Total Elbow Arthroplasty for Primary Osteoarthritis
Editors: Berry, Daniel J.; Steinmann, Scott P.
Title: Adult Reconstruction, 1st Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Section
IV – Elbow Reconstruction > Part C – Operative Treatment Methods
> 60 – Total Elbow Arthroplasty for Primary Osteoarthritis
IV – Elbow Reconstruction > Part C – Operative Treatment Methods
> 60 – Total Elbow Arthroplasty for Primary Osteoarthritis
60
Total Elbow Arthroplasty for Primary Osteoarthritis
Bassem Elhassan
Scott P. Steinmann
Definition
Degenerative primary arthritis of the elbow is an uncommon problem.1
It occurs in less than 2% of the population and principally affects the
dominant extremity in middle-age manual laborers. It has also been
reported in people who require continuous use of a wheelchair or
crutches, athletes, and in patients with a history of osteochondritis
dissecans of the elbow. It has different pathologic changes than the
age-related changes of the distal humerus and the radiohumeral joint.
It occurs in less than 2% of the population and principally affects the
dominant extremity in middle-age manual laborers. It has also been
reported in people who require continuous use of a wheelchair or
crutches, athletes, and in patients with a history of osteochondritis
dissecans of the elbow. It has different pathologic changes than the
age-related changes of the distal humerus and the radiohumeral joint.
Because of the younger age and increased activity levels
of patients with primary osteoarthritis of the elbow, the treatment
options are more limited and the role of total elbow arthroplasty is
less defined in this population of patients.
of patients with primary osteoarthritis of the elbow, the treatment
options are more limited and the role of total elbow arthroplasty is
less defined in this population of patients.
Pathology
Histopathologic Changes in Elbow Osteoarthritis
The degenerative changes of the elbow joint are usually
more advanced in the radiohumeral joint, where bare bone is often in
wide contact and the capitellum appears to have been shaved obliquely (Fig. 60-1).
This is owing to the high axial, shearing, and rotational stresses at
this articulation, which result in marked erosion of the capitellum and
callus hypertrophy formation in a skirtlike pattern on the radial neck.
more advanced in the radiohumeral joint, where bare bone is often in
wide contact and the capitellum appears to have been shaved obliquely (Fig. 60-1).
This is owing to the high axial, shearing, and rotational stresses at
this articulation, which result in marked erosion of the capitellum and
callus hypertrophy formation in a skirtlike pattern on the radial neck.
The ulnohumeral joint is usually less involved in the
beginning of the disease process and becomes more pronounced with more
advanced disease. The central aspect of the ulnohumeral joint is
characteristically spared. The anterior and posterior involvement of
this joint is usually manifested by fibrosis of the anterior capsule in
the form of cordlike band and hypertrophy of the olecranon.
beginning of the disease process and becomes more pronounced with more
advanced disease. The central aspect of the ulnohumeral joint is
characteristically spared. The anterior and posterior involvement of
this joint is usually manifested by fibrosis of the anterior capsule in
the form of cordlike band and hypertrophy of the olecranon.
Osteophyte growths are seen over the olecranon
(especially medially), the coronoid process, and the coronoid fossa.
These changes in the radiohumeral and ulnohumeral joints lead to the
loss and fragmentation of the cartilaginous joint surfaces with
distortion, cyst formation, and bone sclerosis. Kashiwagi noted that
the early stage of the disease is characterized by small, round bony
protuberances that progress into various shapes of osteophytes and bony
sclerosis with more advanced cases.
(especially medially), the coronoid process, and the coronoid fossa.
These changes in the radiohumeral and ulnohumeral joints lead to the
loss and fragmentation of the cartilaginous joint surfaces with
distortion, cyst formation, and bone sclerosis. Kashiwagi noted that
the early stage of the disease is characterized by small, round bony
protuberances that progress into various shapes of osteophytes and bony
sclerosis with more advanced cases.
