Polytrauma
injuries is often complex. Fractures that are complicated by truncal,
burn, or head injuries may be especially challenging. These children
may be in extremis or very unstable at the
time of presentation and thus may be poor candidates for anesthesia.
Nonorthopaedic injuries may take precedence and orthopaedic procedures
postponed. However, because of the unique problems that occur in these
patients both immediately after the injury and in the long term,
operative stabilization of fractures often can provide great benefits.
The sickest patients may benefit the most from surgery; however, unlike
adults, children do not derive any significant protection from
pulmonary complications as a result of long bone fracture stabilization.
of disability in children. Only acute infection causes more morbidity
than trauma. The estimated annual cost of pediatric injury is greater
than 7.5 billion dollars, with estimates of loss of future productivity
at greater than 8 billion dollars.
although the incidence of penetrating injury is rising. Motor vehicle
accidents, pedestrian injuries, recreational vehicle injuries, major
falls, and physical abuse are common causes.
swelling and fluid accumulation, including the cycle of hypoperfusion
and reperfusion, direct contusion, fluid and electrolyte imbalances,
and sepsis. Increased interstitial fluid makes access to and evaluation
of internal structures difficult. Surgery and wound closure are
difficult in swollen tissues. Organ function is diminished by fluid
accumulation and swelling, especially in the brain and lung. It often
takes several days to resorb excess interstitial fluid after resolution
of hemodynamic, metabolic, and septic derangements.
morbidity and mortality. This is worsened when there is polytrauma.
Increased intracranial pressure is always a source of concern and
usually requires intracranial pressure monitoring. Increased pressure
may prevent or delay surgical repair of other internal or skeletal
injuries. The brain injury itself may cause abnormal posturing,
increased muscle tone, or agitated movements—all of which can make
fracture management difficult. Injury-induced or medically induced coma
will render the child immobile and require constant vigilance for
contractures and bedsores. The search for additional injuries is more
difficult in the child who is unresponsive. Special care must be taken
to look for associated injuries which could otherwise be missed.
imbalances, and multiple transfusions may all have an effect on fluid
accumulation in the lung parenchyma that results in decreased
oxygenation of the blood. Intubation and sedation are usually required.
Hypoxemia will prevent prompt orthopaedic surgery. It may take several
days for pulmonary problems to resolve.
within the first several days of injury. Frequently the lungs are the
source of infection. Sepsis may contribute to multiple organ failure.
It may require the use of multiple antibiotics—some with side effects.
It complicates fluid and electrolyte management and provides an
undesirable setting for the placement of internal orthopaedic implants.
over that of orthopaedic injury. Unless simultaneous orthopaedic and
general surgery is possible (and it rarely is), the orthopaedic
procedures must follow treatment of the internal injuries.
transfusion of blood products, multiple injuries often do. Multiple
transfusions will often be associated with interstitial fluid
accumulation, impaired blood clotting, and decreased systemic immunity.
interrupted after severe trauma. Mobilized stores of nutrients will
sustain the child for a few days. After that, alimentation must be
provided either enterally or intravenously to provide substrates for
healing and repair.
care unit setting. Intensivists tend to make the important treatment
decisions and often the orthopaedist must receive permission before
initiating treatment for skeletal injuries. The orthopaedist is often
not familiar with intensive care techniques and procedures. Likewise,
intensivists and intensive care nurses are frequently unfamiliar with
orthopaedic devices and casts. Parents are often distraught or
restless. Patient and diligent communication must be maintained between
medical professionals and with parents.
Treatment decision must not be based on injury scale. Unless the child
is clearly going to die, orthopaedic treatment must proceed as if the
child is going to survive.
-
Deformity: splints and clothing must be removed to really see deformity.
-
Bleeding: watch for poke holes over fracture sites.
-
Swelling and ecchymosis: key to underlying injury but take some time to develop.
-
Tenderness: pain on palpation is always key. Even unconscious patient may manifest a useful response.
-
Abnormal motion: movement in the middle of a long bone or out of the plane of joint motion indicates radiography is necessary.
-
Crepitus: common after displaced fracture and reminds examiner that a splint will be necessary.
