that culminates in a
transscaphoid, transcapitate, or perilunate dislocation of the carpus,
it is not surprising that the capitate fragment can be frequently
rotated 90 to 180 degrees with the articular surface displaced
anteriorly or facing the fracture surface of the capitate neck.188 Without reduction, AVN will result. -
A fall with the wrist in dorsiflexion,
forcing the capitate onto the dorsal rim of the radius. The dorsal
border of the radius will impinge on the capitate and cause a fracture
through its waist. This is the anvil mechanism theory.
standard scaphoid views, although motion studies are recommended to
look for displacement. A lucent line through the neck of the capitate
may be isolated or may be combined with other fractures or
fracture-dislocations. In such instances, the head of the capitate
should be identified on the lateral view to determine if it has been
rotated or displaced. Nonunion of the capitate can occur63
and is diagnosed by CT scans. CT scans and MRI may be necessary to
detect occult capitate fractures. MRI provides further information
regarding the vascularity of the proximal capitate.
fracture. Open reduction and internal fixation with screws or plates
should be used in cases with displacement.
Many fractures of the hamate are associated with fifth or,
occasionally, fourth metacarpal fractures or axial
fracture-dislocations.
injuries, resulting from direct blows to the palm of the hand. They
mainly in sports requiring the use of a racket, baseball bat, or golf
club (Fig. 29-26).160
The fracture generally occurs at the base of the hook although avulsion
fractures of the tip also may be seen. Symptoms are often minimal,
leading the patient to downplay the injury until persistent pain and
nonunion of the hamate are present.24,196 Nonunion is relatively common and can induce ruptures of the little finger flexor tendon.
previously appreciated because of missed diagnosis, with 50% being
missed on first presentation.213
They occur in mostly young men either as a result of a direct blow or a
fall on the outstretched hand. These are benign injuries in which
symptoms usually resolve with immobilisation for a few weeks.
tenderness in the area of the hook of the hamate, although some
patients may present with the symptoms of ulnar nerve entrapment as the
deep branch of the ulnar nerve nerves winds around the
hook
of the hamate. Fractures and dislocations of the hamate are usually
identified on standard scaphoid views. A dislocation usually results in
some rotation that alters the contour of the bone and the normal oval
appearance of the hook. Fracture of the hook of the hamate is best
visualized on the carpal tunnel view. CT scans will confirm the
fracture. The hook of the hamate may ossify independently and
occasionally may fail to fuse with the body of the hamate. This
separate bone, known as the os hamulus proprium, can be mistaken for a
fracture. MRI scans are helpful to differentiate acute injuries from
this developmental anomaly.
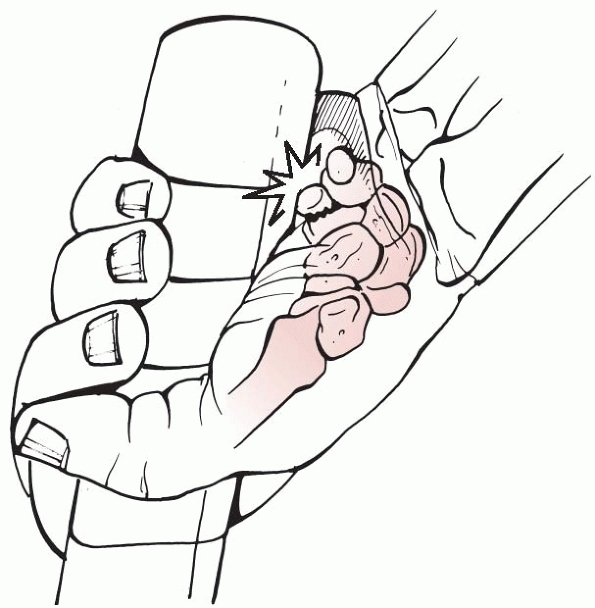 |
|
FIGURE 29-26
Fractures of the hamate usually occur in those who play sports requiring to hold a racket, making them susceptible to a direct blow to the hook of the bone. |
conservatively. Excision might be required in case of nonunion and
entrapment of the ulnar nerve,166 although bone grafting has been advocated to preserve the pulley effect on the flexor tendons.196
If ulnar nerve entrapment occurs, it is important to decompress Guyon
canal as the weakness in the hand may be considerable, because the
hypothenar muscle group, the medial two lumbricales, all seven
interossei, the adductor pollicis, and the flexor pollicis brevis are
involved.160
|
TABLE 29-4 Classifications of Carpal Instability
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
or dislocation, open reduction and internal fixation is required.
Undisplaced fractures can be treated with splintage or casting. The
outcome of promptly treated fractures is good.201
Instability may also be adaptive secondary to malalignment outwith the
carpus such as in distal radius malunion. There may also be complex
combinations of different types of instability.
bones or bone disruption such as a scaphoid fracture. The perilunate
dislocation pattern provides a whole spectrum of wrist sprains,
fractures, dislocations, and instabilities. This injury pattern usually
begins radially and proceeds either through the body of the scaphoid or
through the SL interval resulting in SLD. Further destabilization
passes distally between the capitate and lunate, either through the
space of Poirier between the proximal and distal palmar V-ligaments or
through the capitate, resulting in a transcapitate fracture, and then
ulnar to the lunate, either through the hamate and triquetrum or
through the lunatotriquentral interval. This type of perilunate
dislocation usually results in a DISI collapse pattern because the
stabilizing influence of the scaphoid is lost. A similar pattern of
destabilization can begin ulnarly and propagate radially around the
lunate, such that the lunate is first dissociated from the triquetrum.39
The lunate may retain sufficient connection to the scaphoid that the
residual collapse pattern is VISI. Both of these collapse patterns are
dissociative because there is disruption of the ligament bond or the
bone structure between the lunate and one or both of the adjacent
carpal bones.
the entire carpus that may be purely ligamentous but more commonly
include a fragment of the distal radius. These dislocations
are
either a palmar Barton or a dorsal Barton fracture-dislocation or a
radial styloid fracture-dislocation, known as a chauffeur’s fracture.
Associated VISI or DISI instabilities are possible. These may be either
dissociative or nondissociative depending on the degree of damage to
the ligamentous connections of the proximal carpal row.
These are ulnar translation of the entire carpus, dorsal translation
instabilities, and occasionally palmar translation instabilities.
Combinations of these instabilities may occur, although one deformity
pattern is usually predominant. The basic patterns are similar in
instability dislocations and fracture-dislocations, suggesting that
there is a spectrum of problems that occur in the linkage system within
the carpus. Using these concepts, it is possible to group all known
injuries that result in carpal instability into interrelated categories.
Fractures of the scaphoid, for example, are most tender to pressure in
the anatomic snuffbox. SL and lunate injuries cause tenderness just
distal to Lister tubercle. Triquetral, LT, and triquetrohamate ligament
injuries result in tenderness over the dorsal margin of the appropriate
bone, usually a fingerbreadth distal to the ulnar head. Other clinical
findings are highly variable and depend on the extent of carpal
disruption, with more traumatic carpal disruption seen in perilunate
dislocations.
localized. There may be swelling that is severe and generalized or
discrete and barely detectable. Changes in alignment of the hand,
wrist, and forearm may be clinically evident on inspection of the
extremity. Swelling over the proximal carpal row is suggestive of a
ligament avulsion with or without an associated fracture. Marked
prominence of the entire carpus dorsally is suggestive of a perilunate
dislocation. Compressive stresses applied actively or passively may
produce pain at the site of damage and result in snaps, clicks, shifts,
and thuds, which are palpable and audible.
-
The scaphoid shift test.194
Pressure is applied to the scaphoid tubercle while the wrist is brought
from radial to ulnar deviation. In a positive finding, there is a
“clunk” as the scaphoid subluxes dorsally out of the scaphoid fossa.
The diagnosis is SL disruption. -
The midcarpal shift test.109
Pressure is applied to the dorsum of the capitate as the wrist is moved
from radial to ulnar deviation. A positive finding is a “clunk” as the
lunate reduces from the palmarflexed position. The diagnosis is
midcarpal instability. -
LT ballottement.145
The lunate is fixed with the thumb and index finger of one hand while
the triquetrum is displaced palmarly and dorsally with the thumb of the
other hand. A positive finding is pain. The diagnosis is LT instability
or arthritis. -
Scaphoid lift test. This is a reproduction of pain with dorsopalmar translation of the scaphoid.
there are a number of false positive and false negative results. It is
useful to test the opposite wrist as there is a range of ligamentous
laxity in normal individuals. This may be associated with the ability
to subluxate the midcarpal joint by displacing the carpometacarpal unit
on the distal radius. Tendon displacements with audible snaps are
easily produced by some persons but are seldom symptomatic. Distraction
can be a good clue to a “lax wrist” or a damaged area, particularly
when viewed under fluoroscopic imaging with static traction of
approximately 25 pounds applied. Stress-loading the wrist with
compression and motion from radial to ulnar deviation may simulate
midcarpal instability (MCI) and produce a “catch-up clunk” as the
proximal row of carpal bones snap from a flexion to extension.
fracture-dislocations of the distal radius and carpus: palmar and
dorsal Barton fracture-dislocations, radial styloid
fracture-dislocations, and die-punch fracture-dislocations. Less common
are the pure ligamentous radiocarpal injuries (Fig. 29-27),
which may cause the wrist to translate in an ulnar, dorsal, or palmar
direction. True dislocations without fracture of the bony margins are
rare, and they may sometimes spontaneously reduce, making it even more
difficult to demonstrate them. However, they are occasionally seen
unreduced with the carpus lying dorsal, palmar, or ulnar to the radius.39
appropriate trauma followed by the usual initial findings of swelling,
deformity, tenderness, and pain. Swelling and tenderness are most
noticeable dorsally at the radiocarpal level and are aggravated by
wrist motion. Deformity may be an ulnar, dorsal, or palmar shift of the
carpus.
or a fracture of the tip of the radial styloid when it is assumed that
the radiocarpal ligaments are avulsed from the radius. Type II have a
fracture of the radial styloid involving more than one third of the
scaphoid fossa when it is assumed that the radiocarpal ligaments remain
attached to the styloid process. Moneim128
also classified these injuries into two groups, but his classification
is dependent on the presence or absence of intercarpal ligament injury.
Type I have intact intercarpal ligaments, while Type II have a
combination of radiocarpal and intercarpal dislocation.
 |
|
FIGURE 29-27
Radiocarpal dislocation with torn radiocarpal ligaments. This injury requires K-wire stabilization and direct repair of the radiocarpal ligaments. |
are severe injuries, with the majority of patients having associated
injuries.49,131 A common association is injury to the ipsilateral distal radioulnar joint.
radiographs, although provocative stress tests may be required to
demonstrate dynamic radiocarpal instability.39 Ulnar translation is the most frequent radiocarpal instability.39
It may occur acutely, develop gradually, or be observed as a late
sequela of a perilunate dislocation. It may occur after an injury at
the radiocarpal level, where the radiocarpal ligaments are avulsed from
their origins, or after perilunate injury. Clinically, the carpus and
hand are offset in an ulnar direction. The radiographic appearance is
often dramatic, with the lunate positioned just distal to the ulna and
a large space between the radial styloid and the scaphoid. If
perilunate destabilization is also involved, the lunate and triquetrum
slide ulnarly, opening a gap between scaphoid and lunate. In some
cases, the ulnar shift is subtle, and a decrease in the ulnocarpal
index may provide the only clue to diagnosis. Ulnar translation is also
commonly seen in diseases such as rheumatoid arthritis and in
developmental deformities such as Madelung deformity. It may occur with
an increase in the radial to ulnar slope of the distal radius.
translation can be seen in two modes: one a true instability secondary
to ligament damage, the other an apparent instability due to a carpal
shift in response to a change in position of the distal radial
articular surface. Pure dorsal translation usually occurs after a loss
of the normal palmar slope of the distal radius from a flexion angle to
an extension angle. The latter is a common problem after collapse of a
distal radius fracture.39
reduction because the associated deformity may compromise adjacent
neurovascular structures. Although reduction is usually possible,
maintaining it is often difficult. Open treatment should be considered
in most carpal dislocations. In Dumontier type I injuries, the volar
radiocarpal ligaments should be repaired, often using anchor sutures to
prevent secondary ulnar or volar translation.49
Where there is a substantial fracture fragment, the volar ligaments are
likely to be attached to it. Open reduction and internal fixation of
the fragment should be used. Added stabilization of the radiocarpal
joint is recommended using percutaneous K-wires or external fixation to
prevent late carpal translation, especially in type I injuries.49,94 Concomitant intercarpal ligament injuries should also be repaired.128 Limitation of wrist movement of 30% to 40% of normal should be expected following radiocarpal dislocation.49,131
dorsal or palmar translation deformity has responded poorly to
ligamentous repair. The most certain method of controlling possible
recurrence of deformity is to carry out a partial or total radiocarpal
arthrodesis. RL fusion is an appropriate technique for this situation,
although the variation of joint damage may indicate radioscaphoid
fusion in some cases and radioscapholunate fusion in others. The latter
is usually indicated in the combination of radiocarpal and perilunate
instability.39
frequent pattern of carpal instability. It may occur alone or in
association with wrist fractures.13,35,39,108,130,159,176
Most injuries result from excessive wrist extension and ulnar deviation
with intracarpal supination such as occurs with a fall onto the
outstretched pronated hand. SLD includes a spectrum of injuries ranging
from grade I sprains through all grades of ligament destabilization of
a single SLIL to injuries of multiple ligaments up to scaphoid
dislocation (SLD, SL-instability, rotatory subluxation of scaphoid,
DISI). A variety of ligament injuries are associated with SLD. The
involved ligaments include the SLIL, the radioscapholunate ligament,
the radioscaphocapitate ligament, the scaphotrapezial ligament complex,
the dorsal radiocarpal ligament, and the dorsal intercarpal ligament.