Clinical Presentation
Despite considerable radiographic severity, many
patients with osteoarthritis of the elbow report minimal symptoms. This
is partly related to the fact that the elbow is a slight weight-bearing
joint compared with the lower extremity joints.
patients with osteoarthritis of the elbow report minimal symptoms. This
is partly related to the fact that the elbow is a slight weight-bearing
joint compared with the lower extremity joints.
Mechanical symptoms of locking and catching caused by
intra-articular loose bodies, pain at the end points of the arc of
motion (flexion or extension), and progressive loss of range of motion
are characteristic manifestations of osteoarthritis of the elbow. In
athletes who are required to hyperextend their elbows, pain can be
significant and limits their performance.
intra-articular loose bodies, pain at the end points of the arc of
motion (flexion or extension), and progressive loss of range of motion
are characteristic manifestations of osteoarthritis of the elbow. In
athletes who are required to hyperextend their elbows, pain can be
significant and limits their performance.
With more progressive disease, the patients may have
pain with forearm rotation and throughout the range of elbow motion.
This could lead to disability in this patient population as well as in
the older laborers who extensively use their upper extremity.
pain with forearm rotation and throughout the range of elbow motion.
This could lead to disability in this patient population as well as in
the older laborers who extensively use their upper extremity.
Medial joint pain in patients with advanced
osteoarthritis of the elbow might be the first manifestation of ulnar
neuropathy. It is reported that ≤20% of patients with primary
osteoarthritis of the elbow have some degree of ulnar neuropathy. The
proximity of the ulnar nerve to the arthritic posteromedial aspect of
the ulnohumeral joint makes it susceptible to impingement. The
expansion of the capsule as a result of synovitis and the presence of
osteophytes in that area of the joint result in direct compression and
ischemia of the ulnar nerve. Acute onset of
osteoarthritis of the elbow might be the first manifestation of ulnar
neuropathy. It is reported that ≤20% of patients with primary
osteoarthritis of the elbow have some degree of ulnar neuropathy. The
proximity of the ulnar nerve to the arthritic posteromedial aspect of
the ulnohumeral joint makes it susceptible to impingement. The
expansion of the capsule as a result of synovitis and the presence of
osteophytes in that area of the joint result in direct compression and
ischemia of the ulnar nerve. Acute onset of
P.410
cubital
tunnel syndrome in patients with osteoarthritis of the elbow might be
also the first manifestation of medial elbow ganglion.
 |
|
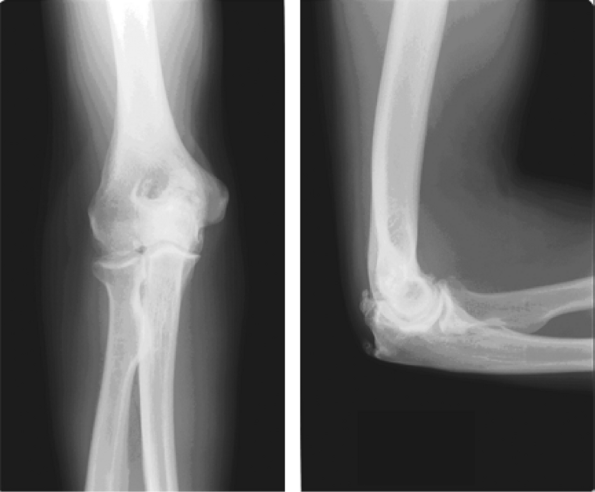
Figure 60-1
A lateral view of the right elbow, showing advanced osteoarthritis specifically involving the radiocapitellar joint. Notice the formation of osteophytes anteriorly and posteriorly. |
Imaging and other Diagnostic Studies
The characteristic radiographic features seen on the
anteroposterior and lateral radiographs of the elbow include
radiocapitellar narrowing, ossification, and osteophyte formation in
the olecranon fossa in almost all patients with osteoarthritis of the
elbow. Loose bodies and fluffy densities might be observed filling the
coronoid and olecranon fossae (Fig. 60-2).
anteroposterior and lateral radiographs of the elbow include
radiocapitellar narrowing, ossification, and osteophyte formation in
the olecranon fossa in almost all patients with osteoarthritis of the
elbow. Loose bodies and fluffy densities might be observed filling the
coronoid and olecranon fossae (Fig. 60-2).