-
Pulses: important to document but not as important as perfusion status.
-
Neurologic function: important to note
before treatment is instituted. If a good neurologic examination isn’t
possible, write a note that explains why and remember to come back
later and keep trying.
|
TABLE 13-1 MODIFIED INJURY SEVERITY SCALE FOR CHILDREN WITH MULTIPLE INJURIES
|
||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||
-
Chest, cervical spine, and pelvis films should be ordered automatically.
-
Spine and extremity films should be requested based on clinical evaluation.
-
Computed tomography (CT) scanning of spine or pelvis is indicated by suspicious radiographic or clinical evaluation.
-
In suspected abuse cases, a skeletal
survey is medicolegally indicated. Multiple fractures in various stages
of healing and metaphyseal corner fractures are highly suggestive of
abuse. Spiral fractures are not. -
Technetium bone scanning will be helpful
to locate skeletal injuries in victims who are very young or unable to
manifest a pain response because of central nervous system injury. -
Magnetic resonance imaging to evaluate joint derangement is not a priority in the acute injury phase.
-
The history is always important and leads the examiner to suspected areas of injury.
-
It is useful to know what the emergency transport team perceived to be injured at the scene.
-
Obviously life-threatening conditions take priority over orthopaedic injuries.
-
Splinted limbs should be rechecked with the splint removed if possible.
-
Obvious deformities should be noted. Open wounds must be noted.
-
Assume spinal injury until proved otherwise.
-
An inconsistent or changing history may suggest nonaccidental trauma. Be on the lookout.
-
Get plain radiographs of suspicious areas.
-
Ensure limb perfusion. If a problem, get help from the surgeons.
-
Provisional splintage decreases pain and limits further soft tissue injury.
-
Obtain special studies—CT scans, arteriograms, and so forth.
-
Think about and look for compartment syndrome, especially in patients unable to feel or speak.
-
Wash out open injuries as soon as it is safe for the patient.
-
Make plans to fix each fracture that would require surgery as if it were an isolated injury as soon as possible.
-
Consider stabilizing major bone fractures (i.e., femur, humerus, pelvis) to facilitate patient care.
-
Work hard to stabilize fractures within
limbs that will require frequent or painful manipulation, like those
with traumatic wounds, skin loss, burns, or compartment syndromes.
|
TABLE 13-2 GLASGOW COMA SCALE
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
-
Treatment of the uncomplicated femur fracture in young children often includes the use of traction or a spica cast.
-
□ Polytraumatized children often need to be turned, transported, and scanned—all of which are made difficult by traction.
-
□ Spica casts limit access to the limbs and abdomen.
-
-
Stabilization of long bone fractures enables transport and leaves the limbs and trunk free for examination or treatment.
-
Stabilization of long bone fractures
eliminates further damage to soft tissue by underlying mobile bone
segments and may limit further bleeding.P.174-
□ This is especially important in patients with head-injuries, who may be agitated or become spastic.
-
-
Patients with traumatic wounds, burns, or
compartment syndrome of limbs will likely need regular and repeated
access to the extremities.-
□ Circumferential casts make this difficult.
-
□ Without support, the fractured limb is painful and repeated manipulations for dressing changes would be cruel.
-
□ Stabilization of the skeleton makes wound management much easier.
-
-
Bony spinal injuries may render the spine unstable and render the neurologic structures at risk.
-
□ Surgical stabilization lessens pain with movement and protects the neural elements from unstable segments.
-
-
Simple closed fractures distal to the elbow or knee should be managed with reduction and splintage or casting.
-
Open fractures need surgical irrigation and drainage.
-
□ Stable fractures can be splinted or casted.
-
□ Unstable fractures or those that require frequent wound care will benefit from surgical stabilization.
