Fractures and Dislocations
authors and do not reflect the official policy or position of the
Department of the Navy, Department of Defense, or the United States
Government.
of all spinal cord and vertebral column injuries affect those 16 years
and under. Although uncommon, spine fractures in children can lead to
chronic instability, deformity, neurologic sequelae, and posttraumatic
stenosis. Injuries to the spinal column can often be subtle and absent
on initial radiographs. Successful treatment is based on knowledge of
the radiographic, anatomic, and developmental differences between the
pediatric and adult spine.
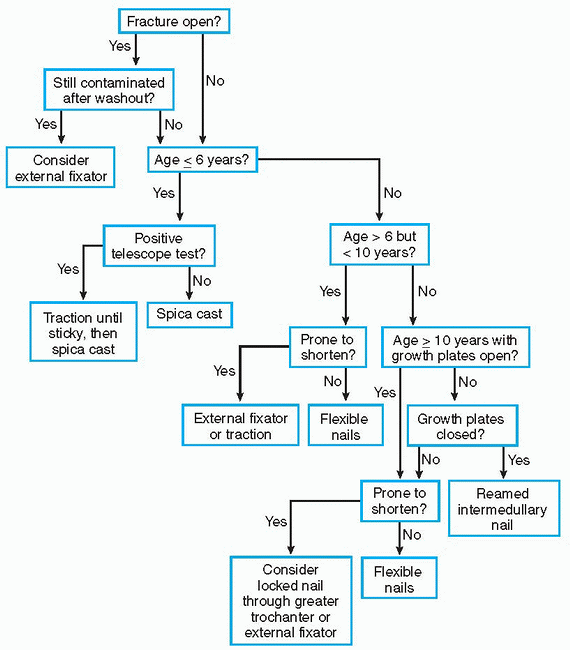
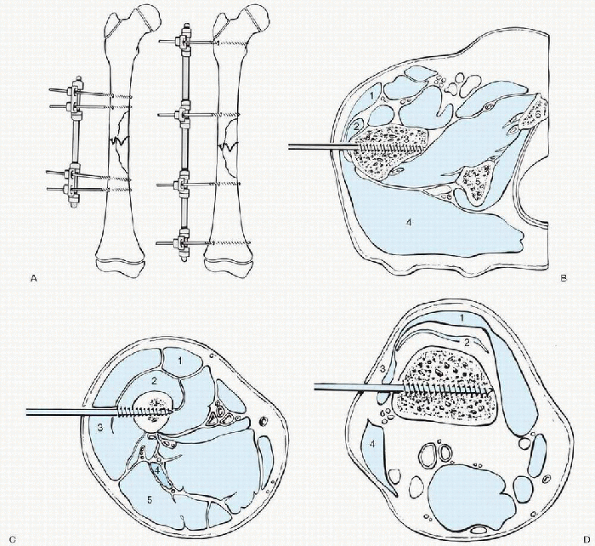
fracture are primarily dependent on the age at the time of injury.
Birth trauma is the major cause of spinal trauma in children under age
2. In patients between the ages of 3 and 8 the most frequent mechanisms
of injury are falls from height, motor vehicle accidents, and child
abuse. Children older than 8 years of age are more commonly injured in
motor vehicle accidents, by gunshot wounds, or from sporting activities
such as swimming, diving, and surfing.
The majority of spinal column fractures in childhood occur in the
thoracolumbar spine. Cervical spine fractures in patients 8 years old
or younger involve the upper cervical spine above C4. These most often
include the occiput, C1, C2 complex and carry an increased risk of
fatality. Patients older than 8 more typically sustain injures below C4
with a much lower fatality rate. Up to 30% of traumatic spine injuries
in children present as a traumatic myelopathy known as spinal cord
injury without radiographic abnormality (SCIWORA).
immature spine is necessary to accurately diagnose spinal trauma.
Several developmental features can be misconstrued as evidence of
injury to the spine (Table 12.1-1).
and facet capsules strengthen, the facets become more vertically
oriented and the vertebral bodies become more rectangular-shaped. By
late childhood the patterns of spinal injuries and healing become
similar to the adult.
anatomy, it is important to be aware of congenital and genetic
conditions manifested in the spine (Table 12.1-2).
-
Large head-to-body ratio
-
Ligamentous laxity
-
Relative muscle weakness
-
Horizontal, shallow facet joints
-
Increased spinal column elasticity
-
Forces dissipated over several adjacent segments
-
SCIWORA possible
-
-
Presence of the ring apophysis
-
Fractures traverse vertebral body growth plate
-
|
TABLE 12.1-1 DEVELOPMENTAL FEATURES THAT CAN BE MISINTERPRETED AS INJURY
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
TABLE 12.1-2 SELECTED CONGENITAL VERTEBRAL ANOMALIES
|
|||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||
 |
|
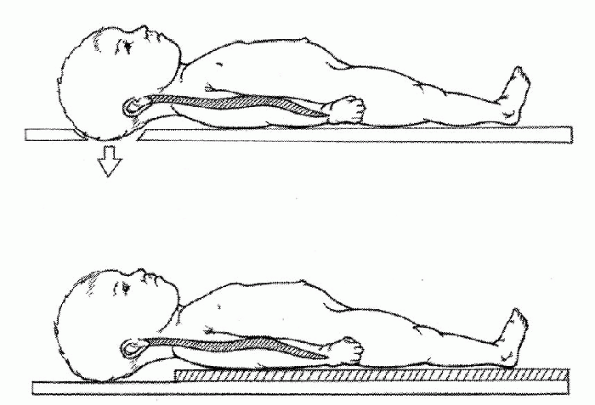
Figure 12.1-1 Diagrams of young children on modified spine boards with either an occipital recess (top figure) or a mattress pad (bottom figure)
to raise the chest. (©1998 American Academy of Orthopaedic Surgeons. Adapted from the Journal of the American Academy of Orthopaedic Surgeons, 1988;6[4]:204-214, with permission.) |
event, potentially life-threatening conditions must be identified and
treated. Once airway, breathing, and circulation are secure, a brief
secondary survey can be accomplished. Early proper immobilization in
all patients with suspected C-spine injury is essential in order to
avoid creating or propagating further spinal cord injury, by increased
neck flexion. In a young child with a proportionally large head, this
can be done using a spine board with an occipital recess or by placing
a mattress or blankets beneath the shoulders and trunk of the child (Fig. 12.1-1).
A screening cross-table lateral x-ray of the spine, in addition to
anteroposterior (AP) pelvis and chest x-rays, should be standard in the
evaluation of all trauma patients.
rigid cervical orthosis, properly designed for infants or children,
should be applied. Sandbags on each side of the head will prevent
motion. Until the cervical spine is cleared (Box 12.1-2), movement of the patient should only be performed with in-line traction using a log-roll technique.
-
Loss of consciousness or GCS <13
-
Neurologic symptoms or complaints
-
Altered mental status
-
Mechanism of injury
-
Motor vehicle vs. pedestrian or cyclist
-
Fall from considerable height
-
Motor vehicle accident as unrestrained passenger
-
Neck pain or guarding
-
Head or facial trauma
-
Ecchymosis from seat belt
-
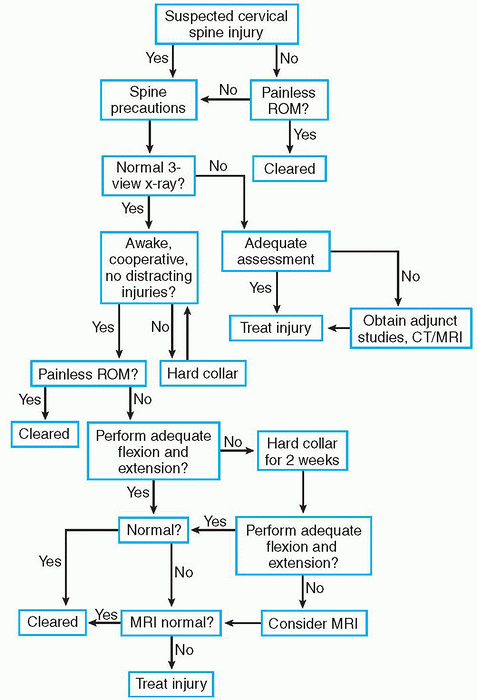
helpful. A spinal cord injury should be suspected in a patient with a
history of numbness, tingling, or brief paralysis. Physical examination
should begin with inspection of skin for any visible evidence of spinal
trauma to include abrasions, edema, or ecchymosis. Pain or step-off
along the spinous processes should also raise suspicion. Range of
motion should only be attempted when the child is conscious and
cooperative and an unstable injury is not suspected.
The cervical orthosis and spine board precautions should be removed
only if the patient has no neck pain or tenderness to palpation and a
full painless range of motion.
 |
|
Algorithm 12.1-1 Clearing the cervical spine.
|
-
Diverting pain from other injuries
-
Altered sensorium
-
Head injury
-
Narcotic pain medication
-
Alcohol use
-
-
Recreational drug use
-
Lateral C-spine radiograph
-
□ Must see top of T1
-
-
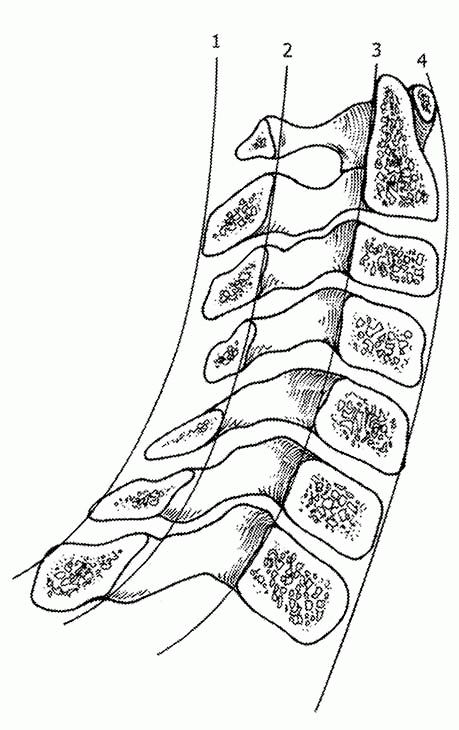
Assess alignment (Fig. 12.1-2)
-
□ Anterior vertebral line
-
□ Posterior vertebral line
-
□ Spinolaminar line
-
□ Spinous process line
-
-
Check radiographic relationships (Table 12.1-3)
-
□ Atlanto-dens interval
-
□ Retropharyngeal and retrotracheal spaces
-
□ Space available for the cord
-
-
AP and open mouth odontoid views
-
□ Alignment of lateral masses
-
□ Odontoid fracture
-
□ Interpedicular distance
-
-
Flexion-extension views
-
□ Assess ligamentous stability
-
□ Active range of motion only
-
□ Physician-supervised
-
□ Fully cooperative patient
-
□ May need to wait until first follow-up visit
-
 |
|
Figure 12.1-2 Normal alignment of the lateral cervical spine. 1, spinous process line; 2, spinolaminar line; 3, posterior vertebral bodyline; 4,
anterior vertebral bodyline. Space available for the cord is the distance between 2 and 3 at the level of C1. (©1998 American Academy of Orthopaedic Surgeons. Adapted from the Journal of the American Academy of Orthopaedic Surgeons, 1998;6:204-214, with permission.) |
|
TABLE 12.1-3 NORMAL PARAMETERS OF THE PEDIATRIC CERVICAL SPINE
|
||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||
-
Compression
-
Lumbar apophyseal injury
-
C2 on C3 or C3 on C4
-
Seen in up to 40% of children between 1 and 7 years of age
-
Up to 4 mm of stepoff in flexion on AP is acceptable
-
Spinolaminar line within 1.5 mm of posterior arch of C1 (Fig. 12.1-2)
-
Should reduce in extension
-
No treatment necessary
-
Seen in midcervical area
-
Seen in up to 14% of children younger than 16 years of age
-
Should reduce in extension
-
Seen in extension
-
20% of those between 1 and 7 years of age
-
Result of nonossified atlas and tip of odontoid
-
Also anterior angulation of odontoid process in as many as 4%
-
Can mimic odontoid fracture
-
Sometimes present until 11 years of age
-
Appears sclerotic unlike true fracture
-
Located well caudad to the base of the odontoid process
-
Flexion with compression
-
Distraction
-
Shear
-
Center plain films over injured area.
-
Obtain “cone down” views of suspicious findings.
-
Always obtain two views 90 degrees apart.
-
Oblique views helpful for spondylolysis in lumbosacral spine.
-
Computed tomography (CT) scan best for evaluating bone “architecture”
-
□ Especially lumbar apophyseal fractures
-
-
Three-dimensional CT often useful in preoperative planning
-
Bone scan useful to detect occult tumors/spondylolysis
-
Magnetic resonance imaging (MRI) very useful in SCIWORA
-
MRI useful in neurocompression by fracture fragments and disc
-
Very unstable
-
Require halo immobilization if neurologically intact (Box. 12.1-5)
-
Fusion if instability remains or neurologic deficit
-
Occiput-C1 fusion if neurologically intact
-
Occiput-C2 fusion if neurologically impaired
-
Halo immobilization or Minerva brace
-
Up to 6 months of immobilization may be necessary
-
Surgical intervention rarely indicated
-
Rotatory subluxation can be treated with temporary immobilization
-
Rarely will require traction for reduction (older than 1 week)
-
Dislocation or ligamentous instability less predictable
-
Initial treatment with Halo immobilization for 8 to 12 weeks
-
C1-C2 fusion if instability persistent
-
Most heal with closed reduction
-
Halo vest or Minerva cast for 4 months
-
Posterior C1-C2 fusion if persistent motion or suspected os odontoideum
-
Most respond to closed reduction and halo vest for 8 weeks
-
Posterior C1-C3 fusion indicated for non-union or significant disc disruption
-
Younger than 8 years, closed reduction and halo vest immobilization
-
Older than 8 years, usually require posterior fusion
-
Younger than 8 years, closed reduction and halo vest immobilization
-
Initial trial of Halo immobilization for 3 months for ligamentous instability
-
Posterior fusion if instability persists beyond 3 months
-
Early surgical stabilization for unstable fractures or spinal cord injury
-
Contact child protective services
-
Obtain skeletal survey
-
Rule out associated injuries
-
□ Retinal hemorrhages
-
□ Intracranial or intraocular hemorrhages
-
□ Visceral injury
-
-
Treat spine injury as indicated
-
Efficacy of steroids in enhancing recovery not established in children
-
Rarely, decompression of spinal cord impingement required
-
□ Retropulsed disc, bone fragments
-
-
Monitor for late spinal deformity
-
□ Nearly universal if children are 10 years of age or younger at time of injury
-
-
Recognize late neurologic deterioration
-
□ Ascending spinal level
-
□ Assess for posttraumatic syrinx with MRI
-
□ Drainage usually required
-
-
-
Immobilization in a rigid cervical collar or Thoracolumbar spinal orthosis (TLSO)
-
Physical activity restriction for 3 months
-
Decompression for progressive deficit, discrete lesion
-
Prognosis for neurologic recovery
-
□ Good in mild cases
-
□ Poor in severe cases
-
□ Usually affects children less than 8 years
-
|
TABLE 12.1-4 CLINICAL AND RADIOLOGIC FEATURES OF SPECIFIC SPINE CONDITIONS OR FRACTURES
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
TABLE 12.1-5 MAGNETIC RESONANCE IMAGING PATTERNS ON T2-WEIGHTED IMAGES OF ACUTE SPINAL CORD INJURIES
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||
|
TABLE 12.1-6 RADIOGRAPHIC CLASSIFICATION OF LUMBAR APOPHYSEAL INJURY
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||
-
Closed reduction, hyperextension casting for pure bony injuries
-
□ Restore lordosis
-
-
Open reduction, posterior fusion for ligamentous injury
-
□ Spinous process wiring with casting for small children
-
□ Compression instrumentation in adolescents
-
-
Surgical excision of retropulsed disc, end-plate and bone fragments
-
□ Prevents healing of lesion to posterior vertebral body
-
□ Avoids subsequent spinal stenosis
-
pediatric spinal trauma can be treated nonoperatively; however, three
primary factors need to be considered in determining if operative
intervention is required.
-
Obtain CT to assess skull thickness in children less than 6 years of age.
-
The ring should sit below the widest skull diameter, about 1 cm above the top of the ear.
-
A 1-cm separation between the halo ring and patient’s head should be present.
-
Use 6 to 8 pins at low insertion torque (2 to 5 ft/lb).
-
Avoid thin bone at temporal region and frontal sinuses
-
Safe zone anteriorly: 1 cm above orbital rim, lateral two thirds of the orbit
-
-
Insert anterior pins with patient’s eyes closed to avoid trapping eyelids open.
-
Tighten opposing pins simultaneously to minimize shifting of the ring.
-
Pins can be retightened once and only if resistance is felt.
-
Remove loose pins after placing a new pin in an adjacent location.
 |
|
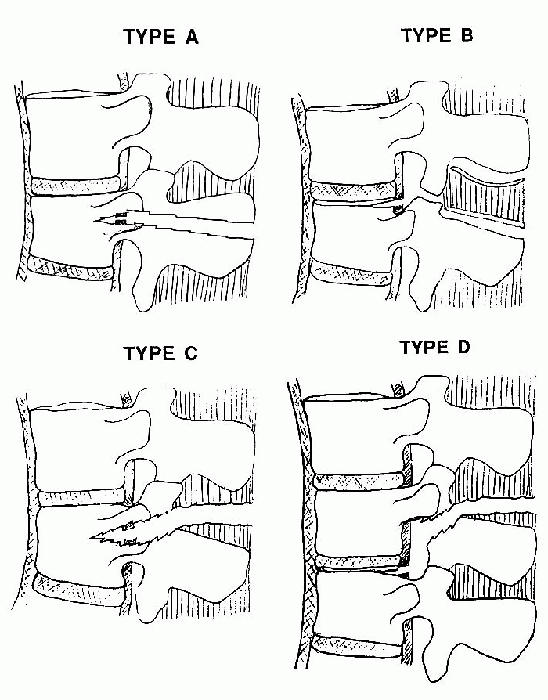
Figure 12.1-3
Pediatric Chance fractures. Type A: Bony disruption of the posterior column with minimal extension into the middle column. Type B: Avulsion of posterior elements with facet joint disruption or fracture and extension into vertebral body apophysis. Type C: Posterior ligamentous disruption with fracture entering vertebra close to pars interarticularis and extending into middle column. Type D: Posterior ligamentous disruption with fracture traversing lamina and extending into apophysis of adjacent vertebral body. (Adapted from Rumball K, Jarvis J. Seat-belt injuries of the spine in young children. J Bone Joint Surg [Br] 1992;74:571-574.) |
|
TABLE 12.1-7 DENIS CLASSIFICATION OF SPINAL COLUMN INSTABILITY
|
|||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||
-
Fundamental considerations
-
□ Alignment
-
□ Stability
-
□ Canal compromise
-
-
Alignment
-
□ Cervical spine
-
□ Radiographic criteria (see Table 12.1-3)
-
-
□ Thoracolumbar spine
-
□ Initial kyphosis less than 20 degrees
-
-
-
Stability of the fracture pattern
-
□ Majority of spine fractures in children are stable
-
□ Cervical spine
-
□ Depends on specific injury
-
-
□ Thoracolumbar spine
-
□ Denis classification (Table 12.1-7)
-
-
-
Canal Compromise
-
□ Insufficient space available for cord
-
□ Encroachment by retropulsed disc, bone fragments
-
-
General surgical indications:
-
□ Unstable, purely ligamentous injuries
-
□ Unstable fractures that cannot be safely braced
-
□ Fracture with neurologic injury
-
-
Incomplete neurologic loss with canal compromise
-
Progressive neurologic deficit
MJ, Byrne TP, Abrams RA, et al. Halo skeletal fixation: techniques of
application and prevention of complications. J (Am) Acad Orthop Surg
1996;4:44-53.
HS, Filtzer DL. Pseudosubluxation and other normal variations in the
cervical spine in children. J Bone Joint Surg (Am) 1965;47:1295-1309.
N, Epstein J, Mauri T. Treatment of fractures of the vertebral limbus
and spinal stenosis in five adolescents and five adults. Neurosurgery
1989;24:595-604.
M, Zabramski JM, Browner C, et al. Pediatric spinal trauma: review of
122 cases of spinal cord and vertebral column injuries. J Neurosurg
1988;68:18-24.
J, Hensinger R, Dedrick D, et al. Emergency transport and positioning
of young children who have an injury of the cervical spine: the
standard backboard may be hazardous. J Bone Joint Surg (Am)
1989;71:15-22.
K, Inoue S-I, Takahashi K, et al. Fracture of the posterior margin of a
lumbar vertebral body. J Bone Joint Surg (Am) 1988;70:589-594.
direct blow to the arm or, more commonly in children, though indirect
twisting injuries. In neonates they may be associated with breech
deliveries or child abuse.
-
Most common in children under 3 and over 12 years of age
-
Represent about 2% of all children’s fractures
fractures in children. The fracture may be described by separation into
proximal, middle, or distal thirds of the shaft, or more commonly by
the fracture pattern (e.g., transverse, spiral, oblique).
 |
|
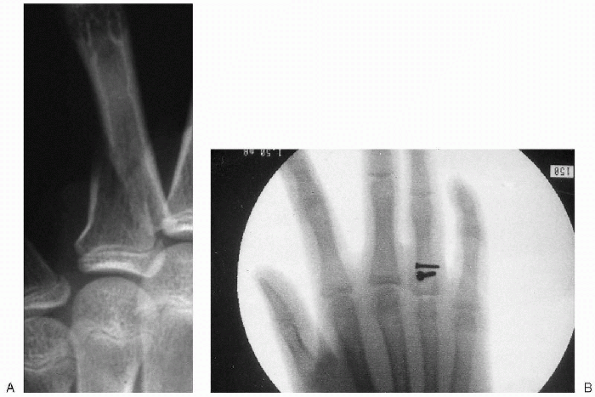
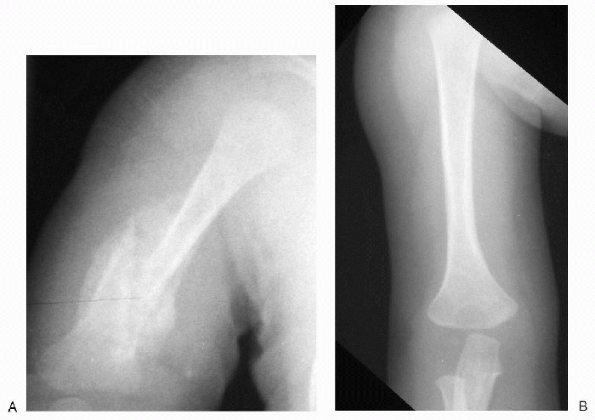
Figure 12.2-1 (A) Anteroposterior radiograph of a humerus fracture sustained at delivery in a 4-week-old girl. (B) Complete remodeling seen at 10 months of age.
|
-
A newborn child will present with inability to move the arm and localized swelling, crepitance, or deformity of the arm.
-
□ A septic shoulder or brachial plexus palsy must also be considered.
-
-
In older children, the history of injury is important, especially to rule out child abuse.
-
□ On physical exam, the extremity will usually be held against the body by the opposite hand.
-
□ Localized swelling, tenderness, and deformity may be noted.
-
□ A good neurologic exam is essential.