Disruption of the SLIL results in separation of the motion between the
scaphoid and lunate in the acute phase and the development of
persisting widening of the SL joint as a late clinical consequence (Fig. 29-28).175
tightness or laxity of the capsuloligamentous system of the wrist and
the presence of any associated palmar radiocarpal or midcarpal ligament
damage. Without treatment, this injury leads to advanced SL collapse
and progressive, painful arthritis of the wrist (see Fig. 29-28). SL injuries in children are rare9 and should be treated operatively.
which is usually consistent with a dorsiflexion ulnar deviation injury
with stress loading of the extended carpus. This combination of
position and axial compression causes injury to the SLIL
and palmar wrist ligaments.19,130
Particularly vulnerable are the radioscaphocapitate and RL ligaments,
which are under maximum tension in dorsiflexion and ulnar deviation. In
Mayfield’s classification, this injury is stage I (Fig. 29-29).
Prior or repetitive injury or the presence of acute or chronic
synovitis modifies the degree of stress required to the point that the
index event may be fairly trivial, such as slamming a car door or
catching a basketball.39
 |
|
FIGURE 29-28 SLD in a 60-year-old woman that was treated conservatively resulting in progressive carpal collapse and painful arthritis.
|
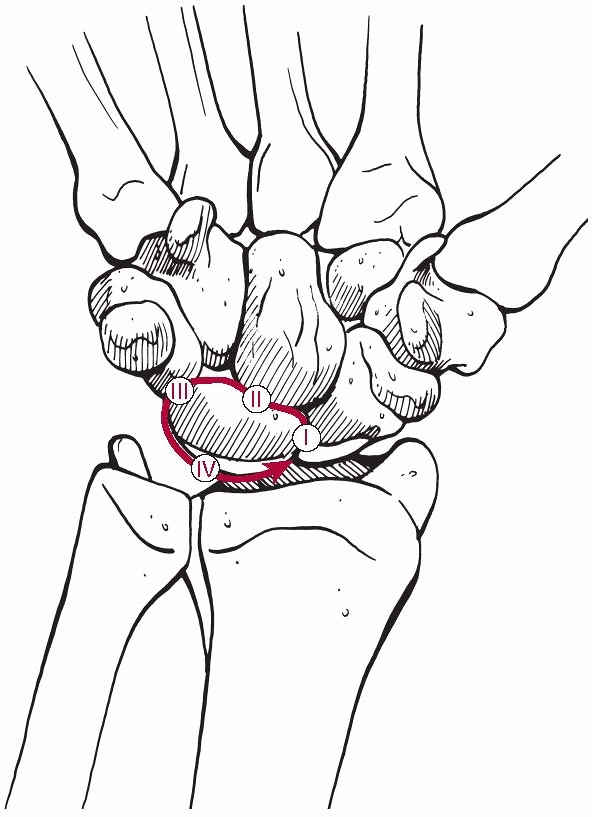 |
|
FIGURE 29-29
The Mayfield stages of progressive perilunate instability. Stage I results in SL instability. Stages II-IV result in progressively worse perilunate instability. |
the SL area. Associated radial styloid fractures may cause pain over
the radial styloid. A neurovascular examination is imperative, as acute
carpal tunnel syndrome can occur with carpal fractures and dislocations.130
The degree of associated stability may be such that only provocative
stress will reveal the classic findings. An easy provocative maneuver
is a vigorous grasp that induces pain; another indication is decreasing
repetitive grip strength. The patient may also demonstrate pain during
flexion-extension or radioulnar deviation.
the region of the proximal scaphoid and sometimes by a visible
deformity dorsally. A positive Watson test is highly suggestive of SL
instability (Fig. 29-30A). This test is not
absolutely specific for SLD, because it may reposition the entire
proximal carpal row if the row, rather than the individual scaphoid, is
unstable. In addition, in individuals with lax ligaments, there may be
false-positive signs of dorsal subluxation of the scaphoid that are not
pathologic. Generalized ligamentous laxity may be present, as many
wrists with an SL injury have some form of preexisting ligamentous
laxity.39,120,130,174
the diagnosis of SL instability. SL injuries may be associated with
fractures of the radius or carpus, especially in younger patients.
Radiographs of patients with fractures of the distal radius should be
evaluated closely for evidence of ligamentous injury. A greater arc
injury is associated with radial styloid fractures and SL ligament
disruption.130 Gilula lines should be examined to evaluate ligamentous instability (see Fig. 29-10A).
The appearance of the lunate should also be assessed. The lunate
projects as a quadrilateral shape on the AP radiograph in normal
wrists. Malrotation of the lunate makes it appear more triangular, this
being commonly seen in perilunate dislocations.
greater than 5 mm confirms SLD if there is a positive cortical ring
sign (see Fig. 29-10B). An AP view with the
fist clenched can be helpful as it accentuates the SL gap. This
increased space between scaphoid and lunate has been named the Terry
Thomas sign61 after the gap-toothed smile of the British comedian (Fig. 29-30B). However, the techniques used to measure the diastasis have not been uniform (Fig. 29-30C). Generally, it is suggested that the SL gap should be compared to the uninjured opposite extremity.32,174 SL diastasis without a dorsiflexed lunate is most likely nontraumatic.134 Similar findings may be apparent on views of the contralateral extremity.
axes of the scaphoid and the lunate. The long axis of the scaphoid is
determined by a line tangential to the palmar convex surfaces of the
proximal and distal poles of the scaphoid. The longitudinal axis of the
lunate is a line perpendicular to the line connecting the dorsal and
palmar lips of the lunate (Fig. 29-30D). Normal
SL angles range from 30 to 60 degrees. The lateral radiographic
appearance of a SL angle greater 60 degrees suggests SL instability,
and if the angle is greater than 80 degrees, the radiographic
appearance confirms SL instability.40,78,89,114,134
The RL angle describes the tilt of the lunate with respect to the
radius. A capitolunate or RL angle greater than 15 degrees is suspect,
but if greater than 20 degrees, it confirms SL instability. Carpal
height ratio (Fig. 29-30E), which is carpal
height divided by the length of the third metacarpal, is used to
quantify carpal collapse. A DISI deformity with a dorsally angulated
lunate and a flexed position of the scaphoid is a typical consequence
of SLD. Another sign suggestive of SL instability is the cortical ring
sign (see Fig. 29-10B), which suggests that
the scaphoid is flexed. The distal tubercle of the scaphoid is seen
end-on on an AP projection of the wrist.32,174
maneuvers discussed earlier may cause them to appear. If SL instability
cannot be seen with clenched-fist views or radioulnar stress
radiographs, then fluoroscopy or cineradiography using standard and
provocative stress motions should be performed. Arthrography has a high
rate of false-positive and false-negative results and is therefore not
recommended. Arthroscopy can be used to determine the extent of
ligament disruption and the presence of radioscaphoid arthritis, as
well as to classify and treat SL injuries.72,91 MRI is helpful in discriminating the extent of ligament injury.
being helpful for planning further treatment procedures. Static
deformity does not occur with isolated injury to the dorsal SL ligament.17
Static instability, which means that the injury can be identified on
plain AP and lateral radiographs, occurs when the dorsal SLIL is
injured along with the palmar ligaments, particularly the RL ligaments
and the radioscaphocapitate ligament. Dynamic instability, which cannot
be determined with plain radiographs, but may be apparent on stress
radiographs or fluoroscopy, is thought to result from isolated injury
to the dorsal SLIL.130,151
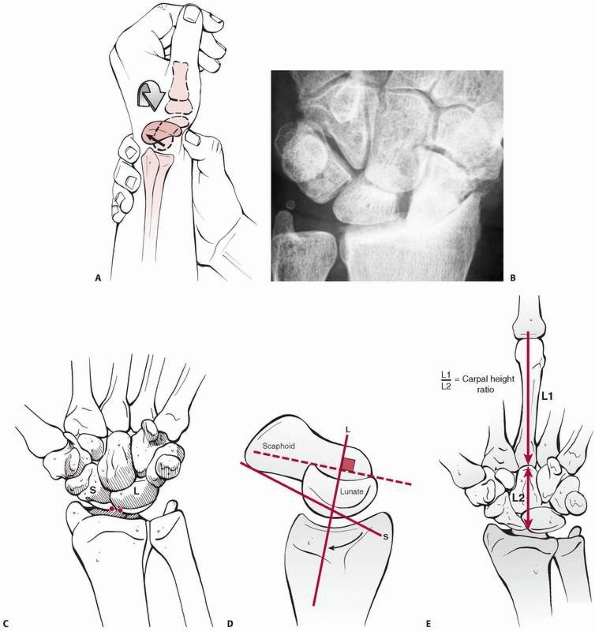 |
|
FIGURE 29-30 A.
Watson test: pressure applied to the palmar aspect of the scaphoid tubercle while moving the wrist from an ulnar to radial deviation. A positive test elicits a combination of pain and a palpable clunk or snapping. B. Radiograph of patient with old SL instability, Terry Thomas sign, and progressive arthritic deformation of the radiocarpal joint. C. Measurement of the SL gap from the proximal ulnar corner of the scaphoid to the proximal radial corner of the lunate. D. The SL angle is created by the long axis of the scaphoid and a line perpendicular to the capitolunate joint. E. Carpal-height ratio. |
identified four grades of ligament injury arthroscopically. In grade I
injury, attenuation or hemorrhage of the ligament is seen from the
midcarpal space but the bones are congruent. In grade II injury, there
is incongruency between the carpal bones when viewed from the midcarpal
space. In grade III and IV injuries, there is a gap between the carpal
bones allowing entry of a 1-mm probe in grade III and a 2.7-mm
arthroscope in grade IV.
on the duration of injury, extent of ligamentous involvement, and the
presence of associated carpal instabilities. The patient with an injury
fewer than 4 weeks old is considered to have an acute tear. If the
injury occurred less than 4 weeks but few than 24 weeks prior, it is a
subacute tear. If it is greater than 6 months from injury, the tear is
chronic and may be reducible or irreducible. Depending on the mechanism
of injury and amount of force across the wrist, the SL ligament may be
accompanied by injuries to the palmar radiocarpal and LT ligament or
the TFCC.
carpal instability may be treated conservatively with cast
immobilization. Cast immobilization is ineffective in unstable cases176 because the scaphoid requires wrist extension to maintain reduction and the lunate requires wrist flexion.
identified arthroscopically (Geissler grade II), percutaneous K-wires
in combination with cast immobilization for 8 weeks can be used. Such
injuries, even if not initially associated with obvious instability,
can progress to SL collapse.192 One
K-wire is placed from the scaphoid to the lunate and another from the
scaphoid to the capitate. Pins can be placed into the scaphoid and
lunate and used as joysticks to reduce the SL joint. Whipple203
reported an 85% success rate in maintaining SL reduction in patients
with an SL interval that was greater than the unaffected wrist by 3 mm
or less and whose injuries were less than 3 months old. Results were
less satisfactory in patients with a wrist injury that was older than 3
months.