Computer tomography (CT) also helps in delineating the
detailed structural anatomy of the articular surface of the elbow with
an accurate determination of the locations of the osteophytes and loose
bodies. When contemplating surgical treatment of the osteoarthritic
elbow, a CT is quite helpful for determining which osteophytes need to
be removed. Radiographs do not allow for accurate visualization of all
osteophytes.
detailed structural anatomy of the articular surface of the elbow with
an accurate determination of the locations of the osteophytes and loose
bodies. When contemplating surgical treatment of the osteoarthritic
elbow, a CT is quite helpful for determining which osteophytes need to
be removed. Radiographs do not allow for accurate visualization of all
osteophytes.
Nonoperative Management
Because of the young age of the patients with primary
osteoarthritis of the elbow, most of these patients tend to be active
and involved in manual labor work, which will place a great demand on
any kind of prosthetic replacement. All limited operative debridement
options should be exhausted before contemplating elbow replacement in
this group of patients.
osteoarthritis of the elbow, most of these patients tend to be active
and involved in manual labor work, which will place a great demand on
any kind of prosthetic replacement. All limited operative debridement
options should be exhausted before contemplating elbow replacement in
this group of patients.
Early in the course of the disease, treatment by
nonsurgical measures should be followed. This consists of activity
modification, physical therapy, anti-inflammatory medications, and
possibly steroid injection. As in other joints arthritis, if there is
no improvement with these symptomatic measures, operative management is
warranted.
nonsurgical measures should be followed. This consists of activity
modification, physical therapy, anti-inflammatory medications, and
possibly steroid injection. As in other joints arthritis, if there is
no improvement with these symptomatic measures, operative management is
warranted.
Surgical Management
Elbow arthroscopy is a good option for removal of
intra-articular loose bodies and is effective in relieving the
patient’s mechanical symptoms of catching and locking. Elbow
arthroscopy has proved quite effective in removing osteophytes and
releasing tight areas of capsule in the arthritic elbow. Surgeons with
significant experience in elbow arthroscopy can remove all restricted
capsule and reach all areas of the anterior and posterior elbow joint
and areas of impinging osteophytes. To release a similar amount of the
elbow joint with an open approach would require a wide exposure.
intra-articular loose bodies and is effective in relieving the
patient’s mechanical symptoms of catching and locking. Elbow
arthroscopy has proved quite effective in removing osteophytes and
releasing tight areas of capsule in the arthritic elbow. Surgeons with
significant experience in elbow arthroscopy can remove all restricted
capsule and reach all areas of the anterior and posterior elbow joint
and areas of impinging osteophytes. To release a similar amount of the
elbow joint with an open approach would require a wide exposure.
Techniques
Kashiwagi popularized the open elbow decompression
described by Outerbridge, which consisted of decompression of the
ulnohumeral joint with resection of the coronoid and olecranon
osteophytes and fenestration of the distal part of the humerus. A
disadvantage of this technique is the difficulty in exposing and
excising the osteophytes in the radial head fossa.
described by Outerbridge, which consisted of decompression of the
ulnohumeral joint with resection of the coronoid and olecranon
osteophytes and fenestration of the distal part of the humerus. A
disadvantage of this technique is the difficulty in exposing and
excising the osteophytes in the radial head fossa.
Savoie et al. reported good results with extensive
arthroscopic debridement involving capsular release, fenestration of
the distal part of the humerus, and removal of osteophytes. Also,
Morrey reported good results with open ulnohumeral arthroplasty, a
variation of the original technique in which a trephine is used to
remove the osteophytes encroaching on the olecranon and coronoid fossae.
arthroscopic debridement involving capsular release, fenestration of
the distal part of the humerus, and removal of osteophytes. Also,
Morrey reported good results with open ulnohumeral arthroplasty, a
variation of the original technique in which a trephine is used to
remove the osteophytes encroaching on the olecranon and coronoid fossae.