-
 |
|
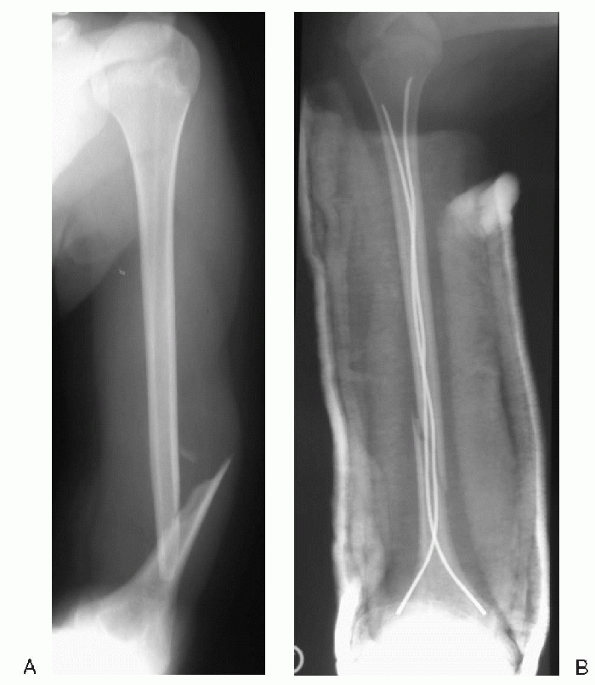
Figure 12.2-2 (A) Anteroposterior radiograph of a humeral diaphyseal fracture in a 15-year-old girl. (B) Postoperative radiograph after retrograde flexible intramedullary nailing.
|
 |
|
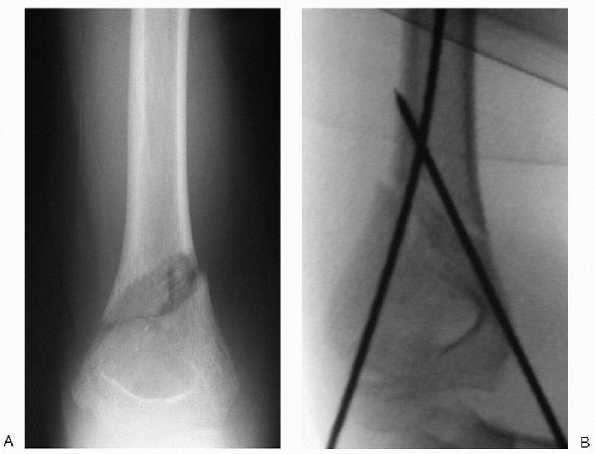
Figure 12.3-3 (A) Anteroposterior radiograph of a fracture at the distal diaphyseal/metaphyseal junction in a 9-year-old boy. (B) The fracture was treated with cross pins, using 0.062-inch K-wires.
|
-
Most humeral shaft fractures can be treated nonoperatively.
-
Neonates with humeral shaft fractures can
be treated by pinning the cuff of the sleeve to the shirt or by
splinting the arm in extension.-
□ Angulation of up to 45 degrees can remodel in infants (Fig. 12.2-1).
-
-
In older children, minimally displaced fractures can be treated in a shoulder immobilizer or Velpeau dressing.
-
□ Displaced or unstable fractures can be
immobilized with a coaptation splint or hanging arm cast, using
sedation if necessary for fracture reduction. -
□ After early callus forms, a functional fracture brace offers protection and early mobilization for the patient.
-
-
Operative treatment is rarely necessary
in children but should be considered for open fractures, in patients
with multiple injuries, and in older patients with unacceptable
reductions. -
The method of choice for fixation of humeral shaft fractures in children is retrograde flexible intramedullary nailing (Fig. 12.2-2).
-
For very distal shaft fractures, a
crossed pinning technique may be performed, as with supracondylar
humerus fractures (Fig. 12.2-3). -
Plating a humeral shaft fracture is
acceptable, but stress risers will be present at the ends of the plate,
and empty screw holes after hardware removal can increase risk of
refracture. -
External fixation is useful with comminuted or open fractures.
-
Humeral shaft fractures in children usually do very well; the vast majority may be treated nonoperatively.
-
Malunion is unusual and nonunion is rare.
-
Nerve palsies should be observed for 2 to
3 months for signs of recovery prior to further investigation or
exploration, as most recover.
-
Occur in all age groups.
-
In neonates, usually secondary to shoulder dystocia or birth trauma.
-
In older children, the mechanism may be direct or indirect trauma.
-
Pathologic fractures are also common in the proximal humerus secondary to unicameral bone cysts or other benign lesions.
-
Proximal humeral fractures are most common at 11 to 15 years of age.
-
Boys are injured up to three times as frequently as girls.
-
The forces generated by the shoulder girdle musculature displace fracture fragments in a characteristic fashion.
-
□ The rotator cuff flexes, abducts, and externally rotates the proximal fragment.
-
□ The distal fragment is adducted and anteriorly translated by the pull of the pectoralis muscles and latissimus dorsi.
-
|
TABLE 12.2-1 SALTER-HARRIS CLASSIFICATION OF THE FRACTURES OF THE PROXIMAL HUMERUS
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
-
A neonate with a proximal humerus fracture will present with the arm held at the side.
-
□ Decreased or no active motion of the extremity will be noted and swelling of the proximal arm may be present.
-
□ Without further diagnostic studies,
this injury will be difficult to differentiate from clavicle fractures,
brachial plexus injuries, septic arthritis, or the rare shoulder
dislocation.
-
-
In an older child, making the diagnosis is easier.
-
□ The patient will usually recount a history of trauma and describe pain in the proximal arm.
-
□ The affected extremity will be held against the body, with swelling and tenderness noted in the proximal arm.
-
-
In neonates, the proximal humeral
epiphysis does not ossify until 6 months of age and an ultrasound or
arthrogram will easily demonstrate the fracture. -
In older children, plain radiographs should be diagnostic.
treated by pinning the cuff of the sleeve to the shirt. The fracture
should be clinically healed in about 2 weeks.
|
TABLE 12.2-2 NEER AND HOROWITZ CLASSIFICATION OF FRACTURES OF THE PROXIMAL HUMERUS
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
treated by simple immobilization in a sling or shoulder immobilizer,
whichever is more comfortable for the patient. In children less than 8
years of age, even significant displaced grade III and IV fractures
should remodel, allowing for most all fractures in this age group to be
treated with simple immobilization.
in need of reduction, are difficult to maintain by simple
immobilization. Casting in a salute or Statue of Liberty position is
mentioned for historical reasons only. These casts are difficult to
apply and are associated with shoulder stiffness, nerve palsies, and
cast sores. If fracture reduction is necessary, percutaneous pin
fixation may be a better alternative.
proximal humerus fractures is debated as similar functional outcomes
have been documented in both operative and nonoperative treatment
regardless of displacement. The remodeling capacity of the proximal
humeral physis is significant and symptomatic malunion is unusual.
Consideration for closed reduction and percutaneous pinning should be
given for those children with Neer and Horowitz Grade III and IV
fractures who are within two years of skeletal maturity. In this group,
full remodeling of physeal fractures may not occur, which can result in
limited range of motion at the shoulder.
reduction. Indications include open fractures, displaced intraarticular
fractures, displaced tuberosity fractures, or fractures irreducible by
closed methods. Failure of closed reduction is often due to entrapment
of the periosteum or biceps tendon at the fracture site, which is
easily removed surgically.
-
Occur through both direct and indirect trauma
-
Only bony constraint between the upper extremity and axial skeleton
-
In the newborn, pressure exerted on the shoulder during delivery can lead to fracture
-
In older children, fractures may occur after a fall on an outstretched arm
-
Direct trauma resulting in fractures is commonly due to the prominent and subcutaneous position of the clavicle
-
Occur in about 5 per 1,000 births
-
Associated with high birth weight and shoulder dystocia
-
Represent up to 15% of all children’s fractures in older children
-
Medial fragment is pulled proximally by the sternoclei-domastoid.
-
Distal fragment is pulled inferiorly by the pectoralis minor.
-
Shortening occurs due to the pull of the subclavius and pectoralis muscles.
-
Fractures of the medial or distal end of the clavicle usually occur through the physis.
-
Lateral physis does not close until 19 years of age; medial physis does not close until 22 to 25 years of age.
-
These fractures differ from those of
adults, where there is associated ligament disruption of either the
sternoclavicular or acromioclavicular joints. -
In children, disruption of the thick
periosteal sleeve allows for displacement of the clavicle. The
periosteum remains in its bed with its associated ligaments still
intact. As remodeling occurs through this periosteum, the healed
clavicle reforms in its anatomic bed and is stable. Often the displaced
portion of the clavicle will resorb. -
Children over 13 years of age are more at risk for ligament disruption and may need to be treated as adults.
-
Fractures of the clavicle are classified as involving the shaft, medial end, or distal end of the clavicle.
-
True dislocations of the sternoclavicular
joint or acromioclavicular joint are rare in children, as the physis
will fail prior to joint dislocation. -
Fractures of the medial end of the
clavicle may be classified by the direction of displacement, anterior
or posterior, or by the Salter-Harris classification of physeal
injuries. -
Fractures of the lateral end of the clavicle may be classified as shown in Table 12.2-3.
-
A newborn presents with the affected extremity held to the side.
-
Swelling or crepitance may be present over the clavicle.
-
Callus formation at the fracture site is palpable about 1 week postinjury.
-
An older child with a clavicle fracture
presents with pain, swelling, tenderness, and often a palpable step off
at the fracture site. -
No active motion is noted.
-
Anteriorly displaced medial clavicular injuries are more obvious than those with posterior displacement.
-
Posteriorly displaced fractures may cause airway compromise or other mediastinal injuries.
|
TABLE 12.2-3 CLASSIFICATION OF FRACTURES OF THE LATERAL END OF THE CLAVICLE
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
-
Fractures of the medial end of the clavicle may not be obvious radiographically.
-
□ A cephalically directed tangential radiograph can show subtle asymmetry between the sternoclavicular joints.
-
□ Computed tomography (CT) scan is the study of choice to visualize the fracture and diagnose mediastinal impingement.
-
-
Displaced fractures of the midshaft of the clavicle are easily demonstrated radiographically.
-
Incomplete or nondisplaced fractures in
infants and young children may not be visualized until callus formation
is radiographically evident, about 7 to 10 days after injury. -
Displaced fractures of the lateral clavicle are usually well-visualized radiographically.
-
Imaging of both acromioclavicular joints
on the same radiograph can demonstrate subtle differences, but stress
views, with weights suspended from both wrists, are needed to reveal
suspected injuries not otherwise evident.
-
In the newborn, clavicle fractures may be treated by pinning the cuff off the sleeve to the shirt for about 10 days.
-
Midshaft clavicle fractures in older
children can be treated conservatively by a sling or figure-of-eight
dressing with excellent functional results. -
Medial clavicle fractures in children do well with nonoperative care.
-
Fractures with anterior displacement can be treated symptomatically as the reduction frequently is unstable.
-
Moderate residual deformity in younger
children will remodel and despite any residual deformity, older
children will do well functionally. -
Mild posterior displacement of the medial clavicle without mediastinal impingement may be treated conservatively.
-
Displacement causing mediastinal
impingement needs to be urgently or emergently reduced by placing the
patient supine with a bolster between the scapulae and applying
longitudinal traction to the arm.-
□ If traction alone does not affect the
reduction, a towel clip may be used, under sterile conditions, to grasp
the clavicle and manually pull it forward. -
□ A vascular or thoracic surgeon should
be on hand, even for closed reductions, as manipulation could start
mediastinal bleeding. -
□ Operative reduction may be needed if this is also unsuccessful.
-
-
Lateral clavicular fractures in children less than 14 years should do well with simple sling immobilization.
-
□ Full functional recovery can be expected.
-
-
Open fractures and fractures with
impingement of underlying structures are indications for operative
treatment of clavicle fractures. -
Closed fractures with displaced bone
fragments endangering the integrity of the overlying skin, may also
need to be treated operatively. -
Midshaft fractures of the clavicle requiring open reduction can be treated with a plate and screws or intramedullary fixation.
-
When operative treatment is indicated for
medial or lateral clavicle fractures, suture repair of the thick
periosteal tube may provide sufficient stabilization.-
□ For medial fractures, this avoids the
potential of hardware migration into the mediastinum, which increases
with transfixation of the sternoclavicular joint.
-
-
Internal fixation of these injuries should be avoided if possible.
usually secondary to high-energy injuries, such as motor vehicle
accidents. The more superficial and prominent parts of the scapula
however, such as the acromion, may sustain a fracture during sports
activities or falls. If a plausible history for a scapula fracture is
not given, consider the possibility of child abuse.
-
Scapula fractures can be classified by the anatomic location of the fracture:
-
Body of the scapula
-
Spine of the scapula
-
Glenoid fossa or neck
-
Acromion and the coracoid processes.
tenderness. Look for injury to structures in proximity to the scapula,
including the ribs, lungs, and brachial plexus. This is especially true
for high-energy injuries.
view, a lateral scapula view, and an axillary view are needed for a
complete radiographic examination of scapula injuries. A CT scan is
often necessary for the evaluation and treatment of glenoid fractures.
using a sling for comfort. Fractures of the scapula body are usually
only minimally displaced because of the overlying muscular envelope.
children may require operative intervention. These are intraarticular
fractures and reduction is necessary for stability and function of the
shoulder joint. Displaced fractures of the glenoid neck may require
operative treatment, especially when associated with ipsilateral
clavicle fractures. Operative intervention for acromion or coracoid
fractures is rare in children.
-
Shoulder dislocations in children are uncommon.
-
Usually secondary to indirect forces transmitted to the shoulder through a twisting of the arm.
-
Direct trauma to the proximal humerus and shoulder area can also result in glenohumeral dislocation.
-
Most occur during sports activity.
-
Neonatal shoulder dislocations are rare.
-
To accommodate its wide range of motion, the shoulder joint has minimal bony constraint.
-
Ligamentous thickenings of the joint
capsule are the primary stabilizers of the shoulder joint and the
rotator cuff acts as a secondary stabilizer. -
Disruption of these capsular ligaments or
their labral attachment (a Bankart lesion) is the mechanism of failure
leading to dislocation. -
Shoulder dislocations are uncommon in
young children, as the proximal humeral physis will often fail prior to
failure of these thick ligaments.
-
Shoulder dislocations can be classified
by the direction of dislocation, including anterior, posterior,
inferior (luxatio erecta), and superior dislocations. -
In children, anterior or anteroinferior
dislocations are by far the most common and occur secondary to
abduction and external rotation of the arm. -
Multidirectional instability is also possible.
-
Dislocations can also be classified as traumatic or atraumatic.
-
□ Atraumatic dislocations are often seen
in habitual dislocators, or in those with conditions associated with
joint laxity (e.g., Larsen syndrome or Ehlers-Danlos syndrome).
-
-
Shoulder dislocations can also be classified as acute, recurrent, or chronic.
-
The patient with a traumatic shoulder dislocation presents with a painful deformity to the shoulder.
-
If anteriorly dislocated, the arm is usually slightly abducted and externally rotated.
-
The acromion will be prominent, and hollowness will be noted beneath it.
-
The humeral head may be palpable anterior to the glenoid.
-
The less common posterior dislocation
will cause the arm to be held in adduction and internal rotation, with
a posterior shoulder prominence. -
The axillary nerve is at risk of injury
after shoulder dislocations and should be examined as part of a full
neurovascular exam prior to initiating treatment.
-
A shoulder dislocation can be visualized
with plain radiographs which include an AP view of the shoulder, a
lateral scapula view, and an axillary view. -
Note any associated proximal humeral fracture that could displace during reduction.
-
After reduction, a compression fracture
of the humeral head, called a Hill-Sachs lesion, can be visualized on
an AP view with internal rotation of the arm.
accomplished under sedation. For both anterior and posterior
dislocations, a traction/countertraction maneuver is effective for the
reduction, using a sheet placed under the axilla. Postreduction
radiographs are compulsory. Once a patient is comfortable, aggressive
physical therapy should be instituted to strengthen the rotator cuff
and shoulder girdle musculature. The family and patient should be made
aware that there is a high risk of recurrence in children necessitating
operative intervention.
stabilization is then recommended. The surgical procedure will depend
upon the type of dislocation, whether there is a Bankart lesion, and
the preference of the surgeon. Surgical intervention may not be
recommended for habitual dislocators due to the high postoperative
recurrence rate.
D, Weiner DS, Noble JS, et al. Severely displaced proximal humeral
epiphyseal fracture: a follow up study. J Pediatr Orthop 1998;18:31-37.
CF, Kiaer T, Lindequist S. Fractures of the proximal humerus in
children: nine year follow-up of 64 unoperated cases. Acta Orthop Scand
1990;61:255-257.
K, Bassett GS. Complete posterior sternoclavicular epiphyseal
separation: a case report and review of the literature. Clin Orthop
1992;281:84-88.
HJ, Angel KR, Schemitsch EH, et al. The fate of traumatic anterior
dislocation of the shoulder in children. J Bone Joint Surg (Am)
1992;74A:1242-1244.
K, Sarwark JF. Proximal humerus, scapula, and clavicle. In: Beaty JH,
Kassar JR, eds. Rockwood and Wilkins’ fractures in children, 5th ed.
Philadelphia: Lippincott Williams & Wilkins, 2001: 741-806.
epiphysis, radial head and neck, and ulnar olecranon process. The
proximity of the radial, median, and ulnar nerves and the brachial
artery to the elbow trauma can be a major source of apprehension and
urgency for the physician.
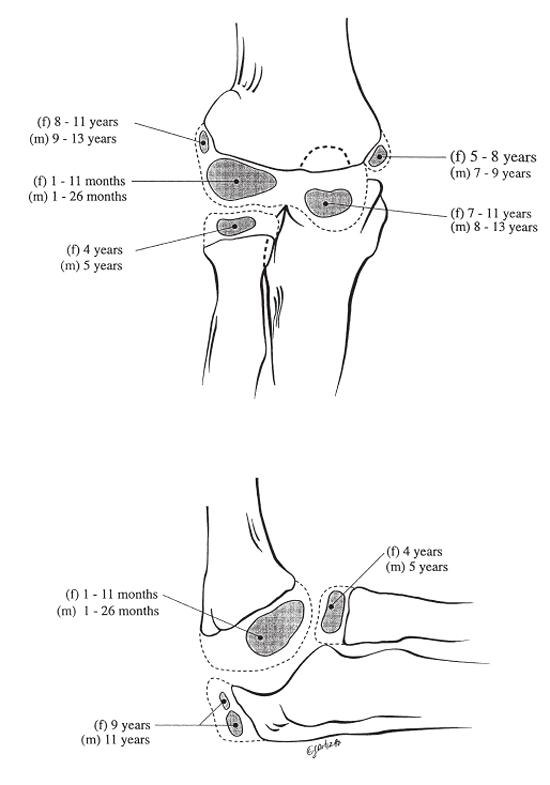
sequential appearance of the ossification centers: “CRITOE” and “Come
rub my tree of life”—capitellum, radius, internal (medial) epicondyle, trochlea, olecranon,
and external (lateral) epicondyle (Fig. 12.3-1).
On a lateral radiograph, the capitellar center is located anteriorly
and tilts downward. Its posterior unossified epiphysis is wider
posteriorly than it is anteriorly. A line drawn down the anterior
surface of the humeral cortex passes through the middle to posterior
half of the capitellum on a lateral roentgenogram (Fig. 12.3-2).
-
Usually caused from a fall on an outstretched extremity with the elbow in full extension.
-
Child abuse must be suspected if child is less than 2 years of age.
 |
|
Figure 12.3-1 Chronologic appearance of the centers of ossification as seen on radiographs.
|
-
The rate of occurrence between boys and girls is 3 to 2.
-
Average age is 7 years.
-
Nerve injury occurs in about 10% of cases (median and radial nerves).
-
Distal radius fracture is the most common associated skeletal injury.
-
Elbow swelling, tenderness, and diminished active movement of extremity.P.112
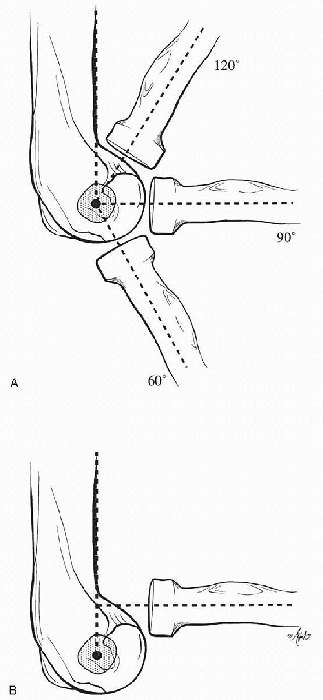 Figure 12.3-2 (A) The normal anterior humeral cortical line transecting the center of the capitellum as seen on a lateral radiograph. (B) Anterior radial head dislocation.
Figure 12.3-2 (A) The normal anterior humeral cortical line transecting the center of the capitellum as seen on a lateral radiograph. (B) Anterior radial head dislocation. -
Anterior Pucker sign occurs when the proximal bone spike penetrates into the subcutaneous tissue.
-
Evaluate humerus, forearm, wrist and hand for associated injuries.
-
Sensory loss is more difficult to assess in young children.
-
Vascular examination: check for pulses, capillary refilling, skin temperature, and forearm compartment tenseness.
-
Painful passive finger extension and flexion may indicate increased forearm compartment pressures.
-
Get good quality x-rays of entire extremity.
-
Contralateral radiographs are controversial and should only be obtained if the diagnosis is unclear.
-
Definitive reduction of the fracture is carried out under general anesthesia with C-arm fluoroscopic control.
-
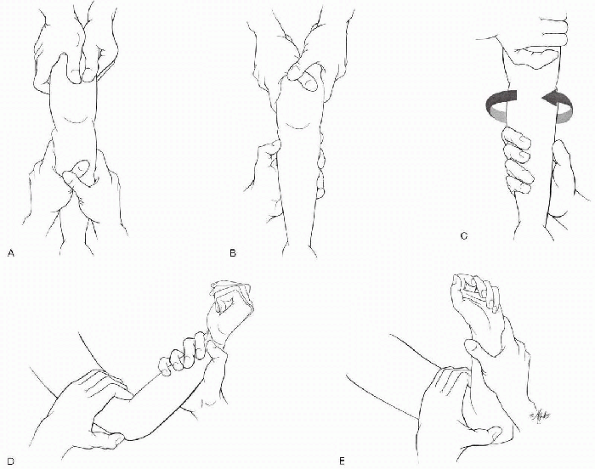
Apply longitudinal traction to reduce the proximal displacement and any varus or valgus angulation (see Fig. 12.3-3A).
-
Reduce medial or lateral displacement (see Fig. 12.3-3B).
-
Internally rotate the forearm if needed to correct external rotation of distal fragment (see Fig. 12.3-3C).
-
Reduce the posterior displacement by applying pressure on the olecranon process while maintaining traction (see Fig. 12.3-3D).
-
Flex elbow acutely with forearm in pronation for both medial and lateral displacement of distal fragment (see Fig. 12.3-3E).
-
Open reduction and internal fixation for the unstable displaced fractures.
-
Use the same treatment principles that apply to adult fractures.
-
Open reduction indicated if vascular compromise exists or soft tissue interposition prevents adequate fracture reduction.
-
Openly reduced fracture can be fixed with percutaneously placed pins.
-
Immediate fracture reduction is the treatment of choice for a distal pulseless extremity.
-
An absent pulse with the following conditions warrants brachial artery exploration:
-
□ Abnormally high forearm compartment pressures and clinical findings of a development of compartment syndrome
-
□ Loss of pulse after closed reduction
-
-
Early clinical findings are worsening forearm pain at rest or with passive finger movement.P.113
![]() Figure 12.3-3 Reduction of supracondylar fractures. (A) Traction. (B) Correction of displacement. (C) Rotation correction. (D) Reduction. (E) Pronation.
Figure 12.3-3 Reduction of supracondylar fractures. (A) Traction. (B) Correction of displacement. (C) Rotation correction. (D) Reduction. (E) Pronation. -
Compartment syndrome can exist in the presence of a palpable pulse.
-
Forearm compartment pressures greater than 30 mm Hg and the presence of clinical findings warrant fasciotomy.