-
-
Fractures of the femoral shaft should be
stabilized in multiply-injured children older than 6 years for the same
reasons as they are in children with fracture only. -
Surgical stabilization should be
considered for shaft fracture of the femur in polytraumatized children
of any age for the following reasons:-
□ Facilitate transport (i.e., in and out of scanners)
-
□ Facilitate hygiene
-
□ Facilitate wound, burn, or skin care
-
□ Facilitate rehabilitation
-
□ Obtain or maintain reasonable bony alignment which cannot be done by closed means
-
□ Control alignment and limit shortening
and further soft tissue injury in patients with head injuries who are
spastic or agitated -
□ Aid in pain control
-
-
Fractures of the pelvis should be
stabilized if there is gross displacement, gross instability, or
expanding hematoma that does not stabilize with transfusion. -
Fractures of humeral shaft do not
generally require surgical fixation, but in general the threshold for
surgical fixation can be lowered in the polytrauma setting. -
Reasons to consider surgical fixation include the following:
-
□ Inability to maintain alignment with usual splintage in a recumbent position
-
□ Difficulty with access to venous or arterial circulation due to splintage of upper arm
-
□ Multiple injuries in the same limb
-
□ Skin or wound problems of chest or upper arm
-
□ Agitation or spasticity in the patient with head injury
-
□ Proximate nerve or vascular injury
-
-
Periarticular fractures that would be managed by surgery in otherwise normal patients should be managed by surgery.
-
□ Postponing surgery because the child has a head injury or truncal injury often leads to problems or a compromised result.
-
□ The following scenario must be avoided:
The child is believed to be too sick to fix an orthopaedic injury and
is likely to die. The child recovers, and the untreated orthopaedic
injury becomes a major problem and a difficult reconstruction.
-
-
Fractures under burns can be safely fixed up to 48 hours after injury.
-
□ Incision through or around burned skin is relatively safe.
-
□ After that, the skin must be considered
to be colonized with bacteria and open reduction with internal fixation
will be prone to infection. -
□ Minimal or external fixation should be considered.
-
□ Otherwise, fixation should be delayed until skin healing or grafting.
-
 |
|
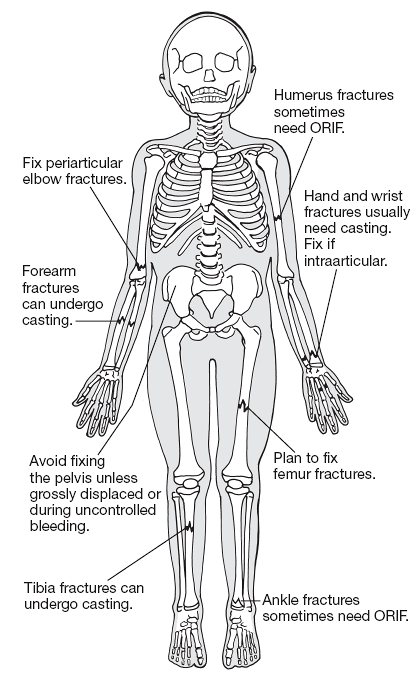
Figure 13-1
Periarticular fractures should be fixed just as indicated in isolated injuries. Fractures distal to knee and elbow can generally be managed in a cast. The threshold should be lowered for fixing the pelvis, humerus, and femur in the polytrauma patient. ORIF, open reduction and internal fixation. |
-
Intramedullary fixation is ideal for closed fractures of long bones (see sections on individual bone injuries).
-
In patients unable to tolerate extreme
positioning or vigorous pushing and pulling, external fixation and
plating may be good solutions. -
External fixation is almost always the
quickest and easiest solution for long bone fracture but commits the
patient to daily pin care. -
Try to avoid operating on the pelvis.
-
□ Use an anterior external fixator if simple stabilization is needed.
-
□ Be prepared to place anterior plates and posterior sacroiliac screws for the unstable pelvis in older children.
-
-
Periarticular fixation should be performed as in patients with isolated injury.
-
Do not harm the patient. Unresponsive shock and severely elevated intracranial pressure are reasons to delay fracture treatment.
-
Try to minimize blood loss and operative time in the sick patient.
-
Try to achieve stability that obviates the need for cast or splintage, especially proximal to the elbow or knee.
-
Goals for stabilization:
-
□ Pain control
-
□ Patient portability
-
□ Free access to trunk and circulation
-
□ Fracture alignment
-
□ Easy access to skin, burns, and traumatic wounds
-
-
Infection is always a possibility in the trauma patient.
