Evaluation of the Painful Total Hip Arthroplasty
– HIP > Part C – Operative Treatment Methods > 14 – Evaluation of
the Painful Total Hip Arthroplasty
performed and successful orthopaedic operations. In 2003 there were
over 230,000 primary THAs performed in the United States alone, and in
terms of quality-adjusted life years gained, THA is one of the most
cost-effective health care interventions available. Despite the
overwhelming success of THA for the treatment of end-stage hip disease,
failures do occur, and the patient with a painful THA is one of the
most difficult challenges for the orthopaedic surgeon to evaluate and
treat. The purpose of this chapter is to review the workup and
evaluation of the painful THA.
because the treatment decisions rendered are fundamentally different if
periprosthetic infection is identified. Mechanical loosening can occur
early as a result of poor surgical technique or failure of
osseointegration of a cementless implant, or it can occur late owing to
failure of the cement mantle with a cemented implant. Stress fractures
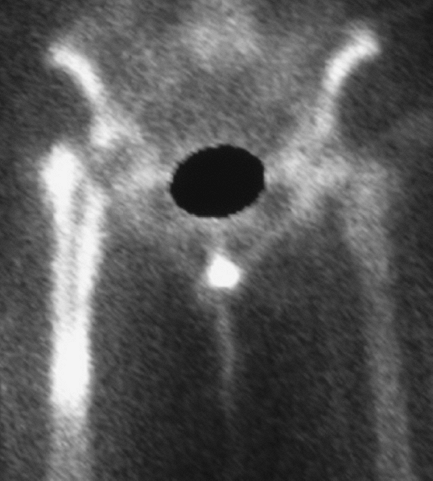
can be seen in the pubic rami (Fig. 14-1), are
most commonly associated with female sex and osteopenia, typically
occur within the first year postoperatively, and present with groin
pain. Periprosthetic fractures, when not associated with obvious
trauma, typically affect the greater trochanter in association with
osteolysis or severe stress shielding. If a transtrochanteric approach
was used for exposure, a nonunion of the greater trochanter can develop
and cause pain. Osteolysis and polyethylene wear can cause pain
secondary to the inflammatory response to wear debris. Occult
instability or subluxation of the prosthetic hip is another potential
cause of pain. Modulus of elasticity mismatch between a stiff implant
(typically a large-diameter, cementless femoral stem) and the host bone
can cause pain in the thigh. Trochanteric bursitis is a relatively
common source of pain and has been associated with an anterolateral
exposure to the hip and changes in femoral offset that occur at the
time of surgery. Iliopsoas tendonitis presents as groin pain and has
been associated with underanteverted, vertically oriented, and
oversized acetabular components.
extrinsic to the hip joint is degenerative disease of the lumbar spine.
Vascular claudication (particularly of the aortoiliac system) may also
cause pain in the groin, buttock, or thigh that can be confused with
pain directly related to the hip joint as can peripheral nerve
dysfunction, hernias, and referred pain from intra-abdominal or
genitourinary pathology. Less frequently seen causes of pain include
metabolic bone disease and primary or metastatic bone cancers.
approximately 15% of all total hip arthroplasties performed in 2003.
With expanding indications for THA including younger and more active
patients, an aging population and an ever-increasing total number of
patients who have undergone THA in the past, even with improvements in
surgical techniques and materials, the number of patients presenting
with pain and failure following THA may rise in the future.
|
TABLE 14-1 Differential Diagnosis of the Painful Total HIP Arthroplasty
|
|
|---|---|
|
critical information that allows the evaluating surgeon to narrow the
differential diagnosis and is the basis for a focused workup of the
patient with a painful THA.
 |
|
Figure 14-1 Healed stress fractures of the pubic rami that occurred subsequent to the THA.
|
character of the pain provide important clues in determining the cause
of the painful THA. Persistent pain since surgery, without a painfree
interval, is suggestive of infection (particularly if the pain
experienced now is of a different nature than that prior to surgery),
failure to obtain initial implant stability, or misdiagnosis of the
original cause of the patient’s pain when seeking total hip
arthroplasty in the first place (particularly if the pain is unchanged
when compared with preoperatively).