-
Median nerve injury can mask the pain associated with Compartment syndrome.
-
Occurs in about 15% of cases.
-
The anterior interosseous branch of the median nerve is commonly involved.
-
Nerve recovery usually occurs within 3 months
-
Cubitus varus is most common.
-
Lateral downward tilt of the medial side of the fracture is the main cause of cubitus varus
-
This rare condition is known to resolve within 2 years.
-
Surgery is rarely indicated.
-
An asymptomatic fishtail deformity may develop.
-
Best treated conservatively.
-
Loss of elbow flexion and increased hyperextension is associated with residual posterior tilt of the distal fragment.
-
Anterior impingement by a medially rotated distal fragment can restrict elbow flexion.
-
The combination of some bone remodeling with growth and therapy usually restores functional range of motion.
|
TABLE 12.3-1 CLASSIFICATION AND TREATMENT OF EXTENSION SUPRACONDYLAR FRACTURES
|
|||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||
-
Accounts for less than 2% of all supracondylar fractures.
-
The mechanism of injury in a direct blow on a flexed elbow.
-
The periosteum is torn posteriorly so that the reduced fracture is unstable in flexion.
-
The ulnar nerve is prone to injury.
-
Similar to extension-type fractures
-
□ Type I: nondisplaced
-
□ Type II: mild angulation
-
□ Type III: displaced
-
-
Swelling and tenderness about elbow.
-
Radiographically, the distal humerus fragment is anteriorly angulated or displaced.
-
Long arm cast with elbow flex for comfort, neutral forearm rotation
-
Home therapy program
-
Closed reduction under general anesthesia by extending elbow
-
Unstable fracture requires percutaneous Kirschner pin fixation
-
Apply a long arm cast with elbow extended and forearm in neutral rotation
-
Closed reduction under general anesthesia
-
Percutaneous pin fixation with elbow in extension or 30-degree flexion
-
Immobilize in a splint or cast with elbow in flexion or extension
-
Remove Kirschner wires (K-wires) in 3 to 4 weeks
for all physeal fractures after phalanx and wrist. The physis fracture
type depends mainly on skeletal age and injury mechanism (Table 12.3-2).
 |
|
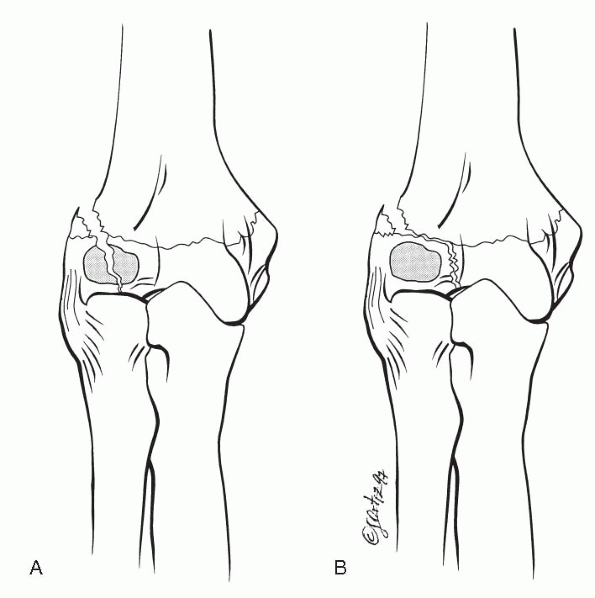
Figure 12.3-4 Classification of lateral condyle fractures. (A) Milch type I, lateral view (Salter-Harris type IV). (B) Milch type II, lateral view (Salter-Harris type II).
|
|
TABLE 12.3-2 THE ROLE OF AGE IN PHYSEAL FRACTURE TYPES
|
||||||||
|---|---|---|---|---|---|---|---|---|
|
-
Account for 20% of distal humerus fractures.
-
Likely mechanism of injury is elbow extension, forearm adduction, and supination.
-
The commonest fracture line travels from
the posterior lateral metaphysis, along the physis, and into the
trochlea (Milch type II) (Fig.12.3-4). -
The rare fracture line type starts from
the posterolateral metaphysis, through the physis and body of the
capitellum (Milch type I) (see Fig. 12.3-4). -
Elbow arthrogram under general anesthesia
and magnetic resonance imaging (MRI) are good for accessing lateral
displacement of elbow if not obvious on radiographs.
-
Seen more frequently in patients treated with cast immobilization.
-
For minimally displaced fractures (≈2 mm) keep immobilization for 2 months if necessary.
-
Delayed in situ pinning is an option.
-
Open reduction after 3 weeks of injury is controversial.
-
Results from inadequate treatment.
-
Untreated nonunion may lead to cubitus valgus and ulnar nerve dysfunction.
-
Specific treatment is controversial—the best goal is prevention.
-
Lateral spur formation most common deformity associated with this fracture.
-
Cubitus varus may result secondary to condylar physeal overgrowth or inadequate fracture reduction.
-
The sharp angle wedge type is caused by a
bony bar from inadequate fracture reduction between the lateral condyle
ossification center and that of the trochlea. -
The smooth curved wedge type is associated with osteonecrosis of the lateral part of the medial crista of the trochlea.
-
Not associated with any significant elbow function deficiency.
-
May be caused by extensive dissection needed for late reduction of fracture.
-
Regeneration of the condyle is likely to occur if union occurs.
-
Loss of joint motion may result.
-
Rare complication with resulting loss of elbow motion.
-
Premature closure of the physis can occur
in conjunction with premature fusion of the secondary centers of
ossification in the epiphysis. -
Limited growth potential of the distal
humeral physis and the non-weightbearing status of the humerus
decreases the adverse effects of a physeal arrest.
|
TABLE 12.3-3 STAGES AND TREATMENT OF LATERAL CONDYLAR PHYSEAL FRACTURES
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
Figure 12.3-5 Rutherford classification of lateral condyle. (A) Type I. (B) Type II. (C) Type III.
|
epiphyseal fractures of the lateral condyle and occasionally the
lateral crista of the trochlea.
-
Usually caused by the impaction of the radial head on the capitellum
-
Rare injury, seen mainly in children older than 12 years
-
Difficult to diagnose in the younger child
-
Radial head fractures seen in one-third of patients
-
Hahn-Steinthal type: includes the capitellum and cancellous bone from the lateral condyle and lateral crista of the trochlea.
-
Kocher-Lorenz type: articular fracture seen mainly in adults.
-
The Rutherford classification.
-
Elbow flexion is restricted.
-
Swelling is limited in isolated injuries.
-
Routine radiographs with oblique views to detect small bone fragments.
-
Computed tomography (CT), arthrogram, and MRI are useful diagnostic tools.
-
Look for associated radial head fractures.
-
Surgery is indicated in most cases because of intraarticular involvement.
-
Excision of the fragment is recommended for comminuted or neglected fractures.
-
Reattachment of large bone fragments with compression screw fixation gives better results than K-wire fixation.
-
Avascular necrosis of the fragment is a potential complication.
-
Isolated medial condylar fractures are
rare, accounting for less than 1% of all elbow fractures in children
between 8 and 14 years. -
Occasionally seen in association with
supracondylar fractures of the humerus, olecranon process fractures,
and posterolateral elbow dislocations. -
The most likely mechanism is a fall on an outstretched arm with a valgus strain or a direct fall on the flexed elbow.
-
Swelling and pain on inner side of elbow.
-
Joint instability on valgus stress.
-
Diagnosis is based on radiograph findings.
-
Before the age of 8 years extraarticular
medial epicondylar apophyseal fractures may be confused with medial
condylar fractures. An MRI or arthrogram may be helpful. -
A posterior fat pad sign is suggestive of intraarticular involvement.
-
Cubitus varus: associated with failure to reduce a displaced fracture, nonunion, or avascular necrosis of the medial condyle.
-
Avascular necrosis of the medial crista of the trochlea may follow open reduction of the fracture.
-
Cubitus valgus can occur secondary to overgrowth.
|
TABLE 12.3-4 KILFOYLE CLASSIFICATION AND TREATMENT OF MEDIAL CONDYLAR FRACTURES
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
-
Primarily cartilaginous epiphysis makes diagnosis difficult.
-
Fracture separation of entire physis usually occurs before 6 years of age.
-
The medial epicondyle apophysis shares a
common physeal line with the distal epiphysis until about 6 years of
age in girls and 8 years of age in boys. -
It is believed that the horizontal line
of the physis and its close proximity to the olecranon fossa are
responsible for this fracture pattern.
-
High index of suspicion is key.
-
Often the result of abuse in non-ambulatory children.
-
Swelling may be minimal in the newborn
-
Swollen elbow in an infant or toddler
-
Crepitus with elbow motion
-
Relationship between the radial head and lateral condylar center of ossification is maintained.
-
Intact proximal radius and ulna displaces posterior and medial; with elbow dislocations the displacement is posterolateral.
-
Arthrography, ultrasound, and MRI are helpful in differentiating the fractures.
-
Closed reduction is attempted in all
cases under sedation. Medial displacement corrected in extension and
elbow, then flexed and pronated.P.119TABLE 12.3-5 CLASSIFICATION OF DISTAL PHYSIS SEPARATIONClassification
Age
Description
Group A (Salter-Harris type I)
Newborn-12 mo
Epiphysis is mainly cartilaginous tissue
Group B (Salter-Harris type I)
12 mos-3 yr
Possible metaphyseal bony flakes with epiphysis
Group C
3-7 yr
Large metaphyseal fragment, usually from the lateral side
-
□ Two percutaneous K-wires can be used to fix the fracture in older children.
-
□ For neglected fractures (more than 5 days) immobilize and expect sufficient remodeling with time.
-
-
Malunion:
-
□ Most frequent complication
-
□ Seen mainly in untreated patients
-
-
Rare: traumatic osteonecrosis of the trochlea, nonunion
-
Male-to-female ratio of 4:1
-
Associated with elbow dislocation in 50% of cases
-
Peak age of incidence is 9 to 12 years.
-
A traction apophysis that does not contribute to longitudinal humeral growth
-
Common origin for forearm flexion muscle mass and medial capsular attachment
-
Becomes an extraarticular structure at age 8 years
-
Indirect:
-
□ Acute hyperextension of elbow with
forced elbow valgus stress. Associated with anterior and distal
displacement of apophysis greater than 5 mm. -
□ Chronic repetitive or dominant overuse of extremity (e.g., Little League pitchers)
-
-
Direct:
-
□ Direct posterior blow to the epicondyle
-
-
Pain, tenderness, and swelling localized medially.
-
Increased pain with resistive wrist flexion or valgus stress to elbow.
-
Loss of elbow motion.
-
Other injuries may complicate the clinical findings (i.e., elbow dislocation, olecranon, or coronoid fractures).
-
Standard anteroposterior, lateral, and oblique views of the elbow joint are required.
-
In children younger than 5 years, MRI or arthrograms are useful.
-
Look for widening of the physis, distal and anterior migration of apophysis.
-
Seen in 60% of cases treated conservatively
-
Elbow function rarely compromised
-
Treatment necessary if pain or tenderness persists
-
Associated with severe displacement or incarceration of the epicondyle in the elbow joint
-
Necessitates exploration of the ulnar nerve and reduction of fracture
-
Seen in 10% of cases
-
Rare
-
Conservative measures recommended since lesions may spontaneously resolve
|
TABLE 12.3-6 TREATMENT OF MEDIAL EPICONDYLAR APOPHYSEAL FRACTURES
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
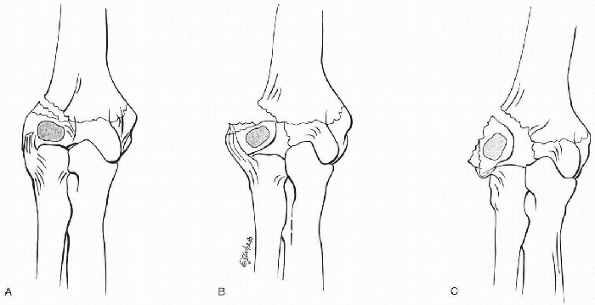
Figure 12.3-6 Degrees of medial epicondylar apophyseal fractures.
|
the natural appearance of this center is frequently confused for a
fracture.
-
Ossification center appears at about 10 years of age.
-
The early bony sliver is normally separated from the metaphysis and epiphysis by 2 to 3 mm.
-
The ossifying epicondylar epiphysis fuses first with the capitellum then the humeral metaphysis.
-
Violent contraction of the common extension muscles of the forearm causes isolated avulsion fractures.
-
Local pain and swelling over outer elbow
-
Elbow joint stiffness
-
Lateral separation of the ossification center from the metaphysis and capitellum is a normal finding.
-
An avulsion fracture is diagnosed when the ossification center lies distal to the osteochondral epiphysis.
-
Immobilization of extremity in a sling or splint for comfort
-
An incarcerated fragment in the elbow requires open reduction and wire fixation.
-
Nonunion: usually asymptomatic
-
Usually caused by an indirect hyperextension and valgus force to elbow with supination of forearm.
-
Uncommon anterior elbow dislocation is caused by a direct force on the flexed joint.
-
Accounts for 3% of all joint dislocations
-
Usually occur at age 13 to 14 years
-
Associated elbow fractures in about 50% of cases
-
Boy-to-girl ratio is 3:1
-
Left-to-right-side ratio is 3:2
-
Elbow hyperextension is the cause in over 90% of cases.
-
Based on the position of the proximal radioulnar joint with regard to the distal humerus:
-
□ Proximal radius and ulna usually displace as a unit.
-
□ Disassociation of the proximal radioulnar joint rarely occurs.
-
□ Divergence of radius and ulna is rare.
-
-
Routine anteroposterior and lateral radiographs are not always possible and multiple views and
-
Comparison radiographs of the contralateral elbow may be helpful.
-
Prompt reduction is necessary to relieve pain, and prevent or minimize neurovascular complications.
-
Check neurovascular status before and after reduction.
-
Radiographs are necessary before and after reduction.
-
Sedation and analgesia are recommended.
-
Hypersupinate forearm and apply traction
-
Apply downward force along the distal arm and proximal forearm while using counter traction
-
Loss of elbow motion:
-
□ Most common complication
-
□ Terminal extension loss of 15 degrees is commonplace
-
-
Neurologic injuries:
-
□ Usually transient
-
□ Ulna nerve most commonly affected
-
-
Arterial insufficiency:
-
□ Can be caused by thrombosis, rupture, or entrapment
-
□ Collateral arterial flow may be
sufficient to permit a weak Doppler radial pulse or a good nailbed
capillary flow in the finger in the presence of an obstructed proximal
radial or brachial artery
-
-
Myositis ossificans and heterotopic ossifications
-
Recurrent posterior dislocation rare, but occurs more commonly in children than adults
-
Anterior elbow dislocation:
-
□ Incidence 1%
-
□ Elbow held in extension and a fullness in the articubital fossa is felt
-
□ Treated by closed reduction: elbow is partially flexed with traction and a downward force on the distal arm
-
-
Medial and lateral elbow dislocations:
-
□ Only lateral elbow dislocations are reported in children
-
□ Lateral subluxation may not be obvious as a complete dislocation on radiographs
-
-
Divergent elbow dislocations:
-
□ Rare injury associated with excessive compressive forces of the elbow
-
□ Usually associated with radial head, neck, and proximal ulnar fractures
-
□ Proximal radius displaced posteriorly and radially
-
-
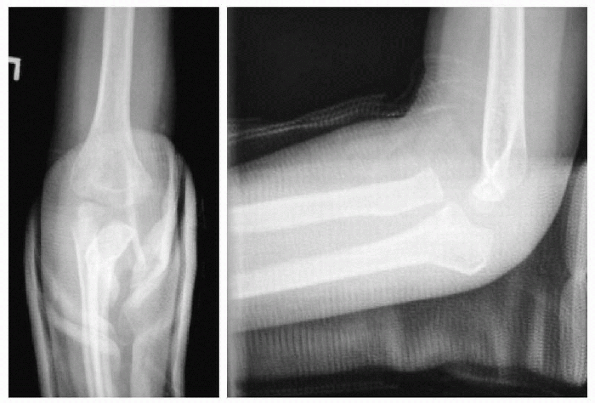
Isolated traumatic dislocations of the radial head are considered a variant of Monteggia fracture, type I.
-
Partial or complete anterior displacement
of the radial head and subtle anterior bowing of the ulnar shaft on
lateral radiographs (ulna bow sign) are diagnostic. -
Other possible causes of anterior radial
head dislocations: cubitus varus after supracondylar fractures,
osteochondritis dissecans of the capitellum, and birth trauma. -
The mechanism of injury is the same as that for Monteggia injuries but without obvious ulna fracture.
-
Unlike acute traumatic dislocations, long-standing traumatic dislocation may mimic congenital dislocations on radiographs.
-
Acute anterior dislocation: closed reduction with flexion and supination
-
Chronic (more than 3 weeks) anterior
dislocation: open reduction is controversial but may be recommended up
to 3 years after injury.
-
Annular ligament slips proximally because of weak distal attachments of the annular ligament to the radial head.
-
Common injury under age 5 years (mean age, 2.5 years)
-
Girls: 65% of the time
-
Left elbow: 70% of the time
-
Mechanism of injury: longitudinal pull on a straight elbow with forearm in pronation
-
In forearm pronation, the lateral head surface is narrower and rounder, but it is wider and squarer in supination.
-
History may not be readily obtainable.
-
Child stops using the extremity.
-
Forearm supination is more painful than pronation.
-
Radiography is often normal.
-
Look for other occult fractures (i.e., supracondylar, lateral condyle, or radial head and neck fractures)
-
Closed reduction by flexion and supination.
-
Spontaneous reductions may occur before patient is seen by physician.
-
Acute injury:
-
□ Usually a combination of forces, compression, angulation, and rotation on a hyperextended valgus elbow
-
□ May be isolated to the radius or in
association with elbow dislocation, where the radius fracture may be
caused as the elbow dislocates or when the joint reduces
-
-
Chronic injury:
-
□ Seen in athletes who stress the elbow in a repetitive fashion (i.e., Little League pitcher)
-
-
7% of elbow fractures
-
Fractures seen at all ages (median age 9.5 years)
-
Equal incidence between sexes
-
Most common fracture pattern is through the less dense neck and physis.
-
Radial head fracture likely to occur in older child.
-
Isolated injury: outer elbow pain,
swelling, and tenderness associated with loss of forearm rotation and
elbow flexion and extension -
Associated with other injuries: elbow
dislocation, olecranon process and ulnar shaft fractures (Monteggia),
medial epicondyle injury, or distal radioulnar joint -
Elbow pain, swelling, and tenderness are more severe.
-
Joint mobility severely restricted due to greater involvement of other elbow structures and hemarthrosis.
-
Wrist and forearm pain may be present.
-
Weak wrist extension with radial deviation occurs if posterior interosseous nerve function is compromised.
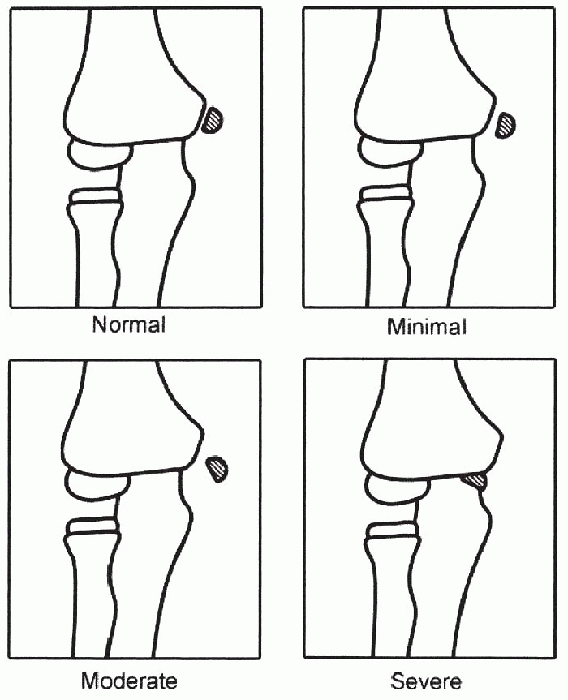
fractures, where the articular surface of the radial head is intact and
the fracture line is through the neck. The two important factors
dictating treatment outcomes are radial head angulation and
displacement.
|
TABLE 12.3-7 COMPARISON OF TWO CLOSED REDUCTION TECHNIQUES FOR RADIAL HEAD AND NECK FRACTURES
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
-
Radial head—angulation ≤30 degrees and displacement ≤3 mm:
-
□ Stable fracture pattern
-
□ No reduction necessary
-
□ Immobilization with long arm splint or cast with elbow flexed at 90 degrees and forearm in neutral rotation
-
□ Discontinue immobilization in 2 to 3 weeks
-
□ Protected physical therapy in tally
-
□ Note: a minimally displaced articular
fracture of the radial head usually seen in older child with closed
physis is treated in a similar fashion -
□ Fracture reduction required to guarantee acceptable elbow function
-
-
Radial head angulation ≥30 degrees and displacement ≥3 mm
-
□ Closed reduction only
-
□ Patterson or Kaufman manipulation (Table 12.3-7)
-
□ Long arm cast with elbow at 90 degrees and forearm pronated
-
□ Remove cast at 3 weeks
-
-
Percutaneous pin reduction or intramedullary pin reduction may be indicated if closed methods fail
-
Open reduction indicated for a residual
angulation ≥40 and displacement ≥3 mm or when there is failure to
regain forearm supination 50% and pronation
-
Elbow stiffness: associated with severe trauma or open reduction
-
Hypertrophic changes of radial head:
-
□ Seen in about 30% of cases
-
□ Associated with a clicking sound with forearm rotation
-
□ No treatment needed
-
-
Avascular necrosis of radial head:
-
□ Seen in about 15% of cases
-
□ Associated with surgical reduction
-
□ Expect unsatisfactory functional results
-
-
Premature physeal closure:
-
□ Can potentially produce cubitus valgus
-
□ Elbow function not significantly affected
-
-
Nonunion of radial neck: rare; treat conservatively
-
Radioulnar synostosis: associated with severe trauma; open reduction and delay fracture treatment
-
Malunion: predisposes the radiocapitellar joint to arthritis
-
Nerve injury: posterior interosseous nerve injury is usually iatrogenic
-
Myositis ossificans:
-
□ Common (30% of cases in one series)
-
□ Supinator muscle usually involved
-
-
Olecranon fracture accounts for 5% of elbow injuries and results from an avulsion force acting across a flexed elbow
-
Triceps muscle insertion extends into the metaphysis, offering some protection to the epiphysis and physis
-
Palpable defect can be felt between the apophysis and metaphysis with displaced fractures
-
Tenderness and local soft tissue swelling present
|
TABLE 12.3-8 CLASSIFICATION OF APOPHYSEAL FRACTURES OF THE PROXIMAL ULNA
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
-
Obvious in the older child after the appearance of ossification centers
-
Elbow arthrogram or MRI useful in the younger child
-
Open reduction and internal fixation with axial pins and figure-of-eight tension—band wiring for displaced fractures
-
Rest for most stress fractures and avoidance of the offending elbow motion
-
Nonunion requires compression screw fixation with bone graft
-
Apophyseal arrest may occur but is not associated with functional loss
-
Indirect traction forces with the elbow flexed
-
Valgus or varus forces with elbow extended
-
A direct blow to the olecranon
-
Seen at all ages, with peak incidence at age 5 to 10 years
-
20% associated with other elbow injuries
-
By Chambers:
-
□ Group A: flexion injuries
-
□ Group B: extension injuries
-
□ Valgus pattern
-
□ Varus pattern
-
-
□ Group C: shear injuries
-
-
By Papavasilouetted:
-
□ Group A: extraarticular
-
□ Group B: intraarticular
-
-
Local swelling over the olecranon
-
Skin abrasions
-
Palpable defect
-
Weakness in elbow extension
-
Get routine radiographs of entire elbow
-
Look for perpendicular fracture lines
-
Residual physeal line is oblique and runs proximal and anterior
-
Look for associated injuries involving medial epicondyle, radial head and neck, and lateral condyle
-
Extension type, minimally displaced:
-
□ Long arm cast or splint immobilization for 3 weeks
-
□ Elbow may be flexed at 80 degrees or 10 degrees
-
□ Supervised rehabilitation
-
-
Extension type, displaced more than 2 mm: open reduction
-
Shear type:
-
Uncommon
-
Loss of elbow function associated with failure to correct alignment or loss of reduction
-
Other uncommon complications include
elongation of olecranon process, ulnar nerve transient neuropraxia,
compartment syndrome, delayed unions, and nonunions
JH, Kasser JA. Rockwood and Wilkins’ fractures in children, 5th ed.