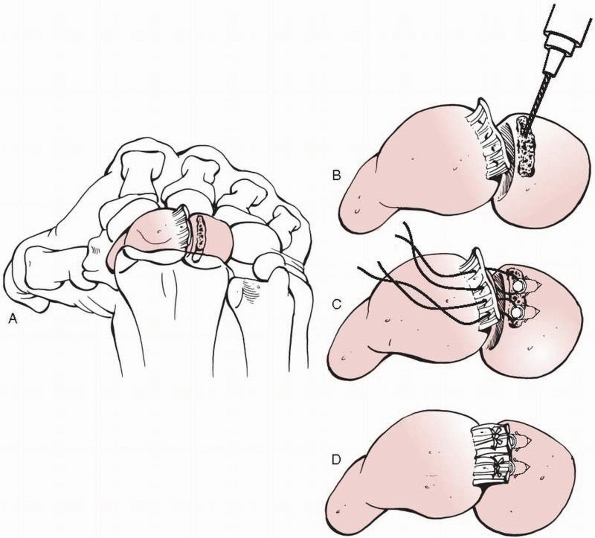 |
|
FIGURE 29-31 A-D.
Ligament reapir for SL instability. Anchors are placed into the lunate (or scaphoid, depending on where the SLIL has ruptured), and the ligament is sutured back into position. |
all acute SL injuries unless the carpus is easily reduced anatomically
by closed techniques and remains reduced in sequential radiographs
without carpal malalignment. An increasing SL angle exceeding 60
degrees, a lunatocapitate angle exceeding 15 degrees, or an increasing
scapholunate gap greater than 3 mm are indications for operative
intervention. Anatomic restoration of the SL complex by open ligament
repair is a realistic goal when the patient presents early. Soft tissue
repair and reconstruction are popular because they attempt to restore
the normal kinematics of the wrist. Arthroscopy of the wrist can assist
in confirming the diagnosis and determining the location and extent of
ligamentous damage. The technique of repair changed considerably with
the introduction of intraosseous suture retaining anchors allowing
ligament attachment directly to the bone (Fig. 29-31).204,210
stabilization of the carpal bones in their proper alignment and the
maintenance of wrist mobility. The earlier ligament repair takes place,
the easier it is to perform a direct repair. The results of direct
ligament repair are superior to ligament reconstruction.65
Experimental studies have shown that reduction of the displaced SL
joint is essential to the recovery of wrist kinematics after SLD.175
reported on the outcome of 12 patients at an average of 19 months. In
10 patients, there was maintenance of a normal SL angle. The average
range of motion was 78%, and the average grip strength was 81% of
normal. Eight patients had excellent or good results. However, there
was no correlation between functional and radiologic results although
one of the two poor results was associated with lunate necrosis. Longer
term outcomes are uncertain.
fractures should be operatively treated as the results of conservative
treatment are unacceptably poor.210
An ulnar positive variance of more than 2 mm in nonosteoporotic
patients with intraarticular fracture of the distal radius has been
shown to be predictive of severe SL injury.58
SLD using a dorsal approach. The approach is centered over Lister’s
tubercle, reflecting the dorsal wrist capsule to preserve the dorsal
intercarpal and dorsal radiotriquetral ligaments, using a radial-based
capsular flap. The radial capsule is reflected from the scaphoid to its
waist. The open technique allows direct visualization of the injured
ligament, reduction, and ligament repair. Most often, the SL ligament
is found to be torn off the scaphoid and still attached to the lunate.
In rare cases, avulsion from the lunate or an oblique tear will be seen.
K-wire joysticks inserted in a dorsal to palmar direction. The rim of
the proximal scaphoid is freshened to subcortical bone with a fine
rongeur to facilitate ligament healing. Ideally, high-speed burrs
should be avoided as thermal necrosis may occur. When the ligament
remains attached to the lunate, intraosseous anchors are inserted into
the waist of the scaphoid. The anchors are placed in such a position
that the suture lies in a slightly oblique direction in order to resist
the rotational forces between scaphoid and lunate (see Fig. 29-31).20
The sutures attached to the anchors are placed in the SL ligament in a
palmar to dorsal direction. If anchors are not available, drill holes
in the scaphoid are required to allow direct attachment of the ligament
onto the scaphoid. When the sutures are positioned, the scaphoid and
lunate are reduced with joysticks and held in the reduced position with
K-wires. One K-wire is placed from the scaphoid to the lunate and
another from the scaphoid to the capitate. The sutures are tied and the
capsule repaired. A forearm cast is applied and retained for 12 weeks,
when the K wires are removed.
reflects a proximally based dorsal capsular flap onto the SL
interspace, and this is sutured tautly to the dorsal scaphoid to act as
a tether to the proximal pole. This flap can be added to the ligament
repair process described earlier by placing nonabsorbable sutures from
the lunate ligament remnant into the capsular tissue and then out
through the scaphoid. An alternative method is to use a strip of tendon
from the radial wrist extensors (extensor carpi radialis longus or
extensor carpi radialis brevis), but tendon tissue is not an ideal
ligament replacement, and capsular tissue is preferred.39
A palmar approach with direct ligament repair by nonabsorbable sutures
can be performed. If there is deficient tissue in the subacute case,
part of the flexor carpi radialis can be used to augment the repair
process by placing drill holes through the proximal scaphoid and radial
half of the lunate and passing one half of the flexor carpi radialis
tendon in a circular fashion to reinforce the dorsal and palmar
ligaments. The radioscaphocapitate and RL ligaments may be advanced
into the gap. With a large, complete SL ligament tear associated with a
wide SL gap of 5 mm or more, palmar ligament repair is usually needed.39
A carpal tunnel incision extended slightly radially is performed, and
the damaged area is identified with a probe inserted from a separate
dorsal incision. The interval between the radioscaphocapitate ligament
and long RL ligament is developed. Sutures may then be placed with
intraosseous anchors into the scaphoid proximal pole or remnants of the
interosseous membrane, which are then used to pull the RL ligament
against the proximal pole to hold the overreduction of the proximal
scaphoid, which is stabilized by K-wires. The purpose of this palmar
repair is to bring the dorsally subluxed and rotated proximal scaphoid
in apposition with the palmar intracapsular ligaments.
tight repair of the capsular structures is required for subacute
dissociation. Internal fixation for a period of 12 weeks is preferred,
supplemented with a supportive Colles cast. After cast removal, an
orthoplast splint is worn as muscle strength and joint motion are
restored. Return to work or sports is best delayed for a minimum of 6
months, with continued protection being used during sports activities.
whether the ligaments can be directly repaired, whether any residual
carpal dislocation is reducible, and whether the joint has developed
arthritis. When possible, restoration of normal carpal anatomy by
repair and reconstruction of the support ligaments of the wrist remains
the preferred treatment. This requires sufficient local tissue for a
repair and a correctable carpal instability. When the patient presents
with a fixed carpal deformity and the rotational subluxation of the
scaphoid or dorsal angulated lunate (DISI) cannot be reduced, or when
local degenerative changes or work demands that require heavy lifting
or repetitive stress loading are present, the alternative of partial or
complete fusion of the wrist may be preferred.39 There are many techniques described to treat chronic SL instability.21,39,158,171 Weiss et al.200
showed that, in patients with a suspected intercarpal ligament tear and
normal radiographs, arthroscopy was useful for both diagnosis and
treatment. Current techniques for ligament reconstruction include
repair with the dorsal capsular flap procedure,
a
palmar ligament reefing procedure, and combined dorsal and palmar
procedures that add flexor or extensor tendon tissue to the repair
site. The goal of each of these repair techniques involves the addition
of local tissue to provide a collagen framework for future stability.21,39,171
Soft tissue reconstructions have several theoretical advantages that
make them attractive alternatives to other procedures. In contrast to
arthrodeses, soft tissue reconstructions preserve more intercarpal
motion.171
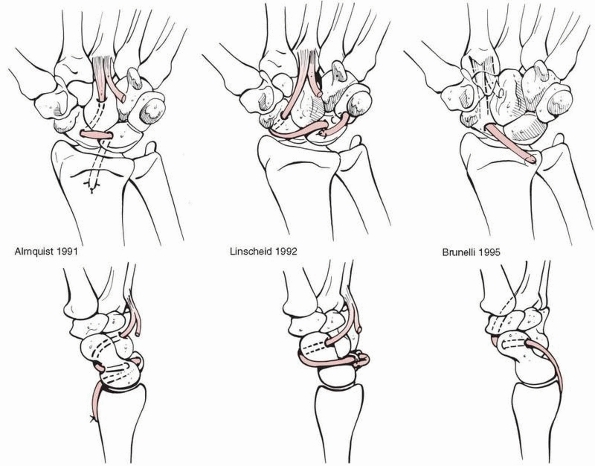 |
|
FIGURE 29-32 Tendon weaves and reconstructions proposed by various authors.
|
described the dorsal intercarpal ligament capsulodesis, which is a soft
tissue reconstruction procedure based on the dorsal intercarpal
ligament of the wrist. The theoretical advantage of this method is that
it avoids a tether between the distal radius and scaphoid. This keeps
the proximal carpal row linked as a functional unit. Clinical results
seem to be encouraging.171
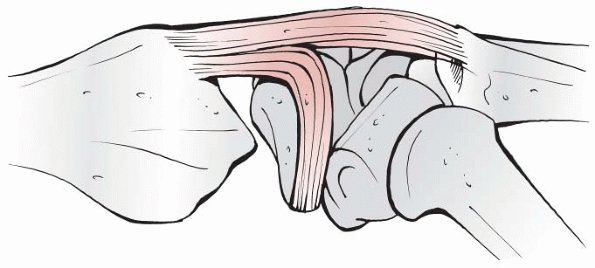 |
|
FIGURE 29-33 Blatt type of dorsal capsulodesis: The scaphoid is reduced and the capsular flap is secured to the distal pole with an anchor.
|
evaluated SL ligament repair and dorsal capsulodesis for static SLD and
found that no patients were free of pain at follow-up. The experience
of Wyrick and others suggests that dorsal capsulodesis is more suited
for patients with dynamic instability than for those with static
instability.13 Dynamic instability
is characterized by normal radiographs of the unloaded wrist, but a
typical step-off between scaphoid and lunate when evaluated
arthroscopically. Axial loading of the wrist can produce a widening of
the SL gap in dynamic instability. Static instability is characterized
by a widening of the SL gap in an unloaded wrist and an SL angle
greater than 60 degrees. Arthroscopy in such a case is grossly abnormal
and there is usually a communication between the radiocarpal and
midcarpal joints. Static instability requires an intercarpal
arthrodesis.
have been attempted with variable success. Wrist extensor or flexor
tendon augmentation procedures require placement of drill holes in
bone. In this procedure, drill holes are carefully placed in a
dorsal-to-palmar direction through the scaphoid and lunate. Tendon
strips are then passed through these holes to attempt a reconstruction
of the SLIL. The large holes required to pass tendon grafts often lead
to carpal fractures. An alternative technique is to take part of an
extensor or flexor tendon and pass it through the capitate, scaphoid,
lunate, and distal radius.5 Another
technique is the reconstruction of the dorsal part of the SL ligament
using a bone-ligament-bone autograft. However, clinical results are not
particularly convincing.98
A probe or needle passed dorsal to palmar is helpful in locating the
ligament tear and palmar ligament intervals. Flaps of
radioscaphocapitate and long RL ligaments are reflected laterally and
medially. The cartilage surfaces of the scaphoid and lunate are denuded
to subchondral bone to encourage a strong syndesmosis. The scaphoid and
lunate are then reduced and pinned with threaded wires that are left in
place for at least 8 weeks. The palmar ligaments are carefully
repaired. Motion is delayed 10 to 12 weeks to encourage adequate
strength of the syndesmosis.