If the above options fail to relieve the patient
symptoms, then total elbow arthroplasty (TEA) may cautiously be
considered as the next alternative of treatment. Most studies in the
literature reporting on total elbow arthroplasty involve large numbers
of patients, mostly with rheumatoid arthritis or other inflammatory
pathologies, but very few patients with primary osteoarthritis. This
makes it difficult to make accurate conclusions on the value of this
treatment option for this population of patients. There are few studies
in the English literature reporting specifically on the
symptoms, then total elbow arthroplasty (TEA) may cautiously be
considered as the next alternative of treatment. Most studies in the
literature reporting on total elbow arthroplasty involve large numbers
of patients, mostly with rheumatoid arthritis or other inflammatory
pathologies, but very few patients with primary osteoarthritis. This
makes it difficult to make accurate conclusions on the value of this
treatment option for this population of patients. There are few studies
in the English literature reporting specifically on the
P.411
outcome and complications of TEA as a treatment option for patients with primary osteoarthritis of the elbow.
 |
|
Figure 60-2
An anterior-posterior and lateral view of a right osteoarthritic elbow showing narrowing of the joint line and subchondral sclerosis, with formation of osteophytes in the coronoid, capitellar, and olecranon fossae. |
Kozak et al. reported on the Mayo clinic experience.
Over a 13-year period, only 5 out of 493 patients (<1%) who
underwent TEA had the procedure performed for primary osteoarthritis of
the elbow. The Coonrad-Morrey prosthesis (Zimmer, Warsaw, IN) cemented
semiconstrained prosthesis was used in three patients, and the
Pritchard elbow-resurfacing system (ERS) (De Puy, Warsaw, IN) cemented
unconstrained prosthesis was used in the other two patients. The
average age of the patients was 67 years, and a follow-up ranged from
37 to 121 months. Two minor and four major complications were reported
in four elbows, two of which required revision. This rate of
complications according to the authors is much higher than the rate of
complication reported in TEA performed for other reasons in the same
institution during the same period of time, including revision TEA,
posttraumatic arthritis, nonunion of distal humerus, and rheumatoid
arthritis.
Over a 13-year period, only 5 out of 493 patients (<1%) who
underwent TEA had the procedure performed for primary osteoarthritis of
the elbow. The Coonrad-Morrey prosthesis (Zimmer, Warsaw, IN) cemented
semiconstrained prosthesis was used in three patients, and the
Pritchard elbow-resurfacing system (ERS) (De Puy, Warsaw, IN) cemented
unconstrained prosthesis was used in the other two patients. The
average age of the patients was 67 years, and a follow-up ranged from
37 to 121 months. Two minor and four major complications were reported
in four elbows, two of which required revision. This rate of
complications according to the authors is much higher than the rate of
complication reported in TEA performed for other reasons in the same
institution during the same period of time, including revision TEA,
posttraumatic arthritis, nonunion of distal humerus, and rheumatoid
arthritis.
Espag et al. reported on 11 Souter-Strathclyde cemented
unlinked primary total elbow arthroplasties in 10 patients with
osteoarthritis of the elbow. The diagnosis was primary osteoarthritis
of the elbow in nine patients and posttraumatic osteoarthritis in two
patients. The average age of the patients was 66 years, with a mean
follow-up of 68 months. Only one patient required revision after 97
months for ulnar component loosening. All patients reported good
symptomatic relief of pain and a significant increase in range of
motion, and all patients considered the procedure to be successful.
unlinked primary total elbow arthroplasties in 10 patients with
osteoarthritis of the elbow. The diagnosis was primary osteoarthritis
of the elbow in nine patients and posttraumatic osteoarthritis in two
patients. The average age of the patients was 66 years, with a mean
follow-up of 68 months. Only one patient required revision after 97
months for ulnar component loosening. All patients reported good
symptomatic relief of pain and a significant increase in range of
motion, and all patients considered the procedure to be successful.
The authors compared these results with the result of
Souter-Strathclyde total elbow arthroplasty used in patients with
rheumatoid arthritis. The revision rate in their series (9%) performed
for ulnar component loosening compares favorably with the revision rate
with the rheumatoid patients (5% to 21%), in which the main indications
for revision included dislocation and perioperative fracture. The
authors attributed the decrease in the incidence of perioperative and
postoperative fracture to the good amount of bone stock in patients
with primary osteoarthritis of the elbow that makes the risk of
fracture very minimal.