Philadelphia: Lippincott Williams & Wilkins, 2001: 483-739.
S. On osteochondrosis deformans juvenilis capituli humeri including
investigation of intra-osseous vasculature in distal humerus. Acta
Orthop Scand [Suppl] 1959;38:81-93.
R, Fowels, JV, Rang M, et al. Observations concerning fractures of the
lateral humeral condyle in children. J Bone Joint Surg Br
1975;57:430-436.
JA, Graham HK. Angulated radial neck fractures in children: a
prospective study of percutaneous reduction. J Bone Joint Surg (Br)
1992;74:760-764.
skeletal injuries in the pediatric population. The mechanism is usually
an axial load, such as a FOOSH (fall onto an outstretched hand), with
varying degrees of rotation. Depending on the amount of force at the
time of impact, the fracture can occur at any location within the
forearm. The distal one-third radius is usually the most common site of
injury. Although most metaphyseal forearm fractures can be
conservatively treated without sequelae in skeletally immature patients
due to remodeling, some fractures at the midshaft and proximal
one-third forearm may need operative intervention to avoid the
occasional poor results. A thorough understanding of forearm fractures
and an awareness of the potential pitfalls that may occur in some of
these can ward off potential complications and assure a more clinically
satisfactory result at the completion of fracture healing.
child’s play. Tripping while running or a resisted fall during sports
are probably the more common causes of fracture, followed closely by a
fall from short heights, such as the monkey bars or trees. Higher
energy trauma, such as from auto-pedestrian or motor vehicle accidents
result in more dissipation of energy and more comminution, as well as
fractures that are located more at the distal metaphysis or epiphysis.
-
Forearm fractures tend to occur during seasons of active play, such as spring and summer, or with changes in the temperature.
-
Boys are affected more often than girls, in a 2.9:1 ratio.
-
Both sexes tend to fracture the nondominant arm most frequently, as it is the free arm available to break a fall.
-
The average age for forearm fractures
tends to be 10.5 years for girls and 12.8 years for boys, although boys
can tend to follow a bimodal peak. -
The first peak occurs around 9 years,
with the second peak happening around 13 to 14 years. The distal third
of the forearm is the most common location for fractures overall, as
well as the most common site in the older child. -
The midshaft region is more commonly
fractured in younger children. This is a reflection of their inherent
anatomy, which includes more cancellous bone extending beyond the
metaphysis into the diaphysis. -
Distal metaphyseal and epiphyseal
fractures occur in the older child (most commonly in boys between 13
and 15 years, and girls between 12 and 13 years). This difference
reflects the difference in the average age of skeletal maturation
between the two genders. Near skeletal maturity, the amount of cortical
bone at the diaphysis
P.126increases and the metaphyseal area decreases, making the distal radius the weaker portion of forearm bone.
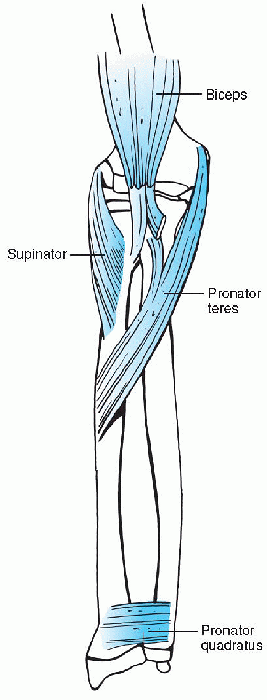
proximal end that articulates with a relatively straight ulna during
forearm rotation. Muscles that attach to the forearm and act as
potential deforming forces in fractures include, proximally, the biceps
and supinator and, more distally, the pronators teres and quadratus.
supinated proximal fragment and the position of reduction should place
the distal fragment into supination. Fracture at the midshaft should be
reduced and stabilized in neutral. Fractures of the distal third of the
radius need to be stabilized in neutral to slight pronation due to the
activity of the pronators on the proximal fragment (Fig. 12.4-1)
 |
|
Figure 12.4-1 Musculature of the forearm.
|
and ecchymosis at the forearm is fairly diagnostic. Gross displacement
and angulation will enhance the deformity further and make the fracture
more obvious on clinical examination. Swelling, crepitus, and gross
motion can usually be elicited at the site of the fracture, which is
associated with pain. Check for any lacerations or areas of fatty blood
to rule out an open fracture (which may necessitate an operative
irrigation and débridement).
-
Examination of the wrist, elbow, and
shoulder on the ipsilateral side should also be performed to rule out
other associated fractures or dislocations [e.g., the radial head in
Monteggia fractures, or distal radioulnar joint (DRUJ) disruption in
Galeazzi fractures]. Supracondylar humeral fractures can occur in up to
5% of forearm fractures. Although rare, the most common ipsilateral
carpal injury is the scaphoid fracture.
-
Radius only
-
Both bones
-
Galeazzi fracture (distal radius fracture with disruption of the distal radioulnar joint)
-
Radius only
-
Both bones
-
Night stick (midshaft transverse ulna fracture)
-
Plastic deformation (failure of elastic limit leading to bowing)
-
Radius only
-
Both bones
-
Monteggia fracture (proximal ulna with radial head dislocation)
-
Maintenance or loss of skin integrity over the fracture
-
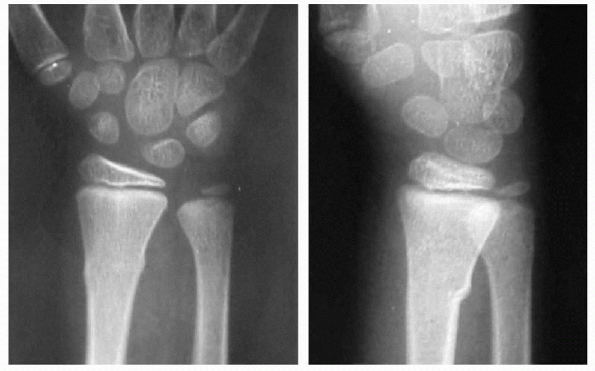
Failure of one cortex in compression with preservation of other cortex, which leads to “buckling” of bone
-
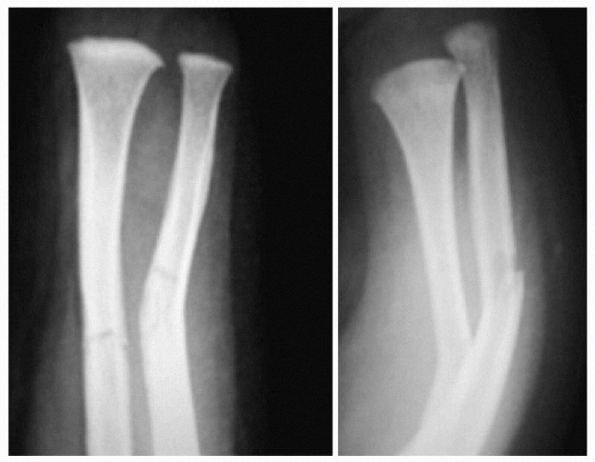
Failure of one cortex in compression and the other in bending/rotation
-
Unstable fracture and may continue to angulate
-
Cortical disruption through all cortices
-
High-energy injury with multiple fragments and usually displaced or unstable
 |
|
Figure 12.4-2 Anterior radial head dislocation with apex anterior ulna fracture.
|
 |
|
Figure 12.4-3 Torus, or buckle, fracture.
|
-
The fingers should be checked for color and capillary refill.
-
The hand should be checked for warmth of the distal limb and the presence of a good radial pulse.
-
Neurovascular exam should include motor
and sensory testing in the radial, ulnar, and median nerves (RUM)
distribution (i.e., radial [motor—thumbs up/sensation—first web space
dorsally], ulnar (motor—spread fingers against
resistance/sensation—little finger), and median distributions
[motor—cross index and middle finger/sensation—tips of index and middle
finger]), including the anterior interosseous branch of the median
nerves (primarily a motor branch to the Hexor indicisproprius (FIP),
Hexor pollicis longus (FPL), and pronator quadratus/okay sign). -
Radiographs should include orthogonal
visews of the entire forearm to include the wrist and elbow in order to
determine rotational alignment and to rule out involvement of the
joints above and below the fracture.
 |
|
Figure 12.4-4 Greenstick fracture.
|
cortical thickness and contour of the fractured ends. This can
sometimes be difficult in comminuted fractures. Other means of checking
for fracture alignment include evaluation of the radial tuberosity
relationship to the radial styloid in the coronal plane. They are
usually 180 degrees apart. Other anatomic landmarks include the
coronoid process and styloid on the ulna, which are not visible on the
anteroposterior radiograph, but could be seen on the lateral x-ray. In
this view, the coronoid process faces anteriorly and the styloid points
posteriorly. The fracture is reduced by appropriately rotating the
distal fragment to reestablish these normal anatomic landmarks.
 |
|
Figure 12.4-5 Complete fracture.
|
occur in skeletally immature individuals, most fractures tend to heal
without sequelae. The goals of treatment are to initially obtain an
acceptable alignment and maintain this alignment until the completion
of healing.
-
Initial immobilization with a sugar tong
splint (Ushaped splint around the wrist and elbow) in the emergency
room (or cast if minimally swollen) is sufficient for buckle or
minimally angulated greenstick fractures of the distal metaphysis. -
In badly angulated greenstick fractures,
complete and displaced fractures or comminuted fractures, a provisional
reduction is attempted under fentanyl/midazolem, or nitrous oxide
conscious sedation in the emergency department, followed by application
of a sugar tong splint. -
The reduction is achieved by first
obtaining gentle traction through the fingers (manually or in finger
traps), followed by exaggeration of the deforming force under traction
to clear any intervening periosteum and reestablish length. -
The arm is then forcefully manipulated to achieve reduction.
-
A three-point mold is placed into the
splint with a good anteroposterior interosseous squeeze. Postreduction
radiographs are always obtained to check the position of the reduction
and to document the institution of treatment.
fracture in order to obtain the reduction. Another benefit of
completing a greenstick fracture is to avoid the stress of refracture.
under 10 years of age, angulations up to 20 degrees, rotation up to 45
degrees, and shortening up to 1 cm will heal without clinical or
functional sequelae (Table 12.4-1). This is
because of the significant amount of longitudinal growth of the distal
forearm, which varies between 75% to 81%. This allows overgrowth to
occur at a rate of almost 6 mm on average in length and 0.8 degrees of
angulation per month of remaining growth. Beyond these limits, and in
more mature individuals, the amount of correction is limited and
malalignment may not completely remodel. This may eventually lead to
limitations of motion. Thus, in children over age 10 or those with less
than 2 years of growth remaining, the acceptable range of angulation is
less than 10 degrees and that of malrotation is less than 30 degrees.
unstable, partially because of deforming muscular forces, and partially
because of the muscle bulk that limits direct molding of the fracture
fragments. Fractures associated with dislocations of the radial head
need complete reduction and immobilization in supination. Closer
monitoring of these fractures is necessary since less angulation, less
rotation, and no joint dislocation can be accepted without clinical
sequelae. As in the older child with more distal fractures, the limits
of acceptability of proximal forearm fractures include 10 degrees of
angulation, 30 degrees of rotation, and complete joint reduction.
obvious fracturing, but there is an increase in the natural bow of the
forearm. These “fractures” need to be manipulated in the operating room
under pressure to restore the natural alignment as plastic deformation
will not remodel over time.
This is due to their thicker periosteum, which may help contain
fractures and limit their displacement as well as enhance the speed of
healing and remodeling. The remodeling potential of the younger child
allows acceptance of a greater degree of displacement, but not all
perfectly aligned fractures will result in normal functioning limbs.
Although Fuller and colleagues demonstrated a direct correlation with
malrotation and the resulting range of motion, others have noted minor
to moderate losses of rotation even in perfectly aligned limbs. In
these cases, it is hypothesized that contractures of the soft tissue or
interosseous membranes occurred, either from the injury or the
subsequent immobilization (especially in pronation where the fibers are
tightened).
anatomic alignment as possible, with acceptance of only what has been
previously outlined as these are well supported by the literature. As
soon as fractures are radiographically healed, gentle range of motion
should be initiated. Refracture at the site of previous injury may
occur
in
up to 30% of patients within the first 6 months of healing. This is
most likely due to weakened bone structure from incomplete
corticalization of a diaphyseal fracture. Patients and parents need to
be forewarned at the time of cast removal that this potential
complication may occur and early protective mobilization, such as a
forearm splint, may be beneficial.
|
TABLE 12.4-1 CLINICAL AND RADIOGRAPHIC CRITERIA FOR TREATMENT OF PEDIATRIC FOREARM FRACTURES
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
TABLE 12.4-2 OPERATIVE OPTIONS FOR THE TREATMENT OF FOREARM FRACTURES
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||
-
Open fractures
-
Neurovascularly compromised fractures
-
Compartment syndrome of the forearm
-
Displaced fractures in patients nearing skeletal maturity
-
Floating elbow (ipsilateral supracondylar elbow fracture)
-
Unstable fracture losing alignment on follow-up
-
Follow-up closely.
-
Pins are removed when the bone appears healed on radiographs.
-
After surgery, the arm is usually in a
long cast for 4 to 6 weeks, followed by initiation of range-of-motion,
depending on the type of fracture.
C, Zaleske D, Erhlich M. Analyzing forearm fractures in children. The
more subtle signs of impending problems. CORR 1984;188:40-53.
T, Strub W, Foad S, Mehlman C, Crawford A. Reduction vs. remodeling in
pediatric distal forearm fractures: a preliminary cost analysis. J
Pediatr Orthop B 2003;12(2):109-15.
KS. Remodeling after distal forearm fractures in children. The effects
of residual angulation on spatial orientation of the epiphyseal plates.
Acta Orthop Scand 1979;50:527-546.
H, Nilsson B, Willner S. Correction with growth following diaphyseal
forearm fractures. Acta Orthop Scand 1976;47: 299-303.
W, Clegg J. Intraoperative wedging of casts: correction of residual
angulation after manipulation. J Pediatr Orthop 1995;15: 826-829.
A, Tredwell S, Mackenzie W. Factors affecting fracture position at cast
removal after pediatric forearm fracture. J Pediatr Orthop
1997;17:332-336.
A, Tredwell S, Mackenzie W, et al. Accurate prediction of outcome after
pediatric forearm fracture. J Pediatr Orthop 1994;14: 200-206.
children. They account for 25% of all pediatric fractures, and many go
unrecognized. Hand fractures have a bimodal distribution. The major
peak occurs in adolescents due to sports injuries. There is a smaller
peak in toddlers due to crush injuries of the distal phalanx. Anytime a
child or adolescent “jams” a finger; this usually results in a
fracture. This is evident by swelling, ecchymoses, and tenderness over
the bone that lasts for 2 to 3 weeks. Fortunately, most of these
fractures have a benign course and heal uneventfully. Most will be
nondisplaced fractures. However, there are specific fractures that
without proper treatment can lead to certain morbidity. This chapter
discusses how to treat simple fractures, as well as how to identify
more serious injuries and understand their treatments.
-
Carpal fractures occur in children less commonly than in adults and may be difficult to diagnose due to a lack of ossification.
-
Many of these fractures result from axial loading with the wrist dorsiflexed or from direct impact.
-
The scaphoid is the most commonly fractured carpal bone, with a peak incidence around 15 years of age.
-
A direct impact mechanism usually causes a distal pole fracture.
-
□ More common in younger children
-
□ Rarely displaced; usually heal without complications
-
-
In adolescents, hyperdorsiflexion
injuries cause the more adultlike waist fracture, carrying an increased
risk for nonunion and avascular necrosis.
-
Scaphoid fractures are frequently occult injuries with normal initial radiographs.
-
Radiographs should include anteroposterior, lateral, scaphoid, and pronated oblique views.
-
Mid-body or “waist” fractures can usually be seen on all views.
-
Pronated oblique radiograph is valuable for distal fractures.
-
When an occult fracture is suspected, magnetic resonance imaging or computed tomography may be useful.
-
Tenderness over the scaphoid and normal radiographs indicate treatment with a short arm-thumb spica cast.
-
□ At 3 weeks, anteroposterior, lateral, and scaphoid views of the wrist are repeated.
-
□ In children with normal clinical and radiographic exams, casting is discontinued.
-
-
If a fracture exists, the child will still be tender and radiographs may be positive.
-
□ These children are treated for 3 more weeks in a cast.
-
-
Nondisplaced fractures, obvious on radiographs, are treated in a short arm-thumb spica cast for 6 weeks and then reassessed.
-
Displaced fractures are treated operatively, as they are in adults.
-
Any child with a scaphoid fracture should
have a final radiographic exam 3 to 6 months after the injury is healed
to avoid undetected late displacement.
-
Other carpal fractures occur, but are rare and are usually a result of direct impact.
-
The most common is the hook of the hamate fracture, which is treated with immobilization in a short arm cast.
-
Rare painful nonunions may be treated with excision.
-
Ligamentous carpal injuries are unusual in young children and occur rarely in adolescents via a dorsiflexion loading mechanism.
-
The most common injury is a scapholunate ligament sprain, diagnosed by tenderness in this region.
-
Without displacement, these patients are treated in a short arm-thumb spica cast for 4 to 6 weeks.
-
Injuries with carpal displacement or instability are rare and should be treated as in adults.
-
Metacarpal fractures are common in
children and most occur through the metacarpal neck proximal to the
physis. Fractures through the shaft and base also occur.
-
These fractures can be treated in a gutter splint or short arm cast for 3 to 4 weeks.
-
If displaced, closed reduction with longitudinal traction and downward pressure is performed.
-
Many of these will be unstable and
require pin fixation across the base of the adjacent metacarpals or
down the shaft of the involved metacarpal. -
Open reduction is rarely needed.
-
Classified as A through D (Fig. 12.5-1).
-
□ Type A fractures are usually treated with closed reduction and immobilization in a thumb spica cast or splint.
-
□ Type B and C fractures are
Salter-Harris type II fractures and are treated with closed reduction
and immobilization. Unstable reductions may require pin fixation. -
□ Open reduction is sometimes needed, especially in type C fractures, as the medial fragment may buttonhole the periosteum.
-
□ Type D fractures are more of an adult injury and when displaced require open reduction and internal fixation.
-
-
Occur mostly in older children.
-
A twist, bend, or crush can result in an oblique or spiral fracture pattern.
-
Careful clinical examination of alignment is important; special attention should be paid to rotational malalignment.
-
In the absence of rotational
malalignment, most of these can be handled by closed reduction and
splinting with pressure on the apex and a three-point mold. -
If the reduction is unstable, pinning will hold the reduction.
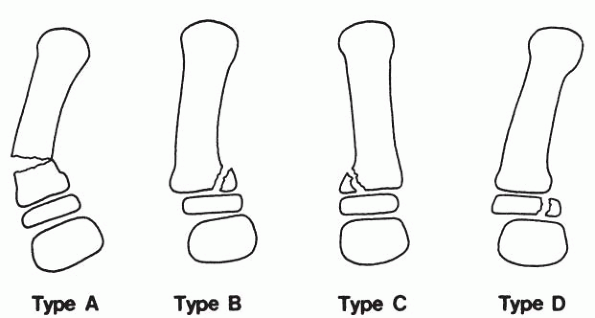 Figure 12.5-1
Figure 12.5-1
Classification of thumb metacarpal fractures. Type A is a metaphyseal
fracture. Types B and C are Salter-Harris type II physeal fractures
with lateral (type B) or medial (type C) angulation. Type D is a
Salter-Harris type II fracture (pediatric Bennett fracture). (Adapted
from Graham TJ, Waters PM. Fractures and dislocations of the hand and
carpus in children. In: Beaty JH, Kasser JR, eds. Rockwood and Wilkins’
fractures in children, 5th ed. Philadelphia: Lippincott Williams &
Wilkins, 2001:269-379.) -
Any significant angulation will leave a bump on the back of the hand, but is of little functional significance.
-
After adequate reduction, most metacarpal shaft fractures require 3 to 4 weeks of immobilization followed by only motion.
-
Common in children and usually result from a direct blow or punch.
-
Frequently volarly angulated.
-
Closed reduction with flexion of the
metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints to
90 degrees is usually successful. -
A gutter splint with 60 to 90 degrees of MCP joint flexion and the PIP joint in extension is applied.
-
Angulation of less than 40 degrees is well tolerated in the fourth and fifth digits
-
□ No more than 20 degrees of angulation should be accepted in the second or third digits.
-
-
Occasionally an unstable fracture will require pin fixation.
-
Intraarticular head fractures are rare but require open reduction and pin fixation when displaced.
-
Some remodeling will occur in younger children with open physes.
-
Common in children, can involve any area.
-
Salter-Harris I and II fractures and metaphyseal fractures at the bases of the proximal and middle phalanges are common.
-
Fractures of the proximal phalanx are most common and result from axial loading, hyperextension, or a twisting mechanism.
-
Nondisplaced fractures are splinted in a position of comfort for 2 to 3 weeks.
-
Fractures with more than 10 degrees of
angulation in the coronal plane usually appear deviated clinically and
reduction is recommended. -
Angulation of up to 25 degrees in the plane of motion in a digit with open physes is well tolerated and will usually remodel.
-
Digital block with longitudinal traction and a reversal of the mechanism will reduce displaced fractures.
-
Coronal malalignment may require a
fulcrum or bolster in the web space of the finger and is incorporated
into the splint for 2 to 3 weeks. -
In the event of an unstable fracture, pinning with smooth Kirschner wires (K-wires) will achieve stability.
-
Need for open reduction is rare.
-
Can occur from bending, hyperextension, rotation, or crush injuries.P.133
![]() Figure 12.5-2 (A) Irreducible proximal phalangeal shaft fracture. (B) After open reduction and internal fixation through a dorsal approach.
Figure 12.5-2 (A) Irreducible proximal phalangeal shaft fracture. (B) After open reduction and internal fixation through a dorsal approach. -
Fractures with more than 10 degrees of
coronal deformity, 20 degrees of sagittal deformity, or any significant
rotational deformity should be reduced.-
□ Remember to check for rotational deformity. Clinically, it will not be visible on x-ray.
-
-
Flexion at the PIP joint is sometimes
needed for proximal phalanx fractures and extension is usually used for
middle phalanx fractures.-
□ The fracture force is reversed. If the reduction is unstable, percutaneous pinning is required.
-
-
If closed reduction is not possible, open reduction is performed.
-
This occurs in spiral fractures with rotational displacement and oblique fractures with shortening.
-
□ The dorsal approach is preferred, though some use a midlateral approach.
-
□ Fixation can be with smooth pins;
however, mini-fragment screws afford earlier mobilization and improved
stability in older children (Fig. 12.5-2). -
□ Fractures undergoing reduction should be splinted for 3 weeks.
-
□ As soon as callus is seen, the pins are removed and motion is begun.
-
-
Occur at the proximal, middle, and distal phalanx.
-
In the proximal phalanx, they are the result of a bending motion.
-
□ The collateral ligament is avulsed with a fragment of bone.
-
□ This results in a Salter-Harris III or IV fracture.
-
□ May involve a significant part of the articular surface.