For the Blatt type of capsule reconstruction, a long rectangular flap,
about 1.5 cm wide, based on the dorsal aspect of the distal radius, is
used. The distal edge of capsule is sutured to the distal pole of the
scaphoid once the scaphoid is placed in a reduced position. A K-wire
can be passed into the dorsum of the lunate to be used as a joystick to
reduce any DISI. The scaphoid is reduced by pressure on the scaphoid
tubercle and then transfixed to the capitate by another K-wire. The
dorsal surface of the scaphoid is roughened with a fine rongeur just
distal to the center of rotation. The dorsal flap of wrist capsule is
sutured under tension with intraosseous anchors distal to the scaphoid
center of rotation so that it tethers the proximal pole in the scaphoid
fossa. The flap is sutured to reinforce the local tissue of the SL
interval. For a distally-based flap, one can raise a rectangular
capsular flap, leaving the distal end of the flap attached to the
scaphoid.87
Colles cast is recommended for 8 weeks. The K-wires are removed at 8
weeks. Splint immobilization for an additional 4 weeks is suggested to
allow for tissue healing with gradual stress loading. Supporting
splints are best worn intermittently for 6 months to prevent sudden
stress to the wrist and to allow further collagen maturation.39
for SLD is based on the length of time from the original injury, the
degree of ligament disruption, and the ability to reduce the carpal
instability. The expectations of the patient are also important. The
presence of radiocarpal and midcarpal arthritis should influence the
decision toward intercarpal fusion. Arthroscopic examination of both
midcarpal and radiocarpal joints may determine the extent of SL
ligament and articular cartilage damage and therefore assist in
determining treatment.91 Of the
partial wrist fusions performed for wrist instability, the
scaphotrapeziotrapezoidal (STT) fusion has had the widest clinical
application.39,41,127
The purpose of this procedure is to stabilize the distal scaphoid and
thereby hold the proximal pole more securely within the scaphoid fossa
of the distal radius.195 This
operation can be performed through a transverse incision centered over
the STT joint or through the universal longitudinal incision.
fusion are undertaken, it is important to reduce the palmarflexed
scaphoid, close the SL interval, and maintain carpal height. Radiograph
control is recommended. The ideal flexion angle of the scaphoid is 45
degrees. Fixation of the STT or scaphocapitate joints is performed with
K-wires, screws, or staples. Bone graft from the distal radius or iliac
crest is placed between the decorticated distal scaphold and the
proximal surfaces of the trapezium and trapezoid (STT fusion) or
between the medial articular surface of the scaphoid and the lateral
surface of the capitate (scaphocapitate fusion). Once scaphoid
alignment is achieved, cancellous bone graft is inserted and K-wires
are placed to support the fusion area. Prereduction placement of
K-wires into the scaphoid facilitates correct orientation after
reduction.39 Clinical studies have shown that STT fusion is reliable and effective, giving pain relief and reasonable functional results.127 However, in the longer term, degenerative changes in adjacent joints may be a problem.59
weeks in a scaphoid cast, followed by a support splint for 4 to 6
weeks. CT scans of the wrist can help determine the degree of
consolidation at the fusion site.
severe arthritis can be treated with excision of the scaphoid and a
four-corner fusion with arthrodesis of the capitate, lunate, hamate,
and triquetrum.
common. Most patients are usually young males as the bone stock of the
distal radius and the scaphoid needs to be strong enough to resist the
amount of torque that is involved in these dislocations. Perilunate
dislocations are characterized by a progressive disruption of most
capsular and ligamentous connections of the lunate to the adjacent
carpal bones and radius. Ligament disruption typically begins radially
and propagates around or through the lunate to the ulnar side of the
carpus (Fig. 29-34). Ligament disruption may be
associated with different carpal fractures around the lunate. The
distal row dislocates in a dorsal or dorsoradial direction followed by
the entire scaphoid and triquetrum in pure perilunate dislocations or
just by the distal portion of these bones in perilunate
fracture-dislocations. SLD or LTD
often
persists even after relocation of the perilunate injury. Recurrence of
carpal instability is common whether the injury involves the lesser arc
injury through ligamentous tissue, the greater arc injury through bone,
or some combination of the two. The most common pattern of perilunate
instability is the transscaphoid perilunate fracture-dislocation.37,39,71,88,181
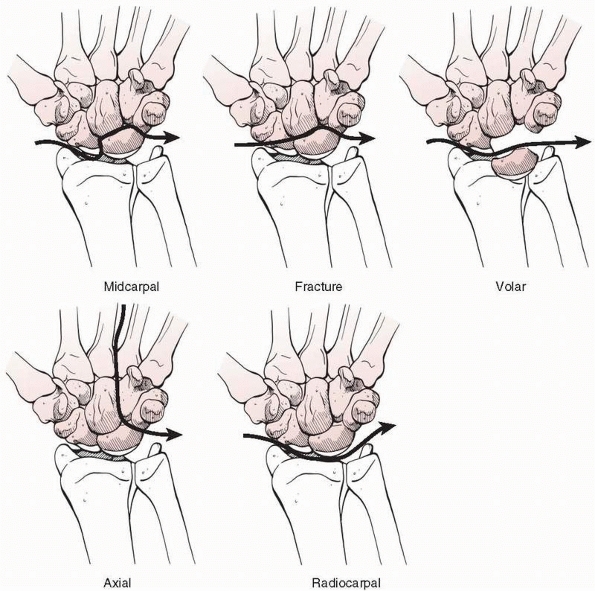 |
|
FIGURE 29-34 Different types of perilunate dislocations.
|
of a fall from a height on the outstretched hand or from motor vehicle
accidents. At the time of impact, the hand is typically extended and
ulnarly deviated.122 The axial
compressive load twists the joint beyond the limits of extension and
ulnar deviation, adding a progressive midcarpal supination stress that
induces the progressive perilunate dissociation. Differences in bone
stock, direction, and magnitude of the deforming forces or position of
the wrist at the time of impact explain the different types of injuries
that occur. These injuries are associated with marked carpal
instability.71,83,119,120,138
There are also rare cases of reversed perilunate instability, when the
wrist is pronated at the time that of impact thus adding an external
force to the hypothenar region, forcing the wrist into extension and
radial deviation. In such cases, the LTD occurs first followed by LTD
and then SLD.71,145
hyperextension injury and persistent pain, swelling, and deformity
often after a fall from a height or a motor vehicle accident. These
high-energy injuries produce significant deformity and soft tissue
damage. Commonly, the clinical presentation includes median nerve
injury, but ulnar neuropathy, arterial injury, and tendon damage may
also be seen. The pattern of skeletal deformity is variable. The hand
and distal carpal row usually remain intact, but the disruption pattern
between distal and proximal carpal rows is quite variable. In the
transscaphoid fracture-dislocation, the distal scaphoid dislocates with
the distal row leaving the proximal scaphoid and lunate in near-normal
relationship to the forearm. When the perilunate ligaments rupture, the
lunate usually remains within the radiocarpal joint and the remainder
of the carpus dislocates, usually dorsally but occasionally in a volar
direction. Occasionally, the lunate is displaced and rotated palmarly
and the remainder of the carpus settles into a seminormal alignment
with the distal radius. Rarely, even the palmar attachment of lunate is
torn, allowing extrusion into the forearm or through the skin.
AP and lateral radiographs. The typical radiographic appearances of a perilunate dislocation are:
 |
|
FIGURE 29-35 Typical radiologic signs of perilunate fracture-dislocation. A.
Gilula arcs show an obvious discontinuity. The dorsally dislocated distal carpal row creates an abnormal overlapping of bones across the midcarpal joint. The lunate appears triangularly shaped. Additionally, there is a typical injury of the radial styloid. B. The lateral view shows that the distal concavity of the lunate no longer contains the proximal convexity of the capitate. C. The oblique view demonstrates the gross dislocation. |
-
The proximal and distal outlines of the proximal carpal rows (Gilula lines) (see Fig. 29-10) present with a discontinuity that indicates a grossly altered intercarpal relationship.
-
The more the lunate is rotated the more it appears triangularly shaped.
-
On the lateral view, the lunate no longer
articulates with the head of the capitate, but appears palmarly
rotated, the so-called “spilled teapot sign.”
leading to late treatment which is difficult and frequently less
successful. It is usually the lesser arc dislocation that is missed
because of the lack of an obvious osseous pathology and inexperience of
the initial observer. Additional useful studies include tomography, CT
scanning, and MRI. Arthrography and arthroscopy may have a useful role
in determining the exact injury.
showed that the disruption of ligaments due to perilunate dislocation
is not random but follows the progressive perilunate instability (PLI)
pattern of joint derangement (see Fig. 29-29). Four stages of PLI have been identified.122
supinated, and ulnarly deviated, the STT and scaphocapitate ligaments
are tightened causing the scaphoid to extend. As the scaphoid extends,
the SL ligaments transmit the forces to the lunate, which cannot rotate
as much as the scaphoid, because it is constrained by the palmarly
located RL and ulnolunate ligaments. As a consequence, a scaphoid
fracture or a progressive tearing of the SL ligaments may occur,
eventually leading to a complete SLD.
once the proximal carpal row has been dislocated, the capitate may
displace and eventually may dislocate dorsally. It is followed by the
rest of the distal carpal row and the radial-most portion of the
dislocated proximal carpal row. This may be the complete scaphoid or
just its distal fragment.
once the capitate is displaced dorsally an LTD or
triquetrum-hamate-capitate ligament disruption may occur. LTDs are more
common. Stage III is complete when the palmar LT ligament, including
the medial expansions of the long RL ligament, is completely disrupted,
and the joint has displaced.
and the dorsally displaced capitate is pulled proximally, pressure is
applied onto the dorsal aspect of the lunate, forcing it to dislocation
in a palmar direction. Because the palmar ligaments are much stronger
than the dorsal capsule, such a dislocation seldom involves a pure
palmar displacement of the lunate, but rather a variable degree of
palmar rotation of the bone into the carpal tunnel, using the intact
palmar ligaments as a hinge. Lunate dislocation is the end stage of
progressive perilunate dislocation.
-
Lesser-arc perilunate dislocations, which are characterized by pure ligamentous injuries around the lunate.
-
Greater-arc perilunate dislocations, which are characterized by a fracture of one or more of the bones around the lunate.
the lunate may appear normally aligned (grade I), rotated palmarly less
than 90 degrees (grade II), rotated palmarly more than 90 degrees but
still attached to the radius by its palmar ligaments (grade III), or
totally enucleated without any connection to the radius (grade IV).
Based on this terminology, the amount of osseous and ligamentous injury
as well as the amount of dislocation can be described exactly; thus a
transscaphoid, transcapitate dorsal perilunate dislocation grade IV
implies the existence of a displaced fracture of the scaphoid and the
capitate, with their distal fragments being dislocated dorsally
together with the rest of the distal carpal row. The lunate is rotated
and totally enucleated without any connection to the radius
perilunate dislocations, (b) acute and irreducible perilunate
dislocations, and (c) chronic perilunate dislocations.
reductions that are so stable that it is difficult to determine whether
a full perilunate-type dislocation took place, and there are others
that reduce and can be maintained in near-normal alignment in casts and
splints. Ideally, reduction should be undertaken in the emergency room.
The most commonly used method of closed reduction is the Tavernier
maneuver, which was discussed by Watson-Jones.197
It consists of locking the capitate into the distal concavity of the
lunate by combined axial traction and flexion of the distal row,
followed by reduction of the capitate -lunate unit onto the radius by
an extension movement, while externally applying a localized dorsally
directed force to the lunate to help reposition it.71
The earlier reduction is performed, the easier it is. Complete
relaxation under general or regional anesthesia is required. Local
anesthesia is not sufficient. Successful closed reduction requires
adequate imaging with good, standardized AP and lateral radiographs of
the wrist or special imaging techniques. An SL angle that is greater
than 80 degrees, an asymmetric SL gap, or both indicates poor reduction
and a poor prognosis if not corrected. It is also important to confirm
ligamentous stability with stress-test imaging, MRI, arthroscopy, or
open exploration.
closed reduction can be treated with a scaphoid cast with the wrist
placed in neutral. They require monitoring on a daily basis for the
first week and on a weekly basis thereafter. Cast immobilization of 12
weeks is required. However, the results of closed reduction and cast
immobilization are unpredictable with loss of reduction with cast
loosening being common.39 It is now
generally agreed that the risk of late deformity after successful
reduction and cast management alone is unacceptably high.2,10
carpus after closed reduction is now recommended. This reduces the
incidence of later loss of reduction and enhances the healing
capability of the intrinsic ligaments by maintaining complete
immobility.71 If possible, pin
fixation should be performed using arthroscopy. Perilunate dislocations
that are stable after reduction require only two pins for fixation. One
transverse pin is placed from the scaphoid into the lunate (this can
also be pinned through the radius into the lunate to neutralize the RL
alignment), and a second pin is placed from the scaphoid into the
capitate. The pins are usually removed at 8 weeks, but wrist
immobilization in a scaphoid cast should be maintained for a total of
12 weeks after reduction.71
majority of perilunate injuries fall into the irreducible or unstable
group. If reduction is not optimal or reduction cannot be achieved at
all, then open exploration and repair is indicated.79
We believe that open reduction should be undertaken in all cases where
there is the slightest doubt about reduction or stability.