Souter-Strathclyde total elbow arthroplasty used in patients with
rheumatoid arthritis. The revision rate in their series (9%) performed
for ulnar component loosening compares favorably with the revision rate
with the rheumatoid patients (5% to 21%), in which the main indications
for revision included dislocation and perioperative fracture. The
authors attributed the decrease in the incidence of perioperative and
postoperative fracture to the good amount of bone stock in patients
with primary osteoarthritis of the elbow that makes the risk of
fracture very minimal.
As evident from this review, the outcome studies of TEA
in patients with primary osteoarthritis of the elbow are very limited.
The above-mentioned studies included small numbers of patients, and no
final recommendation could be drawn at this time.
in patients with primary osteoarthritis of the elbow are very limited.
The above-mentioned studies included small numbers of patients, and no
final recommendation could be drawn at this time.
P.412
It is hoped that a greater understanding of elbow
anatomy and kinematics will lead to advances in prosthetic design and
surgical technique. The newer anatomic unlinked implants may improve
the outcome of elbow replacement in younger patients. More outcome
studies are needed on these implants or any other modern implants
before openly recommending elbow replacement in younger active patients
with primary osteoarthritis of the elbow.
anatomy and kinematics will lead to advances in prosthetic design and
surgical technique. The newer anatomic unlinked implants may improve
the outcome of elbow replacement in younger patients. More outcome
studies are needed on these implants or any other modern implants
before openly recommending elbow replacement in younger active patients
with primary osteoarthritis of the elbow.
Suggested Readings
Antuna
SA, Morrey BF, Adams RA, et al. Ulnohumeral arthroplasty for primary
degenerative arthritis of the elbow: long-term outcome and
complications. J Bone Joint Surg. 2002;84A:2168–2173.
SA, Morrey BF, Adams RA, et al. Ulnohumeral arthroplasty for primary
degenerative arthritis of the elbow: long-term outcome and
complications. J Bone Joint Surg. 2002;84A:2168–2173.
Bullough PG. Atlas of Orthopedic Pathology. 2nd ed. New York: Gower Medical Publishing; 1992;10:4–10.
Doherty M, Preston B. Primary osteoarthritis of the elbow. Ann Rheum Dis. 1989;48:743–747.
Espag
MP, Black DL, Clark DI, et al. Early results of the Souter-Strathclyde
unlinked total elbow arthroplasty in patients with osteoarthritis. J Bone Joint Surg. 2003;85B:351–353.
MP, Black DL, Clark DI, et al. Early results of the Souter-Strathclyde
unlinked total elbow arthroplasty in patients with osteoarthritis. J Bone Joint Surg. 2003;85B:351–353.
Ewald FC. Total elbow replacement. Orthop Clin North Am. 1975;3:685–696.
Goodfellow JW, Bullough PG. The pattern of aging of the articular cartilage of the elbow joint. J Bone Joint Surg. 1967;49B:175–181.
Gramstad GD, King GJ, O’Driscoll SW, et al. Elbow arthroplasty using a convertible implant. Tech Hand Up Extrem Surg. 2005;9(3): 153–163.
Kashiwagi D. Intra-articular changes of the osteoarthritis of the elbow. Orthop Clin North Am. 1995;26:691–706.
Kashiwagi
D. Osteoarthritis of the elbow joint: intra-articular changes and the
special operative procedure, Outerbridge-Kashiwagi method (O-K method).
In: Kashiwagi D, ed. Elbow Joint. Amsterdam: Elsevier Science; 1985:177–188.
D. Osteoarthritis of the elbow joint: intra-articular changes and the
special operative procedure, Outerbridge-Kashiwagi method (O-K method).
In: Kashiwagi D, ed. Elbow Joint. Amsterdam: Elsevier Science; 1985:177–188.