-
□ If the fracture is nondisplaced, treatment is conservative with splinting for 3 to 4 weeks.
-
□ If more than 25% of the joint is involved and there is more than 2.0 mm of displacement, open reduction is recommended.
-
□ Any widely displaced fracture should be reduced.
-
□ Fixation is with smooth pins in younger children.
-
□ In older children, mini-fragment screws may be used.
-
-
Fractures in the middle and distal
phalanges are usually a result of an avulsion of the central slip of
the extensor at the base of the middle phalanx and the terminal
extensor over the distal phalanx.-
□ Rarely these avulsions will present as a Salter-Harris I or II fracture.
-
-
There are four mallet finger equivalent fractures (Fig. 12.5-3).
-
□ These occur from forced flexion, usually during a ball sport.
-
□ A terminal extensor avulsion leads to a mallet finger.
-
□ Closed reduction is attempted with longitudinal traction and pressure over the displaced fragment.
-
□ If successful the finger can be splinted in extension for 3 weeks.
-
□ If significant displacement persists, greater than 2 mm, open reduction should be performed.
-
-
-
Displaced fragments of greater than 25% of the joint surface area may lead to instability in addition to incongruity.
-
In the distal phalanx, the fracture is approached dorsally.P.134
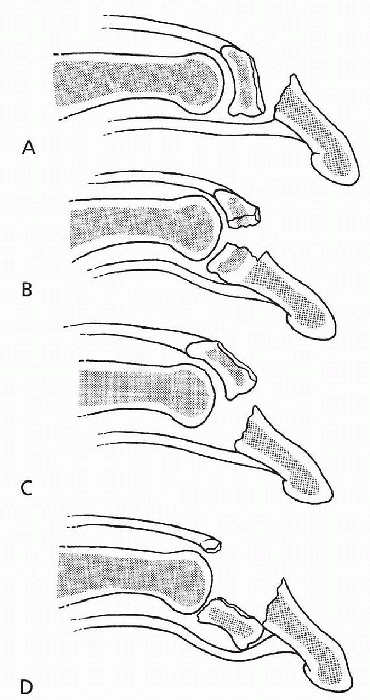 Figure 12.5-3
Figure 12.5-3
Mallet equivalent fractures. (Adapted from Graham TJ, Waters PM.
Fractures and dislocations of the hand and carpus in children. In:
Beaty JH, Kasser JR, eds. Rockwood and Wilkins’ fractures in children,
5th ed. Philadelphia: Lippincott Williams & Wilkins, 2001:269-379.)-
□ A transverse incision within the distal creases with a proximal and distal limb is useful.
-
□ Avoiding the germinal matrix of the nailbed is important.
-
□ This incision leaves a minimal scar.
-
□ The extensor apparatus will be retracted with the avulsed fragment.
-
□ The fracture is reduced and fixed with K-wires or a pull out suture.
-
□ The distal interphalangeal (DIP) joint is splinted in extension for 3 weeks.
-
□ A smooth pin across the joint can be used to protect the repair.
-
□ At 3 to 4 weeks, the splint is removed to begin motion, but should be left on for all other activities for 6 weeks.
-
□ Prolonged splinting, without motion, will lead to a stiff DIP joint.
-
-
Left displaced and untreated, a central slip avulsion may lead to a boutonniere deformity or incongruity of the joint surface.
-
□ Open reduction of middle phalanx fractures consists of a dorsal approach, incising between the central slip and lateral band.
-
□ If small, the fragment is excised and the tendon is reattached.
-
□ When significant, it is repaired with pins or a mini-fragment screw.
-
-
A flexor digitorum profundus (FDP) avulsion may cause a volar Salter-Harris type III, IV, or simple avulsion fracture.
-
□ These are rare in comparison to the dorsal injuries.
-
□ This is known as a reverse mallet or a jersey finger.
-
□ It is analogous to the adult type 2 or 3 FDP avulsion.
-
□ Repair is with open reduction and a pullout suture or other fixation.
-
□ Treated with open reduction when displaced.
-
-
Fractures through the phalangeal necks of the proximal and middle phalanx are particularly bad actors.
-
□ When nondisplaced, treatment consists of splinting and careful follow-up.
-
□ These heal slowly and may require 4 weeks of immobilization.
-
-
□ When displaced, they are highly unstable.
-
□ Their juxtaposition to the joint and tendency to malrotate cause severe deformity (Fig. 12.5-4).
-
□ Closed reduction and cross-pinning can
be attempted in minimally displaced fractures, but most will require
open reduction and pinning. -
□ It is almost impossible to judge rotation without a direct reduction.
-
□ A dorsal approach used, incising between the central slip and lateral band. Cross-pinning of the fragment with 0.45 K-wires (Fig.12.5-5).
![]() Figure 12.5-4 Angulated middle phalanx condylar neck fracture.P.135
Figure 12.5-4 Angulated middle phalanx condylar neck fracture.P.135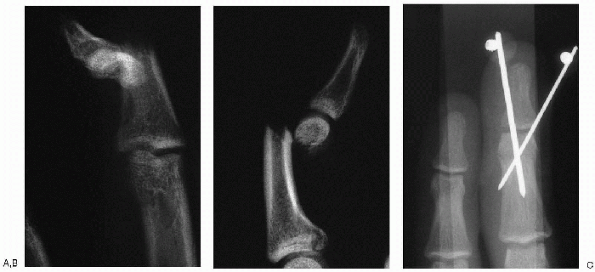 Figure 12.5-5 Anteroposterior (A) and lateral (B) views of a displaced condylar neck fracture. (C) After open reduction and pin fixation through a dorsal approach.
Figure 12.5-5 Anteroposterior (A) and lateral (B) views of a displaced condylar neck fracture. (C) After open reduction and pin fixation through a dorsal approach. -
□ The finger is immobilized for 4 weeks, at which time the pins are removed and motion begun.
-
□ Stiffness is common, necessitating early occupational therapy.
-
-
□ Intraarticular fractures of the distal end of the proximal and middle phalanges are uncommon.
-
□ Except in minimally displaced fractures, open reduction and fixation is required.
-
□ Treatment is similar to condylar neck fractures.
-
□ Fixation is best with mini-fragment screws, which allows for early motion.
-
-
□ Tuft fractures of the distal phalanx
represent more of a soft tissue injury involving the distal pulp of the
finger and the nailbed.-
□ These are usually from a crush mechanism.
-
□ When the nail is avulsed from the fold, the nailbed must be explored and repaired.
-
□ The nail is then sewn back into the fold.
-
□ Some controversy exists about exploring a nailbed due to the presence of hematoma alone.
-
□ The most recent literature suggests
these fingers can be treated with trephination of the hematoma by
placing a hole in the nail. -
□ Outcomes were equal to children undergoing exploration and repair.
-
-
□ The nail is then sewn back into the
eponychial fold. Splinting is of the middle and distal phalanges only
and is discontinued when pain is gone, usually at 2 weeks.
-
JP. Transcarpal injuries associated with distal radial fractures in
children: a series of three cases. J Hand Surg (Br) 1992; 17:311-314.
RL, Dobyns JH, Beabout W, et al. Traumatic instability of the wrist:
diagnosis, classification, and pathomechanics. J Bone Joint Surg (Am)
1972;54:1612-1632.
1% to 2% of all fractures in children. In most cases, these fractures
are the result of high-energy trauma. Identification of a fracture of
the pelvis in a pediatric trauma patient mandates a thorough search for
concomitant, potentially more life-threatening injuries of the brain,
abdominal viscera, and genitourinary system. As opposed to the adult
trauma patient with a pelvic fracture, fatalities rarely occur in
children with pelvic fractures as a direct result of their pelvic
injury, but rather as the result of associated injuries.
or cyclist/motor vehicle accidents, falls from heights, and other
high-energy mechanisms. A subgroup of pelvic injuries—avulsion
fractures—occur during sports activities such as soccer, gymnastics,
and track and field.
 |
|
Figure 12.6-1
Torode and Zieg classification. Type I, avulsion fractures; type II, iliac wing fractures; type III, simple ring fractures (stable pelvic ring); type IV, ring disruption fractures (unstable pelvic ring). (From Canale ST, Beaty JH. Fractures of the pelvis. In: Beaty JH, Kasser JR, eds. Rockwood and Wilkins’ fractures in children, 5th ed. Philadelphia, Lippincott Williams & Wilkins, 2001:883-911.) |
-
Children whose triradiate cartilage is
open most commonly sustain fractures of the pubic rami and iliac wings;
the triradiate cartilage of the acetabulum closes at approximately 14
years of age in boys and 12 years of age in girls.-
□ The elasticity of the ligaments of the
pubic symphysis and the sacroiliac joints, and the plasticity of the
bony pelvis, are most likely responsible for the rare occurrence of
unstable pelvic ring disruptions seen in adults.
-
-
Adolescents approaching skeletal
maturity, whose triradiate cartilage is closed, sustain pelvic injuries
similar to those seen in adults. -
Older children and adolescents are more
likely to require surgical treatment, with morbidity and mortality
related to their pelvic injuries -
Avulsion injuries of the anterior
superior and inferior iliac spines, ilium, and ischium most commonly
occur in adolescent and young adult athletes.
children’s pelvic injuries is not ideal. The Torode and Zieg
classification of pediatric pelvic fractures is the most widely used (Fig. 12.6-1 and Table 12.6-1).
Bucholz and colleagues observed different patterns of physeal
disturbance associated with triradiate cartilage injuries based on the
Salter-Harris classification of these triradiate injuries (Fig. 12.6-2).
|
TABLE 12.6-1 TORODE AND ZIEG CLASSIFICATION OF PELVIC FRACTURES IN CHILDREN
|
||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||
begins with a thorough history of the traumatic events, as well as past
medical and surgical history. The best effort must be made to gather
this information from emergency personnel at the scene of an accident,
emergency room staff, and family members. In a polytraumatized child,
often the pelvic injury is a lower priority. The airway, breathing,
circulation (ABC’s) must be assessed and established as a first
priority. Injuries of the head and spine, chest, and abdominal viscera,
as well as the pelvis, must be carefully evaluated as potential sources
of life-threatening injuries.
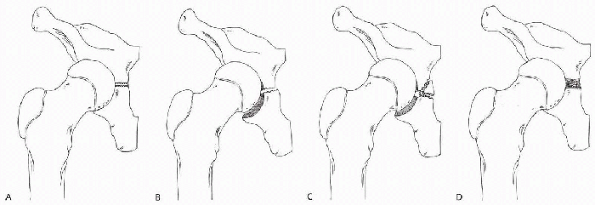 |
|
Figure 12.6-2 Triradiate cartilage injuries. (A) Normal. (B) Salter-Harris type I fracture. (C) Salter-Harris type II fracture. (D)
Salter-Harris type V fracture. Growth disturbance, most commonly seen after type V injuries (compression), results in acetabular dysplasia. (From Scuderi G, Bronson MJ. Triradiate cartilage injury: report of two cases and review of the literature. Clin Orthop 1987;217:179-189.) |
-
Visual inspection of the pelvis and
perineum for lacerations, ecchymosis, hematoma, blood at the urethral
meatus, and vaginal or scrotal injury is indicated. -
The anterior superior iliac spines, iliac crests, sacroiliac joints, and pubic symphysis are palpated.
-
With hands placed on the iliac crests, apply posteriorly directed forces with gentle side-to-side rocking.
-
Pain, crepitus, or excessive mobility is indicative of a potentially serious pelvic injury.
-
Rectal examination is necessary to
identify bony fragments, or a superiorly displaced prostate secondary
to a urethral injury in older males. -
Hip range of motion must be evaluated,
with pain or limits of mobility suggestive of a joint dislocation or
associated acetabular fracture. -
Neurovascular examination of the lower extremities is documented.
-
□ Injuries of the lumbosacral plexus,
femoral and sciatic nerves, as well as vascular injuries, may occur as
the result of severe pelvic trauma.
-
polytraumatized patient is an anteroposterior radiograph of the pelvis
in the emergency room. While this information is rarely necessary to
effectively resuscitate and stabilize the child, early recognition of
an unstable pelvic injury may be critical in the survival of the older
child and adolescent. After the child is initially stabilized, rapid
sequence spiral
computed
tomography (CT) scanning of the pelvis is the most effective method to
fully evaluate the extent of pelvic injury. Often more serious
concomitant injuries of the head and abdomen warrant evaluation by CT
scan. Inclusion of the pelvis in the initial series of imaging studies
allows for a more complete and efficient injury assessment.
pelvis may be useful for preoperative planning. Magnetic resonance
imaging and bone scan have no role in acute evaluation of pelvic
injuries. However, these modalities may be helpful in the analysis of
soft tissue injury, cartilaginous injuries, and occult fractures.
-
Avulsion fractures (type I) are treated
symptomatically with protected weightbearing for 2 to 4 weeks, followed
by a stretching and strengthening program.-
□ Return to sports may be expected within 6 to 8 weeks.
-
-
Fractures of the iliac wing and iliac apophyseal separations (type II) are treated in a similar fashion.
-
Simple ring fractures (type III) are stable fractures of the pelvis with intact posterior structures.
-
□ Cooperative patients without acetabular
involvement may be treated with protected weightbearing with
progression to full weightbearing over a 6-week period. -
□ Bed rest or bed-to-chair activities are indicated for the noncompliant or very young child.
-
□ Type III fractures with nondisplaced
fracture of the acetabulum may be treated with non-weightbearing
ambulation or spica cast immobilization. -
□ Distal femoral skeletal traction may be
useful to improve alignment of minimally displaced fractures or to
prevent premature weightbearing. -
□ Intraarticular and triradiate cartilage displacement greater than 2 mm warrants open reduction and internal fixation.
-
-
Type IV pelvic fractures are unstable ring disruptions.
-
□ A pelvic binder may be used as a temporary measure to assist in resuscitating the hemodynamically unstable child.
-
□ Emergent external fixation is indicated to control hemorrhage and to grossly align and stabilize the pelvis.
-
□ Pelvic arteriography and embolization are indicated if blood loss persists despite external fixation.
-
□ In a hemodynamically stable child,
unstable pelvic disruptions may be treated with bed rest with or
without skeletal traction, or in a spica cast. Progressive
weightbearing and rehabilitation may be started within 6 weeks of
injury. -
□ Open reduction with internal fixation
is indicated for acetabular and triradiate cartilage fractures with
more than 2 mm of displacement. -
□ Reduction and fixation of pelvic ring displacement, beyond the use of external fixation, is rarely indicated in children.
-
□ Displacement of up to 2 cm is
acceptable, since rapid healing and significant remodeling of
extraarticular fractures of the pelvis can be expected in children with
more than 2 years of growth remaining.
-
complications. Nonunion and ligamentous instability of pediatric pelvic
ring injuries do not occur. Malunion of the pelvic ring is
well-tolerated because of the remodeling potential of the pediatric
pelvis; leg length inequality may occur after an unstable fracture if
residual vertical displacement of the hemipelvis exceeds 2 cm.
Fractures involving the triradiate cartilage, especially in children
younger than 10 years of age, may lead to growth disturbance of the
acetabulum secondary to premature physeal closure. Manifestations of
this abnormal growth include acetabular dysplasia, hip subluxation, and
hip joint incongruity. Displaced acetabular fractures, despite anatomic
realignment, may develop premature degenerative joint disease of the
hip. Avascular necrosis of the femoral head may develop after fractures
of the acetabulum associated with hip dislocation.
include myositis ossificans and permanent neurologic deficits of the
lower extremity secondary to associated lumbosacral plexus, sciatic,
and femoral nerve injuries. Death, as direct result of hemorrhage due
to pelvic fracture, occurs in less than 0.5% of children. Nonskeletal
injuries occurring in association with pelvic fractures in children,
however, result in death of the child 10 times more frequently.
ST, Beaty JH. Fractures of the pelvis. In: Beaty JH, Kasser JR, eds.
Rockwood and Wilkins’ fractures in children, 5th ed. Philadelphia:
Lippincott Williams & Wilkins, 2001:883-911
RC Jr, Bensard DD, Moore EE, et al. Pelvic fracture geometry predicts
risk of life-threatening hemorrhage in children. J Trauma
1993;35:423-429.
JS, Flynn, JM. Changing patterns of pediatric pelvic fractures with
skeletal maturation: implications for classification and management. J
Pediatr Orthop 2002;22:22-26.
aspects from those in adults. The bone is generally stronger and
therefore significant trauma is usually required for fracture. The
periosteum is thicker, thus making it possible for a fracture to be
nondisplaced and relatively stable. This, however, does not protect the
tendency for coxa vara if treated without fixation. The presence of the
proximal femoral physis provides a weakened point for potential
fracture. Damage to the physis can cause subsequent deformity of growth
of the proximal femur. This group of fractures, although relatively
rare, provides a significant challenge to the treating orthopedist, due
to the frequency of potential complications including avascular
necrosis, coxa vara, nonunion, premature physeal closure, and
subsequent leg length discrepancy.
severe trauma. Causes include motor vehicle accidents, pedestrian or
cyclist/motor vehicle accidents, falls from heights, and child abuse.
Occasionally, fractures may occur through pathologic bone such as a
cyst or fibrous dysplasia.
-
Type II fractures are most common—45% to 50%
-
Type III—approximately 35%
-
Type IV—12%
-
Type I—8%
|
TABLE 12.7-1 HIP INJURY CLASSIFICATION SYSTEM OF DELBET
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
fractures involves the blood supply to the capital femoral epiphysis
and the manner in which complications are caused by its disruption. The
blood supply to the femoral head from birth to 2 to 3 years of age
comes from the medial and lateral circumflex vessels. This anastomotic
ring courses along the intertrochanteric notch and is extracapsular.
Transphyseal vessels exist up to 18 months of age.
branches of the medial circumflex artery, and the posterosuperior and
posteroinferior arteries, which course along the femoral neck and are
vulnerable to injury from fracture. The posterosuperior artery supplies
the lateral and anterior head, and the posteroinferior artery supplies
the medial head.
accounts for the frequent occurrence of avascular necrosis after fracture of the hip in children.
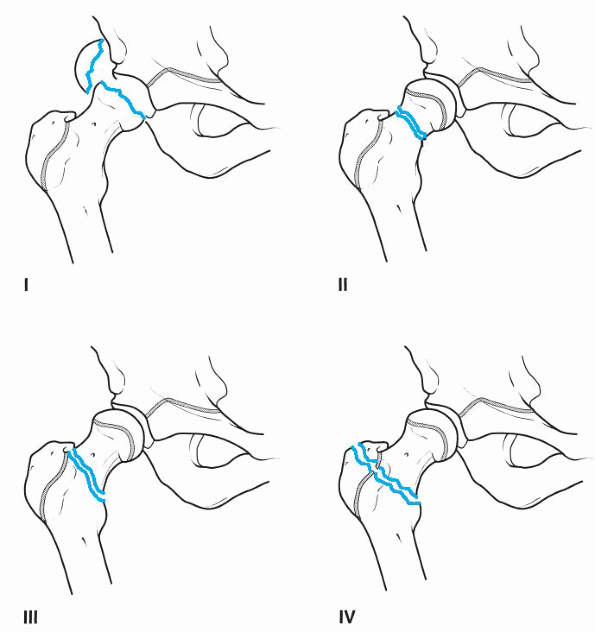 |
|
Figure 12.7-1
Delbet classification for proximal femur fractures. Type I is a transepiphyseal fracture. Type II is a transcervical fracture. Type III is a cervicotrochanteric fracture (basicervical). Type IV is an intertrochanteric fracture. (From Blasier RD, Hughes LO. Fractures and traumatic dislocations of the hip in children. In: Beaty JH, Kasser JR, eds. Rockwood and Wilkins’ fractures in children, 5th ed. Philadelphia: Lippincott Williams & Wilkins, 2001:913-939.) |
significant trauma, a thorough physical and radiologic exam is
necessary to rule out other injuries. With displaced fractures, the leg
is usually shortened and externally rotated. A thorough motor, sensory,
and vascular exam of the extremity should be performed.
Comparison radiographs may be helpful. Magnetic resonance imaging (MRI)
has become increasingly useful to confirm the presence of a fracture.
Also, a hip aspiration can be performed with a bloody aspirate being
diagnostic.
diagnose and often is associated with child abuse. Aspiration,
ultrasound, or MRI also can be useful to confirm the diagnosis.
-
Accurate reduction must be obtained. If closed reduction fails, then open reduction should be performed.
-
Stable fixation must be obtained.
-
□ Fracture stability takes precedence over physis sparing.
-
-
Type I, II, and III fractures should be taken to the operating room emergently, preferably in less than 12 to 24 hours.
-
Hip decompression should be performed with either open arthrotomy or aspiration for all type I, II, and III injuries.
-
Spica cast should be used in younger children or if necessary to supplement internal fixation.
-
Less than 2.5 years of age: closed
reduction and spica cast if a stable reduction is obtained. Insertion
of smooth pins if unstable -
Less than 9 years of age: closed or open reduction and smooth pins with hip decompression. Spica cast immediately
-
More than 9 years of age: closed or open reduction and screw fixation with hip decompression
dislocation of the epiphysis. If the femoral head is dislocated, an
attempt at closed reduction can be performed. If unsuccessful, this
should be followed by immediate open reduction and pinning. The open
reduction is performed on the side of the dislocated head [i.e.,
posterior approach of a posterior dislocation and an anterior
(Watson-Jones) approach for an anterior dislocation].
develop avascular necrosis and premature physeal closure. Avascular
necrosis is less often a problem in the under 2.5-year-old age group,
since these are usually not associated with a dislocation, and
remodeling of a severe varus malunion will occur if a growth arrest
does not develop.
-
Nondisplaced: screw fixation short of the physis if possible. Perform hip decompression.
-
Displaced: closed or open reduction
(anterior Watson-Jones) and screw fixation short of the physis. Hip
decompression should also be performed.
-
Nondisplaced: screw fixation short of the physis and hip decompression
-
Displaced: closed or open reduction (anterior Watson-Jones) with screw fixation short of the physis and hip decompression
-
Nondisplaced:
-
□ Children under 8 years of age may be treated with spica casting.
-
-
Displaced:
-
□ Children under 8 years of age can be
treated in 90-90 traction for 2 to 3 weeks followed by an abduction
spica cast. Most are preferably treated with closed or open reduction,
internal fixation, and spica casting. -
□ For children older than 8 years of age,
treatment should be similar to that of an adult, with open reduction
and internal fixation.
-
complication of pediatric hip fractures. The incidence of avascular
necrosis is directly related to the amount of fracture displacement and
type of fracture.
-
Type I fractures with associated
dislocation have an 80% to 100% incidence, whereas without dislocation,
the incidence is less than 25%. -
Displaced type II fractures—40% to 50% incidence
-
Displaced type III fractures—approximately 25%
-
Type IV fractures—avascular necrosis occurs rarely
as early as 6 weeks after injury and usually develops by 1 year after
injury. The risk of avascular necrosis can be markedly decreased in
displaced fractures by immediate reduction in less than 24 hours, along
with stable internal fixation and evacuation of the intracapsular
hematoma. Recent studies show rates of 0% to 8% incidence of avascular
necrosis with displaced fractures using this approach. Once avascular
necrosis occurs there is no proven effective treatment. The internal
fixation should be removed once the fracture heals.
|
TABLE 12.7-2 THREE TYPES OF AVASCULAR NECROSIS ACCORDING TO RATLIFF
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
eliminated with the routine use of stable internal fixation and spica
casting. However, it may occur as a result of asymmetric physeal
closure. This can be corrected by subtrochanteric valgus osteotomy.
necrosis or internal fixation crossing the physis. The proximal femoral
physis provides 13% of the length of the leg. Therefore, growth arrest
usually does not create significant (more than 2 cm) shortening except
in very young children.
be as high as 10%. Current recommended treatment has reduced this rate
in most studies to 0% to 4%. If nonunion occurs, it should be treated
as soon as it is recognized and usually by subtrochanteric valgus
osteotomy and bone grafting, with internal fixation and spica casting.