Significantly better results have been reported after open reduction
and ligament repair compared to closed reduction and percutaneous
pinning.71,89
However, the prognosis is guarded even with successful reduction and
maintenance of intercarpal relationships. Trumble and Verheyden186
reported on 22 patients with perilunate dislocations treated with open
reduction, cerclage wire fixation, and ligament repair with an average
review period of over 4 years from injury. Patient satisfaction was
high for 15 patients but only 10 patients returned to the same type of
employment as before their injury. Range of movement was 87% and grip
strength 77% of the contralateral wrist.
cases of perilunate dislocation but the majority of patients experience
resolution of their symptoms after closed reduction.2
Immediate median nerve decompression is not usually required but should
be performed where there is no resolution of symptoms or where late
symptoms develop.47
If there are neurovascular problems, an additional palmar approach
allows access for median nerve decompression, vascular repair if
required, and repair of the damaged palmar carpal ligaments. This
allows both intra-articular and extra-articular damage to be assessed
and treated adequately.39,71,167 The surgery is similar to that for treatment
of SLD, except that an extended carpal tunnel release is performed. The
palmar capsule should be examined either along its attachments to the
radial rim or through the frequently damaged space of Poirier. The
dorsal capsule is usually opened along its origin from the dorsal
radial rim, as well as longitudinally in the space between the second
and fourth extensor compartments, and the proximal carpal row is
examined. If a scaphoid fracture is present, it can be reduced through
the dorsal approach, temporarily stabilized with K-wires, and fixed
with a cannulated screw. After the scaphoid is reduced, the lunate is
reduced to the neutral position using a K-wire as a joystick. The
normal SL relationship is restored, while a K-wire is placed through
the scaphoid percutaneously, from radial to ulnar, to stabilize the SL
joint. A second wire is placed through the scaphoid into the capitate.
The LT relationship is restored next and stabilized with another K-wire
from ulnar to radial. Torn ligaments can be repaired through the palmar
and dorsal incisions. Intraosseous bone anchors are used to repair the
SL and lunotriquetral ligaments.
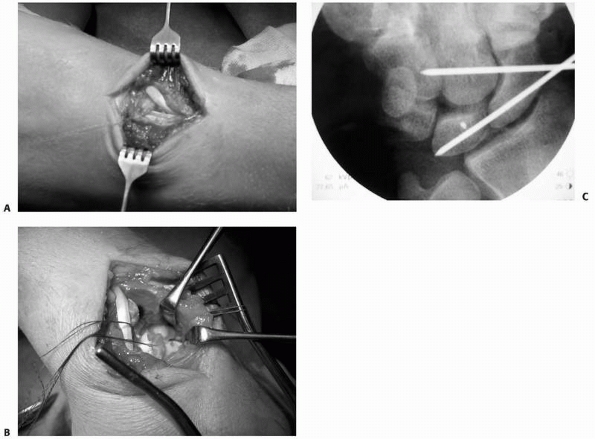 |
|
FIGURE 29-36 A.
The dorsal capsule is exposed through a longitudinal incision that is centered on the Lister tubercle, dividing the extensor retinaculum between the second and third extensor compartments. The fourth compartment is opened by sectioning the septum between the third and fourth compartment. B. A ligament splitting capsulotomy is performed exposing the dorsal structures. C. Reduction and percutaneous pinning is performed under direct control Additional K-wires can be inserted into scaphoid and lunate to help with the reduction. The dorsal SLIL and LT interosseous ligament are repaired then by using anchors and sutures. |
restore the normal bony anatomy, and repair soft tissue damage.
Reduction and K-wire fixation should be centered on the lunate. The
lunate must be aligned and pinned first to the distal radius to
neutralize the RL alignment. The LT joint is then reduced and fixed by
a second K-wire. Ligaments are repaired as needed. The capitolunate
joint alignment is then evaluated and correct colinear alignment is
assessed. Lastly, the SL joint is reduced and held with K-wires. Many
of the patients have an associated radial styloid fracture, which
should be reduced anatomically and stabilized with K-wires or a
compression screw.
This results in pain, reduced wrist motion, and considerable
dysfunction. Several clinical studies have shown that delay between
injury and treatment worsens the prognosis with neglected cases
resulting in pain, weakness, stiffness, posttraumatic osteoarthritis,
and carpal tunnel syndrome.88,89
Those injuries seen within 3 to 6 months are still potentially
treatable by open reduction as long as no cartilage degeneration has
already occurred, although treatment at this stage is often more
difficult because of articular changes and capsular contracture. A good
clue to the potential success of late reduction is gained by examining
radiographs of the carpus under 25 to 30 pounds of traction. An attempt
at open reduction (by palmar and dorsal approaches), repair, and
internal fixation should be offered if carpal bone realignment is
feasible, because even in late cases results can be surprisingly good.39,167
be seen months or years after the initial injury. The patient is more
likely to present because of increasing nerve symptoms or tendon
rupture than because of wrist deformity to which the patient has often
become accustomed. These very late problems nearly always require some
type of salvage operation, usually a proximal row carpectomy or a total
wrist arthrodesis.39
includes those where prior treatment has not been completely
successful. Depending on the time of presentation from injury and the
extent and type of any surgery that has already been undertaken, the
options for treatment are identical to those of acute treatment. When a
bone or bone fragment has been removed such as a proximal scaphoid or
capitate fragment, the alternatives are to rehabilitate the limb and
assess the functional level or to consider a salvage procedure such as
radiocarpal fusion or proximal row carpectomy.39
ruptures, bone avulsions, and various types of fractures, the most
common being the transscaphoid perilunate fracture-dislocation. In a
series of 166 perilunate displocations and fracture-dislocations,
fracture-dislocations were twice as common as pure dislocation.
Sixty-one percent of the whole series were dorsal transscaphoid
perilunate fracture-dislocations.89 Displaced transverse fractures of the neck of the capitate and sagittal fractures of the triquetrum are also quite frequent.9,54,71,88,170,173
The capitate fragment is frequently rotated through 180 degrees so that
its articular surface faces the raw cancellous surface of the major
capitate fragment. Both capitate and scaphoid fragments are
devascularized by displacement. This is known as the scaphocapitate
syndrome. It is important to define any associated ligamentous injuries
such as lunatotriquetral or SL disruption to prevent late carpal
collapse.101
followed by open reduction and internal fixation which is the best
method of achieving anatomic reduction of the fracture fragments. This
also allows repair of associated ligament injury37,54 or primary bone grafting where the scaphoid is comminuted.205
Cases can be performed through either a dorsal or a volar approach,
although a combined approach may be necessary especially if the
dislocation is irreducible closed.89 Some authors use a combined approach in all cases in order to repair the palmar capsule.90 Minimal invasive techniques of fixation and repair have also been used with satisfactory results.214 Arthroscopically assisted techniques have also been described.199
although the majority of cases have radiographic arthritis at longer
term review.89,90 Restoration of function is rarely complete with residual wrist stiffness and weakness of grip strength.89,90,101 Patientrated evaluation reflects loss of function.89,90,101
reduction and internal fixation of the scaphoid fracture. The use of
autogenous bone graft to restore scaphoid length may be required.
Ligamentous structures are assessed and repaired and reinforced with
K-wires in a similar fashion to the treatment of lesser arc injuries.
Soft tissue damage is common in these high-energy lesions, and it may
be obvious that a severe neuropathy or vascular compromise has
occurred. When these are present, open treatment and evaluation of the
structures at risk is essential. Treatment of vascular and nerve
injuries should proceed once the fractures are stabilized. Severe or
increasing median or ulnar neuropathy is an indication for surgical
exploration.
carpal row. Ligament tears between the lunate and triquetrum are
approximately one sixth as common as those between the scaphoid and
lunate.35 The LT ligament is much
thinner than its SL counterpart, and these two bones are much more
tightly coupled during wrist motion. LTD involves sprains as well as
partial or complete tears of the interosseous ligaments between the
lunate and triquetrum. It may present as an isolated injury, as part of
the spectrum of perilunate dislocation, or in association with
ulnocarpal impingement and TFCC injuries.39 Clinical signs are often diffuse and fall into the broad category of ulnar-sided wrist pain.
perilunate dislocation are well known but the mechanism of isolated
injury requires further study. Because the LT joint is more stable than
the SL joint, it seems apparent that associated ligament damage,
particularly to the dorsal radiotriquetral ligament or palmar
ulnocarpal ligaments, must be present before severe, fixed deformities
can occur.39 One of the problems
with LT disorders is that many patients have a normal radiograph.
Although LTD is not associated with the development of degenerative
changes in the carpus, it can have a devastating effect on carpal
mechanics, especially if it advances to a stage of VISI. Even without
this progression, the patient with chronic ulnar-sided pain experiences
significant ongoing disability.18
the articulation between the medial surface of the lunate and the
lateral surface of the triquetrum. The LT joint is also under the
influence of the radiocarpal and midcarpal joints. The radiocarpal
joint is a hybrid articulation between the proximal surfaces of the
lunate and the triquetrum which articulates with the lunate fossa of
the distal radius and the TFCC. Under normal circumstances, no more
than 50% of the lunate articulates with the TFCC.18
the LTIL. The LTIL is C-shaped and interdigitates with the dorsal
radiotriquetral ligament and palmar ulnotriquetral, ulnolunate, and
radiolunatotriquetral insertions. The palmar third of the LTIL is
stronger than the dorsal third, being supported by strong palmar
ulnocarpal ligaments. Dorsal extrinsic ligaments of importance are the
radiotriquetral and scaphotriquetral (dorsal intercarpal) ligaments,
which describe a V-shape from the dorsal aspect of the distal radius
near Lister’s tubercle to the triquetrum and then back to the dorsal
scaphoid rim. On the ulnar side of the wrist, the triquetrocapitate and
the triquetrohamate ligaments are a continuation of the ulnotriquetral
ligament.
into short and long RL ligaments. The radioscapholunate ligament
originates from the palmar aspect of the ridge between the scaphoid and
lunate fossae and inserts into the SLIL. Another important ligament is
the ulnolunate ligament, which arises from the palmar radioulnar
ligament to attach to the ulnar
half
of the palmar cortex of the lunate. The ulnotriquetral ligament arises
proximally from the palmar radioulnar ligament and the ulnar styloid
process. Palmar and superficial to the ulnolunate and ulnotriquetral
ligament is the ulnocapitate ligament, which reinforces both ligaments.
Distally, there are two strong midcarpal ligaments that arise from the
distal edge of the triquetrum: the triquetrocapitate and
triquetrohamate ligaments.18,39,102,122,174,178
such as a fall. There is a consensus that a true LTD is part of a
spectrum of progressive ligament disruption associated with a lunate or
perilunate dislocation. Mayfield et al.120,122
determined that there are two general patterns of damage in progressive
perilunate instability: damage to the greater and lesser arcs.
Greater-arc perilunate dislocations involve fracture-dislocations of
the radial styloid process, scaphoid, capitate, hamate, triquetrum, and
ulnar styloid process. Lesser-arc injuries involve only ligaments with
no associated fractures. The typical pattern of progressive perilunate
instability begins with disruption of the SLIL. The disruption
continues distally and ulnarly. Owing to the strength of the short and
long RL ligaments, the lunate typically remains associated with the
radius, but the radial half of the carpus begins to dislocate dorsally
away form the radius and lunate. The soft tissue disruption propagates
proximally, disrupting the LTIL, and often extending proximally into
the palmar radioulnar ligament of the TFCC. This dissociates the
triquetrum from the lunate.18,54,111,113,120,122
with ulnar-sided wrist pain aggravated by activity. Tenderness is
present directly over the LT joint, and ballottement of the unstable
triquetrum may be possible. Many patients even state that they sense a
“clunk” in their wrist with radial-ulnar deviation.18 Stress loading of the LT joint (compression, ballottement, or shear) helps to confirm the diagnosis.39
The most sensitive test to diagnose LTD is the LT shear test. This is
performed by applying a dorsally directed pressure to the pisiform
(which is directly palmar to the triquetrum) and a palmarly directed
pressure to the lunate (just distal to the palpable dorsoulnar corner
of the distal radius). This maneuver results in a shearing vector
across the lunotriquetral joint and results in crepitation or clicking,
reproducing the patient’s pain.
diagnosis of SLD because the findings are subtle and provocative;
stressinduced deformity is less frequent.39 As in all conditions of the wrist, imaging studies should be considered as confirmatory rather than diagnostic.18
True LTD may result in a disruption of Gilula’s lines. A static VISI
deformity implies an injury to the LT ligament because there is
dissociation between lunate and triquetrum, and the usual pattern is
for the lunate to follow the scaphoid into flexion while the triquetrum
extends.39 Wrist arthrography is not
a reliable diagnostic tool, but videofluoroscopy can be helpful.