Kato
H, Hirayama T, Minami A, et al. Cubital tunnel syndrome associated with
medial elbow ganglia and osteoarthritis of the elbow. J Bone Joint Surg. 2002;84A:1413–1419.
H, Hirayama T, Minami A, et al. Cubital tunnel syndrome associated with
medial elbow ganglia and osteoarthritis of the elbow. J Bone Joint Surg. 2002;84A:1413–1419.
Kellgren JH, Lawrence JS. Radiological assessment of osteoarthrosis. Ann Rheum Dis. 1957;16:494–501.
King GJW, Adams RA, Morrey BF. Total elbow arthroplasty: revision with use of a non-custom semiconstrained prosthesis. J Bone Joint Surg. 1997;79A:394–398.
Kozak TK, Adams RA, Morrey BF. Total elbow arthroplasty in primary osteoarthritis of the elbow. J Arthroplasty. 1998;13:837-842.
Kraay MJ, Figgie MP, Inglis AE, et al. Primary semiconstrained total elbow arthroplasty. J Bone Joint Surg. 1994:76B:636–640.
London JT. Kinematics of the elbow. J Bone Joint Surg. 1981;63A: 529–535.
Meachim G. Age changes in articular cartilage. Clin Orthop. 1969;64:33–44.
Mintz G, Fraga A. Severe osteoarthritis of the elbow in foundry workers. Arch Environ Health. 1973;27:78–80.
Morrey BF, Adams RA, Bryan RS. Total replacement for post-traumatic arthritis of the elbow. J Bone Joint Surg. 1991;73B:607–612.
Morrey BF, Adams RA. Semiconstrained elbow replacement arthroplasty for distal humeral non-union. J Bone Joint Surg. 1995;77B:67–72.
Morrey BF, Bryan RS, Dobyns JH, et al. Total elbow arthroplasty. J Bone Joint Surg. 1981;81A:80–84.
Morrey BF. Primary degenerative arthritis of the elbow. J Bone Joint Surg. 1992;74B:409–413.
O’Driscoll SW. Arthroscopic treatment for osteoarthritis of the elbow. Orthop Clin North Am. 1995;26:691–706.
O’Driscoll SW. Elbow arthritis: treatment options. J Am Acad Orthop Surg. 1993;1:106–116.
Ogilvie-Harris DJ, Schemitsch E. Arthroscopy of the elbow for removal of loose bodies. Arthroscopy. 1993;9:5–8.
Oka Y. Debridement for osteoarthritis of the elbow in athletes. Int Orthop. 1999;23:91–94.
Ortner DJ. Description and classification of degenerative bone changes in the distal joint surfaces of the humerus. Am J Phys Anthop. 1968;28:139–155.
Rozing P. Souter-Strathclyde total elbow arthroplasty. J Bone Joint Surg. 2000;82B:1129–1134.
Savoie FH 3rd, Nunley PD, Field LD. Arthroscopic management of the arthritic elbow: indications, technique, and results. J Shoulder Elbow Surg. 1999;8:214–219.
Stanley D. Prevalence and etiology of symptomatic elbow osteoarthritis. J Shoulder Elbow Surg. 1994;3:386–389.
Trail
IA, Nuttal D, Stanley JK. Survivorship and radiological analysis of the
standard Souter-Strathclyde total elbow arthroplasty. J Bone Joint Surg. 1999;81B:80–84.
IA, Nuttal D, Stanley JK. Survivorship and radiological analysis of the
standard Souter-Strathclyde total elbow arthroplasty. J Bone Joint Surg. 1999;81B:80–84.
Tsuge
K, Mizuseki T. Debridement arthroplasty for advanced primary
osteoarthritis of the elbow. Results of a new technique used for 29
elbows. J Bone Joint Surg. 1994;76B:641–646.
K, Mizuseki T. Debridement arthroplasty for advanced primary
osteoarthritis of the elbow. Results of a new technique used for 29
elbows. J Bone Joint Surg. 1994;76B:641–646.
Wadworth TG. Osteoarthritis. In Wadworth TG, ed. The Elbow. Edinburgh: Churchill Livingstone; 1982;292–293.