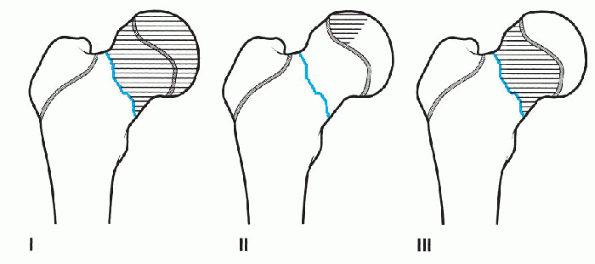 |
|
Figure 12.7-2
Three types of avascular necrosis. (Adapted from Ratliff AHC. Fractures of the neck of the femur in children. J Bone Joint Surg 1962;44B:528.) |
was always associated with avascular necrosis. Three of seven had pin
penetration in the joint. All had a poor result.
but less commonly than adults. All reported cases have involved the
femoral neck.
-
Fatigue fracture: usually a result of overuse in children who have rapidly increased their activities.
-
Insufficiency fractures: these occur in deficient bone in children with underlying disease processes.
with callus present along the inferior neck. A bone scan may be needed
for diagnosis if there is no apparent radiographic abnormality. These
can be treated with non-weightbearing on crutches or in a cast. If the
fracture site widens or is displaced initially, then internal fixation
is necessary.
more frequently than hip fractures and with less severe trauma. Prompt
knowledgeable treatment is important to avoid potentially devastating
complications. Specific treatment guidelines should be followed, thus
avoiding the pitfalls of treating this rare injury.
under 10 years of age from relatively minor trauma, such as a fall.
This is thought to be due to the increased amount of cartilage in the
joint, and the more generalized ligamentous laxity present in children.
For children older than 10 years of age, a more forceful injury such as
that sustained in a
motor vehicle accident or from contact sports is more likely.
being posterior. These occur bilaterally 1% of the time. An associated
fracture about the hip occurs approximately 15% to 20% of the time and
is less frequent in younger children.
has been published. Each hip is described by its direction of
dislocation:
-
Anterior: the femoral head lies medial to the acetabulum.
-
Anteroinferior: the femoral head lies in the region of the obturator foramen.
-
Inferior: the femoral head lies inferior to the acetabulum and lateral to the ischial tuberosity.
-
Posterior: the femoral head lies superior and lateral to the acetabulum.
minor fall to a major high-energy accident. Approximately 65% are due
to lower velocity injuries. Complaints of groin and hip pain will be
evident.
to determine associated injuries. An exam of the position of the limb
will usually indicate the direction of dislocation. The leg is flexed,
adducted, and internally rotated with a posterior dislocation, or
extended, abducted, and externally rotated with an anterior
dislocation. With an inferior dislocation, the hip is hyperflexed. A
thorough neurologic examination of the lower extremity is mandatory,
since sciatic nerve injury occasionally occurs. Pulses should be
palpated, since femoral artery injuries have been reported. An
associated femoral fracture may cause the lower extremity to be
externally rotated.
pelvis x-ray. The entire involved femur should be imaged to exclude
fracture. Careful viewing of the hip x-rays should occur and further
films taken, if necessary, to rule out femoral head, acetabular,
femoral neck, or transphyseal fractures. Judet (45-degree oblique)
views may help to delineate a suspected acetabular fracture.
Prereduction computed tomography (CT) scan may also be useful if
fractures are suspected about the femoral head and acetabulum, as long
as this doesn’t significantly delay reduction.
the first 6 hours following injury to decrease the likelihood of
avascular necrosis. An initial attempt under conscious sedation can be
performed in the emergency department. If this fails, the next attempt
should be performed under general anesthesia in the operating room. A
posterior dislocation is reduced with the hip and knee flexed with
countertraction to the pelvis applied by an assistant. An anterior
dislocation is reduced with the hip extended and the knee flexed. If,
after several attempts, reduction cannot be achieved, an open reduction
should be performed. Failed reduction can occur secondary to interposed
capsule, inverted labrum, and osteocartilagenous fragments. An anterior
dislocation should be opened anteriorly and posterior dislocations
should be opened posteriorly.
should be performed prior to reduction. If the femoral neck fracture is
displaced, open reduction is performed.
assess symmetry of the hip joints. If the joint spaces are not
symmetric following reduction, a CT scan should be performed. If there
is evidence of interposed soft tissue or bony fragments, an open
reduction with removal of the interposed tissue should be performed.
initially by 1 to 2 weeks of skeletal traction. If this fails, open
reduction is indicated.
children under 8 years of age and are rare. The first recurrence should
be treated with closed reduction and spica casting. Further recurrences
should be treated with an open reduction, capsular repair, and spica
casting.
would recommend a spica cast for 6 weeks after reduction in children
less than 6 to 8 years of age. A 6-week period of protected
weightbearing is recommended in older children.
in 95%. Complications include avascular necrosis, sciatic nerve injury, recurrent dislocations, and osteoarthritis.
greater than 6 hours. The incidence ranges from 5% to 58% with most
estimates between 8% and 10%. The risk of avascular necrosis is also
related to the severity of the injury and age greater than 5 years.
This can usually be detected by 6 months after injury, but children
should be followed for up to 4 years.
the time and is usually a transient neuropraxia. Osteoarthritis is
usually associated with the development of avascular necrosis.
ST, Bourland WL. Fracture of the neck and intertrochanteric region of
the femur in children. J Bone Joint Surg (Br) 1977;59: 431-443.
JM, Wong KL, Yeh GL, et al. Displaced fractures of the hip in children:
management by early operation and immobilisation in a hip spica cast. J
Bone Joint Surg (Br) 2002;84:108-112.
CT, Hubbard GW, Crawford AH, et al. Traumatic hip dislocation in
children: long-term follow-up of 42 children. Clin Orthop Rel Res
2000;376: 68-79.
GPK, Cole WG. Effect of early hip decompression on the frequency of
avascular necrosis in children with fractures of the neck of the femur.
Injury 1996;27:419-421.
Pierre P, Staheli LT, Smith JB, et al. Femoral neck stress fractures in
children and adolescents. J Pediatr Orthop 1995;15:470-473.
usually result from moderate to high-energy injury. Fractures after
trivial trauma should prompt a search for weakened bone. Nonoperative
treatment methods are tried and true, but may be best suited for young
children who are unable to walk with crutches. Operative stabilization
is best suited for those who can be taught to ambulate without bearing
weight. The prognosis for healing is excellent. Some overgrowth is to
be expected and should be considered in the treatment plan.
Overtreatment should be avoided.
load, twisting force, three-point bend, or a direct blow. Motor vehicle
accidents, recreational vehicle accidents, sports injuries, and falls
are common causes. Rarely stress fractures or pathologic bone lesions
may progress to overt fracture.
2,000 children sustains a femur fracture each year. Up to 40% of boys
and 25% of girls sustain a femur fracture in childhood.
elastically recoil. Larger amounts of applied energy will cause the
bone to fracture. The more energy applied to the bone, the more
comminution and soft tissue disruption should be expected. Muscles that
span the length of the thigh will tend to shorten the fractured femur.
For this reason, traction—either skeletal or skin—is often applied to
prevent shortening prior to definitive management. These fractures
always heal unless open or operated. Hyperemic overgrowth is to be
expected and should be considered in the treatment plan.
-
Open fracture
-
Closed fracture
-
Polytrauma
-
Isolated injury
-
Stable—not prone to shorteningShort oblique fractureTransverse fracture
-
Unstable—prone to shorteningComminutedLong obliqueSegmental
-
A history of significant trauma is usual.
-
The diagnosis is usually obvious in displaced fractures.
-
Undisplaced fractures occur. Get an x-ray after a history of significant injury.
-
Look for associated injuries.
-
Swelling and deformity are immediate findings. Ecchymosis occurs later.
-
Tense swelling or unremitting pain should
prompt compartment pressure measurement. Thigh compartment syndrome is
rare, but significant. -
Check and document pulses. Vascular injury is rare.
-
Check and document distal nerve status.
Nerve palsy is presumed to be due to treatment unless clearly
documented before treatment. -
Look for associated injuries in relation
to the history of injury. Check the hip after an axial loading injury.
Check the knee after a direct blow to the limb.
-
Make sure the hip and knee joints are visible.
-
Look for undisplaced (ghost) fracture lines which may affect choice of fixation.
![]() Algorithm 12.8-1 Treatment decision algorithm for femur fractures.
Algorithm 12.8-1 Treatment decision algorithm for femur fractures. -
If there is considerable comminution or
bone loss, an x-ray of the uninjured femur will provide an estimate of
original bone length. -
If intramedullary fixation is contemplated, the size of the canal and bone length should be estimated.
-
Patient age is important:
-
□ Patients under 6 years of age should generally be treated with a spica cast as the fractures tend to heal quickly
-
□ Children older than 6 years will benefit from fixation of the femur, which allows ambulation with crutches.
-
-
The presence of growth plates mitigates against treatment with a standard reamed nail placed through the piriform fossa.
-
□ Damage to the ascending vessels of the
femoral neck may cause avascular necrosis, for which there is no
satisfactory treatment. -
□ Skeletally mature patients can be treated with a standard, reamed locked nail.
-
-
The fracture pattern is important.
-
□ Fractures prone to shortening due to
comminution or segmentation should be treated with an external fixator
or locked nail to maintain length.
-
-
Short oblique or transverse fractures are excellent candidates for flexible nails.
-
Femur fractures in polytrauma patients
will benefit from stabilization to facilitate patient care and mobility
or to permit wound or skin care.
-
Casting is the mainstay of treatment for the young.
-
Reduction and casting are performed under sedation or anesthesia
-
Positive piston test (fracture can be
overlapped more than 2.5 cm) indicates preoperative traction until
sticky to prevent shortening in cast. -
The cast can be wedged up to 1 to 2 weeks after application to correct angulation.
-
Two weeks is long enough to heal in infants. Healing takes up to 6 weeks in older children.
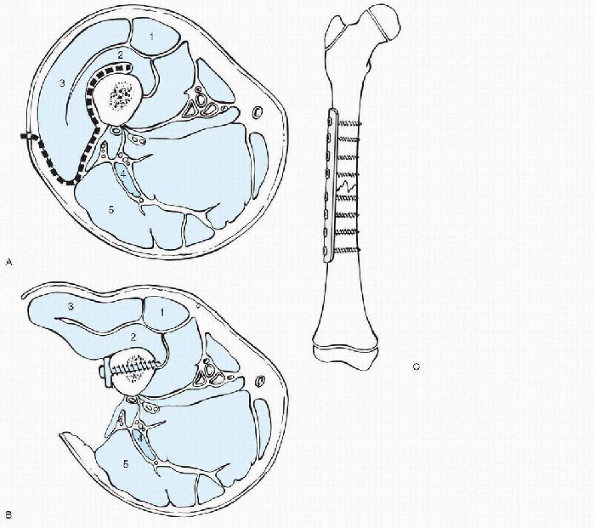 |
|
Figure 12.8-1 Lateral approach to the femur for open reduction and internal fixation. 1, rectus femoris; 2, vastus intermedius; 3, vastus lateralis; 4, sciatic nerve; 5, biceps femoris (long head). (A) A direct lateral skin incision is made. The fascia is sharply incised. Vastus lateralis muscle (3) will be elevated off the intramuscular membrane. (B) With the vastus lateralis elevated, a plate can easily be placed along the lateral femoral cortex. (C)
The plate should span the fracture site and screws should engage six to eight cortices on either side of the fracture to provide adequate purchase. |
-
Safe and effective
-
Prolonged recumbency is a drawback.
-
Skin traction is useful for young
children. Larger children will benefit from a distal femoral traction
pin as the skin will not tolerate large shear forces from skin traction. -
Periodic x-rays needed to check alignment and length. Make corrections.
-
Traction is maintained until fracture is sticky. Spica cast is then applied and maintained until healing.
-
Open reduction and internal fixation with plate and screws (Fig. 12.8-1):
-
□ Relatively safe and effective
-
□ Easily placed by direct lateral approach, elevating the vastus lateralis.P.146
![]() Figure 12.8-2 (A) Fixator pin placement. Placing pins too close to the fracture (left)
Figure 12.8-2 (A) Fixator pin placement. Placing pins too close to the fracture (left)
provides poor control of fracture alignment. Pins in diaphyseal bone
will act as stress risers. Try to limit the number of diaphyseal pins.
Keeping the pins spread out (right) will
provide better mechanical advantage in controlling fracture alignment.
Try to place the proximal pin as proximal as possible and the distal
pin as distal as possible without violating the physes. The
intermediate pins should be close to but not violate the fracture site.
(B) Cross-section of proximal thigh. 1, tensor fascia lata; 2, vastus lateralis; 3, femoral neck; 4, gluteus maximus; 5, ischium; 6,
pubis. The most proximal pin should be in the intertrochanteric region,
which is largely cancellous bone. Cancellous bone is less likely to
fracture through pin tracts than is cortical bone. Because there is
considerable motion of the soft tissues over the greater trochanter,
some irritation is to be expected at this pin tract. (C) Cross-section of midthigh. 1, rectus femoris; 2, vastus intermedius; 3, vastus lateralis; 4, sciatic nerve; 5,
biceps femoris (long head). The diaphyseal pins will be in cortical
bone. Here, they have significant stress riser effect. There will
always be a risk of fracture through a pin tract until the pin has been
removed and the hole refills with bone. The pins will transfix the
vastus lateralis muscle. Few children will want to bend the knee as
long as these pins are in place. (D) Cross-section of distal thigh, just above the distal femoral epiphysis. 1, quadriceps tendon; 2, suprapatellar pouch; 3, vastus lateralis; 4,
biceps femoris. The most distal fixator pin should be in metaphyseal
bone. Fracture through a pin tract here is virtually unheard of. The
pin will transfix the iliotibial band, thereby precluding painless knee
flexion. -
□ Requires a large incision and surgical dissection.
-
□ There are stress risers while the hardware is in place and after removal.
-
□ May be a good choice for patients who cannot be placed on a fracture table or subject to vigorous manipulation.
-
□ Requires non-weightbearing until fracture callus is seen.
P.147 -
-
External fixation (Fig. 12.8-2):
-
□ Usually quite effective; there is occasional delayed healing or refracture.
-
□ Pin tracts require daily cleansing and still may drain or become infected.
-
□ Pins should be spread out to allow control of fracture and limit stress risers.
-
□ Pins through the iliotibial band cause pain. Expect limited knee motion until the fixator is removed.
-
□ Weightbearing must be encouraged to strengthen fracture callus.
-
□ The knee can be manipulated under anesthesia when the fixator is removed at about 3 months after implantation.
-
□ May be a good choice in children (a)
who are too young for a locked nail with fractures prone to shortening,
(b) who have a deformed canal that will not accommodate flexible nails,
and (c) who are too sick to tolerate prolonged anesthesia or vigorous
manipulation.
-
-
Flexible intramedullary nails (Fig. 12.8-3):
-
□ Excellent for fractures in juveniles with short oblique or transverse fracture patterns.
-
□ The fracture must be reducible in order
to pass the nails. If the fracture is not reducible under anesthesia,
open reduction or another method of stabilization should be considered. -
□ Usually placed retrograde from distal femoral metaphyseal portals.
-
□ Must be prebent to provide three-point fixation.
-
□ Must be sized to fit in canal—larger is
stronger. The two nails should be the same size, and should fill 80% of
the canal at the isthmus. -
□ Should be cut just outside femoral cortex to allow later removal. If they protrude, there will be irritation with knee motion.
-
□ Non-weightbearing should be maintained until callus is seen, usually 3 to 4 weeks after implantation.
-
□ Nails should be removed after solid fracture healing.
-
-
Locked intramedullary nail through the piriformis fossa (Fig. 12.8-4A):
-
□ May damage the ascending cervical
vessels so this procedure is contraindicated in the skeletally
immature. There is no satisfactory treatment for avascular necrosis of
the capital femoral epiphysis. -
□ Reaming of the isthmus allow placement of a larger diameter nail.
-
□ Should be the standard treatment for femur fracture in the skeletally mature.
-
-
Locked intramedullary nail through the greater trochanter (see Fig. 12.8-4B):
-
□ Avoids damage to the ascending cervical vessels.
-
□ Passing a small diameter nail prevents obliteration of the greater trochanteric apophysis.
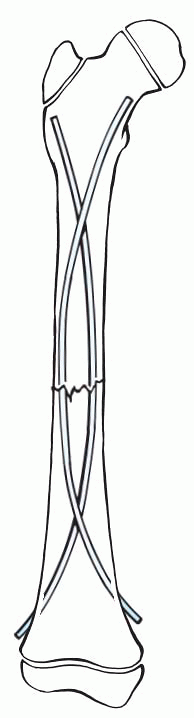 Figure 12.8-3
Figure 12.8-3
Retrograde placement of flexible nails for femoral shaft fracture.
Small incisions just proximal to the knee allow creation of entry holes
into the distal metaphyseal flare. Nails should be prebent with a long,
gentle C-curve, which will provide three-point fixation of the
fracture. Two nails are inserted—one from each side. The prebends
oppose each other. The distal nail tips should be cut just outside the
distal femoral cortex. They should be left long enough to enable future
removal and short enough to prevent irritation of the mobile soft
tissues around the knee—approximately 1 cm outside the bone. -
□ Allows passage of the nail from the
greater trochanter into the intramuscular canal, which is not collinear
with the greater trochanter. -
□ May not fill the canal, so may not be as strong a construct as a standard reamed nail.
-
□ Requires non-weightbearing until callus is seen.
-
-
Débridement of open fractures:
-
□ Open fractures always need prompt débridement.
-
□ The traumatic wound should be extended
to allow visualization and curettage of bone ends. The surgical wound
should be closed and the traumatic wound left open. -
□ Open fracture is not a contraindication
to internal fixation. If there is gross contamination, consider use of
an external fixator and repeated débridement.
-
-
Antibiotics should be given.
-
□ A cephalosporin is indicated for clean wounds.
-
□ Add an aminoglycoside for contaminated wounds and penicillin for barnyard wounds.
-
The isthmus must be scrutinized prior to any planned intramedullary
fixation to make sure it is large enough to
allow
passage on the implant. The distal femur gradually expands into a
metaphyseal flare which is much wider from medial to lateral than front
to back. There is a gradual transition from cortical to cancellous bone.
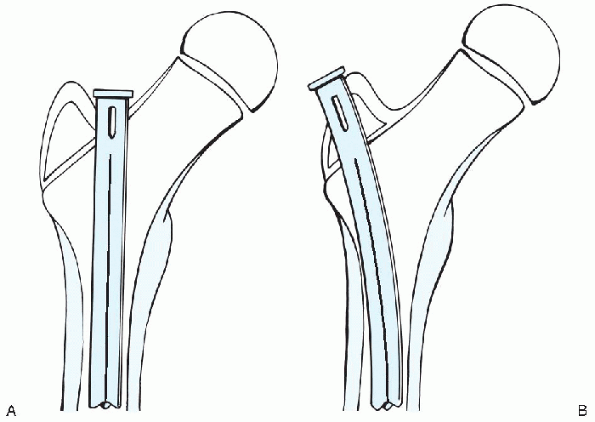 |
|
Figure 12.8-4 (A)
Placement of intramedullary through the piriform fossa. This starting point is ideal for placing a reamed antegrade nail as it is coaxial with the intramedullary canal. Its use must be avoided in the skeletally immature patient due to the risk of damage to the ascending vessels, which supply the capital femoral epiphysis. (B) Placement of intramedullary through the greater trochanteric apophysis. This starting point is not ideal for placing an antegrade nail as it is not coaxial with the intramedullary canal. A smaller diameter nail will be used than with a standard piriform fossa approach to be able to “get around the corner” from the trochanter into the femoral canal and to eliminate the need to ream a very large hole in the trochanteric apophysis. |
-
Routine wound surveillance is indicated.
-
Non-weightbearing should be maintained until callus is seen.
-
Crutches should be used until bridging callus is seen on anteroposterior and lateral radiographs.
-
Hardware should be removed after fracture healing and remodeling.
-
Superficial infection (cellulitis) can sometimes be managed with antibiotics.
-
Deep infections need open débridement.
-
Antibiotics should be tailored to the culture organism.
-
Loose hardware should be removed and an external fixator can provide stability.
-
Stable hardware should be maintained in place.
-
Unusual in children
-
Weightbearing, bone stimulators, and bone grafting can be effective.
-
Extremely rare in the absence of an open fracture or surgical treatment.
-
Fractures tend to heal in children even if the bone ends are not apposed.
-
Treatment is the same as for delayed union.
-
Repeat or more secure fixation may be required.
-
Fractures not reduced out to length can heal shortened.
-
1 cm of overgrowth can be expected in children between 4 and 10 years.
-
The treatment plan should take this into account.
-
The process of overgrowth should be complete 6 to 12 months after injury.
-
Discrepancies of less than 2 cm can generally be treated with shoe modifications.
-
Discrepancies predicted to be from 2 to 4 cm can be managed by epiphysiodesis.
-
Greater discrepancies may require lengthening procedure.
-
Should be prevented.
-
Infants have impressive remodeling potential.
-
Up to 15 degrees of angulation can be accepted in younger children and less angulation can be accepted near skeletal maturity.
-
In general, valgus is better tolerated than varus and procurvatum is better tolerated than recurvatum.
-
Persistently symptomatic angulation, which is not likely to remodel should be treated with osteotomy.
-
Should be prevented.
-
No more than 20 degrees should be accepted.
-
If there is any doubt as to whether
rotation is correct, simultaneous radiographs should be taken of femurs
to include hips and knees in an effort to match version prior to
surgical fixation. -
Persistently symptomatic rotation, which is not likely to remodel should be treated with osteotomy.
-
Parents should be warned about the
possibility of late leg length discrepancy. A few words of early
warning are worth more than volumes of late explanation. -
After cast removal, a limp is to be expected. Parents should be warned. The limp is not permanent.
-
1 cm of overgrowth can be expected in children between 4 and 10 years. The treatment plan should take this into account.
P, Pevny T, Teague D. Early complications with external fixation of
pediatric femoral shaft fractures. J Orthop Trauma 1996; 10:191-198.
SD, Drvaric DM, Darr K, et al. The operative stabilization of pediatric
diaphyseal femur fractures with flexible intramedullary nails: a
prospective analysis. J Pediatr Orthop 1994;14:501-507.
BF, Sponseller PD, Thompson JD. Pediatric femur fractures: effects of
spica cast treatment on family and community. J Pediatr Orthop
1995;15:457-460.
CM, Sponseller PD, Sturm P, et al. Open femur fractures in children:
treatment, complications, and results. J Pediatr Orthop 2000;20:183-188.
PJ, Song KM, Routt ML, et al. Plate fixation of femoral shaft fractures
in multiply injured children. J Bone Joint Surg (Am)1993;75:1774-1780.
KD. Modern trends in internal fixation of femoral shaft fractures in
children: a critical review. J Pediatr Orthop (Part B) 1997; 6:117-125.
DL, Leet AI, Money MD, et al. Secondary fractures associated with
external fixation in pediatric femur fractures. J Pediatr Orthop
1999;19:582-586.
JD, Buehler KC, Sponseller PD, et al. Shortening in femoral shaft
fractures in children treated with spica cast. Clin Orthop
1997;338:74-78.
DR, Hoffinger S. Intramedullary nailing of femoral shaft fractures in
children via the trochanter tip. Clin Orthop 2000;376: 113-118.
sportsrelated injuries, motor vehicles accidents, or falls. Fractures
may disrupt the extensor mechanism, create knee instability, or injure
the physes. Therefore, diagnosis and treatment measures are critical to
the future function and development of the child with a knee fracture.
quadriceps, or a combination of the two may result in patella fracture.