important to ask about any abnormal or persistent wound drainage that
occurred after surgery and to determine if the patient was placed on
antibiotics for an extended period of time or if he or she was returned
to the operating room shortly after surgery as each of these factors
should raise the suspicion for chronic infection. Acute pain following
systemic illness, dental or gastrointestinal procedures, or a distant
site of infection suggests the possibility of an acute hematogenous
infection. Infection should also be considered more likely in patients
with predisposing risk factors such as diabetes mellitus, inflammatory
arthritis, immunocompromised states, renal failure, and skin disorders.
Later onset of pain after a painfree interval suggests aseptic
loosening, periprosthetic stress fracture, osteolysis, or late
infection.
rest suggests loosening, fracture, and neurogenic or vascular
claudication. Constant pain, pain at rest, or pain at night can be
indicative of infection or malignancy. Pain that begins when a patient
starts to walk after sitting or resting (often referred to as “start-up
pain”) has been associated with loosening, micromotion, iliopsoas
tendonitis (particularly groin pain when rising out of bed or out of a
car), or lumbar spine disease. The onset of pain after a traumatic fall
may be caused by fracture or traumatic loosening. Patients with both
lumbar spine and hip disease may find that their symptoms of neurogenic
claudication worsen after successful THA, secondary to increased
activity levels.
associated with acetabular component loosening. Buttock pain that
radiates below the knee suggests a neurogenic cause, such as lumbar
disc disease or spinal stenosis. Thigh pain has been linked to femoral
component loosening or a modulus mismatch as previously described.
Localized pain over the greater trochanter is indicative of
trochanteric bursitis or nonunion.
painful THA should include a comprehensive musculoskeletal examination
focusing on the ipsilateral and contralateral hip, knee, and spine and
starts with a patient who is dressed in a gown for examination.
Inspection of the skin to look for scars and signs of infection,
including warmth, erythema, fluctuance, wound drainage, or sinus tracts
is helpful and surprisingly oftentimes overlooked. The surgeon also
should look for obvious muscle wasting around the hip or in the lower
extremity. The patient’s gait should be observed for evidence of
antalgia, limb-length discrepancy,
muscle
weakness, or a Trendelenburg gait. A Trendelenburg gait is indicative
of abductor muscle weakness and is more common after the use of an
anterolateral approach to the hip. True and apparent leg lengths should
be measured using graduated blocks as patients with lumbar spine
disease and/or fixed pelvic obliquity may present with notable
differences between their true and apparent leg lengths.
to rule out neurogenic and vascular causes of pain. Peripheral nerve
injuries involving the sciatic or femoral nerve may result in distal
muscle weakness such as a foot drop. Surgeons must be sure to establish
the temporal relationship of the muscle weakness and limb-length
inequality in relation to the time of surgery. Progressive limb
shortening after THA documented on serial examinations suggests
mechanical failure of fixation.
bursitis, inguinal hernia, and stress fractures of the pelvic ring.
Range of motion (ROM) should be assessed carefully to determine which
(if any) positions reproduce the patient’s pain. Pain with active ROM
or at extremes of motion is indicative of loosening, whereas pain with
passive ROM may indicate occult infection. Pain with passive straight
leg raising should raise suspicion of sciatic nerve irritation. Pain or
apprehension in certain reproducible positions, particularly at
extremes of motion, is indicative of instability or impingement. Pain
with resisted hip flexion and passive extension often is associated
with iliopsoas tendonitis.
painful THA begins with a critical review of serial plain radiographs
that are of high enough quality to identify subtle changes and to
evaluate for signs of loosening or migration of the prosthesis. Care
should be taken to note differences in radiographic technique,
including orientation, penetration, and rotation.