Arthroscopy has become the most important diagnostic tool for
confirming the presence and degree of LTD. Radiocarpal and midcarpal
arthroscopy allows visualization of the scaphoid-trapezoid-trapezium
joint, midcarpal extrinsic ligaments, the capitohamate joint, and the
articular surfaces of the carpal bones. Arthroscopic staging is
applicable to SLD, LTD, and all other ligamentous dissociations.91
a wellmolded Colles cast using closed reduction and percutaneous
internal fixation of the lunate to the triquetrum if there is
displacement. If conservative measures fail, surgical intervention can
be considered.18
results from previous treatment may need open treatment, particularly
in the subacute or acute phase.39 Arthroscopy can be helpful in acute injuries to guide closed reduction and percutaneous pinning.136
It is suggested that the arthroscope be placed in the radial midcarpal
portal for this procedure because the alignment of the LT joint is much
easier to evaluate from this perspective.18
temporary internal fixation with percutaneous wires across the
triquetrum and lunate left in place for 6 to 8 weeks is recommended for
isolated LT ligament tears if arthroscopy fails. All ligaments that
seem to be concerned with LT stability should be reattached. An open
repair should be attempted only when there are sufficiently strong
ligament remnants present, when the ligament remnants have a reasonable
healing potential, and when the LT relationship is easily reduced.
These criteria limit the application of open repair techniques to acute
injuries.18
a dorsal approach. Care should be taken to avoid injury to the dorsal
sensory branch of the ulnar nerve or to branches of the superficial
radial nerve. The fifth extensor compartment is opened and an
ulnar-based retinacular flap is elevated. The ligament is more likely
to be stripped from the triquetrum. Intraosseous bone anchors with
attached sutures are used for reconstruction. Capsular flaps are useful
for reinforcing the dorsal portion of such a repair or augmenting the
dorsal radiotriquetral and dorsal scaphotriquetral ligaments. For late
presentations with complete ligament disruption and no tissue for
repair, ligament reconstruction using part of the extensor carpi
ulnaris tendon is recommended.39
tendency to recurrent deformity, LT fusion may be indicated. It is
mandatory to correct the VISI deformity. Treatment of the painful wrist
may be accompanied with denervation procedures. Concomitant ulnar
shortening procedures should be considered (especially with ulnar plus
variance) to tighten the palmar ulnocarpal ligaments in addition to LT
fusion or ligament reconstruction.39
More aggressive treatments are proximal row carpectomy and total wrist
arthrodesis in patients with radiologic signs of arthrosis.
-
Radially, there is a universal joint that
is composed of the distal surface of the scaphoid and the concavity
that is formed by the trapezium, the trapezoid, and the radial aspect
of the capitate. -
In the center, there is a ball-and-socket
type of joint, with the socket lying proximally being formed by the
distal surfaces of the scaphoid and lunate. The ball lies distally
being formed by the head of the capitate and, variably, the proximal
pole of the hamate. -
Finally, on the ulnar side of the
midcarpal joint, the triquetrohamate articulation is helicoid, or
screw-shaped, in configuration. A helicoid facet represents a surface
that is generated by the rotation of a plane or a twisted curve about a
fixed line, so that each point of the curve traces a circular helix
with the fixed line as the axis. The surfaces of the triquetrohamate
joint are only in full contact when the wrist is ulnarly deviated.
several anatomic structures including the bones and the intrinsic and
extrinsic ligaments. The intrinsic ligaments are not always well
differentiated and seem to form a continuous palmar capsule that spans
the entire width of the midcarpal joint space. However, it is possible
to discern two V-shaped ligamentous bands that converge centrally
towards the capitate. These bands are formed by the intrinsic palmar
midcarpal ligaments, the extrinsic radiocarpal and ulnocarpal
ligaments, the radioscaphocapitate ligament, and the short and long RL
ligaments. The extrinsic dorsal intercarpal ligament originates from
the dorsal aspect of the triquetrum, crosses the midcarpal joint almost
transversely in a radial direction, and inserts mainly onto the waist
of the scaphoid, the trapezium, and the trapezoid. Despite the fact
that there are no attachments to the capitate or hamate, the dorsal
intercarpal ligament is capable of holding the head of the capitate and
proximal pole of the hamate in position during wrist flexion. The
palmar distal V-shaped ligament, consisting of the radiocapitate and
ulnocapitate ligaments, also does not attach to the head of the
capitate, but forms a support sling commonly referred to as the arcuate
ligament. Together, these bands allow for maximum range of motion at
the level of the midcarpal joint with maximum midcarpal stability.39,134,149
MCI is characterized by a loss of normal alignment between the bones in
the proximal and distal carpal rows when they are placed under
physiologic and pathologic loads, due to ligament injuries of the
wrist. Carpal instabilities have been classified as dissociative and
nondissociative (CIND), which have already been discussed in the
section dealing with carpal instabilities. MCI is a form of CIND and is
difficult to diagnose.
the palmar midcarpal ligaments. This includes the
scaphotrapeziotrapezoid ligaments, the triquetrohamate and
triquetrocapitate ligaments, or both. The direction of subluxation is
palmar.
with an injury to the radioscaphocapitate ligament. The direction of
subluxation is dorsal.
and radiocarpal (dorsal and palmar) ligaments. The direction of
subluxation is dorsal or palmar.
with dorsal (less commonly palmar) angulation with adaptive deformity
of the carpus inducing progressive stretching of the radiocapitate
ligaments, thus reproducing the typical symptoms of a dorsal MCI. The
direction of subluxation is dorsal (rarely palmar).
between radiocarpal and midcarpal types of CIND. Some patients recall a
history of recent hyperextension injury and a localized area of
tenderness. However, many patients do not recall a significant trauma.
Frequently, MCI is associated with congenital ligamentous laxity and a
hypermobile wrist. Either VISI or DISI deformity or alternating
patterns may occur at either level. In the early stages, these patterns
of deformity may be so subtle that they are difficult to detect. Nearly
all patients with MCI present with painful clunking on the ulnar side
of the wrist during activities that involve active ulnar deviation.
Many of these patients have had asymptomatic wrist clunking for many
years.
painful and characteristic clunk (catch-up clunk) can be produced by
applying an axial load to a pronated and slightly flexed wrist, which
is then brought into ulnar deviation. The “catching-up” occurs when the
smooth transition during ulnar deviation lags behind until late in
ulnar deviation, when the proximal row suddenly clunks into a reduced
extended posture.35,149
The contralateral wrist should be examined in similar fashion, as 50%
of patients with MCI may also have a contralateral clunk that is not
yet symptomatic.209
often normal. However, they can show a moderate or even severe VISI
deformity (type I MCI) or a DISI deformity (type II MCI). An extrinsic
MCI (type IV) shows significant angulatory malunion with an adaptive
Z-shaped deformity of the carpus.149
Videofluoroscopy, while moving the compressed carpus through the normal
range of motion and applying ulnar deviation to the pronated wrist,
shows a dramatic and sudden shift at the midcarpal joint, when the
proximal row suddenly clunks into a reduced extended posture.39,149
radiocarpal or midcarpal CIND and drawing a careful distinction between
these uncommon and unusual injuries is difficult. Comparison of video
motion patterns of the symptomatic wrist to the normal contralateral
wrist is often useful.39 These
difficulties are compounded by the fact that ligament insufficiency,
which is usually posttraumatic but occasionally congenital,209
may be present at both radiocarpal and midcarpal levels. Visualizing
both joints and the intervening proximal carpal row by arthroscopy75
or surgery gives the final opportunity to decide where the instability
is most noticeable. Inflammatory synovitis and clear ligament laxity
are the diagnostic signs. Even then, one may have to judge from subtle
deviations from the norm because the attenuation may not be obvious.39
patients with MCI, especially the milder variety, respond well to
nonoperative management. Many of these wrist problems occur in
individuals with congenitally or posttraumatically lax wrists who can
control the subluxation tendency to some degree by muscle contraction.
In such instances, external support to limit the provocative wrist
motion together with musculotendinous training may suffice.
Additionally, patients may be treated with nonsteroidal
anti-inflammatory drugs or steroid injections or modification of their
employment may be suggested.39,149
whom conservative treatment has failed, surgery aims to prevent
pathologic motion at the midcarpal joint and to stabilize the proximal
carpal row. If a specific lesion can be identified, such as damage to
radial arcuate (radioscaphocapitate) ligament, the ulnar palmar arcuate
(triquetrocapitate) ligament, or the scaphotrapeziotrapezoidal
ligament, direct soft tissue reconstruction is indicated with temporary
percutaneous fixation.39,149
In type II MCI, the interligamentous sulcus between the
radioscaphocapitate and the long RL ligaments is closed with strong
sutures constructing a radiocarpal tether between radius and proximal
carpal row that limits proximal row excursion. If manual reduction is
incomplete or there is rapid recurrence after reduction, localized
fusion of the midcarpal joint is the best treatment.39,95,149
In type III MCI, radiocarpal fusion is more likely to control the
unstable proximal carpal row but proximal row carpectomy is a
satisfactory salvage procedure.
bone grafting in combination with plate fixation of the radius is the
treatment of choice. If there is associated instability of the distal
ulna, DRUJ problems, or fixed deformity of the carpus, then further
surgical alternatives, such as ulnar shortening, DRUJ stabilization, or
midcarpal joint fusion, may need to be undertaken at the same time.39,149
instability in which the injury affects longitudinal support or
alignment of the wrist rather than transverse alignment of the proximal
and distal carpal rows. Crush injuries that flatten the hand cause this
“axial” instability. Axial instabilities have been separately
categorized from other carpal injuries (Fig. 29-37).
They represent longitudinal fracture-dislocations of the wrist and, for
the most part, are caused by high-energy injuries. Traumatic causes
have included an exploding truck tire, crushing under heavy objects,
and high-pressure machine compression. The basic pathophysiology is
collapse of the carpal arch, often with tearing or avulsion of the bony
origins of the transverse carpal ligament. The focus of this injury is
usually in the distal carpus and adjacent metacarpals, occasionally
extending either distally into the intermetacarpal area or proximally
through the proximal carpal row.39
The most common pattern is separation of either radial or ulnar
“columns” of the carpus with their metacarpal rays from the central
carpus. From a review of the more common patterns, a proposed
nomenclature is axial-radial, axial-ulnar, or a combination of the two
fracture-dislocations. The carpal elements involved are usually
indicated by the term peri if the
discontinuity is primarily ligamentous, as in peritrapezial or
peritrapezoidal-trapezial. If the discontinuity is through bone, the
term trans is employed, as in
transtrapezial or transtrapeziotrapezoidal. The accompanying soft
tissue disruption is often of more importance than the bone and joint
disruption. Neurovascular injury is frequent, sometimes to the point of
nonviability of the digits.39
propagating in the sagittal plane, with a dorsal to palmar crush, often
with evidence of severe soft tissue damage, swelling, and open wounds.
Standard radiographs should confirm the diagnosis, although the carpal
malalignment may be subtle and escape notice. A high index of suspicion
is needed. Provocative stress radiographs, CT scanning, or MRI should
be obtained preoperatively. Evidence of neurologic, vascular,
musculotendinous, and ligamentous damage is usually present, often to a
severe degree. Instances of median neuropathy are less than expected,
probably because the carpal tunnel is usually decompressed by the
injury.39
planning of both soft tissue and joint repair. Urgent surgical
intervention is often indicated to salvage neurovascular function and
restore skeletal alignment. Massive swelling may necessitate
decompression of compartments not already decompressed by the injury.