Linear or comminuted fractures are characteristic patterns that result
from direct impact to the knee and patella subluxation or dislocation
may result in an osteochondral fracture. Patella fractures can be
classified according to location (Table 12.9-1).
existing knee joint anomalies such as bipartite patella,
Osgood-Schlatter disease, or Sinding-Larsen-Johansson (SLJ) disease.
Additionally, small fracture fragments associated with patella
fractures are easily missed on radiographs.
|
TABLE 12.9-1 FRACTURES OF THE PATELLA
|
|||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
-
Effusion, hemarthrosis
-
Refusal to bear weight
-
Point tenderness
-
Patella alta
-
Inability to fully extend knee
-
Palpable defect (sleeve fracture)
moves proximally with voluntary contraction of the quadriceps while the
patellar ligament remains relaxed. Patients with stable, nondisplaced
fractures will be able to perform straight leg raises. Osteochondral
fractures may result from patellar dislocations which have
spontaneously reduced prior to presentation. A patient who has had a
dislocated patella will resist passive manipulation by contracting the
quadriceps or by physically grabbing the examiner to prevent further
manipulation (positive apprehension test).
-
Fragmentation
-
Fracture lines
-
Patella alta
-
Knee effusion
|
TABLE 12.9-2 RADIOGRAPHIC GUIDELINES FOR IMAGING PATELLA FRACTURES
|
||||||
|---|---|---|---|---|---|---|
|
In patients with large knee effusions who have sustained significant
injury, magnetic resonance imaging (MRI) scans may be valuable to
visualize cartilage damage or fracture fragments.
articular step-off require open reduction and fixation, followed by 4
to 6 weeks of immobilization in a cylinder cast. A torn retinaculum and
other functionally debilitating cartilage or ligament injuries should
be surgically treated.
to 6 weeks of immobilization with the knee held in extension in a
cylinder cast.
achieves acceptable results. Overall, patients with nondisplaced
fractures have good results while patients with comminuted, displaced
fractures experience more complications.
physical therapy program for range of motion and continued muscle
strengthening.
commonly reported patella fracture in children. A small fragment of
bone attached to a sleeve of cartilage avulses from the lower pole of
the patella.
-
Severe knee pain
-
Inability to fully extend the knee
-
Point tenderness
-
Palpable gap
-
Inability to bear weight
-
High-riding patella
-
Effusion
-
No history of direct blow to knee
fractures from SLJ disease. Unlike SLJ disease, patella sleeve
fractures are an acute injury with intense pain. The palpable gap at
the distal pole of the patella is an important clinical sign
characteristic of patella sleeve fractures.
-
Effusion
-
Small fragment avulsed from distal patellar pole
-
Patella alta
radiographically. Sagittal MRI views along the axis of the patellar
tendon are helpful in diagnosis.
treated with open reduction and fixation in order to realign the
articular surfaces. Patients treated by cast immobilization have a
higher rate of complications than those treated surgically.
-
Loss of full knee extension
-
Subchondral articular defect
-
Patellar deformity
-
Loss of reduction
-
Loss of motion
-
Ossification of patellar tendon
weeks in a cylinder cast. Following casting, physical therapy for range
of motion and strengthening is helpful.
association with lateral patellar dislocations. Dislocation may cause a
fragment of the medial patella or lateral femoral condyle to break away
from the bone. Osteochondral fractures can be classified by location
and mechanism of injury.
-
Effusion
-
Knee held in slight flexion
-
Knee pain
-
Inability to bear weight
-
Resist movement
-
Point tenderness
are often difficult to see on plain films, as the fragment size may be
very small or hidden from view. Anteroposterior and lateral as well as
sunrise
and tunnel views should be obtained. Arthrography, computed tomography
(CT) scan, or MRI can be useful in visualizing the cartilaginous nature
of the injury, which may be extensive.
cm) should be treated surgically with pins or screws. The knee is then
immobilized in flexion for 4 to 6 weeks following surgery. Small
fragments (≤1 cm) may be removed arthroscopically.
-
Loss of motion
-
Femoral condyle deformity
-
Patellar deformity
-
Late osteoarthritis changes
-
Blow to the knee with a planted foot
-
Fall on a bent knee
-
A birth injury may occur with a breech presentation
-
Hyperextension of the knee
-
Other factors may also predispose patients to physeal injury:
-
□ Osteomyelitis
-
□ Myelomeningocele
-
□ Leukemia
-
□ Osteosarcoma
-
□ Hemophilia
-
-
Account for about 1% to 6% of all physeal injuries
-
Occur in adolescents between 12 and 16 years of age
-
Associated pathology: ligament, popliteal artery, and peroneal nerve injury possible
-
Classified according to the Salter-Harris classification
-
Swelling and effusion
-
Report hearing a pop at the time of injury
-
Tenderness about the physis
-
Inability to bear weight
valuable. MRI, ultrasound, or arthrography may aid in the diagnosis of
physeal fractures in infants. Arteriography should be performed when
vascular injury is suspected.
-
The patella and femoral condyles in line with the proximal tibia, ruling out knee dislocation
-
Fracture line
-
Degree of displacement
all displaced distal femoral physeal fractures. The joint may be
aspirated prior to manipulation and traction should be applied to
minimize cartilage damage. Closed reduction should be performed under
general anesthesia to prevent muscle spasm, which may cause grinding of
the physis.
be crossed. Many type II fractures can be fixed with interfragmentary
screw fixation through the Thurston-Holland fragment and type III
fractures can be reduced with pins or screws placed transversely
through the epiphysis. Similarly, pins or screws should be placed
transversely through the epiphysis or metaphysis when reducing type IV
fractures.
aspiration of tense effusions, the patient should be placed in a long
leg or hip spica cast with 15 to 20 degrees of knee flexion.
a greater potential for leg length discrepancy and angular deformity
secondary to physeal arrest in younger children.
-
Popliteal artery impairment
-
Angular deformity
-
Compartment syndrome
-
Partial/complete physeal arrest
-
Peroneal nerve palsy
-
Leg length discrepancy
-
Recurrent displacement
-
Knee stiffness
-
Ligamentous injury
in children and its mechanisms are similar to those of distal femoral
fractures. Fractures of the proximal tibial physis account for
approximately 0.8% of all physeal injuries and occur most commonly in
adolescent boys.
to assess the status of the peroneal nerve and popliteal artery.
Compartment syndrome must be ruled out:
-
Tense joint with hemarthrosis
-
Tenderness over the physis 1.0 to 1.5 cm below the joint line
-
Fibular tenderness
-
Fracture line
-
Effusion
-
Associated injuries
difficult to appreciate on plain radiographs alone. CT scanning or MRI
may provide additional information. Arteriography should be performed
when vascular injury is suspected.
IV fractures are candidates for operative treatment. Unstable
Salter-Harris type I fractures may be fixed with percutaneous pins that
cross distal to the physis. The wires should be removed 4 to 6 weeks
after surgery. Open reduction and internal fixation is indicated for
displaced type III and type IV fractures and pins or screws may be
placed horizontally parallel to the physis. Ligamentous and meniscal
injuries should be repaired.
-
Nondisplaced fractures treated in a long leg cast with 30 degrees of flexion for 4 to 6 weeks.
-
Similar to those of patients with distal femur physeal fractures.
-
Popliteal artery impairment
-
Angular deformity
-
Compartment syndrome
-
Partial/complete physeal arrest
-
Peroneal nerve palsy
-
Leg length discrepancy
-
Recurrent displacement
-
Knee stiffness
-
Ligamentous injury
flexion should be immobilized for 6 to 8 weeks. After removal of the
cast, range of motion and quadriceps strengthening exercises should be
initiated.
fragment of the anterior or posterior aspect of the tibial eminence to
avulse. The more common anterior tibial spine injuries result in a bony
fragment with an attached (anterior cruciate ligament) ligament.
estimated incidence of 3 per 100,000 each year. They are thought to
result from a combination of rotational, hyperextension, and valgus
force. Children often sustain this injury after falling from a bicycle,
during athletic activity, or rarely as a result of trauma. The
classification for this injury is based on fragment displacement (Fig. 12.9-1).
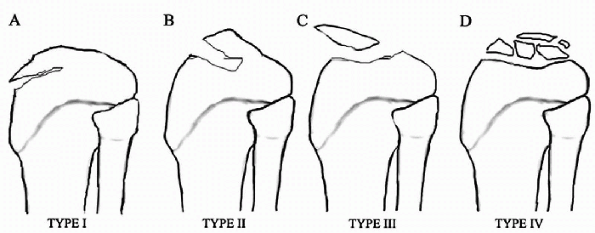 |
|
Figure 12.9-1 (A-D) Meyers and McKeever classification of tibial eminence fractures.
|
-
Pain
-
Hemarthrosis
-
Inability to bear weight
-
Painful and limited range of motion
-
Lachman test
-
Drawer test
-
Pivot shift test
obtained and examined for the presence of a bony fragment. Tunnel or
stress views may also be helpful. The lesion is frequently larger than
it appears radiographically due to cartilaginous involvement not
visible on plain radiographs.
open reduction and internal fixation with sutures, pins, screws, or
Kirschner wires. These injuries have poor outcomes when treated
nonoperatively.
closed reduction in a splint or a cast for 4 to 6 weeks. The knee
should be immobilized in slight flexion (10 to 20 degrees).
-
Anteroposterior laxity
-
Loss of extension due to bony block
-
Late sequelae meniscal injury as a result of cruciate laxity
-
Extensor lag
-
Quadriceps weakness
immobilization or closed reduction through cast immobilization for 4 to
6 weeks, all patients should be assigned range of motion therapy and
muscle strengthening training following cast removal.
or landing during a sporting event. Associated pathology may include
meniscal tear or patellar fractures. This injury represents 1% to 3% of
all physeal injuries and is seen most commonly in athletic adolescent
males. Predisposing factors include:
-
Patella baja
-
Osgood-Schlatter disease
-
Tight hamstrings
-
Physeal abnormalities
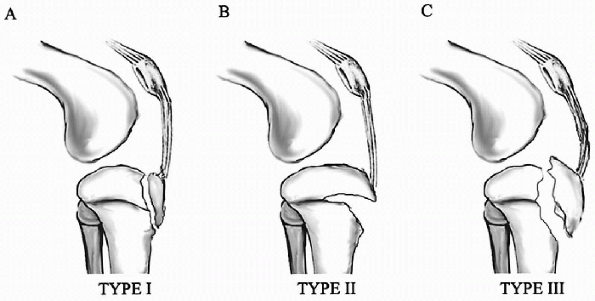 |
|
Figure 12.9-2 (A-C) Watson-Jones classification of tibial tubercle avulsions.
|
-
Swelling and tenderness
-
Lack of full extension (type II and III fractures)
-
Palpable fracture fragment
-
Patella alta
-
Effusion
-
Hemarthrosis
-
Patella alta
-
Fracture fragment
-
Effusion
fractures. Fixation is achieved by smooth pins or small wires if the
patient is more than 3 years from skeletal maturity or if the fracture
fragment is small. Large fragments or older children can have fracture
fixation with screws, threaded Steinmann pins, or tension holding
sutures.
tubercle tend to have a favorable outcome and usually return to normal
activities.
-
Compartment syndrome
-
Loss of flexion or extension
-
Meniscal tear
-
Patella alta
-
Genu recurvatum
knee in extension for 4 to 6 weeks. Physical therapy for quadriceps
strengthening and range of motion exercises are instituted at cast
removal.
JM, Hresko T, Reynolds RA, et al. Titanium elastic nails for pediatric
femur fractures: a multicenter study of early results with analysis of
complications. J Pediatr Orthop 2001;21:4-8.
JM, Luedtke L, Ganley TJ, et al. Titanium elastic nails for pediatric
femur fractures: lessons from the learning curve. Am J Orthop
2002;31:71-74.
GR, Ackroyd CE. Sleeve fractures of the patella in children: a report
of three cases. J Bone Joint Surg (Br) 1979:61:165-168.
LJ, Foster TE. Acute knee injuries in the immature athlete. In Heckman
JD, ed. Instructional Course Lectures 42. Rosemont, IL: American
Academy of Orthopaedic Surgeons, 1993:473-481.
CB, McGinnis DW. Knee. In: Sullivan JA, Anderson SJ, eds. Care of the
young athlete. Rosemont, IL: American Academy of Orthopaedic Surgeons,
2000:377-404.
PD, Stanitski CL. Fractures and dislocations about the knee. In JH
Beaty, JR Kasser, eds. Rockwood and Wilkins’ fractures in children, 5th
ed. Philadelphia: Lippincott Williams & Wilkins, 2001:981-1076.
-
The postnatal development of the tibial tubercle can be divided into four stages (Table 12.10-1).
-
Fractures of the tibial tuberosity can occur during any of the first three stages of development.
-
Most fractures occur while a child or adolescent is involved in athletics, especially in those that involve jumping and landing.
-
Basketball, track and field, and gymnastics are the three sports in which these injuries most commonly occur.
-
The mechanism of these fractures is an
avulsion most often caused by sudden acceleration or deceleration of
the knee extensor mechanism.
-
Fractures of the tibial tuberosity only
occur in children and adolescents in whom the ossification centers are
still open or incompletely closed. -
Some studies suggest that acute
disruptions of the tibial tuberosity occur with increased incidence in
knees with preexisting Osgood-Schlatter disease. -
Despite the considerable force exerted
upon the insertion of the quadriceps muscle when it contracts,
especially when jumping or landing, fractures of the tibial tuberosity
are relatively rare.
-
These avulsion-type fractures occur when
the patellar tendon pulls hard enough to overcome the combined strength
of the growth plate underlying the tubercle, the surrounding
perichondrium, and the adjacent periosteum. -
There are two ways in which this mechanism can occur:
-
□ Violent contraction of the quadriceps muscle against a fixed tibia.
-
□ action occurs when an athlete springs off to jump, as in a basketball game or a track and field event.
-
-
Acute passive flexion of the knee is strong enough to override the contracted quadriceps.
-
□ This variation of the mechanism can
occur, for example, when an athlete makes a bad landing at the end of
the jump or fall, as in a gymnastic event or in the long jump.
-
In general, the difference between the subtypes is in the degree of
separation from the metaphysis and in comminution of the avulsed
fragment.
|
TABLE 12.10-1 STAGES OF DEVELOPMENT OF THE TIBIAL TUBERCLE
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
TABLE 12.10-2 CLASSIFICATION OF INJURY TO THE TIBIAL TUBEROSITY
|
||||||||
|---|---|---|---|---|---|---|---|---|
|
-
Patients with a fracture of the tibial
tuberosity will present with a history of an acute injury, most often
during participation in an athletic event involving jumping. -
They describe immediate marked pain and swelling at the time of injury, and are often unable to stand or walk.
-
These fractures can be distinguished from
Osgood-Schlatter disease because in the latter, onset of symptoms is
often insidious rather than acute. In addition, the symptoms in
Osgood-Schlatter disease are usually mild and intermittent, the
patients have only partial disability as opposed to the inability to
stand or walk, and treatment is only symptomatic and supportive.
-
The tibial tuberosity lies just laterally to the midline of the tibia.
-
The best radiologic view to evaluate this
injury is a lateral radiograph with the tibia rotated slightly
medially. Findings will vary depending upon the type of injury.
-
Anterosuperior displacement of one or more fragments of the tuberosity
-
Extension of the fracture through the proximal tibial ossification center into the joint with disruption of the joint surface
-
In general, the only type of tibial
tuberosity fracture that should be managed without surgery is a type I
fracture that involves small fragments that are either nondisplaced or
only minimally displaced. -
Type II and III fractures are treated with open reduction and internal fixation.
-
In cases of displaced fractures, a periosteal flap may be folded under the avulsed fragments.
-
□ The fracture bed should be cleared of
any debris and any such periosteal flaps should be extracted and spread
out during reduction of the fragment with the knee extended. -
□ Fixation of the fragment should be reinforced by repair of the torn periosteum.
-
-
The outcome of properly reduced or surgically treated fractures of the tibial tuberosity is good.
-
Nearly all patients are able to return to full activity, including participation in athletics.
-
After reduction or repair, a cylinder or long leg cast should be applied for 4 weeks.
-
Rehabilitation should focus on active range of motion and quadriceps strengthening exercises.
-
The patient can return to full
participation in athletics after the mass and strength of the
quadriceps on the affected side is equal to that on the opposite side. -
Patients should be followed for any loss
of range of motion of the knee, atrophy of the quadriceps muscles,
persistent prominence of the tuberosity, the possibility of patella
alta in an inadequately reduced displaced tuberosity, and the
possibility of infection following open reduction.
-
Usually occur in younger children between the ages of 3 and 6 years
-
Result from a valgus stress applied to an extended knee.
-
May be nondisplaced and incomplete versus displaced with valgus opening of the medial cortex
-
Present with swelling and tenderness of the proximal tibia
-
Significant displacement requires a
thorough neurovascular exam to rule out compartment syndrome. Most
patients will have a nondisplaced buckle fracture or valgus greenstick
fracture by radiographs.
-
An acute valgus deformity requires a closed reduction under conscious sedation and placement of a long leg cast in extension.
-
If correction cannot be achieved by
closed techniques, an open reduction with removal of interposed soft
tissue should be performed. -
The most common complication of proximal
metaphyseal tibial fractures, even in anatomically reduced injuries, is
valgus deformity. Most practitioners believe that asymmetric growth
occurs. -
Parents should be informed about the
possibilities of valgus overgrowth occurring the first year after
injury; bracing is ineffective and corrective osteotomies should not be
performed until skeletal maturity. Most patients will correct the
valgus deformity with continued growth.
-
Common injuries to the lower extremities.
-
Closed injuries heal faster and have fewer complications than similar adult injuries.
-
Indirect means through a rotational twisting force, presenting as a spiral or oblique fracture pattern.
-
A direct force presents as a transverse or butterfly-type fracture pattern.
-
Tibial and fibular fractures can be categorized according to which bone is fractured.
-
The most common type of fracture is an isolated tibia fracture in the distal third of the tibia.
-
The intact fibula prevents shortening but
varus angulation can occur secondary to deforming force of the toe
flexors and posterior tibialis tendon.
-
The second type of fracture pattern involves both the tibia and fibular shafts.
-
The most common angular problem is valgus malalignment secondary to deforming forces of the anterior extensor muscles.
-
Maintaining length can be a problem.
-
The third type involves an isolated
fibula fracture, which usually occurs from direct trauma to the lateral
aspect of the leg. One must rule out an associated distal tibial
physeal injury.
-
Pain with local swelling and tenderness will be present.
-
Radiographs should include anteroposterior and lateral views to include the knee and ankle joint.
-
Most will have a nondisplaced buckle fracture or valgus greenstick fracture by radiographs.
-
Most closed tibial and fibular shaft fractures can be treated with closed reduction and long leg casting.
-
There is minimal overgrowth of the tibia so shortening of more than 1 cm is unacceptable.
-
In younger children angulation of up to
10 degrees is acceptable, however angulation of more than 5 degrees in
adolescents may not remodel.
-
Unstable or open tibial fractures that
cannot be adequately reduced and held in a cast can be treated by a
variety of techniques including external fixation, pins and plaster,
lag screws, plating and flexible intramedullary nails, taking care to
avoid the growth plates at the insertion sites of the nails. -
All open tibia and fibular fractures are treated with emergent irrigation and débridement and antibiotics.
-
Gustillo and Anderson grade 1 fractures can be treated with long leg casting.
-
Grade 2 and 3 open fractures can be
treated with various techniques previously mentioned, depending on the
soft tissue injury and wound contamination.
-
Complications such as angulatory
deformity, leg length discrepancy, and malrotation can occur. Adherence
to acceptable amounts of angulation and shortening will prevent these
complications. -
Malrotation will not remodel with growth and should not be accepted.
-
Delayed union and nonunion is unusual in closed tibial shaft fractures.
-
Delayed union and osteomyelitis can occur
in open fractures; however, current treatment techniques can achieve
good results in these types of fractures. -
Compartment syndrome can occur in tibial
shaft fractures and a high index of suspicion must be present when a
child has pain out of proportion to the injury and has pain of passive
stretch of the toes.
-
Stress fractures must be considered in the differential diagnosis of leg pain.
-
Generally tibial stress fractures occur between 10 and 15 years of age without a history of specific injury.
-
Most children have a painful limp and have local bone tenderness usually occurring on the upper tibia.
-
Radiographs may be normal in the first 10 to 14 days, but subsequent radiographs will show periosteal reaction.
-
□ The proximal posterior medial tibia is the most common site.
-
-
Magnetic resonance imaging or bone scan may aid in diagnosis if early plain radiographs are normal.
-
Differential diagnosis includes Ewing sarcoma and osteomyelitis.
-
The treatment of tibial stress fractures is relative rest.
-
If there is significant pain on
weightbearing, crutches and a long leg cast may be used for 4 weeks
followed by gradual increase in activity. -
Nonunion of tibial stress fractures has been reported but is extremely rare.
-
“Toddler’s fracture” is a spiral fracture of the tibia without a concomitant fibular fracture.
-
Mechanism of injury is usually a
rotational force through the tibia, namely internal rotation of the
proximal leg, with the foot and ankle in a fixed position. It most
often occurs when a toddler stumbles while running or walking.
-
The majority of these fractures occur in children less than 2.5 years of age.
-
The most common site of this fracture is the distal metaphysis of the tibia.
-
Spiral fractures of the midshaft of the
tibia can also occur, but are more often associated with child abuse
rather than an accidental twisting or tripping injury.
-
The inability to bear weight and focal
tenderness are the most common presenting features in a child with a
toddler fracture. History of an acute twisting or tripping injury may
be elicited, but more commonly the injury mechanism is not obvious.
-
Radiographs of the tibia and fibula should be obtained in both anteroposterior and lateral projections.
-
An internal oblique view can help in
recognition of nondisplaced toddler’s fractures and sometimes may be
the only view that identifies this type of fracture. -
Follow-up films at 10 to 14 days will usually demonstrate callus formation.
-
A long leg cast, bent knee, is applied for about 3 weeks.
-
Most patients with these fractures recover full preinjury activity and normal growth following immobilization.
JS, Owen HF, Nogrady MB, et al. Obscure tibial fracture of infants: the
toddler’s fracture. J Can Assoc Radiol 1964;25: 136-144.
MF, Finzel KC, Carrion WV, et al. Toddler’s fracture: presumptive
diagnosis and treatment. J Pediatr Orthop 2001;21: 152-156.
HR, Keeler KA, Gabos PG, et al. Posttraumatic tibia valga in children:
a long term follow up note. J Bone Joint Surg (Am) 1999; 81:799-810.
JP, Letts RM. Isolated fractures of the tibia with intact fibula in
children: a review of 95 patients. J Pediatr Orthop 1997;17: 347-351.
distal fibula, distal to the metaphysis. This may affect the ankle
joint by entering the articular cartilage or disrupting the
tibiofibular syndesmosis, thus widening the space between the tibia and
fibula.
in adults, although the mechanism may be similar. The differences are
attributed to the presence of the growth plates, which are weaker than
the ligaments and adjacent bones. These physes also close slowly
resulting in a stress riser at the point where the unossified growth
plate meets the ossified growth plate. Many of these fractures may be
treated nonoperatively. However, it is important to identify, assess,
and operate on those fractures that require open reduction and internal
fixation to prevent complications.
-
Tibial and fibular growth plates are most important features that make these injuries different from adult injuries.
-
Damage to the growth plate may lead to angular or longitudinal growth problems.
-
Tibial growth plate is proximal to the joint line and to the fibular growth plate.
-
Fibular growth plate is level with the ankle joint line.
-
The growth plate is weaker than adjacent ligaments.
-
Distal tibial growth plate closes over a period of 18 months.
-
Order of closure: central, medial, lateral, posterior, anterior.