loosening of cemented femoral stems have been proposed by Harris and
McGann. This classification includes criteria for definite, probable
and possible loosening (Table 14-2). Major
signs of osseointegration of a cementless femoral component were
identified by Engh et al. and include the absence of reactive,
radiodense lines around the porous-coated portion of the implant and
presence of endosteal spot-welds. Minor signs of osseointegration
include calcar atrophy, a stable distal stem, and the absence of a
pedestal. Major signs of failure of osseointegration are extensive
reactive lines around the porous-surfaced portion of the implant,
whereas the absence of endosteal spot-welds is considered a minor sign
of failed osseointegration.
a cemented acetabular component has been divided into definite
loosening (migration of >5 mm or a fracture of the cement mantle),
probable loosening (100% radiolucent line at the bone/cement interface)
and possible loosening (radiolucent line of 50% to 99% at the
bone/cement interface). Criteria for loosening of a cementless
acetabular component include migration (of >5 mm), the presence of
broken screws (if present), and a complete radiolucent line around the
component. Udomkiat et al. reported radiolucent lines that progressed
after 2 years postoperatively, radiolucent lines of ≥1 mm in thickness
that appeared after the second postoperative year, and a radiolucent
line of >2 mm in any zone were particularly useful predictors of
cementless acetabular component loosening.
|
TABLE 14-2 Definitions of Radiographic Loosening of Cemented Femoral Stems
|
||
|---|---|---|
|
the evaluation of infection, certain radiographic findings are highly
indicative of infection including periosteal new bone formation and
endosteal scalloping. Component loosening that occurs within the first
5 years in an otherwise well-performed THA is particularly suggestive
of infection.
guidance, to diagnose infection should be performed on a selective
basis as this test has been associated with a high rate of
false-positives and is time consuming, expensive, and uncomfortable for
the patient. It is typically recommended when the clinical suspicion
for infection is high (based on the history or presence of risk
factors), when the erythrocyte sedimentation rate (ESR) and/or
C-reactive protein (CRP) are elevated, or when failure occurs <5
years postoperatively. When fluid is obtained, specimens should be sent
for aerobic, anaerobic, acid-fast bacilli and fungal cultures as well
as a cell count with differential. The precise cutoff for identifying
infection with a cell count is controversial; however, the use of
>50,000 white blood cells (WBC) as would be applicable to a native
hip is associated with a high rate of false-negatives. At our own
centers, >3,000 WBC has been found to be highly suggestive of
infection, and similar values have been identified for evaluating
infection at the site of a total knee arthroplasty; we typically use
cell counts intraoperatively as an adjunct to or instead of an
intraoperative frozen section as a screening tool for infection.
Similarly, the cutoff value for the differential is somewhat unclear,
with different authors suggesting values of between 65% and 90%
neutrophils. In contrast to an aspiration for
identifying
infection, aspiration arthrography of the hip to delineate component
loosening has been found to have a low sensitivity and specificity,
especially for uncemented implants, and has been abandoned at most
centers.
the origin of pain in a patient with a painful THA and provide
information as to whether the source of pain is intracapsular or
extracapsular. Braunstein et al. reported that 10 of 11 patients with
an identifiable intracapsular cause for pain obtained complete relief
of pain within 20 minutes of an intraarticular bupivacaine injection.
If a patient does not experience relief of symptoms after
intra-articular injection, extra-articular sources of pain should be
sought. Similarly, if a patient is suspected of having pain derived
from the lumbosacral spine, relief from a local anesthetic injection at
this site can assist in ruling out pain arising from a THA.