Traction can help reduce the axial displacement. Fractures and
dislocations, once reduced, can be maintained by K-wires and lag
screws. Transcarpal or metacarpal K-wire fixation is usually necessary
to prevent redisplacement. Early active motion of the hand helps
prevent adhesions of the flexor and extensor tendons. Rehabilitation is
often prolonged, and the prognosis depends mainly on the severity of
soft tissue damage.39
-
Dissociative instability involves disruption of the ligaments or bone structure between the lunate and an adjacent carpal bone.
-
Nondissociative instabilities include
subluxations or incomplete dislocations of the entire carpus with or
without a distal radial fracture. -
Perilunate dislocation patterns include a considerable spectrum of sprains, fracture-dislocations, and instabilities.
-
SLD is the most common pattern of carpal instability.
-
A capitolunate or RL angle greater than 20 degrees confirms SL instability.
-
LT dissocation may result in disruption of Gilula lines on radiograph.
-
There are four types of MCI and the direction of subluxation may be palmar or dorsal.
-
A SLD without a dorsiflexed lunate is probably not traumatic.
-
In SLD, the results of K-wire treatment
are unpredictable. Ligamentous repair should be undertaken if closed
reduction is unsuccessful on serial radiographs. -
In chronic SL instability, partial or complete wrist fusion may be needed.
-
Sixteen to 25% of perilunate dislocations are missed initially.
-
Open repair of the LT ligament is only possible in acute injury.
-
Radiographs in MCI may be normal or may show a VISI or DISI deformity.
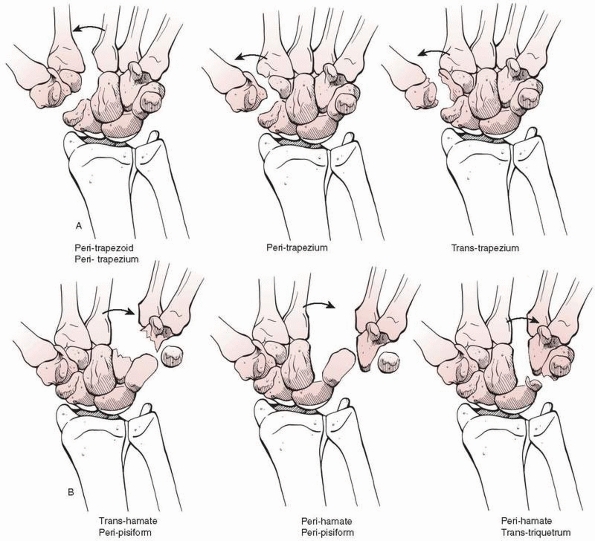 |
|
FIGURE 29-37 Axial disruptions of the carpus. A. Axial radial disruptions of the carpus. B. Axial ulnar disruptions.
|
and detection of carpal fractures and instabilities in the last decade,
mainly because of better imaging techniques. Unfortunately, the
dissemination of knowledge has lagged behind, and it is important that
surgeons appreciate the importance of early diagnosis and treatment of
these relatively common injuries.
better prediction of the evolution of individual carpal instabilities
and therefore determine the requirement for operative treatment at an
earlier stage. It is likely that improved surgical methods will be
devised to treat these problems. The use of closed, fluoroscopically
controlled and arthroscopically controlled techniques, especially in
the scaphoid, should increase and the results of treatment should
improve. It is interesting to speculate whether an increasingly aging
society will affect the diagnosis and management of carpal problems.
Currently, they mainly occur in younger patients, but with altering
patient demographics, this may not continue and a new set of challenges
may emerge.
DC, Mikola EA, Fraser BJ. Percutaneous fixation of the scaphoid through
a dorsal approach: an anatomic study. J Hand Surg Am 2008;33:327-331.
L, Lindau T, Arner M. Acutrak screw fixation versus cast immobilization
for undisplaced scaphoid fractures. J Hand Surg Br 2001;26:192-195.
A, Kankaanpaa U. Management of fractured scaphoid bone: a prospective
study of 100 fractures. Acta Orthop Scand 1975;46:737-743.
EE, Bach AW, Sack JT et al. Four-bone ligament reconstruction for
treatment of chronic complete scapholunate separation. J Hand Surg
1991;16-A:322-327.
G, Raby N. Scaphoid and pronator fat stripes are unreliable soft tissue
signs in the detection of radiographically occult fractures. Clin
Radiol 2003;58:798-800.
EP. The unstable capitolunate and radiolunate joints as a source of
wrist pain in young women. J Hand Surg 1996;21B(4):501-506.
EP, Darmanis S, Kastanis G, et al. Does the term scaphocapitate
syndrome need to be revised? A report of 6 cases. J Hand Surg
2001;26B(5):441-445.
E, Maris J, Theodoratos G, et al. Perilunate dislocations and
fracture-dislocations. Closed and early open reduction compared in 28
cases. Acta Orthop Scand Suppl 1997;275:55-59.
R, Gschwentner M, Krappinger D, et al. Fixation of nondisplaced
scaphoid fractures: making treatment cost effective. Prospective
controlled trial. Arch Orthop Trauma Surg 2007;127:39-46.
ME, Dunn MJ. Ligament injuries and instability of the carpus:
scapholunate joint. In: Berger RA, Weiss APC, eds. Hand Surgery. Vol.
1. Philadelphia: Lippincott Williams & Wilkins, 2004:460-479.
GP, Ferreira L, Johnson JA, et al. Interfragmentary compression across
a simulated scaphoid fracture—analysis of 3 screws. J Hand Surg
2004;29A:273-278.
RA. Lunotriquetral joint. In: Berger RA, Weiss APC, eds. Hand Surgery.
Vol. 1. Philadelphia: Lippincott Williams & Wilkins, 2004:495-509.
G. Capsulodesis in reconstructive hand surgery: dorsal capsulodesis for
the unstable scaphoid and volar capsulodesis following excision of the
distal ulna. Hand Clin 1987;3:81-102.
L, Trojan E, Jahna H. The results of treatment of 734 fresh, simple
fractures of the scaphoid. J Hand Surg Br 2003;28:319-331.
CD, Shin AJ, McBride MT, et al. Percutaneous screw fixation or cast
immobilization for nondisplaced scaphoid fractures. J Bone Joint Surg
Am 2001;83:483-488.
H, Krenn W, Schneider S, Graf M, et al. Arthrographie des
Handgelenkes-Wertigkeit im Nachweis von Komplett-und Partialdefekten
der intrinsischen Ligamente und des TFCC im Vergleich zur Arthroskopie.
Fortschr Röntgenstr 2003;175: 1515-1524.
MJ, Metz VM, Gilula LA, et al. Radiographically occult scaphoid
fractures: value of MR imaging in detection. Radiology 1997;203:245-250.
JH, Duncan SF. Isolated nondisplaced capitate waist fracture diagnosed
by magnetic resonance imaging. J Hand Surg 1999;24-A:856-859.
NR, Dias JJ, Costigan PS, et al. Need the thumb be immobilized in
scaphoid fractures? A randomized prospective trial. J Bone Joint Surg
1991;73B:828-832.
JP. The anatomy of acute scaphoid fractures. A three-dimensional
analysis of patterns. J Bone Joint Surg Br 1998;80:218-224.
WP, Bussey R, Dobyns JH, et al. Difficult wrist fractures. Perilunate
fracture-dislocations of the wrist. Clin Orthop Relat Res
1987;214:136-147.
WP, Linscheid RL, Dobyns JH. Fractures and dislocations of the wrist.
In: Rockwood CA, Green DP, Bucholz RW, et al, eds. Rockwood and Greens
Fractures in Adults. Philadelphia: Lippincott Williams & Wilkins,
1996:745-867.
EN, Chung KC, Kotsis SV, et al. A cost/utility analysis of open
reduction and internal fixation versus cast management for acute
nondisplaced midwaist scaphoid fractures. Plast Reconstr Surg
2006;117:1223-1235.
SC, Givissis D, Belloso D, et al. Blatt’s capsulodesis for chronic
scapholunate dissociation. J Hand Surg 1999;24B(2):215-220.
JJ, Brenkel IJ, Finlay DB. Patterns of union in fractures of the waist
of the scaphoid. J Bone Joint Surg Br 1989;71:307-310.
JJ, Wildin CJ, Bhowal B, et al. Should acute scaphoid fractures be
fixed? A randomised controlled trial. J Bone Joint Surg Am
2005;87:2160-2168.
B, Shaffer J. Treatment of perilunate and transscaphoid perilunate
dislocations of the wrist. Am J Orthop 1995;24:818-826.
AF, Vickers RH. Smoking increases failure rate of operation for
established nonunion of the scaphoid bone. Int Orthop 2007;31:503-505.
C, Meyer zu Reckendorf G, Sautet A, et al. Radiocarpal dislocations:
classification and proposal for treatment. A review of 27 cases. J Bone
Joint Surg Am 2001; 83:212-218.
F, Dautel G. Nonunion fractures of the scaphoid and carpal bones in
children: surgical treatment. J Ped Orthop 2004;13(1):34-38.
S, Fernandez DL, Beck T. Unstable scaphoid fracture nonunion: a
medium-term study of anterior wedge grafting procedures. J Hand Surg
2002;27B(1):36-41.
AG, Mayfield JK, Dorman F, et al. Kinematic and kinetic analysis of the
human wrist by stereoscopic instrumentation. J Biomech Eng
1979;101:124-133.
DP, Lindau T, Melsom D. Intercarpal ligament injuries associated with
fractures of the distal part of the radius. J Bone Joint Surg Am
2007;89:2334-2340.
C, Kukla C, Breitenseher MJ, et al. Die diagnostische Sicherheit von
0,2 Tesla dedizierten MRT Niederfeldgeräten in der Traumatologie. Swiss
Surgery 1998;4: 175-179.
C, Kukla C, Breitenseher MJ, et al. Limited diagnostic value of
macroradiography in scaphoid fractures. Acta Orthop Scand
1998;69:401-403.
CH, Kukla CH, Breitenseher MJ, et al. Diagnosis of occult scaphoid
fractures and other wrist injuries: Are repeated clinical examinations
and plain radiographs still state of the art. Langenbeck’s Archives of
Surgery 2001;386:150-154.
GJ, Jebson PJL, Louis DS. The versatility of a new variable pitch screw
system in hand, wrist and elbow surgery. Minneapolis, MN: Annual
Meeting American Society of Hand Surgery 1998.
M. Carpal bone fractures (excluding scaphoid fractures). In: Watson HK,
Weinberg J, eds. The Wrist. Philadelphia: Lippincott Williams &
Wilkins, 2001: 173-186.
M. Perilunate injuries including fracture dislocations. In: Berger RA,
Weiss APC, eds. Hand Surgery. Vol. 1. Philadelphia: Lippincott Williams
& Wilkins, 2004: 511-523.
WB, Freeland AE, Savoie FH, et al. Intracarpal soft-tissue lesions
associated with an intra-articular fracture of the distal end of the
radius. J Bone Joint Surg Am 1996;78:357-65.
RH, Gross MS. The vascularity of the wrist. Identification of arterial
patterns at risk. Clin Orthop Relat Res 1986;202:40-49.
RH, Panagis JS, Taleisnik J, et al. The arterial anatomy of the human
carpus: part I. The extraosseous vascularity. J Hand Surg
1983;8-A:367-376.
Ý, Öztuna V, Özcelik A, et al. Medium-term results of trapezio-lunate
external fixation of scaphoid fractures. J Hand Surg
2002;27B(5):410-412.
P. Long-term results after silicone prosthesis replacement of the
proximal pole of the scaphoid bone in advanced scaphoid nonunion. J
Hand Surg 2002;27B(5): 417-423.
TJ, Hargreaves IC, Clarke AM. A new surgical technique for treating
rotatory instability of the scaphoid. J Hand Surg1996;21-B:75-77.
G, Comtet JJ, Linscheid RL, et al. Perilunate dislocations and fracture
dislocations: a multicenter study. J Hand Surg 1993;18-A:768-779.
G, Forissier D. Acute dorsal transscaphoid perilunate
fracture-dislocations: medium-term results. J Hand Surg
2002;27B(6):498-502.
KA, Ross DC, Patterson SD, et al. Dorsal perilunate dislocations and
fracture-dislocations: questionnaire, clinical and radiographic
evaluation. J Hand Surg Am 2000;25:1069-1079.