-
Medial: deltoid ligaments—superficial and deep
-
Lateral:
-
□ Anterior talofibular ligament
-
□ Posterior talofibular ligament
-
□ Calcaneofibular ligament
-
-
Central—syndesmosis:
-
□ Anterior inferior tibiofibular ligament
-
□ Posterior inferior tibiofibular ligament
-
□ Interosseous membrane
-
-
Annual incidence:
-
□ 0.1% of children sustain ankle fractures
-
□ Constitute 10% to 25% of all physeal injuries
-
□ Second most common fracture after distal radius
-
-
Sex ratio: boys more than girls by 2:1
-
Especially common at age 10 to 15 years (during which time physes are closing)
-
The ankle joint transmits the whole body weight to the ground through the foot.
-
Resists torsion in all three planes.
-
Indirect mechanism: with a fixed foot,
the body is forced into internal rotation/external rotation,
eversion/inversion, plantarflexion/dorsiflexion -
Direct mechanism: vehicle crash, falls, sports
-
The Salter-Harris classification describes the fracture anatomically relative to the growth plate and joint line (Figs. 12.11-1 and 12.11-2 and Table 12.11-1).
-
Higher grades represent increasing risks of growth complications.
-
Type of fracture can be correlated with patient age.
-
Understanding the injury mechanism
facilitates planning closed or open reduction maneuvers. In general,
this is done by reversing the injury mechanism. -
Dias-Tachdjian system (Fig. 12.11-3):
-
□ Modified Lauge-Hansen classification system of adult ankle fractures.
-
□ Used with descriptors from the Salter-Harris classification system.
-
-
Fracture of adjacent bone:
-
□ Distal tibia proximal to metaphysis
-
□ Proximal fibula fracture
-
□ Hindfoot, especially the talus and base of fifth metatarsal
-
-
Septic arthritis, osteomyelitis
-
Osteochondritis dissecans of talus
-
Tarsal coalition
-
Chronic ankle instability
-
Tendinitis
-
Juvenile chronic arthritis
-
Tumor, osteoid osteoma, osteosarcoma, Ewing sarcoma
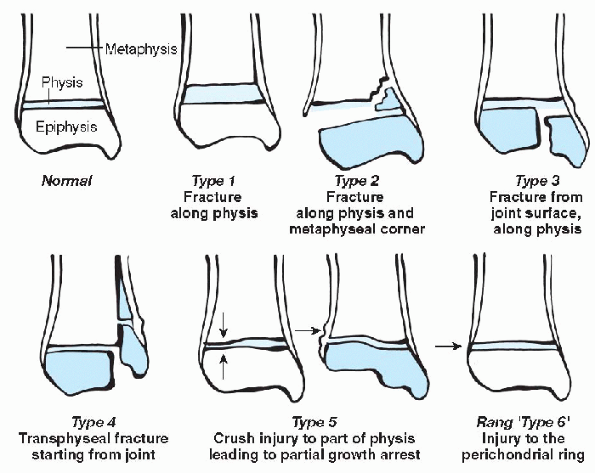 |
|
Figure 12.11-1
Salter-Harris classification system for growth plate fractures. (Adapted from Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone Joint Surg 1963;45A:587-622.) |
|
TABLE 12.11-1 SALTER-HARRIS CLASSIFICATION SYSTEM
|
|||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||
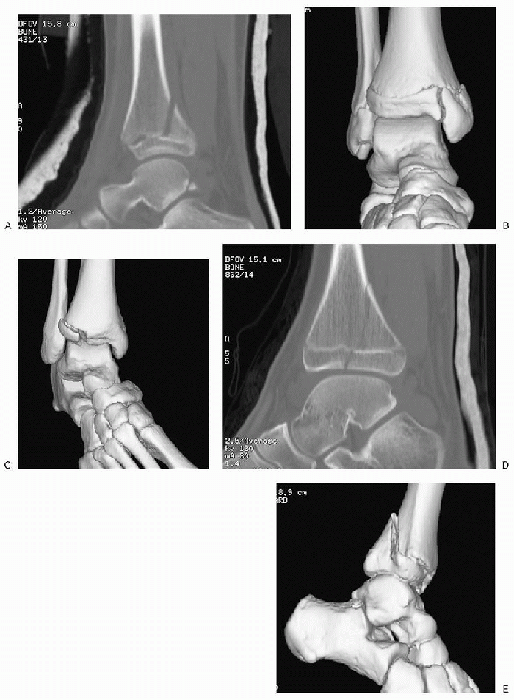 |
|
Figure 12.11-2 Ankle fractures. (A) Sagittal reconstruction of computed tomography (CT) scan of a Salter-Harris type II fracture. (B) Three-dimensional (3D) rendering of CT scan reconstruction of Salter-Harris type III fracture. (C) 3D rendering of CT scan reconstruction of Tillaux fracture. (D) Sagittal reconstruction of CT scan of Salter-Harris type IV fracture. (E) 3D rendering of CT scan reconstruction of triplane fracture. (The fibula has been digitally removed for easier appreciation.)
|
-
Trauma usually not witnessed and details poorly described
-
Important to exclude from history:
-
□ Nonaccidental injury
-
□ Pathologic fracture
-
□ Differential diagnosis (chronic ankle pain)
-
-
Inspection:
-
□ Open/closed
-
□ Impending skin breakdown
-
□ Bruising, swelling, deformity
-
□ Foot perfusion, capillary refill
-
-
Palpation:
-
□ Local tenderness over fracture (may
have tenderness anteriorly only with a Tillaux fracture, not along
medial or lateral malleoli) -
□ Salter-Harris type I fibula fracture: localized tenderness over bone rather than ligaments distinguishes this from sprain
-
□ Pedal pulses
-
□ Crepitus
-
-
Movement:
-
□ Range of motion
-
-
Special tests:
-
□ Neurologic assessment of sensation and foot intrinsic muscle function
-
□ Joint instability (ankle anterior drawer)
-
fracture being missed) if there is isolated pain and tenderness, edema,
and swelling over distal fibula and adjacent ligament below level of
joint line.
-
Standard views: anteroposterior, lateral, mortise view (15- to 20-degree internal rotation oblique)
-
Special views:
-
□ Oblique view in adolescents to exclude lateral fracture distal tibia (that would otherwise be overshadowed by fibula)
-
□ Stress views: occult joint instability
-
-
To determine displacement in Tillaux, triplane fracture
-
Best to do this after initial closed reduction to assess success
-
Aims:
-
□ To obtain and maintain a satisfactory reduction
-
□ To avoid joint incongruity or instability
-
□ To avoid growth plate incongruity and growth plate arrest
-
-
Below-knee walking cast for 3 weeks
-
May be more rotated than appears on anteroposterior and lateral view: consider oblique and assess clinically
-
Closed reduction; hold reduction in molded cast for 3 weeks with weekly x-rays
-
Can accept less than full reduction if no
soft tissue interposition (less than 5 degrees varus, less than 10
degree valgus acceptable) -
If full reduction not possible because of periosteal interposition, open procedure required to remove periosteum
-
Intraarticular fracture requires reduction if displaced 2 mm or more
-
Stabilize with Kirschner wire or screw directed parallel to physis and joint line
-
Avoid crossing physis unless very near complete growth plate closure
-
Intraarticular fracture and transphyseal fracture
-
Requires accurate open reduction and internal fixation
-
Thurston-Holland fragment can be used to stabilize fracture if large
-
Intraarticular fracture and transphyseal fracture
-
Computed tomography (CT) scan required to plan approach, reduction, and fixation
-
Requires accurate open reduction and internal fixation
-
Operation is difficult because of fragmentation and soft tissue swelling
-
Many anatomic variants
-
Order of reduction: posteromedial fragment → fibula fracture → anterolateral fragment
-
If recognized at time of injury, patient
should be maintained non-weightbearing for 3 weeks to avoid further
damage to the crushed part of the physis, although no intervention is
known to reduce risk of partial growth arrest.
-
Requires urgent closed reduction because soft tissues and neurovascular structures at risk.
-
Often associated with open injuries.
-
Should not delay initial manipulation to correct severe deformity to obtain a radiograph.
-
Once reduced, radiographs or special imaging (e.g., CT scans) can be performed.
-
Indications: usually Salter-Harris type I or II fractures of tibia and fibula can be reduced.
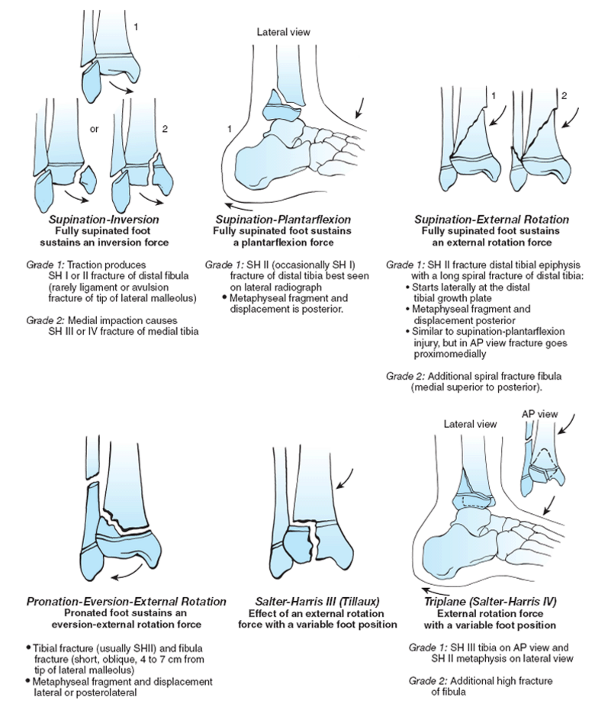 |
|
Figure 12-11.3 Dias and Tachdjian classification system of pediatric ankle fractures. SH,
Salter-Harris. (Adapted from Dias LS, Tachdjian MO. Physeal injuries of the ankle in children. Clin Orthop Rel Res 1978;136:230-233.) |
-
Indications:
-
□ Inability to obtain and maintain a closed reduction
-
□ Displaced intraarticular fracture (Salter-Harris type III or IV)
-
□ Displaced transphyseal fracture
-
□ Open fractures
-
-
CT to plan approach
-
Delay definitive open reduction until severe swelling of soft tissue has diminished (this may be up to 7 days)
-
For 2 years; growth arrest may occur at any time from 6 to 18 months
-
Clinical and radiologic assessment for:
-
□ Angular deformity
-
□ Harris lines (nonparallel, closer together on side of growth arrest)
-
□ Leg length discrepancy: distal tibia contributes 2 to 3 mm of growth per year.
-
-
Inability to obtain reduction
-
Growth plate arrest:
-
□ In general, risk of growth arrest is higher with higher class of fracture in the Salter-Harris fracture classification system.
-
□ Salter-Harris types I and II: central arrest common. Early closure of growth plate compared with opposite ankle
-
□ Salter-Harris types III, IV, V, and VI: peripheral arrest/bone bridge leading to angulation:
-
□ Often varus deformity with supination inversion injury
-
□ Consider completing epiphysiodesis to prevent angulation
-
-
-
Postoperative: wound complication, infection
-
Medial malleolar ossicle
-
Malunion, avascular necrosis, and nonunion—rare
-
Talar dome osteochondral lesion: may become symptomatic after associated fracture is healed
-
Depends on:
-
□ Skeletal age: bone, ligament, physis
-
□ Amount of soft tissue injury
-
□ Involvement of physis
-
□ Involvement of articular surface
-
□ Amount of fragmentation
-
K, Komar L, Jaramillo D, et al. Sensitivity of a clinical examination
to predict need for radiography in children with ankle injuries: a
prospective study. Lancet 2001;358:2118-2121.
A. Fractures and dislocations of the foot and ankle. In: Green NE,
Swiontkowski MF, eds. Skeletal trauma in children, 2nd ed. Vol 3.
Philadelphia: WB Saunders, 1998.
influences fracture patterns, making recognition of injury more
difficult. The calcaneus is the first bone to ossify, followed by the
talus. The major mechanism of injury is direct force from a fall, being
crushed by a heavy object, or indirect injury from a lawn mower or
forceful rotation. Fortunately, the cartilage anlage gives the foot
more resilience to injury.
-
Fractures of the talus are rare in children, and the pattern varies with age.
-
In the very young child, an incompletely ossified talus is able to absorb more energy before disruption.
-
Magnetic resonance imaging (MRI) and
computed tomography (CT) scanning may be necessary to appreciate damage
to the cartilaginous body. -
The mechanism of injury is usually forced dorsiflexion or dorsiflexion and rotation.
-
The main blood supply is provided by an
anastomosis between the laterally arising artery of the sinus tarsi and
medial artery of the tarsal canal. -
Both enter the talus inferiorly at the junction of the neck with the body.P.166
![]() Figure 12.12-1 Hawkins sign.
Figure 12.12-1 Hawkins sign. -
Hawkins sign, the presence of subchondral lucency, indicates an intact blood supply, resulting in osteopenia (Fig. 12.12-1).
-
Marti classifies fractures of the talus by their potential to develop avascular necrosis (Table 12.12-1).
in a long leg cast with the knee bent to prevent weightbearing.
Displaced fractures require open reduction and internal fixation and
weightbearing is not allowed for 6 to 8 weeks.
dislocation, require immediate reduction. The posterior approach does
not disturb the medial blood supply. An anteromedial approach combined
with a medial malleolar osteotomy can be used.
can lead to fractures of the medial and lateral process of the talus.
These are often confused with ankle sprains and are common in
snowboarders. A high index of suspicion is necessary and oblique views
of the foot and ankle and CT are useful. Treatment for large or
displaced fragments is open reduction.
|
TABLE 12.12-1 CLASSIFICATION OF TALAR FRACTURES
|
||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||
|
TABLE 12.12-2 CLASSIFICATION OF OSTEOCHONDRAL FRACTURES OF THE TALUS
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||
are the result of torsional impaction. Forceful plantar flexion and
inversion combined with external rotation of the foot produces the
medial lesion. Inversion and dorsiflexion produces an anterolateral
lesion that can be accompanied by injury to the lateral ankle ligaments.
congruity. Removal of a displaced fragment through medial malleolar
osteotomy is reported and arthroscopic treatment may also be considered.
talar fractures and are usually the result of a fall from a significant
height. Most fractures involve the body and the subtalar joint. In the
younger child, incomplete ossification makes diagnosis more difficult
and an MRI may be indicated.
Wiley’s classification is most applicable to children and CT is helpful for visualization:
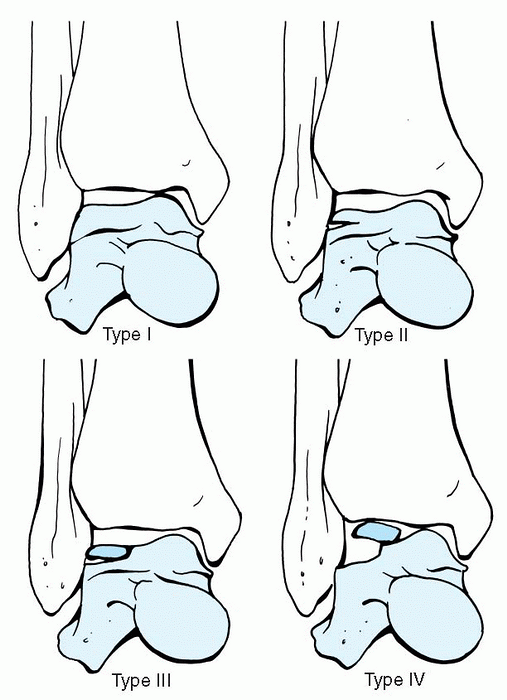 |
|
Figure 12.12-2
Osteochondral fractures of the talus. (Adapted from Marti R. Fractures of the talus and calcaneus. In: Weber BG, Brunner CH, Freuler F, eds. Treatment of fractures in children and adolescents. New York: Springer-Verlag, 1980.) |
-
Type I fractures involve the subtalar joint.
-
Type II fractures do not involve the
joint. Open reduction and restoration of the articular surface in
intraarticular fractures is recommended.
spasm and may be confused with ankle sprains. Accurate diagnosis
requires an oblique x-ray or CT scan. Cast immobilization is usually
successful in acute injuries, but excision of a loose fragment may be
necessary in chronic problems.
fasciitis, or other causes of heel pain. Diagnosis is made by clinical
examination and confirmed by bone scan. A swollen painful heel without
a history of trauma should raise suspicion. Tenderness is localized to
the posterosuperior aspect and the medial and lateral aspect of the
calcaneus. Radiographs are usually negative for up to 3 weeks; however
bone scan or MRI may be useful in establishing an early diagnosis.
Treatment is rest and limited weightbearing and resumption of
activities is not recommended before 4 to 6 weeks.
young children resulting from minor trauma. Pain is elicited by medial
and lateral compression and scintigraphy can confirm the diagnosis.
Treatment is immobilization with follow-up radiographs showing the
fracture and callus.
direct trauma from a falling object or indirect force from a fall
applied on a plantarflexed foot. Fractures of the tarsal navicular are
rare and are classified into three anatomic sites (tuberosity, dorsal
lip, body) plus stress fractures, which are seen in runners.
fragment is usually not displaced. Treatment is cast immobilization
with molding of the medial longitudinal arch. Nonunion can occur and if
associated with recurrent symptoms, excision of the fragment is
recommended. Differentiation from an accessory navicular is made by
smooth contour of the line of separation in the latter.
They are associated with sprains occurring in the inverted,
plantarflexed foot. Treatment is similar to an ankle sprain. If a
significant portion of the joint is involved, open reduction is
necessary to preserve the integrity of the medial longitudinal arch.
A direct force will cause comminuted nondisplaced fractures, whereas
force from a fall on the hyperplantar flexed foot will result in
dislocation and injury to
the
head of the talus and other tarsal bones. Marked displacements will
disrupt the subtalar and midtarsal joints and lead to degenerative
arthritis. Treatment is restoration of the joint surface by closed or
open methods. Severely comminuted type III fractures may require
primary arthrodesis.
|
TABLE 12.12-3 CLASSIFICATION OF NAVICULAR BODY FRACTURES
|
||||||||
|---|---|---|---|---|---|---|---|---|
|
highimpact sports or activities. They are associated with the tight
heel cords limiting dorsiflexion of the foot, a short first metatarsal
or metatarsus adductus, or limited subtalar motion. The presenting
symptom is pain in the medial longitudinal arch with tenderness on
compression of the tarsal navicular. The fracture is best visualized by
a true anteroposterior radiograph of the foot centered on the
navicular. Treatment is a cast immobilization and non-weightbearing for
at least 6 weeks. Surgery is recommended if there is delay in healing
and the fracture extends through two cortices.
-
Metatarsal fractures are usually nondisplaced. Lisfranc injuries mimic adult patterns.
-
Mechanisms of injury as listed in Box 12.12-1.
-
Multiple fractures occur proximally in the first metatarsal and distally in the lateral four rays.
-
Fracture of the first metatarsal is more common before the age of 5 years and often goes unrecognized at the initial evaluation.
-
Cuneiform fractures can also occur and these usually heal uneventfully unless the fracture involves the physis.
-
Accurate reduction is necessary to prevent growth disturbance from early physeal closure.
-
Striking an object while in tiptoe position (jumping from a height to the ground)
-
Heel-to-toe compression (foot crushed while kneeling)
-
Foot fixed in plantarflexion while falling backward
-
In children, the apophysis of the fifth metatarsal does not appear until age 8 and is seen as a line parallel to the shaft.
-
Fractures of the tuberosity are avulsion fractures and have a better prognosis.
-
Avulsion fractures are transverse and are treated in a short leg cast.
-
Usually the result of a crash injury.
-
Treated with compression dressing, casting, and elevation.
-
Reduction is necessary if the metatarsal heads are displaced or plantarflexed.
-
Common in ballet dancers, runners, and gymnasts.
-
Second metatarsal is most commonly involved, followed closely by the third.
-
Predisposing factors include overtraining, delayed menarche, and poor nutrition.
-
Treatment is a short leg cast for 6 to 8 weeks.
-
Fracture of the proximal fifth metatarsal is the most common metatarsal fracture and is common in children over the age of 10.
-
It is a transverse fracture at the junction of the metaphysis and diaphysis (Fig. 12.12-3).
![]() Figure 12.12-3 Jones fracture.
Figure 12.12-3 Jones fracture.
-
Pain that is progressive, not relieved by narcotics, and out of proportion to examination
-
Pain with passive range of motion of the toes
-
Parasthesias: decreased pin, light touch, or two-point discrimination
-
Pulselessness: absent palpable or Doppler pulses
-
Cool, tense foot
-
Motor deficit
-
Treatment is difficult because of poor blood supply.
-
The presence of previous injury, such as
sclerosis or preinstall reaction, often leads to delayed union,
nonunion, and refractors. -
Acute injury is treated with a short leg cast for 6 weeks or until the fracture is healed radiographically.
-
Surgery is recommended for fracture with evidence of chronic injury.
-
Grafting can be done in delayed unions.
-
Return to full activity before complete healing is often associated with treatment failure.
-
Evaluation for compartment syndrome must be considered in all injuries to the foot.
-
It is most common in crush injuries of the foot with fractures of the metatarsals, phalanges, and Lisfranc dislocation.
-
Surgical decompression is required.
-
Box 12.12-2 outlines clinical features.
-
Most common injury of the forefoot.
-
May result from direct axial injury (striking the toe against an object) or a crush injury.
-
Fractures of the proximal phalanx of the great toe require accurate reduction of displacement and angulations.
-
Salter-Harris type III physeal injuries are common and require open reduction if displaced to restore the joint surface.
-
Fractures of the distal phalanx, even if
crushed, require alignment of the toe and nail should be preserved as
it acts as splint. -
Phalanx fractures of the lesser toes can
be treated less aggressively, however reduction is necessary for
displaced plantarflexed fractures of the head as they can cause
abnormal plantar pressure.
finding in the rapidly growing child athlete. The child presents with
heel pain and tenderness is elicited on compression of the metaphysis
and not the apophysis. Treatment is rest, physical therapy, and
orthotics.
pain. Its opposition and intimate association with the posterior tibial
tendon can result in a tendonitis known as a prehallux syndrome. This
is often associated with a pronated flat foot. Ogden describes three
types of accessory navicular: ossicle in substance of posterior tendon,
synchondrosis, and cornuate navicular. Treatment is rest and
immobilization in a cast followed by orthotic support of the medial
longitudinal arch. Persistent pain is relieved by excision of the
accessory navicular. Advancement of the posterior tibial tendon does
not restore the arch.
second metatarsal head and is often confused with a fracture. It is
more common in adolescent girls and is associated with repetitive
trauma. It can be symptomatic for up to 6 months before radiographic
changes are visible. Hamilton describes four types (Table 12.2-4).
Treatment of type I is cast immobilization, while surgery is indicated
in types II and III. Each metatarsal is treated individually.
a painful limp and tenderness of the tarsal navicular. It is more
common in boys, presenting around the age of 5 years. In girls it
presents at age 4 and is unilateral in the majority of cases. Köhler’s
disease is associated with x-ray changes of density and narrowing of
the navicular.
short leg walking cast for 8 weeks. Casting for a shorter period may
result in recurrence of symptoms and prolonged recovery.
|
TABLE 12.12-4 VARIANTS OF FREIBERG INFARCTION
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||
JF, Crichton KJ, Gratten-Smith T, et al. Osteochondral fractures of the
dome of the talus. J Bone Joint Surg (Am) 1989;71A: 1143-1152.
WG. Foot and ankle injuries in dancers. In: Mann RA, Coughlin MJ, eds.
Surgery of the foot and ankle. St Louis: Mosby, 1993.
R. Fractures of the talus and calcaneus. In: Weber BG, Brunner CH,
Freuler F, eds. Treatment of fractures in children and adolescents. New
York: Springer-Verlag, 1980.