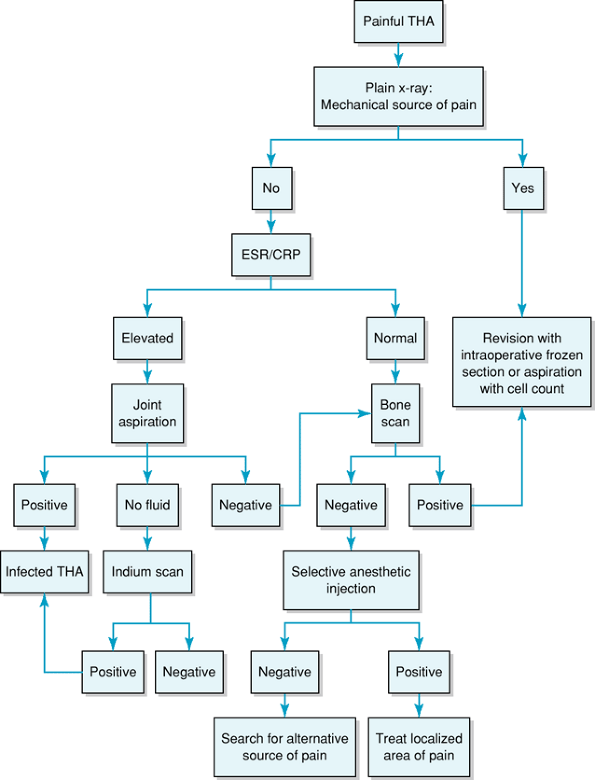
evaluating the patient with a painful THA in whom the history, physical
examination, and plain radiographic studies are unclear and revision
surgery is not otherwise indicated (Fig. 14-2).
Although a highly sensitive indicator of bone turnover and activity,
this technique has a low specificity and the results are generally not
considered accurate within 2 years of prosthetic implantation.
Increased uptake on 99Tc MDP can be seen with various
conditions, including loosening, infection, heterotopic bone formation,
stress fractures, modulus mismatch, tumors, metabolic bone disease, and
reflex sympathetic dystrophy. Lieberman et al., in a series of 54 hips
that subsequently were revised, reported that bone scans were not more
helpful than serial radiographs in determining component stability; the
authors recommended a bone scan only if plain radiographic studies are
inconclusive.
 |
|
Figure 14-2 Three-phase bone scan showing diffuse uptake around the femoral component indicative of loosening.
|
is taken up by leukocytes, has been used in combination with technetium
bone scans to differentiate between septic and aseptic loosening. Both
sensitivity and accuracy have been reported as poor, however, and this
testing modality has been abandoned in most centers.
identify deep infection also has yielded disappointing results that
have been reported to be only slightly better than with gallium citrate
scans. Scher et al. studied 143 hips and knees that had a reoperation
for a painful or loose total joint arthroplasty or a prior resection
arthroplasty. The positive predictive value only was 54%; however, the
negative predictive value was 95%, suggesting that a negative scan is
useful in predicting the absence of infection in a patient who is being
evaluated for a painful total joint arthroplasty. The addition of
technetium-99m–labeled sulfur colloid marrow scanning has been used at
some centers in an attempt to decrease the high rate of false-positive
indium scans secondary to physiologic marrow packing that can cause an
accumulation, slowing, or retardation of flow of (indium-labeled)
leukocytes around a prosthesis. The method provides some improvements;
however, sensitivity has remained low and thus all of these tests are
used only as a second line of investigation when the results of other
testing modalities are unclear.
adjunct, when used selectively, for evaluating the painful THA.
Specific software packages are required to compensate for artifact
generated by metallic prosthesis, and a preprocedure direct
consultation with a radiologist is recommended to optimize the result.
Its greatest utility seems to be in identifying and quantifying
periprosthetic osteolysis and for evaluating component positioning that
may be contributing to instability; it can also be useful for
identifying iliopsoas tendonitis (Fig. 14-3).
 |
|
Figure 14-3 CT scan of the pelvis showing enlarged iliopsoas tendon (arrows).
|
useful tool for evaluating the painful THA; however, the input of a
radiologist is imperative to ensure that appropriate pulse sequences
and software are used to decrease metallic artifact. MRI has been found
to be useful in evaluating the soft tissues to identify iliopsoas
tendonitis, incompetence of the hip capsule, and damage to the abductor
musculature; for identifying and quantitating osteolysis; and for
evaluating the adjacent neurovascular structures; it has also been
suggested as a potential way to evaluate for infection and component
loosening or fracture.