EP, Dao KD, Glowacki KA, et al. The role of midcarpal arthroscopy in
the diagnosis of disorders of the wrist. J Hand Surg 2001;26A:407-414.
S, Schröder HA. Wrist arthrodesis with the AO titanium wrist fusion
plate: a consecutive series of 42 cases. J Hand Surg
2001;26B(4):355-359.
G, Powell G. Scaphoid fixation using the Acutrak screw. Presented at
the Australian/New Zealand Hand Surgery Meeting; Cairns, Australia;
September 25, 1996.
K, Markert S. Erste Erfahrungen mit der Osteoligamentoplastik und
Kapsulodese nach Cuénod zur Behandlung der chronischen skapholunären
Dissoziation. Handchir Mikrochir Plast Chir 2003;35:310-316.
VD, Allan C, Trumble TE. Transscaphoid perilunate fracture
dislocations: results of screw fixation of the scaphoid and
lunatotriquetral repair with the dorsal approach. J Hand Surg Am
2005;30:1145-1152.
JN, Boabighi A, Kirsch JM, et al. An experimental study of plaster
immobilization for fractures of the carpal scaphoid. A clinical
investigation. French J Orthop Surg 1987;1:43-50.
S, Raatikinen T, Kaarela O, et al. Successful treatment of scaphoid
fractures and nonunions using bioabsorbable screws: report of six
cases. J Hand Surg 2004;29A: 68-73.
JD, Hodge JC. Pisiform and hamulus fractures: easily missed wrist
fractures diagnosed on a reverse oblique radiograph. J Emer Medicine
1998;16:445-452.
CJ, Cohen MS, Taleisnik J. Treatment of scapho-lunate dissociation by
ligamentous repair and capsulodesis. J Hand Surg 1992;17-A:354-359.
DM, Schneider JR, Swafford AR, et al. Ulnar midcarpal
instability-clinical and laboratory analysis. J Hand Surg Am
1981;6:515-523.
RL, Dobyns JH, Beabout JW, et al. Traumatic instability of the wrist:
diagnosis, classification, and pathomechanics. J Bone Joint Surg
1972;54-A:1612-1632.
CP, Burston BJ, Hopkinson-Woolley J, et al. Failure of surgery for
scaphoid nonunion is associated with smoking. J Hand Surg Br
2006;31:252-255.
M, Kralinger F, Goldhahn J, et al. Dorsal scapholunate ligament
reconstruction using a periostal flap of the iliac crest. Arch Orthop
Trauma Surg 2004; 124: 197-202.
NM, Linscheid RL. Corrective osteotomy for scaphoid malunion: technique
and long-term follow-up evaluation. J Hand Surg 1997;22A:35-43.
JK, Johnson RP, Kilcoyne RK. The ligaments of the human wrist and their
functional significance. Anat Rec 1976;186:417-428.
JK, Kilcoyne RK, Johnson RP. Carpal dislocations: Pathomechanics and
progressive perilunate instability. J Hand Surg 1980;5:226-241.
HL. Fracture of the carpal navicular (scaphoid) bone. Some observations
based on treatment by open reduction and internal fixation. J Bone
Joint Surg 1954; 36A:765-774.
MM, Gelbke MK, Wakefield A, et al. Percutaneous screw fixation versus
conservative treatment for fractures of the waist of the scaphoid. A
prospective randomised study. J Bone Joint Surg Br 2008;90:66-71.
R, Prommersberger KJ, Krimmer H. Teil-arthrodesen von skaphoid,
trapezium und trapezoideum (STT-Fusion). Handchir Mikrochir Plast Chir
2003;35:323-327.
MS, Bolger JT, Omer GE. Radiocarpal dislocation-classification and
rationale for management. Clin Orthop Relat Res 1985;192:199-209.
H, Viegas SF, Nakamura K, et al. The scaphotrapezio-trapezoidal joint.
Part I: An anatomic and radiographic study. J Hand Surg
1999;25-A:899-910.
J, N’Dow K, Maffulli N, et al. The suspected scaphoid fracture. How
useful is a unit policy? Bull H J Diseases 1998;57:93-95.
H, Gilula LA, Evanoff BA, et al. Midcarpal instability: is capitolunate
instability pattern a clinical condition? J Hand Surg
1996;21B(2):197-201.
AL, Seidman GD. The role of arthroscopy in the treatment of
lunatotriquetral ligament injuries. Hand Clin 1995;11:41-50.
JM, Gelberman RH, Taleisnik J, et al. The arterial anatomy of the human
carpus II. The intraosseous vascularity. J Hand Surg 1983;8:375-382.
R. Proximal and palmar dislocation of the lunate and proximal scaphoid
as a unit in a case of scaphocapitate syndrome-a 32-month follow-up. J
Hand Surg 1998; 23B(2):266-268.
MY, Fusetti C, Christen T, et al. Minimally invasive fixation versus
conservative treatment of undisplaced scaphoid fractures: a
cost-effectiveness study. J Hand Surg 2004;29B(2):116-119.
J, Wayman J, Kelly P, et al. Combining the clinical signs improves
diagnosis of scaphoid fractures. A prospective study with follow-up. J
Hand Surg 1998;23-B: 324-327.
G. Zu einer typischen posttraumatischen und zur Spontanfraktur
führenden Osteitis des Naviculare Carpi. Fortschr Roentgenstr
1910;15:189.
AC, Weidenbener EJ, Gloyeske R. Alternative management of midthird
scaphoid fractures in the athlete. Am J Sports Med 1994:22:711-714.
ME, Dassa GL, Raskin KB, et al. Wrist fractures in the athlete. Distal
radius and carpal fractures. Clin Sports Med 1998;17:469-489.
MJPF. Midcarpal instability. In: Berger RA, Weiss APC, eds. Hand
Surgery. Vol. 1. Philadelphia: Lippincott Williams & Wilkins,
2004;525-532.
W, Tiel-van-Buul MM, Ritt MJ, et al. Experimental evaluation of
scaphoid X-series, carpal box radiographs, planar tomography, computed
tomography, and magnetic resonance imaging in the diagnosis of scaphoid
fracture. J Trauma 1997;42: 247-253.
LK, Stinson J, Belsky MR. The natural history of scaphoid nonunion: a
review of 50 cases. J Bone Joint Surg 1985;67A:428-432.
O. Fracture of the carpal navicular: diagnosis, nonoperative treatment,
and operative treatment. J Bone Joint Surg 1960;42A:759-765.
WE. Evaluation of the humpback scaphoid by computed tomography in the
longitudinal axial plane of the scaphoid. J Hand Surg 1988;13-A:182-187.
B, Tornkvist H, Ponzer S, et al. Fracture of the carpal scaphoid. A
prospective randomised 12-year follow-up comparing conservative and
operative treatment. J Bone Join Surg Br 2001;83:230-234.
M, Martini AK, Eversheim S, et al. Die bedeutung des intraossären
druckes für die pathogenese des morbus kienböck. Handchir Mikrochir
Plast Chir 1996;28: 215-219.
A, Steiger R. Long-term results after repair and augmentation
ligamentoplasty of rotatory subluxation of the scaphoid. J Hand Surg
2002;27A:674-684.
E, Wozasek GE, Hajdu S, et al. Okkulte skapholunäre Dissoziation bei
distaler Radiusfraktur. Wiener Klin Wochenschr 2003;115:580-583.
GR. Carpal bone fractures other than the scaphoid. In: Berger RA, Weiss
APC, eds. Hand Surgery. Vol. 1. Philadelphia: Lippincott Williams &
Wilkins, 2004: 409-423.
JF, Geissler WB, Gutow AP, et al. Percutaneous internal fixation of
selected scaphoid nonunions with an arthroscopically assisted dorsal
approach. J Bone Joint Surg 2003;86-A(Suppl 4):20-32.
RR, Szabo RM, Bay BK, et al. Dorsal intercarpal ligament capsulodesis
for scapholunate association: biomechanical analysis in a cadaver
model. J Hand Surg 1999;24A: 232-239.
BS, Cooney WP. Revision of failed bone grafting for nonunion of the
scaphoid. Treatment options and results. Clin Orthop Relat Res
1996;327:98-109.
P 3rd, Wright TW, Wallace PF, et al. Excision of the hook of the
hamate: a retrospective survey and review of the literature. J Hand
Surg Am 1988;13:612-615.
DG, Mitsionis GJ, Giannakopoulos PN, et al. Perilunate dislocation and
fracture dislocation: a critical analysis of the volar-dorsal approach.
J Hand Surg 1997; 22A:49-56.
PC, Laier P, Müller CA, et al. Erstbeschreibung des beidseitigen
auftretens einer seltenen verletzung. Unfallchirurg 2003;106:339-342.
RM, Slater RR, Palumbo CF, et al. Dorsal intercarpal ligament
capsulodesis for chronic, static scapholunate dissociation: clinical
results. J Hand Surg 2002;27A: 978-984.
JB, Ryu J, Omokawa S, et al. Wrist kinetics after scapholunate
dissociation: the effect of scapholunate interosseous ligament injury
and persistent scapholunate gaps. J Orthop Res 2002;20:215-221.
JB, Shi D, Gu YQ, et al. Can cast immobilization successfully treat
scapholunate dissociation associated with distal radius fractures? J
Hand Surg 1996;21A:583-590.
MMC, vanBeek EJR, Borm JJJ, et al. Radiography and scintigraphy of
suspected scaphoid fracture. A long-term study in 160 patients. J Bone
Joint Surg 1993; 75-B:61-65.
MMC, vanBeek EJR, Borm JJJ, et al. The value of radiographs and bone
scintigraphy in suspected scaphoid fracture. A statistical analysis. J
Hand Surg 1993; 18-B:403-406.
EB, Butler TE, McCormack TJ, et al. A comparison of fixation screws for
the scaphoid during application of cyclical bending loads. J Bone Joint
Surg 1997;79A: 1190-1197.
MM, King J, Pizillo M. Correction of lunate malalignment when bone
grafting scaphoid nonunion with humpback deformity: rationale and
results of a technique revisited. J Hand Surg Am 2000;25:322-329.
AJH, Davis TRC, Barton NJ. Factors influencing the outcome of bone
grafting surgery for scaphoid fracture nonunion. Injury 2000;31:605-607.
T, Verheyden J. Treatment of isolated perilunate and lunate
dislocations with combined dorsal and volar approach and interosseous
cerclage wire. J Hand Surg Am 2004;29:412-417.
V, Westerlund M. Fracture of the carpal scaphoid in children. A
clinical and roentgenological study of 108 cases. Acta Orthop Scand
1980;51:909-913.
B, Pietreanu M, Bodestedt A, et al. Nonoperative compared with
operative treatment of acute scaphoid fractures. A randomized
controlled trial. J Bone Joint Surg Am 2008;90:1176-1185.
JJ, Berger RA, Cooney WP. Current status of scapholunate interosseous
ligament injuries. J Am Acad Orthop Surg 2002;10:32-42.
PM, Stewart SL. Surgical treatment of nonunion and avascular necrosis
of the proximal part of the scaphoid in adolescents. J Bone Joint Surg
2002;84-A(6):915-920.
HK, Rogers WD. Nonunion of the hook of the hamate: an argument for bone
grafting the nonunion. J Hand Surg 1989;14:486-490.
D, Casaletto JA, Choa R, et al. Outcome following coronal fractures of
the hamate. J Hand Surg Eur 2009 Mar 12. [Epub ahead of print]
K, Kettler M, Strassmair MSL. Bandrekonstruktion mit
mitek-fadenankerdübeln. Erste klinische ergebnisse. Unfallchirurg
2001;104:127-130.
SW. Fractures of the carpus: scaphoid fractures. In: Berger RA, Weiss
APC, eds. Hand Surgery. Vol. 1. Philadelphia: Lippincott Williams &
Wilkins, 2004;381-408.
JD, Youse BD, Kiefhaber TR. Scapholunate ligament repair and
capsulodesis for the treatment of static scapholunate dissociation. J
Hand Surg 1998;23-B:776-780.
D, Lieppins P, Laurence M. Fractures of the carpal scaphoid. A critical
study of the standard splint. J Bone Joint Surg 1991;73B:600-602.
HSF, Wu WC, Chang RYP, et al. Percutaneous cannulated screw fixation of
acute scpahoid wrist fracture. J Hand Surg 2002;27B(1):42-46.