-
The possibility of infection should not be a deterrent to skeletal stabilization, but active systemic sepsis should be.
-
Treat wound infection in the trauma patient just as in any other patient.
-
Unlike patients with isolated injuries, polytrauma patients are often manipulated by others who cannot feel the pain.
-
Skeletal fixation should be strong enough to protect against the manipulations of caretakers.
-
Head-injured or previously spastic patients may thrash about or have intense muscle spasms that can overcome weak fixation.
-
Be prepared to use strong fixation devices in these patients.
-
Prevention is easier than treatment.
-
Equinus contracture is ubiquitous in bedridden patients.
-
Ankle-foot orthoses and daily manipulation are helpful.
-
Flexion contractures of elbows, knees, and hips are not uncommon.
-
Daily physical therapy and varied positioning are helpful.
-
Warn the parents about the possibility of missed injury in the obtunded patient.
-
Check the patient at each visitation by palpating and tying to elicit tenderness.
-
Have a low threshold for obtaining radiographs.
-
Not uncommon in the polytrauma patient, especially if there is head injury.
-
Preventive treatment is not indicated.
-
Symptomatic residuals of heterotopic ossification can be treated after the patient is stabilized.
-
Positioning patients to maximize pulmonary care and social interaction is important.
-
Mobilization of joints through active
movement—in those who can—and passive movement—in those who cannot—is
important to maintain function. -
Children who will need their upper limbs
to provide mobility with either crutches or wheelchair after the acute
phase of trauma should begin working on strength as soon as possible in
the hospital. -
Weightbearing should be encouraged as soon as callus is seen unless there are other mitigating factors.
-
For larger children who are unable to transfer, consider the home use of a hospital bed, lift, and bedside commode.
-
Let the lawyer know that it may be years before the permanent residuals of injury can be fully realized in the growing child.
-
Survey and resurvey for injuries. Missed
injuries in the polytrauma setting are an embarrassment for the
physician and may be a cause for medicolegal action. Warn the parents
of the obtunded child that some injuries are hard to find and may not
be apparent at first. -
Fat embolism syndrome does occur in
children and adolescents. Watch for mental status changes with
tachycardia and decrease in arterial oxygenation after long bone
fracture. -
Rib fractures are a danger sign. They
generally occur in two clinical settings: high-energy trauma and abuse.
Look for associated injuries. -
Always assume the child is going to recover.
-
Try to operate before the child gets
sick. Problems with fluid retention, sepsis, respiratory failure, and
skin contamination with hospital flora are likely to worsen in the
first few days after injury. -
Warn parents that recovery may not be
full. Take the time to explain enough pathophysiology so that parents
do not confuse neurologic residuals with bad fracture treatment. -
Don’t lose track of the patient.
Polytrauma patients often are transferred to rehabilitation units after
the acute phase of treatment. It is important that they are followed
for their fractures by an orthopaedic surgeon.
AB, Hunt JL, Purdue GF, et al. Early orthopaedic intervention in burn
patients with major fractures. J Trauma 1991;31:888-893.
D, Starr AJ, Wilson P, et al. Early versus delayed stabilization of
pediatric femur fractures: analysis of 387 patients. J Orthop Trauma
1999;13:490-493.
SD, Gallagher D, Harris M, et al. Undiagnosed fractures in severely
injured children and young adults: identification with technetium
imaging. J Bone Joint Surg (Am) 1994;76:561-572.
RT, Gullahorn LJ, Yian EH, et al. Factors predictive of immobilization
complications in pediatric polytrauma. J Orthop Trauma 2001;15:338-341.
SA, Dominick T, Tyler-Kabara E, et al. Early versus late femoral
fracture stabilization in multiply injured pediatric patients with
closed head injury. J Pediatr Orthop 2001;21:594-599.
S, Milgrom C, Nyska M, et al. Femoral fracture treatment in
head-injured children: use of external fixation. J Trauma 1986;26:81-84.
VT. Orthopaedic treatment of fractures of the long bones and pelvis in
children who have multiple injuries. J Bone Joint Surg (Am)
2000;82:272-282.