 |
|
Figure 14-4 Algorithm for evaluation of the painful total hip arthroplasty. ESR/CRP, erythrocyte sedimentation rate/C-reactive protein.
|
protein (CRP) should be obtained from any patient being evaluated for a
painful THA. If these values are elevated, deep periprosthetic
infection must be suspected and additional evaluation with preoperative
or intraoperative testing (e.g., intraoperative frozen section or
intraoperative cell count) should be done. In one series of 202
revision THAs, all patients with a deep infection had an elevated ESR
(>30 mm/hour) or CRP (>1 mg/dL). In this series, the combination
of a normal ESR and CRP reliably predicted the absence of infection
(100% specificity). It is important to
recognize,
however, that the ESR and CRP are nonspecific markers of inflammation
and may be elevated by chronic inflammatory conditions (such as
rheumatoid arthritis), recent surgical intervention, or systemic
illness. The ESR, although usually normal by 6 months postoperatively,
may be elevated for as much as 1 year after uncomplicated THA.
complex task that requires diligence and patience on the part of the
surgeon and the patient (Fig. 14-4). After a
thorough history and physical examination, a focused and careful
radiographic and laboratory workup can be done at a reasonable cost and
with a high degree of accuracy.
painful THA, a clear diagnosis of the condition that is responsible for
the patient’s symptoms must be sought prior to further operative
intervention as the risks of revision THA can be substantial; also,
repeat surgery without a clear diagnosis of a condition that can be
remedied by surgical intervention may be met with a high rate of
persistent pain and an unsatisfied patient. Patients must be clearly
counseled on the cause of their problem, the treatment options, and the
risks of operative intervention. Nonoperative measures and observation
are the mainstays of treatment until a definitive and treatable
diagnosis can be confirmed.
who is a reasonable risk medically for elective operative intervention
include chronic infection and loose implants. Patients with a diagnosis
of infection should be revised to prevent both worsening of infection
and the associated bone loss that can ensue if treated nonoperatively.
Similarly, patients with loose implants may sustain periprosthetic bone
loss if the problem is neglected, which in turn can lead to greater
operative complexity, a higher risk of complications and a poorer
clinical result when revision surgery finally is performed. Further
details regarding revision of surgical technique, results, and
postoperative management are covered in Chapter 15.
RB, Rorabeck CH, Ghazal ME, et al. Pain in the thigh following total
hip replacement with a porous-coated anatomic prosthesis for
osteoarthrosis. J Bone Joint Surg. 1994;76A:1464–1470.
WH, McGann WA. Loosening of the femoral component after use of the
medullary-plug cementing technique. Follow-up note with a minimum of
five-year follow-up. J Bone Joint Surgery. 1986;68A:1064–1066.
D, Harris WH. Failed total hip replacement: Assessment by plain
radiographs, arthrograms, and aspiration of the hip joint. J Bone Joint Surg. 1984;66A:540–546.
HG, Nestor BJ, Sofka CM, Ho, et al. Magnetic resonance imaging after
total hip arthroplasty: evaluation of periprosthetic soft tissue. J Bone Joint Surg. 2004;86A:1947–1954.
DM, Pak K, Lonner JL, et al. The predictive value of indium-111
leukocyte scans in the diagnosis of infected total hip, knee, or
resection arthroplasties. J Arthroplasty. 2000;15:295–300.
MJ, Masri BA, O’Connell JX, et al. Prospective analysis of preoperative
and intraoperative investigations for the diagnosis of infection at the
sites of two hundred and two revision total hip arthroplasties. J Bone Joint Surg. 1999;81A:672–683.
P, Wan Z, Dorr LD. Comparison of preoperative radiographs and
intraoperative findings of fixation of hemispheric porous-coated
sockets. J Bone Joint Surg. 2001;83:1865–1875.
